Abstract
Both sedentary behavior (SB) and physical activity (PA) are associated with cardiorespiratory fitness (CRF) and independent of each other. Due to the limited time during school for children and adolescents, it is necessary to explore the isotemporal substitution of SB for PA on CRF.
A total 536 eligible participants selected from the 7 traditional administrative regions of China were included in this study. The outcome was CRF, determined using a 20-meter shuttle run test, and exposures were SB, light physical activity (LPA), and moderate-to-vigorous physical activity (MVPA) measured with accelerometers. We analyzed the cross-sectional associations of substituting SB with LPA, MVPA, and combinations of LPA and MVPA with CRF, using an isotemporal substitution model.
Reallocating SB into MVPA was associated with higher CRF for male (P < .01) and female (P < .01) children and female adolescents (P < .05). In the mixed redistribution, the ratio of LPA to MVPA for male children and female adolescents started from 16:4 and 14:6, respectively, tended toward improvements in CRF. For female children, regardless of the ratio of LPA to MVPA, it was always associated with higher CRF.
Reallocating SB into MVPA isotemporally was positively associated with CRF for male and female children and female adolescents but not for male adolescents. MVPA is the key factor to improve CRF when combinations of LPA and MVPA replace SB. The combined approach can provide basis for the selection of target and monitoring variables in intervention studies, and has more flexible choices for improving CRF that are more consistent with the daily PA habits of children and adolescents.
Keywords: cardiorespiratory fitness, isotemporal substitution, physical activity, sedentary behavior
1. Introduction
Cardiorespiratory fitness (CRF) is the core element of physical health.[1] In adulthood, low CRF is highly associated with cardiovascular disease, all-cause death, diabetes, and stroke.[2–4] In childhood and adolescence, good CRF can reduce rates of overweight and obesity,[5] promote healthy bone development, maintain good mental health,[1] and reduce the risk of developing cardiovascular diseases in adulthood.[6] In recent decades, the CRF of children and adolescents worldwide has shown a declining trend.[7] Identifying the factors closely related to CRF has become an important research issue in the field of public health, to explore effective methods to improve the CRF of children and adolescents.
Longitudinal studies have found that physical activity (PA) in children and adolescents is associated with CRF at a low to moderate level.[8,9] Although PA is not as important as genetic factors in CRF,[10] increasing moderate-to-vigorous physical activity (MVPA) can substantially improve CRF in children and adolescents who are physically inactive.[9] At the same time, studies have shown that the effect of sedentary behavior (SB) on CRF is independent of PA, and even an additional increase in MVPA cannot offset the adverse effects of SB on CRF for a long period.[11] Because the available time in each day is limited, adding time for 1 activity inevitably reduces the time for another. Children and adolescents have relatively fixed schedules during the school year, and it is often difficult for them to find additional time for MVPA. Can we replace SB with MVPA and maintain consistency in the overall time spent engaged in PA, to promote the improvement of CRF? The use of an isotemporal substitution (IS) model makes it possible to test this idea. The IS model can well simulate the effect on CRF of replacing SB with time equivalent to MVPA without increasing the overall time. Studies in adults have shown that replacing SB with MVPA or even light physical activity (LPA) can significantly improve CRF in middle-aged and older people.[12,13] Studies in children and adolescents have shown that replacing SB with MVPA or VPA can effectively reduce body mass index (BMI), waist circumference, and the risk of metabolic disease.[14–16] There are fewer studies assessing the association of reallocating SB into MVPA on CRF, but limited evidence suggests that replacing SB with MVPA was positively associated with children's CRF.[17–19] However, compared with children, adolescents are in the period of puberty and changes in body composition may affect the relationship between PA and CRF.[20] Thus, in adolescents, it remains unclear whether there are beneficial effects on CRF from replacing SB with higher-intensity PA. The choices of alternative time length differed widely in the existing research. Santos et al[17] and Jones et al[19] used a 30-minute substitution time to investigate the effect on CRF of replacing SB with PA of different intensities; however, the 30-minute substitution time was clearly too ambitious and difficult to achieve.[17,21] Collings et al[18] chose an alternative length of 10 minutes, which may accumulate less time for MVPA than the recommended amount of 60 minutes. Further research is needed on how to determine the appropriate substitution time duration. In addition, it is difficult to strictly substitute a single intensity of PA for SB in daily life. The components of PA in children and adolescents are complex, and engaging in PA for a period often involves a mixture of different intensities of activity,[22] making it impossible to accurately evaluate the components of PA that replace SB, and leading to a lack of practical guidance in the research findings.
The aim of this study was to determine the associations of reallocating 20 minutes of SB into LPA, MVPA, and combinations of LPA and MVPA with CRF in children and adolescents between the ages of 7 and 18.
2. Methods
2.1. Participants
From March to July 2019, the research team recruited a total of 840 participants aged 7 to 18 years in 7 cities (Shanghai, Taiyuan, Guangzhou, Changsha, Urumqi, Chengdu, and Kunming) to participate in the research project. One primary school, 1 middle school, and 1 high school were randomly selected from each city, and 5 male and female students were randomly selected from each grade in each school. All participants had no health problems and could perform a physical fitness test. To avoid bias in testing methods, the research team conducted a unified training for the physical education teachers. The same instruments were used in the test. Before the investigation, students and parents were told that the purpose of the study was to understand the PA levels of the students. Written informed consent was obtained from all students and parents. This investigation was conducted as an anonymous survey. We excluded 185 participants who did not complete the 20-meter shuttle run test (20-m SRT). As this study relied on the validity of accelerometer data, 119 participants were excluded because they did not meet the criteria for wearing an accelerometer. Thus, a total of 536 eligible participants were included in the study.
2.2. Measurements
2.2.1. CRF
In this study, a 20-m SRT was used to evaluate CRF. After a warm-up, participants stood on 1 of 2 lines 20 meters apart and ran back and forth to a musical tempo, which increased from slow to fast. The initial stage speed was 8.5 km/h, and the second stage was 9.0 km/h. Subsequently, the speed was increased by 0.5 km/h with each step. When participants could no longer maintain the speed set by the music and stopped running halfway, or if they could not reach the end line twice in a row before the music started, the test was terminated. The total number of round trips was taken as the final score.[23] To calculate the maximal oxygen consumption (VO2max), we included 20-m SRT performance, sex, age, and BMI in the following formula: VO2max (mL·kg−1·min−1) = 61.1 − 2.20 (sex: M = 0; F = 1) − 0.462 (age) − 0.862 (BMI) + 0.192 (total laps).[24] 20-m SRT has a high correlation with VO2max, an important index reflecting CRF, which can be used to evaluate CRF for children and adolescents.[25]
2.2.2. PA
PA was measured over 7 consecutive days with a GT3X+ (ActiGraph, Pensacola, FL) worn at the right hip. The epoch duration was set to 5 second. After 7 days of wearing the accelerometer, the participant removed the accelerometer and immediately exported and saved the accelerometer data using ActiLife version 6.10.2 software. As the accelerometer wear time criteria included in the analysis, we followed Adilson et al and defined 1 valid day as a wear time of more than 600 minutes for 1 day of wearing an accelerometer, totaling 3 effective days and above, and including at least 2 school days and 1 weekend day (Saturday and/or Sunday).[26] The cut-points of Evenson et al was adopted to classify SB (0–100 counts/min), LPA (101–2295 counts/min), MPA (2296–4011 counts/min), and VPA (4012 counts/min or more).[27] The cut-points used in this study had high validity and reliability in evaluating PA of children and adolescents.[28]
2.2.3. Covariates
The following variables were considered potential confounders: residence, socioeconomic status (SES), sleep time, and BMI; questionnaires were conducted to collect information on these variables. Residence was divided into urban or rural. Parental education, parental occupation, and household income were used to assess children's SES.[29] Sleep time was reported by the individual, as the time from going to bed at night to getting up in the morning. Body height was determined to the nearest 0.1 cm using a mechanical height gauge, with the participant wearing no shoes. Body weight was measured to the nearest 0.1 kg using an electronic scale, with the participant wearing light clothing and no shoes. BMI was calculated using the weight and height.
2.3. Statistical analysis
A Kolmogorov–Smirnov test was used to test the normality of all variables. One-way ANOVA (for parametric variables) and Mann–Whitney U test (for non-parametric variables) were used to compare the differences between males and females. VO2max was the outcome variable; SB, LPA, and MVPA were the exposure variables; and age, BMI, SES, sleep time, residence, and accelerometer wear time were the covariates. Single, partition, and IS linear regression models were used to analyze the relationship between CRF and SB, LPA, and MVPA.
In the single model, we examined the effects of each type of PA component on CRF, without considering the interaction between different types of PA. The model expression (in the case of SB) is:
Using the partition model, we simultaneously examined the effects of all types of PA on CRF. We omitted monitor wear time because wear time is, by default, the sum of SB and active time. The model expression is:
β1, β2, and β3 represent the effect of increasing a certain type of PA while keeping other types of PA unchanged.
We used the IS model to evaluate the effect of replacing SB with the same LPA and MVPA times, after excluding SB. The model expression is:
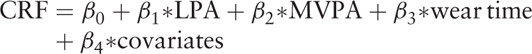 |
β1 and β2 represent the coefficients of replacing SB with LPA and MVPA, respectively, and β3 represents the coefficient of excluding SB.[30]
First, this study adopted 20 minutes as the isochronous substitution time to evaluate the effect of LPA and MVPA isochronous substitution of SB on CRF. Then, to better simulate the daily PA of children and adolescents, different combinations of LPA and MVPA times (LPA or MVPA increased or decreased in increments of 2 minutes) were used to replace SB in this study. Due to the known variability in CRF by pubertal status and sex, participants were categorized as children (7–13 years for males and 7–11 years for females) and adolescents (14–18 years for males and 12–18 years for females) and stratified by sex.[31] Statistical significance was set at .05, and all analyses were conducted using IBM SPSS version 25.0 for Windows (IBM Corp., Armonk, NY).
3. Results
Table 1 shows the descriptive characteristics of the study sample. There was no significant difference between males and females with respect to SES, sleep time, SB, LPA, and accelerometer wear time. The mean VO2max (P < .001) and the median MVPA (P < .001) for males were larger than those of females.
Table 1.
Descriptive characteristics of participants.
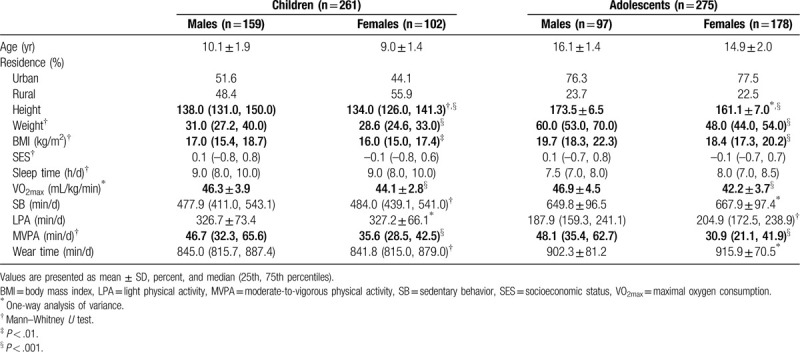
Table 2 shows the associations of SB, LPA, and MVPA with CRF in the single, partition, and IS models in male children and adolescents. In the single and partition models, among children, MVPA was positively associated with CRF (B = 0.03; 95%CI, 0.01–0.05; P < .01). In the IS model, among children, replacing SB (B = 0.57; 95%CI, 0.17–0.97; P < .01) and LPA (B = 0.64; 95%CI, 0.18–1.10; P < .01) with 20 minutes’ MVPA were positively associated with CRF.
Table 2.
Single, partition and isotemporal substitution models examining the associations of sedentary behavior, light physical activity and moderate-to-vigorous physical activity with cardiorespiratory fitness for male children and adolescents.
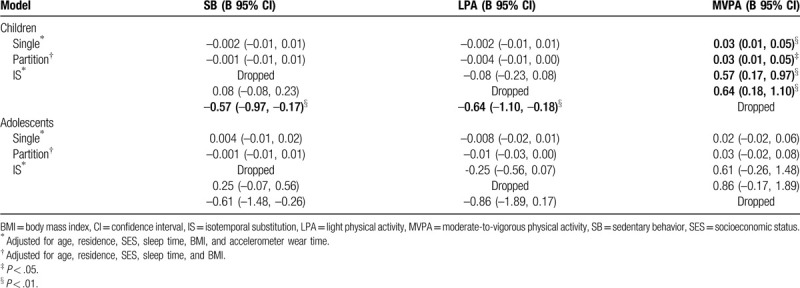
Table 3 shows the associations of SB, LPA, and MVPA with CRF in the single, partition, and IS models in female children and adolescents. In the single model, among children, MVPA was positively associated with CRF (B = 0.03; 95%CI, 0.01–0.06; P < .01). In the partition model, MVPA and CRF were positively associated (B = 0.03; 95%CI, 0.01–0.06; P < .05) in children and adolescents. In the IS model, among children, replacing SB (B = 0.65; 95%CI, 0.12–1.19; P < .05) and LPA (B = 0.64; 95%CI, 0.03–1.25; P < .05) with 20 minutes’ MVPA was positively associated with CRF; among adolescents, reallocating 20 minutes of SB (B = 0.48; 95%CI, –0.01 to 0.97; P < .05) and LPA (B = 0.61; 95%CI, 0.09–1.13; P < .05) to MVPA was positively associated with CRF.
Table 3.
Single, partition and isotemporal substitution models examining the associations of sedentary behavior, light physical activity and moderate-to-vigorous physical activity with cardiorespiratory fitness for female children and adolescents.
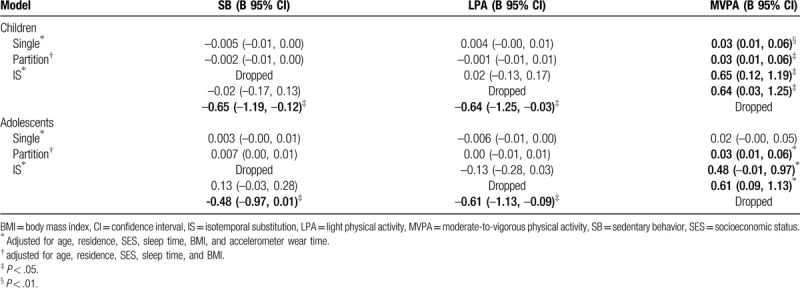
Figure 1 shows the associations of mixed redistributions of the time spent engaged in LPA and MVPA, to replace 20 min/d of SB with CRF. Starting from the mixed redistribution of 16 minutes’ LPA and 4 minutes’ MVPA for male children (Fig. 1A) and 14 minutes’ LPA and 6 minutes’ MVPA for female adolescents (Fig. 1C), combinations of LPA and MVPA tended toward improvements in CRF. MVPA is the key factor for CRF (Fig. 1A and C). Regardless of the ratio of LPA to MVPA, it was always positively associated with CRF among female children (Fig. 1B). There was a null association of mixed redistributions of LPA and MVPA, to replace SB in male adolescents. Therefore, we did not present the results with graph. In summary, each 2 min/d increase of MVPA resulted in greater magnitudes of improvement for CRF, in a linear fashion.
Figure 1.
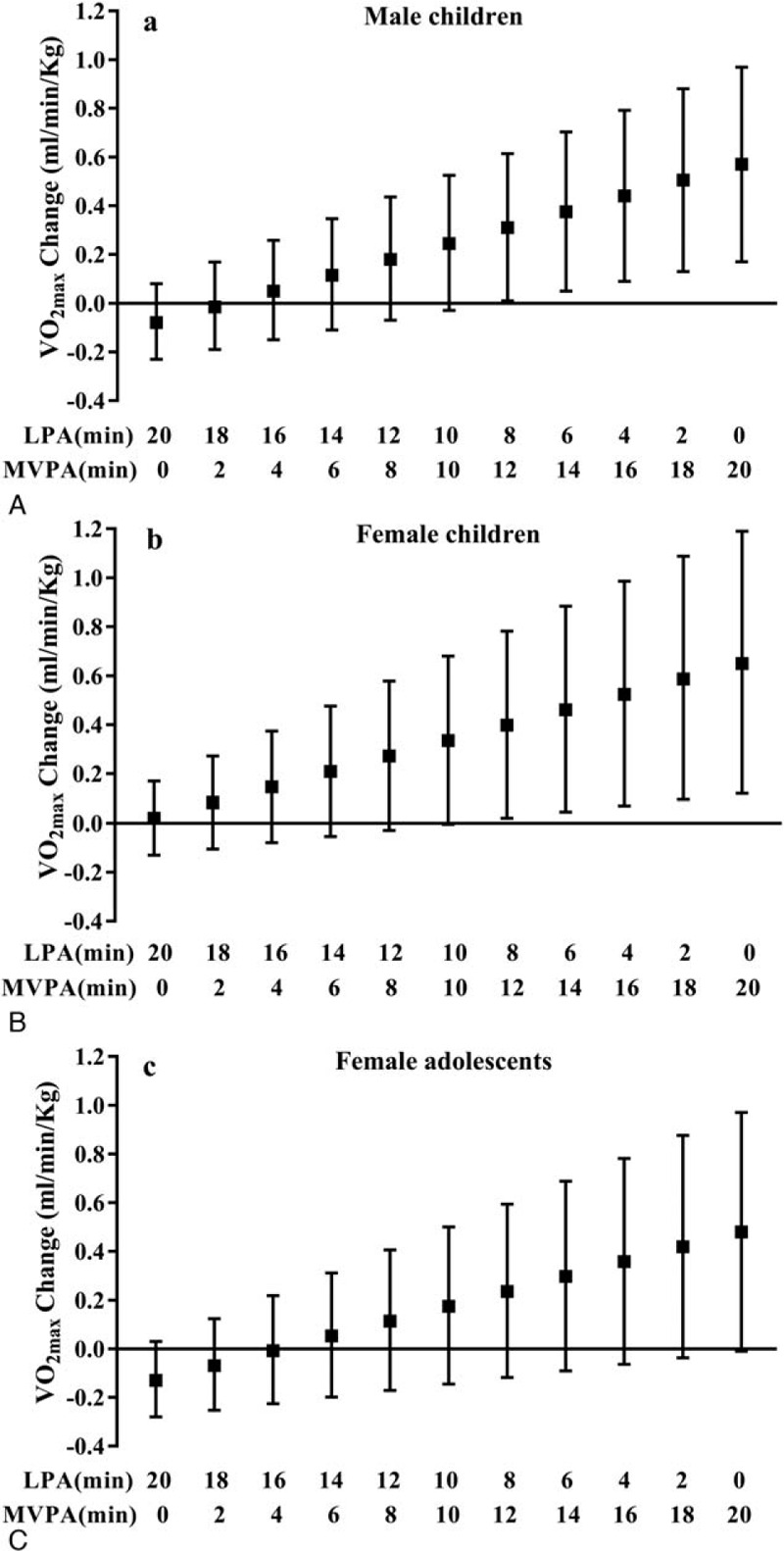
Substitution regression models were performed by redistributing 20 min/d of SB to a mixed share of LPA and MVPA in increments of 2 min/d (ie, 0 min/d MVPA and 20 min/d LPA, 2 min/d MVPA and 18 min/d LPA, …, 20 min/d MVPA and 0 min/d LPA) while keeping total accelerometer wear time constant. The values (black squares) indicate the unstandardized coefficients of LPA and MVPA combinations replacing SB, adjusted for age, residence, SES, sleep time, BMI, and accelerometer wear time. The black solid lines represent the 95% confidence intervals of the coefficients. BMI = body mass index, LPA = light physical activity, MVPA = moderate-to-vigorous physical activity, SB = sedentary behavior, SES = socioeconomic status, VO2max = maximal oxygen consumption.
4. Discussion
In this study, we found that reallocating 20 minutes of SB into MVPA was associated with higher CRF for male and female children and female adolescents but not for male adolescents. Meanwhile, the replacement of LPA with 20 minutes MVPA was also positively associated with CRF, but the replacement of SB with LPA has a null association with CRF. In the mixed redistribution of 20 minutes’ SB, the ratio of LPA:MVPA for male children and female adolescents started at 16:4 and 14:6, respectively, tending toward improvement in CRF. For female children, regardless of the ratio of LPA to MVPA, it was always associated with higher CRF.
The importance of PA for the health of children and adolescents has been confirmed in many studies. Research from the Italian ASSO project found that SB and lack of PA were the primary causes of health problems for children and adolescents,[32,33] and promoting PA was a key means to improve physical fitness and other health factors.[34] The results of this study also confirmed that increasing PA and reducing SB were positively associated with CRF in children. This is consistent with previous studies: Jones et al[19] and Santos et al[17] found that replacing SB with 30 minutes of MVPA or VPA was positively associated with CRF in children. Collings et al used MPA and VPA to replace SB for 10 minutes and also found positive associations; in addition, MPA and VPA replacing LPA still showed benefits in improving CRF.[18] In this study, we found a sex difference for the association of MVPA replacing SB on the CRF of adolescents; only the CRF of female adolescents had a significant association. The main reason for this difference may be that MVPA showed a null association with CRF for male adolescents. For male adolescents, only hard and vigorous PA was significantly associated with CRF, but for female adolescents, moderate and vigorous PA were associated with CRF.[35,36] The possible explanations are as follows: first, because of the interaction between MVPA and SB in male adolescents, the association between MVPA and CRF was weakened by SB.[37] But this interaction was not found in female adolescents;[37] second, compared with male adolescents, females had lower CRF, and the PA intensity threshold required to improve CRF was lower than that of males.[38] Consistent with previous studies, this study showed that MVPA was not associated with CRF for male adolescents in the single and partition models. Therefore, whether MVPA replaced SB or LPA, the correlation between MVPA and CRF was not significant for male adolescents.
Difference from previous studies is that we used 20 minutes as a bout length. Most past studies have used widely varying bout lengths and had no consistent selection criteria. Therefore, the feasibility of bout length is an important issue to be considered in an IS model. In some studies, 30 minutes or 60 minutes of PA with different intensities were used to replace SB.[17,39] Because PA in daily life is mostly LPA, it is relatively easy to replace SB with 30 or 60 minutes of LPA; however, it is too ambitious and difficult to replace SB with 60 or even 30 minutes of MVPA .[21] Another study suggested that the bout length should be at least 10 minutes, as this was the lowest cumulative time of MVPA required to receive health benefits.[40] However, recent studies have shown that participation in MVPA, regardless of duration, can reduce all-cause mortality, cancer mortality, and the risk of cardiovascular disease.[41] The 2018 Physical Activity Guideline for Americans has also omitted its statement that MVPA should last at least 10 minutes per session.[42] In addition, adoption of a 10-minute length may accumulate even less MVPA than the amount recommended by the World Health Organization of 60 minutes per day. Using descriptive statistics, we found that the median MVPA value was 46.7 min/d and 35.6 min/d for male and female children, and 48.1 min/d and 30.9 min/d for male and female adolescents, which are about 20 minutes less than the recommended 60 min/d. For these reasons, we chose 20 minutes as the bout length, which not only met the World Health Organization recommendation for MVPA but is also not difficult to achieve. The finding that more than 82.5% of Chinese children and adolescents were insufficiently physically active, is consistent with recent literature.[43] The data from China is representative. Therefore, the present study suggests that when the IS model is adopted in children and adolescents to investigate replacement of SB with MVPA, attention should be paid to the following 2 aspects in the selection of duration:
-
(1)
the recommended 60 minutes of MVPA every day should be met, as far as possible;
-
(2)
the bout length should not exceed 30 minutes.
To our best knowledge, there are no studies exploring the effect on CRF of mixed redistribution of LPA and MVPA to replace SB among children and adolescents. In this study, we found that MVPA was a key factor to improve the CRF of children and adolescents, especially for male children and female adolescents. First, this study emphasizes the importance for CRF of increasing the MVPA ratio in PA, which can provide important basis for the selection of target and monitoring variables in intervention studies. School-based PA interventions are an important means of improving PA levels among children and adolescents.[44] Previous studies have generally stated that such intervention has a better effect on improving CRF in these populations.[45] However, a recent meta-analysis found that school-based PA interventions had no significant effect on the improvement of high-intensity PA in children and adolescents,[46,47] mainly because the proportion of MVPA in both groups was too low and more than half their time was spent engaged in SB and LPA.[48,49] Therefore, although school-based PA interventions provide a beneficial approach and resources to improve PA, these cannot provide sufficient intensity to ensure health benefits.[50] In addition, this study also found that the replacement of LPA by MVPA also had a positive effect on CRF in children and adolescents. The results of this study suggest that physical education teachers or leaders of sports clubs should pay close attention to the monitoring of the proportion of LPA and MVPA when organizing sports activities and should try to reasonably increase the proportion of MVPA. Second, our study emphasizes that the hybrid substitution model has strong practical significance, which can provide more flexible choices for changing the sedentary lifestyle of children and adolescents, improving CRF to levels that are more in line with the daily PA habits of children and adolescents. Replacing SB with a single intensity of PA has a theoretical effect on CRF. In real life, the components of PA among children and adolescents are more complex, and engaging in PA often involves different intensities.[22] Therefore, it may be closer to the actual situation to evaluate the effect on CRF of substituting SB with a combination of LPA and MVPA.
A strength of the present study is the use of a novel statistical method to examine the theoretical effect on CRF of IS of SB with LPA and MVPA. Additionally, using the mixed redistribution approach, it is more practical to evaluate the effect of LPA and MVPA in replacing SB on CRF. Despite the relevance of the present study, some methodological limitations must be taken into consideration. Because this was a cross-sectional study, it was impossible to determine causality. However, we cannot rule out the possibility of reverse causation, in that children who are fitter may in turn be more active. Furthermore, an accelerometer was used to measure SB in terms of intensity; however, other behaviors, such as standing or lying down, are also lower in intensity and may overestimate SB time.
5. Conclusions
Reallocating SB to MVPA isotemporally was positively associated with CRF for male and female children and female adolescents but not for male adolescents. MVPA is the key factor for CRF when combinations of LPA and MVPA replace SB. The combined approach can provide basis for the selection of target and monitoring variables in intervention studies, and has more flexible choices for improving CRF that are more consistent with the daily PA habits of children and adolescents.
Acknowledgments
We would like to make a grateful acknowledgment to all persons who have helped us with this study. Our deepest gratitude also goes to Pro. Yi Song in Peking University Health Science Center and Dr. Zhenya Chang in East China Normal University for their statistical consultation and selfless assistance.
Author contributions
Conceptualization: Xiaojian Yin.
Data curation: Yi Sun.
Formal analysis: Cunjian Bi, Ming Li.
Funding acquisition: Yuqiang Li.
Investigation: Cunjian Bi, Ming Li, Ting Zhang, Feng Zhang, Ting Yang, Ge Song.
Methodology: Yuqiang Li, Xiaofang Yang.
Software: Junfang Cao, Yaru Guo.
Visualization: Junfang Cao, Yaru Guo.
Writing – original draft: Yi Sun.
Writing – review & editing: Xiaojian Yin.
Footnotes
Abbreviations: BMI = body mass index, CRF = cardiorespiratory fitness, IS = isotemporal substitution, LPA = light physical activity, MVPA = moderate-to-vigorous physical activity, PA = physical activity, SB = sedentary behavior, SES = socioeconomic status.
How to cite this article: Sun Y, Yin X, Li Y, Bi C, Li M, Yang X, Zhang T, Zhang F, Cao J, Guo Y, Yang T, Song G. Isotemporal substitution of sedentary behavior for physical activity on cardiorespiratory fitness in children and adolescents. Medicine. 2020;99:30(e21367).
This study was supported by Shanghai Pujiang Program (17PJC028). The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Human Experimental Ethics Committee of East China Normal University. (HR006-2019).
The authors report no conflicts of interest.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Janssen I, Leblanc AG. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int J Behav Nutr Phys Act 2010;7:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Blair SN, Kampert JB, Kohl HR, et al. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA 1996;276:205–10. [PubMed] [Google Scholar]
- [3].Katzmarzyk PT, Church TS, Janssen I, et al. Metabolic syndrome, obesity, and mortality: impact of cardiorespiratory fitness. Diabetes Care 2005;28:391–7. [DOI] [PubMed] [Google Scholar]
- [4].Lee CD, Blair SN. Cardiorespiratory fitness and stroke mortality in men. Med Sci Sports Exerc 2002;34:592–5. [DOI] [PubMed] [Google Scholar]
- [5].Ortega FB, Tresaco B, Ruiz JR, et al. Cardiorespiratory fitness and sedentary activities are associated with adiposity in adolescents. Obesity (Silver Spring) 2007;15:1589–99. [DOI] [PubMed] [Google Scholar]
- [6].Hogstrom G, Nordstrom A, Nordstrom P. High aerobic fitness in late adolescence is associated with a reduced risk of myocardial infarction later in life: a nationwide cohort study in men. Eur Heart J 2014;35:3133–40. [DOI] [PubMed] [Google Scholar]
- [7].Tomkinson GR, Leger LA, Olds TS, et al. Secular trends in the performance of children and adolescents (1980-2000): an analysis of 55 studies of the 20m shuttle run test in 11 countries. Sports Med 2003;33:285–300. [DOI] [PubMed] [Google Scholar]
- [8].Kemper H, Twisk J, Koppes L, et al. A 15-year physical activity pattern is positively related to aerobic fitness in young males and females (13-27 years]. Eur J Appl Physiol 2001;84:395–402. [DOI] [PubMed] [Google Scholar]
- [9].Kristensen PL, Moeller NC, Korsholm L, et al. The association between aerobic fitness and physical activity in children and adolescents: the European youth heart study. Eur J Appl Physiol 2010;110:267–75. [DOI] [PubMed] [Google Scholar]
- [10].Peter I, Papandonatos GD, Belalcazar LM, et al. Genetic modifiers of cardiorespiratory fitness response to lifestyle intervention. Med Sci Sports Exerc 2014;46:302–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Rute S, Jorge M, Anthony David O, et al. The independent associations of sedentary behaviour and physical activity on cardiorespiratory fitness. Br J Sports Med 2014;48:1508–12. [DOI] [PubMed] [Google Scholar]
- [12].van der Velde JH. Sedentary behavior, physical activity, and fitness—the Maastricht study. Med Sci Sport Exer 2017;49:1583–91. [DOI] [PubMed] [Google Scholar]
- [13].Ekblom-Bak E, Ekblom Ö, Bolam KA, et al. SCAPIS pilot study: sitness, fitness and fatness— is sedentary time substitution by physical activity equally important for everyone's markers of glucose regulation? J Phys Act Health 2016;13:697–703. [DOI] [PubMed] [Google Scholar]
- [14].Dumuid D, Stanford TE, Pedišić Z, et al. Adiposity and the isotemporal substitution of physical activity, sedentary time and sleep among school-aged children: a compositional data analysis approach. BMC Public Health 2018;18:311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Sardinha LB, Marques A, Minderico C, et al. Cross-sectional and prospective impact of reallocating sedentary time to physical activity on children's body composition. Pediatr Obes 2017;12:373–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hansen BH, Anderssen SA, Andersen LB, et al. Cross-sectional associations of reallocating time between sedentary and active behaviours on cardiometabolic risk factors in young people: an international children's accelerometry database (ICAD) analysis. Sports Med 2018;48:2401–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Santos DA, Marques A, Minderico CS, et al. A cross-sectional and prospective analyse of reallocating sedentary time to physical activity on children's cardiorespiratory fitness. J Sports Sci 2018;36:1720–6. [DOI] [PubMed] [Google Scholar]
- [18].Collings PJ, Westgate K, Väistö J, et al. Cross-sectional associations of objectively-neasured physical activity and sedentary time with body composition and cardiorespiratory fitness in mid-childhood: the PANIC study. Sports Med 2017;47:769–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Jones MA, Skidmore PM, Stoner L, et al. Associations of accelerometer-measured sedentary time, sedentary bouts, and physical activity with adiposity and fitness in children. J Sport Sci 2020;38:114–20. [DOI] [PubMed] [Google Scholar]
- [20].Sveinsson T, Arngrimsson SA, Johannsson E. Association between aerobic fitness, body composition, and physical activity in 9- and 15-year-olds. Eur J Sport Sci 2009;9:141–50. [Google Scholar]
- [21].Dalene KE, Anderssen SA, Andersen LB, et al. Cross-sectional and prospective associations between physical activity, body mass index and waist circumference in children and adolescents. Obes Sci Pract 2017;3:249–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Leek D, Carlson JA, Cain KL, et al. Physical activity during youth sports practices. Arch Pediatr Adolesc Med 2011;165:294–9. [DOI] [PubMed] [Google Scholar]
- [23].Léger LA, Mercier D, Gadoury C, et al. The multistage 20 metre shuttle run test for aerobic fitness. J Sports Sci 1988;6:93–101. [DOI] [PubMed] [Google Scholar]
- [24].Matsuzaka A, Takahashi Y, Yamazoe M. Validity of the multistage 20-m shuttle-run test for Japanese children, adolescents, and adults. Pediatr Exerc Sci 2004;16:113–25. [Google Scholar]
- [25].Tomkinson GR, Lang JJ, Tremblay MS, et al. International normative 20 m shuttle run values from 1 142 026 children and youth representing 50 countries. Br J Sports Med 2017;51:1545–54. [DOI] [PubMed] [Google Scholar]
- [26].Adilson M, Rute S, Ulf E, et al. Association between physical activity, sedentary time, and healthy fitness in youth. Med Sci Sports Exerc 2015;47:575–80. [DOI] [PubMed] [Google Scholar]
- [27].Evenson KR, Catellier DJ, Gill K, et al. Calibration of two objective measures of physical activity for children. J Sports Sci 2008;26:1557–65. [DOI] [PubMed] [Google Scholar]
- [28].Trost SG, Loprinzi PD, Moore R, et al. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc 2011;43:1360–8. [DOI] [PubMed] [Google Scholar]
- [29].National Center for Education Statistics. Technical report and user guide for the 2015 program for international student assessment (PISA); 2017. Available at: https://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2017095. Accessed November 5, 2019. [Google Scholar]
- [30].Mekary RA, Willett WC, Hu FB, et al. Isotemporal substitution paradigm for physical activity epidemiology and weight change. Am J Epidemiol 2009;170:519–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Yin XJ, Ji CY. Malnutrition prevalence in lasa xizang children and adolescents. Biomed Environ Sci 2014;27:614–26. [DOI] [PubMed] [Google Scholar]
- [32].Bianco A, Mammina C, Jemni M, et al. A fitness index model for Italian adolescents living in Southern Italy. The ASSO project. J Sport Med Phys Fit 2016;56:1279–88. [PubMed] [Google Scholar]
- [33].Bianco A, Filippi AR, Breda J, et al. Combined effect of different factors on weight status and cardiometabolic risk in Italian adolescents. Ital J Pediatr 2019;45:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Garden T, Avery F, Monèm J, et al. Profiles of physical fitness risk behaviours in school adolescents from the ASSO project: a latent class analysis. Int J Env Res Pub He 2018;15:1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Denton SJ, Trenell MI, Plötz T, et al. Cardiorespiratory fitness is associated with hard and light intensity physical activity but not time spent sedentary in 10-14 year old schoolchildren: the HAPPY study. Plos One 2013;8:e61073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Ekelund U, Poortvliet E, Nilsson A, et al. Physical activity in relation to aerobic fitness and body fat in 14- to 15-year-old boys and girls. Eur J Appl Physiol 2001;85:195–201. [DOI] [PubMed] [Google Scholar]
- [37].Porter AK, Matthews KJ, Salvo D, et al. Associations of physical activity, sedentary time, and screen time with cardiovascular fitness in United States adolescents: results from the NHANES national youth fitness survey. J Phys Act Health 2017;14:506–12. [DOI] [PubMed] [Google Scholar]
- [38].Parikh T, Stratton G. Influence of intensity of physical activity on adiposity and cardiorespiratory fitness in 5-18 year olds. Sports Med 2011;41:477–88. [DOI] [PubMed] [Google Scholar]
- [39].Aggio D, Smith L, Hamer M. Effects of reallocating time in different activity intensities on health and fitness: a cross sectional study. Int J Behav Nutr Phy 2015;12:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Ekblom-Bak E, Ekblom Ö, Bergström G, et al. Isotemporal substitution of sedentary time by physical activity of different intensities and bout lengths, and its associations with metabolic risk. Eur J Prev Cardiol 2015;23:967–74. [DOI] [PubMed] [Google Scholar]
- [41].Lopez JPR, Gebel K, Chia D, et al. Associations of vigorous physical activity with all-cause, cardiovascular and cancer mortality among 64 913 adults. BMJ Open Sport Exerc Med 2019;5:e596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA 2018;320:2020–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Guthold R, Stevens GA, Riley LM, et al. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1.6 million participants. Lancet Child Adolesc Health 2020;4:23–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Weed M. Should we privilege sport for health? The comparative effectiveness of UK Government investment in sport as a public health intervention. Int J Sport Policy 2016;8:1–8. [Google Scholar]
- [45].Kriemler S, Meyer U, Martin E, et al. Effect of school-based interventions on physical activity and fitness in children and adolescents: a review of reviews and systematic update. Br J Sports Med 2011;45:923–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Metcalf B, Henley W, Wilkin T. Effectiveness of intervention on physical activity of children: systematic review and meta-analysis of controlled trials with objectively measured outcomes (Early Bird 54). BMJ 2012;345:e5888. [DOI] [PubMed] [Google Scholar]
- [47].Borde R, Smith JJ, Sutherland R, et al. Methodological considerations and impact of school-based interventions on objectively measured physical activity in adolescents: a systematic review and meta-analysis. Obes Rev 2017;18:476–90. [DOI] [PubMed] [Google Scholar]
- [48].Ridley K, Zabeen S, Lunnay BK. Children's physical activity levels during organised sports practices. J Sci Med Sport 2018;21:930–4. [DOI] [PubMed] [Google Scholar]
- [49].Leek D, Carlson JA, Cain KL, et al. Physical activity during youth sports practices. JAMA Pediatr 2011;165:294–9. [DOI] [PubMed] [Google Scholar]
- [50].Koorts H, Timperio A, Arundell L, et al. Is sport enough? Contribution of sport to overall moderate- to vigorous-intensity physical activity among adolescents. J Sci Med Sport 2019;22:1119–24. [DOI] [PMC free article] [PubMed] [Google Scholar]


