Abstract
A 66‐year‐old man complained of lower limb edema was diagnosed with mesenteric panniculitis because of fat ring sign and tumoral pseudocapsule sign on contrast‐enhanced CT. Patient had edema due to protein‐losing enteropathy associated with mesenteric panniculitis.

Keywords: fat ring sign, lymphangiectasia, mesenteric panniculitis, protein‐losing enteropathy, tumoral pseudocapsule sign
A 66‐year‐old man complained of pitting edema below the knees in both lower extremities in the last 9 months. Low serum albumin (2.4 g/dL) and immunoglobulin G (IgG; 414 mg/dL) levels were observed without other symptoms. Contrast‐enhanced computed tomography (CT) revealed increased thickened adipose tissue concentration in the mesentery. The mesenteric adipose tissue was surrounded by curvilinear bands of soft‐tissue density (Figure 1A, tumoral pseudocapsule). The mesenteric vessels were surrounded by fat (Figure 1B, fat ring sign). Mesenteric panniculitis (MP) was suspected. He refused to undergo surgical mesenteric biopsy. 99m Tc‐Human serum albumin scintigraphy revealed albumin leakage from the small intestine into the colonic area. Capsule endoscopy showed white villi, white spots, and white nodules (Figure 2) in the small intestinal mucosa. Endoscopic colon biopsy revealed intestinal lymphangiectasia. Due to the absence of malignancies, autoimmune diseases, and history of trauma or surgery, he was diagnosed with protein‐losing enteropathy (PLE) caused by intestinal lymphangiectasia associated with idiopathic MP. Leg edema resolved with improvements in the serum albumin (2.8 g/dL) and IgG (950 mg/dL) levels after nutritional guidance regarding medium‐chain fatty acids and a low‐fat diet for 3 months. Follow‐up CT at the 3‐month showed no changes. The patient is being followed up with CT examinations to carefully monitor whether the malignant tumors become apparent.
FIGURE 1.
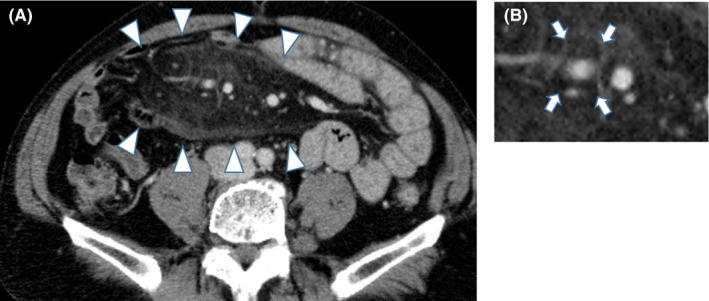
Tumoral pseudocapsule (Panel A; arrowhead); fat ring sign (Panel B; arrows)
FIGURE 2.

Capsule endoscopy: Diffuse whitish villi in the jejunum are observed
Mesenteric panniculitis causes chronic nonspecific inflammation and fibrosis of the mesenteric adipose tissue. Although mostly idiopathic, it may be associated with trauma and abdominal surgery, autoimmune diseases, such as IgG4‐related disease and lymphomas, and gastrointestinal organ malignancies; therefore, adequate testing for background diseases is recommended. 1
Mesenteric vasodilation is observed on CT in 93% of the cases. The fat ring sign (75%–85% of the cases) is characteristic of mesenteric vessels surrounded by thickened adipose tissue; a tumoral pseudocapsule (50%–59% of the cases) presenting as a dense band surrounding the lesion is characteristic of MP. 1 The fat ring sign is associated with reduced risks of concomitant malignancies 2 ; thus, awareness of the sign is critical.
Intestinal lymphangiectasia is a typical disease presenting with PLE; it is rarely associated with MP. 3 The intestinal lymphatic circulatory disorder associated with MP increases the intralymphatic pressure, resulting in intestinal lymphangiectasia. Endoscopic examinations show characteristic lymphangiectasia in the mucosa and submucosa, white villi, white spots, white nodules, and submucosal elevations, reflecting lipid filling. 4 Duodenal lesions are common; capsule endoscopy is effective in the absence of abnormalities in the upper gastrointestinal tract, as observed in our patient. 3 When PLE accompanies MP, aggressive investigation using capsule endoscopy is recommended to identify the possible malignancies and diagnose intestinal lymphangiectasia.
Mesenteric panniculitis has a good prognosis, with no progression reported in 87% of the patients 5 ; however, patients with PLE complications are resistant to medications, such as steroids, and have poor prognoses. 3 Patients with hypoproteinemia show resistance to treatment. 1 Thus, early diagnosis of MP and detection of PLE are important. MP may be detected by paying attention to the fat ring sign and tumoral pseudocapsule sign, in which the mesenteric adipose tissue appears thickened on contrast‐enhanced CT of PLE patients.
CONFLICT OF INTEREST
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
INFORMED CONSENT
We have obtained written informed consent of the patient for publication.
ACKNOWLEDGEMENTS
The authors would like to thank Editage (https://www.editage.jp/) for the English language review.
Hori H, Fukuchi T, Sugawara H. Fat ring sign and tumoral pseudocapsule sign in idiopathic mesenteric panniculitis complicated by protein‐losing enteropathy. J Gen Fam Med. 2020;21:157–158. 10.1002/jgf2.318
REFERENCES
- 1. Sharma P, Yadav S, Needham CM, Feuerstadt P. Sclerosing mesenteritis: a systematic review of 192 cases. Clin J Gastroenterol. 2017;10(2):103–11. [DOI] [PubMed] [Google Scholar]
- 2. Wilkes A, Griffin N, Dixon L, Dobbs B, Frizelle FA. Mesenteric panniculitis: a paraneoplastic phenomenon? Dis Colon Rectum. 2012;55(7):806–9. [DOI] [PubMed] [Google Scholar]
- 3. Saito Y, Hiramatsu K, Nosaka T et al A case of protein‐losing enteropathy caused by sclerosing mesenteritis diagnosed with capsule endoscopy and double‐balloon endoscopy. Clin J Gastroenterol. 2017;10(4):351–6. [DOI] [PubMed] [Google Scholar]
- 4. Chamouard P, Nehme‐Schuster H, Simler JM, Finck G, Baumann R, Pasquali JL. Videocapsule endoscopy is useful for the diagnosis of intestinal lymphangiectasia. Dig Liver Dis. 2006;38(9):699–703. [DOI] [PubMed] [Google Scholar]
- 5. Smith ZL, Sifuentes H, Deepak P, Ecanow DB, Ehrenpreis ED. Relationship between mesenteric abnormalities on computed tomography and malignancy: clinical findings and outcomes of 359 patients. J Clin Gastroenterol. 2013;47(5):409–14. [DOI] [PubMed] [Google Scholar]


