Abstract
Pregnant women with 2019 novel coronavirus disease (COVID-19) pneumonia are a special group of patients in the pandemic. We report a case of pregnant woman with COVID-19 pneumonia in the second trimester. Clinical and imaging features of the patient were similar to that reported in the literatures for both perinatal patients and non-pregnant patients.
Keywords: COVID-19 pneumonia, Pregnant, Chest CT
Highlights
-
•
Pregnant patient with COVID-19 pneumonia in the second trimester showed typical imaging pattern in chest CT.
-
•
Clinical course of the COVID-19 pneumonia patient in the second trimester was similar to non-pregnant adult patients.
-
•
Recovery of white blood cell counts in pregnant COVID-19 patient should be differentiated with secondary infection.
1. Introduction
At the end of December 2019, a new type of infectious pneumonia, 2019 novel coronavirus disease (COVID-19) pneumonia caused by severe acute respiratory syndrome coronavirus 2(SARS-CoV-2), broke out in Wuhan, China [1,2]. Most infected people present with respiratory symptoms at disease onset, some may worsen to acute respiratory distress syndrome [[3], [4], [5]]. Dysfunction of organs other than respiratory system such as hepatic function impairment may occur and indicate higher risk of progression to severe disease [2]. Chest CT scanning is essential for the diagnosis and treatment monitoring of COVID-19 pneumonia. Radiological findings of COVID-19 pneumonia in non-pregnant adults have been extensively described and summarized,ground-glass opacities that progressed to or co-existed with consolidation are common findings in chest CT [[6], [7], [8]]. Several studies have reported chest CT manifestations of perinatal pregnant patients with COVID-19, with imaging findings showed similar features to non-pregnant patients [[9], [10], [11]]. Imaging features of patients with COVID-19 pneumonia in early and middle pregnancy are rarely reported in detail. Here, we report one case of COVID-19 pneumonia in the second trimester of pregnancy. Clinical characteristics and findings of high-resolution thoracic CT of the patient are described.
2. Case presentation
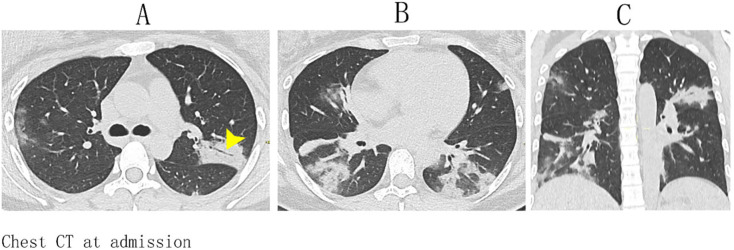
In late January 2020, a 26-year-old woman who was 26 weeks pregnant without underlying illness was admitted to fever clinic of Union Hospital (Tongji Medical College, Wuhan, Hubei Province). She presented a history of fever and myalgia for 10 days followed by dry cough and dyspnea for 3 days. The patient is a healthcare worker in the obstetrics department of a secondary hospital in Wuhan. She had contact history with a COVID-19 patient in maternity ward 2 weeks before onset. On admission (day 1), her vital signs were normal except for elevated body temperature (38.4 °C). Auscultation revealed reduced breath sounds in both lungs. Blood oxygen saturation detected by pulse oximeter was 95%. Complete blood cell count showed normal white blood cell count (WBC, 6.54 × 109/L, normal range 3.5–9.5 × 109/L), mildly elevated neutrophil ratio (76%, normal range 40%–75%) and normal lymphocyte ratio (20%, normal range 20%–50%). Red blood cell count (RBC, 3.43 × 1012/L) and hemoglobin content (106 g/L) decreased slightly. Increased level of interleukin-6 (7.98 pg/mL, normal range 0.1–2.9 pg/mL), was detected. The hypersensitive C-reactive protein level and D-dimer concentration were normal. The liver function test showed elevated alanine aminotransferase (ALT, 94 U/L, normal range 5-35 U/L) and aspartate aminotransferase (AST, 61 U/L, normal range 8-40 U/L), the serum albumin level decreased slightly (Alb, 31.3 g/L, normal range 35-55 g/L) and the total serum bilirubin level was normal (TSB, 14.6 umol/L, normal range 5.1–19.0 umol/L). The patient went through high-resolution chest CT on the day of admission. The examination was performed on a 96 row detector dual source CT scanner (SOMATOM Force, Siemens Healthineers) using the dose saving optimized mode with a lead blanket covering abdomen and pelvis of the patient. Axial images were acquired with tube voltage of 90 kVp and automatically modulated tube current, the volume CT dose index was 3.79 mGy for this scan. Axial images (thickness of 1.5 mm and increment of 1.5 mm) were reconstructed with a matrix size of 512 × 512. Images showed bilateral multifocal peribronchovascular and subpleural areas of airspace disease, affecting lower lobes more than upper lungs. The vast majority of these changes were of mixed density (with groundglass component), with one predominantly dense focus of consolidation with airbronchogram within apicoposterior segment of left upper lobe. No pleural effusion was found (Fig. 1 A–C).
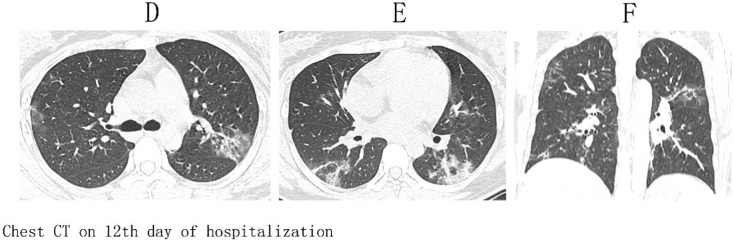
Fig. 1.
CT chest images in axial (A, B) and coronal (C) projections of the pregnant patient at admission. Bilateral multifocal peribronchovascular and subpleural areas of air-space disease, with predilection to the lower lungs demonstrate mixed density. Predominantly dense consolidation with air-bronchogram (arrow head) is present within left upper lobe apicoposterior segment. Scattered opacities of mixed density with groundglass component are identified in subpleural regions of right middle, right upper and bilateral lower lobes.
The throat swabs of the patient were tested positive for nuclear acid of SARS-CoV-2 by real-time fluorescent polymerase chain reaction (RT-PCR). She was treated with antiviral drugs (oseltamivir, recombinant human interferonα-2b and arbidol) and antibiotics (azithromycin, cefdinir). Besides, she received intravenous infusion of magnesium isoglycolate injection to improve hepatic function since admission. Oxygen inhalation through nasal cannula was given to relieve dyspnea with other supportive care. The patient's body temperature has decreased to 37 °C in 6 h after admission without using antipyretics, fluctuated between 36 °C and 37 °C for a week with subsequent stabilization around 36.5 °C thereafter a week later Her dyspnea and cough improved significantly after 2 days of treatment, the blood oxygen saturation rose from 95% at admission to around 98% since day 2. However, hepatic dysfunction has worsened on day 7 (ALT 510 U/L, AST 246 U/L, Alb 27.9 g/L, TSB 13.9 umol/L) despite continuous liver protection treatment. Subsequently, the hepatic function has shown improvement on day 9 after modification of liver protection medication dose and addition of reduced glutathione for injection and showed evident improvement on day 12 (ALT 247 U/L, AST 94 U/L, Alb 32.8 g/L, TSB 10.7 umol/L vs ALT 454 U/L, AST 152 U/L, Alb 31.3 g/L, TSB 10.3 umol/L). Nuclear acid test result of throat swab for the novel coronavirus turned negative on day 11 and the patient was free of symptom. However, the WBC count continued to rise slowly from 6.54 × 109/L at admission to 7.97 × 109/L on day 7, 9.04 × 109/L on day 9 and 10.95 × 109/L on day 12, the ratios of neutrophil and lymphocyte were in normal range in latter tests. To evaluate changes in lung lesions after treatment and look for possible secondary infection indicated by leukocytosis, the patient underwent a chest CT on the same CT scanner with same imaging protocol as previously described, and the volume CT dose index of the scan was 3.86 mGy. Bilateral lesions were greatly improved, the residual disease presented mainly with opacities of mixed density and ground-glass, no new foci of airspace was involved (Fig. 2 D–F). The patient was discharged from hospital on day 13 with the prescription of oral medicine of polyene phosphatidylcholine, and she was asked to stay quarantined at home for another two weeks. By the end of observation, the patient recovered well without any discomfort.
Fig. 2.
Follow-up CT chest images in axial (D, E) and coronal (F) projections of the same patient on the 12th day from admission. Significant improvement of pre-existing foci of air-space disease with decreased size and density is evident, with no new foci of lung involvement.
3. Discussion
We reported a case of pregnant woman with COVID-19 pneumonia in the second trimester, who had a history of exposure to confirmed cases, positive nucleic acid test results and typical clinical manifestations at admission. The clinical characteristics of pregnant woman in this report were similar to those in late pregnancy and non-pregnant adult patients [4,9]. The onset symptoms of the patient were fever and myalgia, followed by dry cough and dyspnea. These clinical presentations were among the most common symptoms in pregnant patients with COVID-19 pneumonia [12]. Similar to most pregnant cases reported in Wuhan city, the patient in our report showed mild to moderate clinical symptoms, and responded well to treatment and recovered completely [12]. Hepatic function impairment was common in patients with COVID-19 including perinatal patients, which occurred more often in the severe course of the disease [2,12]. The liver function abnormality in COVID-19 patients may be result of immune mediated damage due to inflammatory response, direct toxicity to hepatic cells, drug induced liver injury or reactivation of per-existing liver disease [13]. The hepatic dysfunction in our patient at admission is most likely resulted from the combined drug and SARS-CoV-2 viral toxicity. While the worsening of liver function impairment during first week of hospitalization may have greater relation to toxicity of the antiviral drug, as general condition of the patient showed evident improvement after admission. The liver function showed gradual improvement after strengthening liver protection protocol. The rising WBC count raised suspicion of secondary bacterial infection in lungs. However, imaging findings of follow-up chest CT showed significant improvement. As the WBC count could increase physiologically in pregnant population, the slowly rising WBC count with normal granulocyte and lymphocyte ratios in our patient was thought to be the process of normalization recovering from relatively low value caused by virus infection. Because no ultrasound or related examinations were performed on the fetus during treatment, it is unclear what damage the infection and treatment may cause to the fetus. Infection of the novel coronavirus in pregnant women during the perinatal period does not seem to have a significant adverse effect on the neonates [12]. However, there is a lack of data on the impact of maternal infection on the fetus during the second trimester.
Patients with COVID-19 pneumonia usually have a long clinical course, even mild patients with mild to moderate symptoms need 2 to 3 weeks to recover [4]. As the clinical condition changes dynamically during the course, chest CT is of considerable value for diagnosis and treatment monitoring of COVID-19 pneumonia. Chest CT performed at different time points in the process showed dynamic changes [6,8]. Lung lesions often gradually expand in size and increase in density and reached a peak in about 2 weeks after onset, followed by gradual decrease under continuous supportive treatment. Subpleural ground glass opacity is the main imaging finding in the early stage of disease, and the bilateral lower lobes are most often involved. The imaging abnormality may expand quickly with thickening of interlobular interstitium and gradually turned to patchy consolidation. With the support of symptomatic treatment, consolidation within the lungs will undergo a gradual process of resolution [6,8]. Pregnant patients with COVID-19 pneumonia showed similar course in imaging as non-pregnant patients [10]. The initial CT scan of our patient showed multiple subplerual and peribronchovascular areas of air-space disease with various density involving bilateral lower lobes, left upper lobe, and to lesser extent right middle lobe. The mixed densities of opacities containing ground-glass and consolidation demonstrated the dynamic transition of early phase to peak phase in COVID-19 pneumonia. Imaging manifestations in 10 days after symptom onset of the patient was consistent with characteristics of peak period according to staging system by Pan et al. [8]. Follow-up CT chest performed for suspicion of superimposed secondary bacterial infection after 10 days from the initial exam has shown resolving changes of pre-existing areas of air-space disease, with no new areas of lung involvement. Although contradiction between imaging change and clinical condition evolution was reported for a pregnant patient, as described in most studies, the improvement in imaging corresponded to clinical recovery in our report [14].
In conclusion, the patient in the second trimester with COVID-19 pneumonia in our report showed similar clinical and imaging features as patients in late pregnancy and non-pregnant adult patients. Chest CT findings corresponded well to clinical condition evolution while hepatic toxicity of antiviral drugs may cause the delayed recovery of liver function in the patient.
CRediT author statement
Jing Wang, Conceptualization, Resources, Writing - Review & Editing.
Shenglei Shu: Data curation, Writing - Original Draft.
Chuansheng Zheng, Conceptualization, Writing - Review & Editing, Supervision.
Tianjing Zhang: Writing - Review & Editing.
Declaration of competing interest
The authors declare no conflicts interests.
Acknowledgements
None.
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guan W., Ni Z., Hu Y., Liang W., Ou C., He J. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. Jama. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Song F., Shi N., Shan F., Zhang Z., Shen J., Lu H. Emerging coronavirus 2019-nCoV pneumonia. Radiology. 2020:200274. doi: 10.1148/radiol.2020200274. [DOI] [Google Scholar]
- 8.Pan F., Ye T., Sun P., Gui S., Liang B., Li L. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020:200370. doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020 doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu D., Li L., Wu X., Zheng D., Wang J., Yang L. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: a preliminary analysis. Am J Roentgenol. 2020:1–6. doi: 10.2214/AJR.20.23072. [DOI] [PubMed] [Google Scholar]
- 11.Liu H., Liu F., Li J., Zhang T., Wang D., Lan W. Clinical and CT imaging features of the COVID-19 pneumonia: focus on pregnant women and children. J Infect. 2020 doi: 10.1016/j.jinf.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen L., Li Q., Zheng D., Jiang H., Wei Y., Zou L. Clinical characteristics of pregnant women with Covid-19 in Wuhan, China. N Engl J Med. 2020 doi: 10.1056/NEJMc2009226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun J., Aghemo A., Forner A., Valenti L. COVID-19 and liver disease. Liver Int. 2020;40(6):1278–1281. doi: 10.1111/liv.14470. [DOI] [PubMed] [Google Scholar]
- 14.Liao X., Yang H., Kong J., Yang H. Chest CT findings in a pregnant patient with 2019 novel coronavirus disease. Balkan Med J. 2020 doi: 10.4274/balkanmedj.galenos.2020.2020.3.89. [DOI] [PMC free article] [PubMed] [Google Scholar]