Abstract
Background
Cholecystectomy is one of the most frequently performed operations. Open cholecystectomy has been the gold standard for over 100 years. Small‐incision cholecystectomy is a less frequently used alternative.
Objectives
To compare the beneficial and harmful effects of small‐incision versus open cholecystectomy for patients with symptomatic cholecystolithiasis.
Search methods
We searched The Cochrane Hepato‐Biliary Group Controlled Trials Register (6 April 2004), The Cochrane Library (Issue 1, 2004), MEDLINE (1966 to January 2004), EMBASE (1980 to January 2004), Web of Science (1988 to January 2004), and CINAHL (1982 to January 2004) for randomised trials.
Selection criteria
All published and unpublished randomised trials in patients with symptomatic cholecystolithiasis comparing any kind of small‐incision or other kind of minimal incision cholecystectomy versus any kind of open cholecystectomy. No language limitations were applied.
Data collection and analysis
Two authors independently performed selection of trials and data extraction. The methodological quality of the generation of the allocation sequence, allocation concealment, blinding, and follow‐up was evaluated to assess bias risk. Analyses were based on the intention‐to‐treat principle. Authors were requested additional information in case of missing data. Sensitivity and subgroup analyses were performed if appropriate.
Main results
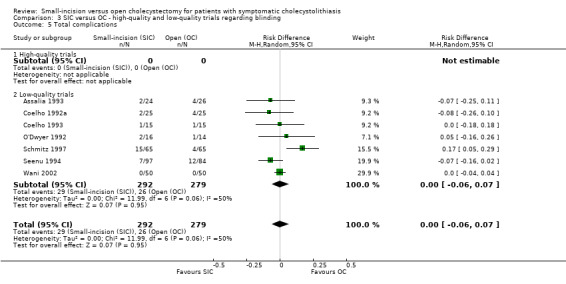
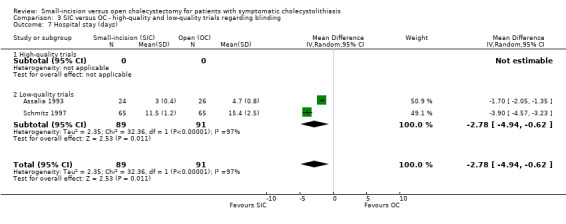
Seven trials randomised 571 patients. Bias risk was high in the included trials. No mortality was reported. The total complication proportions are respectively 9.9% and 9.3% in the small‐incision and open group, which is not significantly different (risk difference all trials, random‐effects 0.00, 95% confidence interval (CI) ‐0.06 to 0.07). There are also no significant differences considering severe complications and bile duct injuries. However, small‐incision cholecystectomy has a shorter hospital stay (weighted mean difference, random‐effects ‐2.8 days (95% CI ‐4.9 to ‐0.6)) compared to open cholecystectomy.
Authors' conclusions
Small‐incision and open cholecystectomy seem to be equivalent regarding risks of complications, but the latter method is associated with a significantly longer hospital stay. The quicker recovery of small‐incision cholecystectomy compared with open cholecystectomy confirms the existing preference of this technique over open cholecystectomy.
Plain language summary
Small‐incision cholecystectomy and open cholecystectomy seem equivalent considering complications, but small‐incision cholecystectomy is associated with a shorter hospital stay
The classical open cholecystectomy and the minimally invasive small‐incision cholecystectomy are two alternative operations for removal of the gallbladder. There seem to be no significant differences in mortality and complications between these two techniques. Hospital stay is shorter using the small‐incision operation. This review shows that the small‐incision and open cholecystectomy should be considered equal, apart from a shorter hospital stay using the small‐incision technique.
Background
Gallstones are one of the major causes of morbidity in western society. It is estimated that the incidence of symptomatic cholecystolithiasis is up to 2.17 per thousand inhabitants (Legorreta 1993; Steiner 1994) with an annual performance rate of cholecystectomies of more than 500,000 in the USA (Olsen 1991; NIH Consensus 1993; Roslyn 1993). Until the end of the 1980s, open cholecystectomy was the gold standard for treatment of stones in the gallbladder. As incisions for cholecystectomy were shortened resulting in 'small‐incision' cholecystectomy, morbidity and complications seemed to decline and patients recovered faster. In the early 1970s small‐incision cholecystectomy was introduced as a minimally invasive procedure (Dubois 1982; Goco 1983), and has been compared in trials with open cholecystectomy. Conflicting data on clinical outcome and effectiveness arose from these randomised trials.
Laparoscopic cholecystectomy was introduced in 1985 (Mühe 1986) and rapidly became the method of choice for surgical removal of the gallbladder (NIH Consensus 1993) although the evidence of superiority over small‐incision and open cholecystectomy was absent. After this consensus, attention was focused on laparoscopic cholecystectomy and the primary question of the comparison of the small‐incision cholecystectomy to the classical open cholecystectomy was never answered.
Differences in primary outcomes like mortality and complication proportions (particularly bile duct injuries) are important reasons to choose one of the operative techniques. When these primary outcomes show no significant difference, then secondary outcomes like non‐severe complications, pulmonary outcomes, differences in health status related quality‐of‐life, hospital stay, and differences in cost‐effectiveness analysis should help decide which technique is superior.
Up to now, despite the availability of numerous randomised trials on this topic, no systematic review or meta‐analysis of randomised trials has been conducted comparing small‐incision and open cholecystectomy. This lack of evidence was the main reason for writing this systematic review. The objective was to evaluate the assumed superiority of the small‐incision cholecystectomy.
Objectives
To evaluate the beneficial and harmful effects of two different types of cholecystectomy for patients with symptomatic cholecystolithiasis. To assess whether small‐incision and open cholecystectomy are different in terms of primary (mortality, complications, and relief of symptoms) and secondary outcomes (conversions to open cholecystectomy, operative time, hospital stay, and convalescence). If data were present, differences in other secondary outcomes like analgesic use, postoperative pain, pulmonary function, and costs were compared as well.
Methods
Criteria for considering studies for this review
Types of studies
All randomised clinical trials comparing small‐incision or other kinds of minimal‐incision open cholecystectomy to any kind of classical open cholecystectomy. Trials were included irrespectively of blinding, number of patients randomised, and language of the article. Quasi‐randomised studies were excluded.
Types of participants
Patients with one or more stones in the gallbladder confirmed by ultrasonography or other imaging technique and symptoms attributable to them, scheduled for cholecystectomy. Acute cholecystitis is a disease with different operative results including the number of complications and conversions. Cholecystectomy in patients suffering from acute cholecystitis should be distinguished from cholecystectomy in patients suffering from symptomatic cholecystolithiasis. Therefore, randomised trials only including patients with acute cholecystitis were excluded from this review. Randomised trials including both symptomatic cholecystolithiasis and acute cholecystitis were included in the review only if the large majority (more than half) of the included patients were operated on because of symptomatic cholecystolithiasis.
Types of interventions
Any kind of small‐incision cholecystectomy was assessed versus any kind of open cholecystectomy.
The following classifications of the surgical procedures (based on intention‐to‐treat) were used: Only if the words 'small‐incision', 'minimal access', 'minilaparotomy', or similar as intended terms were mentioned in the primary classification of the procedure, the surgical intervention was classified as a 'small‐incision' cholecystectomy (ie, length of incision of less than 8 cm). The length of incision up to 8 cm was chosen arbitrary as in literature most authors used this as a cut‐off point between small‐incision and (conversion to) open cholecystectomy.
In all other cases the surgical intervention was classified as 'open cholecystectomy'; this traditional procedure can be carried out through a larger subcostal or transverse incision or a median laparotomy.
Types of outcome measures
The primary outcome measures are mortality, complication proportions (intra‐operative, severe, bile duct injuries, and total complications; except minor complications), and relief of symptoms (pain relief). Although relief of symptoms is the aim of cholecystectomy, some patients continue to suffer from their complaints and have persistent pain. Most important in obtaining a high proportion of patients with relief of symptoms is adequate decision making in setting the indication to operate or not. However, it cannot be ruled out that some of this persistent pain should be attributed to the way of incision for cholecystectomy. Therefore it is of interest to include pain relief as a primary outcome.
Secondary outcome measures are all other outcomes assessed in comparing the two operative techniques. We assessed the following secondary outcomes: operative time, hospital stay, convalescence, analgesic use, postoperative pain (visual analogue scale), pulmonary outcome (pulmonary function tests by flow‐volume curves), and cost‐effectiveness if data were available.
Search methods for identification of studies
We searched the following databases: The Cochrane Hepato‐Biliary Group Controlled Trials Register (6 April 2004), the Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects (DARE), the Cochrane Central Register of Controlled Trials (CENTRAL), Health Technology Assessment (HTA) Database, NHS Economic Evaluation Database, all in The Cochrane Library (Issue 1, 2004), The National Library of Medicine (MEDLINE) (1966 to January 2004), The Intelligent Gateway to Biomedical & Pharmacological Information (EMBASE) (1980 to January 2004), ISI Web of Knowledge (Web of Science) (1988 to January 2004), and CINAHL (1982 to January 2004). The search strategies used are provided in Appendix 1.
Our aim was to perform a maximal sensitive search in order to conduct a more complete review. As describing an operation of the gallbladder in medical terms without the word cholecystectomy is impossible, a maximal sensitive search with the term cholecystectomy was used. For our MEDLINE search, a more sophisticated strategy, advised by the Dutch Cochrane Centre and listed in Appendix 1 was used (with help from Geert van der Heijden, Julius Center, Utrecht).
Additional relevant trials were looked for by cross reference checking of identified randomised trials. Finally all authors of included trials were requested by letter for additional information on any published, unpublished, or ongoing trials.
Furthermore, during data extraction it turned out that in a large number of trials essential data and information on methods were missing. To improve the quality of the analysis, individual trialists were contacted and asked for missing data.
Data collection and analysis
The review was conducted according to the present protocol (Keus 2004) and the recommendations by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2005). All identified trials were listed in the 'Characteristics of included studies' table and an evaluation whether the trials fulfilled the inclusion criteria was made. Excluded trials and the reasons for exclusion were listed as well (table with 'Characteristics of excluded studies').
Assessment of methodological quality Inadequate methodological quality in randomised clinical trials carries the risk of overestimating intervention effects (Schulz 1995; Moher 1998; Kjaergard 2001). Methodological quality, study design, and reporting quality have been recognised as criteria which can restrict bias in the comparisons of interventions (Moher 1998; Kjaergard 2001). Therefore the methodological quality of the randomised clinical trials was assessed using the following components.
Generation of the allocation sequence
Adequate, if the allocation sequence was generated by a computer or random number table. Drawing of lots, tossing of a coin, shuffling of cards, or throwing dice was considered as adequate if a person who was not otherwise involved in the recruitment of participants performed the procedure.
Unclear, if the trial was described as randomised, but the method used for the allocation sequence generation was not described.
Inadequate, if a system involving dates, names, or admittance numbers were used for the allocation of patients. These studies are known as quasi‐randomised and were excluded from the present review.
Allocation concealment
Adequate, if the allocation of patients involved a central independent unit, on‐site locked computer, or sealed envelopes.
Unclear, if the trial was described as randomised, but the method used to conceal the allocation was not described.
Inadequate, if the allocation sequence was known to the investigators who assigned participants or if the study was quasi‐randomised.
Blinding
Adequate, if the trial was described (at least) as blind to participants or assessors and the method of blinding was described. We are well aware that it is very difficult to properly blind trials comparing surgical treatments.
Unclear, if the trial was described as (double) blind, but the method of blinding was not described.
Not performed, if the trial was not blinded.
Follow‐up
Adequate, if the numbers and reasons for dropouts and withdrawals in all intervention groups were described or if it was specified that there were no dropouts or withdrawals.
Unclear, if the report gave the impression that there had been no dropouts or withdrawals, but this was not specifically stated.
Inadequate, if the number or reasons for dropouts and withdrawals were not described.
Extraction of data Inclusion and exclusion criteria used in each trial.
The following data on the randomisation procedure have been extracted: 1. Number of randomised patients. 2. Number of patients not randomised and reasons for non‐randomisation. 3. Exclusion after randomisation. 4. Drop‐outs. 5. 'Intention‐to‐treat' analysis.
Also information on sample size, single‐ or multicentre study design, assessment of primary and secondary outcome measures, use of antibiotic prophylaxis, surgical experience, and intra‐operative cholangiography was registered (Table 1).
1. Randomised, excluded, and included in small‐incision vs open cholecystectomy.
| Trial | Randomised | Excluded | Included SIC | Included OC | Cholangiography | Antibiotics | Surgical expertise |
| Assalia 1993 | 50 | 0 | 24 | 26 | N | Y | S |
| Coelho 1992a | 50 | 0 | 25 | 25 | Y | U | U |
| Coelho 1993 | 45* | 0 | 15 | 15 | U | U | U |
| O'Dwyer 1992a | 30 | 0 | 16 | 14 | Y | U | R |
| Schmitz 1997a | 130 | 0 | 65 | 65 | U | U | U |
| Seenu 1994 | 181 | 0 | 97 | 84 | U | U | R |
| Wani 2002 | 100 | 0 | 50 | 50 | U | U | U |
| Total | 586 | 0 | 292 | 279 | |||
| * three‐arm trial, patients in the LC group not listed in this table. | N = no | Y = yes | U = unknown | S = one surgeon | R = also registrars |
General descriptive data (like sex, age, body mass index (BMI), and American Society of Anaesthesiology (ASA) classification) are supposed to be equally divided due to randomisation (Assmann 2000). These data are presented in Table 2 as far as available. Outcome data on mortality, complications, health‐related quality‐of‐life, pulmonary function, pain, duration of operation, hospital stay, and convalescence were extracted according to availability.
2. Description of background data (age, sex, BMI, and ASA).
| Trial | N | Age | Age | Sex (m/f) | Sex (m/f) | BMI | BMI | ASA (I‐II‐III‐IV) | ASA (I‐II‐III‐IV) |
| SIC vs OC | randomised | SIC | OC | SIC | OC | SIC | OC | SIC | OC |
| Assalia 1993 | 24 / 26 | 60.3 (12.1) | 59.2 (13.4) | 5 / 19 | 7 / 19 | ‐ | ‐ | ‐ | ‐ |
| Coelho 1992a | 25 / 25 | 46 ( ‐ ) | 45 ( ‐ ) | 2 / 23 | 4 / 21 | ‐ | ‐ | ‐ | ‐ |
| Coelho 1993 | 15 / 15 | 42.5 (25‐66) | 45.4 (18‐73) | 2 / 13 | 3 / 12 | ‐ | ‐ | ‐ | ‐ |
| O'Dwyer 1992a | 16 / 14 | 46 (27‐74) | 51 (38‐73) | 3 / 13 | 4 / 10 | ‐ | ‐ | 16 ‐ 0 ‐ 0 ‐ 0 | 14 ‐ 0 ‐ 0 ‐ 0 |
| Schmitz 1997a | 65 / 65 | 52.6 (14.6) | 54.1 (12.2) | 20 / 45 | 23 / 42 | ‐ | ‐ | ‐ | ‐ |
| Seenu 1994 | 97 / 84 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Wani 2002 | 50 / 50 | 34.8 (5.6) | 37.4 (6.2) | 5 / 45 | 5 / 45 | 21.5 (1.9) | 21.6 (1.8) | ‐ | ‐ |
| mean (standard deviation / range) |
Statistical analysis With adequate binary data available, a priori presentation in odds ratios was preferred, based on clinical considerations and statistical robustness of the odds ratio. From this, results could be presented in relative risk (ratio) (RR(R)) or numbers needed to treat (NNT) by recalculation. However, exploring the data showed that for many binary data the outcome was rare or zero in both arms. Odds ratios (OR) and risk ratios (RR) are not estimable in trials with zero events in both arms (Sweeting 2004). Binary outcomes with zero events in both arms can merely be presented in risk differences (RD). Although risk differences are statistically less robust and result in conservative estimates, they are simple measures, easy to understand, and useful for public communication.
For continuous data, authors generally present their results in medians with ranges due to suspicion of skewed data. However, for the analysis of data in a meta‐analysis, means with their corresponding standard deviations (SD) are needed to calculate mean differences (MD) or weighted mean differences (WMD) with 95% confidence intervals (CI). Using means from all trials would ignore a non‐Gaussian distribution. Therefore, skewness ratios (mean divided by the standard deviation) were calculated first (Higgins 2005, page 96). With a ratio larger than two, skewness is ruled out, whereas skewness is suggested when the ratio is between one and two and a ratio less than one indicates strong evidence of skewness. In situations where skewness could be ruled out, assumptions on equality of median to mean was made and used in the sensitivity analyses. For trials presenting confidence intervals or standard error of means, we performed a recalculation to a standard deviation (SD) (Higgins 2005, page 90‐91). In case no data on standard deviation was available, we calculated an average standard deviation from those observed in other studies and imputed this value for the standard deviation in the sensitivity analysis (Higgins 2005, page 92).
Results were considered according to the four different criteria of quality. The existence of an overall difference in outcome was clear when all four criteria showed significance. However, when the different quality criteria showed contradicting results, then an overall conclusion considering one outcome was not obvious and had to be made individually. In each individual component, results from high‐quality trials subgroups were given more weight compared to analyses including all trials or low‐quality trials subgroups. Results with confidence intervals that touched, but did not cross, the line of equivalence were considered not significant. Apart from comparisons in the four individual quality criteria, we also performed a comparison with trials divided into low‐bias risk trials (high methodological quality) and high‐bias risk trials (low methodological quality). Only trials that were assessed as adequate regarding all the four methodological criteria were considered low‐bias risk trials. All trials that were not assessed as adequate with regard to all the four methodological criteria were considered high‐bias risk trials.
Bias detection We have used funnel plots to provide a visual assessment of whether treatment estimates were associated with study size. The presence of publication bias and other biases (Begg 1994; Egger 1997; Macaskill 2001) varies with the magnitude of the treatment effect, the distribution of study size, and whether a one‐ or two‐tailed test is used (Macaskill 2001).
Both the random‐effects model (DerSimonian 1986) and the fixed‐effect model (DeMets 1987) for pooling effect estimates were explored.
In case of no discrepancy (and no heterogeneity) the fixed‐effect models were presented.
In case of discrepancy between the two models (ie, one giving a significant intervention effect and the other no significant intervention effect) both results were reported. Discrepancy will only occur when substantial heterogeneity is present.
Most weight was put on the results of the fixed‐effect model if the meta‐analysis included one or more large trials, provided that they had adequate methodology. (By large trials we refer to those that outnumber the rest of the included trials in terms of numbers of outcomes and participants (ie, more than half of all included events and participants)).
Otherwise, most weight was put on the results of the random‐effects model as it incorporated heterogeneity. The reason for this was that the random‐effects model increases the weight of small trials. Small trials however are more often than large trials conducted with unclear or inadequate methods (Kjaergard 2001).
In situations of excessive heterogeneity we refrained from reporting a pooled estimate when inappropriate.
The main focus of looking at heterogeneity in meta‐analysis is to discriminate true effect modifiers from other sources of heterogeneity. Heterogeneity was calculated by the Cochrane Q test and quantified by measuring I2 (Higgins 2002). If excessive heterogeneity occurred, data were re‐checked first and then adjusted. Extreme outliers were excluded (and tested in sensitivity analyses) when adequate reasons were available. If excessive heterogeneity still remained, depending on the specific research question, alternative methods were considered: subgroup analysis and meta‐regression if appropriate. Subgroup analysis Subgroup analyses were performed to compare the effects of the interventions according to the methodological quality of the trials (adequate compared to unclear/inadequate). Furthermore, causes of heterogeneity (defined as the presence of statistical heterogeneity by chi‐squared test with significance set at P‐value < 0.10 and measured by the quantities of heterogeneity by I2 (Higgins 2002)) were explored by comparing different groups of trials stratified to level of experience of the surgeon and other factors that may explain heterogeneity. Sensitivity analyses were performed imputing medians and using average standard deviations for missing data. In case of outliers and borderline trials sensitivity analyses were performed as well. Subgroup analyses were performed testing the influence of antibiotic prophylaxis, surgical experience and intra‐operative cholangiography on operative time, complications and hospital stay. These subgroup and sensitivity analyses were performed as far as data were available.
The statistical package (RevMan Analyses) was used (RevMan 2003). The statistical analyses were performed by FK and CL.
Results
Description of studies
Searches and trial identification For the search strategies used and the number of hits we refer to Appendix 1.
The search was conducted in The Cochrane Hepato‐Biliary Group Controlled Trials Register (840 hits, 65 selected) and The Cochrane Library, Issue 1, 2004 with the following results: the Cochrane Database of Systematic Reviews (33 hits, none were selected), the Database of Abstracts of Reviews on Effects (DARE) (17 hits, 5 selected), the Cochrane Central Register of Controlled Trials (CENTRAL) (1343 hits, 146 selected), the Health Technology Assessment (HTA) Database (11 hits, 4 selected), and the NHS Economic Evaluation Database (43 hits, 6 selected).
The search further comprised the following databases: The National Library of Medicine (MEDLINE) (8354 hits, 347 selected), The Intelligent Gateway to Biomedical & Pharmacological Information (EMBASE) (685 hits, 131 selected), ISI Web of Knowledge (Web of Science) (1163 hits, 148 selected), and CINAHL (740 hits, 9 selected).
Altogether, the search resulted in 13229 hits. The first selection process was performed based on the title of the publications. In each step of selection, we included the publication in case of any doubt. The total number of selections by title from this group of 13229 publications was 911 hits. After correction for duplicates, 586 remained.
The abstracts of these 586 publications were reviewed independently by two reviewers (FK and JJ) in order to evaluate whether the study should be included in the review. Differences between FK and JJ were discussed with CL. A total of 428 publications could be rejected based on their abstract. Initially, trials which did not clearly mention whether they were randomised clinical trials or not, were given the benefit of the doubt. If appropriate, they were excluded later on. Eventually, 158 publications were selected for further evaluation and these are all listed in this review with reasons for in‐ or exclusion.
A total of 150 publications were excluded (see table with 'Characteristics of excluded studies'). A total of eight publications describing seven trials including 571 patients were included (see table with 'Characteristics of included studies' and Table 1). Critical appraisal and data extraction of these seven trials were done by FK, JJ, and CL, separately. Any disagreements were solved in several consensus meetings.
As no language restrictions were used, one publication (Coelho 1992a) was translated. Double publications of the trial results by the same research group are listed in the references of included studies, and are considered as one trial (eg, Wani 2002). After contacting individual trialists, no additional data or information were obtained.
Patient characteristics All included trials used similar inclusion criteria, ie, patients with symptomatic cholecystolithiasis who were scheduled for elective cholecystectomy. The extensiveness in which exclusion criteria were described varied among the trials, but nearly all trials excluded acute cholecystitis. Trials with exclusively acute cholecystitis as inclusion criterion for cholecystectomy were excluded. Trials that included minorities of patients with acute cholecystitis next to patients with symptomatic cholecystolithiasis were included.
Trial designs Only one trial used a three‐arm design (Coelho 1993). All other trials used a two‐arm parallel‐group design.
Surgical interventions Some trials using the small‐incision technique did not mention the size of the incision. We classified these trials as a small‐incision cholecystectomy and not an open cholecystectomy, based on how the author labelled the operation procedure. Two trials performed small‐incision cholecystectomy by a 5 cm midline incision, the others by a transverse incision in the right hypochondrium, some with muscle splitting, others by transsection of the rectus or oblique muscles. Open cholecystectomy was normally performed by a subcostal or transverse incision, sometimes by midline laparotomy.
Antibiotic prophylaxis administered at induction of anaesthesia was explicitly mentioned in some trials. In others the explicit omission of antibiotic prophylaxis was mentioned, but most trials did not report on its use. Information on surgical experience (one or a few highly experienced surgeons performing all operations or also involving registrars) and intra‐operative cholangiography (attempted in all or only in selected patients) was recorded as well.
Outcome measures A problem considering relief of symptoms and pain is how this outcome is defined and measured. Apart from differences in measurement, very few trials reported on this outcome. Therefore, we were unable to report results considering relief of symptoms and pain. Nearly all trials reported on complications, operative time, and hospital stay. Trials did not clearly mention mortality. Because of the wide range of the types of complications described, we classified (subcategorised) all complications into four subcategories (intra‐operative, minor, severe, or bile duct injury) in addition to a total complication proportion (Table 3). Each complication was classified twice: once in one of the four subcategories (intra‐operative, minor, severe, or bile duct injury) and once again in the total complication proportion. Consequently, all bile duct complications were registered separately from all other complications (and not counted in the severe and minor subcategories). Likewise, all intra‐operative complications (except from the bile duct injuries) were categorised separately from other minor and severe complications.
3. Complications specified per operative technique: small‐incision vs open cholecys.
| Complications | SIC | OC |
| INTRA‐OPERATIVE | (0) | (0) |
| POSTOPERATIVE ‐ MINOR | (25 / 8.6%) | (19 / 6.8%) |
| wound hematoma | 12 | 4 |
| wound infection | 12 | 15 |
| urinary retention | 1 | 0 |
| POSTOPERATIVE ‐ SEVERE | (4 / 1.4%) | (7 / 2.5%) |
| stone left in cystic duct (re‐operation) | 1 | 0 |
| pneumonia | 1 | 5 |
| atelectasis | 1 | 0 |
| cardiovascular | 1 | 0 |
| upper GI bleeding (endoscopy / conservative) | 0 | 2 |
| BILE DUCT INJURY | (0) | (0) |
| TOTAL COMPLICATIONS | 29 (9.9%) | 26 (9.3%) |
| RE‐OPERATIONS (all complications) | 2 (0.7%) | 0 |
| TOTAL NUMBER OF PATIENTS INCLUDED (all trials) | 292 | 279 |
Pain scores and analgesic use as well as health‐related quality of life were frequently examined outcomes, but due to the great variation in the way these were measured and reported, it appeared impossible to pool results. Considering pulmonary function there is some limited data available from randomised trials. However, considering the inconsistency in the type of effect measure reported, as well as the difference in moments in time the outcome was measured, and the statistical problems that arise in pooling these results, we decided to refrain from reporting these results.
Risk of bias in included studies
We evaluated the internal validity of the trials by considering the four quality components, resulting in the following number of high‐quality (ie, adequate) trials. Information that was not mentioned in a trial was scored 'unclear'. When necessary information about randomisation, blinding procedure, or follow‐up was unclear or missing, the authors were contacted to obtain specific additional information on these issues. Trials of which no response was received, remained classified as 'unclear' trials.
Of the seven included trials we assessed the quality as adequate as follows: generation of allocation sequence one trial (14.3%), allocation concealment two trials (28.6%), blinding no trials (0%), and follow‐up one trial (14.3%) (Table 4; Figure 1; Figure 2).
4. Internal validity assessment of included trials: small‐incision vs open cholecys.
| Trial | Generation of alloc | Concealment of alloc | Blinding | Follow‐up |
| Assalia 1993 | U | U | N | U |
| Coelho 1992a | A | U | N | U |
| Coelho 1993 | U | U | N | U |
| O'Dwyer 1992a | U | A | N | U |
| Schmitz 1997a | U | A | N | A |
| Seenu 1994 | U | U | N | U |
| Wani 2002 | U | U | N | U |
| A: Adequate | U: Unclear | I: Inadequate | N: Not performed |
1.
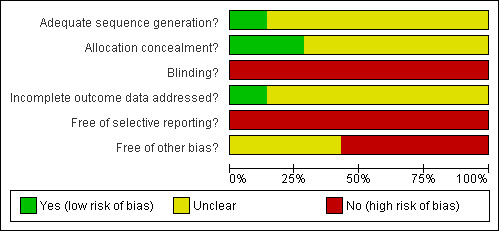
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
2.
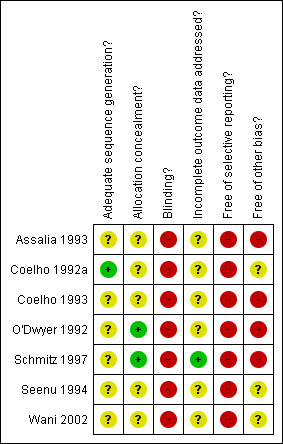
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
A comparison dividing trials into low‐bias risk trials (adequate methodological quality in all four criteria) versus high‐bias risk trials could not be performed as there was no low‐bias risk trial present.
Effects of interventions
We conducted five analyses: four comparisons based on the four methodological quality components including the subgroups high‐ and low‐quality trials, and a fifth comparison containing sensitivity and subgroup analyses. Background data of all trials on age, sex, body mass index (BMI), and American Society of Anaesthesiology (ASA) classification are shown in Table 2 as far as data were available.
We identified a total of seven randomised trials comparing small‐incision versus open cholecystectomy. A total of 292 and 279 patients were included in the small‐incision and open groups, respectively. Data were presented in Table 1 together with data on antibiotic prophylaxis, performance of cholangiography, and experience of the surgeon.
In the analyses, there were no significant differences in mortality, intra‐operative complications, severe complications, bile duct injuries, and operative time considering all trials, neither in the subgroups high‐quality and low‐quality trials, nor between the fixed‐effect model and the random‐effects model. As 'concealment of allocation' is regarded as the most important component of methodological quality, all subgroup results considering this aspect (except for the fore‐mentioned results that were not significantly different) were presented in additional Table 5.
5. Results of small‐incision vs open cholecystectomy: alloc. concealment (compar.2).
| Outcome | RD/WMD | HQ/LQ/AT | Fixed | Random | Discrepancy | Emphasize | HQ‐LQ difference | Significant |
| Minor complications | RD | HQ | 0.12 (0.03, 0.22) * | 0.11 (0.02, 0.21) * | no | |||
| LQ | ‐0.03 (‐0.07, 0.02) | ‐0.01 (‐0.04, 0.02) | no | |||||
| AT | 0.02 (‐0.03, 0.06) | 0.01 (‐0.03, 0.05) | no | random | yes | yes/no | ||
| Total complications | RD | HQ | 0.15 (0.04, 0.25) * | 0.14 (0.04, 0.24) * | no | |||
| LQ | ‐0.05 (‐0.10, 0.00) | ‐0.03 (‐0.10, 0.03) | no | |||||
| AT | 0.01 (‐0.04, 0.05) | 0.00 (‐0.06, 0.07) | no | random | yes | yes/no | ||
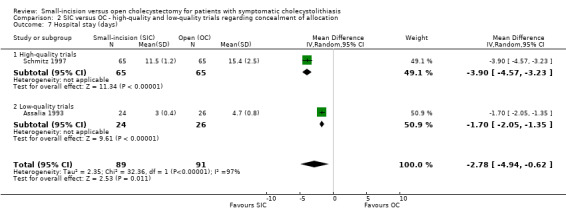
| Hospital stay | WMD | HQ | ‐3.90 (‐4.57, ‐3.23) * | ‐3.90 (‐4.57, ‐3.23) * | no | |||
| LQ | ‐1.70 (‐2.05, ‐1.35) * | ‐1.70 (‐2.05, ‐1.35) * | no | |||||
| AT | ‐2.16 (‐2.47, ‐1.85) * | ‐2.78 (‐4.94, ‐0.62) * | no | random | no | yes | ||
| * significant result | HQ: high‐quality trials | LQ: low‐quality trials | AT: all trials | RD: risk difference | WMD: weighted mean difference | random: random‐effects model |
Sensitivity analyses were performed imputing medians and standard deviations for missing data (operative time and hospital stay) and omitting one outlier in total complications. Other subgroup and sensitivity analyses were considered inappropriate as data were missing.
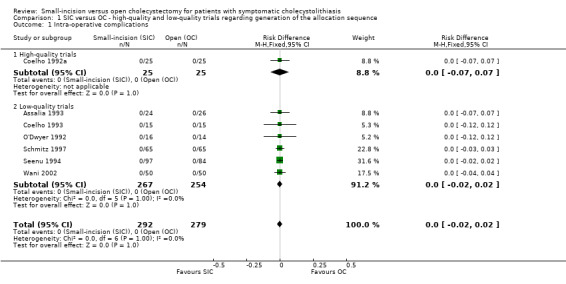
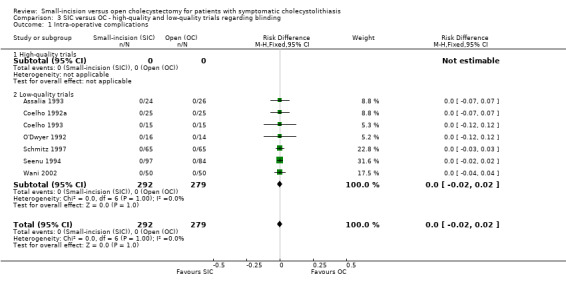
Mortality Mortality was not explicitly mentioned in all seven trials, therefore there were no results for calculating a pooled estimate. Intra‐operative complications In all seven trials complications were explicitly reported, of which zero intra‐operative complications. Consequently, there was no significant difference between the small‐incision and open technique.
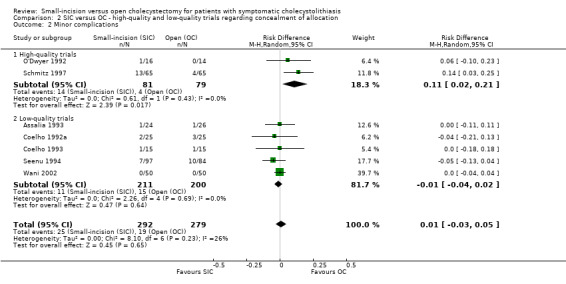
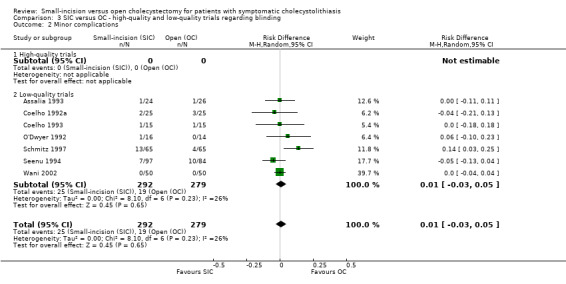
Minor complications The minor complication proportions were 8.6% and 6.8% in the small‐incision and open groups, respectively. In analysis of all trials there was no significant difference in minor complications (risk difference all trials 0.01, 95% CI ‐0.03 to 0.05). As heterogeneity was present, the random‐effects method has been applied. In the high‐quality subgroup in the 'concealment of allocation' comparison only (including two trials) a significant difference is present. In the other subgroups there were no significant differences.
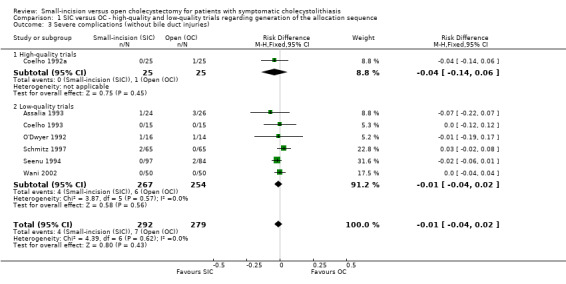
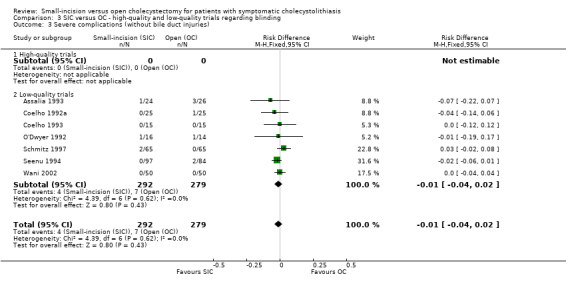
Severe complications The severe complication proportions were 1.4% and 2.5% in the small‐incision and open group, respectively. There were no significant differences between the small‐incision and open technique in all four methodological comparisons in all subgroups. As there was no heterogeneity, the fixed‐effect method has been used (risk difference all trials ‐0.01, 95% CI ‐0.04 to 0.02).
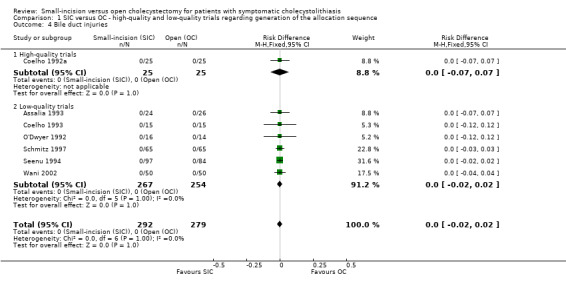
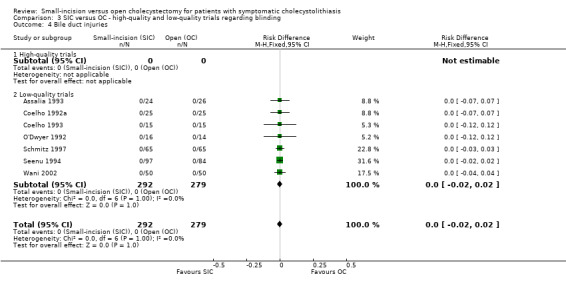
Bile duct injury In all seven trials no bile duct injuries were reported. Consequently, there was no significant difference between the small‐incision and open technique.
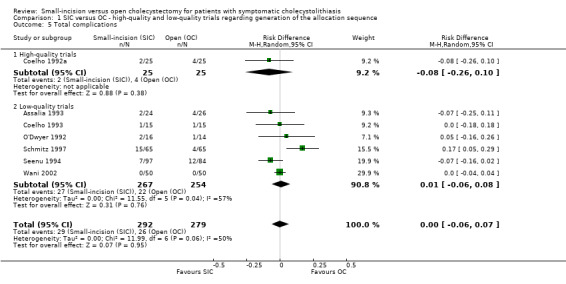
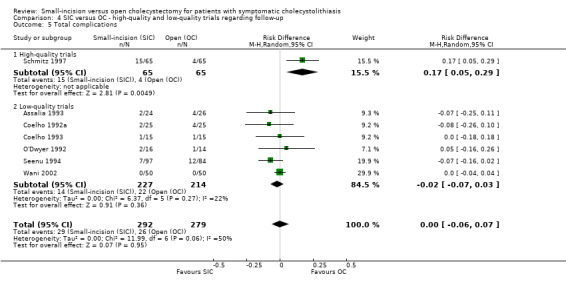
Total complications In a funnel plot using total complication proportions we did not find indication of publication bias (Figure 3). The total complication proportions were 9.9% and 9.3% in the small‐incision and open group, respectively (Table 3). Reoperation proportions are 0.7% and 0% respectively. We have found no significant difference in analysis of all trials (risk difference all trials, random‐effects 0.00, 95% CI ‐0.06 to 0.07). Only in the high‐quality trials subgroups in the 'allocation concealment' and 'follow‐up' comparisons, applying the random‐effects model, a significant difference favouring the open group has been found (caused by one trial only). Performing a sensitivity analysis (15‐3) by omitting the outlier (Schmitz 1997a) led to a reduction of heterogeneity (22%) and showed no significant difference (risk difference, fixed‐effect ‐0.04, 95% CI ‐0.09 to 0.01).
3.
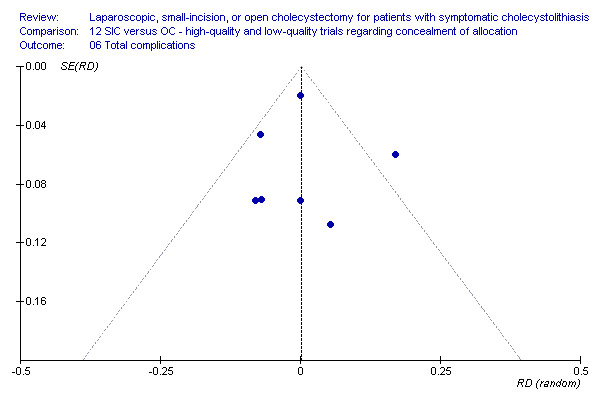
Funnel plot on small‐incision versus open cholecystectomy regarding concealment of allocation considering total complications, including 95% confidence interval lines. No arguments for bias.
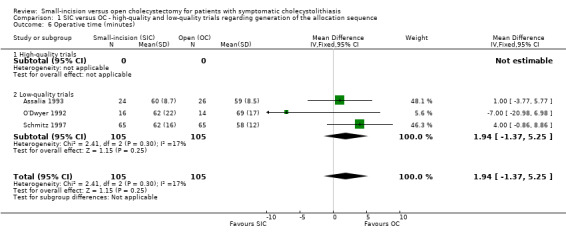
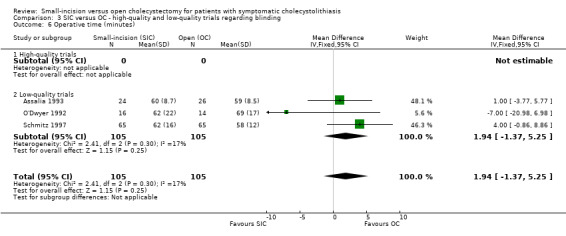
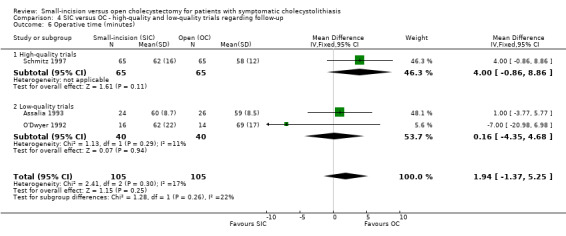
Operative time There were no significant differences between the small‐incision and open technique in all four methodological comparisons considering operative time. As only little heterogeneity was present, the fixed‐effect method was presented (WMD all trials, 1.94 minutes, 95% CI ‐1.37 to 5.25).
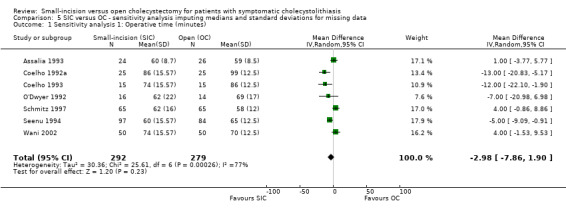
All available data were shown in Table 6. In a sensitivity analysis (15‐1) including the assumptions on standard deviations and medians considering skewness, there was no significant difference. As heterogeneity was present, the random‐effects method was used (WMD ‐2.98 minutes, 95% CI ‐7.86 to 1.90).
6. Operative time small‐incision vs open cholecystectomy: all available data.
| Trial | Type of data | SIC ‐ mean/median | SIC ‐ SD/range | OC ‐ mean/median | OC ‐ SD/range | Skewness SIC | Skewness OC |
| Assalia 1993 | A ‐ SD | 60 | 8.7 | 59 | 8.5 | 6.90 | 6.94 |
| Coelho 1992a | A ‐ | 86 | ‐ | 99 | ‐ | ‐ | ‐ |
| Coelho 1993 | A ‐ range | 74 | 40 ‐ 125 | 86 | 40 ‐ 140 | ‐ | ‐ |
| O'Dwyer 1992a | A ‐ SD | 62 | 22 | 69 | 17 | 2.82 | 4.06 |
| Schmitz 1997a | A ‐ SD | 62 | 16 | 58 | 12 | 3.88 | 4.83 |
| Seenu 1994 | A ‐ range | 60 | 30 ‐ 100 | 65 | 20 ‐ 90 | ‐ | ‐ |
| Wani 2002 | A ‐ range | 74 | 40 ‐ 125 | 70 | 50 ‐ 125 | ‐ | ‐ |
| A: Average / mean | SD: standard deviation |
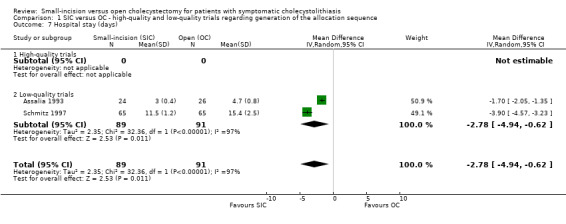
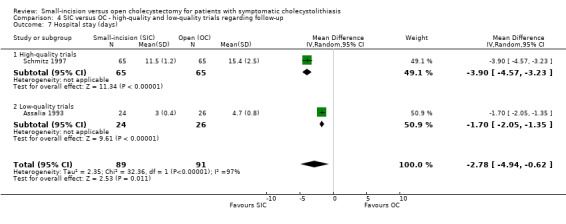
Hospital stay There was a significantly shorter hospital stay favouring the small‐incision technique. As severe heterogeneity was present, the random‐effects method was presented (WMD all trials, random‐effects ‐2.78 days, 95% CI ‐4.94 to ‐0.62). However, this concerns the data of only two trials.
All available data were presented in Table 7. In a sensitivity analysis (15‐2) including the assumptions on standard deviations and medians considering skewness, there was a significant shorter hospital stay in the small‐incision group (WMD, random‐effects ‐1.97 days, 95% CI ‐2.56 to ‐1.39).
7. Hospital stay small‐incision vs open cholecystectomy: all available data.
| Trial | Type of data | SIC ‐ mean/median | SIC ‐ SD/range | OC ‐ mean/median | OC ‐ SD/range | Skewness SIC | Skewness OC |
| Assalia 1993 | A ‐ SD | 3 | 0.4 | 4.7 | 0.8 | 7.5 | 5.88 |
| Coelho 1992a | A ‐ | 1,7 | ‐ | 3,5 | ‐ | ‐ | ‐ |
| Coelho 1993 | A ‐ range | 1 | 1 ‐ 1 | 2 | 2 ‐ 3 | ‐ | ‐ |
| O'Dwyer 1992a | M ‐ range | 3 | 1 ‐ 10 | 5 | 3 ‐ 8 | ‐ | ‐ |
| Schmitz 1997a | A ‐ SD | 11.5 | 1.2 | 15.4 | 2.5 | 9.58 | 6.16 |
| Seenu 1994 | A ‐ range | 2.6 | 1 ‐ 4 | 4 | 3 ‐ 8 | ‐ | ‐ |
| Wani 2002 | A ‐ | 3 | ‐ | 5 | ‐ | ‐ | ‐ |
| A: Average / mean | SD: standard deviation | M: median |
Convalescence No data on convalescence were available.
Discussion
The present systematic review contains three major findings. First, the comparison of the clinical outcome of small‐incision cholecystectomy with open cholecystectomy has been conducted in seven randomised clinical trials, including only 571 patients, and no trial could be classified as low‐bias risk trial (adequate in all four methodological criteria). Secondly, the total numbers of patients with complications were not significantly different for the two procedures. Thirdly, hospital stay was shorter for small‐incision cholecystectomy.
Considering the bias risks as well as the limited data on outcomes in the included trials, there are several questions that remain unanswered like pulmonary consequences after surgery, cost aspects, and more detailed questions on convalescence. High‐quality trials are more likely to estimate the 'true' effects of the interventions (Schulz 1995; Moher 1998; Kjaergard 2001; Jüni 2001; Egger 2003). Remembering this linkage between unclear / inadequate methodological quality to significant overestimation of beneficial effects and underreporting of adverse effects, the question is whether improvement in methodological quality of randomised trials will alter results.
No trial reported on mortality. There was no significant difference in complication proportions. All trials reported on total complications: 9.9% (small‐incision cholecystectomy) and 9.3% (open cholecystectomy). Intra‐operative, severe, and bile duct injury complications were not significantly different applying both the fixed‐effect and the random‐effects models. However, in subgroup analyses on 'allocation concealment' and 'follow‐up' as methodological quality aspect, total complications differed in the high‐quality group in favour of the open cholecystectomy group, both in the fixed‐effect and the random‐effects models. Both results are based on the outcome of one trial (Schmitz 1997a). In the other two methodological quality components, however, there were no significant differences in the subgroups. Therefore, total complications cannot be regarded as significantly different for the small‐incision group compared to the open group. In a sensitivity analysis the outlying trial (Schmitz 1997a) was omitted from the pooled results, which did not result in a significantly different outcome. The methodological quality of the seven randomised trials comparing small‐incision to open cholecystectomy was rather disappointing. Therefore total complication proportions (9.9% and 9.3%) must be interpreted with care. No clear indication of publication bias were found analysing total complication proportions (Figure 3).
There were no significant differences in operative time. In all subgroup comparisons, no significant differences in operating time were found (fixed‐effect and random‐effects models). However, only three trials could be included in the analysis due to missing data. In the sensitivity analysis on operative time, with assumptions on values for missing standard deviations and means and checking for skewness (additional Table 6) again no significant difference was found. Hospital stay was significantly shorter in the small‐incision group in all four subgroup analyses after incorporating the severe heterogeneity in the random‐effects model. In sensitivity analysis on hospital stay, using assumptions on values for missing data, and checking for skewness (additional Table 7), small‐incision cholecystectomy had a shorter hospital stay. No data on convalescence were available.
Authors' conclusions
Implications for practice.
We were unable to demonstrate significant differences between small‐incision versus open cholecystectomy regarding primary outcomes. We observed a significantly shorter duration of hospital stay in patients being treated by small‐incision cholecystectomy. Rationally, if expertise for the small‐incision approach is available, the small‐incision technique is preferable for these patients. Moreover, an intra‐operative conversion to open cholecystectomy remains possible without restrictions.
We recommend that every surgical department is able to offer this kind of elective surgery for patients with symptomatic cholecystolithiasis.
Implications for research.
Future trials on implementation issues of minimally invasive open and laparoscopic techniques in general will dominate surgical research. Randomised comparisons should be made of both minimally invasive techniques as well as traditional open techniques, both regarding clinical and oncological outcome measures as well as cost differences.
In accordance with research in general, the overall quality of the randomised trials included in this systematic review varied, with the majority of trials having several methodological deficiencies. In line with conclusions from other systematic reviews, the quality of included trials needs to improve in order to limit bias. Reports can be improved importantly by adopting the CONSORT Statement while conducting and reporting trials (www.consort‐statement.org).
What's new
| Date | Event | Description |
|---|---|---|
| 23 October 2008 | Amended | Converted to new review format. |
Notes
The protocol for this systematic review was first published in Issue 3, 1997 of The Cochrane Library. The reviewers, Dr T Jørgensen and H Laugesen have abandoned the preparation of the systematic review. This necessitated that an update of the protocol and preparation of the review be performed by a new team of reviewers. They are F Keus, JAF de Jong, HG Gooszen, and CJHM van Laarhoven. Due to the large number of identified trials it was considered wiser in terms of clarity and usability to produce three separate reviews. Thus this review is one of the three.
Correction of name Eric Keus, the lead author of the protocol, and Frederik Keus, the lead author of the review, is one and the same person.
Acknowledgements
The Cochrane Hepato‐Biliary Review Group, Copenhagen, for excellent support; The Dutch Cochrane Centre, Amsterdam for advice; The Library of the University Medical Center, Utrecht for cooperation in the search for full text articles; Geert van der Heijden (Julius Center for Health Sciences and Primary Care, University Medical Center, Utrecht) for advice in systematic searches; Ingeborg van der Tweel (Julius Center for Health Sciences and Primary Care, University Medical Center, Utrecht) for statistical advice; Laura Breuning, Jan Willem Elshof, and Yan Gong (Cochrane Hepato‐Biliary Review Group, Copenhagen) for translations.
Appendices
Appendix 1. Search strategies
| Database | Timespan of search | Search strategy | Hits | Titles selected |
| The Cochrane Hepato‐Biliary Group Controlled Trials Register | 6 April 2004 | "cholelithiasis OR gallstones OR cholecystectomy" | 843 | 65 |
| Cochrane Database of Systematic Reviews in The Cochrane Library | Issue 1, 2004 | "cholecystectomy" | 33 | 0 |
| Database of Abstracts of Reviews of Effects in The Cochrane Library | Issue 1, 2004 | "cholecystectomy" | 17 | 5 |
| Cochrane Central Register of Controlled Trials in The Cochrane Library | Issue 1, 2004 | "cholecystectomy" | 1343 | 146 |
| Health Technology Assessment Database in The Cochrane Library | Issue 1, 2004 | "cholecystectomy" | 11 | 4 |
| NHS Economic Evaluation Database in The Cochrane Library | Issue 1, 2004 | "cholecystectomy" | 43 | 6 |
| MEDLINE | 1950 to January 2004 | (((Gallbladder[Tiab] AND (Surgery[Tiab] OR Endoscopy[Tiab] OR Surgical[Tiab] OR Laparoscopy[Tiab])) OR Cholecystectomy[Tiab]) OR ((("Gallbladder"[MeSH] OR "Gallbladder Diseases"[MeSH]) AND ("Surgery"[MeSH] OR "surgery"[Subheading] OR "Endoscopy, Gastrointestinal"[MeSH] OR "Surgical Procedures, Operative"[MeSH] OR "Surgical Procedures, Minor"[MeSH] OR "Laparoscopy"[MeSH])) OR "Cholecystectomy"[MeSH])) AND (randomized controlled trial[PTYP] OR randomized controlled trials OR controlled clinical trial[PTYP] OR clinical trial[PTYP] OR clinical trials OR (clinical AND trial) OR random allocation OR random* OR double blind method OR single blind method OR (singl* OR doubl* OR trebl* OR tripl*) OR blind* OR mask* OR placebo* OR placebos OR research design OR comparative study OR evaluation studies OR follow up studies OR prospective studies OR control OR controlled OR prospectiv* OR volunteer*) | 8354 | 347 |
| EMBASE | 1966 to January 2004 | "cholecystectomy" | 685 | 131 |
| Web of Science | 1988 to January 2004 | TS=(cholecystectomy AND random*) | 1163 | 148 |
| CINAHL | 1982 to January 2004 | "cholecystectomy" | 740 | 9 |
| Total | 13232 | 586 |
Data and analyses
Comparison 1. SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Intra‐operative complications | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 1.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.07, 0.07] |
| 1.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 2 Minor complications | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| 2.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Random, 95% CI) | ‐0.04 [‐0.21, 0.13] |
| 2.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Random, 95% CI) | 0.02 [‐0.04, 0.07] |
| 3 Severe complications (without bile duct injuries) | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 3.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.04 [‐0.14, 0.06] |
| 3.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 4 Bile duct injuries | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 4.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.07, 0.07] |
| 4.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 5 Total complications | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| 5.1 High‐quality trials | 1 | 50 | Risk Difference (M‐H, Random, 95% CI) | ‐0.08 [‐0.26, 0.10] |
| 5.2 Low‐quality trials | 6 | 521 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.06, 0.08] |
| 6 Operative time (minutes) | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 6.1 High‐quality trials | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Low‐quality trials | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 7 Hospital stay (days) | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| 7.1 High‐quality trials | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Low‐quality trials | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
1.1. Analysis.
Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 1 Intra‐operative complications.
1.2. Analysis.
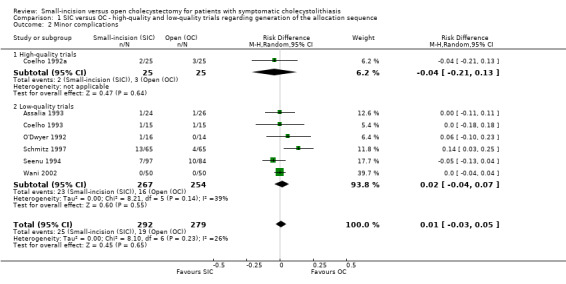
Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 2 Minor complications.
1.3. Analysis.
Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 3 Severe complications (without bile duct injuries).
1.4. Analysis.
Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 4 Bile duct injuries.
1.5. Analysis.
Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 5 Total complications.
1.6. Analysis.
Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 6 Operative time (minutes).
1.7. Analysis.
Comparison 1 SIC versus OC ‐ high‐quality and low‐quality trials regarding generation of the allocation sequence, Outcome 7 Hospital stay (days).
Comparison 2. SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Intra‐operative complications | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 1.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.03, 0.03] |
| 1.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 2 Minor complications | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| 2.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Random, 95% CI) | 0.11 [0.02, 0.21] |
| 2.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Random, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 3 Severe complications (without bile duct injuries) | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 3.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Fixed, 95% CI) | 0.02 [‐0.03, 0.08] |
| 3.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.02 [‐0.06, 0.01] |
| 4 Bile duct injuries | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 4.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.03, 0.03] |
| 4.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 5 Total complications | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| 5.1 High‐quality trials | 2 | 160 | Risk Difference (M‐H, Random, 95% CI) | 0.14 [0.04, 0.24] |
| 5.2 Low‐quality trials | 5 | 411 | Risk Difference (M‐H, Random, 95% CI) | ‐0.03 [‐0.10, 0.03] |
| 6 Operative time (minutes) | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 6.1 High‐quality trials | 2 | 160 | Mean Difference (IV, Fixed, 95% CI) | 2.81 [‐1.78, 7.41] |
| 6.2 Low‐quality trials | 1 | 50 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐3.77, 5.77] |
| 7 Hospital stay (days) | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| 7.1 High‐quality trials | 1 | 130 | Mean Difference (IV, Random, 95% CI) | ‐3.9 [‐4.57, ‐3.23] |
| 7.2 Low‐quality trials | 1 | 50 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐2.05, ‐1.35] |
2.1. Analysis.
Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 1 Intra‐operative complications.
2.2. Analysis.
Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 2 Minor complications.
2.3. Analysis.
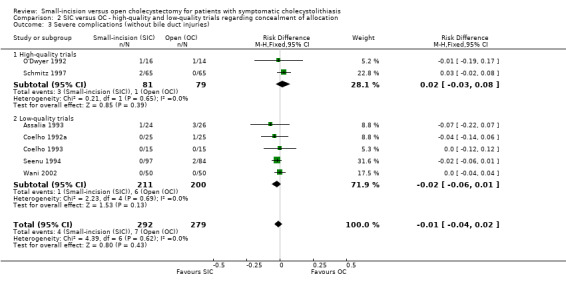
Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 3 Severe complications (without bile duct injuries).
2.4. Analysis.
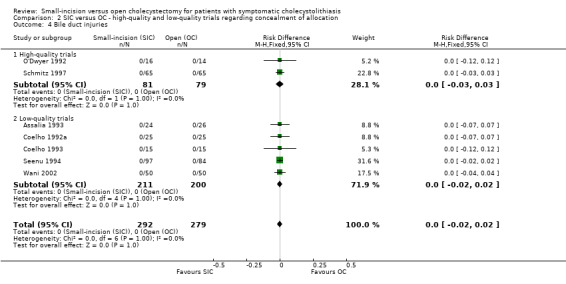
Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 4 Bile duct injuries.
2.5. Analysis.
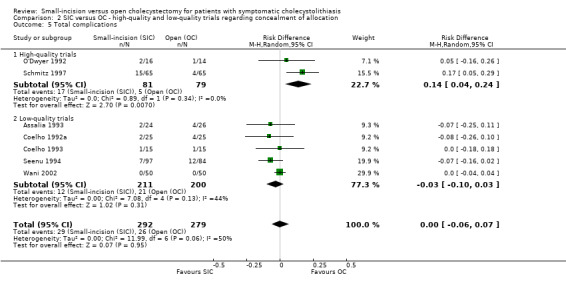
Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 5 Total complications.
2.6. Analysis.
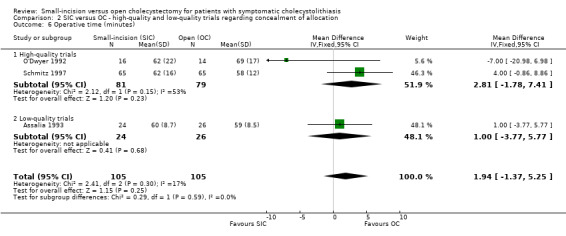
Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 6 Operative time (minutes).
2.7. Analysis.
Comparison 2 SIC versus OC ‐ high‐quality and low‐quality trials regarding concealment of allocation, Outcome 7 Hospital stay (days).
Comparison 3. SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Intra‐operative complications | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 1.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 2 Minor complications | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| 2.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| 3 Severe complications (without bile duct injuries) | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 3.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 4 Bile duct injuries | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 4.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 5 Total complications | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| 5.1 High‐quality trials | 0 | 0 | Risk Difference (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Low‐quality trials | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| 6 Operative time (minutes) | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 6.1 High‐quality trials | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Low‐quality trials | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 7 Hospital stay (days) | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| 7.1 High‐quality trials | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Low‐quality trials | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
3.1. Analysis.
Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 1 Intra‐operative complications.
3.2. Analysis.
Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 2 Minor complications.
3.3. Analysis.
Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 3 Severe complications (without bile duct injuries).
3.4. Analysis.
Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 4 Bile duct injuries.
3.5. Analysis.
Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 5 Total complications.
3.6. Analysis.
Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 6 Operative time (minutes).
3.7. Analysis.
Comparison 3 SIC versus OC ‐ high‐quality and low‐quality trials regarding blinding, Outcome 7 Hospital stay (days).
Comparison 4. SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Intra‐operative complications | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 1.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.03, 0.03] |
| 1.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 2 Minor complications | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.01 [‐0.03, 0.05] |
| 2.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Random, 95% CI) | 0.14 [0.03, 0.25] |
| 2.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Random, 95% CI) | ‐0.01 [‐0.04, 0.03] |
| 3 Severe complications (without bile duct injuries) | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.01 [‐0.04, 0.02] |
| 3.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Fixed, 95% CI) | 0.03 [‐0.02, 0.08] |
| 3.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.02 [‐0.05, 0.01] |
| 4 Bile duct injuries | 7 | 571 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 4.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.03, 0.03] |
| 4.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Fixed, 95% CI) | 0.0 [‐0.02, 0.02] |
| 5 Total complications | 7 | 571 | Risk Difference (M‐H, Random, 95% CI) | 0.00 [‐0.06, 0.07] |
| 5.1 High‐quality trials | 1 | 130 | Risk Difference (M‐H, Random, 95% CI) | 0.17 [0.05, 0.29] |
| 5.2 Low‐quality trials | 6 | 441 | Risk Difference (M‐H, Random, 95% CI) | ‐0.02 [‐0.07, 0.03] |
| 6 Operative time (minutes) | 3 | 210 | Mean Difference (IV, Fixed, 95% CI) | 1.94 [‐1.37, 5.25] |
| 6.1 High‐quality trials | 1 | 130 | Mean Difference (IV, Fixed, 95% CI) | 4.0 [‐0.86, 8.86] |
| 6.2 Low‐quality trials | 2 | 80 | Mean Difference (IV, Fixed, 95% CI) | 0.16 [‐4.35, 4.68] |
| 7 Hospital stay (days) | 2 | 180 | Mean Difference (IV, Random, 95% CI) | ‐2.78 [‐4.94, ‐0.62] |
| 7.1 High‐quality trials | 1 | 130 | Mean Difference (IV, Random, 95% CI) | ‐3.9 [‐4.57, ‐3.23] |
| 7.2 Low‐quality trials | 1 | 50 | Mean Difference (IV, Random, 95% CI) | ‐1.70 [‐2.05, ‐1.35] |
4.1. Analysis.
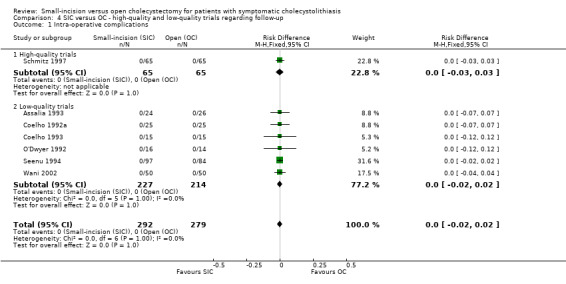
Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 1 Intra‐operative complications.
4.2. Analysis.
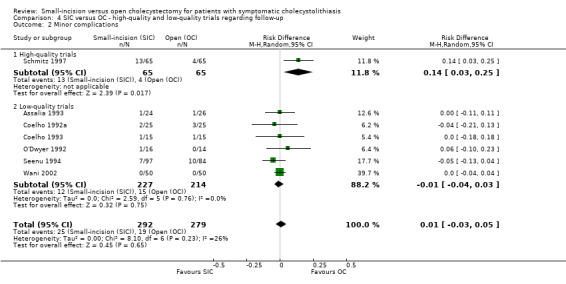
Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 2 Minor complications.
4.3. Analysis.
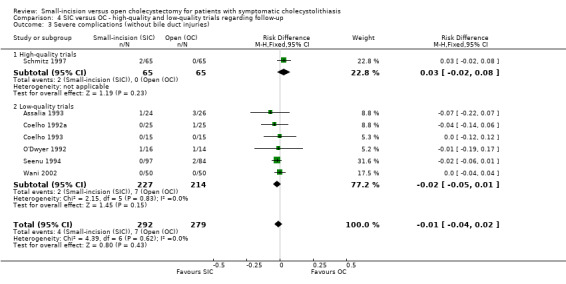
Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 3 Severe complications (without bile duct injuries).
4.4. Analysis.
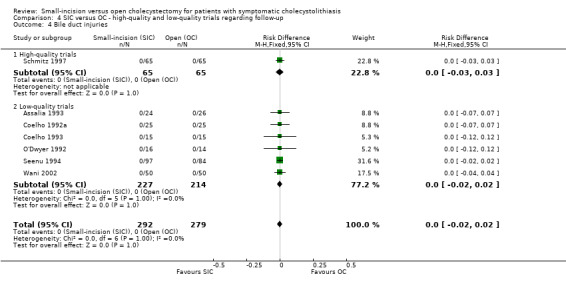
Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 4 Bile duct injuries.
4.5. Analysis.
Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 5 Total complications.
4.6. Analysis.
Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 6 Operative time (minutes).
4.7. Analysis.
Comparison 4 SIC versus OC ‐ high‐quality and low‐quality trials regarding follow‐up, Outcome 7 Hospital stay (days).
Comparison 5. SIC versus OC ‐ sensitivity analysis imputing medians and standard deviations for missing data.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Sensitivity analysis 1: Operative time (minutes) | 7 | 571 | Mean Difference (IV, Random, 95% CI) | ‐2.98 [‐7.86, 1.90] |
| 2 Sensitivity analysis 2: Hospital stay (days) | 7 | 571 | Mean Difference (IV, Random, 95% CI) | ‐1.97 [‐2.56, ‐1.39] |
| 3 Sensitivity analysis 3: Omitting outlier Schmitz in total complications | 6 | 441 | Risk Difference (M‐H, Fixed, 95% CI) | ‐0.04 [‐0.09, 0.01] |
5.1. Analysis.
Comparison 5 SIC versus OC ‐ sensitivity analysis imputing medians and standard deviations for missing data, Outcome 1 Sensitivity analysis 1: Operative time (minutes).
5.2. Analysis.
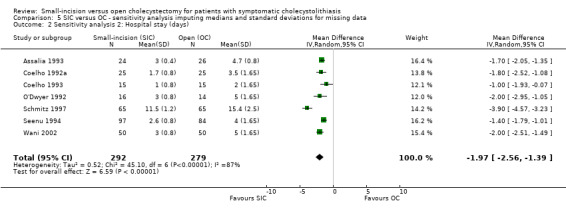
Comparison 5 SIC versus OC ‐ sensitivity analysis imputing medians and standard deviations for missing data, Outcome 2 Sensitivity analysis 2: Hospital stay (days).
5.3. Analysis.
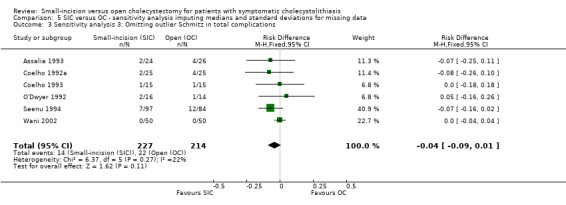
Comparison 5 SIC versus OC ‐ sensitivity analysis imputing medians and standard deviations for missing data, Outcome 3 Sensitivity analysis 3: Omitting outlier Schmitz in total complications.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Assalia 1993.
| Methods | Single‐centre randomised trial. Generation of allocation: unclear. Allocation concealment: unclear. Blinding: not performed. Follow‐up: unclear. Drop‐outs: none mentioned. Intention‐to‐treat: not mentioned. Sample size calculations: no. |
|
| Participants | Elective cholecystectomy for symptomatic cholelithiasis. In‐ and exclusion criteria: not mentioned. Comparability groups: well matched. |
|
| Interventions | SIC versus OC. Minicholecystectomy: initial 5 cm (no preoperative ultrasound location), extended in stages each 1 cm long. Retrograde (fundus down) technique was performed. Open cholecystectomy: technique was left to the individual surgeon. Length of incision: offer comfortable exposure, however, not too generous. Antibiotic prophylaxis: yes. Intra‐operative cholangiography: selectively carried out according to clinical and laboratory indications. |
|
| Outcomes | Primary and secondary outcome: not mentioned. Outcomes: difficulty of the procedure, operative time, degree of pain, total amount of analgesia, hospital stay, patient satisfaction, physical activity limitations. Duration of follow‐up: 2 weeks. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes | High risk | |
| Free of selective reporting? | High risk | |
| Free of other bias? | High risk | short follow‐up of 2 weeks |
Coelho 1992a.
| Methods | Single‐centre trial. Generation of allocation: adequate, by cards. (aleatoriamente = randomised). Allocation concealment: unclear. Blinding: not performed. Follow‐up: unclear. Drop‐outs: none mentioned. Intention‐to‐treat: not mentioned. Sample size calculations: no. |
|
| Participants | Patients admitted for cholecystectomy. In‐ and exclusion criteria: not very well described. Comparability groups: well matched. |
|
| Interventions | SIC versus OC. Both procedures not further specified. Antibiotic prophylaxis: not mentioned. Intra‐operative cholangiography: routinely performed in both groups. |
|
| Outcomes | Primary and secondary outcome: not described. Outcome measures: clinical results. Duration of follow‐up: hospital stay. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes | High risk | |
| Free of selective reporting? | High risk | |
Coelho 1993.
| Methods | Single‐centre trial. Generation of allocation: unclear. Patients randomly and prospectively divided into three groups. Allocation concealment: unclear. Blinding: not performed. Follow‐up: unclear. Drop‐outs: none mentioned. Intention‐to‐treat: not mentioned. Sample size calculations: no. |
|
| Participants | Chronic calculous cholecystitis admitted for elective cholecystectomy. In‐ and exclusion criteria: not described. Comparability groups: well matched. |
|
| Interventions | LC versus SIC versus OC. LC: four‐trocar technique, carbon dioxide insufflated. SIC: right upper quadrant transverse incision of 5 to 8 cm. OC: right upper quadrant subcostal incision of 15 to 20 cm. Antibiotic prophylaxis: not mentioned. Intra‐operative cholangiography: not mentioned. |
|
| Outcomes | Primary and secondary outcome: not defined. Outcome measures: comparison of reduction in pulmonary function. Duration of follow‐up: not mentioned. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes | High risk | |
| Free of selective reporting? | High risk | |
| Free of other bias? | High risk | unclear duration of follow‐up |
O'Dwyer 1992.
| Methods | Two‐centre trial. Generation of allocation: unclear. Allocation concealment: adequate (sealed envelope). Blinding: not performed. Follow‐up: unclear. Drop‐outs: none mentioned. Intention‐to‐treat: not mentioned. Sample size calculations: no. |
|
| Participants | Patients having cholecystectomy for symptomatic gallstones. In‐ and exclusion criteria: well described. Comparability groups: well matched. |
|
| Interventions | SIC versus OC. SIC: through 6 cm incision, rectus muscle divided. OC: not further described. Antibiotic prophylaxis: not mentioned. Routine operative cholangiography in all patients. |
|
| Outcomes | Primary and secondary outcome: not specified. Outcome measures: pulmonary, function tests, analgesia requirements, hospital stay. Duration of follow‐up: hospital stay. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes | High risk | |
| Free of selective reporting? | High risk | |
| Free of other bias? | High risk | short follow‐up (hospital stay) |
Schmitz 1997.
| Methods | Randomised clinical single‐centre trial. Generation of allocation: unclear. Allocation concealment: adequate. Blinding: not performed. Follow‐up: adequate. Drop‐outs: none; postoperative observation was extended to complete the investigation. Intention‐to‐treat: not mentioned. Sample size calculations: no. |
|
| Participants | Patients for elective cholecystectomy. In‐ and exclusion criteria: not very well described. Comparability groups: well matched. |
|
| Interventions | SIC versus OC. SIC: 6 cm subcostal transverse incision with diathermy transsection of the right rectus abdominis muscle. OC: a 13 cm subcostal incision with additional partial extension into the muscle spaces of the right lateral epigastric region. Antibiotic prophylaxis: not mentioned. Intra‐operative cholangiography: not mentioned. |
|
| Outcomes | Primary and secondary outcome: not mentioned. Outcome measures: operating times, level of subjective pain, analgesic intake, complications. Duration of follow‐up: not mentioned. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Blinding? All outcomes | High risk | |
| Incomplete outcome data addressed? All outcomes | Low risk | |
| Free of selective reporting? | High risk | |
| Free of other bias? | High risk | unclear duration of follow‐up |
Seenu 1994.
| Methods | Single‐centre randomised trial, operations performed by consultants and senior residents. Generation of allocation: unclear. Allocation concealment: unclear. Blinding: not performed. Follow‐up: unclear. Drop‐outs: none mentioned. Intention‐to‐treat: not mentioned. Sample size calculations: no. |
|
| Participants | Patients undergoing elective cholecystectomy. In‐ and exclusion criteria: not very well described. Comparability groups: not very well described. |
|
| Interventions | SIC versus OC. SIC: very well described, a 5 cm transverse incision in the right upper quadrant. OC: vertical midline incision. Antibiotic prophylaxis: not mentioned. Intra‐operative cholangiography: no, selective pre‐operative cholangiogram was performed when necessary. |
|
| Outcomes | Primary and secondary outcome: not mentioned. Outcome measures: complications, operative time, hospital stay. Duration of follow‐up: 30 days. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes | High risk | |
| Free of selective reporting? | High risk | |
Wani 2002.
| Methods | Single‐centre trial. Randomised trial: prospective study with patients systematically divided. Generation of allocation: unclear. Allocation concealment: unclear. Blinding: not performed. Follow‐up: unclear. Drop‐outs: none mentioned. Intention‐to‐treat: not mentioned. Sample size calculations: no. |
|
| Participants | Patients with chronic calculus cholecystitis. In‐ and exclusion criteria: not very well described. Comparability groups: well matched. |
|
| Interventions | SIC versus OC. SIC: incision of 5 cm to 7 cm length with two well illuminated retractors, dissected either duct first or fundus first. OC: right subcostal incision of 10 cm to 15 cm. Antibiotic prophylaxis: not mentioned. Intra‐operative cholangiography: not mentioned |
|
| Outcomes | Primary and secondary outcome: not mentioned. Outcome measures: pulmonary function. Duration of follow‐up: not mentioned (hospital stay). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Blinding? All outcomes | High risk | |
| Free of selective reporting? | High risk | |
| Free of other bias? | Unclear risk | short follow‐up |
LC ‐ laparoscopic cholecystectomy, SIC ‐ small‐incision cholecystectomy, OC ‐ open cholecystectomy.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agnifili 1993 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Al Tameem 1995 | Prospective study on three different types of small‐incision cholecystectomy, not randomised. |
| Alexander 1997 | Review on pain after laparoscopy; not a randomised trial. |
| Allen 2002 | Comparison of costs of LC between ten surgeons; no comparison of operative procedures. |
| Alponat 2002 | Randomised clinical trial on conventional LC (two 10 mm and two 5 mm ports) and LC by small instruments (one 10 mm and three 2 mm ports); thus comparison of two types of LC. |
| Anonymous 1995 | Editorial: discussion of other article. |
| Assalia 1997 | Randomised trial only including patients with acute cholecystitis. |
| Bablekos 2003 | Correspondence with GD Bablekos on 11 October 2004: separating patients in triads with allocation according to registration sequence at the emergency ward: quasi‐randomised study of LC versus OC. |
| Barkun 1992 | Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. |
| Barkun 1993 | Comparison of three different time periods; not a randomised trial. |
| Baxter 1992 | Debate, consideration. |
| Bellon 1998 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Berggren 1994 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Bernard 1994 | Economic evaluation. |
| Bigard 1995 | Review on indications and methods of cholecystectomy in treatment of gallstones. |
| Blanc‐Louvry 2000 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Blomstedt 1972 | Study on the frequency of incisional hernias after different types of conventional cholecystectomy; not a randomised trial. |
| Bolke 2000 | Quasi‐randomised trial: "... patients were randomised by alternate number to LC or OC ...". |
| Bruce 1999 | Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. |
| Bukan 2004 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Byrne 1994 | Prospective, not randomised study: " ... equipment was only made available on an intermittent basis ...". |
| Calland 2001 | Prospective study on outpatient LC, comparing with historical (inpatient) LC; not a randomised trial. |
| Caplan 1999 | Study on costs and patient satisfaction before and after re‐engineering of a surgical service in LC patients and elective herniorrhaphy; no comparison of different types of cholecystectomy. |
| Champault 2002 | One‐arm prospective study on costs; not a randomised trial (not two arms). |
| Charlo 1995 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Chaudhary 1999 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Chumillas 1998 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Clezy 1996 | Letter. |
| Coelho 1992 | Not a randomised trial; prospective study of small‐incision cholecystectomy. |
| Coskun 2000 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Da Costa 1995 | Prospective study, not randomised: "... patients were not randomised as it was felt that it was unethical to do so ...". |
| Dauleh 1995 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Decker 1993 | Not randomised; prospective study. |
| Delogu 1999 | Stress response in LC and OC patients, not randomised: "... 22 patients underwent OC and the other 24 had LC according to the availability of laparoscopic equipment ...". |
| Demirer 2000 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Dionigi 1994 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Dohrmann 1993 | Not randomised; randomisation was not possible as most patients opted for the laparoscopic technique. |
| Eickhoff 1997 | Not a randomised trial: patients who were operated by LC or OC were analysed. |
| Engin 1998 | Randomised trial evaluating laparoscopic and open cholecystectomy |
| Essen 1995 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Frazee 1991 | No correct randomisation between two operative techniques: "... patients were randomly assigned to individual staff surgeons, as is our customary practice ...". |
| Gal 1997 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Galizia 2001 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| GarciaCaballero 1993 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Glaser 1995 | Prospective study with control group, not randomised: "... because of the ethical problems associated with randomisation of LC and OC, we decided to conduct a prospective trial without randomisation, but with a control group ...". |
| Go 1995 | Retrospective study on cost‐effectiveness between extracorporeal shock‐wave lithotripsy, conventional cholecystectomy, and laparoscopic cholecystectomy. |
| Grande 2002 | Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. |
| Hagmuller 1997 | Not randomised: the authors felt that randomisation was not possible on ethical grounds. |
| Hasukic 2002 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Hauer‐Jensen 1986 | Randomised trial comparing performing cholecystectomy with or without a routine cholangiography. |
| Hendolin 2000 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Hobbs 1995 | Considerations on laparoscopic cholecystectomy, not a randomised trial. |
| Huang 1996 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Huguier 1997 | Considerations on laparoscopic digestive surgery, not a randomised trial. |
| Hunter 2001 | Editorial. |
| Iwase 1992 | Not a randomised trial. |
| Jan 1993 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Johnson 1997 | Considerations on laparoscopic surgery. |
| Johnson 1998 | Personal view: consideration on efficacy, safety and training; not a randomised trial. |
| Johnson 1998a | Letter. |
| Karayiannakis 1997 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Karayiannakis 2002 | Prospective study in patients having LC and OC, but no randomisation: "... twelve patients who had OC were recruited and served as the control group ...". |
| Kehlet 1993 | Consideration of gallstone treatment modalities. |
| Keus 2006 | Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. |
| Kiviluoto 1997 | Randomised trial between LC and OC on acute cholecystitis. |
| Kjaersgaard 1994 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Koprulu 1996 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Krasinski 1998 | Prospective study on patients who underwent LC: patients with uncomplicated LC were compared to patients who had conversion from LC to OC. |
| Krawczyk 1993 | Not a randomised trial: "the groups were not randomised". |
| Kunz 1992 | Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. |
| Kurzawinski 1992 | Prospective study, but not randomised: "... patients were randomly allocated to either LC or OC, based on the availability of laparoscopic equipment ...". |
| Lam 1996 | Survey in Scotland on cholecystectomy rate; not a randomised trial. |
| Lausten 1999 (1) | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Lausten 1999 (2) | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Lujan 1998 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Lukichev 1983 | Cohort of patients treated by one technique; not a randomised trial. |
| Luo 2003 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Majeed 1996 | Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. |
| Makinen 1995 | Only pilot phase of trial; in pilot phase no randomisation: SIC was performed when LC instruments were not available. |
| Malaysian HTA 2005 | Systematic review on different types of minimal access surgery; not a randomised trial. |
| Maruszynski 1995 | Patients with acute cholecystitis only. |
| Matsunaga 1996 | Comparison of two different types of anaesthesia in cholecystectomy. |
| McGinn 1995 | Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. |
| McKellar 1995 | Comparison of historical cohorts. |
| McMahon 1994 | Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. |
| McMahon 1996 | Letter, not a randomised trial. |
| Mealy 1992 | An unselected group of patients undergoing LC in one hospital was compared with a group undergoing OC in another hospital. |
| Milheiro 1994 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Mimica 2000 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Mrksic 2001 | No randomisation. |
| Novitsky 2002 | Randomised controlled trial on two types of laparoscopic cholecystectomy (mini‐port LC (2 mm) versus conventional LC). |
| Ogawa 2001 | Retrospective study on LC versus OC in patients with cardiac valve replacement. |
| Olsen 1993 | Review of literature from 1970 to 1992 on mini‐lap cholecystectomy: only articles in English were included and data on conventional and laparoscopic cholecystectomy were obtained from large series reported in literature. |
| Ortega 1996 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Plaisier 1995 | Prospective not randomised study: "... allocation to either laparoscopic or conventional cholecystectomy depended on the availability of a laparoscopic set ...". |
| Prisco 2000 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Putensen‐Himmer 1992 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Rademaker 1992 | Patients underwent conventional subcostal cholecystectomy whenever the instrumentation for laparoscopic surgery was not available; the laparoscopic group had on alternating basis general anaesthesia combined with epidural analgesia or general anaesthesia alone; not randomised. |
| Redmond 1994 | Study evaluating laparoscopic and small‐incision cholecystectomy. |
| Rhodes 1996 | Not a randomised trial; comment on other article. |
| Romana 2000 | Not randomised: "patients were divided into two groups". |
| Ros 2001 | Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. |
| Rovina 1996 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Schauer 1993 | No correct randomisation of surgical techniques: ".. patients were randomly assigned to one of four general surgical services; two of these used only the open cholecystectomy technique, and the other two used the laparoscopic approach ..". |
| Schauer 1995 | Not randomised; ".. procedure was determined by the attending physician ..". |
| Schaupp 1988 | Randomised clinical trial on two types of conventional cholecystectomy (with nasogastric tube, iv infusion and subhepatic drain versus no tube, no infusion and no drain). |
| Secco 2002 | Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. |
| Srivastava 2001 | Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. |
| Tate 1993 | Randomised trial evaluating laparoscopic and small‐incision cholecystectomy. |
| Thaler 1995 | Trial on LC and OC patients, but no randomisation as the authors found that laparoscopic cholecystectomy was the method of first choice. |
| Toouli 1998 | Review on gallstones; not a randomised trial. |
| Trondsen 1993 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Ueo 1994 | Prospective comparison between IL‐6 levels in LC and OC patients, but not randomised: " ... patients who underwent cholecystectomy, 12 each for OC and LC, were chosen as subjects in this study ...". |
| Volpino 1998 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Williams 1993 | Prospective study on LC and OC pulmonary function, but not randomised: "... selection for OC or LC depended upon surgeon ...". |
| Yerdel 1997 | Prospective study in cirrhotic patients on laparoscopic versus open cholecystectomy; not randomised ( "... all cirrhotic patients were offered LC ..." ). |
| Zajac 1998 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
| Zulfikaroglu 2002 | Randomised trial evaluating laparoscopic and open cholecystectomy. |
LC: laparoscopic cholecystectomy; OC: open cholecystectomy.
Contributions of authors
F Keus: literature searches and selection, data extraction, statistical analysis, and text writing. JAF de Jong: literature selection and data extraction. HG Gooszen: text editing and supervision. CJHM van Laarhoven: data extraction, statistical analysis, text writing, and final supervision.
Sources of support
Internal sources
Department of Surgery, University Medical Center, Utrecht, Netherlands.
Department of Surgery, St. Elisabeth Hospital, Tilburg, Netherlands.
External sources
No sources of support supplied
Declarations of interest
We (FK, HG, CL) are the coordinating authors of an unpublished trial (Keus 2006), which will be published in the near future.
Edited (no change to conclusions)
References
References to studies included in this review
Assalia 1993 {published data only}
- Assalia A, Schein M, Kopelman D, Hashmonai M. Minicholecystectomy vs conventional cholecystectomy ‐ a prospective randomized trial ‐ implications in the laparoscopic era. World Journal of Surgery 1993;17(6):755‐9. [DOI] [PubMed] [Google Scholar]
Coelho 1992a {published data only}
- Coelho JC, Campos GM, Matias JE. Cholecystectomy through mini‐incision and through classic subcostal incision: a prospective randomized study [Colecistectomia por mini‐incisao subcostal classica: estudo prospectivo randomizado]. Revista Brasileira de Cirurgia 1992;82:67‐9. [Google Scholar]
Coelho 1993 {published data only}
- Coelho JCU, DeAraujo RPM, Marchesini JB, Coelho ICMM, DeAraujo LRR. Pulmonary‐function after cholecystectomy performed through Kocher incision, a mini‐incision, and laparoscopy. World Journal of Surgery 1993;17(4):544‐6. [DOI] [PubMed] [Google Scholar]
O'Dwyer 1992 {published data only}
- O'Dwyer PJ, McGregor JR, McDermott EWM, Murphy JJ, O'Higgins NJ. Patient recovery following cholecystectomy through a 6‐cm or 15‐cm transverse subcostal incision ‐ a prospective randomized clinical trial. Postgraduate Medical Journal 1992;68(804):817‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schmitz 1997 {published data only}
- Schmitz R, Rohde V, Treckmann J, Shah S. Randomized clinical trial of conventional cholecystectomy versus minicholecystectomy. British Journal of Surgery 1997;84(12):1683‐6. [PubMed] [Google Scholar]
Seenu 1994 {published data only}
- Seenu V, Misra MC. Mini‐lap cholecystectomy ‐ an attractive alternative to conventional cholecystectomy. Tropical Gatroenterology 1994;15(1):29‐31. [PubMed] [Google Scholar]
Wani 2002 {published data only}
- Wani KA, Dar HA, Malik AA, Chowdry NA. Comparison of postoperative pulmonary function tests after cholecystectomy performed through Kocher's incision and mini‐incision. International Surgery 2002;87(2):94‐8. [PubMed] [Google Scholar]
- Wani KA, Malik AA, Noor UD, Wani NA, Chowdhry N. Minicholecystectomy vs conventional cholecystectomy: a prospective study. Implications in the laparoscopic era. JK Practitioner 2000;7:30‐3. [Google Scholar]
References to studies excluded from this review
Agnifili 1993 {published data only}
- Agnifili A, Guadagni S, Ibi I, Verzaro R, Gola P, Gianfelice F, et al. Pulmonary function after laparoscopic and open cholecystectomy [abstract]. British Journal of Surgery 1993;80(Suppl):S44. [Google Scholar]
- Agnifili A, Ibi I, Guadagni S, Verzaro R, Gianfelice F, Mancini E, et al. Perioperative pain and stress: a comparison between video laparoscopic cholecystectomy and "open" cholecystectomy [Dolore e stress perioperatori: confronto tra videolaparocolecistectomia e colecistectomia 'open']. Il Giornale di Chirurgia 1993;14(7):344‐8. [PubMed] [Google Scholar]
- Agnifili A, Verzaro R, Colangeli A, Debernardinis G, Ibi I. Perioperative pulmonary‐function, pain and stress‐response after cholecystectomy performed via laparotomy or laparoscopy ‐ comparison between laparoscopy and laparotomy. Minimally Invasive Therapy & Allied Technologies 1993;2(6):283‐8. [Google Scholar]
- Ibi I, Agnifili A, Verzaro R, Carducci G, Marino M, Mancini E, et al. Respiratory function, postoperative pain and stress following videolaparocholecystectomy and traditional cholecystectomy [Funzione respiratoria, dolore e stress perioperatori dopo videolaparocolecistectomia e colecistectomia tradizionale]. Chirurgia 1994;7:97‐102. [Google Scholar]
Al Tameem 1995 {published data only}
- Al Tameem M. Mini‐laparotomy cholecystectomy: splitting versus partial and whole transection of the rectus abdominis muscle. Saudi Medical Journal 1995;16(2):113‐5. [Google Scholar]
Alexander 1997 {published data only}
- Alexander JI. Pain after laparoscopy. British Journal of Anaesthesia 1997;79(3):369‐78. [DOI] [PubMed] [Google Scholar]
Allen 2002 {published data only}
- Allen JW, Polk HC. A study of added costs of laparoscopic cholecystectomy based on surgery preference cards. American Surgeon 2002;68(5):474‐6. [PubMed] [Google Scholar]
Alponat 2002 {published data only}
- Alponat A, Cubukcu A, Gonullu N, Canturk Z, Ozbay O. Is minisite cholecystectomy less traumatic? Prospective randomized study comparing minisite and conventional laparoscopic cholecystectomies. World Journal of Surgery 2002;26(12):1437‐40. [DOI] [PubMed] [Google Scholar]
Anonymous 1995 {published data only}
- Disposables targeted to reduce lap chole cost. OR Manager 1995;11(11):14. [Google Scholar]
Assalia 1997 {published data only}
- Assalia A, Kopelman D, Hashmonai M. Emergency minilaparotomy cholecystectomy for acute cholecystitis: prospective randomized trial‐‐implications for the laparoscopic era. World Journal of Surgery 1997;21(5):534‐9. [DOI] [PubMed] [Google Scholar]
Bablekos 2003 {published data only}
- Bablekos GD, Roussou T, Rasmussen T, Vassiliou MP, Behrakis PK. Postoperative changes on pulmonary function after laparoscopic and open cholecystectomy. Hepato‐Gastroenterology 2003;50(53):1193‐200. [PubMed] [Google Scholar]
Barkun 1992 {published data only}
- Barkun JS, Barkun AN, Sampalis JS, Fried G, Taylor B, Wexler MJ, et al. Randomized controlled trial of laparoscopic versus mini cholecystectomy. Lancet 1992;340(7):1116‐9. [DOI] [PubMed] [Google Scholar]
- Barkun JS, Caro JJ, Barkun AN, Trindade E. Cost‐effectiveness of laparoscopic and mini‐cholecystectomy in a prospective randomized trial. Surgical Endoscopy 1995;9(11):1221‐4. [PubMed] [Google Scholar]
Barkun 1993 {published data only}
- Barkun JS, Barkun AN, Meakins JL, Bailar J, Battista RN, Brassard R, et al. Laparoscopic versus open cholecystectomy ‐ the Canadian experience. American Journal of Surgery 1993;165(4):455‐8. [DOI] [PubMed] [Google Scholar]
Baxter 1992 {published data only}
- Baxter JN, O'Dwyer PJ. Laparoscopic or minilaparotomy cholecystectomy?. BMJ (Clinical Research Ed.) 1992;304(6826):559‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bellon 1998 {published data only}
- Bellon JM, Manzano L, Bernardos L, Ga Honduvilla N, Larrad A, Bujan J, et al. Cytokine levels after open and laparoscopic cholecystectomy. European Surgical Research 1997;29(1):27‐34. [DOI] [PubMed] [Google Scholar]
- Bellon JM, Manzano L, Larrad A, Honduvilla GN, Bujan J, Alvarez‐Mon M. Endocrine and immune response to injury after open and laparoscopic cholecystectomy. International Surgery 1998;83(1):24‐7. [PubMed] [Google Scholar]
Berggren 1994 {published data only}
- Berggren U, Gordh T, Grama D, Haglund U, Rastad J, Arvidsson D. Laparoscopic versus open cholecystectomy ‐ hospitalization, sick leave, analgesia and trauma responses. British Journal of Surgery 1994;81(9):1362‐5. [DOI] [PubMed] [Google Scholar]
Bernard 1994 {published data only}
- Bernard A, Aho S, Charvet‐Protat S, Durieux P. Evaluation of laparoscopy in intestinal surgery and gynecological surgery and its economic implications (Three reports). Paris: Agence Nationale pour le Developpement de l'Evaluation Medicale (ANAES) 1994.
Bigard 1995 {published data only}
- Bigard MA, Bernard A, Cassan P, Deplantez J, Fagniez PL, Fortier B, et al. Indications and methods of cholecystectomy in treatment of gallstones [Indications et modalites de la cholecystectomie dans la lithiase vesiculaire]. Gastroenterologie Clinique et Biologique 1995;19(8‐9):707‐17. [PubMed] [Google Scholar]
Blanc‐Louvry 2000 {published data only}
- Blanc‐Louvry I, Coquerel A, Koning E, Maillot C, Ducrotte P. Operative stress response is reduced after laparoscopic compared to open cholecystectomy ‐ The relationship with postoperative pain and ileus. Digestive Diseases and Sciences 2000;45(9):1703‐13. [DOI] [PubMed] [Google Scholar]
Blomstedt 1972 {published data only}
- Blomstedt B, Welin‐Berger T. Incisional hernias. A comparison between midline, oblique and transrectal incisions. Acta Chirurgica Scandinavica 1972;138(3):275‐8. [PubMed] [Google Scholar]
Bolke 2000 {published data only}
- Bolke E, Jehle PM, Nothnagel B, Seidelmann M, Storck M, Orth K. A prospective randomised study on endotoxaemia, mediator release and morbidity in conventional, compared with laparoscopic cholecystectomy. Minimally Invasive Therapy & Allied Technologies 2000;9(6):387‐92. [Google Scholar]
Bruce 1999 {published data only}
- Bruce DM, Smith M, Walker CBJ, Heys SD, Binnie NR, Gough DB, et al. Minimal access surgery for cholelithiasis induces an attenuated acute phase response. American Journal of Surgery 1999;178(3):232‐4. [DOI] [PubMed] [Google Scholar]
- Walker CB, Bruce DM, Heys SD, Gough DB, Binnie NR, Eremin O. Minimal modulation of lymphocyte and natural killer cell subsets following minimal access surgery. American Journal of Surgery 1999;177(1):48‐54. [DOI] [PubMed] [Google Scholar]
Bukan 2004 {published data only}
- Bukan MH, Bukan N, Kaymakcioglu N, Tufan T. Effects of open vs. laparoscopic cholecystectomy on oxidative stress. Tohoku Journal of Experimental Medicine 2004;202(1):51‐6. [DOI] [PubMed] [Google Scholar]
Byrne 1994 {published data only}
- Byrne J, Timon D, Armstrong C, Horgan PG, Quill DS. A comparison of analgesic requirements and pulmonary‐function in open versus laparoscopic cholecystectomy. Minimally Invasive Therapy & Allied Technologies 1994;3(1):3‐6. [Google Scholar]
Calland 2001 {published data only}
- Calland JF, Tanaka K, Foley E, Bovbjerg VE, Markey DW, Blome S, et al. Outpatient laparoscopic cholecystectomy: patient outcomes after implementation of a clinical pathway. Annals of Surgery 2001;233(5):704‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Caplan 1999 {published data only}
- Caplan G, Board N, Paten A, Tazelaar MJ, Crowe P, Yap SJ, et al. Decreasing lengths of stay: the cost to the community. Australian and New Zealand Journal of Surgery 1999;69(6):433‐7. [DOI] [PubMed] [Google Scholar]
Champault 2002 {published data only}
- Champault A, Vons C, Dagher I, Amerlinck S, Franco D. Low‐cost laparoscopic cholecystectomy. British Journal of Surgery 2002;89(12):1602‐7. [DOI] [PubMed] [Google Scholar]
Charlo 1995 {published data only}
- Charlo DT, Fernandez MM, Tejido SC. A cost analysis of laparoscopic cholecystectomy compared with the open technic [Analisis de costes de la colecistectomia laparoscopica en comparacion con la abierta]. Revista Espanola de Enfermedades Digestivas 1995;87(6):449‐52. [PubMed] [Google Scholar]
Chaudhary 1999 {published data only}
- Chaudhary D, Verma GR, Gupta R, Bose SM, Ganguly NK. Comparative evaluation of the inflammatory mediators in patients undergoing laparoscopic versus conventional cholecystectomy. Australian and New Zealand Journal of Surgery 1999;69(5):369‐72. [DOI] [PubMed] [Google Scholar]
Chumillas 1998 {published data only}
- Chumillas MS, Ponce JL, Delgado F, Viciano V. Pulmonary function and complications after laparoscopic cholecystectomy. European Journal of Surgery 1998;164(6):433‐7. [DOI] [PubMed] [Google Scholar]
Clezy 1996 {published data only}
- Clezy JKA. Randomized trial of laparoscopic cholecystectomy and mini‐cholecystectomy [letter]. British Journal of Surgery 1996;83(2):279. [DOI] [PubMed] [Google Scholar]
Coelho 1992 {published data only}
- Coelho JC, Marchesini JB, Campos AC, Camargo CA, Griilo MA, Campos GM. Cholecystectomy through mini‐laparotomy [Colecistectomia por mini‐laparotomia]. Revista Brasileira de Cirurgia 1992;19:213‐5. [Google Scholar]
Coskun 2000 {published data only}
- Coskun I, Hatipoglu AR, Topaloglu A, Yoruk Y, Yalcinkaya S, Caglar T. Laparoscopic versus open cholecystectomy: effect on pulmonary function tests. Hepato‐Gastroenterology 2000;47(32):341‐2. [PubMed] [Google Scholar]
Da Costa 1995 {published data only}
- Costa ML, Qureshi MA, Brindley NM, Burke PE, Grace PA, Bouchier‐Hayes D. Normal inspiratory muscle strength is restored more rapidly after laparoscopic cholecystectomy. Annals of the Royal College of Surgeons of England 1995;77:252‐5. [PMC free article] [PubMed] [Google Scholar]
Dauleh 1995 {published data only}
- Dauleh MI, Rahman S, Townell NH. Open versus laparoscopic cholecystectomy: a comparison of postoperative temperature. Journal of the Royal College of Surgeons of Edinburgh 1995;40(2):116‐8. [PubMed] [Google Scholar]
Decker 1993 {published data only}
- Decker D, Schondorf M, Decker P, Bidlingmaier F, Hirner A, Rucker A. Evaluation of tissue trauma with the help of activation markers on the cell membrane of leukocytes. A comparison: laparoscopic versus convertional cholecystectomy. Langenbecks Archiv fur Chirurgie 1993;Suppl 1 Forumband:49‐53. [Google Scholar]
Delogu 1999 {published data only}
- Delogu G, Famularo G, Luzzi S, Rubcich P, Giardina A, Masciangelo R, et al. General anesthesia mode does not influence endocrine or immunologic profile after open or laparoscopic cholecystectomy. Surgical Laparoscopy, Endoscopy & Percutaneous Techniques 1999;9(5):326‐32. [PubMed] [Google Scholar]
Demirer 2000 {published data only}
- Demirer S, Karadayi K, Simsek S, Erverdi N, Bumin C. Comparison of postoperative acute‐phase reactants in patients who underwent laparoscopic v open cholecystectomy: a randomized study. Journal of Laparoendoscopic & Advanced Surgical Techniques ‐ Part A 2000;10(5):249‐52. [DOI] [PubMed] [Google Scholar]
Dionigi 1994 {published data only}
- Dionigi R, Dominioni L, Benevento A, Giudice G, Cuffari S, Bordone N, et al. Effects of surgical trauma of laparoscopic vs open cholecystectomy. Hepato‐Gastroenterology 1994;41(5):471‐6. [PubMed] [Google Scholar]
- Dominioni L, Benevento A, Carcano G, Chiappa A, Dionigi R. Acute‐phase response after laparoscopic and open cholecystectomy [abstract]. British Journal of Surgery 1993;80:S44. [Google Scholar]
Dohrmann 1993 {published data only}
- Dohrmann A, Richthammer M, Jochims J, Stremmel W. Postoperative changes in pulmonary function after laparoscopic versus conventional cholecystectomy ‐ a prospective study [Postoperative Veranderungen der Lungenfunktion nach Laparoskopischer versus konventioneller Cholezystektomie ‐ eine prospektive Studie]. Minimal Invasive Chirurgie 1993;2(Suppl 1):19‐20. [Google Scholar]
Eickhoff 1997 {published data only}
- Eickhoff H, Milheiro A, Manso LC, Castro‐Sousa F. Alterations in respiratory function after cholecystectomy‐‐open versus laparoscopic cholecystectomy [Veranderungen der Lungenfunktion nach Cholezystektomie ‐ offene versus laparoskopische Cholezystektomie]. Langenbecks Archiv fur Chirurgie, Suppl II (Kongressbericht 1997) 1997;114:1105‐7. [PubMed] [Google Scholar]
Engin 1998 {published data only}
- Engin A, Bozkurt S, Ersoy E, Oguz M, Gokcora N. Stress hyperglycemia in minimally invasive surgery. Surgical Laparoscopy & Endoscopy 1998;8(6):435‐7. [PubMed] [Google Scholar]
Essen 1995 {published data only}
- Essen P, Thorell A, McNurlan MA, Anderson S, Ljungqvist O, Wernerman J, et al. Laparoscopic cholecystectomy does not prevent the postoperative protein catabolic response in muscle. Annals of Surgery 1995;222:36‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Frazee 1991 {published data only}
- Frazee RC, Roberts JW, Okeson GC, Symmonds RE, Snyder SK, Hendricks JC, et al. Open versus laparoscopic cholecystectomy. A comparison of postoperative pulmonary function. Annals of Surgery 1991;213:651‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gal 1997 {published data only}
- Gal I, Roth E, Lantos J, Varga G, Jaberansari MT. Inflammatory mediators and surgical trauma regarding laparoscopic access: free radical mediated reactions. Acta Chirurgica Hungarica 1997;36:97‐9. [PubMed] [Google Scholar]
Galizia 2001 {published data only}
- Galizia G, Prizio G, Lieto E, Castellano P, Pelosio L, Imperatore V, et al. Hemodynamic and pulmonary changes during open, carbon dioxide pneumoperitoneum, and abdominal wall‐lifting cholecystectomy ‐ A prospective, randomized study. Surgical Endoscopy 2001;15(5):477‐83. [DOI] [PubMed] [Google Scholar]
GarciaCaballero 1993 {published data only}
- Garcia‐Caballero M, Vara‐Thorbeck C. The evolution of postoperative ileus after laparoscopic cholecystectomy ‐ a comparative study with conventional cholecystectomy and sympathetic blockade treatment. Surgical Endoscopy 1993;7(5):416‐9. [DOI] [PubMed] [Google Scholar]
Glaser 1995 {published data only}
- Glaser F, Kuntz C, Klee F, Buhr HJ, Sannwald G, Herfarth C. General stress response to conventional and laparoscopic cholecystectomy. Langenbecks Archiv fur Chirurgie 1993;Suppl 1 Forumband:45‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser F, Sannwald GA, Buhr HJ, Kuntz C, Mayer H, Klee F, et al. General stress response to conventional and laparoscopic cholecystectomy. Annals of Surgery 1995;221(4):372‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Go 1995 {published data only}
- Go PMNYH, Stolk MFJ, Obertop H, Dirksen C, Elst DH, Ament A, et al. Symptomatic gallbladder stones: cost‐effectiveness of treatment with extracorporeal shock‐wave lithotripsy, conventional and laparoscopic cholecystectomy. Surgical Endoscopy 1995;9(1):37‐41. [DOI] [PubMed] [Google Scholar]
Grande 2002 {published data only}
- Grande M, Tucci GF, Adorisio O, Barini A, Rulli F, Neri A, et al. Systemic acute‐phase response after laparoscopic and open cholecystectomy. Surgical Endoscopy 2002;16(2):313‐6. [DOI] [PubMed] [Google Scholar]
Hagmuller 1997 {published data only}
- Hagmuller E, Lorenz D, Gunther HJ, Rumstadt B, Jentschura D. Comparison of catabolic response in muscle after laparoscopic cholecystectomy or conventional cholecystectomy using a 13C‐leucine tracer model [Untersuchungen zum Ausmass der postoperativen Katabolie nach laparoskopischer und konventioneller Cholecystektomie unter Anwendung eines 13C‐leuzin‐tracermodells]. Langenbecks Archiv fur Chirurgie 1997;I Forumband:241‐5. [Google Scholar]
Hasukic 2002 {published data only}
- Hasukic S, Mesic D, Dizdarevic E, Keser D, Hadziselimovic S, Bazardzanovic M. Pulmonary function after laparoscopic and open cholecystectomy. Surgical Endoscopy 2002;16(1):163‐5. [DOI] [PubMed] [Google Scholar]
Hauer‐Jensen 1986 {published data only}
- Hauer‐Jensen M, Karesen R, Nygaard K, Solheim K, Amlie E, Havig O, et al. Consequences of routine peroperative cholangiography during cholecystectomy for gallstone disease: a prospective, randomized study. World Journal of Surgery 1986;10(6):996‐1002. [DOI] [PubMed] [Google Scholar]
Hendolin 2000 {published data only}
- Hendolin HI, Paakkonen ME, Alhava EM, Tarvainen R, Kemppinen T, Lahtinen P. Laparoscopic or open cholecystectomy: a prospective randomised trial to compare postoperative pain, pulmonary function, and stress response. European Journal of Surgery 2000;166(5):394‐9. [DOI] [PubMed] [Google Scholar]
Hobbs 1995 {published data only}
- Hobbs KEF. Laparoscopic cholecystectomy. Gut 1995;36(2):161‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huang 1996 {published data only}
- Huang SM, Wu CW, Lui WY, Peng FK. A prospective randomised study of laparoscopic v. open cholecystectomy in aged patients with cholecystolithiasis. South African Journal of Surgery 1996;34(4):177‐9. [PubMed] [Google Scholar]
Huguier 1997 {published data only}
- Huguier M. Laparoscopic digestive surgery. Hepato‐Gastroenterology 1997;44(13):2‐3. [PubMed] [Google Scholar]
Hunter 2001 {published data only}
- Hunter JG. Clinical trials and the development of laparoscopic surgery. Surgical Endoscopy 2001;15(1):1‐3. [DOI] [PubMed] [Google Scholar]
Iwase 1992 {published data only}
- Iwase K, Takenaka H, Yagura A, Ishizaka T, Takagaki M, Ohata T, et al. Changes of hemodynamic parameters and urine output during laparoscopic cholecystectomy ‐ compared with mini‐laparotomy cholecystectomy: preliminary report. Nippon Geka Gakkai Zasshi 1992;93(6):663. [PubMed] [Google Scholar]
Jan 1993 {published data only}
- Jan YY, Chen MF. Laparoscopic versus open cholecystectomy: a prospective randomized study. Journal of the Formosan Medical Association 1993;92(Suppl 4):S243‐S249. [PubMed] [Google Scholar]
Johnson 1997 {published data only}
- Johnson A. Laparoscopic surgery. Lancet 1997;349(9052):631‐5. [DOI] [PubMed] [Google Scholar]
- Johnson A. Laparoscopic surgery ... reproduced by kind permission of the Lancet (Johnson A 1997 Laparoscopic Surgery. Lancet (349) 636‐41). British Journal of Theatre Nursing 1999;9(3):119‐24. [PubMed] [Google Scholar]
Johnson 1998 {published data only}
- Johnson AG. New interventional procedures: efficacy, safety and training. Australian and New Zealand Journal of Surgery 1998;68(1):3‐5. [DOI] [PubMed] [Google Scholar]
Johnson 1998a {published data only}
- Johnson AG, Majeed AW. Randomized clinical trial of conventional cholecystectomy versus minicholecystectomy [letter]. British Journal of Surgery 1998;85(7):1017‐8. [PubMed] [Google Scholar]
Karayiannakis 1997 {published data only}
- Karayiannakis AJ, Makri GG, Mantzioka A, Karousos D, Karatzas G. Postoperative pulmonary function after laparoscopic and open cholecystectomy. British Journal of Anaesthesia 1996;77(4):448‐52. [DOI] [PubMed] [Google Scholar]
- Karayiannakis AJ, Makri GG, Mantzioka A, Karousos D, Karatzas G. Systemic stress response after laparoscopic or open cholecystectomy: a randomized trial. British Journal of Surgery 1997;84(4):467‐1. [PubMed] [Google Scholar]
Karayiannakis 2002 {published data only}
- Karayiannakis AJ, Syrigos KN, Savva A, Polychronidis A, Karatzas G, Simopoulos C. Serum E‐cadherin concentrations and their response during laparoscopic and open cholecystectomy. Surgical Endoscopy 2002;16(11):1551‐4. [DOI] [PubMed] [Google Scholar]
Kehlet 1993 {published data only}
- Kehlet H. Treatment of gallstones ‐ lithotripsy, classical, mini or laparoscopic cholecystectomy? [Behandling af galdeblaeresten ‐ litotripsi, klassisk, mini‐ eller laparoskopisk kolecystektomi?]. Ugeskrift for Laeger 1993;155(11):816‐7. [PubMed] [Google Scholar]
Keus 2006 {unpublished data only}
- Keus E, Laarhoven CJHM. Small‐incision versus laparoscopic cholecystectomy: blind RCT. Unpublished data.
Kiviluoto 1997 {published data only}
- Kiviluoto T, Siren J, Luukkonen P, Kivilaakso E. Laparoscopic vs. open cholecystectomy for acute cholecystitis. A prospective randomized study. Gastroenterology 1997;112(4):A1452. [Google Scholar]
Kjaersgaard 1994 {published data only}
- Kjaersgaard P, Reiertsen O, Trondsen E, Rosseland AR, Larsen S. Comparison of sequential and fixed‐sample designs in a controlled clinical trial with laparoscopic versus conventional cholecystectomy. Scandinavian Journal of Gastroenterology 1994;29(9):854‐8. [DOI] [PubMed] [Google Scholar]
Koprulu 1996 {published data only}
- Koprulu G, Esen F, Pembeci K, Denkel T. Pulmonary mechanics during laparoscopic surgery. Advances in Experimental Medicine and Biolology 1996;388:643‐6. [DOI] [PubMed] [Google Scholar]
Krasinski 1998 {published data only}
- Krasinski Z, Gabriel M, Oszkinis G, Dzieciuchowicz L, Begier‐Krasinska B. Thrombophlebitis profunda in patients after conventional and laparoscopic cholecystectomy [Trombophlebitis profunda bei Patienten nach der konventionellen und laparoskopischen Gallenblasenentfernung]. Langenbecks Archiv fur Chirurgie 1998;115(Supp lI Kongressbericht):1105‐6. [PubMed] [Google Scholar]
Krawczyk 1993 {published data only}
- Krawczyk M, Zieniewicz K, Najnigier B, Patkowski W, Nyckowski P. Laparoscopic versus open cholecystectomy [abstract]. British Journal of Surgery 1993;80(Suppl):S46. [Google Scholar]
Kunz 1992 {published data only}
- Kunz R. Laparoscopic versus mini‐lap‐cholecystectomy. Results of a prospective randomized study [Cholezystektomie ‐ laparoskopische versus mini‐lap‐Cholezystektomie. Ergebnisse einer prospektiv randomisierten Studie]. Langenbecks Archiv fur Chirurgie 1993;Suppl Kongressbericht:84‐8. [PubMed] [Google Scholar]
- Kunz R, Berger R, Beger HG. Laparoscopic versus conventional cholecystectomy [Laparoskopische versus konventionelle Cholezystektomie]. Minimal Invasive Chirurgie 1993;2(Suppl 1):2. [Google Scholar]
- Kunz R, Orth K, Vogel J, Steinacker JM, Meitinger A, Bruckner U, et al. Laparoscopic cholecystectomy versus mini‐lap cholecystectomy ‐ results of a prospective randomized study [Laparoskopische Cholecystektomie versus mini‐lap‐Cholecystektomie ‐ Ergebnisse einer prospektiven, randomisierten Studie]. Chirurg 1992;63(4):291‐5. [PubMed] [Google Scholar]
- Schutze F, Osswald C, Berger D, Kunz R, Beger HG. Peri‐ and postoperative mediator release: laparoscopic versus laparotomic cholecystectomy [Peri‐ und postoperative Mediatorenfreisetzung: laparoskopische versus laparotomische Cholecystektomie]. Langenbecks Archiv fur Chirurgie 1993;Suppl 1 Forumband:55‐8. [Google Scholar]
Kurzawinski 1992 {published data only}
- Kurzawinski T, Hayter B, Tate J, Davidson B, Hobbs KEF. The cost implications of laparoscopic vs open cholecystectomy [abstract]. Gut 1992;33:S64. [Google Scholar]
Lam 1996 {published data only}
- Lam CM, Murray FE, Cuschieri A. Increased cholecystectomy rate after the introduction of laparoscopic cholecystectomy in Scotland. Gut 1996;38(2):282‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lausten 1999 (1) {published data only}
- Lausten SB, Sefi T, Marwan I, Ibrahim TM, Jensen LS, Grofte T, et al. Postoperative hepatic catabolic stress response in patients with cirrhosis and chronic hepatitis. World Journal of Surgery 2000;24(3):365‐71. [DOI] [PubMed] [Google Scholar]
- Lausten SB, Ibrahim TM, Sefi T, Jensen LS, Gesser B, Larsen CG, et al. Systemic and cell‐mediated immune response after laparoscopic and open cholecystectomy in patients with chronic liver disease ‐ A randomized, prospective study. Digestive Surgery 1999;16(6):471‐7. [DOI] [PubMed] [Google Scholar]
Lausten 1999 (2) {published data only}
- Lausten SB, Sefi T, Marwan I, Ibrahim TM, Jensen LS, Grofte T, et al. Postoperative hepatic catabolic stress response in patients with cirrhosis and chronic hepatitis. World Journal of Surgery 2000;24(3):365‐71. [DOI] [PubMed] [Google Scholar]
- Lausten SB, Ibrahim TM, Sefi T, Jensen LS, Gesser B, Larsen CG, et al. Systemic and cell‐mediated immune response after laparoscopic and open cholecystectomy in patients with chronic liver disease ‐ A randomized, prospective study. Digestive Surgery 1999;16(6):471‐7. [DOI] [PubMed] [Google Scholar]
Lujan 1998 {published data only}
- Lujan JA, Sanchez‐Bueno F, Parrilla P, Robles R, Torralba JA, Gonzalez‐Costea R. Laparoscopic vs. open cholecystectomy in patients aged 65 and older. Surgical Laparoscopy & Endoscopy 1998;8(3):208‐10. [PubMed] [Google Scholar]
Lukichev 1983 {published data only}
- Lukichev OD, Filimonov MI, Zybin IM. A method of laparoscopic cholecystostomy [Metodika laparoskopicheskoi kholetsistostomii]. Khirurgiia 1983;8:125‐7. [PubMed] [Google Scholar]
Luo 2003 {published data only}
- Luo K, Li J, Li L, Wang G, Sun J, Wu S. Operative stress response and energy metabolism after laparoscopic cholecystectomy and open cholecystectomy. Zhonghua Wai Ke Za Zhi [Chinese Journal of Surgery] 2002;40(12):923‐6. [PubMed] [Google Scholar]
- Luo K, Li JS, Li LT, Wang KH, Shun JM. Operative stress response and energy metabolism after laparoscopic cholecystectomy compared to open surgery. World Journal of Gastroenterology 2003;9(4):847‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Majeed 1996 {published data only}
- Calvert NW, Troy GP, Johnson AG. Laparoscopic cholecystectomy: a good buy? A cost comparison with small‐incision (mini) cholecystectomy. European Journal of Surgery 2000;166(10):782‐6. [DOI] [PubMed] [Google Scholar]
- Majeed AW, Troy G, Nicholl JP, Smythe A, Reed MWR, Stoddard CJ, et al. Randomised, prospective, single‐blind comparison of laparoscopic versus small‐incision cholecystectomy. Lancet 1996;347(9007):989‐94. [DOI] [PubMed] [Google Scholar]
- Squirrell DM, Majeed AW, Troy G, Peacock JE, Nicholl JP, Johnson AG. A randomized, prospective, blinded comparison of postoperative pain, metabolic response, and perceived health after laparoscopic and small incision cholecystectomy. Surgery 1998;123(5):485‐95. [DOI] [PubMed] [Google Scholar]
Makinen 1995 {published data only}
- Makinen AMH, Nordback IH. Cholecystectomy ‐ comparison of minilaparotomy and laparoscopy. International Surgery 1995;80(2):99‐101. [PubMed] [Google Scholar]
Malaysian HTA 2005 {published data only}
- Malaysian Health Technology Assessment Unit (MHTAU). Minimal access surgery. Kuala Lumpur: Malaysian Health Technology Assessment Unit (MHTAU) 2003.
Maruszynski 1995 {published data only}
- Maruszynski M, Pojda Z. Interleukin 6 (IL‐6) levels in the monitoring of surgical trauma. A comparison of serum IL‐6 concentrations in patients treated by cholecystectomy via laparotomy or laparoscopy. Surgical Endoscopy 1995;9(8):882‐5. [DOI] [PubMed] [Google Scholar]
Matsunaga 1996 {published data only}
- Matsunaga MA. Postoperativepain relief and epidural analgesia for open cholecystectomy, laparoscopic cholecystectomy, and gastrectomy. Anesthesia and Resuscitation 1996;32:257‐61. [Google Scholar]
McGinn 1995 {published data only}
- Faux JW, Terzi C, McGinn FP. Prospective randomized trial of mini‐cholecystectomy versus laparoscopic cholecystectomy: a single surgeon study. British Journal of Surgery 1998;85(suppl 1):77. [Google Scholar]
- McGinn FP, Miles AJG, Uglow M, Ozmen M, Terzi C, Humby M. Randomized trial of laparoscopic cholecystectomy and mini‐cholecystectomy. British Journal of Surgery 1995;82(10):1374‐7. [DOI] [PubMed] [Google Scholar]
McKellar 1995 {published data only}
- McKellar DP, Johnson RM, Dutro JA, Mellinger JB, Peoples JB. Cost‐effectiveness of laparoscopic cholecystectomy. Surgical Endoscopy 1995;9(2):158‐63. [DOI] [PubMed] [Google Scholar]
McMahon 1994 {published data only}
- McMahon AJ, Baxter JN, Anderson JR, Ramsay G, Galloway D, Russell IT, et al. Assessment of pain after laparoscopic cholecystectomy and minicholecystectomy [abstract]. British Journal of Surgery 1992;79(11):1224. [Google Scholar]
- McMahon AJ, Baxter JN, Anderson JR, Ramsay G, Galloway D, Sunderland G, et al. Pain and pulmonary‐function after laparoscopic and mini‐cholecystectomy ‐ a randomized trial [abstract]. Gastroenterology 1993;104(4):A370. [Google Scholar]
- McMahon AJ, Baxter JN, Anderson JR, Ramsay G, Galloway D, Sunderland G, et al. Postoperative pain and analgesia requirement after laparoscopic and mini‐cholecystectomy ‐ a prospective randomized trial [abstract]. Gut 1992;33(2):S63. [Google Scholar]
- McMahon AJ, Baxter JN, Kenny G, O'Dwyer PJ. Ventilatory and blood‐gas changes during laparoscopic and open cholecystectomy. British Journal of Surgery 1993;80(10):1252‐4. [DOI] [PubMed] [Google Scholar]
- McMahon AJ, Baxter JN, Kenny G, O'Dwyer PJ. Ventilatory changes during laparoscopic and open cholecystectomy: a randomized trial [abstract]. British Journal of Surgery 1993;80(5):647. [DOI] [PubMed] [Google Scholar]
- McMahon AJ, O'Dwyer PJ, Cruikshank A, McMillan D, Lowe G, Rumley A, et al. Metabolic changes after laparoscopic and minilaparoscopic cholecystectomy: a randomized trial [abstract]. British Journal of Surgery 1993;80(5):641. [Google Scholar]
- McMahon AJ, O'Dwyer PJ, Cruikshank AM, McMillan DC, O'Reilly DSJ, Lowe GDO, et al. Comparison of metabolic responses to laparoscopic and minilaparotomy cholecystectomy. British Journal of Surgery 1993;80(10):1255‐8. [DOI] [PubMed] [Google Scholar]
- McMahon AJ, Ross S, Baxter JN, Russell IT, Anderson JR, Morran CG, et al. Symptomatic outcome 1 year after laparoscopic and minilaparotomy cholecystectomy ‐ a randomized trial. British Journal of Surgery 1995;82(10):1378‐82. [DOI] [PubMed] [Google Scholar]
- McMahon AJ, Ross S, Russell IT, Baxter JN, Anderson JR, Morran C, et al. Return to normal activity after laparoscopic and mini‐cholecystectomy: a randomised trial [abstract]. Gut 1993;34:S68. [Google Scholar]
- McMahon AJ, Ross S, Russell IT, Baxter JN, Anderson JR, Ramsay G, et al. Return to normal activity after laparoscopic and mini‐cholecystectomy ‐ a randomized trial [abstract]. Gastroenterology 1993;104(4):A370. [Google Scholar]
- McMahon AJ, Russell IT, Baxter JN, O'Dwyer PJ. Comparison of the cost of laparoscopic and mini‐cholecystectomy: a randomised trial [abstract]. Gut 1993;34:S68. [Google Scholar]
- McMahon AJ, Russell IT, Baxter JN, Ross S, Anderson JR, Morran CG, et al. Laparoscopic versus minilaparotomy cholecystectomy ‐ a randomized trial. Lancet 1994;343(8890):135‐8. [DOI] [PubMed] [Google Scholar]
- McMahon AJ, Russell IT, Ramsay G, Sunderland G, Baxter JN, Anderson JR, et al. Laparoscopic and minilaparotomy cholecystectomy ‐ a randomized trial comparing postoperative pain and pulmonary‐function. Surgery 1994;115(5):533‐9. [PubMed] [Google Scholar]
McMahon 1996 {published data only}
- McMahon AJ, O'Dwyer PJ, Baxter JN. Randomised trial of laparoscopic versus small‐incision cholecystectomy [letter]. Lancet 1996;347(9015):1622. [PubMed] [Google Scholar]
Mealy 1992 {published data only}
- Mealy K, Gallagher H. Comparison of the physiological responses to open and laparoscopic cholecystectomy [abstract]. Irish Journal of Medical Science 1992;161:92. [Google Scholar]
- Mealy K, Gallagher H, Barry M, Lennon F, Traynor O, Hyland J. Physiological and metabolic responses to open and laparoscopic cholecystectomy. British Journal of Surgery 1992;79:1061‐4. [DOI] [PubMed] [Google Scholar]
Milheiro 1994 {published data only}
- Milheiro A, Sousa FC, Manso EC, Leitao F. Metabolic responses to cholecystectomy ‐ open vs laparoscopic approach. Journal of Laparoendoscopic Surgery 1994;4(5):311‐7. [DOI] [PubMed] [Google Scholar]
Mimica 2000 {published data only}
- Mimica Z, Biocic M, Bacic A, Banovic I, Tocilj J, Radonic V, et al. Laparoscopic and laparotomic cholecystectomy: a randomized trial comparing postoperative respiratory function. Respiration 2000;67(2):153‐8. [DOI] [PubMed] [Google Scholar]
Mrksic 2001 {published data only}
- Mrksic M, Cabafi Z, Feher I, Mirkovic M. Operative trauma during laparoscopic and open cholecystectomy [Operativna trauma pri laparoskopskoj i klasicnoj holecistektomiji]. Medicinski Pregled 2001;54(7‐8):327‐31. [PubMed] [Google Scholar]
Novitsky 2002 {published data only}
- Novitsky YW, Czerniach DR, Perugini RA, Yood SM, Kercher KW, Gallagher KA, et al. Prospective randomized trial of mini‐port vs conventional laparoscopic cholecystectomy [abstract]. Gastroenterology 2002;123(1):24. [Google Scholar]
Ogawa 2001 {published data only}
- Ogawa T, Shimizu S, Mizumoto K, Uchiyama A, Yokohata K, Chijiiwa K, et al. Comparison of laparoscopic versus open cholecystectomy in patients with cardiac valve replacement. Journal of Hepato‐Biliary‐Pancreatic Surgery 2001;8(2):158‐60. [DOI] [PubMed] [Google Scholar]
Olsen 1993 {published data only}
- Olsen DO. Mini‐lap cholecystectomy. American Journal of Surgery 1993;165(4):440‐3. [DOI] [PubMed] [Google Scholar]
Ortega 1996 {published data only}
- Ortega AE, Peters JH, Incarbone R, Estrada L, Ehsan A, Kwan Y, et al. A prospective randomized comparison of the metabolic and stress hormonal responses of laparoscopic and open cholecystectomy. Journal of the American College of Surgeons 1996;183(3):249‐56. [PubMed] [Google Scholar]
Plaisier 1995 {published data only}
- Plaisier PW, Hul RL, Nijs HGT, Toom R, Terpstra OT, Bruining HA. Quality of life and the course of biliary and gastrointestinal symptoms after laparoscopic and conventional cholecystectomy. Digestive Surgery 1995;12:87‐91. [Google Scholar]
Prisco 2000 {published data only}
- Prisco D, Gaudio AR, Carla R, Gori AM, Fedi S, Cella AP, et al. Videolaparoscopic cholecystectomy induces a hemostasis activation of lower grade than does open surgery. Surgical Endoscopy 2000;14(2):170‐4. [DOI] [PubMed] [Google Scholar]
Putensen‐Himmer 1992 {published data only}
- Putensen‐Himmer G, Putensen C, Lammer H, Lingnau W, Aigner F, Benzer H. Comparison of postoperative respiratory function after laparoscopy or open laparotomy for cholecystectomy. Anesthesiology 1992;77(4):675‐80. [DOI] [PubMed] [Google Scholar]
Rademaker 1992 {published data only}
- Rademaker BM, Ringers J, Odoom JA, Wit LT, Kalkman CJ, Oosting J. Pulmonary function and stress response after laparoscopic cholecystectomy: comparison with subcostal incision and influence of thoracic epidural analgesia. Anesthesia and Analgesia 1992;75(3):381‐5. [DOI] [PubMed] [Google Scholar]
Redmond 1994 {published data only}
- Redmond HP, Watson RWG, Houghton T, Condron C, Watson RGK, Bouchier‐Hayes D. Immune function in patients undergoing open vs laparoscopic cholecystectomy. Archives of Surgery 1994;129(12):1240‐6. [DOI] [PubMed] [Google Scholar]
Rhodes 1996 {published data only}
- Rhodes MG, Gompertz H, Armstrong K, Lennard T, Rees B. Randomised trial of laparoscopic versus small‐incision cholecystectomy [letter]. Lancet 1996;347(9015):1621‐2. [PubMed] [Google Scholar]
Romana 2000 {published data only}
- Romana K, Avgoustatou K, Paparizou N, Korolanoglou D, Galanaki E, Karamichali E. Neuroendocrine responses to laparoscopic and open cholecystectomy [abstract]. European Journal of Anaesthesiology 2000;17:43. [Google Scholar]
Ros 2001 {published data only}
- Nilsson E, Ros A, Rahmqvist M, Backman K, Carlsson P. Cholecystectomy: costs and health‐related quality of life: a comparison of two techniques. International Journal for Quality in Health Care 2004;16(6):473‐82. [DOI] [PubMed] [Google Scholar]
- Ros A, Gustafsson L, Krook H, Nordgren CE, Thorell A, Wallin G, et al. Laparoscopic cholecystectomy versus mini‐laparotomy cholecystectomy: a prospective, randomized, single‐blind study. Annals of Surgery 2001;234(6):741‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rovina 1996 {published data only}
- Rovina N, Bouros D, Tzanakis N, Velegrakis M, Kandilakis S, Vlasserou F, et al. Effects of laparoscopic cholecystectomy on global respiratory muscle strength. American Journal of Respiratory and Critical Care Medicine 1996;153(1):458‐61. [DOI] [PubMed] [Google Scholar]
Schauer 1993 {published data only}
- Schauer PR, Luna J, Ghiatas AA, Glen ME, Warren JM, Sirinek KR. Pulmonary function after laparoscopic cholecystectomy. Surgery 1993;114(2):389‐97. [DOI] [PubMed] [Google Scholar]
Schauer 1995 {published data only}
- Schauer PR, Sirinek KR. The laparoscopic approach reduces the endocrine response to elective cholecystectomy. American Surgeon 1995;61(2):106‐11. [PubMed] [Google Scholar]
Schaupp 1988 {published data only}
- Schaupp W, Menges HW, Schworm HD. The ideal cholecystectomy ‐ a prospective randomized study [Die 'ideale' Cholecystektomie ‐ eine prospektive, randomisierte Studie]. Chirurg 1988;59(10):661‐4. [PubMed] [Google Scholar]
- Schaupp W, Menges HW, Trede M. The 'ideal' cholecystectomy: a prospective randomized study. Langenbecks Archiv fur Chirurgie 1987;372(Kongressbericht):839. [DOI] [PubMed] [Google Scholar]
Secco 2002 {published data only}
- Secco GB, Cataletti M, Bonfante P, Baldi E, Davini MD, Biasotti B, et al. Laparoscopic versus mini‐cholecystectomy: analysis of hospital costs and social costs in a prospective randomized study [Video‐colecistectomia versus mini‐colecistectomia: analisi dei costi ospedalieri e dei costi sociali in uno studio prospettico randomizzato]. Chirurgia Italiana 2002;54(5):685‐92. [PubMed] [Google Scholar]
Srivastava 2001 {published data only}
- Srinivas G, Srivastava A, Misra MC, Pandav CS. Cost‐effectiveness analysis: laparoscopic versus minilaparotomy cholecystectomy for gallstone disease [abstract]. Clinical Economics 1998;51(Suppl 1):33S. [PubMed] [Google Scholar]
- Srivastava A, Srinivas G, Misra MC, Pandav CS, Seenu V, Goyal A. Cost‐effectiveness analysis of laparoscopic versus minilaparotomy cholecystectomy for gallstone disease ‐ A randomized trial. International Journal of Technology Assessment in Health Care 2001;17(4):497‐502. [PubMed] [Google Scholar]
Tate 1993 {published data only}
- Tate JJ, Lau WY, Leung KL, Li AK. Laparoscopic versus mini‐incision cholecystectomy. Lancet 1993;341(8854):1214‐5. [PubMed] [Google Scholar]
Thaler 1995 {published data only}
- Thaler W, Frey L, Messmer K, Marzoli GP. Assessment of splanchnic blood flow by gastric tonometry in patients undergoing laparoscopic and open cholecystectomy. Langenbecks Archiv fur Chirurgie 1995;Suppl 1 Forumband:23‐6. [Google Scholar]
Toouli 1998 {published data only}
- Toouli J, Wright TA. Gastroenterology ‐ 5. Gallstones. Medical Journal of Australia 1998;169(3):166‐71. [DOI] [PubMed] [Google Scholar]
Trondsen 1993 {published data only}
- Trondsen E, Reiertsen O, Andersen OK, Kjaersgaard P. Laparoscopic and open cholecystectomy ‐ a prospective, randomized study. European Journal of Surgery 1993;159(4):217‐21. [PubMed] [Google Scholar]
Ueo 1994 {published data only}
- Ueo H, Honda M, Adachi M, Inoue H, Nakashima H, Arinaga S, et al. Minimal increase in serum interleukin‐6 levels during laparoscopic cholecystectomy. American Journal of Surgery 1994;168:358‐60. [DOI] [PubMed] [Google Scholar]
Volpino 1998 {published data only}
- Volpino P, Cangemi V, D'Andrea N, Cangemi B, Piat G. Hemodynamic and pulmonary changes during and after laparoscopic cholecystectomy. A comparison with traditional surgery. Surgical Endoscopy 1998;12(2):119‐23. [DOI] [PubMed] [Google Scholar]
Williams 1993 {published data only}
- Williams MD, Sulentich SM, Murr PC. Laparoscopic cholecystectomy produces less postoperative restriction of pulmonary function than open cholecystectomy. Surgical Endoscopy 1993;7(6):489‐92. [DOI] [PubMed] [Google Scholar]
Yerdel 1997 {published data only}
- Yerdel MA, Koksoy C, Aras N, Orita K. Laparoscopic versus open cholecystectomy in cirrhotic patients: a prospective study. Surgical Laparoscopy & Endoscopy 1997;7(6):483‐6. [PubMed] [Google Scholar]
Zajac 1998 {published data only}
- Zajac M, Zajac K, Engel Z. Laparoscopy vs laparotomy for cholecystectomy in elderly patients [abstract]. British Journal of Anaesthesia 1998;80(Suppl 1):2. [Google Scholar]
Zulfikaroglu 2002 {published data only}
- Zulfikaroglu B, Koc M, Soran A, Isman FK, Cinel I. Evaluation of oxidative stress in laparoscopic cholecystectomy. Surgery Today 2002;32(10):869‐74. [DOI] [PubMed] [Google Scholar]
Additional references
Assmann 2000
- Assmann SF, Pocock SJ, Enos LE, Kasten LE. Subgroup analysis and other (mis)uses of baseline data in clinical trials. Lancet 2000;355:1064‐9. [DOI] [PubMed] [Google Scholar]
Begg 1994
- Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50(4):1088‐101. [PubMed] [Google Scholar]
DeMets 1987
- DeMets DL. Methods of combining randomized clinical trials: strengths and limitations. Statistics in Medicine 1987;6(3):341‐50. [DOI] [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7(3):177‐88. [DOI] [PubMed] [Google Scholar]
Dubois 1982
- Dubois F, Berthelot B. [Cholecystectomy through minimal incision (author's translation)]. Nouvelle Presse Medicale 1982;11(15):1139‐41. [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta‐analysis detected by a simple graphical test. BMJ (Clinical Research Ed.) 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Egger 2003
- Egger M, Davey SG, Schneider M, Binder C. Bias in meta‐analysis detected by a simple, graphical test. Health Technology Assessment 2003;7(1):1‐76. [Google Scholar]
Goco 1983
- Goco IR, Chambers LG. "Mini‐cholecystectomy" and operative cholangiography. A means of cost containment. American Surgeon 1983;49(3):143‐5. [PubMed] [Google Scholar]
Higgins 2002
- Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21:1539‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2005
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5 [updated May 2005]. The Cochrane Library, Issue 3. Chichester, UK: John Wiley & Sons, Ltd, 2005. [Google Scholar]
Jüni 2001
- Jüni P, Altman DG, Egger M. Systematic reviews in health care: assessing the quality of controlled clinical trials. BMJ (Clinical Research Ed.) 2001;323(7303):42‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Keus 2004
- Keus, HG Gooszen, I van der Tweel, CJHM van Laarhoven. Laparoscopic, small‐incision, or open cholecystectomy for patients with symptomatic cholecystolithiasis. The Cochrane Database of Systematic Reviews 2004, Issue 2. Art. No.: CD004788. DOI: 10.1002/14651858.CD004788. [DOI] [PMC free article] [PubMed]
Kjaergard 2001
- Kjaergard LL, Villumsen J, Gluud C. Reported methodological quality and discrepancies between large and small randomised trials in meta‐analyses. Annals of Internal Medicine 2001;135(11):982‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Legorreta 1993
- Legorreta AP, Silber JH, Costantino GN, Kobylinski RW, Zatz SL. Increased cholecystectomy rate after the introduction of laparoscopic cholecystectomy. Journal of the American Medical Association 1993;270(12):1429‐32. [PubMed] [Google Scholar]
Macaskill 2001
- Macaskill P, Walter SD, Irwig L. A comparison of methods to detect publication bias in meta‐analysis. Statistics in Medicine 2001;20:641‐54. [DOI] [PubMed] [Google Scholar]
Moher 1998
- Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta‐analyses. Lancet 1998;352(9128):609‐13. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mühe 1986
- Mühe E. The first cholecystectomy through the laparoscope [Die erste Cholecystektomie durch das Laparoskop]. Langenbecks Archiv für Chirurgie 1986;369:804. [Google Scholar]
NIH Consensus 1993
- NIH Consensus Development Panel on Gallstones and Laparoscopic Cholecystectomy. Journal of the American Medical Association 1993;269(8):1018‐24. [MEDLINE: ] [Google Scholar]
Olsen 1991
- Olsen DO. Laparoscopic cholecystectomy. American Journal of Surgery 1991;161:339‐44. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
RevMan 2003 [Computer program]
- Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 4.2 for Windows. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2003.
Roslyn 1993
- Roslyn JJ, Binns GS, Hughes EFX, Saunders‐Kirkwood K, Zinner MJ, Cates JA. Open cholecystectomy. A contemporary analysis of 42474 patients. Annals of Surgery 1993;218(2):129‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schmitz 1997a
- Schmitz R, Rohde V, Treckman J, Shah S. Randomized trial of conventional cholecystectomy versus minicholecystectomy. British Journal of Surgery 1997;84(12):1683‐6. [PubMed] [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayer R, Altman D. Empirical evidence of bias. Journal of the American Medical Association 1995;273(5):408‐12. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Steiner 1994
- Steiner CA, Bass EB, Talamini MA, Pitt HA, Steinberg EP. Surgical rates and operative mortality for open and laparoscopic cholecystectomy in Maryland. New England Journal of Medicine 1994;330(6):403‐8. [DOI] [PubMed] [Google Scholar]
Sweeting 2004
- Sweeting MJ, Sutton AJ, Lambert PC. What to add to nothing? Use and avoidance of continuity corrections in meta‐analysis of sparse data. Statistics in Medicine 2004;23:1351‐75. [DOI] [PubMed] [Google Scholar]


