Abstract
N6-methyladenosine (m6A) RNA modification maintained by N6-methyltransferases and demethylases is involved in multiple biological functions. Methyltransferase like 3 (METTL3) is a major N6-methyltransferase. However, the role of METTL3 and its installed m6A modification in colorectal tumorigenesis remains to be fully elucidated. METTL3 is highly expressed as indicated in colorectal cancer samples in the TCGA and Oncomine databases, implying its potential role in colon tumorigenesis. SW480 cell line with stable METTL3 knockout (METTL3-KO) was generated using CRISPR/Cas9 and were confirmed by the loss of METTL3 expression and suppression of m6A modification. The proliferation of METTL3-KO cells was significantly inhibited compared with that of control cells. METTL3-KO decreased the decay rate of suppressor of cytokine signaling 2 (SOCS2) RNA, resulting in elevated SOCS2 protein expression. m6A-RNA immunoprecipitation-qPCR (MeRIP-qPCR) revealed that SOCS2 mRNA was targeted by METTL3 for m6A modification. Similar to METTL3-KO SW480 cells, SW480 cells treated with 3-deazaadenosine, an RNA methylation inhibitor, exhibited elevated SOCS2 protein expression. Increased levels of SOCS2 in METTL3-KO SW480 cells were associated with decreased expression of leucine-rich repeat-containing G protein-coupled receptor 5 (LGR5), contributing to the inhibition of cell proliferation. The underlying associations among METTL3, SOCS2, and LGR5 were further confirmed in SW480 cells transfected with si-METTL3 and in tumor samples from patients with colorectal cancer. Taken together, our data demonstrate that an increased level of METTL3 may maintain the tumorigenicity of colon cancer cells by suppressing SOCS2.
Keywords: m6A modification, methyltransferase like 3, suppressor of cytokine signaling 2, colorectal cancer, tumorigenesis, leucine-rich repeat-containing G protein-coupled receptor 5
Introduction
Colorectal cancer (CRC) is the third most common cancer and the second leading cause of cancer-related death worldwide (1,2). The incidence of CRC continues to increase in developing countries and is also increasing in individuals younger than 50 years (3). A worldwide health burden, CRC exhibits molecular heterogeneity, which contributes to the variable clinical outcomes (4). The identification of prognostic and predictive biomarkers for early diagnosis, prevention, and targeted therapy is a major challenge in CRC treatment. Progress has been made in the discovery of key oncogenic markers and transcriptional modifications for decades (5,6); for example, RAS mutation testing has shown beneficial effects in predicting the clinical outcome of anti-EGFR therapy in patients with CRC, and immunohistochemical analysis of DNA mismatch repair proteins (MLH1, MSH2, MSH6 and PMS2) has been shown to have predictive value in CRC and is recommended for clinical use. However, the molecular mechanisms of CRC pathogenesis remain unclear. More effective and sensitive biomarkers are still urgently needed for defining therapeutic targets and personalized therapeutic regimens in CRC.
N6-methyladenosine (m6A), a reversible posttranscriptional RNA modification, is installed by methyltransferase like 3 (METTL3) in cooperation with methyltransferase like 14 (METTL14) and Wilms tumor 1-associated protein (WTAP) (7). m6A RNA modification is erased by fat mass and obesity-associated protein (FTO) and the RNA demethylase alkB homolog 5 (ALKBH5) (7). The YT521-B homology (YTH) domain family proteins (YTHDF1, YTHDF2, YTHDF3, and YTHDC1) have been identified as m6A readers (7). The functional effects of m6A RNA modification include RNA splicing, degradation, and translation and RNA-protein interaction (8–10). This type of RNA modification is critical for circadian clock regulation, self-renewal and cell fate transition (11,12). Accumulating studies have demonstrated that m6A modification plays regulatory roles in various malignancies (13–15). METTL3 promotes glioblastoma progression and enhances cancer stem cell (CSC) self-renewal (15), and METTL3 upregulation appears to be critical for cancer cell growth, survival and invasion in lung cancer (16). Moreover, METTL3 dysfunction exerts critical effects in gastrointestinal tract cancers. Elevated METTL3 expression augments tumor proliferation and liver metastasis by increasing the RNA m6A level in gastric cancer (17,18), and METTL3 is involved in cancer progression and therapeutic resistance in pancreatic cancer (19). However, the roles of m6A and METTL3 in CRC still need to be demonstrated, and this knowledge may provide insight into the development of new therapeutic strategies.
Accumulating evidence indicates that the activity of suppressor of cytokine signaling (SOCS) family proteins correlates with progression and poor prognosis in various cancers (20,21). SOCS2, a member of the SOCS family, is well defined as a transcriptional repressor in multiple proliferation-related pathways and acts as a tumor suppressor in multiple malignancies. Previous studies have reported downregulation of SOCS2 in breast and ovarian cancers (22,23). In addition, SOCS2 has been reported to inhibit metastasis in prostate cancer and hepatocellular carcinoma (24,25). However, the molecular mechanisms underlying the role of SOCS2 in tumorigenesis, including CRC tumorigenesis, are still obscure.
Leucine-rich repeat-containing G protein-coupled receptor 5 (LGR5) is characterized as a CSC biomarker and is essential for the maintenance of stemness properties (26,27). Previously, LGR5 upregulation was found in CRC and was found to be positively correlated with the pathological grade and invasiveness of CRC (28). Thus, LGR5 is considered a promising new therapeutic target for CRC. Although LGR5 has been revealed to be associated with the prognosis and progression of CRC, the upstream regulation of LGR5 in CRC is unclear.
Here, we report that METTL3 overexpression promotes tumor cell proliferation in CRC. Mechanistically, METTL3 induces SOCS2 mRNA instability via m6A modification. Aberrant overexpression of LGR5 is caused by SOCS2 instability in CRC, and this effect maintains the high stemness and robust cell proliferation observed in CRC.
Materials and methods
Clinical sample collection
Fresh colon tumor tissues and matched adjacent normal colon tissues (>5 cm from the tumor border) (n=24 pairs) were collected from patients with CRC after surgical resection at the Department of Gastroenterological Surgery, Sun Yat-Sen Memorial Hospital, Sun Yat-Sen University, between June and August 2018. Samples were immediately frozen in liquid nitrogen and stored at −80°C until analysis. Tumor tissues and adjacent normal colon tissues were confirmed by postoperative pathological diagnosis. All patients recruited in the study were confirmed by pathological diagnosis. The exclusion criteria were as follows: i) Patients with a metastatic colon tumor originating in another organ; ii) CRC patients who had already received chemotherapy and/or radiotherapy; and iii) patients with CRC in situ or a benign tumor confirmed by pathological diagnosis. The clinicopathological features of the patients (sex, age, tumor size, pathological type and TNM stage) were collected. All enrolled patients and their respective guardians provided written consent, and the study strictly adhered to the guidelines of the Institutional Review Board Committee of Sun Yat-Sen Memorial Hospital, Sun Yat-Sen University (Guangzhou, Guangdong, China) (Approval no. 58, 2016 record for Ethics).
Cancer database analysis
CRC-related data with entries defined as colorectal adenocarcinoma were downloaded from The Cancer Genome Atlas (TCGA; http://www.cbioportal.org). Expression levels of METTL3, SOCS2 and LGR5 in normal colon tissues were compared with those in CRC tissues. To comprehensively identify the gene expression profile in CRC, we utilized the Oncomine database, an online public cancer database of DNA and RNA sequences, to collect transcriptional expression data for METTL3, SOCS2 and LGR5 in CRC using the ‘Gene summary view’ and ‘Dataset view’ (https://www.oncomine.org/resource/login.html). Transcriptional expression of METTL3, SOCS2 and LGR5 in CRC samples was compared with that in normal colorectal epithelium samples using Student's t-test. A total of 12 datasets were found. Statistically significant differences and fold changes were defined as P<0.05 and ≥2, respectively.
Cytoscape literature mining was performed with the search term ‘METTL3’ to query the whole NCBI database (https://www.ncbi.nlm.nih.gov/pubmed) by default parameters. The software automatically retrieved all articles in PubMed mentioning METTL3. The reported correlations of METTL3 with other genes were assembled and visualized with Cytoscape (29).
Colon cancer cell line culture
SW480 cells (a colon cancer cell line) were obtained from the American Type Culture Collection (ATCC, USA) and cultured in the recommended medium [L-15 medium supplemented with 10% fetal bovine serum (FBS), 100 µg/ml streptomycin, and 100 U/ml penicillin]. Cells were maintained in a humidified incubator without CO2 at 37°C.
CRISPR-Cas9-mediated knockout of METTL3
CRISPR/Cas9 was applied to stably knock out the METTL3 gene (NCBI GeneID 56339) to generate stable cell lines. In brief, SW480 cells were transfected with the METTL3 CRISPR/Cas9 and HDR plasmids (sc-404029, Santa Cruz Biotechnology, Inc.). Colonies were selected, and western blotting was used to detect METTL3 protein expression. The clones with the expected knockdown of METTL3 were further validated by qPCR and Sanger sequencing.
Cell transfection
To transiently knock down METTL3 expression, siRNA transfection was used. Two siRNAs targeting METTL3 (si-METTL3#1 and si-METTL3#2) were synthesized by GenePharma Corporation. The siRNA sequences were as follows: si-METTL3#1, 5′-GGUGACUGCUCUUUCCUUATT-3′ and 3′-UAAGGAAAGAGCAGUCACCTT-5′; si-METTL3#2, 5′-GCUACCUGGACGUCAGUAUTT-3′ and 5′-AUACUGACGUCCAGGUAGCTT-3′. The negative control siRNA sequences were as follows: si-Ctrl, 5′-UUCUCCGAACGUGUCACGUTT-3′ and 5′-ACGUGACACGUUCGGAGAATT-3′. The siRNA targeting SOCS2 (si-SOCS2) was obtained from Santa Cruz Biotechnology, Inc. The pCMV6 plasmid containing the full-length SOCS2 sequence (FULL-SOCS2) was purchased from Origene (RC203163).
Cells were cultured in 6-well plates (1×105 cells per well) overnight prior to the experiment. The following day, siRNA (80 µM) was transfected into cells with Lipofectamine RNAiMAX (5 µl per well) (Thermo Fisher Scientific, Inc.). For plasmid transfection, cells were seeded at a density of 1×105 cells per well in 6-well plates. Twenty-four hours later, Lipofectamine 2000 (5 µl per well; Thermo Fisher Scientific, Inc.) was used to transfect cells with the plasmid (2.5 µg per well) following the manufacturer's instructions. Cells were harvested 48 h after transfection for RNA and protein detection.
Cell proliferation assays
For the MTS assay, cells were seeded in 96-well plates at a density of 1×103 cells per well and cultured for 4 days. The absorbance at 490 nm was measured every 24 h after incubation with 20 µl of MTS reagent (Promega, Corp.) for 2 h.
A cell counting assay was utilized to assess the cell proliferation ability. Cells (1×104 cells per well) were plated in a 12-well plate. On days 1, 2, 3, and 4 after seeding, the plated cells were trypsinized and then stained by trypan blue staining. The total number of cells was counted under Olympus BX63 microscope (Olympus).
For the colony formation assay, cells (1×104 cells per well) were seeded in 6-well plates. On days 7, 10 and 14 after seeding, colonies in each well were fixed with 4% paraformaldehyde and stained with 1% crystal violet. The colony-forming units were recorded and photographed by Olympus BX63 microscope and image software (cellSens Dimension; Olympus).
Tumorsphere formation assay
To investigate the tumorsphere formation capacity, cells were resuspended in tumorsphere-complete medium [DMEM/F12 supplemented with 20 ng/ml human epidermal growth factor (EGF), 10 ng/ml fibroblast growth factor-basic (bFGF), 5 µg/ml insulin, 0.4% BSA, and 1X B27] and were then plated in an ultra-low attachment 6-well plate. The medium was supplemented every other day. The spheroid structures were photographed and counted by Olympus BX63 microscope and image software (cellSens Dimension; Olympus) on days 7 and 14 after plating.
Total RNA isolation and qPCR detection
Total RNA was extracted using TRIzol reagent (Invitrogen; Thermo Fisher Scientific, Inc.) and treated with a DNA-free DNase Treatment & Removal I Kit (Thermo Fisher Scientific, Inc.) to remove any remaining DNA. A total of 500 ng of RNA was used for reverse transcription, which was carried out by using Reverse Transcriptase Buffer and SuperScript II Reverse Transcriptase (Invitrogen; Thermo Fisher Scientific, Inc.). cDNA (25 ng) was subjected to qPCR for each gene of interest with SYBR Green reagent (Bio-Rad Laboratories, Inc.). qPCR was performed using a Bio-Rad CFX96 platform with the following settings: Initial denaturation at 95°C for 30 sec, followed by 40 cycles of denaturation at 95°C for 5 sec, annealing at 60°C for 30 sec, and elongation at 72°C for 30 sec. Fluorescent signals were detected after each cycle. Each sample was run in triplicate. The relative mRNA expression levels were calculated using the 2−ΔΔCq (cycle threshold) method (30) and normalized to GAPDH. The primer sequences are listed in Table SI.
Western blot analysis
Cells were harvested and lysed with M-PER mammalian protein extraction reagent (Thermo Fisher Scientific, Inc.). Following protein quantification, proteins in lysed samples (30 µg per well) were separated on a 10% acrylamide gel and were then transferred to PVDF membranes (Millipore). Membranes were incubated with the following primary antibodies overnight at 4°C: Anti-METTL3 (dilution 1:1,000, 15073-1-AP, Proteintech), anti-SOCS2 (dilution 1:1,000, 2779, Cell Signaling Technology, Inc.), anti-LGR5 (dilution 1:1,000, sc-135238, Santa Cruz Biotechnology, Inc.), and anti-β-actin (dilution 1:1,000, sc-130656, Santa Cruz Biotechnology, Inc.). Positive signals were detected using ECL reagent (Bio-Rad Laboratories, Inc.) in a FluorChem FC2 Imaging System (Alpha Innotech). ImageJ software version 1.51 (National Institutes of Health, USA) was used to measure the band intensities. β-actin was used as the internal reference.
m6A quantification
Total RNA extracted from cells was purified and quantified. The isolated total RNA was subjected to mRNA purification using a Dynabeads mRNA Purification Kit (Thermo Fisher Scientific, Inc.) to deplete rRNA and noncoding RNAs. A total of 200 ng of mRNA from each sample was used, and m6A quantification was carried out by using an EpiQuik m6A Methylation Quantification kit (Colorimetric, Epigentek) according to the manufacturer's instructions.
m6A-RNA immunoprecipitation-qPCR (MeRIP-qPCR)
MeRIP-qPCR was performed as previously reported (31). In brief, mRNA was isolated, purified and chemically shredded into ~100-nt fragments using Ambion fragmentation reagent (Thermo Fisher Scientific, Inc.). mRNA fragments (200 ng) were denatured at 65°C for 5 min and incubated with 20 µl of Magna ChIP Protein A+G Magnetic Beads (2923270, Millipore) conjugated to 1 µg of anti-m6A polyclonal antibody (ab208577, Abcam) or mouse control IgG (sc-2025, Santa Cruz Biotechnology, Inc.) in 1X IPP buffer (15 mM NaCl, 10 mM Tris-HCl and 0.1% NP-40). mRNA was incubated with m6A-bound beads with rotation at 4°C for 3 h in IPP buffer. The beads were washed twice with 1X IPP buffer, twice with low-salt buffer (50 mM NaCl, 10 mM Tris-HCl and 0.1% NP-40), twice with high-salt buffer (500 mM NaCl, 10 mM Tris-HCl and 0.1% NP-40) and once with 1X IPP buffer. RNA was eluted from the beads with 50 µl of RLT buffer and purified through Qiagen RNeasy columns (Qiagen) according to the manufacturer's recommendation. Total RNA was finally eluted in 100 µl of RNase-free water. The relative abundances of RNAs of interest were measured using qPCR and normalized to the input level.
RNA stability
Cells (2×104 cells per well) were plated in 12-well plates. After overnight incubation, cells were treated with actinomycin D (ACD; A9415, Sigma-Aldrich; Merck KGaA) at a final concentration of 10 µg/ml and incubated in a humidified incubator without CO2 at 37°C. Total RNA was extracted at different time points after actinomycin D treatment (0, 1, 2, 4 and 8 h). Following total RNA extraction and quantification, the expression levels of specific genes of interest were quantified using qPCR.
Demethylation treatment with 3-deazaadenosine (DAA)
The global methylation inhibitor DAA (D8296, Sigma-Aldrich; Merck KGaA) was used to inhibit RNA methylation (11,32). After seeding, cells were treated with 10 µg/ml DAA for 48 h. Cells were then collected for mRNA and protein analysis.
Luciferase assay
The LGR5 promoter region sequence (−2 kb~+100 b) was obtained from National Center for Biotechnology Information (NCBI). The LGR5 promoter was cloned using specific primers and was then ligated into the pGL3 vector digested with XhoI and SacI. The pGL3-LGR5 promoter and the FULL-SOCS2 plasmid were cotransfected into SW480 cells. Twenty-four hours after transfection, cells were collected with luciferase lysis buffer (E3971, Promega Corp.). Luciferase Assay Reagent (E1483, Promega Corp.) was used to measure luciferase activity after cotransfection. β-Gal activity was measured as an internal transfection control.
Statistical analysis
Each experiment was performed at least three independent times. All experimental data are presented as the mean ± SEM values. Student's t-test or one-way ANOVA was conducted for evaluating intergroup differences. The correlation of protein expression and clinicopathological features was analyzed by Fisher's exact test or Chi-square test. Linear regression analysis was used to analyze the correlation between two genes. Statistical analysis was performed using GraphPad Prism 5 (GraphPad Software). P<0.05 was considered to indicate a statistically significant difference.
Results
METTL3 expression is increased in CRC
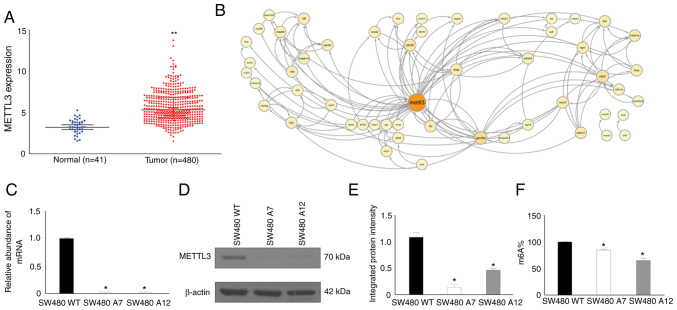
To determine the expression pattern of METTL3 in CRC, we queried the TCGA database. A total of 480 colon cancer samples and 41 normal colon tissues were found. Compared to normal colon tissues, colon cancer samples showed an elevated METTL3 RNA level (P<0.05; Fig. 1A).
Figure 1.
High level of METTL3 expression in colon cancer and the establishment of METTL3-KO SW480 cells. (A) TCGA database analysis showed an elevated expression level of METTL3 in colon cancer (**P<0.01). (B) Literature mining identified 52 candidate genes potentially associated with METTL3. (C-E) METTL3-KO SW480 cells showed diminished expression of METTL3 at both the (C) mRNA and (D and E) protein levels (*P<0.05, compared with the SW480 WT cells). (F) METTL3-KO abolished the maintenance of overall RNA methylation (*P<0.05, compared with the SW480 WT cells). METTL3, methyltransferase like 3; KO, knockout; TCGA, The Cancer Genome Atlas; SW480 A7 and SW480 A12, METTL3-KO SW480 cells.
To explore the potential role of METTL3 expression in CRC tumorigenesis, we conducted literature mining via Cytoscape network analysis and identified 52 candidate genes that may interact with METTL3 (Fig. 1B). Both METTL3 and METTL14 have been reported to act coordinately to maintain m6A modification (7). Cytoscape analysis of METTL14 revealed the same group of genes found for METTL3, suggesting that METTL3 and METTL14 were considered a single complex in the Cytoscape analysis. Those candidates genes were further subjected to Gene Ontology analysis (Table SIIA) via the Database for Annotation, Visualization and Integrated Discovery (DAVID) tool (https://david.ncifcrf.gov/). Our analysis revealed that METTL3 is mainly involved in the following three bioprocesses: Cell proliferation, inflammatory response and RNA processing. Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis indicated that these candidate genes are closely associated with multiple diseases, including acute myeloid leukemia, CRC and prostate cancer (Table SIIB). These results imply a potential role for METTL3 in tumor progression and the regulation of inflammation, cell proliferation and RNA processing.
Establishment of stable METTL3-knockout (METTL3-KO) colon cancer cell lines
We used CRISPR-Cas9 to generate stable METTL3-KO colon cancer cell lines in SW480 cells. Two lines of METTL3-KO cells, SW480 A7 and SW480 A12, were finally obtained through antibiotic selection, and the absence of METTL3 expression in these cell lines was confirmed by qPCR and western blotting (Fig. 1C-E). No qPCR product was detected using the specific primer sets covering the targeted region of METTL3; in addition, the western blot results indicated the knockout of the METTL3 protein in METTL3-KO SW480 cells. Moreover, to verify METTL3 inhibition in METTL3-KO cells, global m6A levels were measured using the EpiQuik m6A Methylation Quantification kit. The overall m6A level was evidently decreased in METTL3-KO SW480 cells when compared with the parental cells (Fig. 1F).
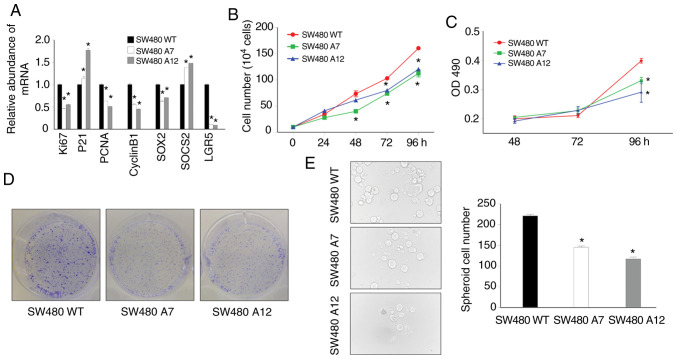
METTL3-KO elicits an inhibitory effect on SW480 cell proliferation
Given the potential function of METTL3 in regulating cell proliferation implied by the above bioinformatic analysis results, we screened the differential expression profiles of proliferation-related genes in METTL3-KO SW480 cells vs. the control SW480 (SW480 WT) cells to determine whether downregulation of METTL3 modulates cell proliferation in CRC. Ki67, LGR5, PCNA, SOX2 and Cyclin B1 have been reported to be positively correlated with cell proliferation (33–36). All five of these genes were significantly downregulated in the METTL3-KO SW480 cells. On the other hand, two antiproliferative genes, SOCS2 and P21, were upregulated (Fig. 2A).
Figure 2.
Inhibition of cell proliferation in METTL3-KO SW480 cells. (A) METTL3-KO SW480 cells showed dysregulation of several proliferation-related genes (*P<0.05, compared with the SW480 WT cells). (B) MTS assay results validated the decreased proliferation of METTL3-KO cells (*P<0.05, compared with the SW480 WT cells). (C) METTL3-KO cells showed a reduced proliferation rate, as measured by cell counting (*P<0.05, compared with the SW480 WT cells). (D) METTL3-KO cells showed a lower colony formation rate than control cells at 7 days after seeding. (E) Tumorigenic ability of METTL3-KO SW480 cells was reduced (*P<0.05, compared with the SW480 WT cells). SOCS2, suppressor of cytokine signaling 2; METTL3, methyltransferase like 3; LGR5, leucine-rich repeat-containing G protein-coupled receptor 5; SOX2, SRY-box transcription factor 2; PCNA, proliferating cell nuclear antigen; KO, knockout; SW480 A7 and SW480 A12, METTL3-KO SW480 cells.
We then examined the effects of METTL3 knockout on SW480 cell proliferation and stemness. Both METTL3-KO lines, SW480 A7 and SW480 A12, showed a decrease in cell proliferation in the MTS assay (Fig. 2B). In addition, the growth of METTL3-KO cells was markedly inhibited, as measured by cell counting and colony formation assays (Fig. 2C and D). Moreover, we performed a tumorsphere formation assay to observe stemness properties arising from METTL3 knockout. Spheroid formation can be used to estimate the percentage of CSCs present in a population of tumor cells. Spheroid formation by METTL3-KO SW480 cell lines was significantly inhibited, suggesting the loss of stemness of these cells (Fig. 2E). Collectively, these data indicate that METTL3 may play an important role in regulating SW480 cell self-renewal.
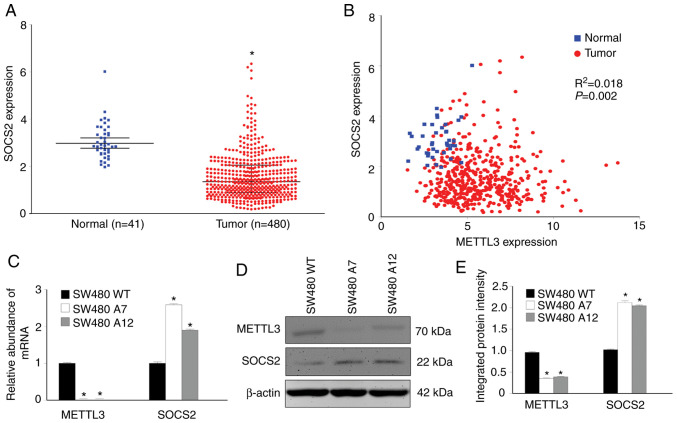
SOCS2 RNA levels are negatively correlated with METTL3 expression levels in CRC
To identify the downstream regulatory effectors controlling the inhibition of cell proliferation in METTL3-KO cells, we sought to determine whether METTL3 regulates the expression of SOCS2 to modulate the transcription of those proliferation-related genes. A previous study indicated a potential correlation between the expression levels of SOCS2 and METTL3 in hepatocellular cancer (37). We utilized the TCGA database to evaluate SOCS2 expression in CRC. In the same set of TCGA samples used for METTL3 analysis, we found a significant decrease in the SOCS2 RNA level in CRC (Fig. 3A). The correlation between the expression levels of METTL3 and SOCS2 was studied by linear regression analysis of data from the TCGA database. A significant inverse association between the expression levels of METTL3 and SOCS2 in CRC was identified (P<0.05; Fig. 3B), and the R2 coefficient was small (0.018). We considered that the correlation between METTL3 and SOCS2 in these TCGA data might not be strong but was significant. The actual correlation still needs in-depth investigation.
Figure 3.
SOCS2 is upregulated in colon cancer and downregulated in METTL3-KO SW480 cells. (A) TCGA database analysis revealed a lower expression level of SOCS2 in colon cancer tissues than in the paired normal tissues (*P<0.05). (B) Expression levels of SOCS2 and METTL3 were negatively correlated in colon cancer tissues. (C-E) METTL3-KO upregulated SOCS2 expression at both the (C) mRNA and (D and E) protein levels in SW480 cells (*P<0.05, compared with the SW480 WT cells). SOCS2, suppressor of cytokine signaling 2; METTL3, methyltransferase like 3; KO, knockout; SW480 A7 and SW480 A12, METTL3-KO SW480 cells.
The correlation between the levels of SOCS2 and METTL3 in CRC samples prompted us to investigate whether this association holds in SW480 cells. We measured the SOCS2 expression levels in METTL3-KO SW480 cells and compared them to those in control SW480 cells. Consistent with the pattern in the TCGA data, knockout of METTL3 was accompanied by SOCS2 upregulation (Fig. 3C-E). Our data thus imply that METTL3 may control SOCS2 expression in CRC.
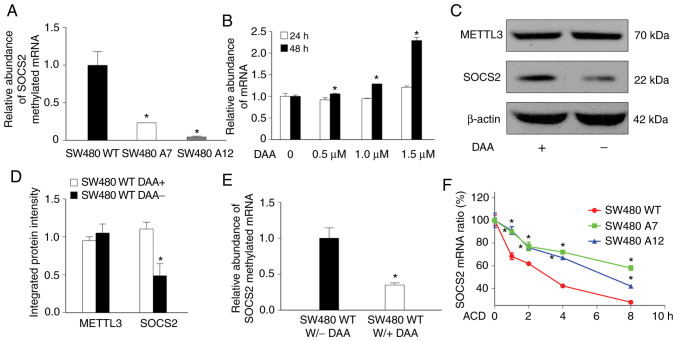
METTL3 controls SOCS2 expression by modulating methylation-mediated SOCS2 RNA degradation
To explore the underlying molecular mechanisms by which METTL3 controls SOCS2 expression, we sought to determine whether SOCS2 is a direct substrate of METTL3 for methylation. We first verified whether METTL3 maintains the methylation status of SOCS2 mRNA in SW480 cells. The MeRIP-qPCR results revealed a significant decrease in SOCS2 RNA m6A methylation in METTL3-KO SW480 cells compared with the control SW480 WT cells (Fig. 4A). To evaluate the effect of m6A modification on SOCS2 expression, we used the global methylation inhibitor DAA to block RNA methylation and quantified SOCS2 mRNA and protein expression in SW480 cells. The abundance of SOCS2 mRNA was increased in the DAA-treated SW480 cells in a DAA dose-dependent manner (P<0.05; Fig. 4B). Consistent with the results from METTL3-KO cells, DAA treatment increased the SOCS2 protein content (P<0.05; Fig. 4C and D). Since DAA globally inhibits all methyltransferase reactions, we used MeRIP-qPCR to confirm its demethylation of SOCS2 mRNA. A significant decrease in m6A-modified SOCS2 mRNA was detected in SW480 cells after DAA intervention (P<0.05; Fig. 4E).
Figure 4.
Methylation status of SOCS2 mRNA in SW480 cells. (A) Comparison of the SOCS2 mRNA methylation status between SW480 WT and METTL3-KO SW480 cells via MeRIP-qPCR (*P<0.05, compared with the SW480 WT cells). (B) Dose-dependent increase in SOCS2 mRNA levels in SW480 cells in response to demethylation treatment with DAA (*P<0.05, compared with non-treated group). (C and D) SOCS2 protein expression was upregulated after demethylation treatment with DAA (*P<0.05, compared with the SW380 WT DAA-group). (E) DAA appreciably decreased the m6A level in SOCS2 mRNA (*P<0.05, compared with the SW380 WT DAA-group). (F) METTL3-KO increased SOCS2 mRNA stability, showing a decreased mRNA decay rate (*P<0.05, compared with the SW480 WT cells). SOCS2, suppressor of cytokine signaling 2; METTL3, methyltransferase like 3; KO, knockout; SW480 A7 and SW480 A12, METTL3-KO SW480 cells; DAA, 3-deazaadenosine.
A previous study showed that RNA m6A methylation exerts its effects via modulation of RNA stability (8). To investigate this possibility, we carried out an RNA stability assay. New RNA synthesis was blocked with actinomycin D, and the decay rate of SOCS2 mRNA was observed to be lower in METTL3-KO SW480 cells than in control SW480 cells (P<0.05; Fig. 4F), suggesting that knockout of METTL3 significantly enhanced SOCS2 mRNA stability. Collectively, our findings revealed that METTL3 controls SOCS2 expression by modulating its mRNA stability.
Changes in SOCS2 expression impact LGR5 expression and disrupt colon cancer cell proliferation
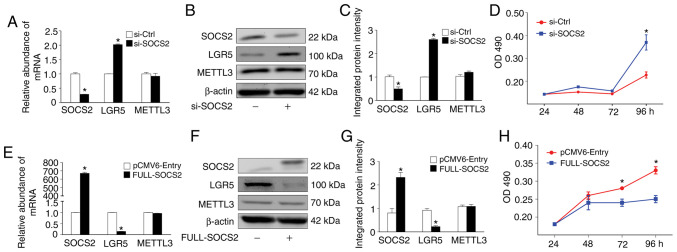
To define whether SOCS2 is an effector regulating colon cancer cell proliferation, we monitored the effects of modulating SOCS2 expression on SW480 cell proliferation. Treatment of cells with a SOCS2-specific siRNA and transfection with the FULL-SOCS2 plasmid effectively downregulated and upregulated SOCS2 expression, respectively (Fig. 5A-C and E-G). Accordingly, a significant increase and a marked decrease in the cell number were detected in siRNA-treated SW480 cells and SOCS2-overexpressing SW480 cells, respectively (Fig. 5D and H).
Figure 5.
Modulation of SOCS2 expression alters the proliferation ability of SW480 cells. (A-C) siRNA (si-SOCS2) was used to successfully knock down SOCS2 expression in SW480 cells. Knockdown of SOCS2 had minor impact on METTL3 expression but significantly increased LGR5 expression in SW480 cells (*P<0.05, compared with the si-Ctrl group). (D) Knockdown of SOCS2 enhanced SW480 cell proliferation, as determined by an MTS assay (*P<0.05, compared with the si-Ctrl group). (E-G) Transfection of the pCMV6-SOCS2 plasmid upregulated SOCS2 expression and decreased LGR5 expression in SW480 cells (*P<0.05, compared with the pCMV6-Entry group). SOCS2 overexpression had minor impact on METTL3 expression (P>0.05, compared with the pCMV6-Entry group). (H) SOCS2 overexpression decreased SW480 cell proliferation, as determined by an MTS assay (*P<0.05, compared with the pCMV6-Entry group). SOCS2, suppressor of cytokine signaling 2; METTL3, methyltransferase like 3; LGR5, leucine-rich repeat-containing G protein-coupled receptor 5.
Previous studies have demonstrated that SOCS2 acts as a negative feedback regulator in multiple signaling pathways. Dysregulation of SOCS2 crucially modulates the cell cycle progression and apoptosis of cancer cells (38–40). Recent research advances suggest that CSCs may be the origin of colon tumorigenesis and tumor growth maintenance (41). As an important CSC marker, LGR5 may enhance the stemness and chemoresistance development of tumor cells (26,27,42). Hence, we measured the abundance of LGR5 in SW480 cells with SOCS2 downregulation or overexpression. SOCS2 knockdown via siRNA significantly elevated both the mRNA and protein expression levels of LGR5 in the SW480 cells (P<0.05; Fig. 5A-C). Correspondingly, SOCS2 overexpression appreciably suppressed LGR5 expression (P<0.05; Fig. 5E-G). Taken together, these results suggest that SOCS2 may regulate colon cancer cell proliferation via LGR5.
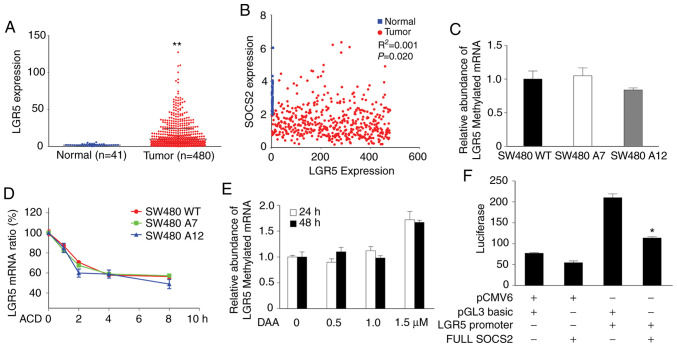
SOCS2 suppresses LGR5 promoter activity
First, we explored the association of LGR5 and SOCS2 in data from the TCGA database. In the same set of TCGA samples used in the present study, we found a distinct increase in the LGR5 RNA level in CRC (Fig. 6A). Although the R2 coefficient was too small to be considered to indicate a strong correlation, linear regression analysis implied a potential negative correlation between the expression levels of SOCS2 and LGR5 in CRC (P<0.05; Fig. 6B). This finding prompted us to investigate the mechanism underlying the correlation between SOCS2 and LGR5. To exclude direct regulatory effects of METTL3 on LGR5 expression, MeRIP-qPCR was applied. The m6A methylation level of LGR5 did not differ between METTL3-KO SW480 cells and control SW480 WT cells (P>0.05; Fig. 6C), nor did METTL3 knockout impact the stability of LGR5 mRNA in SW480 cells (P>0.05; Fig. 6D). Furthermore, DAA treatment had little impact on the stability of LGR5 mRNA in SW480 cells (P>0.05; Fig. 6E). These data did not support a direct modulatory effect of METTL3 on LGR5, indicating the necessity of SOCS2 for the regulation of LGR5 by METTL3. SW480 cells were cotransfected with the FULL-SOCS2 plasmid or the empty vector (as the control) and the luciferase reporter vector containing the LGR5 promoter region, and luciferase activity was then measured. Our luciferase activity assay results showed that SOCS2 overexpression effectively repressed LGR5 promoter activity in SW480 cells, suggesting a suppressive role of SOCS2 in modulating LGR5 transcription (P<0.05; Fig. 6F).
Figure 6.
METTL3 modulates LGR5 transcription through m6A-mediated changes in SOCS2 expression rather than through direct regulatory mechanisms. (A) TCGA database analysis revealed an induction of LGR5 transcription in colon cancer tissues when compared with normal tissues (**P<0.01, compared with the normal tissues). (B) Expression levels of SOCS2 and LGR5 were negatively correlated in colon cancer tissues. (C) METTL3 knockout (KO) did not obviously impact LGR5 mRNA methylation (as measured by MeRIP-qPCR). (D) METTL3 KO had a minor effect on the LGR5 mRNA decay rate. (E) DAA treatment did not impact LGR5 expression in SW480 cells. (F) Luciferase reporter assay results confirmed that SOCS2 negatively controls LGR5 promoter-driven luciferase activity (*P<0.05, pGL3 basic-LGR5 promoter group vs. FULL SOCS2-LGR5 promoter group). METTL3, methyltransferase like 3; LGR5, leucine-rich repeat-containing G protein-coupled receptor 5; SOCS2, suppressor of cytokine signaling 2; TCGA, The Cancer Genome Atlas; SW480 A7 and SW480 A12, METTL3-KO SW480 cells; DAA, 3-deazaadenosine.
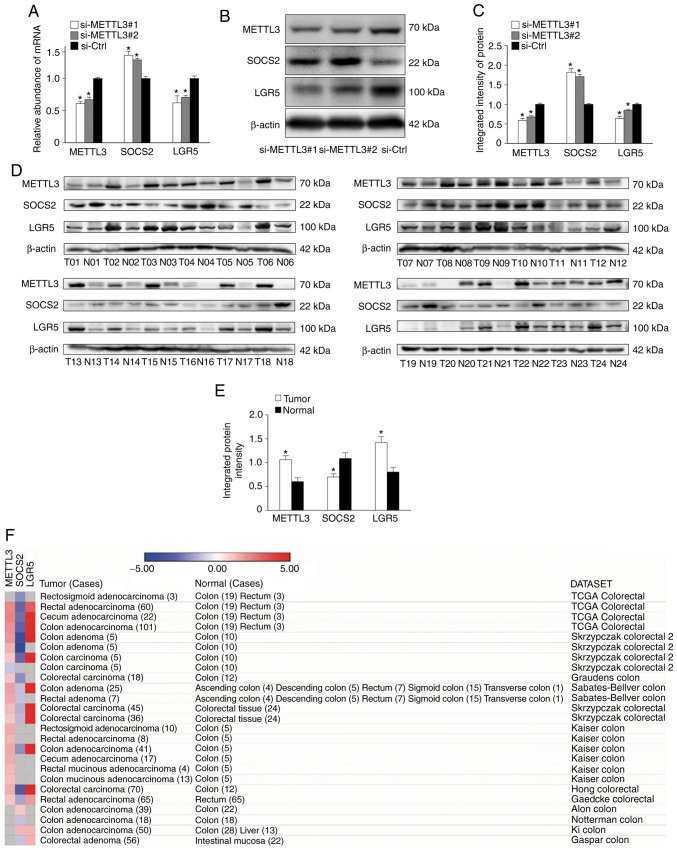
Measurement of SOCS2 and METTL3 expression and their correlation in colon cancer tumorigenesis
To rule out the compensatory effect of other molecules on SOCS2 and LGR5 expression in stable METTL3-KO SW480 cells, we used two separate siRNAs (si-METTL3#1 and si-METTL3#2) to knockdown METTL3 expression in SW480 cells. Transient inhibition of METTL3 via either siRNA resulted in significantly increased SOCS2 expression but significantly decreased LGR5 expression at both the mRNA and protein levels (P<0.05; Fig. 7A-C).
Figure 7.
Correlations among METTL3, SOCS2 and LGR5 expression levels in CRC. (A-C) Knockdown of METTL3 using siRNA (si-METTL3#1 and si-METTL3#2) significantly upregulated SOCS2 expression but downregulated LGR5 expression in SW480 cells (*P<0.05, compared with the si-Ctrl group). (D and E) Western blotting analysis of 24 paired tissues collected from CRC patients showed high protein levels of METTL3 and LGR5 and a relatively low protein level of SOCS2 in colon cancer (T, colon tumor samples; N, adjacent normal colon tissues; *P<0.05, compared to Normal tissues). (F) Visualization of expression profiles of METTL3, SOCS2 and LGR5 in CRC through the Oncomine database. METTL3 and LGR5 were upregulated in CRC datasets. In contrast, SOCS2 was downregulated in CRC datasets. CRC, colorectal cancer; SOCS2, suppressor of cytokine signaling 2; METTL3, methyltransferase like 3; LGR5, leucine-rich repeat-containing G protein-coupled receptor 5.
Moreover, we collected 24 paired samples (i.e., tumor tissues and paired adjacent normal colon tissues) from patients with CRC in the Department of Gastroenterology Surgery, Sun Yat-Sen Memorial Hospital. The protein expression levels of METTL3, SOCS2 and LGR5 were measured in the 24 paired CRC samples and histologically normal adjacent tissues using western blotting. The expression levels of METTL3 and LGR5 were increased in colon tumor samples compared to the paired adjacent colon tissues (fold change ≥1.5) in 19 (79.2%) and 20 (83.3%) cases, respectively. In contrast, the level of SOCS2 was lower in the tumor samples (fold change ≤0.5) in 18 (75.0%) cases (Fig. 7D and Table I). Additionally, we analyzed the correlations between the expression levels of these three genes and clinicopathological features (sex, age, TNM stage). Upregulation of METTL3 or LGR5 was not correlated with sex, age, tumor size, or TNM stage (P>0.05; Table I). Consistent with this result, downregulation of SOCS2 was not associated with these clinical features (P>0.05; Table I). These results demonstrated that in general, the expression levels of METTL3 and LGR5 are increased in CRC, whereas that of SOCS2 is decreased.
Table I.
Association between patient characteristics and gene expression in 24 paired CRC cases.
| Expression of METTL3a | Fisher's exact test | Expression of SOCS2a | Fisher's exact test | Expression of LGR5a | Fisher's exact test | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. of patients n (%) | Low | High | P-value | Low | High | P-value | Low | High | P-value | |
| Total, n (%) | 24 | 5 (20.8) | 19 (79.2) | 18 (75.0) | 6 (25.0) | 4 (16.7) | 20 (83.3) | |||
| Sex | ||||||||||
| Male | 12 (50.0) | 2 | 10 | 0.64 | 8 | 4 | 0.64 | 2 | 10 | >0.99 |
| Female | 12 (50.0) | 4 | 8 | 10 | 2 | 2 | 10 | |||
| Mean age (years) | 61±11.64 | |||||||||
| ≤60 | 10 (41.7) | 1 | 9 | 0.36 | 7 | 3 | 0.67 | 3 | 7 | 0.27 |
| >60 | 14 (58.3) | 4 | 10 | 11 | 3 | 1 | 13 | |||
| Tumor size (cm) | ||||||||||
| ≤5 | 10 (41.7) | 3 | 7 | 0.61 | 8 | 2 | >0.99 | 2 | 8 | >0.99 |
| >5 | 14 (58.3) | 2 | 12 | 10 | 4 | 2 | 12 | |||
| Pathologic type | ||||||||||
| Adenocarcinoma | 24 | 5 | 19 | 18 | 6 | 4 | 20 | |||
| Other | 0 | |||||||||
| pT grade | ||||||||||
| Ta, Tis, T1 | 2 (8.3) | 0 | 2 | 1.00 | 2 | 0 | >0.99 | 1 | 1 | 0.31 |
| T2-T4 | 22 (91.7) | 5 | 17 | 16 | 6 | 3 | 19 | |||
| pN grade | ||||||||||
| N0 | 13 (54.2) | 1 | 12 | 0.14 | 10 | 3 | >0.99 | 1 | 12 | 0.30 |
| N1, N2 | 11 (45.8) | 4 | 7 | 8 | 3 | 3 | 8 | |||
| pM grade | ||||||||||
| M0 | 18 (75.0) | 4 | 14 | 1.00 | 13 | 5 | 0.36 | 2 | 16 | 0.25 |
| M1 | 6 (25.0) | 1 | 5 | 3 | 3 | 2 | 4 | |||
| TNM staging | ||||||||||
| I | 5 (20.8) | 0 | 5 | 0.61b | 3 | 2 | 0.77b | 1 | 4 | 0.33b |
| II | 7 (29.2) | 2 | 5 | 5 | 2 | 0 | 7 | |||
| III | 7 (29.2) | 2 | 5 | 6 | 1 | 1 | 6 | |||
| IV | 5 (20.8) | 1 | 4 | 4 | 1 | 2 | 3 | |||
Protein expression in tumor sample in contrast to adjacent (>5 cm) normal mucosa.
Chi-square test P-value. CRC, colorectal cancer; METTL3, methyltransferase like 3; SOCS2, suppressor of cytokine signaling 2; LGR5, leucine-rich repeat-containing G protein-coupled receptor 5.
To further evaluate the clinical value of our findings, we searched the expression profiles of METTL3, SOCS2 and LGR5 in CRC through the Oncomine database (43–52). Regarding METTL3, analysis confirmed that METTL3 was upregulated in CRC in 13/20 datasets (P<0.05; Fig. 7F and Table SIII). In contrast, analysis revealed that SOCS2 was downregulated in CRC in 13/19 datasets (P<0.05; Fig. 7 and Table SIII). Accordingly, LGR5 expression was significantly increased in all 13 CRC datasets (P<0.05; Fig. 7F and Table SIII).
Discussion
The present study indicates that methyltransferase like 3 (METTL3) is generally upregulated in colorectal cancer (CRC), contributing to the maintenance of m6A modification in cancer cells. As a major m6A writer, METTL3 accelerates suppressor of cytokine signaling 2 (SOCS2) mRNA decay to maintain a high leucine-rich repeat-containing G protein-coupled receptor 5 (LGR5) expression level in colon cancer cells, resulting in enhanced tumorigenicity. Thus, our results provide additional evidence that aberrant METTL3 expression may be involved in tumorigenesis. As the most prevalent internal modification of RNA, m6A modification regulates many biological processes of RNA, including decay, splicing, translation and transport (53). Maintenance of m6A RNA methylation is crucial for embryonic stem cell pluripotency (54,55). Emerging evidence indicates that the cellular status of m6A modification may impact the pathological processes of various types of cancers, including acute myeloid leukemia, glioblastoma, lung cancer and liver cancer (56). METTL3 is often upregulated in malignancies and elicits potentially oncogenic effects by epigenetically silencing the expression of specific genes, such as ADAM19 and SOCS2 (15,37). Previous studies demonstrated that the expression level of METTL3 can critically alter the cell cycle and apoptosis processes in hepatic cancer and acute myeloid leukemia (37,57). Knockdown of METTL3 increases chemosensitivity and radiosensitivity in pancreatic cancer (19).
Having confirmed an elevated expression level of METTL3 in CRC tissues from the TCGA database, we generated METTL3-KO colon cancer (SW480) cell lines. Our m6A quantification analysis results confirmed that CRISPR/Cas9-mediated METTL3 knockout resulted in inhibition of both METTL3 expression and m6A modification in the cells. Functionally, knockout of METTL3 significantly reduced the cell proliferation ability. METTL3 acts as a key m6A methyltransferase and thus may promote cell proliferation via the installation of m6A on key genes critical to cell growth (58–60). Indeed, our data suggest that elevated expression of METTL3 accelerates SOCS2 mRNA decay to maintain a high level of LGR5 and thus promotes the proliferation of colon cancer cells.
SOCS2, a member of the SOCS family, regulates multiple cytokine-induced intracellular signaling pathways essential to numerous biological processes, including immune responses (61,62). For example, SOCS2 can act as a downstream factor of the JAK/STAT pathway, regulating signaling activity via negative feedback (63). Accumulating evidence suggests a carcinostatic effect of SOCS2 in numerous cancers. Disruption of SOCS2 promotes colon tumorigenesis in Apc (Min/+) mice (64). On the other hand, overexpression of SOCS2 has an antiproliferative effect on Caco-2 colon cancer cells (65). A meta-analysis integrating more than 600 CRC patients and normal samples from different datasets revealed that SOCS2 expression is markedly reduced in CRC and may be a novel diagnostic biomarker for CRC (66). Indeed, the JAK/STAT signaling pathway is often dysregulated in CRC (67). Our TCGA database analysis results confirmed the downregulation of SOCS2 in CRC. Furthermore, our data supported the hypothesis that SOCS2 may play an antioncogenic role in colon malignancies. We observed a negative association between SOCS2 expression and the cell proliferation ability in colon cancer cells. Knockdown of SOCS2 increased the proliferation of colon cancer cells, while overexpression of SOCS2 effectively inhibited cell proliferation.
The molecular mechanisms underlying the dysregulation of SOCS2 and SOCS2-mediated cell proliferation in CRC are still unclear. Our data revealed a negative correlation between METTL3 and SOCS2 in clinical CRC tissues and colon cancer cells. Moreover, knockdown of METTL3 in colon cancer cells increased the expression of SOCS2. Given that METTL3 is the predominant m6A RNA methyltransferase and that mRNA stability is confirmed as a cellular biological processes regulated by m6A modification, we speculated that METTL3 may control SOCS2 expression through modulation of SOCS2 RNA stability. The results of our MeRIP-qPCR and RNA decay experiments revealed that METTL3 may directly install m6A on SOCS2 mRNA and decrease its stability. Inhibition of global demethylation with DAA, a global methylation inhibitor, further confirmed the effect of RNA methylation on SOCS2 expression. The effect of DAA on SOCS2 expression was dose-dependent and showed a positive correlation between m6A demethylation and SOCS2 expression.
One pathological hallmark of cancer cells is their potential for uncontrolled self-renewal (68). Targeting biomarkers of significance in self-renewal may be an effective strategy to reverse tumorigenesis. LGR5, which can maintain continuous self-renewal of the intestinal epithelium, is considered a cancer stem cell (CSC) marker in CRC (69). Cancer cells with LGR5 expression in CRC tissues possess an enhanced self-renewal capacity and have been referred to as colon CSCs (26,27). A meta-analysis revealed that tumor tissues from patients with CRC often show upregulated LGR5 expression and that an increased level of LGR5 could be a prognostic factor for CRC (70). Consistent with these results, the results of our TCGA database analysis showed a higher LGR5 expression level in CRC tissues than on their normal counterparts; this finding was further confirmed by our Oncomine database analysis in a larger clinical cohort. Moreover, we collected clinical CRC tissue samples from our hospital to assess the protein expression profiles of METTL3, SOCS2 and LGR5. METTL3 and LGR5 were highly expressed in our CRC samples. Although SOCS2 showed highly heterogeneous expression, the statistical analysis results supported the downregulation of SOCS2 in our CRC samples. Accordingly, the decreased SOCS2 expression level was negatively correlated with the elevated LGR5 expression level and increased tumor spheroid formation rate in colon cancer cell lines, consistent with a previous meta-analysis (55). Alteration of either METTL3 or SOCS2 expression can cause reciprocal alterations in the LGR5 expression level in SW480 cells. Interestingly, METTL3 does not appear to directly regulate LGR5 mRNA stability through m6A methylation but instead appears to maintain LGR5 expression through suppression of SOCS2. However, several limitations should be resolved to fully reveal the precise mechanisms of METTL3 facilitating CRC tumorigenicity. Notably, the expression of METTL3, SOCS2 and LGR5 in our CRC samples was not significantly correlated with the clinicopathological features of the patients (sex, age, tumor size, pathological type and TNM stage). This statistically insignificant correlation may be due to the small enrolled sample size. Moreover, the present study did not measure the gene expression of METTL3, SOCS2 and LGR5 in CRC samples. Both a comprehensive study with a larger sample size and a multicenter clinical study would be conducted to fully evaluate the therapeutic potential of METTL3 for CRC.
In conclusion, our study revealed elevated METTL3 expression in CRC. Upregulation of METTL3 was associated with decreased expression of SOCS2 and promoted tumor cell proliferation via induction of LGR5. To our knowledge, our finding provides the first characterization of the underlying mechanism of METTL3/m6A-mediated posttranscriptional modification in CRC tumorigenesis, suggesting the therapeutic potential of targeting this axis in CRC.
Supplementary Material
Acknowledgements
Not applicable.
Glossary
Abbreviations
- CRC
colorectal cancer
- m6A
N6-methyladenosine
- METTL3
methyltransferase like 3
- METTL14
methyltransferase like 14
- WTAP
Wilms tumor 1-associated protein
- FTO
fat mass and obesity-associated protein
- ALKBH5
RNA demethylase alkB homolog 5
- YTH
YT521-B homology
- CSC
cancer stem cell
- SOCS
suppressor of cytokine signaling
- LGR5
leucine-rich repeat-containing G protein-coupled receptor 5
- TCGA
The Cancer Genome Atlas
- MeRIP-qPCR
m6A-RNA immunoprecipitation-qPCR
- ACD
actinomycin D
- DAA
3-deazaadenosine
- METTL3-KO
METTL3-knockout
Funding
The present study was supported by funding from the Nebraska Cancer and Smoking Disease Research Program (LB595) and the National Natural Science Foundation of China (nos. 81370475 and 81970464). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Nebraska Cancer and Smoking Disease Research Program or the National Natural Science Foundation of China.
Availability of data and materials
All data generated or analyzed in the present study (and its supplementary information files) are fully available without restrictions.
Authors' contributions
JX, QC, TY and XC conceived the project. JX, TC, KT, AG and RL carried out the experiments. JX, AG, QC, TY and XC analyzed and interpreted the data. JX, NWM and XC wrote the study. NWM and RL participated in the bioinformatics research. All authors read and approved the manuscript and agree to be accountable for all aspects of the research in ensuring that the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics approval and consent to participate
All enrolled patients and their respective guardians provided written consent prior to the use of clinical samples and pathological features for research purposes. The overall protocol strictly adhered to the guidelines of the Institutional Review Board Committee of Sun Yat-Sen Memorial Hospital, Sun Yat-Sen University (approval no. 58, 2016 record for Ethics).
Patient consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare.
References
- 1.Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66:683–691. doi: 10.1136/gutjnl-2015-310912. [DOI] [PubMed] [Google Scholar]
- 2.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 3.Dekker E, Tanis PJ, Vleugels JLA, Kasi PM, Wallace MB. Colorectal cancer. Lancet. 2019;394:1467–1480. doi: 10.1016/S0140-6736(19)32319-0. [DOI] [PubMed] [Google Scholar]
- 4.Prasetyanti PR, van Hooff SR, van Herwaarden T, de Vries N, Kalloe K, Rodermond H, van Leersum R, de Jong JH, Franitza M, Nürnberg P, et al. Capturing colorectal cancer inter-tumor heterogeneity in patient-derived xenograft (PDX) models. Int J Cancer. 2019;144:366–371. doi: 10.1002/ijc.31767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahasneh A, Al-Shaheri F, Jamal E. Molecular biomarkers for an early diagnosis, effective treatment and prognosis of colorectal cancer: Current updates. Exp Mol Pathol. 2017;102:475–483. doi: 10.1016/j.yexmp.2017.05.005. [DOI] [PubMed] [Google Scholar]
- 6.Sepulveda AR, Hamilton SR, Allegra CJ, Grody W, Cushman-Vokoun AM, Funkhouser WK, Kopetz SE, Lieu C, Lindor NM, Minsky BD, et al. Molecular biomarkers for the evaluation of colorectal cancer: Guideline from the American society for clinical pathology, college of American Pathologists, Association for Molecular Pathology, and the American Society of Clinical Oncology. J Clin Oncol. 2017;35:1453–1486. doi: 10.1200/JCO.2016.71.9807. [DOI] [PubMed] [Google Scholar]
- 7.Wang S, Sun C, Li J, Zhang E, Ma Z, Xu W, Li H, Qiu M, Xu Y, Xia W, et al. Roles of RNA methylation by means of N6-methyladenosine (m6A) in human cancers. Cancer Lett. 2017;408:112–120. doi: 10.1016/j.canlet.2017.08.030. [DOI] [PubMed] [Google Scholar]
- 8.Wang X, Lu Z, Gomez A, Hon GC, Yue Y, Han D, Fu Y, Parisien M, Dai Q, Jia G, et al. N6-methyladenosine-dependent regulation of messenger RNA stability. Nature. 2014;505:117–120. doi: 10.1038/nature12730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zheng G, Dahl JA, Niu Y, Fedorcsak P, Huang CM, Li CJ, Vågbø CB, Shi Y, Wang WL, Song SH, et al. ALKBH5 is a mammalian RNA demethylase that impacts RNA metabolism and mouse fertility. Mol Cell. 2013;49:18–29. doi: 10.1016/j.molcel.2012.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhao X, Yang Y, Sun BF, Shi Y, Yang X, Xiao W, Hao YJ, Ping XL, Chen YS, Wang WJ, et al. FTO-dependent demethylation of N6-methyladenosine regulates mRNA splicing and is required for adipogenesis. Cell Res. 2014;24:1403–1419. doi: 10.1038/cr.2014.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fustin JM, Doi M, Yamaguchi Y, Hida H, Nishimura S, Yoshida M, Isagawa T, Morioka MS, Kakeya H, Manabe I, et al. RNA-methylation-dependent RNA processing controls the speed of the circadian clock. Cell. 2013;155:793–806. doi: 10.1016/j.cell.2013.10.026. [DOI] [PubMed] [Google Scholar]
- 12.Wang Y, Li Y, Toth JI, Petroski MD, Zhang Z, Zhao JC. N6-methyladenosine modification destabilizes developmental regulators in embryonic stem cells. Nat Cell Biol. 2014;16:191–198. doi: 10.1038/ncb2902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang S, Zhao BS, Zhou A, Lin K, Zheng S, Lu Z, Chen Y, Sulman EP, Xie K, Bögler O, et al. m6A demethylase ALKBH5 maintains tumorigenicity of glioblastoma stem-like cells by sustaining FOXM1 expression and cell proliferation program. Cancer Cell. 2017;31:591–606.e6. doi: 10.1016/j.ccell.2017.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li Z, Weng H, Su R, Weng X, Zuo Z, Li C, Huang H, Nachtergaele S, Dong L, Hu C, et al. FTO plays an oncogenic role in acute myeloid leukemia as a N6-methyladenosine RNA demethylase. Cancer Cell. 2017;31:127–141. doi: 10.1016/j.ccell.2016.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cui Q, Shi H, Ye P, Li L, Qu Q, Sun G, Sun G, Lu Z, Huang Y, Yang CG, et al. m6A RNA methylation regulates the self-renewal and tumorigenesis of glioblastoma stem cells. Cell Rep. 2017;18:2622–2634. doi: 10.1016/j.celrep.2017.02.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin S, Choe J, Du P, Triboulet R, Gregory RI. The m(6)A methyltransferase METTL3 promotes translation in human cancer cells. Mol Cell. 2016;62:335–345. doi: 10.1016/j.molcel.2016.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang Q, Chen C, Ding Q, Zhao Y, Wang Z, Chen J, Jiang Z, Zhang Y, Xu G, Zhang J, et al. METTL3-mediated m6A modification of HDGF mRNA promotes gastric cancer progression and has prognostic significance. Gut. 2020;69:1193–1205. doi: 10.1136/gutjnl-2019-319639. [DOI] [PubMed] [Google Scholar]
- 18.Yue B, Song C, Yang L, Cui R, Cheng X, Zhang Z, Zhao G. METTL3-mediated N6-methyladenosine modification is critical for epithelial-mesenchymal transition and metastasis of gastric cancer. Mol Cancer. 2019;18:142. doi: 10.1186/s12943-019-1065-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taketo K, Konno M, Asai A, Koseki J, Toratani M, Satoh T, Doki Y, Mori M, Ishii H, Ogawa K. The epitranscriptome m6A writer METTL3 promotes chemo- and radioresistance in pancreatic cancer cells. Int J Oncol. 2018;52:621–629. doi: 10.3892/ijo.2017.4219. [DOI] [PubMed] [Google Scholar]
- 20.Wu M, Song D, Li H, Yang Y, Ma X, Deng S, Ren C, Shu X. Negative regulators of STAT3 signaling pathway in cancers. Cancer Manag Res. 2019;11:4957–4969. doi: 10.2147/CMAR.S206175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jiang M, Zhang WW, Liu P, Yu W, Liu T, Yu J. Dysregulation of SOCS-mediated negative feedback of cytokine signaling in carcinogenesis and its significance in cancer treatment. Front Immunol. 2017;8:70. doi: 10.3389/fimmu.2017.00070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sutherland KD, Lindeman GJ, Choong DY, Wittlin S, Brentzell L, Phillips W, Campbell IG, Visvader JE. Differential hypermethylation of SOCS genes in ovarian and breast carcinomas. Oncogene. 2004;23:7726–7733. doi: 10.1038/sj.onc.1207787. [DOI] [PubMed] [Google Scholar]
- 23.Slattery ML, Lundgreen A, Hines LM, Torres-Mejia G, Wolff RK, Stern MC, John EM. Genetic variation in the JAK/STAT/SOCS signaling pathway influences breast cancer-specific mortality through interaction with cigarette smoking and use of aspirin/NSAIDs: The Breast Cancer Health Disparities Study. Breast Cancer Res Treat. 2014;147:145–158. doi: 10.1007/s10549-014-3071-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Das R, Gregory PA, Fernandes RC, Denis I, Wang Q, Townley SL, Zhao SG, Hanson AR, Pickering MA, Armstrong HK, et al. MicroRNA-194 promotes prostate cancer metastasis by inhibiting SOCS2. Cancer Res. 2017;77:1021–1034. doi: 10.1158/0008-5472.CAN-16-2529. [DOI] [PubMed] [Google Scholar]
- 25.Vitali C, Bassani C, Chiodoni C, Fellini E, Guarnotta C, Miotti S, Sangaletti S, Fuligni F, De Cecco L, Piccaluga PP, et al. SOCS2 controls proliferation and stemness of hematopoietic cells under stress conditions and its deregulation marks unfavorable acute leukemias. Cancer Res. 2015;75:2387–2399. doi: 10.1158/0008-5472.CAN-14-3625. [DOI] [PubMed] [Google Scholar]
- 26.de Sousa e Melo F, Kurtova AV, Harnoss JM, Kljavin N, Hoeck JD, Hung J, Anderson JE, Storm EE, Modrusan Z, Koeppen H, et al. A distinct role for Lgr5+ stem cells in primary and metastatic colon cancer. Nature. 2017;543:676–680. doi: 10.1038/nature21713. [DOI] [PubMed] [Google Scholar]
- 27.Shimokawa M, Ohta Y, Nishikori S, Matano M, Takano A, Fujii M, Date S, Sugimoto S, Kanai T, Sato T. Visualization and targeting of LGR5+ human colon cancer stem cells. Nature. 2017;545:187–192. doi: 10.1038/nature22081. [DOI] [PubMed] [Google Scholar]
- 28.Stanisavljević L, Myklebust MP, Leh S, Dahl O. LGR5 and CD133 as prognostic and predictive markers for fluoropyrimidine-based adjuvant chemotherapy in colorectal cancer. Acta Oncol. 2016;55:1425–1433. doi: 10.1080/0284186X.2016.1201215. [DOI] [PubMed] [Google Scholar]
- 29.Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D, Amin N, Schwikowski B, Ideker T. Cytoscape: A software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13:2498–2504. doi: 10.1101/gr.1239303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 31.Li HB, Tong J, Zhu S, Batista PJ, Duffy EE, Zhao J, Bailis W, Cao G, Kroehling L, Chen Y, et al. m6A mRNA methylation controls T cell homeostasis by targeting the IL-7/STAT5/SOCS pathways. Nature. 2017;548:338–342. doi: 10.1038/nature23450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Karoopongse E, Yeung C, Byon J, Ramakrishnan A, Holman ZJ, Jiang PY, Yu Q, Deeg HJ, Marcondes AM. The KDM2B-let-7b-EZH2 axis in myelodysplastic syndromes as a target for combined epigenetic therapy. PLoS One. 2014;9:e107817. doi: 10.1371/journal.pone.0107817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jing N, Huang T, Guo H, Yang J, Li M, Chen Z, Zhang Y. LncRNA CASC15 promotes colon cancer cell proliferation and metastasis by regulating the miR4310/LGR5/Wnt/β-catenin signaling pathway. Mol Med Rep. 2018;18:2269–2276. doi: 10.3892/mmr.2018.9191. [DOI] [PubMed] [Google Scholar]
- 34.Gopalan V, Ebrahimi F, Islam F, Vider J, Qallandar OB, Pillai S, Lu CT, Lam AK. Tumour suppressor properties of miR-15a and its regulatory effects on BCL2 and SOX2 proteins in colorectal carcinomas. Exp Cell Res. 2018;370:245–253. doi: 10.1016/j.yexcr.2018.06.025. [DOI] [PubMed] [Google Scholar]
- 35.Alcantara-Flores E, Brechu-Franco AE, Garcia-Lopez P, Rocha-Zavaleta L, Lopez-Marure R, Martinez-Vazquez M. Argentatin B inhibits proliferation of prostate and colon cancer cells by inducing cell senescence. Molecules. 2015;20:21125–21137. doi: 10.3390/molecules201219757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gong S, Xu D, Zhu J, Zou F, Peng R. Efficacy of the MEK inhibitor cobimetinib and its potential application to colorectal cancer cells. Cell Physiol Biochem. 2018;47:680–693. doi: 10.1159/000490022. [DOI] [PubMed] [Google Scholar]
- 37.Chen M, Wei L, Law CT, Tsang FH, Shen J, Cheng CL, Tsang LH, Ho DW, Chiu DK, Lee JM, et al. RNA N6-methyladenosine methyltransferase-like 3 promotes liver cancer progression through YTHDF2-dependent posttranscriptional silencing of SOCS2. Hepatology. 2018;67:2254–2270. doi: 10.1002/hep.29683. [DOI] [PubMed] [Google Scholar]
- 38.Zhao X, Zhang W, Ji W. miR-196b is a prognostic factor of human laryngeal squamous cell carcinoma and promotes tumor progression by targeting SOCS2. Biochem Biophys Res Commun. 2018;501:584–592. doi: 10.1016/j.bbrc.2018.05.052. [DOI] [PubMed] [Google Scholar]
- 39.Zhou Y, Zhang Z, Wang N, Chen J, Zhang X, Guo M, John ZL, Wang Q. Suppressor of cytokine signalling-2 limits IGF1R-mediated regulation of epithelial-mesenchymal transition in lung adenocarcinoma. Cell Death Dis. 2018;9:429. doi: 10.1038/s41419-018-0457-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chhabra Y, Wong HY, Nikolajsen LF, Steinocher H, Papadopulos A, Tunny KA, Meunier FA, Smith AG, Kragelund BB, Brooks AJ, et al. A growth hormone receptor SNP promotes lung cancer by impairment of SOCS2-mediated degradation. Oncogene. 2018;37:489–501. doi: 10.1038/onc.2017.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hatano Y, Fukuda S, Hisamatsu K, Hirata A, Hara A, Tomita H. Multifaceted Interpretation of Colon Cancer Stem Cells. Int J Mol Sci. 2017;18:1446. doi: 10.3390/ijms18071446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen X, Wei B, Han X, Zheng Z, Huang J, Liu J, Huang Y, Wei H. LGR5 is required for the maintenance of spheroid-derived colon cancer stem cells. Int J Mol Med. 2014;34:35–42. doi: 10.3892/ijmm.2014.1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Skrzypczak M, Goryca K, Rubel T, Paziewska A, Mikula M, Jarosz D, Pachlewski J, Oledzki J, Ostrowski J. Modeling oncogenic signaling in colon tumors by multidirectional analyses of microarray data directed for maximization of analytical reliability. PLoS One. 2010;5:e13091. doi: 10.1371/journal.pone.0013091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Graudens E, Boulanger V, Mollard C, Mariage-Samson R, Barlet X, Gremy G, Couillault C, Lajemi M, Piatier-Tonneau D, Zaborski P, et al. Deciphering cellular states of innate tumor drug responses. Genome Biol. 2006;7:R19. doi: 10.1186/gb-2006-7-3-r19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sabates-Bellver J, Van der Flier LG, de Palo M, Cattaneo E, Maake C, Rehrauer H, Laczko E, Kurowski MA, Bujnicki JM, Menigatti M, et al. Transcriptome profile of human colorectal adenomas. Mol Cancer Res. 2007;5:1263–1275. doi: 10.1158/1541-7786.MCR-07-0267. [DOI] [PubMed] [Google Scholar]
- 46.Kaiser S, Park YK, Franklin JL, Halberg RB, Yu M, Jessen WJ, Freudenberg J, Chen X, Haigis K, Jegga AG, et al. Transcriptional recapitulation and subversion of embryonic colon development by mouse colon tumor models and human colon cancer. Genome Biol. 2007;8:R131. doi: 10.1186/gb-2007-8-7-r131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hong Y, Downey T, Eu KW, Koh PK, Cheah PY. A ‘metastasis-prone’ signature for early-stage mismatch-repair proficient sporadic colorectal cancer patients and its implications for possible therapeutics. Clin Exp Metastasis. 2010;27:83–90. doi: 10.1007/s10585-010-9305-4. [DOI] [PubMed] [Google Scholar]
- 48.Gaedcke J, Grade M, Jung K, Camps J, Jo P, Emons G, Gehoff A, Sax U, Schirmer M, Becker H, et al. Mutated KRAS results in overexpression of DUSP4, a MAP-kinase phosphatase, and SMYD3, a histone methyltransferase, in rectal carcinomas. Genes Chromosomes Cancer. 2010;49:1024–1034. doi: 10.1002/gcc.20811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Alon U, Barkai N, Notterman DA, Gish K, Ybarra S, Mack D, Levine AJ. Broad patterns of gene expression revealed by clustering analysis of tumor and normal colon tissues probed by oligonucleotide arrays. Proc Natl Acad Sci USA. 1999;96:6745–6750. doi: 10.1073/pnas.96.12.6745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Notterman DA, Alon U, Sierk AJ, Levine AJ. Transcriptional gene expression profiles of colorectal adenoma, adenocarcinoma, and normal tissue examined by oligonucleotide arrays. Cancer Res. 2001;61:3124–3130. [PubMed] [Google Scholar]
- 51.Ki DH, Jeung HC, Park CH, Kang SH, Lee GY, Lee WS, Kim NK, Chung HC, Rha SY. Whole genome analysis for liver metastasis gene signatures in colorectal cancer. Int J Cancer. 2007;121:2005–2012. doi: 10.1002/ijc.22975. [DOI] [PubMed] [Google Scholar]
- 52.Gaspar C, Cardoso J, Franken P, Molenaar L, Morreau H, Moslein G, Sampson J, Boer JM, de Menezes RX, Fodde R. Cross-species comparison of human and mouse intestinal polyps reveals conserved mechanisms in adenomatous polyposis coli (APC)-driven tumorigenesis. Am J Pathol. 2008;172:1363–1380. doi: 10.2353/ajpath.2008.070851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dominissini D, Moshitch-Moshkovitz S, Schwartz S, Salmon-Divon M, Ungar L, Osenberg S, Cesarkas K, Jacob-Hirsch J, Amariglio N, Kupiec M, et al. Topology of the human and mouse m6A RNA methylomes revealed by m6A-seq. Nature. 2012;485:201–206. doi: 10.1038/nature11112. [DOI] [PubMed] [Google Scholar]
- 54.Yang D, Qiao J, Wang G, Lan Y, Li G, Guo X, Xi J, Ye D, Zhu S, Chen W, et al. N6-methyladenosine modification of lincRNA 1281 is critically required for mESC differentiation potential. Nucleic Acids Res. 2018;46:3906–3920. doi: 10.1093/nar/gky130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bertero A, Brown S, Madrigal P, Osnato A, Ortmann D, Yiangou L, Kadiwala J, Hubner NC, de Los MI, Sadee C, et al. The SMAD2/3 interactome reveals that TGFβ controls m6A mRNA methylation in pluripotency. Nature. 2018;555:256–259. doi: 10.1038/nature25784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Deng X, Su R, Weng H, Huang H, Li Z, Chen J. RNA N(6)-methyladenosine modification in cancers: Current status and perspectives. Cell Res. 2018;28:507–517. doi: 10.1038/s41422-018-0034-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vu LP, Pickering BF, Cheng Y, Zaccara S, Nguyen D, Minuesa G, Chou T, Chow A, Saletore Y, MacKay M, et al. The N6-methyladenosine (m6A)-forming enzyme METTL3 controls myeloid differentiation of normal hematopoietic and leukemia cells. Nat Med. 2017;23:1369–1376. doi: 10.1038/nm.4416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Visvanathan A, Patil V, Arora A, Hegde AS, Arivazhagan A, Santosh V, Somasundaram K. Essential role of METTL3-mediated m6A modification in glioma stem-like cells maintenance and radioresistance. Oncogene. 2018;37:522–533. doi: 10.1038/onc.2017.351. [DOI] [PubMed] [Google Scholar]
- 59.Cai X, Wang X, Cao C, Gao Y, Zhang S, Yang Z, Liu Y, Zhang X, Zhang W, Ye L. HBXIP-elevated methyltransferase METTL3 promotes the progression of breast cancer via inhibiting tumor suppressor let-7g. Cancer Lett. 2018;415:11–19. doi: 10.1016/j.canlet.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 60.Barbieri I, Tzelepis K, Pandolfini L, Shi J, Millan-Zambrano G, Robson SC, Aspris D, Migliori V, Bannister AJ, Han N, et al. Promoter-bound METTL3 maintains myeloid leukaemia by m6A-dependent translation control. Nature. 2017;552:126–131. doi: 10.1038/nature24678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dimitriou ID, Clemenza L, Scotter AJ, Chen G, Guerra FM, Rottapel R. Putting out the fire: Coordinated suppression of the innate and adaptive immune systems by SOCS1 and SOCS3 proteins. Immunol Rev. 2008;224:265–283. doi: 10.1111/j.1600-065X.2008.00659.x. [DOI] [PubMed] [Google Scholar]
- 62.Palmer DC, Restifo NP. Suppressors of cytokine signaling (SOCS) in T cell differentiation, maturation, and function. Trends Immunol. 2009;30:592–602. doi: 10.1016/j.it.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Letellier E, Haan S. SOCS2: Physiological and pathological functions. Front Biosci (Elite Ed) 2016;8:189–204. doi: 10.2741/E760. [DOI] [PubMed] [Google Scholar]
- 64.Newton VA, Ramocki NM, Scull BP, Simmons JG, McNaughton K, Lund PK. Suppressor of cytokine signaling-2 gene disruption promotes Apc(Min/+) tumorigenesis and activator protein-1 activation. Am J Pathol. 2010;176:2320–2332. doi: 10.2353/ajpath.2010.090684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Miller ME, Michaylira CZ, Simmons JG, Ney DM, Dahly EM, Heath JK, Lund PK. Suppressor of cytokine signaling-2: A growth hormone-inducible inhibitor of intestinal epithelial cell proliferation. Gastroenterology. 2004;127:570–581. doi: 10.1053/j.gastro.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 66.Letellier E, Schmitz M, Baig K, Beaume N, Schwartz C, Frasquilho S, Antunes L, Marcon N, Nazarov PV, Vallar L, et al. Identification of SOCS2 and SOCS6 as biomarkers in human colorectal cancer. Br J Cancer. 2014;111:726–735. doi: 10.1038/bjc.2014.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Slattery ML, Lundgreen A, Kadlubar SA, Bondurant KL, Wolff RK. JAK/STAT/SOCS-signaling pathway and colon and rectal cancer. Mol Carcinog. 2013;52:155–166. doi: 10.1002/mc.21841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hanahan D, Weinberg RA. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 69.Barker N, van Es JH, Kuipers J, Kujala P, van den Born M, Cozijnsen M, Haegebarth A, Korving J, Begthel H, Peters PJ, et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature. 2007;449:1003–1007. doi: 10.1038/nature06196. [DOI] [PubMed] [Google Scholar]
- 70.Jiang Y, Li W, He X, Zhang H, Jiang F, Chen Z. Lgr5 expression is a valuable prognostic factor for colorectal cancer: Evidence from a meta-analysis. BMC Cancer. 2016;16:12. doi: 10.1186/s12885-015-1986-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed in the present study (and its supplementary information files) are fully available without restrictions.