We report an example of longitudinally extensive transverse myelitis (LETM) in a previously healthy three-year-old Navajo girl with novel coronavirus (severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2]) infection who was asymptomatic before the onset of weakness.
Before hospitalization, our patient was living in a large multigenerational household, all of whom eventually tested positive for SARS-CoV-2. Three weeks after the onset of respiratory symptoms among the family members, the girl presented to an outside hospital with progressive extremity weakness and decreased sensation. Head and neck computed tomographic scans were unremarkable, and she was transferred to our emergency department. While there, her weakness progressed to flaccid quadriparesis and neurogenic respiratory failure requiring intubation. She was never encephalopathic. Symptoms evolved from onset to complete quadriplegia over 12 hours.
On neurologic examination, she was aroused easily and was able to close eyes to command. Cough and gag reflexes were absent, but all other cranial nerves were intact. There was flaccid quadriparesis, areflexia, and no response to pain below the neck. She required full ventilatory support.
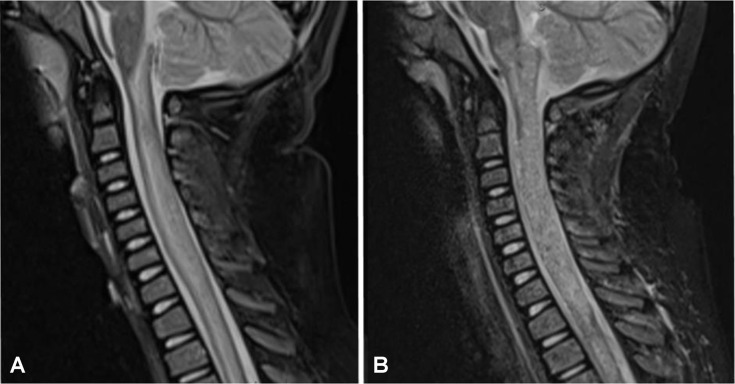
Initial magnetic resonance imaging (MRI) demonstrated swelling of the cervical spinal cord with T2-hyperintense edema involving most of the transverse aspect of the spinal cord, extending from the lower medulla to the midthoracic level (Fig A ); there was no abnormal enhancement. MRI of the brain and orbits showed no additional lesions. Cerebrospinal fluid (CSF) had elevations in red blood cells (282/mm3), total nucleated cells (42/mm3) with neutrophilic predominance (96%), and total protein (58 mg/dL, reference range 15 to 45 mg/dL). Extensive evaluation for causative entities was negative. This evaluation included investigation for rheumatologic disease, aquaporin-4 and myelin oligodendrocyte glycoprotein autoantibodies, and infectious etiologies including varicella zoster virus, herpes simplex virus, enterovirus, human immunodeficiency virus, Epstein-Barr virus, cytomegalovirus, Treponema pallidum, Mycobacterium tuberculosis, and common viral respiratory pathogens including influenza A and B and Mycoplasma pneumonia e. Nasopharyngeal polymerase chain reaction (PCR) was positive for SARS-CoV-2 (Roche COBAS 6800 platform); CSF was negative for SARS-CoV-2 by PCR. Initial chest radiograph was unremarkable.
FIGURE.
Representative sections from sagittal T2 short tau inversion recovery magnetic resonance imaging of the cervical spine on day 1 (A) and day 5 (B) of admission. There is a longitudinally extensive T2-hyperintense lesion extending throughout the entire cervical spine and into the medulla.
A diagnosis of LETM was made based on clinical presentation, lesion characteristics on MRI, and mild CSF pleocytosis; she had a negative evaluation for rheumatologic and infectious causes excepting SARS-CoV-2. Treatment was initially begun with five days of intravenous methylprednisone (30 mg/kg/day) and immunoglobulin (2 g/kg total dose); however, treatment was escalated in the face of unchanged flaccid quadriparesis and imaging on the fifth day of admission, which showed more prominent edema, now extending to the midmedulla (Fig B), with some restricted diffusion and interval appearance of small foci of hemorrhage and patchy contrast enhancement in the cervical spinal cord. Our patient then received seven sessions of therapeutic plasma exchange (1.0 to 1.5 plasma volumes exchanged per session) and is now undergoing an induction course of rituximab (four infusions of 375 mg/m2). She did not receive SARS-CoV-2-directed therapy. Follow-up imaging after plasmapheresis revealed evolution of the injury with interval reduction in lesion length and decreased edema in the medulla and upper cervical cord. The lower cervical cord shows early myelomalacia. Her examination continues to show flaccid quadriparesis. Repeat testing for SARS-CoV-2 by nasopharyngeal PCR was negative by day eight of admission. Serum SARS-CoV-2 IgG was not obtained.
Neurologic complications of coronavirus disease 2019 (COVID-19) include a wide spectrum of disorders with varying pathophysiology in both children and adults.1 , 2 To this evolving literature, we add this child with LETM and a positive SARS-CoV-2 nasopharyngeal PCR without other symptoms of the disease. Acute transverse myelitis was documented in a 66-year-old Chinese man who developed lower extremity weakness less than a week after the onset of symptoms while hospitalized for fever and respiratory insufficiency.3 In contrast, our patient, a young child, was asymptomatic before the onset of weakness. Her symptoms developed three weeks after her family members first developed respiratory symptoms, which fits in the typical time frame of postinfectious demyelinating syndromes.4 With such a rapid and devastating disease course as experienced by our patient, practitioners are encouraged to consider aggressive first-line therapies if further cases of post-COVID-19 transverse myelitis are identified.
Footnotes
Disclosure statement: All authors have nothing to disclose.
Funding sources: All authors have no funding related to this research.
References
- 1.Asadi-Pooya A.A., Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci. 2020;413:116832. doi: 10.1016/j.jns.2020.116832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Helms J., Kremer S., Merdji H. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382:2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhao K., Huang J., Dai D., Feng Y., Liu L., Nie S. Acute myelitis after SARS-CoV-2 infection: a case report. medRxiv. 2020 [Google Scholar]
- 4.Absoud M., Greenberg B., Lim M., Lotze T., Thomas T., Deiva K. Pediatric transverse myelitis. Neurology. 2016;87:S46–S52. doi: 10.1212/WNL.0000000000002820. [DOI] [PubMed] [Google Scholar]