Abstract
Polydrug use is a common problem among patients in opioid-substitution treatment. Polydrug use has been reduced by administering abstinence-reinforcement contingencies in a sequence, such that a single drug is targeted until abstinence is achieved, and then an additional drug is targeted. The present study examined effects of administering abstinence-reinforcement contingencies sequentially based on time rather than on achieved abstinence. Participants accessed paid work (about $10/hr maximum) in the Therapeutic Workplace by providing urine samples three times per week. The urine samples were tested for opiates and cocaine. During an induction period, participants earned maximum pay independent of drug abstinence. Then, maximum pay depended upon urine samples that were negative for opiates. Two weeks later, maximum pay depended upon urine samples that were negative for both opiates and cocaine. Opiate and cocaine abstinence increased following administration of the respective contingencies. The time-based administration of abstinence reinforcement increased opiate and cocaine abstinence.
Keywords: abstinence reinforcement, contingency management, drug addiction, incentives, therapeutic workplace
Drug addiction is associated with a host of societal problems, including poverty (Center for Behavioral Health Statistics and Quality, 2018), unemployment (Henkel, 2011), HIV (Sullivan, Metzger, Fudala, & Fiellin, 2005), and death (Seth et al., 2018) Recent evidence suggests that in the United States, drug addiction and problems associated with it are becoming more common. A recent study estimated that more than 19.7 million Americans have a substance use disorder (Substance Abuse and Mental Health Services Administration, 2018, p. 34). Furthermore, the number of deaths resulting from drug overdose in 2017 (70,200 people; Centers for Disease Control and Prevention, 2019) was more than four times higher than the number recorded in 1999 (16,849; National Center for Health Statistics, 2017). Because of the severity of these problems and the large number of people affected by them, it is important to develop effective and efficient approaches to treat drug addiction.
Treatments based on principles of operant conditioning have decreased drug use (Bigelow & Silverman, 1999; see Silverman et al., 2019 for a review). These treatments are based on the assumption that drug use is operant behavior, which is maintained by the consequences it produces (Schuster & Thompson, 1969). Therefore, drug use and behavior associated with it, may be modified through established behavioral processes such as reinforcement, punishment, and extinction.
A highly effective operant approach to the treatment of drug addiction is abstinence reinforcement. Abstinence reinforcement arranges desirable consequences (e.g., money or vouchers) contingent upon the objective evidence of drug abstinence (Bigelow et al., 1981). Abstinence-reinforcement procedures have effectively established abstinence from a variety of drugs in a variety of populations, including abstinence from opiates or cocaine (e.g., Aklin et al., 2014; Silverman et al., 2001; Silverman et al., 2002), and tobacco (e.g., Donatelle et al., 2000; Heil et al., 2008; see Higgins et al. 2012 for a review) in pregnant and postpartum women, from opiates or cocaine in adults enrolled in methadone treatment (e.g., DeFulio et al., 2009; Preston et al., 2000; Silverman et al., 1996; Silverman et al., 1998; Donlin et al., 2008), from opiates and cocaine in out-of-treatment injection drug users (e.g., Holtyn et al., 2014a; Holtyn et al., 2014b), from tobacco in adolescents (e.g., Krishnan-Sarin et al., 2006), from cocaine and marijuana in cocaine-dependent men (e.g., Budney et al., 1991), and from alcohol in homeless, alcohol-dependent adults (e.g., Koffarnus et al. 2011).
Although abstinence reinforcement procedures have been effective in the treatment of drug addiction, the effectiveness of the procedures may be reduced when polydrug use (i.e., use of more than one drug) is targeted (Downey et al., 2000). Three abstinence-reinforcement methods have been applied to address polydrug use. The first method involves increasing the magnitude of the reinforcers delivered for drug abstinence (Dallery et al., 2001). Although this method is effective, costs associated with providing high-magnitude reinforcers may act as a barrier to wide-scale implementation by researchers and clinicians (Silverman et al., 1999). A second method involves dividing or splitting the total reinforcement across multiple drugs (Epstein et al. 2009). Although this method is potentially effective, it appears that when the reinforcer magnitude for drug abstinence is reduced, abstinence from that drug decreases. A third method involves administering the abstinence-reinforcement contingencies in a sequence, until participants achieve consistent abstinence from each drug (Budney et al., 1991; Holtyn et al., 2014a; Holtyn et al., 2014b). This method has effectively reduced polydrug use; however, in some situations, it may be impractical to wait to expose all participants to multiple contingencies until consistent abstinence is achieved. Long-term exposure to a single abstinence-reinforcement contingency requires sufficient funding to furnish regular urinalyses and staff to monitor each participant’s progress within each condition over an extended period. It also requires a degree of flexibility in the length of time that a participant can be exposed to a single condition and therefore places a limit on the number of conditions to which a participant can be exposed within a given period.
One way to address these barriers while retaining the strategy of sequential administration of abstinence-reinforcement contingencies is to administer the contingencies on the basis of time rather than on achieved abstinence. The present study evaluated effects of time-based, sequential administration of abstinence-reinforcement contingencies on opiate and cocaine abstinence. Whereas prior studies (Budney et al., 1991; Holtyn et al., 2014a; Holtyn et al., 2014b) exposed participants to conditions only after consistent abstinence was achieved, the present study changed conditions based solely on the passage of time.
Method
The results presented in this paper were collected as part of a two-phase clinical trial designed to evaluate effects of the Therapeutic Workplace’s Wage Supplement Model (Silverman et al.,2016) in promoting drug abstinence and employment. In Phase 1 of the trial, substance-abuse patients could earn stipends for participating in job-skills training in the Therapeutic Workplace. In Phase 2, the patients could earn wage supplements for community employment. To promote and maintain drug abstinence, maximum stipend and wage-supplement pay depended upon drug-negative urine samples. The present study took place in Phase 1 of the clinical trial, during which opiate and cocaine abstinence-reinforcement contingencies were administered sequentially based on the passage of time.
Setting and Participant Selection
The clinical trial was conducted in the Therapeutic Workplace at the Center for Learning and Health, a research and treatment unit at the Johns Hopkins Bayview Medical Center in Baltimore, MD. During the trial, participants earned money by attending the workplace and providing urine samples at a urinalysis laboratory when scheduled. The laboratory was located in close proximity to a workroom with individual workstations. Each workstation included a chair, desk, computer, monitor, mouse, and keyboard (see Silverman et al., 2007, for a detailed description of the Therapeutic Workplace setting and procedures).
Participants were recruited between November 2015 and April 2018 through community agencies that served the target population, street outreach, and a referral system in which study participants were paid for successfully referring others to the study. To qualify for the study, inclusion criteria required that an individual was at least 18 years old, enrolled in or eligible for methadone or buprenorphine treatment, living in or near Baltimore, unemployed, interested in obtaining employment, and used an opioid (methadone, buprenorphine, or heroin), as determined by metabolite concentrations in a urinalysis conducted prior to enrollment in the study. Participants were excluded from the study if they had active hallucinations, delusions, or thought disorders, had physical limitations that would interfere with their ability to use a computer keyboard, had current suicidal or homicidal ideation, or were currently considered a prisoner.
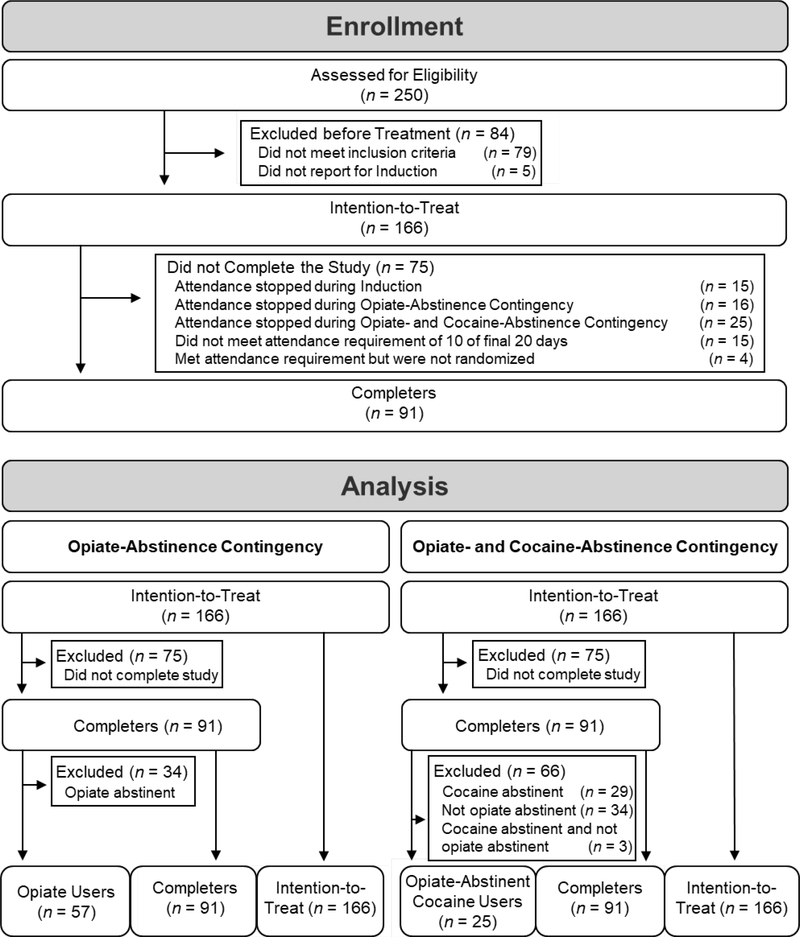
Figure 1 (top panel) is a consort flowchart that illustrates the enrollment of participants. Of the 250 people screened, 79 did not qualify. The remaining 171 were invited to attend the workplace. No participants declined participation, but five never reported to the workplace and were excluded from the study. The remaining 166 participants (i.e., the Intention-to-Treat group) were enrolled in the study. Participants were invited to attend the workplace for three months and were considered Completers if they attended the workplace on at least 10 of the final 20 days of work and were randomized to a group for Phase 2 of the study. The study consisted of three conditions: induction (five weeks), the opiate-abstinence contingency (two weeks), and the opiate- and cocaine-abstinence contingency (remainder of the three months). Of the 166 enrolled participants, 15 stopped attending the Therapeutic Workplace during induction, 16 stopped during the opiate-abstinence contingency, 25 stopped during the opiate- and cocaine-abstinence contingency, 15 continued attending the workplace periodically but did not meet the attendance requirement of working on at least 10 of the final 20 days of work, and four participants met the attendance requirement but did not complete the randomization process. At the end of the study, the 91 participants who completed Phase 1 (i.e., were “Completers”) continued to Phase 2 of the clinical trial. All procedures used were approved by the Johns Hopkins Medicine Institutional Review Board, and all participants provided written informed consent.
Figure 1.
Consort flowchart showing the enrollment of participants (top) and the classification of participants for purposes of data analysis (bottom).
Procedure
Participants were invited to work in the Therapeutic Workplace for three months. During that time, participants could access paid work for four hours each weekday (10am-12pm and 1pm-3pm). At the end of each day, a staff member loaded the money earned onto a reloadable visa card, which was issued to each participant during enrollment. Participants earned money from the combined total of two types of pay: performance pay and base pay. Performance pay was money participants earned from completing educational or job-skills training tasks. These tasks included a computer-based mathematics course (Individual Prescription for Achieving State Standards, iPASS; iLearn, 2019), a typing course using a QWERTY keyboard (Koffarnus et al., 2013), and a key pad course using a number pad (Koffarnus et al., 2013). Participants could earn approximately $2/hr in performance pay, but actual earnings varied depending on the difficulty of tasks and the performance of each participant. Base pay was the hourly pay participants earned for attendance. Participants could earn between $1 and $8/hr in base pay, depending on results of recent urinalyses and the requirements for reinforcement in the prevailing condition (described below).
Participants provided urine samples three times per week on mandatory urine days (typically on Mondays, Wednesdays, and Fridays). Participants provided samples in a bathroom attached to the laboratory under the observation of a same-sex laboratory staff member. The samples were then tested using Abbott Alere urine screening cups (Model No. I-DX-1147–022) for metabolites of select drugs, including morphine (opiates) and benzoylecgonine (cocaine). If a urine sample contained at least 300 ng/ml or 150 ng/ml of the tested metabolite (opiates and cocaine, respectively), it was judged positive for that drug. Abbott Alere urine screening cups test for adulterants and dilution, which can cause false-negative results in drug tests, by determining whether urinary characteristics (e.g., temperature, Oxidants/PCC, specific gravity, pH, nitrite, and creatinine) fall within the normal range. If a sample was judged to be diluted or contain adulterants, the sample was not accepted and the participant was required to submit a replacement urine sample on the same day.
Participants were excused from providing urine samples on days when the Therapeutic Workplace was closed due to bad weather, a holiday or a special event, or if the participant was admitted to a hospital or incarcerated. Excused samples were omitted from analyses and did not affect participant pay. On excused days resulting from bad weather, holidays, or a special event, participants earned the mean of their earnings on the day before and the day after the excused day. For planned excused days (i.e., holidays or special events), an attempt was made to collect a urine sample on the day before or the day after the excused day. Participants were excused for hospitalization or incarceration only if they attended the workplace on the weekdays immediately before and after the hospitalization or incarceration.
Conditions
Induction
After enrolling in the study, participants were exposed to the induction condition for five weeks. The present analysis focuses on the final two weeks of this period, during which time urine samples were collected and tested, but did not influence base pay, which remained at $8/hr. Participants were required to provide urine samples on scheduled days, but there were no consequences for failing to provide a scheduled urine sample.
Opiate-abstinence contingency
The opiate-abstinence contingency was in effect for two weeks immediately following induction. In this condition, each participant’s base pay depended on providing urine samples that tested negative for opiates. At the start of the condition, all participants earned the maximum amount of money in base pay ($8/hr). Each time a participant failed to provide a scheduled urine sample or provided a urine sample that tested positive for opiates, that participant’s base pay was reset to $1/hr. After being reset, the participant was required to provide a urine sample every weekday until that participant provided an opiate-negative urine sample. The participant’s base pay could be raised by $1/hr (to a maximum of $8/hr) each day that the participant met the opiate-abstinence criterion (i.e., provided an opiate-negative sample on the last mandatory urine day) and attended work for a minimum of 5 min. Although abstinence was targeted from both opiates and cocaine eventually, the opiate-abstinence contingency was administered first because participants were receiving an FDA-approved medication for opioid use disorder (methadone or buprenorphine) that can reduce opioid use. There is no FDA-approved medication for cocaine use disorder. Based on logic and experience, we expected that participants may be more likely to contact reinforcement for drug abstinence if opiate abstinence was targeted first.
Opiate- and cocaine-abstinence contingency
The opiate- and cocaine-abstinence contingency was in effect for the remainder of the three-month period following the two-week opiate-abstinence contingency period. As in the previous condition, base pay was reset to $1/hr every time a participant failed to provide a urine sample or provided a sample that tested positive for opiates; however, in this condition, base pay was also reset every time a urine sample tested positive for cocaine. Base pay could be raised by $1/hr (to a maximum of $8/hr) each day that a participant met the opiate- and cocaine-abstinence criterion (provided a urine sample that was negative for opiates and cocaine on the last mandatory urine day) and attended the workplace for at least 5 min.
Instructions
Before the start of each condition, participants received written and oral instructions that described the upcoming condition. Intermixed throughout the instructions, the participant was required to answer several multiple-choice questions based on the content of the instructions. Participants earned $0.20 for every answer that was correct on the initial answer, and $0.10 for every answer that was initially incorrect, but was subsequently corrected. (See Supplementary Material A–F for the instructions and multiple-choice questions used to introduce Therapeutic Workplace hours, urine testing, the rules of behavior, the pay system, the opiate-abstinence contingency, and the opiate- and cocaine-abstinence contingency).
Data Analysis
The data of interest in this study were the participants’ urinalysis results across the three conditions (i.e., induction, opiate-abstinence contingency, and opiate- and cocaine-abstinence contingency). Results were based on the final two weeks of induction (6 samples), two weeks of the opiate-abstinence contingency (6 samples), and a minimum of six weeks of the opiate- and cocaine-abstinence contingency (19 samples).
The bottom panel of Figure 1 shows the classification of participants for purposes of data analysis. Intention-to-Treat includes the 166 participants who began induction. Participants were eligible to complete Phase 1 and begin Phase 2 only if they attended the workplace during 10 of the final 20 work days of the opiate- and cocaine-abstinence contingency (see Supplementary Material G for the attendance requirement notification given to the participants). Completers includes the 91 participants who completed Phase 1 of the study – meaning that they did not drop out of the study, their attendance records did not prevent them from completing the study, and they were randomized to a group for Phase 2.
Two sub-categories of Completers were created to allow a more sensitive evaluation of effects of the opiate-abstinence and opiate- and cocaine-abstinence contingencies. An evaluation of the effects of the opiate-abstinence contingency on abstinence from opiates would be obscured if the analysis included data from participants who were already abstinent from opiates before they were exposed to the contingency. Therefore, Opiate Users included the 57 Completers who did not demonstrate consistent opiate abstinence during the six samples before the opiate-abstinence contingency (i.e., at least one mandatory sample was positive or missing). Similarly, an evaluation of effects of the opiate- and cocaine-abstinence contingency on cocaine abstinence would be obscured if the analysis included participants who were already abstinent from cocaine before exposure to the contingency. Another barrier to observing clear effects of the opiate- and cocaine-abstinence contingencies on cocaine abstinence is that participants could be prevented from contacting the reinforcer programmed for cocaine abstinence if they did not achieve abstinence from opiates before the opiate- and cocaine-abstinence contingency was administered. Opiate-Abstinent Cocaine Users included the 25 Completers who did not demonstrate consistent cocaine abstinence during the six samples before the opiate- and cocaine-abstinence contingency was administered, and who did demonstrate opiate abstinence during those samples. Baseline characteristics of participants that constitute each classification are shown in Table 1.
Table 1.
Participant characteristics at intake.
| Characteristic | Intention-to-Treat (n = 166) | Completers (n = 91) | Opiate Users (n = 57) | Opiate-Abstinent Cocaine Users (n =25) | ||||
|---|---|---|---|---|---|---|---|---|
| Demographic Characteristic, M (SD) | ||||||||
| Age in years | 48 | (10) | 48 | (10) | 47 | (9) | 48 | (8) |
| Drug purchases in past 30 days in $ | 361 | (516) | 259 | (369) | 326 | (409) | 367 | (422) |
| Income in past 30 days in $ | ||||||||
| Pension, benefits, or social security | 295 | (379) | 287 | (365) | 231 | (329) | 201 | (318) |
| Welfare | 198 | (174) | 187 | (150) | 205 | (157) | 189 | (128) |
| Mate, family, or friends | 39 | (171) | 26 | (72) | 22 | (56) | 20 | (32) |
| Illegal | 22 | (137) | 24 | (161) | 30 | (198) | 6 | (29) |
| Employment | 4 | (24) | 8 | (31) | 12 | (39) | 14 | (39) |
| BDI Score | 10 | (9) | 9 | (9) | 9 | (8) | 8 | (7) |
| Demographic Characteristic, n (%) | ||||||||
| Female | 73 | (44) | 41 | (45) | 27 | (47) | 12 | (48) |
| Race | ||||||||
| Black or African American | 104 | (63) | 51 | (56) | 30 | (53) | 13 | (52) |
| White | 56 | (34) | 36 | (40) | 25 | (44) | 12 | (48) |
| Hispanic or Cuban | 3 | (2) | 3 | (3) | 1 | (2) | 0 | (0) |
| American Indian | 3 | (2) | 1 | (1) | 1 | (2) | 0 | (0) |
| Married | 22 | (13) | 15 | (16) | 9 | (16) | 6 | (24) |
| Previously Incarcerated | 136 | (82) | 74 | (81) | 48 | (84) | 18 | (72) |
| Currently on parole or probation | 18 | (11) | 10 | (11) | 6 | (11) | 2 | (8) |
| High school diploma or GED | 98 | (59) | 60 | (66) | 39 | (68) | 19 | (76) |
| Usually unemployed in past 3 years | 72 | (43) | 37 | (41) | 27 | (47) | 15 | (60) |
| Retired or Disability | 50 | (30) | 30 | (33) | 15 | (26) | 6 | (24) |
| Living in Poverty | 162 | (98) | 90 | (99) | 57 | (100) | 25 | (100) |
| Drug use characteristics, n (%) | ||||||||
| Opiates | ||||||||
| Use in past 30 days | 112 | (67) | 51 | (56) | 39 | (68) | 15 | (60) |
| Primarily IV administration | 97 | (58) | 41 | (45) | 27 | (47) | 12 | (48) |
| Initial urinalysis positive | 69 | (42) | 33 | (36) | 27 | (47) | 10 | (40) |
| Cocaine | ||||||||
| Use in past 30 days | 108 | (65) | 48 | (53) | 35 | (61) | 21 | (84) |
| Primarily IV administration | 41 | (25) | 18 | (20) | 11 | (19) | 5 | (20) |
| Initial urinalysis positive | 109 | (66) | 46 | (51) | 34 | (60) | 22 | (88) |
Two types of analyses were conducted to address the problem of missing urine samples on days when urinalyses were scheduled: the missing-positive analysis and the missing-missing analysis. The missing-positive analysis imputed all missing samples as adverse events (i.e., opiate and cocaine positive). This type of analysis is consistent with the treatment of missing samples while abstinence-reinforcement contingencies were in effect: A participant’s base pay was reset if they provided a urine sample that was positive for the targeted drug(s) or if the participant failed to provide a mandatory urine sample. For the missing-missing analyses, missing samples were omitted.
Results
Table 2 reports the mean and the standard error of the percentage of urine samples that tested negative for opiates and cocaine, aggregated for participants of each classification and across the six samples before or after each abstinence-reinforcement contingency was administered. The aggregated urinalysis results and the results of Wilcoxon matched-pairs signed-ranks tests are organized by drug (opiates or cocaine), method of analyzing missing data (missing-missing or missing-positive), and classification of participants (Intention-to-Treat, Completers, Opiate Users, and Opiate-Abstinent Cocaine Users). P-values show comparisons that were statistically significant at .05, .01, and .001 levels, according to the Wilcoxon matched-pairs signed-ranks tests, and dashes represent comparisons that were not significant (p >.05). For some participants in the Intention-to-Treat classification, all six samples before or after the administration of an abstinence-reinforcement contingency were missing. In these situations, results for that participant were omitted from the missing-missing analysis. This resulted in the inclusion of data for 148 and 130 of the 166 participants in the Intention-to-Treat classification for the opiate-abstinence and opiate- and cocaine-abstinence contingencies, respectively.
Table 2.
The percentage of opiate- and cocaine-negative urine samples aggregated across participants during the six consecutive urine samples before and after each abstinence-reinforcement contingency was administered.
| Opiate-Abstinence Contingency | Opiate- and Cocaine-Abstinence Contingency | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Before | After | p < | Before | After | p < | |||||
| Opiate Negative, % (SE) | ||||||||||
| Missing-Positive | ||||||||||
| Intention-to-Treat | 50 | (3.0) | 62 | (3.1) | .001 | 61 | (3.1) | 55 | (3.2) | .01 |
| Completers | 65 | (3.9) | 81 | (3.1) | .001 | 81 | (3.1) | 81 | (2.9) | --- |
| Opiate Users | 45 | (4.2) | 74 | (4.5) | .001 | 71 | (4.5) | 75 | (3.9) | --- |
| Missing-Missing | ||||||||||
| Intention-to-Treat | 64 | (3.2)a | 78 | (2.9)a | .001 | 81 | (3.0)b | 82 | (2.8)b | --- |
| Completers | 71 | (3.9) | 87 | (3.0) | .001 | 87 | (3.0) | 89 | (2.5) | --- |
| Opiate Users | 54 | (5.0) | 81 | (4.4) | .001 | 81 | (4.4) | 84 | (3.8) | --- |
| Cocaine Negative, % (SE) | ||||||||||
| Missing-Positive | ||||||||||
| Intention-to-Treat | 32 | (3.3) | 35 | (3.3) | .05 | 35 | (3.3) | 41 | (3.4) | .01 |
| Completers | 49 | (4.7) | 54 | (4.5) | --- | 54 | (4.5) | 63 | (4.2) | .01 |
| Opiate-Abstinent | 20 | (6.5) | 20 | (5.7) | --- | 20 | (5.7) | 45 | (6.9) | .001 |
| Cocaine Users | ||||||||||
| Missing-Missing | ||||||||||
| Intention-to-Treat | 38 | (3.8)a | 43 | (3.7)a | .05 | 48 | (4.0)b | 57 | (4.0)b | .001 |
| Completers | 52 | (4.9) | 56 | (4.7) | --- | 56 | (4.7) | 69 | (4.4) | .001 |
| Opiate-Abstinent | 20 | (6.5) | 20 | (5.7) | --- | 20 | (5.7) | 52 | (7.6) | .001 |
| Cocaine Users | ||||||||||
Note. Except where indicated, Intention-to-Treat includes 166 participants, Completers includes 91 participants, Opiate Users includes 57 participants, and Opiate-Abstinent Cocaine Users includes 25 participants. If all six samples before or after a contingency were missing for a participant, the participant’s data was excluded from missing-missing analyses. This affected only the Intention-to-Treat classification.
Results are shown for 148 participants before and after the opiate-abstinence contingency.
Results are shown for 130 participants before and after the opiate- and cocaine-abstinence contingency.
P-values show comparisons that were significant at the .05, .01, and .001 levels, as judged by Wilcoxon matched-pairs signed-ranks tests; missing p-values (---) show comparisons that were not significant at p < .05.
In every comparison (12 of 12) across classifications (Intention-to-Treat, Completers, Opiate Users, and Opiate-Abstinent Cocaine Users) and drugs (opiates and cocaine) shown in Table 2, the administration of the abstinence-reinforcement contingency produced significant increases in the percentage of urine samples that tested negative for the drug targeted by the abstinence-reinforcement contingency. When the opiate-abstinence contingency was administered, opiate abstinence increased significantly in all comparisons (6 of 6), as judged by the missing-missing and missing-positive analyses. When the opiate- and cocaine-abstinence contingency was administered, cocaine abstinence also increased significantly in all comparisons (6 of 6) as judged by both missing-missing and missing-positive analyses.
The introduction of abstinence-reinforcement contingencies usually (9 of 12 comparisons) did not produce significant changes in abstinence for the non-targeted drug. When the opiate-abstinence contingency was administered, changes in cocaine abstinence were not significant in most comparisons (4 of 6). In the two cases where changes in cocaine abstinence were judged significant, cocaine abstinence increased for participants in the Intention-to-Treat classification. When the opiate- and cocaine-abstinence contingency was administered, opiate abstinence was unchanged in most comparisons (5 of 6). In the sole case in which opiate abstinence changed significantly with the administration of the opiate- and cocaine-abstinence contingency, opiate abstinence decreased for participants in the Intention-to-Treat classification, as judged by the missing-positive analysis. According to the missing-missing analysis, this decrease was not significant.
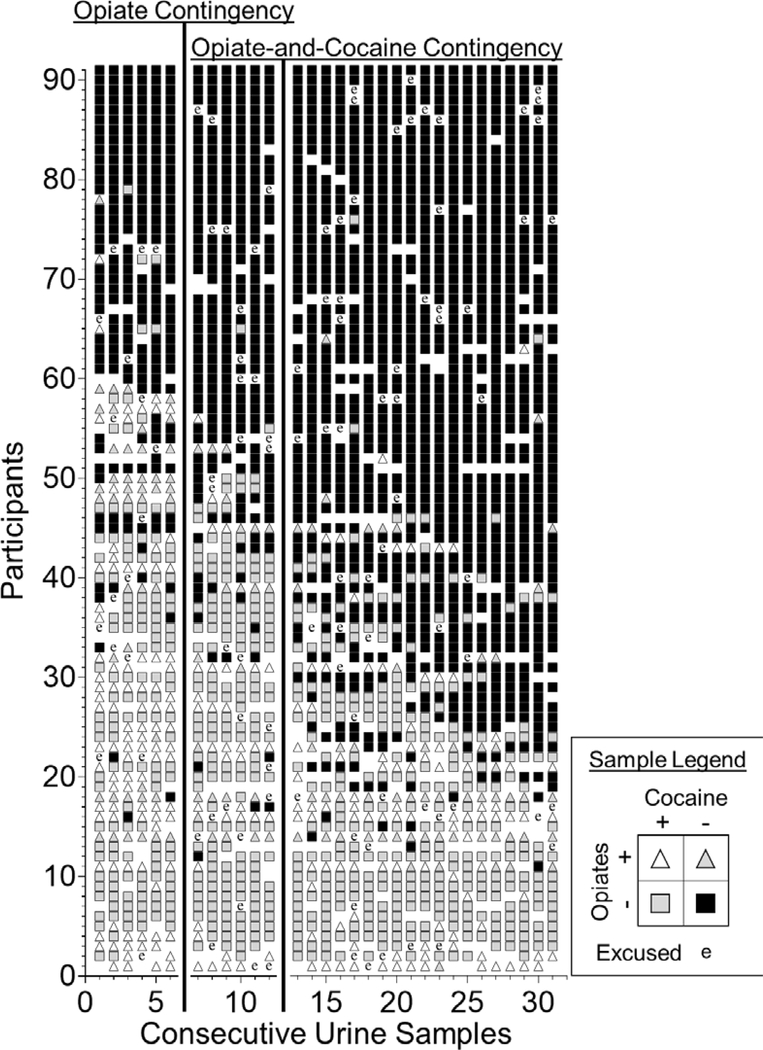
Figure 2 shows the urinalysis results for each of the Completers across the 31 mandatory urine samples. Each row represents the urinalysis results for an individual participant. The order of participants was arranged according to the number of samples that tested negative for both opiates and cocaine. As shown in Figure 2, abstinence generally increased following the administration of the contingency targeting each drug. When the opiate-abstinence contingency was administered, there was a general reduction urine samples that were positive for both opiates and cocaine and in urine samples that were positive for opiates and negative for cocaine and a corresponding increase in urine samples that were negative for opiates and positive for cocaine and urine samples that were negative for both opiates and cocaine – indicating an increase in opiate abstinence. When the opiate- and cocaine-abstinence contingency was administered, there was a general decrease in urine samples that were negative for opiates and positive for cocaine and an increase in urine samples that were negative for both – indicating an increase in abstinence from both opiates and cocaine.
Figure 2.
Urinalysis results across consecutive mandatory urine samples for Completers (n = 91). Each participant is represented by a row of symbols. The symbols shown in each row represent samples that were negative for both opiates and cocaine (filled squares), negative for opiates and positive for cocaine (gray squares), positive for opiates and negative for cocaine (gray triangles), positive for both opiates and cocaine (unfilled triangles), missing (blank), or excused (“e”). Phase lines represent the administration of each abstinence-reinforcement contingency.
Figure 2 includes results from a number of participants who were already abstinent from opiates (n = 34) or cocaine (n = 32) before the contingency targeting that drug was administered. Additionally, some participants whose results were included in this figure were prevented from contacting reinforcement in the opiate- and cocaine-abstinence contingency by a failure to achieve opiate abstinence during the opiate-abstinence contingency (n = 37; note that 3 participants were both abstinent from cocaine before the opiate- and cocaine-abstinence contingency and were not abstinent from opiates). Because the inclusion of these results obscures an interpretation of the effects of the contingencies, Figures 3, 4, and 5 include only results from participants who were not consistently abstinent from opiates before the opiate-abstinence contingency (Opiate Users; n = 57) and people who were abstinent from opiates but were not abstinent from cocaine before the opiate- and cocaine-abstinence contingency (Opiate-Abstinent Cocaine Users; n = 25).
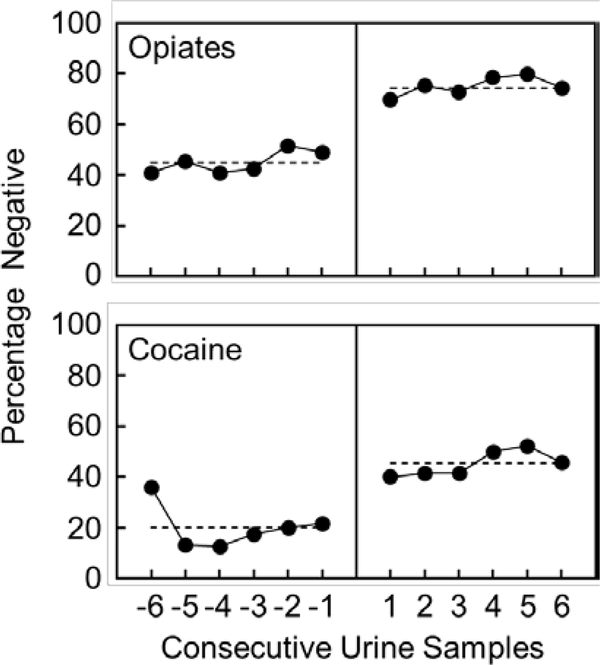
Figure 3.
The percentage of urine samples that were negative for opiates for Opiate Users (top, n = 57) and cocaine for Opiate-Abstinent Cocaine Users (bottom, n = 25) as judged by the missing-positive analysis in the six consecutive mandatory urine samples before and after each contingency was administered. Dots show the mean across participants in each sample and the dashed lines show the mean aggregated across the six samples.
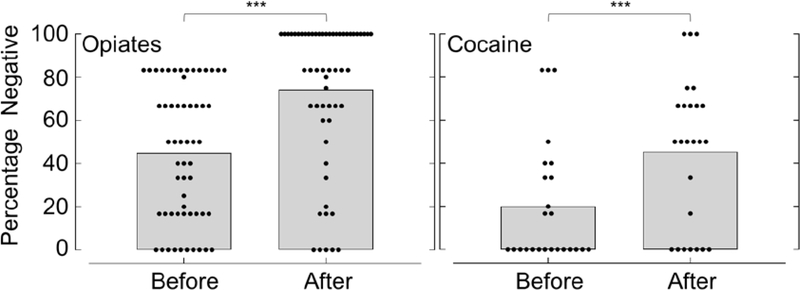
Figure 4.
The percentage of urine samples that were negative for opiates (left) and cocaine (right) aggregated, for each participant, over the six consecutive mandatory urine samples before and after the contingency targeting each drug was administered for Opiate Users (left, n = 57) and Opiate-Abstinent Cocaine Users (right, n = 25), as judged by the missing-positive analysis. Dots show percentages for individual participants and bars show the mean across participants. Asterisks show comparisons that were statically significant as judged by Wilcoxon matched-pairs signed-ranks tests at the p < .001 (***) level.
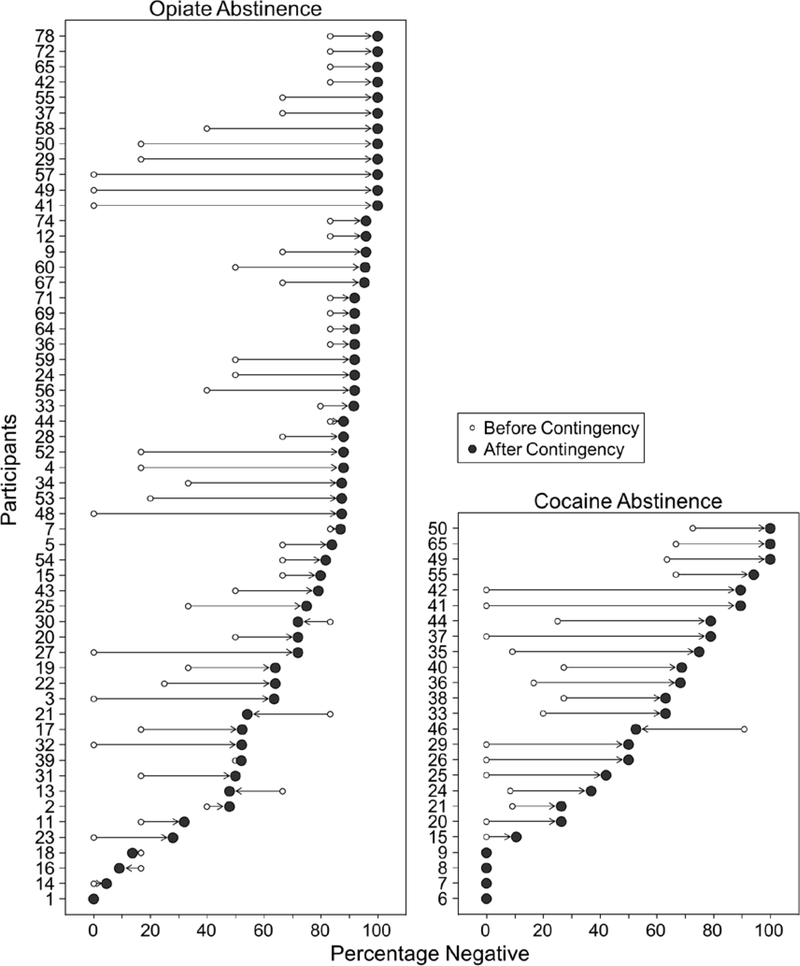
Figure 5.
The mean percentage of urine samples that tested negative for opiates (left) and cocaine (right) aggregated across all urine samples before (unfilled) and after (filled) the contingencies targeting abstinence from opiates (left; Opiate Users; n = 57) and cocaine (right; Opiate-Abstinent Cocaine Users; n = 25) were administered. Results from the missing-positive analysis are shown for each participant, and participant labels are consistent with those used in Figure 2. Arrows show changes in abstinence.
Figure 3 shows the mean percentage of samples that tested negative for opiates for Opiate Users (top) and cocaine for Opiate-Abstinent Cocaine Users (bottom) in each of the six samples before and after the abstinence-reinforcement contingencies were administered, as judged by the missing-positive analysis. Opiate abstinence was stable before the opiate-abstinence contingency was administered, but increased abruptly when the opiate-abstinence contingency was administered to Opiate Users. Opiate abstinence remained stable for these participants for the remainder of the condition. Similarly, cocaine abstinence was stable before the opiate- and cocaine-abstinence contingency was administered, but when the opiate- and cocaine-abstinence contingency was administered for the Opiate-Abstinent Cocaine Users, the percentage of samples that tested negative for cocaine increased abruptly and remained stable for the remainder of the condition. Together, the panels of Figure 3 show the time course of effects of the abstinence-reinforcement contingencies.
Figure 4 shows the mean percentage of urine samples that tested negative for opiates for Opiate Users (left) and cocaine for Opiate-Abstinent Cocaine Users (right) across the six urine samples before and after the administration of each contingency, as judged by the missing-positive analysis. The percentage of urine samples that tested negative for opiates and cocaine increased significantly following administration of the opiate-abstinence contingency and the opiate- and cocaine-abstinence contingency. Additionally, there was a general increase in abstinence following each contingency; however, when reading this figure, it is not possible to tell the number of participants whose abstinence increased following the administration of the contingencies, or by how much abstinence changed for any participant.
Figure 5 shows the change in opiate or cocaine abstinence following administration of each abstinence-reinforcement contingency for each Opiate User and Opiate-Abstinent Cocaine User, as judged by the missing-positive analysis. Participants are shown along the y-axis, with labels that are consistent with those used in Figure 2. The x-axis shows the percentage of urine samples that tested negative for opiates (left panel; Opiate Users) and cocaine (right panel; Opiate-Abstinent Cocaine Users). The administration of the opiate-abstinence contingency was associated with an increase in opiate abstinence for 53 of 57 (93%) Opiate Users, and 12 (21%) Opiate Users demonstrated abstinence from opiates in all 25 samples following the administration of the contingency. Opiate abstinence remained unchanged for 1 Opiate User, and decreased for 5 (9%). The administration of the opiate- and cocaine-abstinence contingency was associated with an increase in cocaine abstinence for 20 of 25 (80%) Opiate-Abstinent Cocaine Users, and 3 (12%) Opiate-Abstinent Cocaine Users demonstrated abstinence from cocaine in all 19 samples following the contingency. Cocaine abstinence remained unchanged for 4 (16%) Opiate-Abstinent Cocaine Users, and decreased for 1 (4%).
Discussion
The present study provides additional evidence that employment-based abstinence reinforcement can increase opiate and cocaine abstinence when the contingencies are arranged sequentially. Findings from the present study expand upon previous research by showing that abstinence from the drug targeted by each contingency was increased when contingencies were administered on the basis of time. Significant increases in opiate and cocaine abstinence occurred immediately after contingencies targeting each drug were administered. These increases occurred across all methods of classifying participants, but results were clearest when analyses targeted Opiate Users and Opiate-Abstinent Cocaine Users. As judged by the missing-positive analysis, abstinence increased for most Opiate Users and Opiate-Abstinent Cocaine Users in the six samples following administration of the contingency targeting each drug.
The present study differed from prior research in the way that the abstinence-reinforcement contingencies were administered. In a similar study (Holtyn et al., 2014b), participants progressed from an opiate-abstinence contingency to an opiate- and cocaine-abstinence contingency only when consistent opiate abstinence was demonstrated for 3 weeks. This requirement resulted in some participants spending an extended period in the opiate-abstinence contingency, and some never progressing to the opiate- and cocaine-abstinence contingency. In contrast, in the present study, participants progressed from the opiate-abstinence contingency to the opiate- and cocaine-abstinence contingency based on time rather than on achieved abstinence.
The procedure used in the present study was generally effective, but it had both advantages and disadvantages. Advantages of time-base contingencies include that participants were exposed to conditions for equivalent amounts of time and it freed staff from the requirement of continuous monitoring of participant urinalyses to determine when new contingencies could be applied. These advantages remove barriers related to limits on time and money, which in some cases, might make the Holtyn et al. (2014b) procedure impractical. The main disadvantage of this procedure is that it exposed some participants to the opiate- and cocaine-abstinence contingency before they achieved abstinence from opiates. In these cases, a participant’s base pay was reset because of opiate use, thereby preventing the reinforcement of cocaine abstinence. This effect is shown in Figure 2 (e.g., samples 9–23 for Participant 23). For example, Participant 23 was positive for opiates and cocaine in the final 5 samples of the opiate-abstinence contingency. This meant that at the start of the opiate- and cocaine-abstinence contingency, the base pay was reset to the minimum – effectively reducing the potential effects of the incentive on cocaine abstinence. This participant did eventually begin providing urine samples that were negative for both opiates and cocaine, but there was a long delay between the administration of the contingency and consistent abstinence.
This study has two main limitations. The first is that it was not designed in a way that allows a direct comparison to Holtyn et al.’s (2014b) study. A way that would allow for a direct comparison would be to randomly assign participants to the two different methods of reinforcing abstinence from opiates and cocaine. In addition, the current study differed in important ways. For example, we addressed drug use in people who were enrolled in or eligible for methadone or buprenorphine treatment, whereas Holtyn et al.’s study addressed drug use in out-of-treatment adults with recent injection drug use (injecting either heroin or cocaine). Thus, the present study left open the possibility that for some individuals, opiate and cocaine use was already controlled to some extent before the administration of the contingencies. This possibility was part of the rationale for analyzing the subset of results for people who used opiates (Opiate Users) and who used cocaine (Opiate-Abstinent Cocaine Users) separately from the rest of the Completers and Intention-to-Treat group. Additionally, the present study measured opiate and cocaine use by a threshold metabolite concentration of 300 ng/ml or 150 ng/ml, respectively. Maximum pay was maintained only if concentrations were less than the threshold. In contrast, participants in Holtyn et al.’s study could maintain maximum pay if metabolite concentrations were reduced by at least 20 percent per day since the last sample or if metabolite concentrations for either drug were less than 300 ng/ml. The difference in measurement of cocaine abstinence may have decreased the number of samples in the present study that were judged to be cocaine abstinent relative to the prior study, and the difference in the reinforcement criteria may have affected the speed by which participants became abstinent. However, it should be noted that results in the present study were not dissimilar from prior research. Opiate and cocaine abstinence increased among Opiate Users and Opiate-Abstinent Cocaine Users (+ 29% and + 25%, respectively), to a similar extent as in Holtyn et al.’s (2014) study (+ 30% and + 20%, respectively).
A second limitation is that administering abstinence reinforcement on the basis of time allowed for a participant to be exposed to the opiate- and cocaine-abstinence contingency before opiate abstinence was achieved. For example, if a participant was cocaine abstinent but not opiate abstinent on the first day of the opiate- and cocaine-abstinence contingency, contact with the reinforcer programmed for cocaine abstinence would be prevented; the participant’s base pay would be reset despite the fact that they were in the condition in which cocaine abstinence reinforcement was programmed. This may represent a missed opportunity to reinforce cocaine abstinence.
There may be other ways to address polydrug use. Epstein et al. (2009) assessed the value of splitting total reinforcement across opiates and cocaine, so that participants could earn half of the total reinforcement for cocaine abstinence and half for opiate abstinence. In a randomized clinical trial, Epstein et al. (2009) compared a full contingency, in which participants earned all of the reinforcement for achieving cocaine abstinence, to a “split” contingency, in which participants earned half of the reinforcement for achieving abstinence from opiates and half of the reinforcement for achieving abstinence from cocaine. Arranging all of the reinforcement for cocaine abstinence increased cocaine abstinence compared to a yoked-control condition, in which participants received incentives independent of abstinence. However, splitting the reinforcement across opiate and cocaine abstinence did not increase cocaine abstinence compared to the control condition. Overall, this study suggests that splitting the reinforcement across multiple drugs reduces the reinforcement magnitude for abstinence from each drug and reduces the abstinence from each drug. It is unclear whether reinforcing abstinence from two drugs simultaneously is better or worse than arranging reinforcement sequentially, as was done in this study.
Findings from the present study replicate and extend prior research by showing that the administration of employment-based abstinence reinforcement in a time-based sequence increased opiate and cocaine abstinence. Drug abstinence increased significantly following administration of the contingency targeting each drug for participants enrolled in the study (Intention-to-Treat), participants who completed the study (Completers), participants who completed the study and were not opiate abstinent before the opiate-abstinence contingency (Opiate Users), and participants who completed the study and were opiate abstinent but not cocaine abstinent before the opiate- and cocaine-abstinence contingency (Opiate-Abstinent Cocaine Users). Overall, the study shows that administering abstinence reinforcement in a time-based sequence increased opiate and cocaine abstinence.
Supplementary Material
Acknowledgments
Shrinidhi Subramaniam is now affiliated with California State University, Stanislaus. This research was supported by Grants R01DA037314 and T32DA07209 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse of the National Institutes of Health. We thank Meghan Arellano, Jackie Hampton, Calvin Jackson, and Andrew Rodewald for their work conducting assessments, recruiting participants, and preparing participants for employment.
References
- Aklin WM, Wong CJ, Hampton J, Svikis DS, Stitzer ML, Bigelow GE, & Silverman K (2014). A therapeutic workplace for the long-term treatment of drug addiction and unemployment: Eight-year outcomes of a social business intervention. Journal of Substance Abuse Treatment, 47, 329–338. 10.1016/j.jsat.2014.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bigelow GE & Silverman K (1999). Theoretical and empirical foundations of contingency management treatments for drug abuse In Higgins ST and Silverman K (Eds.), Motivating Behavior Change Among Illicit-Drug Abusers (pp. 3–31). Washington DC: American Psychological Association; 10.1037/10321-001 [DOI] [Google Scholar]
- Bigelow GE, Stitzer ML, Griffiths RR, & Liebson IA (1981). Contingency management approaches to drug self-administration and drug abuse: Efficacy and limitations. Addictive Behaviors, 6, 241–252. https://doi.org/0306-4603(81)90022-8 [DOI] [PubMed] [Google Scholar]
- Budney AJ, Higgins ST, Delaney DD, Kent L, & Bickel WK (1991). Contingent reinforcement of abstinence with individuals abusing cocaine and marijuana. Journal of Applied Behavior Analysis, 24, 657–665. 10.1901/jaba.1991.24-657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2018). 2017 National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration, Rockville, MD: Retrieved from https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2017/NSDUHDetailedTabs2017.pdf [Google Scholar]
- Centers for Disease Control and Prevention. (2019). Drug overdose deaths. Retrieved from: https://www.cdc.gov/drugoverdose/data/statedeaths.html.
- Dallery J, Silverman K, Chutuape MA, Bigelow GE, & Stitzer ML (2001). Voucher-based reinforcement of opiate plus cocaine abstinence in treatment-resistant methadone patients: Effects of reinforcer magnitude. Experimental and Clinical Psychopharmacology, 9, 317–325. 10.1037//1064-1297.9.3.317 [DOI] [PubMed] [Google Scholar]
- DeFulio A, Donlin WD, Wong CJ, & Silverman K (2009). Employment-based abstinence reinforcement as a maintenance intervention for the treatment of cocaine dependence: A randomized controlled trial. Addiction, 104, 1530–1538. 10.1111/j.1360-0443.2009.02657.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donatelle RJ, Prows SL, Champeau D, & Hudson D (2000). Randomized controlled trial using social support and financial incentives for high risk pregnant smokers: Significant other support (SOS) program. Tobacco Control, 9, 67–69. 10.1136/tc.9.suppl_3.iii67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donlin WD, Knealing TW, Needham M, Wong CJ, & Silverman K (2008). Attendance rates in a workplace predict subsequent outcome of employment-based reinforcement of cocaine abstinence in methadone patients. Journal of Applied Behavior Analysis, 41, 499–516. 10.1901/jaba.2008.41-499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downey KK, Helmus TC, & Schuster CR (2000). Treatment of heroin-dependent poly-drug abusers with contingency management and buprenorphine maintenance. Experimental and Clinical Psychopharmacology, 8, 176–184. 10.1037//1064-1297.8.2.176 [DOI] [PubMed] [Google Scholar]
- Epstein DH, Schmittner J, Umbricht A, Schroeder JR, Moolchan ET, & Preston KL (2009). Promoting abstinence from cocaine and heroin with a methadone dose increase and a novel contingency. Drug and Alcohol Dependence, 101, 92–100. 10.1016/j.drugalcdep.2008.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henkel D (2011). Unemployment and substance use: A review of the literature (1990–2010). Current Drug Abuse Reviews, 4, 4–27. [DOI] [PubMed] [Google Scholar]
- Heil S, Higgins ST, Bernstein IM, Soloman LJ, Rogers RE, Thomas CS, … Lynch ME (2008). Addiction, 103, 1009–1018. 10.1111/j.1360-0443.2008.02237.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Washio Y, Heil SH, Solomon LJ, Gaalema DE, Higgins TM, & Bernstein IM (2012). Financial incentives for smoking cessation among pregnant and newly postpartum women. Preventative Medicine, 55, S33–S40. 10.1016/j.ypmed.2011.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtyn AF, Koffarnus MN, DeFulio A, Sigurdsson SO, Strain EC, Schwartz RP, … Silverman K (2014a). The therapeutic workplace to promote treatment engagement and drug abstinence in out-of-treatment injection drug users: A randomized controlled trial. Preventive Medicine, 68, 62–70. 10.1016/j.ypmed.2014.02.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtyn AF, Koffarnus MN, DeFulio A, Sigurdsson SO, Strain EC, Schwartz RP, & Silverman K (2014b). Employment-based abstinence reinforcement promotes opiate and cocaine abstinence in out-of-treatment injection drug users. Journal of Applied Behavior Analysis, 47, 681–693. 10.1002/jaba.158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- iLearn. (2019). http://www.ilearn.com
- Koffarnus MN, DeFulio A, Sigurdsson SO, & Silverman K (2013). Performance pay improves engagement, progress, and satisfaction in computer-based job skills training of low-income adults. Journal of Applied Behavior Analysis, 46, 395–406. 10.1002/jaba.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koffarnus MN, Wong CJ, Diemer K, Needham M, Hampton J, Fingerhood M, … Silverman K (2011). A randomized clinical trial of a therapeutic workplace for chronically unemployed, homeless, alcohol-dependent adults. Alcohol and Alcoholism, 46, 561–569. 10.1093/alcalc/agr057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Duhig AM, McKee SA, McMahon TJ, Liss T, McFetridge A, & Cavallo DA (2006). Contingency management for smoking cessation in adolescent smokers. Experimental and Clinical Psychopharmacology, 14, 306–310. 10.1037/1064-1297.14.3.306 [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. (2017). National Vital Statistics System. Mortality multiple cause of death files. Drug Overdose Deaths in the United States, 1999–2016. Retrieved from: https://www.cdc.gov/nchs/data/databriefs/db294_table.pdf#page=1 [Google Scholar]
- Preston KL, Umbricht A, & Epstein DH (2000). Methadone dose increase and abstinence reinforcement for treatment of continued heroin use during methadone maintenance. Archives of General Psychiatry, 57, 393–404. 10.1001/archpsyc.57.4.395 [DOI] [PubMed] [Google Scholar]
- Schuster CR & Thompson T (1969). Self administration of and behavioral dependence on drugs. Annual Review of Pharmacology, 9, 483–502. [DOI] [PubMed] [Google Scholar]
- Seth P, Scholl L, Rudd RA, Bacon S (2018). Overdose deaths involving opioids, cocaine, and psychostimulants – United States, 2015–2016. Morbidity and Mortality Weekly Report, 67, 349–358. 10.15585/mmwr.mm6712a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, Chutuape MA, Bigelow GE, & Stitzer ML (1999). Voucher-based reinforcement of cocaine abstinence in treatment-resistant methadone patients: Effects of reinforcement magnitude. Psychopharmacology, 146, 128–138. https://doi.org/91460128.213 [DOI] [PubMed] [Google Scholar]
- Silverman K, Holtyn AF, & Morrison R (2016). The therapeutic utility of employment in treating drug addiction: Science to application. Translational Issues in Psychological Science, 2, 203–212. 10.1037/tps0000061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, Holtyn AF & Toegel F (2019). The Utility of Operant Conditioning to Address Poverty and Drug Addiction. Perspectives on Behavior Science, 42, 525–546. 10.1007/s40614-019-00203-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K, Svikis D, Robles E, Hampton J, Stitzer ML, & Bigelow GE (2001). A reinforcement-based therapeutic workplace for the treatment of drug abuse: Six-month abstinence outcomes. Experimental and Clinical Psychopharmacology, 9, 14–23. 10.1037/1064-1297.9.1.14 [DOI] [PubMed] [Google Scholar]
- Silverman K, Svikis D, Wong CJ, Hampton J, Stitzer ML, & Bigelow GE (2002). A reinforcement-based therapeutic workplace for the treatment of drug abuse: Three-year abstinence outcomes. Experimental and Clinical Psychopharmacology, 10, 228–240. [DOI] [PubMed] [Google Scholar]
- Silverman K, Wong CJ, Higgins ST, Brooner RK, Montoya ID, Contoreggi C, … Preston KL (1996). Increasing opiate abstinence through voucher-based reinforcement therapy. Drug and Alcohol Dependence, 41, 157–165. 10.1016/0376-8716(96)01246-X [DOI] [PubMed] [Google Scholar]
- Silverman K, Wong CJ, Needham M, Diemer KN, Knealing T, Crone-Todd D, … Kolodner K (2007). A randomized trial of employment-based reinforcement of cocaine abstinence in injection drug users. Journal of Applied Behavior Analysis, 40, 387–410. 10.1901/jaba.2007.40-387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman K,Wong CJ, Umbricht-Schneiter A, Montoya ID, Schuster CR, & Preston KL (1998). Broad beneficial effects of cocaine abstinence reinforcement among methadone patients. Journal of Consulting and Clinical Psychology, 66, 811–824. 10.1037/0022-006X.66.5.811 [DOI] [PubMed] [Google Scholar]
- Sullivan LE, Metzgar DS, Fudala PJ, & Fiellin DA (2005). Decreasing international HIV transmission: The role of expanding access to opioid agonist therapies for injection drug users. Addiction, 100, 150–158. 10.1111/j.1360-0443.2004.00963.x [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2018). Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; Retrieved from: https://www.samhsa.gov/data/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.