Abstract
Background:
To compare clinical effect between Er: YAG and CO2 laser in treatment of oral tumorous lesions.
Methods:
A comprehensive search was conducted from 2000 to 2019. The quality assessment was performed by the QUADAS-2 tool (The Cochrane Collaboration, 2011). The clinical value of comparison between Er: YAG and CO2 laser was evaluated by using the pooled estimate of sensitivity and specificity. In addition, sensitivity analysis and bias analysis were applied to ensure the accuracy of the results.
Results:
Finally, 268 patients were enrolled in 6 studies and ultimately met the eligibility criteria. The Er: YAG and CO2 groups were 141 and 127, respectively. The meta-analysis showed significant difference in success (risk ratio = 21.29, 95% confidence interval [1.09, 1.52], P = .002; P for Heterogeneity = .99, I2 = 0%) and time of surgery ((P of heterogeneity = .29, I2 = 20%, Z = 25.69, P of over effect < .00001). The recurrence and complications of CO2
and Er: YAG groups had no difference.
Conclusion:
Er: YAG laser had better effects than CO2 laser in eliminating oral tumorous lesions while it needed longer operation time than CO2 laser.
Keywords: CO2, Er: YAG, meta, oral tumorous lesions
1. Introduction
Oral leukoplakia is one of the precancerous lesions identified by WHO. Common therapies include drugs, excision, freezing, and laser. Laser mainly uses its photothermal effect in treating oral tumor.[1,2] When the laser irradiates the biological tissue, it is absorbed by the water of the tissue and converted into heat energy, thereby heating, and cutting the tissue.[3,4]
The Er: YAG laser has a wavelength of 2940 nm and is a mid-infrared laser. It is consistent with the highest absorption peak of water and can be highly absorbed by water and hydroxyapatite, which produce a corresponding photothermal effect.[5–7]
CO2 laser in treating mucosal leukoplakia mainly uses the thermal effect of laser. When a certain energy CO2 laser irradiates the biological tissue, the tissue absorbs the energy of the laser and converts the light energy into heat energy.[8–10] When the heat energy increases faster than the biological tissue, the biological tissue rises rapidly and reaches hundreds of degrees, which can cause protein to coagulate and necrosis.[11,12]
The aim of this meta-analysis was to compare the role of Er: YAG and CO2 lasers in patients with oral tumorous lesions. To address these concerns, we performed a meta-analysis that examine the difference between Er: YAG and CO2 lasers for patient with oral tumorous lesions.
2. Methods
This study was a meta-analysis. No approval of ethics committee or institutional review board was needed, and all data were available online.
2.1. Literature search strategy
Multiple electronic databases including PubMed, Springer, EMBASE, OVID, and Cochrane databases were searched from January 2000 to September 2019 using combinations of the following key terms: Er: YAG, CO2, oral and tumorous lesions. There is no restriction about the publication language. The studies were initially reviewed by titles and abstracts. The reference lists of the included studies were also examined.
2.2. Study selection
Studies were included if:
-
(a)
They were considered as randomized trials or case-control studies.
-
(b)
They analyzed the Er: YAG and CO2 lasers for oral tumorous lesions.
-
(c)
The details about Er: YAG and CO2 lasers was reported.
Studies were excluded if:
-
(a)
They were case studies/meta-analyses/letter to editors.
-
(b)
Patients without oral tumorous lesions.
-
(c)
Data in research is limited or insufficient.
-
(d)
They were duplicates.
2.3. Data extraction and quality assessment
The full texts of the articles were read carefully and extracted the characteristics from each study using a predetermined form. The data extracted from these studies included the first author's name, year of publication, country, age, sample size (Er: YAG/CO2).
2.4. Statistical analysis
Effect sizes for numerical variables were expressed as difference in means with 95% confidence interval (CI); while that of categorical data were expressed as risk ratio (RR) with 95% CI. We tested for heterogeneity between-study with the I2 measure. Percentages of around 25% (I2 = 25), 50% (I2 = 50), and 75% (I2 = 75) were considered at low, moderate, and high heterogeneity, respectively.
A X2 based Q-test was also performed to check between-study heterogeneity. When an I2 value higher than 50 indicated moderate heterogeneity between the studies the effect size for each study was calculated by the random effect model DerSimonian–Laird approach. Publication bias was evaluated and quantified by the funnel plot, Egger and Begger tests. With regard to outcomes when significant heterogeneity existed across studies, sensitivity analysis was performed by sequentially omitting each study to test the influence of each individual study on pooled data. Most analyses were performed using Review Manager 5.2 (The Cochrane Collaboration, 2011).
3. Results
3.1. Search process
Electronic search ended with a total number of 915 articles. After a thorough reading, 78 papers met the preliminary criteria. In the further screening, 72 articles were excluded because the design of the study, insufficient data, and type of the articles. Finally, 6 papers were selected for analysis. Figure 1 is a flowchart of identification, inclusion, and exclusion, reflecting the search process and the reasons for exclusion.
Figure 1.

Flow diagram of the study selection.
3.2. Characteristics of included studies
Detailed characteristics of the included studies were presented in Table 1. All these studies were published from 2000 to 2019. The sample size ranged from 24 to 75. Totally 141 patients were in Er: YAG group, and 127 patients were in CO2 group.
Table 1.
Characteristics of studies included in the meta-analysis.

3.3. Results of quality assessment
The quality of the studies was assessed through the risk of bias table in the Review Manager 5.2 Tutorial, and Figures 2 and 3 showed the evaluation in this study. As the obvious differences of operative procedure between fertile and infertile, limited risk was observed.
Figure 2.

Assessment of the quality of the included studies: low risk of bias (green hexagons), unclear risk of bias (yellow hexagons), and high risk of bias (red hexagons).
Figure 3.

Quality assessment of included studies.
3.4. Results of heterogeneity test
3.4.1. Meta-analysis about success of oral tumorous lesions
Six included studies involve in success treatment, which means elimination of oral tumor focus. The forest plot for the success between Er: YAG group and CO2 group was shown in Figure 4. The combined result suggested that there was significant difference of success between Er: YAG group and CO2 group, and Er: YAG group had higher success than CO2 group (RR = 21.29, 95%CI [1.09, 1.52], P = .002; P for Heterogeneity = .99, I2 = 0%).
Figure 4.
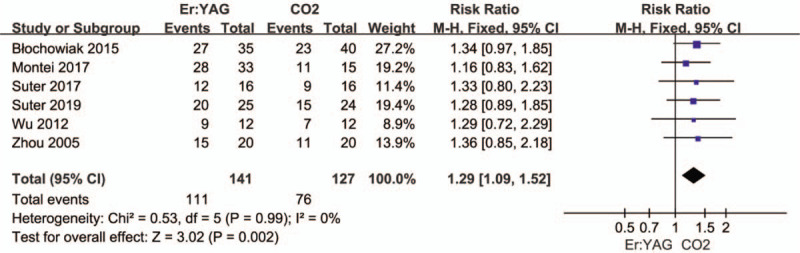
Forest plots of success between Er: YAG group and CO2 group.
3.4.2. Meta-analysis about recurrence of oral tumorous lesions
Five included studies were involved in recurrence of oral tumorous lesions between Er: YAG group and CO2 group. As shown in the forest plot (Fig. 5). The result of meta-analysis showed that there was no significant difference o (RR = 0.70, 95%CI [0.39, 1.25], P = .22; P for Heterogeneity = 1.00, I2 = 0%).
Figure 5.

Forest plots of recurrence of oral tumorous lesions between Er: YAG group and CO2 group.
3.4.3. Meta-analysis about time of surgery(s)
In the analysis, 4 articles were included. The results of heterogeneity test showed that fixed effect model wad was needed to analyze the data (P of heterogeneity = .29, I2 = 20%, Z = 25.69, P of over effect < .00001). The overall effect of time of surgery was significant and the overall mean difference was 57.48, which showed that Er: YAG group had longer time of surgery than CO2 group (Fig. 6).
Figure 6.

Forest plots of time of surgery between Er: YAG group and CO2 group.
3.4.4. Meta-analysis about complications
In the analysis of complications, 4 articles were included. The results of heterogeneity test showed that fixed effect model wad was needed to analyze the data (RR = 1.58, 95%CI [0.54, 4.63], P of heterogeneity = .72, I2 = 0%, Z = 0.84, P of over effect = .40). The overall effect of complications was not significant (Fig. 7).
Figure 7.

Forest plots of complications between Er: YAG group and CO2 group.
3.5. Results of sensitivity analysis and publication bias
According to meta-analysis, the heterogeneity of success was low (I2 = 0%). As shown in Figure 7 the heterogeneity of the success might be attributed to the different results of each study. When the article of Suter in 2019 was excluded, I2 remained unchanged while P of overall effect changed from 0.002 to 0.007 (Fig. 8). This indicated that the result in this article was robust.
Figure 8.

Sensitivity analysis forest plots of success between Er: YAG group and CO2 group.
A funnel plot for success between Er: YAG group and CO2 group groups was performed. All the 6 studies were included in the plot. To some extent, the result indicated that there existed limited publication bias since the symmetrical characteristic of the funnel plot is good (Fig. 9).
Figure 9.

Funnel plot of publication bias.
4. Discussion
The leukoplakia is often accompanied by mild, moderate, and severe dysplasia, which is prone to cancer. The most active treatment is surgical resection, but it is not easy to be promoted in primary hospitals due to difficulties in repairing and skin grafting of mucosal defects after resection.[19,20] The laser has a thermal effect, a pressure effect and an electromagnetic effect to cut the diseased tissue, which can seal the small blood vessel so that the intraoperative blood loss is small.[21,22] The laser can block the peripheral nerves at the wound and have less pain in the child. The laser is operated at high temperatures to disinfect and sterilize, reducing the chance of infection.
CO2 laser treatment of oral leukoplakia is easy to conduct, and oral tumor can be layered cauterized and gasified, until no white spot tissue remains. The Er: YAG laser emits laser light in a short pulse mode, and the short-pulse laser intensity can reach 1000 W or higher.[23,24] These high-intensity, high-absorption lasers are suitable for removing diseased tissues. The Er: YAG laser has a high sterilizing ability even when the output energy is low, and the temperature will not rise excessively. At the same time, the Er: YAG laser can split water molecules and produce OH-free radicals. A large number of oxygen free radicals also have certain bactericidal effects.[25,26]
All studies included have shown that Er: YAG group was better than CO2 group in success treatment of oral tumorous lesions. This study shows the consistent result with previous reports.[2,4] In time of surgery, Er: YAG group had longer surgery time than CO2 group. This is consistent with Almehdi's research[25] that Er: YAG laser had longer surgery time than CO2 laser, CO2 lasers is fast and easy to use, at same time, Er: YAG laser has better effects than CO2 laser in eliminating oral cancer, while it needs more operation time than CO2 laser.
In the analysis of recurrence, Er: YAG group and CO2 group had no difference. Meanwhile, the complications in Er: YAG group and CO2 group had no difference either. These results were similar with Choi's report that Er: YAG and CO2 lasers had no difference in recurrence and complications rate.[26]
In conclusion, the results showed that Er: YAG laser need more operation time than CO2 laser, while Er: YAG laser was better than CO2 laser in eliminating oral tumor. However, some limitations existed in this article. Firstly, the comparison in different age areas was not considered, which could be evaluated in the further research. Secondly, the details about complications were not included, and details could be evaluated in the future.
Author contributions
RL, KJS and HM conceived and designed the study. RL, KJS, YDW, YXJ and JYK collected and analyzed the data and RL and KJS wrote the paper. HM reviewed and edited the manuscript. All authors read and approved the manuscript.
Footnotes
Abbreviations: CI = confidence interval, RR = risk ratio.
How to cite this article: Liu R, Sun K, Wang Y, Jiang Y, Kang J, Ma H. Clinical comparison between Er: YAG and CO2 laser in treatment of oral tumorous lesions: a meta-analysis. Medicine. 2020;99:30(e20942).
RL and KS are co-first authors and contributed equally to this work.
The authors have no funding and conflicts of interest to disclose.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- [1].Zaffe D, Vitale MC, Martignone A, et al. Morphological, histochemical, and immunocytochemical study of CO2 and Er: YAG laser effect on oral soft tissues. Photomed Laser Surg 2004;22:185–90. [DOI] [PubMed] [Google Scholar]
- [2].Schwarz F, Maraki D, Yalcinkaya S, et al. Cytologic and DNA-cytometric follow-up of oral leukoplakia after CO2- and Er: YAG-laser assisted ablation: a pilot study. Lasers Surg Med 2010;37:29–36. [DOI] [PubMed] [Google Scholar]
- [3].White JM, Chaudhry SI, Kudler JJ, et al. CO2 laser therapy of oral mucosal lesions. J Clin Laser Med Surg 1999;16:299–304. [DOI] [PubMed] [Google Scholar]
- [4].Kishore A, Kathariya R, Deshmukh V, et al. Effectiveness of Er: YAG and CO2 lasers in the management of gingival melanin hyperpigmentation. Oral Health Dent Manag 2014;13:486–91. [PubMed] [Google Scholar]
- [5].Błochowiak K, Andrysiak P, Sidorowicz K, et al. Selected applications of Er: YAG and CO2 lasers for treatment of benign neoplasms and tumorous lesions in the mouth. Postepy Dermatol Alergol 2015;5:337–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Yamada MK, Uo M, Ohkawa S, et al. CLSM and SEM quantitative analysis of surface topography of human teeth irradiated by Nd: YAG, Er: YAG and CO 2 lasers. Int Congr 2003;1248:135–7. [Google Scholar]
- [7].Hegde R, Padhye A, Sumanth S, et al. Comparison of surgical stripping; erbium-doped:yttrium, aluminum, and garnet laser; and carbon dioxide laser techniques for gingival depigmentation: a clinical and histologic study. J Periodontol 2013;84:738–48. [DOI] [PubMed] [Google Scholar]
- [8].Mcdaniel DH, Lord J, Ash K, et al. Combined CO2/Erbium: YAG laser resurfacing of peri-oral rhytides and side-by-side comparison with carbon dioxide laser alone 1. Dermatol Surg 1999;25:285–93. [DOI] [PubMed] [Google Scholar]
- [9].Hibst R. Clinical applications of the Er: YAG laser in cariology and oral surgery. Proc SPIE Int Soc Opt Eng 1995;1984:85–94. [Google Scholar]
- [10].Sabaeian M, Shahzadeh M. Simulation of temperature and thermally induced stress of human tooth under CO 2 pulsed laser beams using finite element method. Laser Med Sci 2015;30:645–51. [DOI] [PubMed] [Google Scholar]
- [11].Matsumoto, Koukichi. Laser treatment of hard tissue lesions. J Oral Laser Appl 2004;4:235–48. [Google Scholar]
- [12].Mercer CE, Anderson P, Davis GR. Sequential 3D X-ray microtomographic measurement of enamel and dentine ablation by an Er: YAG laser. Brit Dent J 2003;194:99–109. [DOI] [PubMed] [Google Scholar]
- [13].Błochowiak K, Andrysiak P, Sidorowicz K, et al. Selected applications of Er: YAG and CO2 lasers for treatment of benign neoplasms and tumorous lesions in the mouth. Postep Derm Alergol 2015;32:337–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Monteiro L, Barbieri C, Warnakulasuriya S, et al. Type of surgical treatment and recurrence of oral leukoplakia: A retrospective clinical study. Med Oral Patol Oral Cir Bucal 2017;22:e520–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Suter VGA, Altermatt HJ, Bornstein MM. A randomized controlled clinical and histopathological trial comparing excisional biopsies of oral fibrous hyperplasias using CO2 and Er: YAG laser. Laser Med Sci 2017;32:573–81. [DOI] [PubMed] [Google Scholar]
- [16].Suter VGA, Altermatt HJ, Bornstein MM. A randomized controlled trial comparing surgical excisional biopsies using CO2 laser, Er: YAG laser and scalpel. Int J Oral Max Surg 2019;49:99–106. [DOI] [PubMed] [Google Scholar]
- [17].Wu MZ, Huang H. Laser surgery for oral lymphangioma. Chin J Laser Med Surg 2002;11:111–5. [Google Scholar]
- [18].Zhou G, Zhang Z, Zhang C, et al. Clinical study on laser therapy of the venous malformations and hemangioma in oral and maxillofacial regions. Chin J Stomatol 2005;40:200–2. [PubMed] [Google Scholar]
- [19].Paul P, Duvvuri SNR, Alla RK, et al. Evaluation of shear bond strength of stainless steel brackets bonded to ceramic crowns etched with Er; Cr: YSGG laser and hydrofluoric acid: an in vitro study. Br J Med Med Res 2015;7:550–60. [Google Scholar]
- [20].Sader R. New developments in implantology: laser-and piezo-osteotomy. Int J Oral Maxillofac Surg 2009;38:411–23. [Google Scholar]
- [21].Kathariya R, Pradeep AR. Split mouth de-epithelization techniques for gingival depigmentation: a case series and review of literature. J Indian Soc Periodontol 2011;15:161–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hess CN, Lopes RD, Gibson CM, et al. Saphenous vein graft failure after coronary artery bypass surgery insights from prevent IV. Circulation 2013;257:824–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Punia V, Lath V, Khandelwal M, et al. The current status of laser applications in prosthodontics. Natl J Integr Res Med Title 2012;56:99–108. [Google Scholar]
- [24].Lukac M, Hocevar F, Cencic S, et al. Effects of pulsed CO2 and Er: YAG lasers on enamel and dentin. The International Society for Optical Engineering 1993;18:25–33. [Google Scholar]
- [25].Almehdi A, Aoki A, Ichinose S, et al. Histological and SEM analysis of root cementum following irradiation with Er: YAG and CO2 lasers. Laser Med Sci 2013;28:203–13. [DOI] [PubMed] [Google Scholar]
- [26].Choi Jae Eun, Oh Ga Na, Kim Jong Yeob, et al. Ablative fractional laser treatment for hypertrophic scars: comparison between Er:YAG and CO2 fractional lasers. J Dermatolog Treat 2014;25:299–303. [DOI] [PubMed] [Google Scholar]


