Abstract
AIM
To compare the changes in excyclotorsion after inferior oblique (IO) recession in patients with primary and secondary inferior oblique overaction (IOOA).
METHODS
We retrospectively analyzed the data obtained from patients with IOOA who underwent graded IO recession. The patients were followed up for at least 3mo after surgery. Fundus photographs were taken pre- and postoperatively, and the sum of the angles of torsion in both eyes was used to analyze changes in excyclotorsion. Patients were divided into two groups: those diagnosed with primary IOOA were enrolled in the 1'IOOA group, and those diagnosed with secondary IOOA caused by superior oblique palsy (SOP) were enrolled in the 2'IOOA group. Excyclotorsion before and after surgery were compared between the two groups.
RESULTS
A total of 78 patients were enrolled in this study: 34 eyes in the 1'IOOA group and 44 eyes in the 2'IOOA group. In the 78 patients, torsional angle significantly decreased from 15.31°±7.40° to 12.11°±6.53° after IO recession (P<0.001). Mean preoperative torsional angle was larger in the 2'IOOA group than in the 1'IOOA group (P=0.03). In both groups, excyclotorsion significantly decreased after IO recession (P=0.001 and P<0.001, respectively); however, there was no significant difference in the amounts of changes in excyclotorsion between the two groups.
CONCLUSION
Excyclotorsion is significantly larger in secondary IOOA than in primary IOOA, and a significant decrease in the torsional angle occurs after IO recession in both types of IOOA.
Keywords: inferior oblique overaction, inferior oblique recession, ocular excyclotorsion, strabismus
INTRODUCTION
Inferior oblique overaction (IOOA) is characterized by an over-elevation in adduction on version testing, and is classified as primary and secondary depending on the presence of an identified causative factor[1]–[2]. The primary type, which can be symmetric or asymmetric, is attributed to unknown causes, and the secondary type is caused by paresis or paralysis of the superior oblique muscle or the yoke superior rectus muscle[3].
Because the primary action of the inferior oblique (IO) muscle during ocular movement is excyclotorsion, ocular torsion in IOOA may cause symptomatic excyclotropia[4]–[6]. Therefore, IO weakening surgeries have been used to treat excyclotropia[7]–[10]. Although most previous studies reported that IO weakening surgeries are efficient in reducing torsional deviation, the reported amounts of torsion correction after IO surgery varied from 1.3° to 11°[7]–[9],[11]–[13]. In addition, most previous studies primarily enrolled cases of secondary IOOA related to the superior oblique palsy (SOP)[8]–[9],[12],[14]–[16], and many of these studies focused on comparing the excyclotorsion correction effects among various IO-weakening surgeries[7]–[9],[17].
To the best of our knowledge, no studies have evaluated ocular excyclotorsion in primary and secondary IOOA. Further, no previous study has compared torsion correction effects according to the types of IOOA after IO weakening surgery. Therefore, in the present study, we aimed to compare ocular excyclotorsion in patients with primary and secondary IOOA and to investigate the changes in excyclotorsion after one specific surgical technique: graded IO recession.
SUBJECTS AND METHODS
Ethical Approval
This retrospective study was conducted with approval from the Institutional Review Board (IRB No. 2018-07-013-001), and all procedures adhered to the tenets of the Declaration of Helsinki. Because this is a retrospective study, the study was exempt from patient consent.
We retrospectively analyzed the medical records of patients older than 3y who were diagnosed as having unilateral IOOA at the ophthalmologic clinic from May 2011 to August 2017 and underwent graded IO recession. Fundus photographs were taken pre- and postoperatively, and patients were followed-up at least 3mo after surgery. Patients were excluded from the study if 1) they showed bilateral IOOA, 2) had a history of previous ocular surgery, including extraocular muscle surgery, 3) could not undergo fundus photography due to other concomitant ocular diseases such as corneal opacity, or 4) showed IOOA in the contralateral eye or recurrence of IOOA in the operated eye during the follow-up period. The occurrence and recurrence of IOOA were considered if more than grade +2 IOOA was observed.
Clinical Evaluation
Stereoacuity was measured using the Lang I stereotest (Lang-Stereotest AG, Küsnacht, Switzerland) and the Stereo Fly Stereotest (Stereo Optical Co., Chicago, IL, USA) in cooperative patients. Using the Kowa fundus camera (Kowa Optimed Inc, VK-2, Tokyo, Japan), non-mydriatic fundus photographs were taken. Before imaging, all patients were instructed to fixate on the camera's internal fixation marker with their head in the neutral position on the chin rest and head support by the expert technician. Torsional deviation, which is the angle between a horizontal line passing through the optic disc center and a line connecting the fovea and the optic disc center, was measured using Image J software (Version 1.47; National Institute of Health, Bethesda, MD, USA; Figure 1)[18]. In addition, since excyclotorsion may appear in the opposite eye, the sum of torsional angles in both eyes was evaluated to analyze changes in excyclotorsion in this study. Patients with IOOA accompanied by an under-depression of the affected eye in adducted downgaze and unilateral positive results on Bielschowsky's head tilt test with the hypertropia on the affected side were classified as secondary IOOA caused by SOP. Patients with elevation in adduction but negative Bieschowsky's head tilt test were included in primary IOOA group.
Figure 1. The torsional angle in the fundus photograph.
The angle of excyclotorsion was measured using Image J software.
Included eyes were divided into two groups: those diagnosed with primary IOOA were enrolled in the 1'IOOA group, and those diagnosed with secondary IOOA attributable to the SOP were enrolled in the 2'IOOA group. Excyclotorsion was compared before and after surgery between the two groups.
Surgical Technique
All patients underwent graded IO recession with or without horizontal rectus (HR) muscle surgery according to the severity of IOOA. The severity of IOOA was graded according to the degree of overelevation of the adducted eye using a scale ranging from +1 to +4, as described by Rosenbaum and Santiago[19]. Patients with IOOA severity of +2 or more were candidates for surgeries. Although primary IOOA is clinically characterized by the absence of problems such as positive head tilt, IO recession was performed when patients with primary IOOA showed over grade 2 severity at the primary position along with a significant V-pattern [>15 prism diopters (PD)].
Every surgery was performed by a single surgeon using the fornix approach. After the IO muscle was hooked with a single hook, careful explorations posteriorly along the globe were performed not to miss posterior fibers for complete isolation of the muscle. After the IO muscle was disinserted with the Stevens tenotomy scissors and secured with a double-arm suture, exaggerated traction tests were done for confirming that the entire IO muscle had been cut. The muscle was reattached to the globe at the desired point. The degree of graded IO recession was based on a modified version of the method described by Fink[20] and Parks[21]: 8-mm recession [IO muscle reattachment to the point of 3 mm posterior and 4 mm lateral to the lateral border of inferior rectus (IR) muscle insertion], 10-mm recession (IO muscle reattachment to the point of 3 mm posterior and 2 mm lateral to the lateral border of IR muscle insertion), or 14-mm recession (IO muscle reattachment to the point near the inferotemporal vortex vein) was subsequently performed.
Statistical Analysis
Statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). The paired t-test was used to analyze the changes in excyclotorsion after surgery in each group. The independent t-test, Chi-squared test, and linear by linear association were used to compare preoperative factors between the two groups. A P value of less than 0.05 was considered statistically significant.
RESULTS
One hundred and one eyes of 101 patients with unilateral IOOA who could undergo fundus photography were included in this study. However, 4 eyes showed recurrence of IOOA over grade +2 and 19 eyes showed IOOA over grade +2 in the contralateral eye during the follow-up period. None of the patients showed under-correction of elevation in adduction. Therefore, after excluding these 23 eyes, data for 78 eyes of 78 patients were analyzed retrospectively.
Baseline characteristics of the 78 patients are summarized in Table 1. Thirty-four patients who were diagnosed with primary IOOA were enrolled in the 1'IOOA group and 44 patients diagnosed with secondary IOOA were enrolled in the 2'IOOA group. In the 2'IOOA group, two patients had acquired SOP and the rest had congenital SOP. There were no significant intergroup differences in gender, age at surgery, mean interval between surgery and fundus photography, mean follow-up period, preoperative stereoacuity, and IOOA grade. Thirty-three patients in the 1'IOOA group and 42 in the 2'IOOA were able to cooperate and complete the Lang I test. And, 33 patients in 1'IOOA group and 37 in 2'IOOA were able to cooperate and complete the Stereo Fly stereotest. Comparing the number of cases involving combination of HR muscle surgery between the two groups, we found that the number of patients who underwent IO surgery only was significantly lower in the 1'IOOA group than in the 2'IOOA group (P<0.001, Chi-squared test). The mean preoperative torsional angle was significantly larger in the 2'IOOA group than that in the 1'IOOA group (P=0.03, independent t-test).
Table 1. Baseline characteristics of 78 patients.
| Clinical factors | 1'IOOA group | 2'IOOA group | P |
| Patients (n) | 34 | 44 | |
| Gender (male:female) | 12:22 | 22:22 | 0.194a |
| Age at surgery (y) | 8.09±3.14 | 9.48±8.62 | 0.374b |
| Mean follow up period (mo) | 58.03±24.14 | 46.39±27.37 | 0.054b |
| Preoperative stereoacuity | |||
| Lang I test, passed (n) | 30/33 | 34/42 | 0.226a |
| Stereo Fly Stereotest, ≤ 100 arcsec (n) | 26/33 | 26/37 | 0.416a |
| Mean preoperative torsional angle (°) | 13.25±6.74 | 16.91±7.57 | 0.030b |
| IOOA grade (n) 0.055c | |||
| +2 | 20 | 19 | |
| +3 | 14 | 20 | |
| +4 | 0 | 5 | |
| Surgical techniques (n) <0.001a | |||
| IO only | 4 | 22 | |
| With HR surgery | 30 | 22 | |
| Mean period of fundus photo taken after surgery (mo) | 3.79±2.74 | 3.86±2.06 | 0.899b |
| Mean postoperative torsional angle (°) | 10.84±6.36 | 13.10±6.56 | 0.121b |
IOOA: Inferior oblique overaction; 1'IOOA: Primary inferior oblique overaction; 2'IOOA: Secondary inferior oblique overaction; Arcsec: Seconds of arc; IO: Inferior oblique; HR: Horizontal retus muscle. aChi square test; bIndependent t-test; cLinear by linear association.
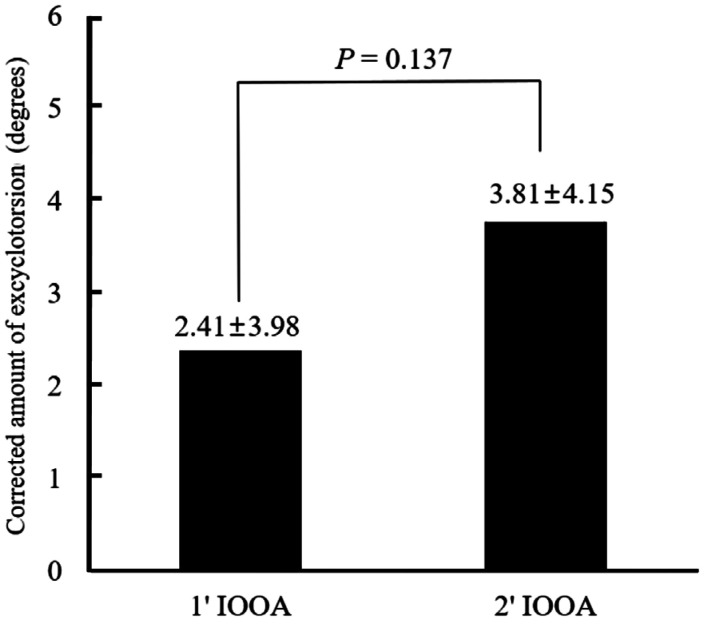
Figure 2 shows the decrease in torsional angle after IO recession. In all 78 patients, the mean preoperative torsional angle was 15.31°±7.40° (range, 0 to 37°), and it significantly decreased to 12.11°±6.53° (range, 0 to 30°; P<0.001, paired t-test). Mean amounts of torsion correction after IO surgery were 3.20°±4.11°. The changes in excyclotorsion in the 1'IOOA and 2'IOOA groups are illustrated in Figure 3. In the 1'IOOA group, the torsional angle significantly decreased from 13.25°±6.74° to 10.84°±6.36° (P=0.001, paired t-test), while in the 2'IOOA group, it decreased from 16.91°±7.57° to 13.10°±6.56° (P<0.001, paired t-test). Figure 4 presents the corrected amounts of excyclotorsion in the two groups. The decrease in excyclotorsion in the 2'IOOA group, 3.81°±4.15°, was numerically larger than that in the 1'IOOA group, 2.41°±3.98°; however, the intergroup difference was not statistically significant (P=0.137, independent t-test). The mean postoperative torsional angle was numerically larger in the 2'IOOA group, however there was no statistically significant difference (P=0.121, independent t-test).
Figure 2. Changes in excyclotorsion after IO recession.
The torsional angle significantly decreased after surgery. A: Preoperative fundus photograph; B: Postoperative fundus photograph.
Figure 3. Changes in excyclotorsion in the 1'IOOA and 2'IOOA groups.
In each group, mean torsional angle significantly decreased after surgery.
Figure 4. Comparison of the corrected amounts of excyclotorsion between the 1'IOOA and 2'IOOA groups.
The degree of angle correction was larger in the 2'IOOA group, but the intergroup difference was not statistically significant.
DISCUSSION
The presence of cyclotorsion is one of the clues for the diagnosis of inferior or superior oblique strabismus[22]–[23]. However, there are relatively fewer studies on ocular torsion, mainly because patients with anomalies of the cyclovertical muscle function rarely complain of image tilting due to compensatory mechanisms through sensory adaptations such as cyclofusion, suppression, and anomalous retinal correspondence[5],[24]. Nevertheless, measurement of the torsional angle in patients with SOP or IOOA may be an important factor in diagnosing and identifying patients' symptoms.
After Ruttum and von Noorden[24] first reported that the normal torsional angle was 7.25° by using fundus photography in 1983, the authors of several studies have evaluated the relationships between IOOA and excyclotorsion and the torsion correction after IO weakening surgery[7]–[9],[11]–[15]. Arici and Oguz[8] reported that ocular torsion decreases after superior oblique tuck and variable IO weakening in SOP. Additionally, excyclotorsional correction was observed in IOOA after IO anteriorization combined with recession[11]. However, that study had a limitation in that the number of enrolled cases was small.
To the best our knowledge, no studies have reported a comparison of the torsional angle between primary and secondary IOOA. Therefore, the most important aim of this study is to evaluate the differences in excyclotorsion between the two types of IOOA after a single IO weakening procedure: graded IO recession. In addition, we also enrolled more patients compared to the previous studies[8],[11]–[12], so that statistical significance in the correction effect of the IO recession procedure was confirmed through this study.
The mean preoperative torsional angle in 78 patients with IOOA was 15.31°±7.40°. Previous studies reported torsional angles from 7.2° to 17.5°[8],[11],[14],[18],[25]–[26]. However, a simple comparison of the preoperative torsional angle with the other existing results seems difficult, because the methods of torsion measurements and patients of inclusion criteria are different from those in other studies. The sum of torsional angles in both eyes was evaluated to analyze changes in excyclotorsion, and patients with both types of IOOA were all included in this study.
The rate of IO recession only without HR muscle surgery was significantly lower in the 1'IOOA group than that in the 2'IOOA group. Thus, there is a tendency not to perform IO recession only for the primary IOOA and the surgery for primary IOOA is performed more commonly when horizontal strabismus is also present. Conversely, even if there is no horizontal strabismus, the signs caused by SOP such as head tilt toward the non-paralyzed side and hypertropia of the paralytic eye in primary position seem to noticeable, the IO recession for treating the secondary IOOA is performed more often.
In addition, the preoperative ocular excyclotorsion was significantly larger in the 2'IOOA group. This is thought to be because in the 2'IOOA group, the effect of the decrease in ocular incyclotorsion caused additional SOP muscle, thus increasing the excyclotorsion to levels greater than those in the torsional angle in the 1'IOOA group, which showed excyclotorsion solely caused by overacting the IO muscle expression.
There was no significant difference in the amounts of changes in excyclotorsion between the two groups. This result shows that the effect on torsion correction in IO recession does not differ depending on the presence of SOP. Only graded IO recession was performed in both groups and as a result, the amounts of changes in excyclotorsion were not different between the two groups.
There were some limitations to this study. There was a report about the relationship between torsional angle and the grade of IOOA[13]. Because there is a report that the degree of IOOA affects the severity of excyclotorsion, subgroup analysis according to the grade of IOOA is required to improve the accuracy of our research. Unfortunately, we could not perform the subgroup analysis due to the small number of patients enrolled, which is the limitation of this study. However, there was no significant difference in the average grade of IOOA of enrolled patients between two groups (P=0.055 in Table 1), it does not seem that this confounding factor had influenced our results.
Moreover, depending on whether the SOP is congenital or acquired, the amounts of torsional angle and effects on the torsional correction of IO weakening surgery can be different. However, evaluation of the torsion correction effect of IO recession according to the type of SOP has not been conducted in this study. Further studies to analyze data by subdividing types of SOP with more cases would be meaningful.
Anatomically, actions of HR muscle from the primary position were only abduction and adduction[22],[27]. However, Khanna et al[27] reported that pathologic torsion decreased after HR muscle surgery in patients with infantile esotropias because their pathologic torsion could be the consequence of abnormal horizontal deviation and impairing binocular visual function[26]–[27]. Of course, Khanna's study was only based on patients with infantile esotropia who have poor binocularity which is different from the patients in this study, from this point of view, a significant difference between both groups regarding HR surgery could have biased our results and this point is a limitation of the study. Therefore, a further study that controlled the number of HR surgery between two groups are required for reasonable comparison.
In conclusion, the mean preoperative torsional angle was significantly larger in secondary IOOA than in primary IOOA, and a significant decrease in torsional angle occurred in both types of IOOA after IO recession. The degree of angle correction was numerically larger in secondary IOOA compared with primary IOOA, but the intergroup difference was not statistically significant.
Acknowledgments
Authors' contributions: Involved in design of study (Lee D, Kim WJ, Kim MM); Conduct of study (Lee D, Kim WJ, Kim MM); Collection and management of data (Lee D); Analysis and interpretation of data (Lee D, Kim WJ); Preparation of manuscript (Lee D, Kim WJ); Review or approval of manuscript (Kim MM).
Conflicts of Interest: Lee D, None; Kim WJ, None; Kim MM, None.
REFERENCES
- 1.Parks MM. The overacting inferior oblique muscle. Am J Ophthalmol. 1974;77(6):787–797. doi: 10.1016/s0002-9394(14)76320-2. [DOI] [PubMed] [Google Scholar]
- 2.Wilson ME, Parks MM. Primary inferior oblique overaction in congenital esotropia, accommodative esotropia, and intermittent exotropia. Ophthalmology. 1989;96(7):950–955. discussion 956–957. doi: 10.1016/s0161-6420(89)32774-6. [DOI] [PubMed] [Google Scholar]
- 3.Rajavi Z, Feizi M, Behradfar N, Yaseri M, Sayanjali S, Motevaseli T, Sabbaghi H, Faghihi M. Inferior oblique overaction: anterior transposition versus myectomy. J Pediatr Ophthalmol Strabismus. 2017;54(4):232–237. doi: 10.3928/01913913-20170309-01. [DOI] [PubMed] [Google Scholar]
- 4.Na KS, Lee SY, Lee YC. Ocular torsion in unilateral superior oblique palsy. J Korean Ophthalmol Soc. 2007;48(10):1388. [Google Scholar]
- 5.von Noorden GK. Clinical and theoretical aspects of cyclotropia. J Pediatr Ophthalmol Strabismus. 1984;21(4):126–132. doi: 10.3928/0191-3913-19840701-03. [DOI] [PubMed] [Google Scholar]
- 6.Pineles SL, Velez FG. Anterior superior oblique tuck: an alternate treatment for excyclotorsion. J AAPOS. 2018;22(5):393–393.e1. doi: 10.1016/j.jaapos.2018.05.019. [DOI] [PubMed] [Google Scholar]
- 7.Mataftsi A, Strickler J, Klainguti G. Vertical and torsional correction in congenital superior oblique palsy by inferior oblique recession. Eur J Ophthalmol. 2006;16(1):3–9. doi: 10.1177/112067210601600102. [DOI] [PubMed] [Google Scholar]
- 8.Arici C, Oguz V. The effect of surgical treatment of superior oblique muscle palsy on ocular torsion. J AAPOS. 2012;16(1):21–25. doi: 10.1016/j.jaapos.2011.09.015. [DOI] [PubMed] [Google Scholar]
- 9.Lee J, Suh SY, Choung HK, Kim SJ. Inferior oblique weakening surgery on ocular torsion in congenital superior oblique palsy. Int J Ophthalmol. 2015;8(3):569–573. doi: 10.3980/j.issn.2222-3959.2015.03.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Awadein A, El-Fayoumi D, Zedan RH. Changes in the axis of astigmatism and in fundus torsion following inferior oblique muscle weakening. J AAPOS. 2016;20(4):289–294. doi: 10.1016/j.jaapos.2016.03.008. [DOI] [PubMed] [Google Scholar]
- 11.Sim JH, Lee SY. The effect of inferior oblique weakening procedures on the correction of ocular torsion. J Korean Ophthalmol Soc. 2005;46(6):1020–1026. [Google Scholar]
- 12.Sharma P, Thanikachalam S, Kedar S, Bhola R. Evaluation of subjective and objective cyclodeviation following oblique muscle weakening procedures. Indian J Ophthalmol. 2008;56(1):39–43. doi: 10.4103/0301-4738.37594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee D, Kim WJ, Kim MM. Changes in ocular excyclotorsion according to graded inferior oblique recession. J Korean Ophthalmol Soc. 2016;57(8):1268. [Google Scholar]
- 14.Roh YR, Hwang JM. Comparison of subjective and objective torsion in patients with acquired unilateral superior oblique muscle palsy. Br J Ophthalmol. 2011;95(11):1583–1587. doi: 10.1136/bjo.2010.197046. [DOI] [PubMed] [Google Scholar]
- 15.Lee JJ, Chun KI, Baek SH, Kim US. Relationship of hypertropia and excyclotorsion in superior oblique palsy. Korean J Ophthalmol. 2013;27(1):39–43. doi: 10.3341/kjo.2013.27.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee JY, Kim HJ, Park KA, Oh SY, Oh SY. Clinical characteristics according to the laterality of ocular torsion in unilateral superior oblique palsy. BMC Ophthalmol. 2018;18(1):325. doi: 10.1186/s12886-018-0977-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stager D, Jr, Dao LM, Felius J. Uses of the inferior oblique muscle in strabismus surgery. Middle East Afr J Ophthalmol. 2015;22(3):292–297. doi: 10.4103/0974-9233.159723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bixenman WW, von Noorden GK. Apparent foveal displacement in normal subjects and in cyclotropia. Ophthalmology. 1982;89(1):58–62. doi: 10.1016/s0161-6420(82)34862-9. [DOI] [PubMed] [Google Scholar]
- 19.Rosenbaum AL, Santiago AP. Clinical strabismus management: principles and surgical techniques. Philadelphia: WB Saunders; 1999. [Google Scholar]
- 20.Fink WH. Surgery of the Oblique Muscles of the Eye. 1st edition. St. Louis: C.V. Mosby; 1951. [Google Scholar]
- 21.Parks MM. Atlas of strabismus surgery. 1st edition. Philadelphia: Harper and Row; 1983. [Google Scholar]
- 22.Von Noorden GK, Campos EC. Binocular vision and ocular motility. Theory and management of strabismus. 6th edition. St. Louis: MO; USA: Mosby; 2002. [Google Scholar]
- 23.Kim DH, Lim HT. Comparison of ocular torsion between congenital and acquired unilateral superior oblique palsy. Eye (Lond) 2019;33(10):1658–1663. doi: 10.1038/s41433-019-0476-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ruttum M, von Noorden GK. Adaptation to tilting of the visual environment in cyclotropia. Am J Ophthalmol. 1983;96(2):229–237. doi: 10.1016/s0002-9394(14)77791-8. [DOI] [PubMed] [Google Scholar]
- 25.Yim JH, Min BM, Xu YG. Surgical results of classic Harada-Ito procedure with intraoperative adjustment for excyclotorsion. J Korean Ophthalmol Soc. 2002;43(11):2227–2233. [Google Scholar]
- 26.Yu X, Mai G, Yu H, Deng D, Lin X, Chen J, Wu H. Study on ocular torsion of V patterns strabismus. Yanke Xuebao. 2003;19(3):160–164. [PubMed] [Google Scholar]
- 27.Khanna RK, Pasco J, Santallier M, Pisella PJ, Arsene S. Objective ocular torsion outcomes after unilateral horizontal rectus surgery in infantile esotropia. Graefes Arch Clin Exp Ophthalmol. 2018;256(9):1783–1788. doi: 10.1007/s00417-018-4027-4. [DOI] [PubMed] [Google Scholar]