Abstract
Background
Surgeons and their assistants are especially at risk of exposure to blood due to glove perforations and needle stick injuries during operations. The use of blunt needles can reduce this risk because they don't penetrate skin easily but still perform sufficiently in other tissues.
Objectives
To determine the effectiveness of blunt needles compared to sharp needles for preventing percutaneous exposure incidents among surgical staff.
Search methods
We searched MEDLINE and EMBASE (until May 2011), CENTRAL, NHSEED, Science Citation Index Expanded, CINAHL, Nioshtic, CISdoc, PsycINFO, and LILACS (until September 2010).
Selection criteria
Randomised controlled trials (RCTs) of blunt versus sharp suture needles for preventing needle stick injuries among surgical staff measured as glove perforations or self‐reported needle stick injuries.
Data collection and analysis
Two authors independently assessed study eligibility and risk of bias in trials and extracted data. We synthesized study results with a fixed‐effect model meta‐analysis.
Main results
We located 10 RCTs involving 2961 participating surgeons performing an operation in which the use of blunt needles was compared to the use of sharp needles. Four studies focused on abdominal closure, two on caesarean section, two on vaginal repair and two on hip replacement. On average, a surgeon that used sharp needles sustained one glove perforation in three operations. The use of blunt needles reduced the risk of glove perforations with a relative risk (RR) of 0.46 (95% confidence interval (CI) 0.38 to 0.54) compared to sharp needles. The use of blunt needles will thus prevent one glove perforation in every six operations.
In four studies, the use of blunt needles reduced the number of self‐reported needle stick injuries with a RR of 0.31 (95% CI 0.14 to 0.68). Because the force needed for the blunt needles is higher, their use was rated as more difficult but still acceptable in five out of six studies.
The quality of the evidence was rated as high.
Authors' conclusions
There is high quality evidence that the use of blunt needles appreciably reduces the risk of exposure to blood and bodily fluids for surgeons and their assistants over a range of operations. It is unlikely that future research will change this conclusion.
Plain language summary
The use of blunt needles compared to sharp needles for preventing needle stick injuries in surgical staff
Surgeons and their assistants are especially at risk of needle stick injuries during operations. This can lead to infection with HIV or other blood‐borne viruses. The use of blunt needles is proposed to prevent needle stick injuries. We reviewed the literature to evaluate the preventive effect of blunt needles compared to sharp needles on needle stick injuries among surgical staff. We searched multiple medical databases (to May 2011). We included studies if they were randomised controlled trials (RCTs) of blunt versus sharp suture needles for preventing needle stick injuries among surgical staff. We located 10 RCTs with 2961 operations in which blunt needles were compared to sharp needles. Six studies focused on abdominal operations, two on vaginal repair and two on hip replacement. On average, a surgeon that used sharp needles sustained one glove perforation per three operations. The use of blunt needles reduced the risk of glove perforations by 54% (95% confidence interval 46% to 62%) compared to sharp needles. The use of blunt needles in six operations will thus prevent one glove perforation. In four studies the use of blunt needles also reduced the number of self‐reported needle stick injuries by 69% (95% confidence interval 14% to 68%). Even though surgeons reported that the force needed for the blunt needles was higher, their use of the needles was still rated as acceptable in five out of six studies. We concluded that there is high quality evidence that the use of blunt needles appreciably reduces the risk of contracting infectious diseases for surgeons and their assistants over a range of operations by reducing the number of needle stick injuries. It is unlikely that future research will change this conclusion.
Summary of findings
Summary of findings for the main comparison. Blunt needles compared to sharp needles for preventing percutaneous exposure injuries.
| Blunt needles compared to sharp needles for preventing percutaneous exposure injuries | ||||||
| Patient or population: surgical staff Intervention: blunt needles Comparison: sharp needles | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| sharp needles | blunt needles | |||||
| glove perforations per surgeon per operation | Study population | RR 0.46 (0.38 to 0.54) | 2961 (10 studies) | ⊕⊕⊕⊕ high | ||
| 293 per 1000 | 135 per 1000 (111 to 158) | |||||
| Low risk population | ||||||
| 20 per 1000 | 9 per 1000 (8 to 11) | |||||
| High risk population | ||||||
| 750 per 1000 | 345 per 1000 (285 to 405) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
Background
Healthcare workers are at risk of acquiring infectious diseases through exposure at work. Exposure to blood or bodily fluids from infected patients can lead to infection with hepatitis B (HBV), hepatitis C (HCV) and HIV, among other pathogens. These are serious viral infections that may cause a chronic disease process or initiate cancer and eventually lead to death. According to the model of Pruss‐Ustun et al, 16,000 HCV, 66,000 HBV and 1000 HIV infections may have occurred worldwide among healthcare workers in the year 2000 due to their occupational exposure to blood and bodily fluids (Pruss‐Ustun 2005). The World Health Organization (WHO) reports that two million healthcare workers across the world experience percutaneous exposure to infectious diseases each year (WHO 2007). The operating room is a special environment in the healthcare setting with a high risk of sharps injuries (Watt 2008; Watt 2010).
Description of the condition
The risk of acquiring an infection is proportional to the prevalence of the infection in the patient population. Thus, in areas where hepatitis B is endemic and HIV is prevalent, such as in Africa, the risks are much higher than in Western Europe or North America. This situation has a significant impact on the health of the workers and also on the healthcare system as a whole. The transmission of occupational blood‐borne infectious diseases leads to absenteeism, morbidity and, in some cases, mortality among healthcare workers, which ultimately leads to a reduction in workforce and consequently affects patients' quality of care and safety. Because of the risk of acquiring an infectious disease at work, healthcare workers may also suffer from psychological stress, which affects both their work and personal life (Fisman 2002; Sohn 2006). There is also the financial burden imposed on hospitals due to occupational exposure to blood‐borne diseases, which includes costs related to blood tests, treatment, outpatient visits and lost working hours.
Description of the intervention
Exposure to blood or bodily fluids is also called percutaneous exposure and happens most often when healthcare workers are injured with sharp needles or instruments, or when blood or body fluids are splashed during medical interventions or accidents. These incidents are called sharps or needle stick injuries, or percutaneous exposure incidents (PEI). The actual causes of a PEI are multi‐factorial and include elements such as, but not limited to, types of devices and procedures, lack of access to or availability of personal protective equipment for the healthcare workers, sub‐optimal use of personal protective equipment, professional inexperience and lack of training and education on infection control and occupational health principles, improper management of sharps, poor organisational climate, high workload and fatigue, working alternative shifts, and high mental pressure and subjective perception of risk (Akduman 1999; Ansa 2002; Clarke 2002; Doebbeling 2003; Fisman 2007; Ilhan 2006; Oh 2005; Orji 2002; Roberts 1999; Smith 2006; Smith 2006b; Wallis 2007). Most of these causes can be addressed by specific interventions. In the operating theatre, one of the specific risks is a needle stick injury caused by suture needles. This accounts for more than half of all percutaneous injuries that occur in the operating room (Meyers 2008). Also, according to the American College of Surgeons, suture needles pose the greatest risk of sharp injuries to surgeons and scrub personnel (ACS 2011). The reporting of these injuries in surgical settings remained quite stable in the US between 1993 and 2003, in spite of the introduction of legislation requiring the use of safety‐engineered sharp devices in 2000. The lack of adoption of safer devices such as blunt suture needles is blamed for the lack of improvement (Jagger 2008; Jagger 2011).
How the intervention might work
There are several possibilities to prevent infection from PEI. For hepatitis B, vaccination has been successful (Chen 2005) but vaccination is not yet possible for HCV or HIV (Mast 2004). Therefore, exposure reduction remains the main preventive strategy. In general, there are several ways of reducing or eliminating exposure, such as elimination of hazards at the source (for example, elimination of unnecessary injections) or along the path (for example, safer medical devices or workplace practices, use of personal protective equipment) (Ellenbecker 1996; Roelofs 2003). For surgical staff, the prevention of sharp injuries related to sharp suture needles could be overcome by using blunt or taper point needles (ACS 2011; Monz 1991; NIOSH 2008). There is also evidence from laboratory studies that gloves give better protection against punctures with tapered needles than with sharp needles (Lefebvre 2008).
Why it is important to do this review
Blunt needles have been advocated for a long time (Wright 1993). It is important to know if this preventive intervention is effective. Some studies indicate that blunt needles would reduce PEIs by more than 50% without leading to less operative dexterity, whereas others argue that blunt needles simply don't work (Nordkam 2005; Wilson 2008). However, there is currently no review that gives a systematic summary of the available evidence on the effectiveness of blunt needles.
Objectives
To determine the effectiveness of blunt needles compared to sharp needles for preventing percutaneous exposure incidents among surgical staff.
Methods
Criteria for considering studies for this review
Types of studies
Randomised clinical trials (RCTs) and cluster‐randomised trials (c‐RCTs).
Types of participants
Persons working in the operation theatre that are exposed to the risk of percutaneous injuries with suture needles.
Types of interventions
Blunted suture needles compared to sharp needles. We defined blunt needles as suture needles that have a rounded blunt point and that are circular in diameter and that can be either curved or straight. Sharp needles are suture needles that have a tapered point and that can be either circular in diameter or square with cutting edges and that can be either curved or straight.
Types of outcome measures
Primary outcomes
Exposure of healthcare workers to contaminated blood or bodily fluids was our primary outcome measure. Exposure can be observed either as self‐reported needle stick injury or glove perforations. Many needle stick injuries and glove perforations are not noticed by the surgeon. A glove perforation means that the skin is exposed to blood or bodily fluids. A needle stick injury means that the skin has been perforated and the wound has been exposed to blood or bodily fluids. A needle stick injury is therefore a more serious exposure than a glove perforation. The occurrence is, however, proportional. In other words, an increase in glove perforations will be accompanied by an increase in percutaneous needle stick injuries. Therefore, we took both occurrences as a measure of outcome. Because it is easy for glove perforations to go unnoticed in situ, the perforations must be observed by means of a water or air test. In the water test the gloves are filled with water and the release of a jet‐stream of water is taken as a sign that there is a hole in the glove. In the air test, the gloves are filled with air and then submersed in water and air bubbling up to the surface indicates a hole in the glove. The combination of both tests was shown to detect all glove perforations that were made on purpose with 19, 21 and 23 gauge needles (Smith 1988; Smith 1990). The water test has been reported to detect only 80% of holes made on purpose (Brough 1988). For needle stick injuries, there are no objective tests so we took all self‐reports of needle stick injuries as an outcome.
Secondary outcomes
We included satisfaction with, or ease of use of, the needles.
Search methods for identification of studies
The search was part of a larger search for all interventions to prevent PEI in healthcare personnel and was intended to also include non‐randomised studies as we also searched for interventions that are more difficult to randomise such as safe work practices.
Electronic searches
First, search terms for PEI were applied. These terms for PEI were then combined with the recommended search strings for randomised trials and for non‐randomised studies. For randomised clinical trials and controlled clinical studies, we used the search strategy that has been developed by Robinson and Dickersin (Robinson 2002). For finding non‐randomised studies we used the sensitive search strategy for occupational health intervention studies (Verbeek 2005).
The strategy was used to search MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library) and the Occupational Safety and Health Review Group Specialised Register, NHSEED, Science Citation Index Expanded, CINAHL, Nioshtic, CISdoc, LILACS and PsycINFO (up until September 2010).
The search strategies for the databases are described in Appendix 1.
We did an additional search for the blunt needle intervention in MEDLINE and EMBASE (up until 27 April 2011), which we detail in Appendix 2.
Searching other resources
We searched the databases of the WHO, UK National Health Service (NHS) and www.med.virginia.edu/epinet. In addition, we checked the references of the included articles.
Data collection and analysis
Selection of studies
Using the inclusion and exclusion criteria, two authors working independently screened the identified titles and abstracts of the references that resulted from the search strategy for potential studies. We obtained the full‐text articles of the references that appeared to meet the inclusion criteria. Disagreements between authors were resolved by discussion. A third author (JV) was consulted if disagreements persisted.
Data extraction and management
Two authors independently extracted the data into a form. The form included essential study characteristics about the participants, the interventions, primary and secondary outcomes and results. We also intended to note any adverse events and the sponsorship of the study, but none were reported. The risk of bias of the studies was also independently assessed by two authors. In case of disagreements, a consensus method was used to come to a conclusion. A third author was consulted if disagreement persisted. We did not mask trial names because we feel that this would not increase validity.
Assessment of risk of bias in included studies
For the assessment of risk of bias in studies, we applied the risk of bias tool as provided in RevMan. We used the items on randomisation, allocation concealment, blinding of participants and outcome assessors, incomplete outcome data and selective outcome reporting, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Studies that had more than four out of the seven items rated as low risk of bias were rated as having low risk of bias, following the advice of the Cochrane Back Review Group (Furlan 2009).
Measures of treatment effect
Authors reported the outcome of their studies in many different ways. We assumed that the most valid estimate of the risk of exposure for a member of the operating staff was provided by the number of holes in gloves used by one surgeon or one assistant during one operation. It would have been more precise if 'operation' could have been defined as 'the number of hours engaged in an operation of average difficulty', comparable to a number of person‐years at risk, but the data were not sufficient to calculate this. We intended to treat the results of all trials as being dichotomous, even though needle stick injuries can be sustained more than once, because the resulting risk ratios are easier to interpret. However, the perforation rates in some studies were so high that the use of risk ratios was not feasible anymore. Therefore we calculated the natural logarithm (ln) of the rate ratios and their standard errors from the number of glove perforations and the number of surgeon‐operations in an Excel sheet, as recommended by the Cochrane Handbook (Higgins 2011). The ln rate ratios and the standard errors were used as input in RevMan where we combined them using the generic inverse variance method.
Unit of analysis issues
We intended to calculate the design effect for studies that employed a cluster‐randomised design but that did not make an allowance for the design effect. In six studies the unit of randomisation was the operation but the outcome was measured for one surgeon only. Therefore we assumed that there was no unit of analysis issue in these cases. In four studies there was more than one person who could sustain needle stick injuries in one operation. Therefore, these studies were effectively cluster‐randomised trials even though the authors did not design them as such (Mingoli 1996; Nordkam 2005; Sullivan 2009; Wilson 2008). There were, however, not enough details to calculate the effect of the clustering of the surgeons per operation. We calculated perforations in gloves per surgeon and per operation. We called this unit of analysis a surgeon‐operation to indicate that this was the perforation risk for one surgeon performing one operation.
Dealing with missing data
We contacted the authors of Meyer 1996, Nordkam 2005, Sullivan 2009, and Wilson 2008 to obtain information about the exact number of gloves and holes in gloves that had occurred during their study. Nordkam 2005 replied that a total of 812 gloves were used by two operators in the intervention arm and two operators in the control arm. The authors wrote that randomisation was achieved by computer generated numbers and that the observers of the outcome were blind to the type of needle used. We were told that the total number of holes was proportional to the number of perforations per operation. Given the total number of 56 holes, we used the proportion of perforations per operation to calculate the number of holes per study arm. Meyer 1996 replied they used a random number list which was not known to the surgeons. The surgeon called the study nurse while changing his gloves before closure of the laparotomy. For this reason they included only elective surgery in their study. The person who assessed the gloves identified the procedure by the patient´s name and operation book number. The surgeon´s opinion was evaluated separately. The authors used a closure technique in which the intestine was protected from needle stick injury by the non‐dominant hand of the surgeon who did the facial closure and not by instruments. This explains the preferential perforation of the left glove of a right‐handed surgeon and may in part explain the quantity of perforations.
For the ease of use of blunt needles for Nordkam 2005, we calculated standard deviations from P values according to the methods given by the Cochrane Handbook (Higgins 2011).
Assessment of heterogeneity
We defined clinically homogeneous studies as those with similar populations, interventions and outcomes measured at the same follow‐up point. We deemed all surgical staff to be similar enough to yield similar treatment effects. We also deemed all blunt and sharp needles to be similar enough to be combined. We did not combine different outcomes such as glove perforations and reported needle stick injuries. All glove perforations, even though measured in slightly different ways, are deemed sufficiently similar to be combined in a single comparison.
We assessed the amount of statistical heterogeneity in the meta‐analysis by means of the I2 statistic. We used the criterion of an I2 = 50%, as mentioned in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), to discern the presence or absence of considerable statistical heterogeneity between studies.
Assessment of reporting biases
We assessed publication bias with a funnel plot.
Data synthesis
We pooled studies with sufficient data, and judged to be clinically homogeneous, with RevMan software (RevMan 2011).
We intended to use a random‐effects model in the meta‐analysis when studies were statistically heterogeneous, but they weren't. We used a fixed‐effect model to pool study results.
For studies with multiple study arms that belonged to the same comparison, we intended to divide the number of events and participants equally over the study arms to prevent double counting of study participants in the meta‐analysis, but no such studies were found.
Finally, we used the GRADE approach to assess the quality of the evidence per comparison and per outcome as described in the Cochrane Handbook of Systematic Reviews (Higgins 2011). Starting from high quality, we reduced the quality of evidence by one or more levels if there was one or more limitations in any of the following domains: risk of bias, consistency, directness of the evidence, precision of the pooled estimate and the possibility of publication bias. We used the programme GRADEPro to generate a 'Summary of findings' table.
Subgroup analysis and investigation of heterogeneity
We investigated if the effects of interventions varied per type of operation involved when we compared abdominal closure and caesarean section versus vaginal repair and versus hip operations. This was however a subgroup analysis that we defined post‐hoc and was not specified in the protocol. We intended to compare surgeons versus their assistants but there were not sufficient data available. We also intended to compare different outcomes but they were measured in a similar way and no subgroup analysis was possible.
Sensitivity analysis
We analysed what the influence of studies with a high risk of bias was by re‐analysing the data only for studies with a low risk of bias.
Results
Description of studies
Results of the search
With the initial search strategy described in Appendix 1 and after removal of duplicates we had a total of 11,239 references. We selected 322 references for full‐text reading. This finally resulted in nine studies that fulfilled our inclusion criteria. In the additional search we found 211 references and one was read as full‐text. One extra study fulfilled our inclusion criteria. This brought the final number of included studies to 10 (Figure 1).
1.

Study flow diagram.
Included studies
The studies were carried out between 1998 and 2005. Seven studies were from before 2000.
The studies were located in the UK (Ablett 1998; Hartley 1996; Thomas 1995; Wright 1993), the US (Sullivan 2009; Wilson 2008), Ireland (Rice 1996), the Netherlands (Nordkam 2005 ), Italy (Mingoli 1996) and Germany (Meyer 1996).
Four studies focused on the risk during abdominal closure (Hartley 1996; Meyer 1996; Mingoli 1996; Nordkam 2005), two studies on vaginal repair (Ablett 1998; Wilson 2008), two studies on caesarean section (Sullivan 2009; Thomas 1995) and two on hip replacement operations (Rice 1996; Wright 1993).
In five studies (Ablett 1998; Hartley 1996; Rice 1996; Wilson 2008; Wright 1993) one surgeon per operation participated in the study, in three studies there was a surgeon and an assistant (Meyer 1996; Nordkam 2005; Sullivan 2009), in one study there was a surgeon and two assistants (Mingoli 1996), and in one study it was unclear how many participated (Thomas 1995). In some studies the number of participants was partly inferred from the number of gloves used.
All studies used blunt or tapered needles as the intervention and compared them to sharp or conventional suture needles.
All studies used perforations in gloves as the measure of outcome and the total number of perforations per operator per operation could be assessed for all but one study. Thomas 1995 reported only the number of perforated gloves per operation and not the number of holes. Only two studies used the combination of water and air tests to detect perforations (Ablett 1998; Hartley 1996); for one study we assumed that the combination was used because the study was reported by the same author that validated the test (Thomas 1995). All the other studies used a water test only (Table 2).
1. Control group perforation rate, ascertainment method, operation type.
| Study | Ascertainment Method | Operation Type | Control Rate /operator /operation |
| Ablett 1998 | air/water | vaginal repair | 0.16 |
| Hartley 1996 | air/water | abdominal surgery | 0.36 |
| Mingoli 1996 | water | abdominal surgery | 0.34 |
| Meyer 1996 | water | abdominal surgery | 1.75 |
| Nordkam 2005 | water | abdominal surgery | 0.20 |
| Rice 1996 | water | hip replacement | 0.31 |
| Sullivan 2009 | water | caesarean section | 0.09 |
| Thomas 1995 | assumed air/water | caesarean section | 0.50 |
| Wilson 2008 | water | vaginal repair | 0.02 |
| Wright 1993 | water | hip replacement | 1.00 |
The perforation rate varied greatly between studies, from two in every 100 surgeon‐operations to 175 in every 100 surgeon‐operations (Table 2). Abdominal operations seemed to provide the highest risk and vaginal repair the lowest. It should also be noted that the method of ascertaining perforations has been reported to be related to the number of perforations, with the combined method detecting 25% more perforations than the water test only (Smith 1988).
Excluded studies
Two studies were excluded because the intervention was a needle handling device and not a blunt needle (Bebbington 1996; Botet 1998). Two other studies were excluded because they were not randomised or controlled (Monz 1991; Tydeman 1995).
Risk of bias in included studies
Taken all together, the risk of bias in most studies was considered low given the technical nature of the intervention. There were three studies that scored as low risk of bias for four items (Figure 2; Figure 3).
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
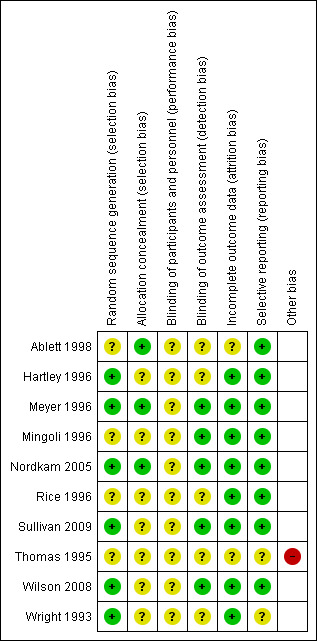
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Six of the 10 studies used a proper method of randomisation and in four studies it was unclear. Allocation was concealed by the use of envelopes until before the operation or the closure of the abdominal fascia in two studies only (Ablett 1998; Nordkam 2005) and in one study by the involvement of a research nurse (Meyer 1996). It is difficult to conceive how influencing of the randomisation procedure could have led to different results. Since the needles were used in the same type of operation, for both intervention and control group, the risk of exposure was similar for both groups. The surgeons could not know in advance how big their risk of exposure would be in an operation and then, for example, mitigate the risk by choosing a blunt needle. Therefore we think that this has not had a great influence on the results.
Blinding
None of the studies could blind the surgeon for the type of needle used because the surgeons will always be aware what type of needle they are using. We indicated this as an unclear risk of bias. Theoretically, it is possible that the surgeon treats sharp needles more carefully than blunt ones and thus influences the risk of exposure.
Outcome assessment can be done blind to the type of needle used. This was only reported for five studies (Mingoli 1996;Meyer 1996; Nordkam 2005; Sullivan 2009; Wilson 2008). For the other studies it was unclear if observers were blinded.
Incomplete outcome data
Eight out of the 10 studies reported holes for all gloves used. Since the gloves were collected immediately after the operation this was fairly easy to achieve. In two studies we weren't sure if all gloves were reported because information was lacking.
Selective reporting
Eight out of 10 studies reported all outcomes that were described in the methods section.
Other potential sources of bias
In one study (Thomas 1995) so much essential information was lacking that we considered this as a serious source of bias.
Effects of interventions
See: Table 1
Blunted versus sharp suture needles
Outcome: number of glove perforations
Ten trials including 2961 surgeon‐operations compared the effect of blunt versus sharp needles on glove perforations and found a significant reduction of glove perforations, with a relative risk (RR) of glove perforation of 0.46 (95% confidence interval (CI) 0.38 to 0.54) (Analysis 1.1; Figure 4).
1.1. Analysis.

Comparison 1 Blunt versus sharp suture needles, Outcome 1 Glove perforation rate.
4.
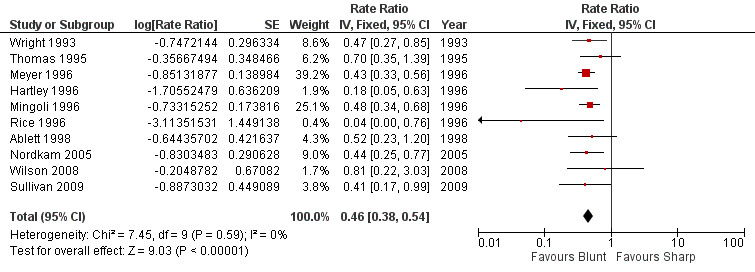
Forest plot of comparison: 1 Blunt versus sharp suture needles, outcome: 1.1 Glove perforation rate.
Outcome: percutaneous injuries
Five studies reported the number of percutaneous injuries but in one study there were no injuries in the intervention and control groups (Hartley 1996). We could combine four studies in a meta‐analysis. The use of blunt needles decreased the risk of a needle stick injury by 69% (RR 0.31, 95% CI 0.14 to 0.68) (Analysis 1.2).
1.2. Analysis.

Comparison 1 Blunt versus sharp suture needles, Outcome 2 Needle Stick Injuries.
Outcome: surgeon satisfaction and needle performance
Data on needle performance could only be extracted for Nordkam 2005 and Meyer 1996. Nordkam 2005 showed that surgeons found the sharp needles 20% easier to use, on a VAS scale from 0 to 100, but Meyer 1996 reported that the blunt needles were easier to use even though clearly more force was needed (Analysis 1.2; Analysis 1.3; Analysis 1.4; Analysis 1.5).
1.3. Analysis.
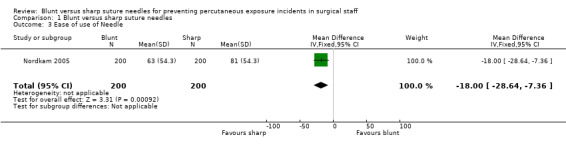
Comparison 1 Blunt versus sharp suture needles, Outcome 3 Ease of use of Needle.
1.4. Analysis.

Comparison 1 Blunt versus sharp suture needles, Outcome 4 Ease of use of needle.
1.5. Analysis.

Comparison 1 Blunt versus sharp suture needles, Outcome 5 Force needed.
Rice 1996 reported that the surgeons had no difficulties with the use of the blunt needles. In Sullivan 2009, 92% of the surgeons reported that the blunt needles were acceptable but they were less satisfied with their use. Wilson 2008 reported that surgeons found the blunt needles significantly more difficult to use. In Wright 1993, the surgeons found the blunt needles slightly more difficult to use but they had minimal effect on their technique.
Sensitivity analysis
We made two subgroups of studies, with high and low risk of bias respectively, to evaluate the impact of risk of bias on our results. There was no difference between the two groups (Analysis 1.6).
1.6. Analysis.

Comparison 1 Blunt versus sharp suture needles, Outcome 6 Sensitivity to ROB.
We checked if the use of risk ratios for those studies that made it feasible would change the results but there was hardly a difference. We also checked if using the number of glove pairs as the nominator in the rates made a difference but it did not substantially change the result.
Subgroup analysis
Even though the effect of the intervention seems to be less in vaginal repair operations, it is difficult to draw conclusions given the small number of studies in each subgroup (Analysis 1.7).
1.7. Analysis.

Comparison 1 Blunt versus sharp suture needles, Outcome 7 Subgroups Type of Operation.
Publication bias
The funnel plot revealed that there was one small study with a very positive outcome. Otherwise the study outcomes are located in all quadrants of the plot (Figure 5).
5.
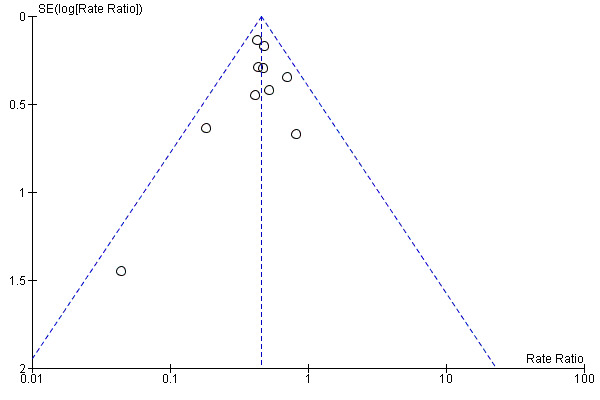
Funnel plot of comparison: 1 Blunt versus sharp suture needles, outcome: 1.1 Glove perforation rate.
Grade assessment
We found that, overall, there was no serious risk of bias in the included studies for the glove perforations outcome. The comparison was direct. There was no heterogeneity, the confidence interval was narrow, and there was no indication of publication bias. Therefore, we kept the level of evidence at high quality and did not downgrade it (Table 1).
For the needle stick injuries outcome, we also concluded that there was no serious risk of bias in the studies. The comparison was direct, there was no heterogeneity but the confidence intervals were much wider. There was no indication of publication bias. Because of the more imprecise results and the less objective nature of the outcome, we downgraded the evidence by one level to moderate quality.
Discussion
Summary of main results
There is high quality evidence that blunt suture needles lead to fewer perforations in surgical gloves than sharp needles. There is moderate quality evidence that blunt needles also reduce the number of needle stick injuries. The results were not influenced by the quality of the studies, albeit in abdominal closure the effect may be more noticeable than in vaginal repair operations.
Overall completeness and applicability of evidence
We performed a comprehensive search for studies that evaluated interventions to prevent needle stick injuries that was further supplemented with an additional search specifically for blunt needle evaluations. We are quite confident that we located all available studies. Most studies were done in the 1990s when surgeons became more aware of the risk of infection with HIV, but there were more recent studies too. The needles were used in a variety of operations and in a variety of countries. However, it was not always clear for which tissues the blunt needles were used. Some authors mentioned that they used them only for fascia and muscle but others were not explicit here. We found one study that described how blunt needles can be used for a subcuticular skin closure (Miller 1994) and because they do not penetrate skin they are actually easier to use for this type of skin closure. It is not clear how well blunt needles perform in other tissues. Knowing in which tissues they don't perform well and thus defining the limitations of blunt needles might help to improve their implementation. . The intervention is simple, easy to apply to many operative techniques and only slightly more costly than conventional needles. Even though there has been evidence of their effectiveness for almost two decades, blunt needles are still not in use where they should be. We found one fairly recent survey article that reported on the implementation of blunt needles in the US (Catanzarite 2007). It states that in 2005 in the US, 71% of perioperative nurses had never tried to use blunt needles. They also report that in a small US region that they surveyed, of 104 obstetricians and gynaecologists in 2006, 63% had never used blunt needles, 25% had tried them but did not use them anymore and only 12% currently used blunt needles. In another survey in France, blunt‐tipped needles were only available in 49% of the operating theatres and 55% of the surgeons said they had never used them (Tarantola 2006). Thus, there seems to be ample room for implementation of this preventive intervention. It is difficult to judge what makes surgeons resist their use. Catanzarite 2007 reports that some surgeons don't like the 'feel' of blunt needles because they move more slowly through the tissue and can produce a noticeable pop as they penetrate fascia. This seems to confirm the satisfaction ratings in the studies included in this review where surgeons say they are less easy to use but still acceptable. Habit and lack of experience are also mentioned but the authors state that the main factor in achieving a higher rate of use of blunt needles is to increase their availability in operating rooms and labour and delivery units.
Quality of the evidence
The overall quality of the evidence in the studies was good even though the reporting of the older studies could have been better. Given the technical nature of the intervention and the objective method of ascertaining that the gloves had holes, used in all studies, we believe that there is no reason to assume a high risk of bias. The newer studies that are better reported and thus score better with regard to risk of bias show similar results to the older studies. It was however disturbing to notice that the habit of testing for perforations has changed over time to water tests only, which were originally reported to be less sensitive than the air test and even less so than the combination of the two tests (Smith 1988; Smith 1990). Everyone who has once repaired a bicycle tyre might know from experience that the air test is very sensitive. Very disturbingly, to support the validity of the water test used most authors referred to an article in which the water test had been described but not validated and stated with great certainty that: "the gloves were tested with a previously validated method". Because all authors tested both study arms with the same test, we don't think that this has influenced the results of this review. A possible effect of detecting fewer perforations could be that the effectiveness of blunt needles has been underestimated.
We used two outcomes: perforations and self‐reported injuries. Perforations are a proxy outcome and they are only assessed as a dichotomous outcome: perforation or no perforation. It could be that blunt needles make worse holes than sharp needles and thus increase the exposure to blood or increase the risk of infection. However, there are laboratory studies that show that circular taper point needles make smaller holes and convey less blood into the glove than sharp cutting needles (Bennett 1994;Edlich 2003; Lefebvre 2008). As far as we are aware there are no similar experiments with blunt tapered circular needles. It seems however justified to assume that a similar effect would occur for blunt circular needles. The risk of infection with blunt needles has been reported in another Cochrane Review which found one study that showed no difference in wound infection with the use of blunt needles for abdominal closure (Anderson 2008).
Potential biases in the review process
We included studies regardless of language or status of publication, which reduces reporting bias. We did data extraction and risk of bias assessment in duplicate and resolved all differences by consensus.
Agreements and disagreements with other studies or reviews
This review confirms the beliefs of professional organisations, such as the American College of Surgeons, that blunt needles reduce the risk of exposure to blood and bodily fluids for surgeons and their assistants (ACS 2011; NIOSH 2008). We found one other non‐systematic review (Berguer 2005) that included only four of the studies that we included. Their conclusions were the same as ours.
Authors' conclusions
Implications for practice.
There is high quality evidence that the use of blunt suture needles appreciably reduces the risk of exposure to blood and bodily fluids for surgeons and their assistants over a range of operations.
Implications for research.
There is high quality evidence that the use of blunt needles is beneficial and it is unlikely that future research will change this conclusion.
Feedback
Lack of patient‐relevant outcomes, 12 January 2016
Summary
Name: Caroline Struthers
Email Address: caroline.struthers@csm.ox.ac.uk
Affiliation: EQUATOR Network
Comment: In the plain language summary there is absolutely no mention of any difference in patient outcomes between the blunt and sharp needle groups. I understand that was not the focus of the review, but to not mention it at all seems strange. It may be the advantage of using sharp needles in terms of patient outcomes is outweighed by the reduction in risk of needle stick injuries and HIV to the surgeons and theatre staff, but it would be good to have that quantified, or at least mentioned in the plain language summary.
I agree with the conflict of interest statement below:
I certify that I have no affiliations with or involvement in any organization or entity with a financial interest in the subject matter of my feedback.
Reply
We thank Ms Struthers for her important comment. We agree that patient‐relevant outcomes are an important element to consider when evaluating the effectiveness of new techniques for ensuring the occupational safety of surgical staff. Unfortunately none of the 10 studies included in our Cochrane review assessed patient‐relevant outcomes such as wound infection or failure of operations. However, another Cochrane review by Anderson 2008 evaluated different techniques for closing the abdominal wall and their effects on patient‐relevant outcomes. They included one study (Stafford 1998) that showed no statistical significant difference in wound infection at discharge when using blunt needles for abdominal closure, albeit the confidence interval was wide. This study was not included in our review because it did not measure needle stick injuries. Given the lack of evidence on patient‐relevant outcomes, we think this issue is worth further study.
We will take this issue better in to account when we update this review and we will then revise all relevant sections of text accordingly.
Contributors
Annika Saarto, Jos Verbeek, Jani Ruotsalainen
What's new
| Date | Event | Description |
|---|---|---|
| 15 March 2016 | Feedback has been incorporated | We received a comment saying that our plain language summary made no reference to patient‐relevant outcomes. Unfortunately none of the 10 studies included in our Cochrane review assessed patient‐relevant outcomes such as wound infection or failure of operations. However, another Cochrane review evaluated different techniques for closing the abdominal wall and their effects on patient‐relevant outcomes. They included one study that showed no statistical significant difference in wound infection at discharge when using blunt needles for abdominal closure, albeit the confidence interval was wide. This study was not included in our review because it did not measure needle stick injuries. Given the lack of evidence on patient‐relevant outcomes, we think this issue is worth further study. We will take this issue better into account when we update this review. We will then revise all relevant sections of text accordingly. |
| 8 May 2012 | Amended | We changed risk ratios to rate ratios |
| 27 February 2011 | Amended | The original version of this protocol was published with the title: "Prevention of percutaneous injuries with risk of hepatitis B, hepatitis C, or other viral infections for health‐care workers". However, it turned out that the scope was far too wide and would result in an unmanageable amount of studies for one review. Therefore the decision was taken to split the protocol into four new ones. The other three new titles are: "Devices to prevent needle recapping for preventing percutaneous exposure injuries in health care personnel", "Education and training for preventing percutaneous exposure injuries in health care personnel" and "Extra gloves versus a single pair of gloves for preventing percutaneous exposure injuries in healthcare personnel". |
Notes
The protocol for this review was first published as "Prevention of percutaneous injuries with risk of hepatitis B, hepatitis C, or other viral infections for healthcare workers" (Parantainen 2008). Our initial idea was to include all interventions used to prevent needle stick injuries. However, after the publication of the protocol it became apparent that very many studies would be eligible for inclusion. The decision was therefore made to split the protocol up into four new protocols, the first one being " Blunt versus sharp suture needles for preventing percutaneous exposure incidents in surgical staff" (Parantainen 2011). The remaining three protocols are titled: "Devices to prevent needle recapping for preventing percutaneous exposure injuries in health care personnel" (Lavoie 2012), "Education and training for preventing sharps injuries and splash exposures in healthcare workers" (Cheetham 2016) and "Extra gloves versus a single pair of gloves for preventing percutaneous exposure injuries in healthcare personnel" (Parantainen 2012).
The original protocol was hosted by the Hepato‐Biliary Group but due to the heavy involvement of Jos Verbeek and the Occupational Safety and Health Group, the new titles were registered under their aegis. The Hepato‐Biliary Group continues to be involved in an advisory capacity.
Acknowledgements
We would like to thank Minna Anthoni and Ulla‐Maija Hellgren who participated in the writing of an early version of this protocol. We would also like to thank Dimitrinka Nikolova and Christian Gluud from the Hepato‐Biliary Group for their comments on the same early version of this protocol and Jani Ruotsalainen from the Occupational Safety and Health Group and Janet Wale from the Bone, Joint and Muscle Trauma Group for copy editing the text.
Appendices
Appendix 1. Search strategies
| Database | Period of search | Search strategy |
| The Cochrane Hepato‐Biliary Group Controlled Trials Register | 1996 to Sept 2010 | ('health care worker*' or 'health personnel' or 'HCWs' ) and ( 'virus disease*' or 'virus*' or 'viral infect*') |
| EMBASE | 1974 to Sept 2010 |
#6 #5 AND [humans]/lim AND [embase]/lim #5 #3 AND #4 #4 [randomized controlled trial]/lim OR [controlled clinical trial]/lim OR random* OR 'double blind' OR 'single blind' OR (singl* OR doubl* OR trebl* OR tripl* AND (blind* OR mask*)) OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'triple blind procedure'/exp OR placebo* OR 'controlled study'/exp OR 'cross sectional study'/exp OR 'crossover procedure'/exp OR 'latin square design'/exp OR 'follow up'/exp OR 'comparative study'/exp OR 'evaluation studies'/exp OR 'evaluation study' OR prospectiv* OR volunteer*] #3 #1 AND #2 #2 'health care personnel'/exp OR 'health care personnel' OR 'health care worker'/exp OR 'health care worker' OR 'health care workers' OR 'health care facilities and services'/exp OR 'medical profession'/exp OR 'nursing as a profession'/exp OR ('virus transmission'/exp AND 'patient'/exp AND professional) #1 'needlestick injury'/exp OR needlestick* OR 'needle stick'/exp OR 'sharp injury' OR 'sharp injuries' OR 'sharp medical' OR 'sharp instrument' OR 'sharp needle' OR 'sharp needles' OR sharps OR 'percutaneous exposure' OR 'percutaneous injury' OR 'percutaneous injuries' OR 'percutaneous trauma' OR 'stick injury' OR 'stick injuries' OR 'stab wound'/exp OR 'face injury'/de OR 'eye injury'/de OR 'arm injury'/de OR 'hand injury'/de OR 'needle'/exp OR (splash* AND ('blood'/exp OR blood OR secretion* OR fluid* OR 'body fluid'/exp OR 'body fluids'/exp)) |
| Wiley InterScience: Cochrane Library Databases: CENTRAL and NHSEED | 1993 to Sept 2010 |
#3 #1 AND #2 #2 EXP Needlestick Injuries (MeSH) OR needlestick* OR "needle stick OR "needle sticks" OR "percutaneous exposure" OR "percutaneous exposures" OR "percutaneous injury" OR "percutaneous injuries2 OR "stick injury" OR "stick injuries" OR Wounds, Stab (MeSH) OR Wounds, Penetrating (MeSH) OR Facial injuries (MeSH) OR EXP Eye Injuries, Penetrating (MeSH) OR Forearm Injuries (MeSH) OR EXP Hand Injuries (MeSH) OR [splash* AND blood OR secretion* OR fluid* OR EXP Body Fluids (MeSH) OR EXP Bodily Secretions (MeSH)] #1 EXP Health Occupations (MeSH) OR EXP Health Personnel (MeSH) OR EXP Health Facilities (MeSH) OR "health care worker" OR "health care workers" OR Disease Transmission, patient‐to‐Professional (MeSH) |
| Science Citation Index Expanded | 1986 to 5 October 2010 |
#4 #1 AND #2 AND #3 #3 TS=(random* OR control* OR trial OR trials OR "single blind" OR "double blind" OR "triple blind" OR "latin square" OR placebo* OR comparative OR "follow up" OR prospectiv* OR "cross over" OR volunteer*) #2 TS=(needlestick* OR "needle stick" OR "needle sticks" OR "stick injury" OR "stick injuries" OR "wound stab" OR "stab wound" OR "penetrating wound" OR "penetrating wounds") OR TS=(sharp* AND ( injury OR injuries OR medical OR instrument*)) OR TS=(percutaneous AND (exposure OR exposures OR injury OR injuries)) OR TS=(injur* AND (facial OR eye OR eyes OR arm OR hand OR finger OR fingers)) OR TS=(splash* AND (blood OR secretion* OR fluid OR fluids)) OR TS="blood borne infection" #1 TS=("health care worker" OR "health care workers" OR "health occupations" OR "health personnel" OR physician* OR nurse* OR hospital* OR clinic OR clinics) |
| CINAHL | 1982 to Sept 2010 |
#5 #3 AND #4 #4 "randomized controlled trial" or "clinical trials" or "clinical trial" or "random allocation" or "double blind". or "single blind" or ((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)) or "latin square" or placebo# or random* or "research design" or "comparative study" or "comparative studies" or "evaluation study" or "evaluation studies" or "follow up study" or "follow up studies" or "prospective study" or "prospective studies" or "cross over study" or "cross over studies" or control* or prospective* or volunteer or (MH "Clinical Trials+") or (MH "Nonrandomized Trials") or (MH "Crossover Design") #3 #1 AND #2 #2 TX "needlestick injury" or needlestick# or "needle stick" or "needle sticks" or "sharp injury" or "sharp injuries" or "sharp medical device" or "sharp medical devices" or "sharp instrument" or "sharp instruments" or "sharp needle" or "sharp needles" or "percutaneous exposure" or "percutaneous exposures" or "percutaneous injury" or "percutaneous injuries" or "stick injury" or "stick injuries" or "wounds, stab" or "wounds, penetrating" or "facial injuries" or "eye injuries, penetrating" or "arm injuries" or "forearm injuries" or "hand injuries" or "finger injuries" or (splash# and (blood or secretion# or fluid#)) or ("occupational exposure" and ("body fluid" or "body fluids" or blood)) #1 (MH "Health Occupations") OR health occupations or (MH "Health Personnel+") or (MH "Health Facilities+") OR health facilities or TX "health care worker" or TX "health care workers" or (MH "Personnel, Health Facility+") or (MH "Occupational Health Services+") or (MH "Occupational Hazards+") or (MH "Occupational Exposure") or TX "health care personnel" or (MH "Health Personnel+") or (MH "HIV Infections+") |
| OSH UPDATE (NIOSHTIC‐2 and CISDOC) | NIOSHTIC‐2: 1900 to Sept 2010 CISDOC: 1987 to Sept 2010 |
#15 #13 AND #14 #14 PY{2007} OR PY{2008} OR PY{2009} #13 #7 AND #12 #12 #8 OR #11 #11 #9 AND #10 #10 GW{blind* OR mask*} #9 GW{singl* OR doubl* OR tripl* OR trebl*} #8 GW{random* OR control* OR trial OR trials OR comparativ* OR evaluation* OR "latin square" OR placebo OR "follow up" OR prospectiv* OR "cross over" OR volunteer*} #7 #1 AND #6 #6 #2 OR #5 #5 #3 AND #4 #4 GW{splash*} #3 GW{blood OR fluid* OR secretion*} #2 GW{"sharp medical" OR "sharp instrument" OR "sharp instruments" OR needlestick* OR "needle stick" OR "needle sticks" OR "sharp injury" OR "sharp injuries" OR "stab wound" OR "stab wounds" OR "wound penetrating" OR "stick injury" OR "stick injuries" OR "percutaneous injury" OR "percutaneous injuries" OR "percutaneous exposure" OR "percutaneous exposures" OR "sharp needle" OR "sharp needles"} #1 GW{nurse OR nurses OR physician OR physicians OR hospital* OR "health occupation" OR "health occupations" OR "health personnel" OR "health care personnel" OR "health care worker" OR "health care workers" OR "health worker" OR "health workers"} |
| MEDLINE in PubMed | from 1950 to Sept 2010 |
#5 Search #1 AND #2 AND (#3 OR #4) #4 Search effect*[tw] OR control[tw] OR controls*[tw] OR controla*[tw] OR controle*[tw] OR controli*[tw] OR controll*[tw] OR control'*[tw] OR evaluation*[tw] OR program*[tw] #3 ("Randomized Controlled Trial"[pt] OR "Controlled Clinical Trial"[pt] OR "Randomized Controlled Trials as Topic"[mh] OR "Random Allocation"[mh] OR "Double‐Blind Method"[mh] OR "Single‐Blind Method"[mh] OR "Clinical Trial"[pt] OR "Clinical Trials as Topic"[mh] OR "clinical trial"[tw] OR ((singl*[tw] OR doubl*[tw] OR trebl*[tw] OR tripl*[tw]) AND (mask*[tw] OR blind*[tw])) OR "latin square"[tw] OR Placebos[mh] OR placebo*[tw] OR random*[tw] OR "Research Design"[mh:noexp] OR "Comparative Study"[pt] OR "Evaluation Studies as Topic"[mh] OR "Follow‐up Studies"[mh] OR "Prospective Studies"[mh] OR "Cross‐over Studies"[mh] OR control[tw] OR controls*[tw] OR controla*[tw] OR controle*[tw] OR controli*[tw] OR controll*[tw] OR control'*[tw] OR prospectiv*[tw] OR volunteer*[tw]) NOT (Animals[mh] NOT Humans[mh) #2 "Needlestick injuries"[mh] OR needlestick*[tw] OR "needle stick"[tw] or "needle sticks"[tw] OR "sharp injury"[tw] OR "sharp injuries"[tw] OR sharps[tw] OR "sharp medical device"[tw] OR "sharp medical devices"[tw] OR "sharp instrument"[tw] OR "sharp instruments"[tw] OR "sharp medical instrument"[tw] OR "sharp medical instruments"[tw] OR "sharp needle"[tw] OR "sharp needles"[tw] OR "percutaneous exposure"[tw] OR "percutaneous exposures"[tw] OR "percutaneous injury"[tw] OR "percutaneous injuries"[tw] OR "stick injury"[tw] OR "stick injuries"[tw] OR "Wounds, Stab"[mh:noexp] OR "Wounds, Penetrating"[mh:noexp] OR "Facial injuries"[mh:noexp] OR "Eye Injuries, Penetrating"[mh] OR "Arm Injuries"[mh:noexp] OR "Forearm Injuries"[mh:noexp] OR "Hand Injuries"[mh] OR (splash* AND (blood[tw] or secretion*[tw] OR fluid*[tw] OR "Body Fluids"[mh])) #1 "Health Occupations"[mh] OR "Health Personnel"[mh] OR "Health Facilities"[mh] OR "health care worker"[tw] OR "health care workers"[tw] OR "Infectious Disease Transmission, Patient‐to‐Professional"[mh] |
| PsycINFO (OvidSP) | 1967 to Sept 2010 |
#5 limit 4 to all journals #4 #1 AND #2 AND #3 #3 random* OR control* OR trial OR trials OR comparativ* OR evaluation* OR ((singl* OR doubl* OR tripl* OR trebl*) AND (blind* OR mask*)) OR "latin square" OR placebo* OR "follow up" OR prospectiv* OR "cross over" OR volunteer* #2 (splash* AND (blood OR secretion* OR fluid OR fluids)) OR ("eye injuries" AND penetrating) OR (wound* AND (stab OR penetrating)) OR "percutaneous exposure" OR "percutaneous exposures" OR "percutaneous injury" OR "percutaneous injuries" OR "stick injury" OR "stick injuries" OR "sharp injury" OR "sharp injuries" OR "sharp medical" OR "sharp instrument" OR "sharp instruments" OR "sharp needle" OR "sharp needles" OR needlestick* OR "needle stick" OR "needle sticks" #1 (nursing or nurse or nurses or physician or physicians or "health care personnel" or "health personnel" or "health care worker" or "health care workers" or "Clinicians*" or "Dentist*" or "Health‐Personnel" or "Medical Personnel" or "Military‐Medical‐Personnel" or "Nurses*" or "Physician*" or "Psychiatric‐Hospital‐Staff*" or "medical students" or "hospitals" or "occupational exposure" or "occupational exposures").mp. [mp=title, abstract, heading word, table of contents, key concepts] |
| LILACS | Sept 2010 | "Health Occupations" or "Health Personnel" OR "Health Facilities" OR "health care worker" OR "health care workers" OR "Disease Transmission, Patient‐to‐Professional" OR "INJURIES" or "WOUNDS AND INJURIES/PC" or "accidents, OCCUPATIONAL" or "injuries, poisonings, and OCCUPATIONAL diseases" or "OCCUPATIONAL exposure" or "OCCUPATIONAL health policy" or "OCCUPATIONAL risks" OR "INJURIES" or "WOUNDS AND INJURIES/PC" or "accidents, OCCUPATIONAL" or "injuries, poisonings, and OCCUPATIONAL diseases" or "OCCUPATIONAL exposure" or "OCCUPATIONAL health policy" or "OCCUPATIONAL risks" [Descritor de assunto] and "CLINICAL TRIAL" OR "CLINICAL TRIAL, PHASE I" OR "CLINICAL TRIAL, PHASE II" OR "CLINICAL TRIAL, PHASE III" OR "CLINICAL TRIAL, PHASE IV" OR "COMPARATIVE STUDY" OR "CONTROLLED CLINICAL TRIAL" OR "EVALUATION STUDIES" OR "META‐ANALYSIS" OR "MULTICENTER STUDY" OR "RANDOMIZED CONTROLLED TRIAL" OR "REVIEW" [Tipo de publicação] and not "ANIMALS" or "HUMANS" [Palavras] |
Appendix 2. Updated search 27 April 2011
PubMed
(taper* OR blunt* OR protective) AND Needle* AND ("Randomized Controlled Trial"[pt] OR "Controlled Clinical Trial"[pt] OR "Randomized Controlled Trials as Topic"[mh] OR "Random Allocation"[mh] OR "Double‐Blind Method"[mh] OR "Single‐Blind Method"[mh] OR "Clinical Trial"[pt] OR "Clinical Trials as Topic"[mh] OR "clinical trial"[tw] OR ((singl*[tw] OR doubl*[tw] OR trebl*[tw] OR tripl*[tw]) AND (mask*[tw] OR blind*[tw])) OR "latin square"[tw] OR Placebos[mh] OR placebo*[tw] OR random*[tw] OR "Research Design"[mh:noexp] OR "Comparative Study"[pt] OR "Evaluation Studies as Topic"[mh] OR "Follow‐up Studies"[mh] OR "Prospective Studies"[mh] OR "Cross‐over Studies"[mh] OR control[tw] OR controls*[tw] OR controla*[tw] OR controle*[tw] OR controli*[tw] OR controll*[tw] OR control'*[tw] OR prospectiv*[tw] OR volunteer*[tw]) NOT (Animals[mh] NOT Humans[mh) N=68 references
EMBASE
(taper* OR blunt* OR protective) AND needle* AND ([randomized controlled trial]/lim OR [controlled clinical trial]/lim OR random* OR 'double blind' OR 'single blind' OR (singl* OR doubl* OR trebl* OR tripl* AND (blind* OR mask*)) OR 'single blind procedure'/exp OR 'double blind procedure'/exp OR 'triple blind procedure'/exp OR placebo*) N=211 references
Data and analyses
Comparison 1. Blunt versus sharp suture needles.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Glove perforation rate | 10 | Rate Ratio (Fixed, 95% CI) | 0.46 [0.38, 0.54] | |
| 2 Needle Stick Injuries | 5 | 1017 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.14, 0.68] |
| 3 Ease of use of Needle | 1 | 400 | Mean Difference (IV, Fixed, 95% CI) | ‐18.0 [‐28.64, ‐7.36] |
| 4 Ease of use of needle | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [1.01, 1.28] |
| 5 Force needed | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.19, 0.51] |
| 6 Sensitivity to ROB | 10 | Rate Ratio (Fixed, 95% CI) | 0.46 [0.38, 0.54] | |
| 6.1 High Risk of Bias | 7 | Rate Ratio (Fixed, 95% CI) | 0.45 [0.38, 0.55] | |
| 6.2 Low Risk of Bias | 3 | Rate Ratio (Fixed, 95% CI) | 0.46 [0.29, 0.72] | |
| 7 Subgroups Type of Operation | 10 | Risk Ratio (Fixed, 95% CI) | 0.46 [0.38, 0.54] | |
| 7.1 Abdominal Closure and Cesarean Section | 6 | Risk Ratio (Fixed, 95% CI) | 0.45 [0.37, 0.54] | |
| 7.2 Vaginal Repair | 2 | Risk Ratio (Fixed, 95% CI) | 0.59 [0.30, 1.20] | |
| 7.3 Hip Replacement | 2 | Risk Ratio (Fixed, 95% CI) | 0.43 [0.24, 0.76] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ablett 1998.
| Methods | Study design: randomised controlled trial. Object of randomisation: patients. | |
| Participants | UK. HCWs performing suturing of perineal tears and episiotomies including perineal skin. Intervention group n = 104 surgeon‐operations. Control group n = 91 surgeon operations. Number observed: 195 pairs of gloves. | |
| Interventions | Suturing with blunt tipped needles. The control group used sharp needles. | |
| Outcomes | Outcome: The number of glove perforations and reported needlestick injuries. Perforation detection: The gloves were filled with air and then immersed in water and perforations were noted as air bubbles.The gloves were thereafter filled with water and perforations were noted as jets of water. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | randomised allocation |
| Allocation concealment (selection bias) | Low risk | into unmarked envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | into unmarked envelopes; blinding to type of needle is impossible for surgeons |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | not reported |
| Selective reporting (reporting bias) | Low risk | all outcomes reported |
Hartley 1996.
| Methods | Study design: randomised controlled trial. Objects randomised: patients. | |
| Participants | UK. Consultants or registrars performing mass closure of the abdomen: fascial and muscle layers. Number studied: 85 patients. Intervention group n = 46 surgeon‐operations, control group n = 39 surgeon‐operations, 85 pairs of gloves observed. Gloves changed before closure commenced. | |
| Interventions | Use of suture needles with blunted end. Control group used conventional sharp pointed suture needles. | |
| Outcomes | Number of perforated glove pairs per total number of procedures. Perforation detection: firstly the gloves were filled with air, immersed in water and perforations were noted as air bubbles. Secondly, the gloves were filled with water and perforations were noted as jet of water. For the second half of the study additional testing was performed with a specifically designed electrical testing device. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | randomisation by random number generator |
| Allocation concealment (selection bias) | Unclear risk | not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not reported; blinding to type of needle is impossible for surgeons |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | no attrition |
| Selective reporting (reporting bias) | Low risk | all outcomes reported |
Meyer 1996.
| Methods | Study design: randomised controlled trial according to operation date and time. Object of randomisation: operations | |
| Participants | Germany. Attending surgeon and assistant during abdominal closure: fascia and muscle. Number studied 100 operations (400 gloves). Intervention group n = 98 surgeon‐operations (196 gloves) Control group n = 102 surgeon‐operations (204 gloves) Gloves changed before closure. | |
| Interventions | Use of blunt needles to close the abdominal fascia. Control group used sharp needles | |
| Outcomes | Outcome 1. Number of perforations in gloves. 2. Force needed to use the needle 3. Ease of use of the needle. Gloves were filled with water and perforations were noted as jets of water | |
| Notes | Information from author:The surgeon called the study nurse while changing his gloves before closure of the laparotomy. Therefore, only elective surgery has been included in this study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done according to operation date and time according to a random number list. |
| Allocation concealment (selection bias) | Low risk | Randomisation was done according to operation date and time |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported; not possible |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The person, who assessed the globes, identified the procedure by participant´s name + OP‐book number. Surgeon´s opinion was evaluated separately. (information from author) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All gloves reported |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
Mingoli 1996.
| Methods | Study design: randomised controlled trial. Object of randomisation: procedures. | |
| Participants | Italy. Attending surgeons, 3rd to 4th year residents and medical students performing abdominal procedures: muscle and fascia. Number studied: 100 operations (1560 gloves). Intervention group n = 300 surgeon operations (780 gloves). Control group n = 300 surgeon‐operations (780 gloves). Gloves changed before closure. | |
| Interventions | Use of blunt needles in closure of the abdominal fascia. Control group used sharp needles. | |
| Outcomes | Outcome: 1. Number of needlestick injuries per total number of operations; 2. Number of perforations per total number of gloves. Perforation detection: The gloves were filled with water and perforations were noted as jets of water. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | by random number allocation |
| Allocation concealment (selection bias) | Unclear risk | not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not reported; blinding to type of needle is impossible for surgeons |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | observers assessed outcome |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | all gloves tested |
| Selective reporting (reporting bias) | Low risk | all outcomes reported |
Nordkam 2005.
| Methods | Study design: randomised controlled trial. Object of randomisation: patients. | |
| Participants | Netherlands. Surgeons and assistants performing laparotomies, abdominal closure: fascia. Number studied: 200 procedures, 400 operators and 406 pairs of gloves. Intervention group n = 200 surgeon‐operations. Control group n = 100 surgeon‐operations. Gloves changed before skin closure. | |
| Interventions | Use of blunt‐tapered needles. Control group used sharp needles. | |
| Outcomes | Outcome: Number of procedures with one or more glove perforations per total number of procedures. Outcome calculated: holes in gloves per operator per operation Perforation detection: The gloves were filled with water and perforations were noted as jets of water. Secondary outcome: Ease of use of the needles. |
|
| Notes | We received additional information from the authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | randomisation by envelope; authors wrote that randomisation was based on a computer generated random number |
| Allocation concealment (selection bias) | Low risk | "just before closure of the fascia"; randomisation by envelope |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | team was aware of type of needle used; blinding to type of needle is impossible for surgeons |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | not reported; authors wrote that observer was blind to which needle was used |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | all gloves retrieved |
| Selective reporting (reporting bias) | Low risk | all outcomes reported |
Rice 1996.
| Methods | Study design: randomised controlled trial. Object of randomisation: operations. | |
| Participants | Ireland. Surgeons performing deep wound closure in primary total hip replacement surgery: fascia, fat and muscle not skin. Number studied: 68 operations. Intervention group n = 34 surgeon‐operations (number of gloves not reported). Control group n = 34 surgeon operations (128 gloves). Fresh outer gloves put on before wound closure and changed again before skin closure. | |
| Interventions | Use of taper pointed suture needle. Control group used standard pointed needles. | |
| Outcomes | Outcome: 1. Number of perforations per total number of gloves; 2. Number of glove perforations per total number of operations. Perforation detection: The gloves were filled with water and perforations were noted as jets of water. | |
| Notes | We assumed that the number of glove pairs in experimental group was the same as the number of procedures, and used outer glove perforations as outcome. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | operation randomly selected |
| Allocation concealment (selection bias) | Unclear risk | not reported; blinding to type of needle is impossible for surgeons |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4/68 pairs of gloves missing |
| Selective reporting (reporting bias) | Low risk | all outcomes reported |
Sullivan 2009.
| Methods | Study design: randomised controlled trial. Object of randomisation: operations. | |
| Participants | USA. Surgeons and assistants performing caesarean sections. Closure of all anatomical layers. Number studied: 194 operations. Intervention group n = 204 surgeon‐operations. Control group n = 204 surgeon‐operations. All gloves collected. | |
| Interventions | Use of blunt needles. The control group used sharp needles. | |
| Outcomes | Outcome: number of glove perforations per operation. Perforation detection: the gloves were filled with water and perforations were noted as jets of water. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computerised random sequence generator |
| Allocation concealment (selection bias) | Unclear risk | surgeon nor assistant blinded to randomisation outcome |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | surgeon nor assistant blinded to randomisation outcome; blinding to type of needle is impossible for surgeons |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | the (testing) author was blind to which needle had been used |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 100% completion of surveys |
| Selective reporting (reporting bias) | Low risk | all outcomes reported |
Thomas 1995.
| Methods | Study design: randomised controlled study. Object of randomisation: procedures. | |
| Participants | UK. Surgeons performing caesarean sections, closing the uterine wound. Number studied: 80 procedures. Sizes of intervention or control group not reported but assumed to be 40 and 40 surgeon‐operations. Glove change not reported. | |
| Interventions | Use of blunt‐tipped needles. Control group used sharp‐tipped needles. | |
| Outcomes | Outcome: percentage of perforated gloves. Detection method not reported but we assumed that this was the combined air and water method developed by one of the authors. | |
| Notes | We used the number of perforated gloves per total number of procedures as outcome. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | a random allocated study |
| Allocation concealment (selection bias) | Unclear risk | not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not reported; blinding to type of needle is impossible for surgeons |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not reported |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | not reported |
| Selective reporting (reporting bias) | Unclear risk | no description in methods |
| Other bias | High risk | The study design made 160 patients desirable but due to surgeons preference at that time only 80 patients were enrolled |
Wilson 2008.
| Methods | Study design: randomised controlled trial. Object of randomisation: patients. | |
| Participants | USA. Physicians performing obstetrical laceration repairs, needle used for whole procedure. Number studied: 438 procedures. Intervention group n = 217 surgeon‐operations. Control group n = 221 surgeon operations. All gloves collected. | |
| Interventions | Use of blunt needles. Control group used sharp needles. | |
| Outcomes | Outcome: number of glove perforations per total number of operations (also in RevMan analyses) but all surgeons were single gloved. Perforation detection: The gloves were filled with water and perforations were noted as jets of water. Secondary outcome: user satisfaction. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer random sequence generator |
| Allocation concealment (selection bias) | Unclear risk | surgeons not blinded to randomisation outcome |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | surgeons not blinded to randomisation outcome; blinding to type of needle is impossible for surgeons |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | the investigator was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | all pairs of gloves were collected |
| Selective reporting (reporting bias) | Low risk | all outcomes reported |
Wright 1993.
| Methods | Study design: randomised controlled trial. Object of randomisation: operations. | |
| Participants | UK. 17 surgeons performing standard wound closure after hip arthroplasties, skin closed with staple machine. Number studied: 69 operations. Surgeons were double gloved. We used only holes in outer gloves for the outcome. Intervention group n = 38 surgeon‐operations. Control group n = 31 surgeon‐operations. Outer pair of gloves changed before insertion of prosthetic components and before wound closure. | |
| Interventions | Use of blunt taper point suture needles. Control group used standard cutting needles. | |
| Outcomes | Outcome: number of outer glove perforations per total number of outer gloves. Perforation detection: The gloves were filled with water and perforations were noted as jets of water. Secondary outcome: Self‐reports of needlestick injuries, ease of use of the needle. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | allocated preoperatively by a random number |
| Allocation concealment (selection bias) | Unclear risk | not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not reported; blinding to type of needle is impossible for surgeons |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 138 gloves from 69 operations reported |
| Selective reporting (reporting bias) | Unclear risk | all outcomes reported |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bebbington 1996 | Not a blunt needle but a device |
| Botet 1998 | Not a blunt needle but a device |
| Monz 1991 | Not a randomised study |
| Tydeman 1995 | Not a randomised study |
Differences between protocol and review
We performed a subgroup analysis of types of operations that was not stated in the protocol.
Contributions of authors
Annika Parantainen is the co‐ordinator of the review work. She participated in the study selection, the data extraction and the writing of the review. Marie‐Claude Lavoie and Manisha Pahwa participated in the study selection and the data extraction. Jos Verbeek participated in the study selection, the data extraction, offered methodological and statistical support and wrote the text of the review.
Sources of support
Internal sources
Occupational Health and Safety Review Group, Finland.
External sources
FinOHTA, Finland.
Declarations of interest
There are no conflicts of interests.
Edited (no change to conclusions), comment added to review
References
References to studies included in this review
Ablett 1998 {published data only}
- Ablett JC, Whitten M, Smith JR. Do blunt tipped needles reduce the risk of glove puncture and needlestick injury in the suture of episiotomy and perineal repair?. Journal of Obstetrics and Gynaecology 1998;18(5):478‐9. [DOI] [PubMed] [Google Scholar]
Hartley 1996 {published data only}
- Hartley JE, Ahmed S, Milkins R, Naylor G, Monson JR, Lee PW. Randomized trial of blunt‐tipped versus cutting needles to reduce glove puncture during mass closure of the abdomen. British Journal of Surgery 1996;83:156‐7. [DOI] [PubMed] [Google Scholar]
Meyer 1996 {published data only}
- Meyer D, Hamelmann GW, Timmermann W, Thiede A. The risk of needlestick injuries during abdominal closure. Zentralblatt für Chirurgie 1996;121:30‐4. [PubMed] [Google Scholar]
Mingoli 1996 {published data only}
- Mingoli A, Sapienza P, Sgarzini G, Luciani G, Angelis G, Modini C, et al. Influence of blunt needles on surgical glove perforation and safety for the surgeon. The American Journal of Surgery 1996;172(5):512‐7. [DOI] [PubMed] [Google Scholar]
Nordkam 2005 {published data only}
- Nordkam RAG, Bluyssen SJM, Goor H, Millat B. Randomized clinical trial comparing blunt tapered and standard needles in closing abdominal fascia. World Journal of Surgery 2005;29(4):441‐5. [DOI] [PubMed] [Google Scholar]
Rice 1996 {published data only}
- Rice JJ, McCabe JB, McManus F. Needle stick injury. Reducing the risk. International Orthopaedics 1996;20:132‐3. [DOI] [PubMed] [Google Scholar]
Sullivan 2009 {published data only}
- Sullivan S, Williamson B, Wilson LK, Korte JE, Soper D. Blunt needles for the reduction of needlestick injuries during cesarean delivery: a randomized controlled trial. Obstetrics and Gynecology 2009;114(2 Pt 1):211‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Thomas 1995 {published data only}
- Thomas PB, Falder S, Jolly M, Saunders NJG, Smith JR. The role of blunt tipped needles and a new needleholder in reducing needlestick injury. Journal of Obstetrics and Gynaecology 1995;15:336‐8. [Google Scholar]
Wilson 2008 {published data only}
- Wilson LK, Sullivan S, Goodnight W, Chang EY, Soper D. The use of blunt needles does not reduce glove perforations during obstetrical laceration repair. American Journal of Obstetrics and Gynecology 2008;199:639.e1‐9.e4. [DOI] [PubMed] [Google Scholar]
Wright 1993 {published data only}
- Wright KU, Moran CG, Briggs PJ. Glove perforation during hip arthroplasty. A randomised prospective study of a new taperpoint needle. Journal of Bone and Joint Surgery 1993;75‐B(6):918‐20. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bebbington 1996 {published data only}
- Bebbington MW, Treissman MJ. The use of a surgical assist device to reduce glove perforations in postdelivery vaginal repair: A randomized controlled trial. American Journal of Obstetrics and Gynecology 1996;175(4):862‐6. [DOI] [PubMed] [Google Scholar]
Botet 1998 {published data only}
- Botet X, Serra J, Padrós R, López S, Boldó E, Llauradó JM, et al. Efficacy of PdB in preventing intraoperative risk of infectious diseases. World Journal of Surgery 1998;22:1092‐7. [DOI] [PubMed] [Google Scholar]
Monz 1991 {published data only}
- Monz FJ, Fowler JM, Farias‐Eisner R, Nash TJ. Blunt needles in fascial closure. Surgery, Gynecology & Obstetrics 1991;173:147‐8. [PubMed] [Google Scholar]
Tydeman 1995 {published data only}
- Tydeman GSJ. Risks to surgeons: a comparison of blunt and sharp tipped suture needles. Journal of Obstetrics and Gynaecology 1995;15:333‐5. [Google Scholar]
Additional references
ACS 2011
- American College of Surgeons. Statement on sharps safety. Statements of the College 2011.
Akduman 1999
- Akduman D, Kim LE, Parks RL, L'Ecuyer PB, Mutha S, Jeffe DB, et al. Use of personal protective equipment and operating room behaviors in four surgical subspecialties: personal protective equipment and behaviors in surgery. Infection Control and Hospital Epidemiology 1999;20(2):110‐4. [DOI] [PubMed] [Google Scholar]
Anderson 2008
- Anderson ER, Gates S. Techniques and materials for closure of the abdominal wall in caesarean section. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD004663.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ansa 2002
- Ansa VO, Udoma EJ, Umoh MS, Anah MU. Occupational risk of infection by human immunodeficiency and hepatitis B viruses among health workers in south‐eastern Nigeria. East African Medical Journal 2002;79(5):254‐6. [DOI] [PubMed] [Google Scholar]
Bennett 1994
- Bennett NT, Howard RJ. Quantity of blood inoculated in a needlestick injury from suture needles. Journal of the American College of Surgeons 1994;178(2):107‐110. [PubMed] [Google Scholar]
Berguer 2005
- Berguer R, Heller PJ. Strategies for preventing sharps injuries in the operating room. Surgical Clinics of North America 2005;85:1299‐305. [DOI] [PubMed] [Google Scholar]
Brough 1988
- Brough SJ, Hunt TM, Barrie WW. Surgical glove perforations. British Journal of Surgery 1988;75:317. [DOI] [PubMed] [Google Scholar]
Catanzarite 2007
- Catanzarite V, Byrd K, McNamara M, Bombard A. Peventing needlestick injuries in obstetrics and gynecology. Obstetrics and Gynecology 2007;110(6):1399‐1403. [DOI] [PubMed] [Google Scholar]
Cheetham 2016
- Cheetham S, Thompson SC, Liira J, Afilaka OA, Liira H. Education and training for preventing sharps injuries and splash exposures in healthcare workers. Cochrane Database of Systematic Reviews 2016, Issue 1. [DOI: 10.1002/14651858.CD012060] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2005
- Chen W, Gluud C. Vaccines for preventing hepatitis B in health‐care workers. Cochrane Database of Systematic Reviews 2005, Issue Issue 4. [DOI: 10.1002/14651858.CD000100.pub3] [DOI] [PubMed] [Google Scholar]
Clarke 2002
- Clarke SP, Rockett JL, Sloane DM, Aiken LH. Organizational climate, staffing, and safety equipment as predictors of needlestick injuries and near‐misses in hospital nurses. American Journal of Infection Control 2002;30(4):207‐16. [DOI] [PubMed] [Google Scholar]
Doebbeling 2003
- Doebbeling BN, Vaughn TE, McCoy KD, Beekmann SE, Woolson RF, Ferguson KJ, et al. Percutaneous injury, blood exposure, and adherence to standard precautions: are hospital‐based health care providers still at risk?. Clinical Infectious Diseases 2003;37(8):1006‐13. [DOI] [PubMed] [Google Scholar]
Edlich 2003
- Edlich RF, Wind TC, Hill LG, Thacker JG, McGregor. Reducing accidental injuries during surgery. Journal of Long‐Term Effects of Medical Implants 2003;13(1):1‐10. [DOI] [PubMed] [Google Scholar]
Ellenbecker 1996
- Ellenbecker MJ. Engineering controls as an intervention to reduce worker exposure. American Journal of Industrial Medicine 1996;29(4):303‐7. [DOI] [PubMed] [Google Scholar]
Fisman 2002
- Fisman DN, Mittleman AM, Sorock GS, Harris AD. Willingness to pay to avoid sharps‐related injuries: a study in injured health care workers. American Journal of Infection Control 2002;30(5):283‐7. [DOI] [PubMed] [Google Scholar]
Fisman 2007
- Fisman DN, Harris AD, Rubin M, Sorock GS, Mittleman AM. Fatigue increases the risk of injury from sharp devices in medical trainees: results from a case‐crossover study. Infection Control and Hospital Epidemiology 2007;28(1):10‐7. [DOI] [PubMed] [Google Scholar]
Furlan 2009
- Furlan AD, Pennick V, Bombardier C, Tulder M. Cochrane Back Review Group, 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phil PA 1976) 2009;34:1929‐41. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 5.1.0.[updated March 2011]. The Cochrane Library, Available from: www.cochrane‐handbook.org.
Ilhan 2006
- Ilhan MN, Durukan E, Aras E, Turkcuoglu S, Aygun R. Long working hours increase the risk of sharp and needlestick injury in nurses: the need for new policy implication. Journal of Advanced Nursing 2006;56(5):563‐8. [DOI] [PubMed] [Google Scholar]
Jagger 2008
- Jagger J, Perry J, Gomaa A, Kornblatt Phillips E. The impact of US policies to protect healthcare workers from bloodborne pathogens: the critical role of safety‐engineered devices. Journal of Infection and Public Health 2008;1:62‐71. [DOI] [PubMed] [Google Scholar]
Jagger 2011
- Jagger J, Berguer R, Philips EK, Parker G, Gomaa AE. Increase in sharps injuries in surgical settings versus non‐surgical settings after passage of national needlestick legislation. Association of periOperative Registered Nurses Journal 2011;93(3):322‐30. [DOI] [PubMed] [Google Scholar]
Lavoie 2012
- Lavoie MC, Verbeek JH, Parantainen A, Pahwa M. Devices for preventing percutaneous exposure injuries caused by needles in health care personnel. Cochrane Database of Systematic Reviews 2012, Issue 4. [DOI: 10.1002/14651858.CD009740] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2008
- Lefebvre DR, Strande LF, Hewitt CW. An enzyme‐mediated assay to quantify inoculation volume delivered by suture needlestick injury: two gloves are better than one. Journal of the American College of Surgeons 2008;206(1):113‐22. [DOI] [PubMed] [Google Scholar]
Mast 2004
- Mast E, Mahoney F, Kane M, Margolis H. Hepatitis B vaccines. In: Plotkin OW editor(s). Vaccines. Philadelphia: Saunders, 2004:299‐337. [Google Scholar]
Meyers 2008
- Meyers DJ, Epling C, Dement J, Hunt D. Risk of sharp device‐related blood and body fluid exposure in operating rooms. Infection control and hospital epidemiology 2008;29:1139‐48. [DOI] [PubMed] [Google Scholar]
Miller 1994
- Miller SS, Sabharwal A. Subcuticular skin closure using a blunt needle. Annals of the Royal College of Surgeons England 1994;76:281. [PMC free article] [PubMed] [Google Scholar]
NIOSH 2008
- NIOSH. Use of blunt‐tip suture needles to decrease percutaneous injuries to surgical personnel. Safety and Health Information Bulletin 2008, issue 101:1‐4.
Oh 2005
- Oh HS, Yi SE, Choe KW. Epidemiological characteristics of occupational blood exposures of healthcare workers in a university hospital in South Korea for 10 years. Journal of Hospital Infection 2005;60(3):269‐75. [DOI] [PubMed] [Google Scholar]
Orji 2002
- Orji EO, Fasubaa OB, Onwudiegwu U, Dare FO, Ogunniyi SO. Occupational health hazards among health care workers in an obstetrics and gynaecology unit of a Nigerian teaching hospital. Journal of Obstetrics and Gynaecology 2002;22(1):75‐8. [DOI] [PubMed] [Google Scholar]
Parantainen 2012
- Parantainen A, Verbeek JH, Lavoie MC, Pahwa M. Extra gloves or special types of gloves versus a single pair of gloves for preventing percutaneous exposure injuries in healthcare personnel. Cochrane Database of Systematic Reviews 2012, Issue 1. [DOI: 10.1002/14651858.CD009573] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pruss‐Ustun 2005
- Pruss‐Ustun A, Rapiti E, Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health‐care workers. American Journal of Industrial Medicine 2005;48(6):482‐90. [DOI] [PubMed] [Google Scholar]
RevMan 2011 [Computer program]
- RevMan. Review Manager (RevMan). Version 5.1 for Windows. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Roberts 1999
- Roberts RB, Lincoff AS, Frankel RE. Occupational exposure to HIV in an urban university hospital setting. Brazilian Journal of Infectious Diseases 1999;3(2):50‐62. [PubMed] [Google Scholar]
Robinson 2002
- Robinson KA, Dickersin K. Development of a highly sensitive search strategy for the retrieval of reports of controlled trials using PubMed. International Journal of Epidemiology 2002;31(1):150‐3. [DOI] [PubMed] [Google Scholar]
Roelofs 2003
- Roelofs CR, Barbeau EM, Ellenbecker MJ, Moure‐Eraso R. Prevention strategies in industrial hygiene: a critical literature review. American Industrial Hygiene Association Journal 2003;64(1):62‐7. [DOI] [PubMed] [Google Scholar]
Smith 1988
- Smith JR, Grant JM. Does wearing two pairs of gloves protect against skin contamination?. BMJ 1988;297:1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 1990
- Smith JR, Grant JM. The incidence of glove puncture during caesarean section. Journal of Obstetrics and Gynaecology 1990;10:317‐8. [Google Scholar]
Smith 2006
- Smith DR, Choe MA, Jeong JS, Jeon MY, Chae YR, An GJ. Epidemiology of needlestick and sharps injuries among professional Korean nurses. Journal of Professional Nursing 2006;22(6):359‐66. [DOI] [PubMed] [Google Scholar]
Smith 2006b
- Smith DR, Mihashi M, Adachi Y, Nakashima Y, Ishitake T. Epidemiology of needlestick and sharps injuries among nurses in a Japanese teaching hospital. Journal of Hospital Infection 2006;64(1):44‐9. [DOI] [PubMed] [Google Scholar]
Sohn 2006
- Sohn JW, Kim BG, Kim SH, Han C. Mental health of healthcare workers who experience needlestick and sharps injuries. Journal of Occupational Health 2006;48(6):474‐9. [DOI] [PubMed] [Google Scholar]
Stafford 1998
- Stafford MK, Pitman MC, Nanthakumaran N, Smith JR. Blunt‐tipped versus sharp‐tipped needles: wound morbidity. Journal of Obstetrics and Gynaecology 1998;Jan 18(1):18‐9. [PUBMED: 15511994] [DOI] [PubMed] [Google Scholar]
Tarantola 2006
- Tarantola A, Golliot F, L'Heriteau F, Lebascle K, Ha C, Farret D, Bignon S, Smail A, Doutrellott‐Philippon C, Astagneau P, Bouvet E. Assessment of preventive measures for accidental blood exposure in operating theaters: a survey of 20 hospitals in Northern France. American Journal of Infection Control 2006;34:376‐382. [DOI] [PubMed] [Google Scholar]
Verbeek 2005
- Verbeek J, Salmi J, Pasternack I, Jauhiainen M, Laamanen I, Schaafsma F, et al. A search strategy for occupational health intervention studies. Journal of Occupational and Environmental Medicine 2005;62(10):682‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wallis 2007
- Wallis GC, Kim WY, Chaudhary BR, Henderson JJ. Perceptions of orthopaedic surgeons regarding hepatitis C viral transmission: a questionnaire survey. Annals of the Royal College of Surgeons of England 2007;89(3):276‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Watt 2008
- Watt AM, Patkin M, Sinnott MJ, Black RJ, Maddern GJ. Scalpel injuries in the operating theatre. BMJ 2008;336:1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
Watt 2010
- Watt AM, Patkin M, Sinnott MJ, Black RJ, Maddern GJ. Scalpel safety in the operative setting: a systematic review. Surgery 2010;147(1):98‐106. [DOI] [PubMed] [Google Scholar]
WHO 2007
- World Health Organization. Needlestick injuries: implementation of pilot projects to reduce sharps injuries in health care workers. http://www.who.int/occupational_health/topics/needinjuries/en/index.html (Accessed 5 September 2007).
References to other published versions of this review
Parantainen 2008
- Parantainen A, Lavoie MC, Pahwa M, Verbeek JH. Prevention of percutaneous injuries with risk of hepatitis B, hepatitis C, or other viral infections for health care workers. Cochrane Database of Systematic Reviews 2008, Issue 2. [DOI: 10.1002/14651858.CD007197] [DOI] [Google Scholar]
Parantainen 2011
- Parantainen A, Verbeek JH, Lavoie MC, Pahwa M. Blunt versus sharp suture needles for preventing percutaneous exposure incidents in surgical staff. Cochrane Database of Systematic Reviews 2011, Issue 6. [DOI: 10.1002/14651858.CD009170] [DOI] [PMC free article] [PubMed] [Google Scholar]


