Abstract
Background
Surrogates frequently are unable to predict which treatment their charges would want and also can experience significant distress as a result of making treatment decisions. A new method, the patient preference predictor (PPP), has been proposed as a possible way to supplement the process of shared decision-making to address these two concerns. The PPP predicts which treatment the patient would want based on which treatment similar patients want in similar circumstances. The present article describes the results of the first evaluation to assess whether patients support the use of a PPP.
Methods
Self-administered survey of patients at a tertiary care centre.
Results
Overall, 1169 respondents completed the survey (response rate=59.8%). In the event that the respondent became unable to make decisions due to a car accident, 78.9% would want the PPP to be incorporated into the process of making treatment decisions for them. In contrast, 15.2% of respondents would not want the PPP to be used for them. Respondents who endorsed the PPP cited the possibility that its use could increase the chances that they receive the treatments they prefer and/or reduce the burdens on their surrogate decision-maker.
Conclusions
The majority of respondents endorsed the possibility of incorporating a PPP into the process of shared decision-making based on its potential to increase surrogates’ predictive accuracy and/or reduce surrogate distress. These data provide strong patient support for further research to assess whether, in practice, the use of a PPP can increase the chances that incapacitated patients receive the treatments they prefer and reduce the burden of making decisions on their surrogates.
INTRODUCTION
Clinical practice attempts to respect individual autonomy by allowing patients to determine the course of their medical treatment. Yet, many patients, such as those with severe dementia and traumatic brain injury, are not able to make decisions at the time treatment is needed.1–4 In these cases, patient-designated or next-of-kin surrogates are asked to make treatment decisions for the patient.5
Many commentators argue that surrogates should not be asked to make treatment decisions on their own. Instead, the patient’s clinicians should share the responsibility and burden of making decisions with the patient’s surrogate.6,7 This process of ‘shared decision-making’ involves the surrogate and clinicians working together to try, to the extent possible, to make treatment decisions based on the patient’s own expressed directives. In the absence of a written or verbal advance directive (AD) that identifies a preferred course of treatment in the circumstances, the surrogate and clinicians appeal to the ‘substituted judgement’ standard, attempting to make the treatment decision they think the patient would have made in the circumstances.8 When this is not possible, the process of shared decision-making attempts to promote the patient’s clinical interests. Finally, in cases where a patient-designated or next-of-kin surrogate cannot be identified, clinicians attempt to implement the ‘substituted judgement’ standard, or else promote the patient’s clinical interests as best they can.9,10
This approach to making treatment decisions is intended to continue to respect patients’ autonomy, even after they lose the ability to make their own decisions.8 Specifically, many patients, including those who never explicitly indicated how they want to be treated in the event of decisional incapacity, endorsed specific values regarding the type of life they wanted to lead and developed preferences regarding how they wanted and did not want to be treated. For example, an individual may have consistently valued the quality of their lives over its quantity, or they may have valued fighting on even when the chances of success were low. Making treatment decisions based on these values and preferences respects the patient’s autonomy by allowing what they endorsed and adopted—their values, goals and aspirations—to determine the course of their treatment.
Shared decision-making, together with the substituted judgement and best interests standards, thus offers a theoretically appealing way to maintain respect for patient autonomy even after patients lose the ability to make their own decisions. Unfortunately, data suggest that patient-designated and next-of-kin surrogates,11 as well as clinicians,12,13 frequently are unable to predict which treatment option the patient would have chosen. In addition, surrogates can experience significant distress as a result of making treatment decisions.14 These data suggest that the combination of shared decision-making, substituted judgement and best interests may not be sufficient to maintain respect for patients’ autonomy during periods of decisional incapacity.
One possible approach that has been described to address these concerns is to incorporate a patient preference predictor (PPP) into the process of shared decision-making.15–17 A PPP predicts which treatment a given patient would want based on the patient’s characteristics and data on which treatment patients who share these characteristics want in similar circumstances. Previous research based on a very preliminary PPP suggested that providing surrogates and clinicians with the PPP prediction might increase the chances that incapacitated patients are treated consistent with their preferences and values.15 In addition, one of the strongest predictors of surrogate distress is not knowing which treatment the patient would want.14 It follows that, if a PPP can accurately predict patients’ treatment preferences, it also may reduce surrogate distress. Finally, the PPP could help clinicians to predict the treatment preferences of decisionally incapacitated patients for whom a patient-designated or next-of-kin surrogate cannot be identified.18
Given the PPP’s potential to address important shortcomings with current approaches, we conducted a survey to assess patients’ views regarding the possibility of incorporating a PPP into the shared decision-making process between surrogates and clinicians. Respondents were asked whether they would endorse the use of a PPP in the event that they lost the ability to make their own decisions and how they would want a PPP to be used in their own case. Respondents were also asked why they would or would not want a PPP to be used in the event that they lost the ability to make treatment decisions for themselves.
METHODS
Study population
The survey was conducted at The George Washington University Hospital and Clinics, a large tertiary care centre in Washington DC, USA. To capture the views of a broad range of patients, eligibility criteria were minimal: (1) inpatient or out-patient; (2) ≥18 years of age; and (3) able to complete a 30 min written survey in English. In addition, eligible respondents were recruited from seven different units and clinics: general medicine, emergency department (ED), dialysis clinic, pain clinic, rheumatology, geriatrics and oncology. Non-responders were asked to provide information on their age, gender, race and ethnicity.
Informed consent
Research assistants trained for this survey approached patients who entered the participating units. The research assistant explained the survey and was available to answer questions. Potential respondents were informed that participation was voluntary, they could skip any questions and they could stop at any time. All respondents gave oral informed consent.
Approvals
The George Washington University institutional review board and the NIH Clinical Center Office of Human Subjects Research Protections judged this anonymous survey to be exempt from the US research regulations because it involved only survey procedures and information was not ‘recorded in such a manner that human subjects can be identified, directly or through identifiers linked to the subjects’ (45CFR46.101 b. 2). As a result, the present survey did not undergo full research ethics committee review.
Survey
Based on the existing literature, the authors drafted a survey. The draft survey was evaluated by four focus groups and revised. The survey then underwent cognitive pretesting with six patients and two academics, using a ‘think-aloud’ approach to ensure the questions were understood. Finally, behavioural pretesting with nine patients and two academics was employed to ensure the survey could be implemented successfully.
The final survey was self-administered, took on average 25 min to complete and included 41 questions, with a mixture of closed-ended and open-ended questions. The survey covered four domains: (1) personal characteristics; (2) experience with decisional incapacity; (3) goals regarding treatment decision-making; and (4) views on a PPP. The present article reports on the fourth domain.
To ensure that the survey was relevant to a broad range of patients, including those with very different health situations, and to avoid the difficulties associated with young and healthy individuals attempting to project their preferences and values into a distant and emotionally uncertain future, we presented respondents with a scenario in which they lose the ability to make decisions due to an automobile accident. For respondents who had previously assigned a surrogate using a durable power of attorney (DPA) form, the survey referred to ‘your DPA’; this terminology reflects common parlance in the USA. For those who indicated that they had not assigned a surrogate, the survey used ‘your family’.
The PPP was explained as follows:
“Your doctors could look up in a database or computer which treatments people like you would want in your situation. People like you are people who are of the same gender, similar age, similar education, and similar cultural background. Your doctors and your DPA [family] could then consider this information when deciding how to treat you”.
Following this description, respondents were asked five questions regarding the use of a PPP. To detect any ordering effects, the response categories in the questions were reversed for half of the surveys.
The first question asked respondents to indicate in general whether they thought use of a PPP sounded ‘like a good idea or like a bad idea to you’. The response options on a four-point Likert scale were: definitely a bad idea; probably a bad idea; probably a good idea; and definitely a good idea.
The second question asked: ‘Giving your DPA [family] information on which treatments people like you would want in your situation might make it less stressful for your DPA [family] to make treatment decisions for you. If it does, what would you want your doctors to do?’ The response options were: give my DPA [family] information on which treatments people like me would want; have my DPA [family] help make decisions without giving my DPA [family] information on which treatments people like me would want; use the approach that is more likely to reduce the stress on my DPA [family]; use the approach my DPA [family] prefers; I do not have a DPA [family].
The third question stated: ‘People who are similar often want the same treatments. So giving your DPA [family] information on which treatments people like you would want in your situation might increase the chances that you get the treatment you would want. If it does, what would you want your doctors to do?’ The response options were: give my DPA [family] information on which treatments people like me would want; have my DPA [family] help make decisions without giving my DPA [family] information on which treatments people like me would want; use the approach that is more likely to give me the treatment I would want (even if this means that my DPA [family] does not help make decisions); use the approach my DPA [family] prefers; I do not have a DPA [family].
The fourth question stated: ‘Consider again the case that you are in a bad car accident. Your doctors could look up in a database or computer which treatments people like you would want in your situation. How would you want your doctors to use this information?’ The response options were: not at all. My DPA [family] should help the doctors make decisions without any information on which treatments people like me would want; the doctors should give my DPA [family] information on which treatments people like me would want, and then let my DPA [family] decide how I am treated; the doctors should give me the treatments people like me would want unless my DPA [family] believes I would want some other treatment; the doctors should give me the treatments people like me would want even if my DPA [family] believes I would want some other treatment; use some other approach: please explain what approach.
Finally, in an open-ended follow-up to question four, respondents were asked: ‘Please explain why you chose the answer you did in the previous question. Why do you want treatment decisions to be made in that way?’ The complete survey is available upon request from the authors.
Statistical analysis
We evaluated 13 potential predictors for each of the first four questions. For predictors with two levels, Fisher’s exact test for 2×2 contingency tables was used. For predictors with more than two (ordered) levels, Cuzick’s non-parametric test (an extension of the Wilcoxon rank-sum test for more than two ordered groups) was used. For predictors that were significant at p<0.05, we conducted multivariate analysis based on a user-guided forward stepwise logistic regression.
RESULTS
Respondents
Of 1955 patients who were invited, 1169 agreed to participate. A total of 34 surveys were excluded due to a lack of substantive answers. Of the 1135 evaluable surveys, information on the recruitment site was missing for four respondents. For the remaining 1131 respondents, the number of respondents and response rate in each of the seven participating units were: general medicine, n=130 (68%); ED, n=697 (52%); dialysis clinic, n=58 (75%); pain clinic, n=50 (82%); rheumatology, n=73 (81%); geriatrics, n=61 (82%); and oncology, n=62 (97%), for an overall response rate of 59.8%.
The 1135 evaluable surveys came from a broad range of respondents in terms of age, race, ethnicity, education and income (table 1). In addition, 49 US states were listed as the place of birth by at least one respondent, 18 US states were listed by 10 or more respondents and 58 countries other than the USA were listed as the place of birth for at least one respondent. Respondents’ self-reported quality of life was good overall and 71.2% had not completed an AD (table 2).
Table 1.
Demographics and personal characteristics (N=1135)
| Demographics and personal characteristics | N (%)* | Missing n (%) |
|---|---|---|
| Age | ||
| Mean (SD) | 42.2 (17.2) | 21 (1.9) |
| Range | 18–95 | |
| <35 years | 468 (42.0) | |
| 35–49 years | 293 (26.3) | |
| 50–64 years | 227 (20.4) | |
| ≥65 years | 126 (11.3) | |
| Gender | ||
| Female | 644 (57.7) | 19 (1.7) |
| Male | 472 (42.3) | |
| Place of birth | ||
| DC, Maryland, Virginia† | 407 (37.4) | 46 (4.1) |
| Other states and territories† | 554 (50.9) | |
| Non-USA‡ | 128 (11.8) | |
| Race/ethnicity | ||
| Black or African-American | 472 (42.0) | 10 (0.9) |
| Native American | 6 (0.5) | |
| Asian | 50 (4.4) | |
| Native Hawaiian/Pacific Islander | 2 (0.2) | |
| Hispanic | 60 (5.3) | |
| White | 517 (46.0) | |
| Multiple races | 18 (1.6) | |
| Education | ||
| Graduate school | 292 (25.7) | 0 (0) |
| College | 383 (33.7) | |
| High school | 430 (37.9) | |
| Grade school | 25 (2.2) | |
| Less than grade school | 5 (0.4) | |
| Income | ||
| <$25 000 | 217 (21.1) | 106 (9.3) |
| $2500–49 999 | 224 (21.8) | |
| $50 000–99 999 | 258 (25.1) | |
| $100 000–249 000 | 243 (23.6) | |
| ≥$250 000 | 87 (8.5) | |
| Relationship with DPA [family] | ||
| Excellent | 481 (42.8) | 10 (0.9) |
| Very good | 354 (31.5) | |
| Good | 203 (18.0) | |
| Fair | 61 (5.4) | |
| Poor | 22 (2.0) | |
| No DPA [family] | 4 (0.4) | |
Totals may not sum to 100% due to rounding.
Forty-nine US states/territories, ≥5 respondents from 29 US states.
Total of 58 countries.
DC, District of Columbia; DPA, durable power of attorney.
Table 2.
Clinical condition and advance care planning (N=1135)
| N (%)* | Missing n (%) | |
|---|---|---|
| Unit or clinic | ||
| Emergency department | 697 (61.6) | 4 (0.4) |
| Medicine | 130 (11.5) | |
| Rheumatology | 73 (6.5) | |
| Oncology | 62 (5.5) | |
| Geriatrics | 61 (5.4) | |
| Dialysis | 58 (5.1) | |
| Pain | 50 (4.4) | |
| Current quality of life | ||
| Excellent | 266 (23.7) | 14 (1.2) |
| Very good | 422 (37.6) | |
| Good | 311 (27.7) | |
| Fair | 99 (8.8) | |
| Poor | 23 (2.1) | |
| Advance directive | ||
| No AD or DPA | 795 (71.2) | 18 (1.6) |
| DPA only | 56 (5.0) | |
| AD only | 82 (7.3) | |
| AD and DPA | 184 (16.5) | |
| If DPA: person named | ||
| Spouse/partner | 105 (43.8) | 0 (0) |
| Other DPA [family] member | 115 (47.9) | |
| Friend | 15 (6.3) | |
| Someone else | 5 (2.1) |
Totals may not sum to 100% due to rounding.
AD, advance directive; DPA, durable power of attorney.
There was no significant difference in gender between respondents and non-respondents. The response rate was higher among younger patients in the ED (p<0.001). Furthermore, Asians and whites in the ED (compared with blacks and Hispanics), and Hispanics and whites in non-ED units (compared with blacks and Asians), were more likely to respond (p<0.001 in each case, comparing combined groups).
General views regarding a PPP
In response to the first question of whether the PPP seemed ‘like a good idea or like a bad idea’, 55.2% initially thought that the PPP sounded like a ‘good idea’ and 44.9% thought it sounded like a ‘bad idea’ (table 3). Of the 13 tested possible predictors, four were significant for this question. Respondents who self-identified as African–American were significantly more likely to regard the PPP as a ‘good idea’ compared with respondents who self-identified as white (p=0.002; Fisher’s exact test). In addition, older respondents (p=0.007; Cuzick’s non-parametric test), respondents with less formal education (p=0.010; Cuzick’s non-parametric test) and respondents with lower gross income in the previous year (p=0.0006; Cuzick’s non-parametric test) were significantly more likely to regard the PPP as a ‘good idea’.
Table 3.
Attitudes towards a PPP (N=1135)
| Attitudes | N (%)* | Missing n (%) |
|---|---|---|
| Question #1 General attitude toward PPP | 155 (13.7) | |
| Definitely good idea | 144 (14.7) | |
| Probably good idea | 397 (40.5) | |
| Probably bad idea | 269 (27.5) | |
| Definitely bad idea | 170 (17.4) | |
| Question #2 If PPP reduces stress on DPA [family] | 166 (14.6) | |
| Provide DPA [family] PPP prediction for consideration | 468 (48.3) | |
| Do not use PPP | 149 (15.4) | |
| Use approach more likely to reduce stress | 137 (14.1) | |
| Use approach DPA [family] prefers | 205 (21.2) | |
| No DPA [family] | (1.0) | |
| Question #3 If PPP increases chances treated consistent with preferences | 174 (15.3) | |
| Provide DPA [family] PPP prediction for consideration | 529 (55.1) | |
| Do not use PPP | 132 (13.7) | |
| Use approach more likely to increase accuracy | 128 (13.3) | |
| Use approach DPA [family] prefers | 165 (17.2) | |
| No DPA [family] | 7 (0.7) | |
| Question #4 How use PPP in own case | 188 (16.6) | |
| Provide DPA [family] PPP prediction for consideration | 512 (54.1) | |
| Treat according to PPP unless DPA [family] objects | 168 (17.7) | |
| Treat according to PPP even if DPA [family] objects | 67 (7.1) | |
| Do not use PPP | 144 (15.2) | |
| Some other approach | 56 (5.9) | |
Totals may not sum to 100% due to rounding.
DPA, durable power of attorney; PPP, patient preference predictor.
In a multivariate analysis of the four significant predictors, the predictiveness of education was largely subsumed by the predictiveness of income and the correlation between the two. The other three predictors—lower income, increased age and self-identifying as African–American—all significantly predicted being more likely to regard the PPP as a ‘good idea’.
Use of a PPP if it increases accuracy or reduces stress
The second question asked how respondent would want the PPP to be used if it ‘might make it less stressful for your DPA [family] to make treatment decisions for you’. In response, 48.3% wanted their DPA [family] to receive the PPP prediction, 21.2% wanted to use the approach their DPA [family] preferred and 14.1% wanted to use whichever approach is most likely to reduce surrogate stress (table 3). In contrast, 15.4% did not want their DPA [family] to receive the PPP prediction. None of the 13 tested possible predictors were significant for this question.
In response to the third question of how they would want the PPP to be used if it ‘might increase the chances that you get the treatment you would want’, 55.1% wanted their DPA [family] to receive the PPP prediction, 17.2% wanted to use the approach their DPA [family] preferred and 13.3% wanted to use whichever approach is most accurate (table 3). In contrast, 13.7% did not want their DPA [family] to receive the PPP prediction. None of the 13 tested possible predictors were significant for this question.
Use of a PPP in the respondent’s own case
The fourth question asked respondents how they would want doctors to use the PPP in the event that they lost the ability to make their own decisions. In response, 78.9% wanted the PPP to be used in their own case, with 54.1% wanting the PPP prediction to be given to their DPA [family], 17.7% wanting to be treated based on the PPP prediction unless their DPA [family] objected and 7.1% wanting to be treated based on the PPP prediction even if their DPA [family] objected (table 3). In contrast, 15.2% of respondents did not want the PPP prediction to be used for them in any way.
None of the 13 tested possible predictors were significant for the fourth question. In particular, the four comparisons that were statistically significant for the first question of whether the PPP seemed like a good idea (white vs African–American; younger vs older; more formal education vs less formal education; greater income vs lower income) were not significant for the fourth question.
Reasons for endorsing or opposing personal use of a PPP
As a follow-up to the fourth question, the final (open-ended) question asked respondents to explain why they would want or not want the PPP to be used in case they lost the ability to make treatment decisions. Most of the respondents who explained why they endorsed the use of a PPP in their own case cited the possibility that providing the PPP prediction might help their DPA [family] determine which treatment the patient would want and/or might reduce the stress on their DPA [family] (figure 1). For example, one respondent indicated: ‘My family could draw on the information the doctor gives them and hopefully make a more informed decision’. Another stated: ‘To help my DPA make a decision that wouldn’t be too stressful on her’.
Figure 1.
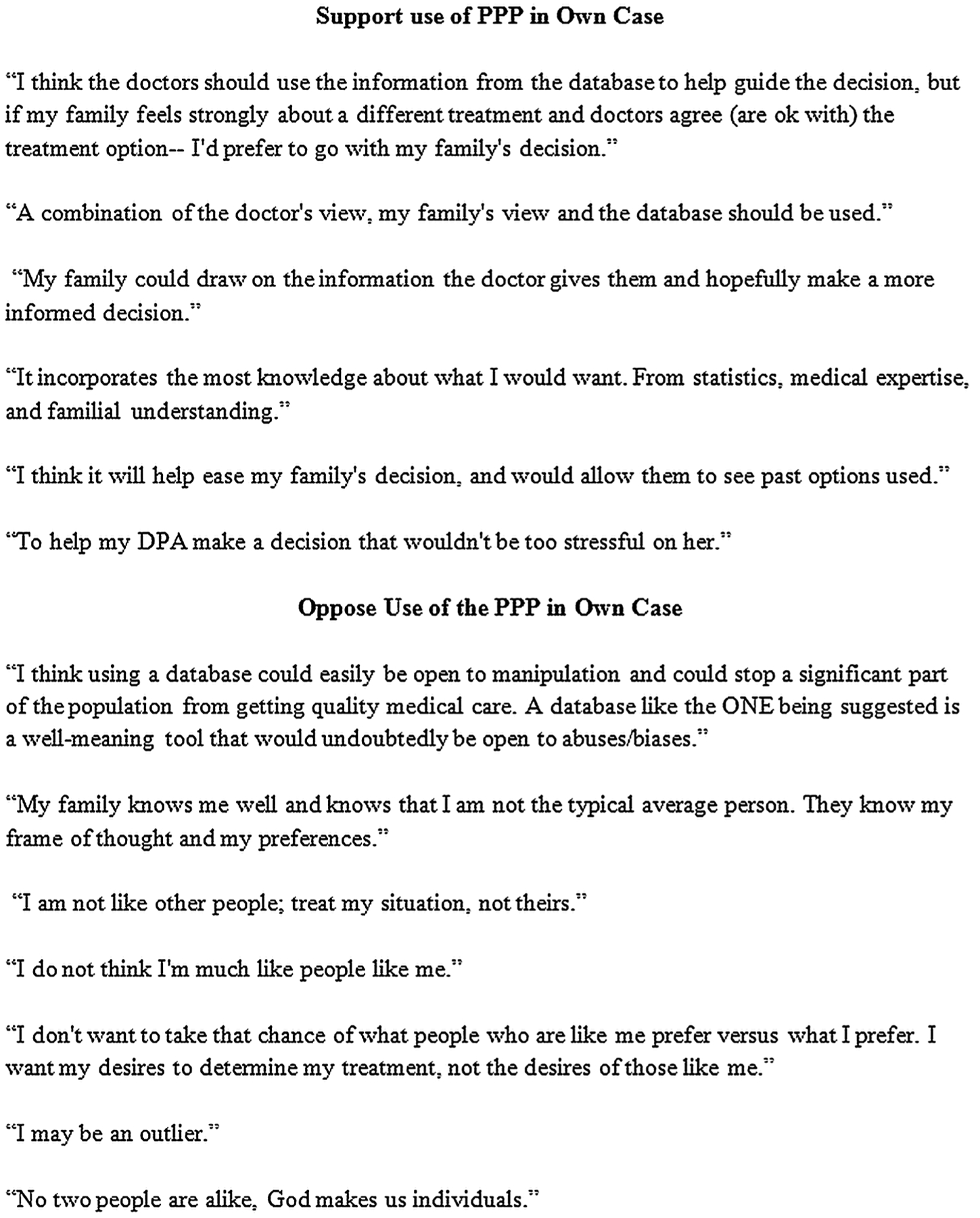
Selected verbatim explanations for endorsing or opposing patient preference predictor (PPP).
With a few exceptions, respondents who provided an explanation for why they opposed the use of the PPP stated that it could not predict their treatment preferences because they were unique, or their DPA [family] already knew their treatment preferences (figure 1). For example, one stated, ‘No two people are alike, God makes us individuals’, and another said: ‘My family knows me well and knows that I am not the typical average person. They know my frame of thought and my preferences’.
The only in-principle objections came from several respondents who were concerned that use of a PPP might encourage or reinforce stereotypes. One said: ‘I do not match my demographics in many ways. Just cause I am a Hispanic, Catholic gay man with a low income does not mean I would want what all Hispanic, Catholic, gay low-income men would want’.
Limitations
The present findings are subject to five important limitations that merit further research. First, recruitment occurred at one site only. At the same time, respondents were diverse in terms of geographic origin, coming from a total of 49 states and territories and a total of 58 countries (table 1). Second, while the response rate was relatively high in six of the seven recruitment units (77.8% overall), it was lower in the ED (52.3%). Third, each of the first four questions was skipped by approximately 15% of respondents. This may have influenced the results. Fourth, the survey used a scenario of sudden incapacity as a result of an automobile accident. While this scenario ensured that the survey was relevant to all respondents, the preferences of some respondents may have been different for other scenarios involving decisional incapacity. Fifth, we excluded patients for whom a 30 min survey was regarded as overly burdensome. As a result, the present findings may not reflect the views of individuals who are very ill.
DISCUSSION
Shared decision-making between surrogates and clinicians is intended to protect and respect patients who have lost the ability to make their own decisions. Yet, empirical studies find that clinicians and surrogates often are unable to predict which treatment is consistent with the patient’s preferences and values.19 In addition, surrogates can experience significant distress as a result of making treatment decisions.14 Incorporating a PPP into the process of shared decision-making has been proposed as one possible way to address these two concerns.17 Before pursuing development of a PPP, however, it is important to evaluate whether patients would support its use.
In the present survey, 78.9% of respondents endorsed the use of a PPP in the event that they lost the ability to make their own decisions. The fact that 16.6% of respondents skipped this question may indicate that actual support for the PPP was lower than 78.9%. However, even if 80% of those who skipped this question were opposed to the PPP, the present findings would still suggest that approximately two-thirds of respondents support use of a PPP in their own case. These findings provide strong patient support for the use of a PPP to the extent that incorporating it into the shared decision-making process can increase predictive accuracy and reduce surrogate distress.
Shared decision-making likely alleviates at least some of the stress and anxiety that surrogates experience. At the same time, empirical studies find that physicians may be even less accurate than surrogates at predicting patients’ treatment preferences.12,13 In response, some commentators have proposed basing treatment decisions for incapacitated patients on the preferences of patients in the same community.20 Unless the community happens to be very homogenous, this approach is unlikely to identify the treatment option most consistent with the patient’s preferences and values. Other proposals, such as relying on ethics committees or judges21 to make treatment decisions for incapacitated patients, seem no more likely to provide treatment consistent with the patient’s preferences and values.
Data reveal that patients’ treatment preferences often are correlated with their individual characteristics, including age,22,23 gender24,25 and race.26,27 These data suggest that it may be possible to more accurately predict which treatment a given patient would want based on his or her individual characteristics, the situation and how these factors influence patients’ treatment preferences. Evaluation of a very preliminary PPP found that it was as accurate as patient-designated surrogates and suggested that a full-scale PPP might be more accurate than surrogates.15
To develop and test a full-scale PPP it would be necessary to gather extensive empirical data from a representative sample regarding how individuals want to be treated in common situations involving decisional incapacity.16 Statistical analysis of these data would identify predictors of patients’ treatment preferences. These predictions could then be incorporated into the shared decision-making process between clinicians and the patient’s DPA [family], testing how different ways of using PPP predictions influence surrogate stress. Accuracy of the PPP could be tested by comparing competent patients’ preferences for how they want to be treated during periods of decisional incapacity with the predictions of the PPP.
The present findings suggest that most patients would prefer that the PPP predictions be provided to their surrogates who could take this information into account when making treatment decisions. The PPP prediction also could guide clinicians and clinical ethics committees when making treatment decisions for patients for whom no surrogate or family can be identified.28
While this approach makes theoretical sense, development of a full-scale PPP would require an upfront investment of at least tens of millions of dollars.16 To assess whether this effort might be justified, it is important to evaluate patients’ attitudes regarding use of a PPP in more detail and then pilot different uses of the PPP in practice. The present findings suggest that many patients are likely to support a PPP to the extent that it can increase predictive accuracy and reduce surrogate distress. These findings provide empirical support for further research to assess whether incorporating a PPP into the shared decision-making process can increase the extent to which incapacitated patients are treated consistent with their preferences and can reduce the stress on their loved ones.
Most of the respondents who provided an explanation for why they opposed the use of the PPP stated they were unique so that a PPP could not predict their preferences, or their DPA [family] already knew their treatment preferences. Even if use of a PPP increases surrogates’ predictive accuracy some patients may still oppose its use. To respect these patients, ADs might be modified to allow patients to indicate their opposition to the use of a PPP.
Finally, although only a few respondents expressed concern that a PPP might be misused or might reinforce stereotypes, these concerns will need to be addressed. In particular, it will be important that both the development and the implementation of a PPP is transparent and includes patient advocates who can ensure that the resulting method is not used to deny treatment to certain patients or groups.
SUMMARY
Current practice for making treatment decisions for incapacitated patients raises two important concerns: surrogates and clinicians often are unable to determine which treatment their charges want, and surrogates can experience significant distress as a result of making treatment decisions. Supplementing the shared decision-making process with a PPP has been proposed as one possible way to address these two concerns. The present findings suggest that a majority of patients would likely support a practice of providing the PPP prediction to their clinicians and surrogates to the extent that doing so increases the chances they are treated consistent with their preferences and values and reduces the stress on their loved ones. These findings provide strong patient support for future research to develop and evaluate a PPP and determine whether it can help to promote these important goals for treatment decision-making for incapacitated patients.
Acknowledgements
Thanks to the patients who participated in the survey and to our clinical collaborators at GW, especially Sharon Maynard and Katalin Roth. Thanks also to the many colleagues who gave critical input into the development of the survey; to Virginia Hines, Jonathan Hill, Michol Holloway, Brenna Kelly and students in the GW ‘Emergency Medicine Research’ class (fall 2009) for their assistance; and to Karen Smith for help with the literature search. Finally, thanks to our colleagues who provided input and suggestions on previous drafts of the manuscript.
Funding NIH Clinical Center.
Footnotes
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
REFERENCES
- 1.Vig EK, Starks H, Taylor JS, et al. Surviving surrogate decision-making: what helps and hampers the experience of making medical decisions for others. J Gen Intern Med 2007;22:1274–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smedira NG, Evans BH, Grais LS, et al. Withholding and withdrawal of life support from the critically ill. N Engl J Med 1990;322:309–15. [DOI] [PubMed] [Google Scholar]
- 3.Sessums LL, Zembrzuska H, Jackson JL. Does this patient have medical decision-making capacity? JAMA 2011;306:420–7. [DOI] [PubMed] [Google Scholar]
- 4.Torke AM, Sachs GA, Helft PR, et al. Scope and outcomes of surrogate decision making among hospitalized older adults. JAMA Intern Med 2014;174:370–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beauchamp TL, Childress JF. Principals of biomedical ethics. 7th edn New York: Oxford University Press, 2012. [Google Scholar]
- 6.Kon AA. The shared decision-making continuum. JAMA 2010;304:903–4. [DOI] [PubMed] [Google Scholar]
- 7.Kon AA, Davidson JE, Morrison W, et al. Shared decision making in Icus: an American college of critical care medicine and American thoracic society policy statement. Crit Care Med 2016;44(1):188–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Buchanan A, Brock D. Deciding for others. Cambridge: Cambridge University Press, 1990. [Google Scholar]
- 9.Williams MA. Unbefriended. Neurology 2006;67:2088. [DOI] [PubMed] [Google Scholar]
- 10.Pope TM, Sellers T. Legal briefing: the unbefriended: making healthcare decisions for patients without surrogates (Part 2). J Clin Ethics 2012;23:177–92. [PubMed] [Google Scholar]
- 11.Rid A, Wendler D. Can we improve treatment decision-making for incapacitated patients? Hastings Cent Rep 2010;40:36–45. [DOI] [PubMed] [Google Scholar]
- 12.Coppola KM, Ditto PH, Danks JH, et al. Accuracy of primary care and hospital-based physicians’ predictions of elderly outpatients’ treatment preferences with and without advance directives. Archives Intern Med 2001;161:431–40. [DOI] [PubMed] [Google Scholar]
- 13.Fischer GS, Tulsky JA, Rose MR, et al. Patient knowledge and physician predictions of treatment preferences after discussion of advance directives. J General Intern Med 1998;13:447–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med 2011;154:336–46. [DOI] [PubMed] [Google Scholar]
- 15.Shalowitz DI, Garrett-Mayer E, Wendler D. How should treatment decisions be made for incapacitated patients, and why? PLoS Med 2007;4:e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rid A, Wendler D. Treatment decision making for incapacitated patients: Is development and use of a Patient Preference Predictor feasible? J Med Philos 2014;39:130–52. [DOI] [PubMed] [Google Scholar]
- 17.Rid A, Wendler D. Use of a patient preference predictor to help make medical decisions for incapacitated patients. J Med Philos 2014;39:104–29. [DOI] [PubMed] [Google Scholar]
- 18.Varma S, Wendler D. Medical decision making for patients without surrogates. Arch Intern Med 2007;167:1711–15. [DOI] [PubMed] [Google Scholar]
- 19.Shalowitz DI, Garrett-Mayer E, Wendler D. The accuracy of surrogate decision-makers: a systematic review. Arch Intern Med 2006; 166:493–7. [DOI] [PubMed] [Google Scholar]
- 20.Emanuel LL, Emanuel EJ. Decisions at the end of life. Guided by communities of patients. Hastings Cent Rep 1993;23:6–14. [PubMed] [Google Scholar]
- 21.Ouslander JG, Tymchuk AJ, Rahbar B. Health care decisions among elderly long-term care residents and their potential proxies. Arch Intern Med 1989;149:1367–72. [PubMed] [Google Scholar]
- 22.Phillips RS, Wenger NS, Teno J, et al. Choices of seriously ill patients about cardiopulmonary resuscitation: correlates and outcomes. SUPPORT investigators. Study to understand prognoses and preferences for outcomes and risks of treatments. American J Med 1996;100:128–37. [DOI] [PubMed] [Google Scholar]
- 23.Rosenfeld KE, Wenger NS, Phillips RS, et al. Factors associated with change in resuscitation preference of seriously ill patients. The SUPPORT investigators. Study to understand prognoses and preferences for outcomes and risks of treatments. Arch Intern Med 1996;156:1558–64. [PubMed] [Google Scholar]
- 24.Pearlman RA, Cain KC, Starks H, et al. Preferences for life-sustaining treatments in advance care planning and surrogate decision making. J Palliat Med 2000;3:37–48. [DOI] [PubMed] [Google Scholar]
- 25.Bookwala J, Coppola KM, Fagerlin A, et al. Gender differences in older adults’ preferences for life-sustaining medical treatments and end-of-life values. Death Stud 2001;25:127–49. [DOI] [PubMed] [Google Scholar]
- 26.Barnato AE, Anthony DL, Skinner J, et al. Racial and ethnic differences in preferences for end-of-life treatment. J Gen Intern Med 2009;24:695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fried TR, Bradley EH, Towle VR, et al. Understanding the treatment preferences of seriously ill patients. N Engl J Med 2002;346:1061–6. [DOI] [PubMed] [Google Scholar]
- 28.White DB, Curtis JR, Lo B, et al. Decisions to limit life-sustaining treatment for critically ill patients who lack both decision-making capacity and surrogate decision-makers. Crit Care Med 2006;34:2053–9. [DOI] [PubMed] [Google Scholar]


