Abstract
Background
Telemedicine is the use of electronic communications technology to provide care for patients when distance separates the practitioner and the patient. As the parents and families of infants admitted to the NICU require major support from health professionals in terms of information and time, telemedicine has the potential to increase this support.
Objectives
To evaluate if the use of telemedicine technology to support families of newborn infants receiving intensive care affects the length of hospital stay and parental/family satisfaction.
Search methods
We searched the following databases: Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, 2011, Issue 8), MEDLINE (from 1966 to September 2011), EMBASE (1980 to September 2011). We also searched ClinicalTrials.gov (http://www.clinicaltrials.gov) and the EudraCT (http://eudract.emea.eu.int) web sites. We searched the proceedings of conferences of the Canadian Society of Telehealth, American Telemedicine Association, the International Society for Telemedicine, the Annual Conference of The International e‐Health Association, American Medical Informatics Association and MedInfo.
Selection criteria
We attempted to identify randomised controlled trials that assessed the use of telemedicine designed to support parents of infants cared for in a Neonatal Intensive Care Unit (NICU) compared with standard support measures. Our primary outcome was the length of hospital stay, and secondary outcomes included parental and staff satisfaction, emergency hospital visits post‐discharge and family utilisation of infant health‐related resources.
Data collection and analysis
Two review authors independently screened the studies, extracted the data and assessed the risk of bias of the one included study using the standard methods of the Cochrane Neonatal Review Group. We planned to express treatment effects as risk ratio (RR), risk difference (RD), number needed to treat (NNT) and mean difference (MD) where appropriate, using a fixed‐effect model.
Main results
A single study was included for analysis in this review. This study compared the use of telemedicine (Baby Carelink) for parents and families of infants in the NICU with a control group without access to this programme and assessed the length of hospital stay for the infants and family satisfaction in multiple components of infant care. The study shows no difference in the length of hospital stay (average length of stay: telemedicine group: 68.5 days (standard deviation (SD) 28.3 days), control group: 70.6 days (SD 35.6 days), MD ‐2.10 days (95% confidence interval: ‐18.85 to 14.65 days). There was insufficient information for further analysis of measures of family satisfaction.
Authors' conclusions
There is insufficient evidence to support or refute the use of telemedicine technology to support the parents of high‐risk newborn infants receiving intensive care. Clinical trials are needed to assess the application of telemedicine to support parents and families of infants in NICU with length of hospital stay and their perception of NICU care as the major outcomes.
Plain language summary
Telemedicine for the support of parents of high‐risk newborn infants
Telemedicine uses information technology so that doctors or nurses can communicate with their patients when they are not in the same room. The parents of sick infants who are treated in neonatal intensive care units require a lot of support when their child is ill and when they are taking their baby home. Telemedicine may be able to help the doctors and nurses to improve provision of support to the parents. This review identified one trial which did not show that telemedicine alters the time these infants stay in hospital. However, there was some imprecision of the published data in this study that makes it difficult to make firm recommendations either way with telemedicine.
Summary of findings
Summary of findings for the main comparison. Telemedicine for the support of parents of high‐risk newborn infants.
| Telemedicine for the support of parents of high‐risk newborn infants | ||||||
| Patient or population: parents of high‐risk newborn infants Settings: NICU Intervention: Telemedicine | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Telemedicine | |||||
| Length of hospital stay Days Follow‐up: 4 months | The mean length of hospital stay in the control groups was 70.6 days | The mean length of hospital stay in the intervention groups was 2.10 lower (18.85 lower to 14.65 higher) | 56 (1 study) | ⊕⊝⊝⊝ very low | Quality assessment of the included study ‐ overall minor downgrade, small sample and major imprecision in the estimate of effects. | |
| *The basis for the assumed risk (e.g., the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
Background
Description of the condition
Telemedicine enables the practitioner or physician to deliver health care without being in the same physical location as the patient (Strehle 2006). One definition relevant to the paediatric population provided by Spooner and Gottlieb is "the use of electronic communications technology to provide and support health care for infants, children, adolescents, and young adults when distance separates the practitioner from the patient, parent, guardian or referring practitioner" (Spooner 2004). In earlier usages of the term, telemedicine (which means "medicine at a distance") implies communication between doctors and patient in different physical locations where direct face‐to‐face consultation is not feasible using ancillary means of communication such as telephone and radio (McLaren 1995).
Description of the intervention
More recently, the meaning of telemedicine has been expanded following the introduction of the Internet and other advances in electronic and information technologies (Currell 2000). The newer applications in telemedicine range from web‐based interactive image‐enriched patient‐specific information resources (Chan 2003) and teleconferencing with audio and video capabilities (Weiner 2001) to the use of electronic accessories in the operating room (Whitten 2004).Telemedicine can thus be seen as a subset within the wider field of medical informatics (Nagendran 2000). The terms "telehealth", "online health" and "e‐health" are now also being used interchangeably with telemedicine (Wootton 2001).
The two main forms of telemedicine are the synchronous or real time variety (face‐to‐face) and the asynchronous variety where the information is recorded (Jaatinen 2002). In the synchronous variety, data, images and sound are transmitted live and the health professional may have direct video contact with the patient. In the asynchronous (store and forward technique), information for example, X‐Ray images may be acquired in one location and then reviewed in another at a later stage (Strehle 2006).
Telemedicine has been developed in countries such as Canada (Roine 2001) and Norway (Pettersen 1999) where a relatively small rural population is spread over a large area, making face‐to‐face medical consultations difficult. The application of telemedicine has been reported in the delivery of primary care (Marcin 2004a; Marcin 2004b), child health (Shiffman 2001), specialist care in cardiology (Sable 2002) and home monitoring of stable chronic patients (Brennan 1997). However, the overall cost effectiveness of telemedicine in child health is still largely unproven (Strehle 2006a). In fact, a recent evaluation suggests that telemedicine is not a cost effective way of delivering health care (Whitten 2002). Telemedicine applications for remote monitoring of infants in the Neonatal Intensive Care Unit (NICU) is technically feasible. A web‐based monitoring application for infants in the NICU (Shin 2003) has been described. However, in this study, the monitoring station was located within the NICU, although it would have been feasible for monitoring to be performed at some distance away from the NICU. The current model of delivery of care in the NICU is for the neonatologists to deliver care in person. However, telemedicine applications for adult intensive care units allow intensivists (critical care physicians) to deliver consultation when they are not physically at the patient's bedside (Rosenfeld 2000).
How the intervention might work
Currently, the development of telemedicine in neonatal care has a different focus, targeting mainly the parents or family. Telemedicine support is needed in neonatal care because of the vast amount of specialised information available regarding the care of the sick newborn, the prognosis of these newborns and the roles and skills expected of the parents at discharge, given the limitations of what most parents can realistically absorb within their visiting time in the neonatal unit. Telemedicine should, therefore, aim not to lessen the parents' need to travel to the hospital, but to provide a portal through which they can access information pertinent to the care of their newborn infants at their own time and place of choice. Hopefully, better understanding by the parents regarding the care of their infants can contribute to improved outcomes. Daily updates may come in the form of "infant's diary" in an attempt to personalize the progress of the infants for the family. An example of this use of telemedicine is the "BabyLink" program, a web‐based program that automatically generates a daily update summarising the infant's clinical progress through a secure web‐based server (Freer 2005). An observational study (comparing two NICUs) has shown that telemedicine used to aid the turnaround time of neonatal echocardiography interpretation may reduce the length of hospital stay of very low birthweight infants (Rendina 1998). This may translate into benefits such as cost reduction from early neonatal discharges (Speer 1998; Spinner 1998).
Why it is important to do this review
A Cochrane review on the effectiveness of telemedicine versus face‐to‐face patient care found variable and inconclusive results, but pointed out the feasibility of conducting randomised controlled trials of telemedicine applications (Currell 2000). However, a lack of uniformity in the definitions of telemedicine has complicated the assessment of its effectiveness. For example, opinions vary on whether the use of telephone in a healthcare setting constitutes telemedicine (McLaren 1995; Thrall 1998; Currell 2000; Hersh 2001; Spooner 2004; Wootton 2006). The evolving characteristics and applications in telemedicine serve only to further broaden its definition. To derive a practical message on the effectiveness of telemedicine, systematic reviews may have to focus on a specific application or setting. This review examines one such application of telemedicine in the NICU that provides information, education and support to the families of sick newborns in the unit. This review assesses whether telemedicine, when applied as an additional resource, can enhance standard parental support.
Objectives
To evaluate if the use of telemedicine technology to provide education and support for the families of newborn infants receiving intensive care effects the length of hospital stay.
Methods
Criteria for considering studies for this review
Types of studies
We planned to include randomised and quasi‐randomised controlled trials. The unit of allocation could be either the individual parental set or centres.
Types of participants
Parents or caretakers of high‐risk newborn infants receiving intensive care (not depending on the distance from the NICU).
Types of interventions
Telemedicine technology focused on education and support to the parents or caretakers of newborn infants receiving intensive care.
Essential requirements that define the use of telemedicine are:
the use of information and communication technology such as the Internet;
the provision of dedicated information relevant to the care of the infants using the above technology;
the information provided above must be tailored to the parents in the settings in which the infant is cared; a series of links to the commonly accessible health web sites or search engines or simply an encouragement to use the Internet would not be considered as a telemedicine intervention;
the intervention could include the use of non‐Internet based information technology (IT), such as regular access to interactive CD ROM on the care of the infants in the neonatal unit concerned;
the use of the telephone could be accepted as a "telemedicine" intervention only if it is used as an additional tool in providing information and education within a structured programme, either people‐based or by using computer programmes, in conjunction with telemedicine applications as defined in points 1 to 4 above, in addition to the standard telephone support given to the caregivers of the infants in the unit. For example, this could involve regular calls made by NICU staff to the caregivers at pre‐defined timing. Where applicable, we planned to perform subgroup analyses for studies using only the telephone as the intervention and for those using other forms of telemedicine applications.
The time of commencement and the duration of intervention were accepted as variously specified by the authors of the included studies. However, we planned that subgroup analyses would be performed where applicable for studies with intervention applied during the following periods:
a) only during the infant's primary hospitalisation;
b) only after the infant's discharge;
c) both during the infant's primary hospitalisation and after discharge.
For comparison, we considered studies that examined the following:
i) comparison of telemedicine support intervention versus no support interventions; ii) comparison of telemedicine support intervention versus standard support interventions; ii) comparison between telemedicine and standard support versus standard support alone.
For studies that fall into groups ii) and iii), the education and support measures for the control group would be accepted as variously defined by the authors of the included studies as long as these measures were clearly stated, were part of the standard educational and support measures for the units concerned at the time of study, and thus were also applicable to the intervention group together with telemedicine. We planned to perform subgroup analyses where applicable for i) and ii).
We did not include studies that compared only different types or forms of telemedicine against each other in this review.
Types of outcome measures
Primary outcome measures
Length of hospital stay (days).
Secondary outcome measures
Families' knowledge on patient's condition, their satisfaction and confidence on the care of infants at discharge, for example the Parenting Stress Index (PSI) (Loyd 1985) and the NCAST Parent Interaction Tool (Farel 1991).
Staff satisfaction on patient care.
Frequency of emergency hospital visits post‐discharge.
Breast feeding rate at discharge and duration of breast feeding.
Frequency of access for infant health‐related resources by the families (including books, journal, CD ROM, Internet), taking into account the use of assigned telemedicine facilities.
Search methods for identification of studies
We used the standard search strategy of the Cochrane Neonatal Review Group. We searched the following databases: Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, 2011, Issue 8), MEDLINE (from 1966 to September 2011), EMBASE (1980 to September 2011) using the search strategy below. We used the following Medical Subject Heading (MESH) terms: "Telemedicine", "Telemetry", "Telehealth", "Software", "Computer Communication Networks", "Online Systems", "Computer‐Assisted Instruction", "Diagnosis, Computer‐Assisted", "Computers", "Medical Informatics", "Computers, Handheld", "Decision Making, Computer‐Assisted", "Internet", "Microcomputers", "Telecommunications", "Remote Consultation", "Telenursing". The terms used in the search strategy were based on a scoping review on the subject of health information technological aid to physician‐patient communication (Gentles 2010). Restriction terms; infants (0 to 23 months), humans and clinical trials were used. We did not use any language restriction.
Search Strategy (Appendix 1).
We also searched ClinicalTrials.gov (http://www.clinicaltrials.gov) and the EudraCT (http://eudract.emea.eu.int) web sites.
We searched the proceedings of conferences to identify relevant published abstracts of the Canadian Society of Telehealth, American Telemedicine Association, the International Society for Telemedicine, the Annual Conference of The International e‐Health Association, American Medical Informatics Association and MedInfo.
Data collection and analysis
We used the standard methods of The Cochrane Collaboration as described in the Cochrane Neonatal Review Group guidelines (http://www.cochrane.org/training/cochrane‐handbook).
Eligible studies were independently selected by the investigators by applying predefined inclusion and exclusion criteria. We resolved any disagreement by discussion.
Data extraction and entry: the review authors separately extracted, assessed and coded all data for each study using a form that was designed specifically for this review. For continuous data, any standard error of the mean would be replaced by the corresponding standard deviation.
Planned subgroup analyses: We planned subgroup analyses according to the setting of newborn care: neonatal intensive care unit, other in‐hospital setting, or community setting.
-
Criteria for assessing the methodological quality of the studies: Each trial was assessed for:
blinding of randomisation;
blinding of intervention;
whether there was complete follow‐up;
blinding of outcome measurement and categorised them into "yes", "no" and "can't tell".
Statistical analyses: Abstracted data were entered into RevMan 5 software and we assessed the one included study for statistical heterogeneity. We performed meta‐analysis using the fixed‐effect model. The standard methods of the Neonatal Review Group were used to synthesise data. We planned to use risk ratio (RR) for dichotomous data, risk difference (RD) and number needed to treat to benefit (NNTB) if there was a statistically significant reduction in RD and number needed to harm (NNTH) if there was a statistically significant increase in the RD.
We had intended to use the I2 test to examine heterogeneity between trials (values of I2 of 25% is low, 50% moderate and 75% high) (Higgins 2003). If moderate or high heterogeneity were noted, sensitivity and subgroup analyses would be used to identify the source of heterogeneity.
For categorical data, risk ratio, risk difference and NNT would have been used with their respective 95% confidence intervals. For continuous data, we used mean difference (MD) with 95% confidence interval.
The methods described in Section 16.3 of the Cochrane Handbook for Systematic Reviews of Interventions (http://www.cochrane.org/training/cochrane‐handbook) would have been used to allow analysis at the level of the individual parent or infant while accounting for the clustering of the data. Such methods might have include a 'multilevel model', a 'variance components analysis' or 'generalised estimating equations (GEEs)'. Effect estimates were analysed using the generic inverse variance method found in the RevMan 5 software (RevMan 2011).
Results
Description of studies
The preliminary MEDLINE search yielded 324 studies. After inspection of the titles, seven studies appeared to be potentially eligible in terms of relevance and methodology or both. After a detailed inspection of the abstracts, we judged that only one out of the seven studies met the selection criteria. The characteristics of the single included study and the six excluded studies are detailed in the tables Characteristics of included studies and Characteristics of excluded studies, respectively.
A search of the online register of clinical trials, www.clinicaltrials.gov did not reveal any study meeting the inclusion criteria.
Gray 2000 was the single study that met the inclusion criteria. It was a single‐centre randomised control trial conducted from 1 November 1997 to 30 March 1999. The population consisted of inborn very low birthweight (VLBW) infants admitted to a NICU in Boston (Beth Israel Deaconess Medical Centre) and their families. Fifty‐six infants had been randomised (30 control and 26 intervention) within 10 days of birth (see Characteristics of included studies). The main exclusion criteria were lack of high speed telephone (ISDN) lines at the family's residence and an expected stay of under two weeks at this NICU. Other exclusion criteria were lack of permanent residence for the family, lack of competence in English, expected discharge to other than the biological family and finally at the decision of the attending neonatologist. The intervention was the Baby CareLink system which was an online resource (with video conferencing facility) that the family could access through the Internet from their home computer. Each family in the intervention group was given a single training session (lasting from 40 to 120 minutes) on the use of the hardware and software. The hardware consisted of the ISDN telephone lines (installed by local telephone company) and computing and videoconferencing hardware (installed by local hardware vendor) which were in place mostly 12 days after randomisation. The Baby CareLink web site had six main sections that each dealt with issues that were of concern to the families during their baby's NICU stay and at the time of discharge;a daily clinical report, a message centre, a 'see your infant' section, a family room, a clinical information section, and a section focused on preparation for discharge to home. The families of infants in the control group received standard information and support from NICU staff. The outcome measures were death or discharge disposition from the NICU, date of discharge from NICU and discharge home as well as the frequency of family visits, telephone calls to the NICU, and holding of the infant (including 'kangaroo care'). The quality of care was rated by the family based on the 80‐item Picker Institure's Neonatal Intensive Care Unit Family Satisfaction survey administered at one and four months post‐discharge.
Among the excluded studies, none was found to be relevant after reading the abstracts, as they either assessed the use of telemedicine technologies for clinical diagnosis rather than for education and support (Robie 1998; Stenson 1998; Bhatikar 2002; Dowie 2009) or they did not include parents of high‐risk newborn infants as participants (Guillen 2002; McCrossan 2007; Dowie 2009).
Risk of bias in included studies
In Gray 2000, based on the published description of the methods, it can be inferred that the sequence generation was adequate but it was unclear whether the allocation was concealed. In terms of concealment, blinding of the intervention was not possible. Although blinding of outcome assessments that depended on parental reporting was not possible, blinding of the researchers when assessing other outcomes such as disposition of discharge and recording of family visits and holding of the infants was not reported. A detailed 'Risk of bias' table is included under Characteristics of included studies, along with a 'Risk of bias' graph (Figure 1) and a 'Risk of bias' summary (Figure 2).
1.
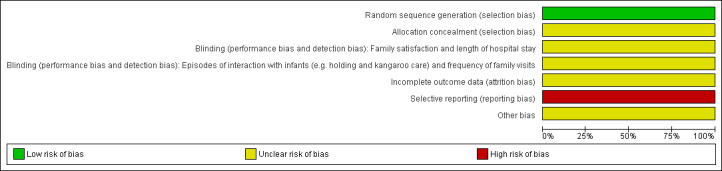
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.
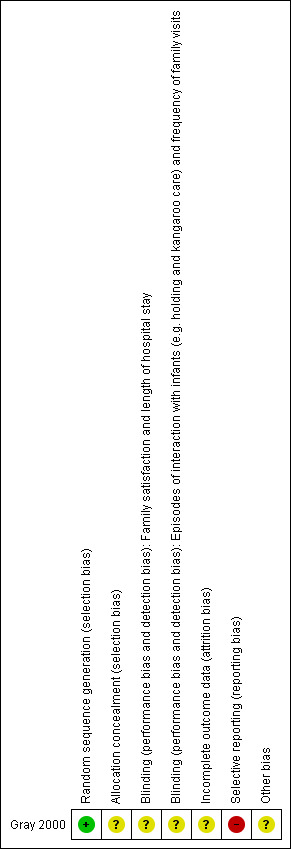
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
In terms of reporting of results, the event rates and/or the total number of participants analysed for all the outcomes were not presented in the published paper, thus not allowing for further meta‐analysis. There was also no description on the assigned groups of the five families who did not complete the postdischarge survey.
Effects of interventions
See: Table 1
Gray 2000 examined the effects of telemedicine support on the level of family satisfaction on infant care and length of hospital stay. The outcome of interest for this review, the length of hospital stay, did not differ between the Baby Carelink telemedicine group and the control groups (68.5 ± 28.3 days in telemedicine group versus 70.6 ± 35.6 days in the control group, mean difference: ‐2.10 days (95% confidence interval ‐18.85 to 14.65 days) (Figure 3 ). The group that was randomised to standard care included a significant number of infants who were back‐transferred to their local level two nurseries. In fact, 20% of the control group were back‐transferred while no infants in the intervention group were back‐transferred.
3.
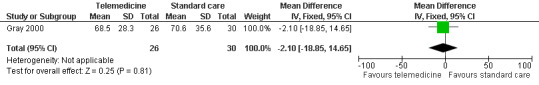
Forest plot of comparison: 1 Baby Carelink versus standard care, outcome: 1.2 Length of hospital stay.
Frequency of accessing telemedicine access (Baby CareLink) was reported for the intervention arm of this study. NICU and project staff initiated 1033 sessions during the study period while 26 families initiated 1744 sessions (26 sessions per family, mostly from home) during the same period. The average time of these sessions for all users was 5.4 minutes. During this time, there were 328 family‐initiated videoconferencing sessions which lasted an average of six minutes. The Baby CareLink areas most likely to be visited by the families were specific to the infants (for example the picture gallery 91%, daily report 57% and message centre 46% of the time). As this outcome was not reported (as it was not applicable) to the control arm, this outcome will not be subjected to more analysis in this review.
For the outcomes of family satisfaction assessed using the Picker Institute’s Neonatal Intensive Care Unit Family Satisfaction Survey, the authors reported that CareLink usage was associated with significant improvements in family satisfaction in the overall quality of care and environment and visitation dimensions (under "Results", paragraph 7, lines 1 to 4). Figures 2 and 3 in the study illustrate, in general, better scoring in the survey favouring the Baby Carelink group. As we did not have the primary data that constitute the figures from the authors, we were not able to apply further analysis to this group of outcomes.
Our summary of findings with the authors' judgment on the overall quality of evidence is presented in Table 1 .
Discussion
There are some deficiencies in the reporting of the results from the single included study. In the selection of the patient group, the study appeared to select families who lived close to urban centres (as evidenced by using lack of ISDN coverage as an exclusion criteria) and who were presumably of higher socioeconomic status (competence in English). This will likely affect the applicability of the findings to other patient populations. The substantial difference in the rates of back‐transfer to the local level two nursery between the intervention group and the control group could represent significant selection or performance bias, or an outcome as a result of the different interventions received. Furthermore, the very wide confidence interval of the difference in the length of hospital stay in this study shows imprecise estimate of the treatment effect size; likely due to a sample size that was inadequately powered. Overall, there was little information available for the authors of this review to make any conclusions regarding most of the outcomes. For the only analysable outcome of the length of hospital stay, the overall quality of evidence (GRADE) was very low (see Table 1).
In view of the rapid advances in information technologies over the recent two decades since this study, it is likely that telemedicine applications have evolved, and there is a possibility that in some NICUs telemedicine applications might have become the standard tools for infant care or parental support. The advent of mobile computing and social networking technology might have facilitated the implementation of telemedicine. There is a need for high‐quality research in the form of randomised controlled trials (RCTs) or cluster‐RCTs on the effects of telemedicine application in the NICU setting as an educational and support tool for parents or caregivers of infants in the NICU. Comparison should be made between telemedicine, either used alone or alongside other educational or support tools and other support or educational methods without telemedicine in settings where telemedicine technologies have not become the standard facilities for infant care. In settings where telemedicine technologies have been implemented, comparison between different forms of telemedicine facilities may be made. Major outcomes that should be considered include any outcome that is reflective of the care process such as the length of hospital stay, parental satisfaction and confidence, and the frequency of emergency hospital visits post‐discharge of infants.
Authors' conclusions
Implications for practice.
There is insufficient evidence to support or refute the use of telemedicine technology to support the parents of high‐risk newborns receiving intensive care.
Implications for research.
Considering the advances in information technologies over the recent decades, there is a remarkable lack of research in the use of telemedicine in supporting caregivers of infants in NICU. Clinical trials are needed to assess the benefits of telemedicine technology to the NICU population and their caregivers in improving infant care, enabling earlier discharge and improving parental support and education pre‐ and post‐discharge of infants. Depending on the study setting, comparisons may be made between the use of telemedicine versus no telemedicine or between different forms of telemedicine facilities.
History
Protocol first published: Issue 4, 2007 Review first published: Issue 6, 2012
| Date | Event | Description |
|---|---|---|
| 27 October 2008 | New search has been performed | Converted to new review format. |
Acknowledgements
We acknowledge the editors of the Cochrane Neonatal review group who have reviewed our protocol and review: Dr Roger Soll, Dr John Sinclair, Dr Jeffrey Horbar, Prof Michael Bracken and to Ms Diane Haugthon, Managing Editor of the Neonatal Review Group for her assistance leading to the publication of the protocol and review.
Editorial support of the Cochrane Neonatal Review Group has been funded with Federal funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA, under Contract No. HHSN267200603418C.
Appendices
Appendix 1. Search Strategy
Search Strategy: 1 exp "Computer Communication Networks+") OR "Computer Communication Networks" [title, original title, abstract, name of substance word, subject heading word] 2 exp "Online Systems+") OR "Online Systems" [title, original title, abstract, name of substance word, subject heading word] 3 exp "Computer‐Assisted Instruction") OR "Computer‐Assisted Instruction" 4 exp "Diagnosis, Computer‐Assisted+") OR "Diagnosis, Computer‐Assisted" [title, original title, abstract, name of substance word, subject heading word] 5 "Therapy, Computer‐Assisted+") OR "Therapy, Computer‐Assisted" 6 "Computers+") OR "Computers" 7 "Medical Informatics+") OR "Medical Informatics" 8 "Computers, Handheld") OR "Computers, Handheld" 9 "Decision Making, Computer‐Assisted+") OR "decision making, computer‐assisted" 10 "Internet+") OR "Internet" 11 "Microcomputers+") OR "microcomputers" 12 "User‐Computer Interface") OR "user‐computer interface" 13 "Software+") OR "Software" 14 "Telecommunications+") OR "Telecommunications" 15 "Telemedicine+") OR "Telemedicine" 16 "Remote Consultation") OR "Remote Consultation" 17 "Telehealth" 18 "Telenursing") OR "Telenursing" 19 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 20 Limit to Human; Age Related: All Infant: birth‐23 months; Publication Type: Clinical Trial
Data and analyses
Comparison 1. Telemedicine versus standard care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Length of hospital stay (days) | 1 | 56 | Mean Difference (IV, Fixed, 95% CI) | ‐2.10 [‐18.85, 14.65] |
1.1. Analysis.
Comparison 1 Telemedicine versus standard care, Outcome 1 Length of hospital stay (days).
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Gray 2000.
| Methods | Randomised controlled trial | |
| Participants | Very low birth weight infants (n = 75) within 10 days of birth born between November 1997 and April 1999. Infants whose family's primary residences do not have ISDN access, families with no permanent address, non‐English speaking families, discharge to other than biological family, and infants expected to stay in the participating NICU for < 14 days for various reasons were excluded. In case of multiple births, one infant is randomly selected to enter the study | |
| Interventions | Families of infants allocated to intervention were given access to the Baby Carelink telemedicine application, with a multimedia computer, Internet access and videoconferencing equipments installed in their homes within 3 weeks of birth. There are six components in the Baby Carelink Web telemedicine application, including a daily clinical report, a message centre, a "see‐your‐infant" section, a family room, a clinical information section and a section on preparing for discharge. 26 infants were randomised into the intervention group; 7 of their siblings also were allocated to the intervention arm, making 33. Control group received standard neonatal care. 30 infants were randomised to the control arm, with 12 of their siblings also allocated to the control arm with them | |
| Outcomes | Quality of care was assessed after discharge using a standardised family satisfaction survey, administered between one to four months after the child's discharge. Other outcomes include length of hospital stay, family visits, interaction with infants and staff | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study design, paragraph 2, lines 1‐3: "....infants were randomised to the intervention or control group using a birth weight‐stratified permuted block design" |
| Allocation concealment (selection bias) | Unclear risk | No statement on who generated the randomisation sequence and how it was implemented |
| Blinding (performance bias and detection bias) Family satisfaction and length of hospital stay | Unclear risk | There was no description on blinding in the article. Blinding of the families of infants was very unlikely and it was not clear whether hospital caregivers and data collectors were blinded to the status of the participants |
| Blinding (performance bias and detection bias) Episodes of interaction with infants (e.g. holding and kangaroo care) and frequency of family visits | Unclear risk | There was no description on blinding in the article. It was not clear whether data collectors who evaluated these outcomes were blinded to the status pf the participants, especially when they recorded the discharge status of the infants (from NICU, from the level two nurseries, death), parental visits, holding of the infants or kangaroo care |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcomes such as length of stay was obtained from the hospital records. With regards to parental/familial satisfaction surveys, 51 out of 56 eligible families were sent surveys with 31 families responding (61% response rate) |
| Selective reporting (reporting bias) | High risk | The outcomes measured are detailed in the abstract, under "Design/Methods: lines 10‐15: Quality of care was assessed using a standardized family satisfaction survey administered after discharge. In addition, the effect of Baby CareLink on hospital length of stay as well as family visitation and interactions with infant and staff were measured." However, the only outcomes related to visitation that were reported were perceptions on visitation policies, which were parts of the family satisfaction survey. There was no additional report on "family visitation", as implied to be a separate outcome based on the statements above. There was also no report of any form on "interactions with infant and staff" in the results The major outcome of family satisfaction, measured using the Picker Institute’s Neonatal Intensive Care Unit Family Satisfaction survey, was presented in the form of charts (Figures 2 and 3 in the paper) with neither corresponding data labels nor accompanying data figures in the text. This makes data extraction and meta‐analysis impossible. The lead author was contacted by e‐mail on three occasions with request for provide data, and we are still awaiting a reply |
| Other bias | Unclear risk | In the study, 20% of the control group were back‐transferred to their local level two nursery while none of the participants in the intervention group was. It was unclear whether this represented a source of selection bias, or indicated possible co‐intervention (performance bias), or an indication of the need to retain participants in the study setting for the purpose of the study, leading to unequal care process between some of the infants in the intervention group and the control group (for example, all the infants in the control group were transferred back to their local nursery when deemed appropriate as usual, while infants in the intervention group were retained in the study setting for the purpose of the study despite having fulfilled the criteria for transfer‐back to their local nursery), or an important outcome as a direct result of the different assigned intervention. It was impossible to distinguish the various possibilities mainly because of the lack of explanation provided by the authors, including the essential information to enable an assessment of the risks of selection and performance biases. Additionally, transfer‐back to the local nursery was not listed a priori as an outcome |
ISDN: Integrated Services Digital Network NICU: Neonatal Intensive Care Unit
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bhatikar 2002 | A descriptive paper on a tool for telemedicine in the form of Internet enabled, intelligent personal handheld computer, mainly to aid diagnosis of cardiac abnormalities. This is not an original study. |
| Dowie 2009 | Prospective cohort study comparing patients assessed by cardiologist using telemedicine versus face‐to‐face consultation, evaluating clinical feature e.g., symptoms of patients and mean NHS costs in these two modes of assessment. Although the study includes newborn infants, it is not a randomised controlled trial, and does not include parents or family as target in intervention. |
| Guillen 2002 | A study that assesses two different types of home telecare services across five locations in Europe, involving medical staff, patients and home caregivers of patients. Quality of telecare services e.g., audio and video are assessed. No specific assessment on the families of infants cared for in the NICU. |
| McCrossan 2007 | A feasibility study assessing the usefulness of videoconferencing facilities in supporting children with major congenital heart disease and their families after hospital discharge. Families of infants in NICU are not included. |
| Robie 1998 | A study assessing the use of desktop computer‐based video‐teleconference in neonatal surgical consultation, involving surgeons and neonates with surgical conditions. The study does not assess telemedicine as a support tool for families of infants in NICU. |
| Stenson 1998 | A randomised controlled trial assessing the usefulness of regular measurement of respiratory system compliance in mechanically ventilated neonates, not a study on telemedicine technology for parental support in NICU. |
NICU: Neonatal Intensive Care Unit
Differences between protocol and review
The following items have been added.
1. Search yields leading to selection of studies.
2. Description of studies and 'Risk of bias' assessment of the included study, with 'Risk of bias' summary and graph included.
3. Summary of results in RevMan and 'Summary of findings' table.
4. DIscussion, conclusions and abstract.
Contributions of authors
KT and NL co‐wrote the protocol and search strategy. They also conducted searches, evaluations of the studies separately and wrote up the review jointly.
Sources of support
Internal sources
-
Southern Health, Australia.
KT is employed by Monash Medical Centre, Southern Health and Monash University
-
Monash University Sunway Campus, Malaysia, Malaysia.
NML is employed by Monash University Sunway Campus, Malaysia
External sources
-
Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA.
Editorial support of the Cochrane Neonatal Review Group has been funded with Federal funds from the Eunice Kennedy Shriver National Institute of Child Health and Human Development National Institutes of Health, Department of Health and Human Services, USA, under Contract No. HHSN275201100016C.
Declarations of interest
None declared by the authors.
New
References
References to studies included in this review
Gray 2000 {published data only}
- Gray JE, Safran C, Davis RB, Pompilio‐Weitzner G, Stewart JE, Zaccagnini L, et al. Baby CareLink: using the internet and telemedicine to improve care for high‐risk infants. Pediatrics 2000;106:1318‐24. [PUBMED: 11099583] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bhatikar 2002 {published data only}
- Bhatikar SR, Mahajan RL, DeGroff C. A novel paradigm for telemedicine using the personal bio‐monitor. Biomedical Sciences Instrumentation 2002;38:59‐70. [PubMed] [Google Scholar]
Dowie 2009 {published data only}
- Dowie R, Mistry H, Rigby M, Young TA, Weatherburn G, Rowlinson G, et al. A paediatric telecardiology service for district hospitals in south‐east England: an observational study. Archives of Disease in Childhood 2009;94:273‐7. [DOI] [PubMed] [Google Scholar]
Guillen 2002 {published data only}
- Guillén S, Arredondo MT, Traver V, Valero MA, Martin S, Traganitis A, et al. User satisfaction with home telecare based on broadband communication. Journal of Telemedicine and Telecare 2002;8:81‐90. [DOI] [PubMed] [Google Scholar]
McCrossan 2007 {published data only}
- McCrossan B, Morgan G, Grant B, Sands A, Craig B, Casey F. Assisting the transition from hospital to home for children with major congenital heart disease by telemedicine: a feasibility study and initial results. Medical Informatics and the Internet in Medicine 2007;32:297‐304. [DOI] [PubMed] [Google Scholar]
Robie 1998 {published data only}
- Robie DK, Naulty CM, Parry RL, Motta C, Darling B, Micheals M, et al. Early experience using telemedicine for neonatal surgical consultations. Journal of Pediatric Surgery 1998;33:1172‐6; discussion 1177. [DOI] [PubMed] [Google Scholar]
Stenson 1998 {published data only}
- Stenson BJ, Glover RM, Wilkie RA, Laing IA, Tarnow‐Mordi WO. Randomised controlled trial of respiratory system compliance measurements in mechanically ventilated neonates. Archives of Disease in Childhood. Fetal and Neonatal Edition 1998;78:F15‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Brennan 1997
- Brennan PF. The ComputerLink projects: a decade of experience. Studies in Health Technology and Informatics 1997;46:521‐6. [PubMed] [Google Scholar]
Chan 2003
- Chan DS, Callahan CW, Sheets SJ, Moreno CN, Malone FJ. An Internet‐based store‐and‐forward video home telehealth system for improving asthma outcomes in children. American Journal of Health‐System Pharmacy 2003;60:1976‐81. [DOI] [PubMed] [Google Scholar]
Currell 2000
- Currell R, Urquhart C, Wainwright P, Lewis R. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews 2000, Issue 2. [DOI: 10.1002/14651858.CD002098] [DOI] [PubMed] [Google Scholar]
Farel 1991
- Farel AM, Freeman VA, Keenan NL, Huber CJ. Interaction between high‐risk infants and their mothers: the NCAST as an assessment tool. Research in Nursing and Health 1991;14:109‐18. [DOI] [PubMed] [Google Scholar]
Freer 2005
- Freer Y, Lyon A, Stevenson B, Russell C. BabyLink ‐ improving communication among clinicians and with the parents of babies in intensive care. The British Journal of Healthcare Computing & Information Management 2005;22:34‐6. [Google Scholar]
Gentles 2010
- Gentles SJ, Lokker C, McKibbon KA. Health information technology to facilitate communication involving health care providers, caregivers, and pediatric patients: a scoping review. Journal of Medical Internet Research 2010;12:e22. [PUBMED: 20562092] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hersh 2001
- Hersh WR, Helfand M, Wallace J, Kraemer D, Patterson P, Shapiro S, et al. Clinical outcomes resulting from telemedicine interventions: a systematic review. BMC Medical Informatics and Decision Making 2001;1:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jaatinen 2002
- Jaatinen PT, Forsstrom J, Loula P. Teleconsultations: who uses them and how?. Journal of Telemedicine and Telecare 2002;8:319‐24. [DOI] [PubMed] [Google Scholar]
Loyd 1985
- Loyd BH, Abidin RR. Revision of the parenting stress index. Journal of Pediatric Psychology 1985;10:169‐77. [DOI] [PubMed] [Google Scholar]
Marcin 2004a
- Marcin JP, Ellis J, Mawis R, Nagrampa E, Nesbitt TS, Dimand RJ. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics 2004;113:1‐6. [DOI] [PubMed] [Google Scholar]
Marcin 2004b
- Marcin JP, Schepps DE, Page KA, Struve SN, Nagrampa E, Dimand RJ. The use of telemedicine to provide pediatric critical care consultations to pediatric trauma patients admitted to a remote trauma intensive care unit: a preliminary report. Pediatric Critical Care Medicine 2004;5:251‐6. [DOI] [PubMed] [Google Scholar]
McLaren 1995
- McLaren P, Ball CJ. Telemedicine: lessons remain unheeded. BMJ 1995;310:1390‐1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nagendran 2000
- Nagendran S, Moores D, Spooner R, Triscott J. Is telemedicine a subset of medical informatics?. Journal of Telemedicine and Telecare 2000;6 (Suppl 2):S50‐1. [DOI] [PubMed] [Google Scholar]
Pettersen 1999
- Pettersen S, Uldal SB, Baardsgard A, Amundsen M, Myrvang R, Nordvag D, et al. The North Norwegian Health Net. Journal of Telemedicine and Telecare 1999;5 Suppl 1:S34‐6. [DOI] [PubMed] [Google Scholar]
Rendina 1998
- Rendina MC. The effect of telemedicine on neonatal intensive care unit length of stay in very low birthweight infants. Proceedings AMIA Symposium. 1998:111‐5. [PMC free article] [PubMed]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre. Review manager (RevMan). Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration 2011, Version 5.1.
Roine 2001
- Roine R, Ohinmaa A, Hailey D. Assessing telemedicine: a systematic review of the literature. CMAJ 2001;165:765‐71. [PMC free article] [PubMed] [Google Scholar]
Rosenfeld 2000
- Rosenfeld BA, Dorman T, Breslow MJ, Pronovost P, Jenckes M, Zhang N, et al. Intensive care unit telemedicine: alternate paradigm for providing continuous intensivist care. Critical Care Medicine 2000;28:3925‐31. [DOI] [PubMed] [Google Scholar]
Sable 2002
- Sable CA, Cummings SD, Pearson GD, Schratz LM, Cross RC, Quivers ES, et al. Impact of telemedicine on the practice of pediatric cardiology in community hospitals. Pediatrics 2002;109:E3. [DOI] [PubMed] [Google Scholar]
Shiffman 2001
- Shiffman RN, Spooner SA, Kwiatkowski K, Brennan PF. Information technology for children's health and health care: report on the Information Technology in Children's Health Care Expert Meeting, September 21‐22, 2000. Journal of the American Medical Informatics Association 2001;8:546‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shin 2003
- Shin DI, Huh SJ, Lee TS, Kim IY. Web‐based remote monitoring of infant incubators in the ICU. International Journal of Medical Informatics 2003;71:151‐6. [DOI] [PubMed] [Google Scholar]
Speer 1998
- Speer ME. Challenges in the NICU: questions or answers?. Journal of Perinatology 1998;18:S1‐S5. [PubMed] [Google Scholar]
Spinner 1998
- Spinner SS, Girifalco RB, Gibson E, Stavis RL, Greenspan JS, Spitzer AR. Earlier discharge of infants from neonatal intensive care units: a pilot program of specialized case management and home care. Delaware Valley Child Health Alliance. Clinical Pediatrics 1998;37:353‐7. [DOI] [PubMed] [Google Scholar]
Spooner 2004
- Spooner SA, Gotlieb EM. Telemedicine: pediatric applications. Pediatrics 2004;113:e639‐43. [DOI] [PubMed] [Google Scholar]
Strehle 2006
- Strehle EM, Shabde N. One hundred years of telemedicine: does this new technology have a place in paediatrics?. Archives of Disease in Childhood 2006;91:956‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Strehle 2006a
- Strehle E, Shabde N. Telemedicine and paediatrics: an overview. Archives of Diseases in Childhood 2006;91:A61‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thrall 1998
- Thrall JH, Boland G. Telemedicine in practice. Seminars in Nuclear Medicine 1998;28:145‐57. [DOI] [PubMed] [Google Scholar]
Weiner 2001
- Weiner M, Schadow G, Lindbergh D, Warvel J, Abernathy G, Dexter P, et al. Secure internet video conferencing for assessing acute medical problems in a nursing facility. Proceedings / AMIA Annual Symposium. 2001:751‐5. [PMC free article] [PubMed]
Whitten 2002
- Whitten PS, Mair FS, Haycox A, May CR, Williams TL, Hellmich S. Systematic review of cost effectiveness studies of telemedicine interventions. BMJ 2002;324:1434‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whitten 2004
- Whitten P, Mair F. Telesurgery versus telemedicine in surgery‐‐an overview. Surgical Technology International 2004;12:68‐72. [PubMed] [Google Scholar]
Wootton 2001
- Wootton R. Recent advances: Telemedicine. BMJ 2001;323:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wootton 2006
- Wootton R. Realtime telemedicine. Journal of Telemedicine and Telecare 2006;12:328‐36. [DOI] [PubMed] [Google Scholar]


