Abstract
Background:
Anterior cruciate ligament (ACL) tear and meniscal injury often co-occur. The protective effect of early ACL reconstruction (ACLR) on meniscal injury and its repair is not clear. Critical literature review can support or change clinical strategies and identify gaps in the available evidence.
Purpose:
To assess the protective effect of ACLR on the meniscus and provide clinical guidelines for managing ACL tears and subsequent meniscal injury. We aimed to answer the following questions: (1) Does ACLR protect the meniscus from subsequent injury? (2) Does early ACLR reduce secondary meniscal injury compared with delayed ACLR? (3) Does ACLR protect the repaired meniscus?
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review was performed through use of MEDLINE and Embase electronic databases according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Search terms included ACL, reconstruction, and meniscus. Studies describing primary ACLR and nonoperative treatment in adult patients were included, as well as studies indicating timing of ACLR. The included articles were assessed individually for risk of bias through use of the modified Cochrane Risk of Bias and MINORS (Methodological Index for Nonrandomized Studies) tools.
Results:
One level 2 randomized controlled trial and several level 3 and 4 studies indicated a protective effect of ACLR on meniscal injury compared with nonoperative treatment. There was weak (level 3) evidence of the protective effect of early ACLR on the meniscus. Meniscal repair failure was less frequent in patients with ACL reconstruction than in patients with ACL deficiency (level 4).
Conclusion:
The evidence collected in this review suggests a protective effect of ACLR for subsequent meniscal injury (level 2 evidence). ACLR should be performed within 3 months of injury (level 3 evidence). Meniscal injury requiring surgical repair in the ACL-deficient knee should be treated with repair accompanied by ACLR (level 3 evidence). The paucity of level 2 studies prevents the formation of guidelines based on level 1 evidence. There is a strong clinical need for randomized or prospective trials to provide guidelines on timing of ACLR and meniscal repair.
Keywords: ACL, meniscus, biology of ligament, biomechanics
Anterior cruciate ligament (ACL) tears affect more than 120,000 patients per year in the United States, and in 48% to 65% of patients, these tears are associated with meniscal injury.16,27,50 Similarly, in a cohort of more than 9000 meniscal repairs, 40.5% of the repairs were performed together with ACL reconstruction (ACLR).35 ACL tears are associated with a high risk of osteoarthritis, with an osteoarthritis incidence of 50% at 10 to 20 years after the tear.8,34 According to a meta-analysis, the most important predictor of osteoarthritis after ACLR was meniscectomy (odds ratio, 3.45).44
ACLR is thought to restore stability in the knee, thereby protecting the knee from further meniscal damage. This is in contrast to findings of a randomized controlled trial (RCT) comparing early ACLR with nonsurgical rehabilitation, in which a similar number of meniscal surgeries was found in both groups.20 It is therefore unclear what effect ACL tears and their reconstruction have on the meniscus. Likewise, no consensus is available regarding the success of meniscal repair in ACL-deficient versus ACL-reconstructed knees. Although retrospective studies23,35 have reported higher success rates of meniscal repair concomitant with ACLR compared with meniscal repair in ACL-deficient knees, these studies are of low methodological quality and prone to bias.
Several studies investigating the effect of ACLR are currently under way. In a prospective cohort including 7 sites in Sweden, patients receive either ACLR or nonoperative care with possible delayed ACLR. Patients at 1 center will undergo diagnostic magnetic resonance imaging (MRI) at several time points during follow-up in order to assess secondary meniscal injury.31 An RCT comparing ACLR versus nonoperative care was recently completed in the Netherlands,10 but data are not yet available in the literature. Therefore, treatment of ACL tear is currently based on expert opinion and personal experience rather than high-level evidence. Critical literature review can provide evidence that supports or changes clinical strategies and can identify gaps in the available evidence.
The purpose of this systematic review was to assess the protective effect of ACLR on the meniscus and provide clinical guidelines for handling ACL tear and subsequent meniscal injury. We aimed to answer the following questions: (1) Does ACLR protect the meniscus from subsequent injury? (2) Does early ACLR reduce secondary meniscal injury compared with delayed ACLR? (3) Does ACLR protect the repaired meniscus? We used the PICOS (participants, interventions, comparisons, outcomes, study designs) process to address the research questions, as described in Table 1.
Table 1.
PICOS (Participants, Interventions, Comparisons, Outcomes, Study Designs) for the Research Questionsa
| Does ACLR Protect the Meniscus From Subsequent Injury? | Does Early ACLR Reduce Secondary Meniscal Injury Compared With Delayed ACLR? | Does ACLR Protect the Repaired Meniscus? | |
|---|---|---|---|
| Participants | Adults | Adults | Adults with concomitant ACL tear and meniscal injury |
| Interventions | Primary ACLR | Primary ACLR (acute) | Primary ACLR with meniscal repair |
| Comparisons | Nonoperative treatment | Primary ACLR (delayed) | Nonoperative treatment for ACL with meniscal repair |
| Outcomes | (Secondary) meniscal injury | (Secondary) meniscal injury | Healing, reoperation, retear, or tear worsening |
| Study designs | All study designs | All prospective studies Retrospective studies describing a total cohort of ACL tears (including a nonoperative group) Retrospective studies that report assessment of meniscal injury at 2 time points |
All study designs |
aACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction.
Methods
A systematic review of the literature was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.32 A search was conducted on November 7, 2019, in the electronic databases of MEDLINE and Embase using the following search strategy: (“anterior cruciate ligament” [mesh] OR (anterior OR cranial) AND cruciate AND ligament*) AND reconstruction AND “meniscus [mesh] OR menisc*). In Embase, conference abstracts, conference papers, conference reviews, and reviews were excluded from the search.
We chose our inclusion criteria carefully in order to minimize risk of bias. Studies were included based on the PICOS listed in Table 1, regardless of whether an item was a primary or secondary outcome. The lead author (J.V.K.) assessed eligibility by screening of the titles and abstracts. The decision rules and extended inclusion and exclusion criteria are described in Appendix 1. For each included study, the following data were extracted: study design, number of patients, inclusion and exclusion criteria, patient age, presence and type of ACL injury, presence and type of meniscal injury, treatment methods and timing, follow-up duration, outcome of the specific research question, and level of evidence.39
The included RCTs were assessed individually for risk of bias using the modified Cochrane Risk of Bias Tool (Table 2).9 Nonrandomized studies were evaluated via the Methodological Index for Nonrandomized Studies (MINORS) criteria (Table 3).47 If outcomes of different studies conflicted, conclusions were based on level 2 studies. If level 2 studies were not available, level 3 or 4 studies with higher MINORS scores and lower risk of bias as discussed in the final part of each paragraph were weighted heavier in the conclusions.
Table 2.
Critical Appraisal of Randomized Studiesa
| Lead Author | Level of Evidence | Random Sequence Generation | Allocation Concealment | Selective Reporting | Other Sources of Bias | Blinding (Participants and Personnel) | Blinding (Outcome Assessment) | Incomplete Outcome Data |
|---|---|---|---|---|---|---|---|---|
| Frobell,20 Snoeker48 | 2 | Low | Low | Low | High | High | High | ? |
| Meunier,38 Andersson,3 Andersson,4 Odesten40 | 2-3 | High | High | ? | ? | High | High | Low |
| Fithian18 | 3 | High | High | ? | ? | High | High | High |
| Raviraj43 | 2 | Low | Low | ? | ? | High | High | Low |
| Bottoni6 | 2 | Low | Low | ? | Highb | High | High | Low |
aFrobell20 and Snoeker48; and Meunier,38 Andersson,3,4 and Odesten40 are combined as these studies describe data obtained from the same patient group and clinical trial. A question mark indicates that the item was not described in sufficient detail; thus, the risk of bias is unclear.
bThe delayed group was not permitted to return to military duty or recreational sport.
Table 3.
Critical Appraisal of Nonrandomized Studies
| Lead Author | Level of Evidence | MINORS Scorea |
|---|---|---|
| Dunn17 | 3 | 21 |
| Kessler28 | 4 | 15 |
| Meuffels37 | 4 | 12 |
| Daniel11 | 3 | 14 |
| Sanders45 | 3 | 14 |
| Hagmeijer22 | 3 | 15 |
| Herbst24 | 3 | 16 |
| Yoo54 | 4 | 13 |
| De Roeck14 | 4 | 13 |
| Foster19 | 4 | 13 |
| van der Wal52 | 4 | 12 |
| Majeed36 | 4 | 11 |
| Gallacher21 | 4 | 9 |
| Albrecht-Olsen1 | 4 | 14 |
| Plasschaert42 | 4 | 10 |
| Kimura29 | 4 | 10 |
| Valen51 | 4 | 9 |
| Jensen26 | 4 | 10 |
| Austin5 | 4 | 10 |
aMINORS (Methodological Index for Nonrandomized Studies) scores were out of a possible ideal of 16 for noncomparative studies and 24 for comparative studies.
Results
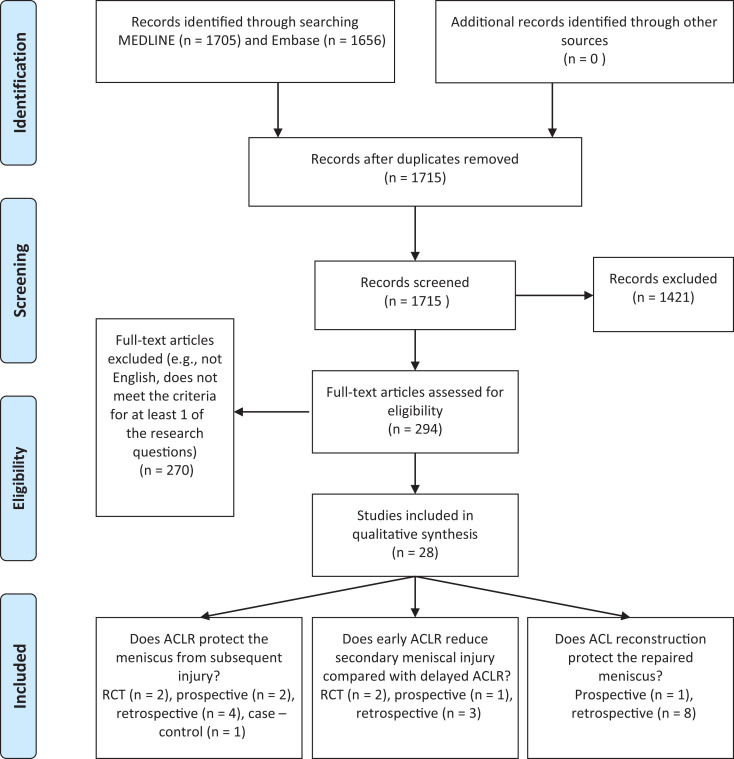
The literature search yielded 1705 articles in MEDLINE and 1656 in Embase, from which 28 studies were ultimately included (Figure 1). Several studies describe data obtained from the same patient group and clinical trial, therefore Frobell20 and Snoeker48; and Meunier,38 Andersson,3,4 and Odesten40 were combined and regarded as 1 study. The extracted data can be found in Appendix 2.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram: summary of literature search. ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; RCT, randomized controlled trial.
Does ACL Reconstruction Prevent Subsequent Meniscal Injury?
In 1 RCT, treatment with early ACLR was compared with rehabilitation with the possibility of delayed ACLR.20 In the early ACLR group, a lower number of meniscal surgeries (5 meniscectomies and 1 repair) were reported during 2-year follow-up (P < .001) than in the nonoperative group (26 meniscectomies and 3 repairs). At baseline, more meniscal surgeries were performed in the early ACLR group (24 partial meniscectomies and 10 repairs) than in the nonoperative group (15 meniscectomies and 6 repairs), and therefore the total amount of meniscal surgeries did not differ statistically between both groups (P = .20). At 5 years of follow-up, half of the patients in the rehabilitation group underwent delayed ACLR. New or worsening meniscal injury occurred in 45% of patients who underwent early ACLR and 53% of patients in the rehabilitation group.48 Patients who did not undergo early ACLR had a relative risk of 2.1 (95% CI, 1.1-3.9) for medial meniscal injury and 1.0 (95% CI, 0.6-1.5) for lateral meniscal injury.
In the trial by Odensten et al,40 surgical treatment was compared with nonoperative treatment.3,4,38,40 Meniscal injury and treatment were comparable between the groups at baseline. During follow-up, there were 5 cases of secondary meniscal injury in the surgical group (total n = 42) and 18 cases in the nonoperative group (n = 52; P = .015). In this trial, 30% of patients allocated to receive nonoperative treatment later underwent ACL repair.38
In the prospective cohort studied by Fithian et al,18 207 patients were assigned a risk level based on preinjury sports participation and degree of laxity. Patients with moderate risk were assigned to receive ACLR within 3 months or nonoperative treatment based on day of presentation. The number of baseline meniscal surgeries was comparable between both groups. During follow-up, 10 meniscectomies (22%) and 3 meniscal repairs (7%) were performed in the nonoperative group, whereas only 1 repair (4%) was performed in the early ACLR group, indicating that ACLR prevents late-phase meniscal injury and that nonoperative therapy might impair reparability of the meniscus.18
Similar results were found in several cohort studies.11,17,22,28,37,45 For instance, ACLR within 6 weeks of trauma decreased secondary meniscal surgery by 56% in the lateral meniscus and by 42% in the medial meniscus (P < .0001) in a US army active-duty population.17 Sanders et al45 reported that 37.4% of patients in their cohort who were treated nonoperatively for ACL tears were later diagnosed with meniscal injury, compared with 19.8% of patients treated with delayed ACLR and 6.1% treated with early ACLR.
Some important confounding effects in the abovementioned studies should be considered. Early meniscal surgery reduces the risk of late-phase meniscal surgery. Subsequently, more aggressive treatment of meniscal injury in the early ACLR group could result in an overestimation of the protective effect of ACLR compared with nonoperative treatment. Such a difference in initial meniscal treatment between patients treated with early ACL or nonoperative treatment was shown in 2 studies,20,37 whereas comparable rates of meniscal surgery in the early phase were reported in other studies.11,18,38 In addition, nonrandomized studies entail a high risk of selection bias based on activity level. In practice, more active patients are often advised to undergo ACLR, whereas other patients are recommended nonoperative treatment. The risk of meniscal injury increases in active patients, and in 2 studies,6,11 nonoperatively treated patients were advised not to participate in cutting or jumping sports or return to military duty. These treatment biases result in an underestimation of the protective effect of ACLR. In contrast, it could also be hypothesized that nonoperatively treated patients have a higher risk of early reinjury owing to a faster return to sport. Additionally, high-level athletes might not enroll in an RCT with a nonoperative group and therefore might be underrepresented in these studies.
Does Early ACLR Reduce Secondary Meniscal Injury Compared With Delayed ACLR?
The number of meniscal injuries after early and delayed ACLR was compared in 2 RCTs and 2 large cohort studies. In 1 RCT,43 no differences in the number of medial or lateral meniscal injuries were found when patients underwent ACLR within 2 weeks after injury (7 days on average) versus within 4 to 6 weeks after injury (32 days on average). Bottoni et al6 reported that the number of medial meniscal tears was comparable between patients who underwent ACLR within 3 weeks after injury (41.2%) and patients who underwent ACLR later than 6 weeks (85 days on average) after injury (42.9%). Importantly, 57.1% of medial tears in the acute group were repairable, whereas only 26.7% of menisci in the delayed group could be repaired.6 Postoperative stiffness, range of motion, and clinical outcomes did not differ between early and delayed ACLR in either trial.6,43
In a cohort containing all inhabitants of Olmsted County (Minnesota, USA), the risk of secondary meniscal injury was higher in patients who underwent delayed (>1 year) ACLR compared with patients who did not have ACL injury (hazard ratio, 4.6). The hazard ratio decreased to 1.6 when patients underwent ACLR within a year after injury.4 In a similar cohort, 19% of patients treated nonoperatively for ACL rupture were found to have a concomitant meniscal injury. Meniscal injury was less prevalent (7%) in the group that was treated with ACLR within 6 months after injury than in the group that underwent delayed ACLR (33%) (P < .01).22
The fate of the meniscus in ACL-deficient knees was studied in 3 case series. The number of meniscal tears increased between 2 preoperative MRI scans54 or between diagnostic arthroscopy and ACLR.14,19 Moreover, existing tears deteriorated.54
Meniscal repair failures and reparability were not different in a prospective cohort of patients with both meniscal and ACL injuries treated within 48 hours or after 3 months.24
The comparability of these studies is limited by the use of different cutoff periods for early or delayed ACLR. The only RCTs comparing early and delayed ACLR used a cutoff of 4 and 6 weeks for delayed ACLR,6,43 although the average time of ACLR in these studies would still be considered early ACLR in the cohort studies. It can be expected that most patients do not return to sports in this time frame, making it difficult to evaluate the protective effect of ACLR. A major confounding effect in the retrospective case series14,19,54 is that only patients who underwent ACLR were included; patients with ACL deficiency who received nonoperative treatment were not included. Meniscal injury could be the reason that patients return to the clinic, whereas the incidence of meniscal injury might be low in the group that remains nonoperative. This is reported in several studies.11,18,22,38
Does ACL Reconstruction Protect the Repaired Meniscus?
The results of meniscal repair combined with ACLR versus meniscal repair in ACL-deficient knees have been described in different studies, although no RCT has been published. Failure of meniscal repair was compared between patients who underwent simultaneous or delayed (>6 weeks) ACLR in a cohort study by Majeed et al.36 Meniscal repair failed in 14.5% of patients who underwent concomitant ACLR (or within 6 weeks) and in 27% of patients who underwent delayed reconstruction (P < .05). Similar results were reported by Gallacher et al21 and several other investigators,5,26,42,52 although in these studies, the results were not statistically significant or no statistical analysis was reported. Only 1 study reported no detrimental effect of ACL deficiency on survival of meniscal repair, although no specific data were provided.51
In 2 studies, healing rates of meniscal repair were assessed with second-look arthroscopy.1,29 In the first study, a residual tear was visible in 18 of 19 menisci in patients who underwent concomitant ACLR, whereas this was the case in 12 of 19 ACL-deficient knees.1 In the second study, healing was reported in all knees that had concomitant ACLR, whereas in the ACL-deficient knees, 4 tears remained unhealed (P < .005).29
Many of these studies were prone to detection bias, because the success of meniscal repair in patients who underwent concomitant ACLR was not evaluated at a later stage, whereas during a delayed ACLR, a repair failure could be detected. Moreover, the 2 retrospective studies both had a high risk of selection bias, because Plasschaert et al42 treated only patients with minor instability and no significant pivot shift nonoperatively, and Albrecht-Olsen et al1 advised ACLR in all high-demand athletes, which could lead to an underestimation of the positive effect of ACLR on healing of meniscal repairs.
Discussion
An overall decrease in meniscal injury after ACLR was found in RCTs as well as prospective studies and large cohorts. This is suggestive of a protective effect of ACLR on the meniscus. Nonetheless, the risk of subsequent meniscal injury remains 3.73 times higher compared with the contralateral knee, as demonstrated in a cohort of 4087 patients with no meniscal injury detected during ACLR.12 This cohort study did not assess the timing of ACLR; therefore, the risk of meniscal injury after early ACLR could be smaller. Patient factors such as age and activity level were not considered in the current review but should be taken into account in the decision-making process. Moreover, cost-effectiveness of ACLR has not been determined but will be analyzed using data from a clinical trial that was recently completed.10
In 2 RCTs,6,43 meniscal injury did not increase between 3 and 6 weeks and between 2 and 4-6 weeks after injury, respectively. ACLR provides a protective effect if performed within 6 to 12 months after injury compared with delayed ACLR, based on large geographical cohort studies (level 3 evidence).22,45 However, these cohort studies did not consider the selection bias to undergo delayed ACLR (patients with symptoms of meniscal injury), and results should be interpreted with care. Return to sports before ACLR was an independent risk factor for lateral meniscal tears in a systematic review evaluating the effect of surgical timing on meniscal injury in adolescents.2 Return to a normal activity level cannot be expected within 4 to 6 weeks, which is the time frame investigated in the abovementioned RCTs.
In all except 1 study,51 failure and healing rates indicated a beneficial effect of ACLR on meniscal repair (level 4 evidence). Therefore, the increased risk of repair failure in unstable knees should be considered, and performing meniscal repair in combination with an ACLR is recommended. A stable environment was also shown to benefit meniscal repair in a recent study,49 in which repair failure of medial meniscal tears decreased when rotatory laxity and residual pivot shift were resolved by reconstruction of the anterolateral ligament in addition to ACLR. Interestingly, higher success rates have been reported for meniscal repair in combination with ACLR than for meniscal repair in stable knees.23,35 Different causes for this observation can be hypothesized. The type of meniscal injury that occurs in combination with ACLR could be more amenable to repair. Alternatively, the healing could be improved owing to biological factors released from the drill holes at ACLR.13,15 Moreover, rehabilitation after ACLR could be more effective and protective of the knee compared with rehabilitation after isolated meniscal repair. The importance of knee stability has been underlined in recent studies that showed comparable healing rates of repaired and untreated stable ramp lesions when ACLR was performed.33,53 Interestingly, all unhealed menisci had a remaining instability of more than 3 mm side-to-side difference after ACLR.33 Moreover, a recent meta-analysis emphasized the role of the meniscus in knee stability, reporting that ACLR with concomitant meniscal repair reduced anterior knee joint laxity compared with ACLR with meniscectomy.46
Limitations
The best available literature has considerable methodological limitations. Because of the lack of standardized and randomized studies and the abundance of low-quality studies, there were several choices to be made. To minimize the risk of bias, we chose to exclude retrospective studies correlating the incidence of meniscal injury with the timing of ACLR. The possible bias in these studies is confirmed by studies that report meniscal injury in patients undergoing early, delayed, or no ACLR,11,18 in which the incidence of meniscal injury is higher in the delayed group than in the nonoperative group. Moreover, if the follow-up duration after surgery is limited, the follow-up times are different between the early and delayed groups, and some of the patients undergoing early ACLR might develop meniscal lesions after this follow-up, which was also shown in the literature.7,25,30,41
The difference in initial meniscal treatment between patients treated with early ACLR compared with nonoperatively treated patients is an important confounder to consider. Increased early-phase meniscal treatment (during ACLR) was shown to decrease late-phase meniscal surgery in 2 studies.20,37 However, few studies distinguished between early- and late-phase meniscal treatment, making it difficult to estimate the effect of this confounder. In an ongoing prospective cohort study,31 a subgroup of patients will undergo multiple MRI scans during a 2-year follow-up period. Results of this study will show the effect of ACLR on meniscal injury in time.
We chose to include all available techniques for ACLR and meniscal repair and did not differentiate between different types of meniscal injury. This could limit the comparability of the studies and explain contradicting findings. However, by using this inclusive approach, we were able to evaluate a broad section of the existing literature. Unfortunately, based on the available literature, it was not possible to perform a meta-analysis. Furthermore, the literature comparing early and delayed ACLR was limited and susceptible to bias.
Although subject to substantial limitations, this is the first comprehensive review that accounts for bias in this field of research. Even though we were not able to draw firm conclusions on all topics, by thoroughly reviewing the current literature we were able to identify the most important questions for future research.
Conclusions and Implications for Future Research
ACLR provides protective effects for subsequent meniscal injury (level 2 evidence). This should be confirmed in an RCT comparing ACLR versus nonoperative treatment. Such an RCT should monitor and report meniscal injury and treatment (meniscal repair or meniscectomy) at the early phase as well as during follow-up in order to differentiate between preexisting and subsequent meniscal injury. Additionally, meniscal treatment should be standardized in trials comparing ACLR and nonoperative treatment, to prevent differences in meniscal treatment at baseline. These trials should attempt to include a good representation of the patient population, including competitive athletes.
If ACLR is performed, it is recommended that this take place within 3 months of injury (level 3). Because of the limited and low quality of current evidence, the effect of timing of ACLR on subsequent meniscal injury should be investigated in a randomized study. It is important to investigate a clinically relevant delay, in which patients are likely to return to normal activity levels. Patients in both treatment groups should undergo the same postoperative rehabilitation and should be comparable in terms of activity levels and preoperative laxity.
Meniscal repair failure is higher in ACL-deficient knees (level 3 evidence), and surgeons and patients should be aware of this risk. The effect of ACLR without meniscal repair should be investigated for stable meniscal injury.
Appendix 1
Screening Criteriaa
| Title/abstract screening |
| Exclusion criteria |
| - Language other than English |
| - No primary ACLR |
| - Case reports describing a single patient |
| - No adult patients |
| - Cadaveric studies |
| - Finite element analysis |
| Full-text screening |
| Exclusion criteria |
| - Language other than English |
| - No primary ACLR |
| - Case reports describing a single patient |
| - No adult patients |
| - Cadaveric studies |
| - Finite element analysis |
| Inclusion criteria |
| - Articles describing both nonoperative treatment and ACLR for ACL rupture and |
| ○ Reporting rates of meniscal injury or |
| ○ Reporting rates of healing, reoperation, rerupture, or tear worsening of meniscal tears |
| - Articles describing different time points of ACLR and |
| ○ Reporting rates of meniscal injury and |
| ▪ Prospective study or |
| ▪ Retrospective study including nonoperative group or |
| ▪ Retrospective study assessing meniscal injury at 2 time points |
aACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction.
Appendix 2
Table A1.
Does ACLR Protect the Meniscus From Subsequent Injury?a
| Lead Author | n | Study Design | ACL Treatment | Meniscal Injury | Meniscal Treatment | Timing of Treatment (Range) | Follow-up Duration (Range) | Outcome | |
|---|---|---|---|---|---|---|---|---|---|
| Nonoperative Treatment | ACLR | ||||||||
| Frobell,20 Snoeker48 | 121 | RCT | BPB; 4S-HT (G+ST) | NS | Partial resection or fixation | <10 wk | 2 y (Frobell); 5 y (Snoeker) |
Baseline: 15 partial resection, 6 fixation 2-y follow-up: 26 partial resection, 3 fixation 5-y follow-up: new or worsening meniscal damage, 53%; delayed ACLR, 51% |
Baseline: 24 partial resection, 10 fixation 2-y follow-up: 5 partial resection, 1 fixation 5-y follow-up: new or worsening meniscal damage 45% |
| Meunier,38 Andersson,3 Andersson,4 Odesten40 | 94 | RCT | Nonsurgical, repair; augmented repair | NS | Meniscectomy or repair | NS | 14-19 y | 18/52 meniscal injury; 42% meniscectomy (intention to treat); 50% delayed ACLR | 5/42 meniscal injury; 29% meniscectomy (intention to treat) |
| Dunn17 | 6576 | Retrospective | ACLR, nonoperative | Medial, lateral, or any meniscal injury | NS | <6 or >6 wk (initial nonsurgical) | Median 29.5 mo | 56% reduction lateral meniscal reoperation; 42% medial meniscal reoperation | |
| Kessler28 | 109 | Retrospective | BPB, nonoperative | NS | NS | NS | 11.1 y (7.5-16.3 y) | 18/68 reoperations for meniscal injury | 7/68 reoperations for meniscal injury |
| Meuffels37 | 50 | Case-control | BPB, nonoperative | NS | Meniscectomy | >6 mo (2-258 mo) | 10 y | 80% meniscectomy, 40% during late phase | 68% meniscectomy; 12% meniscectomy post-ACLR |
| Fithian18 | 209 | Prospective | Early ACLR (mid-third patellar tendon autograft) or nonoperative | NS | Repair or partial meniscectomy | <3 mo | 6.6 y |
Early phase: 5/46 meniscectomy and 2/46 repair Late phase: 1 meniscectomy 16 delayed ACLR → 9/16 meniscectomy, 3/16 meniscal repair |
3/26 repair; 4/26 meniscectomy; 1 repair and 1 revision ACLR |
| Daniel11 | 236 | Prospective | ACLR (not further specified), nonoperative | NS | Early repair recommended | <90 or >90 d | 46-113 mo | 38/191 (20%) meniscal surgery; 44/191 late ACLR (27/44 meniscal injury) | Early ACLR: 2/45 (4%) late-phase meniscal surgery |
| Sanders45 | 1928 | Retrospective | BPB autograft, HT autograft, allograft, nonoperative | New meniscal tear | Meniscectomy or repair | <1 vs >1 y | 13.7 y (2 mo to 25 y) | 37.4% secondary meniscal injury |
Early ACLR: 6.1% secondary meniscal injury Delayed ACLR: 19.8% secondary meniscal injury |
| Hagmeijer22 | 1398 | Retrospective | ACLR (not further specified), nonoperative | Subsequent meniscal injury | Meniscectomy, repair, nonoperative | <6 or >6 mo | 2 y minimal | 19% meniscal injury |
Early ACLR: 7% Delayed ACLR: 33% |
aFrobell20 and Snoeker48; and Meunier,38 Andersson,3,4 and Odesten40 are combined as these studies describe data obtained from the same patient group and clinical trial. 4S-HT, 4-strand hamstring tendon; ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; BPB, bone–patellar tendon–bone; G, gracilis; HT, hamstring tendon; NS, not specified; RCT, randomized controlled trial; ST, semitendinosus tendon.
Table A2.
Does Early ACLR Reduce Secondary Meniscal Injury Compared With Delayed ACLR?a
| Lead Author | n | Study Design | ACL Treatment | Meniscal Injury | Meniscal Treatment | Timing of Treatment | Follow-up Duration | Outcome | |
|---|---|---|---|---|---|---|---|---|---|
| Early ACLR | Delayed ACLR | ||||||||
| Bottoni6 | 69 | RCT | 4S-HT (G+ST) | Medial, lateral | Repair (inside-out) or debridement | <3 wk or >6 wk | 165-869 d |
Medial: 23.5% repair, 17.7% meniscectomy Lateral: 52.9% meniscectomy |
Medial: 11.4% repair, 31.5% meniscectomy Lateral: 0.1% repair, 25.6 meniscectomy |
| Raviraj43 | 105 | RCT | 4S-HT (G+ST) | Medial, lateral | Debridement, partial excision | <2 wk or 4-6 wk | 26 mo |
Medial: 18 meniscal injuries Lateral: 20 meniscal injuries |
Medial: 13 meniscal injuries Lateral: 22 meniscal injuries |
| Herbst24 | 206 | Prospective | Anatomic single-bundle with autologous HT graft | NS | Meniscal repair, meniscectomy | <48 h vs after 3 mo rehabilitation | 24 mo | 23.3% meniscal repair failure | 16.7% meniscal repair failure |
| Foster19 | 75 | Retrospective | 4S-HT | NS | Partial or total meniscectomy, repair | <6 mo or >6 mo between arthroscopy and ACLR | Until surgery | 16% deterioration; 62.9% of deteriorations were meniscal tears | 63% deterioration |
| Yoo54 | 31 | Retrospective | Autologous BPB or 4S-HT | Medial meniscal injury | Arthroscopic all-inside suture | >12 mo after injury | Mean 49.9 mo |
First MRI: 55% meniscal tear Second MRI (average 36 mo later): 84% meniscal tear 42% deterioration of tears (no tear → tear; longitudinal → bucket handle) |
|
| De Roeck14 | 68 | Retrospective | PT autograft, HT | NS | NS | Mean injury to arthroscopy: 10.1 mo; mean time to ACLR: 13.2 mo | Until surgery | Diagnostic arthroscopy: 63.2% tear During ACLR: 73.5% |
|
a4S-HT, 4-strand hamstring tendon; ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; BPB, bone–patellar tendon–bone; G, gracilis; HT, hamstring tendon; MRI, magnetic resonance imaging; NS, not specified; PT, patellar tendon; RCT, randomized controlled trial; ST, semitendinosus tendon.
Table A3.
Does ACLR Protect the Repaired Meniscus?a
| Lead Author | n | Study Design | ACL Treatment | Meniscal Injury | Meniscal Treatment | Timing of Treatment | Follow-up Duration (Range) | Outcome | |
|---|---|---|---|---|---|---|---|---|---|
| ACL-Deficient | ACLR | ||||||||
| van der Wal52 | 238 | Retrospective | Nonoperative, concomitant ACLR, postponed ACLR; autologous 4S-HT (G+ST) | NS | Repair | <2 wk, 2-12 wk, and >12 wk | Median 41 mo | 100% failure of meniscal repair (3/3) |
Concomitant: 20.4% failure Postponed ACLR: 33.3% failure Intact ACL: 31.7% failure |
| Majeed36 | 136 | Retrospective | Nonoperative, concomitant ACLR, postponed ACLR | Medial, lateral | All-inside with FasT-Fix anchors | Repair <6 wk of injury; ACLR concomitant/delayed >6 wk | Mean 9 mo (1-26) |
Concomitant: 14.5% failure of repair Postponed ACLR: 27% failure of meniscal repair |
|
| Gallacher21 | 172 | Retrospective | Delayed ACLR, concomitant ACLR, nonoperative; HT and PT | NS | All-inside (clear fix, or FasT-fix, or ultrafast fix) | Delayed group ACLR 2.8 mo after meniscal repair |
Delayed: mean 6.1 y Concomitant: 5.4 y |
50% success rate | 72% success rate |
| Albrecht-Olsen1 | 68 | RCT | NS | Longitudinal vertical meniscal tears (bucket handle, displaced, or in situ) | Inside-out vs meniscal arrow (all-inside) | <2 mo to >1 y | Repeat arthroscopy after 3-4 mo | 12/19 healed | 18/19 healed |
| Plasschaert42 | 51 | Retrospective | Concomitant ACLR, delayed, nonoperative; BPB | Meniscal lesion in conjunction with ACL tear | Outside-in | <14 d or 14 d to 1 y | 3.5 y | 1/5 failure | 1/8 failure ACL intact: 3/6 failure |
| Kimura29 | 46 | Retrospective | ACLR, nonoperative | Vertical tear (longitudinal part shorter than 2 cm) | Suture, peripheral vascular stimulation, synovial pedicle flap | Mean 15 mo | Repeat arthroscopy 2-30 mo after surgery | 1/5 healed | 26/26 healed ACL intact: 11/15 healed |
| Valen51 | 57 | Retrospective | Concomitant ACLR, earlier ACLR, delayed ACLR; BPB | Medial, lateral, displaced bucket handle, posterior | Outside-in | NS | Mean 2 y | No detrimental effect of ACL deficiency | |
| Jensen26 | 49 | Retrospective | ACLR, nonoperative | Vertical unstable tears in outer third | Arthroscopic repair (inside-out) | <14 d or >14 d | Average 4.5 y (1-6.3) | 46% retear | 0% retear ACL intact: 11% retear |
| Austin5 | 101 | Retrospective | ACLR (PT allograft or autograft), nonoperative | Longitudinal tears within 5 mm of the meniscosynovial junction >1 cm; symptoms on provocation and <1 cm lateral, medial | Inside-out (body and bucket handle) and outside-in (posterior tears) | >3 wk after injury | NS | 2 repair failure | Unclear |
a4S-HT, 4-strand hamstring tendon; ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; BPB, bone–patellar tendon–bone; G, gracilis; HT, hamstring tendon; NS, not specified; PT, patellar tendon; RCT, randomized controlled trial; ST, semitendinosus tendon.
Footnotes
Final revision submitted April 27, 2020; accepted May 11, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: This research was supported by the Dutch Arthritis Foundation (LLP-12 and LLP-22). L.A.V. is employed by CO.DON AG. A.J.K. has received research support from Aesculap/B.Braun, Ceterix, Exactech, Gemini Medical, and Histogenics; consulting fees from Arthrex, JRF Ortho, and Vericel; speaking fees from Arthrex; royalties from Arthrex; and honoraria from Vericel; is a board or committee member for the Musculoskeletal Transplant Foundation; and has stock/stock options in Responsive Arthroscopy. D.B.F.S. has received research support from JRF Ortho. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Albrecht-Olsen P, Kristensen G, Burgaard P, Joergensen U, Toerholm C. The arrow versus horizontal suture in arthroscopic meniscus repair: a prospective randomized study with arthroscopic evaluation. Knee Surg Sports Traumatol Arthrosc. 1999;7(5):268–273. [DOI] [PubMed] [Google Scholar]
- 2. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(2):275–281. [DOI] [PubMed] [Google Scholar]
- 3. Andersson C, Odensten M, Gillquist J. Knee function after surgical or nonsurgical treatment of acute rupture of the anterior cruciate ligament: a randomized study with a long-term follow-up period. Clin Orthop Relat Res. 1991;264:255–263. [PubMed] [Google Scholar]
- 4. Andersson C, Odensten M, Good L, et al. Surgical or non-surgical treatment of acute rupture of the anterior cruciate ligament: a randomized study with long-term follow-up. J Bone Joint Surg Am. 1989;71(7):965–974. [PubMed] [Google Scholar]
- 5. Austin KS, Sherman OH. Complications of arthroscopic meniscal repair. Am J Sports Med. 1993;21(6):864–869. [DOI] [PubMed] [Google Scholar]
- 6. Bottoni CR, Liddell TR, Trainor TJ, Freccero DM, Lindell KK. Postoperative range of motion following anterior cruciate ligament reconstruction using autograft hamstrings: a prospective, randomized clinical trial of early versus delayed reconstructions. Am J Sports Med. 2008;36(4):656–662. [DOI] [PubMed] [Google Scholar]
- 7. Bray RC, Dandy DJ. Meniscal lesions and chronic anterior cruciate ligament deficiency: meniscal tears occurring before and after reconstruction. J Bone Joint Surg Br. 1989;71(1):128–130. [DOI] [PubMed] [Google Scholar]
- 8. Cinque ME, Dornan GJ, Chahla J, Moatshe G, LaPrade RF. High rates of osteoarthritis develop after anterior cruciate ligament surgery: an analysis of 4108 patients. Am J Sports Med. 2018;46(8):2011–2019. [DOI] [PubMed] [Google Scholar]
- 9. Cochrane Collaboration. The Cochrane Collaboration modified tool for assessing risk of bias for RCT. Accessed June 17, 2020 http://www.ncbi.nlm.nih.gov/books/NBK107306/bin/appd-fm1.pdf
- 10. Cost-effectiveness of two treatment strategies of an anterior cruciate ligament rupture: a randomized clinical study. Netherlands Trial Register ID: NTR2746 Updated May 24, 2019 Accessed April 27, 2020 https://www.trialregister.nl/trial/2618
- 11. Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med. 1994;22(5):632–644. [DOI] [PubMed] [Google Scholar]
- 12. Davis BR, Chen J, Inacio MCS, Love R, Prentice HA, Maletis GB. The incidence of subsequent meniscal surgery is higher in the anterior cruciate ligament-reconstructed knee than in the contralateral knee. Am J Sports Med. 2017;45(14):3216–3222. [DOI] [PubMed] [Google Scholar]
- 13. De Girolamo L, Galliera E, Volpi P, et al. Why menisci show higher healing rate when repaired during ACL reconstruction? Growth factors release can be the explanation. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):90–96. [DOI] [PubMed] [Google Scholar]
- 14. De Roeck NJ, Lang-Stevenson A. Meniscal tears sustained awaiting anterior cruciate ligament reconstruction. Injury. 2003;34(5):343–345. [DOI] [PubMed] [Google Scholar]
- 15. Dean CS, Chahla J, Matheny LM, Mitchell JJ, LaPrade RF. Outcomes after biologically augmented isolated meniscal repair with marrow venting are comparable with those after meniscal repair with concomitant anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(6):1341–1348. [DOI] [PubMed] [Google Scholar]
- 16. Dehaven KE. Diagnosis of acute knee injuries with hemarthrosis. Am J Sports Med. 1980;8(1):9–14. [DOI] [PubMed] [Google Scholar]
- 17. Dunn WR, Lyman S, Lincoln AE, et al. The effect of anterior cruciate ligament reconstruction on the risk of knee reinjury. Am J Sports Med. 2004;32(8):1906–1914. [DOI] [PubMed] [Google Scholar]
- 18. Fithian DC, Paxton EW, Stone ML, et al. Prospective trial of a treatment algorithm for the management of the anterior cruciate ligament-injured knee. Am J Sports Med. 2005;33(3):335–346. [DOI] [PubMed] [Google Scholar]
- 19. Foster A, Butcher C, Turner PG. Changes in arthroscopic findings in the anterior cruciate ligament deficient knee prior to reconstructive surgery. Knee. 2005;12(1):33–35. [DOI] [PubMed] [Google Scholar]
- 20. Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363(4):331–342. [DOI] [PubMed] [Google Scholar]
- 21. Gallacher PD, Gilbert RE, Kanes G, et al. Outcome of meniscal repair prior compared with concurrent ACL reconstruction. Knee. 2012;19(4):461–463. [DOI] [PubMed] [Google Scholar]
- 22. Hagmeijer MH, Hevesi M, Desai VS, et al. Secondary meniscal tears in patients with anterior cruciate ligament injury: relationship among operative management, osteoarthritis, and arthroplasty at 18-year mean follow-up. Am J Sports Med. 2019;47(7):1583–1590. [DOI] [PubMed] [Google Scholar]
- 23. Haklar U, Donmez F, Basaran SH, Canbora MK. Results of arthroscopic repair of partial- or full-thickness longitudinal medial meniscal tears by single or double vertical sutures using the inside-out technique. Am J Sports Med. 2013;41(3):596–602. [DOI] [PubMed] [Google Scholar]
- 24. Herbst E, Hoser C, Gfoller P, et al. Impact of surgical timing on the outcome of anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):569–577. [DOI] [PubMed] [Google Scholar]
- 25. Ichinohe S, Yoshida M, Murakami H, Takayama H, Izumiyama S, Shimamura T. Meniscal tearing after ACL reconstruction. J Orthop Surg (Hong Kong). 2000;8(1):53–59. [DOI] [PubMed] [Google Scholar]
- 26. Jensen NC, Riis J, Robertsen K, et al. Arthroscopic repair of the ruptured meniscus: one to 6.3 years follow up. Arthroscopy. 1994;10(2):211–214. [DOI] [PubMed] [Google Scholar]
- 27. Kaeding CC, Léger-St-Jean B, Magnussen RA. Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin Sports Med. 2017;36(1):1–8. [DOI] [PubMed] [Google Scholar]
- 28. Kessler MA, Behrend H, Henz S, Stutz G, Rukavina A, Kuster MS. Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc. 2008;16(5):442–448. [DOI] [PubMed] [Google Scholar]
- 29. Kimura M, Shirakura K, Hasegawa A, et al. Second look arthroscopy after meniscal repair: factors affecting the healing rate. Clin Orthop Relat Res. 1995;314:185–191. [PubMed] [Google Scholar]
- 30. Kobayashi K, Nakayama Y, Shirai Y, et al. Meniscal tears after anterior cruciate ligament reconstruction. J Nippon Med Sch. 2001;68(1):24–28. [DOI] [PubMed] [Google Scholar]
- 31. Kvist J, Gauffin H, Tigerstrand Grevnerts H, et al. Natural corollaries and recovery after acute ACL injury: the NACOX cohort study protocol. BMJ Open. 2018;8(6):e020543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Liu X, Zhang H, Feng H, Hong L, Wang X-S, Song G. Is it necessary to repair stable ramp lesions of the medial meniscus during anterior cruciate ligament reconstruction? A prospective randomized controlled trial. Am J Sports Med. 2017;45(5):1004–1011. [DOI] [PubMed] [Google Scholar]
- 34. Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35(10):1756–1769. [DOI] [PubMed] [Google Scholar]
- 35. Lyman S, Hidaka C, Valdez AS, et al. Risk factors for meniscectomy after meniscal repair. Am J Sports Med. 2013;41(12):2772–2778. [DOI] [PubMed] [Google Scholar]
- 36. Majeed H, Karuppiah S, Sigamoney KV, Geutjens G, Straw RG. All-inside meniscal repair surgery: factors affecting the outcome. J Orthop Traumatol. 2015;16(3):245–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Meuffels DE, Favejee MM, Vissers MM, et al. Ten year follow-up study comparing conservative versus operative treatment of anterior cruciate ligament ruptures: a matched-pair analysis of high level athletes. Br J Sports Med. 2009;43(5):347–351. [DOI] [PubMed] [Google Scholar]
- 38. Meunier A, Odensten M, Good L. Long-term results after primary repair or non-surgical treatment of anterior cruciate ligament rupture: a randomized study with a 15-year follow-up. Scand J Med Sci Sports. 2007;17(3):230–237. [DOI] [PubMed] [Google Scholar]
- 39. OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence. Oxford Centre for Evidence-Based Medicine. Accessed June 17, 2020 http://www.cebm.net/index.aspx?o=5653
- 40. Odensten M, Hamberg P, Nordin M, Lysholm J, Gillquist J. Surgical or conservative treatment of the acutely torn anterior cruciate ligament: a randomized study with a short-term follow-up. Clin Orthop Relat Res. 1985;198:87–93. [PubMed] [Google Scholar]
- 41. Orfaly RM, McConkey JP, Regan WD. The fate of meniscal tears after anterior cruciate ligament reconstruction. Clin J Sport Med. 1998;8(2):102–105. [DOI] [PubMed] [Google Scholar]
- 42. Plasschaert F, Vandekerckhove B, Verdonk R. A known technique for meniscal repair in common practice. Arthroscopy. 1998;14(8):863–868. [DOI] [PubMed] [Google Scholar]
- 43. Raviraj A, Anand A, Kodikal G, et al. A comparison of early and delayed arthroscopically-assisted reconstruction of the anterior cruciate ligament using hamstring autograft. J Bone Joint Surg Br. 2010;92(4):521–526. [DOI] [PubMed] [Google Scholar]
- 44. Ruano JS, Sitler MR, Driban JB. Prevalence of radiographic knee osteoarthritis after anterior cruciate ligament reconstruction, with or without meniscectomy: an evidence-based practice article. J Athl Train. 2017;52(6):606–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Sanders TL, Kremers HM, Bryan AJ, et al. Is anterior cruciate ligament reconstruction effective in preventing secondary meniscal tears and osteoarthritis? Am J Sports Med. 2016;44(7):1699–1707. [DOI] [PubMed] [Google Scholar]
- 46. Sarraj M, Coughlin RP, Solow M, et al. Anterior cruciate ligament reconstruction with concomitant meniscal surgery: a systematic review and meta-analysis of outcomes. Knee Surg Sports Traumatol Arthrosc. 2019;27(11):3441–3452. [DOI] [PubMed] [Google Scholar]
- 47. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 48. Snoeker BA, Roemer FW, Turkiewicz A, Lohmander S, Frobell RB, Englund M. Does early anterior cruciate ligament reconstruction prevent development of meniscal damage? Results from a secondary analysis of a randomised controlled trial. Br J Sports Med. 2020;54(10):612–617. [DOI] [PubMed] [Google Scholar]
- 49. Sonnery-Cottet B, Saithna A, Blakeney WG, et al. Anterolateral ligament reconstruction protects the repaired medial meniscus: a comparative study of 383 anterior cruciate ligament reconstructions from the SANTI Study Group with a minimum follow-up of 2 years. Am J Sports Med. 2018;46(8):1819–1826. [DOI] [PubMed] [Google Scholar]
- 50. Sri-Ram K, Salmon LJ, Pinczewski LA, et al. The incidence of secondary pathology after anterior cruciate ligament rupture in 5086 patients requiring ligament reconstruction. Bone Joint J. 2013;95(1):59–64. [DOI] [PubMed] [Google Scholar]
- 51. Valen B, Molster A. Meniscal lesions treated with suture: a follow-up study using survival analysis. Arthroscopy. 1994;10(6):654–658. [DOI] [PubMed] [Google Scholar]
- 52. van der Wal RJP, Thomassen BJW, Swen J-WA, et al. Time interval between trauma and arthroscopic meniscal repair has no influence on clinical survival. J Knee Surg. 2016;29(5):436–442. [DOI] [PubMed] [Google Scholar]
- 53. Yang J, Guan K, Wang JZ, et al. Clinical study on the arthroscopic refreshing treatment of anterior cruciate ligament injury combined with stable medial meniscus ramp injury. J Musculoskelet Neuronal Interact. 2017;17(2):108–113. [PMC free article] [PubMed] [Google Scholar]
- 54. Yoo JC, Ahn JH, Lee SH, et al. Increasing incidence of medial meniscal tears in nonoperatively treated anterior cruciate ligament insufficiency patients documented by serial magnetic resonance imaging studies. Am J Sports Med. 2009;37(8):1478–1483. [DOI] [PubMed] [Google Scholar]