Abstract
Background.
The authors conducted a study to assess recent trends in dental care provider mix (type of dental professionals visited) and service mix (types of dental procedures) use in the United States and to assess rural-urban disparities.
Methods.
Data were from the 2000 through 2016 Medical Expenditure Panel Survey. The sample was limited to respondents who reported at least 1 dental visit to a dental professional in the survey year (N = 138,734 adults ≥ 18 years). The authors estimated rates of visiting 3 dental professionals and undergoing 5 dental procedures and assessed the time trends by rural-urban residence and variation within rural areas. Multiple logistic regression was used to assess the association between rural and urban residence and service and provider mix.
Results.
A decreasing trend was observed in visiting a general dentist, and an increasing trend was observed in visiting a dental hygienist for both urban and rural residents (trend P values < .001). An increasing trend in having preventive procedures and a decreasing trend in having restorative and oral surgery procedures were observed only for urban residents (trend P values < .001). The combined data for 2000 through 2016 showed that rural residents were less likely to receive diagnostic services (adjusted odds ratio [AOR], 0.82; 95% confidence interval [CI], 0.72 to 0.93) and preventive services (AOR, 0.87; 95% CI, 0.78 to 0.96), and more likely to receive restorative (AOR, 1.11; 95% CI, 1.02 to 1.21) and oral surgery services (AOR, 1.23; 95% CI, 1.11 to 1.37).
Conclusions.
Although preventive dental services increased while surgical procedures decreased from 2000 through 2016 in the United States, significant oral health care disparities were found between rural and urban residents.
Practical Implications.
These results of this study may help inform future initiatives to improve oral health in underserved communities. By understanding the types of providers visited and dental services received, US dentists will be better positioned to meet their patients’ oral health needs.
Keywords: Dental care providers, dental services, rural-urban disparity
Increasing access to preventive and therapeutic oral health services is an objective of Healthy People 2020.1 Disparities in access to these services exist for people living in rural communities.2–4 Of the 62 million Americans living in rural areas, 43% lack regular oral health care,5 resulting in poorer oral health outcomes, such as a higher prevalence of complete tooth loss.6 In addition to barriers in accessing oral health services,’ rural residents may also experience disparities in the type of dental services received once they have accessed care, such as being more likely to undergo a tooth extraction and less likely to undergo dental prophylaxis, which can be an indicator of quality of care.8
Results of studies exploring the issue of the receipt of dental procedures9–14 and use of different dental professionals12,15 found that the receipt of preventive services significantly increased, whereas receipt of restorative services declined from 1999 through 2009.9,11 A few studies examined the rural-urban differences in dental services received but they were limited to single states.16,17
To our knowledge, no study has systematically assessed trends in the use of dental care providers and dental procedures by US adults in rural communities over the past decade and whether the rural-urban disparity in oral health care has narrowed over time. To fill these gaps in the literature, this study aimed to assess the trend of dental professionals visited and the trend of dental services received by rural and urban residents and to evaluate the disparity over time from 2000 through 2016. In addition, extending from prior research that applied binary rural-urban classification, which failed to account for variation among the rural counties such as population size and adjacency to a city, we also aimed to explore the intrarurality variation in dental professionals visited and services received. This study provides important information for initiatives specifically aimed to improve oral health in rural communities.18
METHODS
Data source
Data were from the annual, cross-sectional Medical Expenditure Panel Survey (MEPS) from 2000 through 2016. The MEPS provides nationally representative estimates of health care use, expenditures, sources of payment, and health insurance coverage for the US civilian noninstitutionalized population. Detailed information about MEPS can be found elsewhere.1
The variables used in this analysis are from the MEPS Household Component and the Dental Visits Files. Rural and urban residential data were obtained from the Agency for Healthcare Research and Quality. The sample for this analysis was limited to respondents who reported at least 1 dental visit to any type of dental professional in the survey year, including general dentists, dental hygienists, dental technicians, and dental specialists—138,734 adults 18 years and older who participated in the MEPS 2000-2016. This study used deidentified data; therefore, the East Carolina University institutional review board exempted the study from the need for review.
Measurement
Outcomes
Provider mix.
In MEPS, data on the types of dental professionals visited during the last visit were collected by asking, “What type of dental provider did [you/person] see during this visit?” Response options included the following 8 dental professionals: general dentist, dental hygienist, technician, oral surgeon, orthodontist, endodontist, periodontist, and other. Thus, if any of these 8 dental professionals were recorded in a visit in the past year, then the person was classified as having consulted that type of dental professional. All 8 provider type variables were coded as binary outcomes: Yes or No. The answer “Don’t know” was treated as missing.
Service mix.
To ascertain the procedures provided during the dental visit, respondents were asked: “What had [you/person] done during this visit?” If more than 1 procedure was undergone, respondents were also asked, “What else was done?” The following 9 procedure categories were included: diagnostic, preventive, restorative, prosthetic, periodontic, endodontic, oral surgery, orthodontic, and other.1 If any of these services were provided during the visit, then the respondent was classified as having been provided the service. Procedures that belonged to different categories were treated separately. For example, if a respondent underwent an examination, dental prophylaxis, and a partial denture repair during a particular visit, these 3 services were counted under the diagnostic, preventive, and prosthetic categories, respectively. All 9 categories of services were coded as binary outcomes: “Yes/ No.” The answer “Don’t know” was treated as missing.
Owing to the small sample size in some categories of providers and procedures, as has been done in prior research,12 we focused on 8 outcome variables—3 types of providers (that is, general dentist, dental hygienist, oral surgeon) and 5 dental procedures (that is, diagnostic, preventive, restorative, prosthetic, oral surgery).
Covariates
Covariates were selected according to those variables used in the existing literature on this topic.15 Demographic variables were age (18-44, 45-64, and ≥ 65 years), sex (female, male), race or ethnicity (non-Hispanic white, non-Hispanic black, Hispanic [regardless of race], and other), married (Yes/No), and employed (Yes/No). Socioeconomic status (SES) variables were family income level by the federal poverty threshold (poor, near poor, low income, middle income, high income), educational attainment level (less than high school graduate, high school graduate, some college or above), and dental insurance (Yes/No). Health status included self-reported health status (excellent/very good, good, fair/poor). We also included contextual variables: region (Northeast, Midwest, South, West), and rural residence (Yes/No), defined by the Rural-Urban Continuum Code (RUCC), which classifies metropolitan counties by the population size of their metropolitan area, and nonmetropolitan counties by the degree of urbanization and adjacency to a metropolitan area.20 In this study, we classified RUCC categories 1 through 3 as urban residence and RUCC categories 4 through 9 as rural residence.21
Analysis
The unit of analysis was the number of respondents who reported at least 1 dental visit in the past year. For the 8 outcome variables (3 provider types, 5 dental procedures), we first calculated the proportions of respondents who visited each type of provider and the proportions of respondents who underwent each type of procedure using predictive margins. Predictive margins are a type of direct standardization, in which the predicted values from the logistic regression models are averaged over the covariate distribution in the population.22 Second, we estimated the time trend by regressing these proportions of the 8 outcome variables on the survey year (2000-2016), with the survey year as the independent continuous variable. Third, we assessed factors associated with the 8 outcome variables and whether rural-urban differences in the 8 outcome variables have changed over time from 2000 through 2016 (by assessing an interaction term—year by rural residence). Finally, we compared the proportions of the 8 outcome variables by different RUCC categories to assess the inter-RUCC changes from 2000 through 2016 (between-group comparisons) and the intra-RUCC variation in 2000 and 2016 (within-group comparisons). We conducted the analyses of the merged data files at the Agency for Healthcare Research and Quality Research Data Center in Washington, DC, in April 2019.
Sampling weights embedded in the MEPS were incorporated into all the analyses to obtain national estimates. Because of the large sample size, the significance level was set at P < .01; as an exception we used P < .05 for significance in assessing the time trend. Data analyses were conducted using SAS Version 9.4 (SAS).
RESULTS
Sample characteristics
As shown in Table 1, the composition of the sample changed from 2000 through 2016. For instance, the proportion of MEPS respondents in the rural areas declined from 15.3% to 11.7%, and the proportion of respondents 65 years and older increased from 16.9% to 24.2% during the period.
Table 1.
Descriptive statistics of the study sample (n = 138,734).
| VARIABLES | YEAR, WEIGHTED % | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | |
| Location | |||||||||||||||||
| Rural | 15.3 | 15.2 | 14.8 | 14.6 | 15.0 | 14.4 | 15.1 | 15.1 | 14.6 | 14.5 | 13.3 | 12.3 | 12.9 | 12.3 | 13.6 | 13.4 | 11.7 |
| Urban | 84.7 | 84.8 | 85.2 | 85.4 | 85.0 | 85.6 | 84.9 | 84.9 | 85.4 | 85.5 | 86.7 | 87.7 | 87.1 | 87.7 | 86.4 | 86.6 | 88.3 |
| Age, y | |||||||||||||||||
| 19-44 | 48.4 | 47.6 | 46.4 | 45.8 | 44.9 | 43.7 | 42.8 | 42.2 | 41.3 | 40.9 | 40.2 | 40.0 | 39.3 | 39.0 | 38.4 | 38.1 | 38.9 |
| 45-64 | 34.7 | 36.1 | 36.9 | 37.5 | 37.9 | 38.4 | 39.4 | 39.7 | 40.2 | 40.1 | 40.4 | 39.0 | 39.2 | 38.8 | 38.6 | 38.8 | 36.9 |
| ≥ 65 | 16.9 | 16.3 | 16.7 | 16.7 | 17.2 | 17.9 | 17.8 | 18.1 | 18.5 | 19.0 | 19.4 | 20.9 | 21.5 | 22.1 | 23.0 | 23.2 | 24.2 |
| Sex | |||||||||||||||||
| Male | 42.6 | 42.5 | 42.6 | 42.9 | 43.1 | 43.4 | 43.3 | 43.0 | 42.8 | 43.3 | 43.3 | 43.3 | 43.3 | 43.4 | 43.3 | 44.1 | 43.7 |
| Female | 57.4 | 57.5 | 57.4 | 57.1 | 56.9 | 56.6 | 56.7 | 57.0 | 57.2 | 56.7 | 56.7 | 56.7 | 56.7 | 56.6 | 56.7 | 55.9 | 56.3 |
| Married | |||||||||||||||||
| No | 37.6 | 37.1 | 37.4 | 37.7 | 37.5 | 37.4 | 37.9 | 38.3 | 38.2 | 38.8 | 38.9 | 39.2 | 39.2 | 40.3 | 40.1 | 39.0 | 40.3 |
| Yes | 62.4 | 62.9 | 62.6 | 62.3 | 62.5 | 62.6 | 62.1 | 61.7 | 61.8 | 61.2 | 61.1 | 60.8 | 60.8 | 59.7 | 59.9 | 61.0 | 59.7 |
| Race or Ethnicity | |||||||||||||||||
| Non-Hispanic white | 83.8 | 81.9 | 81.4 | 80.7 | 78.9 | 79.2 | 79.9 | 79.1 | 78.9 | 78.7 | 77.7 | 77.2 | 76.4 | 75.6 | 75.2 | 74.0 | 73.8 |
| Non-Hispanic black | 7.0 | 6.9 | 6.6 | 6.8 | 7.2 | 7.2 | 7.4 | 7.4 | 7.3 | 7.6 | 7.9 | 7.6 | 7.8 | 7.9 | 8.0 | 7.6 | 7.4 |
| Hispanic | 6.2 | 7.1 | 6.8 | 6.9 | 7.7 | 7.4 | 7.1 | 7.8 | 7.6 | 7.6 | 8.3 | 9.1 | 9.1 | 9.3 | 9.4 | 10.4 | 10.4 |
| Other | 3.1 | 4.0 | 5.2 | 5.6 | 6.1 | 6.2 | 5.6 | 5.7 | 6.2 | 6.2 | 6.0 | 6.1 | 6.8 | 7.1 | 7.3 | 8.0 | 8.4 |
| Family Income (% of Poverty Level) | |||||||||||||||||
| Poor | 6.0 | 6.0 | 5.8 | 6.0 | 6.0 | 6.1 | 5.6 | 5.9 | 6.2 | 6.7 | 7.1 | 7.1 | 7.2 | 7.0 | 7.2 | 6.4 | 6.8 |
| Near poor | 2.4 | 2.5 | 2.3 | 2.3 | 2.3 | 2.3 | 2.4 | 2.4 | 2.5 | 2.5 | 2.5 | 2.7 | 2.5 | 2.5 | 3.0 | 2.3 | 2.3 |
| Low income | 8.7 | 8.7 | 8.9 | 9.2 | 8.9 | 8.7 | 7.8 | 8.8 | 9.3 | 8.9 | 9.1 | 9.3 | 8.8 | 9.5 | 8.3 | 8.9 | 7.4 |
| Middle income | 29.8 | 29.4 | 27.8 | 28.1 | 29.4 | 28.7 | 28.2 | 27.5 | 28.0 | 27.7 | 27.9 | 28.2 | 28.7 | 27.7 | 25.5 | 24.4 | 25.1 |
| High income | 53.2 | 53.6 | 55.2 | 54.5 | 53.4 | 54.1 | 55.9 | 55.4 | 54.1 | 54.1 | 53.4 | 52.6 | 52.8 | 53.4 | 56.0 | 58.0 | 58.4 |
| Education Level | |||||||||||||||||
| < High school | 11.3 | 11.2 | 10.7 | 9.6 | 9.2 | 9.9 | 8.7 | 8.9 | 8.2 | 7.6 | 6.9 | 6.1 | 6.6 | 7.0 | 6.1 | 6.6 | 7.1 |
| High school | 29.0 | 30.4 | 30.6 | 29.7 | 28.4 | 28.1 | 27.0 | 26.2 | 26.7 | 26.0 | 23.3 | 23.2 | 22.3 | 20.0 | 20.1 | 22.9 | 23.0 |
| ≥ Some college | 59.7 | 58.3 | 58.7 | 60.7 | 62.4 | 62.0 | 64.3 | 64.9 | 65.1 | 66.5 | 69.9 | 70.7 | 71.1 | 73.0 | 73.8 | 70.5 | 69.9 |
| Dental Insurance | |||||||||||||||||
| Yes | 55.1 | 56.4 | 56.1 | 56.6 | 57.4 | 56.5 | 56.3 | 54.6 | 53.2 | 53.8 | 53.4 | 53.2 | 52.7 | 54.0 | 54.9 | 54.7 | 52.9 |
| No | 44.9 | 43.6 | 43.9 | 43.4 | 42.6 | 43.5 | 43.7 | 45.4 | 46.8 | 46.2 | 46.6 | 46.8 | 47.3 | 46.0 | 45.1 | 45.3 | 47.1 |
| Employment Status | |||||||||||||||||
| Not employed | 27.3 | 27.5 | 28.3 | 28.6 | 28.1 | 29.2 | 28.5 | 28.3 | 29.1 | 30.8 | 29.8 | 31.4 | 32.4 | 31.7 | 31.0 | 31.2 | 31.3 |
| Employed | 72.7 | 72.5 | 71.7 | 71.4 | 71.9 | 70.8 | 71.5 | 71.7 | 70.9 | 69.2 | 70.2 | 68.6 | 67.6 | 68.3 | 69.0 | 68.8 | 68.7 |
| Health Status | |||||||||||||||||
| Excellent/very good | 64.0 | 64.0 | 64.8 | 64.8 | 63.3 | 64.0 | 63.3 | 64.2 | 64.3 | 64.1 | 64.2 | 64.0 | 63.4 | 64.8 | 63.9 | 63.1 | 63.9 |
| Good | 9.9 | 9.2 | 9.2 | 10.1 | 10.3 | 9.7 | 10.0 | 9.5 | 10.3 | 9.7 | 10.1 | 9.9 | 9.8 | 9.8 | 10.0 | 9.7 | 9.8 |
| Poor/fair | 26.1 | 26.8 | 26.1 | 25.1 | 26.4 | 26.2 | 26.8 | 26.3 | 25.4 | 26.2 | 25.7 | 26.1 | 26.8 | 25.4 | 26.1 | 27.1 | 26.3 |
| Region | |||||||||||||||||
| Northeast | 21.5 | 20.9 | 21.6 | 20.9 | 20.4 | 20.5 | 20.5 | 19.8 | 20.3 | 19.6 | 19.2 | 19.5 | 19.0 | 19.4 | 18.5 | 19.4 | 19.5 |
| Midwest | 25.4 | 26.2 | 24.7 | 25.0 | 24.9 | 24.6 | 24.8 | 24.6 | 24.4 | 24.5 | 24.9 | 25.1 | 25.1 | 24.2 | 24.9 | 23.8 | 22.7 |
| South | 31.0 | 31.3 | 31.3 | 31.0 | 31.5 | 31.4 | 31.9 | 32.4 | 32.4 | 32.5 | 31.7 | 32.1 | 32.0 | 32.3 | 31.7 | 32.0 | 32.0 |
| West | 22.1 | 21.7 | 22.4 | 23.1 | 23.1 | 23.4 | 22.7 | 23.3 | 22.8 | 23.4 | 24.2 | 23.3 | 23.9 | 24.2 | 24.8 | 24.8 | 25.8 |
Trend analysis results
Figures 1A, B, and C display trends of the proportions of respondents visiting the 3 dental professionals by rural and urban residents. As shown, the rate of decrease (that is, the slope [b]) was significant in visiting general dentists by both rural (b, −0.23; 95% confidence interval [CI], −0.33 to −0.12; trend P < .001) and urban (b, 0.18; 95% CI, −0.26 to −0.11]; trend P < .001) residents; the rate of increase was significant in visiting dental hygienists by both rural residents (b, 0.71; 95% CI, 0.51 to 0.91; trend P < .001) and urban residents (b, 0.67; 95% CI, 0.52 to 0.82; trend P < .001). The trends of the proportions of respondents visiting oral surgeons were not significant for either rural or urban residents (trend P values > .05). Overall, there was a significant decreasing trend for visiting general dentists (b, −0.19; 95% CI, −0.26 to −0.12; trend P < .001) and a significant increasing trend for visiting dental hygienists (b, 0.68; 95% CI, 0.54 to 0.81; trend P < .001).
Figure 1.
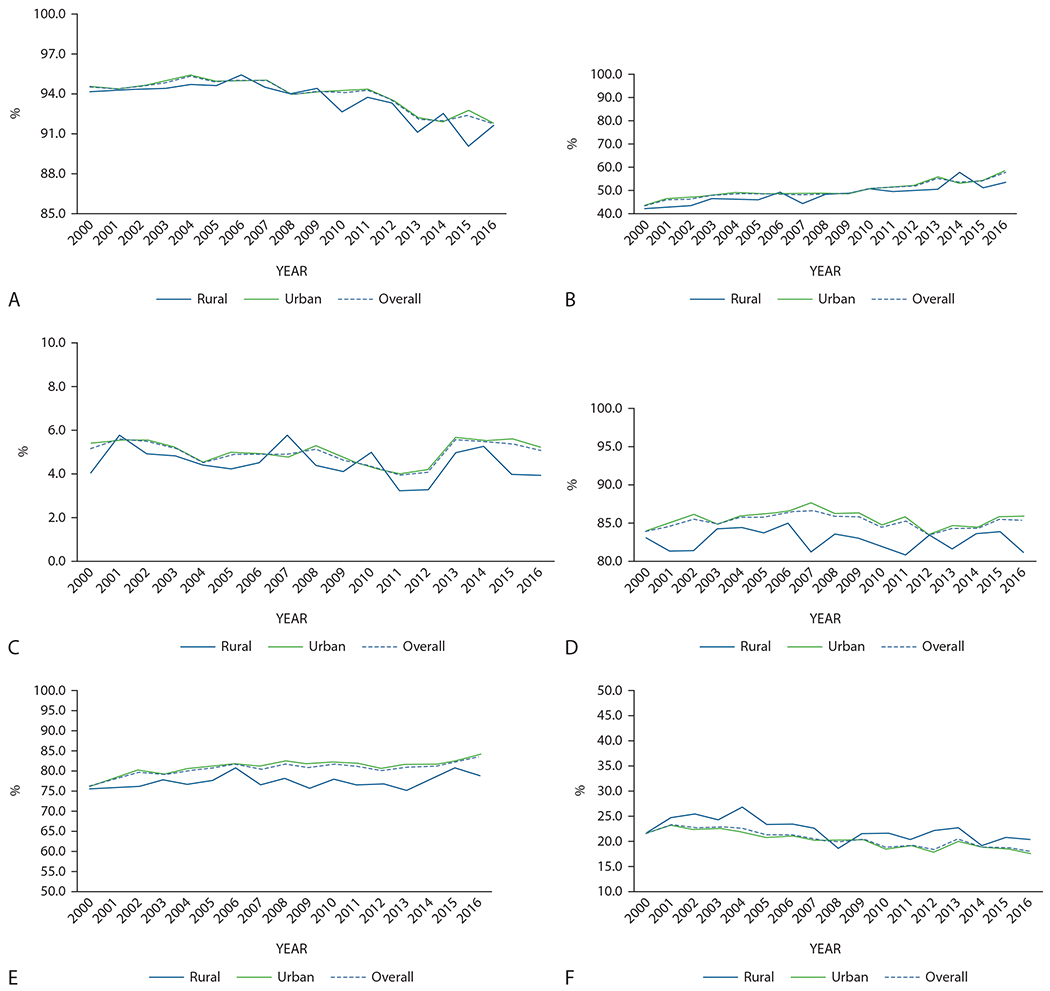
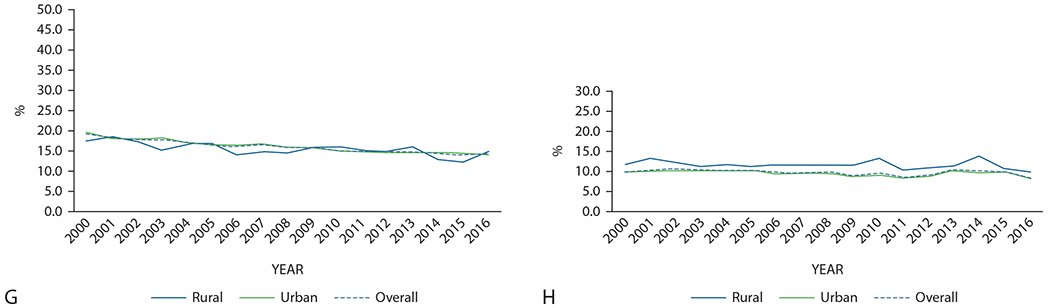
Trend of proportion of respondents visiting general dentists (A), visiting dental hygienists (B), visiting oral surgeons (C), undergoing diagnostic procedures (D), undergoing preventive procedures (E), undergoing restorative procedures (F), undergoing prosthetic procedures (G), and undergoing oral surgery (H).
Figures 1D through 1H present the trends of the proportions of respondents undergoing the 5 dental procedures. The rate of increase in having preventive procedures was significant only for urban residents (b, 0.28; 95% CI, 0.16 to 0.40; trend P < .001). The rates of decrease in having restorative procedures were significant for both rural residents (b, −0.29; 95% CI, −0.47 to 0.11]; trend P < .001) and urban residents (b, −0.31; 95% CI, −0.39 to −0.23; trend P < .001), and were significant for having prosthetic procedures for both rural residents (b, −0.24; 95% CI, −0.36 to −0.11]; trend P < .001) and urban residents (b, −0.31; 95% CI, −0.35 to −0.26; trend P < .001). The rate of decrease in undergoing oral surgerys was significant only for urban residents (b, −0.07; 95% CI, −0.14 to 0.01; trend P = .02). The rates for undergoing diagnostic procedures were not significant for either rural or rural residents. Overall, the trends were all significant except for undergoing diagnostic procedures. There was a significant increasing trend for undergoing preventive procedures (b, 0.26; 95% CI, 0.15 to 0.37; trend P < .001) and decreasing trends for undergoing restorative procedures (b, −0.26; 95% CI, −0.39 to −0.22; trend P < .001), prosthetic procedures (b, −0.30; 95% CI, −0.33 to −0.26; trend P < .001), and oral surgery (b, −0.07; 95% CI, −0.13 to 0.02; trend P = .02).
Multiple logistic regression results
The interaction—year by rural residence—was not significant, indicating that the likelihood of visiting different dental professionals and undergoing different dental procedures for rural and urban residents did not change significantly from 2000 through 2016 (Tables 2 and 3).
Table 2.
Logistic regression model results of factors associated with visiting dental care providers (n = 138,734).
| VARIABLES | TYPE OF PROVIDER* | |||||
|---|---|---|---|---|---|---|
| GENERAL DENTIST | DENTAL HYGIENIST | ORAL SURGEON | ||||
| AOR† (95% CI‡) | P | AOR (95% CI) | P | AOR (95% CI) | P | |
| Year By Rural | NS§ | NS | NS | |||
| Year | 0.97 (0.96 to 0.97) | .0001 | 1.03 (1.02 to 1.04) | < .0001 | 1.00 (0.99 to 1.01) | .693 |
| Rural vs urban | 0.96 (0.79 to 1.16) | .666 | 0.91 (0.73 to 1.15) | .444 | 0.96 (0.78 to 1.19) | .706 |
| Age Group, y (Versus 18-44) | < .0001 | .015 | .079 | |||
| 45-64 | 1.11 (1.04 to 1.18) | .002 | 1.03 (0.98 to 1.07) | .231 | 0.95 (0.88 to 1.03) | .237 |
| ≥ 65 | 1.29 (1.17 to 1.42) | < .0001 | 1.10 (1.03 to 1.18) | .004 | 1.06 (0.96 to 1.17) | .277 |
| Male | 0.96 (0.91 to 1.02) | .194 | 0.90 (0.87 to 0.92) | < .0001 | 1.15 (1.08 to 1.22) | < .0001 |
| Married Versus Other | 1.19 (1.12 to 1.26) | < .0001 | 1.04 (1.01 to 1.08) | .022 | 0.72 (0.67 to 0.77) | < . 0001 |
| Race or Ethnicity (Versus Non-Hispanic White) | < .0001 | < .0001 | < .0001 | |||
| Non-Hispanic black | 0.65 (0.60 to 0.71) | < .0001 | 0.54 (0.50 to 0.59) | < .0001 | 1.27 (1.14 to 1.41) | < .0001 |
| Hispanic | 0.77 (0.69 to 0.85) | < .0001 | 0.51 (0.48 to 0.55) | < .0001 | 0.87 (0.77 to 0.97) | .014 |
| Other | 0.75 (0.67 to 0.84) | < .0001 | 0.51 (0.46 to 0.57) | < .0001 | 1.14 (1.01 to 1.28) | .04 |
| Federal Poverty Threshold (Versus Poor) | .024 | < .0001 | .002 | |||
| Near poor | 1.11 (0.95 to 1.29) | .201 | 1.11 (1.00 to 1.22) | .041 | 0.84 (0.70 to 1.00) | .047 |
| Low income | 1.04 (0.92 to 1.17) | .532 | 1.21 (1.13 to 1.29) | < .0001 | 0.87 (0.76 to 0.99) | .036 |
| Middle income | 1.07 (0.96 to 1.19) | .203 | 1.45 (1.35 to 1.56) | < .0001 | 0.83 (0.74 to 0.93) | .002 |
| High income | 1.16 (1.04 to 1.30) | .008 | 1.72 (1.60 to 1.85) | < .0001 | 0.78 (0.69 to 0.88) | < .0001 |
| Education (Versus < High School) | < .0001 | < .0001 | < .0001 | |||
| High school | 1.09 (0.99 to 1.20) | .094 | 1.31 (1.23 to 1.38) | < .0001 | 0.88 (0.79 to 0.98) | .022 |
| ≥ Some college | 1.27 (1.15 to 1.39) | < .0001 | 1.50 (1.41 to 1.59) | < .0001 | 0.81 (0.72 to 0.90) | < .0001 |
| Dental Insurance | 1.26 (1.19 to 1.35) | < .0001 | 1.24 (1.19 to 1.30) | < .0001 | 0.97 (0.91 to 1.04) | .441 |
| Employed | 1.00 (0.94 to 1.07) | .946 | 0.95 (0.91 to 1.00) | .03 | 0.89 (0.82 to 0.96) | .005 |
| Health Status (Versus Excellent/Very Good) | .709 | < .0001 | < .0001 | |||
| Fair/poor | 0.98 (0.90 to 1.06) | .592 | 0.72 (0.69 to 0.76) | < .001 | 1.43 (1.30 to 1.57) | < .0001 |
| Good | 1.02 (0.95 to 1.09) | .631 | 0.90 (0.87 to 0.93) | < .001 | 1.16 (1.09 to 1.24) | < .0001 |
| Region (Versus Northeast) | < .0001 | < .0001 | < .0001 | |||
| Midwest | 1.59 (1.41 to 1.78) | < .0001 | 1.38 (1.20 to 1.58) | < .0001 | 0.80 (0.72 to 0.88) | < .0001 |
| South | 1.06 (0.95 to 1.18) | .2879 | 0.75 (0.65 to 0.86) | < .0001 | 0.98 (0.88 to 1.09) | .742 |
| West | 0.97 (0.86 to 1.08) | .527 | 0.91 (0.79 to 1.03) | .132 | 0.83 (0.74 to 0.92) | .001 |
Type of provider was the dependent variable.
AOR: Adjusted odds ratio.
CI: Confidence interval.
NS: Not significant.
Table 3.
Logistic regression model results of factors associated with undergoing dental procedures (n = 138,734).
| VARIABLES | TYPE OF PROCEDURE* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| DIAGNOSTIC | PREVENTIVE | RESTORATIVE | PROSTHETIC | SURGERY | ||||||
| AOR† (95% CI‡) | P | AOR (95% CI) | P | AOR (95% CI) | P | AOR (95% CI) | P | AOR (95% CI) | P | |
| Year By Rural | NS§ | NS | NS | NS | NS | |||||
| Year | 1.00 (0.99 to 1.01) | .656 | 1.02 (1.01 to 1.02) | < .0001 | 0.98 (0.98 to 0.99) | < .0001 | 0.98 (0.97 to 0.98) | < .0001 | 0.99 (0.98 to 0.99) | .001 |
| Rural versus urban | 0.82 (0.72 to 0.93) | .003 | 0.87 (0.78 to 0.96) | 007 | 1.11 (1.02 to 1.21) | .012 | 0.92 (0.83 to 1.02) | .098 | 1.23 (1.11 to 1.37) | .000 |
| Age Group, y (Versus 18-44) | .341 | < .0001 | < .0001 | .010 | ||||||
| 45-64 | 0.97 (0.93 to 1.01) | .142 | 1.02 (0.98 to 1.07) | 353 | 0.87 (0.84 to 0.91) | < .0001 | 2.70 (2.57 to 2.83) | < .0001 | 1.01 (0.96 to 1.06) | .782 |
| ≥ 65 | 0.98 (0.92 to 1.05) | .567 | 1.17 (1.10 to 1.24) | < .0001 | 0.94 (0.89 to 0.99) | .021 | 2.46 (3.24 to 3.68) | < .0001 | 0.91 (0.86 to .98) | .007 |
| Male | 0.89 (0.86 to 0.92) | < .0001 | 0.84 (0.82 to 0.87) | < .0001 | 0.99 (0.96 to 1.03) | .702 | 1.00 (0.97 to 1.04) | .838 | 1.30 (1.25 to 1.35) | < .0001 |
| Married Versus Other | 1.07 (1.03 to 1.12) | .002 | 1.13 (1.09 to 1.17) | < .0001 | 0.95 (0.92 to 0.98) | .002 | 0.99 (0.96 to 1.03) | .753 | 0.81 (0.77 to 0.85) | < .0001 |
| Race or Ethnicity (Versus Non-Hispanic White) | < .0001 | < .0001 | < .0001 | .009 | < .0001 | |||||
| Non-Hispanic black | 0.62 (0.58 to 0.66) | < .0001 | 0.56 (0.53 to 0.60) | < .0001 | 0.74 (0.70 to 0.79) | < .0001 | 0.91 (0.85 to 0.97) | .003 | 1.65 (1.54 to 1.76) | < .0001 |
| Hispanic | 0.69 (0.64 to 0.74) | < .0001 | 0.79 (0.75 to 0.84) | < .0001 | 0.96 (0.91 to 1.02) | .160 | 0.93 (0.87 to 0.99) | .028 | 1.10 (1.03 to 1.18) | .005 |
| Other | 0.74 (0.68 to 0.80) | < .0001 | 0.82 (0.76 to 0.89) | < .0001 | 0.89 (0.83 to 0.95) | .001 | 0.94 (0.88 to 1.01) | .095 | 1.18 (1.08 to 1.29) | .000 |
| Federal Poverty Threshold (Versus Poor) | < .0001 | < .0001 | < .0001 | .003 | < .0001 | |||||
| Near poor | 1.01 (0.92 to 1.11) | .89 | 1.07 (0.98 to 1.18) | 142 | 1.02 (0.92 to 1.13) | .751 | 1.08 (0.95 to 1.23) | .217 | 0.95 (0.85 to 1.07) | .415 |
| Low income | 1.09 (1.01 to 1.18) | .021 | 1.23 (1.15 to 1.23) | < .0001 | 1.04 (0.96 to 1.11) | .346 | 0.97 (0.89 to 1.06) | .49 | 0.85 (0.78 to 0.92) | < .0001 |
| Middle income | 1.20 (1.12 to 1.28) | < .0001 | 1.54 (1.44 to 1.64) | < .0001 | 1.04 (0.97 to 1.11) | .276 | 1.07 (0.99 to 1.15) | .102 | 0.66 (0.62 to 0.71) | < .0001 |
| High income | 1.43 (1.33 to 1.53) | < .0001 | 2.19 (2.05 to 2.34) | < .0001 | 0.92 (0.86 to 0.98) | .009 | 1.11 (1.03 to 1.20) | .009 | 0.48 (0.44 to 0.52) | < .0001 |
| Education (Versus < High School) | < .0001 | < .0001 | .006 | .294 | < .0001 | |||||
| High school | 1.22 (1.15 to 1.30) | < .0001 | 1.34 (1.27 to 1.42) | < .0001 | 1.11 (1.04 to 1.18) | .002 | 0.96 (0.89 to 1.02) | .19 | 0.73 (0.69 to 0.77) | < .0001 |
| Some college or above | 1.58 (1.48 to 1.68) | < .0001 | 1.92 (1.81 to 2.04) | < .0001 | 1.10 (1.03 to 1.17) | .03 | 0.98 (0.92 to 1.05) | .601 | 0.48 (0.45 to 0.51) | < .0001 |
| Dental Insurance | 1.26 (1.21 to 1.32) | < .0001 | 1.45 (1.39 to 1.51) | < .0001 | 1.00 (0.97 to 1.04) | .813 | 1.03 (0.98 to 1.07) | .239 | 0.77 (0.73 to 0.81) | < .0001 |
| Employed | 0.92 (0.88 to 0.97) | .003 | 0.94 (0.89 to 0.98) | 007 | 0.94 (0.90 to 0.98) | .004 | 0.93 (0.89 to 0.97) | .002 | 0.99 (0.94 to 1.05) | .761 |
| Health Status (Versus Excellent/Very Good) | < .0001 | < .0001 | < .0001 | < .0001 | < .0001 | |||||
| Fair/poor | 0.76 (0.71 to 0.80) | < .0001 | 0.52 (0.49 to 0.55) | < .0001 | 1.20 (1.14 to 1.27) | < .0001 | 1.40 (1.32 to 1.49) | < .0001 | 1.90 (1.79 to 2.02) | < .0001 |
| Good | 0.89 to (0.850.94) | < .0001 | 0.76 (0.73 to 0.79) | < .0001 | 1.11 (1.06 to 1.15) | < .001 | 1.20 (1.15 to 1.25) | < .0001 | 1.38 (1.31 to 1.44) | < .0001 |
| Region (Versus Northeast) | < .0001 | < .0001 | < .0001 | < .0001 | < .0001 | |||||
| Midwest | 1.38 (1.25 to 1.51) | < .0001 | 1.09 (1.01 to 1.18) | 022 | 0.92 (0.87 to 0.97) | .002 | 1.02 (0.95 to 1.09) | .628 | 1.03 (0.95 to 1.10) | .481 |
| South | 0.93 (0.84 to 1.02) | .131 | 0.88 (0.83 to 0.94) | < .0001 | 0.77 (0.73 to 0.82) | < .0001 | 1.01 (0.94 to 1.08) | .846 | 1.17 (1.09 to 1.25) | < .0001 |
| West | 0.98 (0.90 to 1.07) | .682 | 0.99 (0.93 to 1.06) | 833 | 0.88 (0.83 to 0.93) | < .0001 | 1.18(1.11 to 1.26) | < .0001 | 1.03 (0.96 to 1.10) | .491 |
Type of procedure was the dependent variable.
AOR: Adjusted odds ratio.
CI: Confidence interval
NS: Not significant.
Table 2 presents the results for the 3 types of providers. The year variable was significant in 2 models, suggesting an significant decease in seeing a general dentist (adjusted odds ratio [AOR], 0.97; 95% CI, 0.96 to 0.97) and a significant increase in seeing a dental hyginist (AOR, 1.03; 95% CI, 1.02 to 1.04) during the study period. The rural variable was not signficant. Results of other covariates were mostly significant. Briefly, respondents with higher incomes, higher education levels, and dental insurance were more likely to have visited a general dentist or dental hygienist, whereas respondents from racial or ethnic minority groups were less likely to have done so (all P < .01). Respondents with higher incomes and education levels were less likely to have visited an oral surgeon in the past year, whereas respondents from minority groups were more likely to have done so (all P < .01).
Table 3 presents the results for the 5 types of dental procedures. The year variable was significant in 4 of the 5 models, suggesting a signficant increase in undergoing a preventive procedure (AOR, 1.02; 95% CI, 0.98 to 0.99) and a significant decrease in undergoing restorative, prothetic procedures, and oral surgery procedures (all P < .001) from 2000 through 2016. Rural residents were less likely than urban residents to have received diagnostic services (AOR, 0.82; 95% CI, 0.72 to 0.93) or preventive services (AOR, 0.87; 95% CI, 0.78 to 0.96) and more likely to have received restorative services (AOR, 1.11; 95% CI, 1.02 to 1.21) and oral surgery services (AOR, 1.23; 95% CI, 1.11 to 1.37) than urban residents. Respondents with higher incomes and education levels were more likely to have undergone diagnostic, preventive, restorative, and prosthetic procedures than respondents from minority groups (all P < .01). The opposite was observed for having oral surgery. Respondents with higher income and higher education levels were less likely to have undergone an oral surgery procedure than respondents from racial or ethnic minority groups (all P < .01). The dental insurance variable was positively associated with having recevied diagnostic and preventive procedures but negatively associated with undergoing oral surgery procedures (all P < .01).
Intra-RUCC and inter-RUCC comparisons
Table 4 presents the results of visiting dental care providers in 2000 and 2016 by the 7 RUCC categories (owing to the small sample size, we combined RUCC categories 6 and 8 and coded them as 6 and combined RUCC categories 7 and 9 and coded them as 7). Thus, the rural (nonmetropolitan) counties are RUCC categories 4 through 7. Overall, no significant difference was observed among intra-RUCC categories 1 through 7 (P > .01) in visiting different dental professionals in 2000 or 2016. Yet, residents in the most rural counties (RUCC category 7) were less likely to have visited a dental hygienist (39.8% versus 62.5%) or an oral surgeon (1.5% versus 3.4%) than those residents in the least rural counties (RUCC category 4). An inter-RUCC comparison between 2000 and 2016 showed a significant decrease of 2.4 percentage points (P < .01) in visiting general dentists and a significant increase of 29.7 percentage points (P < .001) in visiting dental hygienists only among those residents in the most populous urban counties (that is, RUCC category 1 counties).
Table 4.
A comparison of 2000 and 2016: proportions of respondents visiting dental care providers (n = 14,700).
| RUCC CATEGORY | TYPE OF PROVIDER | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| GENERAL DENTISTS (%) | DENTAL HYGIENISTS (%) | ORAL SURGEONS (%) | |||||||
| 2000 | 2016 | Relative Change | 2000 | 2016 | Relative Change | 2000 | 2016 | Relative Change | |
| 1 | 94.7 | 92.4 | −2.4† | 42.8 | 55.6 | 29.7‡ | 4.9 | 5.0 | 1.6 |
| 2 | 94.7 | 91.7 | −3.2§ | 46.0 | 60.4 | 31.4§ | 5.6 | 5.8 | 3.4 |
| 3 | 94.5 | 91.6 | −3.2 | 50.6 | 69.5 | 37.4§ | 6.3 | 4.2 | −33.9 |
| 4 | 95.7 | 88.8 | −7.2§ | 48.1 | 62.5 | 29.9 | 3.6 | 3.4 | −5.8 |
| 5 | 95.3 | 96.0 | 0.8 | 46.5 | 53.4 | 14.7 | 5.7 | 1.1 | −80.8§ |
| 6 | 92.8 | 92.1 | −0.7 | 36.0 | 54.8 | 52.0 | 3.0 | 5.7 | 91.8 |
| 7 | 93.4 | 95.7 | 2.5 | 46.1 | 39.8 | −13.6 | 4.7 | 1.3 | −73.1§ |
| P | .935 | .716 | .720 | .015 | .428 | .021 | |||
Rural-Urban Continuum Code (RUCC) categories are defined as 1: metropolitan area with ≥ 1 million population, 2: metropolitan area with 250,000-1 million population, 3: metropolitan area with < 250,000 population, 4: nonmetropolitan area with urban population 2,500-19,999 adjacent, 5: nonmetropolitan area with urban population ≥ 20,000 not adjacent, 6: nonmetropolitan area with urban population 2,500-19,999 adjacent, 7: nonmetropolitan area with urban population 2,500-19,999 not adjacent, 8: nonmetropolitan area with < 2,500 urban population adjacent, 9: nonmetropolitan area with < 2,500 urban population not adjacent. (Category 6 includes RUCC categories 6 and 8, and category 7 includes RUCC categories 7 and 9.) P values indicate significance test values for comparison between RUCC categories.
P < .01.
P < .001.
P < .05.
Table 5 presents similar residential comparisons for receipt of dental services. Significant intra-RUCC differences were observed in undergoing restorative procedures and oral surgery in 2000, having preventive procedures in 2016, and having prosthetic procedures in both 2000 and 2016 (all P < .01). Among residents in rural counties (RUCC categories 4 through 7), similar to the results for dental professionals presented earlier, overall, residents in the most rural counties (RUCC category 7) were less likely to have undergone preventive procedures (68.0% versus 84.0%) and more likely to have undergone prosthetic procedures (19.8% versus 16.4%) than those residents in the least rural counties (RUCC category 4) in 2016. Moreover, the intrarural (among RUCC categories 4 through 7) gaps seemed to have increased from 2000 through 2016. For instance, for the preventive procedures undergone by residents in RUCC categories 4 and 7, the difference was 9 percentage points (70.7% versus 79.7%) in 2000; it increased to 16 percentage points (68.0% versus 84.0%) in 2016. Finally, from 2000 through 2016, a significant inter-RUCC increase in undergoing preventive procedures (P values < .001) and a significant decrease in undergoing restorative procedures (P values < .05) and prosthetic procedures (P values < .01) were found only among those residents in the urban counties (RUCC categories 1 through 3), not among those in rural counties (RUCC categories 4 through 7).
Table 5.
A comparison of 2000 and 2016: proportion of respondents undergoing dental procedures (n = 14,700).
| RUCC CATEGORY | TYPE OF PROCEDURE | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DIAGNOSTIC (%) | PREVENTIVE (%) | RESTORATIVE (%) | PROSTHETIC (%) | ORAL SURGERY (%) | |||||||||||
| 2000 | 2016 | Relative Change | 2000 | 2016 | Relative Change | 2000 | 2016 | Relative Change | 2000 | 2016 | Relative Change | 2000 | 2016 | Relative Change | |
| 1 | 84.6 | 85.4 | 1.0 | 76.2 | 82.5 | 8.3† | 21.4 | 17.6 | −17.8† | 19.7 | 16.0 | −19.2‡ | 9.7 | 8.2 | −15.3 |
| 2 | 82.7 | 86.3 | 4.3 | 76.7 | 86.1 | 12.3† | 22.5 | 17.7 | −21.3§ | 20.8 | 13.1 | −36.9† | 10.4 | 8.8 | −15.1 |
| 3 | 84.0 | 86.8 | 3.4 | 77.9 | 86.7 | 11.4† | 25.3 | 17.5 | −31.0‡ | 15.3 | 11.8 | −23.0 | 11.1 | 7.5 | −32.1 |
| 4 | 82.9 | 79.0 | −4.7 | 79.7 | 84.0 | 5.5 | 19.8 | 15.7 | −21.0 | 15.0 | 16.4 | 8.9 | 9.7 | 9.2 | −5.2 |
| 5 | 85.0 | 77.1 | −9.3 | 82.7 | 76.6 | −7.4 | 18.6 | 21.3 | 14.4 | 13.7 | 11.9 | −13.3 | 11.2 | 9.8 | −12.6 |
| 6 | 82.2 | 87.4 | 6.3 | 71.5 | 79.2 | 10.8 | 22.9 | 24.3 | 6.0 | 15.9 | 12.7 | −20.0 | 15.8 | 9.2 | −42.2* |
| 7 | 84.4 | 72.6 | −14.0 | 70.7 | 68.0 | −3.8 | 27.1 | 20.1 | −26.0 | 24.7 | 19.8 | −19.7 | 11.1 | 16.1 | 44.4 |
| P | .972 | .013 | .425 | < .0001 | .008 | .097 | .007 | .008 | .009 | .045 | |||||
RUCC: Rural−Urban Continuum Code (see Table 4 for category definitions).
P < .001.
P < .01.
P < .05.
DISCUSSION
Disparities in oral health outcomes and care are a significant problem in rural areas. To more fully understand this issue, in this study we took an additional step beyond the dichotomy of visiting or not visiting a dentist to examine the trends of types of services received and providers visited by rural and urban residents from 2000 through 2016. Over this period, the differences in visiting different dental care providers and undergoing different dental procedures between rural and urban residents did not change significantly, as indicated by the insignificant interaction of year by rural residence. Rural residents were less likely to have undergo diagnostic and preventive procedures and more likely to have undergone restorative and oral surgery procedures than urban residents. Moreover, there was intrarurality variation in dental services received. The study results also showed that there was a significant decreasing trend in visiting a general dentist and a significant increasing trend in visiting a dental hygienist for both rural and urban residents. There were significant decreasing trends in having restorative and prosthetic procedures for both rural and urban residents, but a significant increasing trend in having preventive procedures and a significant decreasing trend in having oral surgery procedures were observed only for urban residents.
These findings first showed significant rural-urban differences in the different type of dental services received, with rural residents having more surgical procedures (restorative and surgery) and fewer favorable (preventive and diagnostic) procedures. Second, the rural-urban disparity in dental services persisted and worsened to some extent over time. For instance, the rural-urban gap in having undergone preventive procedures was 0.8 percentage points in 2000; it increased to 5.2 percentage points in 2016 (Figure 1E). The lower likelihood to have undergone preventive procedures and higher likelihood to have undergone invasive or surgical procedures by rural residents might suggest that rural residents were not having regular dental visits, and as a consequence, their oral health status was worse compared with their urban counterparts, which necessitated the more complex surgical procedures.
Rural populations face greater difficulties accessing oral health care, including greater financial barriers and shortages of dentists.6,7 When rural residents seek dental care, the reason is more likely due to dental problems; they are also more likely to report unmet dental needs and less likely to have dental insurance.3 Our study results of less preventive care and more surgical care among rural residents can be an indicator of quality of care,8 which is linked to access of care, and equally important. The use of midlevel dental care providers (for example, dental hygienists) could increase access to care for underserved populations.23,24
In contrast to prior cross-sectional research on rural-urban differences in dental procedures in single states (such as Virginia17 and North Carolina16) and an older analysis of the 1996 MEPS data,15 our study analyzed national data and systematically assessed the trends of rural-urban disparities in dental services received and professionals visited from 2000 through 2016. Nonetheless, consistent with prior study results, our results showed disparities in dental services received by rural residents.
To our knowledge, our study is the first to reveal intrarurality differences in dental services. Even though we did not find a linear relationship between the extent of rurality and the extent of having preventive oral services, there is some evidence that residents in the most rural areas (RUCC category 7) had the least preventive and the most surgical services. Furthermore, the gap in dental procedures between residents in the most rural and those in less rural areas (for example, RUCC category 4) and between those in urban communities was widening. This pattern should be monitored closely in future studies.
Overall, our study results showed an increase in using preventive care and a decrease in restorative, prosthetic, and dental surgery procedures. These findings are consistent with those of prior cross-sectional studies.11,12 One 2014 study found that from 1999 through 2009 a small but statistically significant increase in the proportion of preventive and diagnostic procedures and a decrease in restorative procedures undergone by working adults in the United States.11 Thus, a change in dental care needs as a result of improved oral health status25 might account for these findings from our study and prior studies.11,12 These findings can be useful for practitioners deciding the types of services most needed and shaping their practices in light of dental service trends.
Althought SES was not the focus of this study, the results also showed that people with lower SES and from racial or ethnic minority groups were less likely to receive preventive and diagnostic services than those with higher SES and from non-Hispanic white groups. These findings are consistent with prior research that racial or ethnic minority populations and people with lower SES had limited access to dental care and poor oral health status.26–30 Non-Hispanic black and Hispanic adults are more likely to have a higher rate of untreated dental caries and complete tooth loss than white adults.31
Our study has limitations that should be considered. Treatment and provider data are self-reported, which may be inaccurate. For instance, data are limited to those providers or procedure types reported by respondents, but they may be unable to differentiate among a dentist, dental hygienist, or dental assistant during the visit. The dental procedures reported may not be fully exhaustive, and the variety of dental services actually received might have been broader, potentially limiting the validity of these data. Multiple procedures of the same type reported during a single visit are recorded as a single procedure type. For instance, a respondent may have more than 1 restorative procedure but 1 such procedure was recorded, which could lead to an underestimation. No data on the intensity of the procedures were available. Yet, the MEPS is the only dataset that provides nationally representative estimates on specific procedures and type of provider.
CONCLUSIONS
Although preventive dental procedures increased while surgical procedures decreased from 2000 through 2016 in the United States, significant oral health care disparities were found between rural and urban comunities. Limited access to dental health professionals in rural areas may account for these findings. This study has provided empirical data on the trend of rural-urban inequalities in types of providers visited and dental services received. These results may help inform future initiatives to improve oral health in underserved communities. By understanding the types of providers visited and dental services received, US dentists will be better positioned to meet their patients’ oral health needs.
Acknowledgments
This study was funded by grant 1R03DE027436-01A1 awarded to East Carolina University by the National Institute of Dental and Craniofacial Research.
ABBREVIATION KEY
- MEPS
Medical Expenditure Panel Survey.
- NS
Not significant.
- RUCC
Rural-Urban Continuum Code
- SES
Socioeconomic status.
Footnotes
Disclosure. None of the authors reported any disclosures.
Contributor Information
Huabin Luo, Department of Public Health, Brody School of Medicine, East Carolina University, 115 Heart Dr, Greenville, NC 27834.
Qiang Wu, Department of Biostatistics, College of Allied Health, East Carolina University, Greenville, NC.
Ronny A. Bell, Department of Public Health, Brody School of Medicine, East Carolina University, Greenville, NC.
Wanda G. Wright, Department of Foundational Sciences, Dental Public Health, School of Dental Medicine, East Carolina University, Greenville, NC.
Raul I. Garcia, Department of Health Policy and Health Services Research, Henry M. Goldman School of Dental Medicine, Boston University, Boston, MA.
Sara A. Quandt, Department of Epidemiology and Prevention, Division of Public Health Sciences, Wake Forest School of Medicine, Winston-Salem, NC.
References
- 1.US Department of Health and Human Services. Healthy People 2020: topics and objectives. Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/ Accessed February 12, 2020.
- 2.Vargas CM, Dye BA, Hayes K. Oral health care utilization by US rural residents: National Health Interview Survey 1999. J Public Health Dent 2003;63(3): 150–157. [DOI] [PubMed] [Google Scholar]
- 3.Vargas CM, Dye BA, Hayes KL. Oral health status of rural adults in the United States. JADA. 2002;133(12): 1672–1681. [DOI] [PubMed] [Google Scholar]
- 4.Caldwell JT, Lee H, Cagney KA. The role of primary care for the oral health of rural and urban older adults. J Rural Health. 2017;33(4):409–418. [DOI] [PubMed] [Google Scholar]
- 5.Braswell A, Johnson N. Rural America’s oral health care needs. Available at: https://www.ruralhealthweb.org/getattachment/Advocate/Policy-Documents/RuralAmericasOralHealthCareNeeds-(1).pdf.aspx?lang=en-US Accessed March 20, 2020.
- 6.Doescher MP, Keppel GA. Dentist supply, dental care utilization, and oral health among rural and urban U.S. residents: 2015. Available at: https://www.ruralhealthresearch.org/publications/970 Accessed September 9, 2019.
- 7.Skillman SM, Doescher MP, Mouradian WE, Brunson DK. The challenge to delivering oral health services in rural America. J Public Health Dent. 2010;70 (suppl 1):S49–S57. [DOI] [PubMed] [Google Scholar]
- 8.Manski RJ, Moeller JF, Hupp JR. An analysis of oral surgical dental visits by provider type, 1996. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;94(6):687–691. [DOI] [PubMed] [Google Scholar]
- 9.Manski RJ, Cohen LA, Brown E, Carper KV, Vargas C, Macek MD. Dental service mix among older adults aged 65 and over: United States, 1999 and 2009. J Public Health Dent. 2014;74(3):219–226. [DOI] [PubMed] [Google Scholar]
- 10.Manski RJ, Hyde JS, Chen H, Moeller JF. Differences among older adults in the types of dental services used in the United States. Inquiry. 2016;53 10.1177/0046958016652523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manski RJ, Macek MD, Brown E, Carper KV, Cohen LA, Vargas C. Dental service mix among workingage adults in the United States, 1999 and 2009. J Public Health Dent. 2014;74(2):102–109. [DOI] [PubMed] [Google Scholar]
- 12.Manski RJ, Moeller JF. Use of dental services: an analysis of visits, procedures and providers, 1996. JADA. 2002;133(2):167–175. [DOI] [PubMed] [Google Scholar]
- 13.Meyerhoefer CD, Zuvekas SH, Manski R. The demand for preventive and restorative dental services. Health Econ. 2014;23(1):14–32. [DOI] [PubMed] [Google Scholar]
- 14.Skaar DD, O’Connor H. Dental service trends for older US adults, 1998-2006. Spec Care Dentist. 2012;32(2): 42–48. [DOI] [PubMed] [Google Scholar]
- 15.Goodman HS, Manski MC, Williams JN, Manski RJ. An analysis of preventive dental visits by provider type, 1996. JADA. 2005;136(2):221–228. [DOI] [PubMed] [Google Scholar]
- 16.Bader JD, Scurria MS, Shugars DA. Urban/rural differences in prosthetic dental service rates. J Rural Health. 1994;10(1):26–30. [Google Scholar]
- 17.Janus C, Hunt RJ. Rural and urban differences in prosthodontic care provided by Virginia general dentists. Gen Dent 2008;56(5):438–442. [PubMed] [Google Scholar]
- 18.US Department of Health and Human Services. Office of Rural Health Policy Rural guide to health professions funding 2012. Available at: https://www.hrsa.gov/sites/default/files/ruralhealth/pdf/ruralhealthprofessionsguidance.pdf Accessed September 8, 2019.
- 19.Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey: survey background. Available at: https://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp Accessed June 25, 2019.
- 20.US Department of Agriculture Economic Research Service. Rural-Urban Continuum Codes. Available at: https://www.ers.usda.gov/data-products/rural-urban-continuumcodes/documentation/ Accessed March 2, 2020.
- 21.James WL. All rural places are not created equal: revisiting the rural mortality penalty in the United States. Am J Public Health. 2014;104(11):2122–2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Graubard BI, Korn EL. Predictive margins with survey data. Biometrics. 1999;55(2):652–659. [DOI] [PubMed] [Google Scholar]
- 23.Rodriguez TE, Galka AL, Lacy ES, Pellegrini AD, Sweier DG, Romito LM. Can midlevel dental providers be a benefit to the American public? J Health Care Poor Underserved. 2013;24(2):892–906. [DOI] [PubMed] [Google Scholar]
- 24.Koppelman J, Vitzthum K, Simon L. Expanding where dental therapists can practice could increase Americans’ access to cost-efficient care. Health Aff (Millwood). 2016;35(12):2200–2206. [DOI] [PubMed] [Google Scholar]
- 25.Dye BA, Tan S, Smith V. Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat 11. 2007;11(248):1–92. [PubMed] [Google Scholar]
- 26.Christian B, Chattopadhyay A, Kingman A, Boroumand S, Adams A, Garcia I. Oral health care services utilisation in the adult US population: Medical Expenditure Panel Survey 2006. Community Dent Health 2013;30(3):161–167. [PubMed] [Google Scholar]
- 27.Eke PI, Dye BA, Wei L, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009-2012. J Periodontol. 2015;86(5), 611–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manski RJ, Moeller JF, Maas WR. Dental services: an analysis of utilization over 20 years. JADA. 2001; 132(5):655–664. [DOI] [PubMed] [Google Scholar]
- 29.Wu B, Liang J, Plassman BL, Remle RC, Bai L. Oral health among white, black, and Mexican-American elders: an examination of edentulism and dental caries. J Public Health Dent. 2011;71(4):308–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang Y. Racial/ethnic disparity in utilization of general dental care services among US adults: Medical Expenditure Panel Survey 2012. J Racial Ethnic Health Disparities. 2016;3(4):565–572. [DOI] [PubMed] [Google Scholar]
- 31.Dye B, Thornton-Evans G, Li X, Iafolla T. Dental caries and tooth loss in adults in the United States, 2011-2012. NCHS Data Brief. 2015;(197):197. [PubMed] [Google Scholar]


