Abstract
The present manuscript deals with experimental infections of bonnet macaques (Macaca radiata) to study disease progression for better insights into the Kyasanur Forest Disease (KFD) pathogenesis and transmission. Experimentally, 10 monkeys were inoculated with KFD virus (KFDV) (high or low dose) and were regularly monitored and sampled for various body fluids and tissues at preset time points. We found that only 2 out of the 10 animals showed marked clinical signs becoming moribund, both in the low dose group, even though viremia, virus shedding in the secretions and excretions were evident in all inoculated monkeys. Anti-KFDV immunoglobulin (Ig)M antibody response was observed around a week after inoculation and anti-KFDV IgG antibody response after two weeks. Anaemia, leucopenia, thrombocytopenia, monocytosis, increase in average clotting time, and reduction in the serum protein levels were evident. The virus could be re-isolated from the skin during the viremic period. The persistence of viral RNA in the gastrointestinal tract and lymph nodes was seen up to 53 and 81 days respectively. Neuro-invasion was observed only in moribund macaques. Re-challenge with the virus after 21 days of initial inoculation in a monkey did not result in virus shedding or immune response boosting.
Subject terms: Microbiology, Pathogenesis
Introduction
Kyasanur Forest Disease (KFD) was first discovered in Sagar and Sohrab taluks of Shimoga district of Karnataka state in 19571. The disease, which was endemic to Karnataka state, India, were reported from neighbouring states along the Western Ghats like Tamil Nadu, Goa, Maharashtra and Kerala in the last decade2. Kyasanur forest disease virus (KFDV) belongs to the tick borne encephalitis serogroup of the Flaviviridae family, which causes disease in humans and monkeys3–5. Studies revealed ticks of the species Haemaphysalis as the principal vector and reservoir for the virus6.
The disease in humans is characterized by fever, headache, myalgia, conjunctivitis, diarrhoea, vomiting, and haemorrhagic manifestations with a case fatality rate of up to 4%7–9. Presbytus entellus (Black faced langur) and Macaca radiata (Bonnet macaque), which are abundant in the Western Ghats region of India, are the most affected species of animals; acting as sentinels for the virus spread in an area10,11. The susceptibility of both the species has been proven experimentally too11–13. Though KFDV was isolated in 1957, the disease remained understudied due to lack of biocontainment facilities in India until recently.
Although rodent models were used for KFD study in the past, experimentally induced disease in those differed from published descriptions of human disease (mice developed neurologic disease and did not become febrile and lacked marked spleen and liver pathology) making rodent models less predictive of human KFD14–16. The literature available to date about KFD in Presbytus entellus and Macaca radiata is based on naturally infected dead animals or experimental infections wherein high dose of an early isolate of virus maintained by suckling mouse brain passages were used11–13. A decade long study conducted on monkey mortality in KFD endemic area revealed that, out of 1,046 deaths, 860 were P. entellus and only 186 were M. radiata with virus isolation percentage of 50% and 18.05% in necropsied animals respectively17. In agreement with these findings, an experimental infection studies conducted at Virus Research Centre, Pune between 1958 and 1970 found langurs to be highly susceptible to KFDV with per acute course of the disease compared to bonnet macaques. In bonnet macaques disease course was comparatively prolonged with few deaths during viremic phase and few during third week, with virus recovery from the brain similar to human biphasic disease wherein fever and signs of neurological manifestations are reported in third week12. Another study in bonnet macaques demonstrated, virus-specific gastrointestinal and lymphoid lesions and viral antigens in these same organs by immunohistochemistry in experimentally infected animals11. The above studies confirmed the suitability of bonnet macaque as a model to study viscerotropic KFD seen in humans.
Detailed information about multiple aspects of KFD progression with regard to persistence of viremia, time point of first detection, further persistence and titres of anti-KFD IgM and IgG antibodies, viral kinetics and lesions induced in different organs, duration of virus shedding in different secretions and body fluids, biochemical and hematological changes during infection is not available so far. Study of dynamics of various above mentioned parameters, upon inoculation with high and low dose of virus in bonnet macaques was undertaken with the aim to recapitulate the human disease, as bonnet macaques are known to be the only suitable model for KFD studies.
Results
Experimental design
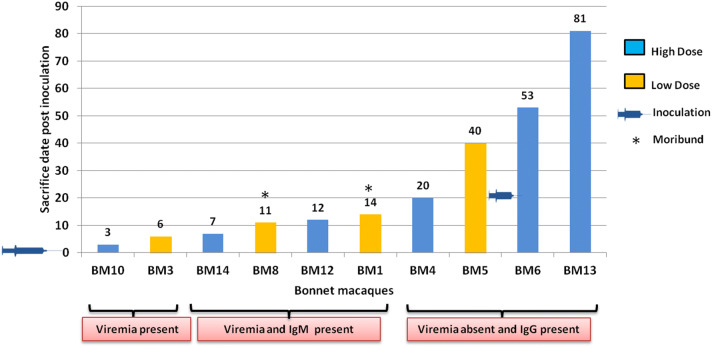
The experiment was performed for duration of 3 months (March to May, 2018). Bonnet macaques (BM) were randomly assigned into three groups: High dose (Monkey nos: BM4, BM6, BM10, BM12, BM13, BM14), low dose (BM1, BM3, BM5, BM8) and control (BM7). The high dose group was inoculated with 105.57 TCID50 of KFDV, low dose group with 103.57 TCID50 and control with uninfected BHK-21 cell supernatant of the same passage by subcutaneous (s/c) route (1 ml) below the nape of the neck under sedation. Animals were observed twice daily for any clinical signs. Rectal temperature was monitored daily, and body weight was measured every third day post infection (PID). One monkey from each group was sacrificed during (1) viremia, (2) viremia along with IgM response and (3) after the end of viremia along with IgG response (Fig. 1). Two macaques, which reached the set humane end points, were sacrificed immediately during the experiment. One macaque was sacrificed on 20th PID, to understand the biphasic nature/neuroinvasion of KFDV and one macaque (BM6) was re-inoculated with 105.57 TCID50 dose on 21st PID. Three macaques (BM-5, BM-6 and BM-13) were kept for longevity study and were sacrificed on 40th, 53rd and 81st PID respectively.
Figure 1.
Bonnet macaque sacrifice time points. Each bar (yellow: low dose, blue: high dose) represents the days on which monkeys were sacrificed post KFDV inoculation. Monkeys which became moribund are highlighted with an asterisk. All the monkeys were inoculated with KFDV on day 0 and BM-6 was re-inoculated on day 21.
Clinical findings
In the low dose group, two (BM-5 and BM-8) monkeys developed fever. BM-5 showed the rise in temperature (102 °F–104 °F) from 5th to 9th PID, which dropped to normal (< 102 °F) by 10th PID. Fever, ocular discharge, and watery diarrhoea were observed in BM-8 from 5th PID. The animal became anorexic and exhibited blood tinged diarrhoea from 7th PID. The body condition deteriorated with weight loss of around 13% and was sacrificed on 11th PID. Another monkey from low dose group (BM-1) became anorexic and showed a weight loss of around 8%. On 14th PID, subnormal rectal temperature of 97 °F was noted in BM-1 and was sacrificed.
In the high dose group, BM-14 and BM-13 showed a slight increase in temperature (102 °F) on 4th PID. Signs of dehydration (reduced skin elasticity), reduced activity and anorexia were observed in BM-14. BM-6 showed an increase in temperature up to 103 °F on 11th PID. The other five monkeys (BM4, BM10, BM12, BM3 and BM7) did not show any clinical signs or weight loss throughout the study period.
Haematology and serum biochemistry
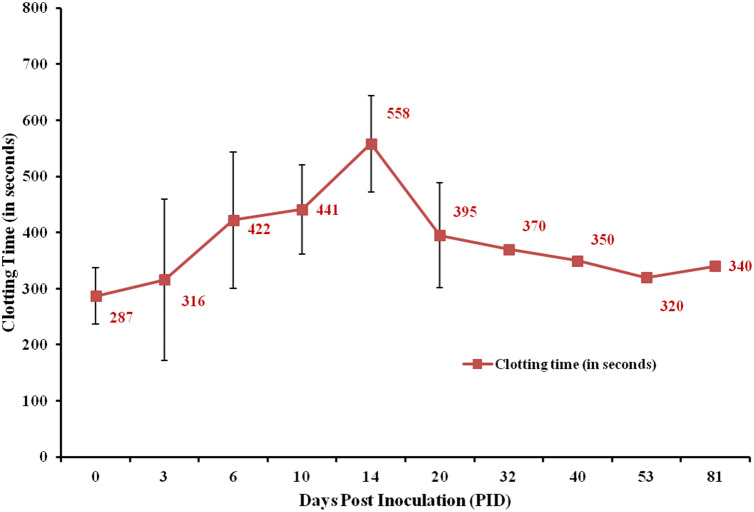
The blood samples were collected daily from the saphenous vein during the first two weeks post inoculation, which was followed by twice a week collection for the next week and once in a week later till they were sacrificed. From the re-inoculated macaque (BM6), minimum quantity of blood was collected on alternate days from 21st to 32nd PID (10 days post re-inoculation) for testing viremia and antibody response, after which blood was collected once every week till sacrifice. The average clotting time increased progressively from an average of 286.91 s at day 0 to 558 s on 14th PID, after which it gradually reduced to 340 s on 81st PID (Fig. 2). There was no significant change in prothrombin time (PT) and activated partial thromboplastin time (aPTT). No change in clotting time was noted for BM7 (control).
Figure 2.
Clotting time. Comparison of average clotting time values at different days post KFDV inoculation. The group sizes at day 0, 3, 6, 10, 14, 20 days post inoculation were 10, 9, 9, 6, 5 and 4 respectively and thereafter 1 animal each.
There was no statistically significant variation in any biochemical parameters when data from macaques inoculated with low and high dose; and from moribund and recovered macaques were compared. Therefore, a comparison was made between various time-points. Time points analysed were broadly distributed between day 0, day 3, day 6, day 10, day 14 and 21. The analysis was not performed after 21st PID, as the number of samples collected after that time point were limited (Table 1). There was statistical significant decrease in haemoglobin between day 0 and day 3 (p = 0.0050), and between day 0 and 6 (p = 0.0076). Other factors which showed significant decrease between day 0 and day 3, and day 3 and day 6 were total leukocyte count (p = 0.0051, 0.0077), platelets (p = 0.0069, 0.0108), RBC count (p = 0.0051, 0.0077), PCV (p = 0.0069, 0.0077), neutrophils (p = 0.0151), ALT (p = 0.0128), AP (p = 0.0109), total protein (p = 0.0069, 0.0077), albumin (p = 0.0051, 0.0077), and globulin (p = 0.0069, 0.0209). A significant increase was seen in percent monocytes (p = 0.0322, 0.0276), total bilirubin (p = 0.0438), conjugated bilirubin (p = 0.0236) and AST (p = 0.0218) values between baseline to beginning of viremia, and between the beginning of viremia to the peak of viremia. No significant change was observed between any other time points and other parameters.
Table 1.
Haematology and serum biochemistry parameters analysed at day 0, 3, 6 and 10 post inoculation.
| Parameter | Mean ± SD | Significance | |||||
|---|---|---|---|---|---|---|---|
| Day 0 (n = 10) | Day 3 (n = 10) | Day 6 (n = 9) | Day 10 (n = 7) |
p value Day 0 vs Day 3 |
p value Day 3 vs Day 6 |
||
| 1 | Hemoglobin, (g/dL) | 13.3 ± 1.1 | 12.2 ± 1.3 | 11.1 ± 1.1 | 10.5 ± 1.1 | 0.0050 | 0.0076 |
| 2 | Total leucocytes (/µL) | 12,650 ± 3,961 | 8,120 ± 3,265 | 5,344 ± 1,165 | 11,671 ± 4,028 | 0.0005 | 0.0077 |
| 3 | Platelets (/µL) | 421,700 ± 85,268 | 323,000 ± 116,264 | 279,111 ± 78,731 | 309,666 ± 161,877 | 0.0069 | 0.0108 |
| 4 | RBC (× 106/µL) | 6.6 ± 0.5 | 6.0 ± 0.7 | 5.5 ± 0.6 | 5.1 ± 0.6 | 0.0051 | 0.0077 |
| 5 | PCV (%) | 42.8 ± 3.0 | 39.5 ± 3.7 | 35.9 ± 3.2 | 33.7 ± 3.3 | 0.0069 | 0.0077 |
| 6 | MCV (fL) | 65.3 ± 5.7 | 65.8 ± 5.3 | 65.2 ± 6.0 | 65.8 ± 4.5 | NS | NS |
| 7 | MCH (pgms) | 20.3 ± 2.1 | 20.4 ± 2.1 | 20.2 ± 2.2 | 20.6 ± 1.9 | NS | NS |
| 8 | MCHC (g/dL) | 31.1 ± 0.8 | 30.9 ± 1.0 | 30.9 ± 0.8 | 31.3 ± 0.9 | NS | NS |
| 9 | RDW (%) | 15.1 ± 1.7 | 15.3 ± 2.3 | 14.7 ± 2.2 | 14.7 ± 1.8 | NS | NS |
| 10 | Neutrophils (%) | 57.6 ± 8.9 | 62.0 ± 12.8 | 49.0 ± 9.9 | 47.9 ± 17.2 | 0.0151 | NS |
| 11 | Eosinophils (%) | 1.1 ± 1.0 | 1.3 ± 1.2 | 0.9 ± 0.8 | 1.4 ± 1.1 | NS | NS |
| 12 | Basophils (%) | 0.1 ± 0.3 | 0.2 ± 0.4 | 0.3 ± 0.5 | 0.0 ± 0.0 | NS | NS |
| 13 | Lymphocytes (%) | 38.3 ± 8.6 | 30.4 ± 13.1 | 42.3 ± 9.2 | 42.1 ± 14.8 | NS | NS |
| 14 | Monocytes (%) | 2.9 ± 1.0 | 6.1 ± 3.4 | 7.4 ± 3.5 | 8.6 ± 2.2 | 0.0322 | 0.0276 |
| 15 | Bilirubin NS total (mg/dL) | 0.1 ± 0.1 | 0.2 ± 0.1 | 0.2 ± 0.1 | 0.2 ± 0.1 | 0.0438 | NS |
| 16 | Bilirubin NS conjugated (mg/dL) | 0.03 ± 0.02 | 0.06 ± 0.02 | 0.05 ± 0.03 | 0.05 ± 0.01 | 0.0236 | NS |
| 17 | Bilirubin NS unconjugated(mg/dL) | 0.07 ± 0.0 | 0.11 ± 0.1 | 0.12 ± 0.1 | 0.12 ± 0.1 | NS | NS |
| 18 | SGOT (AST), (U/L) | 28.5 ± 9.0 | 45.4 ± 18.5↑ | 49.7 ± 15.9 | 229.1 ± 398.6 | 0.0218 | NS |
| 19 | SGPT (ALT), (U/Lt) | 40.8 ± 27.3 | 42.6 ± 20.4 | 27.3 ± 9.2 | 62.0 ± 59.5 | 0.0128 | NS |
| 20 | ALP (U/L) | 447.1 ± 202.4 | 453.6 ± 183.5 | 353.2 ± 147.0 | 394.0 ± 131.8 | 0.0109 | NS |
| 21 | Protein (total) (g/dL) | 8.4 ± 0.5 | 7.5 ± 0.5 | 5.3 ± 1.8 | 6.8 ± 0.7 | 0.0069 | 0.0077 |
| 22 | Albumin (g/dL) | 3.6 ± 0.2 | 3.2 ± 0.2 | 2.6 ± 0.5 | 2.5 ± 0.3 | 0.0051 | 0.0077 |
| 23 | Globulin (g/dL) | 4.9 ± 0.4 | 4.3 ± 0.3 | 2.7 ± 1.5 | 4.4 ± 0.6 | 0.0069 | 0.0209 |
| 24 | Urea (mg/dL) | 25.8 ± 4.3 | 26.0 ± 6.7 | 25.4 ± 9.8 | 87.1 ± 161.6 | NS | NS |
Paired T-tests was used to compare data between various time-points and the p value of parameters which showed significant difference.
NS non significant.
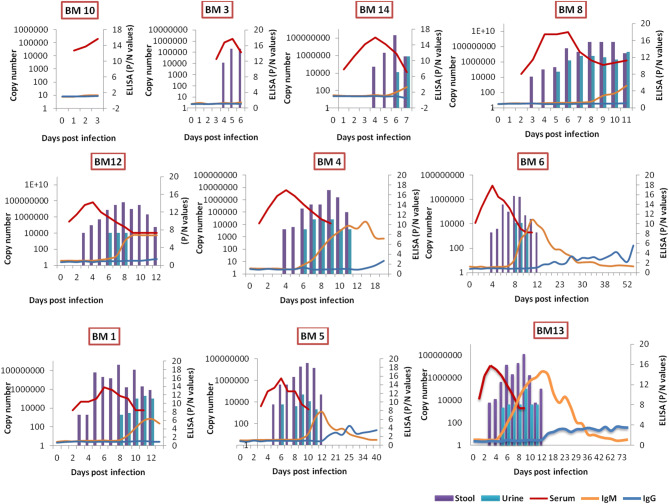
Presence of anti-KFDV IgM and IgG antibodies
In macaques inoculated with high dose, anti-KFDV IgM and IgG antibodies could be detected from 6th to 42nd PID (peak: 11th–12th PID, OD: 1.147, P/N: 14.6) and 14th PID onwards (peak: 45th PID, OD: 0.632, P/N: 4.22), respectively. In macaques inoculated with a low dose, anti-KFDV IgM and IgG antibodies could be detected from 9th to 34th PID (peak PID: 12, OD: 0.878, P/N: 6.381) and IgG from 18th PID onwards (At PID 40, OD: 0.555, P/N: 3.5) (Fig. 3). The longevity of anti-KFDV IgG could not be estimated beyond day 81 due to experimental limitations. BM7 (control) was negative for anti-KFDV antibodies.
Figure 3.
Graphs represent the copy number of KFDV RNA in serum (red line), stool (violet bar) and urine (green bar) (primary y axis) and P/N values of anti-KFDV IgM (orange line) and IgG (blue line) ELISA (secondary y axis) in each macaque at days post KFDV inoculation.
KFDV RNA in serum, other body fluids, and organs
Viremia could be detected from 1st to 13th PID in high dose group, with a peak on 3rd to 4th PID (Fig. 3). The viral RNA detection in rectal swabs, stool and urine ranged from 3rd to 13th PID, 3rd to 12th PID and 7th to 12th PID, respectively (see Supplementary Table S1). KFDV RNA could be detected in conjunctival swabs and oro-pharyngeal swabs on 10th PID in all KFDV inoculated monkeys. Virus shedding was not observed after re-inoculation in BM-6. In the low dose group, viremia was observed from 3rd to10th PID, and the peak was observed at 6th PID. Rectal swabs and urine were found positive for KFDV RNA from 5th to 12th PID and 6th to11th PID respectively.
The organs that showed the presence of virus from 3rd PID onwards were liver, spleen, ovary and skin. The skin was positive for viral RNA from 3rd PID to 20th PID with increasing viral RNA copy numbers. The lymph nodes were positive with consistently high viral RNA from 3rd to 81st PID followed by stomach, small intestine and large intestine from 3rd PID to 53rd PID. Presence of the virus in the brain was observed only in moribund macaques (BM8, BM1). BM14, sacrificed on 7th PID showed the presence of KFDV RNA in cerebrospinal fluid (CSF) but not in the brain (Table 2).
Table 2.
Viral load in serum, other body fluids, and organs.
| S. no | Organ | Viral RNA copy number | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| BM10 (high, sacrifice: PID3) | BM3 (low, sacrifice: PID6) | BM14 (high, sacrifice: PID7) (dehydrated and lethargic) | BM8 (low, sacrifice: PID 11) (Moribund) | BM12 (high, sacrifice: PID12) | BM1 (low, sacrifice: PID14) (Moribund) | BM4 (high, sacrifice: PID 20) | BM5 (low, sacrifice: PID 40) | BM6 (high, sacrifice: PID 53) | BM13 (high, sacrifice: PID 81) | ||
| 1 | CSF | Negative | Negative | 1 × 104 | 6 × 104 | Negative | 3 × 104 | Not collected | Negative | Negative | Negative |
| 2 | Cerebellum | Negative | Negative | Negative | 1 × 109 | Negative | 2.5 × 105 | Negative | Negative | Negative | Negative |
| 3 | Cerebrum | Negative | Negative | Negative | 3 × 107 | Negative | Negative | Negative | Negative | Negative | Negative |
| 4 | Olfactory bulb | Negative | Negative | Negative | 1 × 104 | Negative | Negative | Negative | Negative | Negative | Negative |
| 5 | Hippocampus | Negative | Negative | Negative | 4 × 106 | Negative | Negative | Negative | Negative | Negative | Negative |
| 6 | Medulla oblongata | Negative | Negative | Negative | Not collected | Negative | 6 × 104 | Negative | Negative | Negative | Negative |
| 8 | Pancreas | Negative | 1 × 104 | 3 × 107 | 8 × 106 | Negative | 6 × 108 | 2.5 × 105 | 1.2 × 105 | 6 × 104 | Negative |
| 9 | Liver | 3 × 104 | 2.5 × 105 | 8 × 106 | 4 × 106 | Negative | 3 × 104 | 2.5 × 105 | Negative | Negative | Negative |
| 10 | Spleen | 6 × 104 | 2.5 × 104 | 3 × 107 | 4 × 1010 | 3 × 107 | 1 × 109 | 3 × 107 | 2.5 × 105 | 2.5 × 105 | Negative |
| 11 | Kidney | Negative | 2.5 × 104 | 3 × 104 | 3 × 107 | Negative | 1.2 × 105 | 6 × 104 | Negative | Negative | Negative |
| 12 | Heart | Negative | 2.5 × 104 | 3 × 104 | 3 × 107 | Negative | 1.5 × 104 | Negative | Negative | Negative | Negative |
| 13 | Lungs | Negative | 2 × 104 | 1.2 × 105 | 3 × 108 | Negative | 1 × 106 | 1.2 × 105 | Negative | Negative | Negative |
| 14 | Gall bladder | Negative | 2 × 104 | 2 × 106 | 6 × 104 | Negative | 6 × 104 | Negative | Negative | Negative | Negative |
| 15 | Bile | Negative | Negative | Negative | 1 × 106 | Negative | Negative | Negative | Negative | Negative | Negative |
| 16 | Stomach | 5 × 105 | 1 × 106 | 5 × 109 | 1 × 109 | 7 × 107 | 3 × 107 | 6 × 104 | 2.5 × 104 | 1 × 104 | Negative |
| 17 | Small intestine | 2.5 × 105 | 4 × 106 | 3 × 107 | 1 × 109 | 2.5 × 105 | 6 × 104 | 2 × 109 | 3 × 104 | 1 × 104 | Negative |
| 18 | Large intestine | 5 × 105 | 5 × 108 | 6 × 108 | 6 × 108 | 1 × 107 | 3 × 108 | 5 × 105 | 2.5 × 104 | 6 × 104 | Negative |
| 19 | Mesentric lymph node | 5 × 105 | 5 × 109 | 4 × 1010 | 8 × 106 | 1 × 108 | 5 × 109 | Not collected | 1 × 107 | 3 × 107 | 4 × 106 |
| 20 | Ovary | 3 × 104 | 1.2 × 105 | 3 × 104 | 8 × 106 | Negative | 2.5 × 105 | 6 × 104 | Negative | Negative | Negative |
| 21 | Back skin | 6 × 104 | 1.5 × 104 | 1 × 106 | 250,000 | Negative | 1.2 × 105 | 6 × 108 | Negative | Negative | Negative |
| 22 | Urinary bladder | Negative | 2.5 × 104 | 2 × 106 | 2 × 106 | Negative | 6 × 104 | Negative | Negative | Negative | Negative |
| 23 | Urine | Negative | Not collected | 8 × 106 | Negative | Negative | Negative | Negative | Negative | Negative | Negative |
| 24 | Serum | 106 | 5 × 105 | 6 × 104 | 8 × 106 | Negative | Negative | Negative | Negative | Negative | Negative |
| 25 | Throat swab | Negative | 1.5 × 104 | 3 × 104 | 1.5 × 104 | Negative | 1 × 104 | Negative | Negative | Negative | Negative |
| 26 | Conjunctival swab | Negative | Negative | 1.5 × 104 | 1 × 107 | Negative | 1 × 104 | Negative | Negative | Negative | Negative |
| 27 | Rectal swab/stool | Negative | 1 × 106 | 4 × 106 | 1 × 108 | 3 × 104 | 1 × 106 | 1.5 × 104 | Negative | Negative | Negative |
Virus isolation from skin
The infant mice litters inoculated with monkey skin suspensions of BM10 (sacrificed on 3rd PID) and BM14 (sacrificed on 7th PID) showed sickness. Brain suspensions of sick mice were found positive for KFDV RNA with 1.3 × 1012 (BM10) and 2.7 × 1012 (BM14) copy numbers.
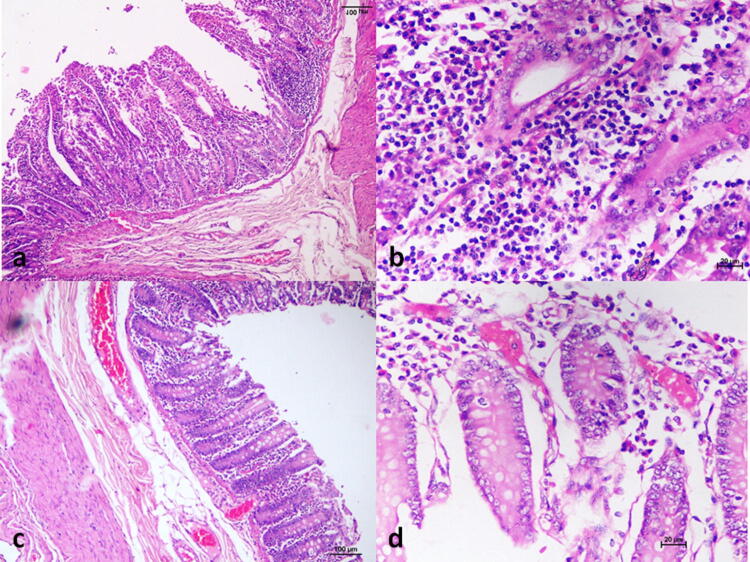
Histopathology
The histopathological changes observed were minimal irrespective of the dose of inoculation, and majority of the changes were observed in the gastrointestinal tract (GIT). Mucosal ulceration and focal/mild mononuclear cell infiltration were observed in stomach (BM-3, BM-4, BM-6, BM-8, BM-10, BM-14), small intestine (Fig. 4a, b) (BM-3, BM-4, BM-10, BM-14) and large intestine (BM-1, BM-3, BM-6, BM-10, BM-13, BM-14, BM-5). Mild sub-mucosal congestion was also observed in the large intestine (Fig. 4c, d) in BM-1, BM-4, and BM-8. Kidneys showed inflammatory cell infiltration in the cortex and medulla in BM-1, BM-5, BM-6, BM-8 and BM-14. Other organs did not show any marked histopathological changes except few focal degenerative foci in liver in BM-8 and BM-14.
Figure 4.
Histopathological observations. (a) Mucosal ulceration and focal mononuclear infiltration in small intestine, H&E, × 100, (b) mononuclear cell infiltration in the small intestine, H&E × 200, (c) sub-mucosal congestion in the large intestine, H&E × 100, (d) submucosal congestion in the large intestine, H&E, × 200.
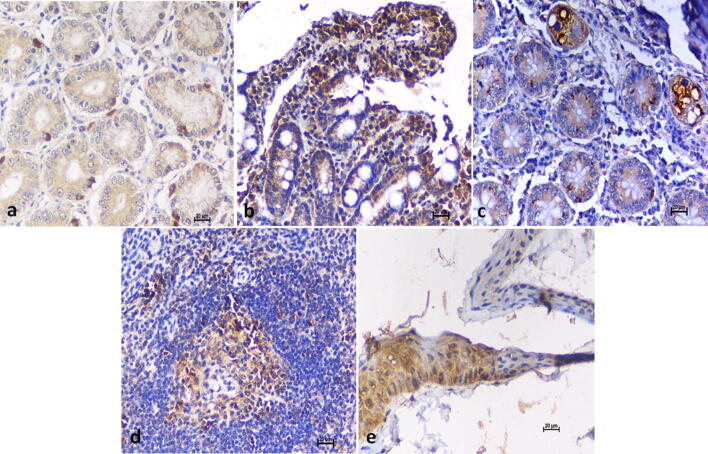
Immunohistochemistry
In case of high dose virus inoculated monkeys, positivity was observed in monkeys sacrificed on 3rd, 7th, 12th and 53rd PID in stomach (Fig. 5a) and small intestine (Fig. 5b). Large intestine showed immunostaining in BM-3, BM-6, BM-8 and BM-14 (Fig. 5c). In case of monkeys inoculated with low dose and sacrificed on 6th, 11th and 14th PID, cytoplasmic immunostaining was observed in stomach, small intestine and spleen (Fig. 5d). Skin positivity was observed in monkeys sacrificed on 3rd, 6th, 7th, 11th, 14th and 53rd PID (Fig. 5e).
Figure 5.
Immunohistochemistry. (a) Stomach: cytoplasmic immunostaining of glandular cells, DAB × 200, (b) Small intestine: immunostaining of intestinal mucosa, DAB × 200. (c) Large intestine: immunostaining of epithelium, DAB × 200, (d) Spleen: immunostaining of splenic white pulp, DAB × 200, (e) Skin: immunostaining of epidermis layer, DAB × 200.
Cytokine analysis
Out of the six cytokines analyzed in stimulated splenocytes, only IL-6 could be detected. A clear pattern of IL-6 secretion was observed from 7th to 14th PID in splenocytes of BM14, BM8 and BM1. The cytokine secretion was found minimal in BM12. Non-stimulated splenocytes did not show any cytokine secretion (Fig. 6).
Figure 6.
Cytokine analysis. Profile of IL-6 secretion of KFDV stimulated splenocytes in different macaques at sacrifice.
Taqman low density array
Out of the 92 genes of the immune panel studied, 15 genes showed marginal fold change (see Supplementary Fig. S1). The fold change did not show any specific trend across various points of sacrifice. Pro-inflammatory cytokines showing up regulation were IL15 (BM12, BM4) and Colony Stimulating Factor 3 (CSF3) (BM10, BM3, BM14, BM8, BM4, BM5).T helper 1 (Th1) specific genes that showed fold increase were IFNγ (BM5), IL18 (BM1, BM4), IL2 (BM1, BM4), IL12A (BM10, BM1). IL2 was found marginally down-regulated in BM8. Th2 specific genes which showed up regulation were Cytotoxic T Lymphocytic Associated Protein-4 (CTLA4) (BM10, BM5, BM6), Human Leukocyte Antigen – DR isotype A (HLA-DRA) (BM14, BM4) and IL13 (BM8, BM12, and BM1) were found to be down regulated. Other genes that showed marginal fold change were Intercellular Adhesion molecule 1 (ICAM1), Selectin P (SELP), Selectin E (SELE),and Fas ligand (FASLG).
Overall the pro-inflammatory genes, namely CSF3, chemokine (C-X-C motif) ligand 10(CXCL10), and SELE, were found consistently marginally elevated in all monkeys except BM12. Th1 genes, namely, IL2, IL12A, IL18, IFN-gamma, and IL15 were found elevated from 14thPID to 40th PID. IL13 was marginally down regulated from 11th PID to 14th PID. Supportive Th2 genes, namely CTLA4 and HLA-DRA were marginally elevated, though not consistently. Other genes showing increased fold change were SELP, cluster of differentiation (CD) 8A, ICAM1. Gene down-regulated at 11thPID in the moribund macaque was FAS-LG. Overall; the immune response pattern was balanced with marginal skewing towards pro-inflammatory and Th1 response.
Discussion
KFD is an important emerging infection in India, as evident by the spread of the disease to newer geographic areas, particularly during the last decade2. Experimental infection studies in animals have been conducted in the past using prototype old isolate maintained by serial passaging in suckling mouse brain11,12,14–16. Arboviruses are maintained in nature via alternate cycles of replication in host and vector. Serial passaging in single host may lead to adaptation owing to increase in mutation rates, a phenomenon commonly observed in arboviruses18. Using such a virus in animal models may not represent true disease profile in natural settings16. Besides that, change in genetic makeup of contemporary virus over a period of time may lead to differential disease outcome compared to the isolates obtained during 1960s19. A recent study on the phylogeography of the KFDV also has shown only 0.86 percent amino acid divergence between KFD recent and older isolates20. We have studied experimental infection in bonnet macaques with contemporary, minimally passaged strain so as to mimic the scenario observed in nature. Unlike 100% mortality observed in previous macaque studies11,12, we observed severe disease in 2/10 macaques. However, the similar low passage strain of KFDV used in an earlier study produced neuropathology in CD1 mice21. The dose of infection in the present study has also not shown any effect on mortality. Level and duration of viremia in macaques was found to be comparable with the previous studies11,12. In spite of considerable and prolonged viremia, disease in 2/10 macaques indicates that apart from virus strain, host cofactors could play important role in disease outcome. Indeed, the host factors leading to the alteration in immune response are known to affect disease outcome in KFD patients22.
Our study revealed that infected macaques can be asymptomatic and shed the virus in stool, urine, oral and conjunctival secretions during the viremic phase. The transmission of the virus in nature from macaque to macaque via bites, open wounds, or direct contact with contaminated fomites could be possible. Moreover, this could act as source of virus to small mammals via contaminated fomites. A decade long study conducted on monkey mortality in KFD endemic area revealed that, out of 1,046 deaths, 860 were P. entellus and only 186 were M. radiata with virus isolation percentage of 50% and 18.05% in necropsied animals respectively17. The findings suggest that bonnet macaques are either not highly susceptible to virus or many macaques could be sub clinically infected. We observed that all infected macaques developed considerable viremia and robust humoral immune response indicating that the latter may be true. In our re-infection study, viremia or virus shedding was not observed, indicating that protective humoral immune response was generated which could counter high dose of virus during re-infection. This is in agreement with the earlier report stating that many macaques in wild survive the unapparent infections due to presence of neutralising antibodies23. In agreement with other macaque studies, fever was not consistently observed in infected animals. Few animals (3/10) exhibited rise in body temperature transiently. Only one animal in which severe disease was observed showed consistent fever. Haemorrhage is not consistent feature of KFD. GIT haemorrhages were observed in patients only with severe disease22. Indeed we could observe frank GIT haemorrhages in macaque with severe disease. None of the animals developed biphasic fever or neurological sequelae although viral RNA could be detected in brains of two macaques with severe disease.
KFD viral RNA in blood could be detected from 1st–13th PID in macaques inoculated with high dose with peak at 4th PID. In macaques inoculated with low dose, detection and peak was delayed by 2 days. Importantly, the peak RNA levels in a macaque with fatal disease was significantly higher than other animals indicating that level of viremia could be a marker of severe disease. Overall pattern of viremia was very similar to that observed in patients and other macaque studies11,12,24. Of note, the detection of viral RNA in faeces/rectal swab coincided with the peak of viremia and continued until the end of viremia. Detection in urine samples was invariably delayed by at least two days. This probably reflects on the primary replication site for the virus. GIT has been shown to be affected in rodent and macaque models11,14. In the macaque sacrificed on 3rd PID, viral RNA could be detected in GIT but not in kidneys or urinary bladder. The experimental studies on faecal detection of Zika virus RNA in neotropical primates is considered a significant advancement for surveillance of Zika in wild reservoir monkeys25. The faecal detection of KFDV RNA could turn out to be a cost effective, non invasive and reliable method to monitor wild monkeys during sentinel surveillance. Viral RNA was also detected in conjunctival swabs and pharyngeal swabs collected on 10th PID. Ocular manifestation in KFD in patients is very common26. Virus shedding in different secretions / excretions has not been studied in patients so far. Such a study would be useful in identifying non invasive specimens to be used in diagnosis / follow up with patients 2.
Kinetics of viral RNA in different organs of macaques was studied throughout the course of disease. Viral RNA could be detected in liver, spleen, GIT, ovary and skin of the macaque sacrificed on 3rd PID and dissemination to other visceral organs was observed in the macaque sacrificed on 6th PID. The findings are in agreement with earlier macaque study in which GIT, organs of lymphoreticular system and liver were found as primary replication sites for the virus11. Earlier rodent model study also reported spleen and GI tract beside brain as the replication site for the virus14. Viral RNA in liver, heart, lungs, bladder, ovary, skin could be detected in macaques sacrificed from 6th PID until 20th PID. Thereafter it could be detected in liver, spleen, GIT and lymph nodes in the macaques sacrificed on 40th and 53rd PID and exclusively in lymph node, in the macaque sacrificed on 81st PID. Further studies are needed to ascertain replication competency of the persistant viral RNA in GIT and lymph nodes. Persistence of replication competent virus in lymph nodes have been observed in macaques experimentally infected with Zika virus27. Only two monkeys which reached the moribund state showed positivity in brain samples suggesting KFDV may affect central nervous system (CNS) at a later stage of infection (11th to 14th PID). Our observations are in unison with earlier studies which reported encephalitis not evident before 12th PID13,28.
Humoral immune response against KFDV in animal model has not been studied so far owing to the acute nature of disease in rodents and macaque models11,14,16. We could study the antibody kinetics over a period of 80 PID. Until 40 PID, at least three animals could be sampled per time point, after that there were only two animals on day 53 and one on day 80. Positive titres of IgM ( P/N > 2) could be detected from the end of first week post infection until 5 weeks post infection, with peak titres coinciding with end of viremia (12 PID). IgG could be detected from 3rd week onwards with peak titres by 6 weeks post infection. Positive titres of IgG could be detected throughout the observation period. The peak IgM was observed on 12th PID (end of viremia) suggesting that IgM efficiently neutralised free virus even before the detectable IgG appeared in the blood. Considerable overlap of at least 6 days was observed in viremia and IgM. Webb and Chatterjea, 1962 has shown antibodies on 65th PID in M. radiata inoculated with KFDV but other time points data was unavailable till date28.
Alterations in hematological parameters were observed in percent monocytes, thrombocytes, total leukocytes and erythrocytes. We observed increase in monocytes with concomitant decrease in thrombocytes and total leukocytes during viremic phase. Increase in absolute number of monocytes within first 5 days after infection was observed in macaques infected with Zika virus29. Transient lymphopenia as observed in our study is commonly observed in viral infections and has been shown to be associated with an early Type I interferon response26. Our finding of increased monocytes with concomitant decrease in erythrocytes is in agreement with elevated myeloid/erythroid ratios observed in KFDV infected macaques by an earlier study11. Marked thrombocytopenia and anaemia, possibly due to erythrophagocytosis were observed earlier in KFD13. A significant decrease was observed in the total protein, globulin and albumin levels points to altered liver function which is supported by an increase in AST and bilirubin levels. But no histopathological lesions were observed in liver. Anorexia or lesions in the GIT (although minimal) contributed by the viral replication might have resulted in protein malabsorption which could also result in decreased serum proteins. High AST level in KFD affected monkeys was earlier demonstrated11.
The IgM antibody rise corresponded to the IL-6 secretion in splenocytes. IL-6 is a multifunctional cytokine with a wide range of functions important in inflammation and immune response30. However, the relation cannot be confirmed due to the limited sample size. In contrast, the IL-6 secretion was minimal in BM12 sacrificed on 12th PID. BM12 also had not shown the presence of KFDV RNA in any organs except spleen, stomach and intestines. Gene expression analysis showed only a marginal fold change in few pro-inflammatory and Th1 genes in comparison to the control monkey. There was a limitation of sample size at different time points.
We have attempted to recapitulate KFD in the macaque model using high and low doses of minimum laboratory passaged, the contemporary strain of virus by closer to natural route (s/c) of inoculation mimicking the tick bite. Majority of the macaques showed minimal clinical signs and the mortality was comparable to humans. Neuro-invasion was observed only in the case of moribund animals without the evidence of encephalitis. Infected macaques were found to shed the virus in stool, urine, oral and conjunctival secretions during viremic phase. Importantly, virus could be isolated from skin during period of viremia. Viral load study in different organs suggested that lymphoid organs and GIT could be the major replication/persistence sites. Viremia, virus shedding in different secretions/ excretions, antibody response, viral RNA load observed in experimentally infected macaques could be used as markers in evaluation of future NHP models.
Materials and methods
Ethics statement
The study (Project no. MCL-1503) was recommended by the Institutional Animal Ethics Committee, Indian Council of Medical Research (ICMR)-National Institute of Virology (NIV), Pune and was approved by the Committee for the purpose of Control and Supervision of Experiments on Animals (CPCSEA), letter F No. 25/28/2016-CPCSEA dated 02.12.16. The permission from forest authorities for trapping of required number of bonnet macaques from the wild was also obtained. The research was conducted in compliance with the guidelines laid down by CPCSEA, Government of India.
Virus
KFDV (NIV-12839) isolated from acute phase human serum sample from Thirthahalli, Karnataka propagated in Baby hamster kidney (BHK) -21 cells (Passage number 6) having a tissue culture infective dose 50 (TCID50) titer of 105.57/ml was used for the study21. 6–8 weeks old, female, BALB/c mice procured from Animal House facility of ICMR-NIV, Pune was used to assess the virus lethal dose 50 (LD50). The animals were housed in individually ventilated cages in the Animal Biosafety level-3 (ABSL-3) facility. Ten-fold serial dilutions of virus stock in minimum essential medium (MEM) (Life Technologies Corporation, USA) was prepared. Six mice were used per dilution and the mice were inoculated by s/c route at a dose of 100 micro L (µl)/mouse. Mice were monitored for 21 days for mortality, and LD50 value was calculated by Reed and Muench method31. The mouse LD50 titre of the KFD virus following subcutaneous inoculation in 6–8 week old BALB/c mice was found to be 105.5/ml.
Bonnet macaques
Eleven, female, adult bonnet macaques weighing 4 to 5.5 kg were caught from the Pune Forest Division of Maharashtra State, India and were kept under quarantine at the animal house facility at the ICMR-NIV, Pune for two months. During the quarantine, veterinary clinical examination, haematology, serum biochemistry, stool examination for parasites and pathogenic bacteria, chest X-ray, tuberculin tests and anti-KFD monkey IgG ELISA were performed to judge if the monkeys were fit for the experiment. After the successful quarantine, the monkeys were shifted to ABSL-3 facility and kept for an acclimatization period for one week. Animals were housed in individual stainless steel cages, fed twice daily with commercial feed pellets, vegetables, fruits, nuts and were given ad libitum access to drinking water. The humane end point for the experiment was decided based on the available literature32, and the monkeys were euthanized by intravenous administration of thiopentone sodium under deep sedation with ketamine hydrochloride33. The humane end points were determined based on their general behaviour, skin condition, body weight, excessive nasal/ocular discharge, diarrhea, vomiting, urination, and body temperature.
Occult blood test
The occult blood test was performed for stool using a commercially available test kit (Hemospot kit, Coral Clinical systems).
Haematology and serum biochemistry
Coagulation parameters were measured every third PID. Clotting time (CT) was assessed using the capillary method. Blood collected in 4% sodium citrate solution was used for testing PT and aPTT using the commercially available human kit (Tulip Diagnostics (P) Ltd).The samples collected on every third day post inoculation were outsourced to a commercial National Accreditation Board for Testing and Calibration Laboratories accredited private laboratory of Pune. Haemoglobin (Hb), total leucocyte count (TLC), differential leucocyte count (DLC), platelet count, packed cell volume (PCV), mean corpuscular volume (MCV), mean corpuscular haemoglobin (MCH), mean corpuscular haemoglobin concentration (MCHC) and red blood cell count were tested. Bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (AP), total protein, albumin, globulin, urea and creatinine were assessed.
Measurement of anti-KFDV antibody response by in-house ELISA
Indigenous serological tests for detecting anti-KFDV IgM and IgG antibodies from monkey sera were developed. The intra-assay and inter-assay variation were determined. The cut-off value was determined by screening normal monkey sera and the sample was considered positive if the Optical Density (OD) value is > 0.2 and the Positive/Negative (P/N) ratio > 1.5 for both the assays.
Anti-KFD monkey IgM detection ELISA
ELISA plates were coated with anti-monkey IgM antibodies (1:100, Sigma SAB 3700778) in carbonate buffer (pH 9.2, 0.025 M) overnight at 4 °C. The wells were blocked with 2% bovine serum albumin (BSA) for 2 h at room temperature. One hundred µl of a diluted sample (1:100 in 1% BSA in 1 × phosphate-buffered saline (PBS) containing 0.1% Tween20) was added to duplicate wells and incubated at 37 °C for one hour. One hundred µl of inactivated KFDV antigen (strain number: 12839) was used as positive antigen; normal BHK-21 cell lysate was used as negative antigen, which were added to the wells and the plates were incubated for one hour at 37 °C. Anti-KFDV biotinylated antibodies (100 µl, 1:2000) were added and incubated for one hour. Streptavidine Horseradish peroxidase (HRP) (100 µl; 1:8,000) was added and incubated for 30 min at 37 °C. Each incubation was followed by 4 washes with wash buffer (1 × PBS containing 0.1% Tween). One hundred µl of 3, 3′,5,5′-Tetramethylbenzidine (TMB) substrate was added and incubated for 10 min. The reaction was stopped by 1 N Sulphuric acid (H2SO4), and the absorbance was measured at 450 nm (nm).
Anti-KFD monkey IgG detection ELISA
ELISA plates were coated with inactivated KFDV antigen (1:10) in carbonate buffer (pH 9.2, 0.025 M) overnight at 4 °C. One hundred µl of 1:100 diluted serum samples were added and incubated for 1 h at 37 °C. Anti-monkey IgG HRP conjugate (1:4,000, 100 µl) was added and incubated for one hour at 370C. The plate was washed four times with wash buffer, after the completion of each incubation period. One hundred µl of TMB substrate was added and incubated for 10 min. The reaction was stopped by 1 N H2SO4, and absorbance was measured at 450 nm.
Measurement of KFDV RNA load by real-time quantitative reverse transcription PCR (qRT-PCR)
Fresh stool/rectal swabs and urine were collected daily. Conjunctival and oro-pharyngeal swabs were collected under sedation. CSF was collected from all macaques by cisterna magna puncture under deep anaesthesia just before sacrifice. All the visceral organs, brain, and skin were collected during necropsy in RNAlater (Sigma), MEM and 10% neutral buffered formalin for further studies.
Viral RNA load was determined in serum, urine, stool/ rectal swabs, oro-pharyngeal swabs, conjunctival swabs, bile, CSF and in organs like skin, heart, lungs, liver, gall bladder, spleen, kidney, urinary bladder, pancreas, stomach, small intestine, large intestine, lymph nodes, ovary, cerebellum, cerebrum, olfactory bulb, hippocampus and medulla oblongata. A 10% homogenate of uniformly weighed tissues in 1 ml of MEM was used for RNA extraction using Magmax RNA extraction kit (Thermo Fisher Scientific, USA) according to manufacturer’s instructions. KFDV qRT-PCR was performed using published primers and probes34.
Virus isolation from skin
Skin samples (below the nape of neck) were collected during necropsy. Infant CD1 mice (1 day old) were inoculated intra-cerebrally with 20 µl of filtered monkey skin suspension prepared in MEM. Mice were observed daily and reduced mobility, hunched posture, paralysis and laboured breathing were considered humane end-points. Mice brains were harvested in aseptic conditions on observation of sickness on 7th PID. 10% of mouse brain suspension was made in 1.25 molar PBS with 10% bovine albumin and tested for the presence of KFDV RNA by qRT-PCR.
Histopathology
Representative tissue samples of heart, lungs, liver, spleen, kidneys, stomach, small and large intestine, pancreas, lymph nodes, urinary bladder, brain and skin were immersion-fixed in 10% neutral buffered formalin. Tissues were processed by routine histopathology technique, embedded in paraffin, and sections of 4 µm (μm) thickness were cut for subsequent haematoxylin and eosin staining35.
Immunohistochemistry
Formalin fixed tissue sections taken on adhesive coated slides were re-hydrated, and antigen retrieval was performed in 0.3% hydrogen peroxide solution in methanol. Further, the sections were blocked with blocking buffer for one hr at 37 °C. The sections were exposed to primary antibody (1:400 dilutions of polyclonal sera against KFDV raised in mice) for one hour at 37 °C followed by HRP labelled secondary antibody. Immuno-reactivity was detected using 3, 3′-diaminobenzidine tetrahydrochloride substrate, and hydrogen peroxide. Sections were counterstained with Haematoxylin stain.
Cytokine analysis by cytometric bead array
Cytokine analysis was performed as described previously36. Briefly, one million freshly harvested splenocytes from sacrificed monkeys were stimulated with 105mouse LD50 live KFDV. The stimulated cells were incubated at 37 °C for 72 h, centrifuged and the supernatant containing secreted cytokines was further used. Six cytokines, namely IL -2, IL-4, IL-5, IL-6, TNF and IFN-γ were measured using cytometric bead array non-human primate Th1/Th2 kit (BD Biosciences San Jose, CA, USA).
Gene expression analysis by Taqman low density array (TLDA)
Taqman based analysis was performed on spleen tissues as previously described37. RNA was extracted using the Qiagen total RNA extraction kit (Qiagen, Hilden, Germany) and was quantified using the Qubit RNA HS assay kit (Thermo Fisher Scientific, Carlsbad, California, USA) according to manufacturer’s instructions. The quality and integrity of total RNA were confirmed by checking the presence of 18S (ribosomal) rRNA and 28S rRNA bands on an agarose gel. One microgram total RNA was used for complementary deoxy ribonucleic acid (cDNA) synthesis using High-Capacity cDNA Reverse Transcription Kit (Thermo Fischer Scientific). The quality of cDNA was confirmed using real time PCR set up with eukaryotic 18S rRNA endogenous control (Thermo Fisher Scientific, Carlsbad, California, USA). TLDA plate (Applied Biosystems, UK) of the immune panel with 10 ng of cDNA per reaction was run on the 7,300 Real-time PCR system (Applied Biosystems, UK). Hypoxanthine phosphoribosyl transferase (Hprt)1 gene (housekeeping gene) was used as endogenous control. Relative gene expression values were calculated with the comparative cycle threshold (Ct) method using Applied Biosystems relative quantification (RQ) manager software v1.2.cDNA from the control monkey (BM7) was considered as the calibrator. A fold change greater or less than 2.5 was considered valid in the experiment.
Statistical analysis
Descriptive statistics were calculated for quantitative variables, mean, and standard deviation. For qualitative variables, percentages were calculated. Paired T-tests was used to compare data between various time-points. Statistical significance was considered at 5% level of significance (p value < 0.05).
Supplementary information
Acknowledgement
Authors acknowledge the support and co-ordination from Principal Chief Conservator of Forests (Wildlife) and Chief Wildlife Warden, Maharashtra state and Chief Conservator of Forests (Wildlife/Territorial), Pune Forest Division for giving permission to capture the macaques for the experimentation. Authors also acknowledge support from Dr.Jayati Mullick (Scientist E and Head, BSL3) for providing the facility, Mr. AB Khare (Engineer and the In-charge, Maintenance department) for his guidance and Mr. Dinesh Singh (Poliovirus Group) and Mr. Babu (Poliovirus Group) for the support during the experiment. Authors also express the gratitude towards the technical team who supported the animal experimentation which include Mr.Sanjay Gopale, Mr. Ankkaiya and the laboratory team which includes Mrs.Sheetal Melag, Mrs.Yogita Chopade, Mr. Anish Srivastava, Mr. Vinod Soman, and Mr. Swapnil Patil for their contribution. We also thank Prof. Sanjeev Galande, Head, Laboratory of Chromatin Biology and Epigenetics, IISER for allowing using the FACS facility.
Author contributions
D.T.M., D.R.P. and P.D.Y. conceived, designed, planned and supervised the whole experiment. D.R.P., S.M., R.R.S. and S.K. performed the planning, animal experimentation and necropsy. P.D.Y, A.S, G.C. and R.J. performed the planning of laboratory work, analysis and interpretation of data. P.D.Y, A.S and R.J. developed the in-house ELISA. C.M., H.K., R.J., G.C., P.P., S.P., T.M., P.S. and R.L. performed sample processing in the laboratory and further tests. P.K., S.F., A.S. and M.K. assisted in animal experimentation, sample collection and necropsy. D.R.P., G.C., S.M. and P.P. have drafted the manuscript. D.T.M., P.D.Y., D.R.P., A.S. and R.R.S. substantively revised it. All authors reviewed the manuscript and agree to its contents.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article or its supplementary materials.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dilip R. Patil, Pragya D. Yadav: These authors contributed equally to this work.
Anita Shete, Gouri Chaubal, Sreelekshmy Mohandas, Rima R. Sahay, Rajlaxmi Jain, Chandrashekhar Mote, Sandeep Kumar: These authors also contributed equally to this work.
Himanshu Kaushal, Pravin Kore, Savita Patil, Triparna Majumdar, Siddharam Fulari, Annasaheb Suryawanshi, Manoj Kadam, Prachi G. Pardeshi, Rajen Lakra, Prasad Sarkale: These authors also contributed equally to this work.
Supplementary information
is available for this paper at 10.1038/s41598-020-67599-x.
References
- 1.Work TH, Trapido H. Kyasanur forest disease a new virus disease in India: Summary of the preliminary report of investigations of the Virus Research Centre on an epidemic disease affecting forest villagers and wild monkeys of Shimoga district, Mysore. Indian J Med Sci. 1957;11:1–2. [PubMed] [Google Scholar]
- 2.Mourya DT, Yadav PD. The recent scenario of the emergence of Kyasanur forest disease in India and public health importance. Curr. Trop. Med. Rep. 2016;3:7–13. [Google Scholar]
- 3.Work TH, Roderiguez FM, Bhatt PN. Virological epidemiology of the 1958 epidemic of Kyasanur Forest disease. Am. J. Public Health Nations Health. 1959;49:869–874. doi: 10.2105/ajph.49.7.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jorge Boshell, M., Rajagopalan, P.K., Goverdhan, M.K. & Pavri, K.M. The isolation of Kyasanur forest disease virus from small mammals of the SagaSorab forests, Mysore state, India. Indian J. Med. Res.56(4), 569–72 (1968). [PubMed]
- 5.Rajagopalan PK, Paul SD, Sreenivasan MA. Involvement of Rattus blanfordi (rodentia: muridae) in the natural cycle of Kyasanur forest disease virus. Indian J Med. Res. 1969;57(6):999–1002. [PubMed] [Google Scholar]
- 6.Singh KRP, Pavri KM, Anderson CR. Transmission of Kyasanur forest disease virus by Haemaphysalis turturis, Haemaphysalis papuanakinneari and Haemaphysalis minuta. Indian J Med Res. 1964;52(6):566–573. [PubMed] [Google Scholar]
- 7.Work, T.H. et al. Kyasanur forest disease. III: A preliminary report on the Nature of the infection and clinical manifestations in human beings. Indian J. Med. Sci. 11(8), 619–645 (1957). [PubMed]
- 8.Iyer, C.G.S., Rao, R.L., Work, T.H. & Murthy, D.P.N. Kyasanur forest disease. Part VI: Findings in three fatal human cases of Kyasanur forest disease. Indian J. Med. Sci. 13(12), 1011–1022 (1959). [PubMed]
- 9.Holbrook MR. Kyasanur forest disease. Antiviral Res. 2012;96(3):353–362. doi: 10.1016/j.antiviral.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Trapido H, Work TH. Non-human vertebrates as hosts and disseminators of Kyasanur forest disease. Proc. 9th Pac. Sci. Cong. 1962;17:85–71. [Google Scholar]
- 11.Kenyon RH, Rippy MK, McKee KT, Jr, Zack PM, Peters CJ. Infection of Macaca radiata with viruses of the tick-borne encephalitis group. Microb. Pathog. 1992;13(5):399–409. doi: 10.1016/0882-4010(92)90083-z. [DOI] [PubMed] [Google Scholar]
- 12.Shah KV, Dandawate CN, Bhatt PN. Kyasanur forest disease virus: viremia and challenge studies in monkeys with evidence of cross-protection by Langat virus infection. F1000Research. 2012;1:61. doi: 10.12688/f1000research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Webb HE, Burston J. Clinical and pathological observations with special reference to the nervous system in Macaca radiata infected with Kyasanur forest disease virus. Trans. R. Soc. Trop. Med. Hyg. 1966;60(3):325–331. doi: 10.1016/0035-9203(66)90296-3. [DOI] [PubMed] [Google Scholar]
- 14.Dodd KA, Bird BH, Jones ME, Nichol ST, Spiropoulou CF. Kyasanur Forest disease virus infection in mice is associated with higher morbidity and mortality than infection with the closely related Alkhurma hemorrhagic fever virus. PLoS ONE. 2014;9:e100301. doi: 10.1371/journal.pone.0100301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nayar M. Kyasanur forest disease virus encephalitis in mice. Effect of cortisone on the encephalitic lesions. Indian J. Med. Res. 1972;60:1427–1431. [PubMed] [Google Scholar]
- 16.Sawatsky B, McAuley AJ, Holbrook MR, Bente DA. Comparative pathogenesis of Alkhumrahemorrhagic fever and Kyasanur forest disease viruses in a mouse model. PLoS Negl. Trop. Dis. 2014;8:e2934. doi: 10.1371/journal.pntd.0002934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sreenivasan, M.A., Bhat, H.R. & Rajagopalan, P, K. The epizootics of Kyasanur forest disease in wild monkeys during 1964 to 1973. Trans. R. Soc. Trop. Med. Hyg.80(5), 810–814 (1986). [DOI] [PubMed]
- 18.Ciota AT, Kramer LD. Insights into arbovirus evolution and adaptation from experimental studies. Viruses. 2010;2:2594–2617. doi: 10.3390/v2122594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kasabi GS, Murhekar MV, Yadav PD, Raghunandan R, Kiran SK, Sandhya VK, et al. Kyasanur forest disease, India, 2011–2012. Emerg. Infect. Dis. 2013;19:278–281. doi: 10.3201/eid1902.120544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yadav PD, et al. Phylogeography of Kyasanur forest disease virus in India (1957–2017) reveals evolution and spread in the Western Ghats region. Sci. Rep. 2020;10(1):1–12. doi: 10.1038/s41598-020-58242-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Basu A, et al. An early passage human isolate of Kyasanur forest disease virus shows acute neuropathology in experimentally infected CD-1 mice. Vector Borne Zoonotic Dis. 2016;16(7):496–498. doi: 10.1089/vbz.2015.1917. [DOI] [PubMed] [Google Scholar]
- 22.Pawri K. Clinical, clinicopathologic, and hematologic features of Kyasanur forest disease. Rev. Infect. Dis. 1989;2(4):854–S859. doi: 10.1093/clinids/11.supplement_4.s854. [DOI] [PubMed] [Google Scholar]
- 23.Work TH. Virological aspects of Kyasanur forest disease. J. Indian Med. Assoc. 1958;31(3):111–113. [PubMed] [Google Scholar]
- 24.Upadhyaya S, Narasimha M, Yashodhara M. Viremia studies of Kyasanur forest disease human cases of 1966. Indian J. Med. Res. 1975;63(7):950–953. [PubMed] [Google Scholar]
- 25.Milich KM, et al. Methods for detecting Zika virus in feces: A case study in captive squirrel monkeys (Saimiri boliviensis boliviensis) PLoS ONE. 2018;13(12):e0209391. doi: 10.1371/journal.pone.0209391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shah SZ, et al. Epidemiology, pathogenesis, and control of a tick-borne disease-Kyasanur forest disease: Current status and future directions. Front. Cell Infect. Microbiol. 2018;8:149. doi: 10.3389/fcimb.2018.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hirsch AJ, et al. Zika virus infection of rhesus macaques leads to viral persistence in multiple tissues. PLoS Pathog. 2017;13:e1006219. doi: 10.1371/journal.ppat.1006219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Webb HE, Chatterjea JB. Clinico-pathological observations on monkeys infected with Kyasanur forest disease virus, with special reference to the haemopoietic system. Br. J. Haematol. 1962;8(4):401–413. doi: 10.1111/j.1365-2141.1962.tb06544.x. [DOI] [PubMed] [Google Scholar]
- 29.Osuna CE, Whitney JB. Nonhuman primate models of Zika virus infection, immunity, and therapeutic development. J. Infect. Dis. 2017;216(S10):S928–934. doi: 10.1093/infdis/jix540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tanaka T, Narazaki M, Kishimoto T. IL-6 in inflammation, immunity, and disease. Cold Spring Harb. Perspect. Biol. 2014;6(10):a016295. doi: 10.1101/cshperspect.a016295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reed LJ, Muench H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938;27(3):493–497. [Google Scholar]
- 32.IACUC Guidelines. https://safetyservices.ucdavis.edu.
- 33.Thurmon, J.C., Tranquilli, W.J., Benson, G.J. & Lumb, W.V. Anesthesia of wild, exotic, and laboratory animals. In Lumb and Jones Veterinary Anesthesia and Analgesia (eds. Thurmon, J.C., Tranquilli, W.J., Benson, G.J.) 727 (Lippincott Williams and Wilkins, 1996).
- 34.Mourya DT, et al. Diagnosis of Kyasanur forest disease by nested RT-PCR, real-time RT-PCR and IgM capture ELISA. J. Virol. Methods. 2012;186(1–2):49–54. doi: 10.1016/j.jviromet.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 35.Culling, C.F.A. Handbook of Histopathological and Histochemical Techniques: Including Museum Techniques (Butterworth-Heinemann, 2013).
- 36.Saravanabalaji S, et al. Viral load, antibody titers, and recombinant open reading frame 2 protein-induced TH1/TH2 cytokines and cellular immune responses in self-limiting and fulminant Hepatitis E. Intervirology. 2009;52(2):78–85. doi: 10.1159/000214862. [DOI] [PubMed] [Google Scholar]
- 37.Arankalle VA, et al. Role of host immune response and viral load in the differential outcome of pandemic H1N1 (2009) influenza virus infection in Indian patients. PLoS ONE. 2010;5(10):e13099. doi: 10.1371/journal.pone.0013099. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article or its supplementary materials.