Abstract
Background
Peer support telephone calls have been used for a wide range of health‐related concerns. However, little is known about their effects.
Objectives
To assess the effects of peer support telephone calls in terms of physical (e.g. blood pressure), psychological (e.g. depressive symptoms), and behavioural health outcomes (e.g. uptake of mammography) and other outcomes.
Search methods
We searched: The Cochrane Library databases (CENTRAL, DARE, CDSR) (issue 4 2007); MEDLINE (OVID) (January 1966 to December 2007); EMBASE (OVID) (January 1985 to December 2007); CINAHL (Athens) (January 1966 to December 2007), trials registers and reference lists of articles, with no language restrictions.
Selection criteria
Randomised controlled trials of peer support interventions delivered by telephone call.
Data collection and analysis
Two review authors independently extracted data. We present results narratively and in tabular format. Meta‐analysis was not possible due to heterogeneity between studies.
Main results
We included seven studies involving 2492 participants.
Peer support telephone calls were associated with an increase in mammography screening, with 49% of women in the intervention group and 34% of women in the control group receiving a mammogram since the start of the intervention (P </ = 0.001). In another study, peer telephone support calls were found to maintain mammography screening uptake for baseline adherent women (P = 0.029).
Peer support telephone calls for post myocardial infarction patients were associated at six months with a change in diet in the intervention and usual care groups of 54% and 44% respectively (P = 0.03). In another study for post myocardial infarction patients there were no significant differences between groups for self‐efficacy, health status and mental health outcomes.
Peer support telephone calls were associated with greater continuation of breastfeeding in mothers at 3 months post partum (P = 0.01).
Peer support telephone calls were associated with reduced depressive symptoms in mothers with postnatal depression (Edinburgh Postnatal Depression Scale (EPDS) > 12). The peer support intervention significantly decreased depressive symptomatology at the 4‐week assessment (odds ratio (OR) 6.23 (95% confidence interval (CI) 1.15 to 33.77; P = 0.02)) and 8‐week assessment (OR 6.23 (95% CI 1.40 to 27.84; P = 0.01).
One study investigated the use of peer support for patients with poorly controlled diabetes. There were no significant differences between groups for self‐efficacy, HbA1C, cholesterol level and body mass index.
Authors' conclusions
Whilst this review provides some evidence that peer support telephone calls can be effective for certain health‐related concerns, few of the studies were of high quality and so results should be interpreted cautiously. There were many methodological limitations thus limiting the generalisability of findings. Overall, there is a need for further well designed randomised controlled studies to clarify the cost and clinical effectiveness of peer support telephone calls for improvement in health and health‐related behaviour.
Plain language summary
Peer support telephone calls to improve health and health behaviours
Telephone peer support is widely available through helplines but its impact on health outcomes and health‐related behaviours is largely unknown. We examined the effects of peer support telephone calls on physical and psychological health and on health behaviours. Seven randomised controlled trials conducted in the USA, UK, Canada and Australia related to a range of conditions and target populations. They provided some evidence of efficacy. Peer support telephone calls may increase mammography screening in women over 40 years, may help patients change their diet and cease smoking after a heart attack; and may help reduce depressive symptoms among mothers with postnatal depression. Findings need to be interpreted cautiously. There is a need for well designed randomised controlled studies to clarify which elements of peer telephone interventions work best to improve health and health‐related behaviour.
Background
Health professionals alone are unable to address all of the healthcare needs of patients (DoH 2001; Stewart 1995). There is increasing interest in developing peer‐led and 'expert patient' type interventions, particularly to support the needs of individuals living with chronic conditions (Barlow 2005; Bodenheimer 2003; Lorig 1998). Peer interventions have been applied to disease‐related, illness‐prevention and health promotion topics (Andersen 2000; Dennis 2002b). A range of approaches such as individual one‐to‐one sessions, self‐help/support groups, online computer‐mediated groups, and telephone contact have been used. Such interventions are intended to meet the support and informational needs of patients, as well as to relieve the pressure on mainstream health services (Stewart 1995). This self‐help movement includes peer/lay individuals "with experiential knowledge who extend natural (embedded) social networks and complement professional health services" (Dennis 2003a).
Definitions
Broad interpretations of the term 'peer support' are used, however the Oxford Dictionary defines support as "carrying all or part of weight of, keep from falling or sinking; provide for; strengthen, encourage, give help or corroboration to; be actively interested in" (Thompson 1996). The most comprehensive definition of peer support describes a peer as a created source of support, internal to a community, who shares salient target population similarities (e.g. age, ethnicity, health concern or stressor) and possesses specific knowledge that is concrete, pragmatic and derived from personal experience rather than formal training. Peer support has also been defined as "the giving of assistance and encouragement by an individual considered equal" (Dennis 2003a). This means that peer support is a complex phenomenon and its application is likely to be highly variable according to the needs and characteristics of the target population. Within a healthcare context, peer support is "the provision of emotional, appraisal and informational assistance by a created social network member who possesses experiential knowledge of a specific behaviour or stressor and similar characteristics as the target population" (Dennis 2003a). Dennis defines emotional, appraisal and informational support as follows:
Emotional support includes expressions of care, encouragement, attentive listening, reflection, reassurance and usually the absence of criticism.
Appraisal support involves the "communication of information that is pertinent to self‐evaluation and encompasses expressions that affirm the appropriateness of emotions, cognitions and behaviours. Specific mechanisms include motivational aspects such as encouragement to persist in problem resolution, reassurance that efforts will result in positive outcomes."
Informational support is the "provision of knowledge relevant to problem‐solving".
Dennis 2003a also believes that peer support occurs primarily without the provision of practical help. In practice, there is considerable variation in the training and preparation in peer support services. Dennis considers that training should be kept to a minimum to ensure the preservation of 'peerness' and to avoid professionalism and the subsequent creation of 'para‐professionals' (i.e. the loss of 'peerness') (Dennis 2003a). The amount of training that leads to para‐professionalism is likely to vary according to the purpose and scope of the intended support and the attributes of the peers that are recruited. We intended to use this review to explore this relationship.
Use of telephone delivered interventions
Alongside the development of peer support, there is increasing interest in telephone support. Such support has the advantage of greater accessibility and potential availability than face‐to‐face contact. The telephone is increasingly used in health care and there are studies on the effects of interventions delivered by telephone for a wide range of health conditions (Monnier 2003; McBride 1999). A Cochrane review showed that telecommunication appeared to have been well accepted by patients (Currell 2000). The increase in the use of telephone‐delivered interventions also reflects the emphasis on containing the costs of healthcare (Fries 1993).
Peer telephone interventions are used in a variety of service designs and for a variety of health conditions or health promotion topics. There is extensive use of telephone‐based support in the voluntary sector through telephone helplines, such as those offering mother‐to‐mother support for breastfeeding or for women experiencing postnatal depression. However, there is little robust evaluation of their effects (Mishara 2007; Sood 2008). Awareness of the benefits derived by peer supporters themselves is growing, particularly in the context of long‐term health conditions. There is evidence that offering support to other people can be beneficial for the helper, as well as the person being helped, and that volunteering can result in:
improved physical health (Moen 1989; Schwartz 1999b);
increased feelings of self‐worth (Barlow 2001; Luks 1998; Mowbray 1996; Omoto 2000);
reduced depressive symptoms (Hainsworth 2001; Luks 1998);
improved communication skills (Mowbray 1996); and
changes in self‐management behaviours (Barlow 2005).
Apart from the use of telephone call interventions in health care, the telephone is increasingly used in health care to support the provision of information and advice in ways that do not involve verbal interaction (Suggs 2006). For example, there is increasing use of internet/email based interventions and peer support (Adler 2002; Hilty 2006), for example in cancer survivors (Meier 2007). However, privacy and confidentiality are key issues in email interactions (Constantino 2007). In addition, there may be a lack of immediacy of response compared to active verbal interaction over the phone.
Relation to existing reviews
Four Cochrane reviews overlap with this systematic review of peer support telephone calls for improving health. Doull 2003 will examine peer support strategies for people with a chronic illness. In this review we included those interventions provided by telephone also assessed by Doull, but we included people with all types of health problems, not just those with chronic conditions. Stead 2006 examined telephone counselling for smoking cessation and included peers and non‐peers; the former were also included in this review. Lewin's review of lay health workers (Lewin 2005) may overlap with this review for studies where being a peer was a prerequisite to becoming a lay health worker. However, the definition of the 'lay health worker' role differs from that of a peer supporter in that a lay health worker does not necessarily have characteristics similar to the people they are helping, and unlike Lewin's review this review covers all settings, not just primary and community care. Britton 1999 examined the effectiveness of support for breastfeeding mothers and included different modes of support (face‐to‐face and/or telephone) and different care providers (midwives, counsellors, volunteers with breastfeeding experience). Britton's review overlaps with the current review for studies where support was provided solely by peers over the telephone.
Two other non‐Cochrane reviews may have included studies of relevance to our review: one looked at social support in diabetes (van Dam 2005) and the other looked at peer support for cancer patients (Tilkeridis 2005). Both focused on single conditions, whereas the scope of this review was broader.
Aims of current review
The aim of this review was to assess the evidence for peer support telephone‐delivered interventions involving verbal communication and aiming to improve health and health behaviours. The review's objectives included determining the health areas in which the interventions have been most successful, and the types of intervention found to be most effective. From this analysis, we aimed to derive a classification of peer support telephone interventions, and identify the factors associated with an intervention's effectiveness. We also considered whether, and to what extent, the studies had involved peer training, the duration of any support provided to peer supporters and the tensions between these issues and the potential for para‐professionalism.
Objectives
To assess the effects of peer support telephone calls for improving the health and quality of life of individuals as well as their carers, on outcomes including physical, psychological, behavioural and other health outcomes.
To determine the health areas in which peer support telephone calls have been most successful.
To identify the factors associated with success in improving health, and the types of intervention found to be most successful, and to use this to develop a classification of peer support telephone calls.
To explore the relationship between training and the development of para‐professionalism among peer supporters.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs), which:
compared peer support telephone calls with other types of intervention and/or with usual care; or
compared different models (e.g. different levels of training) of peer support telephone calls with each other and/or with usual care.
Types of participants
We included people living with acute or long‐term illness, carers of people with acute or long‐term illness, parents, people with psychological symptoms, and people requiring screening or who had any other health and well‐being related concerns.
Types of interventions
We included peer support telephone calls (of any duration) based on verbal communication, in which the peer is someone selected to provide support because they have similar or relevant health experience.
Given the heterogeneity of the trials and the purposes for which peer support telephone calls are provided, we anticipated that the duration of interventions and the frequency of calls included in the review would be highly variable. We planned that where duration and frequency could be compared this would be assessed in a sensitivity analysis.
Exclusions
We excluded studies if:
data on the peer telephone element could not be extracted;
they were not RCTs;
the peer component was not delivered by telephone;
peers were not used for intervention delivery; or
the intervention was facilitated by non‐peers (i.e. intervention was a group design with teleconference calls facilitated by healthcare professional/s).
Types of outcome measures
We included data related to the following types of outcome measure (whether validated or by self report):
physical health outcomes (e.g. blood pressure)
psychological health outcomes (e.g. satisfaction, anxiety, depression, quality of life, self‐efficacy (i.e. ability to manage health‐related problems)
behavioural health outcomes (e.g. duration of maintaining breastfeeding, health‐seeking behaviour, change of diet)
social outcomes (e.g. health service use, repeat attendance to primary care, cost).
impact on the peer supporter (e.g. satisfaction, anxiety).
We included data on adverse effects associated with the intervention, both for the peer supporter and the receiver of support.
Search methods for identification of studies
Electronic searches
We searched:
The Cochrane Library databases (CENTRAL, DARE, CDSR) (Issue 4 2007);
MEDLINE (OVID) (January 1966 to December 2007);
EMBASE (OVID) (January 1985 to December 2007);
CINAHL (Athens) (January 1966 to December 2007)
The strategy for MEDLINE (OVID) is presented as an example at Appendix 1. We tailored the MEDLINE strategy to the other databases.
Searching other resources
We searched the reference lists of included studies, and contacted experts in the field to identify further studies. We also searched trial registers for recent studies (Clinical Trials.gov, Current Controlled Trials, Trials Central, National Research Register, Australian Clinical Trials Register, International Clinical Trials Registry Platform) and grey literature for unpublished work.
There were no language restrictions. We searched all databases in December 2007 from their start date.
Data collection and analysis
Selection of studies
Two review authors independently assessed the potential relevance of all titles and abstracts identified from the searches. We retrieved in full text those studies identified by either author as potentially relevant. Each of these studies was assessed independently for inclusion, against the review selection criteria, by two review authors.
We excluded studies according to the selection criteria (see Types of interventions). In case of disagreement between authors, the decision was referred to a third review author. If agreement was still not reached, the entire review team was involved to resolve the decision by consensus.
Studies that appeared eligible for inclusion but were subsequently judged to not meet the selection criteria were detailed in the table Characteristics of excluded studies including the specific reason(s) for exclusion (e.g. type of intervention not meeting the criteria for peer support or telephone support).
Data extraction and management
Two review authors independently extracted data from included studies. The data extraction forms were based on the Cochrane Consumers and Communication Review Group's Data Extraction Template for Cochrane Reviews. The forms were checked against each other, and where discrepancies occurred we referred to the original paper. When discrepancies remained unresolved after referring to the original paper, agreement was achieved through discussion and by consensus, involving the entire review team where necessary. We contacted study authors to obtain missing data. If there was no response to the initial letter to study authors, we sent a second letter.
In order to describe the elements of the intervention used in each study, for each we extracted data and reported:
aim of intervention;
trial authors' definition of peer support;
description of the participants and peer supporters;
geographic location;
setting;
details of intervention, including theoretical basis (with key references);
details of service provider relevant to the delivery of the intervention, including the recruitment and training of peers;
number of participants (including those lost to follow‐up) and peer supporters in each group;
for both participants and peer supporters, age, gender, ethnicity, principal health problem, other health problems, stage of problem/illness, treatment received/receiving, other social/demographic details (e.g. literacy or reading level);
the number and frequency of calls, call duration, times of day;
whether there was a structured protocol for the call/s;
whether the call was made by a peer, or two‐way, or by a peer support group via teleconference call;
what quality assurance processes were utilised, including whether the call was recorded;
the number/percentage of training sessions attended by participants;
details of control group/usual or routine care;
details of any co‐interventions in all groups;
delivery of intervention (e.g. stages, timing, frequency, duration).
For each study, we extracted the following data on outcome measures:
principal and secondary outcome measures;
method of data collection used to assess each outcome measure (e.g. phone survey, questionnaire, physical measurements);
timing of outcome assessment (including frequency, length of follow up (for each outcome));
adverse events (e.g. complaints, levels of dissatisfaction, adverse incidents);
the impact of the intervention on tthe peers themselves.
We extracted the results of each study in terms of outcome measures, mean (standard deviation (SD))/percentages, and P values.
Assessment of risk of bias of included studies
We assessed and reported on the risk of bias of included studies in accordance with the guidelines of the Cochrane Consumers and Communication Review Group and the Cochrane Handbook (Higgins 2008) which recommended the explicit reporting of the following individual quality elements for RCTs: sequence generation (including the method used); allocation concealment (including the method used); blinding (participants, providers, outcome assessors, data analysts); completeness of outcome data; selective reporting. We incorporated the results of the assessment into the review through systematic narrative description and commentary about each of the these domains, leading to an overall assessment of the risk of bias of included studies and a judgement about the internal validity of the review's results.
Investigation of heterogeneity
We explored qualitatively the degree of heterogeneity between the included studies in terms of: type of condition, type of peer, type of patient, and context of study population, and identified the extent to which each of these parameters overlapped between the studies. We intended to conduct an assessment of the degree of heterogeneity using the I2 statistic except where there was clearly a high degree of heterogeneity in terms of type of interventions, participants, study designs and outcome measures (Higgins 2003).
We present the results of included studies narratively and in tabular form. We presented the results according to the outcome categorisation identified at protocol stage, as well as by health need/condition, and within that, by the attributes of the intervention. This was used to inform the development of a classification of peer support telephone calls. The classification of peer support telephone calls was developed by conducting a content analysis of interventions to identify themes and classify component elements.
We intended that where there was sufficient overlap between two or more studies to designate them as a subgroup, we would conduct a meta‐analysis. Where deemed feasible, we planned to pool the results in RevMan using a random‐effects model with standardised mean differences (SMDs) for continuous data and odd ratios (OR) for dichotomous data.
Sensitivity analyses
We had intended that, if feasible, we would undertake sensitivity analyses where several studies related to the same health‐related need or condition. For such studies, we planned to categorise the extent of training, the duration of the intervention and the theoretical frameworks underpinning them, establish the median and range for each parameter, and from this classify interventions according to whether they incorporated, for example, a greater or lesser degree of training, duration of contact etc. These data were intended to be used in a sensitivity analysis.
Consumer involvement
We contacted INVOLVE for feedback on the review. INVOLVE is a national advisory group, involving members of the public, and funded through the National Institute for Health Research, UK (www.invo.org.uk/). Its role is to support and promote active public involvement in NHS, public health as well as social care research. We also invited comments from the Telephone Helpline Association (THA), an organisation that provides specialist information on setting up and running helplines in the UK and Ireland, offers advice, consultancy and training on issues relating to the provision of quality helpline services for the voluntary and statutory sectors. Representatives from the THA and INVOLVE commented on the protocol and the final draft of the review. Consumers were also involved in the standard peer review processes of the Cochrane Consumers and Communication Review Group, providing feedback at protocol and review stages.
Results
Description of studies
Results of the search
By electronic and manual searching (to 31 December 2007) we identified 61 studies that were potentially eligible for inclusion. After assessing the full text of studies against the Criteria for considering studies for this review, we excluded 54 studies.
Included studies
We included seven randomised controlled trials (RCTs) (Calle 1994; Carroll 2006; Dale 2007; Dennis 2002aDennis 2003b; Duan 2000; Heller 1995). Six studies were published in English language journals and one was submitted for publication in an English language journal.
The included studies had high heterogeneity in terms of their setting, the health‐related concerns/topics that were the focus of the interventions, the content of the interventions and the outcomes measured. Five studies compared a peer telephone intervention against a control arm receiving usual care or no intervention (Calle 1994; Dennis 2002a; Dennis 2003b; Duan 2000; Heller 1995). Two studies had an additional third arm with professional telephone support (Dale 2007;Carroll 2006).
Contact with authors
We attempted to contact authors of all the included studies for information on any data missing from the published reports, with one reminder after a few weeks. We obtained two replies with additional data provided (Carroll 2006; Dale 2007), and in two other replies authors stated that the study was performed too long ago to supply the information requested (Calle 1994; Heller 1995).
Sample sizes
Sample sizes ranged from 42 to 813 people, with a total of 2492 people recruited in the seven studies.
Setting
Three studies were conducted in the USA (Duan 2000; Calle 1994; Carroll 2006), two in Canada (Dennis 2002a; Dennis 2003b), one in Australia (Heller 1995) and one in the UK (Dale 2007).
Participants
People participating in the included studies were as follows:
people over 65 years old who had suffered a myocardial infarction (Carroll 2006);
people with type 2 diabetes with glycated haemoglobin over 7.4% (Dale 2007);
primiparous, breastfeeding women over 16 years old who had a singleton birth at 37 weeks' gestation or later (Dennis 2002a);
new mothers over 18 years old who had a singleton birth at 37 weeks' gestation or later and scored > 9 on the Edinburgh Postnatal Depression Scale (Dennis 2003b);
women aged over 40 years and therefore eligible for mammography screening (Calle 1994; Duan 2000);
people aged 25 to 74 years with a diagnosis of myocardial infarction or angina (Heller 1995).
Interventions
In all seven studies the intervention was delivered by telephone to participants in their homes. We present a summary of intervention characteristics in the table Characteristics of included studies. Interventions were aimed at:
improving depressive symptoms in women at high risk for post‐partum depression (Dennis 2003b);
increasing self‐efficacy and improving diet in patients recovering from a myocardial infarction (Carroll 2006; Heller 1995);
encouraging breastfeeding in new mothers (Dennis 2002a);
increasing mammography usage in women aged over 40 years (Duan 2000; Calle 1994); and
increasing self‐efficacy in people with Type 2 diabetes (Dale 2007).
Peers
The number of peers contributing to the intervention varied between studies: there were 80 in Calle 1994, 58 in Dennis 2002a, 19 in Dennis 2003b, 9 in Dale 2007, and 8 in Carroll 2006. The total number of peers providing the intervention was unclear in two studies (Duan 2000; Heller 1995). No study justified the number of peers recruited in relation to the number of participants.
The included studies described a wide variety of methods for recruiting peer advisors. In Calle 1994 peer advisors were recruited from two local American Cancer Society (ACS) units through volunteer coordinators, primarily by a word‐of‐mouth campaign encouraging peer advisors to participate and recruit further volunteers among their acquaintances and organizations. In Dennis 2002a and Dennis 2003b peers were mothers with experience of breastfeeding and post‐partum depression respectively. They were recruited using flyers, advertisements in the local newspapers and word‐of‐mouth. In Dale 2007 peer advisors were lay people with diabetes who were recruited via a local user group and an email support group.
In Heller 1995 peer advisors were recruited from members of the Australian Cardiacs Association, a group whose members have themselves suffered from heart disease. Carroll 2006 recruited peer advisors from those who had successfully completed a local cardiac rehabilitation program. In Duan 2000, part‐time peer supporters were recruited from participating churches.
Theoretical basis
The theoretical basis informing the design of the intervention was unclear in three studies (Dennis 2002a; Dennis 2003b; Heller 1995). The other four studies used different models of health behaviour to inform the peer support intervention. In Calle 1994 the theoretical basis was research that showed success with personal intervention strategies in increasing mammography usage. Carroll 2006 used the self‐efficacy model of health behaviour (Bandura 1977) to design a peer telephone intervention to aid rehabilitation after a myocardial infarction. In Dale 2007 the intervention was based on a theoretical background to successful behaviour change as described by Anderson 2000 and Rollnick 2002, and practical counselling skills to enhance personal decision making (Egan 1998). In Duan 2000 the intervention was based on the Health Belief Model which advocates increasing awareness of vulnerability as well as cues to action (Rosenstock 1966).
Peer training
Six of the seven studies reported that they provided some form of peer training (Calle 1994; Carroll 2006; Dennis 2002a; Dennis 2003b; Dale 2007; Duan 2000) (see table Characteristics of included studies). Three studies provided additional support material consisting of fact sheets, resources guides, and handbooks (Calle 1994; Dale 2007; Dennis 2003b). Three studies provided follow‐up support in the form of monthly meetings (Dennis 2002a), or supervision (Duan 2000) or both (Dale 2007). The format for training varied considerably and included: part‐day sessions (Calle 1994, Dennis 2003b); and multiple‐day sessions (Dale 2007; Dennis 2002a).
Number of calls/duration/timing
Five of the seven studies reported the number of calls made by peers. It ranged from 1 call in 6 months to up to 12 calls over 12 weeks. In Carroll 2006, peers provided 1 call per week for 12 weeks for patients after a myocardial infarction. In Duan 2000 peers made a call once a year for two years to improve uptake of mammography screening. In another study to increase the use of mammography screening, peers called their five intervention participants up to three times during a six month period (Calle 1994). In the study on postnatal depression (Dennis 2003b) peers were asked to contact the mother within 48 hours and as frequently thereafter as the individual mother deemed necessary (mean 5.4, SD 3.5). In the study to increase self‐efficacy in people with Type 2 diabetes, participants received one to six calls over a six‐month period, with frequency of calls negotiated between peer volunteer and participant (Dale 2007). In the remaining two studies the number of calls and how often they were made was unclear (Dennis 2002a; Heller 1995).
Recording and documentation of calls
Five studies documented the telephone calls in some way. Two studies did not (Duan 2000; Heller 1995). Dale 2007 was the only study that reported recording telephone calls. This was for quality assurance and content analysis. In three studies the intervention was documented using tracking sheets to record interactions with trial participants (Calle 1994; Dennis 2002a; Dennis 2003b). In Carroll 2006, peer advisors used advisor logs, a focus group and telephone interviews with peer advisors to provide information on the peer advisor experience.
Classification of peer support telephone calls
Analysis of the content of interventions in all studies revealed intervention elements consistent with the definition of peer support outlined by Dennis 2003a. The interventions were categorised in terms of their emotional, appraisal and informational content according to the aspects of peer support described as having been provided to participants. As shown in Figure 1, interventions varied from those that were categorised as either comprising a single type of support including informational support (Calle 1994; Duan 2000; Heller 1995) or emotional support (Carroll 2006); two types of support that is emotional and appraisal support (Dale 2007); or a combination of all three types of support (Dennis 2002a; Dennis 2003b).
1.
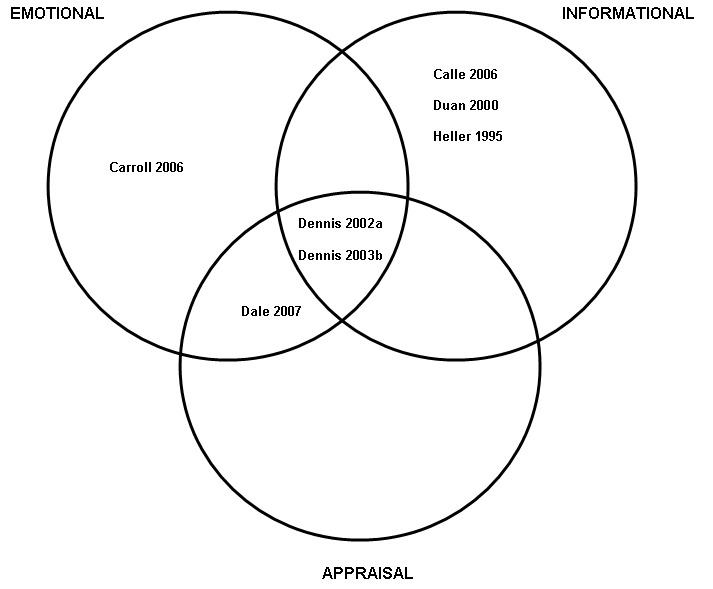
Content analysis of the interventions of the RCTs included in this review, highlighting the different aspects of peer support
Emotional support only
In Carroll 2006 the main type of support provided was emotional, with each peer advisor's training based on the premise that the strength of the intervention was the peer advisor's ability to identify with the people they were helping. The peer advisor in this study was encouraged to share personal experiences with subjects during telephone contact but was warned to avoid sharing clinical information or health advice.
Informational support only
Heller 1995 described the main type of support from peers as a low level of advice. Duan 2000 and Calle 1994 attributed the peer role as giving mainly informational support which included advice about the need for screening, risk status and cancer prevalence rates.
Emotional and appraisal support
In Dale 2007 the main types of support provided by peers were emotional and appraisal support. All peer advisors attended a training programme that focused on empowerment, motivational interviewing and active listening skills. The intended role of the peer advisor was to reinforce advice already provided by the patient's health professional at the time of a change in the patient's diabetes management, including medication and/or lifestyle changes.
Emotional, informational and appraisal support
In Dennis 2002a peer supporters were provided with a handbook that outlined professional services available for referral and incorporated topics such as volunteer role description, breastfeeding benefits, tips for effective telephone support, general breastfeeding information and principles, fact sheets and breastfeeding myths.
In Dennis 2003b the intervention aimed to improve depressive symptoms in women at high risk of post‐partum depression. Peer advisors were provided with training materials that covered various topics including a definition of peer support, potential benefits, how to develop a relationship, skills and techniques for effective telephone support, general post‐partum depression information and the helping process.
Excluded studies
In the table Characteristics of excluded studies, we list the 54 studies we excluded after assessment of the full text (according to the criteria specified at Types of interventions) and specify the reasons for exclusion.
Risk of bias in included studies
Assessments of study quality are shown in the tables Characteristics of included studies and in the risk of bias tables. The overall quality of the included studies was fairly poor.
Summary of the risk of bias tables
Adequate sequence generation: Fulfilled in four studies (Carroll 2006; Dale 2007; Dennis 2002a; Dennis 2003b). The others were unclear.
Allocation concealment: Fulfilled in three studies (Dale 2007;Dennis 2002a; Dennis 2003b). The others were unclear.
Blinding (Participants): Not blinded in two studies (Carroll 2007; Dale 2007). The others were unclear.
Blinding (Providers): Not blinded in two studies (Carroll 2006; Dale 2007). The others were unclear.
Blinding (Outcome assessors): Fulfilled in four studies (Calle 1994; Dale 2007; Dennis 2002a; Dennis 2003b); not fulfilled in one study (Carroll 2006). The others were unclear.
Blinding (Data analysts): Fulfilled in three studies (Dale 2007; Dennis 2002a; Dennis 2003b); not fulfilled in one study (Carroll 2006). The others were unclear.
Incomplete outcome data assessed: Fulfilled in four studies (Carroll 2006; Dale 2007; Dennis 2002a; Dennis 2003b) not fulfilled in one study (Calle 1994). The others were unclear.
Free of selective reporting: Fulfilled in all studies.
See also the risk of bias summary for all included studies at Figure 2.
2.
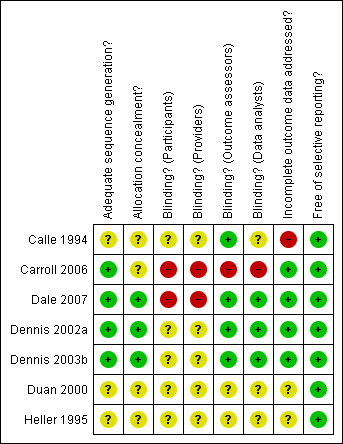
Risk of bias summary: review authors' judgements about each methodological quality item for each included study, as reported in the risk of bias table for each study.
Effects of interventions
The overall heterogeneity of outcomes prevented us from conducting a meta‐analysis for any of the outcomes. We present the results first organised in terms of the outcomes listed at Types of outcome measures, and second organised in terms of the intervention aim.
The main results from all studies are presented in additional tables. Table 1 is a summary of the results and the findings from each individual study are presented in tables 2 to 9 (Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9).
1. Summary of results.
| Author Date | Results summary |
| Calle 1994 | For women in the intervention group, 49% had received their most recent mammogram within 6 months of the start of the trial compared to 34% of the women in the control group (p = 0.0005); a 40% relative increase in mammography uptake (RR 1.4 (95% CI 1.2 to 1.7)). |
| Carroll 2006 | At 12 weeks post‐myocardial infarction there were no significant differences for self‐efficacy (Jenkins Self Efficacy Scale), recovery behaviours (Duke Activity Status Index), or health status (Medical Outcomes Survey (SF‐36)). |
| Dale 2007 | At the 6 month assessment there were no significant differences for self‐efficacy (Diabetes Self‐Efficacy Scale) or clinical outcomes (glycated haemoglobin, cholesterol, and Body Mass Index) between intervention and control group patients |
| Dennis 2002a | Significantly more mothers in the peer support group than in the control group continued to breastfeed exclusively at 3 months post partum (56.8% versus 40.3%, P = 0.01). Breastfeeding rates at 4, 8 and 12 weeks post partum were 92.4%, 84.8% and 81.1% respectively among mothers in the peer support group as compared with 83.9%, 75.0% and 66.9% among those in the control group (P </ = 0.05 for all time periods). Fewer mothers in the peer support group than in the control group expressed dissatisfaction with breastfeeding (1.5% versus 10.5%; P = 0.02). |
| Dennis 2003b | Significant group differences were found for probable major depressive symptomatology (Edinburgh Postnatal Depression Scale (EPDS)) at the 4 week (P = 0.02) and 8 week (P = 0.01) follow‐up assessments. At the 4 week assessment 40.9% (n = 9) of mothers in the control group scored >12 on the EPDS compared with only 10% (n = 2) in the experimental group. At the 8 week assessment 52.4% (n = 11) of the mothers in the control group scored > 12 on the EPDS compared with 15% (n = 3) of mothers in the experimental group. |
| Duan 2000 | At one year follow‐up, 7.5% more participants in the peer telephone support group showed a continuation in the uptake of mammography screening than the control group (P = 0.029). |
| Heller 1995 | At six months follow‐up, there was no significant difference in cigarette smoking rates, but 54% of participants in the intervention group and 44% respectively of those in the control group reported having changed their diet (P = 0.03). There were no significant differences for quality of life. |
2. Findings from Calle 1994.
| Outcome | Timing | Intervention group | Control group | P | ||
| Observed (n) | Total (N) | Observed (n) | Total (N) | |||
| Most recent mammogram in study period | 8 months after start of study | 141 | 289 | 104 | 305 | P = 0.0005 |
3. Findings from Carroll 2006.
| Outcome | Timing of outcome assessments |
Intervention group Peer telephone |
Intervention group Nurse calls |
Control group | P | |||
| Mean/ Mean change | SD | Mean/ Mean change | SD | Mean/ Mean change | SD | |||
| Self‐efficacy | Baseline | 5.5 | 2.2 | 6.5 | 6.2 | 5.6 | 2.4 | NS |
| 12 weeks | 7.0/1.5 | 2.0/2.5 | 7.1/1.1 | 2.0/2.3 | 6.8/1.2 | 2.3/2.2 | ||
| Recovery behaviours (DASI) |
Baseline | 15.6 | 6.5 | 17.2 | 9.9 | 17.3 | 8.2 | NS |
| 12 weeks | 18.8/3.2 | 6.6/8.9 | 19.8/1.1 | 7.3/2.3 | 19.5/2.2 | 8.1/10.7 | ||
| MOS SF‐36 physical health | Baseline | 54 | 19 | 59 | 26 | 59 | 21 | NS |
| 12 weeks | 58/3.6 | 21/16 | 67/4.5 | 21/19 | 61/2.8 | 20/20 | ||
| MOS SF‐36 mental health | Baseline | 67 | 23 | 62 | 21 | 66 | 22 | NS |
| 12 weeks | 72/5.2 | 20/18 | 74/11.8 | 20/19 | 68/1.9 | 19/31 | ||
4. Findings from Dale 2007.
| Outcome | Group | Baseline | 6 months | Difference | P | |||||
| N | Mean | SD | N | Mean | SD | N | Mean (95% CI) | |||
| Self‐efficacy (DMSES) | Peer support | 80 | 108 | 30.4 | 73 | 116.3 | 25.7 | 67 | 7.3 (2.6 to ‐12.1) | NS |
| Diabetes Specialist nurse | 37 | 109.9 | 21.5 | 33 | 109.4 | 27.4 | 29 | 3.8 (‐5.2 to 12.9) | ||
| Control | 84 | 106.4 | 30.8 | 77 | 111.3 | 30.7 | 72 | 3.1 (‐4.1, 10.3) | ||
| Diabetes distress (PAID) | Peer support | 85 | 14.6 | 12.7 | 75 | 13.3 | 14.1 | 72 | ‐1.7 (‐4.1 to ‐0.7) | NS |
| Diabetes Specialist nurse | 39 | 22.7 | 18.8 | 33 | 17.5 | 15 | 30 | ‐5.1 (‐9.2 to ‐1.0) | ||
| Control | 85 | 19.8 | 15.5 | 77 | 13.0 | 14.7 | 72 | ‐4.5 (‐7.4 to ‐1.6) | ||
| Glycated haemoglobin (HbA1C) | Peer support | 90 | 8.4 | 1.1 | 78 | 8.0 | 1.5 | 78 | ‐0.4 (‐0.8 to ‐0.1) | NS |
| Diabetes Specialist nurse | 44 | 8.9 | 1.5 | 37 | 7.9 | 0.9 | 37 | ‐0.9 (‐1.6 to ‐0.3) | ||
| Control | 97 | 8.7 | 1.3 | 86 | 7.9 | 1.1 | 86 | ‐0.8 (‐1.0 to ‐0.5) | ||
| Cholesterol | Peer support | 88 | 4.7 | 1.1 | 67 | 4.5 | 0.8 | 67 | ‐0.3 (‐0.5 to ‐0.1) | NS |
| Diabetes Specialist nurse | 44 | 4.7 | 1 | 35 | 4.5 | 0.8 | 35 | ‐0.2 (‐0.5 to 0.1) | ||
| Control | 97 | 4.6 | 1 | 78 | 4.4 | 1 | 78 | ‐0.3 (‐0.5 to ‐0.1) | ||
| Body Mass Index | Peer support | 88 | 32.4 | 5.9 | 78 | 32.8 | 5.8 | 77 | ‐0.2 (‐0.5 to 0.1) | NS |
| Diabetes Specialist nurse | 44 | 33.0 | 7.4 | 36 | 33.3 | 8.3 | 36 | ‐0.2 (‐0.8 to 0.4) | ||
| Control | 96 | 31.9 | 6.3 | 85 | 32.6 | 7.5 | 84 | 0.5 (‐0.3 to 1.4) | ||
5. Findings from Dennis 2002a.
| Outcome | Timing of outcome assessments | Intervention group | Control group | Relative risk (and 95% CI) | P | ||
| Observed (n) | Total (N) | Observed (n) | Total (N) | ||||
| Mothers breastfeeding | 4 weeks | 122 | 132 | 104 | 124 | 1.10 (1.01 to 2.72) | P = 0.03 |
| 8 weeks | 112 | 132 | 93 | 124 | 1.13 (1.00 to 1.28) | P = 0.05 | |
| 12 weeks | 107 | 132 | 83 | 124 | 1.21 (1.04 to 1.41) | P = 0.01 | |
6. Findings from Dennis 2003b.
| Outcome | Timing of outcome assessment | Intervention group | Control group | 95% CI | p | ||
| Observed (n) | Total (N) | Observed (n) | Total (N) | ||||
| EPDS >9 | 4 weeks | 9 | 20 | 16 | 22 | 0.9 to 11.81 | P = 0.06 |
| 8 weeks | 7 | 20 | 16 | 22 | 1.52 to 23.18 | P = 0.008 | |
| EPDS > 12 | 4 weeks | 2 | 20 | 9 | 22 | 1.15 to 33.77 | P = 0.02 |
| 8 weeks | 3 | 20 | 11 | 22 | 1.40 to 27.84 | P = 0.01 | |
7. Findings from Dennis 2003b.
| Outcome | Time | Experimental group (n = 20) Mean (SD) | Control group (n = 22) Mean (SD) | Mean difference | P |
| Maternal self esteem | Baseline | 28.25 (4.19) | 27.8 (3.92) | 0.43 | NS |
| 8 weeks | 30.00 (4.21) | 28.57 (3.83)a | 1.43 | NS | |
| Child care stress | Baseline | 7.10 (3.24) | 7.40 (3.44) | 0.30 | NS |
| 8 weeks | 4.95 (2.68) | 6.48 (3.63)a | 1.53 | NS | |
| Maternal loneliness | Baseline | 24.75 (4.88) | 25.18 (5.50) | 0.43 | NS |
| 8 weeks | 20.37 (5.23) | 23.91 (6.07)a | 3.54 | NS | |
| a n = 21 | |||||
8. Findings from Duan 2000.
| Outcome | Control No. | Peer support No. | Control % |
Peer support % | Difference % | P | relative reduction Nonadherence c |
| Maintenance mammography screening a | 258 | 264 | 23.3 | 15.8 | 7.5 | 0.029 | 32 |
| Conversion of nonadherent to adherent b | 139 | 152 | 37.4 | 34.8 | 2.6 | 0.324 | 7 |
|
a Proportion of participants who were attending mammograms at baseline and continued to do so. b Conversion of participants who were not receiving mammograms at baseline to uptake of mammography screening. c Relative to year 1 nonadherence rate under control condition. | |||||||
9. Findings from Heller 1995.
| Quality of Life factor | Intervention group | Usual care group | P |
| Emotional | |||
| Baseline | 5.20 (0.09) | 5.31 (0.10) | 0.44 |
| Six weeks | 5.07 (0.11) | 4.98 (0.11) | 0.54 |
| Six weeks change from baseline | ‐0.13 (0.09) | ‐0.33 (0.10) | 0.14 |
| 95% CI for change | (‐0.31 to 0.05) | (‐0.53 to ‐0.13) | |
| Baseline | 5.34 (0.09) | 5.34 (0.10) | 0.99 |
| Six months | 5.32 (0.12) | 5.22 (0.11) | 0.55 |
| Six months change from baseline | ‐0.02 (0.11) | ‐0.12 (0.11) | 0.54 |
| 95% CI for change | (‐0.24 to 0.20) | (‐0.34 to 0.10) | |
| Physical | |||
| Six weeks | 5.02 (0.10) | 4.97 (0.10) | 0.72 |
| Six months | 5.35 (0.11) | 5.29 (0.11) | 0.67 |
| Social | |||
| Six weeks | 5.45 (0.09) | 5.31 (0.09) | 0.28 |
| Six months | 5.72 (0.10) | 5.65 (0.10) | 0.62 |
Adverse effects
We included data on adverse effects associated with the intervention, both for the peer supporter and the receiver of support.
Key findings, by types of outcome
Physical health outcomes
Three of the seven studies investigated physical health outcomes, either as clinical outcomes (Dale 2007) or as assessments of physical health status (Carroll 2006; Heller 1995). Carroll 2006 investigated differences between a peer support group, advanced practice nurse group and a control group. Dale 2007 investigated differences between a peer support group, a specialist diabetes nurse and a control group. Heller 1995 investigated differences between a peer support group and a control group.
Dale 2007 compared cholesterol levels, body mass index, glycated haemoglobin levels and diabetes distress among people with Type 2 diabetes at six months. Carroll 2006 used the Medical Outcome Survey SF‐36 to report physical health status at 12 weeks and Heller 1995 used a non‐validated self‐report questionnaire for Quality of Life (Physical) at six weeks and six months.
No studies found any difference between intervention and control groups over time.
Psychological health outcomes
Psychological health outcomes were measured in terms of: self‐efficacy in two studies (Carroll 2006; Dale 2007); mental health status in two studies (Carroll 2006; Dennis 2003b), quality of life (emotional) in one study (Heller 1995); and satisfaction with infant feeding in one study (Dennis 2002a).
Peer support telephone interventions were associated with reduced postnatal depression (Dennis 2003b) and increased satisfaction with infant feeding (Dennis 2002a). No differences were found with other psychological outcomes.
Self‐efficacy
Two studies measured self‐efficacy, using different validated self‐report scales. Carroll 2006 used the Jenkins Self‐Efficacy Scale and Dale 2007 used the Diabetes Management Self‐Efficacy Scale. No differences were found between intervention and control groups.
Mental health status
Five validated self‐report tools were used to assess mental health status in two studies (Carroll 2006; Dennis 2003b). Carroll 2006 measured mental health status using the SF‐36. Dennis 2003b measured postnatal depression using the EPDS; Maternal self‐esteem using the Rosenberg Self‐Esteem Scale; Child Care Stress using the Child Care Stress Checklist (reported as validated but unpublished) and Maternal loneliness using the short version of the UCLA Loneliness Scale.
Postnatal depression scores were lower among the intervention group participants at four and eight weeks, using two different cut‐off points (> 9 and >12) for the Edinburgh Postnatal Depression Scale (EPDS) (Dennis 2003b). Peer support telephone calls significantly reduced depressive symptom scores compared with usual care. Significant group differences were found in probable major depressive symptomatology (EPDS > 12 (score range 0 to 30)). A score greater than 12 indicates that the person is likely to suffer from postnatal depression. The peer support intervention significantly decreased depressive symptomatology at the 4 week assessment (OR 6.23 (95% CI 1.15 to 33.77; P = 0.02)) and 8 week assessment (OR 6.23 (95% CI 1.40 to 27.84; P = 0.01).
No other difference in mental health status was found between intervention and control groups (Carroll 2006; Dennis 2003b).
Quality of life
Quality of life (emotional) was measured in one study using a self‐report questionnaire validated for post‐myocardial infarction (Heller 1995). The study found no difference between intervention and control groups.
Satisfaction
One study measured the impact of peer support telephone calls on maternal satisfaction with the method of infant feeding, using an unvalidated self‐report questionnaire (Dennis 2002a). Women who received peer support telephone interventions were more satisfied with their method of infant feeding compared with those who did not receive the calls. Fewer mothers in the peer support group than in the control group expressed dissatisfaction (1.5% versus 10.5%; P = 0.02) (Dennis 2002a).
Dale 2007 reported on the satisfaction of participants in a study investigating the efficacy of peer telephone support calls for people with Type 2 diabetes. In all, 77% (53/69) of respondents in the peer support group compared to 94% (29/31) of respondents in the diabetes nurse group stated at study completion that they would recommend the telephone support to other patients (P = 0.04).Therefore more participants in the diabetes specialist nurse group were positive about the intervention experience than the participants in the peer support group.
Behavioural health outcomes
Five studies measured behavioural health outcomes. Dennis 2002a assessed the duration of breastfeeding. Carroll 2006 assessed recovery behaviours after myocardial infarction. Two studies measured three aspects of mammography screening: Calle 1994 compared the rate of recent mammographies; while Duan 2000 investigated maintenance of mammography screening among women who had previously undergone this type of screening and the rate of conversion to mammography screening among women who had not previously been screened. Heller 1995 investigated rates of smoking and change in diet by people after myocardial infarction.
As described in detail below, peer support telephone interventions were associated with prolonging health behaviours among populations who had already taken up such behaviour, such as breastfeeding and regular mammography screening. Peer support telephone calls were associated with a change in diet for people who had suffered a myocardial infarction (Heller 1995). In another study peer support telephone calls did not affect health behaviours for people who had suffered a myocardial infarction (Carroll 2006).
Duration of exclusive breastfeeding
In the study by Dennis 2002a based on self report using an unvalidated instrument, there were significantly more mothers in the peer support group than in the control group that continued to breastfeed exclusively at 12 weeks post partum (relative risk (RR) 1.21 (95% CI 1.04 to 1.41; P = 0.01)). Breastfeeding rates were also higher in the intervention group compared with the control group at 4 weeks (RR 1.10 (95% CI 1.01 to 2.72; P = 0.03)) and 8 weeks post partum (RR 1.13 (95% CI 1.00 to 1.28; P = 0.05)).
Behaviours after myocardial infarction
There were no significant differences between groups for performance in recovery behaviours as measured by the Duke Activity Status Index (DASI) at 12 weeks (Carroll 2006).
In Heller 1995 there were no significant differences for smoking rates at six months. At six months in the intervention and usual care groups based on self report, 54% and 44% respectively reported having changed their diet (P = 0.03) (Heller 1995).
Mammography screening
Two studies used telephone peer support calls to increase the uptake of mammography screening (Calle 1994; Duan 2000). Both studies showed an increased rate in the uptake of mammography screening among some population groups. All results were based on self report.
The intervention was associated with higher maintenance of mammography screening at one year (23.3% versus 15.8%; P = 0.029) in Duan 2000. However, among women who had previously had mammograms the effect on uptake was small and statistically insignificant (Duan 2000). In Calle 1994 49% of women in the intervention group received their most recent mammogram since the start of the trial period compared with 34% of women in the control group over the same time period (RR 1.4, 95% CI 1.2 to 1.7; P</=0.001).
Social outcomes
Increase in health service use through mammography screening reported above could also be seen as having a social impact.
Heller 1995 included the number of investigations and interventions performed on participants in the self‐report questionnaire assessing the outcome of the intervention. The authors also added three 'social' items to their Quality of Life scale.There were no differences between groups at six weeks and six months follow‐up. No other included studies assessed outcomes categorised as social outcomes.
Impact on peer supporters
Three studies (Carroll 2006; Dale 2007; Dennis 2002a) provided qualitative data reporting on the peers' experience.
Key findings, by aim of intervention
The key findings from each of the studies included in this review are described below in terms of aims of the intervention.
Peer telephone interventions to improve uptake of mammography screening
Two studies used telephone peer support calls to increase the uptake of mammography screening. Both provided informational support only and both assessed the impact of peer telephone support using health behaviour outcomes related to the uptake of mammography screening. Both studies showed improved rates of mammography uptake for some populations. Despite these similarities the studies could not be combined because of heterogeneity in terms of rates of telephone calls and times of follow‐up. In Duan 2000 the intervention was one session of telephone support conducted annually for two years. In Calle 1994 peer advisors made calls to women already known to them, up to three times in a six month period.
Peer telephone interventions for people with ischaemic heart disease
Two studies investigated the efficacy of peer support telephone calls for people after suffering a myocardial infarction. One provided emotional support (Carroll 2006) and the other provided informational support (Heller 1995). Both studies reported physical health outcomes, psychological health outcomes and behavioural health outcomes but none were common to both studies. Carroll 2006 investigated the efficacy of two interventions (one call per week for 12 weeks from a peer advisor and one call per week for 12 weeks from an Advanced Practice Nurse). Heller 1995 investigated the efficacy of peer support from a member of the Australian Cardiac Association (whose members had themselves suffered from heart disease). The intervention was most often a single call from the peer advisor. One study showed no significant differences between groups (Carroll 2006) and the other showed a significant improvement in diet in the intervention group (Heller 1995).
Peer telephone interventions for new mothers
Two studies looked at the impact of peer support telephone calls for new mothers. Both studies provided emotional, informational and appraisal support. Dennis 2002a investigated the efficacy of peer telephone support on the duration of breastfeeding, where the intervention was a call within 48 hours after hospital discharge and as frequently thereafter as the mother deemed necessary. Rates of exclusive breastfeeding were determined using self report questionnaires developed for the study. Breast feeding continuation rates were significantly improved in the intervention group. Fewer mothers in the peer support group than the control group expressed dissatisfaction. In a qualitative paper it was reported that mothers found that their peer volunteers were available when difficulties were experienced, increased their confidence, decreased their concerns and assisted them reaching their breastfeeding goals (Dennis 2002b). Also 85% of mothers (n = 111) in the intervention group stated that, if offered, they would choose to have a peer volunteer again.
Dennis 2003b investigated the efficacy of peer telephone calls on post‐partum depression, the intervention was a call within 48 to 72 hours of randomisation and as frequently thereafter as the mother deemed necessary. The primary outcome measure was depressive symptomatology determined using the EPDS. Telephone peer support significantly reduced depressive scores compared with usual care. In a post hoc analysis the frequency and occurrence of peer‐volunteer interactions were not correlated with EPDS scores at the eight week assessment, suggesting that there was not a simple 'dose effect' between the amount of the intervention received and its benefit.
Peer telephone intervention for people with Type 2 diabetes
In Dale 2007, investigating the efficacy of peer support telephone calls for people with Type 2 diabetes, the intervention was a call 3 to 5 days after recruitment and as frequently thereafter as the participant deemed necessary with the provision of emotional and appraisal support. Outcome measures were objective clinical measures and validated questionnaires. No significant differences were found between groups.
The experience of being a peer telephone supporter, including adverse effects
No studies reported quantitative data on the experience of being a telephone supporter. Three studies provided qualitative data reporting on the peers' experience of providing support (Carroll 2006; Dale 2007; Dennis 2002a). In all three studies, the peers provided emotional support. Three key themes emerged:
peer supporters needed to feel that they were of help to the recipient,
peer supporters valued the sharing of experience, and
peer supporters sometimes felt confronted by their own anxieties and vulnerability.
There were also responses to the issue of supervision.
In relation to the first theme, linked to Carroll 2006, a qualitative paper by Whittemore 2000 reported that peer advisors identified helping as the most significant aspect of their role. Helping was described as: giving advice and assisting with problem solving; being advocates; and alleviating fear. When the helping role was absent, the peer experience became more difficult and less satisfying. Peer advisors tended to limit their emotional involvement when they did not feel that their calls were making a difference or that the person did not really need what the peer advisor had to offer. Dennis 2002b reported similar experiences in relation to the study Dennis 2002a investigating the efficacy of telephone peer support on breastfeeding. Sixty percent (n = 18) of peer volunteers felt 'uncomfortable' at least once. The frequently‐cited situations included when a mother stopping breastfeeding, feeling bothersome, perceived nonreceptiveness, and conflicting values.
The second theme that emerged across studies was that of sharing of experience. In Carroll 2006 peers felt that the common bond of shared experiences was enough to establish rapport with someone they had never met, usually occurring by the second or third call (Whittemore 2000). Mutual sharing was also found to be important in Dale 2007. Peer supporters reported that they themselves appreciated the interchange of ideas and sharing of common experiences when talking with the diabetes patients (Caramlau 2007). Some peer supporters even reported having established 'really budding friendships'. It was also reported that participants who felt their diabetes was well controlled were less likely to set goals but used the telephone calls as an opportunity to have a casual chat rather than a therapeutic interchange. Some described the last call as being quite sad (Caramlau 2007). Peer volunteer difficulty in severing relationships was also reported in the study by Carroll 2006 (Whittemore 2000).
The third theme related to some of the difficulties associated with peers becoming aware of their own hidden feelings and sensitivities. In Carroll 2006 (Whittemore 2000), for example, peers reported problems associated with the intimacy and dynamics of mutual sharing. This not only included difficulties in severing relationships, but also how peers felt when discussions resulted in the recollection of difficult and distressing aspects of their own experience.
In the study by Dennis 2002a supervision was perceived positively by many peer volunteers either in the form of calls "to ensure that program expectations were being met" (37%) or supportive calls "to see how one is doing" (63%). In the study by Dale 2007 it was reported that a few peer volunteers felt that more guidance and feedback would have been helpful, particularly in the early stages of the intervention. The need for constant proactive support and regular calls from the training facilitator was emphasised, despite the fact that they could contact someone at any time. Dale 2007 highlights the need for adequate training, ongoing support and reinforcement as key elements required to ensure peer supporter retention and intervention fidelity. Semi‐structured interviews conducted with peer supporters one year into the intervention revealed concerns related to challenging calls (i.e. participants resistant to changes), and difficulties associated with finding convenient times for the calls/attempts sometimes needed to contact participants.
Relationship between training and development of para‐professionalism among peer supporters
There was insufficient reporting of the exact nature of the training, and content analysis of calls, to explore this relationship.
Discussion
This review identified seven randomised controlled trials (RCTs) that have evaluated the effects of peer support telephone calls on aspects of health and health behaviour. These studies were conducted in the USA, UK, Canada and Australia, and related to a range of conditions and target populations. All calls were initiated by the peer supporter, but for some the time of the subsequent call was negotiated between the peer supporter and the participant. Most studies were small scale and undertaken over comparatively short time periods. Overall, while some studies showed no significant positive impacts, none showed negative impacts of the interventions. However, the studies reviewed provided some evidence of the intervention's effectiveness in: reducing potential depressive symptoms among mothers with postnatal depression; encouraging dietary change in patients after myocardial infarction; attaining greater continuation of breastfeeding in mothers with newborn babies; and prolonging regular mammography screening in women aged over 40 years who had previously been screened
A number of methodological limitations were identified. Few interventions were underpinned by a clear theoretical basis, which is consistent with the findings of the review by van Dam 2005. Details of how peers were recruited, trained and supported were often lacking. The studies involved widely diverse practices in terms of the numbers of calls, ranging from interventions that had one call to others that involved multiple calls. Overall the quality of the studies reviewed was fairly poor in regard to reporting adequate allocation concealment and intention‐to‐treat analysis. The blinding of participants, providers/caregivers, outcome assessors and data analysts was unclear in the majority of studies. Only one study reported tape recording calls for the purpose of content analysis and quality assurance (Dale 2007). Intention‐to‐treat analysis was only performed in two studies and was unclear in the remaining five studies. Outcomes across the studies generally relied heavily on self report, with little corroboration of actual change. Reporting of how many peers dropped out of the respective studies was lacking. In addition, the design of the interventions varied considerably despite common goals, and outcomes were diverse which meant that data could not be pooled statistically. Hence, the findings of this review need to be interpreted cautiously.
Peer support is a complex phenomenon, and poor reporting of the exact nature of the support provided in these studies posed challenges in the interpretation of their elements key to achieving effective peer support. Content analysis of the interventions utilised in these studies confirmed three themes that were consistent with the definition of peer support provided by Dennis 2003a: informational support, appraisal support and emotional support. There was evidence that informational support may be effective in encouraging dietary change in patients post‐myocardial infarction (Heller 1995); and in increasing mammography usage in women aged over 40 years who had previously undergone screening (Calle 1994; Duan 2000).
There was also evidence that a combination of informational, appraisal and emotional support contributed to the intervention's effectiveness when targeting more complex behaviours and conditions, such as encouraging breastfeeding in new mothers (Dennis 2002a); and improving depressive symptoms in women at high risk for post‐partum depression (Dennis 2003b). However, emotional support alone failed to encourage the performance of recovery behaviours in people post‐myocardial infarction (Carroll 2006), and emotional and appraisal support was not effective in increasing self‐efficacy or improving glycaemic control in people with type 2 diabetes (Dale 2007). This suggests that emotional and/or appraisal peer telephone support may need to be combined with informational support to have a beneficial effect on more complex health behavioural changes. In Dale 2007, for example, the intervention was designed to provide motivational support to encourage adherence to advice already offered by the healthcare professionals supporting the management of the patient's diabetes. However, the trial authors noted that there were several patients in the intervention group who commented that they would have liked information as well as support from the peer advisors.
Informational support appears likely to require tailoring to individual and local circumstances, and a peer may be much better placed to achieve this than a lay person. However, studies that compared support provided by peers and lay persons were lacking, and without such evidence it is not possible to quantify the added benefit associated with the 'peer' effect. It seems doubtful that informational support by peers ever occurs in the absence of at least some emotional or appraisal support. The social interaction implicit in all types of peer support may be particularly important, even when the main intent of a peer telephone intervention is the imparting of information. For example, Duan 2000 utilised a church‐based peer telephone support intervention to encourage mammography screening, which was principally intended to provide informational support. However, within the context of a shared spiritual beliefs and practices it is likely that the support involved much more than an objective sharing of information. Similarly, peer support was effective in providing support to mothers to increase the continuation of breastfeeding among new mothers in a semi‐urban setting, in which most (75%) of the mothers were college or university educated (Dennis 2002a). The extent to which this intervention would have been effective in a more socially disadvantaged population is unknown. A shared cultural, educational and socio‐economic background may be important in contributing to the impact of peer support telephone calls. Given the heterogeneity of studies included in the review, it was not possible to undertake sensitivity analyses to explore the impact of the approach taken towards peer recruitment, and the quantity and quality of training offered to peers, on the effectiveness of peer support telephone calls. These aspects are likely to be important, especially for interventions that include appraisal support and emotional support, but none of the studies appeared to have tested different approaches to training and recruitment during either the intervention design or trial phases. This is an aspect that requires more detailed consideration in future research.
In addition, few studies had compared different approaches to telephone support within the same study. No studies compared 'novice' peer supporters and more experienced supporters. While it is possible that with increasing experience, peer supporters may become more effective in their support, conversely increasing experience may lead to a loss in 'peer effect' if this is associated with an increase in para‐professionalism. The studies reviewed did not report the extent of telephone support experience that peers had prior to entering the trials.
We found no evidence related to the cost‐effectiveness of interventions, or their sustainability. There was no reporting of the attrition rates of peers, the caseload that peers find manageable, or about the incentives for continuation in the role as peer supporters (e.g. personal/psychological or financial). All these are likely to influence sustainability of peer support telephone calls, and require further study.
All calls were made by peer supporters to participants, but in some studies the time and date of the next call was negotiated between the peer supporter and the recipient. There is a need for further work on the differences in efficacy of proactive versus reactive telephone support. Helplines are usually client‐led and reactive; in this way the caller is choosing when to call, and is leading the call. The caller's identity is confidential and he or she is free to call as often or as little as needed. This is very different to models in some of the included studies where the peer supporter instigated the call. In the UK, the National Institute for Health and Clinical Excellence recommends a change in the way breastfeeding support is delivered, from a reactive service to a proactive service where all new mothers (particularly those who are least likely to start and continue to breastfeed, such as those who have low educational achievement and those from disadvantaged groups) are called by a peer supporter within 48 hours of returning home from hospital (or 48 hours after a home birth) (NICE 2008). It is also recommended that commissioners and managers of maternity and children's services ensure that peer supporters: attend a recognised, externally accredited training course in breastfeeding peer support; offer new mothers ongoing support according to their individual needs which could be delivered face‐to‐face, via telephone or through local groups; can consult a health professional and are provided with ongoing support; and gain appropriate child protection clearance.
Future research
There is a need for high‐quality research to assess the cost and clinical effectiveness of peer support telephone call interventions. In future research more detailed attention to intervention design appears to be needed. This includes developing theory‐based interventions; testing different recruitment, training and supervision/support strategies; and providing clear, detailed information about the interventions, so that others can learn lessons from such research. The frequency and length of calls, the times of calls, the use of a structured protocol to guide peers, and the workload of peers need to be carefully reported. Such information was lacking in most of the studies we reviewed.
The methodological limitations identified in this review need to be addressed in future studies. This includes the use of adequate methods of randomisation and allocation concealment to prevent selection bias, and clear reporting on the use of blinding to prevent performance and detection bias. There is also a need for clear reporting of how those who drop out of the study (or were excluded post‐randomisation) were treated in the analysis. In addition, assessment of the risk of bias showed that triallists must consider the measurement of possible confounders, such as antidepressant or complementary medicine usage, and, where possible, controlling for these in the data analysis.
Most of the studies identified in this review failed to describe how the integrity of interventions was managed and maintained. In future, greater attention should be given to content analysis (e.g. by audiotaping calls), training and quality assurance. Such exploration may help identify the specific elements of peer support telephone calls most associated with positive outcomes. In contrast, in this review little or no information was reported about how far the peer advisors actually utilised the resource materials and their own experiences when conversing with the participants.
Authors' conclusions
Implications for practice.
This review identified some evidence that peer support telephone calls are effective in changing health outcomes and health behaviours. Although the intervention may be beneficial for a wide range of health‐related concerns and health behaviours, the evidence identified in this review was too limited to recommend any change in current practice.
The review found insufficient information about the training of peers to understand the levels of training or support required to meet the different target needs and populations to produce optimal performance. This is consistent with the findings of Lewin's review of lay health workers in primary and community health care (Lewin 2005). There was also insufficient information about the organisational arrangements associated with providing peer telephone support; the sustainability of interventions; and their cost‐effectiveness. Such evidence is needed before widespread adoption of peer support telephone calls could be recommended.
From the thematic analysis of interventions it was not possible to draw conclusions about the elements of interventions most likely to be effective with particular types of health‐related concerns. However from the studies reviewed here, those that included informational support (with or without appraisal support and emotional support) emerged as being more effective than those that lacked an informational support component. The classification of interventions according to the extent to which they include the three elements of peer support (information support, appraisal support and emotional support) may help with the design of the different dimensions of support in future interventions.
Two studies reported on the experience of support received by the telephone peer volunteers. The issue of providing adequate support to peer volunteers needs to be considered, both in future research and any practice‐related developments.
Implications for research.
Overall further randomised controlled trials are needed in the area of peer support telephone calls to improve health and health behaviour that take into consideration the methodological issues highlighted in this review. These need to be of larger scale, involve more diverse populations, and take place over longer timescales. It is recommended that future trials use validated outcomes where possible. Greater clarity in reporting the telephone elements of the study (including the intervention's content, number of calls, length of calls) is needed to assess their impact. There is also a need for greater quality control to ensure the fidelity of interventions, including the content of peer support telephone calls, documentation and follow‐up. Future triallists should audio record calls and conduct content analysis to discover more about the types of interchanges most effective in improving health and health‐related behaviour. More detailed reporting of the training provided to peer supporters is required. More research into the impact of peer support telephone calls on the peers themselves, and the potential for negative impact on receivers of support such as inappropriate or erroneous advice, is also needed.
What's new
| Date | Event | Description |
|---|---|---|
| 23 March 2009 | Amended | Correction of text formatting problem |
Acknowledgements
We thank the members of the consumer advisory groups for providing very useful feedback on the current review. We also express great thanks to the editors, staff and peer reviewers of the Cochrane Consumers and Communication Review Group for their highly useful comments; particularly our contact editor Dr Dell Horey, the Review Group Coordinator Dr Megan Prictor, Cooordinating Editor Dr Sophie Hill and the Group's former Trials Search Coordinator Ms Shirley Ward.
Appendices
Appendix 1. MEDLINE (Ovid) search strategy
1. Self‐Help Groups/ or Self Help Groups/ or Support Groups/ 2. Social Support/ 3. (Support Groups or Group Support or Groups, Support).mp. [mp = title, original title, abstract, name of substance word, subject heading word] 4. helpline/ or help‐line/ 5. (helpline or help‐line).mp. 6. (Peer support or Peer Group or Peer$).mp. [mp = title, original title, abstract, name of substance word, subject heading word] 7. (peer adj5 (expert$ or worker$ or advisor$ or consultant$ or leader$ or educator$ or tutor$ or instructor$ or facilitator$)).tw. 8. (lay led or lay run).tw. 9. (lay adj5 (expert$ or worker$ or person$ or advisor$ or consultant$ or leader$ or educator$ or tutor$ or instructor$ or facilitator$)).tw. 10. layperson$.tw. 11. ((Voluntary worker$ or voluntary) adj3 worker$).mp. [mp = title, original title, abstract, name of substance word, subject heading word] 12. (volunteer$ adj5 (trained or aide$)).tw. 13. expert patient$.tw. 14. user led.tw. 15. non professional.mp. or non‐professional.tw. [mp = title, original title, abstract, name of substance word, subject heading word] 16. (non medical or non‐medical).tw. 17. mutual aid.tw. 18. Psychosocial care/ 19. (Telephone$ or phone$ or (cellular adj phone$)).mp. [mp = title, original title, abstract, name of substance word, subject heading word] 20. (Telephone intervention$ or Phone intervention$).mp. [mp = title, original title, abstract, name of substance word, subject heading word] 21. or/19‐20 22. randomized controlled trial.pt. 23. controlled clinical trial.pt. 24. randomized controlled trials.sh. 25. random allocation.sh. 26. double blind method.sh. 27. single blind method.sh. 28. or/22‐27 29. animal/s not (human/ and animal/) 30. 28 not 29 31. clinical trial.pt. 32. exp clinical trials/ 33. (clin$ adj25 trial$).ti,ab. 34. ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).ti,ab. 35. placebos.sh. 36. placebo$.ti,ab. 37. random$.ti,ab. 38. research design.sh. 39. or/31‐38 40. 39 not 29 41. 21 and 40
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Calle 1994.
| Methods | Setting: Florida, USA Recruitment: Volunteers from two local American Cancer Society (ACS) units. Recruitment was primarily through a word‐of‐mouth campaign encouraging current volunteers to participate and recruit others among their acquaintances and organisations. Each volunteer was asked to list the names, addresses and phone numbers of 10 women whom she knew and would be willing to contact by telephone over a six‐month period and encourage to have a mammogram. Randomisation: RCT 2 arm. There was no clear definition of peer support, however study met the inclusion criteria of using peers that shared one or several key characteristics of the target population. Peer training: There was a half day training session including presentations on mammography and details of facilities, American Cancer Society Breast Health Guidelines, instructions for intervention, practice sessions, a breast cancer fact sheet and a resource guide for local mammography centres. |
|
| Participants | 594 women aged over 40 years. | |
| Interventions | Intervention: During a six month intervention period volunteers called their five intervention participants up to three times. At initial contact they emphasized the importance of receiving regular mammograms and asked the participant to set a date by which she would schedule an appointment for screening. During subsequent calls, volunteers determined if the appointment had been made and kept. If at the initial contact, the participant said she had had a mammogram within the last year, she was not called again but congratulated and encouraged to continue receiving regular mammograms. Control group: No intervention. Caller: Calls made by peer supporters. |
|
| Outcomes |
Method of assessing outcome measures: phone survey. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear. |
| Allocation concealment? | Unclear risk | B ‐ Unclear. |
| Blinding? Participants | Unclear risk | Unclear. |
| Blinding? Providers | Unclear risk | Unclear. |
| Blinding? Outcome assessors | Low risk | Quote "The interviews were administered during a two week period by an outside contractor unknown to the participants." |
| Blinding? Data analysts | Unclear risk | Unclear. |
| Incomplete outcome data addressed? All outcomes | High risk | The response rate for the post‐intervention interview was 76% for women in the intervention group and 79% in the control group. Total lost to follow‐up 23% (175). |
| Free of selective reporting? | Low risk | Mammography usage was the only outcome measured. |
Carroll 2006.
| Methods | Setting: Boston, San Francisco, USA. Recruitment: Subjects were over age of 65 years, unpartnered (i.e. widowed, divorced, never married and not in a relationship), had a telephone in their home and were able to speak and understand English Randomisation: RCT 3 arm. There was no clear definition of peer support, however study met the inclusion criteria of using peers that shared one or several key characteristics of the target population. Peer training: Training was based on the self‐efficacy model. |
|
| Participants | 132 older adults (over age of 65 years) who had experienced a myocardial infarction. | |
| Interventions | Intervention 1: Peer advisor intervention group. The peer advisor was a 'graduate' of a local cardiac rehabilitation program. The peer advisor was encouraged to share personal experiences and information with subjects during telephone contact but was warned to avoid sharing clinical information or health advice. Subjects assigned to the peer advisor group received a telephone call from the peer advisor once a week for the 12 weeks after discharge from the hospital. Intervention 2: Advanced Practice Nurse (APN) group. The APN provided additional patient information. Subjects assigned to the APN group received a telephone call from the APN once a week for the 12 weeks after discharge from the hospital. Both intervention groups received standard care. Control group: Standard care consisting of discharge instructions provided by the clinical nurse. Discharge instructions included a review of medications, diet, physical activity, symptom management and follow‐up appointments. Caller: Calls made by peer supporters. |
|
| Outcomes |
Method of assessing outcome measures: phone survey |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Table of random numbers. |
| Allocation concealment? | Unclear risk | B ‐ Unclear. |
| Blinding? Participants | High risk | Not done. |
| Blinding? Providers | High risk | Not done. |
| Blinding? Outcome assessors | High risk | Not done. |
| Blinding? Data analysts | High risk | Not done. |
| Incomplete outcome data addressed? All outcomes | Low risk | Intention‐to‐treat analysis. |
| Free of selective reporting? | Low risk | All measures reported. |
Dale 2007.
| Methods | Setting: Midlands, England. Recruitment: Participants recruited through 43 general practices in the West Midlands. Randomisation: RCT 3 arm. This study explicitly drew on the definition of peer support by Dennis as "the provision of emotional, appraisal and informational assistance by a created social network member who possesses experiential knowledge of a specific behaviour or stressor and similar characteristics as the target population" (Dennis 2003a). Peer training: Peer supporters were trained at a two day training event on motivational interviewing and listening skills. |
|
| Participants | 231 patients with a recent glycated haemoglobin greater than 7.4% and who had been advised of the benefit of reducing their glycated haemoglobin with or without a change in prescribed tablet based therapy. | |
| Interventions | Intervention:Diabetes Specialist Nurses and peer telephone supporters attended a 2‐day training programme that focused on empowerment, motivational interviewing and active listening skills. For both intervention arms the first call was made 3 to 5 days after recruitment. Caller: Calls were made by peer supporters but timing was negotiated with the recipient and the number of calls were as often as the participant deemed necessary. Control group: No intervention. Participants were encouraged to follow medical advice given to them by their GP or practice nurse. |
|
| Outcomes |
Method of assessing outcome measures: paper questionnaire and clinical records. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Table of random numbers. |
| Allocation concealment? | Low risk | A ‐ Adequate. |
| Blinding? Participants | High risk | Not done. |
| Blinding? Providers | High risk | Not done. |
| Blinding? Outcome assessors | Low risk | Reported by authors. |
| Blinding? Data analysts | Low risk | Reported by authors. |
| Incomplete outcome data addressed? All outcomes | Low risk | Intention‐to‐treat analysis. |
| Free of selective reporting? | Low risk | All outcomes reported. |
Dennis 2002a.
| Methods | Setting: Toronto, Canada. Recruitment: Participants recruited from 2 semi‐urban community hospitals. Randomisation: RCT 2 arm. This study explicitly drew on the definition of peer support by Dennis as "the provision of emotional, appraisal and informational assistance by a created social network member who possesses experiential knowledge of a specific behaviour or stressor and similar characteristics as the target population" (Dennis 2003a). Peer training: There was a two and a half hour orientation session where the researcher described the study and answered questions. Training was three sessions, each of three hours duration on the prevention and treatment of problems relating to breastfeeding. There were also monthly support meetings. |
|
| Participants | 256 breastfeeding first‐time mothers from 2 semi‐urban community hospitals near Toronto. | |
| Interventions | Intervention: Peer volunteers were asked to contact the new mother within 48 hours after hospital discharge. Frequency of contact was not standardized in order to individualize the intervention to the mother's specific needs and to give credibility to the peer volunteer's experiential knowledge. Caller: Calls were made by peer supporters but timing was negotiated with the recipient and calls were made as often as the mother deemed necessary. Control group: Women allocated to the control group had access to the conventional in‐hospital and community post‐partum support services. |
|
| Outcomes |
Method of assessing outcome measures: phone survey |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: ".....randomly generated numbers constructed by a biostatistician who was not involved in the recruitment process." |
| Allocation concealment? | Low risk | A ‐ Adequate, Quote: "Randomization was achieved using consecutively numbered, sealed opaque envelopes..." |
| Blinding? Participants | Unclear risk | Unclear. |
| Blinding? Providers | Unclear risk | Unclear. |
| Blinding? Outcome assessors | Low risk | Quote: "A research assistant blinded to group allocation telephoned all participants at 4, 8 and 12 weeks post partum to collect data..." |
| Blinding? Data analysts | Low risk | Quote: " Data were entered...by 2 research assistants blinded to group allocation." |
| Incomplete outcome data addressed? All outcomes | Low risk | Quote: "....an 'intention to treat' approach was used to analyse the data." |
| Free of selective reporting? | Low risk | All outcomes reported. |
Dennis 2003b.
| Methods | Setting: British Columbia, Canada. Recruitment: participants recruited from a health region near Vancouver. Randomisation: RCT 2 arm. This study explicitly drew on the definition of peer support by Dennis as "the provision of emotional, appraisal and informational assistance by a created social network member who possesses experiential knowledge of a specific behaviour or stressor and similar characteristics as the target population" (Dennis 2003a). Peer training: There was a 118 page handbook that outlined professional services available for referral, definition of peer support, tips and techniques for phone support and post‐partum depression information to be used as a reference guide provided to peer volunteers. |
|
| Participants | 42 mothers at high risk for post‐partum depression (PPD) according to the Edinburgh Postnatal Depression Scale (EPDS) | |
| Interventions | Intervention group: Peer volunteers (mothers with a history of and recovery from PPD) completed a 4 hour training session. There was also a 118 page handbook that outlined professional services available for referral. Peer volunteers were asked to contact the new mother within 48 to 72 hours of randomization. Caller: Calls were made by peer supporters but timing was negotiated with the recipient and calls were made as often as the participant deemed necessary. Control group: Standard community post‐partum care. |
|
| Outcomes |
Method of assessing outcome measures: phone survey |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "envelopes containing randomly generated numbers. This procedure was constructed by a research assistant who was not involved in the recruitment process." |
| Allocation concealment? | Low risk | A ‐ Adequate. Quote: "Randomisation was achieved by using consecutively numbered, sealed, opaque envelopes.." |
| Blinding? Participants | Unclear risk | Unclear. |
| Blinding? Providers | Unclear risk | Unclear. |
| Blinding? Outcome assessors | Low risk | Quote: "Research assistants blind to group allocation telephoned all participants at 4 weeks post‐randomization to assess depressive symptomology and again at 8 weeks post‐randomization to assess all outcome data." |
| Blinding? Data analysts | Low risk | Quote: "Data were entered into a data management system by a research assistant blind to group allocation." |
| Incomplete outcome data addressed? All outcomes | Low risk | Quote: "an 'intention to treat' approach was used to analyse the data." |
| Free of selective reporting? | Low risk | All outcomes reported. |
Duan 2000.
| Methods | Setting: Los Angeles, USA. Recruitment: 30 churches. Recruitment of women was achieved through announcements during services, meetings and events, special open houses and recruitment events. Randomisation: RCT 2 arm. There was no clear definition of peer support, however study met the inclusion criterion of using peers that shared one or several key characteristics of the target population. Peer training: A survey firm trained and supervised peer volunteers. |
|
| Participants | 813 women aged 40 to 80 years. | |
| Interventions | Intervention: One session of telephone counselling was conducted annually for 2 years by trained peer counsellors. The counselling was individualised to address barriers. Women were informed about their risk status and about breast cancer prevalence rates. They were also encouraged to ask their physicians for a referral and information about convenient screening facilities. Thus both educational and behavioural goals were embedded in the intervention. Caller: Calls were made by peer supporters. Control group: No intervention. |
|
| Outcomes |
Method of assessing outcome measures: phone survey |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear. |
| Allocation concealment? | Unclear risk | B ‐ Unclear. |
| Blinding? Participants | Unclear risk | Unclear. |
| Blinding? Providers | Unclear risk | Unclear. |
| Blinding? Outcome assessors | Unclear risk | Unclear. |
| Blinding? Data analysts | Unclear risk | Unclear. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Intention‐to‐treat analysis ‐ not stated. |
| Free of selective reporting? | Low risk | All outcomes reported. |
Heller 1995.
| Methods | Setting: New South Wales, Australia. Recruitment. Patients were identified whilst in hospital by nurses. Randomisation: RCT 2 arm. There was no clear definition of peer support, however study met the inclusion criteria of using peers that shared one or several key characteristics of the target population. Peer training: No information was provided on peer training. |
|
| Participants | 424 patients aged less than 75 years discharged from hospital with a diagnosis of myocardial infarction or other ischaemic heart disease. | |
| Interventions | Intervention: low level of advice by lay persons from the Australian Cardiac Association (ACA) who had suffered from heart disease ‐ most subjects received only a single telephone call. Caller: Call was made by peer supporters. Control group: Usual care. |
|
| Outcomes |
Method of assessing outcome measures: mailed questionnaire |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Unclear. |
| Allocation concealment? | Unclear risk | B ‐ Unclear. |
| Blinding? Participants | Unclear risk | Unclear. |
| Blinding? Providers | Unclear risk | Unclear. |
| Blinding? Outcome assessors | Unclear risk | Unclear. |
| Blinding? Data analysts | Unclear risk | Unclear. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Intention to treat analysis ‐ not stated. |
| Free of selective reporting? | Low risk | All outcomes reported. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Andersen 2000 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Anderson 2005 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Brindis 2005 | Not an RCT. |
| Bullock 1995 | RCT where there are trained volunteers ‐ no information about whether the volunteers were peers. |
| Carroll 2007 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Caulfield 1998 | Not an RCT. Peer component not by telephone. |
| Chapman 2004 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Emmons 2005 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Gattellari 2005 | RCT where peers are GPs (i.e. healthcare professionals). |
| Goodman 1990a | Not an RCT ‐ a randomised comparative trial. |
| Goodman 1990b | Not an RCT. |
| Gotay 2007 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Heckman 2002 | Not an RCT. Not investigating efficacy of intervention ‐ report on prevalence rates. |
| Heckman 2006a | RCT where intervention facilitated by non‐peers. |
| Heckman 2006b | RCT where intervention facilitated by non‐peers. |
| Heiney 2003 | RCT where intervention led by non‐peers. |
| Heisler 2005 | Not an RCT. |
| Heller 1991 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Hunkeler 2000 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Ireys 1996 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Ireys 2001 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Keyserling 2002 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Krieger 2000 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Lando 1992 | RCT where lay interventionists were used as opposed to ex‐smokers to provide intervention. |
| Mohr 2005 | Not a RCT. |
| Mongeon 1995 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Ossip‐Klein 1991 | Not an RCT. Trial where intervention is conducted by trained 'paraprofessional' counsellors. |
| Ossip‐Klein 1997 | Not an RCT. |
| Park 2006 | Not an RCT. |
| Preyde 2003 | Not an RCT. |
| Pugh 2002 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Rene 1992 | Not an RCT. Trained lay personnel not peers providing the intervention. |
| Ritchie 2000 | Not an RCT. |
| Rudy 2001 | Not an RCT. |
| Samuel‐Hodge 2006 | RCT where intervention led by non‐peers. |
| Schwartz 1999a | Not an RCT. |
| Schwartz 1999b | Not an RCT and investigating impact of peer support on the provider. |
| Silver 1997 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Simoni 2007 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Solomon 2000a | Not an RCT. |
| Solomon 2000b | Not an RCT ‐ a randomised comparative trial. |
| Solomon 2005 | Not an RCT ‐ a randomised comparative trial. |
| Stewart 2001 | Not an RCT. |
| Stockdale 2000 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Sullivan‐Bolyai 2004 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Sutton 2006 | Not an RCT ‐ before and after study. |
| Walker 2002 | Not an RCT. |
| Weinberger 1989 | RCT where intervention is education not peer support. |
| Wewers 2000 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Whittemore 2000 | Qualitative study of peers ‐ not RCT. |
| Wiggins 2005 | RCT where the data relating to the peer support telephone component could not be extracted. |
| Wolke 1994 | Not an RCT. |
| Wong 2007 | RCT where the data relating to the peer support telephone component could not be extracted. |
Contributions of authors
Draft the protocol: Isabela Caramlau (+ Jeremy Dale, Antje Lindenmeyer, Susan Willliams)
Develop a search strategy: Isabela Caramlau, Antje Lindenmeyer
Search for trials: Antje Lindenmeyer, Susan Williams, Isabela Caramlau
Obtain copies of trials: Antje Lindenmeyer
Select which trials to include: Antje Lindenmeyer, Susan Williams + Isabela Caramlau
Extract data from trials: Susan Williams, Antje Lindenmeyer
Enter data into RevMan: Susan Williams, Isabela Caramlau
Carry out the analysis: Susan Williams
Interpret the analysis: Susan Williams, Antje Lindenmeyer, Isabela Caramlau, Jeremy Dale
Draft the final review: Susan Williams (+ Jeremy Dale, Antje Lindenmeyer, Isabela Caramlau)
Update the review: Jeremy Dale
Sources of support
Internal sources
No sources of support supplied
External sources
-
Department of Health Systematic Review Fund, UK.
£5,000
-
Warwick and Coventry Primary Care Research, UK.
(an academic unit funded by the NCCRCD, Department of Health (UK)
Declarations of interest
Jeremy Dale and Isabela Caramlau are authors of the included study Dale 2007. Both are currently undertaking intervention development and piloting of a peer support telephone call intervention for postnatal depression. The data was assessed and extracted by the two other authors (Sue and Antje) to avoid any bias in reporting.
Edited (no change to conclusions)
References
References to studies included in this review
Calle 1994 {published data only (unpublished sought but not used)}
- Calle EE, Miracle‐McMahill HL, Moss RE, Heath CW. Personal contact from friends to increase mammography usage. American Journal of Preventive Medicine 1994;10:361‐6. [PubMed] [Google Scholar]
Carroll 2006 {published and unpublished data}
- Carroll DL, Rankin SH. Comparing interventions in older unpartnered adults after myocardial infarction. European Journal of Cardiovascular Nursing 2006;5:83‐9. [DOI] [PubMed] [Google Scholar]
Dale 2007 {published and unpublished data}
Dennis 2002a {published and unpublished data}
- Dennis, CL, Hodnett E, Gallop R, Chalmers B. The effect of peer support on breast‐feeding duration among primiparous women: a randomized controlled trial. CMAJ 2002;166(1):21‐8. [PMC free article] [PubMed] [Google Scholar]
Dennis 2003b {published data only (unpublished sought but not used)}
- Dennis CL. The effect of peer support on post‐partum depression: a pilot randomised controlled trial. Canadian Journal of Psychiatry 2003;48(2):115‐24. [DOI] [PubMed] [Google Scholar]
Duan 2000 {published data only (unpublished sought but not used)}
- Duan N, Fox SA, Pitkin Derose K, Carson S. Maintaining mammography adherence through telephone counseling in a church‐based trial. American Journal of Public Health 2000;90:1468‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Heller 1995 {published data only (unpublished sought but not used)}
- Heller RF, Lim L, Valenti L, Knapp J. A randomised controlled trial of community based counselling among those discharged from hospital with ischaemic heart disease. Australian and New Zealand Journal of Medicine 1995;25(4):362‐4. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Andersen 2000 {published data only}
- Andersen MR. The effectiveness of mammography promotion by volunteers in rural communities. American Journal of Preventive Medicine 2000;18:199‐207. [DOI] [PubMed] [Google Scholar]
Anderson 2005 {published data only}
- Anderson AK, Damio G, Young S, Chapman DJ, Perez‐Escamilla R. A randomized trial assessing the efficacy of peer counseling on exclusive breast‐feeding in a predominantly Latina low‐income community. Archives of Pediatric and Adolescent Medicine 2005;159:836‐41. [DOI] [PubMed] [Google Scholar]
Brindis 2005 {published data only}
- Brindis CD, Geierstanger SP, Wilcox N, McCarter V, Hubbard A. Evaluation of a peer provider reproductive health service model for adolescents. Perspectives on Sexual and Reproductive Health 2005;37:85‐91. [DOI] [PubMed] [Google Scholar]
Bullock 1995 {published data only}
- Bullock LFC, Wells JE, Duff GB, Hornblow AR. Telephone support for pregnant women: outcome in late pregnancy. New Zealand Medical Journal 1995;108:476‐8. [PubMed] [Google Scholar]
Carroll 2007 {published data only}
- Carroll DL, Rankin SH, Cooper BA. The effects of a collaborative peer advisor/advanced practice nurse intervention: cardiac rehabilitation participation and rehospitalization in older adults after a cardiac event. The Journal of Cardiovascular Nursing 2007;22:313‐19. [DOI] [PubMed] [Google Scholar]
Caulfield 1998 {published data only}
- Caulfield LE, Gross SM, Bentley ME, Bronner Y, Kessler L, Jensen J, et al. WIC‐based interventions to promote breastfeeding among African‐American women in Baltimore: effects on breastfeeding initiation and continuation. Journal of Human Lactation 1998;14:15‐22. [DOI] [PubMed] [Google Scholar]
Chapman 2004 {published data only}
- Chapman DJ, Damio G, Young S, Perez‐Escamilla R. Effectiveness of breastfeeding peer counselling in a low‐income, predominantly Latina population. Archives of Pediatric and Adolescent Medicine 2004;158:897‐902. [DOI] [PubMed] [Google Scholar]
Emmons 2005 {published data only}
- Emmons KM, Puleo E, Park E, Gritz ER, Butterfield RM, Weeks JC, et al. Peer‐delivered smoking counseling for childhood cancer survivors increases rate of cessation: the partnership for health study. Journal of Clinical Oncology 2005;23:6516‐23. [DOI] [PubMed] [Google Scholar]
Gattellari 2005 {published data only}
- Gattellari M, Donnelly N, Taylor N, Meerkin M, Hirst G, Ward JE. Does 'peer coaching' increase GP capacity to promote informed decision making about PSA screening? A cluster randomised trial. Family Practice 2005;22:253‐65. [DOI] [PubMed] [Google Scholar]
Goodman 1990a {published data only}
- Goodman CC, Pynoos J. A model telephone information and support program for caregivers of Alzheimer's patients. The Gerontologist 1990;30:399‐404. [DOI] [PubMed] [Google Scholar]
Goodman 1990b {published data only}
- Goodman C. Evaluation of a model self‐help telephone program: impact on natural networks. Social Work 1990;35:556‐62. [DOI] [PubMed] [Google Scholar]
Gotay 2007 {published data only}
- Gotay CC, Moinpour CM, Unger JM, Jiang CS, Coleman D, Martino S, et al. Impact of a peer‐delivered telephone intervention for women experiencing a breast cancer recurrence. Journal of Clinical Oncology 2007;15:2093‐9. [DOI] [PubMed] [Google Scholar]
Heckman 2002 {published data only}
- Heckman TG, Miller J, Kochman A, Kalichman SC, Carlson B, Silverthorn M. Thoughts of suicide among HIV‐infected rural persons enrolled in a telephone‐delivered mental health intervention. Annals of Behavioural Medicine 2002;24:141‐8. [DOI] [PubMed] [Google Scholar]
Heckman 2006a {published data only}
- Heckman TG, Carlson B. A randomised clinical trial of two telephone‐delivered, mental health interventions for HIV‐infected persons in rural areas of the United States. AIDS and Behaviour 2007;11(1):5‐14. [DOI] [PubMed] [Google Scholar]
Heckman 2006b {published data only}
- Heckman TG, Barcikowski R, Ogles B, Suhr J, Carlson B, Holroyd K, et al. A telephone‐delivered coping improvement group intervention for middle‐aged and older adults living with HIV/AIDS. Annals of Behavioural Medicine 2006;32(1):27‐38. [DOI] [PubMed] [Google Scholar]
Heiney 2003 {published data only}
- Heiney SP, McWayne J, Hurley TG, Lamb LS, Bryant LH, Butler W, et al. Efficacy of therapeutic group by telephone for women with breast cancer. Cancer Nursing 2003;26:439‐47. [DOI] [PubMed] [Google Scholar]
Heisler 2005 {published data only}
- Heisler M, Piette JD. "I help you, and you help me": facilitated telephone peer support among patients with diabetes. The Diabetes Educator 2005;31:869‐79. [DOI] [PubMed] [Google Scholar]
Heller 1991 {published data only}
- Heller K, Thompson MG, Trueba PE, Hogg JR, Vlachos‐Weber I. Peer support telephone dyads for elderly women: was this the wrong intervention?. American Journal of Community Psychology 1991;19:53‐73. [DOI] [PubMed] [Google Scholar]
Hunkeler 2000 {published data only}
- Hunkeler EM, Meresman JF, Hargreaves WA, Fireman B, Berman WH, Kirsch AJ, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Archives of Family Medicine 2000;9:700‐8. [DOI] [PubMed] [Google Scholar]
Ireys 1996 {published data only}
- Ireys HT, Sills EM, Kolodner KB, Walsh BB. A social support intervention for parents of children with juvenile rheumatoid arthritis: results of a randomized trial. Journal of Pediatric Psychology 1996;21:633‐41. [DOI] [PubMed] [Google Scholar]
Ireys 2001 {published data only}
- Ireys H, Chernoff R, Vet KA, Kim Y. Maternal outcomes of a randomized controlled trial of a community‐based support program for families of children with chronic illness. Archives of Pediatric and Adolescent Medicine 2001;155:771‐6. [DOI] [PubMed] [Google Scholar]
Keyserling 2002 {published data only}
- Keyserling TC, Samuel‐Hodge CD, Ammerman AS, Ainsworth BE, Henriquez‐Roldan CF, Elasy TA, et al. A randomized trial of an intervention to improve self‐care behaviours of African‐American women with type 2 diabetes: impact on physical activity. Diabetes Care 2002;25:1576‐83. [DOI] [PubMed] [Google Scholar]
Krieger 2000 {published data only}
- Krieger JW, Castorina JS, Walls ML, Weaver MR Ciske S. Increasing influenza and pneumococcal immunization rates: a randomized controlled study of a senior center‐based intervention. American Journal Of Preventative Medicine 2000;18:123‐31. [DOI] [PubMed] [Google Scholar]
Lando 1992 {published data only}
- Lando HA, Hellerstedt WL, Pirie PL, McGovern PG. Brief supportive telephone outreach as a recruitment and intervention strategy for smoking cessation. American Journal for Public Health 1992;82:41‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mohr 2005 {published data only}
- Mohr DC, Burke H, Beckner V, Merluzzi N. A preliminary report on a skills‐based telephone‐administered peer support programme for patients with multiple sclerosis. Multiple Sclerosis 2005;11:222‐6. [DOI] [PubMed] [Google Scholar]
Mongeon 1995 {published data only}
- Mongeon M. Essai controlé d'un soutien telephonique regulier donne par une benevole sur le deroulement et l'issue de l'allaitement. Revue Canadienne De Santé Publique 1995;86:124‐7. [PubMed] [Google Scholar]
Ossip‐Klein 1991 {published data only}
- Ossip‐Klein DJ, Giovino GA, Megahed N, Black PM, Emont SL, Stiggins J, et al. Effects of a smoker's hotline: results of a 10‐county self‐help trial. Journal of Consulting and Clinical Psychology 1991;59:325‐32. [DOI] [PubMed] [Google Scholar]
Ossip‐Klein 1997 {published data only}
- Ossip‐Klein DJ, Carosella AM, Krusch D. Self‐help interventions for older smokers. Tobacco Control 1997;6:188‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Park 2006 {published data only}
- Park ER, Puleo E, Butterfield RM, Zorn M, Mertens AC, Gritz ER, et al. A process evaluation of a telephone‐based peer‐delivered smoking cessation intervention for adult survivors of childhood cancer: the partnership for health study. Preventive Medicine 2006;42:435‐42. [DOI] [PubMed] [Google Scholar]
Preyde 2003 {published data only}
- Preyde M, Ardal F. Effectiveness of a parent "buddy" program for mothers of very preterm infants in a neonatal intensive care unit. CMAJ 2003;168:969‐73. [PMC free article] [PubMed] [Google Scholar]
Pugh 2002 {published data only}
- Pugh LC, Milligan RA, Frick KD, Spatz D, Bronner Y. Breastfeeding duration, costs and benefits of a support program for low‐income breastfeeding women. Birth 2002;29:95‐100. [DOI] [PubMed] [Google Scholar]
Rene 1992 {published data only}
- Rene J, Weinberger M, Mazzuca SA, Brandt KD, Katz BP. Reduction of joint pain in patients with knee osteoarthritis who have received monthly telephone calls from lay personnel and whose medical treatment regimens have remained stable. Arthritis and Rheumatism 1992;35:511‐5. [DOI] [PubMed] [Google Scholar]
Ritchie 2000 {published data only}
- Ritchie J, Stewart M, Ellerton ML, Thompson D, Meade D, Viscount PW. Parents' perceptions of the impact of a telephone support group intervention. Journal of Family Nursing 2000;6:25‐45. [Google Scholar]
Rudy 2001 {published data only}
- Rudy RR, Rosenfeld LB, Galassi JP, Parker J, Schanberg R. Participants' perceptions of a peer‐helper, telephone‐based social support intervention for melanoma patients. Health Communication 2001;13:285‐305. [DOI] [PubMed] [Google Scholar]
Samuel‐Hodge 2006 {published data only}
- Samuel‐Hodge CD, Keyserling TC, France R, Ingram AF, Johnston LF, Pullen Davis L, et al. A church‐based diabetes self‐management education program for African Americans with type 2 diabetes. Prevention of Chronic Diseases 2006;3:A93. [PMC free article] [PubMed] [Google Scholar]
Schwartz 1999a {published data only}
- Schwartz CE. Teaching coping skills enhances quality of life more than peer support: results of a randomized trial with multiple sclerosis patients. Health Psychology 1999;18:211‐20. [DOI] [PubMed] [Google Scholar]
Schwartz 1999b {published data only}
- Schwartz CE, Sendor RM. Helping others helps oneself: response shift effects in peer support. Social Science and Medicine 1999;48:1563‐75. [DOI] [PubMed] [Google Scholar]
Silver 1997 {published data only}
- Silver E, Ireys HT, Bauman LJ, Stein RE. Psychological outcomes of a support intervention in mothers of children with ongoing health conditions. The parent‐to‐parent network.. Journal of Community Psychology 1997;25:249‐64. [Google Scholar]
Simoni 2007 {published data only}
- Simoni JM, Pantalone DW, Plummer MD, Huang B. A randomized controlled trial of a peer support intervention targeting antiretroviral medication adherence and depressive symptomology in HIV‐positive men and women. Health Psychology 2007;26:488‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Solomon 2000a {published data only}
- Solomon LJ, Secker‐Walker RH, Flynn BS, Skelly JM, Capeless EL. Proactive telephone peer support to help pregnant women stop smoking. Tobacco Control 2000;9:iii72‐iii74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Solomon 2000b {published data only}
- Solomon LJ, Scharoun GM, Flynn BS, Secker‐Walker RH, Sepinwall D. Free nicotine patches plus proactive telephone peer support to help low‐income women stop smoking. Preventive Medicine 2000;31:68‐74. [DOI] [PubMed] [Google Scholar]
Solomon 2005 {published data only}
- Solomon LJ, Flynn BS. Telephone support for pregnant smokers who want to stop smoking. Health Promotion Practice 2005;6:105‐8. [DOI] [PubMed] [Google Scholar]
Stewart 2001 {published data only}
- Stewart MJ, Hart G, Mann K, Jackson S, Langille L, Reidy M. Telephone support group intervention for persons with hemophilia and HIV/AIDS and family caregivers. International Journal of Nursing Studies 2001;38:209‐25. [DOI] [PubMed] [Google Scholar]
Stockdale 2000 {published data only}
- Stockdale SE, Keeler E, Duan N, Pitkin Deerose K, Fox SA. Costs and cost‐effectiveness of a church‐based intervention to promote mammography screening. Health Services Research 2000;35:1037‐57. [PMC free article] [PubMed] [Google Scholar]
Sullivan‐Bolyai 2004 {published data only}
- Sullivan‐Bolyai S, Grey M, Deatrick J, Gruppuso P, Giraitis P, Tamborlane W. Helping other mothers effectively work at raising young children with type 1 diabetes. The Diabetes Educator 2004;30:476‐84. [DOI] [PubMed] [Google Scholar]
Sutton 2006 {published data only}
- Sutton LB, Erlen JA. Effects of mutual dyad support on quality of life in women with breast cancer. Cancer Nursing 2006;29:488‐98. [DOI] [PubMed] [Google Scholar]
Walker 2002 {published data only}
- Walker ML. Telephone based peer support increased duration of breast feeding in primiparous mothers. Evidence Based Nursing 2002;5:75. [DOI] [PubMed] [Google Scholar]
Weinberger 1989 {published data only}
- Weinberger M, Tierney WM, Booher P, Katz BP. Can the provision of information to patients with osteoarthritis improve functional status? A randomised controlled trial. Arthritis and Rheumatism 1989;32:1577‐83. [DOI] [PubMed] [Google Scholar]
Wewers 2000 {published data only}
- Wewers ME, Neidig JL, Kihm KE. The feasibility of a nurse‐managed, peer‐led tobacco cessation intervention. The Journal of the Association of Nurses in AIDS Care 2000;11:37‐44. [DOI] [PubMed] [Google Scholar]
Whittemore 2000 {published data only}
- Whittemore R, Rankin SH, Callahan CD, Leder MC, Carroll Dl. The peer advisor experience providing social support. Qualitative Health Research 2000;10:260‐76. [DOI] [PubMed] [Google Scholar]
Wiggins 2005 {published data only}
- Wiggins M, Oakley A, Roberts I, Turner H, Rajan L, Austerberry H, et al. Postnatal support for mothers living in disadvantaged inner city areas: a randomised controlled trial. Journal of Epidemiology and Community Health 2005;59:288‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wolke 1994 {published data only}
- Wolke D, Gray P, Meyer R. Excessive infant crying: a controlled study of mothers helping mothers. Pediatrics 1994;94(3):322‐32. [PubMed] [Google Scholar]
Wong 2007 {published data only}
- Wong EHY, Nelson EAS, Choi KC, Wong KP, Carmen IP, Lau Cheung HO. Evaluation of a peer counselling programme to sustain breastfeeding practice in Hong Kong. International Breastfeeding Journal 2007;2:12‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Adler 2002
- Adler CI, Zarchin TR. The "virtual focus group": using the Internet to reach pregnant women on home bed rest. Journal of Obstetric Gynecological and Neonatal Nursing 2002;31:418‐27. [DOI] [PubMed] [Google Scholar]
Anderson 2000
- Anderson B, Funnell M. The Art of Empowerment. American Diabetes Association, 2000. [Google Scholar]
Bandura 1977
- Bandura A. Exercise of personal agency through self‐efficacy mechanism. In: Schwarzer R editor(s). Self‐efficacy: the exercise of control. W. H. Freeman Company, 1977. [Google Scholar]
Barlow 2001
- Barlow JH, Hainsworth J. Volunteerism among older people with arthritis. Aging Society 2001;21:203‐17. [Google Scholar]
Barlow 2005
- Barlow JH, Bancroft GV, Turner AP. Volunteer, lay tutors' experiences of the Chronic Disease Self‐Management Course: being valued and adding value. Health Education Research: Theory & Practice 2005;20:128‐36. [DOI] [PubMed] [Google Scholar]
Bodenheimer 2003
- Bodenheimer T. Primary care in the United States: Innovations in primary care in the United States. BMJ 2003;326:796‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Britton 1999
- Britton C, McCormick FM, Renfrew MJ, Wade A, King SE. Support for breastfeeding mothers. Cochrane Database of Systematic Reviews 1999, Issue 1. [DOI: 10.1002/14651858.CD001141.pub3] [DOI] [PubMed] [Google Scholar]
Caramlau 2007
- Caramlau I, Dale J, Walker R, Sturt J. Telecare supporters for people living with diabetes: the benefit of helping others. Submitted.
Constantino 2007
- Constantino R, Crane PA, Noll BS, Doswell WM, Braxter B. Exploring the feasibility of email‐mediated interaction in survivors of abuse. Journal of Psychiatric and Mental Health Nursing 2007;14:291‐301. [DOI] [PubMed] [Google Scholar]
Currell 2000
- Currell R, Urquhart C, Wainwright P, Lewis R. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews 2000, Issue 2. [DOI: 10.1002/14651858.CD002098] [DOI] [PubMed] [Google Scholar]
Dennis 2002b
- Dennis CL. Breastfeeding peer support: maternal and volunteer perceptions from a randomized controlled trial. Birth 2002;29:169‐76. [DOI] [PubMed] [Google Scholar]
Dennis 2003a
- Dennis CL. Peer support within a health care context: a concept analysis. International Journal of Nursing Studies 2003;40:321‐32. [DOI] [PubMed] [Google Scholar]
DoH 2001
- Department of Health. The Expert Patient: A new approach to chronic disease management for the 21st Century. Department of Health 2001.
Doull 2003
- Doull M, O'Connor AM, Robinson V, Tugwell P, Wells GA. Peer support strategies for improving the health and well‐being of individuals with chronic diseases. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD005352] [DOI] [Google Scholar]
Egan 1998
- Egan G. The skilled helper: a systematic approach to effective helping. CA: Brooks/Cole: Pacific Grove, 1998. [Google Scholar]
Fries 1993
- Fries JF, Koop CE, Beadle CE, Cooper PP, England JM, Greaves RF, et al. Reducing health care costs by reducing the need and demand for medical services. The New England Journal of Medicine 1993;329:321‐5. [DOI] [PubMed] [Google Scholar]
Hainsworth 2001
- Hainsworth J, Barlow JH. Volunteers' experiences of becoming an arthritis self‐management lay‐leader: 'It's almost as if I've stopped ageing and started to get younger!'. Arthritis Care and Research 2001;45:378‐83. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [updated February 2008]. The Cochrane Collaboration 2008. Available from www.cochrane‐handbook.org..
Hilty 2006
- Hilty DM, Yellowlees PM, Cobb HC, Neufeld JD, Bourgeois JA. Use of secure e‐mail and telephone psychiatric consultations to accelerate rural health service delivery. Telemedicine Journal and e‐health: the official journal of the American Telemedicine Association 2006;12:490‐5. [DOI] [PubMed] [Google Scholar]
Lewin 2005
- Lewin SA, Dick J, Pond P, Zwarenstein M, Aja G, Wyk B, et al. Lay health workers in primary and community health care. Cochrane Database of Systematic Reviews 2005, Issue 1. [DOI: 10.1002/14651858.CD004015.pub2] [DOI] [PubMed] [Google Scholar]
Lorig 1998
- Lorig K, Gonzales M, Laurent DD, Morgan L, Laris BA. Arthritis self management program variations: three studies. Arthritis Care and Research 1998;11:448‐54. [DOI] [PubMed] [Google Scholar]
Luks 1998
- Luks A. Helper's high. Psychology Today 1998;October:39‐40. [Google Scholar]
McBride 1999
- McBride CM, Rimer BK. Using the telephone to improve health behaviour and health service delivery. Patient Education and Counseling 1999;37:3‐18. [DOI] [PubMed] [Google Scholar]
Meier 2007
- Meier A, Lyons EJ, Frydman G, Forlenza M, Rimer BK. How cancer survivors provide support on cancer‐related Internet mailing lists. Journal of Medical Internet Research 2007;9:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mishara 2007
- Mishara BL, Chagnon F, Daigle M, Balan B, Raymond S, Marcoux I, et al. Which helper behaviours and intervention styles are related to better short‐term outcomes in telephone crisis intervention? Results from a Silent Monitoring Study of Calls to the U.S. 1‐800‐SUICIDE Network. Suicide and Life threatening behaviour 2007;37:308‐21. [DOI] [PubMed] [Google Scholar]
Moen 1989
- Moen P, Dempster‐McClain D, Williams RM. Social integration and longevity: an event history analysis of women's roles and resilience. American Sociological Review 1989;54:635‐47. [Google Scholar]
Monnier 2003
- Monnier J, Knapp RG, Frueh BC. Recent advances in telepsychiatry: an updated review. Psychiatric Services 2003;54:1604‐9. [DOI] [PubMed] [Google Scholar]
Mowbray 1996
- Mowbray CT, Moxley DP, Thrasher S, Bybee D, McCrohan N, Harris S, et al. Consumers as community support providers: issues created by role intervention. Community Mental Health Journal 1996;32:47‐67. [DOI] [PubMed] [Google Scholar]
NICE 2008
- Maternal and Child Nutrition: guidance. National Institute for Health and Clinical Excellence 2008, issue PH 11.
Omoto 2000
- Omoto AM, Snyder M, Martino SC. Volunteering and mortality among older adults: findings from a national sample. Journal of Gerontology: Social Sciences 2000;54:173‐80. [DOI] [PubMed] [Google Scholar]
Rollnick 2002
- Rollnick S, Mason P, Butler C. Health Behavior Change: A Guide for Practitioners. Churchill Livingstone, 2002. [Google Scholar]
Rosenstock 1966
- Rosenstock IM. Why people use health services. Milbank Quarterly 1966;44 (suppl 3):94‐127. [PubMed] [Google Scholar]
Sood 2008
- Sood A, Andoh J, Rajoli N, Hopkins‐Price P, Verhulst SJ. Characteristics of smokers calling a national reactive telephone helpline. American Journal of Health Promotion 2008;22:176‐9. [DOI] [PubMed] [Google Scholar]
Stead 2006
- Stead LF, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD002850.pub2] [DOI] [PubMed] [Google Scholar]
Stewart 1995
- Stewart MJ, Tilden V. The contributions of health care science to social support. International Journal of Nursing Studies 1995;32:535‐44. [DOI] [PubMed] [Google Scholar]
Suggs 2006
- Suggs LS. A 10 year retrospective of research in new technologies for health communication. Journal of Health Communication 2006;11:61‐74. [DOI] [PubMed] [Google Scholar]
Thompson 1996
- Thompson D. The Oxford dictionary of current English. Oxford University Press, 1996. [Google Scholar]
Tilkeridis 2005
- Tilkeridis J, O'Connor L, Pignalosa G, Bramwell M, Jefford M. Peer support for cancer patients. Australian Family Physician 2005;34:288‐9. [PubMed] [Google Scholar]
van Dam 2005
- Dam HA, Horst FG, Knoops L, Pychman RM, Crebolder HF, Borne BH. Social support in diabetes: a systematic review of controlled intervention studies. Patient Education and Counselling 2005;59:1‐12. [DOI] [PubMed] [Google Scholar]


