Abstract
Monckeberg medial calcific sclerosis (MCS) is an infrequent finding in the temporal artery and can clinically present almost indistinguishably from giant cell arteritis (GCA). To our knowledge, there have been only two case reports of suspected GCA found to be MCS only after a temporal artery biopsy (TAB).
Herein, we present two cases. The first case is a 69-year-old female with hypertension, type-2 diabetes mellitus, and chronic headaches who presented with left temporal headaches and scalp tenderness. She had a prominently dilated, tortuous, and tender left temporal artery. Initial labs showed a leukocyte count of 11.1x103/L, erythrocyte sedimentation rate (ESR) of 29 mm/hr, and C-reactive protein (CRP) of 5.8 mg/L. The patient was started on prednisone 60 mg for presumptive GCA. Left TAB was negative for inflammatory changes, with findings consistent with MCS. Steroids were discontinued, and symptoms resolved. The second case is a 67-year-old male with hypertension, asthma, hyperlipidemia, status-post left eye cataract phacoemulsification, with intraocular lens insertion one-month prior, who presented with left eye blurriness in the inferior visual field and intermittent headache for 15 days. Left ophthalmoscopy showed retinal pallor and edema. Initial labs revealed ESR of 25 mm/hr, CRP of 11.2 mg/L, leukocyte count of 13.01x103/L. The patient was given solumedrol 120 mg once and prednisone 70 mg daily for presumptive GCA. Left TAB was negative for GCA but reported damaged elastic fibers by calcification consistent with MCS. Partial visual blurriness remained, and steroids were discontinued.
This report accentuates the importance of MCS as a temporal GCA simulator. Physicians should be aware that TAB potentially changes management and may help surface underlying conditions.
Keywords: monckeberg medial calcific sclerosis, giant cell arteritis, temporal artery biopsy
Introduction
Giant cell arteritis (GCA) is a chronic, idiopathic, granulomatous vasculitis of the medium and large arteries [1]. It is mostly found in people above 50 years of age and usually involves the branches of the external and internal carotid arteries, predominantly the temporal artery, leading to the classical symptoms of headache, scalp tenderness, jaw claudication, and visual impairment.
Monckeberg medial calcific sclerosis (MCS) is described as calcification of the tunica media and/or internal elastic lamina in small and medium-sized arteries, commonly, but not exclusively, associated with aging and numerous comorbidities ranging from type 2 diabetes mellitus and renal dysfunction to hormone disorders and vitamin deficiencies [2]. This form of arteriosclerosis is most often detected in the muscular arteries of the extremities and, sporadically, the visceral ones.
Clinically, GCA of the temporal artery is a medical emergency and should be treated punctually since it can progress to permanent vision loss [3], while MCS is usually asymptomatic, often discovered incidentally on radiographs or ultrasounds of the pelvis or lower limbs, and identified as linear radiopaque lesions with an ankle-brachial index greater than 1.1 [1].
To date, few cases of MCS involving the temporal artery have been documented. In this case report, we describe two cases of MCS of the temporal artery presenting as suspected GCA.
Case presentation
Case 1
A 69-year-old female, with a past medical history of hypertension, type 2 diabetes mellitus, and chronic headaches, was sent to the emergency room by her private ophthalmologist for the evaluation of worsening left temporal headaches and left scalp tenderness.
The patient reported worsening bitemporal headaches for the last six months (left worse than right), described as throbbing in nature and associated with photophobia, phonophobia, and nausea. She also noted left scalp tenderness, jaw claudication with chewing, and bilateral shoulder pain. She denied any visual changes, neck stiffness, tinnitus, focal neurological deficit, fever, weight loss, or rash.
On physical examination, a prominently dilated and tortuous left temporal artery was noted, which was tender to palpation. Initial labs were notable for a leukocyte count of 11.1 x103/L, hemoglobin of 12 g/dL, platelet count of 199 x103/L, creatinine of 1.14 mg/dL, erythrocyte sedimentation rate (ESR) of 29 mm/hr and C-reactive protein (CRP) of 5.8 mg/L. Non-contrast CT head was negative for pathology.
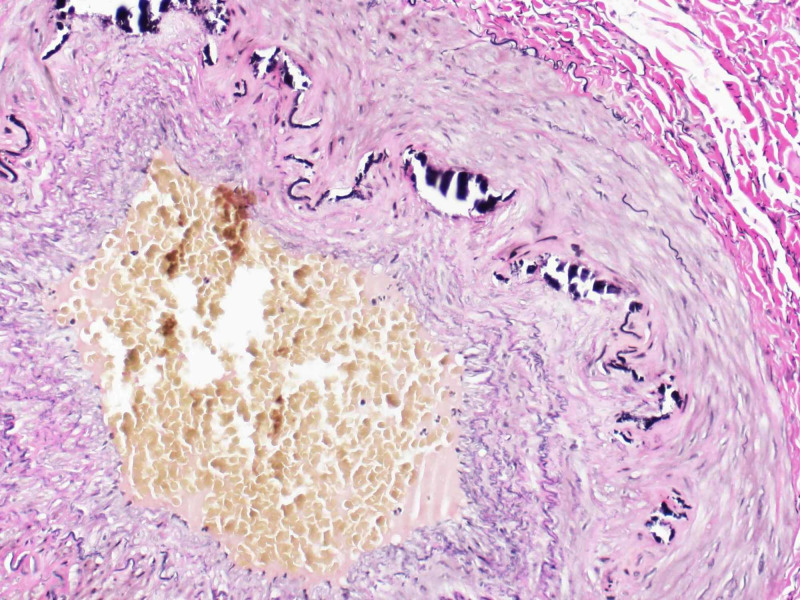
Based on clinical findings and the presumed diagnosis of GCA, the patient was started on prednisone 60 mg daily. Left temporal artery biopsy (TAB) was performed two days after steroid therapy was initiated. The pathology report was negative for any inflammatory changes and demonstrated findings consistent with MCS (Figure 1). Symptoms resolved, and steroids were discontinued after one week. The patient remained asymptomatic at the three-week follow-up visit and was diagnosed with temporomandibular joint dysfunction.
Figure 1. Temporal artery biopsy showing calcification of tunica media.
Case 2
A 67-year-old male with a past medical history of hypertension, asthma, hyperlipidemia, status-post left eye phacoemulsification cataract procedure, with the insertion of an intraocular lens in the left eye one month prior, presented to the emergency room with complaints of blurry vision in the inferior visual field of the left eye and intermittent headache for 15 days.
Upon presentation, the patient reported that, initially, his vision was clear postoperative for one week but became blurry in the inferior field of vision of the left eye with gradual deterioration. The patient denied eye pain, redness, vision loss, neck pain, fever, ataxia, diplopia, or jaw claudication.
Evaluation of the left eye showed retinal pallor and edema. No prominent temporal artery or scalp tenderness was appreciated, and the rest of the physical examination was unremarkable. Laboratory results upon presentation revealed an ESR of 25 mm/hr, CRP of 11.2 mg/L, white blood cell (WBC) count of 13.01 x103/L, hemoglobin of 13.3 g/dL, hematocrit of 40.8%, neutrophil count of 78.7%, and lymphocyte count of 13.2%. Non-contrast computed tomography (CT) head and the carotid duplex was negative for pathology.
Based on clinical findings and concern for potential GCA, solumedrol 120 mg was given in the emergency room and the patient was started on prednisone 70 mg daily. Left temporal artery biopsy was performed six days after steroid therapy was initiated. The pathology report was negative for GCA and demonstrated damage to elastic fibers by calcification consistent with MCS (Figures 2-3). Prednisone was discontinued and, due to persistently blurry vision, the patient was diagnosed with nonarteritic anterior ischemic optic neuropathy on his three-week follow-up visit.
Figure 2. Temporal artery biopsy.
Calcium stain demonstrating Monckeberg medial calcific sclerosis
Figure 3. Temporal artery biopsy.
Elastic fiber stain showing disruption secondary to calcification
Discussion
This report describes two cases of temporal artery MCS simulating GCA. To the best of our knowledge, only two other cases were published with similar presentations and biopsy reports (Table 1).
Table 1. Summary of reported cases in the literature.
ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; GERD: gastroesophageal reflux disease
| Case report | Age/sex | Clinical presentation | Inflammatory markers (ESR in mm/hour, CRP in mg/L) | Comorbidities | Biopsy report | Outcome |
| Present case 1 (2020) | 69 / F | Chief complaint: Bitemporal headache x 6 months. Pertinent findings: Photophobia, phonophobia, nausea, jaw claudication, left scalp tenderness, dilated, tortuous left temporal artery | ESR: 29, CRP: 5.8 | Hypertension, type 2 diabetes, headaches | Focal internal elastic lamina destruction, mild atherosclerosis with intimal hyperplasia, no inflammation | Symptoms resolved |
| Present case 2 (2020) | 67 / M | Chief complaint: Blurry vision in left eye for 3 days, intermittent headache for 15 days. Pertinent findings: Dizziness | ESR: 25, CRP: 11.2 | Hypertension, asthma, hyperlipidemia, GERD | Partial damage of elastic fibers by calcification | Blurry vision in the lower visual field of the left eye persists |
| Phelps PO et al. (2015) [3] | Not reported | Chief complaint: Acute vision loss. Pertinent findings: Hard artery to palpation | ESR: normal, CRP: normal | Not reported | Mineralization of internal elastic lamina | Irreversible vision loss |
| Belliveau et al. (2013) [4] | 85 / F | Chief complaint: Left temporal tenderness for 2 weeks, intermittent headache for 15 days. Pertinent findings: Left-sided hearing loss, jaw claudication | ESR: 23, CPR: 1.0 | Osteoporosis, hypothyroidism, coronary artery disease, osteoarthritis, lung neoplasm (active) | Focal ossification of media and internal elastic lamina, visible osteoclast-type giant cells, lumen was patent | Not specified |
Out of the four cases, three of them were above 50 years of age and experienced headaches; two of them manifested tenderness in the temporal area; and one of the cases presented with acute vision loss and temporal artery hardening. Although these four cases portrayed normal ESR, the concurrence of temporal arteritis and normal ESR has been described in the literature, where a meta-analysis of 114 studies suggested that physical findings characteristic of this vasculitis yielded more value for positive diagnosis than the significance of an elevated ESR for ruling out GCA [5-6].
Currently, in the setting of signs and symptoms suggestive of GCA [7], prompt evaluation of the temporal artery via color Doppler ultrasound (CDUS) or temporal artery biopsy is recommended. CDUS of the head, neck, and upper extremities has been suggested as a diagnostic aid for GCA due to its non-invasiveness and the specificity reported of the “halo sign” (which represents mural edema) [8], although results are operator-dependent in nature and the procedure has not yet been standardized. In our case reports, CDUS was not performed due to a lack of extensive experience.
TAB remains the gold standard for the diagnosis of temporal arteritis, in which case, intimal thickening with luminal stenosis, mononuclear inflammatory cell infiltrate with medial invasion, necrosis, and medial giant cell formation are hallmark features [5]. False-negative TAB in suspected GCA can occur, likely due to the sampling of skip lesions. Nonetheless, in a study of TAB results performed on patients with suspected GCA, 6% of specimens showed MCS associated with disorganization around the calcification and disruption of the internal elastic lamina, findings that should not be erroneously interpreted as sequelae of previous arterial inflammation [9].
Initially defined in 1903 in the arteries of the extremities [10], medial calcification has been observed histologically in the ascending aorta, medium-sized renal arteries, and, less commonly, small arteries, including the coronaries, the temporals, and others [2,11-12], with an approximate prevalence of 27% [13] in patients with end-stage renal disease, 17% in newly diagnosed diabetics [14], and 41% in those with more advanced disease [15]. In the microcirculation, this leads to altered hemodynamics, loss of autoregulation, and impaired compensatory remodeling [16].
As vascular compromise progresses, there is a loss of arterial wall elasticity, progressively deteriorating anterior arterial flow, thrombus formation, and decreased organ perfusion [2]. It is important to distinguish MCS from other forms of vascular calcification, such as calciphylaxis, since the former is an innocuous form where calcium deposits assume a quiescent pattern of deposition without true endoluminal calcification or vascular compromise, while the latter describes a sudden precipitous deposition of calcium in soft tissue and is associated with endoluminal calcification and vascular thrombotic occlusion [17].
The physiologic underpinnings, clinical consequences, and therapies for MCS remain elusive, including whether the condition is localized or systemic. Nonetheless, medial calcification has been recognized as an independent risk factor for cardiovascular events and all-cause mortality [13-14,18].
Conclusions
To conclude, this article accentuates the significance of MCS as a simulator of temporal GCA. Primary physicians, rheumatologists, ophthalmologists, and pathologists should be aware of this diagnosis since its identification on TAB greatly changes the management of patients with suspected temporal arteritis and may be a sign of potential underlying conditions such as diabetes mellitus, chronic kidney disease, and cardiovascular risk factors.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
References
- 1.Large-vessel giant cell arteritis: diagnosis, monitoring and management. Koster MJ, Matteson EL, Warrington KJ. Rheumatology. 2018;57:32–42. doi: 10.1093/rheumatology/kex424. [DOI] [PubMed] [Google Scholar]
- 2.Medial vascular calcification revisited: review and perspectives. Lanzer P, Boehm M, Sorribas V, et al. Eur Heart J. 2014;35:1515–1525. doi: 10.1093/eurheartj/ehu163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Monckeberg's arteriosclerosis in temporal arteritis suspect. Phelps P, Surapaneni K, Potter H. Ophthalmology. 2015;122:1186. doi: 10.1016/j.ophtha.2014.12.023. [DOI] [PubMed] [Google Scholar]
- 4.Mönckeberg medial calcific sclerosis mimicking giant cell arteritis clinically. Belliveau MJ, Almeida DRP, Eneh A, Farmer J. Can J Ophthalmol. 2013;48:71–72. doi: 10.1016/j.jcjo.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 5.Temporal arteritis with erythrocyte sedimentation rate <50 mm/h: a clinical reminder. Muhammad Raza Cheema, Shakawan M Ismaeel. Clinical Interventions in Aging. 2016;11:185–188. doi: 10.2147/CIA.S40919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Does this patient have temporal arteritis? Smetana GW, Shmerling RH. JAMA. 2002;287:92–101. doi: 10.1001/jama.287.1.92. [DOI] [PubMed] [Google Scholar]
- 7.The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Hunder GG, Bloch DA, Michel BA, et al. Arthritis Rheum. 1990;33:1122–1128. doi: 10.1002/art.1780330810. [DOI] [PubMed] [Google Scholar]
- 8.Color duplex ultrasonography in the diagnosis of temporal arteritis. Schmidt WA, Kraft HE, Vorpahl K, Völker L, Gromnica-Ihle EJ. N Engl J Med. 1997;337:1336–1342. doi: 10.1056/NEJM199711063371902. [DOI] [PubMed] [Google Scholar]
- 9.Monckeberg’s sclerosis in temporal artery biopsy specimens. Castillo BV Jr, Torcynski E, Edward DP. Br J Ophthalmol. 1999;83:1088. doi: 10.1136/bjo.83.9.e1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Über die reine Mediaverkalkung der Extremitätenarterien und ihr Verhalten zur Arteriosklerose [Article in German] Mönckeberg J. Virchows Arch Pathol Anat Physiol Klin Med. 1903;171:141–167. [Google Scholar]
- 11.Monckeberg medial calcific sclerosis mimicking malignant calcification pattern at mammography. Saxena A, Waddell IC, Friesen RW, Michalski RT. https://jcp.bmj.com/content/58/4/447.2. J Clin Pathol. 2005;58:447–448. [PMC free article] [PubMed] [Google Scholar]
- 12.Media calcification and intima calcification are distinct entities in chronic kidney disease. Amann K. Clin J Am Soc Nephrol. 2008;3:1599–1605. doi: 10.2215/CJN.02120508. [DOI] [PubMed] [Google Scholar]
- 13.Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality. London GM, Guérin AP, Marchais SJ, Métivier F, Pannier B, Adda H. Nephrol Dial Transplant. 2003;18:1731–1740. doi: 10.1093/ndt/gfg414. [DOI] [PubMed] [Google Scholar]
- 14.Medial artery calcification predicts cardiovascular mortality in patients with NIDDM. Niskanen L, Siitonen O, Suhonen M, Uusitupa MI. Diabetes Care. 1994;17:1252–1256. doi: 10.2337/diacare.17.11.1252. [DOI] [PubMed] [Google Scholar]
- 15.Medial artery calcification: a neglected harbinger of cardiovascular complications in non-insulin-dependent diabetes mellitus. Lehto S, Niskanen L, Suhonen M, Rönnemaa T, Laakso M. Arterioscler Thromb Vasc Biol. 1996;16:978–983. doi: 10.1161/01.atv.16.8.978. [DOI] [PubMed] [Google Scholar]
- 16.Radiographic manifestations of Mönckeberg arteriosclerosis in the head and neck region. Tahmasbi-Arashlow M, Barghan S, Kashtwari D, Nair MK. Imaging Sci Dent. 2016;6:53–56. doi: 10.5624/isd.2016.46.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Calciphylaxis: a review. Magro CM, Simman R, Jackson S. J Amer College Clin Wound Specialists. 2010;2:66–72. doi: 10.1016/j.jcws.2011.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vascular calcifications as a marker of increased cardiovascular risk: a meta-analysis. Rennenberg R, Kessels A, Schurgers Schurgers, Van Engelshoven J, de Leeuw P, Kroon A. Vasc Health Risk Manag. 2009;5:185–197. doi: 10.2147/vhrm.s4822. [DOI] [PMC free article] [PubMed] [Google Scholar]