Abstract
Background
Crowns for primary molars are preformed and come in a variety of sizes and materials to be placed over decayed or developmentally defective teeth. They can be made completely of stainless steel (know as 'preformed metal crowns' or PMCs), or to give better aesthetics, may be made of stainless steel with a white veneer cover or made wholly of a white ceramic material. In most cases, teeth are trimmed for the crowns to be fitted conventionally using a local anaesthetic. However, in the case of the Hall Technique, PMCs are pushed over the tooth with no local anaesthetic, carious tissue removal or tooth preparation. Crowns are recommended for restoring primary molar teeth that have had a pulp treatment, are very decayed or are badly broken down. However, few dental practitioners use them in clinical practice. This review updates the original review published in 2007.
Objectives
Primary objective
To evaluate the clinical effectiveness and safety of all types of preformed crowns for restoring primary teeth compared with conventional filling materials (such as amalgam, composite, glass ionomer, resin modified glass ionomer and compomers), other types of crowns or methods of crown placement, non‐restorative caries treatment or no treatment.
Secondary objective
To explore whether the extent of decay has an effect on the clinical outcome of primary teeth restored with all types of preformed crowns compared with those restored with conventional filling materials.
Search methods
We searched the following electronic databases: Cochrane Oral Health Group Trials Register (to 21 January 2015), Cochrane Central Register of Controlled Trials (CENTRAL; The Cochrane Library, 2014, Issue 12), MEDLINE via Ovid (1946 to 21 January 2015) and EMBASE via Ovid (1980 to 21 January 2015). We searched the US National Institutes of Health Trials Register (http://clinicaltrials.gov) and the World Health Organization (WHO) International Clinical Trials Registry Platform for ongoing trials and Open Grey for grey literature (to 21 January 2015). No restrictions were placed on the language or date of publication when searching the databases.
Selection criteria
Randomised controlled trials (RCTs) that assessed the effectiveness of crowns compared with fillings, other types of crowns, non‐restorative approaches or no treatment in children with untreated tooth decay in one or more primary molar teeth. We would also have included trials comparing different methods of fitting crowns.
For trials to be considered for this review, the success or failure of the interventions and other clinical outcomes had to be reported at least six months after intervention (with the exception of 'pain/discomfort during treatment and immediately postoperatively').
Data collection and analysis
Two review authors independently assessed the title and abstracts for each article from the search results. and independently assessed the full text for each potentially relevant study. At least two authors assessed risk of bias and extracted data using a piloted data extraction form.
Main results
We included five studies that evaluated three comparisons. Four studies compared crowns with fillings; two of them compared conventional PMCs with open sandwich restorations, and two compared PMCs fitted using the Hall Technique with fillings. One of these studies included a third arm, which allowed the comparison of PMCs (fitted using the Hall Technique) versus non‐restorative caries treatment. In the two studies using crowns fitted using the conventional method, all teeth had undergone pulpotomy prior to the crown being placed. The final study compared two different types of crowns: PMCs versus aesthetic stainless steel crowns with white veneers. No RCT evidence was found that compared different methods of fitting preformed metal crowns (i.e. Hall Technique versus conventional technique).
We considered outcomes reported at the dental appointment or within 24 hours of it, and in the short term (less than 12 months) or long term (12 months or more). Some of our outcomes of interest were not measured in the studies: time to restoration failure or retreatment, patient satisfaction and costs.
Crowns versus fillings
All studies in this comparison used PMCs. One study reported outcomes in the short term and found no reports of major failure or pain in either group. There was moderate quality evidence that the risk of major failure was lower in the crowns group in the long term (risk ratio (RR) 0.18, 95% confidence interval (CI) 0.06 to 0.56; 346 teeth in three studies, one conventional and two using Hall Technique). Similarly, there was moderate quality evidence that the risk of pain was lower in the long term for the crown group (RR 0.15, 95% CI 0.04 to 0.67; 312 teeth in two studies).
Discomfort associated with the procedure was lower for crowns fitted using the Hall Technique than for fillings (RR 0.56, 95% CI 0.36 to 0.87; 381 teeth) (moderate quality evidence).
It is uncertain whether there is a clinically important difference in the risk of gingival bleeding when using crowns rather than fillings, either in the short term (RR 1.69, 95% CI 0.61 to 4.66; 226 teeth) or long term (RR 1.74, 95% CI 0.99 to 3.06; 195 teeth, two studies using PMCs with conventional technique at 12 months) (low quality evidence).
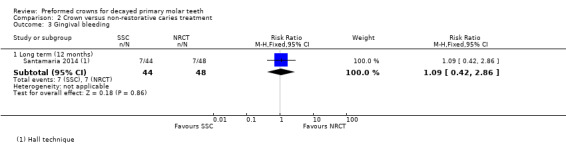
Crowns versus non‐restorative caries treatment
Only one study compared PMCs (fitted with the Hall Technique) with non‐restorative caries treatment; the evidence quality was very low and we are therefore we are uncertain about the estimates.
Metal crowns versus aesthetic crowns
One split‐mouth study (11 participants) compared PMCs versus aesthetic crowns (stainless steel with white veneers). It provided very low quality evidence so no conclusions could be drawn.
Authors' conclusions
Crowns placed on primary molar teeth with carious lesions, or following pulp treatment, are likely to reduce the risk of major failure or pain in the long term compared to fillings. Crowns fitted using the Hall Technique may reduce discomfort at the time of treatment compared to fillings. The amount and quality of evidence for crowns compared to non‐restorative caries, and for metal compared with aesthetic crowns, is very low. There are no RCTs comparing crowns fitted conventionally versus using the Hall Technique.
Keywords: Child; Child, Preschool; Female; Humans; Male; Crowns; Crowns/adverse effects; Tooth, Deciduous; Dental Care for Children; Dental Care for Children/adverse effects; Dental Care for Children/methods; Dental Caries; Dental Caries/rehabilitation; Dental Restoration Failure; Dental Restoration, Permanent; Dental Restoration, Permanent/methods; Molar; Randomized Controlled Trials as Topic
Plain language summary
Preformed crowns for managing decayed primary molar teeth in children
Background
To stop further damage and restore function of primary molar teeth that are decayed or malformed, a dentist will usually use a filling (a soft material that is placed in the cavity and hardened) to restore the tooth to its original shape. Alternatively the dentist may place a crown over the tooth to cover it. This usually requires an injection in the gum to numb the tooth before trimming it down (conventional technique). These crowns are pre‐made (i.e. preformed) in a variety of sizes and can be metal or white, with the correct size being chosen to fit the trimmed down tooth. The Hall Technique is an alternative method for fitting metal crowns, where there is no need for an injection or tooth trimming as the crown is simply pushed over the tooth. Preformed crowns are recommended by specialists in children's dentistry for the management of baby back teeth (molars) when they are affected by moderate to advanced tooth decay, or where the enamel has malformed during development or the tooth has had to have root canal treatment.
Review question
This Cochrane review asked whether crowns are better than other ways of managing decay in children's baby teeth for reducing 'major failure' (an outcome that includes aspects such as toothache and dental abscess), pain during treatment and harm, and for improving satisfaction with treatment. It also asked whether metal or white crowns were better and whether a new fitting method called the Hall Technique was better than the conventional fitting technique. The review updates one originally published in 2007.
Study characteristics
We searched medical and dental sources for studies up to 21 January 2015. We identified five relevant studies. They were at high risk of bias because the participants knew which treatment they received and so did the people who treated them.
Four studies compared crowns with fillings. Two of them compared metal crowns fitted using the conventional method with fillings and two compared metal crowns fitted using the Hall Technique with fillings. One of the studies also compared the Hall Technique with 'non‐restorative caries treatment' (not using either a filling or crown but opening the cavity to make it possible to clean with a toothbrush, sealing with fluoride varnish and encouraging toothbrushing). The final study compared crowns made of two different materials (stainless steel versus stainless steel with a white covering). We looked at what happened for each treatment at the time of the dental appointment or within 24 hours of treatment, in the short term (less than 12 months) and long term (12 months to 48 months).
Key results
Teeth restored with preformed crowns are less likely to develop problems (e.g. abscess) or cause pain in the long term, compared to fillings. Crowns fitted using the Hall Technique (no injections or tooth trimming) gave less discomfort at the time of the appointment, when compared with fillings. Crowns may increase the risk of gingival bleeding but this result was unclear. Only one small study compared crowns with non‐restorative caries treatment and one small study compared metal and white crowns, and we could draw no reliable conclusions from these. Some of our outcomes of interest were not measured in any of the studies: these included time to restoration failure or retreatment, patient satisfaction and costs.
Quality of the evidence
There is moderate quality evidence that crowns are more effective than fillings for managing decay in primary molar teeth. There is moderate quality evidence that crowns fitted using the Hall Technique are less likely to cause abscesses and pain than fillings. The evidence comparing preformed crowns with non‐restorative caries management, and comparing preformed metal crowns with preformed white crowns, is very low quality so we do not know which is better.
Author's conclusion
Crowns placed on primary molar teeth with decay, or that have had pulp treatment, are likely to reduce the risk of major failure or pain in the long term compared to fillings. Crowns fitted using the Hall Technique may reduce discomfort at the time of treatment compared to fillings.
Summary of findings
Summary of findings for the main comparison. Preformed crowns compared to fillings for decayed primary molar teeth.
| Preformed crowns compared to fillings for decayed primary molar teeth | ||||||
| Patient or population: decayed primary molar teeth Settings: secondary care, UK and Germany Intervention: preformed crown Comparison: filling | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Filling | Preformed crown | |||||
| Major failure ‐ long term (12 months to 48 months) | Study population | RR 0.18 (0.06 to 0.56) | 346 (3 RCTs) | ⊕⊕⊕⊝ moderate 1,2 | ||
| 112 per 1000 | 20 per 1000 (7 to 63) | |||||
| Pain ‐ long term (12 months to 24 months) | Study population | RR 0.15 (0.04 to 0.67) | 312 (2 RCTs) | ⊕⊕⊕⊝ moderate 1 | This was based on patient and/or parent reports | |
| 83 per 1000 | 12 per 1000 (3 to 56) | |||||
| Satisfaction with treatment | ||||||
| Discomfort associated with the procedure | Study population | RR 0.56 (0.36 to 0.87) | 381 (2 RCTs) | ⊕⊕⊕⊝ moderate 1 | This was patient‐reported in one study, and dentist‐reported in another study. Outcomes were recorded using different 5‐point scales, but dichotomised for analyses, with all partients who scored 'moderate' or more severe levels of discomfort considered as having experienced discomfort | |
| 239 per 1000 | 134 per 1000 (86 to 208) | |||||
| Gingival bleeding ‐ long term (12 months) | Study population | RR 1.74 (0.99 to 3.06) | 195 (2 RCTs) | ⊕⊕⊝⊝ low 1,3 | ||
| 156 per 1000 | 272 per 1000 (155 to 478) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio, RCT: randomised controlled trial | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Intervention and comparison look different. Blinding of outcome assessor, patients and the person doing the procedures was not possible. Outcomes have subjective elements. Although pain was not measured using validated tools, there was no further downgrading for this.
2 One of the studies only had data from 87% of randomised participants from one country (from a multinational study of three countries); the study is still ongoing at the time of publication.
3 Small sample size; event rates were low. Confidence intervals were wide.
Summary of findings 2. Preformed crowns compared to non‐restorative caries treatment for decayed primary molar teeth.
| Preformed crowns compared to non‐restorative caries treatment for decayed primary molar teeth | ||||||
| Patient or population: children with decayed primary molar teeth Settings: secondary care, Germany Intervention: preformed crown Comparison: non‐restorative caries treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Non‐restorative caries treatment | Preformed crown | |||||
| Major failure (12 months) | Study population | RR 0.12 (0.01 to 2.18) | 92 (1 RCT) | ⊕⊝⊝⊝ very low 1,2 | ||
| 83 per 1000 | 10 per 1000 (1 to 162) | |||||
| Pain | No evidence available | |||||
| Satisfaction with treatment | No evidence available | |||||
| Discomfort associated with the procedure | Study population | RR 1.67 (0.65 to 4.25) | 104 (1 RCT) | ⊕⊝⊝⊝ very low 1,2 | Data were measured on different 5‐point scales, but dichotomised for analyses, with all patients who scored 'moderate' or more severe levels of discomfort considered as having experienced discomfort | |
| 115 per 1000 | 193 per 1000 (75 to 490) | |||||
| Gingival bleeding ‐ long term (12 months) | Study population | RR 1.09 (0.42 to 2.86) | 92 (1 RCT) | ⊕⊝⊝⊝ very low 1,2 | ||
| 146 per 1000 | 159 per 1000 (61 to 417) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RCT: randomised controlled trial, CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 There was a very serious risk of bias for this trial. Blinding was impossible as the intervention and comparison looked different, and the outcome had subjective elements in its assessment. Futhermore only 87% of the data from one country (this was a multinational study with three countries) were available. Although pain was not measured using validated tools, there was no further downgrading for this. The study is still ongoing.
2 Very serious imprecision; small sample size; wide confidence intervals.
Background
Description of the condition
Dental caries (tooth decay) affects around 60% to 90% of children globally (WHO Report 2003). It most commonly occurs in primary (baby) molar (back) teeth. If left unmanaged, dental caries will progress to give pain and infection, the consequences of which are unnecessary suffering, and lost days at school (Gift 1992). There is evidence of a linear relationship between higher levels of caries and anthropometric outcomes (height, weight and body mass index (BMI)) (Alkarimi 2014). Untreated dental caries has an adverse effect on children's ability to grow and thrive (Sheiham 2006), and in underweight children, extraction of severely carious primary teeth can improve weight gain (Monse 2012).
Teeth undergo a constant process of demineralisation (caused by the acids and enzymes produced by cariogenic bacteria in the dental biofilm (plaque)) and remineralisation (from protective factors such as fluoride and salivary components). Dental caries occurs when the rate of demineralisation is greater than that of remineralisation. When dissolution of enamel and dentine leads to cavitation (a hole in the tooth), the carious lesion can no longer be cleaned and it becomes more difficult to arrest the caries process as the biofilm becomes more sheltered, which favours the cariogenic bacteria (Fejerskov 2015). This is when a restoration (filling) is usually considered necessary, to protect vulnerable tissue and to allow the tooth tissue to be able to be cleaned again.
Primary molar teeth can also be affected by conditions that disrupt the development of the dental hard tissues (i.e. hypoplasia, hypomineralisation, dentinogenesis imperfecta, amelogenesis imperfecta). These reduce the integrity and strength of the tooth and therefore, its longevity.
Description of the intervention
Materials for managing primary molar teeth with decay or developmental defects
Restorations that can be provided can either be filling materials or preformed crowns. Traditionally, preformed crowns have been made of metal and referred to as either preformed metal crowns (PMCs) or stainless steel crowns. They are silver in colour. More recently, aesthetic preformed crowns have been developed and used for primary teeth, which are white in colour. For the purposes of this review, the term 'crown' will be used when referring to preformed crowns of any type, while 'PMC' is used specifically to refer to preformed crowns made of metal and 'aesthetic crown' used specifically to refer to preformed crowns with a non‐metallic appearance.
Fillings can be made of amalgam or various tooth‐coloured materials (resin composite, compomers, resin‐modified glass ionomer, glass ionomer) . There is very little high quality evidence to support the use of one type of restoration over another for primary teeth. A Cochrane Review that examined the use of filling materials in primary teeth was able to include only two studies of direct filling comparisons and was unable to draw conclusions about which was better (Yengopal 2009).
Current guidelines from both the American Association of Paediatric Dentistry (AAPD 2014), and the British Society for Paediatric Dentistry (Kindelan 2008), recommend treating dental decay in primary molar teeth by removing carious tissue before restoring the tooth with either a filling or a crown. These guidelines indicate that crowns are appropriate where “more than two surfaces are affected, or where one or two surface caries are extensive” (Kindelan 2008), and they may also be indicated for “restoration of primary molars affected by localised or generalised developmental problems, e.g. enamel hypoplasia, amelogenesis imperfecta, dentinogenesis imperfecta”.
Placement of a preformed crown is intended to provide a more durable restoration than a filling. The process of preparing a tooth for filling materials can leave it structurally weak, as carious tissue needs to be removed from the cavity to allow a restoration to be placed. Additionally, sound tissue may need to be removed to gain access to the carious tissue. Furthermore, for certain filling materials, such as amalgam, the cavity has to be prepared to an 'ideal' shape to allow the incorporation of a mechanical resistance form and so prevent loss of the restoration. Re‐establishing the original form of primary molar teeth with a filling material can be difficult, particularly with multi‐surface cavities. The increased occlusal loading that multi‐surface fillings are subjected to, often leads to premature restoration failure. Using atraumatic restorative treatment (ART) and selective carious tissue removal, the tooth can be prepared for a filling without the need for local anaesthetic; however, ART restorations have shorter lifespans in multisurface restorations than in single surface ones (Frencken 2014).
Conventionally, preparing a primary tooth for a crown requires complete removal of carious tissue and trimming the tooth for the crown to fit, under local anaesthesia. This approach is used by specialists in paediatric dentistry and considered “subject to minimal technique sensitivity during placement" (Seale 2002). However, PMCs are rarely placed by general dental practitioners (Maggs‐Rapport 2000), as they are viewed as demanding more skill on the part of the dentist and co‐operation on the part of the child patient than is required for placing a filling (Chadwick 2007). There is evidence that general dental practitioners' (GDPs) reluctance to use PMCs as part of their routine treatment may be related more to factors such as perceived difficulties in placing PMCs and funding issues (Maggs‐Rapport 2000; Threlfall 2005), rather than doubts about whether PMCs are an effective restoration. There is another, more recent method for placing PMCs, which is less invasive, called the 'Hall Technique'. In this no local anaesthesia is used, no carious tissue is removed and no tooth preparation carried out, but the PMC is pushed over the tooth and the decay sealed in (Innes 2011). However, this does not overcome the disadvantage of the aesthetics of the metal crowns in children’s mouths (Foster Page 2014). The use of aesthetic (white) crowns for children’s back teeth is of growing interest, but they are not yet commonly used. It is unlikely that aesthetic crowns would be able to be fitted using the non‐invasive Hall Technique approach, as pushing the crown over the tooth without preparation relies on being able to distort the metallic leading edge of the crown slightly during placement. Although aesthetic crowns are made of a variety of materials, these are all rigid and have no ability to distort.
Techniques for managing primary molar teeth with decay or developmental defects
Dental interventions to manage dental decay and developmental defects can be challenging for children to cope with, and for clinicians to carry out successfully. There are different methods for managing carious tissue prior to providing a restoration (ART and selective carious tissue removal) and for fitting crowns (the Hall Technique) that do not require the use of local anaesthesia. A recent update of the Cochrane Review on carious lesion management supported selective carious tissue removal methods in primary teeth (Ricketts 2013). These newer approaches to carious lesion management have advantages over complete carious tissue removal that include reduction in pulp exposure without causing an increase in symptoms from the dental pulp in primary teeth. However, the evidence was insufficient to determine whether there was a difference in restoration longevity where selective carious tissue removal was carried out, apart from when PMCs were used with the Hall Technique, where longevity was improved. These newer techniques should be considered alongside conventional restorative approaches. The Hall Technique is an extension of the 'sealing in' decay approach where carious tissue is not removed. When teeth are affected by extensive developmental defects it is often necessary to cover them fully with a PMC to preserve their integrity. The Hall Technique has been used for primary molar teeth in this situation and does not require any of the defective tooth tissue to be removed, but simply covered with the crown. The Hall Technique method of using preformed metal crowns should be compared with fillings, non‐restorative approaches and conventional crowns (metal or other materials).
Alternative techniques to crowns and fillings
In addition to managing teeth with crowns or fillings, non‐restorative options for arresting the progress of decay in primary teeth have recently been advocated and are being investigated as cost‐effective, non‐invasive solutions for managing decay (Vermaire 2014). These approaches rely on control of the biofilm through its frequent and successful removal by toothbrushing and have been investigated in comparison to fillings and crowns (Santamaria 2014).
Use of crowns
Fitting a crown can be demanding in terms of both of clinical skill and child co‐operation. In the UK, primary care dental practitioners do not routinely use crowns as part of their daily practice (Roshan 2003). In addition, there are considerable variations in opinion about when to place crowns and when a filling would be more clinically appropriate (Pair 2004; Tran 2003). In a prescribed case scenario that investigated which restoration dentists would place on a decayed primary molar tooth, Blinkhorn 2003 found that 88% of USA dentists would place a crown compared to 4% of UK respondents.
However, their use is still recommended in guideline documents as the restoration of choice for teeth with extensive cavitation, as well as for teeth with developmental defects (e.g. hypoplasia, hypomineralisation).
How the intervention might work
Primary molar teeth are usually restored to their previous anatomical form using filling materials. With multisurface cavities, there can be increased occlusal loading and this could be a cause of premature restoration failure. In view of this, current guidelines recommend placing a preformed crown. They cover primary molar teeth affected with moderate to severe dental carious lesions involving two or more surfaces completely, in order to provide a more durable restoration than simply placing a filling (AAPD 2014; Kindelan 2008; Seale 2015). The PMC can be fitted either by using the 'conventional method' (where the carious tissue and the pulp are treated with an appropriate technique) or the Hall Technique, where the crown is simply pushed onto the tooth with no carious tissue removal, local anaesthesia or tooth preparation. Aesthetic crowns also cover the entire primary molar tooth, but always require tooth preparation to place them and may require additional tooth tissue removal to create sufficient space compared to PMCs. However, regardless of the materials that crowns are made of, or the method used to place them, it is generally believed that by encasing the tooth the structural integrity of the tooth is increased.
Why it is important to do this review
There is little high quality comparative evidence to support the use of crowns over filling materials, or aesthetic crowns over metal ones. A narrative literature review found 14 studies that investigated comparison of PMCs in prospective or retrospective studies (Attari 2006). The studies were scored for the degree to which they met certain criteria: no studies reached the A standard (meeting 100% of the criteria) or B1 (over 75% of the criteria), seven scored B2 (50% to 75%) and the remaining seven scored C (below 50%). Failure rates of PMCs were 1.9% to 30.3%, which was lower than for fillings, but the study designs and quality made it difficult to interpret the findings meaningfully. A systematic review that compared the durability of PMCs with amalgam fillings in primary molars found PMCs more effective (Randall 2000). However, there was no analysis for heterogeneity within the review and Ismail and Sohn (Ismail 2002), who reanalysed the data later using a random‐effects model, noted that the 10 studies had a significant degree of heterogeneity and, although there was still an improved performance for PMCs compared with amalgam fillings, the extent of the improvement was reduced. Amalgam is now being used less often because of environmental concerns related to its disposal. With the advent and increasing use of more aesthetic, adhesive materials, the performance of crowns needs to be compared with these newer materials.
The previous version of this Cochrane systematic review focused only on conventional preformed metal crown placement compared with all fillings. However, there are several reasons for expanding the scope of the review further. New studies are available, and developments in the materials used to make aesthetic crowns for primary molar teeth ‐ see Ram 2003 and Leith 2011 ‐ have been stimulated by the profession and consumer (parent/carer mainly) concerns about appearance of PMCs (Beattie 2011; Randall 2002). Different restorative filling materials now need to be compared, not only with the traditional PMCs and aesthetic crowns, but also with new techniques for placing PMCs and to non‐restorative approaches to caries management.
There are a growing number of options for managing decay and developmental defects in primary teeth; different types of fillings, different types of crowns and different methods for managing carious tissues. There is a lack of clarity around the evidence comparing crowns with different filling materials, different crowns and other methods for managing decay. This makes it difficult for clinicians to decide on a course of action, and also to present patients with the information they need to make informed choices about how to restore a primary molar tooth in a child. This review will provide information on how these techniques compare.
The Cochrane Oral Health Group undertook an extensive prioritisation exercise in 2014 to identify a core portfolio of titles that were the most clinically important ones to maintain on the Cochrane Library. This review was identified as a clinically important priority title by the paediatric expert panel (Cochrane OHG priority review portfolio; Worthington 2015).
Objectives
Primary objective
To evaluate the clinical effectiveness and safety of all types of preformed crowns for restoring primary teeth compared with conventional filling materials (such as amalgam, composite, glass ionomer cement, resin‐modified glass ionomer, and compomers), other types of crowns or methods of crown placement and non‐restorative caries treatment or no treatment.
Secondary objective
To explore whether the extent of decay has an effect on the clinical outcome of primary teeth restored with all types of PCs compared with those restored with conventional filling materials.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs), including split‐mouth studies.
Given that crowns look quite different from fillings, we did not expect studies to be blinded. We included non‐blinded studies.
Types of participants
Children with at least one primary molar tooth affected by decay or developmental defects.
Preformed crowns are not routinely used in the restoration of permanent teeth apart from in temporary management of teeth with molar incisor hypomineralisation or other developmental defects (Lygidakis 2010; Seale 2015), and, as this review focuses on primary teeth, we planned to include only the results from primary teeth where studies presented data for permanent and primary teeth.
Types of interventions
Preformed crowns of any material placed using any method. We included interventions with incomplete or no carious tissue removal, or any pulp therapy prior to placement of the crown. The comparison was with another crown, or any type of restoration, or another method for managing carious tissue.
For trials to be considered for this review, the success or failure of the interventions and other clinical outcomes had to be reported at least six months after intervention, with the exception of pain/discomfort at treatment time, which had to be measured at the time of treatment.
Comparisons
Comparison 1: Crown (regardless of technique or material) versus filling (with or without complete carious tissue excavation; with or without pulp treatment)
Crown (made of any material and fitted using the conventional technique) versus filling (using any material with complete carious tissue removal).
Crown (metal crown fitted using the Hall Technique) versus filling (using any material with or without complete carious tissue excavation).
Crown (with pulp treatment) versus filling (with pulp treatment).
Comparison 2: Crown (regardless of technique or material) versus no crown or filling
Crown (made of any material and fitted using any technique) versus no treatment.
Crown (made of any material and fitted using any technique) versus non‐restorative caries treatment, or other non‐operative cavity management.
Comparison 3: Crown (metal) versus crown (aesthetic)
Comparison 4: Crown (fitted using the Hall Technique) versus crown (fitted using a conventional technique)
Types of outcome measures
Primary outcomes
Major failure: this outcome is a composite measure of signs and symptoms leading to diagnosis of irreversible pulpitis or periradicular periodontitis, and so includes one or more of the following; pain, pulp infection, discharging sinus, dental abscess, or periradicular pathology on radiographs. Where that was not discernable from the data, authors were contacted for further details, to allow a sensitivity analysis to be undertaken to investigate the impact of including all restoration failure data as major failures.
Pain.
Satisfaction with treatment (including satisfaction with aesthetics).
Secondary outcomes
Time to restoration failure/retreatment.
Discomfort associated with procedure.
Cost.
Adverse events (e.g. bone loss, gingival inflammation or others).
Timing of outcome assessment
For major failures, pain, satisfaction with treatment, time to failure, cost, and adverse events, the time points considered were:
short term (less than 12 months);
long term (12 months or more).
Discomfort associated with the procedure had to be reported at time of the dental appointment or within 24 hours of treatment.
Search methods for identification of studies
For the identification of studies included or considered for this review, we developed detailed search strategies for each database searched. These were based on the search strategy developed for MEDLINE (Ovid) and were revised appropriately for each database. The search strategy used a combination of controlled vocabulary and free‐text terms and was linked with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials (RCTs) in MEDLINE: sensitivity maximising version (2008 revision) (Lefebvre 2011). Details of the MEDLINE search are provided in Appendix 1. The Embase search was linked to the Cochrane Oral Health Group filter for identifying RCTs.
Electronic searches
We searched the following electronic databases:
the Cochrane Oral Health Group's Trials Register (to 21 January 2015; see Appendix 2);
the Cochrane Central Register of Controlled Trials (CENTRAL; The Cochrane Library 2014, Issue 12; see Appendix 3);
MEDLINE via Ovid (1946 to 21 January 2015; see Appendix 1); and
Embase via Ovid (1980 to 21 January 2015; see Appendix 4).
We placed no restrictions on the language or date of publication when searching the electronic databases.
Searching other resources
We searched the following databases for ongoing trials (see Appendix 5 for search strategies applied):
US National Institutes of Health Trials Register (http://clinicaltrials.gov) (to 21 January 2015);
The WHO Clinical Trials Registry Platform (http://apps.who.int/trialsearch/default.aspx) (to 21 January 2015).
We searched the Open Grey database for grey literature (to 21 January 2015; see Appendix 6).
We sent requests for information about unpublished studies/studies published in the 'grey literature' to relevant companies, relevant investigators and relevant professional organisations.
Data collection and analysis
Selection of studies
At least two review authors independently scanned the titles and abstracts of all reports identified by the search strategy. Full reports were obtained for studies that appeared to meet the inclusion criteria, but where there was insufficient information in the title and abstract for the review authors to be certain, and the two review authors assessed these independently to establish whether the studies met the inclusion criteria. Disagreements were resolved by discussion and, where they could not be resolved, through consultation with a third review author.
Data extraction and management
At least two review authors extracted data from all included studies independently and in duplicate using specially designed data extraction forms. We extracted data on the following:
study design and methods;
study setting: location, number of centres, year conducted, other information that might provide some indication of the type of patients or level of training/specialisation of the operators;
participants: demographic characteristics (age, male:female), numbers of patients recruited and randomised to each group, how these patients were selected or screened, number of dropouts and number evaluated; inclusion and exclusion criteria;
intervention and control used: including type and method of restoration;
outcomes reported: including method of assessment;
declarations of interest of investigators and source of study funding; and
information related to risk of bias assessments.
For data on the outcomes reported at the time of the dental appointment or within 24 hours of treatment, our prespecified priority was to extract and analyse data as reported by children. When these data were not available, we extracted ratings by parents and dentists (in this order of preference) for analysis.
We contacted trial authors for clarification and missing information.
Assessment of risk of bias in included studies
At least two review authors undertook the assessment of the risk of bias in the included trials independently and in duplicate. The assessments were based on the information given in the articles and conducted using the standard recommended approach for assessing the risk of bias in studies included in Cochrane systematic reviews (Higgins 2011). The Cochrane 'Risk of bias' tool is available in Review Manager 5.3 (RevMan 2014), it assesses the following domains:
sequence generation;
allocation concealment;
blinding of participants and personnel;
blinding of outcome assessment;
incomplete outcome data;
selective outcome reporting; and
'other bias'.
The review authors assigned a judgement for the risk of bias for each domain as being 'high', 'low' or 'unclear'. We based our judgements on the criteria for making judgements listed in Section 8.5 of the Cochrane Handbook for Systematic Reviews of Interventions, which focuses on whether the risk is of importance (i.e. whether the presence of the risk could have an important impact on the results or the conclusion of the trial) rather than whether a risk of bias is present or not (Higgins 2011).
If insufficient detail about what happened in the study was reported, the judgement made was usually ‘unclear' risk of bias. An ‘unclear’ judgement was also made if what happened in the study was known, but the risk of bias was unknown; or if an entry was not relevant to the study at hand (particularly for assessing blinding and incomplete outcome data, when the outcome being assessed had not been measured in the study).
Measures of treatment effect
For dichotomous outcomes (where the outcome of interest was either present or absent), we expressed the estimate of treatment effect of an intervention as risk ratios (RR) together with 95% confidence intervals (CIs). We had planned to present hazard ratios if there were time‐to‐event data.
In future updates, should continuous outcomes (such as mean visual analogue scores (VAS)) be reported, we will use mean differences and standard deviations. We will use standardised mean difference (SMD) as a summary statistic in meta‐analysis when the studies all assess the same outcome, but measure it in a variety of ways (for example, all studies measure pain but use different psychometric scales).
Unit of analysis issues
Apart from simple parallel randomised control trials (where the unit of randomisation is at the individual level), it was also possible to have 'split‐mouth' studies, in which different areas of the mouth are assigned different interventions. When split‐mouth studies were included and each individual trial participant had one tooth randomised to the intervention and another randomised to the control, our analyses took into account the paired nature of the data (Elbourne 2002) .
For clustered data, in trials where the unit of randomisation was the tooth, and the number of teeth included in the trial was not more than twice the number of participants, the data were treated as if the unit of randomisation was the individual. It was recognised that the resulting 95% confidence intervals produced would appear narrower (i.e. the estimate would seem to be more precise) than they should have been, and we therefore interpreted these accordingly.
Dealing with missing data
Where data were missing from the published report of a trial, we attempted to contact the author(s) to obtain the data and clarify any uncertainty. The review was based on an available case analysis where data were missing, followed by sensitivity analysis, where possible, if the missing data posed a high risk of bias. For continuous data, we used methods for estimating missing standard deviations that are recommended in section 7.7.3 of the Cochrane Handbook for Systematic Reviews of Interventions, if appropriate (Higgins 2011). Otherwise we did not undertake any imputations or use any statistical methods to impute missing data.
Assessment of heterogeneity
We assessed clinical heterogeneity by examining the types of participants (e.g. age), interventions (e.g. method of restoration) and outcomes (e.g. pain relief) in each study.
We assessed heterogeneity by inspection of the point estimates and confidence intervals on the forest plots. The variation in treatment effects was assessed by means of Cochran's test for heterogeneity and quantified by the I2 statistic. Heterogeneity was considered statistically significant if the P value was less than 0.1.
A rough guide to interpretation of the I2 statistic is as follows (Higgins 2011):
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%: may represent substantial heterogeneity;
75% to 100%: represents considerable heterogeneity.
The importance of the observed value of I2 depends on the magnitude and direction of effects and also the strength of evidence for heterogeneity (e.g. P value from the Chi2 test, or a confidence interval for I2).
Assessment of reporting biases
We assessed reporting bias as between‐study publication bias or within‐study reporting bias.
We assessed within‐study reporting bias by comparing the outcomes reported in the published report against the study protocol, whenever this could be obtained. If this was not obtainable, then we compared outcomes listed in the methods section with those whose results were reported. If non‐significant results were mentioned but not reported adequately, we considered that bias was likely to occur in a meta‐analysis and we sought further information from the authors of the study reports. Otherwise, this was noted as being at high risk of bias. If there was insufficient information to judge the risk of bias, this was noted as being at unclear risk of bias.
If there had been a sufficient number of trials (more than 10) in any meta‐analysis, we would have assessed publication bias according to the recommendations on testing for funnel plot asymmetry as described in section 10.4 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). If asymmetry had been identified, we would have examined possible causes or assessed it using a table to list the outcomes reported by each study included in the review, to identify whether there were any studies that did not report outcomes that had been reported by most studies.
Data synthesis
For dichotomous data, the estimate of effect of an intervention was expressed as risk ratios, together with 95% confidence intervals using a random‐effects model. For continuous outcomes, we planned to use mean differences and 95% confidence intervals to summarise the data for each group. We combined data from split‐mouth studies with data from parallel group trials using the method outlined by Elbourne 2002, using the generic inverse variance method in RevMan.
Subgroup analysis and investigation of heterogeneity
Where possible, we would have performed subgroup analyses on trials involving:
different types of intervention technique (e.g. conventional method for fitting crown versus Hall Technique);
different age groups (five years of age or younger versus more than five years old);
types of service delivery and types of funding;
depth of lesion.
Sensitivity analysis
We planned sensitivity analyses to examine the effect of inadequate randomisation, allocation concealment, and missing data on the overall estimates of effect. In addition, we would have examined the effect of including unpublished literature on the review's findings, had data been available.
'Summary of findings' table and quality assessment using the GRADE approach
We used the GRADE approach to rate the overall 'quality of evidence' for each outcome assessed in this review, and used this approach in our interpretation and discussion of the findings of this review. The outcomes that are most relevant to patients and decision making are summarised in the 'Summary of findings' table, along with GRADE quality ratings (Table 1; Table 2).
There are four possible ratings for the quality of evidence; 'high', 'moderate', low' and 'very low'. A rating of 'high quality' of evidence implies that we were confident in our estimate of effect and further research is very unlikely to change our confidence in the estimate of effect. A rating of 'very low' quality implies that any estimates of effect obtained are very uncertain.
The GRADE approach judges evidence from RCTs that do not have serious limitations as being 'high quality'. The following factors decrease the quality of evidence:
study limitations (risk of bias);
inconsistency;
indirectness of evidence;
imprecision; and
publication bias.
Depending on the severity of these factors, the quality of evidence may be downgraded by one or two levels for each aspect.
Results
Description of studies
Results of the search
The electronic searches identified 746 titles and abstracts. Data on the flow of results from the literature search is shown in Figure 1.
1.

Study flow diagram
Included studies
We found five studies suitable for inclusion. See Characteristics of included studies tables for more information about the studies.
Participants
Across the five trials, there were 438 child participants with 693 teeth.
Only three of the studies specified how many of the participants were boys and girls (Atieh 2008; Innes 2011; Santamaria 2014), with the breakdowns being quite even: 206 boys and 182 girls (see Characteristics of included studies). The ages of the participants were reported in all but one study (Ram 2003), and ranged from two to 10 years. All studies only reported data from primary teeth.
Setting and design
The studies were set in Saudi Arabia (Atieh 2008), the USA (Hutcheson 2012), the UK (Innes 2011), Israel (Ram 2003), and Germany (Santamaria 2014).
Three of the five included studies were of split‐mouth design (Hutcheson 2012; Innes 2011; Ram 2003), one was a parallel group study with only one tooth treated per child (Santamaria 2014), and the other was a randomised trial with randomisation at tooth level (Atieh 2008), although children could have more than one tooth treated and the clustering was not taken into consideration in the statistical analysis. The number of teeth was less than twice the number of participants and may have had a small effect on reduction of the size of confidence intervals; however, we did not consider that this would have a significant impact on the findings.
Two studies had a maximum of one‐year of follow‐up data (Hutcheson 2012; Santamaria 2014), one had a two‐year follow‐up (Atieh 2008), one had both six‐month and four‐year data (Ram 2003), and the last one had data available for one year, two years and five years (Innes 2011).
In two of the studies (Atieh 2008; Hutcheson 2012), all of the teeth had pulpotomies before the crowns or restorations were carried out.
In two of the studies, treatment was carried out by single operators (Atieh 2008; Hutcheson 2012), and although there was no information about whether the operators were specialists, the studies were both set in dental clinics for children. In Santamaria 2014, treatments were carried out by 12 dentists (seven specialists and five postgraduate trainees), in Innes 2011 the treatments involved 17 general dentists in 10 primary care general practices. while the Ram 2003 study did not specify who treated the children or how many clinicians there were.
Two studies compared PMCs with open sandwich restorations (Atieh 2008; Hutcheson 2012). Both Innes 2011 and Santamaria 2014 compared Hall crowns with fillings. However, the Santamaria 2014 study included a third comparison arm of non‐restorative caries treatment, which opened out cavities and taught parents to keep them clean and applied a fluoride varnish, and this arm was compared to both Hall crowns and fillings. In Ram 2003, two types of crown were compared: a stainless steel one similar to the other studies, and an aesthetic one where a stainless steel crown had a composite veneer added to cover its facial, occlusal, mesial and distal aspects. A greater reduction in tooth surface was required for the aesthetic crown (around 1.5 mm) to allow for its greater thickness.
To summarise, the following were the comparisons and interventions used:
PMCs versus fillings (Atieh 2008; Hutcheson 2012; Innes 2011; Santamaria 2014). Both Innes 2011 and Santamaria 2014 used the Hall Technique in the crown group. Atieh 2008 and Hutcheson 2012 used conventional methods of fitting the crowns;
PC versus non‐restorative caries treatment (Santamaria 2014);
different types of PC: PMCs versus composite or aesthetic crowns (Ram 2003). Both types of crown were fitted using the conventional technique.
Outcomes
Clinical and radiographic outcomes were recorded in all five studies.
Four studies recorded clinical/radiographic measures of success, that is, where there was no pain, no signs or symptoms of infection, and where the restoration was intact (Atieh 2008; Hutcheson 2012; Innes 2011; Santamaria 2014). These outcomes were grouped to give a composite measure of success.
Two of these studies grouped outcomes for clinical/radiographic failure into minor failure (restoration repaired or tooth managed with no pulpal intervention required) and major failure (irreversible pulpitis, periradicular periodontitis) (Innes 2011; Santamaria 2014).
Only one study recorded use of a "modified US Public Health Service" scale for clinical characteristics of the restoration (Atieh 2008).
Four studies measured gingival health. Atieh 2008 and Ram 2003 measured bleeding on probing and Santamaria 2014 recorded gingival swelling as 'none', 'mild' (with bleeding on probing) or 'moderate/severe' (with bleeding after air drying). Hutcheson 2012 only reported presence or absence of inflammation, but did not give data on bleeding.
Only one study measured bone resorption (Ram 2003).
Patient‐reported outcomes were only investigated in two trials (Innes 2011; Santamaria 2014), with one study recording patient/parent and dentist treatment preferences (Innes 2011), and the other measuring the child’s discomfort and behaviour during treatment, and parent and dentist ratings of child’s discomfort and behaviour during treatment (Santamaria 2014).These outcomes were reported as number of patients in each category of the scale. Different 5‐point Likert scales were used to rate whether discomfort was experienced during the procedure. In Innes 2011, the dentist(s) ratings based on this scale were: 1 no apparent discomfort; 2 very mild, almost trivial; 3 mild, not significant; 4 moderate, but child coped; 5 significant, unacceptable. For Santamaria 2014, children rated pain on this scale as: 'very low', 'low', 'moderate', 'intense', or 'very intense'. For the purpose of analysis, we dichotomised these scales so that all children who rated 'moderate' and above were considered as having experienced discomfort.
Excluded studies
Reasons for exclusion of studies are described in the Characteristics of excluded studies tables.
We excluded eight studies.
Six were not RCTs: four of them were retrospective in design (Braff 1975; Einwag 1996; Farooq 2000; Holan 2002); one study was unclear about whether it was a prospective or retrospective analysis (Eriksson 1988); the other study was Roberts' prospective analysis reported outcomes of different restorations placed in a private practice where treatment was dictated by the clinical presentation of the tooth in question and not based on random allocation (Roberts 2005). Six compared PCs with fillings (Braff 1975; Einwag 1996; Eriksson 1988; Farooq 2000; Holan 2002; Roberts 2005). In five studies, PCs were compared with amalgam restorations (Braff 1975; Einwag 1996; Eriksson 1988; Farooq 2000; Holan 2002), and in the sixth study, with a resin‐modified glass ionomer (Roberts 2005). Two studies investigated the success rates of restoration type placed over teeth that had undergone formocresol pulpotomy (Farooq 2000; Holan 2002).
The seventh study compared two different types of veneered preformed crowns (Leith 2011), but as these were both essentially the same material rather than our preplanned comparison of metal versus aesthetic crowns, we excluded this study.
The eighth excluded study involved crowns for permanent teeth (Zagdwon 2003) (the other seven excluded studies were carried out with primary teeth).
Risk of bias in included studies
This is summarised in Figure 2 and Figure 3.
2.
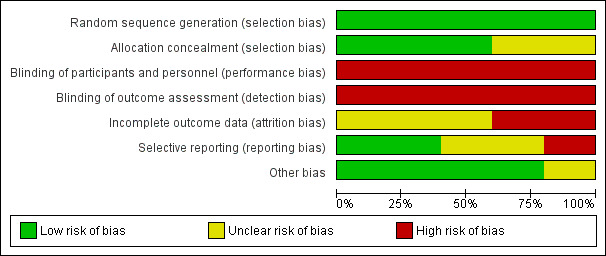
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.
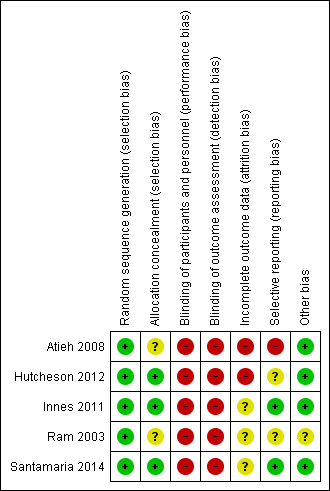
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
We judged all the included studies to be at low risk of bias for random sequence generation. For allocation concealment, descriptions of adequate methods were provided, with the exceptions of Atieh 2008 and Ram 2003, which did not provide information on the methods used.
Blinding
Blinding of participants and personnel
The interventions compared in the studies looked different (i.e. usually crowns compared with fillings or no fillings, or a metal crown compared with a white crown). It was therefore, not possible to blind the dentist and other personnel involved in providing care, or the participants and their parents. Whether the knowledge of which intervention the participant was getting was going to affect the care provided was not apparent and, in line with Cochrane guidance, we rated this domain for all trials as being at a high risk of bias.
Blinding of outcome assessment
There was a high risk of bias for outcome assessment for all the included trials, as the assessments of treatment success and failure could depend on various factors. Some of these criteria require judgement that could be affected by the outcome assessors' knowledge of the type of intervention used.
Incomplete outcome data
In Atieh 2008, in addition to participants who were lost to follow‐up (15% of participants from the PC group and 19% in the restoration group at two‐year follow‐up), participants who had bleeding during pulpotomy were excluded from the analysis. In Hutcheson 2012, 77.5% of participants were analysed at 12 months, but no data were given about the similarity of key characteristics between the groups with regard to dropouts, so the level of attrition bias was unknown. We judged the risk of biases for the other studies as being low (Innes 2011; Ram 2003; Santamaria 2014); for Innes 2011, 94% of teeth were available for analysis at two years, but this decreased to 70% at four years. As this was a split‐mouth study, numbers of losses and reasons for loss were similar in both arms and so attrition bias was low. Similarly, Santamaria 2014 analysed 87.5% of participants at one year, but the reasons for losses were balanced. The Ram 2003 split‐mouth study only had 11 participants and lost one, but did not state a reason for the loss.
Selective reporting
The protocols for Atieh 2008, Hutcheson 2012 and Ram 2003 were not available. We judged Atieh 2008 as being at high risk of selective outcome reporting as the statistical analysis had not taken clustering into account and there was insufficient information reported to allow for an analysis for the two‐year data. We considered the other two studies as being at unclear risk of bias.
The protocols for Innes 2011 and Santamaria 2014 were registered online and we could verify that the outcomes were reported as planned so we considered them to be at low risk of selective outcome reporting.
Other potential sources of bias
We found no evidence of other sources of bias.
Effects of interventions
Comparison 1: Crown (regardless of technique/material) versus filling (with and without carious tissue excavation)
Four out of the six included studies used teeth as the unit of randomisation (Atieh 2008; Hutcheson 2012; Innes 2011; Ram 2003), with paired split‐mouth studies conducted in three of these (Hutcheson 2012; Innes 2011; Ram 2003). As planned in the protocol, we conducted adjustments for the split‐mouth design using generic inverse variance for the initial analysis. However, there was no material difference between the results obtained with this method compared to those obtained without adjustments (i.e. a difference of only around +/‐ odds ratio 0.01 to 0.02).
For Atieh 2008, we conducted a sensitivity analysis (summarised in Table 3), and found that although the precision could be affected, there was no real impact on the conclusions drawn.
1. Sensitivity analysis of Analysis 1.1 (with and without Ateih 2008).
| Outcome (Analysis) | With all studies included | Excluding Atieh 2008 | ||||
| Studies | Participants | Effect estimate | Studies | Participants | Effect estimate | |
| 1.1 Major failure | ||||||
| 1.1.1 Short term (less than 12 months) | 1 | 76 | Not estimable | Not affected | ||
| 1.1.2 Long term 12 months or more | 3 | 346 | RR 0.18 (CI 0.06 to 0.56) | Not affected | ||
| 1.2 Pain | ||||||
| 1.2.1 Short term (less than 12 months) | 1 | 64 | Not estimable | Not affected | ||
| 1.2.2 Long term (12 months or more) | 2 | 312 | RR 0.15 (0.04 to 0.67) | Not affected | ||
| 1.3. Peri/postoperative discomfort/pain | 2 | 381 | RR 0.56 (0.36 to 0.87) | Not affected | ||
| 1.4 Gingival bleeding | ||||||
| 1.4.2 Short term (less than 12 months) | 2 | 226 | RR 1.69 (0.61, 4.66) | 1 | 76 | 5.00 (0.25, 100.80) |
| 1.4.3 Long term (12 months or more) | 2 | 195 | 1.74 (0.99, 3.06) | 1 | 62 | 1.50 (0.47, 4.80) |
Therefore, the results are presented without adjustments for within patient randomisations, using RR as the effect measure and including all studies for completeness and ease of interpretation.
Major failures
Three studies evaluated this comparison and data were available for both time points of interest (Hutcheson 2012; Innes 2011; Santamaria 2014). In the short term, there were no failures in either group (Analysis 1.1.1; 76 teeth, 38 participants; one study, Hutcheson 2012). In the long term (12 to 48 months), crowns were less likely to fail than fillings (Analysis 1.1.2; RR 0.18, 95% CI 0.06 to 0.56; 346 teeth; three studies (Hutcheson 2012; Innes 2011; Santamaria 2014); I2 = 0%).
1.1. Analysis.
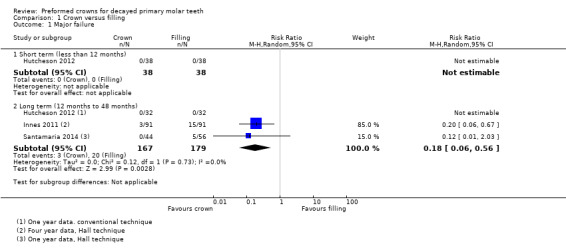
Comparison 1 Crown versus filling, Outcome 1 Major failure.
Pain
Data were only available for up to two years for this outcome and came from two studies (Hutcheson 2012; Innes 2011). In the long term (12 months to 24 months), crowns were less likely to cause pain than fillings (Analysis 1.2.2: RR 0.15, 95% CI 0.04 to 0.67; 312 teeth; two studies; I2 = 0%). The results for the short term were not estimable (Analysis 1.2.1: 64 teeth, 32 participants; one study, Hutcheson 2012).
1.2. Analysis.
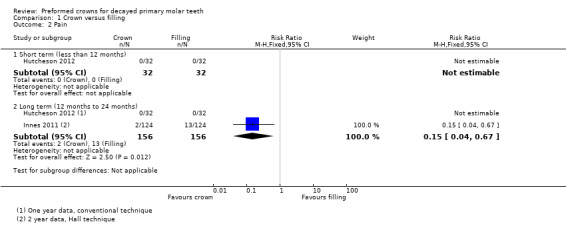
Comparison 1 Crown versus filling, Outcome 2 Pain.
Satisfaction with treatment
The studies did not measure this outcome.
Time to restoration failure/retreatment
The studies did not measure this outcome.
Discomfort associated with procedure
Participants had more discomfort with fillings than crowns (Analysis 1.3; RR 0.56, 95% CI 0.36 to 0.87; 381 participants; two studies; I2 = 0%). Pain was considered present when children rated their pain as 'moderate', 'intense' or 'very intense' in Santamaria 2014, and when dentists rated their patients' discomfort during treatment as 'moderate' or 'significant' in Innes 2011.
1.3. Analysis.
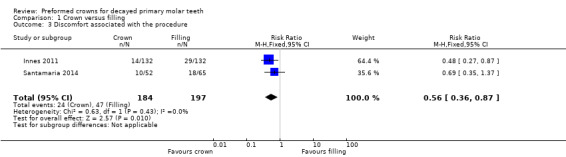
Comparison 1 Crown versus filling, Outcome 3 Discomfort associated with the procedure.
Cost
The studies did not measure this outcome.
Adverse events (e.g. bone loss, gingival inflammation or others)
The only adverse event recorded for crowns versus fillings was gingival bleeding. This was reported in three studies (Atieh 2008; Hutcheson 2012; Santamaria 2014). Although the results were not conclusive, there appeared to be an increased risk of bleeding from crowns when compared to fillings:
short term (up to 12 months): Analysis 1.4.1: RR 1.69, 95% CI 0.61 to 4.66; 226 participants; two studies (Atieh 2008; Hutcheson 2012); I2 = 0%
long term (12 months): Analysis 1.4.2: RR 1.74, 95% CI 0.99 to 3.06; 195 teeth; two studies (Atieh 2008; Hutcheson 2012); I2 = 0%
1.4. Analysis.
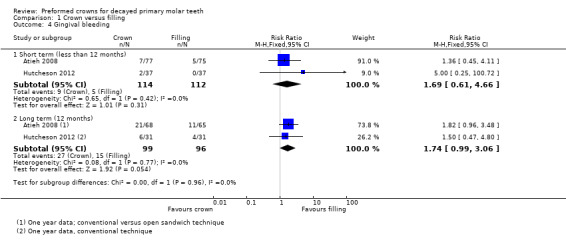
Comparison 1 Crown versus filling, Outcome 4 Gingival bleeding.
Comparison 2: Crown (regardless of technique/material) versus no crown or filling (non‐restorative treatment)
One study had three comparison arms: 1) PMC using the Hall Technique, 2) filling and 3) non‐restorative caries treatment (Santamaria 2014). The results of the study are shown in Analysis 2.1; Analysis 2.2; Analysis 2.3.
2.1. Analysis.

Comparison 2 Crown versus non‐restorative caries treatment, Outcome 1 Major failure.
2.2. Analysis.

Comparison 2 Crown versus non‐restorative caries treatment, Outcome 2 Discomfort associated with the procedure.
2.3. Analysis.
Comparison 2 Crown versus non‐restorative caries treatment, Outcome 3 Gingival bleeding.
Three outcomes were reported in this study, which applied fluoride varnish to the non‐restorative treatment group. The total number of participants analysed for this comparison was 92 (44 in the Hall Technique arm and 48 in the non‐restorative arm) at one year, and 52 in each arm immediately after treatment.
Major failures
Crowns seemed less likely to result in a major failure assessed at one year after treatment, though the result was inconclusive (Analysis 2.1; RR 0.12; 95% CI 0.01 to 2.18; 92 participants).
Pain (long term) following treatment
The studies did not measure this outcome.
Satisfaction with treatment
The studies did not measure this outcome.
Time to restoration failure/retreatment
The studies did not measure this outcome.
Discomfort associated with procedure
Crowns seemed more likely to result in children reporting 'moderate', 'intense' or 'very intense' pain during treatment (reported immediately after treatment was completed), though the result was inconclusive (Analysis 2.2; RR 1.67; 95% CI 0.65 to 4.25; 104 participants).
Cost
The studies did not measure this outcome.
Adverse events (e.g. bone loss, gingival inflammation or others)
Crowns seemed to be more likely to cause gingival bleeding when assessed one year after treatment, though the result was inconclusive (Analysis 2.3; RR was 1.09; 95% CI 0.42 to 2.86; 92 participants).
Comparison 3: Crown (stainless steel) versus crown (aesthetic veneer) using the conventional technique
Only one small split‐mouth study (11 participants) reported adverse events at six months and four years (Ram 2003). No other outcomes of interest to this review were reported.
Adverse events
At six months, none (0/11) of the PMC sites had gingival bleeding, but all (11/11) veneer sites had bleeding, 10 of which bled on probing. This was statistically significant using McNemar's test (P < 0.001).
At four years, there was one case of gingival bleeding with a PMC and one with a veneer crown, from the 10 participants followed up.
Bone resorption was reported. There was one case at six months in a tooth treated with a veneer crown. There was no bone resorption at either the veneer crown or stainless steel sites at four‐year follow‐up.
The findings of this study are shown visually in Analysis 3.1 and Analysis 3.2.
3.1. Analysis.
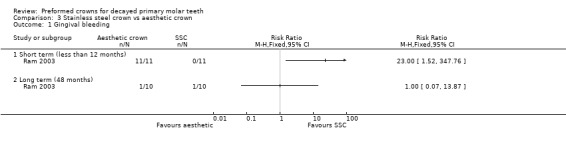
Comparison 3 Stainless steel crown vs aesthetic crown, Outcome 1 Gingival bleeding.
3.2. Analysis.

Comparison 3 Stainless steel crown vs aesthetic crown, Outcome 2 Bone resorption.
Comparison 4: Crown (Hall Technique) versus crown (conventional technique)
None of the included studies compared the effectiveness or safety of the Hall Technique versus the conventional technique of fitting a crown.
Discussion
Summary of main results
Our aim was to evaluate the clinical effectiveness and safety of crowns compared with fillings, another type of crowns or method of crown placement, or non‐restorative or no treatment approaches. We found five studies that met the inclusion criteria for this review (Atieh 2008; Hutcheson 2012; Innes 2011; Ram 2003; Santamaria 2014), which provided data on three out of the four comparisons of interest (crown versus filling; crown versus no crown/filling; metal crowns (PMC) versus aesthetic crowns).
Most of the evidence looked at the first comparison, crowns compared to fillings (four out of five studies). Crowns outperformed fillings for major failure and pain in the long term. There may be an increased risk of gingival bleeding; however, this result was inconclusive and its clinical relevance debatable. Data from two studies that used the Hall Technique showed that discomfort during treatment was lower for crowns than fillings.
The benefits and harms for crowns versus non‐restorative caries treatment were uncertain due to the very low quality of the evidence. Only one study (analysing between 92 to 104 participants per outcome) evaluated this comparison, and this study reported no major failures in the metal crowns fitted using the Hall Technique arm and four in the non‐restorative arm within one year. The gingival bleeding risk may have been higher in the crowns group but the result was unclear. The risk of experiencing discomfort appeared to be higher in the PMC group, though this result was also unclear.
There was even less data for comparison of PMC versus aesthetic crowns; one very small study (11 pairs of teeth) reported only on gingival bleeding and bone resorption, with more gingival bleeding for the teeth with aesthetic crowns than for those with PMC.
Due to a lack of detail on the extent of the carious lesions, it was not possible to draw any conclusions concerning our secondary objective of determining whether the extent of decay had an effect on the clinical outcome of primary teeth restored with PCs compared with fillings.
In summary, most of the findings in this review favoured crowns compared to conventional fillings, particularly when the Hall Technique was used. There were very limited data to assess whether crowns are better than non‐restorative caries treatment. There were no data to assess the most effective technique for using crowns (conventional or Hall).
Overall completeness and applicability of evidence
We included five studies in the review, however, this does not provide a complete picture for all comparisons, all outcomes and all timepoints. Nonetheless, crowns seemed to perform better than fillings, and the variability between the studies reinforces the applicability of this finding to different settings. Only one study compared crowns to non‐restorative caries treatment and none compared different crown fitting techniques, so these comparisons lack evidence. The findings for metal crowns compared to aesthetic crowns was only for one particular type of white crown and, while there are now many others available, no randomised studies have compared them yet.
One of the studies was still ongoing at the time of publication of this review (Santamaria 2014), and only data from one of the three countries involved were available.
There were no data available from any of the studies that would allow us to investigate our secondary objective of determining the influence of the extent of carious lesions in a tooth on the clinical outcome.
Interventions
For crowns versus fillings, we found five studies that compared preformed crowns against filling materials or non‐restorative caries treatment, and included data from three studies in our primary meta‐analysis of major failure in the long term. Only one study compared stainless steel crowns against aesthetic crowns. There were no studies that compared the Hall Technique with conventional crowns and this leaves the question of which of these crown‐fitting methods is likely to be better.
Interpreting the data is complicated because of the relatively low number of studies and the degree of heterogeneity between the interventions. So although four studies investigated crowns, two looked at crowns using the Hall Technique and two looked at conventional crowns, but even within those two groups, there were other differences. In both of the studies that looked at conventional crowns (Atieh 2008; Hutcheson 2012), crowns were placed on teeth that had undergone pulp treatment whereas none of the teeth in the Hall Technique studies had pulp treatments before the crowns were fitted. Each of the four studies used different types of filling materials in the control arm. Of the two studies of Hall Technique crowns, one was carried out by general dental practitioners (GDPs) in general dental practice (Innes 2011), and the other was carried out by specialists in a secondary care setting (Santamaria 2014).
There was no standardisation and often poor reporting for the extent of carious lesion in the teeth included in the studies. One included teeth where the carious tissue involved at least two surfaces (Santamaria 2014), and one included a variety of carious lesions (although almost half of the lesions were more than half‐way through dentine radiographically) (Innes 2011). Two of the studies included teeth where pulp treatment was carried out for extensive carious lesions or following pulp exposure (Atieh 2008; Hutcheson 2012). One study did not report the extent of the carious lesion in the teeth (Ram 2003). This variation meant we could not investigate or draw conclusions about how extensive the carious lesion needs to be to result in an improved outcome from crowns over fillings.
Nevertheless in all cases, crowns performed either as well as, or better than, fillings. So the heterogeneity perhaps strengthens, rather than weakens the case for crowns improving outcomes for primary molar teeth.
Outcomes
All but one of the studies included data on two of our primary outcomes (Ram 2003), major failures and pain. However, it is of note that none of them ‐ even the study of PMCs compared with aesthetic crowns (Ram 2003) ‐ reported on the third of our primary outcomes, which was satisfaction with treatment (which included satisfaction with aesthetics). This presents a gap in the evidence and is another example of the lack of patient‐reported outcomes in clinical dental trials.
We did not find any studies that reported on 'time to restoration failure/retreatment' as an outcome. In the next update of this review, we will include 'minor failures', which will be a composite measure that includes restoration loss, fractured or worn restorations that need to be repaired or replaced, carious tissue around the margin of a restoration that needs to be repaired or the replacement of the restoration. These outcomes were reported in all of the studies to some extent.
Time points
There was no common time point at which the studies could be compared. Since the studies measured so many different time points (six months, up to one year, up to two years, up to five years), and several of the studies reported data at several time points, combining the data to present a true picture of the comparisons proved problematic. To give the most realistic picture, we have presented data within the comparisons as up to 12 months (i.e. what is likely to happen in the short term) and then have combined the data for over 12 months (i.e. what is likely to happen in the long term). This has meant that the forest plots (Analysis 1.1, Analysis 1.2 and Analysis 1.4) contain data from studies where the data ranged from 0 to 12 months with studies that included data that ranged from 0 to 48 months. Whilst this is not ideal, and may introduce an unknown bias, we think this presents dentists and parents with evidence of how they can expect the different interventions to fare relatively in the short and long term.
Quality of the evidence
The evidence was obtained from well conducted randomised controlled trials (split‐mouth, and with tooth as unit of randomisation) with a generally low risk of bias for randomisation and allocation concealment. However, the overall risk of bias for the studies was high, due to inadequate blinding and risks in attrition bias. In addition, there was imprecision as the study sizes were relatively small, and therefore large confidence intervals were observed.
For the comparisons of crowns against fillings, we downgraded all outcomes one level due to the lack of blinding, and gingival bleeding a second level due to imprecision. For the comparison of crowns fitted using the Hall Technique versus non‐restorative caries treatment, we downgraded outcomes three levels for serious risk of bias and imprecision. The quality of evidence therefore ranged from moderate (we have moderate confidence in the estimate of the effect) to very low (we are very uncertain of the estimate of the effect).
Very little information was available for the comparison of metal versus aesthetic crowns, and we consider the quality of evidence for all the outcomes in this comparison ‐ which came from only one small study (Ram 2003) ‐ as very low.
Potential biases in the review process
Two of the review authors (NI, RS), were involved in two of the studies included (Innes 2011; Santamaria 2014). However, data extraction and risk of bias assessment for these studies were performed by two other review authors and compared against data from another Cochrane Review (Ricketts 2013).
There are many variations in the techniques and materials used in the type of interventions investigated in this review. Therefore, certain assumptions had to be made about whether data could be pooled, despite these variations. We had decided to investigate some variations as subgroups. These subgroups were determined a priori, and carried out as planned whenever data were available. However, the small number of studies available and the large confidence intervals observed in some studies means that these subgroup analyses are not likely to be of sufficient power to detect a difference. We made a priori decisions to pool data unless subgroup analyses showed a difference for certain variations in technique. For example, in our analysis of major failures, there was only one small study of conventional crown technique, which showed no difference between crowns and the conventional methods of restorations, whereas the studies using the Hall Technique seemed to show a large effect size. We pooled this as planned, but we may have to revisit the assumption when more data become available, and any potential heterogeneity or differences in effectiveness due to variations in technique may become more apparent.
Four out of the five included studies used teeth as the unit of randomisation (Atieh 2008; Hutcheson 2012; Innes 2011; Ram 2003), and paired split‐mouth randomisation was conducted in three of these (Hutcheson 2012; Innes 2011; Ram 2003). As planned in the protocol, we conducted adjustments for the split‐mouth design using the generic inverse variance technique, and tested whether the adjustments had an impact on the effect estimate obtained. We found minimal or no difference (a maximum difference of odds ratio 0.02) and took the pragmatic approach of reporting the results without adjustments, using relative risk as the effect estimate for ease of interpretation.
Another study contained clustered data with 47 children having more than one molar treated in the study, but no further information was given (Atieh 2008); this meant we could not determine the extent of the clustering (some children could have had up to eight molars treated with crowns). Because of the uncertainty around the effect this would have on the meta‐analyses, we initially excluded this study when the analyses with adjustments were conducted. After deciding to present results without adjustments, we conducted a sensitivity analysis to see whether the inclusion of the study affected the meta‐analysis results. There were no real impacts on the conclusions drawn, therefore the results of this study were included. In future updates of this review when more studies are available for inclusion, the impact of adjustments required for clustering should be revisited and a pragmatic decision taken on whether to continue presenting the unadjusted results.
Agreements and disagreements with other studies or reviews
It is interesting to note that in the following excluded studies (where allocation method was reported), there was a general bias towards placing PMCs on teeth with more extensive carious lesions (Eriksson 1988; Roberts 2005), or where there was less remaining tooth structure (Holan 2002), and both Eriksson and Holan both reported reported greater success rates for the crowned teeth.
In Randall's systematic review of the literature, comparing PMCs with amalgam, it was noted that, despite the heterogeneity of the 10 studies included, there was a positive outcome in all studies in favour of the PMC compared with amalgam restorations (Randall 2000). However, there were no RCTs available for inclusion in the review and the potential for bias must be taken into consideration.
Only one study has compared the Hall Technique to conventional crowns; this was a retrospective study of one specialist practitioner's records that assessed the clinical and radiographic success of both techniques (Ludwig 2014). Failure was defined as a lost crown and/or the requirement for further treatment for carious tissues or pulp pathology, clinically or radiographically. There was a high degree of success for both techniques (97% for the Hall Technique, mean follow‐up 15 months and 94% for conventionally placed crowns, mean follow‐up 52 months) and no statistically significant difference between them.
One study compared one type of aesthetic crown with another (Leith 2011). This study was excluded because the crowns were essentially the same (with the same metal framework) and the method for placing them was the same. They differed only in the method by which the white facing adhered to the underlying crown and showed equally successful outcomes for intact facings, gingival inflammation, radiographic success and parental satisfaction for success.
A recent comprehensive systematic review of the literature around the use of PCs agreed with the findings of our review, and concluded that metal crowns (fitted conventionally or using the Hall Technique) and aesthetic crowns had superior clinical performance as restorative options for primary molar teeth (Seale 2015). The review included reports on 22 clinical studies, three case reports, 21 reviews and surveys and 13 in vitro studies on all types of crowns for both primary and permanent molar teeth. Although an assessment of the quality of the literature was carried out, this was not done through use of a recognised tool. No meta‐analysis was carried out, but the authors reported assigning weighting criteria to the reports that assessed clinical research with a threshold for inclusion of 60%. How the quality assessment, weighting criteria and threshold were derived is not clear.
Authors' conclusions
Implications for practice.
Crowns placed on primary molar teeth with carious lesions, or where pulp treatment has been carried out, are likely to reduce the risk of major failure or pain in the long term compared to fillings. Crowns fitted using the Hall Technique may reduce discomfort at the time of treatment compared to fillings.
Implications for research.
The population investigated included only fit and healthy children. The performance of restorative interventions is important for children with special needs and may be different in those children with limited ability to tolerate invasive dental procedures. This should be considered when designing future trials and considering generalisability of findings. As most restorative procedures in children are undertaken by non‐specialists, these clinicians should be included in future research to improve generalisability of the results.
Future research should include discomfort at the time of treatment and pain following treatment. Reporting should include adequate detail about how these were assessed and who reported them, as well as consideration of the multi‐dimensionality of pain and its expression, especially with children.
There were no studies that compared the Hall Technique to conventional crowns. So, although crowns outperformed fillings, it is not possible to say whether crowns should be fitted conventionally (involving local anaesthesia and removal of tooth substance), or fitted less invasively. This is an important question in terms of best clinical outcome (fewer major failures and less gingival bleeding), as well as from children's and parents' perspectives, and that of cost. There was very little measurement and reporting of patient‐reported outcomes. Only the two trials that involved the Hall Technique investigated pain or discomfort at time of treatment. The studies investigated adverse events in a limited way, with gingival bleeding measured in three studies and bone resorption in one, but other adverse events, as well as cost and satisfaction with treatment, were not investigated. A core outcome set is not available yet for trials investigating restorative interventions, but would be helpful to guide researchers in the design of trials and would improve the ease of comparing and collating findings. Longer follow‐up in studies should be considered. We found no studies that investigated the management of primary teeth with developmental defects. These should also be investigated in the future, as well as the implications of the depth of carious lesions.
What's new
| Date | Event | Description |
|---|---|---|
| 25 November 2015 | New citation required and conclusions have changed | In the previous version of the review, there were no randomised controlled trials. There are now five, which provide moderate quality evidence that preformed crowns reduce risk of major failure and long‐term pain compared to fillings. |
| 21 January 2015 | New search has been performed | Search updated. Scope expanded from preformed metal crowns to include preformed crowns of other materials. Five new studies included. |
History
Protocol first published: Issue 4, 2005 Review first published: Issue 1, 2007
| Date | Event | Description |
|---|---|---|
| 1 August 2008 | Amended | Converted to new review format. |
Acknowledgements
The review authors would like to thank Sylvia Bickley and Anne Littlewood for assistance with searching, the peer referees who commented on this review as part of the pre‐publication process (David Manton, Nicky Kilpatrick, Barbara Chadwick), Laura MacDonald for her assistance with editorial processing and Jan Clarkson and Helen Worthington for insight into the implications of the methodological inadequacies of some of the clinical trials.
We would also like to thank Dafydd Evans, one of the authors of version one of this review who also conceived the original review, and contributed to its search strategy, screening of search results and retrieved papers, screening of retrieved papers against inclusion criteria and resolving conflicts related to risk of bias.
Appendices
Appendix 1. MEDLINE (Ovid) search strategy
1. Tooth crown/ 2. crown$.mp. 3. "indirect restor$".mp. 4. "fixed dental prosthes$".mp. 5. (prosthodontic adj3 fix$ adj3 restor$).mp. 6. or/1‐5 7. exp Tooth/ 8. (tooth or teeth or dentition or dental).mp. 9. 7 or 8 10. (deciduous or primary or milk or baby or natal).mp. 11. exp Child/ 12. (child$ or baby or babies or toddler$ or infant$ or adolescen$).mp. 13. or/10‐12 14. 6 and 9 and 13
The above subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomized trials in MEDLINE: sensitivity maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of The Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011].
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 2. Cochrane Oral Health Group Trials Register search strategy
1 (crown*:ti,ab) AND (INREGISTER) 2 ("indirect restor*":ti,ab) AND (INREGISTER) 3 ("fixed dental prosthes*":ti,ab) AND (INREGISTER) 4 ((prosthodontic* AND fix* AND restor*):ti,ab) AND (INREGISTER) 5 (#1 or #2 or #3 or #4) AND (INREGISTER) 6 ((deciduous or primary or milk or natal):ti,ab) AND (INREGISTER) 7 ((child* or baby or babies or todder* or infant* or adolesc*):ti,ab) AND (INREGISTER) 8 (#6 or #7) AND (INREGISTER) 9 (#5 and #8) AND (INREGISTER)
Appendix 3. Central Register of Controlled Trials (CENTRAL) search strategy
#1 MeSH descriptor: [Crowns] explode all trees #2 crown* #3 "indirect restor*" #4 "fixed dental prosthes*" #5 (prosthodontic* and fix* and restor*) #6 {or #1‐#5} #7 [mh Tooth] #8 (tooth or teeth or dentition or dental) #9 #7 or #8 #10 MeSH descriptor: [Child] explode all trees #11 (child* or baby or babies or toddler* or infant* or adolescen*) #12 {or #10‐#11} #13 #6 and #9 and #12
Appendix 4. EMBASE (Ovid) search strategy
1. Tooth crown/ 2. crown$.mp. 3. "indirect restor$".mp. 4. "fixed dental prosthes$".mp. 5. (prosthodontic adj3 fix$ adj3 restor$).mp. 6. or/1‐5 7. exp Tooth/ 8. (tooth or teeth or dentition or dental).mp. 9. 7 or 8 10. (deciduous or primary or milk or baby or natal).mp. 11. exp Child/ 12. (child$ or baby or babies or toddler$ or infant$ or adolescen$).mp. 13. or/10‐12 14. 6 and 9 and 13
The above subject search was linked to the Cochrane Oral Health Group filter for identifying RCTs in EMBASE via OVID:
1. random$.ti,ab. 2. factorial$.ti,ab. 3. (crossover$ or cross over$ or cross‐over$).ti,ab. 4. placebo$.ti,ab. 5. (doubl$ adj blind$).ti,ab. 6. (singl$ adj blind$).ti,ab. 7. assign$.ti,ab. 8. allocat$.ti,ab. 9. volunteer$.ti,ab. 10. CROSSOVER PROCEDURE.sh. 11. DOUBLE‐BLIND PROCEDURE.sh. 12. RANDOMIZED CONTROLLED TRIAL.sh. 13. SINGLE BLIND PROCEDURE.sh. 14. or/1‐13 15. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 16. 14 NOT 15
Appendix 5. US National Institutes of Health Trials Register (ClinicalTrials.gov) and WHO International Clinical Trials Registry Platform search strategy
crown and tooth and child
Appendix 6. Open Grey search strategy
crown and tooth and child
Data and analyses
Comparison 1. Crown versus filling.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Major failure | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Short term (less than 12 months) | 1 | 76 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Long term (12 months to 48 months) | 3 | 346 | Risk Ratio (M‐H, Random, 95% CI) | 0.18 [0.06, 0.56] |
| 2 Pain | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Short term (less than 12 months) | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Long term (12 months to 24 months) | 2 | 312 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.04, 0.67] |
| 3 Discomfort associated with the procedure | 2 | 381 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.36, 0.87] |
| 4 Gingival bleeding | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Short term (less than 12 months) | 2 | 226 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.61, 4.66] |
| 4.2 Long term (12 months) | 2 | 195 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.74 [0.99, 3.06] |
Comparison 2. Crown versus non‐restorative caries treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Major failure | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Long term (12 months) | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.01, 2.18] |
| 2 Discomfort associated with the procedure | 1 | 104 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.65, 4.25] |
| 3 Gingival bleeding | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Long term (12 months) | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.42, 2.86] |
Comparison 3. Stainless steel crown vs aesthetic crown.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Gingival bleeding | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Short term (less than 12 months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Long term (48 months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Bone resorption | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 Short term (less than 12 months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Long term (48 months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Atieh 2008.
| Methods | RCT with 2‐year follow‐up Unit of randomisation: teeth |
|
| Participants |
Setting: Dammam Medical Center (DMC) in the Eastern Province of Saudi Arabia between January 2003 and January 2004. Single site. Single operator Sample size Number screened: 535 children Number eligible: 126 (39 refused) Number randomised: 87 participants (160 teeth), 47 treated for more than one tooth Number analysed: at 24 months, 65 teeth with fillings (81%) and 68 teeth with crowns (85%) Age: 4–7 years, mean 5.5 years; SD 1.1 Sex: 41 boys and 46 girls Teeth/lesions: not reported Inclusion criteria for participants:
Inclusion criteria for teeth:
Exclusion criteria for teeth:
|
|
| Interventions |
Intervention: PMCs Control: modified open‐sandwich technique using resin‐modified glass ionomer cement or composite resin restorations All teeth had pulpotomies carried out before the crowns or restorations were placed. All participants were given oral hygiene instructions after treatment |
|
| Outcomes | Outcomes were assessed at 6, 12, 18 and 24 months ± 2 weeks, or until tooth exfoliation or participant dropout and included:
|
|
| Source of Funding | No information provided | |
| Declaration of interest | No information provided | |
| Notes | All teeth had pulptotomies carried out before the interventions Follow‐up numbers: initially: fillings 80 (100%), crowns 80 (100%) 6 months: fillings 75 (94%), crowns 77 (96%) 12 months: fillings 73 (91%), crowns 74 (93%) 18 months: fillings 69 (86%), crowns 71 (89%) 24 months: fillings 65 (81%), crowns 68 (85%) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was generated through a computer program where each primary molar had an equal chance to be assigned to either SSC or RMGIC/CRR" |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment method provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Both the participants and the dentist could not be blinded to the intervention because of the different appearance of the two types of restoration" Comment: no blinding, patient and operator aware of different treatments, as restorations looked different. Unclear whether this affected level or quality of care |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "At each follow‐up visit, the children were examined by the same dentist in a dental chair with a dental mirror and a probe" Comment: Participant and operator were aware of different treatments, which could affect judgement of subjective outcomes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Participants who had bleeding during pulpotomy were excluded from analysis (total of 6: 2 teeth from the SSC group, 4 from the control group) In addition, 4 participants in each group were lost to follow‐up after 24 months. Only 68/80 from the SSC and 65/80 from the control group were analysed for clinical outcome Not all exclusions/losses were fully accounted for |
| Selective reporting (reporting bias) | High risk | No access to protocol Statistical analysis did not take clustering into account, and insufficient information was reported to allow for an analysis for the year 2 data. Data could not be analysed in a meta‐analysis |
| Other bias | Low risk | No other potential biases detected |
Hutcheson 2012.
| Methods | RCT, split‐mouth study, with 1‐year follow‐up Unit of randomisation: teeth |
|
| Participants |
Setting: Recruited from 2 dental clinics in Texas, 15 treated in clinic, 25 treated in operating theatre. Single site. Single operator Sample size Number screened: not reported Number eligible: not reported Number randomised: 40 participants (80 teeth) Number analysed: 37 participants (74 teeth) at 6 months, 31 participants (62 teeth) at follow‐up Sex: not reported Age: mean 5.1 years old (range 2.6 to 8) Teeth/lesions: "large carious lesions of similar size approaching the pulp" Inclusion criteria for participants:
Inclusion criteria for teeth:
|
|
| Interventions |
Intervention: stainless steel crown Control: resin composite multi‐surface, fitted using open sandwich technique. A layer of glass ionomer was used to cover the MTA before resin was applied All participants had MTA pulpotomy All teeth had pulptomies carried out before the crowns or restorations were placed |
|
| Outcomes | Outcomes assessed at 6 months and 12 months:
|
|
| Source of Funding | No information provided | |
| Declaration of interest | No information provided | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A tooth in each pair was randomly allocated by coin toss to either the experimental group (MTA/composite) or the control group (MTA/SSC), with the contralateral‐paired tooth assigned to the other treatment" |
| Allocation concealment (selection bias) | Low risk | Coin toss provided adequate concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: No blinding, participant and operator aware of different treatments. Blinding to type of treatment was not possible as the restorations look different. Unclear whether this affected level or quality of care |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "All pre‐ and postoperative radiographs were either digital or digitally scanned and evaluated by 2 blinded, standardized, and calibrated examiners. Coronal portions of the treated teeth were blackened‐out to ensure that the examiners were blinded." Comment: Blinding adequate for radiological findings, but most of the outcomes (clinical and patient‐reported) could not be blinded in the assessment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropouts were participants who failed to return, despite reminders 31/40 participants (77.5%) available at 12 months, 37/40 (92.5%) available at 6 months Percentage of losses quite large compared to the effect size of the trial |
| Selective reporting (reporting bias) | Unclear risk | All outcomes outlined in methods section were reported. Provided scale used for radiological ratings Definitions of 'radiologically successful' and 'clinically successful' were not provided |
| Other bias | Low risk | No other potential biases detected |
Innes 2011.
| Methods | Randomised controlled split‐mouth trial with 2‐year and 5‐year follow‐up 1 pair of teeth randomised for each patient. Teeth matched for lesion and across arch for tooth type |
|
| Participants |
Setting: Primary care (general dental practice) based in Tayside, Scotland (regional dmft 2.47, d3 1.71, mt 0.54, ft 0.22). 17 general dental practitioners from 10 NHS dental practices performed the procedures Sample size: Number screened: not known Number eligible: not known Number randomised: 132 participants (264 teeth) Number treated: 128 children (256 teeth) Number analysed: 124 participants (124/124 teeth) 6% drop‐outs at 1 year Age: 3‐10 years, mean 6.8 years; SD 1.58 Sex: 69 boys and 63 girls Teeth/lesions: Carious primary molars; 68% approximal lesions and 42% > half way into dentine radiographically (where radiographs were available). 73 study teeth pairs ( 55%) were first primary molars and 59 (45%) were second primary molars Inclusion criteria for participants:
Inclusion criteria for teeth:
Where more than 1 pair of matched carious lesions were present in a child's mouth, the dentist chose which pair should be part of the study. Any carious teeth outwith the study were managed as per the dentists' normal treatment regime |
|
| Interventions |
Intervention (132 teeth): PMC (SSC) placed by the Hall Technique with no caries removal. 4 teeth were not successfully fitted with crown but were managed under intention‐to‐treat protocol Control (132 teeth): restorations of the operator's choice: glass ionomer (69%), amalgam (8%), compomer (5%), composite (11%), SSC (1% ‐ with tooth preparation), fissure sealant (2%), and no restoration provided (3%) The majority of these teeth (n = 103), received complete caries removal, whilst some received partial caries removal (n = 29) |
|
| Outcomes |
|
|
| Source of Funding | Research Training Fellowship grant from the Chief Scientist Office of Scottish Executive and financial support from 3M/ESPE and EastRen. "The Sponsors of this trial had no role in its design; the collection, analysis or interpretation of data; or dissemination of results" | |
| Declaration of interest | None declared. Note: One of the author of the study (NI) is an author of this review | |
| Notes | Study showing 23‐month data, however 1 year and other relevant data obtained from author. Further publications give data up to 5 years | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Computer generated randomisation for sequence and side were held centrally" |
| Allocation concealment (selection bias) | Low risk | Quote: "...(randomisation) accessed by telephone to a distant coordinator prior to treatment" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The tooth on one side was restored using the Hall Technique and the contralateral tooth with the restorative technique the GDP would normally use". Comment: No blinding, patient and operator were aware of different treatments as restorations look different. Unclear whether this would affect level or quality of care. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Masking not possible ‐ different restorations for each group, therefore the outcome assessor could not be masked Comment: Patient and operator were aware of different treatments, which could affect judgement of subjective outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | CONSORT flow diagram provided information on drop‐outs and accounted for all participants. 4 teeth from each treatment arm (a total of 6 participants) were not successfully treated. Reasons were clearly reported. Data for outcomes available for 124 to 132 teeth (at least 94%) at up to 23 months. At 4 years, data were available for 91/132 teeth for both arms (70%). Numbers lost and reasons for loss were similar in both groups |
| Selective reporting (reporting bias) | Low risk | All expected outcomes were reported. Outcomes were reported as planned in the protocol |
| Other bias | Low risk | No other potential biases detected |
Ram 2003.
| Methods | Randomised controlled split‐mouth trial followed up at 6 months and 4 years 1 pair of teeth randomised for each patient. No detail on tooth matching for type |
|
| Participants |
Setting: Postgraduate clinic of the Department of Pediatric Dentistry at the Hadassah School of Dental Medicine, Israel Sample size: Number screened: not reported Number eligible: not reported Number randomised: 11 participants (22 teeth) Number analysed: 22 teeth Age: not reported Sex: not reported Teeth/lesions: not reported Inclusion criteria for patients:
Inclusion criteria for teeth:
|
|
| Interventions |
Intervention: SSC Control: aesthetic crown ‐ a composite veneer had been added to cover the facial, occlusal, mesial and distal aspects The conventional technique was used for both groups. Glass ionomer cement was used. However, the occlusal surface reduction was more extensive for the aesthetic crown (approximately 1.5 mm), as the crowns were thicker |
|
| Outcomes | Outcomes assessed at after 6 months and also at 4 years:
|
|
| Source of Funding | No information provided | |
| Declaration of interest | No information provided | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "selected by toss of coin" |
| Allocation concealment (selection bias) | Unclear risk | No description of allocation concealment method |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: No blinding, patient and operator were aware of different treatments as restorations look different. Unclear whether this would affect level or quality of care |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: No blinding mentioned; restorations look different |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: All participants/teeth were analysed at 6 months. 1/11 participants was not analysed at 4 years, and reason for exclusion was not stated |
| Selective reporting (reporting bias) | Unclear risk | No access to protocol, so insufficient information to judge |
| Other bias | Unclear risk | No information about the participants or baseline characteristics was provided |
Santamaria 2014.
| Methods | 3‐arm parallel group RCT followed up for 2 years (but data currently only available up to 1 year follow‐up). Unit of randomisation: patient | |
| Participants |
Setting: Germany (2 other countries, Lithuania and the UK, are involved in this study but no data were available for them yet). All children attended secondary care Sample size: 169 randomised from 181 eligible, all analysed Number screened: not stated in manuscript, researcher contacted and number unknown Number eligible: 181 Number randomised: 169 Number analysed: 148 Age: 3‐8 years old Sex: 96 boys and 73 girls Teeth/lesions: primary molars; maxillary first = 62; maxillary second = 29; mandibular first = 54; mandibular second = 24. ICDAS; code 3 = 6 teeth, 4 = 25 teeth, 5 = 138 teeth Inclusion criteria for participants:
Inclusion criteria for teeth:
Where more than 1 tooth per child was eligible for inclusion, the next tooth on the prescribed treatment plan, at the time of screening by one of the researchers (RS), was chosen for the study |
|
| Interventions |
Group 1 (n = 52): SSC, using the Hall Technique Group 2 (n = 65): fillings using resin composite Group 3 (n = 52): non‐restorative caries treatment |
|
| Outcomes |
|
|
| Source of Funding | The study was supported by the Paediatric Dentistry Department of Greifswald University, Germany | |
| Declaration of interest | No conflict of interest declared | |
| Notes |
NCT01797458 Study completion expected in December 2014. These are only the preliminary results for outcomes assessed immediately after treatment completion, and at up to 1 year of follow‐up in 1 of the 3 countries (Lithuania, Germany, Scotland (UK)) participating in the study |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Following consent, participants were sequentially randomised, using a computer‐generated random number list with allocation concealment, to one of three arms." Comment: The randomisations were done independently by each country participating in the study |
| Allocation concealment (selection bias) | Low risk | Comment: Randomisation only performed after participant consented to participation (based on preference paper and communication from authors.) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: No blinding, participant and operator aware of different treatments as restorations look different. Unclear whether this would affect level or quality of care |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: Unclear whether participants were blinded when questions related to intraoperative pain were asked immediately after procedure. Outcome assessors (dentists) could not be blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Data for the full trial are currently incomplete and were not available for 2 of the 3 countries involved in the study. Only the data from Germany are currently available. 148/169 (87.5%) participants randomised available for analysis at 1 year. Proportion of exclusions balanced across treatment arms (15.3% for Hall Technique, 15.3% for filling, 14.8% for non restorative caries). Study stated that "characteristics of participants who left during the study were comparable to those who remained in the study." Main reasons for dropout were in general: failure to return 67% (n = 14) or participants moved to another city/country 33% (n = 7) (information obtained from study authors) |
| Selective reporting (reporting bias) | Low risk | All outcomes regarding pain or discomfort were measured immediately after the procedure as stated in the protocol Only the 1‐year data were available for the 2014 review. The study is still ongoing; this paper reported only the German study population |
| Other bias | Low risk | No other potential biases detected |
Abbreviations
d3: decayed at the d3 level dmft: number of decayed, missing and filled primary teeth ft: number of filled primary teeth GDP: general dental practitioner ICDAS: International Caries Detection and Assessment System mt: number of missing primary teeth MTA: mineral trioxide aggregate MTA/SSC: mineral trioxide aggregate/ stainless steel crown NHS: National Heatlh Service PMC: preformed metal crown RCT: randomised controlled trial RMGIC/CRRs: resin modified glass ionomer cement/ composite resin restorations SD: standard deviation SSC: stainless steel crown USPHS: United States Public Health Service VASOF: visual analogue scale of faces
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Braff 1975 | Retrospective Not randomised Went on to limit within selected group of 131 PMCs (on basis of treating dentist and failure to fulfil follow‐up criteria) leaving only 76 PMCs with presented data |
| Einwag 1996 | Retrospective Not randomised Selected group of participants initially and only 66 out of 106 traced for follow‐up |
| Eriksson 1988 | Unclear whether retrospective or prospective Not randomised ‐ PMC placed on tooth in worst condition |
| Farooq 2000 | Retrospective Not randomised |
| Holan 2002 | Retrospective Not randomised Primary outcome related to success of pulpotomy treatment, so related to restoration rather than success of restoration itself |
| Leith 2011 | Compared 2 types of veneered preformed metal based crowns, not different methods of restoration |
| Roberts 2005 | Not randomised Although prospective, treatment was dictated by clinical status of tooth |
| Zagdwon 2003 | Crowns were placed on permanent teeth |
Abbreviation
PMC = preformed metal crown
Differences between protocol and review
Following a prioritisation project carried out by the Cochrane Oral Health Group, a decision was taken to expand the scope of the review. The earlier protocol only included studies with preformed metal crowns (PMCs). The current protocol includes studies using any type of crown material, compared to usual restoration methods or non‐restorative caries treatment.
We have broadened the objectives for this updated review compared to the 2008 version (Innes 2007). In the previous version, in the first objective we compared only PMCs with commonly used filling materials. This updated version has widened to include all preformed crowns (metal and aesthetic) compared to the same commonly used filling materials, and also non‐restorative caries treatment, as well as comparisons between different types of crowns and different methods for placing crowns. The second objective of the previous version of the review compared whether the extent of decay had an effect on outcome; this has not changed apart from now including all of the interventions in our first objective. The third objective in the original version of the review, dealt with adverse events and safety and this has now been incorporated into our first objective in this review.
We have also updated the outcomes. In the original review the primary outcomes were: freedom from clinical or radiographic signs or symptoms of pulp pathology including pain/pulp infection/discharging sinus/swelling; time until filling or crown needs to be replaced or requires further intervention; and proportion of filled or crowned teeth retained until appropriate age of shedding. We had included other measures of success: absence of clinical or radiographic evidence of secondary caries; other clinical signs of pathology (fracture of tooth or filling, wear of crown, inflammation of gingival (gum) tissue); patient satisfaction; costs to patient and provider; and adverse events. To reduce the number of outcomes but still maintain the applicability of the findings, we have used 'major failure', as a primary outcome. This is a composite outcome measure made up of different clinical and radiographic findings and comprises a number of outcomes from the previous review. Clinically, this is a reasonable outcome, as it requires the same treatment to manage. Our other two primary outcomes are pain and satisfaction with treatment (including satisfaction with aesthetics). The secondary outcomes were rationalised to: time to restoration failure/retreatment; peri/postoperative discomfort/pain; cost; and adverse events (e.g. bone loss, gingival inflammation or others).
In our protocol, we had planned to conducted adjustments for the study designs where within‐patient randomisation was conducted and investigate any impact of clustering. We conducted these analyses in our review using generic inverse variance as planned, but decided to present the results without adjustment. This decision is based on the fact that the adjustments did not make a real difference to the effect estimates obtained, and took into account the easier interpretability of unadjusted results in the usual dichotomous outcome format for clinicians. In future versions of this review we will revisit this decision on the basis of the data obtained.
We did not calculate the number needed to treat for an additional beneficial outcome (NNTB) as we had planned to.
Contributions of authors
The review was conceived and co‐ordinated by Nicola Innes (NI). All review authors (NI, David Ricketts (DR), Ruth Santamaria (RS), Alex Keightley (AK), Thomas Lamont (TL), Lee Yee Chong (LC)) participated in updating the review, developing the search strategy and the screening the search results and retrieved papers. All authors contributed to screening retrieved papers against inclusion criteria and assessing risk of bias. All review authors contributed to writing and revising the review.
Sources of support
Internal sources
School of Dentistry, The University of Manchester, UK.
External sources
-
Cochrane Oral Health Group Global Alliance, Other.
Through our Global Alliance (http://ohg.cochrane.org/partnerships‐alliances), the Cochrane Oral Health Group has received support from: British Association for the Study of Community Dentistry, UK; British Association of Oral Surgeons, UK; British Orthodontic Society, UK; British Society of Paediatric Dentistry, UK; British Society of Periodontology, UK; Canadian Dental Hygienists Association, Canada; Mayo Clinic, USA; National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; and Royal College of Surgeons of Edinburgh, UK.
-
National Institute for Health Research (NIHR), UK.
This project was supported by the NIHR, via Cochrane Infrastructure funding to the Cochrane Oral Health Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Declarations of interest
Original 2007 review
Whilst there is no conflict of interest with regard to one of the review authors (David Ricketts (DR)), two of the review authors (Nicola Innes (NI) and Dafydd Evans (DE)) received partial sponsorship in 2000, from 3M/ESPE, for a clinical trial investigating the use of preformed metal crowns to seal carious tissues into primary molar teeth using a different technique (the Hall Technique) to that investigated in this review. These authors have not taken part in the decision to include the study into the review or assessment of risk of bias of the study.
2015 update
Nicola PT Innes: received partial sponsorship in 2000 from 3M/ESPE for a clinical trial investigating the use of preformed metal crowns to seal carious tissues into primary molar teeth using the Hall Technique. She was an author on another included study. She did not take part in the decision to include these studies (Innes 2011; Santamaria 2014), nor did she conduct the risk of bias assessment or data extraction for them. David Ricketts: none known Lee Yee Chong: none known Alexander J Keightley: none known Thomas Lamont: none known Ruth Santamaria: was an author on one of the included studies (Santamaria 2014), but did not have any involvement in study selection, risk of bias assessment or data extraction for that study.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Atieh 2008 {published data only}
- Atieh M. Stainless steel crown versus modified open‐sandwich restorations for primary molars: a 2‐year randomized clinical trial. International Journal of Paediatric Dentistry 2008 Sep;18(5):325‐32. [PUBMED: 18328050] [DOI] [PubMed] [Google Scholar]
Hutcheson 2012 {published data only}
- Hutcheson C, Seale NS, McWhorter A, Kerins C, Wright J. Multi‐surface composite vs stainless steel crown restorations after mineral trioxide aggregate pulpotomy: a randomized controlled trial. Pediatric Dentistry 2012;34:460‐7. [PUBMED: 23265162] [PubMed] [Google Scholar]
Innes 2011 {published and unpublished data}
- Innes NP, Evans DJ, Stirrups DR. Sealing caries in primary molars: randomized control trial, 5‐year results. Journal of Dental Research 2011;90:1405‐10. [DOI: 10.1177/0022034511422064] [DOI] [PubMed] [Google Scholar]
- Innes NP, Evans DJP, Stirrups DR. The Hall Technique: a randomized controlled clinical trial of a novel method of managing carious primary molars in general dental practice; acceptability of the technique and outcomes at 23 months. BMC Oral Health 2007;7:18. [PUBMED: 18096042] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ram 2003 {published data only}
- Fuks AB, Ram D, Eidelman E. Clinical performance of esthetic posterior crowns in primary molars: a pilot study. Pediatric Dentistry 1999;21(7):445‐8. [PUBMED: 10633519] [PubMed] [Google Scholar]
- Ram D, Fuks AB, Eidelman E. Long‐term clinical performance of esthetic primary molar crowns. Pediatric Dentistry 2003;25(6):582‐4. [PUBMED: 14733474] [PubMed] [Google Scholar]
Santamaria 2014 {published and unpublished data}
- European Study on Three Different Approaches to Managing Class 2 Cavities in Primary Teeth [ongoing trial]. http://clinicaltrials.gov/show/NCT01797458 2013.
- Santamaria RM, Innes NP, Machiulskiene V, Evans DJ, Alkilzy M, Splieth CH. Acceptability of different caries management methods for primary molars in a RCT. International Journal of Paediatric Dentistry / the British Paedodontic Society [and] the International Association of Dentistry for Children 2015;25(1):9‐17. [PUBMED: 24602167] [DOI] [PubMed] [Google Scholar]
- Santamaria RM, Innes NP, Machiulskiene V, Evans DJ, Splieth CH. Caries management strategies for primary molars: 1‐yr randomized control trial results. Journal of Dental Research 2014;93(11):1062‐9. [DOI: 10.1177/0022034514550717] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Braff 1975 {published data only}
- Braff MH. A comparison between stainless steel crowns and multisurface amalgams in primary molars. ASDC Journal of Dentistry for Children 1975;42(6):474‐8. [PubMed] [Google Scholar]
Einwag 1996 {published data only}
- Einwag J, Dunninger P. Stainless steel crown versus multisurface amalgam restorations: an 8‐year longitudinal clinical study. Quintessence International 1996;27(5):321‐3. [PubMed] [Google Scholar]
Eriksson 1988 {published data only}
- Eriksson AL, Paunio P, Isotupa K. Restoration of deciduous molars with ion‐crowns: retention and subsequent treatment. Proceedings of the Finnish Dental Society 1988;84(2):95‐9. [PubMed] [Google Scholar]
Farooq 2000 {published data only}
- Farooq NS, Coll JA, Kuwabara A, Shelton P. Success rates of formocresol pulpotomy and indirect pulp therapy in the treatment of deep dentinal caries in primary teeth. Pediatric Dentistry 2000;22(4):278‐86. [PubMed] [Google Scholar]
Holan 2002 {published data only}
- Holan G, Fuks AB, Keltz N. Success rate of formocresol pulpotomy in primary molars restored with stainless steel crown vs amalgam. Pediatric Dentistry 2002;24(3):212‐6. [PubMed] [Google Scholar]
Leith 2011 {published data only}
- Leith R, O'Connell AC. A clinical study evaluating success of 2 commercially available preveneered primary molar stainless steel crowns. Pediatric Dentistry 2011;33:300‐6. [PubMed] [Google Scholar]
Roberts 2005 {published data only}
- Roberts JF, Attari N, Sherriff M. The survival of resin modified glass ionomer and stainless steel crown restorations in primary molars, placed in a specialist paediatric dental practice. British Dental Journal 2005;198(7):427‐31. [DOI] [PubMed] [Google Scholar]
Zagdwon 2003 {published data only}
- Zagdwon AM, Fayle SA, Pollard MA. A prospective clinical trial comparing preformed metal crowns and cast restorations for defective first permanent molars. European Journal of Paediatric Dentistry 2003;4:138‐42. [PubMed] [Google Scholar]
Additional references
AAPD 2014
- American Academy of Paediatric Dentistry. Guideline on Paediatric Restorative Dentistry. Reference Manual 2014;37(6):226‐34. [Google Scholar]
Alkarimi 2014
- Alkarimi H, Watt R, Pikhart H, Sheiham A, Tsakos G. Dental caries and growth in school‐age children. Pediatrics 2014;133:e616‐23. [DOI: ] [DOI] [PubMed] [Google Scholar]
Attari 2006
- Attari N, Roberts JF. Restoration of primary teeth with crowns: a systematic review of the literature. European Archives of Paediatric Dentistry 2006;7(2):58‐62. [DOI] [PubMed] [Google Scholar]
Beattie 2011
- Beattie S, Taskonak B, Jones J, Chin J, Sanders B, Tomlin A, et al. Fracture resistance of 3 types of primary esthetic stainless steel crowns. Journal of the Canadian Dental Association 2011;77:b90. [PubMed] [Google Scholar]
Blinkhorn 2003
- Blinkhorn A, Zadeh‐Kabir R. Dental care of a child in pain ‐ a comparison of treatment planning options offered by GDPs in California and the north‐west of England. International Journal of Paediatric Dentistry 2003;13(3):165‐71. [DOI] [PubMed] [Google Scholar]
Chadwick 2007
- Chadwick BL, Gash C, Stewart K. Preformed metal crowns: views of a group of dental practitioners in North Wales. Primary Dental Care 2007;14(4):140‐4. [DOI] [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta‐analyses involving cross‐over trials: methodological issues. International Journal of Epidemiology 2002;31(1):140‐9. [PUBMED: 11914310] [DOI] [PubMed] [Google Scholar]
Fejerskov 2015
- Fejerskov O, Nyvad B, Kidd EA. Pathology of dental caries. In: Fejerskov O, Nyvad B, Kidd EAM editor(s). Dental caries: The disease and its clinical management. 3. Vol. 3, Oxford: Wiley Blackwell, 2015:7‐9. [Google Scholar]
Foster Page 2014
- Foster‐Page LA, Boyd DH, Davidson SE, McKay SK, Thomson WM, Innes NPT. Acceptability of the Hall Technique in New Zealand. New Zealand Dental Journal March 2014:12‐7. [PubMed] [Google Scholar]
Frencken 2014
- Frencken JE. The state‐of‐the‐art of ART restorations. Dental Update 2014;41:218–24. [DOI] [PubMed] [Google Scholar]
Gift 1992
- Gift HC, Reisine ST, Larach DC. The social impact of dental problems and visits. American Journal of Public Health 1992;82(12):1663‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. Chichester, UK: John Wiley & Sons, Ltd.
Ismail 2002
- Ismail AI, Sohn W. Evidence suggests more favourable outcomes with preformed metal crowns than amalgam restorations in primary molars. Evidence‐Based Dentistry 2002;3(1):10. [Google Scholar]
Kindelan 2008
- Kindelan SA, Day P, Nichol R, Willmott N, Fayle SA. UK National Clinical Guidelines in Paediatric Dentistry: stainless steel preformed crowns for primary molars. International Journal of Paediatric Dentistry 2008;18(Suppl 1):20‐8. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Ludwig 2014
- Ludwig KH, Fontana M, Vinson LA, Platt JA, Dean JA. The success of stainless steel crowns placed with the Hall technique. Journal of the American Dental Association Dec 2014;145(12):1248‐53. [DOI] [PubMed] [Google Scholar]
Lygidakis 2010
- Lygidakis NA, Wong F, Jälevik B, Vierrou AM, Alaluusua S, Espelid I. Best Clinical Practice Guidance for clinicians dealing with children presenting with Molar‐Incisor‐Hypomineralisation (MIH): An EAPD Policy Document. European Archives of Paediatric Dentistry 2010;11(2):75‐81. [DOI] [PubMed] [Google Scholar]
Maggs‐Rapport 2000
- Maggs‐Rapport FL, Treasure ET, Chadwick BL. Community dental officers' use and knowledge of restorative techniques for primary molars: an audit of two Trusts in Wales. International Journal of Paediatric Dentistry 2000;10(2):133‐9. [DOI] [PubMed] [Google Scholar]
Monse 2012
- Monse B, Duijster D, Sheiham A, Carlos S Grijalva‐Eternod CS, Palenstein Helderman W, et al. The effects of extraction of pulpally involved primary teeth on weight, height and BMI in underweight Filipino children. A cluster randomized clinical trial. BMC Public Health 2012;12:725. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pair 2004
- Pair RL, Udin RD, Tanbonliong T. Materials used to restore class II lesions in primary molars: a survey of California pediatric dentists. Pediatric Dentistry 2004;26(6):501‐7. [PubMed] [Google Scholar]
Randall 2000
- Randall RC, Vrijhoef MMA, Wilson NHF. Efficacy of preformed metal crowns vs amalgam restorations in primary molars: a systematic review. Journal of the American Dental Association 2000;131:337‐43. [DOI] [PubMed] [Google Scholar]
Randall 2002
- Randall RC. Preformed metal crowns for primary and permanent teeth: review of the literature. Pediatric Dentistry 2002;24(5):489‐500. [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Ricketts 2013
- Ricketts D, Lamont T, Innes NPT, Kidd E, Clarkson JE. Operative caries management in adults and children. Cochrane Database of Systematic Reviews 2013, Issue 3. [DOI: 10.1002/14651858.CD003808.pub3] [DOI] [PubMed] [Google Scholar]
Roshan 2003
- Roshan D, Curzon ME, Fairpo CG. Changes in dentists' attitudes and practice in paediatric dentistry. European Journal of Paediatric Dentistry 2003;4(1):21‐7. [PubMed] [Google Scholar]
Seale 2002
- Seale S. The use of stainless steel crowns. Pediatric Dentistry 2002;24(5):501‐4. [PubMed] [Google Scholar]
Seale 2015
- Seale S, Randall R. The use of stainless steel crowns: a systematic literature review. Pediatric Dentistry 2015;37(2):147‐62. [PUBMED: 25905656] [PubMed] [Google Scholar]
Sheiham 2006
- Sheiham A. Dental caries affects body weight, growth and quality of life in pre‐school children. British Dental Journal Nov 2006;201(10):625‐6. [DOI] [PubMed] [Google Scholar]
Threlfall 2005
- Threlfall AG, Pilkington L, Milsom KN, Blinkhorn AS, Tickle M. General dental practitioners' views on the use of stainless steel crowns to restore primary molars. British Dental Journal 2005;199(7):453‐5. [DOI] [PubMed] [Google Scholar]
Tran 2003
- Tran LA, Messer LB. Clinicians' choices of restorative materials for children. Australian Dental Journal 2003;48(4):221‐32. [DOI] [PubMed] [Google Scholar]
Vermaire 2014
- Vermaire JH, Poorterman JH, Herwijnen L, Loveren C. A three‐year randomized controlled trial in 6‐year‐old children on caries‐preventive strategies in a general dental practice in the Netherlands. Caries Research 2014;48(6):524‐33. [DOI: ] [DOI] [PubMed] [Google Scholar]
WHO Report 2003
- World Health Organization. The World Oral Health Report 2003. http://www.who.int/oral_health/media/en/orh/_report03_en.pdf 2003:4.
Worthington 2015
- Worthington H, Clarkson J, Weldon J. Priority oral health research identification for clinical decision‐making. Evidence Based Dentistry 2015;16(3):69‐71. [DOI] [PubMed] [Google Scholar]
Yengopal 2009
- Yengopal V, Harneker SY, Patel N, Siegfried N. Dental fillings for the treatment of caries in the primary dentition. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD004483.pub2] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Innes 2007
- Innes NPT, Ricketts D, Evans DJP. Preformed metal crowns for decayed primary molar teeth. Cochrane Database of Systematic Reviews 2007, Issue 1. [DOI: 10.1002/14651858.CD005512.pub2] [DOI] [PubMed] [Google Scholar]


