Supplemental Digital Content is available in the text
Keywords: drug therapy, injections, low back pain, radiculopathy, sciatica
Abstract
Background:
Previous systemic reviews have examined the efficacy of individual therapeutic agents, but which type of treatment is superior to another has not been pooled or analyzed. The objective of the current study was to compare the clinical effectiveness of epidural steroid injection (ESI) versus conservative treatment for patients with lumbosacral radicular pain.
Methods:
A systematic search was conducted with MEDLINE, EMBASE, and CENTRAL databases with a double-extraction technique for relevant studies published between 2000 and January 10, 2019. The randomized controlled trials which directly compared the efficacy of ESI with conservative treatment in patients with lumbosacral radicular pain were included. Outcomes included visual analog scale, numeric rating scale, Oswetry disability index, or successful events. Two reviewers extracted data and evaluated the methodological quality of papers using the Cochrane Collaboration Handbook. A meta-analysis was performed using Revman 5.2 software. The heterogeneity of the meta-analysis was also assessed.
Results:
Of 1071 titles initially identified, 6 randomized controlled trials (249 patients with ESI and 241 patients with conservative treatment) were identified and included in this meta-analysis. The outcome of the pooled analysis showed that ESI was beneficial for pain relief at short-term and intermediate-term follow-up when compared with conservative treatment, but this effect was not maintained at long-term follow-up. Successful event rates were significantly higher in patients who received ESI than in patients who received conservative treatment. There were no statistically significant differences in functional improvement after ESI and conservative treatment at short-term and intermediate-term follow-up. The limitations of this meta-analysis resulted from the variation in types of interventions and small sample size.
Conclusions:
According to the results of this meta-analysis, the use of ESI is more effective for alleviating lumbosacral radicular pain than conservative treatments in terms of short-term and intermediate-term. Patients also reported more successful outcomes after receiving ESI when compared to conservative treatment. However, this effect was not maintained at long-term follow-up. This meta-analysis will help guide clinicians in making decisions for the treatment of patients with lumbosacral radicular pain, including the use of ESI, particularly in the management of pain at short-term.
1. Introduction
Lumbosacral radicular pain, which is characterized by back pain radiating into the lower limbs,[1] is usually caused by the compression of a nerve root due to lumbar disc herniation or spinal stenosis.[2] Common nonsurgical treatments for lumbosacral radicular pain involve lifestyle modification, education, analgesic medication, physical therapy, exercise, and/or epidural steroid injections (ESIs).[3] Among them, ESIs are the most commonly performed procedures for the relief of lumbosacral radicular pain.[4] They may be performed to deliver steroids or local anesthetics to the site of pathology in the epidural space via a transforaminal, interlaminar, or caudal approach. Surgical treatment is considered in patients who do not respond to these nonsurgical treatments.
Previous systemic reviews on the efficacy of conservative treatments for lumbosacral radicular pain have indicated a lack of evidence that 1 type of treatment is superior to another.[5,6] Recent meta-analyses on ESI have focused on either the surgery-sparing effects of ESI compared to control injections [7] or a comparison of the 2 approach techniques.[8] There are many conservative treatment options for lumbosacral radicular pain such as bed rest, pharmacologic therapy, exercise, and physiotherapy, but the outcomes associated with these treatments are still questionable. Previous studies have examined the efficacy of these individual therapeutic agents, but which type of treatment is superior to another has not been pooled or analyzed. To date, no meta-analysis has directly compared the clinical efficacy of ESI and conservative treatment in patients with lumbosacral radicular pain. A meta-analysis regarding this subject would provide useful information and evidence for clinicians to decide on a treatment method in patients with lumbosacral pain. Thus, this study was performed to investigate whether ESI was better than conservative treatment for achieving clinical outcomes such as pain control and functional improvement in patients with lumbosacral radicular pain.
2. Methods
Multiple comprehensive databases were used to find literature that has compared ESI and conservative treatment for the management of lumbosacral radicular pain. This study is based on the Cochrane review methods.
2.1. Data source & literature source
A systematic search was performed using MEDLINE, EMBASE, and the Cochrane Central Register of Controlled Trials (CENTRAL) for studies comparing ESI with conservative treatment for the treatment of lumbosacral radicular pain, which were published up to January 10, 2019. No date limits were applied to the searches. There were no restrictions on language or year of publication in the search. The detailed searches of keywords and medical subject headings are presented in Supplemental file. These keywords included “spinal disease”, sciatica”, “spinal stenosis”, “epidural steroid injection”, and conservative treatment methods including “rehabilitation”, “laser therapy”, “ultrasound therapy”, “manual therapy”, “electric stimulation therapy”, “traction”, “exercise”, and “oral drug administration”. For other databases, search strategies were applied based on the MEDLINE strategy. Further relevant articles were hand-searched from the identified studies and were assessed individually for inclusion.
2.2. Study selection
Two reviewers (SYY and WK) independently determined the inclusion of all studies based on predefined selection criteria. Study selection was made through two levels of screening. At the first level, titles and abstracts of identified studies were screened. At the second level, the full texts were retrieved and assessed. Ethical approval and patient informed consent were not required because this is a meta-analysis of previously published studies and did not involve direct contact with patients or alterations to patient care.
The study was guided by the PICOS framework. P (population): patients aged over eighteen years with lumbosacral radicular pain and lumbosacral radicular pain was secondary to lumbar disc herniation or spinal stenosis. I (intervention): ESI. C (comparator): conservative treatments, including bed rest, pharmacologic therapy, exercise, and physiotherapy. O (outcomes): visual analog scale (VAS), numeric rating scale (NRS), Oswestry disability index (ODI), or successful events. All clinical outcomes were reported within 1 year after the interventions. S (study design): meta-analysis including only randomized controlled trials (RCTs). The exclusion criteria were as follows: review articles, abstracts, letters, and case reports; an absence of any outcome of interest; or back pain due to fracture, trauma, cancer, or infection.
2.3. Data extraction
The two reviewers (SYY and WK) independently extracted data from each study using a predefined data extraction form. Any disagreements were resolved by a third author (KHC) through consensus. The following data were extracted from each eligible study: first author's name; publication year; number of patients who received either ESI or conservative treatment; intervention protocol type (the type and amount of steroid and local anesthetics used for ESI and therapies or medication used for conservative treatment); outcome parameters including VAS, NRS, ODI, and successful events; duration of follow-up; cause of pain; and summary of findings. The extracted data were organized into a Microsoft Excel file and the data were verified for accuracy by a third author (KHC). The end-of-search date was January 10, 2019.
2.4. Assessment of methodological quality
The methodological quality and risk of bias of each study were assessed using the Cochrane Handbook for Systematic Reviews of Interventions.[9] This included random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of the outcome assessor (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other biases. Any disagreements were resolved by discussion and consensus.
2.5. Statistical analysis
Data were synthesized and a meta-analysis was performed using Review Manager Software version 5.2 (Cochrane Collaboration, Copenhagen, Denmark) when there were at least 3 studies. For continuous outcomes, such as pain and functional score, mean difference (MD) and 95% confidence intervals (CIs) were calculated for each study. VAS and NRS were used to evaluate pain scores, and ODI was applied to assess functional improvement. For dichotomous outcomes, such as successful events (as defined in the trial), relative risks were pooled. Planned subgroup analyses were conducted according to the duration of the treatment effect. Outcomes were analyzed as short-term (≤ 1 month), intermediate-term (1 to 3 months) and long-term (6 months to ≤1 year) for pain relief and as short-term (1 to 3 months) and intermediate-term (3 to 6 months) for functional improvement. The difference in the degree of improvement between two groups was assessed by comparing the difference on scales pre- and post-treatment. A correlation of 0.5 was used to estimate the change in standard deviation if standard deviation was given for baseline and endpoint instead of change.[10] Heterogeneity was assessed using the χ2-based Q-statistic method and I2 measurement. An I2 statistic > 50% or P < .1 indicated substantial heterogeneity.[11] In this case, a random-effects model was selected. In the absence of heterogeneity, a fixed- effects model was applied for the meta-analysis. The pooled effect was considered to be significant if P < .05. Publication bias was not applicable since less than 10 studies were included in this meta-analysis.[12]
3. Results
3.1. Study characteristics and patient populations
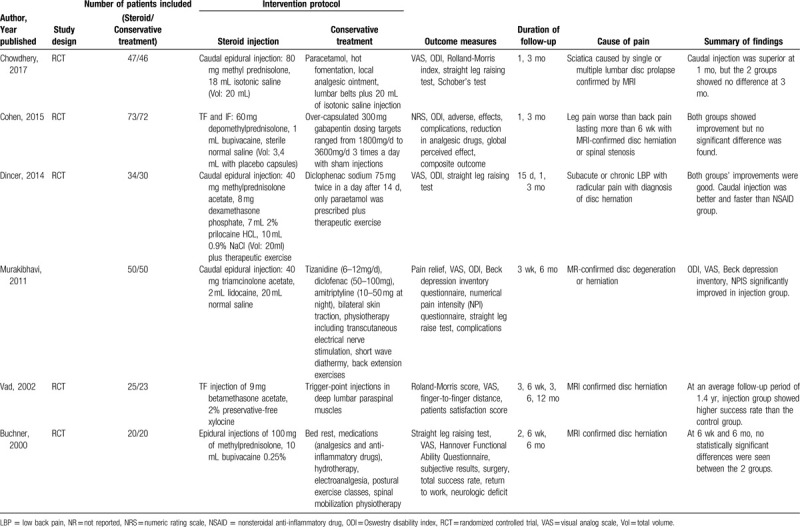
This meta-analysis involved patients with chronic lumbosacral radicular pain which persisted for at least 1 month. Patients were older than 18 years and were diagnosed with lumbar disc herniation or spinal stenosis using clinical and radiological evaluation. Of the 490 total patients in the studies analyzed, 249 patients were treated with ESI and 241 patients were treated with conservative treatment. The total number of participants in the analyzed studies ranged from 40 to 145 in the ESI and conservative treatment groups. Disc herniation and spinal stenosis were confirmed with MRI and patients suffered from sciatica with or without the presence of low back pain. The main characteristics of the included RCTs are summarized in Table 1.
Table 1.
Clinical characteristics of the included studies.
3.2. Identification of studies
A flowchart of the literature search and selection is shown in Figure 1. Searches of the databases resulted in 1,071 articles. After removing duplicates, a further 921 articles were excluded after the titles and abstracts were reviewed; 14 articles remained for further screening. Two studies were not RCTs.[13,14] One study on patients with non-specific low back pain was excluded.[15] Five studies were excluded due to the absence of data at follow-up pain evaluation.[16–20] Finally, 6 RCTs[10,21–25] were eligible and were included in the meta-analysis.
Figure 1.
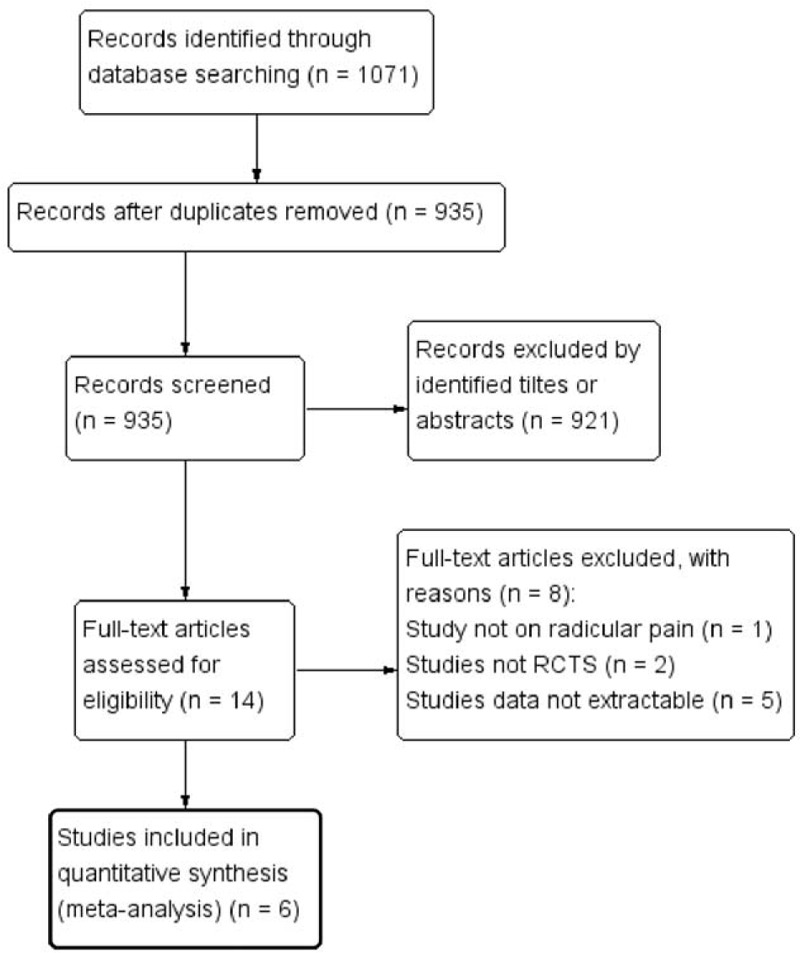
Flow diagram of the literature search.
3.3. Risk of bias in included studies
The risk of bias of the included RCTs is presented in Figures 2 and 3. One RCT was graded as high risk because it showed flaws in randomization process [22] and another study [21] was graded as high risk because they did not describe the procedure for blinding of participants. Three studies were rated as unclear because they did not adequately describe the procedure for random sequence generation [21] and allocation concealment.[22,25] The rest of domains of risk of bias were assessed as low risk in all 6 RCTs. Thus, the overall risk of bias was considered low.
Figure 2.
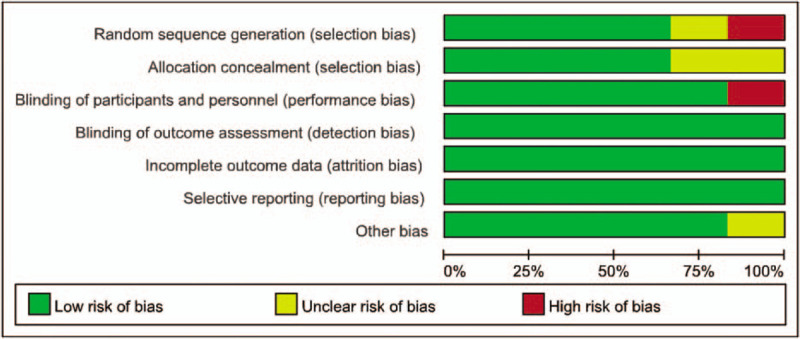
Risk of bias graph.
Figure 3.
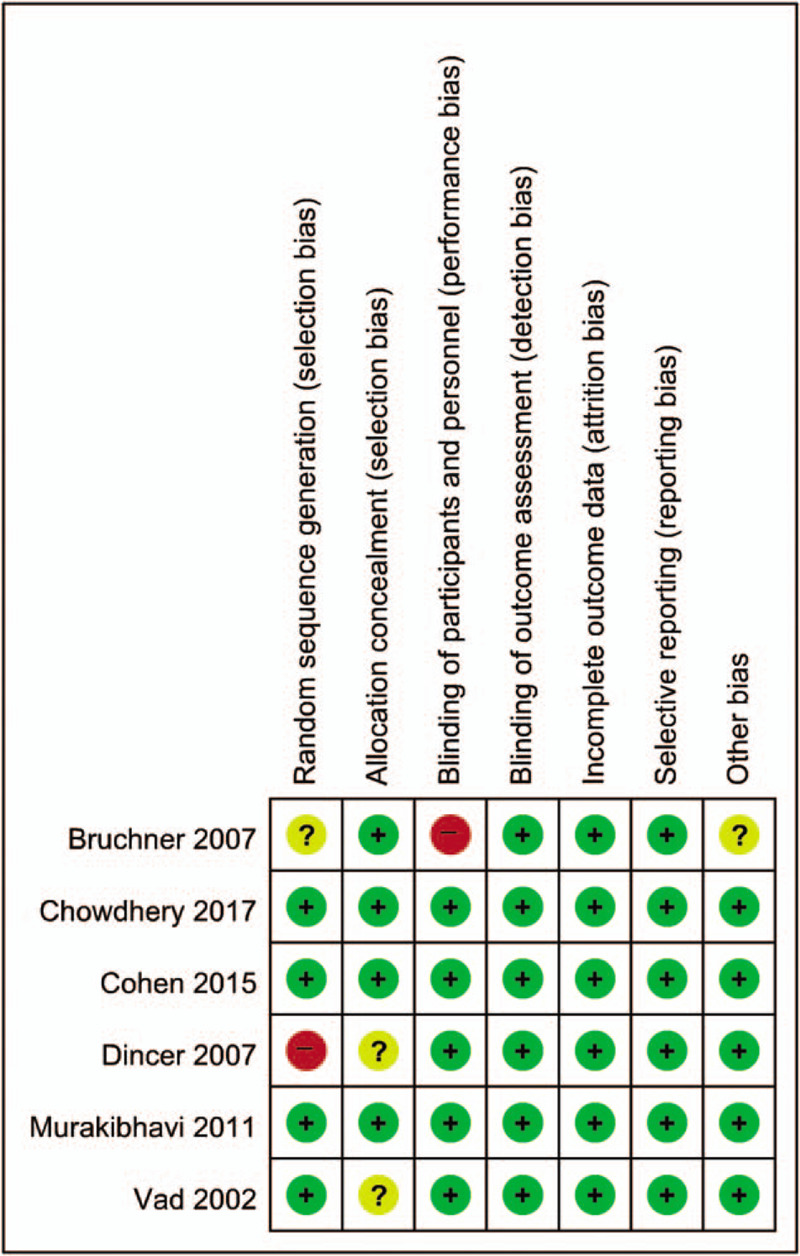
Risk of bias summary.
3.4. Primary outcomes
3.4.1. Pain relief
Five RCTs [10,22–25] reported data regarding post-injection follow-up pain scores and were included in the analysis of pain. One study [21] was excluded because the results for pain was not reported. Subgroup analyses were done according to the follow-up period. Outcomes were analyzed as short-term (≤1 month), intermediate-term (1 to 3 months) and long-term (6 months to ≤1 year) to show the duration of treatment effect regarding pain relief.
Three RCTs [10,22,24] documented pain scores at short-term follow-up. The pooled analysis of these studies showed that ESI patients showed a significant reduction in pain scores compared to conservative treatment (MD 1.24, 95% CI 0.58–1.91; P = .0002, Fig. 4). Patient's pain relief at intermediate-term follow-up was recorded in these same RCTs [10,22,24] and the results also demonstrated that ESI showed superior effect over conservative treatment (MD 0.87, 95% CI 0.48–1.26; P < .0001). There was no indication of statistical heterogeneity when data were pooled for intermediate-term follow-up (I2 = 0%, Fig. 4). Two RCTs [23,25] provided data regarding pain relief at long-term follow-up. The result of the meta-analysis, however, did not show that ESI was more effective than conservative treatment in reducing pain scores. The differences of pain relief in patients who received ESI or conservative treatment were not significant at long-term (MD 2.43, 95% CI 0.47–4.38; P = .02) and the studies showed significant heterogeneity (I2 = 87%, Fig. 5).
Figure 4.
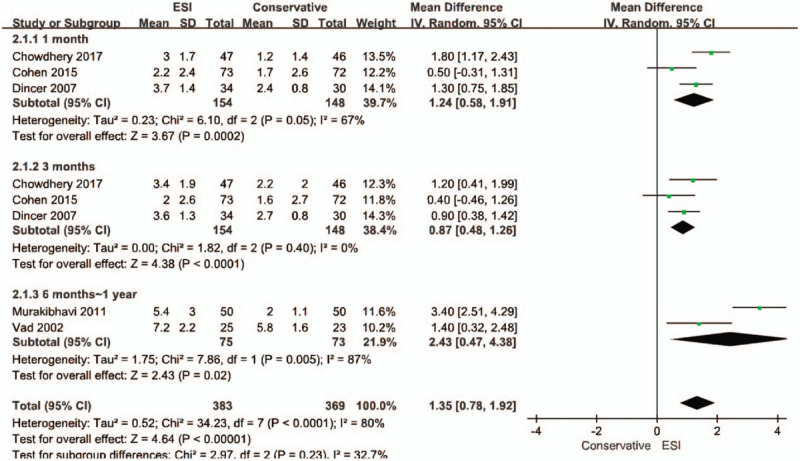
Forest plot of pain relief.
Figure 5.
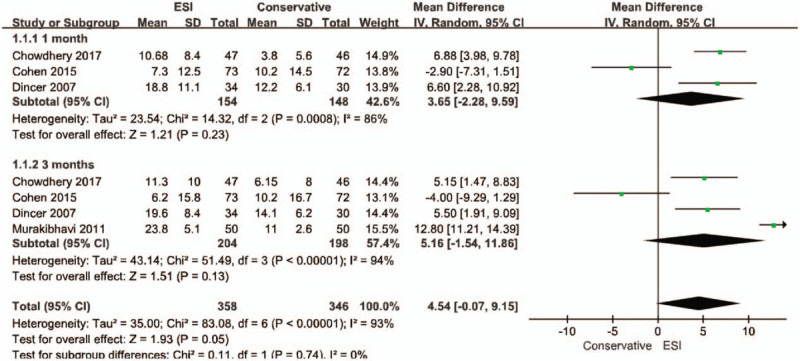
Forest plot of functional improvement.
3.4.2. Functional improvement
Four studies [10,22–24] measured functional level using the ODI score and were included in meta-analysis. Two studies [23,25] were excluded because the results for functional improvement were not reported. Functional improvement was analyzed according to follow-up period as short-term (1 to 3 months) and intermediate-term (3 to 6 months).
Three studies [10,22,24] reported functional score data at short-term follow-up. The result of meta-analysis showed that patients who received conservative treatment showed an equal effect compared to patients who received ESI (MD 3.65; 95% CI -2.28–9.59; P = .23). There was significant heterogeneity in these studies (I2 = 86%, Fig. 5).
Four studies [10,22–24] documented data on functional score regarding intermediate-term follow-up. The meta-analysis revealed that there were no significant differences among the groups (MD 5.16; 95% CI -1.54–11.86; P = .13) and significant heterogeneity was detected in these studies (I2 = 94%, Fig. 5).
3.4.3. Successful events
Data on successful events, as defined in the trial, were reported in 5 RCTs.[10,21,23–25] Successful events were defined mainly according to the reduction of pain among the studies. One study [22] was excluded because the result for successful event was not reported. In the study of Chowdhery et al[24] patients themselves rated perceived degree of overall improvement on a descriptive 4 item scale (recovery, marked improvement, slight improvement, or worse). Patients rating the improvement as “recovery” or “marked improvement” were considered as success. Cohen et al[10] defined a successful outcome as a decrease of ≥2 points in average leg pain score coupled with a positive global perceived effect. Murakibhavi et al[23] defined a successful event as when there was complete or partial pain relief with a VAS score reduction of more than 20%. Vad et al[25] defined a successful outcome as a patient satisfaction score of 2 (good) or 3 (very good), improvement on the Roland-Morris score of 5 or more, and pain reduction greater than 50% at least 1 year after treatment. Buchner et al[21] defined total success rate as when values were above 0 after Z transformation of the raw data of VAS, the straight leg raising test results, and functional status.
A meta-analysis was performed for successful events using the data of these 5 RCTs. A fixed-effect model of the pooled data showed that successful event rates were significantly higher in patients who received ESI than in those who received conservative treatment (relative risk 1.36; 95% CI 1.17–1.58; P < .0001). There was no indication of statistical heterogeneity in these 5 RCTs (I2 = 0%, Fig. 6).
Figure 6.
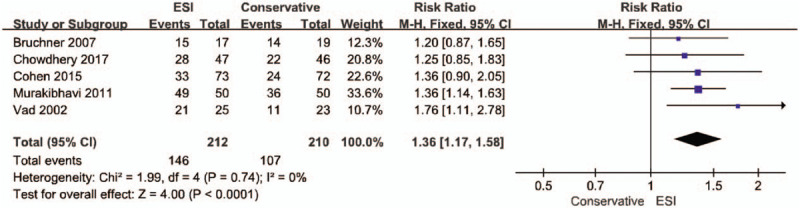
Forest plot of successful events.
4. Discussion
In the current study, we included 6 studies that evaluated the effectiveness of ESI for lumbosacral radicular pain caused by lumbar disc herniation or spinal stenosis in the meta-analysis. The results of the meta-analysis revealed that ESI was more beneficial than conservative treatment in relieving pain in the short-term (less than 1 month) and in the intermediate-term (1 to 3 months). However, there was no overall evidence that ESI was more effective than conservative treatment in improving lumbosacral radicular pain in the long-term (6 months to 1 year). In terms of functional improvement, the overall outcome of meta-analysis showed that ESI did not have any advantage over conservative treatment at short-term (1 to 3 months) and intermediate-term (3 to 6 months) follow-up. We also analyzed the data on successful events. Patients who received ESI reported more successful events that patients who received conservative treatment and the results were significant.
Previous systemic reviews including meta-analyses have investigated the efficacies of ESI [26,27] and conservative treatment [5,6] for patients with lumbosacral radicular pain. Some studies have attempted to compare the effects of surgery versus conservative treatment.[28,29] However, no meta-analysis has directly compared the efficacies of ESI and conservative treatment. A main strength of this study is that this is the first meta-analysis of RCTs to report the comparative efficacy of ESI and conservative treatment for lumbosacral radicular pain. Initial conservative treatment is generally recommended for patients with lumbosacral radicular pain and ESIs are being suggested as a reasonable treatment option for these patients. At present, there is limited evidence regarding the superiority of ESIs compared with conservative treatment for lumbosacral radicular pain. Meta-analysis is efficient to present a combined result on the efficacy of ESIs compared with conservative treatment than to describe the results of each individual RCT. Hence, we focused on investigating which type of treatment is superior to another for the treatment of lumbosacral radicular pain via meta-analysis. To enhance the validity of the current results, this meta-analysis was restricted to RCTs which directly compared ESI and conservative treatment. Patients in included studies had mean pain scores of more than 4 out of 10, which indicated that their pain intensity was more than moderate. Rather than focusing on the efficacy of the individual therapeutic agents, ESI and conservative treatment were compared to investigate the efficacies of the methods themselves.
Compared to previous systemic reviews [30–33] which showed that ESI was associated with greater reduction in pain than placebo or local anesthetic injections, the results of our meta-analysis are in agreement that ESI provided more analgesic benefit than conservative treatment at short-term. Regarding physical disability as measured by the ODI score, both ESI and conservative treatment showed similar effect on functional improvement after the interventions. This is in agreement with the previous study of Bhatia et al[30] which suggested that ESI did not reduce physical disability more than local anesthetic injection. The authors hypothesized that ODI may be better at detecting changes in more seriously disabled patients.
As for the mechanism of ESI on pain reduction, some possible proposals were suggested. Steroids have an analgesic effect through reducing the inflammation of the nerve root, blocking afferent C fiber nociception, and inhibiting pro-inflammatory mediators and phospholipase A2 activity.[20,34] In addition, the injection may break down the adhesions and scars and compress neural tissue.[35] Local injection of steroid may provide more benefit by yielding higher local concentrations than oral dosing,[22] but it seems that such effect of steroid does not last for a long period of time.
There are some limitations which should be noted regarding this study. First, the effects of 2 interventions were assessed over a wide range of time periods. To simplify this variation, time periods were divided into 3 intervals: short-term, intermediate-term, and long-term. Second, accurate direct comparison of interventions was not possible, due to the variation in types of interventions, such as the types of conservative treatment included (eg, pharmacologic or physical therapy) or doses of steroids. There were various components of conservative treatment in most studies and these consisted of several sessions with different modalities. Also, detailed prescriptions of analgesics (eg, number of pills needed) and rehabilitation programs were not thoroughly reported. Third, conservative treatment could not be compared with two different procedures of ESI. Considering that transforminal ESI has been shown to be more beneficial in short-term pain relief than interlaminar ESI, comparison of conservative treatment with ESI according to two different procedures may be needed in the future. Lastly, the number of RCTs included in this meta-analysis was small, and most trials involved short follow-up duration. If the number of samples included in the trials had been larger and the follow-up period had been longer, the results could have provided more valuable information for future clinical practice. It is also important to note that significant heterogeneity exists in the current meta-analysis. Caution must be taken when interpreting the results of this meta-analysis, considering the existing heterogeneity among the studies and the above limitations.
5. Conclusion
According to the results of our meta-analysis, the use of ESI is more effective for alleviating lumbosacral radicular pain than conservative treatments in terms of short-term and intermediate-term. However, this effect was not maintained in long term follow-up and there were no differences in functional improvement.
Acknowledgments
We would like to thank the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2017R1A2B2005321), for help with language editing of the manuscript.
Author contributions
SY and KHC conceived the study and its design; SY, WK, HHK, and KHD collected the data; SY, WK, HHK, and KHD managed, analyzed, and interpreted the data. All authors have read and approved the final manuscript. This manuscript has not been published or presented elsewhere in part or in entirety and is not under consideration by another journal.
Conceptualization: Seoyon Yang, Kyoung Hyo Choi.
Data curation: Seoyon Yang, Won Kim, Hyun Ho Kong, Kyung Hee Do, Kyoung Hyo Choi.
Formal analysis: Seoyon Yang.
Funding acquisition: Seoyon Yang.
Investigation: Kyung Hee Do.
Methodology: Seoyon Yang, Won Kim, Hyun Ho Kong, Kyung Hee Do.
Project administration: Seoyon Yang.
Software: Seoyon Yang.
Supervision: Won Kim, Hyun Ho Kong.
Validation: Seoyon Yang, Hyun Ho Kong.
Visualization: Seoyon Yang.
Writing – original draft: Seoyon Yang.
Writing – review and editing: Kyoung Hyo Choi, Won Kim, Seoyon Yang.
Supplementary Material
Footnotes
Abbreviations: CI = confidence interval, ESI = epidural steroid injection, LBP = low back pain, MD = mean difference, NRS = numeric rating scale, ODI = Oswestry disability index, RCT = randomized controlled trial, VAS = visual analog scale.
How to cite this article: Yang S, Kim W, Kong HH, Do KH, Choi KH. Epidural steroid injection versus conservative treatment for patients with lumbosacral radicular pain: a meta-analysis of randomized controlled trials. Medicine. 2020;99:30(e21283).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
All data generated or analyzed during this study are included in this published article [and its supplementary information files].
References
- [1].Tarulli AW, Raynor EM. Lumbosacral radiculopathy. Neurol Clin 2007;25:387–405. [DOI] [PubMed] [Google Scholar]
- [2].Ng L, Chaudhary N, Sell P. The efficacy of corticosteroids in periradicular infiltration for chronic radicular pain: a randomized, double-blind, controlled trial. Spine (Phila Pa 1976) 2005;30:857–62. [DOI] [PubMed] [Google Scholar]
- [3].Cooper G, Lutz GE, Boachie-Adjei O, et al. Effectiveness of transforaminal epidural steroid injections in patients with degenerative lumbar scoliotic stenosis and radiculopathy. Pain Physician 2004;7:311–7. [PubMed] [Google Scholar]
- [4].Manchikanti L, Falco FJ, Singh V, et al. Utilization of interventional techniques in managing chronic pain in the Medicare population: analysis of growth patterns from 2000 to 2011. Pain Physician 2012;15:E969–982. [PubMed] [Google Scholar]
- [5].Luijsterburg PA, Verhagen AP, Ostelo RW, et al. Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Eur Spine J 2007;16:881–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Vroomen PC, de Krom MC, Slofstra PD, et al. Conservative treatment of sciatica: a systematic review. J Spinal Disord 2000;13:463–9. [DOI] [PubMed] [Google Scholar]
- [7].Bicket MC, Horowitz JM, Benzon HT, et al. Epidural injections in prevention of surgery for spinal pain: systematic review and meta-analysis of randomized controlled trials. Spine J 2015;15:348–62. [DOI] [PubMed] [Google Scholar]
- [8].Wei G, Liang J, Chen B, et al. Comparison of transforaminal verse interlaminar epidural steroid injection in low back pain with lumbosacral radicular pain: a meta-analysis of the literature. Int Orthop 2016;40:2533–45. [DOI] [PubMed] [Google Scholar]
- [9].Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Cohen SP, Hanling S, Bicket MC, et al. Epidural steroid injections compared with gabapentin for lumbosacral radicular pain: multicenter randomized double blind comparative efficacy study. BMJ 2015;350:h1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Song F, Eastwood AJ, Gilbody S, et al. Publication and related biases. Health Technol Assess 2000;4:1–15. [PubMed] [Google Scholar]
- [13].Buttermann GR. Lumbar disc herniation regression after successful epidural steroid injection. J Spinal Disord Tech 2002;15:469–76. [DOI] [PubMed] [Google Scholar]
- [14].Peterson CK, Leemann S, Lechmann M, et al. Symptomatic magnetic resonance imaging-confirmed lumbar disk herniation patients: a comparative effectiveness prospective observational study of 2 age- and sex-matched cohorts treated with either high-velocity, low-amplitude spinal manipulative therapy or imaging-guided lumbar nerve root injections. J Manipulative Physiol Ther 2013;36:218–25. [DOI] [PubMed] [Google Scholar]
- [15].Kader D, Radha S, Smith F, et al. Evaluation of perifacet injections and paraspinal muscle rehabilitation in treatment of low back pain. A randomised controlled trial. Ortop Traumatol Rehabil 2012;14:251–9. [DOI] [PubMed] [Google Scholar]
- [16].Bronfort G, Evans RL, Anderson AV, et al. Nonoperative treatments for sciatica: a pilot study for a randomized clinical trial. J Manipulative Physiol Ther 2000;23:536–44. [DOI] [PubMed] [Google Scholar]
- [17].Bronfort G, Evans RL, Maiers M, et al. Spinal manipulation, epidural injections, and self-care for sciatica: a pilot study for a randomized clinical trial. J Manipulative Physiol Ther 2004;27:503–8. [DOI] [PubMed] [Google Scholar]
- [18].Koc Z, Ozcakir S, Sivrioglu K, et al. Effectiveness of physical therapy and epidural steroid injections in lumbar spinal stenosis. Spine (Phila Pa 1976) 2009;34:985–9. [DOI] [PubMed] [Google Scholar]
- [19].Zambello A, Fara B, Tabaracci G, et al. Epidural steroid injection vs paravertebral O2O3 infiltration for symptomatic herniated disc refractory to conventional treatment: a prospective randomized study. Rivista Italiana di Ossigeno-Ozonoterapia 2006;5:123–7. [Google Scholar]
- [20].Laiq N, Khan MN, Iqbal MJ, et al. Comparison of epidural steroid injections with conservative management in patients with lumbar radiculopathy. J Coll Physicians Surg Pak 2009;19:539–43. [PubMed] [Google Scholar]
- [21].Buchner M, Zeifang F, Brocai DR, et al. Epidural corticosteroid injection in the conservative management of sciatica. Clin Orthop Relat Res 2000;149–56. [DOI] [PubMed] [Google Scholar]
- [22].Dincer U, Kiralp MZ, Cakar E, et al. Caudal epidural injection versus non-steroidal anti-inflammatory drugs in the treatment of low back pain accompanied with radicular pain. Joint Bone Spine 2007;74:467–71. [DOI] [PubMed] [Google Scholar]
- [23].Murakibhavi VG, Khemka AG. Caudal epidural steroid injection: a randomized controlled trial. Evid Based Spine Care J 2011;2:19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Nandi J, Chowdhery A. A Randomized controlled clinical trial to determine the effectiveness of caudal epidural steroid injection in Lumbosacral Sciatica. J Clin Diagn Res 2017;11:Rc04–rc08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Vad VB, Bhat AL, Lutz GE, et al. Transforaminal epidural steroid injections in lumbosacral radiculopathy: a prospective randomized study. Spine (Phila Pa 1976) 2002;27:11–6. [DOI] [PubMed] [Google Scholar]
- [26].Abdi S, Datta S, Trescot AM, et al. Epidural steroids in the management of chronic spinal pain: a systematic review. Pain Physician 2007;10:185–212. [PubMed] [Google Scholar]
- [27].Boswell MV, Hansen HC, Trescot AM, et al. Epidural steroids in the management of chronic spinal pain and radiculopathy. Pain Physician 2003;6:319–34. [PubMed] [Google Scholar]
- [28].Fernandez M, Ferreira ML, Refshauge KM, et al. Surgery or physical activity in the management of sciatica: a systematic review and meta-analysis. Eur Spine J 2015;25:3495–512. [DOI] [PubMed] [Google Scholar]
- [29].Jacobs WC, van Tulder M, Arts M, et al. Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. Eur Spine J 2011;20:513–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Bhatia A, Flamer D, Shah PS, et al. Transforaminal epidural steroid injections for treating lumbosacral radicular pain from herniated intervertebral discs: a systematic review and meta-analysis. Anesth Analg 2016;122:857–70. [DOI] [PubMed] [Google Scholar]
- [31].Chou R, Hashimoto R, Friedly J. Epidural corticosteroid injections for radiculopathy and spinal stenosis. Ann Intern Med 2016;164:635–6. [DOI] [PubMed] [Google Scholar]
- [32].Pinto RZ, Maher CG, Ferreira ML, et al. Epidural corticosteroid injections in the management of sciatica: a systematic review and meta-analysis. Ann Intern Med 2012;157:865–77. [DOI] [PubMed] [Google Scholar]
- [33].Quraishi NA. Transforaminal injection of corticosteroids for lumbar radiculopathy: systematic review and meta-analysis. Eur Spine J 2012;21:214–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Ozawa K, Atsuta Y, Kato T. Chronic effects of the nucleus pulposus applied to nerve roots on ectopic firing and conduction velocity. Spine (Phila Pa 1976) 2001;26:2661–5. [DOI] [PubMed] [Google Scholar]
- [35].Kim KM, Kim HS, Choi KH, et al. Cephalic spreading levels after volumetric caudal epidural injections in chronic low back pain. J Korean Med Sci 2001;16:193–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


