Abstract
We analyzed cardiopulmonary resuscitation (CPR) rates, deaths preceded by CPR, and survival trends after in-hospital CPR, using a sample of nationwide Korean claims data for the period 2003 to 2013.
The Korean National Health Insurance Service–National Sample Cohort is a stratified random sample of 1,025,340 subjects selected from among approximately 46 million Koreans. We evaluated the annual incidence of CPR per 1000 admissions in various age groups, hospital deaths preceded by CPR, and survival rate following in-hospital CPR. Analyses of the relationships between survival and patient and hospital characteristics were performed using logistic regression analysis.
A total of 5918 in-hospital CPR cases from 2003 to 2013 were identified among eligible patients. The cumulative incidence of in-hospital CPR was 3.71 events per 1000 admissions (95% confidence interval 3.62–3.80). The CPR rate per 1000 admissions was highest among the oldest age group, and the rate decreased throughout the study period in all groups except the youngest age group. Hospital deaths were preceded by in-hospital CPR in 18.1% of cases, and the rate decreased in the oldest age group. The survival-to-discharge rate in all study subjects was 11.7% during study period, while the 6-month and 1-year survival rates were 8.0% and 7.2%, respectively. Survival tended to increase throughout the study period; however, this was not the case in the oldest age group. Age and malignancy were associated with lower survival rates, whereas myocardial infarction and diabetes mellitus were associated with higher survival rates.
Our result shows that hospital deaths were preceded by in-hospital CPR in 18.1% of case, and the survival-to-discharge rate in all study subjects was 11.7% during the study period. Survival tended to increase throughout the study period except for the oldest age group. Our results provide reliable data that can be used to inform judicious decisions on the implementation of CPR, with the ultimate goal of optimizing survival rates and resource utilization.
Keywords: advance care planning, cardiopulmonary resuscitation, survival
1. Introduction
Cardiopulmonary arrest is a disastrous event with a high rate of mortality. Cardiopulmonary resuscitation (CPR) is an emergency procedure that involves chest compression and ventilation to provide immediate blood supply to the brain in cases of cardiopulmonary arrest.[1] Initially, it was touted as a life-saving measure that can be performed anytime and anywhere regardless of the situation, resulting in widespread layperson training and media coverage. However, CPR gradually transformed from an intervention used in specific clinical settings to the default practice in response to cardiac arrest, to avoid medico-legal lawsuits. This trend has been accompanied by a remarkable decrease in its success rate, and thus performing CPR has been controversial for patients near death.[2,3] However, it is difficult to make sound decisions on whether to perform CPR or not, even for patients near death, without information on its success rate, because CPR may result in a small, if transient, chance of recovery while the outcome without its application is generally fatal.
The CPR success rate is related to the circumstances of cardiopulmonary arrest (in-hospital vs out-of-hospital, witnessed vs unwitnessed, etc). While innovations such as the defibrillators used by emergency medical service personnel, which allow for prompt CPR, resulted in improved out-of-hospital CPR outcomes, it is unclear whether advances in CPR technology have improved outcomes after in-hospital cardiac arrest.[4] The success rate of in-hospital CPR varies widely and is dependent on the age and comorbidities of the patient. In a study of Medicare Provider Analysis and Review (MedPAR) hospital claims of 433,985 patients who underwent in-hospital CPR, 18.3% survived to hospital discharge, where the rate of survival did not change substantially during the period 1992 to 2005.[2] The proportion of in-hospital deaths preceded by CPR increased, whereas the proportion of survivors discharged home after undergoing CPR decreased.[2] This is in contrast to out-of-hospital CPR survival rates, which improved significantly and were accompanied by lower rates of neurologic disability after 2010.[5] A meta-analysis compared the outcomes of in-hospital CPR according to 2 guidelines: The 2010 CPR guidelines published by the American Heart Association emphasized the use of high-quality chest compressions, recommending a compressions, airway, breathing sequence, instead of the airway, breathing, compressions sequence of the 2005 guidelines, to minimize delays in the initiation of compressions and resuscitation.[6] In the analysis of 77,605 patients, there was actually no significant difference in the return of spontaneous circulation or survival-to-discharge outcomes between the 2 groups.[7] These results imply that there is still much to be done to improve CPR success rates for in-hospital cardiac arrest, involving not only specific techniques and rapid response systems, but also better guidance on advanced life support decisions at end-of-life.
There is currently a paucity of data on in-hospital CPR survival rates and end-of-life care practices in Asia, where aging occurs at a faster pace than in any other part of the world, and where aged patients with critical illness and under advanced life-support account for at least half of all such patients globally.[8] The purpose of this study was to observe trends in in-hospital CPR rates and survival-to-discharge rates after CPR for the period 2003 to 2013, which represents period before legislation on the Life-sustaining Treatment Decision-making Act by using nationwide claims data in Korea. Patient and hospital characteristics associated with survival were examined as well.
2. Methods
2.1. Data sources
Data for the period 2003 to 2013 were obtained from the National Health Insurance Service–National Sample Cohort (NHIS-NSC). As a compulsory social insurance program, the Korean health program covers the population of the entire country, and there are 2 tiers: The National Health Insurance (NHI) program is a wage-based, contributory insurance program covering approximately 96% of the population, while the Korean Medical Aid program is a government-subsidized public assistance program for medically indigent individuals with low income.[9] The NHIS-NSC includes medical treatment and prescription data of 2.2% of all Koreans (1,025,340 subjects among the entire national population of approximately 46 million)[10] The data set was generated using a stratified sampling method according to sex (2 strata) and age (18 strata: infants <1 year, age 1–4 years, 5-year age groups between 5 and 79 years, and >80 years), and participant eligibility status and income level (41 strata: 20 for insured employees, 20 for insured self-employed individuals, and 1 for medical aid beneficiaries at the lowest level of income), comprising a total of 1476 strata. The representativeness and validity of this sample database was confirmed by comparing estimates based on the sample data and the entire population.[11] The NHIS-NSC contains each patient's unique encrypted identification number, age, sex, primary diagnosis, secondary diagnosis, surgical or medical treatment administered, whether the individual was an inpatient or outpatient, type of insurance (i.e., NHI or medical aid), medical expenses, medical institution identification, and prescriptions.[12] Diagnoses were coded according to the International Classification of Disease, Tenth Revision (ICD-10). We defined 6 most frequent coexisting illnesses in patients admitted to intensive care in Korea as follows (with coding variance among physicians for the same syndrome accounted for): diabetes mellitus (DM; E10-14), myocardial infarction (MI; I21–I25), chronic heart failure (I50), stroke (I60–63), chronic obstructive pulmonary disease (J43, J44, J47), and cancer (C).[13] The analysis of regional distribution was based on 17 districts: Seoul, Busan, Incheon, Daegu, Gwangju, Daejeon, Ulsan, Sejong, Gyeonggi-do, Gangwon-do, Chungcheongbuk-do, Chungcheongnam-do, Jeollabuk-do, Jeollanam-do, Gyeongsangbuk-do, Gyeongsangnam-do, and Jeju-do. Hospital characteristics, including number of beds and location, were determined using the medical institution identification.
2.2. Study population
The study population consisted of subjects aged ≥20 years old who were admitted in hospitals between January 1, 2003 and December 31, 2013 and had at least 1 episode of CPR during the admission identified by payment claims. In-hospital CPR was defined as the presence of either of the following 2 procedure codes for payment in the International Classification of Diseases, Ninth Revision (ICD-9): 99.60 (CPR, not otherwise specified) or 99.63 (closed chest cardiac massage).[14]
Because the survival data for the year 2013 were incomplete in the data set, the annual survival rates were analyzed for the period 2003 to 2012. Those who had received CPR and were hospitalized for <24 hours were considered dead on arrival and excluded from the analysis. For patients with more than 1 CPR event, we analyzed the survival rate and prognostic factors for the first occurrence only. The primary outcome was survival to hospital discharge. Potential predictors included age, sex, coexisting illnesses, income level, hospital size (i.e., <250, 250–499, or ≥500 beds), and the location (metropolitan/nonmetropolitan) of the hospital.
2.3. Statistical analyses
Annual trends in CPR rate, death preceded by CPR and CPR survival rates were evaluated using the Cochran–Armitage trend test. Analyses of the associations of survival with patient and hospital characteristics were performed by logistic regression analysis. Variables with a statistically significant association (P < .05) were included in multivariable models. The relationship was considered statistically significant at P < .05. All analyses were performed using SPSS for Windows (ver. 18.0; SPSS Inc, Chicago, IL).
2.4. Ethical approval
This is a study using sample data derived from deidentified administrative database. According to Hallym University Sacred Heart Hospital Institutional Review Board research guideline, IRB approval was waived for this study (2014-I147).
3. Results
A total of 1,595,423 hospital admissions for the period 2003 to 2013 were identified among eligible patients, and 5918 in-hospital CPRs were identified. The most common primary diagnoses for the admission in which in-hospital CPR occurred were as follows: other forms of heart disease, malignant neoplasm, ischemic heart diseases, cerebrovascular diseases, influenza and pneumonia, other bacterial diseases, renal failure, and other diseases of the respiratory system (17, 10.9, 10.1, 8.1, 5.2, 5.0, 3.2, and 2.6%, respectively). The cumulative incidence of in-hospital CPR was 3.71 events per 1000 admissions (95% confidence interval 3.62–3.80). The CPR rate per 1000 admissions was highest for the oldest age group (≥80 years). The rate tended to decrease over time among all ages except for the youngest age group (20–39 years) (Fig. 1). Because the number of admissions per patient increased steeply for the oldest age group throughout the study period (from 1.68 in 2003 to 4.07 in 2013 for those >80 years old), CPR rate was recalculated based only on CPR during the first admission in a given year; again, the CPR rate was highest among the oldest age group while it decreased over time compared to the younger age groups (data not shown). Among the 28,397 hospital deaths identified during the study period, 5,148 patients died after receiving CPR; thus, hospital deaths were preceded by in-hospital CPR in 18.1% of cases. The rate was the highest in the youngest age group and lowest in the oldest age group (Fig. 2). The proportion of hospital deaths preceded by in-hospital CPR increased in the youngest and decreased in the oldest age group over the years (Fig. 2).
Figure 1.
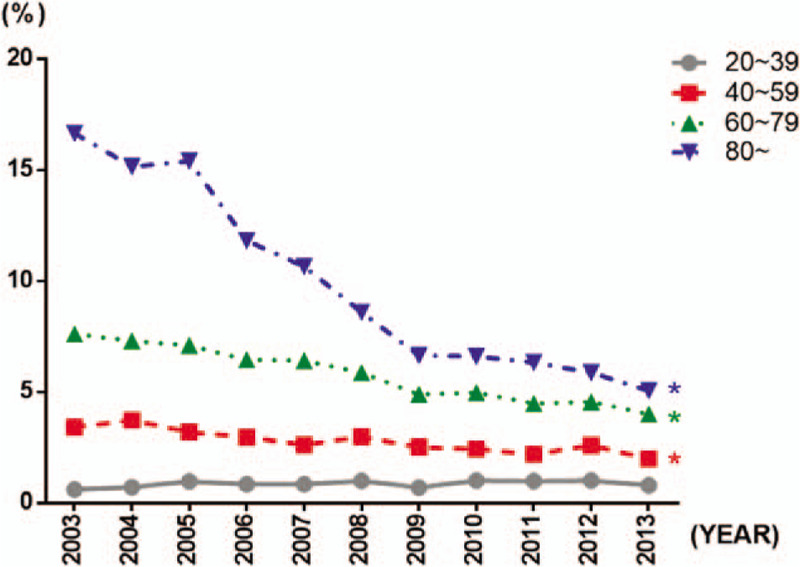
In-hospital cardiopulmonary resuscitation rates per 1000 admissions from 2003 to 2013. The rate decreased over time among all ages except for the youngest age group (20–39 years). (∗P < .01 by the Cochran–Armitage trend test).
Figure 2.
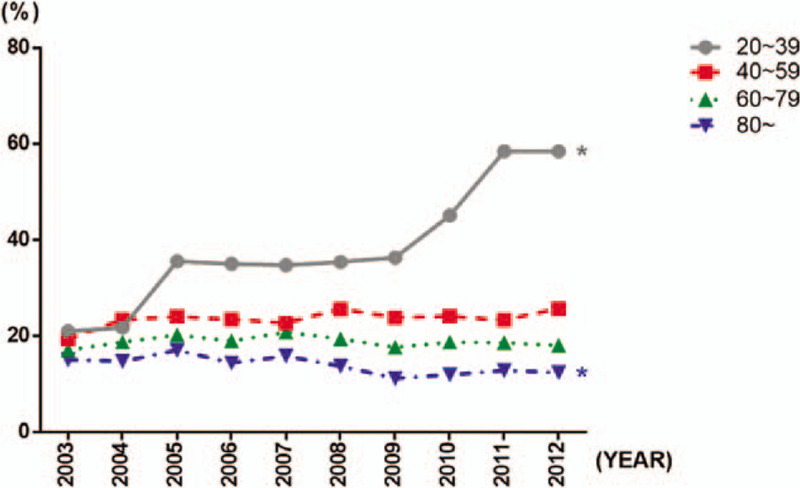
The rates of hospital death preceded by in-hospital cardiopulmonary resuscitation from 2003 to 2012. The rate significantly increased in the youngest and decreased in the oldest age group (P < .01 by the Cochran–Armitage trend test).
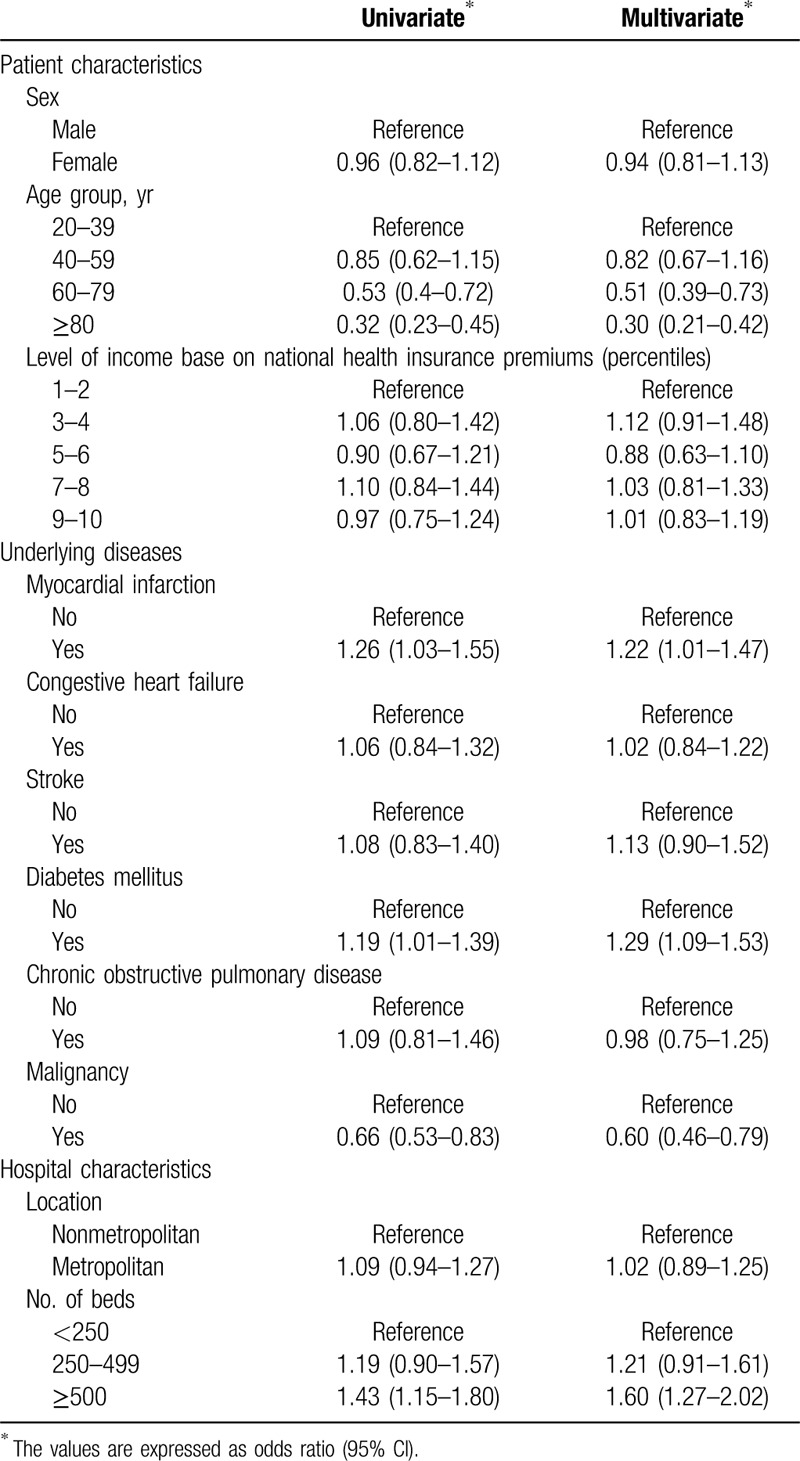
The survival-to-discharge rate was 11.7% during the study period, while the 6-month and 1-year survival rates were 8.0% and 7.2%, respectively (Fig. 3). Survival-to-discharge, 6-month survival, and 1-year survival rates tended to increase throughout the study period; however, this was not the case in the oldest age group. In a univariable analysis, age and malignancy were associated with lower survival-to-discharge rates, while MI and DM were associated with higher rates. Performance of CPR in ≥500-bed size hospitals was associated with a higher rate of survival. All of these factors remained significant in the multivariable analysis (Table 1).
Figure 3.
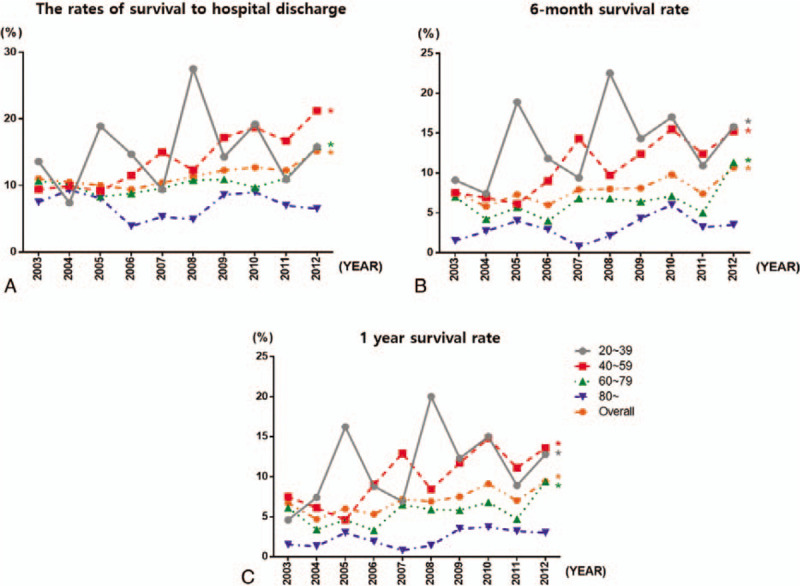
(A) The rates of survival to hospital discharge after in-hospital cardiopulmonary resuscitation (CPR), according to year and age. The rate increased over time among all ages except for the oldest age group (P < .05 by the Cochran–Armitage trend test). (B) The 6-month survival rate after in-hospital CPR according to year and age. The rate increased over time among all ages except for the oldest age group (P < .05 by the Cochran–Armitage trend test). (C) The 1-year survival rate after in-hospital CPR, according to year and age. The rate increased over time among all ages except for the oldest age group (P < .05 by the Cochran–Armitage trend test).
Table 1.
Patient and hospital characteristics associated with survival after in-hospital cardiopulmonary resuscitation.
4. Discussion
In this study, which used claims data from a random sample representative of the entire Korean population under the NHI program, the survival-to-discharge rate after in-hospital CPR was 11.7%. The CPR incidence per 1000 admissions decreased over time except for in the youngest age group (20–39 years), whereas death preceded by CPR decreased only in the oldest age group (>80 years) over the course of the study period. Older age and malignancy were significantly associated with lower odds of survival. The survival rate did not improve in the oldest age group during any time period.
Compared to out-of-hospital cardiac arrests, the time interval from collapse to initiation of CPR for in-hospital CPR is often shorter; moreover, basic life support is provided by trained personnel, and expert medical assistance is available. However, in a study evaluating in-hospital CPR survival rates from 1992 to 2005 among participants ≥65 years of age, it was shown that while the proportion of in-hospital deaths preceded by CPR increased, the proportion of survivors discharged home after undergoing CPR decreased.[2] The authors speculated that changes in the severity of illness and the underlying cause of cardiac arrest over time, and thus increases in the proportion of patients with nonsurvivable primary illnesses who received CPR, might have offset any improvement in the delivery of CPR.
A meta-analysis of CPR among cancer patients showed that nearly 9 in 10 initial CPR survivors died in hospital.[15] This means that for the sickest patients, initial resuscitation success usually leads to death, often in the intensive care unit (ICU), along with all the agony associated with end-of-life decisions, and it may merely prolong the dying process and increase suffering. A previous study reported that the use of do not resuscitate (DNR) orders to exclude patients who were inappropriate candidates for CPR have led to high overall CPR survival rates.[16] Although concerns exist regarding under-treatment due to stringent criteria for the initiation of CPR, another study showed that the absence of a formally approved DNR order policy did not result in better survival rates for brain-damaged patients.[17] A policy that assigns patients to care categories, and includes CPR and subsequent mechanical ventilatory support, was found to dramatically decrease the rates of CPR and mechanical ventilation with no change in mortality.[18]
Although Asian societies show the fastest rates of aging, and Asians comprise approximately half of all patients with critical illnesses worldwide, a paucity of data exists regarding end-of-life care, including in-hospital CPR survival rates.[19] Because substantial differences are expected in the way people approach end-of-life care between Asia and the West, data derived from the West cannot be extrapolated to Asian society. A recent report evaluated the incidence and outcomes of in-hospital cardiac arrest in 12 Beijing hospitals.[20] Of the 10,198 in-hospital cardiac arrests recorded, CPR was initiated in 26.6% of cases, and restoration of spontaneous circulation was achieved in 962 (35.5%) patients. However, only 9.1% of patients were discharged alive and 6.4% had good neurologic outcomes. Although the authors concluded that the poorer outcomes compared to other industrialized countries may stem from the lack of trained resuscitation teams, differences in attitudes toward end-of-life care and the absence of DNR protocols may have also played a role. In a study of a single hospital in Taiwan, among 382 patients with in-hospital cardiac arrest who required resuscitation, the ROSC and survival-to-discharge rates were 66% and 11.8%, respectively.[21] Independent predictors for survival to hospital discharge were female gender, a resuscitation duration of <20 minutes, and no use of epinephrine during resuscitation.[21] In a Korean multicenter cohort study of 22 ICUs in 15 hospitals, the survival of patients admitted to ICUs after in-hospital CPR was reported. Among 150 patients who were admitted post-CPR, about half (74 patients) survived. Interestingly, the mortality of patients did not differ between hospitals with and without rapid response systems.[22] Although more data are required, this result suggests that the survival of in-hospital CPR depends more on intrinsic patient related factors than on technology and the implementation of response systems.
This study is the first to analyze CPR data from a representative population of Koreans. The in-hospital CPR survival rate of 11.8% is in agreement with previous studies in Asia. Korea is currently in the process of formally implementing DNR, and data derived before the year 2013 are considered representative of the pre-DNR era. Survival rates tended to improve throughout the study period; however, it is uncertain whether the survival improvement stems from improvements in the CPR delivery system, which was a “work in progress” in Korea and subject to a policy designed to improve the quality of hospital care, or from better selection of CPR candidates by improvement of end-of-life care discussions. CPR rate and death preceded by CPR decreased among the oldest age group, and it might have affected the improvement in overall survival. It is worth noting that survival did not improve in the oldest age group (>80 years) during any time period. As was expected, we found that older age and the presence of malignancy were significantly associated with a lower chance of survival. Although previous studies found a positive correlation between income level and survival rates, it was not associated with survival in our study. Patients with MI and DM had higher survival after CPR. It is probable that cardiac arrest after MI resulted from problems such as cardiac arrhythmia, which is more responsive to CPR. It is more difficult to explain why DM patients had better survival, although this group may have included less critical patients compared to other diagnosis groups such as malignancy or chronic obstructive pulmonary disease.
It is obvious that age alone cannot be used to inform the decision to perform resuscitation or not; however, our study provides useful information for elderly patients. A study of patients >60 years of age were asked about their preference if they suffered cardiac arrest during an acute illness. While 41% opted for CPR, only 22% did so after learning that the probability of survival-to-discharge was 10% to 17%; only 6% of patients ≥86 years of age wanted CPR in these circumstances.[3] This is important because elderly patients often hold erroneous beliefs regarding the outcomes of in-hospital CPR.[23]
This study was the first to observe in-hospital CPR survival trends among a representative Asian population. The limitations inherent to administrative claims data apply, however, including the lack of detailed information on premorbid conditions that determine long-term prognoses. Although we used sample data instead of whole-population data, the representativeness of the current study sample was reported previously.[15] Last follow-up year for this cohort included patients in year 2013, which is outdated. It is possible that the survival rate has changed since 2016, when “Life-sustaining Treatment Decision-making Act” was finalized. It is of interest whether this legislation led to better implementation of end-of-life care and changed the practice of futile CPR in the hospitals and thus, improved its efficiency reflected by survival rate. This is the subject of our future research, for which the survival data would be collected from year 2016 to year 2025. The reason behind the marked increase of death preceded by CPR in the young age group since 2010 partly resulted from the small denominator (that is to say, there were low number of young subjects who had in-hospital CPR) which made the data in this age bracket rather unstable.
Educating patients and their families about the probability of survival after CPR would allow them to make more informed decisions regarding end-of-life care. CPR is not an innocuous procedure, as it can have serious consequences, such as liver laceration or mediastinal hematoma, in a significant number of patients.[24] Our results provide reliable data that could inform judicious decisions on the implementation of CPR and advanced life support, with the ultimate goal of optimizing survival rates and resource utilization.
Author contributions
Conceptualization: Hyun Ah Kim.
Data curation: Young-Su Ju, Sung Yeon Lee, Hyun Sun Cho.
Formal analysis: Young-Su Ju.
Funding acquisition: Hyun Ah Kim.
Visualization: In Young Park, Jeong-Im Hong.
Footnotes
Abbreviations: CPR = cardiopulmonary resuscitation, DM = diabetes mellitus, DNR = do not resuscitate, ICD = International Classification of Disease, ICU = intensive care unit, MI = myocardial infarction, NHI = National Health Insurance, NHIS-NSC = National Health Insurance Service–National Sample Cohort.
How to cite this article: Park IY, Ju YS, Lee SY, Cho HS, Hong JI, Kim HA. Survival after in-hospital cardiopulmonary resuscitation from 2003 to 2013: an observational study before legislation on the life-sustaining treatment decision-making act of Korean patients. Medicine. 2020;99:30(e21274).
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI15C2699), and by the Hallym University Research Fund.
The English in this document has been checked by at least 2 professional editors, both native speakers of English. For a certificate, please see: http://www.textcheck.com/certificate/yN2s4A.
The authors have no conflicts of interest to disclose.
The data that support the findings of this study are available from a third party, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are available from the authors upon reasonable request and with permission of the third party.
References
- [1].Fowler R, Chang MP, Idris AH. Evolution and revolution in cardiopulmonary resuscitation. Curr Opin Crit Care 2017;23:183–7. [DOI] [PubMed] [Google Scholar]
- [2].Ehlenbach WJ, Barnato AE, Curtis JR, et al. Epidemiologic study of in-hospital cardiopulmonary resuscitation in the elderly. N Engl J Med 2009;361:22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Murphy DJ, Burrows D, Santilli S, et al. The influence of the probability of survival on patients’ preferences regarding cardiopulmonary resuscitation. N Engl J Med 1994;330:545–9. [DOI] [PubMed] [Google Scholar]
- [4].Schluep M, Gravesteijn BY, Stolker RJ, et al. One-year survival after in-hospital cardiac arrest: a systematic review and meta-analysis. Resuscitation 2018;132:90–100. [DOI] [PubMed] [Google Scholar]
- [5].Larribau R, Deham H, Niquille M, et al. Improvement of out-of-hospital cardiac arrest survival rate after implementation of the 2010 resuscitation guidelines. PLoS One 2018;13:e0204169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hazinski MF, Nolan JP, Billi JE, et al. Part 1: executive summary: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2010;122: Suppl 2: S250–75. [DOI] [PubMed] [Google Scholar]
- [7].Zhu A, Zhang J. Meta-analysis of outcomes of the 2005 and 2010 cardiopulmonary resuscitation guidelines for adults with in-hospital cardiac arrest. Am J Emerg Med 2016;34:1133–9. [DOI] [PubMed] [Google Scholar]
- [8].Lin MH, Peng LN, Chen LK, et al. Cardiopulmonary resuscitation for hospital inpatients in Taiwan: an 8-year nationwide survey. Resuscitation 2012;83:343–6. [DOI] [PubMed] [Google Scholar]
- [9].Kim JH, Lee KS, Yoo KB, et al. The differences in health care utilization between medical aid and health insurance: a longitudinal study using propensity score matching. PLoS One 2015;10:e0119939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Kim HA, Shin JY, Kim MH, et al. Prevalence and predictors of polypharmacy among Korean elderly. PLoS One 2014;9:e98043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Lee J, Lee JS, Park SH, et al. Cohort profile: the national health insurance service-national sample cohort (NHIS-NSC), South Korea. Int J Epidemiol 2017;46:e15. [DOI] [PubMed] [Google Scholar]
- [12].Boo S, Yoon YJ, Oh H. Evaluating the prevalence, awareness, and control of hypertension, diabetes, and dyslipidemia in Korea using the NHIS-NSC database: a cross-sectional analysis. Medicine (Baltimore) 2018;97:e13713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kim DY, Lee MH, Lee SY, et al. Survival rates following medical intensive care unit admission from 2003 to 2013: an observational study based on a representative population-based sample cohort of Korean patients. Medicine (Baltimore) 2019;98:e17090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kim T, Kwon OK, Bang JS, et al. Epidemiology of ruptured brain arteriovenous malformation: a National Cohort Study in Korea. J Neurosurg 2018;1–6. [DOI] [PubMed] [Google Scholar]
- [15].Reisfield GM, Wallace SK, Munsell MF, et al. Survival in cancer patients undergoing in-hospital cardiopulmonary resuscitation: a meta-analysis. Resuscitation 2006;71:152–60. [DOI] [PubMed] [Google Scholar]
- [16].Ballew KA, Philbrick JT, Caven DE, et al. Predictors of survival following in-hospital cardiopulmonary resuscitation: a moving target. Arch Intern Med 1994;154:2426–32. [PubMed] [Google Scholar]
- [17].Skogvoll E, Isern E, Sangolt GK, et al. In-hospital cardiopulmonary resuscitation. 5 years’ incidence and survival according to the Utstein template. Acta Anaesthesiol Scand 1999;43:177–84. [DOI] [PubMed] [Google Scholar]
- [18].Davila F. The impact of do-not-resuscitate and patient care category policies on CPR and ventilator support rates. Arch Intern Med 1996;156:405–8. [PubMed] [Google Scholar]
- [19].Adhikari NK, Fowler RA, Bhagwanjee S, et al. Critical care and the global burden of critical illness in adults. Lancet 2010;376:1339–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Shao F, Li CS, Liang LR, et al. Incidence and outcome of adult in-hospital cardiac arrest in Beijing, China. Resuscitation 2016;102:51–6. [DOI] [PubMed] [Google Scholar]
- [21].Chen C, Chiu P, Tang CY, et al. Prognostic factors for survival outcome after in-hospital cardiac arrest: an observational study of the oriental population in Taiwan. J Chin Med Assoc 2016;79:11–6. [DOI] [PubMed] [Google Scholar]
- [22].Kim HC, Yoo JW, Lim SY, et al. Mortality after in-hospital cardiopulmonary resuscitation: multicenter analysis in Korea. J Crit Care 2013;28:942–6. [DOI] [PubMed] [Google Scholar]
- [23].Adams D, Snedden D. How misconceptions among elderly patients regarding survival outcomes of inpatient cardiopulmonary resuscitation affect do-not-resuscitate orders. J Am Osteopath Assoc 2006;106:402–4. [PubMed] [Google Scholar]
- [24].Beom JH, You JS, Kim MJ, et al. Investigation of complications secondary to chest compressions before and after the 2010 cardiopulmonary resuscitation guideline changes by using multi-detector computed tomography: a retrospective study. Scand J Trauma Resusc Emerg Med 2017;25:8. [DOI] [PMC free article] [PubMed] [Google Scholar]


