Abstract
Operating room (OR) traffic and door openings increase potential for air contamination in the OR and create distractions for surgical teams. A multidisciplinary intervention was developed among OR staff, surgical staff, vendors, radiology, and anesthesia and approved by the hospital system’s patient and quality safety department for implementation. Interventions included education, OR signage, and team-based accountability and behavioral interventions. After interventions were implemented, a second prospective, observational data collection was performed and compared to preintervention OR traffic. A total of 35 cases were observed over the 3-month period in the preintervention group; 42 cases were observed in the postintervention group. Average door openings per minute decreased by 22% (P = .0011) after intervention. All surgical groups excluding anesthesia had significant reductions in OR traffic following the intervention. Behavioral interventions that focus on education, awareness, and efficiency strategies can decrease overall OR traffic for orthopedic cases.
Keywords: operating room traffic, surgical site infections, hospital quality, interventions
Unnecessary operating room (OR) traffic has been identified as a potential source for a variety of patient safety factors, quality concerns, and infectious risks.1–3 For example, a positive correlation between total colony forming units (CFUs) per operation on culture plates and OR air contamination exists with total room traffic flow (door openings and number of persons present).1,2,4 This has the potential to increase the risk of surgical site infections (SSIs).
This increase in CFUs may, in turn, increase SSI risk. OR traffic also creates additional noise and potential distraction that may lead to minor or even potentially catastrophic clinical care errors.5–7 Collectively, OR traffic has the potential to critically affect patient safety and quality outcomes.
Numerous studies have identified OR traffic as a potential quality and patient safety threat as well as an infectious risk and have implemented interventions to decrease OR traffic through education, communication technology, and physical deterrents.8–10 For example, Esser et al8 demonstrated a significant decrease in door openings after implementation of an education and process change project using an intercom system for staff communication. Other authors have targeted OR room traffic using pull shades on OR windows, yellow magnetic caution tape on OR doors, door alarms, and covers for case carts—all in an effort to decrease room traffic and potential infectious and patient safety risks.9,10
Room traffic in orthopedic surgery, specifically, raises several additional concerns as it relates to infectious risk and distraction. First, implantation of foreign hardware is often a necessity in orthopedic cases. Unfortunately, foreign hardware implantation has been shown to be a significant infectious risk because of the potential to develop biofilm-related, deep surgical infections, potentially necessitating removal of hardware altogether for definitive eradication of infection.11–16 In addition, implantation of surgical hardware frequently necessitates additional people being present in the OR (implant vendors), and the addition of people may lead to increased room traffic and distraction, potentially increasing infectious risk.17,18 And although infections are rare—rates of 1.6% to 2.4% are commonly reported for hip and knee arthroplasty, respectively—when SSIs do occur in orthopedics, they can be devastating for the patient, surgeon, and health care system as a whole.19–21
The purpose of this study was to evaluate the effect of a safety and quality improvement (QI) effort to reduce room traffic during orthopedic surgery cases. The methods and interventions from a previously published OR room traffic study in orthopedics were used to inform the design of the safety and quality intervention as well as outcome measures used for the study.22 The Revised Standards for Quality Improvement Reporting Excellence (SQUIRE 2.0) were used to structure the interventions and results of the study.23
Methods
This study was given approval for exempt status by the study organization’s institutional review board. A pragmatic, before–after interrupted time series study design was used to assess room traffic outcomes after QI initiative implementation at a large, academic, metropolitan, level 1 trauma center between June 2015 and August 2016. Baseline data collection from June to August 2015 revealed that the average number of staff members in the OR was substantially higher than that reported at other institutions in the literature.22 Study QI interventions were implemented from August 2015 through June 2016 and consisted of the following: staff educational sessions, reduction in break frequency, creation of door entry/exit guidelines, educational brochure dissemination, and door labeling. It was hypothesized that through interventions targeting OR traffic, OR traffic rates would decrease by at least 10%. Conventional pre and post statistical analyses and interrupted time series analyses were performed to evaluate change in door openings per case, relative to the intervention implemented.
Baseline Data Collection (June to August 2015)
The types of cases observed included orthopedic trauma and adult reconstruction (arthroplasty). All cases included implantation of metallic hardware. Implanted hardware consisted of standard fracture fixation devices such as metal screws and pins, intramedullary rods/nails, and/or metal plates. Additionally, standard joint replacement components included plastic polymers and metal implants composed of cobalt-chromium and titanium. Operations observed were performed by 5 different fellowship-trained orthopedic surgeons (3 trauma, 2 arthroplasty).
Room traffic was reported as the number of door openings per minute and recorded by a trained human monitor. A door opening was recorded as any opening of the door for person passage (in or out of the OR) or for information exchange. Also, all doors that provided access to the OR were included in data collection and analysis because all traffic at any door may lead to potential contamination, air mixture, and distraction. Furthermore, each OR team member was classified into one of 5 groups that included perioperative staff (nurses and scrub technicians), surgical staff (surgeons, residents, and medical students), anesthesia staff (anesthesiologists, nurse anesthetists, medical students, and anesthesia techs), vendors (medical equipment representatives), and radiology (radiology technicians).
Intervention
In August 2015, strategic QI initiatives to decrease room traffic were established and implemented with perioperative staff, anesthesia staff, surgeons, radiology technicians, and medical equipment representatives. Three committees were formed among specific groups to disseminate initiative information related to OR traffic reduction: (1) perioperative staff (surgical technicians, circulating nurses, and other OR staff), (2) anesthesia staff, and (3) surgical staff, medical equipment representatives, and radiology technicians. As part of the intervention, each committee identified strategies and obstacles for room traffic reduction. Unnecessary OR behavior and processes also were identified.
A practice guideline for room traffic reduction was implemented. The guideline consisted primarily of staff education concerning the potential risks associated with a high volume of OR traffic, decreasing staff break frequency, creating rules for door openings, and placing signs on the doors to remind people to open the door only if necessary. Another product of the intervention was the installation of electronic door counters (Enforcer Entry Alert System E-931CS22RRCQ, Seco-Larm, Irvine, CA) on the OR doors—a visual reminder to staff of how many times the doors had opened during the case. The door counters were not used as a means to collect data; rather, they served as a constant and real-time reminder to reduce room traffic. These electronic counters were installed as part of the study intervention and, thus, were present for the postintervention data collection period. They were retained during the entire postintervention data collection period but were not retained after the study data collection period completed.
Postintervention Data Collection
From June to August 2016, after the study intervention, OR traffic was observed in orthopedic trauma and arthroplasty procedures using the same methods described for the preintervention data collection.
Statistical Analysis
Statistical and data analyses were performed using STATA 14.0 (StataCorp LLC, College Station, Texas) and QI Charts (a control chart add-in for Microsoft Excel; Process Improvement Products, Austin, Texas). Unpaired, 2-sample Student t tests were used to compare pre-and postintervention groups. A multiple variable linear regression statistical methodology was considered for analysis but because of inadequate sample size, t tests with sub-group analysis were chosen instead. An α = 0.05 was considered statistically significant. Assuming 80% power and α = 0.05, a power analysis indicated that at least 35 cases per group were needed to detect a 10% difference in room traffic rate, the primary study outcome. In addition, interrater reliability values of >0.999 revealed that case observers achieved excellent intraclass correlation with respect to data collection. In addition, evaluation of stability of room traffic rate changes over time was evaluated using Shewhart’s individuals/moving-range control charts (also known as XmR Charts), which compared number of door openings per minute per case for the baseline period compared to the postintervention period. Control limits with ±3 SDs were calculated to identify special-cause variation with adjusted centerline and control limits in accordance with recommendations by Provost and Murray.24
Results
A total of 35 cases were included in the preintervention group, and 42 cases were included in the postintervention group. Case length was defined as sterile case cart opening until dressing placement as described by Patel et al.22 Overall, the mean case length (sterile case cart open to dressing placement) for the preintervention group was 219.1 minutes (SD = 70.6; range = 114–465) and was 206.6 minutes (SD = 52.3; range = 94–301) for the postintervention group (Supplemental Table 1, available with the article online).
The total door openings in the preintervention group were 124.3 openings per case (SD = 42.7, range = 48–220; Supplemental Table 1) and were 86.7 (SD = 22.2; range = 41–131) in the postintervention group. There was a statistically significant difference in room traffic rate (openings per minute) between pre (0.58 openings/min; SD = 0.16; range = 0.22–1.01) and post intervention (0.45 openings/min; SD = 0.17, range = 0.26–1.05, P = .0011; Supplemental Table 1, Figure 1).
Figure 1.
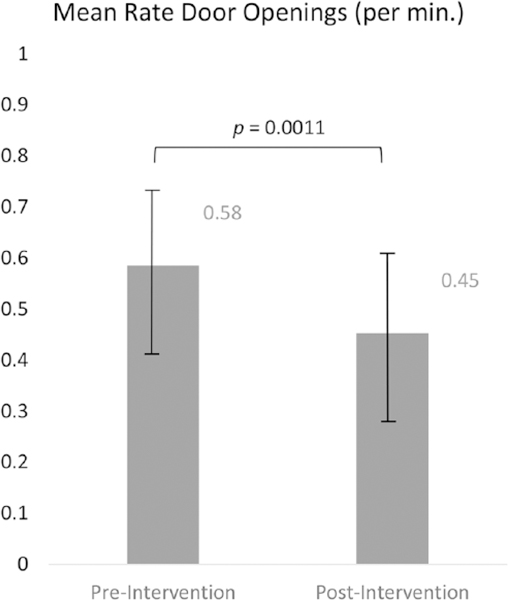
Bar chart indicating mean rate of door openings. Abbreviation: min, minute.
Time series analysis demonstrated that the total number of door openings per minute, per case, decreased immediately post intervention (Figure 2) from an average of 0.58 door openings per minute per case to 0.45 per minute per case. As indicated by the control limit changes in Figure 2, variability in the openings per minute per case also decreased. However, as indicated by the control chart centerline shifts and changes in the upper and lower control limits, there was a steady increase in the rate of door openings per minute per case the further out from the interventions, indicating a potential lack of sustainable improvement in rate of OR openings.
Figure 2.
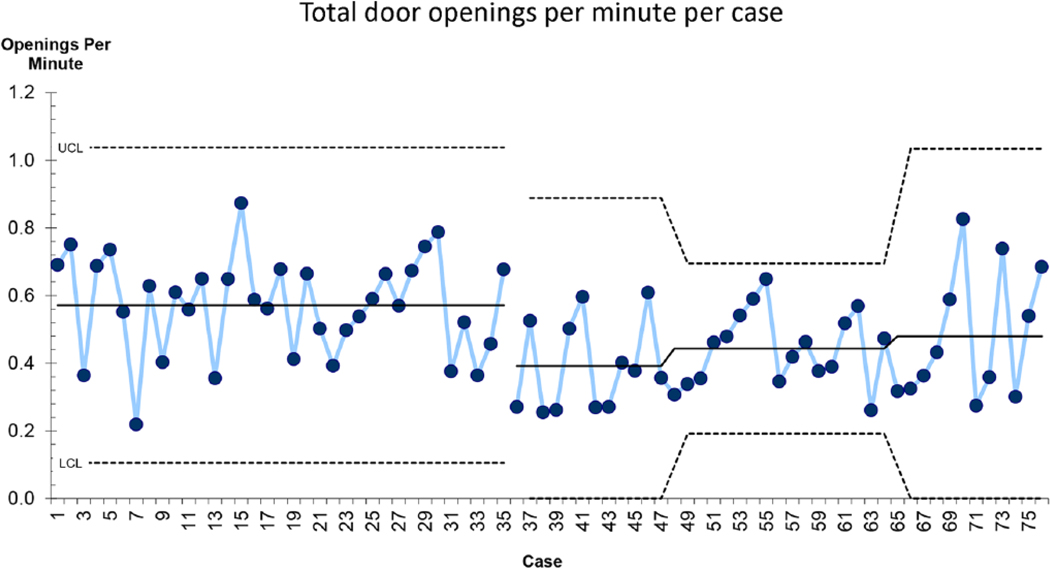
Shewart’s individual/moving-range control chart demonstrating the change in door openings over time. The gap in the time series demarcates the preintervention and postintervention cases. The downward shift post intervention indicates that a decrease in the rate of door openings was observed. The upward shifts in the postintervention time series indicate that although the rate was still lower than pre intervention, there was a steady increase in door openings as time progressed.
Pre Incision
In addition, room traffic was recorded and analyzed with respect to occurring before or after incision. The average preincision openings per minute decreased slightly from 0.76 (SD = 0.20) before the intervention to 0.72 (SD = 0.19) after the intervention. However, this difference was not statistically significant (Supplemental Table 2). Time series analysis demonstrated that after the intervention, there was a slight decrease in door openings per minute prior to incision early after the intervention (Figure 3). However, there was a steady upward trend in pre-incision door openings per minute per case further out from the interventions.
Figure 3.
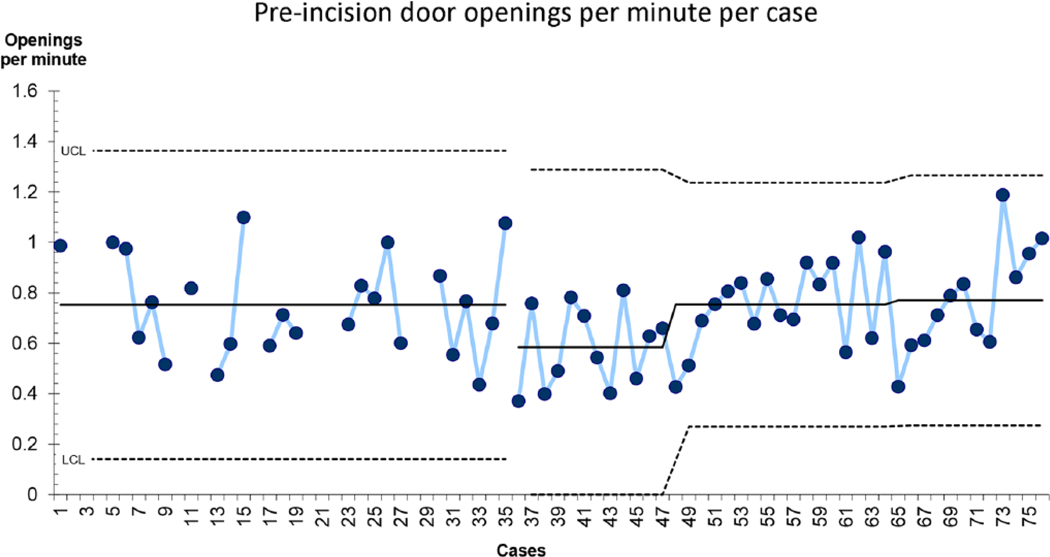
Shewart’s individual/moving-range control chart demonstrating the change in door openings over time. The gap in the time series demarcates the preintervention and postintervention cases. The downward shift post intervention indicates that a decrease in the rate of door openings was observed. The upward shifts in the post intervention time series indicate that although the rate was still lower than pre intervention, there was a steady increase in the door openings as time progressed.
Post Incision
Although pre-incision room traffic rates remained largely unchanged by the intervention, post-incision room traffic rates were significantly different when comparing average preintervention door openings of 0.41 (SD = 0.20) per minute to the postintervention average of 0.12 openings per minute (SD = 0.08, P < .0001; Supplemental Table 2). The time series analysis indicates that this post-incision change was evident both early after the intervention and in the later cases as well (Figure 4).
Figure 4.
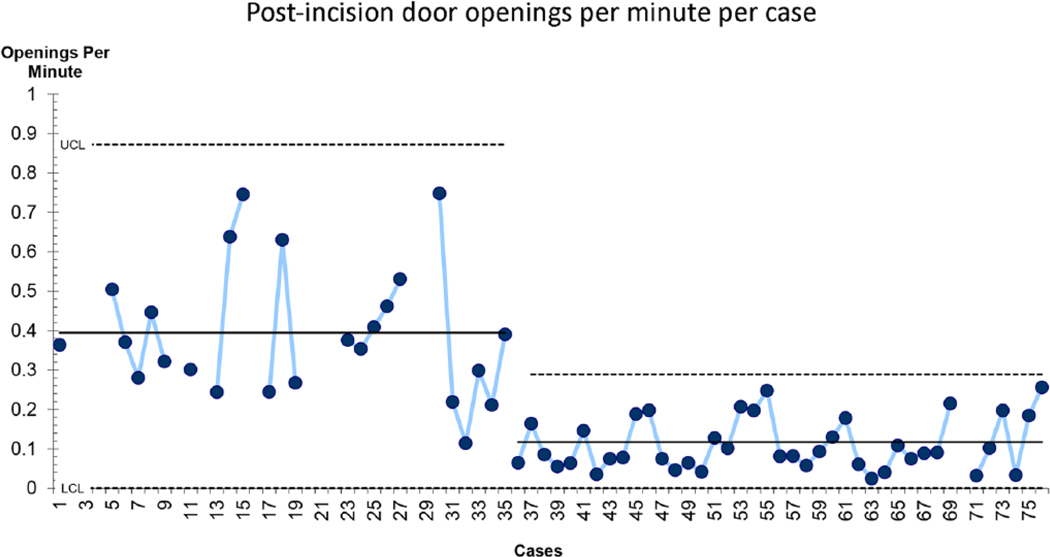
Shewart’s individual/moving-range control chart demonstrating the change in door openings over time. The gap in the time series demarcates the preintervention and postintervention cases. The downward shift post intervention indicates that a decrease in the rate of door openings was observed, and this shift was maintained through the planned observation period.
Surgical Team Group Comparisons
Finally, surgical team member roles were compared to identify if groups of OR members’ room traffic were influenced more or less by the study intervention. Nursing staff, surgical staff, vendor, and radiology team members all had significant reductions in postintervention room traffic when compared to preintervention traffic (Supplemental Table 3, Figure 5). Only the anesthesia team did not have a significant change in room traffic; that team had overall low room traffic prior to intervention strategies.
Figure 5.
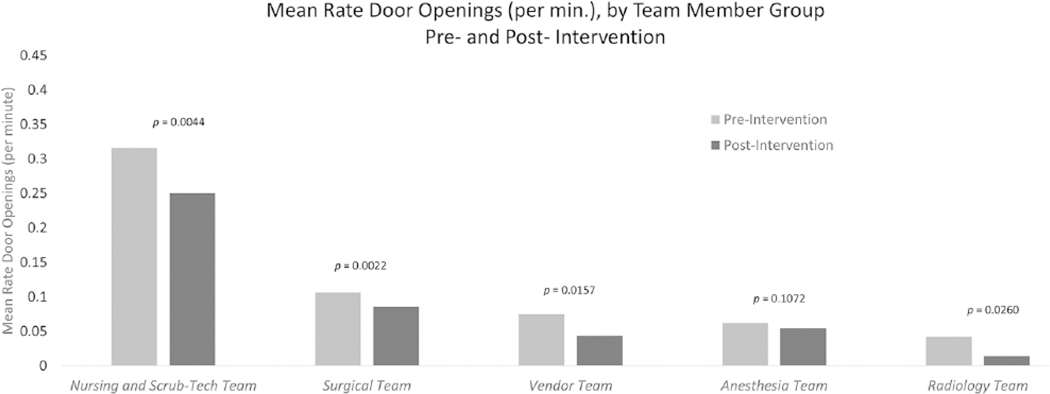
Bar chart indicating team member role room traffic rates.
Abbreviation: min, minute.
Discussion
Using a multidisciplinary QI initiative to lower room traffic during orthopedic implant cases was effective in reducing overall room traffic rates. There was a 22% decrease in overall mean number of door openings across all cases from pre intervention to post intervention. In addition, there were 37.6 fewer door openings per case, and a 71% decrease in the post-incision per minute door opening rates. In addition, time series analysis revealed a postintervention narrowing of the upper and lower control limits for room traffic patterns, representing a decrease in variation. This result indicates that the system as a whole came under tighter control with regard to OR traffic as a result of the intervention.
These results indicate that QI interventions related to OR behavior have the potential to significantly affect surgical personnel activity in the OR across many different OR team member roles and case types. Traditionally, the OR has been a difficult setting in which to implement behavioral changes; however, there is literature to inform behavioral change in such environments. For instance, multiple studies have evaluated factors that influence surgical team behaviors and found that many OR team members may hold dissimilar beliefs and goals related to which behaviors enhance teamwork in the OR.25–27 In addition, others have suggested that QI and awareness campaigns are vital to changing OR behavior as it relates to adherence to infection control practices in the OR.26,28 Moreover, despite differences in team dynamics, studies indicate that positive behavior change in the OR is possible.29,30
Even so, the time series analysis in the present study suggests that lasting behavior change may be difficult to maintain because reductions in some room traffic parameters lessened over time. These findings are consistent with other QI studies that note difficulties in sustaining lasting change in health care systems.31 In particular, interventions focusing on behavior change often rely on accountability and real-time feedback in order to maintain behavioral change.32 In the present study, the visual reminder of a human OR monitor may have given OR team members a greater awareness of room traffic practices post intervention and reinforced mindfulness of best practices. However, because incorporating a full-time, human OR monitor is impractical in the long term, additional research that explores automated auditing and feedback methods to sustain behavior change in the OR is currently under way. There are data to support the assertion that use of automated, real-time feedback in the OR may lead to more substantial behavior changes.33
It is important to note that several notable behavior modifications emerged as grassroots approaches that were not included in the specific planned interventions. For example, the OR monitors noted many door openings pertained to a need for supplies or information. Some surgical team members made an extra effort to anticipate and proactively address these needs prior to case start time, which may have substantially decreased their room traffic post incision. Additional organic strategies developed by OR team members included surgeon briefings for nurses and surgical techs on the specifics of the case, use of additional time-outs prior to opening the sterile case cart, and the creation of lists of anticipated supplies on OR whiteboards. Furthermore, given the elective nature of arthroplasty cases, the aforementioned “organic” techniques developed mostly during these case types and likely contributed to the more substantial postintervention reduction in room traffic during arthroplasty cases.
Limitations
The current study has several limitations. First, given the observational nature of the data collection and the behavioral changes expected, the study was subject to the Hawthorne Effect.34,35 It is possible that OR staff may have altered their behavior as a result of being observed by the data collector, and in cases where a human monitor was not present, OR traffic rates may not have improved. Although this effect has the potential to introduce bias, there was no indication that it did during data collection. Not all surgical staff members were aware of the purpose of the data collector in the OR, and the data collector attempted to remain unobtrusive and discrete. Furthermore, the data collector was present for collection of both baseline and intervention data, and therefore, any likely effects would have been equalized across pre-and postintervention data. Nonetheless, using automated monitoring of door openings in the future may eliminate biasing of the Hawthorne Effect by creating a context wherein all OR cases are monitored instead of a sample of cases.
Another limitation is the instability in OR traffic behavior change over time. Although data collected after the study intervention demonstrated initial stability in behavior changes, room traffic patterns demonstrated slow regression to preintervention states with the time series analysis. Future studies should explore different interventions to create more lasting awareness and behavioral modifications in the OR.
Finally, although conceptually OR room traffic has been linked to SSIs and surgical team distraction, the low rates of SSI in orthopedics and the complexity of measuring distraction were outside the scope of the current study. The primary focus of this study was to identify modifiable trends related to OR traffic and to implement QI initiatives to decrease room traffic behavior. Further research is needed to establish any potential link between room traffic behaviors, surgical team distractions, and SSIs.
Conclusions
Behavioral interventions that focus on education and raising awareness can create important behavior changes in OR traffic rates. Given that room traffic and door openings can contribute significantly to air contamination risk, this intervention may provide a simple and effective method for hospitals to modify their risk for SSIs. Behavior change sustainability, however, may necessitate generating the capacity for ongoing monitoring and feedback of behaviors.
Supplementary Material
Acknowledgments
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Footnotes
Declaration of Conflicting Interests
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Carmen E. Quatman and Laura S. Phieffer are con-sultants to Johnson & Johnson (New Brunswick, NJ, USA).
Supplemental Material
Supplemental material for this article is available online.
References
- 1.Andersson AE, Bergh I, Karlsson J, Eriksson BI, Nilsson K. Traffic flow in the operating room: an explorative and descriptive study on air quality during orthopedic trauma implant surgery. Am J Infect Control. 2012;40:750–755. [DOI] [PubMed] [Google Scholar]
- 2.Scaltriti S, Cencetti S, Rovesti S, Marchesi I, Bargellini A, Borella P. Risk factors for particulate and microbial contamination of air in operating theatres. J Hosp Infect. 2007;66:320–326. [DOI] [PubMed] [Google Scholar]
- 3.Mears SC, Blanding R, Belkoff SM. Door opening affects operating room pressure during joint arthroplasty. Orthopedics. 2015;38:e991–e994. [DOI] [PubMed] [Google Scholar]
- 4.Stauning MT, Bediako-Bowan A, Andersen LP, et al. Traffic flow and microbial air contamination in operating rooms at a major teaching hospital in Ghana. J Hosp Infect. 2018;99:263–270. [DOI] [PubMed] [Google Scholar]
- 5.Healey AN, Primus CP, Koutantji M. Quantifying distraction and interruption in urological surgery. Qual Saf Health Care. 2007;16:135–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cochran A, Elder WB. Effects of disruptive surgeon behavior in the operating room. Am J Surg. 2015;209:65–70. [DOI] [PubMed] [Google Scholar]
- 7.Wheelock A, Suliman A, Wharton R, et al. The impact of operating room distractions on stress, workload, and teamwork. Ann Surg. 2015;261:1079–1084. [DOI] [PubMed] [Google Scholar]
- 8.Esser J, Shrinski K, Cady R, Belew J. Reducing OR traffic using education, policy development, and communication technology. AORN J. 2016;103:82–88. [DOI] [PubMed] [Google Scholar]
- 9.Rovaldi CJ, King PJ. The effect of an interdisciplinary QI project to reduce OR foot traffic. AORN J. 2015;101:666–678; quiz 679–681. [DOI] [PubMed] [Google Scholar]
- 10.Eskildsen SM, Moskal PT, Laux J, Del Gaizo DJ. The effect of a door alarm on operating room traffic during total joint arthroplasty. Orthopedics. 2017;40:e1081–e1085. [DOI] [PubMed] [Google Scholar]
- 11.Swearingen MC, DiBartola AC, Dusane D, Granger J, Stoodley P. 16S rRNA analysis provides evidence of biofilms on all components of three infected periprosthetic knees including permanent braided suture. Pathog Dis. 2016;74:pii: ftw083. doi: 10.1093/femspd/ftw083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mavrogenis AF, Papagelopoulos PJ, Coll-Mesa L, Pala E, Guerra G, Ruggieri P. Infected tumor prostheses. Orthopedics. 2011;34:991–998; quiz 999–1000. [DOI] [PubMed] [Google Scholar]
- 13.Costerton JW, Post JC, Ehrlich GD, et al. New methods for the detection of orthopedic and other biofilm infections. FEMS Immunol Med Microbiol. 2011;61:133–140. [DOI] [PubMed] [Google Scholar]
- 14.McConoughey SJ, Howlin R, Granger JF, et al. Biofilms in periprosthetic orthopedic infections. Future Microbiol. 2014;9:987–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stoodley P, Conti SF, DeMeo PJ, et al. Characterization of a mixed MRSA/MRSE biofilm in an explanted total ankle arthroplasty. FEMS Immunol Med Microbiol. 2011;62:66–74. [DOI] [PubMed] [Google Scholar]
- 16.Kathju S, Nistico L, Hall-Stoodley L, Post JC, Ehrlich GD, Stoodley P. Chronic surgical site infection due to suture-associated polymicrobial biofilm. Surg Infect (Larchmt). 2009;10:457–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Salassa TE, Swiontkowski MF. Surgical attire and the operating room: role in infection prevention. J Bone Joint Surg Am. 2014;96:1485–1492. [DOI] [PubMed] [Google Scholar]
- 18.Birgand G, Saliou P, Lucet JC. Influence of staff behavior on infectious risk in operating rooms: what is the evidence? Infect Control Hosp Epidemiol. 2015;36:93–106. [DOI] [PubMed] [Google Scholar]
- 19.Edwards JR, Peterson KD, Mu Y, et al. National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008, issued December 2009. Am J Infect Control. 2009;37:783–805. [DOI] [PubMed] [Google Scholar]
- 20.Patzakis MJ, Zalavras CG. Chronic posttraumatic osteomyelitis and infected nonunion of the tibia: current management concepts. J Am Acad Orthop Surg. 2005;13: 417–427. [DOI] [PubMed] [Google Scholar]
- 21.Whitehouse JD, Friedman ND, Kirkland KB, Richardson WJ, Sexton DJ. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: adverse quality of life, excess length of stay, and extra cost. Infect Control Hosp Epidemiol. 2002;23:183–189. [DOI] [PubMed] [Google Scholar]
- 22.Patel PG, DiBartola AC, Phieffer LS, et al. Room traffic in orthopedic surgery: a prospective clinical observational study of time of day [published online November 4, 2017]. J Patient Saf. doi: 10.1097/PTS.0000000000000330 [DOI] [PubMed] [Google Scholar]
- 23.Revised Standards for Quality Improvement Reporting Excellence. SQUIRE 2.0. http://www.squire-statement.org/index.cfm?fuseaction=page.viewpage&pageid=471. Accessed June 8, 2018.
- 24.Provost L, Murray S. The Health Care Data Guide: Learning From Data for Improvement. New York, NY: Wiley; 2011. [Google Scholar]
- 25.Aveling EL, Stone J, Sundt T, Wright C, Gino F, Singer S. Factors influencing team behaviors in surgery: a qualitative study to inform teamwork interventions. Ann Thorac Surg. 2018;106:115–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoeper K, Kriependorf M, Felix C, Nyhuis P, Tecklenburg A. Role-specific targets and teamwork in the operating room [in German]. Anaesthesist. 2017;66:953–960. [DOI] [PubMed] [Google Scholar]
- 27.Prati G, Pietrantoni L. Attitudes to teamwork and safety among Italian surgeons and operating room nurses. Work. 2014;49:669–677. [DOI] [PubMed] [Google Scholar]
- 28.Dallolio L, Raggi A, Sanna T, et al. Surveillance of environmental and procedural measures of infection control in the operating theatre setting. Int J Environ Res Public Health. 2017;15:pii: E46. doi: 10.3390/ijerph15010046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Attarian DE, Wahl JE, Wellman SS, Bolognesi MP. Developing a high-efficiency operating room for total joint arthroplasty in an academic setting. Clin Orthop Relat Res. 2013;471:1832–1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hicks CW, Rosen M, Hobson DB, Ko C, Wick EC. Improving safety and quality of care with enhanced teamwork through operating room briefings. JAMA Surg. 2014;149:863–868. [DOI] [PubMed] [Google Scholar]
- 31.Huang J, Jiang D, Wang X, et al. Changing knowledge, behavior, and practice related to universal precautions among hospital nurses in China. J Contin Educ Nurs. 2002;33:217–224. [DOI] [PubMed] [Google Scholar]
- 32.Al-Tawfiq JA, Abed MS, Al-Yami N, Birrer RB. Promoting and sustaining a hospital-wide, multifaceted hand hygiene program resulted in significant reduction in health care-associated infections. Am J Infect Control. 2013;41:482–486. [DOI] [PubMed] [Google Scholar]
- 33.Vigoda MM, Lubarsky DA. The medicolegal importance of enhancing timeliness of documentation when using an anesthesia information system and the response to automated feedback in an academic practice. Anesth Analg. 2006;103:131–136. [DOI] [PubMed] [Google Scholar]
- 34.Sedgwick P, Greenwood N. Understanding the Hawthorne effect. BMJ. 2015;351:h4672. [DOI] [PubMed] [Google Scholar]
- 35.Chen LF, Vander Weg MW, Hofmann DA, Reisinger HS. The Hawthorne effect in infection prevention and epidemiology. Infect Control Hosp Epidemiol. 2015;36: 1444–1450. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


