Abstract
Lesbian, gay, bisexual, and transgender (LGBT) youth are at elevated risk for self-injurious thoughts and behaviors (SITBs). However, few studies have comprehensively examined SITBs and their longitudinal course in LGBT youth at high risk for suicide. The aims of the present study were to characterize histories of SITBs among high-risk LGBT youth and to examine prospective associations with suicidal behavior. Participants were 285 youth (41.8% LGBT) ages 13–25 years receiving psychiatric emergency department (ED) services. Post-discharge suicidal behavior was assessed via 4-month phone interviews and 12 month chart reviews. The sample was 42.1% male, 57.9% female, 2.5% gender minority, 41.8% sexual minority. LGBT participants were more likely to have prior psychiatric ED visits and hospitalizations, more frequent past week suicide ideation, and more severe nonsuicidal self-injury (NSSI). We conducted stratified survival analyses to identify predictors of time to suicidal behavior post discharge. The final model for LGBT youth included past week suicide ideation and past month NSSI episodes. Among non-LGBT youth, the final model included number of lifetime NSSI methods and use of a highly lethal suicide attempt method. Within this sample of youth receiving psychiatric emergency services, LGBT youth were overrepresented and had more severe histories of SITBs. Results suggest the importance of assessing both lifetime and recent factors (i.e., past week and month), particularly for LGBT youth. Future research should replicate these findings in larger samples to explore whether there are unique risk factors that can aid in predicting and preventing suicide among LGBT youth.
Introduction
Suicide consistently ranks among the leading causes of death for young people worldwide (Global Burden of Disease Pediatrics Collaboration, 2016). Converging epidemiological evidence from several countries indicates that lesbian, gay, bisexual, and transgender (LGBT) individuals are more likely to consider, attempt, and die by suicide than heterosexual and cisgender peers (Björkenstam et al., 2016; Haas et al., 2010; McNeil et al., 2017; Miranda-Mendizábal et al., 2017). Despite ample evidence of disparities, little is known about the developmental course of self-injurious thoughts and behaviors (SITBs) in this population, due largely to the paucity of longitudinal research. A recent review of 50 years of longitudinal suicide research found that 1.9% of studies reported LGBT status (Cha et al., 2018). Prospective research is crucial to advancing our understanding of why some LGBT youth attempt suicide whereas most do not.
Research innovations are needed in several key areas. First, longitudinal risk factors for suicidal behavior should be examined among LGBT youth. Previous research has examined general correlates (e.g., hopelessness, internalizing symptoms, alcohol use) and population-specific correlates (e.g., LGBT-related victimization and gender nonconformity; Miranda-Mendizábal et al., 2017). However, only one published study to date has examined longitudinal predictors of suicide attempts among LGBT youth specifically (Mustanski and Liu, 2013). In a community sample of 237 LGBT youth, a past attempt was the only predictor of future attempts over a one-year follow-up period (Mustanski and Liu, 2013). Given higher rates of suicidal behavior and risk factors, research should examine whether longitudinal predictors differ as well.
Second, the severity of suicide attempt history and related SITBs should be comprehensively assessed. Suicide risk among LGBT youth has frequently been operationalized as self-reported history of any attempt, often using measures with unknown predictive validity (di Giacomo et al., 2018; Savin -Williams, 2001). Markers of SITB severity, such as duration of suicidal thoughts, are prospectively associated with future attempts (Gipson et al., 2015; Horwitz et al., 2015; Ribeiro et al., 2016). Highly lethal and violent attempt methods (e.g., hanging, jumping from a height, or use of a firearm) account for the majority of youth suicide deaths globally (Glenn et al., 2019), are more likely to be fatal during a first attempt (McKean et al., 2018), and are more predictive of future deaths than other common methods such as overdose (Beckman et al., 2018). Retrospective data suggest that these features may be more prevalent, severe, and chronic among LGBT individuals (Fox et al., 2018). Recently developed instruments, such as the Columbia Suicide Severity Rating Scale (C-SSRS), are relatively brief in administration, demonstrate predictive validity, and may aid in characterizing risk trajectories (Posner et al., 2011).
Finally, the low prevalence of suicidal behavior presents challenges in longitudinal research (Franklin et al., 2017; King et al., 2018). As treatment history is a relatively strong predictor of suicidal behavior (Franklin et al., 2017), targeted recruitment in clinical settings could enhance the feasibility of examining prospective relationships with suicidal behavior outcomes. Emergency departments (EDs) are conducive to identifying youth at high risk for suicide, and visits to pediatric EDs for suicide-related reasons have been increasing for the past decade (Babeva et al., 2016; Carubia et al., 2016). LGBT individuals report frequent use of ED services and may be overrepresented among ED patients at risk for suicide (Arias et al., 2016; Asarnow et al., 2017; Currier et al., 2015; Sánchez et al., 2007). In a recent longitudinal study of 2,104 adolescents receiving pediatric ED services, LGBT youth comprised 30.5% of the sample and 58.7% of youth who attempted or died by suicide at 3-month follow-up (King et al., 2019). Thus, characterizing suicide risk among LGBT youth receiving ED services represents a crucial avenue for future research.
LGBT youth experience higher rates of suicidal ideation and behavior. However, few studies have comprehensively examined severity of suicidal ideation and behavior and longitudinal associations with future risk. The current study utilized a purposive sample of LGBT youth receiving psychiatric ED services. The aims were two-fold. First, we sought to characterize SITBs among LGBT youth. Second, we examined which SITBs were associated with suicidal behavior within one year of discharge.
Method
Participants and procedures
Participants were 285 adolescents and young adults ages 13–25 years (mean [SD] = 18.0 [3.5]) recruited from patients receiving psychiatric emergency services at a large Midwestern university hospital between June 2014 and January 2015. At triage, patients were assessed for the type of presenting clinical concern (e.g., medical, injury, psychiatric). All individuals reporting a psychiatric chief complaint were routed to psychiatric emergency services within the ED. Among those patients, individuals ages 13 to 25 were assessed for potential eligibility for this study. Exclusion criteria included cognitive impairment, alcohol/substance intoxication, mania, psychosis, and agitation. Among eligible individuals, 79.7% provided informed written assent or consent to participate in this IRB-approved study that included a follow-up phone interview. Adolescents were informed that their responses on self-report measures were confidential and would not be shared with their parents. There were no differences in demographic characteristics or reasons for visit between eligible participants who did and did not consent to the study (χ2 values < 3, p-values > .10). The sample was 42.1% male, 57.9% female, 2.5% gender minority, 41.8% sexual minority. The racial distribution was as follows: 77% Caucasian, 10% African American/Black, 4% Asian, 3% Hispanic, and 6% multiracial. Most (n = 204, 71.6%) presented to the ED for suicide ideation or attempt. Other common reasons for the ED visit included anxious and/or depressive symptoms (n = 38, 13.3%), aggressive behavior (n = 16, 5.6%), or a psychiatric evaluation (n = 13, 4.6%). A total of 226 participants (79.3% retention) completed a 4-month follow-up phone interview. For adolescents, caregivers were contacted prior to phone interviews to confirm their availability in the case of safety concerns (e.g., current suicide ideation with intent reported on the C-SSRS). There were no demographic or clinical differences between participants who did and did not complete the phone interview.
Patient data from psychiatric ED visits were extracted from electronic medical records at the index visit. Data were obtained for participants’ race/ethnicity, natal sex, reason for psychiatric ED visit, number of past psychiatric ED visits and hospitalizations, and history of SITBs. Records were also reviewed to obtain SITB information from return visits within 12 months following the index visit.
Measures
LGBT status.
Participants were asked “Which of the following do you identify most closely with? Check all that apply.” Response options included heterosexual, mostly heterosexual (straight), mostly gay or lesbian, gay or lesbian, bisexual, pansexual, asexual, demisexual, queer, unlabeled, not sure, and other (free response). They were also given two items adapted from the Youth Risk Behavior Survey (Brener et al., 2004), “To whom have you had a romantic attraction” and “With whom have you had sexual contact?”. Response options include male, female, both, or neither.
Gender nonconformity.
Gender nonconformity before age 12 years was assessed retrospectively using 6 items from the Recalled Childhood Gender Identity/Gender Role Questionnaire (Zucker et al., 2006). The two-subscale questionnaire assesses gender identity and parent-child relations, with example items such as preferred toys and games and identification or admiration of characters on TV or in movies. Responses are rated on a 5-point scale from 1 (Always “feminine”/ always girls or women) to 5 (Always “masculine”/always boys or men). Responses include variations of a neutral option (e.g. neither “masculine” nor “feminine”). In the initial sample for which this scale was developed, Cronbach’s α was .92 for the gender role subscale.
Interpersonal victimization.
Past experiences with victimization were assessed using 5 items from the victimization subscale of the Peer Experiences Questionnaire (Prinstein et al., 2001). Each scale assesses the frequency of recent experiences of overt and relational aggression. The victimization subscale has good internal consistency (α = 0.85).
Hopelessness.
The Brief Hopelessness Scale (Bolland et al., 2001) was used to assess hopelessness and is an adapted form of the Hopelessness Scale for Children (Kazdin et al., 1986). Studies have indicated that this measure has strong internal consistency (α = 0.75) and is comparable to the full measure of hopelessness (Bolland et al., 2001). This scale contains 6 items and is rated on a 4 point Likert scale ranging from strongly disagree to strongly agree.
Internalizing symptoms.
The Patient Health Questionnaire-4 is a screening measure used to assess symptoms of depression and anxiety in the last two weeks (Löwe et al., 2010). It is derived from the PHQ-9 and GAD-7, and has psychometric properties that are comparable to the full scales, has strong reliability, and is associated with functional impairment. It contains the two items assessing depressive symptoms (anhedonia and negative affect) and two items assessing anxious symptoms (hyperarousal and worrying) Frequency of symptoms are rated on a scale ranging from “not at all” to “nearly every day”.
Alcohol use.
The 3-item AUDIT-C (Saunders et al., 1993) was used to assess the quantity of alcohol use and frequency of consumption. The AUDIT has been validated for use in the ED as a screen for youth with alcohol use disorders (Chung et al., 2002).
Suicidal thoughts and behavior.
The C-SSRS (Posner et al., 2011) was administered to all patients by ED staff as part of standard clinical practice at baseline and return visits and by master’s level clinicians at follow-up interviews. The C-SSRS assessed past week suicide ideation and lifetime histories of NSSI and suicidal behavior including actual, aborted, and interrupted suicide attempts as well as preparatory behavior. When present, suicide ideation severity was rated on a 1–5 scale: wish to be dead, suicide ideation, suicidal ideation with considerations of method, suicide ideation with intent, and suicide ideation with a specific plan. Number, lethality, and dates were assessed for preparation and actual, aborted, and interrupted suicide attempts. Attempts were considered highly lethal if methods included hanging, jumping, or firearms.
NSSI.
Severity and chronicity of NSSI was assessed using a brief self-report form adapted from the Self-Injurious Thoughts and Behaviors Interview (Nock et al., 2007). Participants reported number of lifetime and past month episodes, methods used, and age of onset of the first episode.
Data Analysis
Stata 16 was used for statistical analyses. Cross-tabulations and t tests compared LGBT and non-LGBT participants at baseline. Consistent with previous studies using the C-SSRS for follow-up with high-risk and ED samples (King et al., 2015; Miller et al., 2017; Posner et al., 2011; Yen et al., 2019), we examined suicide ideation severity continuously (i.e., on a 0–5 scale) and categorically (i.e., the presence of suicide ideation with intent). We operationally defined suicidal behavior as a composite outcome that includes a suicide attempt, interrupted attempt, aborted attempt, and preparatory behavior. Exploratory analyses were conducted with the log-rank test and Cox proportional hazards regressions to model time to suicidal behavior post-discharge. The proportional hazards assumption was upheld for all predictors. We estimated bivariate models to examine associations between baseline characteristics and suicidal behavior at follow-up. To control the false discovery rate and reduce the risk of Type I errors due to multiple testing, we applied the Benjamini-Hochberg step-up procedure. This method adjusts for multiple testing without increasing risk of Type II errors, as occurs in other methods such as the Bonferroni correction (Perneger, 1998). Variables associated with suicidal behavior were then entered into a multivariate model. To identify the most parsimonious set of predictors we removed non-significant variables (p > .05) individually, beginning with the largest p-values. We also conducted post hoc analyses to explore diagnostic correlates in key predictors identified above. In sensitivity analyses, results were in the same direction when examining suicidal behavior and actual suicide attempts separately.
Results
Descriptive Data at Index Visit
Baseline characteristics of the sample are detailed in Table 1. Over a third reported past psychiatric ED visits (35.1%) and hospitalizations (36.1%). Participants received the following diagnoses during their ED visit: mood disorder (n = 243, 85.3%); anxiety disorder (n = 84, 29.5%); eating disorder (n = 7, 2.5%); impulse control disorder (n = 31, 10.9%); psychotic disorder (n = 7, 2.5%); alcohol/substance use disorder (n = 40, 14.0%); antisocial personality disorder (n = 1, 0.4%); and borderline personality disorder (n = 7, 2.5%). Among the 285 participants, the majority reported past week suicide ideation (n = 226; 79.3%) and at least one incident of suicidal behavior (actual, interrupted, aborted suicide attempt, preparatory behavior) in their lifetime (n = 149; 52.3%). A third of participants reported attempting suicide at least once (n = 102; 35.8%). Most participants endorsed lifetime NSSI (n = 193; 67.7%) with mean (SD) age of onset of 13.3 (3.1) years. Nearly half of participants endorsing NSSI (n = 90; 46.6%) also reported a suicide attempt. In most cases (96.7%) NSSI preceded the first suicide attempt, and by an average of 3.3 (3.2) years.
Table 1.
Baseline characteristics of the full sample, LGBT participants, and Non-LGBT participants
| Full Sample | LGBT | Non-LGBT | |||
|---|---|---|---|---|---|
| Characteristic | (N=285) | (n=119) | (n=166) | p-valuea | Effect Sizeb |
| Gender nonconformityc | 16.5 (3.8) | 17.6 (4.1) | 15.7 (3.5) | <.001 | .51 |
| Victimizationd | 17.3 (30.0) | 22.2 (34.3) | 13.8 (25.9) | .02 | .28 |
| Hopelessnesse | 14.9 (4.3) | 15.5 (4.4) | 14.4 (4.2) | .03 | .26 |
| Internalizing symptomsf | 8.0 (3.0) | 8.7 (2.9) | 7.5 (3.0) | .001 | .41 |
| Alcohol use | 1.9 (2.5) | 1.9 (2.6) | 1.9 (2.4) | .655 | .00 |
| Previous ED visits | 100 (35.1) | 55 (46.2) | 45 (27.1) | .001 | .20 |
| Previous hospitalizations | 103 (36.1) | 53 (44.5) | 50 (30.1) | .01 | .12 |
| Past week suicide ideation severityg | 3.0 (1.6) | 3.4 (1.1) | 3.3 (1.2) | .13 | .09 |
| Ideation with intenth | 79 (27.7) | 34 (29.4) | 44 (26.5) | .59 | .03 |
| Frequencyi | 2.5 (1.9) | 2.9 (1.8) | 2.3 (2.0) | .01 | .32 |
| Durationj | 1.9 (1.6) | 2.1 (1.5) | 1.8 (1.6) | .13 | .19 |
| Lifetime suicidal behavior | 149 (51.3) | 68 (57.1) | 81 (48.8) | .16 | .08 |
| Lifetime suicide attempts | 102 (35.8) | 49 (41.2) | 53 (31.9) | .11 | .10 |
| Number of attempts | 2.3 (2.6) | 2.2 (1.9) | 2.5 (3.1) | .58 | .12 |
| Highly lethal method | 30 (10.5) | 15 (12.6) | 15 (9.0) | .33 | .06 |
| Past month attempts | 36 (12.6) | 17 (14.3) | 19 (11.4) | .48 | .04 |
| Lifetime NSSI | 193 (67.7) | 94 (79.0) | 99 (59.6) | < .001 | .20 |
| Lifetime episodes | 33.4 (36.0) | 40.2 (38.5) | 27.0 (32.4) | .01 | .37 |
| Lifetime methods | 3.4 (2.0) | 3.9 (2.1) | 2.9 (1.8) | < .001 | .51 |
| Past month episodes | 3.4 (6.2) | 3.0 (5.6) | 3.9 (6.8) | .34 | .33 |
| NSSI and suicide attempt | 90 (31.6) | 45 (37.8) | 45 (27.1) | .06 | .11 |
| NSSI to attempt (years) | 3.3 (3.2) | 4.0 (3.3) | 2.6 (2.9) | .05 | .45 |
Abbreviations: LGBT = lesbian, gay, bisexual, and transgender. ED = emergency department. NSSI = nonsuicidal self-injury. Continuous variables are given as mean (SD). Categorical variables are given as number (%).
Results are based on t-tests for continuous variables and cross-tabulations for categorical variables.
Effect sizes are Cohen’s d for continuous variables and Cramer’s phi coefficients for categorical variables.
Recalled Childhood Gender Identity/Gender Role Questionnaire (score range: 6–30).
Peer Experiences Questionnaire (score range: 0–20).
Brief Hopelessness Scale (score range: 6–24).
Patient Health Questionnaire-4 (score range: 0–12).
Columbia-Suicide Severity Rating Scale, ideation severity scale (score range: 0–5).
Columbia-Suicide Severity Rating Scale, ideation with intent or intent with a plan (score range: 4–5).
Columbia-Suicide Severity Rating Scale, intensity subscales (score range: 0–5).
Suicidal behavior includes actual, aborted, and interrupted attempts and preparatory behaviors.
A large number of participants (n=119; 41.8%) reported LGBT status (Figure 1). The most frequently endorsed identities were mostly heterosexual (19%), bisexual (20%), and multiple identities (25%). LGBT and non-LGBT participants did not differ by gender, race/ethnicity, and reason for ED visit. LGBT participants were more likely to receive a mood disorder diagnosis (n=109, 91.6%) than non LGBT youth (n=134, 80.7%), χ2 = 6.52, p = .01. Participants did not differ on other psychiatric diagnoses. On self-report measures, LGBT participants reported more childhood gender nonconformity, victimization, hopelessness, and internalizing symptoms. LGBT participants were more likely to have prior psychiatric ED visits and hospitalizations, more frequent past week suicide ideation, and a more severe history of NSSI. Specifically, LGBT youth were more likely to endorse lifetime NSSI and a higher number of lifetime episodes and methods. LGBT participants were more likely to report a lifetime history of both NSSI and suicide attempt but the transition to attempts occurred more slowly. LGBT participants did not significantly differ from non-LGBT youth in severity or duration of past week suicide ideation, lifetime history of any suicidal behavior, or suicide attempt number, lethality, or recency.
Figure 1.
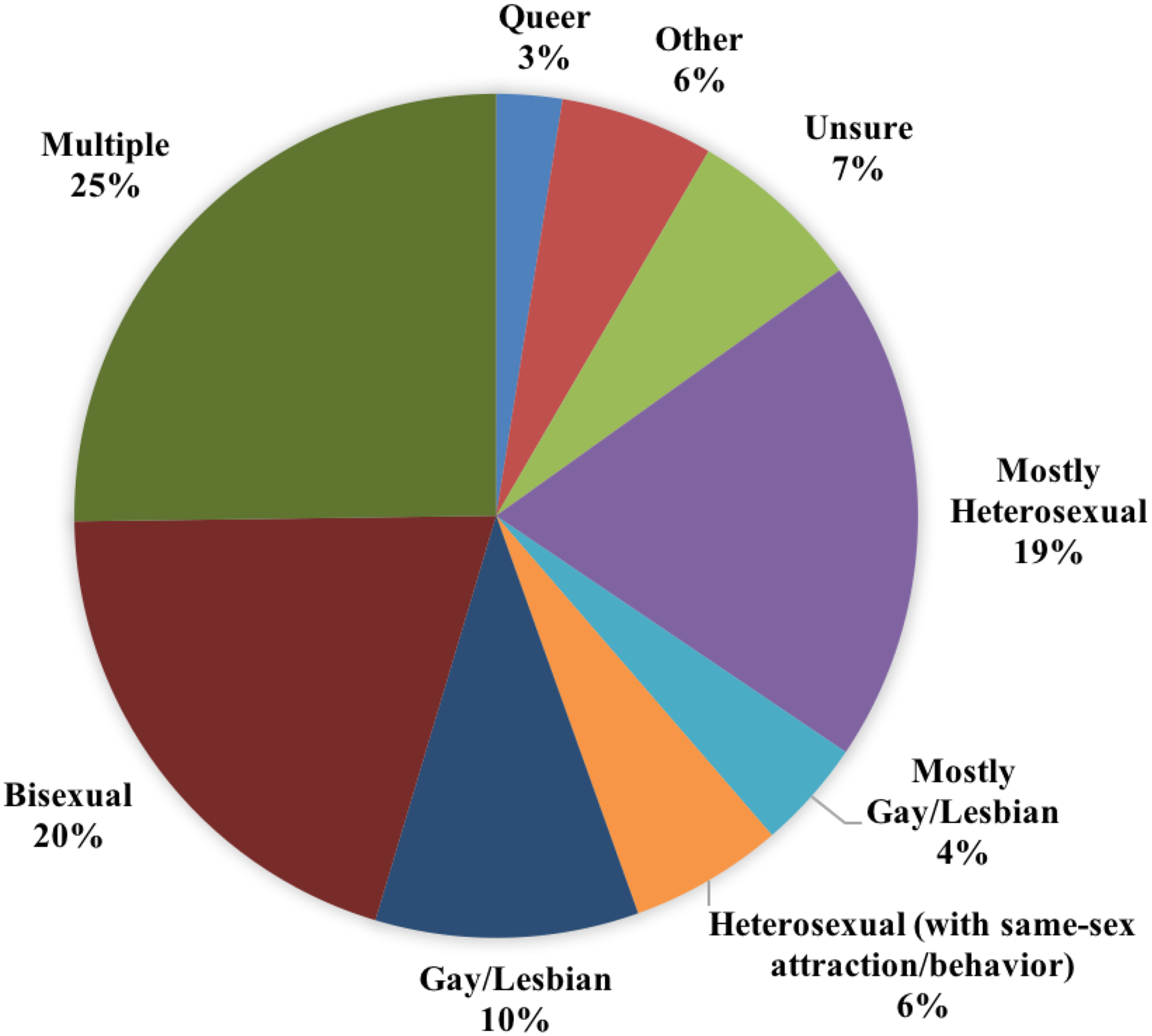
Distribution of sexual orientations endorsed by sexual minorities (n = 119) within the sample.
Longitudinal Analysis
At follow-up, 12.3% (n = 35) of the sample reported at least one suicide attempt and 21.1% (n = 60) reported any suicidal behavior. Actual suicide attempts were reported by 19 (16.0%) LGBT youth and 16 non-LGBT youth (9.6%), χ2 = 2.58, p = .11. Any suicidal behavior was reported by 30 (25.2%) LGBT youth and by 30 (18.1%) non-LGBT youth, χ2 = 2.13, p = .15. In a log-rank test, LGBT youth did not differ in time to suicidal behavior (χ2 = 2.55; p = .11).
Bivariate associations between study variables and prospectively observed suicidal behavior are detailed in Table 2. Among LGBT youth, hopelessness, suicide ideation severity and frequency, and NSSI characteristics (lifetime methods, recency) were associated with future suicidal behavior. Among non-LGBT youth victimization, hopelessness, internalizing symptoms, suicide ideation severity, NSSI characteristics (lifetime episodes and methods, recency), lifetime suicidal behavior, and suicide attempt history (number, use of a highly lethal method) were associated with suicidal behavior.
Table 2.
Hazard ratios for factors associated with suicidal behavior among participants during follow-up
| LGBT | Non-LGBT | |||
|---|---|---|---|---|
| (n=119) | (n=166) | |||
| Hazard Ratio (95% CI) | p-value | Hazard Ratio (95% CI) | p-value | |
| Childhood gender nonconformity | 0.97 (0.89–1.07) | .58 | 0.99 (0.89–1.10) | .86 |
| Victimization | 1.02 (0.94–1.12) | .59 | 1.11 (1.01–1.21) | .03 |
| Hopelessness | 1.10 (1.01–1.20) | .03 | 1.12 (1.03–1.22) | .01 |
| Internalizing symptoms | 1.10 (0.96–1.26) | .16 | 1.12 (0.99–1.28) | .08 |
| Alcohol use | 0.87 (0.74–1.03) | .11 | 1.08 (0.95–1.23) | .26 |
| Past week suicide ideation | ||||
| Severity (continuous) | 1.44 (1.11–1.87) | .006 | 1.21 (0.98–1.50) | .07 |
| Ideation with intent | 3.25 (1.58–6.67) | .001 | 1.67 (0.78–3.58) | .19 |
| Frequency | 1.52 (1.01–2.28) | .05 | 1.34 (0.93–1.93) | .12 |
| Duration | 1.2 (0.88–1.67) | .25 | 0.95 (0.67–1.36) | .78 |
| Lifetime suicidal behavior | 1.11 (0.96–1.28) | .15 | 1.13 (1.05–1.21) | .001 |
| Lifetime suicide attempts | ||||
| Number of attempts | 1.08 (0.91–1.28) | .36 | 1.14 (1.05–1.24) | .002 |
| Highly lethal method | 1.53 (0.62–3.76) | .35 | 3.10 (1.33–7.25) | .009 |
| Recency (past month) | 1.12 (0.43–2.92) | .82 | 1.10 (0.42–2.88) | .85 |
| Lifetime NSSI | ||||
| Number of episodes | 1.00 (0.99–1.01) | .89 | 1.02 (1.01–1.03) | <.001 |
| Number of methods | 1.18 (1.02–1.36) | .03 | 1.29 (1.12–1.49) | <.001 |
| Recency (past month) | 1.06 (1.01–1.11) | .01 | 1.05 (1.00–1.09) | .04 |
Note. LGBT = lesbian, gay, bisexual, and transgender. NSSI = nonsuicidal self-injury.
In multivariate analyses, number of past month NSSI episodes (HR = 1.06; 95% CI, 1.01–1.11, p = .02) and past week suicide ideation with intent (HR = 2.29; 95% CI: 1.07–4.90; p = .03) predicted suicidal behavior among LGBT youth. The number of lifetime NSSI methods (HR = 1.32; 95% CI, 1.14–1.53, p < .001) and use of a highly lethal suicide attempt method (HR = 3.64; 95% CI: 1.54–8.61; p = .003) predicted suicidal behavior among non-LGBT youth.
In light of previously documented disparities across psychopathology and SITBs, diagnostic correlates were examined across these longitudinal predictors. Mood disorders were associated with a higher number of lifetime NSSI methods [F(1, 283) = 22.09, p < .001) and greater likelihood of reporting suicide ideation with intent (χ2 = 12.96; p < .001). Participants with eating disorders were more likely to report suicide ideation with intent (χ2 = 6.84, p < .01). When added to multivariate models, there were no main or interaction effects of mood or eating disorders (p-value range: .20-.95).
Discussion
To our knowledge, this is the first study to comprehensively assess the severity of SITBs and their prospective associations with suicidal behavior among LGBT youth. In this study severity of SITBs were assessed at baseline and follow-up using the C-SSRS, which has validity in predicting future suicidal behavior (Posner et al., 2011). Key findings include overrepresentation of LGBT youth, differences in severity of NSSI history, and time frame of predictors of suicidal behavior.
Using a multicomponent assessment, LGBT youth comprised 41.8% of this sample of adolescents and young adults receiving psychiatric emergency services. Adolescents may be reticent to disclose their sexual orientation or gender identity/expression when their parents are involved in research. As such, our findings are likely an underestimate of the number of LGBT adolescents receiving psychiatric emergency services. Nevertheless, when considering studies with similar methodological designs, this proportion is 3 times higher than other ED studies (Arias et al., 2016; Asarnow et al., 2017; Currier et al., 2015). This difference is likely due to measurement of LGBT status. We provided several options and allowed participants to endorse multiple identities. Additionally, this study enrolled participants ages 13 to 25 years. Cohort differences in age of coming out may account for the relatively higher proportion of LGBT participants. Future work should consider utilizing inclusive measures to examine whether clinical outcomes differ in naturalistic and intervention studies.
Consistent with prior studies finding disparities in SITBs and their risk factors, LGBT youth reported more victimization, hopelessness, and internalizing symptoms. Further, findings underscore the utility of structured assessment of SITBs. While we did not find significant differences in histories of suicidal behavior, several differences emerged in examining NSSI. Within an already high-risk sample LGBT youth were more likely to endorse a lifetime history of NSSI, to report multiple episodes and methods, and to transition to suicide attempts. Notably, LGBT youth had a much slower transition to suicide attempts than non-LGBT youth. This pattern of findings may indicate a greater reliance on NSSI as a maladaptive coping strategy as well as a wider window of opportunity for intervention. Future studies should clarify the mechanisms linking minority stress to NSSI and associations between NSSI and suicidal behavior.
Prospective analyses revealed that components of SITBs were the most robust predictors of suicidal behavior over and above previously examined risk factors. Stratified multivariate models found that severity of SITBs were relevant for all youth, but factors that emerged as significant to time course differed by group. In the final model for LGBT youth, past week suicidal intent and past month NSSI episodes were associated with suicidal behavior. Among non-LGBT youth, the final model included lifetime number of NSSI methods and use of a highly lethal method in a previous suicide attempt. These findings are consistent with previous studies of LGBT youth. In particular, a previous longitudinal study of LGBT youth found that a history of suicide attempts predicted future attempts whereas childhood gender nonconformity, victimization, internalizing symptoms, and alcohol use did not (Mustanski and Liu, 2013). Additionally, previous studies have found that NSSI is a relatively strong predictor of future suicidal behavior (Franklin et al., 2017). Most LGBT youth (79%) reported NSSI. The smaller range of variability in NSSI history may partially explain why recency of NSSI was the most salient predictor of future suicidal behavior for this subgroup. These findings should be replicated in larger samples to ascertain whether temporality of risk factors differs among LGBT youth.
This study had several methodological strengths. The longitudinal design and use of a large high-risk sample increased the likelihood of observing post-discharge outcomes, enhancing statistical power to stratify analyses and explore within-group risk factors. The combination of closed- and open-ended measures of LGBT status aided in identifying several high-risk subgroups of youth, including bisexual, mostly heterosexual, and transgender youth. Moreover, suicidal behaviors were assessed by the C-SSRS interview at baseline and follow-up. Few studies of LGBT youth have explicitly differentiated between self-harm behaviors with and without suicidal intent. These data expand the literature by exploring factors associated with the progression and recurrence of risk. Further, this study informs our understanding of the temporal relationships between types of self-harm behaviors.
Results of this study should be considered in light of its limitations. Participants were clinically high risk, and findings may not generalize to community samples. Due to the exploratory nature of the study, we conducted multiple tests. Although we adjusted for multiple testing, these findings should be replicated within cohort studies with larger sample sizes. Most participants reported SITBs, which may have limited the sensitivity of statistical models. The incidences of post-discharge suicide attempts and suicidal behavior were approximately 12% and 20% respectively. Although these incidence rates are comparable to other clinical samples, this study was still underpowered to examine whether predictors differ within LGBT subgroups and specific tests of whether predictors were moderated by LGBT status. Medical record review allowed us to extend the follow-up period beyond the 4-month phone interviews but most suicide attempts are not treated. As such, combining interview and medical chart data yields more inclusive estimates of suicidal behavior during the first few months of the year post-discharge. Further, participants were included in the study only if they presented with a psychiatric chief complaint. Including youth with medical and injury-related complaints would expand the range of risk in the sample and should be considered in future research. Method of previous suicide attempt was used as a proxy for lethality because information about degree of physical harm was not recorded in patient charts. Actual physical harm would be a more proximal indicator of lethality and should be examined in future studies. Additionally, the areas of social connectedness, peer relationships, and family functioning are highly relevant to the experiences of LGBT minority stress (Miranda-Mendizábal et al., 2017). While these domains were not assessed here, they should be examined in future studies of social determinants of suicide risk disparities in this population.
Despite the aforementioned limitations, this study’s design and findings provide some direction for future research. This study sought to characterize SITBs among LGBT youth and their associations with future suicidal behavior. Suicidal behavior can have relatively low incidence rates even in clinical samples. Nevertheless, the purposive sampling implemented in this study allowed for the observation of suicidal behavior in a sizeable number of participants. Future research should examine in further detail the which the relationships considered here may portend longer term outcomes such as suicide- and all-cause mortality following discharge from the ED. Moreover, cohort studies of LGBT youth would bolster statistical power to detect group-specific relationships that may influence suicide risk factors. Although LGBT youth presented with more severe histories of NSSI and other suicide risk factors, only recent ED- based interventions were significantly associated with future suicidal behavior. Future studies should examine the extent to which existing brief ED-based interventions are efficacious in targeting these risk factors among LGBT youth. Such research would aid in discerning which factors could be addressed through preventative intervention as well as more broadly informing our understanding of developmental trajectories of LGBT youth.
Acknowledgments
This work was supported by an Active Minds Emerging Scholars Fellowship (JB), a Blue Cross Blue Shield of Michigan Foundation Student Award Grant (AGH), a University of Michigan Institute for Research on Women & Gender Community of Scholars Fellowship (JB), and University of Michigan Rackham Graduate Student Research Grants (EKC, AGH).
Footnotes
Declaration of competing interest
The authors do not have conflicts of interest to disclose.
References
- Arias SA, Miller I, Camargo CA, Sullivan AF, Goldstein AB, Allen MH, Manton AP, Boudreaux ED, 2016. Factors associated with screening positive for suicide risk in the emergency department. Psychiatric Services 67, 206–213. 10.1176/appi.ps.201400513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asarnow J, Berk M, Zhang L, Wang P, Tang L, 2017. Emergency department youth patients with suicidal ideation or attempts: Predicting suicide attempts through 18 months of follow-up. Suicide and Life-Threatening Behavior 47, 551–566. 10.1111/sltb.12309 [DOI] [PubMed] [Google Scholar]
- Babeva K, Hughes JL, Asarnow J, 2016. Emergency department screening for suicide and mental health risk. Current Psychiatry Reports 18 10.1007/s11920-016-0738-6 [DOI] [PubMed] [Google Scholar]
- Beckman K, Mittendorfer-Rutz E, Waern M, Larsson H, Runeson B, Dahlin M, 2018. Method of self-harm in adolescents and young adults and risk of subsequent suicide. Journal of Child Psychology and Psychiatry 59, 948–956. 10.1111/jcpp.12883 [DOI] [PubMed] [Google Scholar]
- Björkenstam C, Andersson G, Dalman C, Cochran S, Kosidou K, 2016. Suicide in married couples in Sweden: Is the risk greater in same-sex couples? European Journal of Epidemiology 31, 685–690. 10.1007/s10654-016-0154-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolland JM, McCallum DM, Lian B, Bailey CJ, Rowan P, 2001. Hopelessness and violence among inner-city youths. Maternal and Child Health Journal 8. [DOI] [PubMed] [Google Scholar]
- Brener ND, Kann L, Kinchen SA, Grunbaum JA, Whalen L, Eaton D, Hawkins J, Ross JG, 2004. Methodology of the youth risk behavior surveillance system. MMWR. Recommendations and reports: Morbidity and mortality weekly report. Recommendations and reports/Centers for Disease Control 53, 1–13. [PubMed] [Google Scholar]
- Carubia B, Becker A, Levine BH, 2016. Child psychiatric emergencies: Updates on trends, clinical care, and practice challenges. Current Psychiatry Reports 18 10.1007/s11920-016-0670-9 [DOI] [PubMed] [Google Scholar]
- Cha CB, Tezanos KM, Peros OM, Ng MY, Ribeiro JD, Nock MK, Franklin JC, 2018. Accounting for diversity in suicide research: Sample and sample reporting practices in the United States. Suicide and Life-Threatening Behavior 48, 131–139. 10.1111/sltb.12344 [DOI] [PubMed] [Google Scholar]
- Chung T, Colby SM, Barnett NP, Monti PM, 2002. Alcohol use disorders identification test: Factor structure in an adolescent emergency department sample. Alcoholism: Clinical and Experimental Research 26, 223–231. 10.1111/j.1530-0277.2002.tb02528.x [DOI] [PubMed] [Google Scholar]
- Currier G, Brown G, Walsh P, Jager-Hyman S, Chaudhury S, Stanley B, 2015. Screening for sexual orientation in psychiatric emergency departments. Western Journal of Emergency Medicine 16, 80–84. 10.5811/westjem.2014.12.22254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- di Giacomo E, Krausz M, Colmegna F, Aspesi F, Clerici M, 2018. Estimating the risk of attempted suicide among sexual minority youths: A systematic review and meta-analysis. JAMA Pediatrics 172, 1145 10.1001/jamapediatrics.2018.2731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox KR, Hooley JM, Smith DMY, Ribeiro JD, Huang X, Nock MK, Franklin JC, 2018. Self-injurious thoughts and behaviors may be more common and severe among people identifying as a sexual minority. Behavior Therapy 49, 768–780. 10.1016/j.beth.2017.11.009 [DOI] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, Musacchio KM, Jaroszewski AC, Chang BP, Nock MK, 2017. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin 143, 187–232. 10.1037/bul0000084 [DOI] [PubMed] [Google Scholar]
- Gipson PY, Agarwala P, Opperman KJ, Horwitz A, King CA, 2015. Columbia-Suicide Severity Rating Scale: Predictive validity with adolescent psychiatric emergency patients. Pediatric Emergency Care 31, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn CR, Kleiman EM, Kellerman J, Pollak O, Cha CB, Esposito EC, Porter AC, Wyman PA, Boatman AE, 2019. Annual Research Review: A meta‐analytic review of worldwide suicide rates in adolescents. Journal of Child Psychology and Psychiatry. 10.1111/jcpp.13106 [DOI] [PubMed] [Google Scholar]
- Global Burden of Disease Pediatrics Collaboration, 2016. Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: Findings from the global burden of disease 2013 study. JAMA Pediatrics 170, 267 10.1001/jamapediatrics.2015.4276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas A, Eliason M, Mays VM, Mathy RM, Cochran SD, D’Augelli AR, Silverman MM, Fisher PW, Hughes T, Rosario M, Russell ST, Malley E, Reed J, Litts DA, Haller E, Sell RL, Remafedi G, Bradford J, Beautrais AL, Brown GK, Diamond GM, Friedman MS, Garofalo R, Turner MS, Hollibaugh A, Clayton PJ, 2010. Suicide and suicide risk in lesbian, gay, bisexual, and transgender populations: Review and recommendations. Journal of Homosexuality 58, 10–51. 10.1080/00918369.2011.534038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horwitz AG, Czyz EK, King CA, 2015. Predicting future suicide attempts among adolescent and emerging adult psychiatric emergency patients. Journal of Clinical Child & Adolescent Psychology 44, 751–761. 10.1080/15374416.2014.910789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE, Rodgers A, Colbus D, 1986. The Hopelessness Scale for Children: Psychometric characteristics and concurrent validity. Journal of Consulting and Clinical Psychology 54, 241–245. [DOI] [PubMed] [Google Scholar]
- King CA, Arango A, Ewell Foster C, 2018. Emerging trends in adolescent suicide prevention research. Current Opinion in Psychology 22, 89–94. 10.1016/j.copsyc.2017.08.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Berona J, Czyz E, Horwitz AG, Gipson PY, 2015. Identifying Adolescents at Highly Elevated Risk for Suicidal Behavior in the Emergency Department. Journal of Child and Adolescent Psychopharmacology 25, 100–108. 10.1089/cap.2014.0049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Grupp‐Phelan J, Brent D, Dean JM, Webb M, Bridge JA, Spirito A, Chernick LS, Mahabee‐Gittens EM, Mistry RD, Rea M, Keller A, Rogers A, Shenoi R, Cwik M, Busby DR, Casper TC, the Pediatric Emergency Care Applied Research Network, 2019. Predicting 3‐month risk for adolescent suicide attempts among pediatric emergency department patients. Journal of Child Psychology and Psychiatry. 10.1111/jcpp.13087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, Schneider A, Brähler E, 2010. A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of Affective Disorders 122, 86–95. 10.1016/j.jad.2009.06.019 [DOI] [PubMed] [Google Scholar]
- McKean AJS, Pabbati CP, Geske JR, Bostwick JM, 2018. Rethinking Lethality in Youth Suicide Attempts: First Suicide Attempt Outcomes in Youth Ages 10 to 24. Journal of the American Academy of Child & Adolescent Psychiatry 57, 786–791. 10.1016/j.jaac.2018.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeil J, Ellis SJ, Eccles FJR, 2017. Suicide in trans populations: A systematic review of prevalence and correlates. Psychology of Sexual Orientation and Gender Diversity 4, 341–353. 10.1037/sgd0000235 [DOI] [Google Scholar]
- Miller IW, Camargo CA, Arias SA, Sullivan AF, Allen MH, Goldstein AB, Manton AP, Espinola JA, Jones R, Hasegawa K, Boudreaux ED, for the ED-SAFE Investigators, 2017. Suicide Prevention in an Emergency Department Population: The ED-SAFE Study. JAMA Psychiatry 74, 563 10.1001/jamapsychiatry.2017.0678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda-Mendizábal A, Castellví P, Parés-Badell O, Almenara J, Alonso I, Blasco MJ, Cebrià A, Gabilondo A, Gili M, Lagares C, Piqueras JA, Roca M, Rodríguez-Marín J, Rodríguez-Jiménez T, Soto-Sanz V, Vilagut G, Alonso J, 2017. Sexual orientation and suicidal behaviour in adolescents and young adults: systematic review and meta-analysis. British Journal of Psychiatry 211, 77–87. 10.1192/bjp.bp.116.196345 [DOI] [PubMed] [Google Scholar]
- Mustanski B, Liu RT, 2013. A longitudinal study of predictors of suicide attempts among lesbian, gay, bisexual, and transgender youth. Archives of Sexual Behavior 42, 437–448. 10.1007/s10508-012-0013-9 [DOI] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, Michel BD, 2007. Self-Injurious Thoughts and Behaviors Interview: Development, reliability, and validity in an adolescent sample. Psychological Assessment 19, 309–317. 10.1037/1040-3590.19.3.309 [DOI] [PubMed] [Google Scholar]
- Perneger TV, 1998. What’s wrong with Bonferroni adjustments. BMJ 316, 1236–1238. 10.1136/bmj.316.7139.1236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, Currier GW, Melvin GA, Greenhill L, Shen S, Mann JJ, 2011. The Columbia–Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. American Journal of Psychiatry 168, 1266–1277. 10.1176/appi.ajp.2011.10111704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prinstein MJ, Boergers J, Vernberg EM, 2001. Overt and relational aggression in adolescents: Social-psychological adjustment of aggressors and victims. Journal of Clinical Child & Adolescent Psychology 30, 479–491. 10.1207/S15374424JCCP3004_05 [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Franklin JC, Fox KR, Bentley KH, Kleiman EM, Chang BP, Nock MK, 2016. Self-injurious thoughts and behaviors as risk factors for future suicide ideation, attempts, and death: A meta-analysis of longitudinal studies. Psychological Medicine 46, 225–236. 10.1017/S0033291715001804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sánchez JP, Hailpern S, Lowe C, Calderon Y, 2007. Factors associated with emergency department utilization by urban lesbian, gay, and bisexual individuals. Journal of Community Health 32, 149–156. 10.1007/s10900-006-9037-1 [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M, 1993. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction 88, 791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Savin-Williams RC, 2001. Suicide attempts among sexual-minority youths: Population and measurement issues. Journal of Consulting and Clinical Psychology 69, 983–991. 10.1037//0022-006X.69.6.983 [DOI] [PubMed] [Google Scholar]
- Yen S, Spirito A, Weinstock LM, Tezanos K, Kolobaric A, Miller I, 2019. Coping long term with active suicide in adolescents: Results from a pilot randomized controlled trial. Clinical Child Psychology and Psychiatry 24, 847–859. 10.1177/1359104519843956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zucker KJ, Mitchell JN, Bradley SJ, Tkachuk J, Cantor JM, Allin SM, 2006. The Recalled Childhood Gender Identity/Gender Role Questionnaire: Psychometric properties. Sex Roles 54, 469–483. 10.1007/s11199-006-9019-x [DOI] [Google Scholar]


