Abstract
Background
The current COVID‐19 pandemic has been identified as a possible trigger for increases in loneliness and social isolation among older people due to the restrictions on movement that many countries have put in place. Loneliness and social isolation are consistently identified as risk factors for poor mental and physical health in older people. Video calls may help older people stay connected during the current crisis by widening the participant’s social circle or by increasing the frequency of contact with existing acquaintances.
Objectives
The primary objective of this rapid review is to assess the effectiveness of video calls for reducing social isolation and loneliness in older adults. The review also sought to address the effectiveness of video calls on reducing symptoms of depression and improving quality of life.
Search methods
We searched CENTRAL, MEDLINE, PsycINFO and CINAHL from 1 January 2004 to 7 April 2020. We also searched the references of relevant systematic reviews.
Selection criteria
Randomised controlled trials (RCTs) and quasi‐RCTs (including cluster designs) were eligible for inclusion. We excluded all other study designs. The samples in included studies needed to have a mean age of at least 65 years. We included studies that included participants whether or not they were experiencing symptoms of loneliness or social isolation at baseline. Any intervention in which a core component involved the use of the internet to facilitate video calls or video conferencing through computers, smartphones or tablets with the intention of reducing loneliness or social isolation, or both, in older adults was eligible for inclusion. We included studies in the review if they reported self‐report measures of loneliness, social isolation, symptoms of depression or quality of life.
Two review authors screened 25% of abstracts; a third review author resolved conflicts. A single review author screened the remaining abstracts. The second review author screened all excluded abstracts and we resolved conflicts by consensus or by involving a third review author. We followed the same process for full‐text articles.
Data collection and analysis
One review author extracted data, which another review author checked. The primary outcomes were loneliness and social isolation and the secondary outcomes were symptoms of depression and quality of life. One review author rated the certainty of evidence for the primary outcomes according to the GRADE approach and another review author checked the ratings. We conducted fixed‐effect meta‐analyses for the primary outcome, loneliness, and the secondary outcome, symptoms of depression.
Main results
We identified three cluster quasi‐randomised trials, which together included 201 participants. The included studies compared video call interventions to usual care in nursing homes. None of these studies were conducted during the COVID‐19 pandemic.
Each study measured loneliness using the UCLA Loneliness Scale. Total scores range from 20 (least lonely) to 80 (most lonely). The evidence was very uncertain and suggests that video calls may result in little to no difference in scores on the UCLA Loneliness Scale compared to usual care at three months (mean difference (MD) −0.44, 95% confidence interval (CI) −3.28 to 2.41; 3 studies; 201 participants), at six months (MD −0.34, 95% CI −3.41 to 2.72; 2 studies; 152 participants) and at 12 months (MD −2.40, 95% CI −7.20 to 2.40; 1 study; 90 participants). We downgraded the certainty of this evidence by three levels for study limitations, imprecision and indirectness.
None of the included studies reported social isolation as an outcome.
Each study measured symptoms of depression using the Geriatric Depression Scale. Total scores range from 0 (better) to 30 (worse). The evidence was very uncertain and suggests that video calls may result in little to no difference in scores on the Geriatric Depression Scale compared to usual care at three months' follow‐up (MD 0.41, 95% CI −0.90 to 1.72; 3 studies; 201 participants) or six months' follow‐up (MD −0.83, 95% CI −2.43 to 0.76; 2 studies, 152 participants). The evidence suggests that video calls may have a small effect on symptoms of depression at one‐year follow‐up, though this finding is imprecise (MD −2.04, 95% CI −3.98 to −0.10; 1 study; 90 participants). We downgraded the certainty of this evidence by three levels for study limitations, imprecision and indirectness.
Only one study, with 62 participants, reported quality of life. The study measured quality of life using a Taiwanese adaptation of the Short‐Form 36‐question health survey (SF‐36), which consists of eight subscales that measure different aspects of quality of life: physical function; physical role; emotional role; social function; pain: vitality; mental health; and physical health. Each subscale is scored from 0 (poor health) to 100 (good health). The evidence is very uncertain and suggests that there may be little to no difference between people allocated to usual care and those allocated to video calls in three‐month scores in physical function (MD 2.88, 95% CI −5.01 to 10.77), physical role (MD −7.66, 95% CI −24.08 to 8.76), emotional role (MD −7.18, 95% CI −16.23 to 1.87), social function (MD 2.77, 95% CI −8.87 to 14.41), pain scores (MD −3.25, 95% CI −15.11 to 8.61), vitality scores (MD −3.60, 95% CI −9.01 to 1.81), mental health (MD 9.19, 95% CI 0.36 to 18.02) and physical health (MD 5.16, 95% CI −2.48 to 12.80). We downgraded the certainty of this evidence by three levels for study limitations, imprecision and indirectness.
Authors' conclusions
Based on this review there is currently very uncertain evidence on the effectiveness of video call interventions to reduce loneliness in older adults. The review did not include any studies that reported evidence of the effectiveness of video call interventions to address social isolation in older adults. The evidence regarding the effectiveness of video calls for outcomes of symptoms of depression was very uncertain.
Future research in this area needs to use more rigorous methods and more diverse and representative participants. Specifically, future studies should target older adults, who are demonstrably lonely or socially isolated, or both, across a range of settings to determine whether video call interventions are effective in a population in which these outcomes are in need of improvement.
Plain language summary
Video calls for reducing social isolation and loneliness in older people
Background
Coronavirus (COVID‐19) is a new virus that has spread quickly throughout the world. Countries have introduced restrictions on people’s movement to protect them from COVID‐19, but an unwanted result is that older people may feel lonely and isolated, which may lead to poor mental and physical health.
A video call is a phone call that uses an internet connection. Video calls allow callers to see – as well as hear – each other. This technology could help older people keep in touch with family and friends safely, and this may reduce their feelings of loneliness and social isolation.
What did we want to find out?
We wanted to find out if older people who used video calls felt less lonely than those who did not. We also looked at whether video calls affected symptoms of depression or quality of life.
Our methods
We looked for studies that randomly allocated older people to different groups to use either video calls, another method of keeping in touch, or no particular method (usual care), with the aim of examining their effects on loneliness or social isolation. For our review, we considered older people to be aged 65 years or above. We considered video calls to be calls made via the internet, using computers, tablets or smartphones.
COVID‐19 is spreading rapidly, so we needed to answer this question quickly. This meant that we shortened some steps of the normal Cochrane Review process. Two review authors checked 25% of our search results for studies and one review author checked the remaining 75% of our results, where normally two review authors would check all the results. Similarly, only one review author collected data and assessed the quality of the studies, and a second review author checked this work.
Results
We included three studies, with 201 participants, in our review. All three studies took place in nursing homes in Taiwan between 2010 and 2020 and compared video calls to usual care.
The evidence from these three studies suggests that video calls have little to no effect on loneliness after three, six or 12 months. There is also little to no difference in symptoms of depression after three or six months, although after a year, older people who used video calls may have had a small reduction in depression compared to those who received usual care. Similarly, video calls may make little to no difference to older people’s quality of life.
Certainty of the evidence
Our certainty (confidence) in the evidence was limited because we found few studies with a small number of participants, and they either used unreliable methods or did not fully describe their methods. Also, all of the participants were in nursing homes, so our findings may not apply to older people living in other places, such as their own homes. Also, some of the participants may not have been feeling lonely or socially isolated.
Conclusion
Based on the current evidence, we are unable to say whether video calls help to reduce loneliness in older people. We need more studies, that use rigorous methods to investigate this question, and focus on older people who are lonely or socially isolated.
Search date
This review includes evidence published up to 7 April 2020.
Summary of findings
Summary of findings 1. Videoconferencing interventions compared with usual care for reducing loneliness.
| Videoconferencing interventions compared with usual care for reducing loneliness | ||||
|
Patient or population: older adults Settings: nursing homes Intervention: use of the internet to facilitate video calls or video conferencing through computers, smartphones or tablets with the intention of reducing loneliness Comparison: usual care | ||||
| Outcomes | Illustrative comparative risks (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | |||
| Usual care | Intervention | |||
|
Loneliness Assessed with the UCLA Loneliness Scale Scale from 20 to 80 (higher = worse) |
The mean loneliness score across control groups was 48.45 | At 3 months' follow‐up, there was a mean difference of ‐0.44 (95% −3.28 to 2.41) | 201 (3) | ⊕⊕⊝⊝ Very lowa,b,c |
| Social Isolation | No studies reported this outcome | ‐ | 0 | ‐ |
|
Symptoms of depression Assessed with the Geriatric Depression Scale Scale from 0 to 30 (higher = worse) |
The mean score for symptoms of depression across control groups was 12.16 | At 3 months' follow‐up, there was a mean difference of 0.41 (95% CI −0.90 to 1.72) | 201 (3) | ⊕⊕⊝⊝ Very lowa,b,c |
|
Quality of life Assessed with a Taiwanese adaptation of the SF‐36 Scale from 0 to 100 (higher = better) |
The mean quality‐of‐life score across domains was 52.63 | There may be little to no difference between people allocated to usual care and those allocated to video calls in 3‐month scores:
|
62 (1) |
⊕⊕⊝⊝ Very lowa,b,c |
| CI: confidence interval; MD: mean difference; SF‐36: Short‐Form 36‐item health survey; UCLA: University of California, Los Angeles | ||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||
aDowngraded for high risk of bias in most studies. bDowngraded for indirectness as most studies focus on nursing homes rather than the general population. cDowngraded for serious imprecision.
Background
Description of the condition
The COVID‐19 pandemic has resulted in many countries implementing physical distancing and restriction of movement, particularly for older adults and other vulnerable populations. This requires millions of older people to remain in their homes, many of whom may be isolated from their usual social support network (Armitage 2020). Older people are the group most at risk in relation to COVID‐19 (Wu 2020), and in addition to the many isolating at home, many others are currently confined to nursing homes, rooms in old age homes and frail care units.
Loneliness and social isolation can be more commonly experienced in old age (Fakoya 2020). The two concepts are discrete but related. Loneliness has been defined as "a subjective negative feeling associated with a perceived lack of a wider social network (social loneliness) or the absence of a specific desired social companion (emotional loneliness)” and social isolation as “the objective lack or paucity of contacts and interactions with family members, friends or the wider community” (Valtorta 2012, p. 518). Associations between loneliness and depression (Cacioppo 2010), and loneliness and quality of life have been well established (Musich 2015; Singh 2015). Social isolation has also been shown to be associated with both depression (Ge 2017), and quality of life (Hawton 2011). Based on these links, we decided to also include depression and quality of life as secondary outcomes, which provide further indications of effects of the intervention, if any, on well‐being.
Loneliness and social isolation are identified consistently as risk factors for poor mental and physical health in older people (Courtin 2017). A range of interventions have been developed to reduce loneliness and social isolation among older adults (Fakoya 2020), with a recent focus on the use of video calls (Baker 2018; Chen 2016).
Description of the intervention
Video calls, which combine visual and audio communication between people in separate locations, may facilitate older people in staying connected during the current crisis. Video calls can be one‐to‐one with just two participants in separate locations or group calls involving multiple participants across multiple locations. Video calls are the focus of this review as it is thought that the combination of audio and video might be superior to audio alone in simulating real‐life contact and thus potentially addressing social isolation and feelings of loneliness in a time of physical distancing.
How the intervention might work
Video calls to reduce loneliness or social isolation may work by widening the participant’s social circle or by increasing frequency of contact with existing acquaintances (Valtorta 2012; Weiss 1973). This widened social circle or increased frequency of contact with existing acquaintances might therefore address social isolation which, as described above, refers to an objective lack of contacts and/or interactions with contacts. Feelings of loneliness, which refers to the perception that one’s social contacts are less than one would like in terms of quantity or quality, might also be addressed through the increased contact with new or existing contacts that video calls could provide. These interventions may involve unstructured video calls with family members or others (e.g. Tsai 2010), or more structured videoconferences with specific topics suggested for discussion (e.g. Tsai 2020).
As noted by Zamir and colleagues in their recent video call intervention study, social engagement and attachment theory point to the importance of seeing each other’s faces during communication and how important this face‐to‐face interaction and shared expressions and body language can be in maintaining social bonds and thus possibly reducing loneliness and social isolation (Porges 2003; Zamir 2018). This indicates that video calls may be more effective compared to audio alone.
There was a need for updated evidence in this area, as the last search of the primary effectiveness of digital interventions (including video calls) on social isolation was carried out in 2016 (Baker 2018).
Objectives
The primary objective of this rapid review is to assess the effectiveness of video calls for reducing social isolation and loneliness in older adults. The review also sought to address the effectiveness of video calls on symptoms of depression and quality of life.
Methods
Criteria for considering studies for this review
Study design
Randomised controlled trials (RCTs) and quasi‐RCTs (including cluster designs) were eligible for inclusion. We excluded all other study designs.
Population
Given the heterogeneity in the definition of older adults, for this review we defined older adults broadly as adults over the age of 65 years. We included studies that met other inclusion criteria and where the mean age of the sample was over 65 years of age as this is a commonly used cut‐off in aging research (Shenkin 2017). We included studies that included participants whether or not they were experiencing symptoms of loneliness or social isolation at baseline.
We excluded studies where the mean age of the participants was under the age of 65 years. We also excluded studies that included participants with major neurocognitive disorders, or sight and hearing impairments.
Intervention
We included studies that examined interventions that used the internet to facilitate video calls through computers, smartphones or tablets with the intention of reducing loneliness or social isolation, or both, in older adults.
For multiple‐component interventions, we included studies that examined interventions where video calls were a core component included in the intervention with the aim of reducing loneliness or social isolation, or both. We used Fixsen 2005's definition of 'a core component' as, "the most essential and indispensable components of an intervention".
We excluded interventions that did not use video calls or used video calls to deliver telemedicine. We followed the World Health Organization's definition of telemedicine, “The delivery of health care services, where distance is a critical factor, by all health care professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of health care providers, all in the interests of advancing the health of individuals and their communities.” (WHO 2010).
Comparator(s)
Studies could compare the intervention of interest to an alternative intervention (e.g. in‐person visits, chat bots, phone calls), usual care or waitlist control groups.
Outcome(s)
We included studies in the review if they were reported in a peer‐reviewed journal and included any of the outcomes below, irrespective of whether the measured outcome data were reported and irrespective of the psychometric properties of the measures employed. We excluded studies if they did not report measures of any of these outcomes.
Primary outcomes
Self‐report measures of loneliness (i.e. scores on any self‐report questionnaire that is designed to quantify how lonely a person feels)
Self‐report measures of social isolation (i.e. scores on any self‐report questionnaire that is designed to quantify the extent to which a person is socially isolated)
Secondary outcomes
Self‐report measures of symptoms of depression (i.e. scores on any self‐report questionnaire that is designed to quantify the severity of symptoms of depression experienced by a person)
Self‐report measures of quality of life (i.e. scores on any self‐report questionnaire that is designed to allow people to rate their quality of life, either overall or within specific domains)
Search methods for identification of studies
We adhered to the following methods prespecified in the protocol (Noone 2020).
An experienced information specialist (MS) designed and conducted all searches, which were verified by a content expert (AB) and independently peer reviewed (Robin Featherstone).
Electronic databases
We searched the following databases. See Appendix 1 for the search strategy.
Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 4) in the Cochrane Library (searched 7 April 2020);
MEDLINE (via OVID; 1 January 2004 to 7 April 2020);
PsycINFO (via Ovid; 1 January 2004 to 7 April 2020);
CINAHL (via EBSCO; 1 January 2004 to 7 April 2020).
Other searches
We searched the references of relevant systematic reviews included in three reviews of reviews on reducing social isolation and loneliness in older adults using technology (Chipps 2017; Fakoya 2020; Jarvis 2019).
Screening
Two review authors (JMS, AB) screened 25% of abstracts, with conflict resolution by another review author (CN). A single review author (JMS) screened the remaining abstracts. The second review author (AB) screened all excluded abstracts and we resolved conflicts by consensus and the involvement of a third review author (CN). We followed the same process for full‐text articles. We excluded conference abstracts and conference proceedings. We used Covidence to conduct screening. We recorded reasons for exclusion for all studies excluded after full‐text review and have documented them in the Characteristics of excluded studies table.
Inclusion of non‐English language studies
We excluded abstracts and full‐text articles in non‐English languages.
Data collection and analysis
We adhered to the following methods prespecified in the protocol (Noone 2020).
Data extraction and management
We extracted data using pilot‐tested data extraction forms in Microsoft Excel (Microsoft Corporation 2018). CN performed data extraction, which EM checked using a piloted form. We extracted the following data.
Report characteristics (which included year, authors, title, journal and source of funding)
Study design (which included methods, location, groups, and number of participants)
Participant characteristics (which included age, gender, and any morbidities)
Intervention characteristics (which included setting, type of video call technology used, person contacted, mode of delivery, duration of the intervention and follow‐up periods)
Comparator characteristics
Outcomes assessed and measures
Numerical data for outcomes of interest (which included means and standard deviation at each follow‐up)
Information relevant to 'Risk of bias' assessment
Assessment of risk of bias in included studies
One review author (EM) applied the Cochrane RCT 'Risk of bias' tool to the included studies for each primary outcome and a second review author (CN) verified their judgments (Higgins 2017).
Other sources of bias included those related to clustering, that is: recruitment bias; baseline imbalance; loss of clusters; incorrect analysis; and comparability with individually randomised trials.
We deemed studies to be at highest risk of bias overall if they were scored at high or unclear risk of bias for the sequence generation or the allocation concealment domain (Higgins 2017).
We resolved discrepancies by discussion. We visualised the 'Risk of bias' assessments using robvis (McGuinness 2019).
Contacting study authors
We contacted study authors to clarify issues related to clustering within the studies included for meta‐analysis.
Measures of treatment effect
We computed mean differences and 95% confidence intervals as a measure of the treatment effect for each outcome at each follow‐up.
Unit of analysis issues
The included studies all involved clustered data. The studies did not state clearly whether they accounted for clustering and the study authors confirmed that they did not account for clustering (Tsai 2020 [pers comm]). For the current analyses, we assumed intra‐cluster coefficient (ICC) values of 0.01 to adjust for clustering in the meta‐analysis. In the absence of data that we could use to calculate the ICC, we chose this value as it has been reported to be common in health research (Killip 2004). We also did a sensitivity analysis using an ICC of 0.05, since values below 0.05 are typical (Deeks 2019).
Assessment of heterogeneity
We assessed the presence of heterogeneity by inspecting forest plots, conducting a Chi2 test for heterogeneity (P < 0.10; Sutton 2000), and calculating the I2 statistic (Higgins 2003). We considered that an I2 statistic value of 30% to 60% may represent moderate heterogeneity; while 50% to 90% may represent substantial heterogeneity; and 75% to 100% may represent considerable heterogeneity (Deeks 2019).
Assessment of reporting biases
There were not enough data to assess reporting biases.
Data synthesis
We conducted fixed‐effect meta‐analyses for the outcomes of loneliness and symptoms of depression at follow‐ups of three months, six months and 12 months.
Subgroup analyses
The only planned analysis was a comparison between studies conducted in nursing homes and studies conducted in home settings. However, all included studies took place in nursing homes, so we did not conduct this analysis.
Sensitivity analyses
We planned to conduct a sensitivity analysis by excluding studies at high risk of bias in relation to random sequence generation, incomplete outcome data or allocation sequence concealment. However, all studies included for meta‐analysis were at high risk of bias for incomplete outcome data, and unclear risk of bias for random sequence generation and allocation sequence concealment for the outcome of loneliness, so we did not conduct these analyses. We conducted unplanned sensitivity analyses using a 0.05 ICC value to adjust for clustering in the meta‐analysed studies.
Summary of findings and assessment of the certainty of the evidence
We created a 'Summary of findings' table using standard Cochrane methodology to present results at three months' follow‐up for each outcome (Schünemann 2019). We applied the GRADE approach to assess the certainty of the body of evidence to all outcomes of interest. A single review author (EM) applied GRADE and a second review author (CN) verified all judgements and added rationales for judgements to footnotes (CN).
Results
Description of studies
Results of the search
We carried out searches on 7 April 2020. We screened 1802 abstracts and excluded 1778 records. We assessed 24 full‐text articles. Three studies met the inclusion criteria and we excluded 21 studies. We have summarised the screening process in Figure 1 (Moher 2009). We have presented the ratings of the certainty of the evidence for the primary outcomes in Table 2.
1.
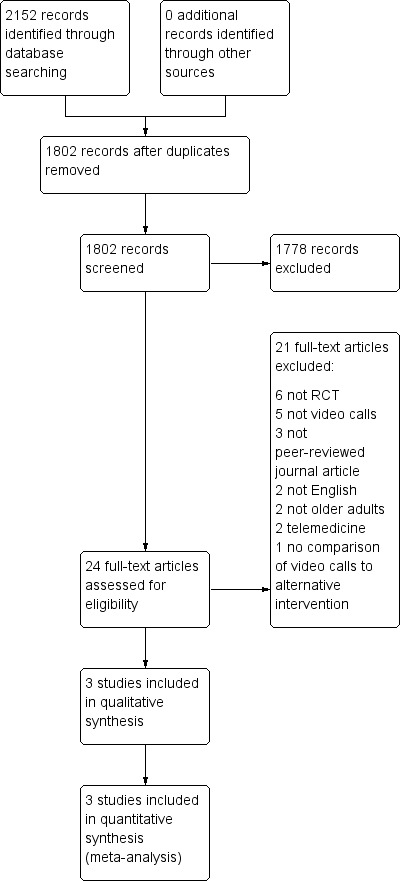
Study flow diagram
1. Certainty of evidence ratings for the effectiveness of video call interventions.
| Outcome | Number of studies | Risk of bias | Indirectness | Imprecision | Inconsistency | Other considerations | Summary effect size/outcome | Certainty of the evidence |
| Loneliness | 3 | Very serious | No serious inconsistency | Serious | Serious | None | No effect | Very low |
| Social Isolation | 0 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Symptoms of depression | 3 | Very serious | No serious inconsistency | Serious | Serious | None | No effect | Very low |
|
Quality of life |
1 | Very serious | No serious inconsistency | Serious | Serious | None | No effect | Very low |
Included studies
We identified three cluster quasi‐randomised trials (Tsai 2010; Tsai 2011; Tsai 2020). All these studies focused on participants with a mean age of 65 years or older. The included studies compared video call interventions to usual care in nursing homes. All three studies measured loneliness using the UCLA Loneliness Scale. This scale has been validated for use in older adults (Tsai 2007). None of the studies reported measures of social isolation. All three studies measured symptoms of depression using the Geriatric Depression Scale, which has been extensively validated (Stiles 1998). Just one study reported a measure of quality of life and it used a Taiwanese adaptation of the Short‐Form 36‐questions health survey (SF‐36; Tsai 2020). This scale has been validated for use in older adults in Taiwan (Huang 2006). All three studies were conducted in Taiwan and were led by the same author.
The interventions in the included studies were similar in that each involved the use of video calls once per week for at least five minutes to facilitate communication between nursing home residents and members of their family. Research assistants facilitated these calls in two of the studies (Tsai 2010; Tsai 2011), while in the third, they were facilitated by both research assistants and staff (Tsai 2020). The technology used varied across the studies. Two studies used laptops to facilitate video calls (Tsai 2010; Tsai 2011), and the third used smartphones (Tsai 2020). The interventions in all three of these studies were intended to reduce loneliness in those who received the intervention. The mean baseline score on the UCLA Loneliness Scale across all of the included studies was 51 out of possible 80, with higher scores indicating more loneliness.
Excluded studies
Most studies that we excluded used a design other than RCT or quasi‐RCT or did not report a relevant intervention. The Characteristics of excluded studies table outlines the reasons for exclusion of each study.
Risk of bias in included studies
For loneliness, we judged overall risk of bias to be high (see Figure 2; Figure 3). None of the included studies reported social isolation as an outcome which precluded judgment of the risk of bias for this outcome.
2.
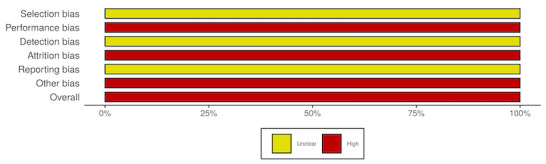
'Risk of bias' graph for loneliness: review authors' judgements about each 'Risk of bias' item presented as percentages across all included studies
3.
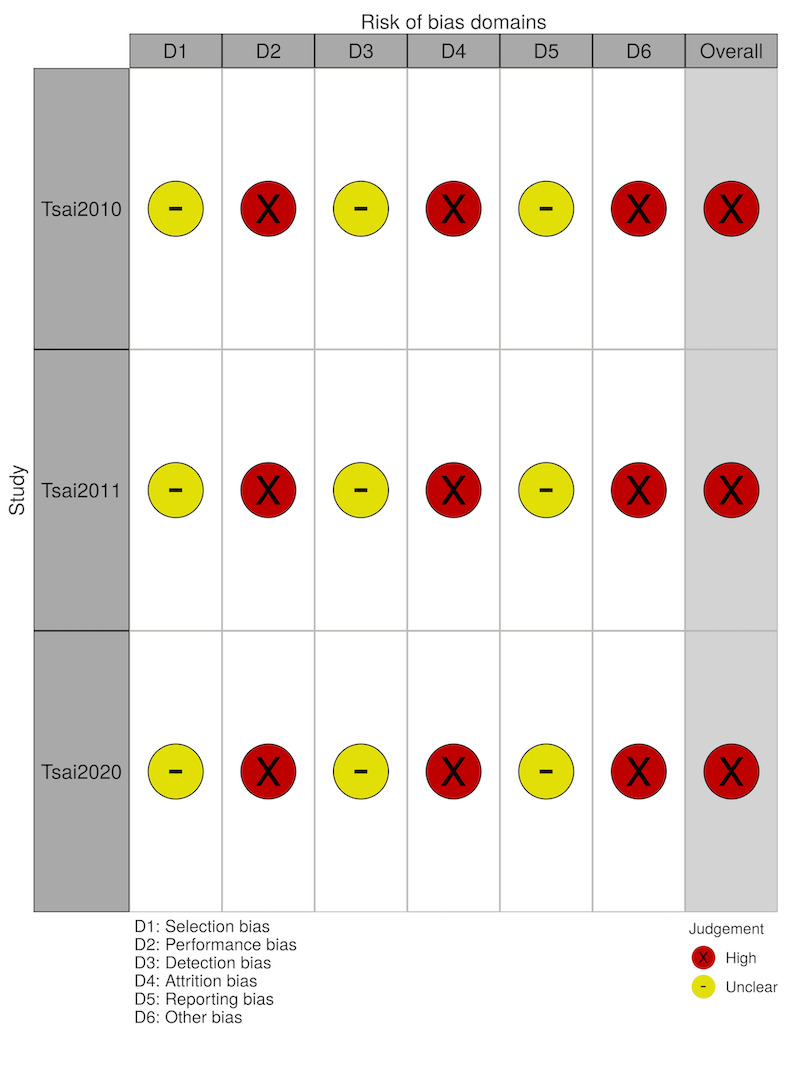
'Risk of bias' summary for loneliness: review authors' judgements about each 'Risk of bias' item for each included study
Selection Bias
In terms of selection bias, none of the studies adequately described their randomisation or allocation procedures to allow judgement.
Performance Bias
We judged risk of performance bias to be high in each study (Tsai 2010; Tsai 2011; Tsai 2020). This is because the nature of these studies meant that allocation concealment was not possible.
Detection Bias
None of the studies describe in enough detail their methods for assessing to allow judgement of detection bias.
Attrition Bias
We judged attrition bias to be high as the study authors did not use an intention‐to‐treat approach to analysis, despite having missing data at follow‐up.
Reporting Bias
None of the three studies made any reference to study protocol or analysis intentions, precluding judgment of reporting bias.
Other Sources of Bias
Other possible sources of bias included those related to clustering. We judged this domain to have a high risk of bias as none of the studies adjusted for the clustered nature of the data (Tsai 2020 [pers comm]).
Effects of interventions
Data were available for the primary outcome, loneliness, and the secondary outcomes, symptoms of depression and quality of life. However, not every included study reported these outcomes. We present narrative syntheses for each outcome and meta‐analyses for loneliness and depression.
Loneliness
The included studies compared the effects on loneliness of videoconferencing interventions compared with usual care (Tsai 2010; Tsai 2011; Tsai 2020). Each study measured loneliness using the UCLA Loneliness Scale, which consists of 10 items with 4‐point Likert scales. Total scores range from 20 (least lonely) to 80 (most lonely). Assuming an ICC of 0.01, the evidence was very uncertain and suggests that video calls may result in little to no difference in loneliness compared to usual care at three months (MD −0.44, 95% CI −3.28 to 2.41; 3 studies, 201 participants), at six months (MD −0.34, 95% CI −3.41 to 2.72; 2 studies, 152 participants) and at 12 months (MD −2.40, 95% CI −7.20 to 2.40; 1 study, 90 participants; very low‐certainty evidence; Analysis 1.1; Figure 4). A sensitivity analysis assuming an ICC of 0.05, resulted in the same conclusion at three months (MD −0.43, 95% CI −3.56 to 2.70; 3 studies, 201 participants), six months (MD −0.40, 95% CI −3.80 to 3.01; 2 studies, 152 participants), and 12 months (MD −2.40, 95% CI −7.61 to 2.81; 1 study, 90 participants; Analysis 1.2; Figure 5). We downgraded the certainty of this evidence by three levels for study limitations, imprecision and indirectness.
1.1. Analysis.

Comparison 1: Video calls versus usual care, Outcome 1: Loneliness (ICC = 0.01)
4.

Forest plot of comparison 1. Video calls versus usual care, outcome 1.1, loneliness (ICC = 0.01)
1.2. Analysis.

Comparison 1: Video calls versus usual care, Outcome 2: Loneliness (ICC = 0.05)
5.

Forest plot of comparison 1. Video calls versus usual care, outcome 1.3, loneliness (ICC = 0.05)
Social isolation
None of the included studies reported this outcome.
Symptoms of depression
Three studies comparing video calls and usual care examined symptoms of depression using the Geriatric Depression Scale (Tsai 2010; Tsai 2011; Tsai 2020). This scale consists of 30 yes or no items. Total scores range from 0 (better) to 30 (worse). Assuming an ICC of 0.01, the evidence suggests that video calls may result in little to no difference in symptoms of depression compared to usual care at three months' follow‐up (MD 0.41, 95% CI −0.90 to 1.72; 3 studies; 201 participants) or six months' follow−up (MD −0.83, 95% CI −2.43 to 0.76; 2 studies; 152 participants). The evidence suggests that video calls may have a small effect on symptoms of depression at 12‐month follow‐up, though this finding is imprecise (MD −2.04, 95% CI −3.98 to −0.10; 1 study, 90 participants; Analysis 1.4; Figure 6). A sensitivity analysis assuming an ICC of 0.05 suggests that video calls may result in little to no difference in symptoms of depression compared to usual care at three months (MD 0.45, 95% CI −0.97 to 1.87; 3 studies, 201 participants), six months (MD −0.87, 95% CI −2.63 to 0.90; 2 studies, 152 participants) or 12 months (MD −2.04, 95% CI −4.14 to 0.06; 1 study; 90 participants; Analysis 1.5; Figure 7). We downgraded the certainty of this evidence by three levels for study limitations, imprecision and indirectness.
1.4. Analysis.

Comparison 1: Video calls versus usual care, Outcome 4: Depression (ICC = 0.01)
6.

Forest plot of comparison 1. Video calls versus usual care, outcome 1.2, depression (ICC = 0.01)
1.5. Analysis.

Comparison 1: Video calls versus usual care, Outcome 5: Depression (ICC = 0.05)
7.

Forest plot of comparison 1. Video calls versus usual care, outcome 1.4, depression (ICC = 0.05)
Quality of life
Only one study, with 62 participants, reported quality of life (Tsai 2020). It was measured using a Taiwanese adaptation of the SF‐36, which consists of eight subscales that measure different aspects of quality of life: physical function; physical role; emotional role; social function; pain; vitality; mental health; and physical health on a scale of 0 (poor health) to 100 (good health).
There may be little to no difference between people allocated to usual care and those allocated to video calls in one‐month scores in physical function (MD 1.50, 95% CI −7.66 to 10.66), physical role (MD −24.17, 95% CI −41.62 to 6.72), emotional role (MD −3.33, 95% CI −15.39 to 8.73), social function (MD −10.41, 95% CI −23.20 to 2.38), pain scores (MD −11.14, 95% CI −22.77 to 0.49), vitality scores (MD −6.17, 95% CI −12.97 to 0.63), mental health (MD 2.00, 95% CI −7.52 to 11.52) and physical health (MD 1.54, 95% CI −6.31 to 9.39).
Similarly, there may be little to no difference between people allocated to usual care and those allocated to video calls in three‐month scores in physical function (MD 2.88, 95% CI −5.01 to 10.77), physical role (MD −7.66, 95% CI −24.08 to 8.76), emotional role (MD −7.18, 95% CI −16.23 to 1.87), social function (MD 2.77, 95% CI −8.87 to 14.41), pain scores (MD −3.25, 95% CI −15.11 to 8.61), vitality scores (MD −3.60, 95% CI −9.01 to 1.81), mental health (MD 9.19, 95% CI 0.36 to 18.02) and physical health (MD 5.16, 95% CI −2.48 to 12.80).
Finally, there may be little to no difference between people allocated to usual care and those allocated to video calls in six‐month scores in physical function (MD −4.48, 95% CI −10.42 to 1.46), physical role (MD 8.17, 95% CI −7.19 to 23.53), emotional role (MD −3.59, 95% CI −12.36 to 5.18), social function (MD 9.52, 95% CI −0.41 to 19.45), pain scores (MD −1.73, 95% CI −12.68 to 9.22), vitality scores (MD 3.63, 95% CI −1.70 to 8.96), mental health (MD 5.23, 95% CI −2.86 to 13.32) and physical health (MD 0.93, 95% CI −5.39 to 7.25).
We downgraded the certainty of this evidence by three levels for study limitations, imprecision and indirectness.
Discussion
Summary of main findings
This rapid review found very‐low certainty evidence to support the effectiveness of video calls for reducing loneliness in older people. The included studies also produced imprecise evidence regarding the effectiveness of video calls for outcomes of symptoms of depression and quality of life. None of the studies were of high quality and none reported measures of social isolation. Therefore, the evidence available for addressing the objectives of this review is limited.
Limitations in the body of evidence
We rated the certainty of the evidence using GRADE and found very low‐certainty evidence for loneliness. This suggests that it is possible that further research may have an impact on our effect estimates and confidence in the estimates. The certainty of the evidence is shown in Table 2. These ratings reflect concerns about imprecision (the combined number of participants is very low), indirectness (the population of the three studies was limited to nursing home residents only), and possible publication bias (we could not address this statistically as the number of included studies was too low). We judged the risk of bias for each study to be high. This is because blinding was not possible in the studies due to the nature of the intervention, none of the studies used an intention‐to‐treat approach to analysis, despite each having missing data at follow‐up, and none of the studies adjusted for the clustered nature of the data (Tsai 2020 [pers comm]). We judged the remaining 'Risk of bias' domains to be unclear due to a lack of adequate description in the methods. Given the high risk of bias for the loneliness outcome, the results should be interpreted cautiously.
In addition, the generalisability of the evidence is limited since all of the included studies took place in nursing homes in Taiwan and were led by the same author.
A major limitation of this body of evidence is that the included studies did not specifically recruit older adults who were demonstrably lonely or socially isolated to determine whether video call interventions are effective in a population in which these outcomes are in need of improvement.
Limitations of the review
By following the Cochrane Rapid Reviews Methods Group guidelines, this review deviates in several ways from standard Cochrane methodology. Our review was limited to articles in peer‐reviewed journals, so we did not consider grey literature, conference abstracts and proceedings, or preprints. We also excluded articles in non‐English languages, which may have resulted in the exclusion of potentially relevant articles. In addition, we took steps to reduce the time spent screening by only dually screening 25% of abstracts and full texts, and checking excluded studies. We also carried out data collection in an expedited manner by using a single review author with checks by a second review author for data extraction, 'Risk of bias' assessment and application of the GRADE approach.
The meta‐analyses that we conducted were limited by the lack of available data that would have allowed the calculation of accurate ICC values for each study.
There is considerable variation in the definition of older adults, and for this review, we defined older adults broadly as adults over the age of 65 years. Previous reviews have included articles that self‐identified as focusing on older adults instead of specifying a lower age limit (Fakoya 2020). Our use of an inclusion criterion based on a somewhat arbitrary age cut‐off is a potential limitation of this review and the lack of clarity in defining older populations is a challenge for research in this area more generally. Notably, none of the studies we excluded based on this criterion would have been included had we included articles that self‐identified as focusing on older adults instead.
The exclusive focus on video calls in this review limits its applicability globally as smartphone and internet use is much lower in emerging economies compared to advanced economies (Pew Research Center 2019).
Our review was limited to RCTs that examined the effectiveness of interventions in which a core component involved the use of video calls and we identified only three eligible studies. Exploring information and communications technology more broadly and including a wider range of study designs may have identified more evidence on the role of technology in reducing loneliness and social isolation among older people. For example, an umbrella review of interventions to reduce loneliness in older adults found that, in general, digital interventions may have a greater effect than non‐digital interventions (Jarvis 2019). However, this analysis included a small number of studies with diverse characteristics. Similarly, a review of systematic reviews on the reduction of social isolation in older adults through digital interventions found weak and inconsistent evidence regarding their effectiveness (Chipps 2017). Another review with a similar focus but broader inclusion criteria found that most of the studies examining the use of technology to reduce loneliness and social isolation among older adults employed qualitative methods (Baker 2018). This review found that video call interventions tend to give participants a sense of their communication partner being present. The review also emphasised that there is a need for high‐quality studies of the effectiveness of these interventions. The results of these reviews appear to be consistent with the findings of our review.
Authors' conclusions
Implications for practice
Based on this review there is currently very uncertain evidence on the effectiveness of video call interventions to reduce loneliness in older adults. The review did not include any studies that reported evidence on the effectiveness of video call interventions to address social isolation in older adults. The evidence regarding the effectiveness of video calls for outcomes of symptoms of depression and quality of life were imprecise and at high risk of bias due to study limitations.
Implications for research
Given the very small number of studies included in this review (and considering the current pandemic and associated physical distancing measures) further studies testing the effectiveness of video calls for loneliness or isolation in older adults are needed. Beyond the limited number of studies to date, attention is also needed towards the rigour within studies given the current low participant numbers observed and lack of pre‐registered designs and analysis plans. Finally, more diverse stakeholder groups and settings are needed in future studies, given the current homogeneity of populations with a strong focus on nursing home residents observed. Specifically, future studies should target older adults across a range of settings who are demonstrably lonely or socially isolated, or both, to determine whether video call interventions are effective in a population in which these outcomes are in need of improvement.
What's new
| Date | Event | Description |
|---|---|---|
| 24 July 2020 | Amended | Republished to change the review type from Prototype to Rapid (no changes to content) |
History
Review first published: Issue 5, 2020
Acknowledgements
Thanks to Robin Featherstone, Cochrane Information Specialist, for her work on topic refinement and reviewing the search strategy.
Thanks to the Cochrane Editorial and Methods Department (EMD) Editorial Service, including Helen Wakeford, Anne‐Marie Stephani, Liz Bickerdike and Jenny Bellorini, who managed the editorial process for this review, and Denise Mitchell, who copy‐edited this review.
Thank you to the peer reviewers: Thea Franke, Peter Schulz and Jennifer Chipps.
Thanks to Martin Burton of the Analysis of Review Group Output for valuable feedback.
Thanks to Andy Anglmeyer for acting as methods editor for this review.
Thanks to Luke Wolfenden, joint Co‐ordinating Editor of Cochrane Public Health, for editing this review.
Appendices
Appendix 1. Search strategy
Database(s): Ovid MEDLINE(R) and Epub Ahead of Print, In‐Process & Other Non‐Indexed Citations, Daily and Versions(R) 1 January 1946 to 7 April 2020
1. exp Aged/ (3074019)
2. exp Geriatrics/ (29740)
3. Homes for the Aged/ (13720)
4. Nursing Homes/ (34370)
5. (elderly or ageing or aging or aged or geriatric* or senior* or old age or late* life or elder* care).tw,kf. (1020033)
6. (Nursing home* or retirement home*).tw,kf. (30363)
7. (older adj3 (age or m?n or male** or wom?n or female* or people or adult* or population or person*)).tw,kf. (215543)
8. ("65 year*" or "over 65" or "over 70" or "over 75" or "over 80" or "over 85" or "85 year*").tw,kf. (125062)
9. or/1‐8 (3788892)
10. exp Computer Communication Networks/ (90964)
11. exp Videoconferencing/ (1774)
12. (voice over internet protocol or VoIP or video call* or videoconferenc* or video conferenc* or videophone communication).tw,kf. (2954)
13. (mobile phone* or smartphone* or smart phone* or cell phone* or cellular phone* or viber or viber app or skype or video call* or facetime or WhatsApp or ICTs or iPAD or iPhone or google hangouts).tw,kf. (24396)
14. ((virtual or online) adj3 communication*).tw,kf. (783)
15. (tablet adj3 (device* or comput*)).tw,kf. (1366)
16. or/10‐15 (117689)
17. Social Isolation/ (13059)
18. *Loneliness/ (2082)
19. *Quarantine/ (958)
20. (Seclu* or confin* or separat* or quarantine* or alienat* or solitude or remote* or aloneness or alone or lonel* or emotional deprivation).tw,kf. (1436225)
21. (social adj2 (alienat* or isolat* or exclu* or deprivation or network or support or contact or connect* or engagement or participat*)).tw,kf. (66621)
22. Depression/ (116161)
23. "Quality of Life"/ (190202)
24. (depress* or life qualit* or living qualit* or QoL).tw,kf. (493152)
25. or/17‐24 (2102184)
26. 9 and 16 and 25 (3086)
27. randomized controlled trial.pt. (503262)
28. controlled clinical trial.pt. (93600)
29. randomized.ab. (475105)
30. placebo.ab. (206579)
31. clinical trials as topic.sh. (190638)
32. randomly.ab. (330506)
33. trial.ti. (216002)
34. or/27‐33 (1279416)
35. exp animals/ not humans.sh. (4686037)
36. 34 not 35 (1177000)
37. 26 and 36 (920)
38. limit 37 to yr="2004 ‐Current" (904)
Database(s): CINAHL Plus (via EBSCOhost)
| Line # | Query |
| S26 | S9 AND S16 AND S24 (2004‐ Current) |
| S25 | S9 AND S16 AND S24 |
| S24 | S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 |
| S23 | TI ( (depress* or “life qualit*” or “living qualit*” or QoL) ) OR AB ( (depress* or “life qualit*” or “living qualit*” or QoL) ) |
| S22 | (MH "Quality of Life+") |
| S21 | (MH "Depression+") |
| S20 | (social n2 (alienat* or isolat* or exclu* or deprivation or network or support or contact or connect* or engagement or participat*) |
| S19 | TI ( (Seclu* or confin* or separat* or quarantine* or solitude or remote* or aloneness or alone or lonel* or “emotional deprivation”) ) OR AB ( (Seclu* or confin* or separat* or quarantine* or solitude or remote* or aloneness or alone or lonel* or “emotional deprivation”) ) |
| S18 | (MH "Quarantine") |
| S17 | (MH "Social Isolation+") |
| S16 | S10 OR S11 OR S12 OR S13 OR S14 OR S15 |
| S15 | tablet n3 (device* or comput*) |
| S14 | (virtual or online) n3 communication* |
| S13 | TI ( (“mobile phone*” or smartphone* or “smart phone*” or “cell phone*” or “cellular phone*” or viber or “viber app” or skype or “video call*” or facetime or WhatsApp or ICTs or iPAD or iPhone or “google hangouts”) ) OR AB ( (“mobile phone*” or smartphone* or “smart phone*” or “cell phone*” or “cellular phone*” or viber or “viber app” or skype or “video call*” or facetime or WhatsApp or ICTs or iPAD or iPhone or “google hangouts”) ) |
| S12 | TI ( (voice over internet protocol or VoIP or “video call*” or videoconferenc* or “video conferenc*” or “videophone communication”) ) OR AB ( (voice over internet protocol or VoIP or “video call*” or videoconferenc* or “video conferenc*” or “videophone communication”) ) |
| S11 | (MH "Computer Communication Networks") |
| S10 | (MH "Videoconferencing") |
| S9 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 |
| S8 | TI ( ("65 year*" or "over 65" or "over 70" or "over 75" or "over 80" or "over 85" or "85 year*") ) OR AB ( ("65 year*" or "over 65" or "over 70" or "over 75" or "over 80" or "over 85" or "85 year*") ) |
| S7 | TI ( (“Nursing home*” or “retirement home*” or “care home*” or “aged nursing home” or “care facilit*” or “homes for the aged”) ) OR AB ( (“Nursing home*” or “retirement home*” or “care home*” or “aged nursing home” or “care facilit*” or “homes for the aged”) ) |
| S6 | (old* n1 (age or m?n or male* or wom?n or female* or people or adult* or population or person*) |
| S5 | TI ( (elderly or ageing or aging or aged or geriatric* or senior* or “old age” or “late* life” or “elder* care”) ) OR AB ( (elderly or ageing or aging or aged or geriatric* or senior* or “old age” or “late* life” or “elder* care”) ) |
| S4 | (MH "Housing for the Elderly") |
| S3 | (MH "Nursing Homes") |
| S2 | (MH "Geriatrics") |
| S1 | (MH "Aged+") |
Database(s): APA PsycInfo 1806 to March Week 4 2020
1. exp Aging/
2. exp Geriatrics/
3. exp residential care institutions/
4. Elder Care/
5. (elderly or ageing or aging or aged or geriatric* or senior* or old age or late* life or elder* care).tw.
6. (Nursing home* or retirement home*).tw.
7. (old* adj3 (age or m?n or male* or wom?n or female* or people or adult* or population or pe. son*)).tw.
8. ("65 year*" or "over 65" or "over 70" or "over 75" or "over 80" or "over 85" or "85 year*").tw.
9. "homes for the aged".tw.
10. or/1‐9
11. exp videoconferencing/
12. exp computer mediated communication/
13. (voice over internet protocol or VoIP or video call* or videoconferenc* or video conferenc* or videophone communication).tw.
14. (mobile phone* or smartphone* or smart phone* or cell phone* or cellular phone* or viber or viber app or skype or video call* or facetime or WhatsApp or ICTs or iPAD or iPhone or google hangouts).tw.
15. ((virtual or online) adj3 communication*).tw.
16. (tablet adj3 (device* or comput*)).tw.
17. or/11‐16
18. Social Isolation/
19. loneliness/
20. (Seclu* or confin* or separat* or quarantine* or solitude or remote* or aloneness or alone or lonel* or emotional deprivation).tw.
21. (social adj2 (alienat* or isolat* or exclu* or deprivation or network or support or contact or connect* or engagement or participat*)).tw.
22. exp Major Depression/
23. exp "Quality of Life"/
24. (depress* or life qualit* or living qualit* or QoL).tw.
25. or/18‐24
26. 10 and 17 and 25
27. limit 26 to yr="2004 ‐Current"
Data and analyses
Comparison 1. Video calls versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Loneliness (ICC = 0.01) | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1.1 3 months | 3 | Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐3.28, 2.41] | |
| 1.1.2 6 months | 2 | Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐3.41, 2.72] | |
| 1.1.3 1 year | 1 | Mean Difference (IV, Random, 95% CI) | ‐2.40 [‐7.20, 2.40] | |
| 1.2 Loneliness (ICC = 0.05) | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.2.1 3 months | 3 | Mean Difference (IV, Fixed, 95% CI) | ‐0.43 [‐3.56, 2.70] | |
| 1.2.2 6 months | 2 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐3.80, 3.01] | |
| 1.2.3 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | ‐2.40 [‐7.61, 2.81] | |
| 1.3 Social isolation | 0 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.4 Depression (ICC = 0.01) | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.4.1 3 months | 3 | Mean Difference (IV, Fixed, 95% CI) | 0.41 [‐0.90, 1.72] | |
| 1.4.2 6 months | 2 | Mean Difference (IV, Fixed, 95% CI) | ‐0.83 [‐2.43, 0.76] | |
| 1.4.3 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | ‐2.04 [‐3.98, ‐0.10] | |
| 1.5 Depression (ICC = 0.05) | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.5.1 3 months | 3 | Mean Difference (IV, Fixed, 95% CI) | 0.45 [‐0.97, 1.87] | |
| 1.5.2 6 months | 2 | Mean Difference (IV, Fixed, 95% CI) | ‐0.87 [‐2.63, 0.90] | |
| 1.5.3 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | ‐2.04 [‐4.14, 0.06] | |
| 1.6 Quality of life ‐ physical function | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.6.1 1 month | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.6.2 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.6.3 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.7 Quality of life ‐ physical role | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.7.1 1 month | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.7.2 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.7.3 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.8 Quality of life ‐ emotional role | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.8.1 1 month | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.8.2 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.8.3 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.9 Quality of life ‐ social function | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.9.1 1 month | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.9.2 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.9.3 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.10 Quality of life ‐ pain | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.10.1 1 month | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.10.2 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.10.3 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.11 Quality of life ‐ vitality | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.11.1 1 month | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.11.2 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.11.3 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.12 Quality of life ‐ mental health | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.12.1 1 month | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.12.2 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.12.3 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.13 Quality of life ‐ physical health | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.13.1 1 month | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.13.2 3 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.13.3 6 months | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
1.3. Analysis.

Comparison 1: Video calls versus usual care, Outcome 3: Social isolation
1.6. Analysis.

Comparison 1: Video calls versus usual care, Outcome 6: Quality of life ‐ physical function
1.7. Analysis.

Comparison 1: Video calls versus usual care, Outcome 7: Quality of life ‐ physical role
1.8. Analysis.

Comparison 1: Video calls versus usual care, Outcome 8: Quality of life ‐ emotional role
1.9. Analysis.

Comparison 1: Video calls versus usual care, Outcome 9: Quality of life ‐ social function
1.10. Analysis.

Comparison 1: Video calls versus usual care, Outcome 10: Quality of life ‐ pain
1.11. Analysis.

Comparison 1: Video calls versus usual care, Outcome 11: Quality of life ‐ vitality
1.12. Analysis.

Comparison 1: Video calls versus usual care, Outcome 12: Quality of life ‐ mental health
1.13. Analysis.

Comparison 1: Video calls versus usual care, Outcome 13: Quality of life ‐ physical health
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Tsai 2010.
| Study characteristics | ||
| Method | Quasi‐RCT | |
| Participants | Participants were recruited from participating nursing homes in Taiwan. The mean age of the control group was 78.48 and the mean age in the intervention group was 74.42. In the control group, 57.6% of participants were female and 58.3% of the participants in the intervention group were female. | |
| Intervention | A trained research assistant helped the participants to use the videoconference technology and spent at least 5 min/week with the participants at the appointment time for their videoconference with family members. | |
| Usual care | ||
| Notes | ||
| Item | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias): loneliness | Unclear | Not enough information available for judgement |
| Allocation concealment (selection bias): loneliness | Unclear | Not enough information available for judgement |
| Blinding of participants and personnel (performance bias) | No | Nursing homes were cluster‐randomised. The participants probably did know which group they were allocated to as recruitment happened after randomisation. It would be difficult to blind participants and personnel due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear | No detail provided on who conducted the outcome assessment and whether they were blinded. |
| Incomplete outcome data (attrition bias): loneliness | No | Used per protocol analysis |
| Selective reporting (reporting bias): loneliness | Unclear | No reference made to a protocol or analysis intentions |
Tsai 2011.
| Study characteristics | ||
| Method | Quasi‐RCT | |
| Participants | Participants were recruited from participating nursing homes in Taiwan. The mean age of the control group was 79.26 and the mean age in the intervention group was 73.82. In the control group, 60% of participants were female and 55% of the participants in the intervention group were female. | |
| Intervention | For the first 3 months, a trained research assistant helped the participants to use the videoconference technology in a private room to contact family members. Then, for the next 9 months, participants were helped by trained nursing home staff. | |
| Usual care | ||
| Notes | ||
| Item | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias): loneliness | Unclear | Not enough information available for judgement |
| Allocation concealment (selection bias): loneliness | Unclear | Not enough information available for judgement |
| Blinding of participants and personnel (performance bias) | No | Nursing homes were cluster‐randomised. The participants probably did know which group they were allocated to as recruitment happened after randomisation. It would be difficult to blind participants and personnel due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear | No detail provided on who conducted the outcome assessment and whether they were blinded. |
| Incomplete outcome data (attrition bias): loneliness | No | Used per protocol analysis and did not report follow‐up data at 9 months |
| Selective reporting (reporting bias): loneliness | Unclear | No reference made to a protocol or analysis intentions |
Tsai 2020.
| Study characteristics | ||
| Method | Quasi‐RCT | |
| Participants | Participants were recruited from participating nursing homes in Taiwan. The mean age of the control group was 68.95 and the mean age in the intervention group was 81.07. In the control group, 57.6% of participants were female and 75% of the participants in the intervention group were female. | |
| Intervention | Researchers demonstrated how to use a smartphone and initiate videoconferencing for the participants and their family. The participants then made appointments to use videoconferencing, with or without the assistance of nursing home staff. The smartphone‐based video conferencing program was designed to be used once a week, which was similar to the in‐person visiting frequency for the majority of families. Yet, residents could videoconference with their family as many times as they wished. The goal of the duration of each videoconference was set for a minimum of 5 min. | |
| Usual care | ||
| Notes | ||
| Item | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias): loneliness | Unclear | Not enough information available for judgement |
| Allocation concealment (selection bias): loneliness | Unclear | Not enough information available for judgement |
| Blinding of participants and personnel (performance bias) | No | Nursing homes were cluster‐randomised. The participants probably did know which group they were allocated to as recruitment happened after randomisation. It would be difficult to blind participants and personnel due to the nature of the intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear | No detail provided on who conducted the outcome assessment and whether they were blinded |
| Incomplete outcome data (attrition bias): loneliness | No | Used per protocol analysis |
| Selective reporting (reporting bias): loneliness | Unclear | No reference made to a protocol or analysis intentions |
RCT: randomised controlled trial; SF‐36: short‐form questionnaire; UCLA: University of California, Los Angeles
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Arthanat 2016 | Not a peer‐reviewed journal article |
| Banbury 2020 | No relevant outcome |
| Brown 2007 | Not video calls |
| Choi 2020 | No comparison of video calls to alternative intervention |
| Clinician's Research Digest 2012 | Telemedecine |
| Dowling 2014 | Not older adults |
| Elliott 2008 | Not older adults |
| Ferreira 2015 | Not video calls |
| Fokin 2011 | Not in English |
| Hicken 2017 | Not video calls |
| Hori 2009 | Not in English |
| Mongan 2016 | Not a peer‐reviewed journal article |
| Morton 2018 | Not video calls |
| Schwindenhammer 2015 | Not a peer‐reviewed journal article |
| Siniscarco 2017 | Not a RCT |
| Slegers 2008 | Not video calls |
| Smith 2017 | Not a RCT |
| Sánchez‐Rico 2017 | Not a RCT |
| Turnbull 2012 | Not a RCT |
| VanderPloeg 2016 | No relevant outcome |
| Zamir 2018 | Not a RCT |
RCT: randomised controlled trial
Differences between protocol and review
We deviated from the protocol (Noone 2020) in four ways.
An additional systematic review of systematic reviews on interventions to reduce loneliness in older adults was identified by a peer reviewer. We checked the references of this review and did not find any additional studies which met the inclusion criteria.
We did not find enough eligible studies to allow the assessment of reporting biases. If we had found enough studies, we would have assessed reporting biases by inspecting forest plots, conducting a chi‐squared test for heterogeneity and computing the I2 statistic.
All of the studies that we found were conducted in nursing homes. If we had found studies that included interventions delivered at the homes of the participants, then we would have conducted a sensitivity analysis to assess differences across settings.
Since all of the studies that were found used a cluster design, and information regarding the intracluster correlation coefficient (ICC) was not available, we adjusted for clustering using an assumed ICC of .01 and conducted a sensitivity analysis using an assumed ICC of.05.
Contributions of authors
All review authors designed the protocol.
MS designed (with AB) and performed the electronic searches.
JMS and AB completed study selection, with input from CN.
KD, EM and CN conducted data extraction, data analysis, risk of bias assessment and application of the GRADE approach.
CN, AB, EM, JMS, DD and KD drafted the manuscript.
All review authors read and approved the final manuscript.
Declarations of interest
Noone C: none Mc Sharry J: none Smalle M: none Burns A: none Dwan K: none Devane D: none Morrissey E: none
Edited (no change to conclusions)
References
References to studies included in this review
Tsai 2010 {published data only (unpublished sought but not used)}
- Tsai HH, Tsai YF, Wang HH, Chang YC, Chu HH. Videoconference program enhances social support, loneliness, and depressive status of elderly nursing home residents. Aging & Mental Health 2010;14(8):947-54. [DOI: 10.1080/13607863.2010.501057] [DOI] [PubMed] [Google Scholar]
Tsai 2011 {published data only (unpublished sought but not used)}
- Tsai HH, Tsai YF. Changes in depressive symptoms, social support, and loneliness over 1 year after a minimum 3-month videoconference program for older nursing home residents. Journal of Medical Internet Research 2011;13(4):373-84. [DOI: 10.2196/jmir.1678] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsai 2020 {published data only (unpublished sought but not used)}
- Tsai HH, Cheng CY, Shieh WY, Chang YC. Effects of a smartphone-based videoconferencing program for older nursing home residents on depression, loneliness, and quality of life: a quasi-experimental study. BMC Geriatrics 2020;20(1):27. [DOI: 10.1186/s12877-020-1426-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Arthanat 2016 {published data only}
- Arthanat S, Vroman K. A home-based information communication technology training for older adults: effectiveness, value, and perspectives. American Journal of Occupational Therapy 2016;70 Suppl 1. [Google Scholar]
Banbury 2020 {published data only}
- Banbury A, Nancarrow S, Dart J, Gray L, Dodson S, Osborne R, et al. Adding value to remote monitoring: co-design of a health literacy intervention for older people with chronic disease delivered by telehealth - the Telehealth Literacy Project. Patient Education and Counseling 2020;103(3):597-606. [DOI] [PubMed] [Google Scholar]
Brown 2007 {published data only}
- Brown EV. Remote control training. Health Management Technology 2007;28(3):18-19. [PubMed] [Google Scholar]
Choi 2020 {published data only}
- Choi NG, Pepin R, Marti CN, Stevens CJ, Bruce ML. Improving social connectedness for homebound older adults: randomized controlled trial of tele-delivered behavioral activation versus tele-delivered friendly visits. American Journal of Geriatric Psychiatry (in press). [DOI: 10.1016/j.jagp.2020.02.008] [DOI] [PMC free article] [PubMed]
Clinician's Research Digest 2012 {published data only}
- Clinician's Research Digest. Videoconferencing as a method of treatment delivery for older adults: the effectiveness of a behavioral activation treatment. Clinician's Research Digest: Adult Populations 2012;30(1):1. [Google Scholar]
Dowling 2014 {published data only}
- Dowling GA, Merrilees J, Mastick J, Chang VY, Hubbard E, Moskowitz JT. Life enhancing activities for family caregivers of people with frontotemporal dementia. Alzheimer Disease and Associated Disorders 2014;28(2):175-81. [DOI] [PubMed] [Google Scholar]
Elliott 2008 {published data only}
- Elliott TR, Brossart D, Berry JW, Fine PR. Problem-solving training via videoconferencing for family caregivers of persons with spinal cord injuries: a randomized controlled trial. Behaviour Research and Therapy 2008;46(11):1220-9. [DOI] [PubMed] [Google Scholar]
Ferreira 2015 {published data only}
- Ferreira S, Torres A, Mealha Ó, Veloso A. Training effects on older adults in information and communication technologies considering psychosocial variables. Educational Gerontology 2015;41(7):482-93. [Google Scholar]
Fokin 2011 {published data only}
- Fokin VA, Fokin IV. The possibilities of electronic-social network in services for old citizens. Uspekhi Gerontologii/Advances in Gerontology 2011;242011(124):162-7. [PubMed] [Google Scholar]
Hicken 2017 {published data only}
- Hicken BL, Daniel C, Luptak M, Grant M, Kilian S, Rupper RW. Supporting caregivers of rural veterans electronically (SCORE). Journal of Rural Health 2017;33(3):305-13. [DOI] [PubMed] [Google Scholar]
Hori 2009 {published data only}
- Hori M, Kubota M, Ando K, Kihara T, Takahashi R, Kinoshita A. The effect of videophone communication (with Skype and webcam) for elderly patients with dementia and their caregivers. Gan to Kagaku Ryoho. Cancer & Chemotherapy 2009;36:36-8. [PubMed] [Google Scholar]
Mongan 2016 {published data only}
- Mongan E. Social media a new medicine? McKnight's Long-Term Care News 2016;37(10):2. [Google Scholar]
Morton 2018 {published data only}
- Morton TA, Wilson N, Haslam C, Birney M, Kingston R, McCloskey LG. Activating and guiding the engagement of seniors with online social networking: experimental findings from the AGES 2.0 project. Journal of Aging and Health 2018;30(1):27-51. [DOI] [PubMed] [Google Scholar]
Sánchez‐Rico 2017 {published data only}
- Sánchez-Rico A, Garel P, Notarangelo I, Quintana M, Hernández G, Asteriadis S, et al. ICT services for life improvement for the elderly. Studies in Health Technology and Informatics 2017;242:600-5. [PubMed] [Google Scholar]
Schwindenhammer 2015 {published data only}
- Schwindenhammer TM. Videoconferencing intervention for depressive symptoms and loneliness in nursing home elders [PhD thesis]. Illinois State University, 2014. [Google Scholar]
Siniscarco 2017 {published data only}
- Siniscarco MT, Love-Williams C, Burnett-Wolle S. Video conferencing: an intervention for emotional loneliness in long-term care. Activities, Adaptation & Aging 2017;41(4):316-29. [Google Scholar]
Slegers 2008 {published data only}
- Slegers K, Van Boxtel MP, Jolles J. Effects of computer training and internet usage on the well-being and quality of life of older adults: a randomized, controlled study. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences 2008;63(3):176-84. [DOI] [PubMed] [Google Scholar]
Smith 2017 {published data only}
- Smith SK, Astell AJ. Independent living functions for the elderly (IN-LIFE): supporting communication in dementia. In: Cudd P, Witte L, editors(s). Harnessing the Power of Technology to Improve Lives. Vol. 242. IOS Press, 2017:16-22. [DOI: 10.3233/978-1-61499-798-6-16] [DOI] [PubMed] [Google Scholar]
Turnbull 2012 {published data only}
- Turnbull H. SPAD (Speech Pathologists in Adult Disability) top 10. Journal of Clinical Practice in Speech-Language Pathology 2012;14(3):153-4. [Google Scholar]
VanderPloeg 2016 {published data only}
- Van der Ploeg ES, Eppingstall B, O’Connor DW. Internet video chat (Skype) family conversations as a treatment of agitation in nursing home residents with dementia. International Psychogeriatrics / IPA 2016;28(4):697-8. [DOI] [PubMed] [Google Scholar]
Zamir 2018 {published data only}
- Zamir S, Hennessy CH, Taylor AH, Jones RB. Video-calls to reduce loneliness and social isolation within care environments for older people: an implementation study using collaborative action research. BMC Geriatrics 2018;18(1):62. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Armitage 2020
- Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health 2020 Mar 19 [Epub ahead of print]. [DOI: 10.1016/S2468-2667(20)30061-X] [DOI] [PMC free article] [PubMed]
Baker 2018
- Baker S, Warburton J, Waycott J, Batchelor F, Hoang T, Dow B, et al. Combatting social isolation and increasing social participation of older adults through the use of technology: a systematic review of existing evidence. Australasian Journal on Ageing 2018;37(3):184-93. [DOI] [PubMed] [Google Scholar]
Cacioppo 2010
- Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychology and Aging 2010;25(2):453. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chen 2016
- Chen YR, Schulz PJ. The effect of information communication technology interventions on reducing social isolation in the elderly: a systematic review. Journal of Medical Internet Research 2016;18(1):e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chipps 2017
- Chipps J, Jarvis MA, Ramlall S. The effectiveness of e-interventions on reducing social isolation in older persons: a systematic review of systematic reviews. Journal of Telemedicine and Telecare 2017;23(10):817-27. [DOI] [PubMed] [Google Scholar]
Courtin 2017
- Courtin E, Knapp M. Social isolation, loneliness and health in old age: a scoping review. Health & Social Care in the Community 2017;25(3):799-812. [DOI] [PubMed] [Google Scholar]
Covidence [Computer program]
- Veritas Health Innovation Covidence. Version accessed after 7 April 2020. Melbourne, Australia: Veritas Health Innovation, 2020. Available at covidence.org.
Deeks 2019
- Deeks JJ, Higgins JP, Altman DG (editors). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Fakoya 2020
- Fakoya OA, McCorry NK, Donnelly M. Loneliness and social isolation interventions for older adults: a scoping review of reviews. BMC Public Health 2020;20(1):1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fixsen 2005
- Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. Implementation Research: A Synthesis of the Literature. The National Implementation Research Network, 2005. [Google Scholar]
Ge 2017
- Ge L, Yap CW, Ong R, Heng BH. Social isolation, loneliness and their relationships with depressive symptoms: a population-based study. PloS One 2017;12(8):e0182145. [DOI: 10.1371/journal.pone.0182145] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hawton 2011
- Hawton A, Green C, Dickens AP, Richards SH, Taylor RS, Edwards R, et al. The impact of social isolation on the health status and health-related quality of life of older people. Quality of Life Research 2011;20(1):57-67. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JP, Altman DG, Sterne JA (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS (editors), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017), Cochrane, 2017. Available from www.training.cochrane.org/handbook.
Huang 2006
- Huang IC, Wu AW, Frangakis C. Do the SF-36 and WHOQOL-BREF measure the same constructs? Evidence from the Taiwan population. Quality of Life Research 2006;15(1):15-24. [DOI] [PubMed] [Google Scholar]
Jarvis 2019
- Jarvis M, Padmanabhanunni A, Balakrishna Y, Chipps J. The effectiveness of interventions addressing loneliness in older persons: an umbrella review. International Journal of Africa Nursing Sciences 2019;12:100177. [DOI: 10.1016/j.ijans.2019.100177] [DOI] [Google Scholar]
Killip 2004
- Killip S, Mahfoud Z, Pearce K. What is an intracluster correlation coefficient? Crucial concepts for primary care researchers. Annals of Family Medicine 2004;2(3):204-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
McGuinness 2019 [Computer program]
- robvis: an R package and web application for visualising risk-of-bias assessments. Version accessed after 7 April 2020. McGuinness LA, 2019. github.com/mcguinlu/robvis.
Microsoft Corporation 2018 [Computer program]
- Microsoft Excel. Microsoft Corporation, 2018. available at office.microsoft.com/excel.
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLoS Medicine 6;7:e1000097. [DOI: 10.1371/journal.pmed1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
Musich 2015
- Musich S, Wang SS, Hawkins K, Yeh CS. The impact of loneliness on quality of life and patient satisfaction among older, sicker adults. Gerontology and Geriatric Medicine 2015;1:1-9. [DOI: 10.1177/2333721415582119] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pew Research Center 2019
- Pew Research Center. Smartphone ownership is growing rapidly around the world, but not always equally. Available from www.pewresearch.org/global/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally/ 2019.
Porges 2003
- Porges SW. Social engagement and attachment: a phylogenetic perspective. Annals of the New York Academy of Sciences 2003;1008:31-47. [DOI] [PubMed] [Google Scholar]
Schünemann 2019
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Cochrane, 2019. Available from www.training.cochrane.org/handbook.
Shenkin 2017
- Shenkin SD, Harrison JK, Wilkinson T, Dodds RM, Ioannidis JP. Systematic reviews: guidance relevant for studies of older people. Age and Ageing 2017;46(5):722-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Singh 2015
- Singh K, Srivastava SK. Loneliness and quality of life among elderly people. Journal of Psychosocial Research 2014;9(1):11-8. [Google Scholar]
Stiles 1998
- Stiles PG, McGarrahan JF. The Geriatric Depression Scale: a comprehensive review. Journal of Clinical Geropsychology 1998;4(2):89-110. [Google Scholar]
Sutton 2000
- Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F. Methods for Meta-Analysis in Medical Research. Chichester: Wiley, 2000. [Google Scholar]
Tsai 2007
- Tsai YF. Self-care management and risk factors for depressive symptoms among Taiwanese institutionalized residents. Nursing Research 2007;56(2):124-31. [DOI] [PubMed] [Google Scholar]
Tsai 2020 [pers comm]
- Tsai H. Cochrane Rapid Review on videoconferencing to reduce loneliness [personal communication]. Email to: C Noone 23 April 2020.
Valtorta 2012
- Valtorta N, Hanratty B. Loneliness, isolation and the health of older adults: do we need a new research agenda? Journal of the Royal Society of Medicine 2012;105(12):518-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Weiss 1973
- Weiss RS. Loneliness: The Experience of Emotional and Social Isolation. Cambridge, MA: MIT Press, 1973. [Google Scholar]
WHO 2010
- World Health Organization. Telemedicine: opportunities and developments in Member States: report on the second global survey on eHealth. World Health Organization. [ISBN: 9789241564144]
Wu 2020
- Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China. Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020;323(13):1239-42. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Noone 2020
- Noone C, Morrissey EC, Sharry JM, Devane D, Burns A, Smalle M, et al. Cochrane rapid review protocol - the effectiveness of video calls for reducing social isolation and loneliness in older people. Available from osf.io/rfxky. [DOI: 10.17605/OSF.IO/RFXKY] [DOI] [PMC free article] [PubMed]


