Abstract
Agoraphobia is frequently accompanied by panic disorder and causes considerable suffering. The aim of this study was to compare clinical features and treatment courses between patients with and without agoraphobia in panic disorder.
In this retrospective study, 87 patients with panic disorder were divided into two groups depending on the presence of agoraphobia: patients with agoraphobia (PDA, n = 41) and patients without agoraphobia (PD, n = 46). Agoraphobia subscale score of the Albany Panic and Phobia Questionnaire was used to identify correlations between agoraphobia and panic and affective symptoms.
The PDA group showed more severe panic and affective symptoms than the PD group. Patients with PDA were more likely to be younger at the age of onset, take benzodiazepines for longer durations, and be treated with antipsychotics augmentation. Agoraphobia subscale was associated with panic symptoms, depression, anxiety, and the duration of benzodiazepines use.
The findings suggest that patients with PDA experienced more severe panic symptoms, more profound psychiatric comorbidity, and worse illness progression than those with PD.
Keywords: agoraphobia, anxiety, depression, panic disorder
1. Introduction
Panic disorder is an anxiety disorder exhibited by repeated and sudden panic attacks which include palpitations, sweating, shortness of breath, chest discomfort, abdominal distress, dizziness, and fear of dying.[1] Patients with panic disorder suffer from psychiatric comorbidities such as depression, substance abuse, and suicide ideation.[2–4] Also, individuals in bereavement often show long-lasting psychological symptoms including panic attacks.[5,6] Panic disorder frequently occurs with agoraphobia,[7] which presents with fear and anxiety that caused by being in a place where it is difficult to get help or escape if a panic attack or similar symptom occurs.[1]
The relationship between agoraphobia and panic disorder remains not been clearly established. Regarding this issue, 2 hypotheses have been proposed. It has been suggested that agoraphobia is a subtype of panic disorder. Grant et al reported that panic disorder accompanied by agoraphobia could be a severe complication of panic disorder,[8] and agoraphobia was considered to result from recurrent panic attacks.[1] On the other hand, agoraphobia could be a distinct disease independent of panic disorder.[9,10] Recently, in the DSM-5, agoraphobia has been separated from panic disorder as an independent condition, based on the following findings. Agoraphobia could occur without panic symptoms,[11] is not always secondary to panic symptoms,[1,12] and there are differences in prevalence, sex specific incidence rate, and treatment outcome between agoraphobia and panic disorder.[11,13]
There are evidences that presence of agoraphobia in panic disorder patients carries significant clinical implications,[14–16] however, few comprehensive assessment has been reported how comorbid agoraphobic symptoms affects the patient with panic disorder in terms of symptoms severity, psychological comorbidity and clinical course. In this study, we aimed to compare the symptom severity of panic disorder, comorbid psychiatric symptoms and clinical course including medication between patients who have panic disorder with agoraphobia (PDA) and those with panic disorder alone (PD).
2. Methods
2.1. Study design and participants
The present study is a retrospective study, and the setting was a university-affiliated tertiary hospital. In total, 87 patients who had recently been diagnosed with panic disorder according to the DSM-IV-TR, between June 2014 and September 2018 were included in the study. They were divided into two groups based on the comorbidity of agoraphobia: PDA (n = 41) and PD (n = 46). Diagnosis of PDA was made for patients who responded “yes” to Item 4 of the Panic Disorder Severity Scale (PDSS) which reflects agoraphobic fear, and had agoraphobia subscale score (referred to as “agoraphobia score” in the present study) above 65 in the Albany Panic and Phobia Questionnaire (APPQ). This study was approved by the institutional review board (IRB) of Konkuk University Hospital, and written informed consent was waived by the IRB (approval number: KUH 1050107).
2.2. Measurements
Demographic data, the result of psychological tests, and the information on the treatment course were collected. Psychological tests included PDSS, APPQ, anxiety sensitivity index–revised (ASI-R), beck depression inventory (BDI), state-trait anxiety inventory (STAI), and Minnesota multiphasic personality inventory (MMPI).
The PDSS is a standard measurement scale for panic disorder.[12,17] The instrument includes 7 items associated with symptoms accompanied by panic disorder.[17,18] The Korean version of the PDSS, which proved out good test–retest reliability (r = 0.96) and inter-rater reliability (r = 0.88),[19] was used in the study. The APPQ is a scale designed to assess three types of fear related to panic disorder. The scale consisted of 27 items is categorized into 3 subscales:
-
1)
agoraphobia,
-
2)
social phobia,
-
3)
and interoceptive fear (i.e., fear of activities that cause painful bodily sensation).[20]
We used the Korean version of the APPQ, which was standardized by Kim et al and has demonstrated high levels of psychometric qualities.[19,21] The ASI-R is a self-reported questionnaire used to measure the degree of fear arising from believing that body sensations will produce dangerous consequences. The Korean version of the ASI-R has been validated and evidenced good test–retest reliability (r = 0.82) and internal consistency (α = 0.92).[19,22] The BDI is a self-report checklist for assessing the severity of depressive symptoms.[23] The 21 items include emotional, physiological, and cognitive symptoms of depression.[21] We used a Korean version of the BDI which has been considered valid and reliable tool.[19] The STAI is a 40-item self-report instrument to evaluate anxiety symptoms. The State Anxiety Scale measures the individual's current state of anxiety, and the Trait Anxiety Scale evaluates the individual's stable tendency toward anxiety.[24] We adopted the Korean version of the scale, which was translated by Kim et al and has demonstrated fine psychometric properties.[19,22] The MMPI is widely used in personality and psychopathology assessments of patients in clinical settings[25] and was revised and re-standardized in 1989.[26] The Korean version of the MMPI-2 was reported to be reliable in assessing personality and psychological symptoms in Korean adults.[26]
The treatment-related items included benzodiazepines (BZD) dose, duration of BZD use, total treatment duration, as-needed BZD use, number of antidepressants used, augmentation treatment with mood stabilizers or antipsychotics, and hospitalization. Doses of different classes of BZD were compared by the defined daily dose (DDD), which is the average maintenance dose per day for a drug used for its main indication and is an international standard quantitative unit.[27]
2.3. Statistical analysis
Mann-Whitney test was performed to compare continuous variables such as age, age of onset, years of education, scores for psychological scales, BZD dose, duration of BZD use, and total treatment duration. A chi-square test was used to compare categorical variables such as sex, employment status, as-needed BZD use, concomitant use of antipsychotics, and hospitalization between two groups. Augmentation with mood stabilizers was analyzed by Fisher exact test, and linear by linear association was used to identify the number of antidepressants prescribed concomitantly. The relationships between agoraphobia score and other psychological variables were exhibited using Spearman's rank correlation analysis. Statistical significance level was defined at P < .05.
3. Results
The mean age of PDA onset was 28.8 ± 11.7 years, whereas that of PD was 34.9 ± 13.0 years (P = .016). In addition, there was a significant difference in age at hospital visit (31.4 ± 11.4 years vs 37.2 ± 13.2 years, P = .018) between two groups. However, patients with PDA did not differ significantly from those with PD in sex, employment status, and years of education.
The PDA group's total PDSS score was significantly higher than those of the PD group (17.1 ± 5.3 vs 12.8 ± 5.5, P < .001). In addition, the agoraphobia score of the APPQ was higher in the PDA compared to that of PD patients (78.1 ± 8.1 vs 49.6 ± 8.6). Furthermore, the ASI-R score was significantly higher in PDA (82.6 ± 9.7 vs 65.7 ± 14.4, P < .001). Moreover, the PDA group showed higher levels of depressive symptoms measured by the BDI (36.3 ± 12.0 vs 22.0 ± 13.1), and anxiety symptoms measured by the STAI than the PD group (Table 1). Regarding the MMPI profiles, all of the clinical scales other than the masculinity-feminity and hypomania scales revealed statistically higher values in the PDA compared to the PD group (Fig. 1). Among the clinical scales, depression and psychasthenia were particularly higher in PDA patients (scores were over 70, P < .001).
Table 1.
Comparison between patients with and without agoraphobia in panic disorder: clinical and demographic variables.
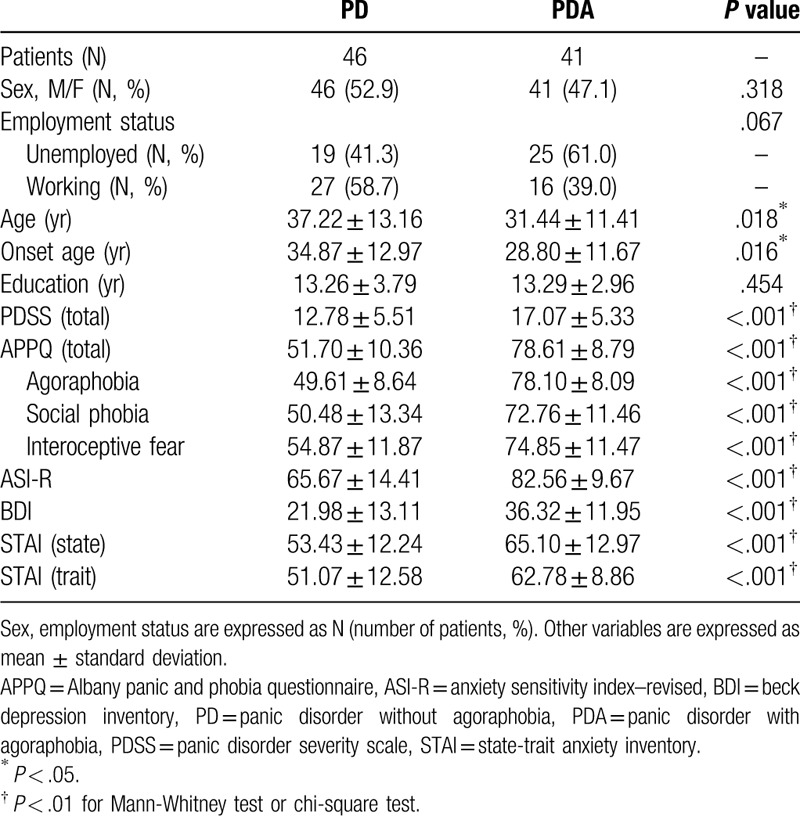
Figure 1.
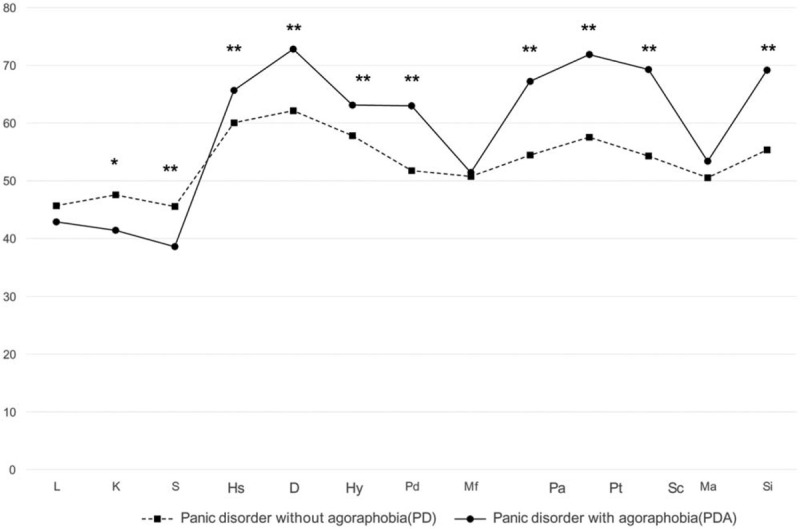
MMPI clinical scales of patients with and without agoraphobia in panic disorder. ∗P < .05, †P < .01.
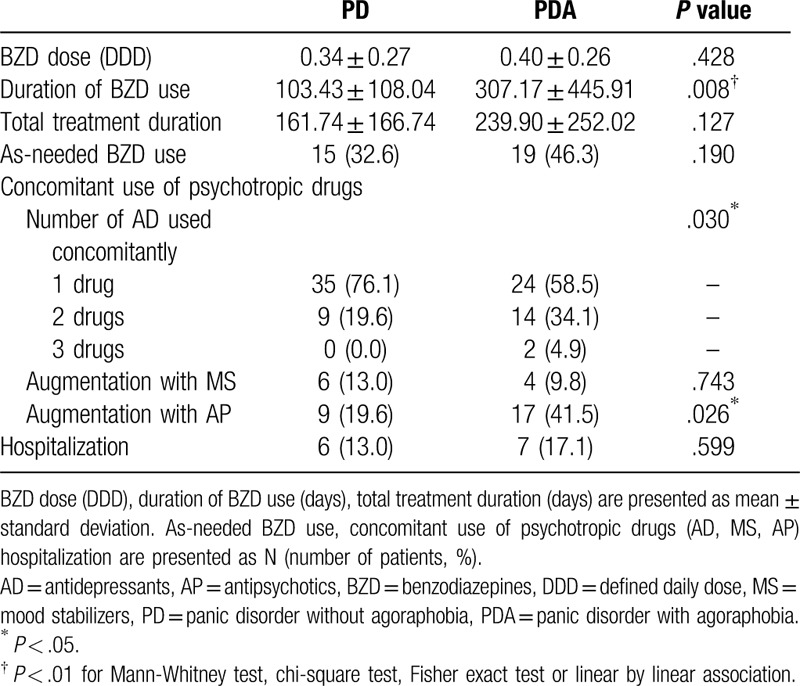
The duration of BZD use in the PDA was longer than that observed in the PD group (307.2 ± 445.9 days vs 103.4 ± 108.0 days, P = .008). In addition, the PDA was more likely to be prescribed two antidepressants concomitantly than the PD patients (34.1% vs 19.6%, P = .030). Moreover, 4.9% of participants in the PDA had been prescribed more than three antidepressants, whereas it had not occurred to any of those in the PD group. The proportion of patients who had antipsychotics augmentation therapy was also significantly higher in PDA (41.5% vs 19.6%, P = .026). However, total treatment duration and BZD doses did not differ significantly between the two groups. There was no statistically significant difference in the proportions of patients who were hospitalized, doses of as-needed BZD, and the percentage of patients who had received mood stabilizer augmentation therapy between the two groups also (Table 2).
Table 2.
Comparison between patients with and without agoraphobia in panic disorder: treatment course.
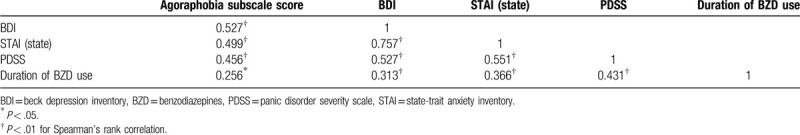
The results of correlation analysis between agoraphobia score and psychological scale scores and treatment course-related items were shown in Table 3. BDI (rs = 0.527, P < .001), STAI-state (rs = 0.499, P < .001), PDSS (rs = 0.456, P < .001) scores and the duration of BZD use (rs = 0.256, P = .017) indicated significantly positive correlation with agoraphobia score.
Table 3.
Correlation between the agoraphobia subscale score and panic-related variables.
4. Discussion
The object of this study was to compare demographic characteristics, severity of symptoms, comorbid symptoms and treatment courses between patients with and without agoraphobia in panic disorder. Patients with PDA showed younger age of onset, more severe panic symptoms, and higher level of affective symptoms including depression than those with PD. In addition, the PDA group were more likely to receive combination and augmentation pharmacological treatment and BZD for longer duration compared to the PD group. Moreover, the PDA's agoraphobia and total PDSS scores were higher than those of the PD group, which indicates that the PDA patients experienced more severe panic symptoms than the PD patients.
In this study, PDSS score was positively associated with agoraphobic score in APPQ. Previous studies also showed that agoraphobia was related to the severity of panic attacks, distress and poor functional outcome, and the findings suggested that agoraphobia could be a marker of severely aggravated panic disorder.[13,28] To our best knowledge, we firstly report that the severity of agoraphobic symptom is statistically correlated with the severity of panic symptom, which indicates that panic and agoraphobic symptoms are strongly associated. However, the causal relationship between the two symptoms remains not clearly known. There have been contradictory results about the temporal relationship between panic symptoms and agoraphobia. According to Garvey, agoraphobic avoidance usually started within a few months after first panic attack.[12,29] Clum et al also suggested that panic attacks was followed by agoraphobia.[30] On the contrary, some studies have shown that panic disorder was aggravated by agoraphobia.[28,31] In the present study, we could not examine the temporal relationship between panic attack and agoraphobic symptoms, therefore it is difficult to draw a conclusion on this issue.
In the current study, the PDA patients were more depressed and it was proved by higher BDI score, depression and social introversion MMPI scale scores compared to those of the PD patients. There have been several previous studies have examined the links between panic disorder, agoraphobia, and depression. Panic disorder patients with agoraphobia are likely to experience greater limitations in their work or social lives compared to those with PD alone, and this could cause depression.[1,15] Clum et al also suggested that patients with PDA in the state of loss of control showed “learned helplessness”, because they believed that there were no useful coping strategies.[30] Choi et al reported that PDA patients displayed greater self-criticism and fatalism than those with PD alone.[32] In addition, we found that patients with PDA had more severe anxiety, even when they were not experiencing a panic attack, and exhibited higher STAI score, ASI-R score and psychasthenia MMPI scale than patients with PD. According to Ken et al, panic disorder patients with high anxiety sensitivity and trait anxiety were more likely to detect agoraphobic fear rapidly.[28] Regarding anxiety sensitivity, Chambless found that the severity of fear of bodily sensation increases when panic disorder was accompanied by agoraphobia.[33] Anxiety sensitivity may contribute to trigger panic attacks and could directly amplify agoraphobia and enhance avoidance in patients with PD.[10,34] Few studies have compared MMPI in panic disorder patients with and without agoraphobia. One study revealed that PDA patients’ psychasthenia score was higher than those with PD,[35] which is consistent with the current findings. Overall, patients with PDA are prone to more affective symptoms compared to patients with PD.
The onset of disease was earlier in patients with PDA than PD in our study, and this finding is consistent with previous studies.[12,15,30] Panic disorder patients with more earlier onset have a higher genetic tendency and are more likely to experience agoraphobia and other comorbidities compared to those with late disease onset.[36] Moreover, greater familial loading has been related with earlier onset age of PDA.[12,37,38] Although the DSM-5 classifies panic disorder and agoraphobia as independent disorders, the genetic association between panic disorder and agoraphobia implies that there could be a close pathophysiological relationship between the 2 diseases.[7,8]
The PDA group was more likely to be prescribed combined antidepressant treatment and antipsychotic augmentation than PD group. In addition, they were prone to be prescribed BZD for longer duration than PD group. This suggests that patients with PDA show poorer prognosis than patients with PD. Evidence also shows that PDA patients are more difficult to be treated and exhibit higher recurrence rate than the PD.[14,39] Brook et al reported that 35% of patients with PDA took BZD whereas only 8% of patient with PD were prescribed BZD.[40] Tiller also reported that doses of BZD and antidepressants to alleviate symptoms in patients with PDA were higher than those for patients with PD only.[41] Antipsychotic augmentation for the treatment of panic disorder in relation with agoraphobia has not been reported previously. Evidence support that antidepressants augmented with atypical antipsychotics could result in a superior therapeutic effect than antidepressant monotherapy for treatment-resistant panic disorder.[42,43] Altogether, these results shows that PDA is more difficult condition to treat than PD as previous studies have suggested.[16,44]
The limitations of this study come as follows. First, the small sample size limits the generalizability of our results. Second, the retrospective nature of the study may introduce selection bias, although we included all consecutive patients to prevent it. In addition, we could not obtain the information on the treatment effect; instead we speculated the clinical course based on the prescribed medication. Finally, the self-report questionnaire was used to assess the severity of symptoms. It has been proposed that psychological symptoms are associated with dysregulation of biological factors such as neuro-endocrine system.[45] However, we measured the symptoms of subjects by using standardized tools which were validated in various populations.
Despite these limitations, this study had the following strengths. We could obtain various psychological symptoms of the subjects from the questionnaires that the patients completed before the treatment. Based on this, we could observe that agoraphobic score was significantly correlated with several psychological symptoms including panic disorder severity which has not been reported before. Also, we evaluate various parameters regarding treatment course such as BZD dose, the duration of BZD use, as-needed BZD prescription, total duration of treatment, and hospitalization. This makes our study different from previous ones and gives clinicians comprehensive perspectives view from psychopathology to pharmacological treatment. Longitudinal studies are needed to identify the causal relationship between agoraphobia and panic disorder.
In conclusion, patients with PDA may show worse prognosis coming from more severe symptoms and poorer treatment responses than patients with PD. This suggests that it is still crucial to identify the presence of agoraphobia in panic disorder, even though it is no more a specifier of panic disorder in the diagnostic system and more careful clinical attentions are required for those with agoraphobia. More intensive pharmacological and psychological treatment should be introduced for patients with PDA. Combining CBT with pharmacological treatment can be a helpful strategy in treating PDA, since it has been known that CBT effectively alleviate symptoms of panic disorder with psychological comorbidities.
Acknowledgments
The authors thank all the patients who participated in the study.
Author contributions
J.S, H.J.J and S.M.K collected and analyzed the data, and designed this study. J.S and H.J.J conducted and wrote the manuscript. D.H.P, S.H.R and J.H.H edited and supervised this study process. All authors reviewed and approved the final article.
Footnotes
Abbreviations: APPQ = Albany panic and phobia questionnaire, ASI-R = anxiety sensitivity index–revised, BDI = beck depression inventory, MMPI = Minnesota multiphasic personality inventory, PD = panic disorder, PDA = panic disorder with agoraphobia, PDSS = panic disorder severity scale, STAI = state-trait anxiety inventory.
How to cite this article: Shin J, Park DH, Ryu SH, Ha JH, Kim SM, Jeon HJ. Clinical implications of agoraphobia in patients with panic disorder. Medicine. 2020;99:30(e21414).
The authors have no potential conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Grant BF, Hasin DS, Stinson FS, et al. The epidemiology of DSM-IV panic disorder and agoraphobia in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry 2006;67:363–74. [DOI] [PubMed] [Google Scholar]
- [2].Johnson J, Weissman MM, Klerman GL. Panic disorder, comorbidity, and suicide attempts. Arch Gen Psychiatry 1990;47:805–8. [DOI] [PubMed] [Google Scholar]
- [3].George DT, Nutt D, Dwyer B, et al. Alcoholism and panic disorder: is the comorbidity more than coincidence? Acta Psychiatr Scand 1990;81:97–107. [DOI] [PubMed] [Google Scholar]
- [4].Gorman JM, Coplan JD. Comorbidity of depression and panic disorder. J Clin Psychiatry 1996;57: Suppl 10: 34–43. [PubMed] [Google Scholar]
- [5].Zisook S, Iglewicz A, Avanzino J, et al. Bereavement: course, consequences, and care. Curr Psychiatry Rep 2014;16:482. [DOI] [PubMed] [Google Scholar]
- [6].Pompili M, Shrivastava A, Serafini G, et al. Bereavement after the suicide of a significant other. Indian J Psychiatry 2013;55:256–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Rothe C, Gutknecht L, Freitag C, et al. Association of a functional 1019C > G 5-HT1A receptor gene polymorphism with panic disorder with agoraphobia. Int J Neuropsychopharmacol 2004;7:189–92. [DOI] [PubMed] [Google Scholar]
- [8].Noyes R, Crowe RR, Harris EL, et al. Relationship between panic disorder and agoraphobia: a family study. Arch Gen Psychiatry 1986;43:227–32. [DOI] [PubMed] [Google Scholar]
- [9].Maier W, Roth M, Buller R, et al. Agoraphobia in panic disorder: an indicator of the severity of panic disorder or a distinct diagnostic entity? Psychiatr Ann 1991;21:374–81. [Google Scholar]
- [10].Kim JBJC. A comparison study between panic disorder with agoraphobia and panic disorder without agoraphobia. J Korean Soc Biol Ther Psychiatry 1998;4:196–203. [Google Scholar]
- [11].Asmundson GJ, Taylor S, Smits AJ, et al. Panic disorder and agoraphobia: An overview and commentary on DSM-5 changes. Depress Anxiety 2014;31:480–6. [DOI] [PubMed] [Google Scholar]
- [12].Langs G, Quehenberger F, Fabisch K, et al. The development of agoraphobia in panic disorder: a predictable process? J Affect Disord 2000;58:43–50. [DOI] [PubMed] [Google Scholar]
- [13].Kessler RC, Chiu WT, Jin R, et al. The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2006;63:415–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Francis JL, Weisberg RB, Dyck IR, et al. Characteristics and course of panic disorder and panic disorder with agoraphobia in primary care patients. Prim Care Companion J Clin Psychiatry 2007;9:173–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Noyes R, Reich J, Christiansen J, et al. Outcome of panic disorder: relationship to diagnostic subtypes and comorbidity. Arch Gen Psychiatry 1990;47:809–18. [DOI] [PubMed] [Google Scholar]
- [16].Kikuchi M, Komuro R, Oka H, et al. Panic disorder with and without agoraphobia: comorbidity within a half-year of the onset of panic disorder. Psychiatry Clin Neurosci 2005;59:639–43. [DOI] [PubMed] [Google Scholar]
- [17].Furukawa TA, Katherine Shear M, Barlow DH, et al. Evidence-based guidelines for interpretation of the panic disorder severity scale. Depress Anxiety 2009;26:922–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Shear MK, Brown TA, Barlow DH, et al. Multicenter collaborative panic disorder severity scale. Am J Psychiatry 1997;154:1571–5. [DOI] [PubMed] [Google Scholar]
- [19].Lee EH, Kim JH, Yu BH. Reliability and validity of the self-report version of the Panic Disorder Severity Scale in Korea. Depress Anxiety 2009;26:E120–3. [DOI] [PubMed] [Google Scholar]
- [20].Brown TA, White KS, Barlow DH. A psychometric reanalysis of the Albany Panic and Phobia Questionnaire. Behav Res Ther 2005;43:337–55. [DOI] [PubMed] [Google Scholar]
- [21].Kim JH, Yang JC, Kim JB, et al. A validation study of Korean Albany panic and Phobia Questionnaire (APPQ). J Korean Neuropsychiatr Assoc 2004;43:329–36. [Google Scholar]
- [22].Kim JH, Yu BH, Yang JC, et al. A validation study of Korean anxiety sensitivity index-revised (ASI-R). J Korean Neuropsychiatr Assoc 2004;43:54–61. [Google Scholar]
- [23].Jackson-Koku G. Beck depression inventory. Occup Med 2016;66:174–5. [DOI] [PubMed] [Google Scholar]
- [24].Julian LJ. Measures of anxiety: state-trait anxiety inventory (STAI), Beck anxiety inventory (BAI), and Hospital anxiety and Depression scale-anxiety (HADS-A). Arthritis Care Res 2011;63: Suppl 110 11: S467–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Heo EH, Jeong SH, Kang HY. Comparative study on personality assessment inventory and MMPI-2 profiles of groups with high and low depression and suicide ideation in psychiatry patients and discriminant variables of depression and suicide ideation. J Korean Neuropsychiatr Assoc 2018;57:86–95. [Google Scholar]
- [26].Han K, Lim J, Min B, et al. Korean MMPI-2 standardization study. Korean J Clin Psychol 2006;25:533–64. [Google Scholar]
- [27].Oh SH, Oh KS, Lee KU, et al. In-depth investigation for prescribing trends of benzodiazepines in South Korea. Int J Clin Pharmacol Ther 2014;52:460–70. [DOI] [PubMed] [Google Scholar]
- [28].Inoue K, Kaiya H, Hara N, et al. A discussion of various aspects of panic disorder depending on presence or absence of agoraphobia. Compr Psychiatry 2016;69:132–5. [DOI] [PubMed] [Google Scholar]
- [29].Garvey MJ, Tuason V. The relationship of panic disorder to agoraphobia. Compr Psychiatry 1984;25:529–31. [DOI] [PubMed] [Google Scholar]
- [30].Clum GA, Knowles SL. Why do some people with panic disorders become avoidant? A review. Clin Psychol Rev 1991;11:295–313. [Google Scholar]
- [31].Nukariya K, Nakayama K. Phobic disorder concept/diagnosis/psychosocial study. Clin Psychiatry 2006;35:777–82. [Google Scholar]
- [32].Choi EY, Lee JY, Jung DS, et al. Differences of coping strategies for stress between the patients of panic disorder with and without agoraphobia. J Korean Soc Biol Ther Psychiatry 2001;7:45–52. [Google Scholar]
- [33].Chambless DL, Gracely EJ. Fear of fear and the anxiety disorders. Cognit Ther Res 1989;13:9–20. [Google Scholar]
- [34].Reiss S. Expectancy model of fear, anxiety, and panic. Clin Psychol Rev 1991;11:141–53. [Google Scholar]
- [35].Faravelli C, Pallanti S, Frassine R, et al. Panic attacks with and without agoraphobia: a comparison. Psychopathology 1988;21:51–6. [DOI] [PubMed] [Google Scholar]
- [36].Venturello S, Barzega G, Maina G, et al. Premorbid conditions and precipitating events in early-onset panic disorder. Compr Psychiatry 2002;43:28–36. [DOI] [PubMed] [Google Scholar]
- [37].Goldstein RB, Wickramaratne PJ, Horwath E, et al. Familial aggregation and phenomenology of ’early’-onset (at or before age 20 years) panic disorder. Arch Gen Psychiatry 1997;54:271–8. [DOI] [PubMed] [Google Scholar]
- [38].Battaglia M, Bertella S, Politi E, et al. Age at onset of panic disorder: influence of familial liability to the disease and of childhood separation anxiety disorder. Am J Psychiatry 1995;152:1362–4. [DOI] [PubMed] [Google Scholar]
- [39].Nay W, Brown R, Roberson-Nay R. Longitudinal course of panic disorder with and without agoraphobia using the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Psychiatry Res 2013;208:54–61. [DOI] [PubMed] [Google Scholar]
- [40].Marcks BA, Weisberg RB, Keller MB. Psychiatric treatment received by primary care patients with panic disorder with and without agoraphobia. Psychiatr Serv 2009;60:823–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Tiller JW. Treatment of panic disorder. Aust Prescr 2000;23:124–6. [Google Scholar]
- [42].Chen MH, Tsai SJ. Treatment-resistant panic disorder: clinical significance, concept and management. Prog Neuropsychopharmacol Biol Psychiatry 2016;70:219–26. [DOI] [PubMed] [Google Scholar]
- [43].Ravindran LN, Stein MB. The pharmacologic treatment of anxiety disorders: a review of progress. J Clin Psychiatry 2010;71:839–54. [DOI] [PubMed] [Google Scholar]
- [44].Carpiniello B, Baita A, Carta MG, et al. Clinical and psychosocial outcome of patients affected by panic disorder with or without agoraphobia: results from a naturalistic follow-up study. Eur Psychiatry 2002;17:394–8. [DOI] [PubMed] [Google Scholar]
- [45].Pompili M, Gibiino S, Innamorati M, et al. Prolactin and thyroid hormone levels are associated with suicide attempts in psychiatric patients. Psychiatry Res 2012;200:389–94. [DOI] [PubMed] [Google Scholar]


