Highlights
-
•
Human factors in public sectors for epidemic prevention need systematic analysis.
-
•
The Human Factors Analysis and Classification System is suitable for this purpose.
-
•
Bayesian Network theory enables probability prediction and key factors diagnosis.
-
•
Hybrid model’s feasibility is tested by analyzing the COVID-19 outbreak in China.
Keywords: Epidemic, COVID-19, Governance, Human factor, Risk analysis
Abstract
Pervasive human and organizational factors (HOFs) within the public sectors play a vital role in the prevention and control of epidemic (PCE). Insufficient analysis of HOFs has helped continue the use of flawed precautions. In this study, we attempted to establish a quantitative model to (a) clarify HOFs within the public sectors with regard to PCE, (b) predict the probability of relevant risk factors and an epidemic, and (c) diagnose the critical factors. First, we systematically identified 47 HOFs based on the Human Factors Analysis and Classification System (HFACS). We then converted the HFACS framework into a Bayesian Network (BN) after determining the causalities among these factors. Finally, we applied the hybrid HFACS-BN model to analyze the COVID-19 outbreak in China by virtue of its efficacy in probability prediction and diagnosis of key risk factors, and thus to test the feasibility of the model itself. This study contributes to a holistic analysis of HOFs within the public sectors with regard to PCE by providing a risk assessment model for epidemics or pandemics, and developing risk analysis methods for the public health field.
1. Introduction
The coronavirus disease 2019 (COVID-19) has engulfed the world. Statistics from the World Health Organization (WHO) show that as of July 9, 2020, 11,874,226 cases and 545,481 deaths are attributable to COVID-19, worldwide (WHO, 2020a). Epidemics like SARS and MERS, and pandemics like 2009 H1N1 and COVID-19 cause fear, threaten people’s lives and have a negative impact on economic development, social stability, and diplomatic relationships all over the world. Therefore, the prevention and control of epidemic (PCE) is of critical importance for all national governments and their implementation triggers increasing investment (Duan and Zhu, 2020, Nicola et al., 2020, Zhang, 2020).
The public sectors, including government departments (GD), medical institutions (MI), and centers for disease control and prevention (CDC), act as key leaders and enforcers in PCE (Dong et al., 2020, Jarquín et al., 2020, Nicola et al., 2020). The management of pervasive human and organizational factors (HOFs) within these sectors is a crucial task and determines the responsible sector’s success or failure. Accordingly, it is necessary to systematically and proactively analyze the pervasive HOFs for PCE (de Bruin et al., 2020, Gasmi et al., 2020, Peng et al., 2020).
Although there have been a number of studies on PCE, their focus has been on prior risk assessment, clinical and epidemiological investigation, viral genome analysis, vaccine development, establishment of evolution and transmission models, and epidemic management mechanisms (Ahn et al., 2020, Alhazzani et al., 2020, Chen et al., 2020, Phua et al., 2020, Shao et al., 2020, Wu et al., 2020, Zhang, 2020, Zhao et al., 2020a, Zhou et al., 2020). Conversely, regarding the pervasive and significant HOFs in the public sectors with regard to PCE, there have only been qualitative analyses of understaffing, lack of medical and emergency supplies, lack of emergency drills, improper safety protection operation, improper administration of epidemic areas, improper surveillance of imported cases of infection, concealed report on or release of epidemic information, poor technical ability of MI and CDC, insufficient public intervention, and imperfect management and response mechanisms for emergencies (de Bruin et al., 2020, Elavarasan and Pugazhendhi, 2020, Gasmi et al., 2020, Lancet, 2020, Lau et al., 2004, Law et al., 2020, Liu et al., 2020, Nicola et al., 2020, Peng et al., 2020, Rutayisire et al., 2020, Wang and Wang, 2020, WHO, 2020b, WHO, 2020c, Zhang et al., 2020). To the best of our knowledge, no studies have investigated these HOFs using quantitative analysis methods. As the saying goes, “If you cannot measure it, you cannot manage it.” Therefore, a quantitative model for analyzing these HOFs is a prerequisite for assessing their integrated impact on PCE and for diagnosing the critical risk factors, thereby effectively reducing the probability of a new epidemic.
The aim of this study is to construct a quantitative model to analyze HOFs in the public sectors with regard to PCE, and thus for predicting the probability of relevant risk factors and an epidemic, as well as diagnosing the key factors that can precipitate an epidemic. Specifically, we (a) identify and classify HOFs based on the Human Factors Analysis and Classification System (HFACS), (b) convert the HFACS framework into a Bayesian Network (BN) after determining the causalities among the HOFs, and (c) apply the constructed HFACS-BN model to quantitatively analyze the HOFs and to test the model’s feasibility, based on empirical data collected from Tianjin, China, in April 2020.
2. Methodology and research framework
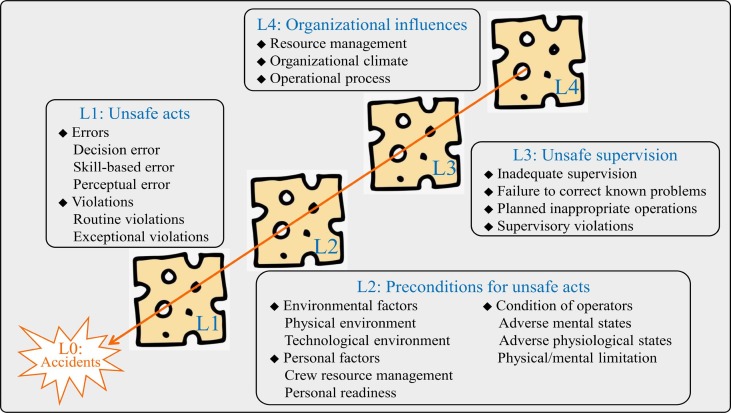
2.1. Human factors analysis and classification system
A variety of techniques have been developed for HOFs modeling, such as the Swiss cheese model (Reason, 1990), the cognitive reliability and error analysis method (Hollnagel, 1998), the HFACS (Shappell and Wiegmann, 2000), and the standardized plant analysis risk-human reliability analysis (Gertman et al., 2004). Of these methods, the one particularly suitable for our research purpose is the HFACS (see Fig. 1 ). With its systematic methodology and taxonomic nature, the HFACS helps to reduce the incompleteness caused by experts’ limited knowledge and missing information during the identification and classification of HOFs. The original HFACS framework describes the direct causes and latent causes of accidents. The former refers to individual unsafe acts (L1), while the latter includes preconditions for unsafe acts (L2), unsafe supervision (L3), and organizational influences (L4) (Shappell and Wiegmann, 2000). By virtue of its clear logical architecture, the HFACS enables us to systematically excavate the latent HOFs within the public sectors with regard to PCE, and thus to compensate for the insufficient focus on the potential impact of organizational and environmental factors on PCE by relevant public sectors.
Fig. 1.
The original HFACS framework.
2.2. Bayesian network
The HFACS can be only used as an auxiliary tool for identifying and classifying HOFs, i.e., constructing a conceptual framework of HOFs (Fu et al., 2020). Thus, in this study, the BN was employed to quantitatively investigate the interactions among the HOFs within the public sectors with regard to PCE. The BN is a powerful probabilistic network for reasoning and decision-making under uncertainty, and has been widely used for human reliability assessment and human error probability assessment (Abrishami et al., 2020, Fu et al., 2020). The integration of the HFACS and BN contributes to strengthening the risk analysis process. A simple instance of the BN is presented in Fig. 2 , which is composed of nodes representing variables (i.e., risk factors) and directed edges describing the causalities among variables. More details of the BN could be found in Pearl (1988).
Fig. 2.
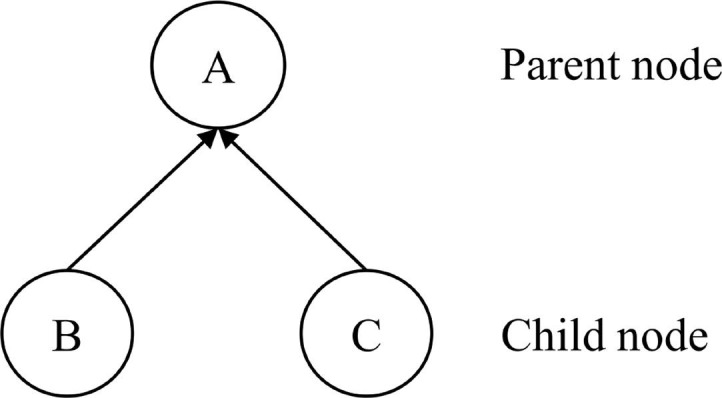
A simple instance of the BN.
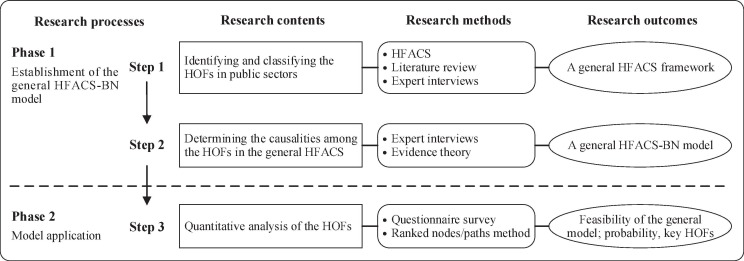
2.3. Research framework
Fig. 3 presents the research framework. Phase 1 involves the establishment of the general HFACS-BN model, including the identification and classification of the HOFs within the public sectors (Step 1), and the determination of the causalities among the HOFs (Step 2). In Phase 2, using the COVID-19 outbreak in Tianjin, China as an example, we quantitatively analyze the identified HOFs and then test the feasibility of the hybrid HFACS-BN model (Step 3). The two phases are detailed in subsequent sections.
Fig. 3.
Research framework.
3. Establishment of the HFACS-BN model
3.1. Systematic identification of HOFs
In most countries, the public sectors involved in PCE include government departments (GD), medical institutions (MI), and centers for disease control and prevention (CDC) (de Bruin et al., 2020, Nicola et al., 2020, Peng et al., 2020). These three public sectors are the research subjects in this study and their interrelationships are shown in Fig. 4 .
Fig. 4.
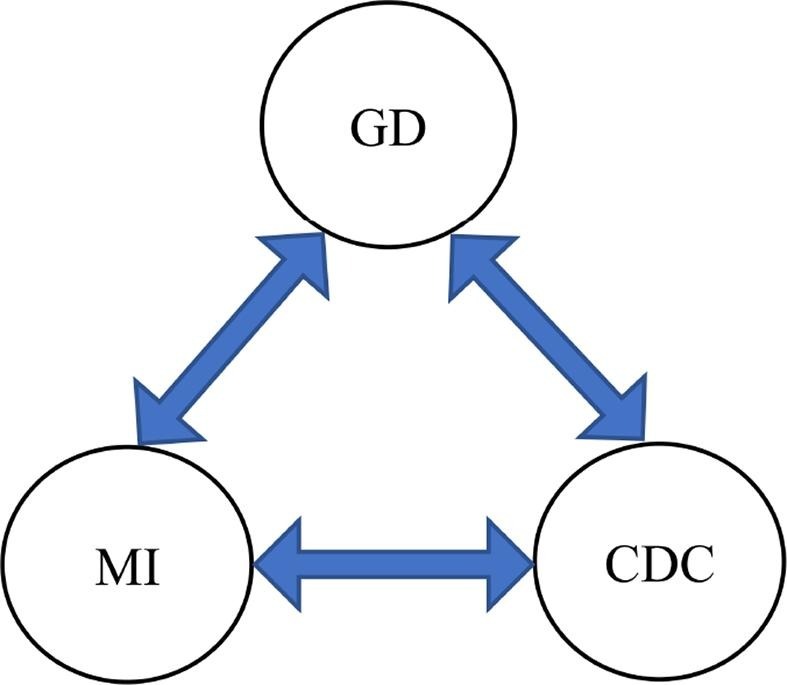
The interrelationships between the three sectors.
Based on the findings of previous research and on experts’ knowledge, the HOFs within the three central public sectors were extracted and classified based on the HFACS. The specific identification steps, based on the study by Fu et al. (2020), were as follows:
Step 1. The HOFs discussed in the literature were extracted and classified into corresponding locations in HFACS, according to their definitions.
Step 2. The child factors in original HFACS were extracted item by item and taken as references. Then, the literature was analyzed again to infer and identify new HOFs consistent with or similar to the references.
Step 3. To enrich the relevant HOFs and to consolidate the foundation of the constructed general HFACS framework, in April 2020, we consulted three experts working at the three public sectors for additional HOFs (e.g., improper sanitization of epidemic areas, imperfect legislation). They had experienced and fought against the COVID-19 epidemic in Wuhan, Hubei Province, China, including one professor (medical doctor) from Tianjin University of Traditional Chinese Medicine, one official from Chinese Center for Disease Control and Prevention, and one official from Wuhan Municipal Health Commission.
Step 4. To distill the list of HOFs elicited from the above different channels, the overlapping factors were further integrated into the HFACS framework.
We identified 92 child factors first and then consolidated them into 47. Table 1 presents the results and distribution. The new HFACS framework is comprised of six progressive levels, from external environmental influences (L5) to the outbreak of an epidemic (L0). They are described as follows:
Table 1.
Descriptions of HOFs in the general HFACS framework.
| Parent and intermediate factor | Child factor | Description |
|---|---|---|
| L0: Outbreak of an epidemic | ||
| L1: Unsafe acts | ||
| M1: Skill-based error of MI | R1 | Improper safety protection operation |
| R2 | Failure to detect the pathogenic factor | |
| M2: Decision error of MI | R3 | Not wearing appropriate medical protective equipment |
| M3: Routine violations of MI | R4 | Failure to receive and treat confirmed or suspected cases in a timely manner |
| R5 | Failure to isolate and monitor patient with unknown etiology | |
| R6 | Delayed report on special cases | |
| R7 | False, concealed, delayed, or omitted report on epidemic information | |
| R8 | Failure to reexamine cases | |
| M4: Skill-based error of CDC | R9 | Insufficient epidemiological investigation |
| R10 | Inappropriate dynamic surveillance for disease | |
| M5: Decision error of CDC | R11 | Delayed collection of epidemic information. Inaccurate information analysis or risk assessment |
| M6: Routine violations of CDC | R12 | False, concealed, delayed, or omitted report on epidemic information |
| R13 | Improper sanitization of epidemic areas | |
| R14 | Improper verification of close contacts' information | |
| M7: Skill-based error of GD | R15 | Delayed or incorrect division of epidemic areas. Improper administration of epidemic areas |
| M8: Decision error of GD | R16 | Improper prevention and surveillance of imported cases |
| R17 | Failure to organize experts to reexamine the patients | |
| R18 | Insufficient patient screening | |
| M9: Routine violations of GD | R19 | Improper administration of close contacts |
| R20 | False, concealed, or omitted report on, or delayed release of epidemic information | |
| L2: Preconditions for unsafe acts | ||
| M1: Condition of operators | R1 | Poor mental states |
| R2 | Poor physiological states | |
| M2: Personal readiness | R3 | A lack of knowledge of diseases |
| R4 | A lack of responsibility, consciousness, and enthusiasm | |
| R5 | A lack of crisis awareness | |
| R6 | A lack of experience. Poor emergency capacity | |
| R7 | Uncertainty over individual authority and responsibility. A lack of specific work instructions | |
| M3: Crew resource management | R8 | Understaffing or inappropriate deployments |
| R9 | Delayed arrangement of rescue personnel | |
| M4: Internal environment | R10 | A lack of medical and emergency supplies |
| R11 | Poor detective technology of MI | |
| R12 | Poor technical ability of CDC | |
| L3: Unsafe supervision | ||
| M1: Inadequate supervision | R1 | A lack of emergency drills |
| R2 | Inadequate personnel education or training | |
| R3 | Inadequate public mobilization, publicity, and education on epidemic prevention | |
| M2: Inappropriate plan | R4 | Insufficient coordination among sectors and unclear responsibilities |
| R5 | Delayed production, supply, and dispatch of goods and materials | |
| R6 | Imperfect infection monitoring system | |
| R7 | Unclear assignment of tasks | |
| M3: Supervisory violations | R8 | Non-standard implementation of the supervision system |
| L4: Organizational influences | ||
| M1: Resource management | R1 | Insufficient funds |
| R2 | Imperfect mechanisms for requisition and dispatch of emergency supplies | |
| M2: Operational process | R3 | Imperfect organizational system |
| R4 | Imperfect management and response mechanisms for emergencies | |
| L5: External environmental influences | ||
| R1 | Poor medical and technical level | |
| R2 | The need to maintain social stability at all costs | |
| R3 | Imperfect legislation | |
L1 (unsafe acts) is the direct cause of L0. The constructed HFACS framework includes the skill-based error, decision error, and routine violations by officials at the MI, CDC, and GD. Skill-based error refers to errors in skill-related behavior, such as memory error and operation error. Decision error is a behavior that serves a valuable purpose but does not meet the actual requirements. Habitual violations are violations that are recognized by most regulators due to their long-term status and high frequency (Shappell and Wiegmann, 2000).
L2 (preconditions for unsafe acts) is the direct cause of L1. The constructed HFACS framework includes the condition of operators, personal readiness, crew resource management, and the internal environment. Condition of operators refers to the mental and physical states and limitations of human beings. Personal readiness includes knowledge reserve and psychological preparation. Crew resource management means the management of resources and tasks within a team. Internal environment is a type of objective limitation, including physical and technological components (Shappell and Wiegmann, 2000).
L3 (unsafe supervision) is the direct cause of L2. The constructed HFACS framework contains the inadequate supervision, planned inappropriate operations, and supervisory violations. Inadequate supervision refers to a lack of guidance or emergency drills and failure to provide operating standards. Planned inappropriate operations include inappropriate deployments of human resources and unclear assignment of tasks. Supervisory violations refer to the intentional violation of regulations by regulators (Shappell and Wiegmann, 2000).
L4 (organizational influences) is the direct cause of L3. The constructed HFACS framework includes resource management and operational processes. Resource management means the management of funds and equipment. Operational processes refer to the organizational system and management mechanisms (Shappell and Wiegmann, 2000).
Compared with the traditional HFACS framework, L5 (environmental influences) is a new supplemental level, which is recognized to have a significant influence on L4 (Fu et al., 2020, Xia et al., 2018). L5 includes the poor medical and technical level, the need to maintain social stability at all costs, and imperfect legislation. Poor medical and technical level interferes with how quickly the virus can be detected and may even slow the development of a vaccine. For the sake of maintaining social stability, government departments may be conservative with regard to decision-making and releasing epidemic information, which may then lead to a lack of public understanding of the virus (Rundle et al., 2020, Zhao et al., 2020b). Imperfect legislation restricts the duties and powers of relevant public sectors, leading to an unclear understanding of responsibilities among the key actors.
3.2. Determination of causalities among HOFs
After constructing the general HFACS framework, we converted it into a BN by further determining causalities among the risk factors in this framework (i.e., network structure). Each risk factor was treated as a node, and each causality between two nodes was treated as a directed edge. Due to insufficient historical data, the BN structure was developed on the basis of expert knowledge. For a BN with n nodes, there are n(n-1)/2 sets of causalities. To reduce the workload of experts, we adopted four simplifying assumptions based on the taxonomic features of the HFACS as follows (Xia et al., 2018, Zhao et al., 2012):
Assumption 1. The outbreak of an epidemic (L0) is only and directly affected by unsafe acts (L1). Other HOFs at L2–L5 have an indirect effect on L0 through L1.
Assumption 2. The child factors only and directly affect the parent factor to which they belong.
Assumption 3. The child factors belonging to the same parent factor are independent of each other.
Assumption 4. There is no direct influence among the child factors belonging to different parent factors.
Based on the above four assumptions, the causalities among the nodes in the HFACS-BN model have been greatly reduced. However, the cross-level influence relationships among the parent nodes (e.g., the causality between L5 and L2) remain uncertain. To address this issue, we invited the three experts to determine whether a cross-level effect among the parent nodes exists. They were asked to assign a probability value (belief) to the two possible relationships between each pair of parent nodes, as follows: causality exists, and causality does not exist or is uncertain. The relationship with the maximum belief was adopted. In order to control for the inconsistencies in the opinions provided by the experts, Dempster’s rule of combination from evidence theory was employed (Dempster, 1967). The integration process is shown in Equations (1) and (2), as follows:
| (1) |
| (2) |
where , , and are the beliefs assigned by experts , , and for the two possible relationships between each pair of parent nodes. satisfies the conditions as follows: K means the degree of conflict among the three experts.
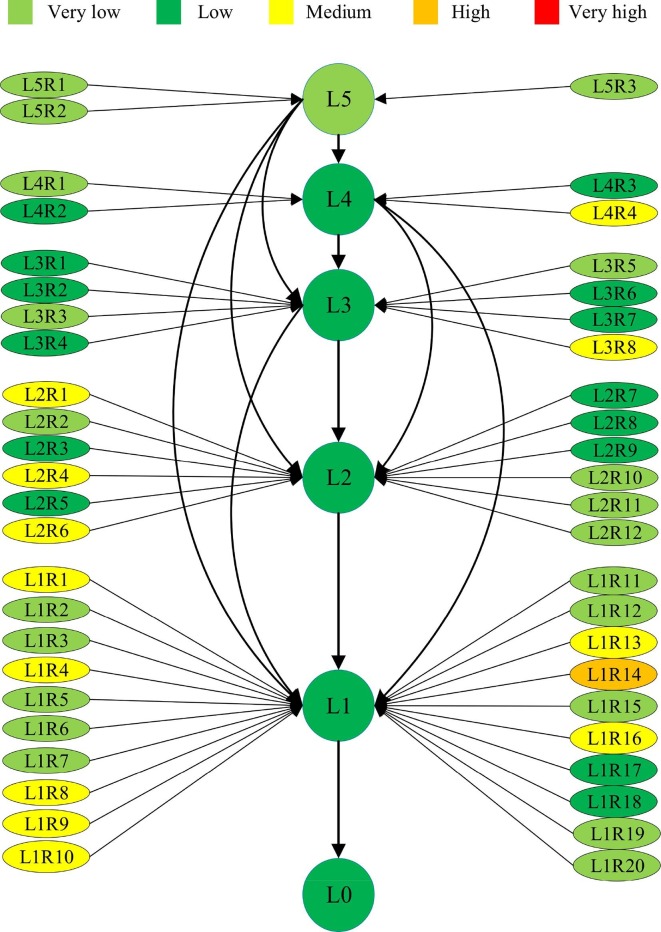
Table 2 shows the aggregating process. The final HFACS-BN model is shown in Fig. 5 comprising six levels, 53 nodes, and 58 directed edges.
Table 2.
The aggregating process of expert knowledge based on Dempster’s rule of combination.
| # | L5→L3 | L5↑L3 | L5→L2 | L5↑L2 | L5→L1 | L5↑1 | L4→L2 | L4↑L2 | L4→L1 | L4↑L1 | L3→L1 | L3↑L1 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Expert 1 | 1.00 | 0.00 | 0.90 | 0.10 | 0.90 | 0.10 | 0.90 | 0.10 | 0.80 | 0.20 | 0.90 | 0.10 |
| Expert 2 | 0.80 | 0.20 | 0.80 | 0.20 | 0.80 | 0.20 | 0.90 | 0.10 | 0.90 | 0.10 | 0.90 | 0.10 |
| Expert 3 | 0.80 | 0.20 | 0.80 | 0.20 | 0.70 | 0.30 | 0.80 | 0.20 | 0.70 | 0.30 | 0.70 | 0.30 |
| Belief () | 1.00 | 0.00 | 0.99 | 0.01 | 0.99 | 0.01 | 1.00 | 0.00 | 0.99 | 0.01 | 1.00 | 0.00 |
Note: Li → Lj means Li directly causes Lj; Li ↑ Lj means causality does not exist between Fi and Fj or is uncertain.
Fig. 5.
The general HFACS-BN model with the risk level of each node.
4. Model application
After the outbreak of COVID-19 in Wuhan in December 2019, a majority of the cities in China were affected to various degrees. Tianjin, a northern economic center of China, has confirmed a total of 199 people with COVID-19 (including 62 cases from abroad) as of July 9, 2020, of which 195 people have been cured (National Health Commission of the PRC, 2020). With the COVID-19 outbreak in Tianjin as an example, we will show how the constructed HFACS-BN model was applied to quantitatively analyze the HOFs within the three public sectors (GD, MI, and CDC) with regard to PCE. Probability prediction and diagnosis of key factors were also applied to test the feasibility of the model.
4.1. Elicitation of parameters
Traditionally, the clarification of prior probabilities of child nodes and conditional probability tables of parent nodes is the prerequisite for applying the reasoning function of a BN (Pearl, 1988). Due to the large number of nodes in the HFACS-BN model, and for the purpose of improving the practicability of the model, we employed the ranked nodes/paths method in this study instead of the traditional method. With this method, only two types of parameters are required—the criticality of each child node and the degree of each causality between two nodes (Fenton et al., 2007).
In April 2020, a total of 164 experts from the GD, MI, and CDC in Tianjin were invited to participate in this research. They were asked to complete a questionnaire in which the levels of the two types of parameters described above ranged from 1 (very low) to 5 (very high). Finally, 117 valid questionnaires were obtained (with a valid response rate = 71.3%). Table 3 shows participants’ demographics. The average scores of the experts’ ratings were treated as the final parameter values (see Table 4, Table 5 ).
Table 3.
Respondents’ demographic information.
| Item | Frequency | Percent (%) |
|---|---|---|
| Sector (position) | ||
| MI | 94 | 80.3 |
| Doctor | 52 | 44.4 |
| Nurse | 27 | 23.1 |
| Administrative personnel | 15 | 12.8 |
| CDC | 14 | 12.0 |
| GD | 9 | 7.70 |
| Work experience (years) | ||
| ≤5 | 42 | 35.9 |
| 6–10 | 39 | 33.3 |
| 11–15 | 27 | 23.1 |
| ≥16 | 9 | 7.70 |
Table 4.
Criticality of each child node.
| Child node | Mean | SD | Rank | Child node | Mean | SD | Rank |
|---|---|---|---|---|---|---|---|
| Level 1 | |||||||
| L1R1 | 3.08 | 0.51 | 4 | L1R11 | 1.47 | 0.03 | 38 |
| L1R2 | 1.46 | 0.34 | 39 | L1R12 | 1.76 | 0.27 | 28 |
| L1R3 | 1.00 | 0.00 | 47 | L1R13 | 2.77 | 0.47 | 10 |
| L1R4 | 2.71 | 0.62 | 11 | L1R14 | 3.42 | 0.72 | 1 |
| L1R5 | 1.32 | 0.21 | 42 | L1R15 | 1.72 | 0.35 | 30 |
| L1R6 | 1.13 | 0.09 | 45 | L1R16 | 2.61 | 0.67 | 13 |
| L1R7 | 1.04 | 0.02 | 46 | L1R17 | 1.87 | 0.41 | 26 |
| L1R8 | 3.11 | 0.93 | 3 | L1R18 | 2.18 | 0.53 | 19 |
| L1R9 | 3.02 | 0.51 | 5 | L1R19 | 1.44 | 0.18 | 40 |
| L1R10 | 3.28 | 0.32 | 2 | L1R20 | 1.28 | 0.07 | 43 |
| Level 2 | |||||||
| L2R1 | 2.62 | 0.84 | 12 | L2R7 | 2.13 | 0.74 | 21 |
| L2R2 | 1.58 | 0.09 | 34 | L2R8 | 1.83 | 0.06 | 27 |
| L2R3 | 2.14 | 0.78 | 20 | L2R9 | 1.94 | 0.05 | 25 |
| L2R4 | 2.81 | 0.49 | 9 | L2R10 | 1.61 | 0.07 | 33 |
| L2R5 | 2.11 | 0.73 | 22 | L2R11 | 1.22 | 0.03 | 44 |
| L2R6 | 2.94 | 0.91 | 6 | L2R12 | 1.69 | 0.27 | 32 |
| Level 3 | |||||||
| L3R1 | 2.56 | 0.71 | 14 | L3R5 | 1.51 | 0.11 | 35 |
| L3R2 | 2.28 | 0.83 | 18 | L3R6 | 2.49 | 0.59 | 16 |
| L3R3 | 1.41 | 0.16 | 41 | L3R7 | 2.10 | 0.73 | 23 |
| L3R4 | 2.51 | 0.85 | 15 | L3R8 | 2.91 | 0.77 | 7 |
| Level 4 | |||||||
| L4R1 | 1.50 | 0.48 | 36 | L4R3 | 2.38 | 0.96 | 17 |
| L4R2 | 1.97 | 0.43 | 24 | L4R4 | 2.87 | 0.79 | 8 |
| Level 5 | |||||||
| L5R1 | 1.70 | 0.30 | 31 | L5R3 | 1.49 | 0.12 | 37 |
| L5R2 | 1.75 | 0.35 | 29 | ||||
Table 5.
The degree of each causality.
| Causality | Mean | SD | Rank | Causality | Mean | SD | Rank |
|---|---|---|---|---|---|---|---|
| Causalities among levels | |||||||
| L5 → L4 | 3.24 | 0.91 | 44 | L4 → L1 | 2.89 | 1.32 | 57 |
| L5 → L3 | 3.08 | 1.13 | 51 | L3 → L2 | 3.95 | 1.03 | 18 |
| L5 → L2 | 3.18 | 0.89 | 46 | L3 → L1 | 3.71 | 1.01 | 33 |
| L5 → L1 | 2.87 | 0.93 | 58 | L2 → L1 | 3.97 | 1.01 | 16 |
| L4 → L3 | 3.52 | 0.86 | 37 | L1 → L0 | 4.51 | 1.07 | 1 |
| L4 → L2 | 3.29 | 1.22 | 40 | ||||
| Causalities at Level 1 | |||||||
| L1R1 → L1 | 3.85 | 1.25 | 27 | L1R11 → L1 | 4.09 | 1.09 | 10 |
| L1R2 → L1 | 3.41 | 1.18 | 38 | L1R12 → L1 | 4.29 | 1.14 | 5 |
| L1R3 → L1 | 4.33 | 1.04 | 3 | L1R13 → L1 | 3.11 | 1.12 | 49 |
| L1R4 → L1 | 3.94 | 1.05 | 19 | L1R14 → L1 | 3.55 | 1.21 | 35 |
| L1R5 → L1 | 3.17 | 1.12 | 47 | L1R15 → L1 | 3.26 | 1.05 | 42 |
| L1R6 → L1 | 3.88 | 1.02 | 24 | L1R16 → L1 | 3.12 | 1.04 | 48 |
| L1R7 → L1 | 4.08 | 1.25 | 11 | L1R17 → L1 | 3.06 | 0.79 | 53 |
| L1R8 → L1 | 3.36 | 1.22 | 39 | L1R18 → L1 | 4.30 | 1.09 | 4 |
| L1R9 → L1 | 3.99 | 1.04 | 14 | L1R19 → L1 | 4.06 | 1.04 | 12 |
| L1R10 → L1 | 3.01 | 1.08 | 56 | L1R20 → L1 | 4.12 | 1.13 | 8 |
| Causalities at Level 2 | |||||||
| L2R1 → L2 | 3.54 | 1.05 | 36 | L2R7 → L2 | 3.81 | 1.03 | 28 |
| L2R2 → L2 | 3.03 | 1.12 | 55 | L2R8 → L2 | 3.67 | 1.07 | 34 |
| L2R3 → L2 | 3.92 | 1.02 | 20 | L2R9 → L2 | 3.04 | 1.06 | 54 |
| L2R4 → L2 | 3.91 | 1.02 | 21 | L2R10 → L2 | 4.12 | 1.25 | 9 |
| L2R5 → L2 | 3.76 | 1.32 | 30 | L2R11 → L2 | 4.03 | 1.04 | 13 |
| L2R6 → L2 | 3.74 | 1.06 | 31 | L2R12 → L2 | 4.37 | 1.05 | 2 |
| Causalities at Level 3 | |||||||
| L3R1 → L3 | 3.90 | 1.10 | 22 | L3R5 → L3 | 3.96 | 1.04 | 17 |
| L3R2 → L3 | 3.79 | 1.31 | 29 | L3R6 → L3 | 3.98 | 1.03 | 15 |
| L3R3 → L3 | 3.73 | 1.21 | 32 | L3R7 → L3 | 3.87 | 1.13 | 25 |
| L3R4 → L3 | 3.27 | 1.12 | 41 | L3R8 → L3 | 3.25 | 1.05 | 43 |
| Causalities at Level 4 | |||||||
| L4R1 → L4 | 4.22 | 1.09 | 6 | L4R3 → L4 | 4.13 | 1.13 | 7 |
| L4R2 → L4 | 3.89 | 1.24 | 23 | L4R4 → L4 | 3.86 | 1.12 | 26 |
| Causalities at Level 5 | |||||||
| L5R1 → L5 | 3.20 | 1.03 | 45 | L5R3 → L5 | 3.07 | 1.24 | 52 |
| L5R2 → L5 | 3.09 | 1.07 | 50 | ||||
4.2. Reasoning and sensitivity analysis
The probabilistic reasoning and sensitivity analysis functions of the HFACS-BN model can help management personnel in the public sectors to intuitively realize the risk level of each factor and the outbreak of an epidemic, and to diagnose the critical risk factors, which currently relies heavily on the limited experience of experts (Nicola et al., 2020). To test the feasibility of the HFACS-BN model, we input the HFACS-BN structure, the criticalities of child nodes, and the degree of each causality into the AgenaRisk software (2019) and ran a quantitative analysis of the data, including the reasoning and sensitivity analysis.
Fig. 5 shows the results of probability prediction where different colors represent different risk levels. The risk of the outbreak of an epidemic (L0) is at a low level. In May and June 2020, Tianjin confirmed only seven people with COVID-19 from abroad, and one local case infected by his colleague who had traveled to Beijing several times (National Health Commission of the PRC, 2020). It means that in the two months after the questionnaire, the PCE by relevant public sectors in Tianjin was productive, and the COVID-19 outbreak did not turn into an epidemic. Thus, the predicted results of the constructed HFACS-BN model are consistent with the actual situation in Tianjin, which verifies the feasibility of the hybrid HFACS-BN model.
Moreover, it can be seen that the risk levels of factors that are closer to L0 are higher. At L1 (unsafe acts), there are eight child factors at the medium or high level, while this number at L2 (preconditions for unsafe acts), L3 (unsafe supervision), L4 (organizational influences) and L5 (external environmental influences) is 3, 1, 1, and 0 respectively. This indicates that individual unsafe acts are the main risk factors with a relatively high probability of occurrence in PCE in Tianjin. Such unsafe acts cover improper safety protection operation (L1R1), failure to receive and treat confirmed or suspected cases in a timely manner (L1R4), failure to reexamine cases (L1R8), insufficient epidemiological investigation (L1R9), inappropriate dynamic surveillance for disease (L1R10), improper sanitization of epidemic areas (L1R13), improper verification of close contacts' information (L1R14), and improper prevention and surveillance of imported cases (L1R16).
The most likely risk factors for COVID-19 at L2 include poor personal mental states (L2R1), a lack of responsibility, consciousness, and enthusiasm (L2R4), and a lack of experience and emergency capacity (L2R6). These three factors are the main causes of individual unsafe acts at L1. Non-standard implementation of the supervision system (L3R8) and imperfect management and response mechanisms for emergencies (L4R4) are also risk factors with a relatively high probability of occurrence with regard to COVID-19 epidemic in Tianjin, and thus can undermine PCE efforts.
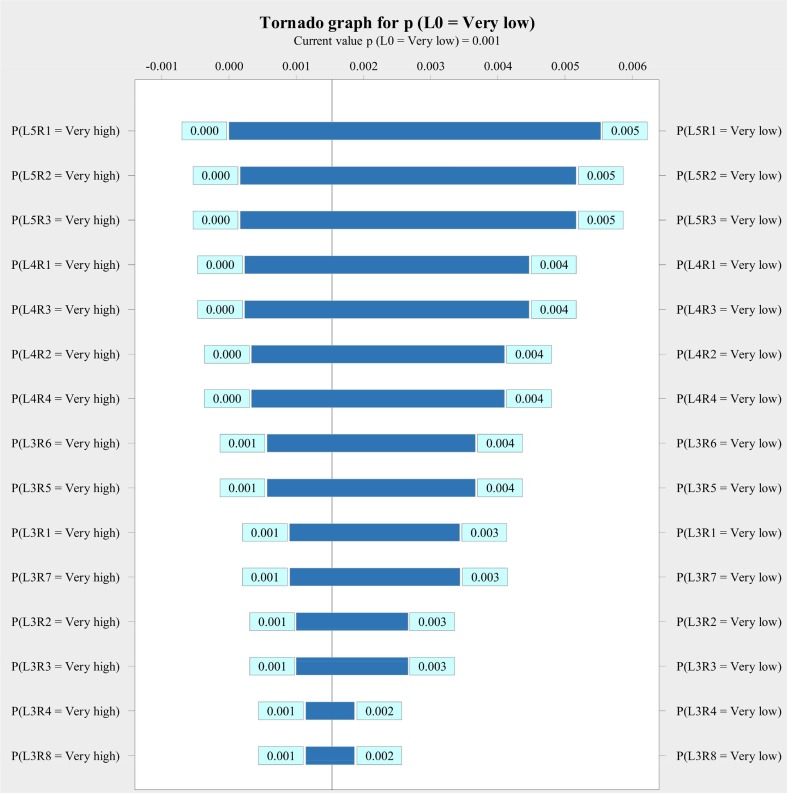
Fig. 6 shows the sensitivity analysis results. It can be seen that L0 (outbreak of an epidemic) is most sensitive to L5. This indicates that external environmental factors like the medical and technical level (L5R1), the need to maintain social stability (L5R2), and legislation (L5R3) contribute greatly to the spread of COVID-19 virus. The poor medical and technical level limits the technical abilities of the MI and CDC, while the imperfect legislation may lead to uncertainty over the responsibilities of relevant public sectors and imperfect coordination mechanisms. Although improvements of these two aspects cannot be achieved overnight and require the long-term efforts of health workers and legal personnel, management personnel at the public sectors should continue to focus on the changes of these two factors for adopting more effective measures. The need to maintain social stability at all costs has proved to be a contributing factor to COVID-19 outbreaks (Zhao et al., 2020b). In fact, during the outbreak of COVID-19 in Wuhan, several doctors had become aware of a new infectious virus and reported it to the authorities. Unfortunately, as the Chinese New Year was approaching at the time, some officials chose to conceal relevant information about the epidemic in order to maintain social stability and normal production of enterprises (Zhang, 2020). As a result, tens of millions of citizens did not take timely protective measures and were exposed to a dangerous situation. It was not until the COVID-19 outbreak became an epidemic in Wuhan that the authorities in China began to restrict public transportation and mass gatherings and, on January 23, 2020, to lock down the entire city of Wuhan (Zhang et al., 2020). This suggests that the public sectors should strengthen the assessment of epidemic-related information to avoid adopting the wrong or delayed response strategies.
Fig. 6.
Results of sensitivity analysis (only the sensitive factors at high levels are shown).
L0 is also sensitive to L4, including insufficient funds (L4R1), imperfect organizational system (L4R3), and imperfect management and response mechanisms for emergencies (L4R2, L4R4). It indicates that sufficient funds are crucial for PCE, which reinforces the argument that resources play a vital role in disaster management (Chen et al., 2008). It is also clear that the PCE cannot be undertaken effectively without a strong organizational system and rapid response mechanisms (Peng et al., 2020). Particularly, as Zhang (2020) stressed, a strong leadership and perfect logistics distribution system play critical roles in the requisition and dispatch of emergency supplies.
The more sensitive factors at L3 include unclear assignment of tasks (L3R7), inadequate personnel education and mobilization (L3R2, L3R3), a lack of emergency drills (L3R1), imperfect infection monitoring systems (L3R6), delayed production, supply, and dispatch of goods (L3R5), insufficient coordination among sectors (L3R4), and non-standard implementation of the supervision system (L3R8). Since the first four factors have a great impact on personnel readiness at L2, managers at the relevant public sectors should proactively clarify the responsibilities of each employee and organize regular training and emergency drills. This is so employees will not have to “cram” in information and improve their skills at the last minute. Because the COVID-19 virus spreads rapidly, a well-developed infection monitoring system is an essential tool for management personnel so they can accurately come to grips with the situation (Lau et al., 2004, Peng et al., 2020). Sufficient reserves of goods and equipment are of critical importance for health workers in hospitals. It's worth noting that as the protective equipment is firstly supplied to infectious diseases departments and intensive care units, health workers in other departments are likely to be affected the worst because of the lack of adequate protective equipment. In addition, the PCE requires a multi-agency engagement, which means that a sound command and coordination mechanism and the strict implementation of the supervision system are the prerequisite for effectively integrating all forces to fight the virus (Lancet, 2020, WHO, 2020b).
At L1 and L2, the more sensitive factors include the following:
-
•
Not or incorrectly wearing medical protective equipment (L1R1, L1R3).
-
•
Poor personal readiness (L2R3-L2R7).
-
•
Insufficient patient screening (L1R18).
-
•
Failure to receive and treat confirmed or suspected cases in a timely manner (L1R4).
-
•
Improper verification and administration of close contacts (L1R14, L1R19).
-
•
Inaccurate information analysis or risk assessment (L1R11).
-
•
Concealed report on or delayed release of epidemic information (L1R6, L1R7, L1R12,
-
•
L1R20).
-
•
Poor technical ability of MI and CDC (L2R11, L2R12).
-
•
Insufficient epidemiological investigation (L1R9).
-
•
Insufficient medical and emergency supplies (L2R10).
Although these manifest factors are caused by latent risk factors at L3, L4, and L5, management personnel at the public sectors should be cautious about these factors in their daily work. Despite the low frequency of an epidemic, health workers should insist on wearing appropriate protective equipment at work and try to maintain a healthy physical and mental state so as to avoid internal cross-infection when the virus hit (Chan et al., 2020, Law et al., 2020). In fact, in the early days of the COVID-19 epidemic in Wuhan, a large number of health workers became infected with the virus since many patients had atypical clinical manifestations and visited different medical departments (Wang et al., 2020, Zhang, 2020).
Comprehensive screening of patients, reception and treatment of confirmed and suspected cases, and verification and administration of close contacts are at the core of the PCE (Nicola et al., 2020, WHO, 2020b). Only by carrying out these measures can the spread of the virus be controlled effectively. However, close contacts of infected patients are difficult to verify because the virus has an incubation period of 14 days and the whereabouts of potentially infected close contacts are not monitored until they show COVID-19 symptoms. Therefore, most countries and regions have had to suspend public transportation, close public places, restrict human movements, conduct grid-based management of populated communities, and improve big data-based infection monitoring systems (Anderson et al., 2020, Jarquín et al., 2020, Liu et al., 2020).
Accurate risk assessment is a prerequisite for the public sectors to launch emergency response plans in a timely manner. Therefore, the collection and analysis of information on the scale and spread of the epidemic should be strengthened, personnel training should be made more rigorous, and the consulting experts should be highly competence (WHO, 2020c). The timely and transparent release of epidemic information by the authorities will serve to inform the public of the situation and enable it to take the appropriate countermeasures. Such proactive and transparent actions require greater institutional flexibility and a show of courage by officials (Zhao et al., 2020b). Finally, the MI and the CDC should continuously improve their technical capabilities, and the GD should coordinate the work of the relevant sectors and ensure adequate supply of goods and materials to support the PCE.
5. Discussion
In this study, we constructed a hybrid HFACS-BN model for assessing the probability of an epidemic and quantitatively investigated the role of HOFs within the public sectors with regard to PCE. The feasibility of the model was successfully tested by its application to the COVID-19 outbreak in Tianjin. We found that individual unsafe acts are the main internal risk factors with a relatively high probability of occurrence, and that adverse external environmental factors contribute greatly to the COVID-19 epidemic.
5.1. Theoretical implications
This study enhances the understanding of the role of HOFs within the public sectors with regard to PCE. We extracted 47 human, organizational, and environmental factors, and built a general HFACS-BN model for epidemic assessment. The model covers six interactional levels as follows: External environmental influences (L5); organizational influences (L4); unsafe supervision (L3); preconditions for unsafe acts (L2); unsafe acts (L1); and outbreak of an epidemic (L0). Although previous studies have discussed most of these risk factors, they have neglected to assess the integrated impact of these human, organizational, and environmental factors on the outbreak of an epidemic. Compared with previous studies by de Bruin et al., 2020, Gasmi et al., 2020, Law et al., 2020, Peng et al., 2020, Zhang, 2020, our study used empirical data and quantitative methods to show the influences of these internal and external factors on PCE. Specifically, with the COVID-19 outbreak in Tianjin as a case-study, the constructed HFACS-BN model predicted the risk level of each factor in the model and identified the crucial roles played by individual unsafe acts and external environmental factors. In this respect, our study provides new insights into the vulnerability assessment of the prevention and control system of epidemics or pandemics.
Notably, the HFACS and BN methods have rarely been used together to analyze the HOFs within the public sectors with regard to PCE. In this study, we integrated these two methods to investigate the role of relevant HOFs and demonstrate their application for developing risk analysis methods in the public health field.
5.2. Practical implications
In their interviews, the experts said that management personnel at public health sectors in China lacked a quantitative tool with which to assess the actual risk level of an infection and diagnose the critical risk factors. The constructed HFACS-BN model with its functions of probabilistic reasoning and sensitivity analysis relieves this predicament. The application of the HFACS-BN model to the COVID-19 outbreak in Tianjin, China has validated its effectiveness and operability. Specifically, the model identified the most critical risk factors as poor medical and technical level, the need to maintain social stability at all costs, imperfect legislation, organizational systems, and management mechanisms for emergencies, and insufficient funds. Other risk factors were unsafe supervision, poor personal readiness, and individual unsafe acts. In view of these findings, this study contributes to a scientific and quantitative assessment of epidemic risk and to an accurate formulation of precautions.
5.3. Limitations and future research
Despite the above findings, this study has some limitations. First, the constructed HFACS-BN model can only be used as an auxiliary tool for macro management because the identified HOFs are not specific enough. Therefore, we suggest future research refine these factors based on exhaustive incident records, so as to extend the application of the model. Second, we did not consider the interaction among the child factors at different levels, which may affect the objectivity and accuracy of the results calculated by the model. Therefore, we recommended a further exploration of the interrelationships among the child factors.
6. Conclusion
The pervasive HOFs within the public sectors play a crucial role in PCE. Insufficient investigation of HOFs is likely to result in imperfect management, and the possibility of a nationwide epidemic or global pandemic. In this study, we constructed a general HFACS-BN model to systematically and quantitatively analyze the risk factors. The hybrid model was used to analyze the COVID-19 outbreak in Tianjin, China, including probability predictions and sensitivity analysis. The feasibility of the model was also tested in this process. This study contributes to the development of assessment tools for epidemics or pandemics, which can facilitate a more holistic analysis of HOFs and the development of risk assessment methods in the public health field.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Grant No. 71772136). Many thanks to the participants who contributed to this study.
References
- Abrishami S., Khakzad N., Hosseini S.M., Van Gelder P. BN-SLIM: A Bayesian Network methodology for human reliability assessment based on Success Likelihood Index Method (SLIM) Reliab. Eng. Syst. Saf. 2020;193 [Google Scholar]
- Agenarisk, 2019. Accessed at http://www.agenarisk.com on April 29, 2020.
- Ahn D.G., Shin H.J., Kim M.H., Lee S., Kim H.S., Myoung J. Current status of epidemiology, diagnosis, therapeutics, and vaccines for novel coronavirus disease 2019 (COVID-19) J. Microbiol. Biotechn. 2020;30(3):313–324. doi: 10.4014/jmb.2003.03011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alhazzani W., Møller M.H., Arabi Y.M., Loeb M., Gong M.N., Fan E. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19) Intens. Care. Med. 2020;46:854–887. doi: 10.1007/s00134-020-06022-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J.F.W., Yuan S., Kok K.H., To K.K.W., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R., Liang W., Jiang M., Guan W., Zhan C., Wang T. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest. 2020;185:97–105. doi: 10.1016/j.chest.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R., Sharman R., Rao H.R., Upadhyaya S.J. Coordination in emergency response management. Commun. ACM. 2008;51(5):66–73. [Google Scholar]
- de Bruin Y.B., Lequarre A.S., McCourt J., Clevestig P., Pigazzani F., Jeddi M.Z. Initial impacts of global risk mitigation measures taken during the combatting of the COVID-19 pandemic. Saf. Sci. 2020;128 doi: 10.1016/j.ssci.2020.104773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempster A.P. Upper and lower probabilities induced by a multivalued mapping. Ann. Math. Stat. 1967;38:325–339. [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychiat. 2020;7(4):300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elavarasan R.M., Pugazhendhi R. Restructured society and environment: A review on potential technological strategies to control the COVID-19 pandemic. Sci. Total Environ. 2020;725 doi: 10.1016/j.scitotenv.2020.138858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenton N.E., Neil M., Caballero J.G. Using ranked nodes to model qualitative judgments in Bayesian networks. IEEE Trans. Knowl. Data Eng. 2007;19(10):1420–1432. [Google Scholar]
- Fu L., Wang X., Liu B., Li L. Investigation into the role of human and organizational factors in security work against terrorism at large-scale events. Saf. Sci. 2020;128 [Google Scholar]
- Gasmi A., Noor S., Tippairote T., Dadar M., Menzel A., Bjørklund G. Individual risk management strategy and potential therapeutic options for the COVID-19 pandemic. Clin. Immunol. 2020;215 doi: 10.1016/j.clim.2020.108409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gertman, D.I., Blackman, H.S., Marble, J.L., Smith, C., Boring, R.L., 2004. The SPAR-H human reliability analysis method. Fourth American Nuclear Society International Topical Meeting on Nuclear Plant Instrumentation, Controls and Human-Machine Interface Technologies (NPIC&HMIT 2004), Columbus, Ohio.
- Hollnagel E. Elsevier; Amsterdam: 1998. Cognitive Reliability and Error Analysis Method (CREAM) [Google Scholar]
- Jarquín M.C., Prado A.M., Marin B.G. Nicaragua's response to COVID-19–Authors' reply. Lancet Glob. Health. 2020;8(7) doi: 10.1016/S2214-109X(20)30220-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancet T. COVID-19: too little, too late? Lancet. 2020;395(10226):755. doi: 10.1016/S0140-6736(20)30522-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau J.T., Fung K.S., Wong T.W., Kim J.H., Wong E., Chung S. SARS transmission among hospital workers in Hong Kong. Emerg. Infect. Dis. 2004;10(2):280. doi: 10.3201/eid1002.030534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law S., Leung A.W., Xu C. Severe acute respiratory syndrome (SARS) and coronavirus disease-2019 (COVID-19): From causes to preventions in Hong Kong. Int. J. Infect. Dis. 2020;94:156–163. doi: 10.1016/j.ijid.2020.03.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W., Yue X.G., Tchounwou P.B. Response to the COVID-19 epidemic: The Chinese experience and implications for other countries. Int. J. Env. Res. Pub. He. 2020;17:2304. doi: 10.3390/ijerph17072304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Commission of the PRC, 2020. Accessed at http://www.nhc.gov.cn/ on July 10, 2020.
- Nicola M., O’Neill N., Sohrabi C., Khan M., Agha M., Agha R. Evidence based management guideline for the COVID-19 pandemic-review article. Int. J. Surg. 2020;77:206–216. doi: 10.1016/j.ijsu.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl J. Morgan Kaufman; San Mateo, CA: 1988. Probabilistic Reasoning in Intelligent Systems: Networks of Plausible Inference. [Google Scholar]
- Peng F., Tu L., Yang Y., Hu P., Wang R., Hu Q. Management and treatment of COVID-19: The Chinese experience. Can. J. Cardiol. 2020;36(6):915–930. doi: 10.1016/j.cjca.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phua J., Weng L., Ling L., Egi M., Lim C.M., Divatia J.V. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Resp. Med. 2020;8:506–517. doi: 10.1016/S2213-2600(20)30161-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reason J. Cambridge University Press; New York: 1990. Human Error. [Google Scholar]
- Rundle A.G., Park Y., Herbstman J.B., Kinsey E.W., Wang Y.C. COVID-19 related school closings and risk of weight gain among children. Obesity. 2020;28(6):1008–1009. doi: 10.1002/oby.22813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutayisire E., Nkundimana G., Mitonga H.K., Boye A., Nikwigize S. What works and what does not work in response to COVID-19 prevention and control in Africa. Int. J. Infect. Dis. 2020;97:267–269. doi: 10.1016/j.ijid.2020.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao N., Zhong M., Yan Y., Pan H., Cheng J., Chen W. Dynamic models for Coronavirus Disease 2019 and data analysis. Math. Method. Appl. Sci. 2020;43(7):4943–4949. doi: 10.1002/mma.6345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shappell, S.A., Wiegmann, D.A., 2000. The human factors analysis and classification system–HFACS [microform]: final report/Scott A. Shappell, Douglas A. Wiegmann.Washington, DC: Office of Aviation Medicine, U.S. Dept. of Transportation, Federal Aviation Administration; Springfield, Va.: This document is available to the public through the National Technical Information Service.
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Env. Res. Pub. He. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Wang Z. Strengths, weaknesses, opportunities and threats (swot) analysis of China’s prevention and control strategy for the COVID-19 epidemic. Int. J. Env. Res. Pub. He. 2020;17(7):2235. doi: 10.3390/ijerph17072235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, 2020a. Coronavirus disease (COVID-19) situation report-171. Accessed at https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200709-covid-19-sitrep-171.pdf?sfvrsn=9aba7ec7_2 on July 10, 2020.
- WHO, 2020b. Country & Technical Guidance - Coronavirus disease (COVID-19). Accessed at https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance on April 14, 2020.
- WHO, 2020c. Strategies and plans. Accessed at https://www.who.int/emergencies/diseases/novel-coronavirus-2019/strategies-and-plans on April 14, 2020.
- Wu J., Leung K., Leung G. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCov outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395(10225):689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xia N., Zou P.X., Liu X., Wang X., Zhu R. A hybrid BN-HFACS model for predicting safety performance in construction projects. Saf. Sci. 2018;101:332–343. [Google Scholar]
- Zhang H. Early lessons from the frontline of the 2019-nCoV outbreak. Lancet. 2020;395:687. doi: 10.1016/S0140-6736(20)30356-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S., Wang Z., Chang R., Wang H., Xu C., Yu X. COVID-19 containment: China provides important lessons for global response. Front. Med-Prc. 2020;14(2):215–219. doi: 10.1007/s11684-020-0766-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Yuan Q., Wang H., Liu W., Liao X., Su Y. Antibody responses to SARS-CoV-2 in patients of novel coronavirus disease 2019. Infect. Dis. Clin. 2020 doi: 10.1093/cid/ciaa344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao L., Wang X., Qian Y. Analysis of factors that influence hazardous material transportation accidents based on Bayesian networks: A case study in China. Saf. Sci. 2012;50:1049–1055. [Google Scholar]
- Zhao W., Zhang J., Meadows M.E., Liu Y., Hua T., Fu B. A systematic approach is needed to contain COVID-19 globally. Sci. Bull. 2020;65(11):876–878. doi: 10.1016/j.scib.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]