Abstract
Tattoo pigment can precipitate numerous inflammatory states, and granulomatous tattoo reactions are a diagnostically challenging form. The skin is the most common site of inflammation, but systemic inflammation can occur. Reactions to black tattoo ink have a broad differential of cutaneous and systemic conditions. Sarcoidosis is an important consideration because it is unclear whether it is a separate entity. Here we present a 31-year-old male who developed an inflammatory eruption where he had black tattoos. He also developed circular patches of scalp alopecia, monocular uveitis, and an enlarged axillary lymph node, initially thought to represent lymphoma. Tissue biopsy of the skin and lymph node revealed findings consistent with granulomatous tattoo reaction. Investigations for other diagnoses, including sarcoidosis, were negative. He was treated with systemic corticosteroids and then with topical corticosteroids and oral hydroxychloroquine. This case report demonstrates the diagnostic challenge associated with granulomatous tattoo ink reactions. Further studies are needed to improve characterization and management of this condition.
Keywords: Tattoo reaction, granulomatous reaction, systemic tattoo reaction, sarcoidal, tattoo ink
Introduction
Tattoo pigment can precipitate many inflammatory states. The skin is the most common site of inflammation, but tattoo ink can become disseminated and cause systemic inflammation.1 Granulomatous reactions are a rare type of tattoo reaction, often caused by black tattoo ink, and are challenging to manage.2
Granulomatous reactions to black tattoo ink have a wide range of differential diagnoses. Examples include allergic contact dermatitis (pseudolymphomatous type), foreign body granuloma, melanoma, sarcoidosis, hematologic malignancies, and metastatic solid organ cancers.2 Importantly, there are many similarities between granulomatous tattoo reactions and sarcoidosis, but there is controversy over whether or not they are separate entities or are part of a spectrum.
Rarely, tattoo pigment can be deposited in extracutaneous locations (i.e. lymph nodes and internal organs), sometimes even years after the initial tattoo.3,4 The diagnostic challenge is that extracutaneous ink deposition, particularly in lymph nodes, can cause painless lymphadenopathy and closely resemble malignant melanoma, other cancers that can metastasize to lymph nodes, lymphoma/leukemia, and sarcoidosis. Each of these differential diagnoses have different management and prognoses, making diagnostic accuracy and appropriate treatment of paramount importance.4,5 There is an association between tattoo ink reactions and systemic inflammation (e.g. uveitis, arthritis, and enteritis), but this is not well understood.1,2
Case report
A 31-year-old, First Nations, male with whole body tattoos was admitted to hospital with seizures and symptoms of alcohol withdrawal. He was found to have a significant inflammatory eruption consisting of red–brown plaques with some areas of desquamation, localized to skin with black tattoo ink. He also had numerous circular patches of alopecia on his scalp. He had left-sided uveitis that may have occurred concomitantly with the tattoo reaction. Most of the tattoos were over 3 years old, except for a tattoo above his left eyebrow which was done 1–2 months before the cutaneous eruption.
His medical history includes childhood eczema, mild rosacea, seizures, steatohepatitis, depression, anxiety, and agoraphobia. He has no known history or family history of autoimmune conditions such as sarcoidosis. Medications at time of presentation included clobetasol ointment, mirtazapine, fluoxetine, prazosin, and gabapentin. No medications were started or re-started prior to his eruption and none of his medications are known to cause drug-induced sarcoidosis.6
Skin biopsy revealed a normal epidermis and non-caseating granulomas in the dermis with black ink–laden macrophages. He was incidentally found to have an enlarged, painless, axillary lymph node. The lymph node was biopsied to rule out malignancy and revealed black ink particles and ink-laden macrophages.
He did not have other findings consistent with sarcoidosis (e.g. bilateral hilar lymphadenopathy, erythema nodosum, hypopigmented patches, lupus pernio, or arthritis). CT chest, abdomen, pelvis, and MRI brain were unremarkable. His bloodwork was normal apart from transaminitis, attributed to alcohol intake, and high inflammatory markers (C-reactive protein (CRP) = 63.3 mg/L and erythrocyte sedimentation rate (ESR) = 18 mm/h). Rheumatologic workup, HIV, and syphilis testing were negative. An angiotensin-converting enzyme level was not obtained, but serum calcium was within normal limits.
He received oral prednisone 40 mg daily, tapered over 3 weeks, and was transitioned to clobetasol ointment and oral hydroxychloroquine. Over 1 year, the alopecia (Figure 1), tattoo ink reaction (Figure 2), and uveitis significantly improved, and he has not had any recurrence.
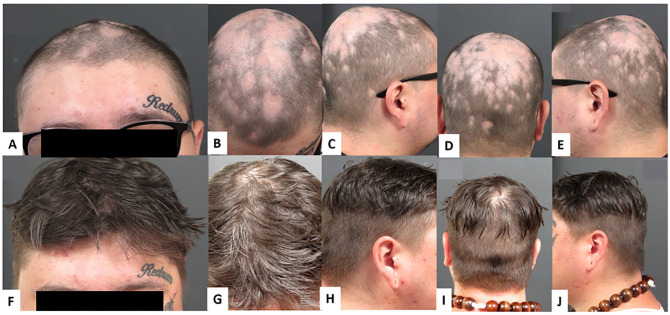
Figure 1.
Scalp alopecia with some scale at presentation (A–E) and resolution at 1-year follow-up (F–J).
Figure 2.
Cutaneous eruption on upper and lower extremities at sites of black tattoo ink at presentation (A–E) and at 1-year follow-up (F–J). Red–brown, inflamed, desquamating plaques on areas of black ink with erythema bordering black ink.
Discussion
Tattooing involves injecting large amounts of colorant particles into skin. Tattoo particles can be regarded as foreign by the immune system leading to recruitment of immune cells, namely macrophages, which form granulomas intended to wall off the foreign material. A hypersensitivity reaction to the tattoo particles and the possibility of precipitating sarcoidosis has also been hypothesized, but this has yet to be established.7
Tattoo particles are small and can migrate to distant sites. This is thought to be due to either direct spread through blood vessels and lymphatics, or through macrophages which engulf tattoo particles and travel to lymph nodes where they present this antigenic material to activate and recruit lymphocytes.8,9 Mouse studies have shown that tattoo ink from the skin can be found in other lymphatic tissue such as the liver, spleen, kidney, and lung tissue.1 Other than case reports, there have been no investigations to determine to what extent tattoo colorants can be found in other organs of the human body.10
The colorants in tattoos can be divided into two groups: Carbon Black and azo/polycyclic pigments. Amorphous carbon particles (i.e. Carbon Black/India ink) are mainly present in black tattoos along with iron oxide and logwood. Azo and polycyclic pigments can create nearly all colors of the visible spectrum. Tattoo colorants also have by-products and impurities which can contribute to inflammatory states and hypersensitivity reactions.8,10
Studies in humans have reported tattoo pigment incidentally found in sentinel lymph nodes in patients being staged for malignant melanoma. Pigment from black tattoo ink can look very similar to metastatic melanoma, histologically, because pigment-laden histeocytes can resemble melanoma cells.3
Granulomatous tattoo reactions can also look very similar to sarcoidosis, clinically and histologically. These tattoo reactions can cause systemic inflammation and granuloma formation, but other manifestations of sarcoidosis are usually absent (e.g. hilar lymphadenopathy, erythema nodosum, lupus pernio, uveitis, and Lofgren’s syndrome). There exists controversy over this distinction and some experts say that granulomatous tattoo reactions are separate from sarcoidosis, while others believe it can be an early presentation of systemic sarcoidosis and will eventually declare itself with time.2,11 Kluger, 2018,7 reported the co-existence of tattoo granulomas with uveitis (TAGU), an entity reserved for cases where other differential diagnoses are excluded and there are insufficient findings to diagnose sarcoidosis.
Regardless of the distinction, the pathophysiology is of granulomatous-type inflammation and parallels sarcoidosis. Therefore, treatments for sarcoidosis such as topical/systemic corticosteroids and anti-malarial medications such as hydroxychloroquine, quinacrine, and chloroquine, have shown to be effective in treating granulomatous tattoo ink reactions. Laser tattoo removal is often contraindicated as this could precipitate systemic dispersion of tattoo pigment.2,11
Black tattoo pigment has been linked to local cutaneous and systemic immune activation. It can be a diagnostic challenge to separate granulomatous tattoo ink reactions and primary diseases such as sarcoidosis, as well as other entities such as allergic contact dermatitis (pseudolymphomatous type), leukemia/lymphoma cutis, hematologic malignancies, metastatic melanoma, and other metastatic cancers. This case study adds to the understanding of the link between autoimmune disease and exogenous precipitants such as tattoo ink. Further investigation with larger numbers of patients and long-term follow-up is needed to better understand this phenomenon, and improve diagnostic accuracy and management.
Footnotes
Author contributions: All authors contributed equally to the manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the patient for clinical and photographic material used for research and peer-reviewed publication.
References
- 1. Sepehri M, Sejersen T, Qvortrup K, et al. Tattoo pigments are observed in the Kupffer cells of the liver indicating blood-borne distribution of tattoo ink. Dermatology 2017; 233(1): 86–93. [DOI] [PubMed] [Google Scholar]
- 2. Morales-Callaghan AM, Aguilar-Bernier M, Martínez-García G, et al. Sarcoid granuloma on black tattoo. J Am Acad Dermatol 2006; 55(5 Suppl.): S71–S73. [DOI] [PubMed] [Google Scholar]
- 3. Manganoni AM, Sereni E, Pata G, et al. Pigmentation of axillary sentinel nodes from extensive skin tattoo mimics metastatic melanoma: case report. Int J Dermatol 2014; 53(6): 773–776. [DOI] [PubMed] [Google Scholar]
- 4. Chikkamuniyappa S, Sjuve-Scott R, Lancaster-Weiss K, et al. Tattoo pigment in sentinel lymph nodes: a mimicker of metastatic malignant melanoma. Dermatol Online J 2005; 11(1): 14. [PubMed] [Google Scholar]
- 5. Grove N, Zheng M, Bristow RE, et al. Extensive tattoos mimicking lymphatic metastasis on positron emission tomography scan in a patient with cervical cancer. Obstet Gynecol 2015; 126(1): 182–185. [DOI] [PubMed] [Google Scholar]
- 6. Cohen Aubart F, Lhote R, Amoura A, et al. Drug-induced sarcoidosis: an overview of the WHO pharmacovigilance database. J Intern Med. Epub ahead of print 15 October 2019. DOI: 10.1111/joim.12991. [DOI] [PubMed] [Google Scholar]
- 7. Kluger N. Tattoo-associated uveitis with or without systemic sarcoidosis: a comparative review of the literature. J Eur Acad Dermatol Venereol 2018; 32(11): 1852–1861. [DOI] [PubMed] [Google Scholar]
- 8. Kürle S, Schulte KW, Homey B. Accumulation of tattoo pigment in sentinel lymph nodes. Hautarzt 2009; 60(10): 781–783. [DOI] [PubMed] [Google Scholar]
- 9. Schlager A, Laser A, Melamed J, et al. A tattoo-pigmented node masquerading as the sentinel node in a case of breast cancer. Breast J 2008; 14(3): 299–300. [DOI] [PubMed] [Google Scholar]
- 10. Bäumler W. Absorption, distribution, metabolism and excretion of tattoo colorants and ingredients in mouse and man: the known and the unknown. Curr Probl Dermatol 2015; 48: 176–184. [DOI] [PubMed] [Google Scholar]
- 11. Anolik R, Mandal R, Franks AG. Sarcoidal tattoo granuloma. Dermatol Online J 2010; 16(11): 19. [PubMed] [Google Scholar]