Abstract
Background
Resilience can be defined as maintaining or regaining mental health during or after significant adversities such as a potentially traumatising event, challenging life circumstances, a critical life transition or physical illness. Healthcare students, such as medical, nursing, psychology and social work students, are exposed to various study‐ and work‐related stressors, the latter particularly during later phases of health professional education. They are at increased risk of developing symptoms of burnout or mental disorders. This population may benefit from resilience‐promoting training programmes.
Objectives
To assess the effects of interventions to foster resilience in healthcare students, that is, students in training for health professions delivering direct medical care (e.g. medical, nursing, midwifery or paramedic students), and those in training for allied health professions, as distinct from medical care (e.g. psychology, physical therapy or social work students).
Search methods
We searched CENTRAL, MEDLINE, Embase, 11 other databases and three trial registries from 1990 to June 2019. We checked reference lists and contacted researchers in the field. We updated this search in four key databases in June 2020, but we have not yet incorporated these results.
Selection criteria
Randomised controlled trials (RCTs) comparing any form of psychological intervention to foster resilience, hardiness or post‐traumatic growth versus no intervention, waiting list, usual care, and active or attention control, in adults (18 years and older), who are healthcare students. Primary outcomes were resilience, anxiety, depression, stress or stress perception, and well‐being or quality of life. Secondary outcomes were resilience factors.
Data collection and analysis
Two review authors independently selected studies, extracted data, assessed risks of bias, and rated the certainty of the evidence using the GRADE approach (at post‐test only).
Main results
We included 30 RCTs, of which 24 were set in high‐income countries and six in (upper‐ to lower‐) middle‐income countries. Twenty‐two studies focused solely on healthcare students (1315 participants; number randomised not specified for two studies), including both students in health professions delivering direct medical care and those in allied health professions, such as psychology and physical therapy. Half of the studies were conducted in a university or school setting, including nursing/midwifery students or medical students. Eight studies investigated mixed samples (1365 participants), with healthcare students and participants outside of a health professional study field.
Participants mainly included women (63.3% to 67.3% in mixed samples) from young adulthood (mean age range, if reported: 19.5 to 26.83 years; 19.35 to 38.14 years in mixed samples). Seventeen of the studies investigated group interventions of high training intensity (11 studies; > 12 hours/sessions), that were delivered face‐to‐face (17 studies). Of the included studies, eight compared a resilience training based on mindfulness versus unspecific comparators (e.g. wait‐list).
The studies were funded by different sources (e.g. universities, foundations), or a combination of various sources (four studies). Seven studies did not specify a potential funder, and three studies received no funding support.
Risk of bias was high or unclear, with main flaws in performance, detection, attrition and reporting bias domains.
At post‐intervention, very‐low certainty evidence indicated that, compared to controls, healthcare students receiving resilience training may report higher levels of resilience (standardised mean difference (SMD) 0.43, 95% confidence interval (CI) 0.07 to 0.78; 9 studies, 561 participants), lower levels of anxiety (SMD −0.45, 95% CI −0.84 to −0.06; 7 studies, 362 participants), and lower levels of stress or stress perception (SMD −0.28, 95% CI −0.48 to −0.09; 7 studies, 420 participants). Effect sizes varied between small and moderate. There was little or no evidence of any effect of resilience training on depression (SMD −0.20, 95% CI −0.52 to 0.11; 6 studies, 332 participants; very‐low certainty evidence) or well‐being or quality of life (SMD 0.15, 95% CI −0.14 to 0.43; 4 studies, 251 participants; very‐low certainty evidence).
Adverse effects were measured in four studies, but data were only reported for three of them. None of the three studies reported any adverse events occurring during the study (very‐low certainty of evidence).
Authors' conclusions
For healthcare students, there is very‐low certainty evidence for the effect of resilience training on resilience, anxiety, and stress or stress perception at post‐intervention.
The heterogeneous interventions, the paucity of short‐, medium‐ or long‐term data, and the geographical distribution restricted to high‐income countries limit the generalisability of results. Conclusions should therefore be drawn cautiously. Since the findings suggest positive effects of resilience training for healthcare students with very‐low certainty evidence, high‐quality replications and improved study designs (e.g. a consensus on the definition of resilience, the assessment of individual stressor exposure, more attention controls, and longer follow‐up periods) are clearly needed.
Plain language summary
Psychological interventions to foster resilience in healthcare students
Background Healthcare students (e.g. medical, nursing, midwifery, paramedic, psychology, physical therapy, or social work students) have a high academic work load, are required to pass examinations and are exposed to human suffering. This can adversely affect their physical and mental health. Interventions to protect them against such stresses are known as resilience interventions. Previous systematic reviews suggest that resilience interventions can help students cope with stress and protect them against adverse consequences on their physical and mental health.
Review question Do psychological interventions designed to foster resilience improve resilience, mental health, and other factors associated with resilience in healthcare students?
Search dates The evidence is current to June 2019. The results of an updated search of four key databases in June 2020 have not yet been included in the review.
Study characteristics We found 30 randomised controlled trials (studies in which participants are assigned to either an intervention or a control group by a procedure similar to tossing a coin). The studies evaluated a range of resilience interventions in participants aged on average between 19 and 38 years.
Healthcare students were the focus of 22 studies, with a total of 1315 participants (not specified for two studies). Eight studies included mixed samples (1365 participants) of healthcare students and non‐healthcare students.
Eight of the included studies compared a mindfulness‐based resilience intervention (i.e. an intervention fostering attention on the present moment, without judgements) versus unspecific comparators (e.g. wait‐list control receiving the training after a waiting period). Most interventions were performed in groups (17/30), with high training intensity of more than 12 hours or sessions (11/30), and were delivered face‐to‐face (i.e. with direct contact and face‐to‐face meetings between the intervention provider and the participants; 17/30).
The included studies were funded by different sources (e.g. universities, foundations), or a combination of various sources (four studies). Seven studies did not specify a potential funder, and three studies received no funding support.
Certainty of the evidence A number of things reduce the certainty about whether resilience interventions are effective. These include limitations in the methods of the studies, different results across studies, the small number of participants in most studies, and the fact that the findings are limited to certain participants, interventions and comparators.
Key results Resilience training for healthcare students may improve resilience, and may reduce symptoms of anxiety and stress immediately after the end of treatment. Resilience interventions do not appear to reduce depressive symptoms or to improve well‐being. However, the evidence from this review is limited and very uncertain. This means that we currently have very little confidence that resilience interventions make a difference to these outcomes and that further research is very likely to change the findings.
Very few studies reported on the short‐ and medium‐term impact of resilience interventions. Long‐term follow‐up assessments were not available for any outcome. Studies used a variety of different outcome measures and intervention designs, making it difficult to draw general conclusions from the findings. Potential adverse events were only examined in four studies, with three of them showing no undesired effects and one reporting no results. More research is needed, of high methodological quality and with improved study designs.
Summary of findings
Summary of findings 1. Resilience interventions versus control conditions for healthcare students.
| Resilience interventions versus control conditions for healthcare students | ||||||
|
Patient or population: healthcare students, including students in training for health professions delivering direct medical care (e.g. medical students, nursing students), and allied health professions as distinct from medical care (e.g. psychology students, social work students); aged 18 years and older, irrespective of health status Setting: any setting of health professional education (e.g. medical school, nursing school, psychology or social work department at university) Intervention: any psychological intervention focused on fostering resilience or the related concepts of hardiness or post‐traumatic growth by strengthening well‐evidenced resilience factors that are thought to be modifiable by training (see Appendix 3), irrespective of content, duration, setting or delivery mode Comparison: no intervention, wait‐list control, treatment as usual (TAU), active control, attention control | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with control conditions | Risk with resilience interventions | |||||
|
Resilience
Measured by: investigators measured resilience using different instruments; higher scores mean higher resilience Timing of outcome assessment: post‐intervention |
‐ | The mean resilience score in the intervention groups was, on average, 0.43 standard deviations higher (0.07 higher to 0.78 higher) | ‐ | 561 (9 RCTs) | ⊕⊝⊝⊝ Very lowa | SMD of 0.43 represents a moderate effect size (Cohen 1988b)b |
|
Mental health and well‐being: anxiety
Measured by: investigators measured anxiety using different instruments; lower scores mean lower anxiety Timing of outcome assessment: post‐intervention |
‐ | The mean anxiety score in the intervention groups was, on average, 0.45 standard deviations lower (0.84 lower to 0.06 lower) | ‐ | 362 (7 RCTs) | ⊕⊝⊝⊝ Very lowc | SMD of 0.45 represents a moderate effect size (Cohen 1988b)b |
|
Mental health and well‐being: depression
Measured by: investigators measured depression using different instruments; lower scores mean lower depression Timing of outcome assessment: post‐intervention |
‐ | The mean depression score in the intervention groups was, on average, 0.20 standard deviations lower (0.52 lower to 0.11 higher) | ‐ | 332 (6 RCTs) | ⊕⊝⊝⊝ Very lowd | SMD of 0.20 represents a small effect size (Cohen 1988b)b |
|
Mental health and well‐being: stress or stress perception: Measured by: investigators measured stress or stress perception using different instruments; lower scores mean lower stress or stress perception Timing of outcome assessment: post‐intervention |
‐ | The mean stress or stress perception score in the intervention groups was, on average, 0.28 standard deviations lower (0.48 lower to 0.09 lower) | ‐ | 420 (7 RCTs) | ⊕⊝⊝⊝ Very lowe | SMD of 0.28 represents a small effect size (Cohen 1988b)b |
|
Mental health and well‐being: well‐being or quality of life: Measured by: investigators measured well‐being or quality of life using different instruments; higher scores mean higher well‐being or quality of life Timing of outcome assessment: post‐intervention |
‐ | The mean well‐being or quality of life score in the intervention groups was, on average, 0.15 standard deviations higher (0.14 lower to 0.43 higher) | ‐ | 251 (4 RCTs) | ⊕⊝⊝⊝ Very lowf | SMD of 0.15 represents a small effect size (Cohen 1988b)b |
| Adverse events | There were no adverse events reported in association with study participation in 3 of 4 studies measuring potential adverse events.g | ‐ | 566 (3 RCTs)h |
⊕⊝⊝⊝ Very lowi | ‐ | |
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; SMD: standardised mean difference. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect | ||||||
aDowngraded by two levels due to study limitations (unclear risk of selection bias, high and unclear risk of performance, detection and attrition bias), by one level due to unexplained inconsistency (I2 = 75%), and by one level due to indirectness (studies limited to certain interventions (e.g. group setting, face‐to‐face delivery, moderate and high intensity, unspecified theoretical foundation) and comparators (no intervention, wait‐list)).
bAccording to Cohen 1988b, a standardised mean difference (SMD) of 0.2 represents a small difference (i.e. small effect size), 0.5 a moderate difference, and 0.8 a large difference. cDowngraded by two levels due to study limitations (unclear risk of selection bias, high and unclear risk of detection and attrition bias, high risk of performance bias), by one level due to unexplained inconsistency (I2 = 66%), and by one level due to indirectness (studies limited to certain participants (medical students), interventions (e.g. group setting, moderate and high intensity) and comparators (no intervention, wait‐list)). dDowngraded by two levels due to study limitations (unclear risk of selection bias, high and unclear risk of detection bias, high risk of performance and attrition bias), by one level due to unexplained inconsistency (I2 = 45%), by one level due to indirectness (studies limited to certain participants (medical students), interventions (e.g. group and individual setting, low and high intensity) and comparators (no intervention, wait‐list)), and by two levels due to imprecision (< 400 participants; 95% CI wide and inconsistent). eDowngraded by two levels due to study limitations (unclear risk of selection bias, high and unclear risk of detection bias, high risk of performance, attrition and reporting bias), and by one level due to indirectness (studies limited to certain participants (medical and nursing students), interventions (group and individual setting, low and high intensity, mindfulness and unspecific theoretical foundation) and comparators (no intervention, wait‐list)). fDowngraded by two levels due to study limitations (unclear risk of selection and detection bias, high and unclear risk of attrition bias, high risk of performance bias), by one level due to indirectness (studies limited to certain interventions (group setting, face‐to‐face and combined delivery, high intensity)), and by two levels due to imprecision (< 400 participants; 95% CI and inconsistent).
gKötter 2016 also assessed adverse events but did not report the respective data in the report. hFor Galante 2018, subgroup data in healthcare students were not available; number of participants in total sample at post‐test (CORE‐OM data) was 482. iDowngraded by two levels due to study limitations (unclear risk of selection and detection bias, unclear and high risk of attrition bias, high risk of performance and other bias (no systematic and validated assessment of adverse events)), and by one level due to indirectness (studies limited to certain interventions (individual setting, face‐to‐face, mindfulness based) and comparators (TAU)).
Background
For a description of abbreviations used in this review, please see Appendix 1.
Description of the condition
Since the introduction of Antonovsky’s salutogenesis as a basis for health promotion (Antonovsky 1979), and the Ottawa Charter for Health Promotion (WHO 1986), the concept of resilience has stimulated extensive research. Resilience describes the phenomenon under which an individual does not, or only temporarily, experiences mental health problems despite being subjected to psychological or physical stressors of short (acute) or long (chronic) duration (Kalisch 2015; Kalisch 2017). By definition, resilience always presupposes the exposure to substantial risk or adversity (Earvolino‐Ramirez 2007; Jackson 2007; Luthar 2000; Masten 2001).
Stressor exposure in healthcare students and its consequences
Healthcare students are exposed to a large number of academic, clinical and psychosocial stressors. Substantial academic stressors include, for example, excessive academic workload (e.g. long hours of study, volume of information, difficult academic work), difficulties with studying and time management, competition with peers, examinations (e.g. high frequency), and fear of failing (Edwards 2010; Gazzaz 2018; Hill 2018). Further categories of stressor exposure may include social stressors such as conflicts with work‐life balance and relationship management, financial concerns, or uncertainty about the future (Chang 2012; Gazzaz 2018; Santen 2010). In addition to typical life changes during the transition from training (e.g. nursing or medical school) to (clinical) practice, healthcare students also have to adapt to challenges that are specific to their chosen field of work. Due to patient contact in later phases of training, they are exposed to patient‐related stressors such as exposure to human suffering and death (Hill 2018). Furthermore, clinical stressors identified among students and trainees in the healthcare sector include, for example, lack of practical skills, a theory‐to‐practice gap, tense atmosphere among clinical staff and negative attitudes of healthcare professionals, being criticised in front of staff and patients, or hospital ward rotations (Dyrbye 2009; Edwards 2010; Evans 2004; Hill 2018).
Chronic stressor exposure during health professional education has the potential to impact on the students' physical and mental health; for example, medical and nursing students have reported debilitating sleep disorders (Azad 2015; Belingheri 2020). Health professional education is perceived as stressful by many students, with many reporting increased levels of perceived stress (Edwards 2010; Fares 2016; Foster 2018; Heinen 2017; Jacob 2013; Wilks 2010). Healthcare students, especially medical students, are at increased risk of developing symptoms of burnout, such as high emotional exhaustion (Cecil 2014; Dyrbye 2009; Dyrbye 2016; Fares 2016; Santen 2010), and stress‐related mental disorders such as depression (Bunevicius 2008; Compton 2008; Dyrbye 2006; Mao 2019; Tung 2018) and anxiety (Bunevicius 2008; Dyrbye 2006; Mao 2019). The experience of stressors and the resulting health impact may negatively affect students' academic (e.g. grades) and clinical performance (e.g. decline in empathy) (Gazzaz 2018; Kötter 2017; Neumann 2011; Yamada 2014; Ye 2018), and could possibly affect also the high attrition rates found among healthcare students (Hamshire 2019) and new graduates (Pine 2007), as demonstrated by some studies (Dyrbye 2011).
Overall, based on these findings, the concept of resilience has become increasingly important for health professional education in recent years (Eley 2014; Hodges 2008; McAllister 2009; Pines 2012; Sanderson 2017; Stephens 2013; Tempski 2012; Thomas 2016; Waddell 2015; Wright 2019).
Definition of resilience
Three different approaches have been discussed in the definition of resilience (Hu 2015; Kalisch 2015). Trait resilience refers to resilience defined as personal resources or static, positive personality characteristics that enhance individual adaptation (Block 1996; Nowack 1989; Wagnild 1993). This approach has been superceded largely by a view of resilience as an outcome rather than a static personality trait (Kalisch 2015; Mancini 2009), i.e. mental health despite significant stress or trauma. According to this outcome‐oriented definition, the positive outcome of resilience is partially determined by several resilience factors (Kalisch 2015). To date, a large range of genetic, psychological, social and environmental factors have been discussed in resilience research that often overlap and may interact (Bengel 2012; Bonanno 2013; Carver 2010; Connor 2006; Earvolino‐Ramirez 2007; Feder 2011; Forgeard 2012; Haglund 2007; Iacoviello 2014; Kuiper 2012; Mancini 2009; Michael 2003; Ozbay 2007; Rutten 2013; Sapienza 2011; Sarkar 2014; Southwick 2005; Southwick 2012; Stewart 2011; Wu 2013; Zauszniewski 2010). Psychosocial resilience factors that are well‐evidenced according to the current state of knowledge and thought to be modifiable include: meaning or purpose in life, a sense of coherence, positive emotions, hardiness, self‐esteem, active coping, self‐efficacy, optimism, social support, cognitive flexibility (including positive reappraisal and acceptance), and religiosity or spirituality or religious coping (see Appendix 2: level 1). Most recently, resilience has been conceptualised as a multidimensional and dynamic process (Johnston 2015; Kalisch 2015; Kent 2014; Mancini 2009; Norris 2009; Rutten 2013; Sapienza 2011; Southwick 2012). This resilient process is characterised either by a trajectory of undisturbed mental health during or after adversities, or temporary dysfunction followed by successful recovery (Kalisch 2015). In general, resilience is viewed as the outcome of an interaction between the individual and his or her environment (Cicchetti 2012; Rutten 2013), which may be influenced through personal (e.g. optimism) as well as environmental resources (e.g. social support) (Haglund 2007; Iacoviello 2014; Kalisch 2015; Southwick 2005; Wu 2013). As such, resilience is modifiable and can be improved by interventions (Bengel 2012; Connor 2006; Southwick 2011).
Interventions to foster resilience
Interventions to foster resilience have been developed for and conducted in a variety of clinical and non‐clinical populations using various formats, such as multimedia programmes or face‐to‐face settings, and have been delivered in a group or individual context (see Bengel 2012 and Southwick 2011 for an overview). To date, several resilience‐training programmes that focus specifically on fostering resilience in healthcare students have been tested (Anderson 2017; Peng 2014). However, the empirical evidence for the efficacy of these interventions is still unclear and requires further research.
Description of the intervention
There is currently little consensus about when to consider a programme as ‘resilience training’, or what components are needed for effective programmes (Leppin 2014). The diversity across resilience‐training programmes in their theoretical assumptions, operationalisation of the construct, and inclusion of core components reflect the current state of knowledge (Joyce 2018; Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016), with leading guidelines still under discussion (compare Kalisch 2015; Robertson 2015).
Most training programmes, whether individual or group‐based, are implemented face‐to‐face. Alternative formats include online interventions or combinations of different formats. Resilience‐training programmes often use methods such as discussions, role plays, practical exercises and homework to reinforce training content. They usually contain a psycho‐educative element to provide information on the concept of resilience, or specific training elements (e.g. cognitive restructuring).
In general, resilience interventions are based on different psychotherapeutic approaches: cognitive‐behavioural therapy (CBT; Abbott 2009); acceptance and commitment therapy (ACT; Ryan 2014); mindfulness‐based therapy (Geschwind 2011); attention and interpretation therapy (AIT; Sood 2014); problem‐solving therapy (Bekki 2013), as well as stress inoculation (Farchi 2010). A number of training programmes focus on fostering single or multiple psychosocial resilience factors (Kanekar 2010), without being assignable to a certain approach. Few interventions base their work on a defined resilience model (Schachman 2004; Steinhardt 2008).
How the intervention might work
Depending on the underlying resilience concept, resilience interventions target different resources and skills. The theoretical foundations of training programmes and the hypotheses on how they might maintain or regain mental health are as diverse as their content. Currently, no empirically‐validated theoretical framework exists that outlines the mode of action of resilience interventions (Bengel 2012; Leppin 2014).
As resilience as an outcome is determined by several potentially modifiable resilience factors (see Description of the condition), resilience interventions might work by strengthening these factors (see Appendix 3 for examples of possible training methods). However, depending on the underlying theoretical foundation, there are different theories of change on how certain factors and hence resilience might be affected.
From a cognitive‐behavioural perspective, stress‐related mental dysfunctions (e.g. depression) are considered to be the result of dysfunctional thinking (Beck 2011; Benjamin 2011). When confronted with adversity, people show maladaptive behavioural responses or experience negative mood states, or both, due to irrational cognition (Beck 1976; Ellis 1975). This is in line with other stress and resilience theories, which assume that it is not the stressor itself, but its cognitive appraisal that may lead to stress reactions (Kalisch 2015; Lazarus 1987). Modifying cognitive processes into more adaptive patterns of thought will therefore probably produce more adaptive responses to stress (Beck 1964). By challenging an individual’s maladaptive thoughts, and by teaching coping strategies, CBT‐based resilience interventions might be beneficial in promoting the resilience factors of cognitive flexibility and active coping.
As one form of CBT, stress inoculation therapy is based on the assumption that exposing individuals to milder forms of stress can strengthen coping strategies and the individual’s confidence in using his or her coping repertoire (Meichenbaum 2007). Resilience‐training programmes grounded in stress inoculation therapy might therefore foster resilience by enhancing factors such as self‐efficacy.
Problem‐solving therapy is closely related to CBT and based on problem‐solving theory. According to the problem‐solving model of stress and adaptation, effective problem‐solving can attenuate the negative effects of stress and adversity on well‐being by moderating or mediating (or both) the effects of stressors on emotional distress (Nezu 2013). Resilience interventions based on problem‐solving that enhance an individual’s positive problem orientation and planful problem‐solving might foster participants’ psychological adaptation to stress by increasing the resilience factor of active coping.
According to ACT (Hayes 2004; Hayes 2006), psychopathology is primarily the consequence of psychological inflexibility (Hayes 2006), which is also relevant when an individual is confronted with stressors. By teaching acceptance and mindfulness skills on the one hand (e.g. being in contact with the present moment), and commitment and behaviour‐change skills on the other (e.g. values, committed action), several resilience factors might be fostered in ACT‐based resilience interventions (e.g. cognitive flexibility, purpose in life). In particular, the acceptance of a full range of emotions taught in ACT might result in a better adjustment to stressful conditions.
In mindfulness‐based therapy (e.g. mindfulness‐based stress reduction (MBSR; Stahl 2010); AIT (Sood 2010)), mindfulness is characterised by the nonjudging awareness of the present moment and its accompanying mental phenomena (i.e. body sensations, thoughts and emotions). Since practitioners learn to accept whatever occurs in the present moment, they are thought to adapt more efficiently to stress (Grossman 2004; Shapiro 2005). As being more aware of the 'here and now' may enhance the sensitivity to positive aspects in life, mindfulness‐based resilience interventions might also help participants to gain a brighter outlook for the future (i.e. optimism) or to experience positive emotions more regularly. Teaching mindfulness might also increase participants’ cognitive flexibility by learning to accept negative situations and emotions.
Independently of the underlying theory, resilience training might work differently depending on the respective 'delivery format' and 'intervention setting' (Robertson 2015; Vanhove 2016). For example, interventions implemented face‐to‐face could work better than online formats in increasing resilience, due to the more direct contact between trainers and participants (Vanhove 2016), which might also increase compliance. Resilience training in an individual setting could be more efficient than group‐based interventions, as trainers might be better able to attend to participants’ individual needs and provide feedback more easily (Vanhove 2016). On the other hand, group‐based interventions could enhance participants’ social resources. No previous review has examined the role of training duration on effect sizes of resilience interventions. As participants have the opportunity to apply the taught skills in daily life, high‐intensity resilience interventions that include weekly sessions over several weeks (e.g. combined with homework assignments or daily practice) could be more efficient than low‐intensity training (e.g. a single session). Joyce 2018, who examined the role of the theoretical foundation of resilience interventions for the first time, found positive effect sizes on resilience for CBT‐based, mindfulness‐based and mixed interventions (i.e. CBT and mindfulness) compared to control. However, differences in the effects of resilience training based on other theoretical foundations have not so far been considered.
Why it is important to do this review
A large number of systematic reviews and meta‐analyses have investigated various forms of interventions to foster healthcare students' mental health, such as stress management, mentoring programmes, emotional intelligence interventions and mindfulness‐based training to reduce or prevent burnout, and crisis‐focused programmes (see Appendix 4). Although some of these reviews also identified interventions to foster resilience (e.g. Griffiths 2019), the primary review question did not specifically refer to such programmes.
A considerable number of systematic reviews and meta‐analyses of interventions to foster resilience (see Appendix 4) have synthesised the efficacy of resilience‐training programmes in clinical and non‐clinical adult populations (Bauer 2018; Joyce 2018; Leppin 2014; Macedo 2014; Massey 2019; Milne 2016; Pallavicini 2016; Pesantes 2015; Petriwskyj 2016; Reyes 2018; Robertson 2015; Skeffington 2013; Townshend 2016; Vanhove 2016; Van Kessel 2014; Wainwright 2019), or at least have searched for 'resilience' and related constructs (Deady 2017; Tams 2016). In a recent Cochrane Review, our group synthesised the evidence on the efficacy of resilience training in healthcare professionals (Kunzler 2020). There are so far only four relevant meta‐analyses (Joyce 2018; Kunzler 2020; Leppin 2014; Vanhove 2016). Previous reviews agree in their conclusion that resilience interventions can generally improve resilience, mental health and (job) performance. Nevertheless, there are some methodological and quality differences between the reviews, which complicate statements about the efficacy of resilience training or result in a variety of effect sizes. These include, for example, heterogeneous eligibility criteria and definitions of resilience training, rather simple and limited search strategies, the lack of a review protocol or PROSPERO registration for most reviews, and different guidelines for the conduct and reporting of the review.
Four systematic reviews of healthcare students (see Appendix 4) have synthesised evidence on the efficacy of resilience‐training programmes in this target group (Gilmartin 2017; McGowan 2016; Rogers 2016; Sanderson 2017), with Sanderson 2017 not focusing only on resilience interventions. One other review (Pezaro 2017) and a meta‐analysis (Lo 2018) also searched for 'resilience'. The six publications either investigated healthcare students such as medical students (Lo 2018) or combinations of healthcare students and healthcare professionals (i.e. with completed training) (Gilmartin 2017). Overall, they found mixed results for the efficacy of resilience‐training programmes. On the one hand, they identified some benefits to healthcare students, for example, in improving resilience or mental health outcomes (e.g. Gilmartin 2017; Pezaro 2017; Rogers 2016). On the other hand, as pointed out by some authors (e.g. McGowan 2016), the reviews' conclusions have been restricted by current limitations of resilience intervention research (e.g. heterogeneous definitions of resilience, and the low methodological rigour of studies). Comparable with reviews in other populations, the publications also suffer from methodological weaknesses, which limit the robustness of their findings (see Appendix 4). Most importantly, the number of RCTs included in previous reviews is rather limited (0 to 24 RCTs among 5 to 36 studies included in the six reviews), and the search period covered by the reviews is up to January 2017 (Gilmartin 2017), thus precluding any conclusions about the efficacy of resilience interventions in healthcare students that have been developed since then.
In our review, which seeks to address the methodological weaknesses of previous reviews, we were also particularly interested in psychological resilience interventions offered to this target group. The interventions had to be scientifically founded, i.e. they had to address one or more of the resilience factors stated above that are known to be associated with resilience in adults according to the state of current research (see Appendix 2: levels 1a to 1c). They also had to state the intention of promoting resilience or a related construct (hardiness, post‐traumatic growth). Lastly, the trained population had to fulfil the condition of potential stress or trauma exposure (the concept implicated for resilience), i.e. being a healthcare student (see Description of the condition), in order to clearly distinguish genuine resilience interventions from other interventions focused on fostering associated constructs such as mental health (Windle 2011a).
Resilience as a concept of prevention is highly current, and there is increasing interest worldwide in promoting mental health and preventing disease (WHO 1986; WHO 2004). Due to chronic stressor exposure in healthcare students, and the potentially negative consequences for the students’ health (see Description of the condition), healthcare students are viewed as an important target group for resilience interventions (McAllister 2009). This review therefore aims to provide further and more detailed evidence about which interventions are most likely to foster resilience and to prevent stress‐related mental health problems in healthcare students. The evidence base for this review might contribute to improving existing interventions and to facilitating the future development of training programmes. In this way, researchers, practitioners and policymakers could benefit from our work.
Objectives
To assess the effects of interventions to foster resilience in healthcare students, that is, students in training for health professions delivering direct medical care (e.g. medical, nursing, midwifery or paramedic students), and those in training for allied health professions, as distinct from medical care (e.g. psychology, physical therapy or social work students; see Differences between protocol and review).
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs), including cluster‐RCTs.
Types of participants
Adults aged 18 years and older, who are healthcare students, i.e. students in training for health professions delivering direct medical care (e.g. medical, nursing, midwifery or paramedic students) and those in training for allied health professions, as distinct from medical care (e.g. psychology, physical therapy, social work, counselling, occupational therapy, speech therapy, medical assistant or medical technician students).
Participants were included irrespective of health status.
At the time of the intervention, individuals had to be exposed to potential risk or stressors, which was ensured by focusing on healthcare students in this review (see Description of the condition; see Differences between protocol and review).
We included studies involving mixed samples (e.g. healthcare and non‐healthcare students) in the review. We also considered these studies in meta‐analyses (see Data synthesis) provided the data for healthcare students were reported separately or could be obtained by contacting the study authors.
Types of interventions
Any psychological resilience intervention, irrespective of content, duration, setting or delivery mode.
For the purpose of this review, we define psychological resilience interventions as follows: interventions focused on fostering resilience or the related concepts of hardiness or post‐traumatic growth, by strengthening well‐evidenced resilience factors that are thought to be modifiable by training (see above and Appendix 2; level 1). In order to use highly‐objective inclusion criteria, we considered only interventions that explicitly defined the objective of fostering resilience, hardiness, or post‐traumatic growth by using one or more of these terms in the publication (see Differences between protocol and review). We did not include studies that examined the efficacy of disorder‐specific psychotherapy (e.g. CBT for depression).
We considered the following comparators in this review: no intervention, wait‐list control, treatment as usual (TAU), active control, and attention control. We used the term ‘attention control’ for alternative treatments that mimicked the amount of time and attention received (e.g. by the trainer) in the treatment group. We also considered active controls to involve an alternative treatment (no TAU; for example, treatment developed specifically for the study), but that did not control for the amount of time and attention in the intervention group and was not attention control in a narrow sense.
Types of outcome measures
Due to the different ways in which resilience has been operationalised in previous research, resilience as an intervention outcome could not always be guaranteed in studies. We therefore also defined assessments of psychological adaptation (e.g. mental health) as primary outcomes.
Secondary outcomes included a range of psychological factors associated with resilience, according to the current state of knowledge, and were selected based on conceptual clarity and measurability (levels 1a and 1b; see Appendix 2).
Measures for the assessment of psychological resilience and psychological adaptation, as well as resilience factors, are specified on the basis of previous reviews on resilience interventions (Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016) and reviews on resilience measurements (Pangallo 2015; Windle 2011b); see Helmreich 2017 and Appendix 5, Appendix 6, Appendix 7 in this review, respectively.
We considered self‐rated and observer‐ or clinician‐rated measures, as well as study outcomes at all time points. The lack of reporting of the primary or secondary outcomes described above was not an exclusion criterion for this review.
Primary outcomes
Resilience*, measured by improvements in specific resilience scales (Bengel 2012; Earvolino‐Ramirez 2007; Pangallo 2015; Windle 2011b), such as the Resilience Scale for Adults (Friborg 2003).
-
Mental health and well‐being, subsumed into the categories below, and measured by improvements in the respective assessment scales, such as the Depression Anxiety and Stress Scale (DASS‐21; Lovibond 1995). See Appendix 6 for further examples.
Anxiety*
Depression*
Stress or stress perception*
Well‐being or quality of life* (e.g. well‐being, life satisfaction, (health‐related) quality of life, vitality, vigour)
Adverse events*
Secondary outcomes
Resilience factors (Bengel 2012; Haglund 2007; Iacoviello 2014; Southwick 2005; Southwick 2012; Wu 2013), whenever they were available as outcomes, assessed by an increase in the respective instruments (e.g. Life Orientation Test ‐ Revised (LOT‐R); Scheier 1994). For further examples see Appendix 7.
Social support
Optimism
Self‐efficacy
Active coping
Self‐esteem
Hardiness (although hardiness is often used as a synonym for resilience in the literature, we conceptualised it as a resilience factor in this review. See Appendix 2.)
Positive emotions
We extracted and reported data on secondary outcomes whenever they were assessed. If possible, we calculated and reported effect sizes.
Where data were available, we used outcomes marked by an asterisk (*) to generate the ‘Summary of findings’ table. If there was insufficient information, we provided a narrative description of the evidence.
Search methods for identification of studies
We ran the first searches for this review in October 2016, based on the MEDLINE search strategy in the protocol (Helmreich 2017) before changing the inclusion criteria of the review to focus on healthcare students (see Differences between protocol and review). For the top‐up searches in June 2019, we added a new section to the original search strategy using search terms to limit the search to healthcare sector workers and students.
Electronic searches
We searched the electronic sources listed below.
Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 6) in the Cochrane Library, which includes the Cochrane Developmental, Psychosocial and Learning Problems Specialised Register (searched 26 June 2019).
MEDLINE Ovid (1946 to 21 June 2019).
Embase Ovid (1974 to 2019 Week 25).
PsycINFO Ovid (1806 to June Week 3 2019).
CINAHL EBSCOhost (Cumulative Index to Nursing and Allied Health Literature; 1981 to 24 June 2019).
PSYNDEX EBSCOhost (1977 to 24 June 2019).
Web of Science Core Collection Clarivate (Science Citation Index; Social Science Citation Index; Conference Proceedings Citation Index ‐ Science; Conference Proceedings Citation Index ‐ Social Science & Humanities; 1970 to 26 June 2019).
International Bibliography of the Social Sciences ProQuest (IBSS; 1951 to 25 June 2019).
Applied Social Sciences Index & Abstracts ProQuest (ASSIA; 1987 to 24 June 2019).
ProQuest Dissertations & Theses (PQDT; 1743 to 24 June 2019).
Cochrane Database of Systematic Reviews (CDSR; 2019, Issue 6), part of the Cochrane Library (searched 26 June 2019).
Database of Abstracts of Reviews of Effects (DARE; 2015, Issue 4) part of the Cochrane Library (final issue; searched 27 October 2016).
Epistemonikos (epistemonikos.org; all available years, searched 24 June 2019).
ERIC EBSCOhost (Education Resources Information Center; 1966 to 26 June 2019).
Current Controlled Trials now ISTRCN registry (www.isrctn.com; 1 January 1990 to 24 June 2019).
ClinicalTrials.gov (clinicaltrials.gov; 1 January 1990 to 24 June 2019).
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP; who.int/trialsearch; 1 January 1990 to 24 June 2019)
We report the search strategies for each database in Appendix 8 (up to 2016) and for the revised inclusion criteria, Appendix 9 (2016 onwards). We used the Cochrane Highly Sensitive Search Strategy to identify RCTs in MEDLINE (Lefebvre 2019). We adapted the search terms and syntax for other databases. The searches were not restricted by language, publication status or publication format. We limited our search to the period January 1990 onwards, to account for the fact that the concept of resilience and its operationalisation have developed significantly over the past decades (Fletcher 2013; Hu 2015; Kalisch 2015; Pangallo 2015). Because of the lack of homogeneity for the period 1990 to 2014 (Robertson 2015), it is likely that using a broader time frame would have made it even more difficult to detect resilience‐training studies with similar resilience concepts and assessments. Moreover, it appeared plausible to concentrate on the period 1990 to the present, since the idea of resilience as an outcome and a modifiable process has only emerged in recent years, and paved the way for the development of resilience‐promoting interventions (Bengel 2009; Southwick 2011). The idea of fostering resilience by specific training was therefore relatively new (Leppin 2014), which can also be seen in the review by Macedo 2014, who searched for studies on resilience interventions every year until 2013 but only found RCTs published after 1990.
As resilience‐training programmes should be adapted to scientific findings on a regular basis, and with the current research focusing on the detection of general resilience mechanisms (Kalisch 2015; Luthar 2000), the last five years seemed especially important in synthesising the evidence on newly‐developed resilience training.
We performed a further scoping search of four key databases (CENTRAL, CINAHL EBSCOhost, PsycINFO Ovid, ClinicalTrials.gov) in June 2020 prior to the publication of this review. The results are awaiting classification and will be incorporated into the review at the next update.
Searching other resources
In addition to the electronic searches, we inspected the reference lists of all included RCTs and relevant reviews, and contacted researchers in the field as well as the authors of selected studies, to check if there were any unpublished or ongoing studies. If data were missing or unclear, we contacted the study authors.
Data collection and analysis
We report only the methods we used in successive sections in this review. We report preplanned but unused methods in Table 2.
1. Unused methods table.
| Method | Approach planned for analysis | Reason for non‐use |
| Measures of treatment effect | Dichotomous data We had planned to analyse dichotomous outcomes by calculating the risk ratio (RR) of a successful outcome (i.e. improvement in relevant variables) for each trial. We had intended to express uncertainty in each result using 95% confidence intervals (CIs). | No study provided relevant dichotomous data for any of the primary or secondary outcomes included in this review. |
| Unit of analysis issues | Cluster‐randomised trials In cluster‐randomised trials, if the clustering is ignored and the unit of analysis is different from the unit of allocation (‘unit‐of‐analysis error’) (Whiting‐O'Keefe 1984), P values may be artificially small and may result in false‐positive conclusions (Higgins 2019c). Had we encountered such cases, we would have accounted for the clustering in the data and followed the recommendations given in the literature (Higgins 2019c; White 2005). For those cluster‐randomised trials that did not report correct standard errors, we would have tried to recover correct standard errors by applying the usual formula for the variance inflation factor 1 + (M ‐ 1) ICC, where M is the average cluster size and ICC the intra‐cluster correlation coefficient (Higgins 2019c). If it had not been possible to extract ICC values from the study, we would have used the ICC of all cluster‐randomised trials in our review that investigated the same primary outcome scale in a similar setting. If this was not available, we would have used the average ICC of all other cluster‐randomised trials in our review. If no such studies were available, we would have used ICC = 0.05 as a mildly conservative guess for the primary analysis, and conducted a sensitivity analysis using ICC = 0.10. We had also planned to conduct sensitivity analyses based on the unit of randomisation as well as the ICC estimate in cluster‐randomised trials (see Sensitivity analysis). | No cluster‐RCT was identified and included in this review. |
|
Multiple treatment groups Had multiple groups in a study been relevant, we would have accounted for the correlation between the effect sizes from multi‐arm studies in a pair‐wise meta‐analysis (Higgins 2019c). We would have treated each comparison between a control group and a treatment group as an independent study. We would have multiplied the standard errors of the effect estimates by an adjustment factor to account for correlation between effect estimates. In so doing, we would have acknowledged heterogeneity between different treatment groups. |
For studies with multiple treatment groups, we considered only one intervention group to be relevant for the review and meta‐analyses, based on the independent judgement of two review authors. Thus, in a pair‐wise meta‐analysis, we did not have to account for the correlation between the effect sizes for multi‐arm studies. | |
| […] If there is an adequate evidence base, we will consider performing a network meta‐analysis (see Data synthesis). | The evidence base was insufficient to conduct a network meta‐analysis. | |
| Dealing with missing data | If standard deviations could neither be recovered from reported results nor obtained from the authors, we would have considered single imputation by means of pooled within‐treatment standard deviations from all other studies, provided that fewer than five studies had missing standard deviations. If more than five studies had missing standard deviations, we would have performed multiple imputation on the basis of the hierarchical model fitted to the non‐missing standard deviations. | We found no studies using the same scale that had missing standard deviations. Missing standard deviations could always be recovered from alternative statistical values or be obtained from the study authors. |
| Data synthesis | Had a trial reported more than one resilience scale, we planned to use the scale with better psychometric qualities (as specified in Appendix 3 in Helmreich 2017), to calculate effect sizes. | All studies measuring resilience only used one resilience scale. |
| If a study provided data from two instruments used equally in the included RCTs, two review authors (AK, IH) would have identified the appropriate measure through discussion (compare Storebø 2020). | This did not occur in this review. | |
| Network meta‐analyses (NMAs) would have been merely exploratory and would only have been conducted if the review results had a sufficient and adequate evidence base. Network meta‐analyses offer the possibility of comparing multiple treatments simultaneously (Caldwell 2005). They combine both direct (head‐to‐head) and indirect evidence (Caldwell 2005; Mills 2012), by using direct comparisons of interventions within RCTs, as well as indirect comparisons across trials, on the basis of a common reference group (e.g. an identical control group) (Li 2011). A network meta‐analysis on resilience‐training programmes does not exist. According to Mills 2012, Linde 2016 and the Cochrane Handbook (Chaimani 2019), there are three important conditions for the conduct of NMAs: transitivity, homogeneity, consistency. Had an NMA been possible, i.e. if the three conditions had been fulfilled, we would have conducted an analysis ‐ with expert statistical support as suggested by Cochrane (Chaimani 2019) ‐ using a frequentist approach in R (Rücker 2020; Viechtbauer 2010). For sensitivity analyses, we had planned to fit the same models using the restricted maximum likelihood method (Piepho 2012; Piepho 2014; Rücker 2020). We had intended to consider categorising resilience training into seven groups, based on the underlying training concept: (1) cognitive behavioural therapy, (2) acceptance and commitment therapy, (3) mindfulness‐based therapy, (4) attention and interpretation therapy, (5) problem‐solving therapy, (6) stress inoculation therapy and (7) multimodal resilience training. We may have included additional groups after conducting the full literature search. Reference groups that might have been included in the NMA were: attention control, wait‐list, treatment as usual or no intervention. We had planned to investigate inconsistency and flow of evidence in accordance with recommendations in the literature (e.g. Chaimani 2019; Dias 2010; König 2013; Krahn 2013; Krahn 2014; Lu 2006; Lumley 2002; Rücker 2020; Salanti 2008; White 2012b). |
The evidence base was insufficient to conduct a network meta‐analysis. | |
| Summary of findings | Depending on the assessment of heterogeneity and possible effect modifiers (see Subgroup analysis and investigation of heterogeneity), we would have created several ‘Summary of findings’ tables; for example, the clinical status of study populations or the comparator group. | We were not able to investigate potential effect modifiers for the primary outcomes in subgroup analyses and therefore created no additional ‘Summary of findings’ tables. |
| Subgroup analysis and investigation of heterogeneity | Where we detected substantial heterogeneity, we had planned to examine characteristics of studies that may be associated with this diversity (Deeks 2019). The selection of potential effect modifiers was based on experiences from previous reviews (Leppin 2014; Robertson 2015; Vanhove 2016). We had intended to perform the following subgroup analyses on our primary outcomes, if we identified 10 or more studies during the review process (Deeks 2019):
|
For the primary outcomes at each time point, we identified fewer than 10 studies in a pair‐wise meta‐analysis. |
| Sensitivity analysis | Comparable with the planned subgroup analyses, we had planned to perform sensitivity analyses if more than 10 RCTs were included in a meta‐analysis. We had intended to restrict the sensitivity analyses to the primary outcomes.
For intervention studies assessing resilience with resilience scales, we had planned to perform a sensitivity analysis on the basis of the underlying concept (state versus trait) in these measures, and to limit the analysis to scales assessing resilience as an outcome of an intervention. To examine the impact of the risk of bias of included trials, we had intended to limit the studies included in the sensitivity analysis to those whose risk of bias was rated as low or unclear, and to exclude studies assessed at high risk of bias; for studies with low or unclear risk of bias, we had planned to conduct subgroup analyses. We had also intended to consider the restriction to registered studies. We had planned to identify registration, both by recording whether we found a study in a trial registry and by noting whether the study author claimed to have registered it. We had planned to perform sensitivity analyses by limiting analysis to those studies with low levels of missing data (less than 10% missing primary outcome). We had intended to limit the analysis to studies where missing data had been imputed or accounted for by fitting a model for longitudinal data, or where the proportion of missing primary outcome data was less than 10%. We had also intended to perform sensitivity analyses based on the ICC estimate in cluster‐randomised trials that had not adjusted for clustering, by excluding cluster‐RCTs where standard errors had not been corrected or corrected only on the basis of an externally‐estimated ICC. In an additional sensitivity analysis, we had planned to replace all externally‐estimated ICCs less than 0.10 by 0.10. Finally, we had intended to conduct a sensitivity analysis based on the unit of randomisation, by limiting the analysis to individually randomised trials. |
For the primary outcomes at each time point, we identified fewer than 10 studies in a pair‐wise meta‐analysis. |
This table provides details of analyses that had been planned and described in the protocol (Helmreich 2017), including revisions made at review stage, but were not used as they were not required or not feasible.
ACT: acceptance and commitment therapy; AIT: attention and interpretation therapy; CBT: cognitive‐behavioural therapy; RCT(s): randomised controlled trial(s); TAU: treatment as usual; vs: versus
Selection of studies
Two review authors (AK, IH) independently screened titles and abstracts in order to determine eligible studies. We immediately excluded clearly irrelevant papers. At full text level, the same two review authors (AK, IH), working independently, inspected for eligibility in duplicate. We calculated inter‐rater reliability at both stages (title and abstract screening and full text screening), resolving any disagreements in study selection by discussion. Where we could reach no consensus, a third review author (AC or KL) arbitrated. If necessary, we contacted the study authors to seek additional information. We recorded all decisions in a PRISMA flow diagram (Moher 2009).
We assessed the feasibility of the selection criteria a priori, by screening 500 studies in order to attain acceptable inter‐rater reliability (see Differences between protocol and review). There was good agreement between the review authors (kappa = 0.72), and thus no need to refine or clarify the criteria. For scientific reasons, however, we adapted the eligibility criteria during review development (see Differences between protocol and review).
Data extraction and management
We developed a data extraction sheet (see Appendix 10), based on Cochrane guidelines (Li 2019), and tested it on 10 randomly‐selected included studies. This initial test resulted in sufficient agreement between the review authors. For each included study, two review authors (AK, IH) independently extracted the data in duplicate. The extraction sheet contained the following elements:
source and eligibility;
study methods (e.g. design);
allocation process;
participant characteristics;
interventions and comparators;
outcomes and assessment instruments (means and standard deviations (SDs) in any standardised scale);
results;
miscellaneous aspects.
We resolved any disagreements in data collection by discussion. Where we could reach no consensus, a third review author (AC or KL) arbitrated. If necessary, we contacted the study authors to seek additional information.
Assessment of risk of bias in included studies
Two review authors (AK, IH) independently assessed the risks of bias of the included studies. We checked the risk of bias for each study using the criteria presented in the Cochrane Handbook for Systematic Reviews of Interventions, hereafter referred to as the Cochrane Handbook (Higgins 2011a) (see Appendix 11). We resolved any disagreements by discussion or by consulting a third review author (AC or KL). In accordance with Cochrane’s 'Risk of bias' tool (Higgins 2011b), we critically assessed each study across the following domains:
sequence generation and allocation concealment (selection bias);
blinding of participants and personnel (performance bias);
blinding of outcome assessment (detection bias);
incomplete outcome data (attrition bias);
selective outcome reporting (reporting bias).
We also considered the baseline comparability between study conditions as part of selection bias (random‐sequence generation), which is not defined in the Cochrane Handbook. In the first part of the assessment, we described what was reported to have happened in the study for each domain, before assigning a judgement for the risk of bias (low, high or unclear) for the entry.
Measures of treatment effect
Dichotomous data
We did not need to use our preplanned methods for analysing dichotomous outcomes (Helmreich 2017), as none of the included studies reported relevant dichotomous data for any of the prespecified primary or secondary outcomes.
Continuous data
Because the included resilience‐training studies used different measurement scales to assess resilience and related constructs (see Table 3; Table 4), we used standardised mean difference (SMD) effect sizes (Cohen's d) and their 95% confidence intervals (CIs) for continuous data in pair‐wise meta‐analyses. We calculated effect sizes on the basis of means, standard deviations (SDs) and sample sizes for each study condition. If the respective data were not provided, we computed Cohen's d from alternative statistics (e.g. t test, change scores). We assessed the magnitude of effect for continuous outcomes using the criteria for interpreting SMDs suggested in the Cochrane Handbook (Schünemann 2019a): a value of 0.2 indicates a small effect; 0.5 a moderate effect; and 0.8 a large effect (Cohen 1988b).
2. Primary outcomes: scales used.
| Outcomes | Number of studies | Studies and instruments |
| Resilience | 17 |
|
| Anxiety | 9 |
|
| Depression | 10 |
|
| Stress or stress perception | 13 |
|
| Well‐being or quality of life | 6 |
|
aFor depression, we preferred depression scales over burnout scales if both measures were reported. bConcerning Barry 2019, we included the values for the PSS‐10 in the pooled analysis, as this measure was used more often among the included studies.
3. Secondary outcomes: scales used.
| Outcomes | Number of studies | Studies and instruments |
| Social support (perceived) | 4 |
|
| Optimism | 4 |
|
| Self‐efficacy | 7 |
|
| Active coping | 2 |
|
| Self‐esteem | 2 |
|
| Hardiness | 1 |
|
| Positive emotions | 6 |
|
Unit of analysis issues
Cluster‐randomised trials
As the allocation of individuals to different conditions in resilience intervention studies partly occurs by groups (e.g. work sites, hospitals), we intended to include cluster‐randomised studies along with individually‐randomised studies. Since we identified no cluster‐RCTs, we only included individually‐randomised studies in meta‐analyses.
Repeated observations on participants
If there were longitudinal designs with repeated observations on participants, we defined several outcomes based on different follow‐up periods and conducted separate analyses, as recommended in the Cochrane Handbook (Higgins 2019b). One analysis included all studies with measurement at the end of intervention (post‐test), while other analyses were based on the period of follow‐up (short‐term: three months or less; medium‐term: more than three months to six months; and long‐term follow‐up: more than six months). We rated assessments as post‐intervention if performed within one week after the intervention. Assessments at more than one week after the intervention were counted as short‐term follow‐up.
Studies with multiple treatment groups
If selected studies contained two or more intervention groups, two review authors (AK, IH) determined which group was relevant to the review and the particular meta‐analysis, based on the inclusion criteria for interventions (see Types of interventions). For all studies that included several intervention groups, we considered only one intervention group as relevant for the review (see Results, specifically 'Interventions').
Dealing with missing data
In the case of studies where there were missing data, such as missing SDs, or where healthcare students had been combined with other participants, we contacted the original authors to enquire if the missing data or subgroup (summary outcome) data were available. To obtain missing summary outcome data for studies solely conducted in healthcare students, we contacted the study authors (at least twice) to request the respective data (i.e. means, SDs and sample sizes for the relevant study conditions, or alternative information to calculate the SMDs; see Measures of treatment effect).
We did not ask for individual‐level missing data for outcome data missing due to attrition, and performed no re‐analysis using imputation methods. We rated studies with high levels of missing data (≥ 10%) that used no imputation methods at high attrition risk of bias (see Assessment of risk of bias in included studies). If the study authors had reported a complete‐case analysis as well as imputed data, we used the summary outcome data based on the imputed dataset (e.g. last observation carried forward (LOCF) in two studies, or ideally expectation maximisation or multiple imputation).
Following the recommendations in the Cochrane Handbook (Higgins 2019b), we computed missing SDs for continuous outcomes on the basis of other statistical information (e.g. t values, P values), since, as expected, we found enough information in all papers to restore SDs from the reported results.
Studies for which authors provided additional data not originally reported (e.g. number of participants analysed) are described in detail in the Characteristics of included studies tables. We recorded missing data and attrition levels for each included study in the ‘Risk of bias’ tables (beneath the Characteristics of included studies tables).
Assessment of heterogeneity
We assessed the presence of clinical heterogeneity by comparing study and population characteristics across all eligible studies, by generating descriptive statistics. In accordance with the Cochrane Handbook (Deeks 2019), we explored if studies were sufficiently homogeneous for participant characteristics, interventions and outcomes.
We assessed methodological diversity by inspecting the included studies for variability in study design and risks of bias (e.g. method of randomisation). In accordance with previous reviews that have already described the great heterogeneity in resilience intervention studies (Joyce 2018; Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016), we discuss the similarities and differences between the included studies for these study characteristics in the Results and Discussion sections.
To assess statistical heterogeneity between the included studies within each pair‐wise meta‐analysis (i.e. heterogeneity in observed treatment effects that exceeds sampling error alone), we relied on forest plots, Chi2 test, tau2, and I2 statistic, as suggested by Deeks 2019. We also considered G2, in order to take small‐study effects into account (Rücker 2011). Significant statistical heterogeneity is indicated by a P value in the Chi2 test lower than 0.10. Since resilience‐training studies are often conducted with relatively small sample sizes (e.g. Loprinzi 2011; Sood 2014), we acknowledge that the Chi2 test has only limited power in such cases. Tau2 also provides an estimate of between‐study variance in a random‐effects meta‐analysis. The I2 is a descriptive statistic, which reflects the percentage of total variation across studies that is due to heterogeneity rather than to chance. In accordance with guidelines (Deeks 2019), we assumed non‐important heterogeneity for I2 values of 0% to 40%, moderate heterogeneity for I2 values of 30% to 60%, substantial heterogeneity for I2 values of 50% to 90%, and considerable heterogeneity for I2 values between 75% and 100%. G2 indicates the proportion of unexplained variance, having allowed for possible small‐study effects (Rücker 2011). No statistical heterogeneity is indicated by a G2 near zero. We also calculated the 95% prediction intervals from random‐effects meta‐analyses (see Data synthesis; pooled analyses with more than two studies) to present the extent of between‐study variation (Deeks 2019).
Assessment of reporting biases
We produced (contour‐enhanced) funnel plots for the primary outcomes at post‐test, plotting the effect estimates of studies against their standard errors on reversed scales (Page 2019; Peters 2008), in order to explore potential publication bias as part of our assessment of the certainty of the evidence and to create the 'Summary of findings' table (see Data synthesis). We considered the fact that funnel plot asymmetry does not necessarily reflect publication bias but can stem from a number of reasons (Page 2019). To differentiate between real asymmetry and chance, we followed the recommendations in Page 2019, and also used Egger’s test (regression test; Egger 1997) to test for funnel plot asymmetry.
We did not assess reporting bias as planned for the remaining outcomes at other time points (Helmreich 2017), due to an insufficient number of studies (fewer than 10 studies) included in the meta‐analyses for each outcome (see Effects of interventions).
Data synthesis
We synthesised the results, in narrative and tabular form, by describing the resilience interventions, their theoretical concept (when possible), as well as the populations and outcomes studied (see Results). We performed the statistical analyses either in Review Manager 5 (RevMan 5; Review Manager 2014) or in R (R 3.6.3 2019; libraries used: meta (Balduzzi 2019) metafor (Viechtbauer 2010) and metasens (Schwarzer 2019), when appropriate.
We combined outcome measures of included studies through pair‐wise meta‐analyses (any resilience training versus control), in order to determine summary (pooled) intervention effects of resilience‐training programmes in healthcare students. The decision to summarise numerical results of RCTs in pair‐wise meta‐analyses depended on the number of studies found (at least two studies for a specific outcome and time point), as well as the homogeneity of the included studies by population (for age, sex), resilience interventions (i.e. comparable content and modalities), comparisons, outcomes measured (i.e. the same prespecified outcome, albeit with different assessment tools), and methodological quality (risk of bias) of selected studies. We conducted meta‐analyses where intervention studies did not differ excessively in their content, outcomes (measures) were not too diverse and there were no individual studies predominantly at high risk of bias.
For summary statistics for continuous data, we reported SMDs using an inverse variance random‐effects model. We used random‐effects pair‐wise meta‐analyses since we anticipated a certain degree of heterogeneity between studies, as indicated by the results of previous reviews (Joyce 2018; Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016), and given the nature of the interventions included. We calculated the 95% prediction intervals from random‐effects meta‐analyses (see Assessment of heterogeneity). As part of our sensitivity analyses, we also performed fixed‐effect analyses (see Sensitivity analysis). We analysed continuous data reported as means and SDs in some studies separately from outcomes where SMDs and the respective standard error were taken from different data (e.g. independent t test). We subsequently combined these values using the generic invariance method in RevMan 5 (Review Manager 2014).
We also included studies with mixed samples (i.e. healthcare students and non‐healthcare students) in meta‐analyses, provided the subgroup data for healthcare students were reported separately or could be obtained from the study authors. If subgroup data were not available, we provided a narrative report of the findings of these studies in a separate section (see Effects of interventions, studies with mixed samples) for each outcome.
All studies measuring resilience used only one resilience scale. If a study reported more than one instrument for mental health and well‐being outcomes or for a specific resilience factor, we used the measure most often used among the included studies for effect size calculation. For the outcome of depression, we preferred depression scales over burnout scales if both measures were reported. Where studies reported both general measures of well‐being or quality of life and work‐related assessments (e.g. job satisfaction, work‐related vitality), we preferred general measures.
Once we had produced a summary of the evidence to date, and only if a pair‐wise meta‐analysis (any resilience training versus control) was possible, we examined whether the data were also suitable for a network meta‐analysis (NMA). There was insufficient evidence to perform a NMA.
Summary of findings
In this review, we used the software developed by the GRADE Working Group, GRADEpro: Guideline Development Tool (GRADEpro GDT), to create a 'Summary of findings' table for the comparison: resilience interventions versus control conditions for healthcare students.
We included all primary outcomes at post‐test in the ‘Summary of findings’ table. For each outcome, we assessed the certainty of the body of evidence using the GRADE approach proposed by the GRADE working group (Schünemann 2013; Schünemann 2019b), across the following five GRADE considerations:
limitations in the design and implementation of available studies (i.e. unclear or high risk of bias of studies contributing to the respective outcome; Guyatt 2011a);
high probability of publication bias (i.e. high risk of selective outcome reporting bias for studies contributing to the outcome, based on funnel plot asymmetry, Egger's test, different results of published versus unpublished studies, and whether the evidence consisted of many small studies with potential conflicts of interest) (Guyatt 2011b);
imprecision of results (i.e. small number of participants included in an outcome and wide CIs; Guyatt 2011c);
unexplained heterogeneity or inconsistency of results (i.e. heterogeneity based on variation of effect estimates, CIs, the statistical test of heterogeneity and I2, but the subgroup analyses fail to identify a plausible explanation; Guyatt 2011d); and
indirectness of evidence (i.e. included studies limited to certain participants, intervention types, or comparators; Guyatt 2011e).
According to the GRADE system, meta‐analyses for continuous outcomes should include sample sizes of at least 400 participants for sufficient statistical precision. Where there was both substantial inconsistency (I2 ≥ 60%) for an outcome and imprecision, we did not downgrade for imprecision, as the heterogeneity might have influenced the CI (i.e. precision) and we did not wish to double‐downgrade for the same problem.
Two review authors (AK, IH), working independently, conducted the assessment of the certainty of the evidence in duplicate, resolving any disagreements by discussion or by consulting a third review author (AC, KL). We interpreted the magnitude of effect for continuous outcomes according to the criteria suggested in the Cochrane Handbook (Schünemann 2019a) (i.e. 0.2 as a small effect, 0.5 as a moderate effect, 0.8 as a large effect).
We rated the certainty of the evidence as high, moderate, low or very low (Schünemann 2013). High‐certainty evidence indicates high confidence that the true effect lies close to that of the estimate of effect. Very‐low certainty evidence indicates that we have very little confidence in the effect estimate and that the true effect is likely to be substantially different from the estimate of effect.
Subgroup analysis and investigation of heterogeneity
Due to the limited number of studies that we could include in our meta‐analyses for the primary outcomes (fewer than 10 studies; Deeks 2019), we were not able to conduct the planned subgroup analyses to examine key characteristics of studies that may be associated with the substantial heterogeneity detected for several outcomes (see Effects of interventions). We were also unable to perform a subgroup analysis for training intensity (post hoc addition).
Sensitivity analysis
Due to the limited number of studies we were able to include in our meta‐analyses for the primary outcomes (fewer than 10 studies; Deeks 2019), we did not conduct most of the planned sensitivity analyses to test the robustness of the findings of this review.
However, for the primary outcomes at post‐test (i.e. the main analyses of this review), we performed the planned sensitivity analysis using a fixed‐effect model in addition to random‐effects meta‐analyses.
Results
Description of studies
Results of the search
We ran the first searches for this review in October 2016 according to the protocol (Helmreich 2017). We used the strategies in Appendix 8 to find studies in which the participants included any adults aged 18 years and older. Due to the large number of potentially eligible studies, we decided to split the review and changed the inclusion criteria to focus on healthcare sector workers and students (see Differences between protocol and review). Before running the top‐up searches in June 2019, we revised the original search strategy by limiting the population to healthcare sector workers and students (Appendix 9). Following these searches, we further revised the inclusion criteria to healthcare students only, which is the focus of this review.
In total, the database searches retrieved 37,737 records. We found an additional 663 records by searching other resources. Following de‐duplication, we screened the remaining 24,703 records by title and abstract. We deemed 21,629 records to be irrelevant and sought the full texts of the remaining 3074 records for further assessment. At the level of title/abstract screening, we achieved a good agreement (kappa = 0.70) for the original search, and an excellent agreement for the top‐up searches (kappa = 0.99). The full‐text screening resulted in excellent inter‐rater reliability for both the original search (kappa = 0.95) and the top‐up searches (kappa = 1).
After revising the eligibility criteria to focus broadly on the healthcare sector (including healthcare professionals and healthcare students; see Differences between protocol and review), we identified 80 studies that were performed in any of these groups. We also identified nine ongoing studies and 29 studies awaiting classification. We found six additional reports of studies during the top‐up searches.
Finally, after revising the eligibility criteria to focus on healthcare students, we reassessed these 118 studies (from 144 reports). In total, for healthcare students, we included 30 studies (from 34 reports). We excluded a total of 3010 full text reports (see Figure 1); this figure includes 15 reports (13 excluded studies), which we needed to examine in detail to determine eligibility, and which are described in the Characteristics of excluded studies. We identified 22 studies awaiting classification (see Studies awaiting classification) and three ongoing studies (see Ongoing studies). For further details of our screening process, see the study flow diagram (Figure 1). We present the results of both searches in more detail in Appendix 12.
1.
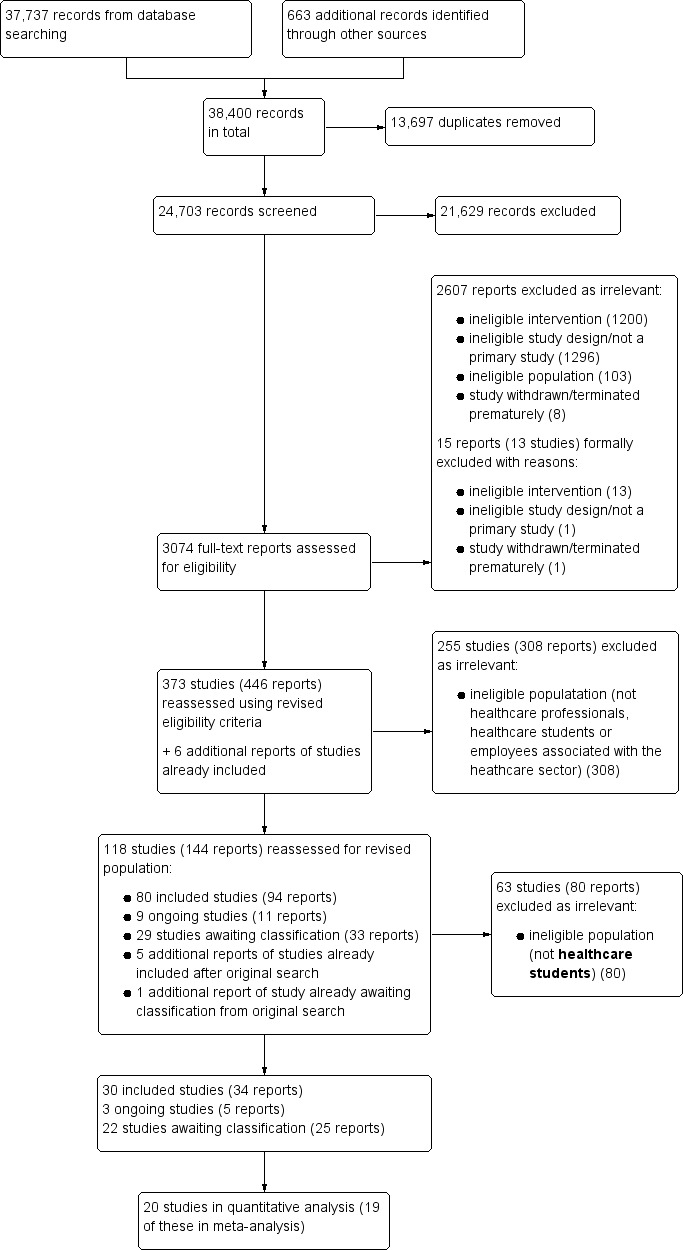
Study flow diagram for all searches.
From an updated (pre‐publication) search of four key databases in June 2020, we have added 16 studies (from 16 reports) to the Characteristics of studies awaiting classification tables. The results of these studies are not yet included in this review and will be incorporated at the next update. We also found an additional report of the included study by Houston 2017 (First 2018: a qualitative study in a subsample of Houston 2017).
Included studies
We present the corresponding references for the description of included studies in Appendix 13.
Study design
All 30 included studies were parallel‐group designs, published between 2005 and 2019, with the exception of one completed but unpublished trial: ISRCTN64217625.
Location
Eleven studies were conducted in the USA, four in Canada, and three in Iran. Two studies apiece were performed in Australia, Germany, China, and the UK. The remaining studies took place in Belgium (Geschwind 2015), India (Mathad 2017), Switzerland (Recabarren 2019), and The Netherlands (Smeets 2014).
Settings
Training programmes were delivered at university or in schools (e.g. nursing school, school of medicine) in 11 studies. For nine studies, the intervention site was not further specified. As four studies included online or mobile resilience interventions, there was no concrete venue and participants could participate regardless of location. Three interventions took place in a laboratory. Two training programmes could be performed in the home setting (using a spoken compact disc (CD)). One resilience training was conducted in a mixed setting (online training plus face‐to‐face sessions with implementation site not further specified) (ISRCTN64217625).
Participants
Participants were mainly young women, due to the student sample (one study in doctoral candidates, Barry 2019). Most studies evaluated a resilience‐training programme in nursing or midwifery students, closely followed by medical students with an almost equal number of studies.
The total number of healthcare students randomised across 20 of the 30 included studies was 1315 (including one completed but unpublished study: ISRCTN64217625 (targeting number: 50)). For eight studies with mixed samples (Barry 2019; Galante 2018; Geschwind 2015; Goldstein 2019; Houston 2017; Recabarren 2019; Venieris 2017; Victor 2018), the total number of participants randomised was 1365 participants. While the original number of healthcare students randomised in most of these mixed‐sample studies is unclear, we received information from the authors for five studies (Barry 2019; Geschwind 2015; Houston 2017; Recabarren 2019; Victor 2018). For two studies, Kelleher 2018 and Samouei 2015, it was unclear how many participants were randomised. Overall, eight studies randomised 100 or more participants, and five studies randomised 30 participants or fewer.
Where data on age were available, the mean age across 13 studies in healthcare students (no studies with mixed samples) ranged from 19.5 to 26.83 years (SDs ranging from 0.77 to 5.12 years), with an average of 22.29 years (mean SD = 2.12 years). For mean age in studies with mixed samples, six out of eight studies reported a range of 19.35 to 38.14 years (SD ranging from 1.98 to 11.33 years) for the total samples, including healthcare students, with an average of 25.14 years (mean SD = 4.65 years). Three studies did not report mean age, but only the age range of participants (Houston 2017; Waddell 2005; Waddell 2015), and two studies (Galante 2018; Delaney 2016) considered participants aged 17 or 18 years and above, respectively. Six studies did not specify the age of the sample or were unclear (Chen 2018a; ISRCTN64217625; Kelleher 2018; Mejia‐Downs 2016; Miu 2016; Samouei 2015).
Women outnumbered men in seven studies conducted solely in healthcare students, and men predominated in a further six studies. Three studies included only women. For six studies, the sex of the participants was unclear (Chen 2018a; ISRCTN64217625; Kelleher 2018; Mejia‐Downs 2016; Samouei 2015; Waddell 2005). For 14 studies presenting the total numbers of men and women investigated, the proportion of women was 63.3%. Women outnumbered men in seven of the eight studies with mixed samples; one mixed‐sample study included only women. The proportion of women in eight studies with mixed samples that reported total numbers by sex was approximately 67.3%.
Eight studies included solely nursing or midwifery students, and seven were conducted in medical students. Three studies involved paramedic students and two involved psychology students. Two studies included physical therapy students. The eight remaining studies were performed with mixed samples, i.e. healthcare students combined with other individuals such as volunteers or students in other fields. Relevant subgroups within these studies included: university students (Goldstein 2019; Houston 2017); doctoral candidates in different health fields (Barry 2019); psychology students (Geschwind 2015; Recabarren 2019; Victor 2018); 'Clinical medicine' and 'Humanities and social sciences' students (p e76; Galante 2018); students in 'Health & Wellness' and 'Social and Behavioral Sciences' (p 146; Venieris 2017).
Twelve of the 30 studies assessed mental health at baseline. All studies measuring mental health used self‐report (screening) measures covering one or a small number of mental dysfunctions (e.g. Depression Anxiety and Stress Scales (DASS) in Barry 2019). Only one of these studies also conducted comprehensive baseline diagnostics with the use of a structured interview (Mini‐International Neuropsychiatric Interview (MINI); (Recabarren 2019). Seventeen studies provided no data about the mental health status of the sample. For one unpublished trial (ISRCTN64217625) and one study published as a conference abstract (Goldstein 2019), the baseline mental health status was unclear, although both of them assessed mental health at baseline. Eight studies included mentally healthy participants only (Akbari 2017; Recabarren 2019), participants without severe psychiatric illness (not further specified; Mathad 2017), participants showing symptoms below a cut‐off on a screening instrument (Barry 2019; Wang 2012; Warnecke 2011) or participants without certain mental disorders or suicidality, e.g. bipolar disorder, psychosis (Miu 2016; Victor 2018). Wang 2012 only considered participants with a mental crisis. Since Victor 2018 focused on burdened students, they included participants with a symptom burden of four or more on the Global Severity Index of the Brief Symptom Inventory.
Interventions
All 30 studies examined the effects of a psychological intervention to foster resilience, hardiness or post‐traumatic growth in healthcare students, compared to a control condition. Most studies evaluated group interventions (17 studies), that were delivered face‐to‐face (17 studies) and were structured on mindfulness‐based theoretical approaches (eight studies). High‐intensity interventions (11 studies) and training programmes of low intensity (10 studies) were relatively balanced.
Two studies had multiple intervention arms (Kötter 2016; Venieris 2017). In a three‐arm study (Kötter 2016), one intervention group (IG1) participated in a one‐hour psycho‐educative seminar (e.g. emotional reactions towards stressors) plus two individual coaching sessions, with the latter designed to foster individual stress‐management resources (i.e. resilience) using techniques such as eye movement desensitisation and neurolinguistic programming. IG2 received the psycho‐educative seminar only. Due to an unexpected shortfall in the sample size, the study authors combined both intervention arms in the quantitative analyses. Venieris 2017 was a three‐arm study comparing a positive psychology intervention (PPI; IG1) to an informative stress intervention (IG2) or a wait‐list control group. The PPI asked participants to engage in one of five activities (e.g. '3 grateful things') everyday for three weeks, whereas IG2 provided information about stress and positive coping mechanisms. Since the study authors hypothesised an increase in resilience in the PPI group compared to the remaining groups, we considered this group to be relevant for our review.
Setting
Seventeen interventions were performed in groups. Seven studies were conducted in an individual setting. Four studies were performed in a variety of training settings. Two studies did not specify the type of setting (Chen 2018a; Miu 2016).
Delivery format
Seventeen studies delivered resilience interventions face‐to‐face. Five studies used multimodal delivery of interventions (e.g. face‐to‐face group sessions and internet‐based training). Four studies examined online or mobile‐based resilience‐training programmes, and two studies tested interventions that were conducted in a laboratory setting and unlikely with face‐to‐face contact.Two studies used an audio intervention.
Training intensity
Treatment duration varied between a 20‐minute single intervention session (Geschwind 2015) and 40 hours in total, i.e. one hour a day for five days a week over eight weeks (Mathad 2017). Eleven studies included high‐intensity training (more than 12 hours or more than 12 sessions). Ten RCTs investigated low‐intensity interventions (i.e. less than five hours or three sessions or fewer), and seven studies evaluated moderate‐intensity training (i.e. more than five hours to 12 hours or less, or more than three sessions to 12 sessions or fewer). The intensity of the training was unclear for two interventions (Barry 2019; Venieris 2017).
Theoretical foundations
We categorised the interventions into six groups, based on their content and the descriptions provided by the study authors. We present a synthesis of the characteristics of studies within a specific theoretical foundation and the respective intervention content in Appendix 14.
Eight studies evaluated mindfulness‐based resilience interventions, including MBSR (Erogul 2014; Kelleher 2018) and content related to mindfulness‐based (self‐)compassion (e.g. Chen 2018a; Smeets 2014). Seven RCTs examined nonspecific resilience interventions that did not give details of the type of resilience‐training programmes conducted or their theoretical orientation, but aimed at fostering one or several prespecified resilience factors (see Appendix 2, level 1, e.g. self‐esteem, social support, active coping by problem‐solving, spirituality). Six studies included interventions based on a combination of two or more explicit theoretical foundations (e.g. CBT and positive psychology). Of these, two were based on mindfulness (e.g. MBSR) and CBT or cognitive therapy (ISRCTN64217625; Recabarren 2019), and four combined interventions that could not be clustered any further (Delaney 2016; Goldstein 2019; Kötter 2016; Victor 2018). Four resilience‐training programmes were based on positive psychology. Three interventions included only elements of CBT. Resilience‐training programmes based on coaching approaches were tested in two studies.
Comparators
With the exception of one study (Victor 2018), all 30 included studies involved only one comparator. In Victor 2018, the intervention group PRM (see Interventions) was compared to attention control and wait‐list control groups. For this review, we considered only the attention‐control group to be relevant.
Most studies included wait‐list control groups (10/30 studies) and no intervention comparators (7/30 studies), followed by attention control (6/30 studies; Victor 2018 (second CG)), active control (3/30 studies) and TAU (3/30 studies). Two studies did not specify the type of control group (Anderson 2017; Wang 2012).
Of the six studies comparing a resilience intervention with an attention‐control group, two studies conducted in a laboratory setting either instructed participants to think about a typical day and visualise this scenario for five minutes (Geschwind 2015), or used the ‘Wisdom On Wellness’ (WOW) intervention, which included some level of social interaction (Goldstein 2019). Further attention‐control comparators included a single laboratory session on the role of the brain and information processing (participants had to read an article, read testimonials from others and write to others about what they learned; Miu 2016); a time management intervention (Smeets 2014); an educational intervention on Twitter consisting of nursing trivia or questions related to nursing knowledge (Stephens 2012); and individual coaching sessions on the ABC (Activating event, Belief, Consequences) model (e.g. challenging dysfunctional and testing alternative thoughts) (Victor 2018).
In three studies, active control groups included a booklet and a worksheet on therapeutic communication (Delaney 2016); brochures about scientific information unrelated to psychology (Samouei 2015); and a standard, group‐based resilience training (Mind's resilience intervention; ISRCTN64217625). We considered the last intervention to use an active control group, rather than TAU, because the Mind’s group‐based resilience intervention for emergency personnel had been newly developed in a recent study (Wild 2016), and was not yet considered as established standard care.
In three studies, TAU referred to usual mental health support (Galante 2018), or a standard undergraduate curriculum group for nursing students (Waddell 2015). Warnecke 2011 did not further specify the content of the TAU group.
One study used a design where a control group plus resilience intervention was compared to the control group alone (Galante 2018). One completed but unpublished study (ISRCTN64217625) examined the impact of a face‐to‐face resilience intervention (control group) versus the same resilience intervention with an additional internet‐based top‐up session (intervention group).
Outcome measures
The included RCTs used a diversity of outcome measures, but some studies measuring the same outcomes (e.g. perceived stress) used the same instrument (e.g. Perceived Stress Scale; Cohen 1983b; Cohen 1988a). All outcomes were based on self‐reported assessments and most studies used validated scales.
Primary outcomes
We defined treatment efficacy as an improvement in resilience, assessed by specific resilience scales, or an improvement in four categories of mental health and well‐being (i.e. anxiety, depression, stress or stress perception, and well‐being or quality of life). For each outcome, the studies used heterogeneous scales (see details in Table 3). Among the 30 included studies, 17 assessed resilience using a resilience scale, followed by stress or stress perception (13 studies), depression (e.g. depressive symptoms; 10 studies), anxiety (nine studies) and well‐being or quality of life (six studies).
Secondary outcomes
The authors of the included studies used a heterogeneous group of instruments to assess the secondary outcomes (see details in Table 4). Most of the included studies assessed self‐efficacy (seven studies), followed by positive emotions (six studies). Social support and optimism were assessed by four studies each. Active coping and self‐esteem were assessed by two studies each, while hardiness was an outcome measure in one study.
Funding sources
Funding sources for the included studies were various, and in six studies included universities (e.g. certain faculties, medical schools) and university research funds. In four studies, further funding was provided by different foundations. Two studies received funding from the nursing organisation Sigma Theta Tau. Single studies were supported by a scholarship (Waddell 2005), the Graduate and Professional Student Association (Venieris 2017), the US Substance Abuse and Mental Health Services Administration through a university's Disaster and Community Crisis Center (Houston 2017), and the Social Sciences and Humanities Council (Waddell 2015). Four studies reported a combination of funding sources (e.g. Canadian Mental Health Association, Campus Capacity Development Grant and Justice Institute of British Columbia; university, National Institute for Health Research Collaboration and Care East England; award and graduate research fellowship; university and charity). Seven studies did not report their funding sources (Mathad 2017; Miu 2016; Smeets 2014; Victor 2018; Wang 2012) or did not offer the information (e.g. conference abstract) (Chen 2018a; Kelleher 2018). Three studies received no funding support (Mueller 2018; Samouei 2015; Sahranavard 2018).
Excluded studies
We excluded 3010 irrelevant full text reports.
We excluded 13 studies that seemed to merit inclusion but on closer inspection did not (see Characteristics of excluded studies). Most of these studies (11/13) were excluded for an ineligible intervention (Brady 2016; De la Fuente 2018; De Vibe 2013; Duan 2019; Dvořáková 2017; Esch 2013; Huennekens 2018; Pogrebtsova 2018; Sampl 2017; Song 2015; Van Dijk 2015). Of these, eight studies only briefly mentioned the concept of resilience or a related construct (e.g. in the introduction or discussion section of a publication), but did not explicitly state the aim of fostering resilience, hardiness or post‐traumatic growth through the intervention (Brady 2016; De la Fuente 2018; De Vibe 2013; Dvořáková 2017; Esch 2013; Huennekens 2018; Pogrebtsova 2018; Song 2015). It was also unclear in Dvořáková 2017 whether healthcare students were included. Duan 2019 evaluated an intervention based on strengths‐based CBT to build resilience (Padesky 2012). However, the authors did not specify the intention of fostering resilience. Sampl 2017 (psychology students included) often mentioned the concept of resilience, but we excluded the study as, according to the investigators, it primarily focused on (measured) constructs such as mindfulness. Van Dijk 2015 was excluded, as the study mentioned resilience in a publication reporting baseline results of the RCT, but not in the final report.
We excluded one study due to ineligible study design: Victor 2017 evaluated a strengths‐based CBT intervention to foster resilience in first‐year psychology students by randomising participants to either the training or to a no‐intervention control group. However, as participants were free not to follow the invitation, the authors pointed out that randomisation may have been jeopardised by self‐selection bias. We therefore excluded this study for an ineligible study design.
Finally, we did not include ACTRN12617000300370, as we received information from the primary investigators that the trial in university staff failed to obtain human resources approval to proceed, and that the authors did not have any data relevant to the meta‐analysis.
Studies awaiting classification
We identified 22 studies awaiting classification.
For 20 studies, it was unclear whether the final sample also included healthcare students (Arch 2014; Bauman 2014; Beadel 2016; Chen 2018b; DRKS00011265; DRKS00013765; Enrique 2019; Gerson 2013 (study 1); Gerson 2013 (study 2); Harrer 2018; Herrero 2019; ISRCTN17156687; Kanekar 2010; Liu 2016; NCT02867657; NCT03903978; Oman 2008; Roghanchi 2013; Seligman 2007; Zhang 2018). In six studies (Arch 2014; Bauman 2014; Beadel 2016; Gerson 2013 (study 1); Gerson 2013 (study 2); Oman 2008), for example, the study authors reported partial recruitment in psychology departments. However, whether psychology students had been included in the final sample was not specified in the reports and could not be obtained from the study authors. Similarly, 14 studies only described recruiting university or college students in general, and based on the available reports it was unclear if the final samples included healthcare students at all (Chen 2018b; DRKS00011265; DRKS00013765; Enrique 2019; Harrer 2018; Herrero 2019; ISRCTN17156687; Kanekar 2010; Liu 2016; NCT02867657; NCT03903978; Roghanchi 2013; Seligman 2007; Zhang 2018).
In one study (NCT03669016) resilience was assessed as a secondary outcome, but we could not clearly determine the extent to which the trial focused on fostering this construct based on the trial registration, and received no response from the authors. The same applied to Chen 2018b, for which resilience or a related construct was not mentioned in the available conference abstract.
The study design of Ye 2016 could not be clearly determined, since the full text was not available and we identified no contact details to ask the study authors for more information. The same applied to Zhang 2018 (available as a conference abstract) and to Liu 2016, for which, besides the potential inclusion of healthcare students, randomisation was also unclear.
Details of these studies can be found in the Characteristics of studies awaiting classification tables.
Sixteen studies from the updated search in June 2020 were also added to the Characteristics of studies awaiting classification tables. They will be incorporated into this review at the update stage.
Ongoing studies
We found three ongoing studies that are likely to meet our inclusion criteria (Harrer 2019; NL7623; Wild 2018). All three studies are RCTs with parallel assignment. In a sample of German distance‐learning students experiencing elevated levels of depression (including psychology students), Harrer 2019 assessed the impact of TAU (e.g. general practitioner visits, counselling services) plus StudiCare Fernstudierende (a seven‐week online intervention with feedback on demand) versus usual care plus attention control (online psycho‐education). The intervention involved information about stress, systematic problem‐solving, muscle and breath relaxation, mindfulness, acceptance and tolerance, self‐compassion and creating a master plan (e.g. recognising physiological warning signs, creating a plan for the future). Using a longitudinal observation cohort study with a nested RCT, a Dutch study (NL7623) randomised students at the Erasmus University Medical Center in Rotterdam to either resilience training or an active control (psycho‐education about chronic stress and burnout prevention). In contrast to the other ongoing studies, the intervention group did not receive only one treatment, but followed a maximum of three intervention periods (e.g. mindfulness training, stress management training) of eight weeks each. Wild 2018 examined the impact of an internet‐based cognitive training for resilience (iCT‐R) versus attention control (mind‐online) and TAU (usual support by university) in a sample of paramedic students.
Further details of these studies can be found in the Characteristics of ongoing studies tables.
Risk of bias in included studies
The main limitations we found for risks of bias (≥ 20% high risk) across the 30 studies were in the following domains: performance bias, detection bias, attrition bias, and reporting bias. See Figure 2 and Figure 3 for ‘Risk of bias’ graphs, and Characteristics of included studies tables for further information. A large number of studies provided insufficient information to adequately judge the risk of selection bias. We identified the greatest variation across studies for attrition and reporting biases.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Sequence generation
We rated eight studies at low risk of selection bias, since the investigators described a random component in the sequence‐generation process (e.g. computer‐generated random sequence, shuffling cards). For five of these, there was verified baseline comparability between study groups for sociodemographic characteristics (i.e. potential confounding factors) as well as outcome variables (Mueller 2018; Smeets 2014; Venieris 2017; Victor 2018; Waddell 2015). For three studies, there was evidence of a genuine random assignment (e.g. computer‐generated random sequence), but the authors provided no information (Galante 2018) or only partial information about potential baseline differences in sociodemographic and outcome measures (Recabarren 2019; Stephens 2012).
We rated 14 studies as having unclear risk of selection bias because there was no description of the sequence‐generation process (Akbari 2017; Anderson 2017; Delaney 2016; Erogul 2014; Houston 2017, Kötter 2016; Mathad 2017; Peng 2014; Porter 2008; Sahranavard 2018; Samouei 2015; Waddell 2005; Wang 2012; Warnecke 2011). Nine of these RCTs did not specify further the baseline comparability of groups for (some) sociodemographic characteristics or outcomes of interest, or both (Akbari 2017; Houston 2017; Kötter 2016; Mathad 2017; Peng 2014; Porter 2008; Sahranavard 2018; Samouei 2015; Waddell 2005). Based on the limited information in conference abstracts or trial registrations, we considered five further studies at unclear risk of bias (Chen 2018a; Goldstein 2019; ISRCTN64217625; Kelleher 2018; Mejia‐Downs 2016).
We judged three studies to be at high risk of selection bias since, despite randomisation, baseline comparability in sociodemographic characteristics or outcomes (or both) could not be verified by the investigators based on statistical analysis (Barry 2019; Geschwind 2015; Miu 2016).
Allocation concealment
Allocation concealment was not well reported and we rated all 30 included studies at unclear risk of selection bias for this domain.
Five studies described the randomisation process being concealed from participants or from personnel recruiting participants, or both, but neglected to specify further the method of allocation concealment (Erogul 2014; Miu 2016; Mueller 2018; Recabarren 2019; Waddell 2015).
The authors of 20 studies provided either insufficient or no information about the allocation concealment process (Akbari 2017; Anderson 2017; Barry 2019; Delaney 2016; Galante 2018; Geschwind 2015; Houston 2017; Kötter 2016; Mathad 2017; Peng 2014; Porter 2008; Sahranavard 2018; Samouei 2015; Smeets 2014; Stephens 2012; Venieris 2017; Victor 2018; Waddell 2005; Wang 2012; Warnecke 2011). In Barry 2019, the random‐sequence generation was probably concealed from the participants (sealed trial pack that participants were instructed to open only after the baseline assessment), but the allocation concealment for the investigators enrolling the participants was not specified. Similarly, for the two randomisation procedures used in Kötter 2016, the study authors described the allocation concealment in sufficient detail (sealed, opaque envelopes) for the second randomisation (IG1 versus IG2), but it was unclear for the first randomisation to either treatment or control group.
There was limited information in conference abstracts or trial registrations to reach a decision on the risk of bias for five studies, and we therefore rated them as having an unclear risk of bias (Chen 2018a; Goldstein 2019; ISRCTN64217625; Kelleher 2018; Mejia‐Downs 2016).
Blinding
Blinding of participants and personnel
Objective outcomes
Five of the 30 studies assessed one or several objective outcomes such as physical activity by accelerometers, heart/breathing rate or grade point average (Delaney 2016; Galante 2018; Goldstein 2019; ISRCTN64217625; Kelleher 2018). Although study personnel were not blinded in most of these studies (see next paragraph on subjective outcomes below), we judged these studies to be at low risk of performance bias in relation to objective outcomes.
Subjective outcomes
We considered only one of the 30 studies to be at low risk of performance bias for subjective outcomes (Miu 2016), as this was a double‐blind RCT.
We rated two studies at unclear risk of performance bias (Anderson 2017; Venieris 2017). Anderson 2017 performed a (blended) online resilience intervention without specifying the blinding of participants and personnel. Venieris 2017 also delivered a training programme through an online educational system, and the blinding of participants was probably ensured (i.e. participants were not specifically informed about the number or nature of study conditions, but only informed that they may or may not be asked to participate in different activities), but there was insufficient information about the potential blinding of study personnel.
We judged 22 studies to be at high risk of performance bias because resilience interventions were performed entirely face‐to‐face (Akbari 2017; Chen 2018a; Delaney 2016; Erogul 2014; Galante 2018; Goldstein 2019; Houston 2017; Kelleher 2018; Kötter 2016; Mathad 2017; Mejia‐Downs 2016; Peng 2014; Porter 2008; Recabarren 2019; Sahranavard 2018; Samouei 2015; Victor 2018; Waddell 2015; Wang 2012), or included face‐to‐face elements (ISRCTN64217625; Smeets 2014; Waddell 2005), resulting in a lack of blinding of personnel. Some of these studies explicitly indicated the lack of blinding of both participants and personnel (e.g. Galante 2018; Kötter 2016; Recabarren 2019). We also rated five other studies at high risk of performance bias for the following reasons. Barry 2019 and Warnecke 2011, which were described as single‐blind studies, provided participants with a spoken CD. While Warnecke 2011 described no blinding of participants, it was unclear whether or not study personnel or participants had been blinded in Barry 2019. Mueller 2018 performed an online, self‐guided intervention and indicated no blinding of participants; blinding of study personnel was unlikely also, as they monitored discussion‐board postings within the intervention. Stephens 2012 conducted a resilience‐training programme on Twitter by only one researcher who also performed the outcome assessment. Geschwind 2015 included a resilience intervention that was conducted in a laboratory. Although there was no face‐to‐face contact, the study personnel in these studies were not blinded, as verbal communication with participants was possible and participants were observed by the intervention providers.
Blinding of outcome assessment
Objective outcomes
We considered all five studies measuring objective outcomes to be at low risk of detection bias. Although two of these studies did not adequately describe the blinding of outcome assessment (Delaney 2016; Galante 2018), we judged them to be at low risk of detection bias, since they used objective outcomes (e.g. physiological parameters), which we considered unlikely to be influenced by the lack of blinding. We applied the same rating to three other studies that used objective outcomes, even though there was insufficient information in the conference abstracts, posters or trial registrations (Goldstein 2019; Kelleher 2018; ISRCTN64217625).
Subjective outcomes
We judged only two studies to be at low risk of detection bias for the assessment of subjective outcomes (Galante 2018; Miu 2016), for the following reasons: data were collected using web‐based software to ensure masking of outcome assessors (Galante 2018), or researchers blind to condition provided a link to an online survey (Miu 2016).
We considered four studies to be at unclear risk of detection bias, because the study authors did not adequately describe the blinding of the results (Anderson 2017; Barry 2019; Geschwind 2015; Venieris 2017), and the risk of performance bias (i.e. blinding of participants) was low or unclear (see blinding of participants and personnel).
Finally, we rated 24 studies at high risk of detection bias. Blinding of outcome assessment seemed unlikely in Kötter 2016 for the assessment after first randomisation, since the group allocation was concealed neither from study personnel nor from the participants (unclear blinding for the second assessment). In Stephens 2012, the outcome assessor was the same individual who provided the intervention and therefore could not be blinded. For the remaining 22 studies, due to (potential) performance bias (no blinding of participants), we judged that the participants' responses to questionnaires may be likely to be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) (Akbari 2017; Chen 2018a; Delaney 2016; Erogul 2014; Goldstein 2019; Houston 2017; ISRCTN64217625; Kelleher 2018; Mathad 2017; Mejia‐Downs 2016; Mueller 2018; Peng 2014; Porter 2008; Recabarren 2019; Sahranavard 2018; Samouei 2015; Smeets 2014; Victor 2018; Waddell 2005; Waddell 2015; Wang 2012; Warnecke 2011).
Incomplete outcome data
We assessed 13 studies as having low attrition bias because they met at least one of the following criteria: the losses were similar across intervention and control groups; the reasons for missing data were unlikely to be related to the true outcome (e.g. dropout due to pregnancy); the losses were not substantial (< 10% from number of randomised participants; e.g. two dropouts from 70 participants in Wang 2012) and/or study authors accounted for dropouts and losses to follow‐up by using statistical analyses aimed at reducing bias (e.g. multiple imputation) or preventing false‐positive conclusions (e.g. last observation carried forward) (Delaney 2016; Erogul 2014; Galante 2018; Houston 2017; Kötter 2016; Mejia‐Downs 2016; Mueller 2018; Peng 2014; Recabarren 2019; Smeets 2014; Stephens 2012; Victor 2018; Wang 2012). Four studies performed an intention‐to‐treat (ITT) analysis (Galante 2018; Kötter 2016; Recabarren 2019; Victor 2018). Based on data provided by the original investigator, Mejia‐Downs 2016 analysed all randomised participants, but it is unclear if there were any missing data that were imputed. The same applied to Peng 2014, who reported results for all participants randomised but did not state the level of missing data. Smeets 2014 provided contradictory information about the number of participants analysed (available‐case analysis according to p 797 versus ITT analysis according to Table 2 in the report), but we judged the study to be at low risk of bias, as the dropout was not substantial. Delaney 2016 did not clearly specify the number of participants analysed and we relied on the numbers reported in the publications, as we had no response from the study authors.
We rated eight studies at unclear risk of attrition bias. Four studies did not fully account for dropouts throughout the study or whether this differed between groups (Akbari 2017; Anderson 2017; Geschwind 2015; Samouei 2015). Samouei 2015 did not report the number of participants randomly allocated to each group. Anderson 2017 and two other studies (Sahranavard 2018; Waddell 2005: especially after phase two) did not clearly specify the number of participants analysed and we relied on the numbers reported in the publications, having received no response from the study authors, or had to derive these indirectly from other statistical values in the report with the help of the statistician (JK). We could not judge the risk of attrition bias from the information available in conference abstracts or trial registrations for two studies (ISRCTN64217625; Kelleher 2018), which we consequently rated at unclear risk of bias.
We considered nine studies to be at high risk of attrition bias. In three of these, the reasons for missing data were unlikely to be related to the true outcome (e.g. similar levels of missing data between groups with a difference of two or less lost individuals); however, there was substantial attrition (10% or more compared to the randomised sample), and study authors did not impute the missing data and performed an available‐case analysis (i.e. participants for whom outcomes were obtained at assessments) or a per‐protocol analysis (i.e. only participants who complied with their allocated intervention or attended a certain number of sessions), or both (Mathad 2017; Porter 2008; Warnecke 2011). Despite an imbalance in the levels of missing data between groups in Warnecke 2011, the investigators ensured that reasons for missing data were unlikely to be related to the true outcome, based on non‐significant differences in demographic and outcome variables between completers and non‐completers of the study (i.e. random loss). Missing data in the study were treated as absent and the study authors performed an available‐case analysis. Two studies did not provide sufficient information about dropouts, such as the number of participants randomised to each group or attrition by group (Chen 2018a; Waddell 2015). Based on the number of participants analysed, we presumed an available‐case or per‐protocol analysis, or both (e.g. no hypothesis testing in Chen 2018a due to dropout), and considered both studies to be at high risk of bias because of substantial dropout (≥ 10%). In four other studies at high risk of attrition bias (Barry 2019;Goldstein 2019; Miu 2016; Venieris 2017), reasons for missing data were likely to be related to the true outcome because of imbalance in missing data between groups, and an available‐case or per‐protocol analysis (or both) was conducted in all four studies. Not all studies reported reasons for missing data (e.g. Venieris 2017).
Selective reporting
To assess potential reporting bias for 22 non‐registered studies or those without a published study protocol (Anderson 2017; Barry 2019; Delaney 2016; Erogul 2014; Galante 2018; Geschwind 2015; Houston 2017; Mathad 2017; Miu 2016; Mueller 2018; Peng 2014; Porter 2008; Sahranavard 2018; Samouei 2015; Smeets 2014; Stephens 2012; Venieris 2017; Victor 2018; Waddell 2005; Waddell 2015; Wang 2012; Warnecke 2011), we considered whether the outcome measures described in the Methods section of the paper were reported in the Results section. We were unable to assess reporting bias for three additional, non‐registered studies, for which only conference abstracts were available (Chen 2018a; Goldstein 2019; Kelleher 2018).
Of the 25 non‐registered studies, we considered 19 to be free of reporting bias because the published results corresponded to those expected in these types of studies (Anderson 2017; Barry 2019; Delaney 2016; Erogul 2014; Geschwind 2015; Houston 2017; Mathad 2017; Miu 2016; Mueller 2018; Peng 2014; Porter 2008; Sahranavard 2018; Smeets 2014; Stephens 2012; Venieris 2017; Victor 2018; Waddell 2005; Wang 2012; Warnecke 2011). We rated four studies (including three reported as conference abstracts) at unclear risk of reporting bias (Chen 2018a; Goldstein 2019; Kelleher 2018; Waddell 2015); in Waddell 2015, although the published report seemed to include all expected outcomes, the reported assessment at time four was not further specified (i.e. it is unclear whether it is a 12‐month follow‐up period or a post‐test assessment). We judged two studies to be at high risk of bias, largely because not all prespecified outcomes were reported (Galante 2018; Samouei 2015).
Five studies were prospectively or retrospectively registered (Akbari 2017; ISRCTN64217625; Kötter 2016; Mejia‐Downs 2016; Recabarren 2019). Of these registered studies, we considered one study to be at low risk of reporting bias as the (unpublished) report included all expected outcomes in the prespecified way (Mejia‐Downs 2016); no full text (dissertation) was available for this study, but we considered the risk of reporting bias to be low based on the Results section, which was provided by the study author in response to our email request. For one registered trial (ISRCTN64217625) we could not determine the risk of reporting bias on the basis of trial registration, as the study was completed but unpublished and no further information was provided by the study authors during the publication process. We judged three registered studies to be at high risk of reporting bias because not all of the prespecified outcomes (Recabarren 2019) or time points (Akbari 2017; Kötter 2016) were reported. According to the study authors, Recabarren 2019 was only the first publication for this study, so future publications reporting the other prespecified outcomes are possible.
Effects of interventions
See: Table 1
See: Table 1.
Overall, across the included studies in healthcare students, we were able to perform 14 pooled analyses that combined at least two studies.
We analysed effects on all primary outcomes at immediate post‐intervention and at short‐term follow‐up (except for well‐being or quality of life). No meta‐analyses were possible for any of the primary outcomes at medium‐term or long‐term follow‐up. For the secondary outcomes, we performed meta‐analyses for social support, optimism, self‐efficacy and positive emotions at post‐intervention, and social support at short‐term follow‐up. For several secondary outcomes, i.e. active coping, self‐esteem and positive emotions, only single‐study results were available at short‐term follow‐up (three months or less). No secondary outcome was measured at medium‐ or long‐term follow‐up.
We present the different outcome measures that we used to assess the primary and secondary outcomes in the included studies in Table 3 and Table 4, respectively. For the primary outcomes of resilience and well‐being or quality of life, as well as all secondary outcomes (social support, optimism, self‐efficacy, active coping, self‐esteem, hardiness, positive emotions), positive values indicate a higher (i.e. better) level of the corresponding outcome in the intervention group compared to the control group (e.g. higher resilience), whereas negative values refer to lower levels of the respective outcome in the intervention arm. For the remaining primary outcomes of anxiety, depression and stress or stress perception, negative values indicate a lower (i.e. better) level of these outcomes in the intervention arm (e.g. fewer depressive symptoms) compared to the control arm, while positive values refer to a higher level of depression, anxiety and stress or stress perception in the intervention group compared to control.
We report P values exactly, and where provided by the study authors, unless P values are lower than 0.001, in which case they are expressed as P < 0.001. T values and P values of Egger's tests were rounded.
Resilience interventions versus control conditions in healthcare students
Primary outcomes
Resilience
Post‐intervention
Thirteen studies evaluated the effect of resilience interventions compared to control groups on resilience at immediate post‐intervention.
Nine studies reported data suitable for quantitative analysis (Anderson 2017; Barry 2019; Erogul 2014; Houston 2017; Mathad 2017; Mueller 2018; Peng 2014; Stephens 2012; Wang 2012), including two studies with mixed samples (Barry 2019; Houston 2017) for which we obtained subgroup data for healthcare students by contacting the study authors. The pooled effect estimate suggests evidence of a moderate effect of resilience interventions on resilience at post‐intervention (standardised mean difference (SMD) 0.43, 95% confidence interval (CI) 0.07 to 0.78; P = 0.02; 9 studies, 561 participants; I2 = 75%; Tau2 = 0.21; P for heterogeneity < 0.001; G2 = 55.9%; 95% prediction interval: −0.54 to 1.41; Analysis 1.1; very‐low certainty evidence, see Table 1).
1.1. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 1: Resilience: post‐intervention
For resilience at post‐intervention, we found no evidence of asymmetry based on funnel plots and Egger’s test (t = −1.42; df = 7; P = 0.20; see Appendix 15 and Appendix 16).
Indicators of statistical heterogeneity were mixed, with I2 and Chi2 values indicating substantial to considerable heterogeneity, while G2 suggested moderate heterogeneity.
Single‐study results
Four studies also measuring resilience at post‐intervention could not be pooled with the studies above for the following reasons: for one unpublished study (ISRCTN64217625) we could not obtain the data from the study authors (i.e. trial completed, but publication process still ongoing). The same applied to two studies only available as conference abstracts (Chen 2018a; Kelleher 2018). Without indicating statistical values, Kelleher 2018 (sample size not specified) reported higher resilience scores at post‐intervention in the intervention group compared to the control group. For another study graphically reporting the results for resilience (Delaney 2016), we could not obtain the quantitative data from the study authors. However, Delaney 2016 (probably 37 participants included) reported no evidence of a difference in resilience between intervention and control groups at post‐test.
Short‐term follow‐up (≤ 3 months)
Seven individually‐randomised studies, including one study with a mixed sample (Victor 2018), assessed the effect of resilience‐training programmes versus control groups on resilience at short‐term follow‐up. We were able to combine the data from four of these studies, including one mixed‐sample study with available subgroup data (Victor 2018), in a meta‐analysis (Mejia‐Downs 2016; Stephens 2012; Victor 2018; Wang 2012). The pooled SMD for resilience was 0.20 (95% CI −0.44 to 0.84; P = 0.53; 4 studies, 209 participants; I2 = 80%; Tau2 = 0.34; P for heterogeneity = 0.002; G2 = 99.7%; 95% prediction interval: −2.66 to 3.07; Analysis 1.2), suggesting little or no evidence of a difference between resilience training and control.
1.2. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 2: Resilience: short‐term follow‐up (≤ 3 months)
The statistical values indicated substantial to considerable heterogeneity for this outcome.
Single‐study results
Three studies also measuring resilience at short‐term follow‐up could not be pooled with the studies above, for the following reasons: we could not obtain data by contacting the authors of two studies available as conference abstracts (Chen 2018a; Kelleher 2018). One of these (Kelleher 2018; sample size not specified) reported higher resilience scores for the resilience intervention compared to the control group at one‐month follow‐up. Samouei 2015 reported statistical values (e.g. means), but the number of participants randomised to and analysed in each group was not specified and not available from the study authors. The investigators found no significant difference between intervention and control groups for resilience at three‐month follow‐up (P = 0.27).
Medium‐term follow‐up (> 3 to ≤ 6 months)
One of three studies comparing a resilience intervention to control at medium‐term follow‐up provided suitable data for quantitative analysis (Erogul 2014). Using the Resilience Scale (RS‐14; range 14 (worst) to 98 (best); Wagnild 1993) in 57 participants, Erogul 2014 reported no statistically significant difference between the intervention group (mean = 82.4; SD = 9.8) compared no intervention (mean = 77.3; SD = 12.5) at six‐month follow‐up (P = 0.12). Similarly, the calculated mean difference (MD) for this outcome showed little or no evidence of a difference between resilience intervention and control at medium‐term follow‐up (MD 5.10, 95% CI −0.72 to 10.92; P = 0.09; Analysis 1.3)
1.3. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 3: Resilience: medium‐term follow‐up (> 3 to ≤ 6 months)
Single‐study results
For one study presenting only graphical results for resilience (Delaney 2016), we could not obtain the numerical data from the study authors. The same applied to one unpublished study (ISRCTN64217625). Delaney 2016 (probably 37 participants included) showed no evidence of a difference between resilience training and control at four‐month follow‐up.
Mental health and well‐being: anxiety
Post‐intervention
Eight studies (including four with mixed samples: Barry 2019; Goldstein 2019; Houston 2017; Recabarren 2019) evaluated the effect of resilience interventions compared to controls on self‐reported anxiety at immediate post‐intervention. Seven studies reported data suitable for quantitative analysis (Barry 2019; Houston 2017; Kötter 2016; Recabarren 2019; Sahranavard 2018; Wang 2012; Warnecke 2011), including three studies with mixed samples for which subgroup data in healthcare students were available (Barry 2019; Houston 2017; Recabarren 2019). The pooled effect estimate for 362 participants suggests evidence for a moderate effect of resilience training on post‐intervention anxiety (SMD −0.45, 95% CI −0.84 to −0.06; P = 0.02; I2 = 66%; Tau2 = 0.17; P for heterogeneity = 0.008; G2 = 99.3%; Analysis 1.4; 95% prediction interval: −2.09 to 1.13; very‐low certainty evidence, see Table 1).
1.4. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 4: Anxiety: post‐intervention
Based on funnel plots and Egger’s test, we found no statistically significant asymmetry for anxiety at post‐intervention (Egger’s test: t = −1.61; df = 5; P = 0.17; see Appendix 15 and Appendix 16).
The statistical indicators of heterogeneity suggest there is substantial (I2 and Chi2) or considerable heterogeneity (G2) in the results for anxiety at post‐test.
Studies with mixed samples
One study with a mixed sample (Goldstein 2019; 45 participants analysed in total sample), measured anxiety at post‐intervention. However, the (subgroup) results for healthcare students were neither reported in the conference abstract nor in the poster, and we could not obtain them from the study authors.
Short‐term follow‐up (≤ 3 months)
At short‐term follow‐up, three studies compared the impact of resilience interventions versus controls on anxiety. We were able to combine the data from two studies with a total of 91 participants in a meta‐analysis (Porter 2008; Wang 2012). The pooled SMD for short‐term, self‐reported anxiety was −0.88 (95% CI −1.32 to −0.45; P < 0.001; I2 = 0%; Tau2 = 0; P for heterogeneity = 0.80; G2 = 0%; 95% prediction interval: incalculable due to only two studies; Analysis 1.5), and revealed evidence of a large difference between groups in favour of resilience training for this outcome (large effect size).
1.5. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 5: Anxiety: short‐term follow‐up (≤ 3 months)
We detected no statistical heterogeneity for anxiety at short‐term follow‐up.
Studies with mixed samples
We were unable to pool the data from one study measuring anxiety at short‐term follow‐up in a mixed sample with the data from the above studies, due to unavailable subgroup data for healthcare students (Goldstein 2019; 45 participants analysed in total sample).
Mental health and well‐being: depression
Post‐intervention
Seven studies (including four mixed studies: Barry 2019; Goldstein 2019; Houston 2017; Recabarren 2019) assessed the effect of resilience interventions versus controls on self‐reported depression (or burnout; see Helmreich 2017 and Appendix 6 in this review) at post‐intervention. For three studies investigating healthcare and non‐healthcare students, we were able to retrieve the relevant subgroup data from the study authors (Barry 2019; Houston 2017; Recabarren 2019). Analysis of six studies (332 participants) providing data suitable for pooling (Barry 2019; Houston 2017; Kötter 2016; Recabarren 2019; Wang 2012; Warnecke 2011) suggested little or no evidence for a difference between resilience training and control group for post‐intervention depression (SMD −0.20, 95% CI −0.52 to 0.11; P = 0.20; I2 = 45%; Tau2 = 0.07; P for heterogeneity = 0.11; G2 = 99.1%; 95% prediction interval: −1.16 to 0.74; Analysis 1.6; very‐low certainty evidence, see Table 1).
1.6. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 6: Depression: post‐intervention
We found no indication of asymmetry for depression immediately post‐intervention (see Appendix 15 and Appendix 16; Egger’ test: t = −0.85; df = 4; P = 0.44).
The results for statistical heterogeneity were mixed, with no important heterogeneity indicated by Chi2 test, moderate heterogeneity indicated by the I2 value, and the G2 value suggesting considerable heterogeneity.
Studies with mixed samples
One study with a mixed sample (Goldstein 2019; 45 participants analysed in total sample) provided only a narrative report of improvements in self‐reported depression for the resilience‐training programme. We were not able to obtain the (subgroup) results for healthcare students from the study authors.
Short‐term follow‐up (≤ 3 months)
Five studies (including two studies with mixed samples: Goldstein 2019; Victor 2018) evaluated the effect of resilience training compared to controls on self‐reported depression at short‐term follow‐up. A meta‐analysis of four studies (including one mixed‐sample study with available subgroup data: Victor 2018) that could be combined (Miu 2016; Porter 2008; Victor 2018; Wang 2012) revealed evidence of a moderate difference between groups, in favour of resilience training for this outcome (SMD −0.65, 95% CI −1.26 to −0.04; P = 0.04; 4 studies, 226 participants; I2 = 76%; Tau2 = 0.28; P for heterogeneity = 0.006; G2 = 99.7%; 95% prediction interval: −2.90 to 1.62; Analysis 1.7; moderate effect size).
1.7. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 7: Depression: short‐term follow‐up (≤ 3 months)
Based on statistical indicators, we found substantial (I2 and Chi2 test) to considerable heterogeneity (I2 and G2) for depression at short‐term follow‐up.
Studies with mixed samples
One study with a mixed sample (Goldstein 2019), measured the effects of a resilience intervention versus control on depression at short‐term follow‐up but could not be pooled with the above studies. Goldstein 2019 (45 participants analysed in total sample) provided only a narrative report of improvements in self‐reported depression for the resilience‐training programme, and we were not able to obtain the (subgroup) results for this time point from the study authors.
Mental health and well‐being: stress or stress perception
Post‐intervention
Eleven studies (three with mixed samples: Barry 2019; Goldstein 2019; Houston 2017) evaluated the effect of resilience interventions compared to control groups on self‐reported stress symptoms or the subjective perception of stress at immediately post‐intervention. We obtained the relevant subgroup data from the study authors for two studies involving both healthcare and non‐healthcare students (Barry 2019; Houston 2017), resulting in seven studies that could be combined (Barry 2019; Erogul 2014; Houston 2017; Kötter 2016; Mathad 2017; Stephens 2012; Warnecke 2011). The pooled effect estimate suggests evidence for a small effect of resilience interventions on stress or stress perception at post‐intervention (SMD −0.28, 95% CI −0.48 to −0.09; P = 0.004; 7 studies, 420 participants; I2 = 0%; Tau2 = 0; P for heterogeneity = 0.58; G2 = 99.1%; 95% prediction interval: −0.74 to 0.15; Analysis 1.8; very‐low certainty evidence, see Table 1).
1.8. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 8: Stress or stress perception: post‐intervention
Based on funnel plots and Egger’s test, we found no statistically significant asymmetry for stress or stress perception at post‐test (see Appendix 15 and Appendix 16; Egger’s test: t = −1.55; df = 5; P = 0.18).
We found mixed results for heterogeneity in stress or stress perception at post‐test, with three values (I2, Tau2, Chi2 test) indicating no heterogeneity, while G2 suggested considerable heterogeneity.
Single‐study results
Three studies also measuring stress or stress perception at post‐intervention could not be pooled with the studies above, for the following reasons. For two studies available only as conference abstracts (Chen 2018a, Kelleher 2018), we could not obtain the data from the authors. Kelleher 2018 (sample size not specified) reported lower stress scores at post‐intervention in the intervention group compared to the control group, but did not indicate statistical values. Delaney 2016 reported the results for perceived stress graphically and we could not retrieve the quantitative data from the study authors; however, Delaney 2016 (probably 37 participants included) reported no evidence of a difference in perceived stress between intervention and control groups at post‐test.
Studies with mixed samples
Another study with a mixed sample measuring perceived stress at post‐intervention could not be pooled with the studies above, due to unavailable subgroup data (Goldstein 2019). For the total sample, including medical and nursing students (45 participants analysed), the study authors reported evidence of a between‐group difference for changes in perceived stress between baseline and post‐intervention (intervention arm: −24.6% average change, P = 0.017, d = −0.58; control arm: 0.8% average change, P > 0.05).
Short‐term follow‐up (≤ 3 months)
At short‐term follow‐up, five studies (including Goldstein 2019 with a mixed sample) compared the impact of resilience training compared to controls for self‐reported stress or stress perception. We combined two studies reporting data suitable for quantitative analysis (Mejia‐Downs 2016; Stephens 2012). Analysis of these studies (113 participants) suggests little or no evidence for a difference between groups in stress or stress perception within three months post‐intervention (SMD 0.13, 95% CI −0.79 to 1.06; P = 0.78; I2 = 83%; Tau2 = 0.37; P for heterogeneity = 0.02; G2 = 0%; 95% prediction interval: incalculable due to only two studies; Analysis 1.9).
1.9. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 9: Stress or stress perception: short‐term follow‐up (≤ 3 months)
The findings for statistical heterogeneity for stress or stress perception at short‐term follow‐up were also mixed, with some values (I2, Chi2) indicating substantial to considerable heterogeneity, while no heterogeneity was suggested by G2.
Single study‐results
Two additional studies measuring stress or stress perception at short‐term follow‐up and available as conference abstracts (Chen 2018a; Kelleher 2018), could not be pooled with the above studies, since we were unable to obtain the relevant data from the study authors. Of these, Kelleher 2018 (sample size not specified) reported lower stress scores for the resilience intervention compared to control group at one‐month follow‐up.
Studies with mixed samples
Comparable with immediate post‐intervention, data from Goldstein 2019, who examined a mixed sample of medical and nursing students along with students from other fields (45 participants analysed in total sample), could not be combined with the other studies. The study authors identified evidence of a between‐group difference in changes in perceived stress between baseline and three‐month follow‐up in the total sample (intervention arm: −22.3% average change, P = 0.002, d = −0.84; control arm: −10.5% average change, P > 0.05).
Medium‐term follow‐up (> 3 to ≤ 6 months)
Two studies reported on stress or stress perception at medium‐term follow‐up (Delaney 2016; Erogul 2014), with quantitative data available for only one study (Erogul 2014). Using the Perceived Stress Scale (PSS; range = 0 (best) to 40 (worst); Cohen 2012) in 57 participants, the study authors reported no evidence for a difference between resilience training (mean = 14.9; SD = 6.6) and no intervention (mean = 18.4; SD = 6.9) at six‐month follow‐up (P = 0.08). The calculated MD indicated evidence for a difference in favour of the resilience intervention at medium‐term follow‐up (MD −3.50, 95% CI −7.00 to 0.00; P = 0.05; Analysis 1.10).
1.10. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 10: Stress or stress perception: medium‐term follow‐up (> 3 to ≤ 6 months)
Single‐study results
One study measuring perceived stress at this time point could not be combined with Erogul 2014, as numerical data were not available (Delaney 2016). At four‐month follow‐up, Delaney 2016 (probably 37 participants included) provide a narrative report of no evidence of a difference between the resilience intervention and control for perceived stress.
Mental health and well‐being: well‐being or quality of life
Post‐intervention
At post‐intervention, five studies (including two with mixed samples: Goldstein 2019; Recabarren 2019) assessed the effect of resilience interventions compared to controls on self‐reported well‐being or quality of life. Including one mixed‐sample study for which we obtained subgroup data for healthcare students from the study authors (Recabarren 2019), four studies (251 participants) provided data suitable for quantitative analysis (Mathad 2017; Recabarren 2019; Smeets 2014; Wang 2012). The analysis revealed little or no evidence of an effect of resilience training (SMD 0.15, 95% CI −0.14 to 0.43; P = 0.31; I2 = 23%; Tau2 = 0.02; P for heterogeneity = 0.27; G2 = 99.9%; 95% prediction interval: −0.90 to 1.20; Analysis 1.11; very‐low certainty evidence, see Table 1).
1.11. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 11: Well‐being or quality of life: post‐intervention
There was no statistical indication of asymmetry for well‐being or quality of life at post‐intervention (see Appendix 15 and Appendix 16; Egger’s test: t = 0.12; df = 2; P = 0.91).
We found mixed results for statistical heterogeneity. While I2 suggested unimportant heterogeneity, G2 indicated considerable heterogeneity.
Studies with mixed samples
One mixed‐sample study (Goldstein 2019), which examined healthcare and non‐healthcare students, could not be included in the meta‐analysis of well‐being or quality of life at post‐test, as relevant subgroup data were not available. Goldstein 2019 (45 participants analysed in total sample) provided a narrative report of improvements in self‐reported life satisfaction for resilience training compared to control.
Short‐term follow‐up (≤ 3 months)
Two studies (including one with a mixed sample: Goldstein 2019), evaluated the effect of resilience training compared to controls on self‐reported well‐being or quality of life at short‐term follow‐up, with quantitative data available for only one study (Wang 2012). Using the General Well‐Being Schedule (GWB; range = 0 (worst) to 110 (best)), the study authors reported higher well‐being scores in the intervention group (mean = 78.00; SD = 8.90) compared to the control group (mean = 69.60; SD = 7.20) at three‐month follow‐up, with a significant time × group interaction (F = 5.25; P < 0.01). Similarly, the calculated MD indicated evidence for a difference in favour of resilience training at this time point (MD 8.40, 95% 4.54 to 12.26; P < 0.001; Analysis 1.12).
1.12. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 12: Well‐being or quality of life: short‐term follow‐up (≤ 3 months)
Studies with mixed samples
One study with a mixed sample also compared the effects of a resilience intervention to control on well‐being or quality of life at short‐term follow‐up (Goldstein 2019), but could not be combined in analysis due to unavailable subgroup data. Except for correlations between life satisfaction and other outcomes, Goldstein 2019 (45 participants analysed in total sample) provided only a narrative report of improvements in self‐reported life satisfaction for resilience training compared to control in a sample of university students (including medical and nursing students).
Adverse events
Only four studies assessed the adverse or undesired effects of resilience training in healthcare students (Galante 2018; Kötter 2016; Victor 2018; Warnecke 2011), with three of them reporting no such effects (Galante 2018; Victor 2018; Warnecke 2011).
Galante 2018 reported no participants with adverse reactions related to self‐harm, suicidality or harm to others. The study authors also determined the number of adverse events by exceeding cut‐off scores for Clinical Outcomes in Routine Evaluation Outcome Measure (CORE‐OM; Evans 2000) risk subscales for psychological distress. In the intervention arm, 20 participants triggered this adverse event reporting protocol compared to 25 participants in the control arm. For the total sample (n = 482), the study authors found a lower score of psychological distress in the intervention arm (mean = 0.88; SD = 0.53) compared to the control group (mean = 1.04; SD = 0.54), with a significant difference in favour of the intervention arm (P = 0.001).
Victor 2018 did not systematically assess adverse events, but no negative effects were mentioned by the participants in verbal feedback. Similarly, according to Warnecke 2011, no adverse effects of the intervention were reported in the study, although the method of assessment is unclear. Kötter 2016 also measured adverse events but did not provide the relevant data in the available publication. Most studies in healthcare students provided no data on adverse effects.
Secondary outcomes
Resilience factors: social support
Post‐intervention
Two studies (including one with a mixed sample: Recabarren 2019) reported on perceived social support at post‐intervention. Recabarren 2019 provided subgroup data for psychology students, which we pooled with data from Stephens 2012. The analysis indicated little or no evidence of a difference in social support at post‐test (SMD 0.21, 95% CI −0.15 to 0.57; P = 0.25; I2 = 0%; Tau2 = 0; P for heterogeneity = 0.83; 2 studies, 121 participants; G2 = 0%; 95% prediction interval: incalculable due to only two studies; Analysis 1.13).
1.13. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 13: Social support: post‐intervention
We found no heterogeneity for social support at short‐term follow‐up, based on statistical indicators.
Short‐term follow‐up (≤ 3 months)
We combined data from two studies (Porter 2008; Stephens 2012), to estimate the effects of a resilience intervention compared to control on social support at short‐term follow‐up. The pooled SMD of social support across the studies was 0.23 (95% CI −0.18 to 0.64; P = 0.28; I2 = 0%; Tau2 = 0; P for heterogeneity = 0.96; 2 studies, 92 participants; G2 = 0%; 95% prediction interval: incalculable due to only two studies; Analysis 1.14), suggesting little or no evidence for an effect of a resilience intervention on social support within three months post‐intervention.
1.14. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 14: Social support: short‐term follow‐up (≤ 3 months)
There was no statistical heterogeneity for social support at short‐term follow‐up.
Single‐study results
One additional study assessed social support at short‐term follow‐up (Mejia‐Downs 2016). We could not pool this study with the others because we could not estimate the SDs from the interquartile ranges due to skewed distribution (see Higgins 2019b). The study authors reported the median social support using the Social Provisions Scale (Cutrona 1987) in 43 participants at two‐week follow‐up: 83.0 (interquartile range = 17.0) in the intervention arm and 85.0 (interquartile range = 13.0) in the control arm (study author‐reported P > 0.05, no further detail available).
Resilience factors: optimism
Post‐intervention
At post‐intervention, two studies reported the effects of resilience interventions compared to controls on self‐reported optimism (Barry 2019; Smeets 2014). We combined the data from these studies in a meta‐analysis, which revealed little or no evidence for an effect of resilience training (SMD 0.29, 95% CI −0.20 to 0.78; P = 0.24; I2 = 0%; Tau2 = 0; P for heterogeneity = 0.54; 2 studies, 66 participants; G2 = 0%; 95% prediction interval: incalculable due to only two studies; Analysis 1.15), compared to control.
1.15. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 15: Optimism: post‐intervention
There was no indication of heterogeneity for optimism at post‐test in any statistical values.
Short‐term follow‐up (≤ 3 months)
Single‐study results
Two studies assessed the effect of resilience‐training programmes versus controls on optimism at short‐term follow‐up (Mejia‐Downs 2016; Samouei 2015), but could not be pooled in meta‐analysis. Because of skewed distribution of data for optimism, we could not compute the SDs on the basis of interquartile ranges for one study (Mejia‐Downs 2016; see Higgins 2019b). The study authors reported the median optimism using the Life Orientation Test‐Revised (Scheier 1994): 25.0 (interquartile range = 8.0) in the intervention arm and 25.0 (interquartile range = 5.0) in the control arm (study author‐reported P > 0.05, no further details available; 43 participants). Samouei 2015 (sample size not specified) reported statistical values (e.g. means), but the number of participants randomised and analysed in each group was not specified and not available from the study authors. The investigators identified no significant difference between intervention and control groups for optimism at three‐month follow‐up (P = 0.23).
Resilience factors: self‐efficacy
Post‐intervention
Five individually‐randomised studies assessed the effect of resilience interventions compared to controls on self‐reported self‐efficacy at immediate post‐intervention (including two studies with mixed samples: Barry 2019; Recabarren 2019). We were able to retrieve the subgroup data for the two studies with mixed samples at post‐test from the study authors, resulting in five studies providing data suitable for quantitative analysis (Barry 2019; Recabarren 2019; Sahranavard 2018; Smeets 2014; Waddell 2015). The analysis (219 participants) revealed evidence for a moderate difference in favour of resilience training for self‐efficacy at post‐test (SMD 0.51, 95% CI 0.14 to 0.88; P = 0.008; I2 = 41%; Tau2 = 0.07; P for heterogeneity = 0.15; 5 studies, 219 participants; G2 = 74.5%; 95% prediction interval: −0.96 to 1.96; Analysis 1.16).
1.16. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 16: Self‐efficacy: post‐intervention
Moderate (I2) to substantial heterogeneity (G2) was indicated by the statistical values for self‐efficacy at post‐test, .
Short‐term follow‐up (≤ 3 months)
At short‐term follow‐up, only Waddell 2005 reported quantitative data on self‐efficacy. After phase two in this study with 20 participants, the study authors reported higher scores for career decision‐making self‐efficacy, assessed using the Career Decision‐Making Self‐Efficacy Scale (CDMSES; Betz 1996; Taylor 1983; range not specified; higher values indicate higher self‐efficacy), for the intervention arm (mean = 112.0) compared to the control arm (mean = 110.4), with no significant between‐group difference (t = 0.19; P = 0.85). The calculated MD also indicated little or no evidence for an effect of training on self‐efficacy (MD 1.60, 95% CI −14.65 to 17.85; P = 0.85; 1 study, 20 participants; Analysis 1.17).
1.17. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 17: Self‐efficacy: short‐term follow‐up (≤ 3 months)
Single‐study results
One study reporting on self‐reported self‐efficacy at short‐term follow‐up could not be pooled with Waddell 2005. Samouei 2015, for which the number of participants randomised and analysed in each group was unclear, reported no significant difference between the intervention and control groups for self‐efficacy at three‐month follow‐up (P = 0.36).
Resilience factors: active coping
Post‐intervention
One mixed‐sample study (Houston 2017) assessed the effect of a resilience intervention compared to control on the resilience factor of active coping at immediate post‐intervention. We received the relevant subgroup data from the investigators. Using the newly‐created 'taking action' subscale, based on original items of the Brief Coping Orientations to Problems Experience scale (Brief COPE; range 1 (worst) to 4 (best) Carver 1997) in 38 participants, the study authors found lower values of active coping (taking action) in the intervention arm (mean = 3.06; SD = 0.50) compared to the control arm (mean = 3.13; SD = 0.65) in healthcare students at post‐test. The calculated MD indicated little or no evidence for an effect of resilience training (MD −0.06, 95% CI −0.45 to 0.32; P = 0.74; 1 study, 38 participants; Analysis 1.18).
1.18. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 18: Active coping: post‐intervention
Short‐term follow‐up (≤ 3 months)
Only one study compared the effects of resilience training to control on active coping at short‐term follow‐up (Porter 2008). Based on data from 22 participants and using the 'planful problem‐solving' scale of the Ways of Coping Questionnaire (WOC; Folkman 1988; range not specified; higher values indicate higher planful problem‐solving), Porter 2008 reported higher values of active coping in the intervention group (mean = 1.78; SD = 0.43) compared to the control group (mean = 1.32; SD = 0.54) at two‐month follow‐up, with a significant time × group interaction (F = 13.20; P < 0.006). The calculated MD suggested evidence for a difference between resilience training and control in favour of training (MD 0.46, 95% CI 0.05 to 0.87; P = 0.03; 1 study, 22 participants; Analysis 1.19).
1.19. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 19: Active coping: short‐term follow‐up (≤ 3 months)
Resilience factors: self‐esteem
Post‐intervention
Only one study in a mixed sample, for which subgroup data were not available, reported on self‐reported self‐esteem at immediate post‐intervention (Goldstein 2019). For the total sample (45 participants analysed), the study authors only provided a narrative report of improvements in self‐esteem, and we therefore could not calculate an MD.
Short‐term follow‐up (≤ 3 months)
At short‐term follow‐up, two studies with mixed samples compared the effect of resilience interventions to controls on self‐esteem (Goldstein 2019; Victor 2018). The study authors of Victor 2018 provided the subgroup data for psychology students. Using the Rosenberg Self‐Esteem Scale (RSES; Ferring 1996; range not specified; higher values indicate higher self‐esteem) in 28 participants, the study authors found slightly higher values for self‐esteem in the intervention arm (mean = 2.42; SD = 0.45) compared to attention control (mean = 2.34; SD = 0.51) at three‐week follow‐up. The calculated MD of 0.08 (95% CI −0.28 to 0.44; P = 0.67; 1 study, 28 participants; Analysis 1.20) indicated little or no evidence for an effect of resilience intervention on this outcome.
1.20. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 20: Self‐esteem: short‐term follow‐up (≤ 3 months)
Studies with mixed samples
In a mixed sample of medical and nursing students, Goldstein 2019 measured self‐esteem at three‐month follow‐up and provided a narrative report of improvements in this outcome (45 participants analysed in total sample). Subgroup data were not available.
Resilience factors: hardiness
Post‐intervention
One study assessed the effects of hardiness training compared to wait‐list control on hardiness at post‐intervention (Sahranavard 2018). The Ahvaz Hardiness Inventory (AHI; Kiamarthi 1998) was used to measure hardiness in 30 participants (15 in each group). However, considering the possible range of scores for this outcome measure (0 (worst) to 81 (best); i.e. range of 0 to 1215 for the sum scores in each group), the reported values for hardiness at post‐test did not seem plausible (intervention arm: mean = 175.80 (SD = 6.00); control arm: mean = 167.80 (SD = 13.06)). We therefore decided against calculating the MD for this study.
Resilience factors: positive emotions
Post‐intervention
Five studies (including Geschwind 2015, who used a mixed sample) assessed the effect of resilience interventions compared to controls on self‐reported positive emotions at immediate post‐intervention. Two studies (Peng 2014; Smeets 2014) provided data suitable for quantitative analysis (112 participants). The pooled effect estimate revealed a moderate effect on positive emotions at post‐test in favour of resilience training (SMD 0.51, 95% CI 0.01 to 1.01; P = 0.05; I2 = 43%; Tau2 = 0.06; P for heterogeneity = 0.19; 2 studies, 112 participants; G2 = 0%; 95% prediction interval incalculable due to only two studies; Analysis 1.21).
1.21. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 21: Positive emotions: post‐intervention
There were mixed findings for statistical heterogeneity for positive emotions at post‐test. While I2 suggested moderate heterogeneity, there was no indication of heterogeneity using G2.
Single‐study results
Two other studies also measured the effects of resilience interventions compared to controls on positive emotions at post‐intervention (Akbari 2017; Sahranavard 2018), but could not be pooled with the aforementioned studies. Although Akbari 2017 (number of participants analysed not specified) demonstrated an increasing effect of resilience training compared to no intervention on happiness (Oxford Happiness Questionnaire; Alipour 1993; Hills 2002; higher values indicate more happiness) at post‐test (F = 22.412, P < 0.001), the report indicated lower values of happiness in the intervention arm (mean = 27.82; SD = 2.25) than in the control arm (mean = 42.11; SD = 2.25). We contacted the study authors but were unable to resolve this uncertainty. Sahranavard 2018 only presented the combined results for both positive and negative affect (assessed with the Positive and Negative Affect Schedule; PANAS; Watson 1988) and reported a significant effect of condition on this outcome (F = 4.96, P = 0.035) in a covariance analysis (30 participants). We could not obtain the separate data for positive affect after contacting the study authors.
Studies with mixed samples
In Geschwind 2015, the subgroup data for psychology students were not available. For the total sample of 50 participants (i.e. psychology students and healthy volunteers), the study authors reported a significant interaction for time x condition (F = 6.632, P = 0.002), with significantly higher positive affect in the intervention arm compared to the control arm after affect induction (t = 3.369, P = 0.002).
Short‐term follow‐up (≤ 3 months)
At short‐term follow‐up, one study compared the effects of a resilience intervention to wait‐list control on self‐reported positive emotions (Mejia‐Downs 2016). Using the positive affect subscale of the Modified Differential Emotion Scale (mDES; Fredrickson 2003; range not specified; higher values indicate more positive affect) in 43 participants, the study authors reported a significant time × group interaction for positive emotions (F = 5.73; P = 0.02), with higher values in the intervention arm (mean = 3.20; SD = 0.47) compared to the control arm (mean = 3.01; SD = 0.65) at two‐week follow‐up. The calculated MD suggested little or no evidence for an effect of resilience training at short‐term follow‐up (MD 0.19, 95% CI −0.15 to 0.53; P = 0.27; 1 study, 43 participants; Analysis 1.22).
1.22. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 22: Positive emotions: short‐term follow‐up (≤ 3 months)
Studies with mixed samples
Geschwind 2015 also assessed the effects of a resilience intervention compared to an attention control group at short‐term follow‐up. We could not pool the data from this study with the above study, as we could not obtain the subgroup data for psychology students from the study authors. For the total sample (50 participants), the effect of positive affect induction compared to control on positive affect was shown to be maintained at 20‐minute follow‐up (t = 2.053, P = 0.047).
Sensitivity analyses
We performed five sensitivity analyses using fixed‐effect pair‐wise meta‐analysis for the primary outcomes at post‐intervention. For each outcome, the results were consistent with the findings from the random‐effects meta‐analyses.
Resilience
Post‐intervention
We found evidence for a moderate difference in favour of resilience training (SMD 0.52, 95% CI 0.36 to 0.69; P < 0.001; 9 studies, 561 participants; Analysis 1.23).
1.23. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 23: Resilience: post‐intervention, sensitivity analysis (fixed‐effect analysis)
Anxiety
Post‐intervention
We found evidence for a moderate difference in favour of resilience training (SMD −0.35, 95% CI −0.57 to −0.14; P = 0.001; 7 studies, 362 participants; Analysis 1.24).
1.24. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 24: Anxiety: post‐intervention, sensitivity analysis (fixed‐effect analysis)
Depression
Post‐intervention
We found little or no evidence for an effect of resilience training (SMD −0.18, 95% CI −0.40 to 0.04; P = 0.12; 6 studies, 332 participants; Analysis 1.25).
1.25. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 25: Depression: post‐intervention, sensitivity analysis (fixed‐effect analysis)
Stress or stress perception
Post‐intervention
We found evidence for a small difference in favour of resilience training (SMD −0.28, 95% CI −0.48 to −0.09; P = 0.004; 7 studies, 420 participants; Analysis 1.26).
1.26. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 26: Stress or stress perception: post‐intervention, sensitivity analysis (fixed‐effect analysis)
Well‐being or quality of life
Post‐intervention
We found little or no evidence for an effect of resilience training (SMD 0.14 95% CI −0.10 to 0.39; P = 0.25; 4 studies, 251 participants; Analysis 1.27).
1.27. Analysis.

Comparison 1: Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes, Outcome 27: Well‐being or quality of life: post‐intervention, sensitivity analysis (fixed‐effect analysis)
Discussion
Summary of main results
We identified 30 RCTs that fulfilled the inclusion criteria for this review, eight of which were conducted in mixed samples.
There is very‐low certainty evidence (meaning that the true effect may differ markedly from the estimated effect) that resilience interventions might be more effective than control for improving resilience, self‐reported symptoms of anxiety, and stress or stress perception at post‐test. Effect sizes ranged from small to moderate. We found little or no evidence for an effect of training on depressive symptoms and well‐being or quality of life at post‐intervention. At short‐term follow‐up (three months or less post‐intervention), the effect size for the reduction in anxiety symptoms increased from moderate to large. We also found some evidence for a moderate effect in favour of resilience training on depressive symptoms, and a single study provided evidence of an increase in well‐being. The moderate or small effects for resilience and stress or stress perception found at post‐test, respectively, were no longer evident at short‐term follow‐up. At medium‐term follow‐up (more than three months to six months or less), we no longer found evidence for a difference between a resilience intervention and control for resilience, while a single study still provided evidence for a decrease in stress symptoms. Anxiety, depression, and well‐being or quality of life were not measured at medium‐term follow‐up by any study. Long‐term follow‐up assessments (more than six months post‐intervention) were not available for any primary outcome.
For secondary outcomes at post‐test and short‐term follow‐up, we found some evidence for moderate effects in favour of resilience training for self‐efficacy and positive emotions at post‐intervention, that were not maintained in the short‐term follow‐up, based on the evidence from single studies. While there was no evidence for an effect of training on active coping at post‐test, we found evidence for an effect in favour of resilience training at short‐term follow‐up. Neither at post‐intervention nor within three months post‐intervention was there evidence for a difference between training and control for social support, optimism (only at post‐intervention), or self‐esteem (only at short‐term follow‐up). Hardiness was not measured at short‐term follow‐up. None of the secondary outcomes were assessed at medium‐term or at long‐term follow‐up.
The planned subgroup analyses to test for possible effect modifiers were not possible, due to the limited number of studies. The same applied to the planned sensitivity analyses to examine the robustness of the conclusions of this review, the exception being the sensitivity analyses using a fixed‐effect model for the primary outcomes at post‐test. Compared with the main analyses, the calculation of fixed‐effect instead of random‐effects pairwise meta‐analyses showed no changes in the evidence found.
Overall, we found very‐low certainty evidence in this review, meaning that we can draw no clear conclusions.
Overall completeness and applicability of evidence
The review highlights some issues about the completeness and applicability of the evidence for the effects of resilience interventions in healthcare students (for details, see Appendix 17).
Participants
Since stress‐related mental disorders are more prevalent in women (Kuehner 2017; Li 2017; WHO 2019) and since women report lower resilience (e.g. Kunzler 2018), the high proportion of women among the study participants may be explained by a higher interest among women to participate in resilience interventions. The applicability of the findings of this review to men may be limited, since gender differences in the prevalence of stress‐related mental disorders may reflect differences in biological vulnerability, social roles, or stress reactivity (Nazroo 1998; Verma 2011; WHO 2019), thereby possibly causing a different effect of resilience training in men and women.
The included studies mainly considered young individuals, but this was to be expected, given that the population of interest in this review is healthcare students.
Students in allied health professions were less represented, restricting the applicability of our findings to these fields of study.
The clinical relevance of mental symptoms at baseline, i.e. whether symptom load justified a diagnosis of a mental disorder, is unclear for most studies. However, to get a clear picture of the participants' baseline mental health could be important, as the large effect sizes in some studies (e.g. Wang 2012) might be explained in part by the inclusion of participants with a pre‐existing burden of mental symptoms or even clinical diagnoses.
The evidence was concentrated in North America, Europe and Asia (including the Near East), with only two studies from Australia. The applicability of the findings to other locations and ethnicities (e.g. South America, Africa, Oceania) therefore remains unclear. Twenty‐four of the 30 included studies were conducted in high‐income countries (e.g. USA) and five in an upper‐middle income country (e.g. China), with only one study performed in a lower‐ to middle‐income country. We therefore also advise some caution about the cross‐cultural applicability of the evidence.
In summary, the findings may be most applicable to young adult, female healthcare students, living in high‐income countries.
Interventions
Although the benefits of online‐ and mobile‐based interventions (e.g. 24/7 availability) have been recently discussed (Cuijpers 2017; Heber 2017; Heron 2010), we identified only four studies delivered in this format. Furthermore, most of the interventions were of high or low intensity with treatment durations varying considerably. Theoretical approaches were relatively balanced between mindfulness‐based training, unspecified interventions and combinations. Overall, the findings of this review are mostly applicable to group interventions of high intensity, delivered face‐to‐face, and using a mindfulness‐based theoretical approach.
Comparators
The primary use of no intervention and wait‐list controls, in particular, in the evidence found here is problematic, since these control groups are demonstrated to yield inflated effect sizes compared to active comparators in psychotherapy research (Mohr 2014). The evidence does not allow us to answer this question, because we were not able to conduct the relevant subgroup analysis (see Table 2).
Outcomes
There were a large number of different measures for resilience in the studies (see Table 3). We were not able to investigate the potential effect of the underlying concept of resilience in these scales (see Table 2).
A large variety of assessments was also used for the primary outcomes of mental health and well‐being (e.g. burnout and depression scales for depression; see Helmreich 2017). This diversity of measures has to be considered as a potential source of heterogeneity in our meta‐analyses, and might have an impact on the interpretation of results.
Although resilience factors, such as social support, are discussed as well‐evidenced resilience factors (see Helmreich 2017), relatively few of the included studies assessed these outcomes at the different periods of follow‐up.
Adverse or undesired effects were not specified in most included studies, with three studies reporting no adverse or undesired effects. For psychotherapy, however, possible adverse outcomes have been discussed (Berk 2009; Moritz 2019). As resilience interventions often include confronting participants with individual problems, some of these training programmes might also have the potential to harm certain participants.
Lastly, very few studies had medium‐term follow‐up assessments and no study performed long‐term follow‐up, which might be explained by the students' restricted time in universities and schools, and general difficulties in establishing long‐term outcomes. Our ability to examine whether any benefits of resilience interventions are sustained in the medium‐ and long‐term was therefore also limited.
Quality of the evidence
Using the GRADE approach (Schünemann 2013; Schünemann 2019a), we rated the overall certainty of evidence at post‐intervention for all primary outcomes as very low for several reasons. First, important methodological limitations reduced the certainty of the evidence offered by most included studies. There was unclear and high risk of bias for several domains across the studies; notably, there was a high risk of bias in blinding of participants and personnel and loss to follow‐up, and unclear risk of bias for methods of sequence generation, allocation concealment and blinding of outcome assessment. Selective outcome reporting was also occasionally an issue. Second, three outcomes had moderate (I2 > 30%; depression) or substantial (I2 > 50%; resilience, anxiety) levels of unexplained heterogeneity and only partially overlapping CIs leading to inconsistency. Third, for all (primary) outcomes at post‐intervention, the evidence was indirect, as studies were limited to certain participants (e.g. certain fields of health professional study), particular versions of resilience intervention (e.g. group setting, high training intensity) and certain comparators (e.g. no intervention, waiting list). Finally, due to the small number of participants included in the meta‐analyses for anxiety, depression and well‐being or quality of life (fewer than 400 participants), inconsistent messages about the 95% CI for the intervention effect (depression, well‐being or quality of life), and the 95% CI encompassing both a very small treatment effect and crossing the threshold for appreciable benefit of the intervention (resilience, anxiety), imprecision was a problem for four outcomes at post‐intervention. However, in the case of post‐intervention resilience and anxiety, we did not downgrade for imprecision. Rather, we downgraded only for inconsistency, as the substantial heterogeneity (I2 = 75% or 66%, respectively) for these outcomes might also have affected the CIs (i.e. precision) and we did not wish to double‐downgrade for the same problem.
We did not downgrade for publication bias for any of the primary outcomes at post‐intervention. Despite the small number of studies per meta‐analysis (fewer than 10 studies; see Assessment of reporting biases), inspection of funnel plots (see Appendix 16) and Egger's test revealed no statistical or visual evidence of asymmetry (see also Effects of interventions and Appendix 15). The funnel plots were symmetrical in shape and, where available, the results from grey literature did not differ from other published studies for the (non‐)evidence or the direction of effect. Due to the scarcity of larger studies across the primary outcomes at post‐test, a small‐study effect was difficult to assess and cannot not be ruled out completely. Nevertheless, an overestimation of effects in smaller studies seemed unlikely, since the meta‐analyses mostly included small studies with significant and non‐significant results. Although the evidence was largely based on small studies, there was almost no indication of potential conflicts of interest of relevance for the post‐test meta‐analyses, except for one study (Kötter 2016) included in the meta‐analyses for anxiety, depression and stress or stress perception (see Appendix 15).
Regarding adverse events, several GRADE domains (e.g. precision, inconsistency, publication bias) could not be assessed due to the small number of studies documenting any adverse effects of study participation (e.g. by verbal feedback from participants; Galante 2018; Victor 2018; Warnecke 2011; for Kötter 2016: adverse events measured, but not reported). Based on the narrative reporting in these studies, we downgraded the certainty of the evidence for this outcome for study limitations and indirectness.
Overall, the GRADE certainty rating was very low for all primary outcomes at post‐intervention, which means that there is a high degree of uncertainty about the estimates of effect observed. Future research in this area is very likely to substantially impact the effect estimates of resilience interventions.
Search methods
Appendix 18 includes further information on how potential biases in the search methods were prevented in this review.
Except for five completed, but unpublished studies (Chen 2018a; Goldstein 2019; ISRCTN64217625; Kelleher 2018; Mejia‐Downs 2016), we were able to retrieve the full texts for all included studies. In accordance with the CDPLP Editorial Team, we considered alternative sources (e.g. trial register entry) for these five studies. In 22 cases, we did not receive any reply from the study authors (i.e. eligibility criteria not verifiable due to unavailable full text or alternative information), or the responses were inadequate and did not provide sufficient information to enable us to reach a decision about the eligibility of the studies (see Characteristics of studies awaiting classification). We attempted to conduct a comprehensive search; however, the fact that 16 studies have not yet been incorporated, and will only be added in the update of this review could be considered a potential source bias.
Correspondence with the authors about data analysis was required for 25 included studies. For six studies for which we aimed to double‐check the available information (e.g. amount of missing data; per‐protocol analysis) by contacting the authors, we decided to rely on the reports and to include the studies in the meta‐analyses despite the missing response (Anderson 2017; Miu 2016; Sahranavard 2018; Smeets 2014; Waddell 2005; Waddell 2015). For three studies (Chen 2018a; ISRCTN64217625; Kelleher 2018), we received information that no data could be provided as the studies were completed and in the process of analysis or publication. For one study (Venieris 2017) the authors responded, but relevant subgroup data could not be retrieved, since the data had been collected several years ago and were saved on another computer. The primary investigators of three studies responded to our first enquiry, but did not react to a second enquiry (Geschwind 2015; Goldstein 2019) or were not able to provide the relevant subgroup data at the time of data analysis (Galante 2018).
Post hoc changes
We made a post hoc change to the eligibility criteria for the Types of interventions (see Differences between protocol and review) by subsequently limiting the study selection to interventions that explicitly stated the aim of fostering resilience, hardiness or post‐traumatic growth. Although the change raises the possibility of bias in the review process, we felt it was necessary to guarantee highly‐objective eligibility criteria and transparency. We do not believe that this divergence from the protocol (Helmreich 2017) is a serious bias. Due to the focus on interventions with the mention of at least one of the three terms, general health‐promoting interventions (e.g. well‐being therapy, chronic disease self‐management, self‐management training after negative life events) not meeting this criterion were excluded from this review. However, other psychological interventions in healthcare students, that are eventually more economic than the theoretical approaches found in this review, might also foster mental health despite stressors (i.e. resilience), although not being labelled as 'resilience training'.
We also made a post hoc change to the eligibility criteria for Types of participants (see Differences between protocol and review) by limiting the included studies to healthcare students. Although the change raises the possibility of bias, we felt it was necessary because the restriction to healthcare students guarantees a systematic review with sufficiently homogeneous comparisons.
Further potential biases
Even within each type of theoretical foundation, there was partial clinical heterogeneity, in terms of intervention setting, delivery or intensity. However, as there is still no consensus or 'gold standard' about how to design resilience‐training programmes leading to a variety (see previous reviews, e.g. Leppin 2014), we decided to pool the data. We took this decision as this review had a larger evidence base than previous meta‐analyses, but we were not able to perform the planned subgroup analyses to investigate potential explanations for heterogeneity.
Beyond the five main results for the primary outcomes at post‐test, the large number of pooled analyses in this review might have increased the probability of a type I error, potentially leading to false‐positive results.
Another important limitation of this review is the unknown stressor or risk exposure in the included studies (see Implications for research). Although the health professional education might be associated with substantial stressors among participants of the included studies, a proven risk or stressor exposure was not applied as an inclusion criterion for this review (see Types of participants), only potential stressor exposure. Based on the definition of resilience (Windle 2011a), the effects of resilience interventions on resilience cannot be determined without ensuring a significant risk. The missing assessment of stressor exposure is a general problem in resilience intervention research (Chmitorz 2018). For healthcare students in particular, the stressor exposure might also vary at different time points of training (e.g. more stressors in year one versus year four or vice versa, due to expectations or fears about the transition to professional life). The students' limited time in institutions (e.g. university) should also be considered. As the number of potential risks or stressors (i.e. stressor load) is naturally restricted to the years of training, healthcare students might be exposed to fewer stressors than groups experiencing the same stressors over a longer period of time (e.g. healthcare professionals).
Agreements and disagreements with other studies or reviews
Studies or reviews in different clinical and non‐clinical adult populations
As mentioned under Why it is important to do this review, the efficacy of resilience interventions for adult populations has been previously examined in 13 systematic reviews and six meta‐analyses, including a recent Cochrane Review by our group on resilience interventions in healthcare professionals (Kunzler 2020). Overall, the reviews largely found positive effects of resilience training on different outcomes (e.g. resilience, mental health, physical health, performance); however, many review authors have pointed out the need for further research, due to elements such as the low methodological quality of the primary studies. Many of the reviews also considered study designs other than RCTs (e.g. Bauer 2018; Massey 2019), and focused on certain target groups (e.g. Milne 2016; Pallavicini 2016; Pesantes 2015; Petriwskyj 2016), or certain forms of intervention (e.g. Deady 2017). The number of RCTs on resilience training specifically was therefore rather limited, making comparisons with our review difficult.
Some of the previous reviews used broader eligibility criteria (e.g. clinical and non‐clinical individuals, employees) and identified more RCTs (Joyce 2018; Macedo 2014; Leppin 2014; Robertson 2015; Vanhove 2016), compared to other reviews. Our review is focused on healthcare students, which is different from the mixed target groups in the previous reviews. Despite varying inclusion criteria, the findings of our review mostly agree with the previous research, although our review is based on evidence from a larger group of studies. For example, Macedo 2014 (seven RCTs in non‐clinical adult samples), whilst not pooling any data, identified some degree of effectiveness of resilience‐training programmes. Similarly, Robertson 2015 (eight RCTs in employees) found indications of benefits for personal resilience, mental health, well‐being and work performance in employees. With the exception of job performance, which was not examined here, these findings were confirmed by our review. With respect to the positive effects for resilience at post‐test, our review is consistent with and even showed evidence of a larger (moderate) effect than Joyce 2018 (17 RCTs in adults), who found a small positive effect of training on resilience at immediate post‐intervention. However, compared with Leppin 2014 (25 RCTs in diverse adults populations and persons with chronic diseases), who also found a moderate effect in favour of resilience training for up to three months after the end of training, our review suggested little or no evidence for a maintained positive effect for resilience at short‐term follow‐up. In contrast to Vanhove 2016, who identified positive effects on well‐being and psychological deficits (e.g. depressive symptoms) within one month post‐intervention, we found little or no evidence for an effect on these outcomes at immediately post‐test. However, the maintained positive effects for anxiety and the delayed effect on depression between post‐test and short‐term follow‐up in our review are comparable to Vanhove 2016, who, as well as the positive effects at one‐month follow‐up or less, also observed sustained effects of training for the prevention of psychological deficits at more than one month after training. In general, our findings on mental health differ from Leppin 2014, who found no evidence for an effect of training for mental health outcomes (depression, quality of life) aside from resilience. Due to the limited number of studies in our review (fewer than 10 studies per meta‐analysis; Deeks 2019), we were not able to replicate the findings of previous reviews for effect modifiers such as training setting (Vanhove 2016), theoretical foundation (Joyce 2018), or study comparator (Leppin 2014).
Compared to our review on healthcare professionals (Kunzler 2020), this review delivers similar findings for healthcare students, although we identified a smaller number of studies for individuals in health professional education (30 RCTs) compared with studies in healthcare professionals who have completed training (44 RCTs). The moderate positive effect on resilience immediately after training, which we identified in this review, is consistent with Kunzler 2020. However, while the positive effect on resilience was maintained in the short term (three months or less after training) in healthcare professionals, we could not replicate this finding in healthcare students. The same applies to symptoms of stress or perceived stress: while we found evidence for a small, positive effect of training on post‐intervention stress in healthcare students, with no evidence of an effect at short‐term follow‐up and only a single study measuring this outcome at medium‐term follow‐up, there was a moderate, positive effect on post‐test stress in healthcare professionals, which was also sustained over time. Similar to our findings in healthcare professionals (i.e. increase from a small to a moderate positive effect size for depression between post‐test and short‐term follow‐up), we observed a similar delayed effect on depression in healthcare students, with evidence for a moderate, positive effect on depressive symptoms emerging only in the short‐term. In contrast with our review on healthcare professionals (no evidence of any effect), we found evidence for a positive effect of resilience interventions on healthcare students' well‐being or quality of life at short‐term follow‐up (single study), as well as on symptoms of anxiety at post‐test, which for anxiety were maintained at short‐term follow‐up. Comparable with our findings in Kunzler 2020, resilience factors (i.e. secondary outcomes in both reviews) were hardly assessed in healthcare students. Finally, several methodological weaknesses (e.g. paucity of medium‐ and long‐term follow‐ups), that we identified for RCTs in healthcare staff were also found in this review or were even more evident here (see Implications for research). We therefore judged the certainty of the evidence to be very uncertain for both reviews.
Studies or reviews in healthcare students
Five systematic reviews (Gilmartin 2017; McGowan 2016; Pezaro 2017; Rogers 2016; Sanderson 2017) and one meta‐analysis (Lo 2018) have synthesised the efficacy of resilience‐training programmes for healthcare students to date, although not all of them have focused solely on interventions (see Why it is important to do this review). Comparable with our review, two of these previous publications examined healthcare students in general (Lo 2018; Sanderson 2017), but most only targeted a subgroup of healthcare students (e.g. nursing and midwifery students; McGowan 2016) or a combination of qualified staff and (certain) students (Gilmartin 2017; Rogers 2016; Pezaro 2017). Similar to the problems for the reviews described above, most previous reviews in healthcare students (Lo 2018) also considered study designs other than RCTs. The number of RCTs on resilience training is therefore rather limited (i.e. 0 to 24 RCTs among 5 to 36 included studies in the six reviews), in contrast with our review, which identified 30 RCTs across various groups of healthcare students. Since the review questions of some of the six reviews did not focus solely on the construct of resilience or on intervention studies, the primary studies included here did not always explicitly mention the intention of fostering resilience. Instead, broader mental health interventions (e.g. Gilmartin 2017) were also considered, which renders comparisons with our review difficult.
Our review is most comparable with McGowan 2016 and Rogers 2016, who included educational interventions to promote resilience (McGowan 2016), or considered (qualitative) research covering educational interventions and resilience (Rogers 2016), with Rogers 2016 considering different groups of healthcare students in addition to healthcare professionals. McGowan 2016 identified no RCTs, and Rogers 2016 found only one RCT in healthcare students (Peng 2014), which we also included in our review. Comparable with Rogers 2016, we also identified Steinhardt 2008, but excluded it due to an 'ineligible population' based on information obtained from the study authors that they did not target healthcare students. Furthermore, we also identified several non‐RCTs found in McGowan 2016 (e.g. Jameson 2014; Judkins 2005b) during the study identification process for our review.
In the only previous meta‐analysis, Lo 2018, who included 24 RCTs (19 in meta‐analysis) on any group intervention to enhance or maintain mental health in healthcare students, identified only two studies that explicitly stated the intention of fostering resilience (Erogul 2014; Porter 2008), both of which are included in this review. The meta‐analyses on mental health (depression, anxiety), burnout and stress symptoms, which the study authors calculated for different theoretical foundations (e.g. mindfulness‐based training) and which resulted in some positive effect sizes (e.g. stress reduction by mindfulness interventions compared to control), cannot readily be contrasted with the findings of this review.
Authors' conclusions
Implications for practice.
There is very uncertain evidence that resilience interventions are effective in improving resilience or self‐reported symptoms of anxiety, and stress or stress perception at post‐test (small and moderate effect sizes).
The generalisability and applicability of the evidence is limited by the heterogeneous design and content of interventions (with a predominance of high‐intensity, face‐to‐face interventions delivered in a group setting), the scarcity of studies with short‐, medium‐ and long‐term follow‐up, the divergent efficacy measures used, for example, to measure resilience, and the limited geographical location (i.e. high‐income countries). We rated the certainty of the evidence in this review as being very low across all primary outcomes at post‐test. We therefore cannot draw strong conclusions about the effects of resilience interventions, as the true effect may be markedly different from the estimated effect.
We know little about the longer‐term effects of resilience training on most outcomes, because few studies included follow‐up assessments. Booster sessions were not conducted in any of the included studies.
The limited evidence that resilience training improves well‐being or quality of life (post‐test) and several resilience factors might indicate the need to adapt the current intervention techniques used and the protective factors trained.
The results of our review provide very uncertain evidence about whether resilience‐training programmes may be helpful in stabilising and improving the mental health of healthcare students as a group of students with high stressor exposure.
Implications for research.
The findings of this review point to the need for further research of high methodological quality in order to determine the efficacy of resilience interventions in healthcare students.
A consensus on the definition of resilience and adequate outcome measures to be used consistently across the field would be important for future research. Following the growing consensus on resilience as a dynamic outcome (Bonanno 2015; Kalisch 2017), intervention studies might be guided by this definition and examine resilience as a primary outcome (Chmitorz 2018). Because none of the studies in healthcare students measured the participants' stressor exposure, it remains unclear whether healthcare students really benefit from resilience training by being better able to cope with stressors. Future studies should therefore measure resilience as a person’s mental health in relation to individual stressor load. Only if the risk or stressor exposure is assessed (which is different from the subjective perception of stress), may researchers gain knowledge about the changes in resilience by an intervention. In addition to the number of stressors, certain covariates should be assessed, such as the type of stressors (e.g. micro‐ versus macro stressors, psychological versus physiological stressors, acute versus chronic stressors) or the perceived severity of occurred stressors.
Study designs: there is a need for improved comparators, at least treatment as usual (TAU) or ideally active and attention control (Chmitorz 2018), to allow fair comparisons between resilience interventions and control. As already suggested (Chmitorz 2018), resilience‐training programmes could be implemented during or after the presence of a stressor. However, future studies should also use designs in which resilience training is provided prior to circumscribed stress situations (e.g. examinations; rotation of a healthcare student to a demanding hospital ward, such as emergency), in order to determine the resilience effects of the intervention, and to see whether the training does indeed improve resilience to the specific stress situation (Chmitorz 2018; Kalisch 2015).
In general, pre‐ and post‐assessments of the outcome indicators (e.g. for resilience) should be conducted, with future studies also filling the gap of longer follow‐up periods and measuring the stressor exposure before, throughout and after the intervention. Also, it could be interesting to investigate whether or not booster sessions might help maintain the effects of training over time.
The use of adequate sample sizes based on a priori analyses seems to be an urgent need in this field, to ensure sufficient statistical power.
Intervention studies might also benefit from more comprehensive baseline diagnostics of mental health (e.g. clinical interview) and a better reporting of eligibility criteria for pre‐existing mental symptoms. This would allow more precise conclusions about whether resilience training reduces (clinically relevant) mental symptoms. Furthermore, the implications of the resilience concept would require a baseline mental health assessment. In order to investigate the effects of interventions on resilience (i.e. mental health in relation to stressor load) and to determine a specific 'resilience pattern or trajectory' under consideration, the status of psychological functioning as an outcome of interest at baseline is important. For example, when researchers are interested in testing the effects of an intervention in stressor‐exposed individuals on the resilience trajectory of sustained mental health (see also Description of the condition), they would have to prove a positive mental health level at baseline and at post‐intervention. On the other hand, researchers considering a sample with elevated levels of mental symptoms at pre‐test (Harrer 2019) would be able to investigate the resilience trajectory of recovery or even of post‐traumatic growth (i.e. increased level of functioning compared to outset prior to stressors).
Beyond RCTs, dismantling designs could be helpful in clarifying the efficacy of single components of resilience training.
In general, there is a need for a better reporting of intervention studies using international guidelines, such as the CONSORT statement (Schulz 2010). To guarantee higher transparency of study conduct and reporting, primary investigators should register trials or publish study protocols according to the SPIRIT guidelines (Standard Protocol Items: Recommendations for Interventional Trials; Chan 2013a; Chan 2013b).
Finally, future studies in this field should focus more on men. Research efforts should be intensified in low‐ and middle‐income countries in order to reach more robust conclusions about the effectiveness of training across various settings. More studies would be desirable with particular formats of intervention (e.g. online‐ and mobile‐based). Based on the varying relevance of resilience factors in different age groups (see long‐time cohort studies; Werner 1992; Werner 2001) and given that this review was limited to young adults (students), the participants' age and the protective factors trained might also have affected the findings. Future studies should therefore focus their efforts on the development and evaluation of resilience interventions that foster specific and validated age‐relevant factors in specific target groups.
In sum, there is still an urgent need for additional evidence to answer the question of which resilience interventions are really effective in healthcare students, and how they should be implemented. A larger number of RCTs in the field might then allow potential effect modifiers to be explored.
History
Review first published: Issue 7, 2020
Acknowledgements
The authors wish to acknowledge the support of the Cochrane Developmental, Psychosocial and Learning Problems (DPLP) Editorial Team, based at Queen's University Belfast and the University of Bristol, UK. We would like to thank especially Professor Geraldine Macdonald, Co‐ordinating Editor; Dr Joanne Duffield, Managing Editor; Dr Sarah Davies, Deputy Managing Editor; Gemma O'Loughlin, Former Assistant Managing Editor; and Margaret Anderson, Information Specialist, for their advice and assistance throughout the editorial process. Furthermore, we would like to acknowledge the support and recommendations of Dr Nuala Livingstone, Editor with DPLP and the Cochrane Editorial and Methods Department; members of the Cochrane Editorial Unit; and the following peer reviewers for their time and comments: Professor Kate M Bennett, Department of Psychology, University of Liverpool; Dr Srini Chary, University of Calgary; Dr Martha Höfler, Mercator Institute, University of Cologne, and ResilienzExpertise, Bonn; and Dr Dimitris Mavridis, University of Ioannina.
We highly appreciate the contributions of Johanna Greesz, Svenja Kamp, Svenja Frenzel, Anastasia Doré, Paul Ludolph, Bruno Richter, Sophie Walter, Manpreet Blessin, Alice Zobel, Charlotte Böhme and Marlene Stoll to the completion of this review. We thank Steffen Reinecke and Donya A Gilan for their kind assistance with the translations of some of the included studies.
We thank the Ministry of Science (MWWK) of the State Rhineland‐Palatinate, Germany, for providing the funding for this review.
Appendices
Appendix 1. Glossary of relevant terms in this review
Acceptance and commitment therapy: form of psychotherapy (third wave of cognitive behaviour therapy) that uses acceptance and mindfulness strategies (e.g. being in contact with present moment) and commitment and behaviour‐change skills (e.g. values, committed action) in order to increase psychological flexibility
Active control (in this review): alternative treatment (no standard care; for example, treatment developed specifically for the treatment study) that does not control for the amount of time and attention in the intervention group, and is not attention control in a narrow sense
Adverse event: an adverse outcome that occurs during or after the use of an intervention but is not necessarily caused by it
Allied healthcare professionals: healthcare staff working in allied health professions distinct from medical care (e.g. psychologists, social workers, counsellors, physical therapists, occupational therapists, speech therapists, medical assistants, medical technicians)
Allied healthcare students: students in training for allied health professions, as distinct from direct medical care (e.g. psychology, physical therapy, social work, counselling, occupational therapy, speech therapy, medical assistant or medical technician students)
Arm(e.g. intervention arm, control arm): group of participants allocated to the intervention or control group
Attention and interpretation therapy: mindfulness‐based approach to reduce stress and increase resilience that teaches to delay judgements and to focus the attention on the novelty of the world as well as higher‐order principles (e.g. acceptance, gratitude)
Attention control: alternative treatment in the control group that mimics the amount of time and attention received (e.g. by the trainer) in the intervention group
Attrition: loss of participants during the course of a study (also referred to as loss to follow‐up)
Attrition bias: systematic differences between comparison groups in withdrawals or exclusions of participants from the results of a study (e.g. number or reasons, or both)
Available‐case analysis: analysis in which data are analysed for every participant for whom the outcome was obtained; subset may be defined after considering exposure to treatment, availability of measurements
Baseline characteristics: values of demographic, clinical and other variables collected for each participant at the beginning of a study, before the intervention is administered
Baseline comparability: data on the potential (statistical) differences between the study groups in baseline characteristics
Bias: a systematic error or deviation in results or inferences from the truth
Bibliotherapy: resilience intervention is delivered via a self‐help book/self‐help materials
Blinding: process of preventing those involved in a trial from knowing to which comparison group a particular participant belongs. The risk of bias is minimised when as few people as possible know who is receiving the experimental intervention and who the control intervention. Participants, outcome assessors, and analysts are all candidates for being blinded
Cluster randomised trial: a trial in which clusters of individuals (e.g. clinics, geographical areas), rather than individuals themselves, are randomised to different arms
Coaching: resilience intervention uses a coaching approach (e.g. executive coaching, life coaching); individual problems of one or several clients are discussed with a coach; coaching approaches often include goal setting
Cochrane Handbook for Systematic Reviews of Interventions(formerly Cochrane Reviewers’ Handbook): document containing guidance and advice on how to prepare and maintain Cochrane reviews
Cognitive‐behavioural therapy/training (CBT): form of psychotherapy that is based on the assumption that mental health problems (e.g. depression) result from dysfunctional thinking and therefore aims to modify cognitive processes (e.g. identify and challenge dysfunctional thoughts in order to find functional ones)
Combined setting: resilience interventions delivered as combination of group and individual setting
Combined theoretical foundation/combination: resilience interventions that are based on two or more explicit theoretical foundations, such as CBT and ACT or CBT and mindfulness
Comorbidity: presence of one or more diseases or conditions other than those of primary interest
Concealment of allocation: process used to ensure that the person deciding to enter a participant into a randomised controlled trial does not know the comparison group into which that individual will be allocated. This is distinct from blinding, and is aimed at preventing selection bias. Some attempts at concealing allocation are more prone to manipulation than others, and the method of allocation concealment is used as an assessment of the quality of a trial
Conference abstract: short summary of presentations at conferences, which may be published
Confidence interval: a measure of the uncertainty around the main finding of a statistical analysis. Estimates of an effect, such as the standardised mean difference comparing an experimental intervention with a control, are usually presented as a point estimate and a 95% confidence interval. This means that if someone were to keep repeating a study in other samples from the same population, 95% of the confidence intervals from those studies would contain the true value of the unknown quantity. Wider intervals indicate lower precision; narrow intervals, greater precision
Conflict of interest: personal, financial, or other interests that could have influenced a person's contributions to a study
Control group/control: comparison group that receives no intervention, identical training after waiting period or an alternative intervention
Degrees of freedom: concept that refers to the number of independent contributions to a sampling distribution (such as Chi2 distribution)
Detection bias: systematic difference between comparison groups in how outcomes are ascertained, diagnosed or verified
Dichotomous data: data that can take one of two possible values, such as depressive/non‐depressive (depending on cut‐off for clinically relevant mental disorder)
Effect size: 1. generic term for the estimate of effect of treatment for a study; 2. dimensionless measure of effect used for continuous data when different scales (e.g. for measuring resilience) are used to measure an outcome
Estimate of effect: observed relationship between an intervention and an outcome expressed as standardised mean difference in this review
Face‐to‐face: resilience intervention delivered via face‐to‐face contact between trainer and one or several participants
F test: statistical hypothesis test derived from the F distribution; typically used to compare continuous data between more than two groups
False positive: a falsely drawn positive conclusion
Fixed‐effect model (in meta‐analysis): model that calculates a pooled effect estimate using the assumption that all observed variation between studies is caused by the play of chance; studies assumed to be measuring the same overall effect
Follow‐up: observation over a period of time of study/trial participants to measure outcomes under investigation; in this review: short‐term: three months or less; medium‐term: more than three to six months; and long‐term follow‐up: more than six months
Forest plot: graphical representation of the individual results of each study included in a meta‐analysis together with the combined meta‐analysis result; plot also allows readers to see the heterogeneity among the results of the studies. The results of individual studies are shown as squares centred on each study’s point estimate. A horizontal line runs through each square to show each study’s confidence interval (in this review: 95% confidence interval). The overall estimate from the meta‐analysis and its confidence interval are shown at the bottom, represented as a diamond. The centre of the diamond represents the pooled point estimate, and its horizontal tips represent the confidence interval.
Funnel plot: graphical display of some measure of study precision plotted against effect size that can be used to investigate whether there is a link between study size and treatment effect; one possible cause of an observed association is reporting bias
Grey literature: kind of material that is not published in easily accessible journals or databases (e.g. conference proceedings that include the abstracts of the research presented at conferences, unpublished theses, etc.)
Group setting: resilience intervention delivered in group of several participants
Hardiness: a (modifiable) personality characteristic ('a hardy person') that consists of three elements (challenge, commitment and control); partly used as synonym of resilience; in this review, hardiness is viewed as one of several resilience factors which partially determines resilience as outcome
Healthcare professionals: healthcare staff delivering direct medical care (e.g. nurses, physicians, hospital personnel)
Healthcare students: students in training for health professions delivering direct medical care (e.g. medical, nursing, midwifery or paramedic students)
Heterogeneity: 1. used in a general sense to describe the variation in, or diversity of, participants, interventions, and measurement of outcomes across a set of studies; 2. used specifically, as statistical heterogeneity, to describe the degree of variation in the effect estimates from a set of studies
Heterogeneous: used to describe a set of studies or participants with sizeable heterogeneity
Homogeneous: 1. used in a general sense to mean that the participants, interventions, and measurement of outcomes are similar across a set of studies; 2. used specifically to describe the effect estimates from a set of studies where they do not vary more than would be expected by chance
Individual setting: resilience interventions delivered in one‐on‐one setting
Intention to treat analysis: a strategy for analysing data from a randomised controlled trial; all participants are included in the arm to which they were allocated, whether or not they received (or completed) the intervention given to that arm. Intention‐to‐treat analysis prevents bias caused by the loss of participants, which may disrupt the baseline equivalence established by randomisation and which may reflect non‐adherence to the protocol
Inter‐rater reliability: degree of stability exhibited when a measurement is repeated under identical conditions by different raters; reliability refers to the degree to which the results obtained by a measurement procedure can be replicated. Lack of inter‐rater reliability may arise from divergences between observers or instability of the attribute being measured
Interaction: situation in which the effect of one independent variable on the outcome is affected by the value of a second independent variable
Intervention: the process of intervening on people in an experimental study (in this review: by resilience‐training programmes)
Intervention group: a group of participants in a study receiving a particular intervention (in this review: resilience intervention)
Laboratory delivery: resilience intervention is provided in the laboratory (under standardised conditions)
Mean: an average value, calculated by adding all the observations and dividing by the number of observations
Mean difference: difference between two estimated means (e.g. used in this review to present the results for single studies that could not be combined in meta‐analysis together with other studies)
MeSH headings (Medical Subject Headings): terms used by the United States National Library of Medicine to index articles in Index Medicus and MEDLINE. The MeSH system has a tree structure in which broad subject terms branch into a series of progressively narrower subject terms.
Meta‐analysis: use of statistical techniques in a systematic review to integrate the results of included studies
Mindfulness‐based training: intervention that aims to foster mindfulness (i.e. non‐judging awareness of the present moment and its accompanying mental phenomena, like body sensations, thoughts and emotions), by teaching formal and informal mindfulness practices (e.g. body scan, breathing awareness) (e.g. mindfulness‐based stress reduction, MBSR)
Mixed samples: studies with samples including healthcare professionals and participants from the non‐healthcare sector (e.g. ambulance personnel and firefighters)
Multimodal delivery: intervention is delivered by a combination of different formats (e.g. face‐to‐face and online)
No intervention control: control group that received no intervention
Online‐ or mobile‐based delivery: resilience intervention is delivered online/internet‐based or via smartphones (e.g. smartphone application)
Outcome: a component of a participant's clinical and functional status after an intervention has been applied, which is used to assess the effectiveness of an intervention
P value: the probability (ranging from zero to one) that the results observed in a study (or results more extreme) could have occurred by chance if in reality the null hypothesis was true. In a meta‐analysis, the P value for the overall effect assesses the overall statistical significance of the difference between the intervention groups, whilst the P value for the heterogeneity statistic assesses the statistical significance of differences between the effects observed in each study.
Parallel group trial: a trial that compares two groups of people concurrently, one of which receives the intervention of interest and one of which is a control group; some parallel trials have more than two comparison groups
Participant: an individual who is studied in a trial
Per protocol analysis: an analysis of the subset of participants from a randomised controlled trial who completed the trial or complied with the protocol sufficiently (e.g. specific dose of treatment) to ensure that their data would be likely to exhibit the effect of treatment; this subset may be defined after considering exposure to treatment and absence of major protocol violations. The per protocol analysis strategy may be subject to bias as the reasons for non‐compliance may be related to treatment.
Performance bias: systematic differences between intervention groups in care provided apart from the intervention being evaluated; for example, if participants know they are in the control group, they might act differently, and if intervention providers are aware of the group a particular participant is in, they might act differently. Blinding of study participants (both the recipients and providers of intervention) is used to protect against performance bias.
Positive psychology: scientific study of character strengths and positive aspects of human life (e.g. happiness) that allow individuals to thrive; interventions based on positive psychology aim to foster these factors
Post‐traumatic growth (also stress‐related growth): often used synonymously with resilience; however, in contrast to resilience (i.e. maintaining or restoring mental health after a stressor), post‐traumatic or stress‐related growth refers to increasing the level of functioning compared to that prior to the stressor
Post‐test/post‐intervention: the assessment immediately after the end of treatment (in this review: within one week after the end of training)
Precision: a measure of the likelihood of random errors in the results of the meta‐analysis; the greater the precision, the less random error. Confidence intervals around the estimate of effect from each study are one way of expressing precision, with a narrower confidence interval meaning more precision.
Primary outcome: the outcome of greatest importance
Primary study: ‘original research’ in which data are collected
Problem‐solving training: closely related to CBT; training based on problem‐solving theory (e.g. to foster a positive problem orientation and to teach structured problem‐solving)
Random allocation: method that uses the play of chance to assign participants to comparison groups in a trial, e.g. by using a random numbers table or a computer‐generated random sequence. Random allocation implies that each individual or unit being entered into a trial has the same chance of receiving each of the possible interventions. It also implies that the probability that an individual will receive a particular intervention is independent of the probability that any other individual will receive the same intervention.
Random‐effects model (in meta‐analysis): a statistical model in which both within‐study sampling error (variance) and between‐studies variation are included in the assessment of the uncertainty (confidence interval) of the results of a meta‐analysis; when there is heterogeneity among the results of the included studies beyond chance, random‐effects models will give wider confidence intervals than fixed‐effect models
Randomisation: the process of randomly allocating participants into one of the arms of a controlled trial. There are two components to randomisation: the generation of a random sequence; and its implementation, ideally in a way so that those entering participants into a study are not aware of the sequence (concealment of allocation).
Randomised controlled trial: study in which two or more conditions, possibly including a control intervention or no intervention, are compared by being randomly allocated to participants
Reporting bias: bias caused by only a subset of all the relevant data being available. The publication of research can depend on the nature and direction of the study results. Studies in which an intervention is not found to be effective are sometimes not published. In addition, a published report might present a biased set of results (e.g. only outcomes or subgroups where a statistically significant difference was found).
Resilience: maintenance or fast recovery of mental health during or after substantial adversities; different definitions exist, however, there is a consensus about two essentials: 1. exposure to substantial stressors or adversities; 2. successful coping with these adversities
Resilience factor: psychological or social factors associated to resilience, e.g. optimism
Search strategy: 1. the methods used to identify trials within the review's scope (including searching electronic databases, trial registers, personal contact with researchers/study authors and checking reference lists); 2. the combination of terms used to identify studies in an electronic database such as MEDLINE
Secondary outcome: an outcome used to evaluate additional effects of the intervention deemed a priori as being less important than the primary outcomes
Selection bias: systematic differences between comparison groups in prognosis or responsiveness to treatment; random allocation with adequate concealment of allocation protects against selection bias. Other means of selecting who receives the intervention are more prone to bias because decisions may be related to prognosis or responsiveness to treatment
Sensitivity analysis: analysis used to determine how sensitive the results of the systematic review are to changes in how it was done; sensitivity analyses are used to assess how robust the results are to uncertain decisions or assumptions about the data and the methods that were used.
Single blind: single masked
Standard deviation: measure of the spread or dispersion of a set of observations, calculated as the average difference from the mean value in the sample
Standard error: standard deviation of the sampling distribution of a statistic; measurements taken from a sample of the population will vary from sample to sample. The standard error is a measure of the variation in the sample statistic over all possible samples of the same size. The standard error decreases as the sample size increases.
Standardised mean difference: difference between two estimated means divided by an estimate of the standard deviation; used to combine results from studies using different ways of measuring the same concept, e.g. resilience or mental health. By expressing the effects as a standardised value, the results can be combined since they have no units.
Stress inoculation: form of CBT; psychotherapeutic method to prepare participants to deal with stressors successfully and to achieve coping strategies by exposing them to milder forms of stress
Subgroup analysis: an analysis in which the intervention effect is evaluated in a defined subset of the participants/interventions in a trial, or in complementary subsets, such as by intervention setting or delivery format
Telephone delivery: resilience intervention that are provided via the telephone (e.g. calls between trainer and participant)
Training intensity: intensity of intervention as indicated by the number of sessions or the number of hours (i.e. duration); in this review: low intensity: total duration of ≤ five hours or ≤ three sessions; moderate intensity: > 5 hours to ≤ 12 hours or > 3 to ≤ 12 sessions; high intensity: > 12 hours or > 12 sessions
Treatment as usual (TAU): the control group receives a (established) standard treatment (synonyms: standard care, usual care)
t test: a statistical hypothesis test derived from the t distribution; used to compare continuous data in two groups
Trialist: refers to a person conducting or publishing a controlled trial
Type I error (also false positive): conclusion that a treatment works, when it actually does not work; the risk of a Type I error is often called alpha. In a statistical test, it describes the chance of rejecting the null hypothesis when it is in fact true.
Unspecific theoretical foundation/unspecific training programmes: resilience interventions fostering one or several resilience factors but without specifying any explicit theoretical foundation or where the underlying framework cannot be assigned to a certain theoretical approach
Unspecified/not specified setting, delivery, training intensity or comparator: no information on the respective intervention characteristic or the comparator are available and could not be received by the study authors
Variable: a factor that differs among and between groups of people, e.g. patient characteristics such as age, sex, and smoking, or measurements such as blood pressure or depression score; there can also be treatment or condition variables (e.g. length of treatment dose) and outcome variables
Wait‐list control: control group receiving the training after a waiting period
Footnotes
This glossary is based, in part, on the glossary of the Cochrane Community (Cochrane Community 2020).
Appendix 2. Evidence rating of modifiable resilience factors
Although an immense number of factors have been discussed in the literature, only a set of psychosocial factors has been scientifically validated as being appropriate determinants of resilience by cross‐sectional and longitudinal (frequently observational) studies in different populations (e.g. patients affected by physical diseases like cancer, diabetes, spinal cord injury, coronary heart disease, etc.; different caregiver groups; individuals after trauma exposure). Upon closer examination, only some of the discussed resilience factors may be viewed as well‐evidenced factors that have also been found to be protective factors in systematic reviews and meta‐analyses (level 1). These factors are most likely to be related to adult resilience, as they were proven in different populations facing various adversities and stressors. However, it has to be kept in mind that the chosen factors represent the current state of knowledge on psychosocial resilience‐promoting factors, and that other factors, which are not yet well researched, could also contribute to resilience.
| Level of evidence and criteria | Resilience factors |
Level 1: strong evidence (SRs and MAs)
| |
| Level 1a: there is evidence for this factor from several SRs AND several MAs (both across different populations) |
|
| Level 1b: there is evidence for this factor from several SRs AND a single MA (both across different populations) |
|
| Level 1c: there is evidence for this factor from several SRs (across different populations) AND a single MA (in the same population) |
|
Level 2: moderate evidence (only SRs or single MA)
| |
| Level 2a: there is evidence for this factor from several SRs (across different populations) OR there is no evidence from SRs, but from a MA (across different populations) |
|
| Level 2b: there is evidence for this factor from several SRs (in the same population) |
|
| Level 2c: there is evidence for this factor from a single SR (in the same population) |
|
Level 3: weak evidence (no SR or MA)
| |
|
|
| MA: Meta‐analysis; SR: Systematic review. | |
Footnotes
Results of systematic reviews and meta‐analyses based on a literature search for potentially modifiable resilience factors in MEDLINE (search strategy: respective resilience factor.tw. AND (review or meta‐analy$).tw.; search limited to “All adults (19 plus years)” and 1990 to 2016).
aCognitive flexibility and religiosity or spirituality are multidimensional concepts resulting in highly ambiguous operationalisations. Cognitive flexibility comprises several concepts, such as positive reappraisal and acceptance (Southwick 2005). Religiosity or spirituality combines affective, behavioural and cognitive dimensions, each measured differently (Ano 2005; Pargament 2000; Salsman 2015).
Appendix 3. Examples of training methods to address resilience factors
| Evidence‐based resilience factor | Examples of training methods to address the resilience factor |
| Meaning in life or purpose in life | Introduce the benefits of purpose in life; support individuals in identifying important sources of meaning (e.g. social relationships, work) as well as in setting priorities and guiding values for their life (e.g. Sood 2011) |
| Sense of coherence (comprehensibility, meaningfulness, manageability) | Promote the understanding of external life challenges, personal beliefs and emotions; encourage participants to reflect on personal (internal or external) resources and to use them more frequently (e.g. Tan 2016) |
| Positive emotions or positive affect | Psycho‐education on emotions; mindfulness techniques; support individuals in identifying pleasant activities to enhance positive emotions (e.g. Jennings 2013) |
| Hardiness(challenge, commitment, control) | Situational reconstruction (i.e. imagination of stressful circumstances); focusing (i.e. reflection on bodily sensations of emotional upset) (e.g. Maddi 1998; Maddi 2009) |
| Self‐esteem | Support participants in identifying personal strengths |
| Active coping (e.g. problem‐solving, planning) | Introduce the problem‐solving model and familiarise participants with the use of active coping strategies in stressful situations (e.g. making action plans) (e.g. Abbott 2009; Bekki 2013; Sahler 2013) |
| Self‐efficacy | Support participants in identifying personal strengths and other sources of self‐efficacy (e.g. social connections); support individuals in realising previous successes (e.g. coping with negative situations) |
| Optimism or positive attributional style | Teach participants to adopt a more positive attributional style for stressful (i.e. external, unstable, specific) and pleasant events (i.e. internal, stable, global); encourage individuals to gain a brighter outlook for the future by enhancing their attention for and the discovery of positive aspects in their lives (e.g. Carver 2010; Sadow 1993) |
| Social support | Encourage the individual’s reflection on his or her current network (i.e. magnitude of social network, positive or negative aspects in social relationships); enhance the individual’s support network by providing them with communication techniques (e.g. Kent 2011; Schachman 2004; Sood 2011; Steinhardt 2008) |
| Cognitive flexibility (e.g. positive reappraisal, acceptance of negative situations and emotions) | Positive reappraisal: introduction of ABC (Activating event, Belief, Consequence) Technique of Irrational Beliefs (Ellis 1957) of cognitive therapy; train participants in identifying and challenging maladaptive thoughts and replacing them by more positive ones (e.g. Abbott 2009; Farchi 2010; Songprakun 2012; Steinhardt 2008) Acceptance: relaxation or mindfulness techniques |
| Religiosity or spirituality or religious coping(e.g. frequent religious attendance) | Spiritual exercises like meditation or yoga; psycho‐education on coping strategies like regular praying or participating in religious community activities (e.g. worship) (e.g. Sood 2011) |
Appendix 4. Previous systematic reviews and meta‐analyses and their methodological weaknesses
There are a number of systematic reviews and meta‐analyses of various forms of interventions to foster healthcare students' mental health e.g. Buddeberg‐Fischer 2006; Dawson 2019; Dobkin 2013; Foster 2015; Frei 2010; Gao 2019; Griffiths 2019; Jones 2000; Lovell 2018; Shiralkar 2013; Turner 2017; Williams 2015.
Systematic reviews and meta‐analyses on resilience interventions in clinical and non‐clinical adult populations
| Category | Details of previous reviews/meta‐analyses |
| Number of reviews and meta‐analyses |
|
| Methodological characteristics | Eligibility critieria: heterogeneous eligibility criteria (e.g. by study design) and definitions of resilience training (e.g. the aim of fostering resilience was not always stated in the included primary studies) |
| Search strategy: Some reviews used rather simple, limited search strategies to identify relevant studies (e.g. only resilience/hardiness combined with training terms in, for example, Joyce 2018; Robertson 2015; restriction to English language), which may bias the search results | |
| Review protocol/registration: A review protocol or PROSPERO registration was available for 5 publications only (Bauer 2018; Kunzler 2020; Leppin 2014; Townshend 2016; Wainwright 2019) | |
| Review according to guidelines: Most reviews report having been conducted according to the PRISMA or alternative guidelines, such as the guidance for undertaking reviews in healthcare (CRD 2009; e.g. Milne 2016; Van Kessel 2014) or Cochrane guidelines (Higgins 2019a; e.g. Kunzler 2020) | |
| Quality assessment of included studies: Most reviews performed a quality assessment of the primary studies (the exceptions being Milne 2016; Pallavicini 2016; Reyes 2018; Skeffington 2013; Vanhove 2016, who only judged publication bias; we were also unable to verify if Tams 2016 conducted a quality assessment because we were unable to retrieve the full text). For studies included in several reviews, the reported risk of bias also differed between publications (e.g. detection bias for Abbott 2009 differed between Leppin 2014 and Robertson 2015) |
Footnotes aDeady 2017 and Tams 2016 searched for 'resilience' and related constructs, but did not formulate specific eligibility criteria for resilience‐training programmes.
Systematic reviews and meta‐analyses on resilience interventions in healthcare students
| Category | Details of previous reviews/meta‐analyses |
| Number of reviews and meta‐analyses |
|
| Methodological characteristics |
Eligibility criteria:
|
Search strategy:
| |
| Review protocol/registration: Aside from Gilmartin 2017 and Pezaro 2017, most of these reviews did not have a published protocol or protocol registration, which reduces transparency and comparability in the reviews' procedures and potentially restricts the evidence found | |
| Review according to guidelines: 1 review did not specify whether it had been conducted according to guidelines, such as PRISMA or Cochrane guidelines, or other validated frameworks (Rogers 2016) | |
Quality assessment of included studies:
| |
| RCT: Randomised controlled trial | |
Footnotes
aLo 2018 and Pezaro 2017 searched for resilience and identified resilience intervention studies for healthcare students but did not initially focus on identifying such programmes (e.g. no respective eligibility criteria).
Appendix 5. Potential instruments for the measurement of psychological resilience based on previous reviews (Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016) and additional literature searchesa
| N° | Measure | Theory and item selection | Internal consistency | Validity | Rating |
| 1 | Resilience Scale (RS‐25) (Wagnild 1993)b | + | +++ | +++ | 6✦ |
| 2 | Brief Resilience Scale (BRS) (Smith 2008) | + | +++ | +++ | 6✦ |
| 3 | Ego Resiliency (Klohnen 1996)b | + | ++ | +++ | 5✦ |
| 4 | Connor‐Davidson Resilience Scale (CD‐RISC) (Connor 2003) | + | ++ | +++ | 5✦ |
| 5 | Resilience Scale for Adults (RSA33) (Friborg 2005) | + | ++ | +++ | 5✦ |
| 6 | Trauma Resilience Scale (TRS37) (Madsen 2010) | + | +++ | ++ | 5✦ |
| 7 | Ego‐Resiliency Scale (ER89) (Block 1996)b | ‐ | ++ | +++ | 5✧ |
| 8 | Resilience Scale (RS‐14) (Wagnild 2009)b | + | +++ | + | 4✦ |
| 9 | Resilience Scale for Adults (RSA37) (Friborg 2003) | + | ++ | ++ | 4✦ |
| 10 | Resilience at Work Scale (Winwood 2013) | + | ++ | ++ | 4✦ |
| 11 | Workplace Resilience Inventory (WRI) (McLarnon 2013) | + | ++ | ++ | 4✦ |
| 12 | Multidimensional Trauma Recovery and Resiliency Scale (MTRR) (Harvey 2003) | + | +++ | + | 4✦ |
| 13 | Resiliency Attitudes and Skills Profile (RASP) (Hurtes 2001) | + | +++ | + | 4✦ |
| 14 | Resilience Appraisals Scale (RAS) (Johnson 2010) | ‐ | +++ | + | 4✧ |
| 15 | Revised Ego Resiliency 89 Scale (ER89‐R) (Alessandri 2007)b | + | ++ | + | 3✦ |
| 16 | Ego Resiliency (Bromley 2006)b | + | ++ | + | 3✦ |
| 17 | Connor‐Davidson Resilience Scale (CD‐RISC‐10) (Campbell‐Sills 2007) | + | ++ | + | 3✦ |
| 18 | Resilience Scale for Adults (RSA45) (Hjemdal 2001) | + | +++ | ‐ | 3✦ |
| 19 | Brief Resilient Coping Scale (BRCS) (Sinclair 2004) | + | + | ++ | 3✦ |
| 20 | Trauma Resilience Scale (TRS48) (Madsen 2010) | + | +++ | ‐ | 3✦ |
| 21 | Child and Youth Resilience Measure ‐ 28 (CYRM‐28) (Liebenberg 2012; Ungar 2008) | + | +++ | ‐ | 3✦ |
| 22 | Post‐traumatic Growth Inventory (PTGI) (Tedeschi 1996)c | + | ++ | + | 3✦ |
| 23 | Adolescent Resilience Scale (Oshio 2002; Oshio 2003) | ‐ | ++ | + | 3✧ |
| 24 | Resilience and Reintegration (20 items drawn from Spirit Core Scale) (Waite 2004) | ‐ | +++ | ‐ | 3✧ |
| 25 | Psychological resilience (Windle 2008) | + | ++ | ‐ | 2✦ |
| 26 | Child and Youth Resilience Measure ‐ 12 (CYRM‐12) (Liebenberg 2013) | + | ++ | ‐ | 2✦ |
| 27 | Resilience scale (Bekki 2013) | + | ++ | ‐ | 2✦ |
| 28 | Perceived Resilience (Van der Kleij 2011) | ‐ | ++ | ‐ | 2✧ |
| 29 | Romanian Scale of Resilience to Occupational Stress (SROS) (Aniţei 2012) | ‐ | ‐ | ‐ | 0✧ |
Footnotes
The resilience scales are organised hierarchically according to psychometric quality criteria.
Theory & item selection: ‐ (✧): no description of theory or item selection process available; and + (✦): description of theory or item selection process available.
Internal consistency (Cronbach’s alpha): ‐ (0): no information; + (1): α < 0.70; ++ (2): α ≥ 0.70; and +++ (3): α > 0.90.
Validity (convergent/divergent or criterion validity): ‐ (0): no information; + (1): correlations (r) with construct‐related measures or criteria available, all correlations < 0.50 or resilience measure only correlated with original instrument/long‐form or no correlations but alternative results reported (e.g. odds ratio); ++ (2): correlations (r) with construct‐related measures or criteria available, ≤ 50% of correlations ≥ 0.50; and +++ (3): correlations (r) with construct‐related measures or criteria available, > 50% of correlations ≥ 0.50.
a At the time of prespecifying these measures, and the publication of our protocol (Helmreich 2017), the systematic review of Joyce 2018 had not yet been published and was not considered in the development of this appendix. bScales assessing resilience as personality characteristic. cScale assessing post‐traumatic growth.
Appendix 6. Possible assessment instruments for the measurement of mental health and well‐being based on intervention studies included in previous reviews and meta‐analyses (Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016)a
-
Anxiety
Depression Anxiety and Stress Scales (DASS‐21) (Lovibond 1995)
Smith Anxiety Scale (SAS) (Smith 2007)
Beck Anxiety Inventory (BAI) (Beck 1993)
State‐Trait Anxiety Inventory (STAI) (Spielberger 1970)
-
Depression
Depression Anxiety and Stress Scales (DASS‐21) (Lovibond 1995)
Center for Epidemiological Studies ‐ Depression Scale (CES‐D) (Radloff 1977)
Maslach Burnout Inventory (MBI) (Maslach 1997)
Oldenburg Burnout Inventory (Demerouti 2010)
Beck Depression Inventory (BDI) (Beck 1961)
Beck Depression Inventory ‐ II (BDI‐II) (Beck 1996)
Visual Analogue Scale ‐ Fatigue (VAS‐Fatigue) (Wolfe 2004)
Patient Health Questionnaire for Depression (PHQ‐D) (Spitzer 1999)
Hospital Anxiety and Depression Scale (HADS) (Zigmond 1983)
Time Urgency Scale (TUS) (Landy 1991)
-
Stress or stress perception
Depression Anxiety and Stress Scales (DASS‐21) (Lovibond 1995)
Perceived Stress Scale (PSS) (Cohen 1988a)
Personal Stress Scale (PSS) (self‐developed) (Petree 2012)
Subjective Units of Distress (SUDS) (Wolpe 1958)
Visual Analogue Scale (VAS) (Arnetz 1985; Hasson 2005)
Stress and Perception of Control Scale (SPOCS) (unpublished instrument) (Rose 2013)
-
Well‐being or life satisfaction or quality of life or vitality or vigour
-
Well‐being
-
Life satisfaction:
Satisfaction with Life Scale (Diener 1985)
-
(Health‐related) Quality of life (QOL):
Linear Analog Self‐Assessment Scale (QOL‐LASA) (Locke 2007)
Medical Outcomes Study (MOS) 36‐item short‐form health survey (SF‐36) (Ware 1994)
World Health Organization Quality of Life – BREF (WHOQOL‐BREF) (WHOQOL Group 1998)
-
Vitality
Subscale of the MOS 36‐item short‐form health survey (SF‐36) (Ware 1994)
-
Vigour
Work Vigour subscale of the Utrecht Work Engagement scale (Schaufeli 2002)
-
aAt the time of prespecifying these measures, and the publication of the protocol (Helmreich 2017), the systematic review of Joyce 2018 had not yet been published and was not considered in the development of this appendix.
Appendix 7. Possible assessment instruments for the measurement of resilience factors based on intervention studies included in previous reviews and meta‐analyses (Leppin 2014; Macedo 2014; Robertson 2015; Vanhove 2016)a
-
Social support
Interpersonal Support Evaluation List ‐ 12 (ISEL‐12) (Cohen 1983a)
Personal Resources Questionnaire (PRQ‐85) (Brandt 1981)
Social Provisions Scale (Cutrona 1987)
Subscale Interpersonal relations of the Health‐Promoting Lifestyle Profile II (Walker 1987)
Interpersonal Relationship Inventory (IPR) (Tilden 1990)
Support questionnaire (Cushway 1996)
MOS Social Support Survey (Sherbourne 1991)
Total of four scales devised by Moos (1979) for perceived social support (Maddi 1998)
-
Optimism
Life Orientation Test ‐ Revised (LOT‐R) (Scheier 1994)
-
Self‐efficacy
Coping self‐efficacy (CSE) (Chesney 2003)
Self‐efficacy scale (Sherer 1982)
Teachers’ Sense of Efficacy Questionnaire (TSES) (Tschannen‐Moran 2001)
New General Self‐Efficacy Scale (NGSE) (Chen 2004)
Coping Efficacy Scale (self‐developed) (Bekki 2013)
-
Active coping
Brief Coping Orientations to Problems Experienced scale (Brief COPE) (Carver 1997)
Ways of Coping Questionnaire (WOC) (Folkman 1988)
Coping Styles Questionnaire (CSQ) (Williams 1997)
Coping Styles (self‐developed) (Bekki 2013)
-
Self‐esteem
Rosenberg Self‐Esteem Scale (RSES) (Rosenberg 1965)
Self‐Esteem Rating Scale (SERS) (Nugent 1993)
-
Hardiness
HardiSurvey III ‐ R (Maddi 2001)
Personal Views Survey (Maddi 1987)
Hardiness Scale or College Student Hardiness Measure (CSHM) (Atri 2007a; Atri 2007b; Kanekar 2010)
Cognitive Hardiness Scale (Nowack 1990)
-
Positive emotions or positive affect
Positive and Negative Affect Schedule (PANAS) (Watson 1988)
Positive and Negative Affect Schedule Expanded Form (PANAS‐X) (Watson 1994)
Authentic Happiness Inventory (AHI; unpublished measure) (Abbott 2009)
aAt the time of prespecifying these measures, and the publication of our protocol (Helmreich 2017), the systematic review of Joyce 2018 had not yet been published and was not considered in the development of this appendix.
Appendix 8. Search strategies up to 2016
In order to get a comprehensive understanding of the evidence in the field of psychological resilience interventions, and to identify training programmes that can really be assumed to enhance resilience in adults based on scientific findings, we performed a literature search that combined and complemented the search approaches from previous reviews and meta‐analyses.
In contrast to the search strategy of Joyce 2018, Leppin 2014, Robertson 2015 and Vanhove 2016, who used very narrow search terms (e.g. ‘resilience programme’ or 'hardiness training’), we also searched for broader intervention terms. These broader search terms were based on the search performed by Macedo 2014, but were also supplemented by new terms (e.g. ‘acceptance and commitment therapy’, ‘stress management’, ‘mindfulness’).
We searched the databases below in October 2016 using search strategies based on the original inclusion criteria for this review.
Cochrane Central Register of Controlled Trials (CENTRAL), in the Cochrane Library
Searched 27 October 2016 [5168 records]
#1 [mh "Resilience, Psychological"] #2 [mh "social adjustment"] #3 [mh "Adaptation, Psychological"] #4 ("post‐traumatic growth" or "posttraumatic growth" or "stress‐related growth") #5 (positiv* near/1 (adapt* or adjust*)) #6 (psychol* near/1 (adapt* or adjust*)) #7 (resilien* or hardiness*) #8 (cope or coping) #9 ((withstand* or overcom* or resist* or recover* or thriv* or adapt* or adjust* or bounc* back) near/5 (stress* or trauma* or adversit*)) #10 {or #1‐#9} #11 [mh psychotherapy] #12 MeSH descriptor: [Stress, Psychological] this term only and with qualifier(s): [Therapy ‐ TH] #13 (psychotherap* or psycho next therap*) #14 (behav* near/3 (intervention* or program* or therap*)) #15 ((cognit* or cognitive next behavior* or CBT) near/3 (intervention* or program* or therap*)) #16 (psycho* near/3 (intervention* or program* or therap*)) #17 relaxation #18 mindful* #19 (counsel*ing or coaching) #20 (third next wave next (psycho* or therap*)) #21 cognit* next restructur* #22 positive next psychology #23 (refram* or re next fram* or reapprais*) #24 (stress near/1 (inoculation or manag* or reduc* or resist*)) #25 (anxiety near/3 manage*) #26 "acceptance and commitment " #27 [mh "Combined Modality Therapy"] #28 (multimodal* or multi next modal* or combined modal*) #29 [mh "Health promotion"] #30 (health near/3 (educat* or promot*)) #31 {or #11‐#30} #32 #10 and #31, Publication Year from 1990 to 2016, in Trials
MEDLINE Ovid
Searched 28 October 2016 [6723 records]
1 Resilience, Psychological/ 2 social adjustment/ 3 Adaptation, Psychological/ 4 (post‐traumatic growth or posttraumatic growth or stress‐related growth).tw,kf. 5 (positiv$ adj1 (adapt$ or adjust$)).tw,kf. 6 (psychol$ adj1 (adapt$ or adjust$)).tw,kf. 7 (resilien$ or hardiness$).tw,kf. 8 (cope or coping).tw,kf. 9 ((withstand$ or overcom$ or resist$ or recover$ or thriv$ or adapt$ or adjust$ or bounc$ back) adj5 (stress$ or trauma$ or adversit$)).tw,kf. 10 or/1‐9 11 exp psychotherapy/ 12 Stress, Psychological/th 13 (psychotherap$ or psycho‐therap$).tw,kf. 14 (behav$ adj3 (intervention$ or program$ or therap$)).tw,kf. 15 ((cognit$ or cognitive behavior$ or CBT) adj3 (intervention$ or program$ or therap$)).tw,kf. 16 (psycho$ adj3 (intervention$ or program$ or therap$)).tw,kf. 17 relaxation.tw,kf. 18 mindful$.tw,kf. 19 (counsel?ing or coaching).tw,kf. 20 (third wave adj (psycho$ or therap$)).tw,kf. 21 cognit$ restructur$.tw,kf. 22 positive psychology.tw,kf. 23 (refram$ or re‐fram$ or reapprais$).tw,kf. 24 (stress adj1 (inoculation or manag$ or reduc$ or resist$)).tw,kf. 25 (anxiety adj3 manage$).tw,kf. 26 "acceptance and commitment ".tw,kf. 27 Combined Modality Therapy/ 28 (multimodal or multi‐modal or combined modal$).tw,kf. 29 exp Health promotion/ 30 (health adj3 (educat$ or promot$)).tw,kf. 31 or/11‐30 32 10 and 31 33 (resilien$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kf. 34 (hardiness$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kf. 35 or/32‐34 36 randomized controlled trial.pt. 37 controlled clinical trial.pt. 38 randomi#ed.ab. 39 placebo$.ab. 40 drug therapy.fs. 41 randomly.ab. 42 trial.ab. 43 groups.ab. 44 or/36‐43 45 exp animals/ not humans.sh. 46 44 not 45 47 35 and 46 48 limit 47 to yr="1990 ‐Current"
Embase Ovid
Searched 26 October 2016 [6709 records]
1 exp coping behavior/ 2 psychological adjustment/ 3 social adaptation/ 4 "personal resource"/ 5 (post‐traumatic growth or posttraumatic growth or stress‐related growth).tw,kw. 6 (positiv$ adj1 (adapt$ or adjust$)).tw,kw. 7 (psychol$ adj1 (adapt$ or adjust$)).tw,kw. 8 (resilien$ or hardiness$).tw,kw. 9 (cope or coping).tw,kw. 10 ((withstand$ or overcom$ or resist$ or recover$ or thriv$ or adapt$ or adjust$ or bounc$ back) adj5 (stress$ or trauma$ or advers$)).tw,kw. 11 or/1‐10 12 exp psychotherapy/ 13 posttraumatic stress disorder/th [Therapy] 14 mental stress/th [Therapy] 15 (psychotherap$ or psycho‐therap$).tw,kw. 16 (behav$ adj3 (intervention$ or program$ or therap$)).tw,kw. 17 ((cognit$ or cognitive behavior$ or CBT) adj3 (intervention$ or program$ or therap$)).tw,kw. 18 (psycho$ adj3 (intervention$ or program$ or therap$)).tw,kw. 19 mindful$.tw,kw. 20 exp counseling/ 21 (counsel?ing or coaching).tw,kw. 22 mindfulness/ 23 mindful$.tw,kw. 24 (third wave adj (psycho$ or therap$)).tw,kw. 25 cognit$ restructur$.tw,kw. 26 positive psychology.tw,kw. 27 (refram$ or re‐fram$ or reapprais$).tw,kw. 28 (stress adj1 (inoculation or manag$ or reduc$ or resist$)).tw,kw. 29 (anxiety adj3 manage$).tw,kw. 30 "acceptance and commitment ".tw,kw. 31 (multimodal$ or multi‐modal$ or combined modal$).tw,kw. 32 exp health promotion/ 33 (health adj3 (educat$ or promot$)).tw,kw. 34 or/12‐33 35 11 and 34 36 (resilien$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kw. 37 (hardiness$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kw. 38 or/35‐37 39 Randomized controlled trial/ 40 controlled clinical trial/ 41 Single blind procedure/ 42 Double blind procedure/ 43 triple blind procedure/ 44 Crossover procedure/ 45 (crossover or cross‐over).tw. 46 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 47 Placebo/ 48 placebo.tw. 49 prospective.tw. 50 factorial$.tw. 51 random$.tw. 52 assign$.ab. 53 allocat$.tw. 54 volunteer$.ab. 55 or/39‐54 56 38 and 55 57 limit 56 to yr="1990 ‐Current" 58 exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/ 59 human/ or normal human/ or human cell/ (18144770) 60 58 and 59 61 58 not 60 62 57 not 61
PsycINFO Ovid
Searched 27 October 2016 [5005 records]
1 "resilience (psychological)"/ 2 "adaptability (personality)"/ 3 emotional adjustment/ 4 coping behavior/ 5 posttraumatic growth/ 6 protective factors/ 7 (post‐traumatic growth or posttraumatic growth or stress‐related growth).tw. 8 (positiv$ adj1 (adapt$ or adjust$)).tw. 9 (psychol$ adj1 (adapt$ or adjust$)).tw. 10 (resilien$ or hardiness$).tw. 11 (cope or coping).tw. 12 ((withstand$ or overcom$ or resist$ or recover$ or thriv$ or adapt$ or adjust$ or bounc$ back) adj3 (stress$ or trauma$ or advers$)).tw. 13 or/1‐12 14 exp psychotherapy/ 15 exp cognitive techniques/ 16 psychotherapeutic techniques/ 17 relaxation therapy/ 18 mindfulness/ 19 stress management/ 20 (psychotherap$ or psycho‐therap$).tw. 21 (behav$ adj3 (intervention$ or program$ or therap$)).tw. 22 ((cognit$ or cognitive behavior$ or CBT) adj3 (intervention$ or program$ or therap$)).tw. 23 (psycho$ adj3 (intervention$ or program$ or therap$)).tw. 24 relaxation.tw. 25 mindful$.tw. 26 (counsel?ing or coaching).tw. 27 (third wave adj (psycho$ or therap$)).tw. 28 cognit$ restructur$.tw. 29 positive psychology.tw. 30 (refram$ or re‐fram$ or reapprais$).tw. 31 (stress adj1 (inoculation or manag$ or reduc$ or resist$)).tw. 32 (anxiety adj3 manage$).tw. 33 "acceptance and commitment".tw. 34 multimodal treatment approach/ 35 (multimodal$ or multi‐modal$ or combined modal$).tw. 36 health promotion/ 37 (health adj3 (educat$ or promot$)).tw. 38 or/14‐37 39 13 and 38 40 (resilien$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw. 41 (hardiness$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw. 42 or/39‐41 43 clinical trials/ 44 longitudinal studies/ 45 exp program evaluation/ 46 treatment effectiveness evaluation/ 47 random$.tw. 48 (allocat$ or assign$).tw. 49 ((clinic$ or control$) adj trial$).tw. 50 ((control$ or experiment$ or intervention$) adj3 group$).tw. 51 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw. 52 (crossover$ or "cross over$").tw. 53 (placebo$ or (usual adj1 treatment$) or wait$ list).tw. 54 prospectiv$.tw. 55 (crossover or cross‐over).tw. 56 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 57 ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw. 58 or/43‐57 59 42 and 58 60 limit 59 to yr="1990 ‐Current"
CINAHL EBSCOhost
Searched 28 October 2016 [1355 records]
1 (MH "Hardiness") 2 (MH "Social Adjustment") 3 (MH "Adaptation, Psychological") 4 TI ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") 5 TI (positiv* N1 (adapt* OR adjust*)) OR AB (positiv* N1 (adapt* OR adjust*)) 6 TI (psychol* N1 (adapt* OR adjust*)) OR AB (psychol* N1 (adapt* OR adjust*)) 7 TI (resilien* OR hardiness*) OR AB (resilien* OR hardiness*) 8 (MH "Coping") 9 TI (cope OR coping) OR AB (cope OR coping) 10 TI ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR AB ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) 11 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 12 (MH "Psychotherapy+") 13 (MH "Stress, Psychological/TH") 14 TI (psychotherap* OR psychotherap*) OR AB (psychotherap* OR psychotherap*) 15 TI (behav* N3 (intervention* OR program* OR therap*)) OR AB (behav* N3 (intervention* OR program* OR therap*)) 16 TI ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR AB ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) 17 TI (psycho* N3 (intervention* OR program* OR therap*)) OR AB (psycho* N3 (intervention* OR program* OR therap*)) 18 TI relaxation OR AB relaxation 19 TI mindful* OR AB mindful* 20 TI (counsel?ing OR coaching) OR AB (counsel?ing OR coaching) 21 TI ("third wave" N1 (psycho* OR therap*)) OR AB ("third wave" N1 (psycho* OR therap*)) 22 TI "cognit* restructur*" OR AB "cognit* restructur*" 23 TI "positive psychology" OR AB "positive psychology" 24 TI (refram* OR refram* OR reapprais*) OR AB (refram* OR refram* OR reapprais*) 25 TI (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR AB (stress N1 (inoculation OR manag* OR reduc* OR resist*)) 26 TI (anxiety N3 manage*) OR AB (anxiety N3 manage*) 27 TI "acceptance and commitment" OR AB "acceptance and commitment" 28 (MH "Combined Modality Therapy") 29 TI (multimodal OR multimodal OR "combined modal*") OR AB (multimodal OR multimodal OR "combined modal*") 30 (MH "Health Promotion+") 31 TI (health N3 (educat* OR promot*)) OR AB (health N3 (educat* OR promot*)) 32 S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 33 S11 AND S32 34 TI (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 35 TI (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 36 S33 S34 OR S35 37 PT randomized controlled trial 38 TI "randomi?ed control* trial*" OR AB "randomi?ed control* trial*" 39 TI "control* clinical trial*" OR AB "control* clinical trial*" 40 AB randomi?ed 41 AB placebo* 42 AB randomly 43 AB trial 44 S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 45 S36 AND S44 46 S36 AND S44, Limiters Published Date: 1990010120161031
PSYNDEX EBSCOhost
Searched 27 October 2016 [156 records]
1 DE "Resilience (Psychological)" 2 DE "Emotional Adjustment" OR DE "Social Adjustment" 3 DE "Posttraumatic Growth" 4 TI ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR SU ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") 5 TI (positiv* N1 (adapt* OR adjust*)) OR AB (positiv* N1 (adapt* OR adjust*)) OR SU (positiv* N1 (adapt* OR adjust*)) 6 TI (psychol* N1 (adapt* OR adjust*)) OR AB (psychol* N1 (adapt* OR adjust*)) OR SU (psychol* N1 (adapt* OR adjust*)) 7 TI (resilien* OR hardiness*) OR AB (resilien* OR hardiness*) OR SU (resilien* OR hardiness*) 8 DE "Coping Behavior" 9 TI (cope OR coping) OR AB (cope OR coping) OR SU (cope OR coping) 10 TI ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR AB ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR SU ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) 11 DE "Psychological Stress" 12 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 13 DE "Psychotherapy" OR DE "Adlerian Psychotherapy" OR DE "Adolescent Psychotherapy" OR DE "Affirmative Therapy" OR DE "Analytical Psychotherapy" OR DE "Autogenic Training" OR DE "Behavior Therapy" OR DE "Brief Psychotherapy" OR DE "Brief Relational Therapy" OR DE "Child Psychotherapy" OR DE "Client Centered Therapy" OR DE "Cognitive Behavior Therapy" OR DE "Conversion Therapy" OR DE "Eclectic Psychotherapy" OR DE "Emotion Focused Therapy" OR DE "Existential Therapy" OR DE "Experiential Psychotherapy" OR DE "Expressive Psychotherapy" OR DE "Eye Movement Desensitization Therapy" OR DE "Feminist Therapy" OR DE "Geriatric Psychotherapy" OR DE "Gestalt Therapy" OR DE "Group Psychotherapy" OR DE "Guided Imagery" OR DE "Humanistic Psychotherapy" OR DE "Hypnotherapy" OR DE "Individual Psychotherapy" OR DE "Insight Therapy" OR DE "Integrative Psychotherapy" OR DE "Interpersonal Psychotherapy" OR DE "Logotherapy" OR DE "Narrative Therapy" OR DE "Network Therapy" OR DE "Persuasion Therapy" OR DE "Primal Therapy" OR DE "Psychoanalysis" OR DE "Psychodrama" OR DE "Psychodynamic Psychotherapy" OR DE "Psychotherapeutic Counseling" OR DE "Rational Emotive Behavior Therapy" OR DE "Reality Therapy" OR DE "Relationship Therapy" OR DE "Solution Focused Therapy" OR DE "Supportive Psychotherapy" OR DE "Transactional Analysis" OR DE Individualpsychologische Therapie" OR DE "Jugendlichenpsychotherapie" OR DE "Affirmative Therapie" OR DE "Analytische Psychotherapie (C. G. Jung)" OR DE "Autogenes Training" OR DE "Verhaltenstherapie" OR DE "Kurzpsychotherapie" OR DE "Beziehungsorientierte Kurzpsychotherapie" OR DE "Kinderpsychotherapie" OR DE "Klientenzentrierte Psychotherapie" OR DE "Kognitive Verhaltenstherapie" OR DE "Konversionstherapie (Homosexualität)" OR DE "Eklektische Psychotherapie" OR DE "Emotionsfokussierte Therapie" OR DE "Existenzialtherapie" OR DE "Erfahrungsorientierte Psychotherapie" OR DE "Expressive Psychotherapie" OR DE "Augenbewegungsdesensibilisierung" OR DE "Feministische Therapie" OR DE "Geriatrische Psychotherapie" OR DE "Gestalttherapie" OR DE "Gruppenpsychotherapie" OR DE "Geleitete Fantasievorstellung" OR DE "Humanistische Psychotherapie" OR DE "Hypnotherapie" OR DE "Einzelpsychotherapie" OR DE "Einsichtstherapie" OR DE "Integrative Psychotherapie" OR DE "Interpersonelle Psychotherapie" OR DE "Logotherapie" OR DE "Narrative Therapie" OR DE "Netzwerktherapie" OR DE "Persuasionstherapie" OR DE "Primärtherapie" OR DE "Psychoanalytische Therapie" OR DE "Psychodrama" OR DE "Psychodynamische Psychotherapie" OR DE "Psychotherapeutische Beratung" OR DE "Rational‐Emotive Verhaltenstherapie" OR DE "Realitätstherapie" OR DE "Relationship Therapy" OR DE "Lösungsorientierte Therapie" OR DE "Unterstützende Psychotherapie" OR DE "Transaktionsanalyse" 14 TI (psychotherap* OR psycho‐therap*) OR AB (psychotherap* OR psycho‐therap*) OR SU (psychotherap* OR psychotherap*) 15 TI (behav* N3 (intervention* OR program* OR therap*)) OR AB (behav* N3 (intervention* OR program* OR therap*)) 16 TI ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR AB ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR SU ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) 17 TI (psycho* N3 (intervention* OR program* OR therap*)) OR AB (psycho* N3 (intervention* OR program* OR therap*)) OR SU (psycho* N3 (intervention* OR program* OR therap*)) 18 TI relaxation OR AB relaxation OR SU relaxation 19 TI mindful* OR AB mindful* OR SU mindful* 20 TI (counsel?ing OR coaching) OR AB (counsel?ing OR coaching) OR SU (counsel?ing OR coaching) 21 TI ("third wave" N1 (psycho* OR therap*)) OR AB ("third wave" N1 (psycho* OR therap*)) OR SU ("third wave" N1 (psycho* OR therap*)) 22 TI "cognit* restructur*" OR AB "cognit* restructur*" OR SU "cognit* restructur*" 23 TI "positive psychology" OR AB "positive psychology" OR SU "positive psychology" 24 TI (refram* OR re‐fram* OR reapprais*) OR AB (refram* OR re‐fram* OR reapprais*) OR SU (refram* OR re‐fram* OR reapprais*) 25 TI (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR AB (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR SU (stress N1 (inoculation OR manag* OR reduc* OR resist*)) 26 TI (anxiety N3 manage*) OR AB (anxiety N3 manage*) OR SU (anxiety N3 manage*) 27 TI "acceptance and commitment" OR AB "acceptance and commitment" OR SU "acceptance and commitment" 28 TI (multimodal OR multi‐modal OR "combined modal*") OR AB (multimodal OR multi‐modal OR "combined modal*") OR SU (multimodal OR multi‐modal OR "combined modal*") 29 DE "Health Promotion" 30 TI (health N3 (educat* OR promot*)) OR AB (health N3 (educat* OR promot*)) OR SU (health N3 (educat* OR promot*)) 31 S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 32 S12 AND S31 33 TI (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR SU (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 34 TI (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR SU (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 35 S32 OR S33 OR S34 36 TI "randomi?ed control* trial*" OR AB "randomi?ed control* trial*" 37 TI "control* clinical trial*" OR AB "control* clinical trial*" 38 AB randomi?ed 39 AB placebo* 40 AB randomly 41 AB trial 42 S36 OR S37 OR S38 OR S39 OR S40 OR S41 43 S35 AND S42
Web of Science Core Collection (SCI, SSCI, CPCI‐S, CPCI‐SSH)
Searched 1990 to 2 November 2016 [2812 records]
# 19 #17 AND #16 Refined by: WEB OF SCIENCE CATEGORIES: ( PSYCHIATRY OR PUBLIC ENVIRONMENTAL OCCUPATIONAL HEALTH OR PSYCHOLOGY CLINICAL OR PSYCHOLOGY MULTIDISCIPLINARY OR PSYCHOLOGY OR PSYCHOLOGY DEVELOPMENTAL OR NURSING OR SOCIAL WORK OR EDUCATION EDUCATIONAL RESEARCH ) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 18 #17 AND #16 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 17 TS=(random* or trial* or assign* or control* or group* or placebo* or blind* or prospectiv* or longitudinal* or meta‐analys* or systematic review*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 16 #14 or #15 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 15 TS=((resilience or hardiness) near/3 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 14 #13 AND #6 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 13 #12 OR #11 OR #10 OR #9 OR #8 OR #7 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 12 TS=(health near/3 (educat* or promot*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 11 TS= ((multimodal* or "multi modal*" or "combined modal*") NEAR/3 (treat* or therap* or intervention* or program*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 10 TS=("acceptance and commitment") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 9 TS=((anxiety near/1 manag*) or relaxation or mindful* or counsel*ing or coaching or "third wave" or refram* or "re fram*" or "cognitive restructur*" or "positive psychology") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 8 TS=(stress near/3 (inoculat* or manag* or reduc* or resist*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 7TS=((psychotherap* or "psycho therap*") or CBT or mindful* or (behav* near/3 (intervention* or program* or therap*)) OR ((cognit* or "cognitive behavior*" or CBT) near/3 (intervention* or program* or therap*)) OR (psycho* near/3 (intervention* or program* or therap*))) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 6 #5 OR #4 OR #3 OR #2 OR #1 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 5 TS= ((withstand* or overcom* or resist* or recover* or thriv* or adapt* or adjust* or "bounc* back" ) near/1 (stress* or trauma* or advers*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 4 TS=(psychol* near/1 (adapt* or adjust*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 3 TS=(positiv* near/1 (adapt* or adjust*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 2 TS=("post traumatic growth" or "posttraumatic growth" or "stress related growth") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 # 1TS=(resilien* or hardiness*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016
International Bibliography of the Social Sciences ProQuest
Searched 3 November 2016 [593 records]
((MAINSUBJECT.EXACT("Coping") OR TI(resilien* OR hardiness) OR AB(resilien* OR hardiness)) OR (TI((psychol* OR social) NEAR/1 (adapt* OR adjust*)) OR AB((psychol* OR social) NEAR/1 (adapt* OR adjust*))) OR (TI(positiv* NEAR/1 (adapt* OR adjust*)) OR AB(positiv* NEAR/1 (adapt* OR adjust*))) OR (TI("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (TI(cope OR coping) OR AB(cope OR coping)) OR (TI((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") NEAR/5 (stress* OR trauma* OR adversit*)) OR AB((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") NEAR/5 (stress* OR trauma* OR adversit*)))) AND ((MAINSUBJECT.EXACT("Psychotherapy") OR MAINSUBJECT.EXACT("Cognitive therapy") OR MAINSUBJECT.EXACT("Group therapy") OR TI(psychotherap* OR psycho‐therap*) OR AB(psychotherap* OR psycho‐therap*) OR TI(behav* NEAR/3 (intervention* OR program* OR therap*)) OR AB(behav* NEAR/3 (intervention* OR program* OR therap*)) OR TI(cognit* OR "cognitive behavior*" OR CBT) OR AB(cognit* OR "cognitive behavior*" OR CBT) OR TI(psycho* NEAR/3 (intervention* OR program* OR therap*)) OR AB(psycho* NEAR/3 (intervention* OR program* OR therap*)) OR TI(relaxation OR mindful* OR counsel?ing OR coaching OR "third wave") OR AB(relaxation OR mindful* OR counsel?ing OR coaching OR "third wave") OR TI(cognit* NEAR/1 restructur*) OR AB(cognit* NEAR/1 restructur*) OR TI("positive psychology") OR AB("positive psychology")) AND yr(1960‐2019)) AND (MAINSUBJECT.EXACT("Clinical trials") OR (TI(control* OR group OR random* OR placebo* OR longitudinal OR prospective* OR blind* OR trial*) OR AB(control* OR group OR random* OR placebo* OR longitudinal OR prospective* OR blind* OR trial*))) Limited to 1990 to 2016
Applied Social Sciences Index & Abstracts ProQuest
Searched 28 October 2016 [634 records]
1 SU.EXACT("Resilience") 2 SU.EXACT("Hardiness") 3 SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment") 4 SU.EXACT("Adaptation") 5 ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") 6 ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) 7 ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) 8 ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) 9 ti(cope OR coping) OR ab(cope OR coping) 10 ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) 11 SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress") 12 SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") ) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress") 13 SU.EXACT("Psychotherapy") 14 ti((psychotherap* OR psychotherap*)) OR ab((psychotherap* OR psychotherap*)) 15 ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) 16 ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) 17 ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*))) 18 ti(relaxation) OR ab(relaxation) 19 ti(mindful*) OR ab(mindful*) 20 ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) 21 ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1 (psycho* OR therap*))) 22 ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) 23 ti(("positive psychology")) OR ab(("positive psychology")) 24 ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) 25 ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) 26 ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) 27 ti("acceptance and commitment") OR ab("acceptance and commitment") 28 ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) 29 SU.EXACT("Health promotion" OR "Mental health promotion") 30 ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) 31 SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation)) OR (ti(mindful*) OR ab(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1 (psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*)))) 32 (SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") ) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation)) OR (ti(mindful*) OR ab(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1 (psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))))) 33 ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 34 ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 35 (SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") ) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation)) OR (ti(mindful*) OR ab(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1 (psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 36 ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*) 37 ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*) 38 ti(randomi?ed) OR ab(randomi?ed) 39 ti(placebo*) OR ab(placebo*) 40 ti(randomly) OR ab(randomly) 41 ti(trial) OR ab(trial) 42 (ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)) 43 ((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") ) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation)) OR (ti(mindful*) OR ab(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1 (psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial))) 44 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") ) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation)) OR (ti(mindful*) OR ab(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1 (psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial))) AND pd(19900101‐20161231)
ProQuest Dissertations & Theses ProQuest
Searched 28 October 2016 [989 records]
1 SU.EXACT("Resilience") 2 SU.EXACT("Hardiness") 3 SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment") 4 SU.EXACT("Adaptation") 5 ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR diskw("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") 6 ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) OR diskw((positiv* N/1 (adapt* OR adjust*))) 7 ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) OR diskw((psychol* N/1 (adapt* OR adjust*))) 8 ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) OR diskw(resilien* OR hardiness*) 9 ti(cope OR coping) OR ab(cope OR coping) OR diskw(cope OR coping) 10 ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR diskw((withstand* OR overcom* OR resist* OR recover* OR OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) 11 SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress") 12 SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR diskw("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) OR diskw((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) OR diskw((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) OR diskw(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping) OR diskw(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR diskw((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress") 13 SU.EXACT("Psychotherapy") 14 ti((psychotherap* OR psychotherap*)) OR ab((psychotherap* OR psychotherap*)) 15 ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) OR diskw((behav* N/3 (intervention* OR program* OR therap*))) 16 ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR diskw(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) 17 ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 intervention* OR program* OR therap*))) OR diskw((psycho* N/3 (intervention* OR program* OR therap*))) 18 ti(relaxation) OR ab(relaxation) OR diskw(relaxation) 19 ti(mindful*) OR ab(mindful*) OR diskw(mindful*) 20 ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) OR diskw(counsel?ing OR coaching 21 ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1(psycho* OR therap*))) OR diskw(("third wave" N/1(psycho* OR therap*))) 22 ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) OR diskw((cognit* N/1 restructur*)) 23 ti(("positive psychology")) OR ab(("positive psychology")) OR diskw(("positive psychology")) 24 ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) OR diskw((refram* OR re‐fram* OR reapprais*)) 25 ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR diskw((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) 26 ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) OR diskw((anxiety N/3 manage*)) 27 ti("acceptance and commitment") OR ab("acceptance and commitment") OR diskw("acceptance and commitment") 28 ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) OR diskw((multimodal OR multimodal OR "combined modal*")) 29 SU.EXACT("Health promotion" OR "Mental health promotion") 30 ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) OR diskw((health N/3 (educat* OR promot*))) 31 SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) OR diskw((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR diskw(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*))) OR diskw((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation) OR diskw(relaxation)) OR (ti(mindful*) OR ab(mindful*) OR diskw(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) OR diskw(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1(psycho* OR therap*))) OR diskw(("third wave" N/1(psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) OR diskw((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology")) OR diskw(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) OR diskw((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR diskw((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) OR diskw((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment") OR diskw("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) OR diskw((multimodal OR multimodal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) OR diskw((health N/3 (educat* OR promot*)))) 32 (SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR diskw("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) OR diskw((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) OR diskw((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) OR diskw(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping) OR diskw(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR diskw((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) OR diskw((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR diskw(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*))) OR diskw((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation) OR diskw(relaxation)) OR (ti(mindful*) OR ab(mindful*) OR diskw(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) OR diskw(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1(psycho* OR therap*))) OR diskw(("third wave" N/1(psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) OR diskw((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology")) OR diskw(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) OR diskw((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR diskw((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) OR diskw((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment") OR diskw("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) OR diskw((multimodal OR multimodal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) OR diskw((health N/3 (educat* OR promot*))))) 33 ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 34 ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 35 (SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR diskw("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) OR diskw((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) OR diskw((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) OR diskw(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping) OR diskw(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR diskw((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) OR diskw((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR diskw(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*))) OR diskw((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation) OR diskw(relaxation)) OR (ti(mindful*) OR ab(mindful*) OR diskw(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) OR diskw(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1(psycho* OR therap*))) OR diskw(("third wave" N/1(psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) OR diskw((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology")) OR diskw(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) OR diskw((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR diskw((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) OR diskw((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment") OR diskw("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) OR diskw((multimodal OR multimodal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) OR diskw((health N/3 (educat* OR promot*))))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 36 ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*) 37 ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*) 38 ti(randomi?ed) OR ab(randomi?ed) 39 ti(placebo*) OR ab(placebo*) 40 ti(randomly) OR ab(randomly) 41 ti(trial) OR ab(trial) 42 (ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)) 43 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR diskw("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) OR diskw((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) OR diskw((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) OR diskw(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping) OR diskw(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR diskw((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) OR diskw((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR diskw(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*))) OR diskw((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation) OR diskw(relaxation)) OR (ti(mindful*) OR ab(mindful*) OR diskw(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) OR diskw(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1(psycho* OR therap*))) OR diskw(("third wave" N/1(psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) OR diskw((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology")) OR diskw(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) OR diskw((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR diskw((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) OR diskw((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment") OR diskw("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) OR diskw((multimodal OR multimodal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) OR diskw((health N/3 (educat* OR promot*))))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial))) 44 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (SU.EXACT("Social adjustment") OR SU.EXACT("Psychosocial adjustment")) OR SU.EXACT("Adaptation") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR diskw("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti((positiv* N/1 (adapt* OR adjust*))) OR ab((positiv* N/1 (adapt* OR adjust*))) OR diskw((positiv* N/1 (adapt* OR adjust*)))) OR (ti((psychol* N/1 (adapt* OR adjust*))) OR ab((psychol* N/1 (adapt* OR adjust*))) OR diskw((psychol* N/1 (adapt* OR adjust*)))) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) OR diskw(resilien* OR hardiness*)) OR (ti(cope OR coping) OR ab(cope OR coping) OR diskw(cope OR coping)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR diskw((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) OR SU.EXACT("Anticipatory stress" OR "behavioural stress" OR "Burnout" OR "Critical incident stress" OR "Daily stress" OR "Economic stress" OR "Family stress" OR "Life stress" OR "Marital stress" OR "Maternal stress" OR "Nervous breakdown" OR "Occupational stress" OR "Parental stress" OR "Postnatal stress" OR "Role stress" OR "School stress" OR "Secondary stressors" OR "Social stress" OR "Stress" OR "Traumatic stress")) AND (SU.EXACT("Psychotherapy") OR (ti((psychotherap* OR psycho‐therap*)) OR ab((psychotherap* OR psychotherap*))) OR (ti((behav* N/3 (intervention* OR program* OR therap*))) OR ab((behav* N/3 (intervention* OR program* OR therap*))) OR diskw((behav* N/3 (intervention* OR program* OR therap*)))) OR (ti(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR ab(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*))) OR diskw(((cognit* OR "cognitive behavior*" OR CBT) N/3 (intervention* OR program* OR therap*)))) OR (ti((psycho* N/3 (intervention* OR program* OR therap*))) OR ab((psycho* N/3 (intervention* OR program* OR therap*))) OR diskw((psycho* N/3 (intervention* OR program* OR therap*)))) OR (ti(relaxation) OR ab(relaxation) OR diskw(relaxation)) OR (ti(mindful*) OR ab(mindful*) OR diskw(mindful*)) OR (ti(counsel?ing OR coaching) OR ab(counsel?ing OR coaching) OR diskw(counsel?ing OR coaching)) OR (ti(("third wave" N/1 (psycho* OR therap*))) OR ab(("third wave" N/1(psycho* OR therap*))) OR diskw(("third wave" N/1(psycho* OR therap*)))) OR (ti((cognit* N/1 restructur*)) OR ab((cognit* N/1 restructur*)) OR diskw((cognit* N/1 restructur*))) OR (ti(("positive psychology")) OR ab(("positive psychology")) OR diskw(("positive psychology"))) OR (ti((refram* OR re‐fram* OR reapprais*)) OR ab((refram* OR re‐fram* OR reapprais*)) OR diskw((refram* OR re‐fram* OR reapprais*))) OR (ti((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR ab((stress N/1 (inoculation OR manag* OR reduc* OR resist*))) OR diskw((stress N/1 (inoculation OR manag* OR reduc* OR resist*)))) OR (ti((anxiety N/3 manage*)) OR ab((anxiety N/3 manage*)) OR diskw((anxiety N/3 manage*))) OR (ti("acceptance and commitment") OR ab("acceptance and commitment") OR diskw("acceptance and commitment")) OR (ti((multimodal OR multi‐modal OR "combined modal*")) OR ab((multimodal OR multi‐modal OR "combined modal*")) OR diskw((multimodal OR multimodal OR "combined modal*"))) OR SU.EXACT("Health promotion" OR "Mental health promotion") OR (ti((health N/3 (educat* OR promot*))) OR ab((health N/3 (educat* OR promot*))) OR diskw((health N/3 (educat* OR promot*))))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ab((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR diskw((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial))) AND pd(19900101‐20161231)
Cochrane Database of Systematic Reviews (CDSR), part of the Cochrane Library
Searched 27 October 2016 [57 records]
#1(resilien* or hardiness*):ti,ab #2(post next traumatic growth or posttraumatic growth or stress next related growth) #3(positiv* near/1 (adapt* or adjust*)):ti,ab #4(psychol* near/1 (adapt* or adjust*)):ti,ab #5{or #1‐#4} #6(behav* or psycho* or cbt or cognit* or mindful* or reframe* or re next fram*):ti,ab #7(stress near/3 (inoculat* or manag* or reduc* or resist*)):ti,ab #8(anxiety near/3 manag*):ti,ab #9"acceptance and commitment":ti,ab #10(multimodal* or multi next modal* or combined next modal*):ti,ab #11(health near/3 (educat* or promot*)):ti,ab #12{or #6‐#11} Publication Year from 1990 to 2016, in Cochrane Reviews (Reviews and Protocols) #13#5 and #12
Database of Abstracts of Reviews of Effects (DARE), part of the Cochrane Library
Searched 27 October 2016 [3 records]
#1(resilien* or hardiness*):ti,ab #2(post next traumatic growth or posttraumatic growth or stress next related growth) #3(positiv* near/1 (adapt* or adjust*)):ti,ab #4(psychol* near/1 (adapt* or adjust*)):ti,ab #5{or #1‐#4} #6(behav* or psycho* or cbt or cognit* or mindful* or reframe* or re next fram*):ti,ab #7(stress near/3 (inoculat* or manag* or reduc* or resist*)):ti,ab #8(anxiety near/3 manag*):ti,ab #9"acceptance and commitment":ti,ab #10(multimodal* or multi next modal* or combined next modal*):ti,ab #11(health near/3 (educat* or promot*)):ti,ab #12{or #6‐#11} Publication Year from 1990 to 2016, in Other Reviews #13#5 and #12
Epistemonikos (www.epistemonikos.org)
Searched 28 October 2016 [173 records]
1 (title:(resilien* OR hardiness*) OR abstract:(resilien* OR hardiness*)) 2 (title:("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR abstract:("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) 3 (title:("positive adaptation" OR "positive adjustment") OR abstract:("positive adaptation" OR "positive adjustment")) 4 (title:("psychological adaptation" OR "psychological adjustment") OR abstract:("psychological adaptation" OR "psychological adjustment")) 5 OR/#1‐#4 6 #5; Publication year (Custom year range): 1990 – 2016; Publication type: Systematic Review; Systematic review question: All; Cochrane review: All; Type of meta‐analysis: All
ERIC EBSCOhost
Searched 28 October 2016 [206 records]
1 DE "Resilience (Psychology)" 2 DE "Social Adjustment" OR DE "Emotional Adjustment" 3 TI ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") 4 TI (positiv* N1 (adapt* OR adjust*)) OR AB (positiv* N1 (adapt* OR adjust*)) 5 TI (psychol* N1 (adapt* OR adjust*)) OR AB (psychol* N1 (adapt* OR adjust*)) 6 TI (resilien* OR hardiness*) OR AB (resilien* OR hardiness*) OR SU (resilien* 7 TI (cope OR coping) OR AB (cope OR coping) OR SU (cope OR coping) 8 TI ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR AB ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) 9 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 10 DE "Psychotherapy" OR DE "Milieu Therapy" OR DE "Relaxation Training" 11 TI (psychotherap* OR psychotherap*) OR AB (psychotherap* OR psychotherap*) OR SU (psychotherap* OR psychotherap*) 12 TI (behav* N3 (intervention* OR program* OR therap*)) OR AB (behav* N3 (intervention* OR program* OR therap*)) 13 TI ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR AB ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) 14 TI (psycho* N3 (intervention* OR program* OR therap*)) OR AB (psycho* N3 (intervention* OR program* OR therap*)) 15 TI relaxation OR AB relaxation OR SU relaxation 16 TI mindful* OR AB mindful* 17 TI (counsel?ing OR coaching) OR AB (counsel?ing OR coaching) OR SU (counsel?ing OR coaching) 18 TI ("third wave" N1 (psycho* OR therap*)) OR AB ("third wave" N1 (psycho* OR therap*)) 19 TI "cognit* restructur*" OR AB "cognit* restructur*" OR SU "cognit* restructur*" 20 TI "positive psychology" OR AB "positive psychology" 21 TI (refram* OR refram* OR reapprais*) OR AB (refram* OR refram* OR reapprais*) 22 TI (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR AB (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR SU (stress N1 (inoculation OR manag* OR reduc* OR resist*)) 23 TI (anxiety N3 manage*) OR AB (anxiety N3 manage*) 24 TI "acceptance and commitment" OR AB "acceptance and commitment" 25 TI (multimodal OR multimodal OR "combined modal*") OR AB (multimodal OR multimodal OR "combined modal*") 26 TI (health N3 (educat* OR promot*)) OR AB (health N3 (educat* OR promot*)) OR SU (health N3 (educat* OR promot*)) 27 S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 28 S9 AND S27 29 TI (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 30 TI (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 31 S28 OR S29 OR S30 32 TI "randomi?ed control* trial*" OR AB "randomi? ed control* trial*" 33 TI "control* clinical trial*" OR AB "control* clinical trial*" 34 AB randomi?ed 35 AB placebo* 36 AB randomly 37 AB trial 38 S32 OR S33 OR S34 OR S35 OR S36 OR S37 39 S31 AND S38 40 S31 AND S38, Limiters Date Published:1990010120161031
Current Controlled Trials (ISRCTN registry; www.isrctn.com)
Searched 24 November 2016 [47 records]
Text search: (((resilience OR hardiness OR "posttraumatic growth" OR stress OR trauma) AND (psychotherap OR relaxation OR mindfulness OR coaching OR "positive psychology" OR reappraisal OR "stress inoculation" OR "stress management" OR multimodal OR "health promotion")) OR ((resilience OR hardiness) AND (training OR program OR intervention OR promot OR prevent OR enhanc OR learn OR teach OR educat OR increas or develop OR manag OR therap OR protocol OR treat)))
ClinicalTrials.gov (clinicaltrials.gov)
Searched 24 November 2016 [675 records]
title = resilience OR hardiness OR posttraumatic growth OR stress OR trauma condition = resilience OR hardiness OR posttraumatic growth OR stress OR trauma intervention = resilience training OR hardiness training OR psychotherapy OR relaxation OR mindfulness OR coaching OR positive psychology OR reappraisal OR stress inoculation OR stress management OR multimodal OR health promotion Limitation: 01/01/1990 – 03/11/2016
WHO ICTRP (apps.who.int/trialsearch)
Searched 24 November 2016 [879 records]
title = resilience OR hardiness OR posttraumatic growth OR stress OR trauma condition = resilience OR hardiness OR posttraumatic growth OR stress OR trauma intervention = resilience training OR hardiness training OR psychotherapy OR relaxation OR mindfulness OR coaching OR positive psychology OR reappraisal OR stress inoculation OR stress management OR multimodal OR health promotion Recruitment status: ALL Limitation: 01/01/1990 – 03/11/2016
Appendix 9. Search strategies 2016 onwards
Cochrane Central Register of Controlled Trials (CENTRAL), in the Cochrane Library
Searched 26 June 2019 [218 records]
#1[mh "Resilience, Psychological"] #2[mh "social adjustment"] #3[mh "Adaptation, Psychological"] #4("post‐traumatic growth" or "posttraumatic growth" or "stress‐related growth") #5(positiv* near/1 (adapt* or adjust*)) #6(psychol* near/1 (adapt* or adjust*)) #7(resilien* or hardiness*) #8(cope or coping) #9((withstand* or overcom* or resist* or recover* or thriv* or adapt* or adjust* or bounc* back) near/5 (stress* or trauma* or adversit*)) #10{or #1‐#9} #11[mh psychotherapy] #12MeSH descriptor: [Stress, Psychological] this term only and with qualifier(s): [therapy ‐ TH] #13(psychotherap* or psycho next therap*) #14(behav* near/3 (intervention* or program* or therap*)) #15((cognit* or cognitive next behavior* or CBT) near/3 (intervention* or program* or therap*)) #16(psycho* near/3 (intervention* or program* or therap*)) #17relaxation #18mindful* #19(counsel*ing or coaching) #20(third next wave next (psycho* or therap*)) #21cognit* next restructur* #22positive next psychology #23(refram* or re next fram* or reapprais*) #24(stress near/1 (inoculation or manag* or reduc* or resist*)) #25(anxiety near/3 manage*) #26"acceptance and commitment" #27[mh "Combined Modality Therapy"] #28(multimodal* or multi next modal* or combined modal*) #29[mh "Health promotion"] #30(health near/3 (educat* or promot*)) #31{or #11‐#30} #32MeSH descriptor: [Health Personnel] explode all trees #33(health* NEAR/3 (personnel or profession* or worker* or practitioner* or provider* or staff)) #34(medical NEAR/3 (personnel or profession* or worker* or practitioner* or provider* or staff)) #35(care* NEAR/1 (personnel or profession* or worker* or practitioner* or provider* or staff)) #36(doctor* or physician* or general practitioner* or ("primary care" NEAR/2 practitioner*) or surgeon*) #37(nurse* or nursing) #38((hospital or ambulance) NEAR/1 (staff or personnel)) #39((intensive NEAR/2 care) or ICU) #40((allied NEXT health*) NEAR/2 (personnel* or profession* or worker* or practitioner* or provider* or staff)) #41(psychologist* or psychotherapist* or psychiatrist* or mental NEXT health NEXT clinician* or mental NEXT health NEXT profession* or mental NEXT health NEXT worker* or social NEXT worker*) #42(paramedic* or para NEXT medic* or ambulance ) #43(first or emergency or disaster) NEAR/1 (response or responder*) #44(professional NEAR/1 (caregiver* or care‐giver*)) #45(anesthetist* or anaesthetist* or audiologist* or dental NEXT hygienist* or dentist* or dietitian* or midwi*e* or nutritionist* or pathologist* or physiologist* or physiotherapist* or therapist or osteopath* or sonographer* or radiographer* or radiotherapist* or ((radiology or radiation) NEAR/1 ( technician* or technologist* or assistant* or scientist*)) or ((anesthesia or anesthesiologist) NEAR/1 (technician* or assistant*)) or (surgical NEAR/1 (technician* or technologist*)) or orthotist* or orthoptist* or podiatrist* or perfusionist*) #46(counsellor* or counselor*) #47((clinical or medical*) NEAR/1 (technician* or technologist* or assistant* or scientist*)) #48(public NEXT health NEXT service* or public NEXT health NEXT agenc*) #49(secondary NEXT trauma* or (work* NEAR/2 trauma NEXT survivor*)) #50((nursing or medical or midwifery or premedical or paramedic or psychology or physical NEXT therapy or occupational NEXT therapy) NEAR/2 student*) #51college NEXT student* #52{OR #32 ‐#51} #53#10 and #31 with Publication Year from 1990 to 2016, in Trials [ Note: Final line 2016] #54#10 and #31 AND #52 with Publication Year from 2016 to 2019, in Trials [ Note: Final line 2019]
MEDLINE Ovid
Searched 25 June 2019 [725 records]
1 Resilience, Psychological/ 2 social adjustment/ 3 Adaptation, Psychological/ 4 (post‐traumatic growth or posttraumatic growth or stress‐related growth).tw,kf. 5 (positiv$ adj1 (adapt$ or adjust$)).tw,kf. 6 (psychol$ adj1 (adapt$ or adjust$)).tw,kf. 7 (resilien$ or hardiness$).tw,kf. 8 (cope or coping).tw,kf. 9 ((withstand$ or overcom$ or resist$ or recover$ or thriv$ or adapt$ or adjust$ or bounc$ back) adj5 (stress$ or trauma$ or adversit$)).tw,kf. 10 or/1‐9 11 exp psychotherapy/ 12 Stress, Psychological/th 13 (psychotherap$ or psycho‐therap$).tw,kf. 14 (behav$ adj3 (intervention$ or program$ or therap$)).tw,kf. 15 ((cognit$ or cognitive behavior$ or CBT) adj3 (intervention$ or program$ or therap$)).tw,kf. 16 (psycho$ adj3 (intervention$ or program$ or therap$)).tw,kf. 17 relaxation.tw,kf. 18 mindful$.tw,kf. 19 (counsel?ing or coaching).tw,kf. 20 (third wave adj (psycho$ or therap$)).tw,kf. 21 cognit$ restructur$.tw,kf. 22 positive psychology.tw,kf. 23 (refram$ or re‐fram$ or reapprais$).tw,kf. 24 (stress adj1 (inoculation or manag$ or reduc$ or resist$)).tw,kf. 25 (anxiety adj3 manage$).tw,kf. 26 "acceptance and commitment ".tw,kf. 27 Combined Modality Therapy/ 28 (multimodal or multi‐modal or combined modal$).tw,kf. 29 exp Health promotion/ 30 (health adj3 (educat$ or promot$)).tw,kf. 31 or/11‐30 32 10 and 31 33 (resilien$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kf. 34 (hardiness$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kf. 35 or/32‐34 36 randomized controlled trial.pt. 37 controlled clinical trial.pt. 38 randomi#ed.ab. 39 placebo$.ab. 40 drug therapy.fs. 41 randomly.ab. 42 trial.ab. 43 groups.ab. 44 or/36‐43 45 exp animals/ not humans.sh. 46 44 not 45 47 35 and 46 48 Health personnel/ 49 (health$ adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw,kf. 50 ((medical care adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)) or (medical adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff))).tw,kf. 51 (care adj1 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw,kf. 52 (doctor$ or physician$ or general practitioner$ or (primary care adj2 practitioner$) or surgeon$).tw,kf. 53 (nurse$ or (nursing adj3 assistant$) or (nursing adj3 staff)).tw,kf. 54 nursing.tw,kf. 55 ((hospital or ambulance) adj1 personnel).tw,kf. 56 ((intensive adj2 care) or ICU or (intensive adj2 care adj2 unit adj3 personnel$)).tw,kf. 57 ((allied health$) adj2 (personnel or profession$ or worker$ or practitioner* or provider$ or staff)).tw,kf. 58 (psychologist$ or psychotherapist$ or psychiatrist$ or (mental health adj2 clinician$) or (mental health adj2 profession$) or (mental health adj2 worker$)).tw,kf. 59 (social worker$).tw,kf. 60 (paramedic$ or ambulance or medic$ or ((first or emergency or disaster) adj1 (response or responder$))).tw,kf. 61 (professional adj1 (caregiver$ or care‐giver$)).tw,kf. 62 ((physical therapist$) or physiotherapist$ or occupational therapist$ or recreational therapist$ or music therapist$ or art therapist$ or dietitian$ or nutritionist$ or ((speech and language) adj1 therapist$) or speech pathologist$ or audiologist$ or exercise physiologist$ or osteopath$ or sonographer$ or radiographer$ or radiotherapist$ or ((radiology or radiation) adj1 (therapist$ or technician$ or technologist$ or assistant$ or scientist$)) or respiratory therapist$ or ((anesthesia or anesthesiologist) adj1 (technician$ or assistant$)) or dental hygienist$ or (surgical adj1 (technician$ or technologist$)) or orthotist$ or orthoptist$ or podiatrist$ or perfusionist$).tw,kf. 63 counsel?or$.tw,kf. 64 ((clinical or clinical laboratory or medical$ or medical$ laboratory) adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw,kf. 65 ((human or health) adj1 service adj3 profession$).tw,kf. 66 (public health adj2 (service or agency)).tw,kf. 67 (secondary traumati?ation or (work$ adj2 (trauma survivor$))).tw,kf. 68 ((nursing or medical or premedical or paramedic or psychology or physical therapy or occupational therapy) adj2 student$).tw,kf. 69 (college adj2 student$).tw,kf. 70 ((nurs$ adj1 (graduate$ or education)) or (medic$ adj1 train$) or (student adj1 nurse$)).tw,kf. 71 or/48‐70 72 47 and 71 73 limit 72 to yr="1990 ‐Current" 74 limit 73 to yr="2016 ‐Current"
Embase Ovid
Searched 25 June 2019 [991 records]
1 exp coping behavior/ 2 psychological adjustment/ 3 Psychological resilience/ [Annotation: New Emtree term in 2017] 4 social adaptation/ 5 "personal resource"/ 6 (post‐traumatic growth or posttraumatic growth or stress‐related growth).tw,kw. 7 (positiv$ adj1 (adapt$ or adjust$)).tw,kw. 8 (psychol$ adj1 (adapt$ or adjust$)).tw,kw. 9 (resilien$ or hardiness$).tw,kw. 10 (cope or coping).tw,kw. 11 ((withstand$ or overcom$ or resist$ or recover$ or thriv$ or adapt$ or adjust$ or bounc$ back) adj5 (stress$ or trauma$ or advers$)).tw,kw. 12 or/1‐11 13 exp psychotherapy/ 14 posttraumatic stress disorder/th [Therapy] 15 mental stress/th [Therapy] 16 (psychotherap$ or psycho‐therap$).tw,kw. 17 (behav$ adj3 (intervention$ or program$ or therap$)).tw,kw. 18 ((cognit$ or cognitive behavior$ or CBT) adj3 (intervention$ or program$ or therap$)).tw,kw. 19 (psycho$ adj3 (intervention$ or program$ or therap$)).tw,kw. 20 mindful$.tw,kw. 21 exp counseling/ 22 (counsel?ing or coaching).tw,kw. 23 mindfulness/ 24 mindful$.tw,kw. 25 (third wave adj (psycho$ or therap$)).tw,kw. 26 cognit$ restructur$.tw,kw. 27 positive psychology.tw,kw. 28 (refram$ or re‐fram$ or reapprais$).tw,kw. 29 (stress adj1 (inoculation or manag$ or reduc$ or resist$)).tw,kw. 30 (anxiety adj3 manage$).tw,kw. 31 "acceptance and commitment ".tw,kw. 32 (multimodal$ or multi‐modal$ or combined modal$).tw,kw. 33 exp health promotion/ 34 (health adj3 (educat$ or promot$)).tw,kw. 35 or/13‐34 36 12 and 35 37 (resilien$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kw. 38 (hardiness$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw,kw. 39 or/36‐38 40 exp health care personnel/ 41 (health$ adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw,kw. 42 (medical adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw,kw. 43 (care adj1 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw,kw. 44 (doctor$ or physician$ or general practitioner$ or (primary care adj2 practitioner$) or surgeon$).tw,kw. 45 (nurse$1 or nursing).tw,kw. 46 ((hospital or ambulance) adj1 personnel).tw,kw. 47 ((intensive adj2 care) or ICU).tw,kw. 48 (allied health$ adj2 (personnel$ or profession$ or worker$ or practitioner$ or provider$ or staff)).tw,kw. 49 (psychologist$ or psychotherapist$ or psychiatrist$ or mental health clinician$ or mental health profession$ or mental health worker$).tw,kw. 50 social worker$.tw,kw. 51 (paramedic$ or ambulance or medic$).tw,kw. 52 ((first or emergency or disaster) adj1 (response or responder$)).tw,kw. 53 (professional adj (caregiver$ or care‐giver$)).tw,kw. 54 (physical therapist$ or physiotherapist$ or occupational therapist$ or recreational therapist$ or music therapist$ or art therapist$ or dietitian$ or nutritionist$ or ((speech and language) adj1 therapist$) or speech pathologist$ or audiologist$ or exercise physiologist$ or osteopath$ or sonographer$ or radiographer$ or radiotherapist$ or ((radiology or radiation) adj1 (therapist$ or technician$ or technologist$ or assistant$ or scientist$)) or respiratory therapist$ or ((anesthesia or anesthesiologist) adj1 (technician$ or assistant$)) or dental hygienist$ or (surgical adj1 (technician$ or technologist$)) or orthotist$ or orthoptist$ or podiatrist$ or perfusionist$).tw,kw. 55 counsel?or$.tw,kw. 56 (clinical adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw,kw. 57 (clinical laboratory adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw,kw. 58 (medical$ adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw,kw. 59 (medical$ laboratory adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw,kw. 60 (public health service$ or public health agenc$).tw,kw. 61 (secondary traumati?ation or (work$ adj2 trauma survivor$)).tw,kw. 62 ((nursing or medical or premedical or paramedic or psychology or physical therapy or occupational therapy) adj2 student$).tw,kw. 63 college student$.tw,kw. 64 ((nurs$ adj1 graduate$) or (nurs$ adj1 education) or (medic$ adj1 train$)).tw,kw. 65 or/40‐64 66 39 and 65 67 Randomized controlled trial/ 68 controlled clinical trial/ 69 Single blind procedure/ 70 Double blind procedure/ 71 triple blind procedure/ 72 Crossover procedure/ 73 (crossover or cross‐over).tw. 74 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 75 Placebo/ 76 placebo.tw. 77 prospective.tw. 78 factorial$.tw. 79 random$.tw. 80 assign$.ab. 81 allocat$.tw. 82 volunteer$.ab. 83 or/67‐82 84 66 and 83 85 limit 84 to yr="2016 ‐Current"
PsycINFO Ovid
Searched 26 June 2019 [454 records]
All years searched in 2019 to correct for possible error in the 2016 search
1 "resilience (psychological)"/ 2 "adaptability (personality)"/ 3 emotional adjustment/ 4 coping behavior/ 5 posttraumatic growth/ 6 protective factors/ 7 (post‐traumatic growth or posttraumatic growth or stress‐related growth).tw. 8 (positiv$ adj1 (adapt$ or adjust$)).tw. 9 (psychol$ adj1 (adapt$ or adjust$)).tw. 10 (resilien$ or hardiness$).tw. 11 (cope or coping).tw. 12 ((withstand$ or overcom$ or resist$ or recover$ or thriv$ or adapt$ or adjust$ or bounc$ back) adj3 (stress$ or trauma$ or advers$)).tw. 13 or/1‐12 14 exp psychotherapy/ ) 15 exp cognitive techniques/ 16 psychotherapeutic techniques/ 17 relaxation therapy/ 18 mindfulness/ 19 stress management/ 20 (psychotherap$ or psycho‐therap$).tw. 21 (behav$ adj3 (intervention$ or program$ or therap$)).tw. 22 ((cognit$ or cognitive behavior$ or CBT) adj3 (intervention$ or program$ or therap$)).tw. 23 (psycho$ adj3 (intervention$ or program$ or therap$)).tw. 24 relaxation.tw. 25 mindful$.tw. 26 (counsel?ing or coaching).tw. 27 (third wave adj (psycho$ or therap$)).tw. 28 cognit$ restructur$.tw. 29 positive psychology.tw. 30 (refram$ or re‐fram$ or reapprais$).tw. 31 (stress adj1 (inoculation or manag$ or reduc$ or resist$)).tw. 32 (anxiety adj3 manage$).tw. 33 "acceptance and commitment".tw. 34 multimodal treatment approach/ 35 (multimodal$ or multi‐modal$ or combined modal$).tw. 36 health promotion/ 37 (health adj3 (educat$ or promot$)).tw. 38 or/14‐37 39 13 and 38 40 (resilien$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw. 41 (hardiness$ adj5 (train$ or program$ or intervention$ or promot$ or prevent$ or enhanc$ or learn$ or teach$ or educat$ or increas$ or develop$ or manag$ or therap$ or protocol$ or treat$)).tw. 42 or/39‐41 43 exp health personnel/ 44 exp therapists/ 45 exp clinicians/ 46 exp counselors/ 47 home care personnel/ 48 professional measures/ 49 rescue workers/ 50 exp social workers/ 51 (health$ adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw. 52 (medical adj3 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw. 53 (care adj1 (personnel or profession$ or worker$ or practitioner$ or provider$ or staff)).tw. 54 (doctor$ or physician$ or general practitioner$ or (primary care adj2 practitioner$) or surgeon$).tw. 55 (nurse$1 or nursing).tw. 56 ((hospital or ambulance) adj1 personnel).tw. 57 ((intensive adj2 care) or ICU).tw. 58 (allied health$ adj2 (personnel$ or profession$ or worker$ or practitioner$ or provider$ or staff)).tw. 59 (psychologist$ or psychotherapist$ or psychiatrist$ or mental health clinician$ or mental health profession$ or mental health worker$).tw. 60 social worker$.tw. 61 (paramedic$ or ambulance or medic$).tw. 62 ((first or emergency or disaster) adj1 (response or responder$)).tw. 63 (professional adj (carer$ or caregiver$ or care‐giver$)).tw. 64 (physical therapist$ or physiotherapist$ or occupational therapist$ or recreational therapist$ or music therapist$ or art therapist$ or dietitian$ or nutritionist$ or ((speech and language) adj1 therapist$) or speech pathologist$ or audiologist$ or exercise physiologist$ or midwi?e$ or osteopath$ or sonographer$ or radiographer$ or radiotherapist$ or ((radiology or radiation) adj1 (therapist$ or technician$ or technologist$ or assistant$ or scientist$)) or respiratory therapist$ or ((anesthesia or anesthesiologist) adj1 (technician$ or assistant$)) or dental hygienist$ or (surgical adj1 (technician$ or technologist$)) or orthotist$ or orthoptist$ or podiatrist$ or perfusionist$).tw. 65 counsel?or$.tw. 66 (clinical adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw. 67 (clinical laboratory adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw. 68 (medical$ adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw. 69 (medical$ laboratory adj1 (technician$ or technologist$ or assistant$ or scientist$)).tw. 70 (public health service$ or public health agenc$).tw. 71 (secondary trauma$ or (work$ adj2 trauma survivor$)).tw. 72 ((nursing or medical or premedical or paramedic or psychology or physical therapy or occupational therapy) adj2 student$).tw. 73 ((nursing or medical or midwifery or premedical or paramedic or psychology or physical therapy or occupational therapy) adj2 student$).tw. 74 college student$.tw. (154347) 75 ((nurs$ adj1 graduate$) or (nurs$ adj1 education) or (medic$ adj1 train$)).tw. (7743) 76 or/43‐75 77 42 and 76 78 clinical trials/ 79 longitudinal studies/ 80 exp program evaluation/ 81 treatment effectiveness evaluation/ 82 random$.tw. 83 (allocat$ or assign$).tw. 84 ((clinic$ or control$) adj trial$).tw. 85 ((control$ or experiment$ or intervention$) adj3 group$).tw. 86 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw. 87 (crossover$ or "cross over$").tw. 88 (placebo$ or (usual adj1 treatment$) or wait$ list).tw. 89 prospectiv$.tw. 90 (crossover or cross‐over).tw. 91 ((singl$ or doubl$ or tripl$ or trebl$) adj1 (blind$ or mask$)).tw. 92 ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw. 93 or/78‐92 94 77 and 93 95 limit 94 to yr="2016 ‐Current"
CINAHL EBSCOhost
Searched 24 June 2019 [476 records]
1 (MH "Hardiness") 2 (MH "Social Adjustment") 3 (MH "Adaptation, Psychological") 4 TI ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") 5 TI (positiv* N1 (adapt* OR adjust*)) OR AB (positiv* N1 (adapt* OR adjust*)) 6 TI (psychol* N1 (adapt* OR adjust*)) OR AB (psychol* N1 (adapt* OR adjust*)) 7 TI (resilien* OR hardiness*) OR AB (resilien* OR hardiness*) 8 (MH "Coping") 9 TI (cope OR coping) OR AB (cope OR coping) 10 TI ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR AB ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) 11 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 12 (MH "Psychotherapy+") 13 (MH "Stress, Psychological/TH") 14 TI (psychotherap* OR psychotherap*) OR AB (psychotherap* OR psychotherap*) 15 TI (behav* N3 (intervention* OR program* OR therap*)) OR AB (behav* N3 (intervention* OR program* OR therap*)) 16 TI ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR AB ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) 17 TI (psycho* N3 (intervention* OR program* OR therap*)) OR AB (psycho* N3 (intervention* OR program* OR therap*)) 18 TI relaxation OR AB relaxation 19 TI mindful* OR AB mindful* 20 TI (counsel?ing OR coaching) OR AB (counsel?ing OR coaching) 21 TI ("third wave" N1 (psycho* OR therap*)) OR AB ("third wave" N1 (psycho* OR therap*)) 22 TI "cognit* restructur*" OR AB "cognit* restructur*" 23 TI "positive psychology" OR AB "positive psychology" 24 TI (refram* OR refram* OR reapprais*) OR AB (refram* OR refram* OR reapprais*) 25 TI (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR AB (stress N1 (inoculation OR manag* OR reduc* OR resist*)) 26 TI (anxiety N3 manage*) OR AB (anxiety N3 manage*) 27 TI "acceptance and commitment" OR AB "acceptance and commitment" 28 (MH "Combined Modality Therapy") 29 TI (multimodal OR multimodal OR "combined modal*") OR AB (multimodal OR multimodal OR "combined modal*") 30 (MH "Health Promotion+") 31 TI (health N3 (educat* OR promot*)) OR AB (health N3 (educat* OR promot*)) 32 S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 33 S11 AND S32 34 TI (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 35 TI (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 36 S33 OR S34 OR S35 37 MH randomized controlled trials 38 MH double‐blind studies 39 MH single‐blind studies 40 MH random assignment 41 MH pretest‐posttest design 42 MH cluster sample 43 TI (randomised OR randomized) 44 AB (random*) 45 TI (trial) 46 MH (sample size) AND AB (assigned OR allocated OR control) 47 MH (placebos) 48 PT (randomized controlled trial) 49 AB (control W5 group) 50 MH (crossover design) OR MH (comparative studies) 51 AB (cluster W3 RCT) 52 MH animals+ 53 MH (animal studies) 54 TI (animal model*) 55 S52 OR S53 OR S54 56 MH (human) 57 S55 NOT S56 58 S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 59 S58 NOT S57 60 S36 AND S59 61 (MH "Health Personnel") OR (MH "Health professional") 62 TI (health* N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR AB (health* N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR SU (health* N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) 63 TI (“medical care” N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR AB (“medical care” N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR SU (“medical care” N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR TI (medical N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR AB (medical N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR SU (medical N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) 64 TI (care N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR AB (care N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR SU (care N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) 65 TI (doctor* OR physician* OR "general practitioner" OR ("primary care" N2 practitioner*) OR surgeon*) OR AB (doctor* OR physician* OR "general practitioner" OR ("primary care" N2 practitioner*) or surgeon*) OR SU (doctor* OR physician* OR "general practitioner" OR ("primary care" N2 practitioner*) or surgeon*) 66 TI (nurse* OR (nursing N1 assistant*) OR (nursing N1 staff)) OR AB (nurse* OR (nursing N1 assistant*) OR (nursing N1 staff)) OR SU (nurse* OR (nursing N1 assistant*) OR (nursing N1 staff)) 67 (MH "nursing") 68 TI nursing OR AB nursing OR SU nursing 69 TI ((hospital OR ambulance) N1 personnel) OR AB ((hospital OR ambulance) N1 personnel) OR SU ((hospital OR ambulance) N1 personnel) 70 TI ((intensive N1 care) OR ICU OR (intensive N1 care N1 unit N1 personnel*)) OR AB ((intensive N1 care) OR ICU OR (intensive N1 care N1 unit N1 personnel*)) OR SU ((intensive N1 care) OR ICU OR (intensive N1 care N1 unit N1 personnel*)) 71 TI ((allied N1 health) N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR AB ((allied N1 health) N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR SU ((allied N1 health) N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) 72 TI (psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR AB (psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR SU (psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) 73 TI (social N1 worker*) OR AB (social N1 worker*) OR SU (social N1 worker*) 74 TI (paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N1 responder*)) OR AB (paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N1 responder*)) OR SU (paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N1 responder*)) 75 TI (professional N1 caregiver*) OR AB (professional N1 caregiver*) OR SU (professional N1 caregiver*) 76 TI ((physical N1 therapist*) OR physiotherapist* OR (occupational N1 therapist*) OR (recreational N1 therapist*) OR (music N1 therapist*) OR (art N1 therapist*) OR dietitian* OR nutritionist* OR ((speech and language) N1 therapist*) OR (speech N1 pathologist*) OR audiologist* OR (exercise N1 physiologist*) OR osteopath* OR (sonographer* OR radiographer* OR radiotherapist*) OR ((radiology OR radiation) N1 (therapist* OR technician* OR technologist* OR assistant* OR scientist*)) OR (respiratory N1 therapist*) OR ((anesthesia OR anesthesiologist) N1 (technician* OR assistant*)) OR (dental N1 hygienist*) OR (surgical N1 (technician* OR technologist*)) OR orthotist* OR orthoptist* OR podiatrist* OR perfusionist*) OR AB ((physical N1 therapist*) OR physiotherapist* OR (occupational N1 therapist*) OR (recreational N1 therapist*) OR (music N1 therapist*) OR (art N1 therapist*) OR dietitian* OR nutritionist* OR ((speech and language) N1 therapist*) OR (speech N1 pathologist*) OR audiologist* OR (exercise N1 physiologist*) OR osteopath* OR (sonographer* OR radiographer* OR radiotherapist*) OR ((radiology OR radiation) N1 (therapist* OR technician* OR technologist* OR assistant* OR scientist*)) OR (respiratory N1 therapist*) OR ((anesthesia OR anesthesiologist) N1 (technician* OR assistant*)) OR (dental N1 hygienist*) OR (surgical N1 (technician* OR technologist*)) OR orthotist* OR orthoptist* OR podiatrist* OR perfusionist*) OR SU ((physical N1 therapist*) OR physiotherapist* OR (occupational N1 therapist*) OR (recreational N1 therapist*) OR (music N1 therapist*) OR (art N1 therapist*) OR dietitian* OR nutritionist* OR ((speech and language) N1 therapist*) OR (speech N1 pathologist*) OR audiologist* OR (exercise N1 physiologist*) OR osteopath* OR (sonographer* OR radiographer* OR radiotherapist*) OR ((radiology OR radiation) N1 (therapist* OR technician* OR technologist* OR assistant* OR scientist*)) OR (respiratory N1 therapist*) OR ((anesthesia OR anesthesiologist) N1 (technician* OR assistant*)) OR (dental N1 hygienist*) OR (surgical N1 (technician* OR technologist*)) OR orthotist* OR orthoptist* OR podiatrist* OR perfusionist*) 77 TI counsel?or* OR AB counsel?or* OR SU counsel?or* 78 TI ((clinical OR (clinical N1 laboratory) OR medical OR (medical N1 laboratory)) N1 (technician* OR technologist* OR assistant* OR scientist*)) OR AB ((clinical OR (clinical N1 laboratory) OR medical OR (medical N1 laboratory)) N1 (technician* OR technologist* OR assistant* OR scientist*)) OR SU ((clinical OR (clinical N1 laboratory) OR medical OR (medical N1 laboratory)) N1 (technician* OR technologist* OR assistant* OR scientist*)) 79 TI ((human or health) N1 service N1 profession*) OR AB ((human or health) N1 service N1 profession*) OR SU ((human or health) N1 service N1 profession*) 80 TI (public N1 health N1 (service or agency)) OR AB (public N1 health N1 (service or agency)) OR SU (public N1 health N1 (service or agency)) 81 TI ("secondary traumati?ation" or (work* N2 (trauma survivor*))) OR AB ("secondary traumati?ation" or (work* N2 (trauma survivor*))) OR SU ("secondary traumati?ation" or (work* N2 (trauma survivor*))) 82 TI ((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N1 therapy) OR (occupational N1 therapy)) N1 student*) OR AB ((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N1 therapy) OR (occupational N1 therapy)) N1 student*) OR SU ((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N1 therapy) OR (occupational N1 therapy)) N1 student*) 83 TI (college N1 student*) OR AB (college N1 student*) OR SU (college N1 student*) 84 TI (nursing N1 (graduates OR education)) OR AB (nursing N1 (graduates OR education)) OR SU (nursing N1 (graduates OR education)) OR TI (medical N2 train*) OR AB (medical N2 train*) OR SU (medical N2 train*) OR TI (student N1 nurse*) OR AB (student N1 nurse*) OR SU (student N1 nurse*) 85 S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81 OR S82 OR S83 OR S84 86 S60 AND S85 87 S60 AND S85, Limiters ‐ Published Date: 19900101‐20190631 88 S60 AND S85, Limiters ‐ Published Date: 20161001‐20190631
PSYNDEX EBSCOhost
Searched 24 June 2019 [31 records]
1 DE "Resilience (Psychological)" 2 DE "Adaptability (Personality)" 3 DE "Emotional Adjustment" OR DE "Social Adjustment" 4 DE "Coping Behavior" 5 DE "Posttraumatic Growth" 6 DE "Protective Factors" 7 TI ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR SU ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") 8 TI (positiv* N1 (adapt* OR adjust*)) OR AB (positiv* N1 (adapt* OR adjust*)) OR SU (positiv* N1 (adapt* OR adjust*)) 9 TI (psychol* N1 (adapt* OR adjust*)) OR AB (psychol* N1 (adapt* OR adjust*)) OR SU (psychol* N1 (adapt* OR adjust*)) 10 TI (resilien* OR hardiness*) OR AB (resilien* OR hardiness*) OR SU (resilien* OR hardiness*) 11 TI (cope OR coping) OR AB (cope OR coping) OR SU (cope OR coping) 12 TI ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR AB ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR SU ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) 13 DE "Psychological Stress" 14 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 15 DE "Psychotherapy" OR DE "Adlerian Psychotherapy" OR DE "Adolescent Psychotherapy" OR DE "Affirmative Therapy" OR DE "Analytical Psychotherapy" OR DE "Autogenic Training" OR DE "Behavior Therapy" OR DE "Brief Psychotherapy" OR DE "Brief Relational Therapy" OR DE "Child Psychotherapy" OR DE "Client Centered Therapy" OR DE "Cognitive Behavior Therapy" OR DE "Conversion Therapy" OR DE "Eclectic Psychotherapy" OR DE "Emotion Focused Therapy" OR DE "Existential Therapy" OR DE "Experiential Psychotherapy" OR DE "Expressive Psychotherapy" OR DE "Eye Movement Desensitization Therapy" OR DE "Feminist Therapy" OR DE "Geriatric Psychotherapy" OR DE "Gestalt Therapy" OR DE "Group Psychotherapy" OR DE "Guided Imagery" OR DE "Humanistic Psychotherapy" OR DE "Hypnotherapy" OR DE "Individual Psychotherapy" OR DE "Insight Therapy" OR DE "Integrative Psychotherapy" OR DE "Interpersonal Psychotherapy" OR DE "Logotherapy" OR DE "Narrative Therapy" OR DE "Network Therapy" OR DE "Persuasion Therapy" OR DE "Primal Therapy" OR DE "Psychoanalysis" OR DE "Psychodrama" OR DE "Psychodynamic Psychotherapy" OR DE "Psychotherapeutic Counseling" OR DE "Rational Emotive Behavior Therapy" OR DE "Reality Therapy" OR DE "Relationship Therapy" OR DE "Solution Focused Therapy" OR DE "Supportive Psychotherapy" OR DE "Transactional Analysis" OR DE "Individualpsychologische Therapie" OR DE "Jugendlichenpsychotherapie" OR DE "Affirmative Therapie" OR DE "Analytische Psychotherapie (C. G. Jung)" OR DE "Autogenes Training" OR DE "Verhaltenstherapie" OR DE "Kurzpsychotherapie" OR DE "Beziehungsorientierte Kurzpsychotherapie" OR DE "Kinderpsychotherapie" OR DE "Klientenzentrierte Psychotherapie" OR DE "Kognitive Verhaltenstherapie" OR DE "Konversionstherapie (Homosexualität)" OR DE "Eklektische Psychotherapie" OR DE "Emotionsfokussierte Therapie" OR DE "Existenzialtherapie" OR DE "Erfahrungsorientierte Psychotherapie" OR DE "Expressive Psychotherapie" OR DE "Augenbewegungsdesensibilisierung" OR DE "Feministische Therapie" OR DE "Geriatrische Psychotherapie" OR DE "Gestalttherapie" OR DE "Gruppenpsychotherapie" OR DE "Geleitete Fantasievorstellung" OR DE "Humanistische Psychotherapie" OR DE "Hypnotherapie" OR DE "Einzelpsychotherapie" OR DE "Einsichtstherapie" OR DE "Integrative Psychotherapie" OR DE "Interpersonelle Psychotherapie" OR DE "Logotherapie" OR DE "Narrative Therapie" OR DE "Netzwerktherapie" OR DE "Persuasionstherapie" OR DE "Primärtherapie" OR DE "Psychoanalytische Therapie" OR DE "Psychodrama" OR DE "Psychodynamische Psychotherapie" OR DE "Psychotherapeutische Beratung" OR DE "Rational‐Emotive Verhaltenstherapie" OR DE "Realitätstherapie" OR DE "Relationship Therapy" OR DE "Lösungsorientierte Therapie" OR DE "Unterstützende Psychotherapie" OR DE "Transaktionsanalyse" 16 DE "Cognitive Techniques" 17 DE "Psychotherapeutic Techniques" 18 DE "Relaxation Therapy" 19 DE "Mindfulness" 20 DE "Stress Management" 21 TI (psychotherap* OR psycho‐therap*) OR AB (psychotherap* OR psycho‐therap*) OR SU (psychotherap* OR psycho‐therap*) 22 TI (behav* N3 (intervention* OR program* OR therap*)) OR AB (behav* N3 (intervention* OR program* OR therap*)) OR SU (behav* N3 (intervention* OR program* OR therap*)) 23 TI ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR AB ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR SU ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) 24 TI (psycho* N3 (intervention* OR program* OR therap*)) OR AB (psycho* N3 (intervention* OR program* OR therap*)) OR SU (psycho* N3 (intervention* OR program* OR therap*)) 25 TI relaxation OR AB relaxation OR SU relaxation 26 TI mindful* OR AB mindful* OR SU mindful* 27 TI (counsel?ing OR coaching) OR AB (counsel?ing OR coaching) OR SU (counsel?ing OR coaching) 28 TI ("third wave" N1 (psycho* OR therap*)) OR AB ("third wave" N1 (psycho* OR therap*)) OR SU ("third wave" N1 (psycho* OR therap*)) 29 TI "cognit* restructur*" OR AB "cognit* restructur*" OR SU "cognit* restructur*" 30 TI "positive psychology" OR AB "positive psychology" OR SU "positive psychology" 31 TI (refram* OR re‐fram* OR reapprais*) OR AB (refram* OR re‐fram* OR reapprais*) OR SU (refram* OR re‐fram* OR reapprais*) 32 TI (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR AB (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR SU (stress N1 (inoculation OR manag* OR reduc* OR resist*)) 33 TI (anxiety N3 manage*) OR AB (anxiety N3 manage*) OR SU (anxiety N3 manage*) 34 TI "acceptance and commitment" OR AB "acceptance and commitment" OR SU "acceptance and commitment" 35 DE "Multimodal Treatment Approach" 36 TI (multimodal OR multi‐modal OR "combined modal*") OR AB (multimodal OR multi‐modal OR "combined modal*") OR SU (multimodal OR multi‐modal OR "combined modal*") 37 DE "Health Promotion" 38 TI (health N3 (educat* OR promot*)) OR AB (health N3 (educat* OR promot*)) OR SU (health N3 (educat* OR promot*)) 39 S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 40 S14 AND S39 41 TI (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR SU (resilien* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 42 TI (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR AB (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) OR SU (hardiness* N5 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) 43 S40 OR S41 OR S42 44 DE "Clinical Trials" 45 DE "Longitudinal Studies" 46 DE "Program Evaluation" 47 DE "Treatment Effectiveness Evaluation" 48 TI random* OR AB random* 49 TI (allocat* OR assign*) OR AB (allocat* OR assign*) 50 TI (clinic* OR control*) N1 trial*)) OR AB (clinic* OR control*) N1 trial*)) 51 TI ((control* OR experiment* OR intervention*) N3 group*) OR AB ((control* OR experiment* OR intervention*) N3 group*) 52 TI ((singl* OR doubl* OR trebl* OR tripl*) N3 (blind* OR mask*)) OR AB ((singl* OR doubl* OR trebl* OR tripl*) N3 (blind* OR mask*)) 53 TI (crossover* OR "cross over*") OR AB (crossover* OR "cross over*") 54 TI (placebo* OR (usual N1 treatment*) OR waitlist OR wait‐list) OR AB (placebo* OR (usual N1 treatment*) OR waitlist OR wait‐list) 55 TI prospectiv* OR AB prospectiv* 56 TI (crossover OR cross‐over) OR AB (crossover OR cross‐over) 57 TI ((singl* OR doubl* OR tripl* OR trebl*) N1 (blind* OR mask*)) OR AB ((singl* OR doubl* OR tripl* OR trebl*) N1 (blind* OR mask*)) 58 TI ((effectiveness OR evaluat*) N3 (stud* OR research*)) OR AB ((effectiveness OR evaluat*) N3 (stud* OR research*)) 59 S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 OR S52 OR S53 OR S54 OR S55 OR S56 OR S57 OR S58 60 S43 AND S59 61 DE "Health Personnel" OR DE "Health professional" 62 TI (health* N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR AB (health* N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR SU (health* N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) 63 TI (“medical care” N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR AB (“medical care” N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR SU (“medical care” N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR TI (medical N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR AB (medical N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR SU (medical N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) 64 TI (care N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR AB (care N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR SU (care N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) 65 TI (doctor* OR physician* OR "general practitioner" OR ("primary care" N2 practitioner*) OR surgeon*) OR AB (doctor* OR physician* OR "general practitioner" OR ("primary care" N2 practitioner*) or surgeon*) OR SU (doctor* OR physician* OR "general practitioner" OR ("primary care" N2 practitioner*) or surgeon*) 66 TI (nurse* OR (nursing N1 assistant*) OR (nursing N1 staff)) OR AB (nurse* OR (nursing N1 assistant*) OR (nursing N1 staff)) OR SU (nurse* OR (nursing N1 assistant*) OR (nursing N1 staff)) 67 DE "nursing" 68 TI nursing OR AB nursing OR SU nursing 69 TI ((hospital OR ambulance) N1 personnel) OR AB ((hospital OR ambulance) N1 personnel) OR SU ((hospital OR ambulance) N1 personnel) 70 TI ((intensive N1 care) OR ICU OR (intensive N1 care N1 unit N1 personnel*)) OR AB ((intensive N1 care) OR ICU OR (intensive N1 care N1 unit N1 personnel*)) OR SU ((intensive N1 care) OR ICU OR (intensive N1 care N1 unit N1 personnel*)) 71 TI ((allied N1 health) N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR AB ((allied N1 health) N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) OR SU ((allied N1 health) N1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)) 72 TI (psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR AB (psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR SU (psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) 73 TI (social N1 worker*) OR AB (social N1 worker*) OR SU (social N1 worker*) 74 TI (paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N1 responder*)) OR AB (paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N1 responder*)) OR SU (paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N1 responder*)) 75 TI (professional N1 caregiver*) OR AB (professional N1 caregiver*) OR SU (professional N1 caregiver*) 76 TI ((physical N1 therapist*) OR physiotherapist* OR (occupational N1 therapist*) OR (recreational N1 therapist*) OR (music N1 therapist*) OR (art N1 therapist*) OR dietitian* OR nutritionist* OR ((speech and language) N1 therapist*) OR (speech N1 pathologist*) OR audiologist* OR (exercise N1 physiologist*) OR osteopath* OR (sonographer* OR radiographer* OR radiotherapist*) OR ((radiology OR radiation) N1 (therapist* OR technician* OR technologist* OR assistant* OR scientist*)) OR (respiratory N1 therapist*) OR ((anesthesia OR anesthesiologist) N1 (technician* OR assistant*)) OR (dental N1 hygienist*) OR (surgical N1 (technician* OR technologist*)) OR orthotist* OR orthoptist* OR podiatrist* OR perfusionist*) OR AB ((physical N1 therapist*) OR physiotherapist* OR (occupational N1 therapist*) OR (recreational N1 therapist*) OR (music N1 therapist*) OR (art N1 therapist*) OR dietitian* OR nutritionist* OR ((speech and language) N1 therapist*) OR (speech N1 pathologist*) OR audiologist* OR (exercise N1 physiologist*) OR osteopath* OR (sonographer* OR radiographer* OR radiotherapist*) OR ((radiology OR radiation) N1 (therapist* OR technician* OR technologist* OR assistant* OR scientist*)) OR (respiratory N1 therapist*) OR ((anesthesia OR anesthesiologist) N1 (technician* OR assistant*)) OR (dental N1 hygienist*) OR (surgical N1 (technician* OR technologist*)) OR orthotist* OR orthoptist* OR podiatrist* OR perfusionist*) OR SU ((physical N1 therapist*) OR physiotherapist* OR (occupational N1 therapist*) OR (recreational N1 therapist*) OR (music N1 therapist*) OR (art N1 therapist*) OR dietitian* OR nutritionist* OR ((speech and language) N1 therapist*) OR (speech N1 pathologist*) OR audiologist* OR (exercise N1 physiologist*) OR osteopath* OR (sonographer* OR radiographer* OR radiotherapist*) OR ((radiology OR radiation) N1 (therapist* OR technician* OR technologist* OR assistant* OR scientist*)) OR (respiratory N1 therapist*) OR ((anesthesia OR anesthesiologist) N1 (technician* OR assistant*)) OR (dental N1 hygienist*) OR (surgical N1 (technician* OR technologist*)) OR orthotist* OR orthoptist* OR podiatrist* OR perfusionist*) 77 TI counsel?or* OR AB counsel?or* OR SU counsel?or* 78 TI ((clinical OR (clinical N1 laboratory) OR medical OR (medical N1 laboratory)) N1 (technician* OR technologist* OR assistant* OR scientist*)) OR AB ((clinical OR (clinical N1 laboratory) OR medical OR (medical N1 laboratory)) N1 (technician* OR technologist* OR assistant* OR scientist*)) OR SU ((clinical OR (clinical N1 laboratory) OR medical OR (medical N1 laboratory)) N1 (technician* OR technologist* OR assistant* OR scientist*)) 79 TI ((human or health) N1 service N1 profession*) OR AB ((human or health) N1 service N1 profession*) OR SU ((human or health) N1 service N1 profession*) 80 TI (public N1 health N1 (service or agency)) OR AB (public N1 health N1 (service or agency)) OR SU (public N1 health N1 (service or agency)) 81 TI ("secondary traumati?ation" or (work* N2 (trauma survivor*))) OR AB ("secondary traumati?ation" or (work* N2 (trauma survivor*))) OR SU ("secondary traumati?ation" or (work* N2 (trauma survivor*))) 82 TI ((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N1 therapy) OR (occupational N1 therapy)) N1 student*) OR AB ((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N1 therapy) OR (occupational N1 therapy)) N1 student*) OR SU ((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N1 therapy) OR (occupational N1 therapy)) N1 student*) 83 TI (college N1 student*) OR AB (college N1 student*) OR SU (college N1 student*) 84 TI (nursing N1 (graduates OR education)) OR AB (nursing N1 (graduates OR education)) OR SU (nursing N1 (graduates OR education)) OR TI (medical N2 train*) OR AB (medical N2 train*) OR SU (medical N2 train*) OR TI (student N1 nurse*) OR AB (student N1 nurse*) OR SU (student N1 nurse*) 85 S61 OR S62 OR S63 OR S64 OR S65 OR S66 OR S67 OR S68 OR S69 OR S70 OR S71 OR S72 OR S73 OR S74 OR S75 OR S76 OR S77 OR S78 OR S79 OR S80 OR S81 OR S82 OR S83 OR S84 86 S60 AND S85 87 S60 AND S85, Limiters ‐ Published Date: 1990‐2019 88 S60 AND S85, Limiters ‐ Published Date: 2016‐2019
Web Of Science Core Collection (SCI, SSCI, CPCI‐S, CPCI‐SSH)
Searched 26 June 2019 [515 records]
#40 #18 AND #38 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2016‐2019 #39 #16 AND #17 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=1990‐2016 #38 #37 OR #36 OR #35 OR #34 OR #33 OR #32 OR #31 OR #30 OR #29 OR #28 OR #27 OR #26 OR #25 OR #24 OR #23 OR #22 OR #21 OR #20 OR #19 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #37 TS=("college student*") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #36 TS=((nursing or medical or premedical or paramedic or psychology or "physical therapy" or "occupational therapy") NEAR/2 student*) #35 ts=("secondary trauma*" or (work* NEAR/2 "trauma survivor*")) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #34 TS=("public health service*" or "public health agenc*") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #33 TS=((clinical or medical*) NEAR/1 (technician* or technologist* or assistant* or scientist*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #32 TS=(counsellor* or counselor*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #31 TS=(anesthetist* or anaesthetist* or audiologist* or "dental hygienist*" or dentist* or dietitian* or "midwi*e*" or nutritionist* or pathologist* or physiologist* or physiotherapist* or therapist or osteopath* or sonographer* or radiographer* or radiotherapist* or ((radiology or radiation) NEAR/1 ( technician* or technologist* or assistant* or scientist*)) or ((anesthesia or anesthesiologist) NEAR/1 (technician* or assistant*)) or (surgical NEAR/1 (technician* or technologist*)) or orthotist* or orthoptist* or podiatrist* or perfusionist*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #30 TS=(professional NEAR/1 (caregiver* or care‐giver*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #29 TS=((first or emergency or disaster) NEAR/1 (response or responder*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #28 TS=(paramedic* or para‐medic* or ambulance ) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #27 ts=(psychologist* or psychotherapist* or psychiatrist* or "mental health clinician*" or "mental health profession*" or "mental health worker*" or "social worker*") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #26 TS= ("allied health*" NEAR/2 (personnel* or profession* or worker* or practitioner* or provider* or staff)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #25 TS=((intensive NEAR/2 care) or ICU) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #24 TS=((hospital or ambulance) NEAR/1 (staff or personnel)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #23 ts=(nurse* or nursing) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #22 TS=(doctor* or physician* or general practitioner* or ("primary care" NEAR/2 practitioner*) or surgeon*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #21 TS=(care* NEAR/1 (personnel or profession* or worker* or practitioner* or provider* or staff)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #20 TS=(medical NEAR/3 (personnel or profession* or worker* or practitioner* or provider* or staff)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #19 TS=(health* NEAR/3 (personnel or profession* or worker* or practitioner* or provider* or staff)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #18 #17 AND #16 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #17 TS=(random* or trial* or assign* or control* or group* or placebo* or blind* or prospectiv* or longitudinal* or meta‐analys* or systematic review*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #16 #14 or #15 #15 TS=((resilience or hardiness) near/3 (train* or program* or intervention* or promot* or prevent* or enhanc* or learn* or teach* or educat* or increas* or develop* or manag* or therap* or protocol* or treat*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #14 #13 AND #6 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #13 #12 OR #11 OR #10 OR #9 OR #8 OR #7 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #12 TS=(health near/3 (educat* or promot*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #11 TS= ((multimodal* or "multi modal*" or "combined modal*") NEAR/3 (treat* or therap* or intervention* or program*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #10 TS=("acceptance and commitment") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #9 TS=((anxiety near/1 manag*) or relaxation or mindful* or counsel*ing or coaching or "third wave" or refram* or "re fram*" or "cognitive restructur*" or "positive psychology") Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #8 TS=(stress near/3 (inoculat* or manag* or reduc* or resist*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #7 TS=((psychotherap* or "psycho therap*") or CBT or mindful* or (behav* near/3 (intervention* or program* or therap*)) OR ((cognit* or "cognitive behavior*" or CBT) near/3 (intervention* or program* or therap*)) OR (psycho* near/3 (intervention* or program* or therap*))) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years #6 #5 OR #4 OR #3 OR #2 OR #1 Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years # 5 TS= ((withstand* or overcom* or resist* or recover* or thriv* or adapt* or adjust* or "bounc* back" ) near/1 (stress* or trauma* or advers*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years # 4 TS=(psychol* near/1 (adapt* or adjust*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years # 3 TS=(positiv* near/1 (adapt* or adjust*)) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years # 2 TS=("post traumatic growth" or "posttraumatic growth" or "stress related growth") TS=(resilien* or hardiness*) Indexes=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=All years
International Bibliography of the Social Sciences ProQuest
Searched 25 June 2019 [135 records]
(((MAINSUBJECT.EXACT("Coping") OR TI(resilien* OR hardiness) OR AB(resilien* OR hardiness)) OR (TI((psychol* OR social) NEAR/1 (adapt* OR adjust*)) OR AB((psychol* OR social) NEAR/1 (adapt* OR adjust*))) OR (TI(positiv* NEAR/1 (adapt* OR adjust*)) OR AB(positiv* NEAR/1 (adapt* OR adjust*))) OR (TI("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (TI(cope OR coping) OR AB(cope OR coping)) OR (TI((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") NEAR/5 (stress* OR trauma* OR adversit*)) OR AB((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") NEAR/5 (stress* OR trauma* OR adversit*)))) AND ((MAINSUBJECT.EXACT("Psychotherapy") OR MAINSUBJECT.EXACT("Cognitive therapy") OR MAINSUBJECT.EXACT("Group therapy") OR TI(psychotherap* OR psycho‐therap*) OR AB(psychotherap* OR psycho‐therap*) OR TI(behav* NEAR/3 (intervention* OR program* OR therap*)) OR AB(behav* NEAR/3 (intervention* OR program* OR therap*)) OR TI(cognit* OR "cognitive behavior*" OR CBT) OR AB(cognit* OR "cognitive behavior*" OR CBT) OR TI(psycho* NEAR/3 (intervention* OR program* OR therap*)) OR AB(psycho* NEAR/3 (intervention* OR program* OR therap*)) OR TI(relaxation OR mindful* OR counsel?ing OR coaching OR "third wave") OR AB(relaxation OR mindful* OR counsel?ing OR coaching OR "third wave") OR TI(cognit* NEAR/1 restructur*) OR AB(cognit* NEAR/1 restructur*) OR TI("positive psychology") OR AB("positive psychology")) AND (MAINSUBJECT.EXACT("Clinical trials") OR (TI(control* OR group OR random* OR placebo* OR longitudinal OR prospective* OR blind* OR trial*) OR AB(control* OR group OR random* OR placebo* OR longitudinal OR prospective* OR blind* OR trial*)))) Limited to publication year 2016‐2019
Applied Social Sciences Index & Abstracts ProQuest
Searched 24 June 2019 [41 records]
1 SU.EXACT("Resilience") 2 SU.EXACT("Hardiness") 3 ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") 4 ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) 5 ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) 6 SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) 7 ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 8 ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 9 (SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 10 ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*) 11 ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*) 12 ti(randomi?ed) OR ab(randomi?ed) 13 ti(placebo*) OR ab(placebo*) 14 ti(randomly) OR ab(randomly) 15 ti(trial) OR ab(trial) 16 (ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)) 17 ((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial))) 18 ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) 19 ti((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) 20 ti(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*) 21 ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) 22 SU.EXACT("nursing") 23 ti(nursing) OR ab(nursing) 24 ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) 25 ti(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*") OR ab(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*") 26 ti(social N/1 worker*) OR ab(social N/1 worker*) 27 ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) 28 ti(physiotherapist* OR (occupational N/1 therapist*)) OR ab(physiotherapist* OR (occupational N/1 therapist)) 29 ti(counsel?or*) OR ab(counsel?or*) 30 ti((human or health) N/1 service N/1 profession*) OR ab((human or health) N/1 service N/1 profession*) 31 ti(public N/1 health N/1 (service or agency)) OR ab(public N/1 health N/1 (service or agency)) 32 ti("secondary traumati?ation" OR (work* N/2 ("trauma survivor*"))) OR ab("secondary traumati?ation" OR (work* N/2 ("trauma survivor*"))) 33 ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) 34 ti(college N/1 student*) OR ab(college N/1 student*) 35 (ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)))) OR (ti((care NEAR/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care NEAR/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)))) OR (ti(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*)) OR (ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff))) OR SU.EXACT("nursing") OR (ti(nursing) OR ab(nursing)) OR (ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*))) OR (ti(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*") OR ab(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*")) OR (ti(social N/1 worker*) OR ab(social N/1 worker*)) OR (ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*))) OR (ti(physiotherapist* OR (occupational N/1 therapist*)) OR ab(physiotherapist* OR (occupational N/1 therapist))) OR (ti(counsel?or*) OR ab(counsel?or*)) OR (ti((human or health) N/1 service N/1 profession*) OR ab((human or health) N/1 service N/1 profession*)) OR (ti(public N/1 health N/1 (service or agency)) OR ab(public N/1 health N/1 (service or agency))) OR (ti("secondary traumati?ation" OR (work* N/2 ("trauma survivor*"))) OR ab("secondary traumati?ation" OR (work* N/2 ("trauma survivor*")))) OR (ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*)) OR (ti(college N/1 student*) OR ab(college N/1 student*)) 36 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)))) 37 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)))) AND pd(20161001‐20190624), 2016‐10‐01 ‐ 2019‐06‐20 38 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((care NEAR/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care NEAR/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)))) 39 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((care NEAR/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care NEAR/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)))), 2016‐10‐01 ‐ 2019‐06‐20 40 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*)) 41 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR "general practitioner" OR ("primary care" N/2 practitioner*) OR surgeon*)), 2016‐10‐01 ‐ 2019‐06‐20 42 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff))) 43 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff))), 2016‐10‐01 ‐ 2019‐06‐20 44 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND SU.EXACT("nursing") 45 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND SU.EXACT("nursing"), 2016‐10‐01 ‐ 2019‐06‐20 46 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nursing) OR ab(nursing)) 47 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nursing) OR ab(nursing)), 2016‐10‐01 ‐ 2019‐06‐20 48 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*))) 49 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*))), 2016‐10‐01 ‐ 2019‐06‐20 50 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*") OR ab(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*")) 51 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*") OR ab(psychologist* OR psychotherapist* OR "mental health clinician*" OR "mental health profession*" OR "mental health worker*")), 2016‐10‐01 ‐ 2019‐06‐20 52 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(social N/1 worker*) OR ab(social N/1 worker*)) 53 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(social N/1 worker*) OR ab(social N/1 worker*)), 2016‐10‐01 ‐ 2019‐06‐20 54 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*))) 55 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*))), 2016‐10‐01 ‐ 2019‐06‐20 56 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(physiotherapist* OR (occupational N/1 therapist*)) OR ab(physiotherapist* OR (occupational N/1 therapist))) 57 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(physiotherapist* OR (occupational N/1 therapist*)) OR ab(physiotherapist* OR (occupational N/1 therapist))), 2016‐10‐01 ‐ 2019‐06‐20 58 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(counsel?or*) OR ab(counsel?or*)) 59 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(counsel?or*) OR ab(counsel?or*)), 2016‐10‐01 ‐ 2019‐06‐20 60 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR anag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((human or health) N/1 service N/1 profession*) OR ab((human or health) N/1 service N/1 profession*)) 61 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR anag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((human or health) N/1 service N/1 profession*) OR ab((human or health) N/1 service N/1 profession*)), 2016‐10‐01 ‐ 2019‐06‐20 62 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(public N/1 health N/1 (service or agency)) OR ab(public N/1 health N/1 (service or agency))) 63 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(public N/1 health N/1 (service or agency)) OR ab(public N/1 health N/1 (service or agency))), 2016‐10‐01 ‐ 2019‐06‐20 64 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti("secondary traumati?ation" OR (work* N/2 ("trauma survivor*"))) OR ab("secondary traumati?ation" OR (work* N/2 ("trauma survivor*")))) 65 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti("secondary traumati?ation" OR (work* N/2 ("trauma survivor*"))) OR ab("secondary traumati?ation" OR (work* N/2 ("trauma survivor*")))), 2016‐10‐01 ‐ 2019‐06‐20 66 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*))OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*)) 67 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*))OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*)), 2016‐10‐01 ‐ 2019‐06‐20 68 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(college N/1 student*) OR ab(college N/1 student*)) 69 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(college N/1 student*) OR ab(college N/1 student*)), 2016‐10‐01 ‐ 2019‐06‐200 Subsequent (individual) export of results in lines 37, 39, 41, 43, 45, 47, 49, 51, 53, 55, 57, 59, 61, 63, 65, 67, 69
ProQuest Dissertations & Theses ProQuest
Searched 24 June 2019 [22 records]
1 SU.EXACT("Resilience") 2 SU.EXACT("Hardiness") 3 ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") 4 ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*) 5 ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) 6 SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*))) 7 ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 8 ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 9 (SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) 10 ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*) 11 ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*) 12 ti(randomi?ed) OR ab(randomi?ed) 13 ti(placebo*) OR ab(placebo*) 14 ti(randomly) OR ab(randomly) 15 ti(trial) OR ab(trial) 16 (ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)) 17 ((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial))) 18 ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) 19 ti(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR ab(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) 20 ti((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) 21 ti(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*) 22 ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) 23 SU.EXACT(“nursing”) 24 ti(nursing) OR ab(nursing) 25 ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) 26 ti(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR ab(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) 27 ti(social N/1 worker*) OR ab(social N/1 worker*) 28 ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) 29 ti(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*)) OR ab(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*)) 30 ti(counsel?or*) OR ab(counsel?or*) 31 ti(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”))) OR ab(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”))) 32 ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) 33 ti(college N/1 student*) OR ab(college N/1 student*) 34 ti(nursing N/1 (graduates OR education)) OR ab(nursing N/1 (graduates OR education)) 35 (ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)))) OR (ti(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR ab(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR (ti((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)))) OR (ti(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*)) OR (ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff))) OR SU.EXACT(“nursing”) OR (ti(nursing) OR ab(nursing)) OR (ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*))) OR (ti(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR ab(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”)) OR (ti(social N/1 worker*) OR ab(social N/1 worker*)) OR (ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*))) OR (ti(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*)) OR ab(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*))) OR (ti(counsel?or*) OR ab(counsel?or*)) OR (ti(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”))) OR ab(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”)))) OR (ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*)) OR (ti(college N/1 student*) OR ab(college N/1 student*)) OR (ti(nursing N/1 (graduates OR education)) OR ab(nursing N/1 (graduates OR education))) 36 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)))) 37 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff))) OR ab((health* N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff)))), 2016‐10‐01 ‐ 2019‐06‐20 38 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR ab(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) 39 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)) OR ab(medical N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))), 2016‐10‐01 ‐ 2019‐06‐20 40 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)))) 41 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*))) OR ab((care N/1 (personnel OR profession* OR worker* OR practitioner* OR provider* OR staff*)))), 2016‐10‐01 ‐ 2019‐06‐20 42 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*)) 43 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*) OR ab(doctor* OR physician* OR “general practitioner” OR (“primary care” N/2 practitioner*) OR surgeon*)), 2016‐10‐01 ‐ 2019‐06‐20 44 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff))) 45 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff)) OR ab(nurse* OR (nursing N/1 assistant*) OR (nursing N/1 staff))), 2016‐10‐01 ‐ 2019‐06‐20 46 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND SU.EXACT(“nursing”) 47 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND SU.EXACT(“nursing”), 2016‐10‐01 ‐ 2019‐06‐20 48 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nursing) OR ab(nursing)) 49 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nursing) OR ab(nursing)), 2016‐10‐01 ‐ 2019‐06‐20 50 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*))) 51 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*)) OR ab((intensive N/1 care) OR ICU OR (intensive N/1 care N/1 unit N/1 personnel*))), 2016‐10‐01 ‐ 2019‐06‐20 52 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR ab(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”)) 53 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”) OR ab(psychologist* OR psychotherapist* OR “mental health clinician*” OR “mental health profession*” OR “mental health worker*”)), 2016‐10‐01 ‐ 2019‐06‐20 54 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(social N/1 worker*) OR ab(social N/1 worker*)) 55 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(social N/1 worker*) OR ab(social N/1 worker*)), 2016‐10‐01 ‐ 2019‐06‐20 56 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*))) 57 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*)) OR ab(paramedic* OR ambulance OR medic* OR ((first OR emergency OR disaster) N/1 responder*))), 2016‐10‐01 ‐ 2019‐06‐20 58 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*)) OR ab(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*))) 59 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*)) OR ab(physiotherapist* OR (art N/1 therapist*) OR dietitian* OR (dental N/1 hygienist*))), 2016‐10‐01 ‐ 2019‐06‐20 60 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(counsel?or*) OR ab(counsel?or*)) 61 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(counsel?or*) OR ab(counsel?or*)), 2016‐10‐01 ‐ 2019‐06‐20 62 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”))) OR ab(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”)))) 63 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”))) OR ab(“secondary traumati?ation” OR (work* N/2 (“trauma survivor*”)))), 2016‐10‐01 ‐ 2019‐06‐20 64 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*)) 65 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*) OR ab((nursing OR medical OR premedical OR paramedic OR psychology OR (physical N/1 therapy) OR (occupational N/1 therapy)) N/1 student*)), 2016‐10‐01 ‐ 2019‐06‐20 66 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(college N/1 student*) OR ab(college N/1 student*)) 67 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(college N/1 student*) OR ab(college N/1 student*)), 2016‐10‐01 ‐ 2019‐06‐20 68 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nursing N/1 (graduates OR education)) OR ab(nursing N/1 (graduates OR education))) 69 (((SU.EXACT("Resilience") OR SU.EXACT("Hardiness") OR (ti("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR ab("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) OR (ti(resilien* OR hardiness*) OR ab(resilien* OR hardiness*)) OR (ti((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)) OR ab((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N/5 (stress* OR trauma* OR adversit*)))) OR ti((resilien* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*))) OR ti((hardiness* N/5 (train* OR program* OR intervention* OR promot* OR prevent* OR enhanc* OR learn* OR teach* OR educat* OR increas* OR develop* OR manag* OR therap* OR protocol* OR treat*)))) AND ((ti(randomi?ed N/1 control* N/1 trial*) OR ab(randomi?ed N/1 control* N/1 trial*)) OR (ti(control* N/1 clinical N/1 trial*) OR ab(control* N/1 clinical N/1 trial*)) OR (ti(randomi?ed) OR ab(randomi?ed)) OR (ti(placebo*) OR ab(placebo*)) OR (ti(randomly) OR ab(randomly)) OR (ti(trial) OR ab(trial)))) AND (ti(nursing N/1 (graduates OR education)) OR ab(nursing N/1 (graduates OR education))), 2016‐10‐01 ‐ 2019‐06‐20 Subsequent (individual) export of results in lines 37, 39, 41, 43, 45, 47, 49, 51, 53, 55, 57, 59, 61, 63, 65, 67, 69
Cochrane Database of Systematic Reviews (CDSR), part of the Cochrane Library
Searched 26 June 2019 (5 records)
IDSearchHits #1(resilien* or hardiness*):ti,ab #2(post next traumatic next growth or posttraumatic NEXT growth or stress next related next growth):ti,ab #3(positiv* near/1 (adapt* or adjust*)):ti,ab #4(psychol* near/1 (adapt* or adjust*)):ti,ab #5{or #1‐#4} #6(behav* or psycho* or cbt or cognit* or mindful* or reframe* or re next fram*):ti,ab #7(stress near/3 (inoculat* or manag* or reduc* or resist*)):ti,ab #8(anxiety near/3 manag*):ti,ab #9"acceptance and commitment":ti,ab #10(multimodal* or multi next modal* or combined next modal*):ti,ab #11(health near/3 (educat* or promot*)):ti,ab #12{or #6‐#11} #13#5 and #12 with Cochrane Library publication date Between Oct 2016 and Jun 2019, in Cochrane Reviews, Cochrane Protocolss
Epistemonikos (www.epistemonikos.org/)
Searched 24 June 2019 [6 records]
1 (title:(resilien* OR hardiness*) OR abstract:(resilien* OR hardiness*)) 2 (title:("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth") OR abstract:("posttraumatic growth" OR "post‐traumatic growth" OR "stress‐related growth")) 3 (title:("positive adaptation" OR "positive adjustment") OR abstract:("positive adaptation" OR "positive adjustment")) 4 (title:("psychological adaptation" OR "psychological adjustment") OR abstract:("psychological adaptation" OR "psychological adjustment")) 5 OR/#1‐#4 6 (title:("health personnel*" OR "health profession*" OR "health professional*" OR "health worker*" OR "health practitioner*" OR "health provider*" OR "health staff") OR abstract:("health personnel*" OR "health profession*" OR "health professional*" OR "health worker*" OR "health practitioner*" OR "health provider*" OR "health staff")) 7 (title:("healthcare personnel*" OR "healthcare profession*" OR "healthcare professional*" OR "healthcare worker*" OR "healthcare practitioner*" OR "healthcare provider*" OR "healthcare staff") OR abstract:("healthcare personnel*" OR "healthcare profession*" OR "healthcare professional*" OR "healthcare worker*" OR "healthcare practitioner*" OR "healthcare provider*" OR "healthcare staff")) 8 (title:("health care personnel*" OR "health care profession*" OR "health care professional*" OR "health care worker*" OR "health care practitioner*" OR "health care provider*" OR "health care staff") OR abstract:("health care personnel*" OR "health care profession*" OR "health care professional*" OR "health care worker*" OR "health care practitioner*" OR "health care provider*" OR "health care staff")) 9 OR/#6‐#8 10 AND/#5‐#9; Publication year (Custom year range): 1990 – 2019; Publication type: Systematic Review; Systematic review question: All; Cochrane review: All; Type of meta‐analysis: All
ERIC EBSCOhost
26 June 2019 (505 records)
All years searched in 2019 as there were errors in the 2016 search
S1DE "Resilience (Psychology)" Database ‐ ERIC S2DE "Social Adjustment" OR DE "Emotional Adjustment" Database ‐ ERIC S3TI ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") OR AB ("posttraumatic growth" OR "posttraumatic growth" OR "stress‐related growth") Database ‐ ERIC S4TI (positiv* N1 (adapt* OR adjust*)) OR AB (positiv* N1 (adapt* OR adjust*)) Database ‐ ERIC S5TI (psychol* N1 (adapt* OR adjust*)) OR AB (psychol* N1 (adapt* OR adjust*)) Database ‐ ERIC S6TI (resilien* OR hardiness*) OR AB (resilien* OR hardiness*) OR SU (resilien*) Database ‐ ERIC S7TI (cope OR coping) OR AB (cope OR coping) OR SU (cope OR coping) Database ‐ ERIC S8TI ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) OR AB ((withstand* OR overcom* OR resist* OR recover* OR thriv* OR adapt* OR adjust* OR "bounc* back") N5 (stress* OR trauma* OR adversit*)) Database ‐ ERIC S9S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 Database ‐ ERIC S10DE "Psychotherapy" OR DE "Milieu Therapy" OR DE "Relaxation Training" Database ‐ ERIC S11TI (psycho‐therap* OR psychotherap* ) OR AB (psychotherap* OR psychotherap*) OR SU (psycho‐therap* OR psychotherap*) Database ‐ ERIC S12TI (behav* N3 (intervention* OR program* OR therap*)) OR AB (behav* N3 (intervention* OR program* OR therap*)) Database ‐ ERIC S13TI ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) OR AB ((cognit* OR "cognitive behavior*" OR CBT) N3 (intervention* OR program* OR therap*)) Database ‐ ERIC S14TI (psycho* N3 (intervention* OR program* OR therap*)) OR AB (psycho* N3 (intervention* OR program* OR therap*)) Database ‐ ERIC S15TI relaxation OR AB relaxation OR SU relaxation Database ‐ ERIC S16TI mindful* OR AB mindful* Database ‐ ERIC S17TI (counsel?ing OR coaching) OR AB (counsel?ing OR coaching) OR SU (counsel?ing OR coaching) Database ‐ ERIC S18TI ("third wave" N1 (psycho* OR therap*)) OR AB ("third wave" N1 (psycho* OR therap*)) Database ‐ ERIC S19TI ("cognit* restructur*") OR AB ("cognit* restructur*") OR SU ("cognit* restructur*") Database ‐ ERIC S20TI "positive psychology" OR AB "positive psychology" Database ‐ ERIC S21TI (refram* OR refram* OR reapprais*) OR AB (refram* OR refram* OR reapprais*)Interface ‐ EBSCOhost Research Databases Database ‐ ERIC S22TI (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR AB (stress N1 (inoculation OR manag* OR reduc* OR resist*)) OR SU (stress N1 (inoculation OR manag* OR reduc* OR resist*)) Database ‐ ERIC S23TI (anxiety N3 manage*) OR AB (anxiety N3 manage*) Database ‐ ERIC S24TI "acceptance and commitment" OR AB "acceptance and commitment" Database ‐ ERIC S25TI (multimodal OR multimodal OR "combined modal*") OR AB (multimodal OR multimodal OR "combined modal*") Database ‐ ERIC S26TI (health N3 (educat* OR promot*)) OR AB (health N3 (educat* OR promot*)) OR SU (health N3 (educat* OR promot*)) Database ‐ ERIC S27S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 Database ‐ ERIC S28S9 AND S27 Database ‐ ERIC S29((DE "Health Occupations" OR DE "Allied Health Occupations" OR DE "Medical Education" OR DE "Health Personnel" OR DE "Allied Health Personnel" OR DE "Mental Health Workers" OR DE "Nurses" OR DE "Physicians" OR DE "Psychologists" OR DE "Graduate Medical Education" OR DE "Nursing Education" OR DE "Allied Health Occupations Education" OR DE "Clinical Experience" OR DE "Medical Schools" OR DE "Medical Students" OR DE "Premedical Students" Database ‐ ERIC S30DE "Counselors" OR DE "School Social Workers" OR DE "Social Work" Database ‐ ERIC S31TI(health* N3 (personnel or profession* or worker* or practitioner* or provider* or staff)) OR AB(health* N3 (personnel or profession* or worker* or practitioner* or provider* or staff)) Database ‐ ERIC S32TI(medical N3 (personnel or profession* or worker* or practitioner* or provider* or staff)) OR AB(medical N3 (personnel or profession* or worker* or practitioner* or provider* or staff)) Database ‐ ERIC S33TI(care N1 (personnel or profession* or worker* or practitioner* or provider* or staff)) OR AB(care N1 (personnel or profession* or worker* or practitioner* or provider* or staff))Database ‐ ERIC S34TI(doctor* or physician* or general practitioner* or (primary care N2 practitioner*) or surgeon*) OR AB(doctor* or physician* or general practitioner* or (primary care N2 practitioner*) or surgeon*) Database ‐ ERIC S35TI(nurse* or nursing) OR AB(nurse* or nursing) Database ‐ ERIC S36TI(hospital or ambulance) OR AB(hospital or ambulance) Database ‐ ERIC S37TI((intensive N2 care) or ICU) OR AB((intensive N2 care) or ICU) Database ‐ ERIC S38TI(allied health* N2 (personnel* or profession* or worker* or practitioner* or provider* or staff)) OR AB(allied health* N2 (personnel* or profession* or worker* or practitioner* or provider* or staff)) Database ‐ ERIC S39TI(psychologist* or psychotherapist* or psychiatrist* or mental health clinician* or mental health profession* or mental health worker*) OR AB(psychologist* or psychotherapist* or psychiatrist* or mental health clinician* or mental health profession* or mental health worker*) Database ‐ ERIC S40TI(social worker*) OR AB(social worker*) Database ‐ ERIC S41TI(paramedic* or para‐medic* or ambulance ) OR AB(paramedic* or para‐medic* or ambulance ) Database ‐ ERIC S42TI(first or emergency or disaster) N1 (response or responder*)) OR AB(first or emergency or disaster) N1 (response or responder*)) Database ‐ ERIC S43TI(professional N1 (caregiver* or care‐giver*)) OR AB(professional N1 (caregiver* or care‐giver*)) Database ‐ ERIC S44TI (physical therapist* or physiotherapist* or occupational therapist* or recreational therapist* or music therapist* or art therapist* or dietitian* or nutritionist* or ((speech and language) N1 therapist*) or speech pathologist* or audiologist* or exercise physiologist* or osteopath* or sonographer* or radiographer* or radiotherapist* or ((radiology or radiation) N1 (therapist* or technician* or technologist* or assistant* or scientist*)) or respiratory therapist* or ((anesthesia or anesthesiologist) N1 (technician* or assistant*)) or dental hygienist* or (surgical N1 (technician* or technologist*)) or orthotist* or orthoptist* or podiatrist* or perfusionist*) OR AB (physical therapist* or physiotherapist* or occupational therapist* or recreational therapist* or music therapist* or art therapist* or dietitian* or nutritionist* or ((speech and language) N1 therapist*) or speech pathologist* or audiologist* or exercise physiologist* or osteopath* or sonographer* or radiographer* or radiotherapist* or ((radiology or radiation) N1 (therapist* or technician* or technologist* or assistant* or scientist*)) or respiratory therapist* or ((anesthesia or anesthesiologist) N1 (technician* or assistant*)) or dental hygienist* or (surgical N1 (technician* or technologist*)) or orthotist* or orthoptist* or podiatrist* or perfusionist*) Database ‐ ERIC S45TI(counsel*or* ) OR AB(counsel*or* ) S46TI((clinical OR medical*) N1 (technician* or technologist* or assistant* or scientist*)) OR AB((clinical OR medical*) N1 (technician* or technologist* or assistant* or scientist*)) Database ‐ ERIC S47TI(public health service* or public health agenc*) OR AB(public health service* or public health agenc*) Database ‐ ERIC S48TI(secondary trauma* or (work* N2 trauma survivor*)) OR AB(secondary trauma* or (work* N2 trauma survivor*)) Database ‐ ERIC S49TI (nursing or medical or midwifery OR premedical or paramedic or psychology or physical therapy or occupational therapy) N2 student*) OR AB (nursing or medical or midwifery OR premedical or paramedic or psychology or physical therapy or occupational therapy) N2 student*) Database ‐ ERIC S50TI(college student*) OR AB(college student*) Database ‐ ERIC S51TI((nurs* N1 graduate*) or (nurs* N1 education) or (medic* N1 train*)) OR AB((nurs* N1 graduate*) or (nurs* N1 education) or (medic* N1 train*)) Database ‐ ERIC S52S29 OR S30 OR S31 OR S32 OR S33 OR S34 OR S35 OR S36 OR S37 OR S38 OR S39 OR S40 OR S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48 OR S49 OR S50 OR S51 Database ‐ ERIC S53S28 AND S52 Database ‐ ERIC S54DE "Meta Analysis" OR DE "Evaluation Research" OR DE "Control Groups" OR DE "Experimental Groups" OR DE "Longitudinal Studies" OR DE "Followup Studies" OR DE "Program Effectiveness" OR DE "Program Evaluation" Database ‐ ERIC S55(random* or trial* or group or experiment* or PROSPECTIVE* OR longitudinal or BLIND* or CONTROL* or treatment as usual or TAU) Database ‐ ERIC S56S54 OR S55 Database ‐ ERIC S57S53 AND S56 Database ‐ ERIC
Current Controlled Trials (now ISRCTN registry; www.isrctn.com)
Searched 24 June 2019 [33 records]
Text search: (((((resilience OR hardiness OR "posttraumatic growth" OR stress OR trauma) AND (psychotherap OR relaxation OR mindfulness OR coaching OR "positive psychology" OR reappraisal OR "stress inoculation" OR "stress management" OR multimodal OR "health promotion")) OR ((resilience OR hardiness) AND (training OR program OR intervention OR promot OR prevent OR enhanc OR learn OR teach OR educat OR increas or develop OR manag OR therap OR protocol OR treat)))) AND ("health personnel" OR "health professional" OR "health worker" OR "health practitioner" OR "health provider" OR "health staff" OR students OR "human service professional")) Date assigned from 01/10/2016 to 24/06/2019
ClinicalTrials.gov (clinicaltrials.gov)
Searched 24 June 2019 [147 records]
Condition or disease = resilience OR hardiness OR posttraumatic growth OR stress OR trauma Other terms = health personnel OR health professional OR health worker OR health practitioner OR health provider OR health staff OR students OR human service professional Study type: Interventional studies (clinical trials) Intervention/treatment: resilience training OR hardiness training OR psychotherapy OR relaxation OR mindfulness OR coaching OR positive psychology OR reappraisal OR stress inoculation OR stress management OR multimodal OR health promotion Title or acronym: resilience OR hardiness OR posttraumatic growth OR stress OR trauma Study start: 01/10/2016 to 24/06/2019
WHO ICTRP (apps.who.int/trialsearch)
Searched 24 June 2019 [145 records]
title = health personnel OR health professional OR health worker OR health practitioner OR health provider OR health staff OR students OR human service professional intervention = resilience OR hardiness OR posttraumatic growth OR stress OR trauma OR psychotherapy OR relaxation OR mindfulness OR coaching OR positive psychology OR reappraisal OR stress inoculation OR stress management OR multimodal OR health promotion Recruitment status: ALL Date of registration: 01/10/2016 – 24/06/2019
Appendix 10. Data collection/extraction sheet (items according to Li 2019)
| Source |
|
| Eligibility |
|
| Methods |
|
| Participants |
|
| Interventions |
|
| Outcomes |
|
| Results |
|
| Miscellaneous aspects |
|
| CI: confidence interval;ID: identifier; SD: standard deviation. | |
Footnotes
aFull description required for standard items in ‘Risk of bias’ tool.
Appendix 11. Criteria for 'Risk of bias’ assessment in included RCTs (according to Higgins 2011a)
| Item | Judgment | Description |
| 1. Random sequence generation (selection bias). We described the method used to generate the allocation sequence in sufficient detail for each included trial to allow an assessment of whether it should have produced comparable groups | Low risk | The investigators described a random component in the sequence generation process such as:
*Minimisation may be implemented without a random element (treatment sums are equal), and this is considered to be equivalent to being random |
| High risk | The researchers described a (systematic or non‐systematic) non‐random component in the sequence generation process such as:
|
|
| Unclear risk | Insufficient information provided to permit a judgement of ‘Low risk’ or ‘High risk’. | |
| 2. Allocation concealment (selection bias). For each RCT we described the method used to conceal the allocation sequence in sufficient detail to determine whether intervention allocations could have been foreseen in advance of, or during, enrolment | Low risk | Participants and investigators enrolling participants could not have foreseen assignment because one of the following, or an equivalent method, was used to conceal allocation:
|
| High risk | Participants or investigators enrolling participants could possibly have foreseen assignment and thus introduced selection bias because one of the following methods was used:
|
|
| Unclear risk | Insufficient information was provided to permit a judgement of ‘Low risk’ or ‘High risk’. This was usually the case if the method of concealment was not described or not described in sufficient detail to allow a definite judgement (e.g. if the use of assignment envelopes was described, but it remained unclear whether envelopes were sequentially numbered, opaque and sealed) | |
| 3. Blinding of participants and personnel (performance bias): objective outcomes. For each included trial we described all methods used to blind trial participants and personnel from knowledge of which intervention a participant received. We provided any information relating to whether the intended blinding was effective. We assessed blinding separately for different classes of outcomes. Outcomes were divided into objective (e.g. cortisol) and subjective (e.g. self‐reported resilience and other psychological outcomes). We considered the same outcomes at different time points | Low risk | Any one of the following:
|
| 4. Blinding of participants and personnel (performance bias): subjective outcomes. For each included trial we described all methods used to blind trial participants and personnel from knowledge of which intervention a participant received. We provided any information relating to whether the intended blinding was effective. We assessed blinding separately for different classes of outcomes. Outcomes were divided into objective (e.g. cortisol) and subjective (e.g. self‐reported resilience and other psychological outcomes). We considered the same outcomes at different time points | Low risk | Blinding of participants and intervention providers, and unlikely that the blinding could have been broken |
| High risk | Any one of the following:
|
|
| Unclear risk | Insufficient information provided to permit a judgement of ‘Low risk’ or ‘High risk’ | |
| 5. Blinding of outcome assessors (detection bias): objective outcomes. For each included trial we described all methods used to blind outcome assessors from knowledge of which intervention a participant received. We provided any information relating to whether the intended blinding was effective. We assessed blinding separately for different classes of outcomes. Outcomes were divided into objective (e.g. cortisol) and subjective (e.g. self‐reported resilience and other psychological outcomes). We considered the same outcomes at different time points | Low risk | Any one of the following:
|
| 6. Blinding of outcome assessors (detection bias): subjective outcomes. For each included trial we described all methods used to blind outcome assessors from knowledge of which intervention a participant received. We provided any information relating to whether the intended blinding was effective. We assessed blinding separately for different classes of outcomes. Outcomes were divided into objective (e.g. cortisol) and subjective (e.g. self‐reported resilience and other psychological outcomes). We considered the same outcomes at different time points | Low risk | Any one of the following:
|
| High risk | Any one of the following:
|
|
| Unclear risk | Insufficient information provided to permit a judgment of ‘Low risk’ or ‘High risk’ | |
| 7. Incomplete outcome data (attrition bias). For each RCT we described the completeness of outcome data for each main outcome, including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported, the numbers included at each stage (compared with the total number of participants randomised), reasons for attrition or exclusions (where reported), and whether missing data were balanced across groups or were related to outcomes. Where sufficient data were reported, or could be provided by the study authors, we re‐included the missing data in the analyses | Low risk | Any one of the following:
|
| High risk | Any one of the following:
|
|
| Unclear risk | Insufficient reporting of attrition or exclusions to permit a judgement of ‘Low risk’ or ‘High risk’ (e.g. number randomised not stated, no reasons for missing data provided, number of dropouts not reported for each group) | |
| 8. Selective outcome reporting (reporting bias). For each included trial we described how the possibility of selective outcome reporting was examined, and what was found | Low risk | Any one of the following:
|
| High risk | Any one of the following:
|
|
| Unclear risk | Insufficient information provided to permit a judgement of ‘Low risk’ or ‘High risk. | |
| RCT(s): randomised controlled trial(s) | ||
Appendix 12. Detailed results of both searches
Using the original search strategy (Appendix 8), our database searches retrieved 32,184 records (including 1601 from trials registers). We found an additional 100 records by searching other resources. Following de‐duplication, we screened the remaining 20,410 records by title and abstract. We deemed 18,116 records to be irrelevant and sought the full texts of the remaining 2294 records for further assessment. In terms of title/abstract screening, a good agreement (kappa = 0.70) between review authors was achieved.
We retrieved 2294 full text reports. Based on the original eligibility criteria of this review (see Differences between protocol and review), 251 studies met the inclusion criteria. We identified 18 ongoing studies and 46 studies awaiting classification (in total: 315 studies from 376 reports). We excluded 1918 reports as irrelevant (Excluded studies). The full text screening for the first search resulted in excellent inter‐rater reliability (kappa = 0.95). After revising the eligibility criteria to focus on healthcare professionals based on a broad definition of this target group (including healthcare students; see Differences between protocol and review), we re‐assessed the studies found by the initial screening. From these, we identified 49 studies that were performed in any of these groups. We also identified one ongoing study and 10 studies awaiting classification. Finally, after revising the eligibility criteria to focus on healthcare students, we also reassessed these 60 studies. From these, we identified 15 studies that fulfilled our inclusion criteria (Criteria for considering studies for this review). We also identified 10 studies awaiting classification (see Studies awaiting classification). The results of the original search are presented in Figure 31.
4.
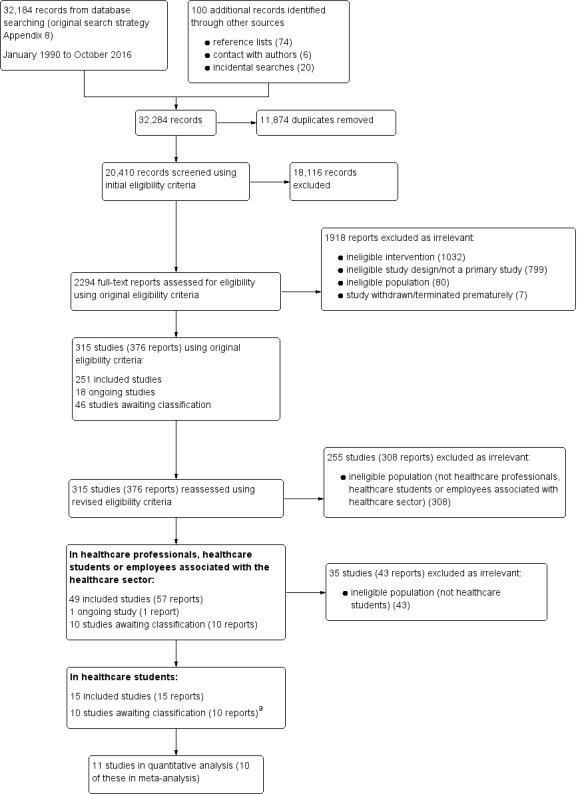
Study flow diagram for first searches (January 1990 to October 2016).
aOne ongoing study in the box above is now awaiting classification.
From 2016 onwards, we refined our search strategy to focus broadly on the healthcare sector (including healthcare students; Appendix 9). The searches yielded 6116 records (5553 + 563). Based on these broad criteria, we identified six additional reports of studies identified by earlier searches. We newly identified 31 studies, eight ongoing studies and 19 studies awaiting classification. We re‐assessed these 58 studies according to the narrower population which is the focus of this review (healthcare students only). From these, we identified 15 studies that fulfilled our inclusion criteria. We also identified three ongoing studies and 12 studies awaiting classification. The full text screening for the top‐up searches also resulted in excellent inter‐rater reliability (kappa = 1). The results of the top‐up searches are presented in Figure 32.
5.
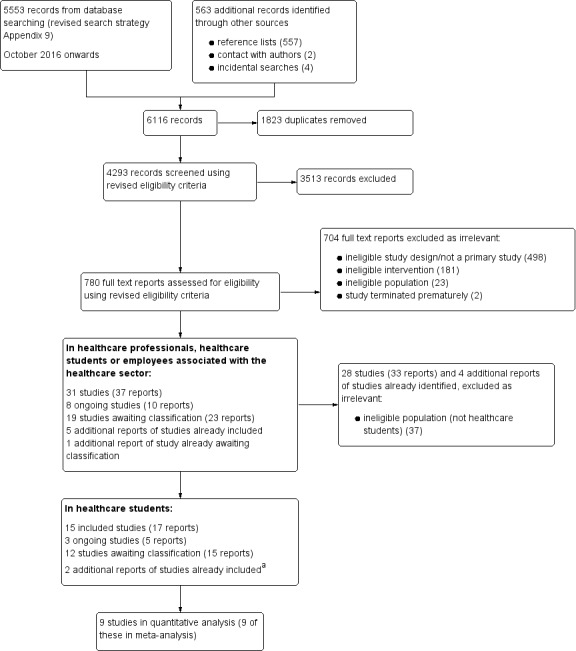
Study flow diagram for second searches (October 2016 onwards). aPeng 2014; Galante 2018.
Appendix 13. References concerning the description of included studies
| Key characteristic | Number of studies with respective references |
| Location |
|
| Settings (venue or implementation sites of interventions) |
|
| Participants ‐ number randomised |
|
| Participants ‐ age |
|
| Participants ‐ sex |
|
| Participants ‐ target group |
|
| Participants ‐ mental health assessment at baseline |
|
| Intervention ‐ setting |
|
| Intervention ‐ delivery format |
|
| Intervention ‐ training intensity |
|
| Intervention ‐ theoretical foundation | See Appendix 14 |
| Comparator |
|
| Funding sources |
|
Appendix 14. Intervention content depending on theoretical foundation
| Theoretical foundation (number of studies) | Studies | Characteristics of studies within theoretical foundation | Intervention content |
| Mindfulness‐based resilience interventions (8) | Barry 2019; Chen 2018a; Erogul 2014; Galante 2018; Kelleher 2018; Samouei 2015; Smeets 2014; Warnecke 2011 |
|
|
| Unspecific resilience interventions (7) | Akbari 2017; Anderson 2017; Houston 2017; Mathad 2017; Mejia‐Downs 2016; Miu 2016; Stephens 2012 |
|
|
| Combined resilience interventions (6) | Delaney 2016; Goldstein 2019; ISRCTN64217625; Kötter 2016; Recabarren 2019; Victor 2018 |
|
|
| Positive psychology (4) | Geschwind 2015; Mueller 2018; Venieris 2017; Wang 2012 |
|
|
| Cognitive‐behavioural therapy (3) | Peng 2014; Porter 2008; Sahranavard 2018 |
|
|
| Coaching approaches (2) | Waddell 2005; Waddell 2015 |
|
|
Appendix 15. Assessment of publication bias for the primary outcomes
| Outcome, time point (number of included studies) | Assessment of publication bias |
| Resilience, post‐intervention (9 studies)a |
|
| Anxiety, post‐intervention (7 studies)a |
|
| Depression, post‐intervention (6 studies)a |
|
| Stress or stress perception, post‐intervention (7 studies)a |
|
| Well‐being or quality of life, post‐intervention (4 studies)a |
|
| df: Degrees of freedom; P: P value of Egger's test; t: T value of Egger's test | |
Footnotes
aDespite there being fewer than 10 studies included in the meta‐analysis, we drew a funnel plot and inspected it for asymmetry, and conducted Egger's test for the purpose of assessing the certainty of the evidence using the GRADE approach. bAccording to the GRADE approach (Guyatt 2011e), publication bias should be suspected when available evidence comes from a number of small studies, most of which have been commercially funded or where there are perceived conflicts of interest.
Appendix 16. Funnel plots
In order to assess reporting bias and to examine potential funnel plot asymmetry (see Assessment of reporting biases), we drew contour‐enhanced funnel plots for the comparison between resilience intervention and control for the five primary outcomes at post‐test (see Effects of interventions and Appendix 15). We drew a contour‐enhanced funnel plot for resilience at post‐intervention (Figure 33), which is rather symmetrical in shape and shows no clear visual evidence of asymmetry. The same applies to the contour‐enhanced funnel plot for anxiety at post‐test (Figure 34). The contour‐enhanced funnel plot for depression at post‐test (Figure 35) is also rather symmetrical in shape and provides no visual evidence of asymmetry. We also found rather symmetrical, contour‐enhanced funnel plots and no visual evidence of asymmetry for stress or stress perception at post‐intervention (Figure 36) and well‐being or quality of life (Figure 37).
6.
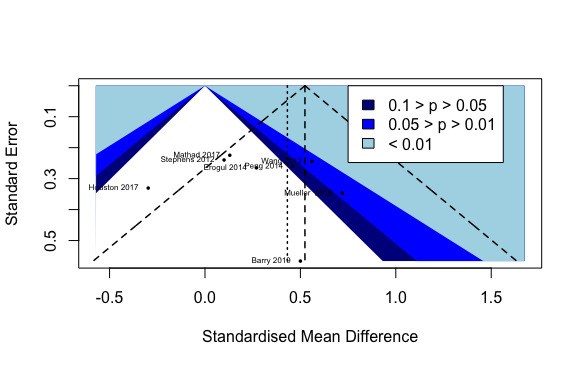
Contour‐enhanced funnel plot of comparison 1: Resilience intervention vs control, healthcare students, Resilience: post‐intervention.
7.
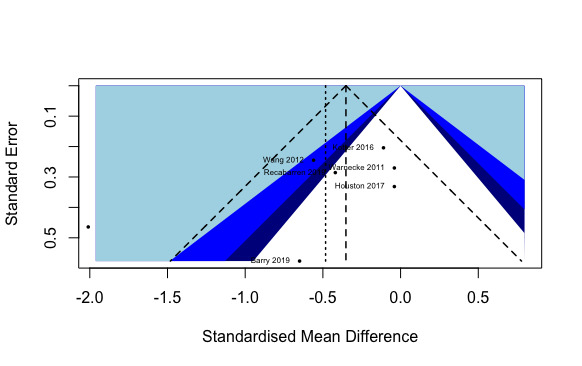
Contour‐enhanced funnel plot of comparison 1: Resilience intervention vs control, healthcare students, Anxiety: post‐intervention.
8.
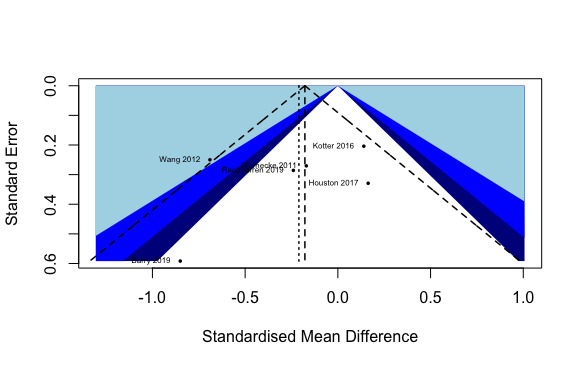
Contour‐enhanced funnel plot of comparison 1: Resilience intervention vs control, healthcare students, Depression: post‐intervention.
9.
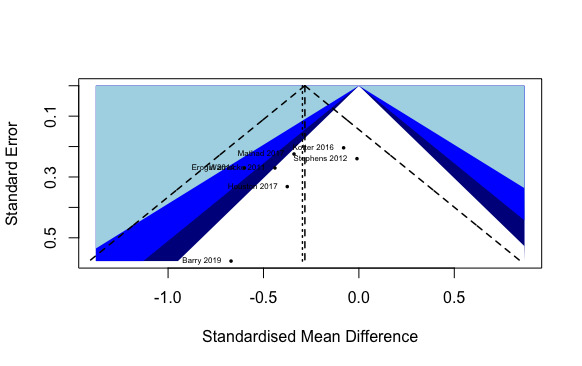
Contour‐enhanced funnel plot of comparison 1: Resilience intervention vs control, healthcare students, Stress or stress perception: post‐intervention.
10.
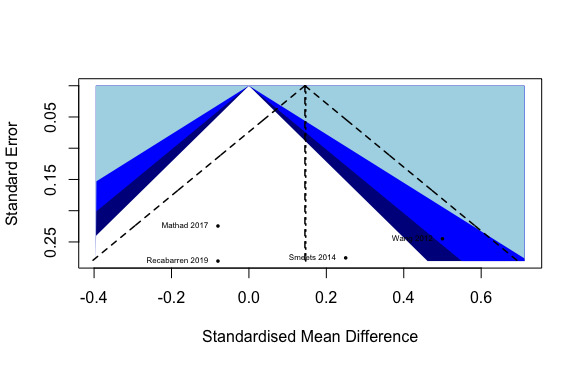
Contour‐enhanced funnel plot of comparison 1: Resilience intervention vs control, healthcare students, Well‐being or quality of life: post‐intervention.
Appendix 17. Further details on the overall completeness and applicability of evidence
-
Participants:
-
Study field:
The included studies were conducted mainly in healthcare students who already dealt with the provision of direct medical care, such as nursing or midwifery students (18/30 studies).
-
Mental health at baseline:
40% of the 30 studies assessed mental health at baseline.
All studies measuring mental functioning used self‐reported (screening) measures covering one or a small number of mental dysfunctions.
Comprehensive baseline diagnostics of mental health by the use of a structured interview were only conducted in one study (Recabarren 2019).
Overall, drawing from those studies assessing mental health, the severity of impairment ranged between no mental symptoms (e.g. normal range, Barry 2019) to increased levels of mental dysfunctions (Miu 2016; Victor 2018).
-
Study location:
North America (15 studies), Europe (7 studies), Asia (including the Near East, 6 studies), only two studies from Australia.
High‐income countries in 24 studies: Australia, Belgium, Canada, Germany, The Netherlands, Switzerland, UK, USA
Upper‐middle income countries in five studies: China, Iran
Lower‐middle income country in one study: India
-
-
Comparators:
There was large heterogeneity in active and attention controls by setting, delivery format and content, rendering the comparability between single‐study comparisons difficult.
-
Interventions:
The evidence found is restricted to certain types of intervention settings, delivery formats, training intensities and theoretical foundations.
Seventeen of the 30 studies assessed the effectiveness of resilience interventions in group settings that were delivered face‐to‐face.
Most of the interventions were of high intensity (11/30: > 12 hours or sessions) or low intensity (10/30; ≤ 5 hours or ≤ 3 sessions). Treatment durations ranging considerably, from a 20‐minute single session to 40 hours in total.
Except for stress inoculation, problem‐solving training, ACT and AIT, all prespecified theoretical foundations (Helmreich 2017) have been tested in RCTs found in this review.
The number of RCTs varies, with a relative balance between studies investigating mindfulness‐based training (8/30), unspecified interventions (7/30) and combined theoretical foundations (6/30; e.g. CBT and positive psychology).
-
Outcomes:
Although there is still no consensus about the definition of resilience, two aspects are viewed as essential: the exposure to substantial risk or adversity and the maintenance or fast recovery of mental health despite this adversity (e.g. Earvolino‐Ramirez 2007). By considering studies in healthcare students – a target group often exposed to significant stressors – that assessed resilience or another measure of psychological adjustment, we ensured a greater homogeneity between the included studies.
Potential adverse or undesired effects were not specified in most included studies (see Adverse events in Effects of interventions). Three studies reported no adverse or undesired effects (unavailable data for fourth study).
Since most included studies had small sample sizes, the attrition bias found for nine studies has to be interpreted with caution.
Appendix 18. Prevention of potential biases by the search methods of this review
We performed extensive searches of relevant databases and checked reference lists of reviews and included studies. We also considered grey literature (e.g. conference abstracts). The search process was designed in conjunction with, and supervised by, the Cochrane Developmental, Psychosocial and Learning Problems (CDPLP) Information Specialist, in order to minimise bias in the acquisition of potentially relevant references. We contacted the authors of (included) studies to ask, for example, for full texts or additional data where reported data were insufficient or missing. In all phases of the review process, we repeatedly (at least twice) tried to contact the study authors by email, when needed.
Correspondence with the authors about data analysis was required for 25 included studies. For 11 studies, the replies we received allowed us to include those studies in the quantitative analyses (e.g. Barry 2019).
Data and analyses
Comparison 1. Resilience interventions versus control conditions in healthcare students: primary and secondary outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Resilience: post‐intervention | 9 | 561 | Std. Mean Difference (IV, Random, 95% CI) | 0.43 [0.07, 0.78] |
| 1.2 Resilience: short‐term follow‐up (≤ 3 months) | 4 | 209 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.44, 0.84] |
| 1.3 Resilience: medium‐term follow‐up (> 3 to ≤ 6 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.4 Anxiety: post‐intervention | 7 | 362 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐0.84, ‐0.06] |
| 1.5 Anxiety: short‐term follow‐up (≤ 3 months) | 2 | 91 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐1.32, ‐0.45] |
| 1.6 Depression: post‐intervention | 6 | 332 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.52, 0.11] |
| 1.7 Depression: short‐term follow‐up (≤ 3 months) | 4 | 226 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.65 [‐1.26, ‐0.04] |
| 1.8 Stress or stress perception: post‐intervention | 7 | 420 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.48, ‐0.09] |
| 1.9 Stress or stress perception: short‐term follow‐up (≤ 3 months) | 2 | 113 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.79, 1.06] |
| 1.10 Stress or stress perception: medium‐term follow‐up (> 3 to ≤ 6 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.11 Well‐being or quality of life: post‐intervention | 4 | 251 | Std. Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.14, 0.43] |
| 1.12 Well‐being or quality of life: short‐term follow‐up (≤ 3 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.13 Social support: post‐intervention | 2 | 121 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.15, 0.57] |
| 1.14 Social support: short‐term follow‐up (≤ 3 months) | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | 0.23 [‐0.18, 0.64] |
| 1.15 Optimism: post‐intervention | 2 | 66 | Std. Mean Difference (IV, Random, 95% CI) | 0.29 [‐0.20, 0.78] |
| 1.16 Self‐efficacy: post‐intervention | 5 | 219 | Std. Mean Difference (IV, Random, 95% CI) | 0.51 [0.14, 0.88] |
| 1.17 Self‐efficacy: short‐term follow‐up (≤ 3 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.18 Active coping: post‐intervention | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.19 Active coping: short‐term follow‐up (≤ 3 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.20 Self‐esteem: short‐term follow‐up (≤ 3 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.21 Positive emotions: post‐intervention | 2 | 112 | Std. Mean Difference (IV, Random, 95% CI) | 0.51 [0.01, 1.01] |
| 1.22 Positive emotions: short‐term follow‐up (≤ 3 months) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.23 Resilience: post‐intervention, sensitivity analysis (fixed‐effect analysis) | 9 | 561 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.52 [0.36, 0.69] |
| 1.24 Anxiety: post‐intervention, sensitivity analysis (fixed‐effect analysis) | 7 | 362 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.35 [‐0.57, ‐0.14] |
| 1.25 Depression: post‐intervention, sensitivity analysis (fixed‐effect analysis) | 6 | 332 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.18 [‐0.40, 0.04] |
| 1.26 Stress or stress perception: post‐intervention, sensitivity analysis (fixed‐effect analysis) | 7 | 420 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐0.48, ‐0.09] |
| 1.27 Well‐being or quality of life: post‐intervention, sensitivity analysis (fixed‐effect analysis) | 4 | 251 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.14 [‐0.10, 0.39] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Akbari 2017.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
|
| Participants |
Country: Iran Setting: university Age: mean = 21.58 (SD = 5.12); range = 18 ‐ 27 years Sample size (randomised): 30 Sex: 18 women, 12 men Comorbidity (mean (SD) of respective measures in indicated, if available): not specified Population description: nursing and midwifery students Inclusion criteria: 1) willingness to participate in the study; 2) no history of mental illnesses; 3) low happiness score; 4) high aggression score Exclusion criteria: 1) unwillingness to participate in the study; 2) diagnosed psychological disorders; 3) use of psychotropic medications and sedatives Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: resilience training (n = 15)
Control: no intervention (n = 15) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; only 2) post‐intervention reported Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the study authors to get the information about potential attrition and missing data in the study, the pre‐test means and SDs for both outcomes. We also inquired whether the means reported for happiness in Table 2 for the 2 groups were correct (lower score in IG compared to CG, but in the text the authors reported an increase of happiness through resilience training). We received no response to 2 inquiries. Study start/end date: not specified; study conducted during academic years 2013 ‐ 2014 Funding source: Islamic Azad University of Rasht Branch (see trial registration) Declaration of interest: not specified Ethical approval needed/obtained for study: approved by the Islamic Azad University (51172910725013) Comments by study authors: paper obtained from a research project approved by the Islamic Azad University of Rasht Branch; registered in the Iranian Registry of Clinical Trials (IRCT2016112231016N1) Miscellaneous outcomes by the review authors: not relevant Correspondence: Bahman Akbari; Department of Psychology, Rasht branch, Islamic Azad University, Rasht, Iran; Bakbari44@yahoo.com |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Then they were randomly assigned to the intervention and control groups (15 per group)." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; no information about comparability of groups at baseline or respective analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: insufficient reporting of attrition/exclusions to permit judgement of ‘Low risk’ or ‘High risk’ (e.g. unclear if there were any missing data in the 2 groups; unclear how many participants were analysed) |
| Selective reporting (reporting bias) | High risk | Judgement comment: trial registration (IRCT2016112231016N1) available and all of the study’s prespecified outcomes have been reported but only post‐intervention assessment is reported and time effect is not considered in MANCOVA |
Anderson 2017.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
|
| Participants |
Country: Canada Setting: online, self‐guided intervention Age: mean = 25.5 years Sample size (randomised): 138 Sex: 50 women, 88 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: primary care paramedic (PCP) student volunteers Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: self‐paced online resiliency training programme (n = 81)
Control: not specified (n = 57) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention (prior to practicum experience and resiliency training); 2) post‐intervention (after resiliency training and following completion of practice experience) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to get the information about any missing data (withdrawals/exclusions) in the study, the number of participants analysed in each group and the SDs for the outcomes reported in Table II. We received no response to 2 inquiries. Study start/end date: not specified Funding source: partially funded by the Canadian Mental Health Association, Campus Capacity Development Grant, and partially by the Justice Institute of British Columbia Declaration of interest: The authors state that there are no conflicts of interest Ethical approval needed/obtained for study: not specified Comments by study authors: not relevant Miscellaneous outcomes by the review authors: not relevant Correspondence: Gregory S. Anderson; Office of Applied Research and Graduate Studies, Justice Institute of British Columbia (JIBC), 715 McBride Blvd., New Westminster, BC V3L 5T4, Canada; aganderson@jibc.ca |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Using a randomized control trial, cohorts of students were randomly assigned to either the experimental (with the online course as an intervention) or control group. Two cohorts were randomly assigned to receive the online course intervention designed to build capacity for resilient behaviour, while two cohorts acted as the control group." Quote: "Baseline demographic results were examined using bivariate comparisons between the control and experimental, and all were found to be statistically insignificant at p < 0.05 which suggests that there were no differences between the two groups on the pre‐test demographic variables." Quote: "Prior to the intervention there were no significant differences in total resilience or any of the sub‐scales (self‐ reliance, meaningfulness, equanimity, perseverance, and existential aloneness)." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; verified baseline comparability of groups for sociodemographic characteristics and outcome variables on the basis of analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | Unclear risk | Judgement comment: insufficient information about blinding of participants and personnel to permit judgement of ‘Low risk’ or ‘High risk’ (online self‐guided intervention) |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Unclear risk | Judgement comment: insufficient information about blinding of outcome assessment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: insufficient reporting of attrition/exclusions to permit judgement of ‘Low risk’ or ‘High risk’ (e.g. unclear if there were any missing data and if missing data were imputed, for example; number of participants analysed in each group not stated) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Barry 2019.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: Individuals Power (power & sample size calculation, level of power achieved): To ensure sufficient statistical power to enable comparison of treatments, the trialists sought to recruit at least 84 participants, based on the related trial previously (Warnecke 2011); that trial was powered to detect a 4‐point difference (SD 0.6) in the Perceived Stress Scale (PSS) score, using a 2‐tailed test, α = 0.05 and power = 0.80, and allowing for a 10% dropout; this calculation was based on data from a study of university students which found a mean pretest PSS score of 18.11 (SD = 6.19); while only 66 participants were recruited in that study, statistical differences were still detected between the groups Imputation of missing data: no imputation of missing data specified; intervention designed as “intention to treat” study (i.e. adherence to daily practice for whole period not essential); intention‐to‐treat analysis (i.e. including participants who withdrew during study period) |
|
| Participants |
Country: Australia
Setting: CD‐guided intervention; sealed trial packs are posted to participants, i.e. training setting at home
Age: mean = 38.14 (SD = 11.33) years
Sample size (randomised): 82, including 17 doctoral students in health professions
Sex: 61 women, 21 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline:
Population description: doctoral candidates Inclusion criteria: 1) 18 years of age or older; 2) studying on campus; 3) having completed > 3 months of candidature Exclusion criteria: 1) participants with score of 30+ in K10 questionnaire for psychological distress (indicates severe levels of distress; participants immediately referred to appropriate health service provider; n = 3) Attrition (withdrawals and exclusions): pre‐intervention: 1 did not return survey (IG); during study period: 9 withdrawals (IG: 8, CG: 1); post‐intervention: same 9 participants did not return survey (IG: 8, CG: 1) Reasons for missing data: not specified |
|
| Interventions |
Intervention: guided mindfulness practice (n = 43)
Control: no intervention (n = 39)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to ask for the subgroup outcome data of doctoral candidates in health professions (Barry 2019 [pers comm]). Study start/end date: not specified; recruitment in July 2015 Funding source: This research was conducted with funding from the authors’ university Declaration of interest: The authors have no conflicts of interest to report Ethical approval needed/obtained for study: received approval from the Human Research Ethics Committee (H14833) of the University of Tasmania Comments by study authors: not relevant Miscellaneous outcomes by the review authors: response from Dr Barry concerning health professions: “Yes, several of the doctoral candidates in our study were in health related areas of study. In fact, they represented about 25% of the participants.“; subgroup data for doctoral candidates in health professions sent from authors Correspondence: Karen May Barry, PhD; Tasmanian Institute of Agriculture, University of Tasmania, Private Bag 98, Hobart, Tasmania 7001, Australi; aKaren.Barry@utas.edu.au |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Participants were block randomized, with block sizes of two, to either the intervention or usual care control." Quote: "As reported elsewhere, for all recruited participants the mean age was 38 years, 81.5% were female and 22.2% were international candidates. When randomly allocated to the control or intervention group, there were no statistically significant differences in baseline characteristics, with the exception of significantly lower total PsyCap for the intervention participants (Table 1)." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’ (method of random‐sequence generation is not described); verified baseline comparability of groups for sociodemographic characteristics and most outcome variables except for total PsyCap score (significantly lower in IG compared to CG, P = 0.049) |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The survey questionnaire and a sealed trial pack (including mindfulness CD, instructions, and record sheet for the intervention group, while an empty CD case and information sheet was included for the control group) were posted to the participants. Participants were instructed to complete the baseline questionnaire prior to opening the sealed trial pack. This ensured allocation to the control or intervention group was concealed until after baseline data were collected." Judgement comment: participants could probably not foresee assignment (sealed trial pack that participants are instructed to open only after completing the baseline questionnaire); insufficient information about allocation concealment from investigators enrolling participants to permit judgement of 'Low risk' or 'High risk' |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "A single‐blinded randomized control trial of a 30‐min mindfulness intervention 17 was conducted" Quote: "Due to the nature of the intervention, it was not possible to conduct a double‐blinded trial." Judgement comment: single‐blind study (unclear if study personnel or participants were blinded) and the outcome could be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Unclear risk | Judgement comment: insufficient information about blinding of outcome assessment to permit judgement of ‘Low risk’ or ‘High risk’; unclear if participants' responses to questionnaires were affected by lack of blinding, since it is unclear if study personnel or participants were blinded in the single‐blind study (see performance bias) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "One participant withdrew from the control group of the study during the trial period and nine withdrew from the intervention group, including one prior to the trial and eight during the trial. Therefore, 72 participants progressed through the whole trial (Figure 1)." Quote: "The intervention was designed as an “intention to treat” trial, therefore adherence to the daily practice for the whole period was not essential." Judgement comment: reasons for missing data likely to be related to true outcome with imbalance in amount of missing data between groups (pre‐intervention: IG: 1 did not return survey vs CG: n = 0; IG: 8 withdrew during study period and did not return post‐intervention survey vs CG: 1); intervention designed as intention‐to‐treat (i.e. participants included irrespective of adherence to daily practice); but available‐case analysis (only participants for whom outcomes were obtained at pre‐ and post‐intervention surveys) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Chen 2018a.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified in conference abstract Imputation of missing data: probably no imputation of missing data; only 9 did not withdraw and completed all surveys, i.e. yielding an analytic sample of 9 (due to small sample size, no analysis of hypotheses) |
|
| Participants |
Country: USASetting: not specifiedAge: not specified Sample size (randomised): 22Sex: not specifiedComorbidity (mean(SD) of respective measures in indicated, if available) at baseline: not specified Population description: fall and spring first‐semester baccalaureate students in nursing (BSNs) Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): n = 9/22 withdrawals (not specified which group); 9 of 13 remaining participants completed all surveys (not specified which group), i.e. 4 with incomplete surveys Withdrawals and exclusions: 9/22 withdrawals (not specified which group); 9 of 13 remaining participants completed all surveys (not specified which group), i.e. 4 with incomplete surveys |
|
| Interventions |
Intervention: Brief Mindfulness‐based Compassion (MSC) (n randomised not specified)
Control: wait‐list control (n randomised not specified)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 1‐month follow‐up (at 8 weeks after baseline, i.e. 4 weeks after 4‐week intervention); time points reported not specified Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to see if the study was already published (Kelleher 2019 [pers comm]). Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: not specifiedComments by study authors: not relevantMiscellaneous outcomes by the review authors: not relevantCorrespondence: Catherine Kelleher; University of Maryland, School of Nursing; kelleher@umaryland.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (see conference abstract): "During year 1, participants were randomized to MBSR and MSC programs as originally planned but enrollment was low. During year 2, the randomized design was modified to drop the MBSR arm, focus only on the MSC program, and use a control group in which participants would get the MSC program in a consolidated half‐day program at the beginning of the following semester. The simplified design permitted testing student interest in signing up for an MSC study and the impact on enrollment if there was no uncertainty about being randomized to 1 of 2 programs which met at different times." Judgement comment: based on conference abstract, insufficient information about random‐sequence generation to permit judgement of 'Low risk' or 'High risk'; no judgement on baseline comparability possible |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: based on conference abstract, insufficient information about allocation concealment to permit judgement of 'Low risk' or 'High risk'. |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: based on conference abstract, blinding of participants probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: based on conference abstract, insufficient information about blinding of outcome assessment; but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about the intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote (see conference abstract): "In year 2, total recruitment=22, total withdrawal=9, and 9 of the 13 participants completed all surveys, yielding an analytic sample=9. Due to small sample size, analysis for both pilot years was limited to descriptive statistics, and hypotheses could not be tested" Judgement comment: unclear if reasons for missing data likely to be related to true outcome (number of participants randomised to each group and number of dropouts in each group not stated); probably per‐protocol analysis and available‐case analysis (analyses restricted to descriptive statistics and no testing of hypotheses due to withdrawals and incomplete surveys; i.e. only 9 participants who did not withdrew and completed the surveys were considered) |
| Selective reporting (reporting bias) | Unclear risk | Judgement comment: no judgement possible based on conference abstract |
Delaney 2016.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): For this pilot study, a sample size goal for initial testing of the stress management intervention was 30 to 40 participants. POST‐HOC POWER ANALYSES: performed on nonsignificant outcomes of perceived stress, resilience, GPA, and attrition to determine if there was sufficient power to accept nonsignificant results; power analysis based on the primary dependent variable in this study, perceived stress. When applied to a large national sample, the mean and SD of the PSS were 19.92 and 7.49, respectively. If the PSS has a comparable SD when used in this study, a sample size of 72 participants would be needed to achieve 80% power; further power analyses revealed that to obtain sufficient power for the other study variables, BRS, GPA, and attrition a sample size of 72 to 100 participants would be required; analyses confirmed that the study was UNDERPOWERED to detect meaningful differences in the study outcomes Imputation of missing data: not specified |
|
| Participants |
Country: USA Setting: 2 large universities in Connecticut (simulation laboratories) Age: mean age not reported; 33 participants aged 18 ‐ 21 and 7 participants aged ≥ 22 years Sample size (randomised): 40 Sex: 4 women, 36 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: junior nursing students from 2 universities in Connecticut Inclusion criteria: 1) English‐speaking junior nursing students age 18+; 2) currently enrolled in a baccalaureate nursing programme at one of the participating schools; 3) willing to participate Exclusion criteria: not specified Attrition (withdrawals and exclusions): 3 withdrawals (IG: 2; CG: 1) Reasons for missing data: for 3 withdrawals: 2 in IG unable to attend 2. NURSE session; 1 in CG had other academic commitments |
|
| Interventions |
Intervention: NURSE (Nurture nurse, Use resources, foster Resilience, Stress and Environment management) (n = 20)
Control: active control (n = 20)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (= end of fall semester); 3) 4‐month follow‐up (4 months post‐intervention, = end of spring semester); attrition rates only assessed at post‐intervention and 4‐month follow‐up Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for whether the 2 dropouts occurred in the IG or CG, and to get the means and SDs for resilience and perceived stress in both groups with the number of participants analysed, respectively. We also asked if the treatment duration in the NURSE group was also 2 months. We received no response to 2 inquiries. Study start/end date: not specified Funding source: The authors thank Sigma Theta Tau, International Mu Chapter, for providing funding for this study. Declaration of interest: not specified Ethical approval needed/obtained for study: Study protocols were approved by the IRBs at the 2 universities participating in this study before participants were recruited. Comments by study authors: Authors thank Jean Watson, PhD, Director of the Watson Caring Science Institute, for consulting on this project Miscellaneous outcomes by the review authors: not relevant Correspondence: Colleen Delaney, PhD; University of Connecticut, 231 Glenbrook Road, Storrs, CT 06269, USA; colleen.delaney@uconn.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Students were randomly assigned to the NURSE intervention (n = 20) or Attention Control Condition (n = 20)." Quote: "No statistically significant differences between the control and intervention groups across baseline demographic characteristics were found." Quote: "In addition, no significant differences between groups were found in the baseline scores for perceived stress, resilience, and GPA." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; verified baseline comparability of groups for sociodemographic characteristics (see Table 2; all Ps > 0.338) and outcomes of interest (resilience, perceived stress, GPA) on the basis of analysis (self‐reported knowledge only in IG) |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention), but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to face‐intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: insufficient information about blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment to permit judgement of ‘Low risk’ or ‘High risk’ (unclear if study personnel who conducted the in‐person interview, assessments immediately post‐intervention and follow‐up telephone interview was blinded); but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Thirty‐seven (37) students completed the study, 19 in the intervention group and 18 in the control group." Quote: "Three students dropped out of the study (two intervention students were unable to attend the second NURSE session and one control group student had other academic commitments)." Judgement comment: reasons for missing data unlikely to be related to true outcome with relative balance in missing data between groups (IG: 2 unable to attend 2. NURSE session; CG: 1 due to other academic commitments); number of participants analysed in each group not specified |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Erogul 2014.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): A sample size calculation determined that 26 participants per group would be required to detect a difference with an effect size of 0.8, with a power of 80% at significance level of 0.05; in part no significant results, according to publication may be due to study being underpowered Imputation of missing data: no imputation of missing data; per‐protocol analysis (only participants who took part in allocated intervention) |
|
| Participants |
Country: USA Setting: SUNY Downstate School of Medicine in Brooklyn Age: mean = 23.5 (SD = 1.7) years Sample size (randomised): 59 (not specified; according to authors at baseline) Sex: 26 women, 33 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: both control and treatment groups statistically comparable to the norm for resilience, perceived stress and self‐compassion Population description: first‐year class of medical students Method of recruitment: recruited from 2010 ‐ 2011 first‐year class of medical students at SUNY Downstate School of Medicine in Brooklyn, New York Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): after replacement of 22 participants (IG: 10, CG: 10) who refused to participate in allocated intervention: 2 dropouts (IG: 1/29 (3.4%); CG: 1/30 (3.3%); information about 1 dropout in CG received from authors) Reasons for missing data: 1 dropout from IG: scholastic reasons; for other withdrawals unclear; reasons for refusal of 22 randomised participants not specified |
|
| Interventions |
Intervention: abridged MBSR (initially randomised: 39; after refusal of 10 randomised participants to take part in allocated group: n = 29)
Control: no intervention (initially randomised: 42; after refusal of 12 randomised participants to take part in allocated group: n = 30) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (at conclusion of intervention); 3) 6‐month follow‐up (6 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted authors for the number of participants randomised in total and to each group (refusals from participants after randomisation) as well as the number of participants analysed at each time point (Erogul 2018 [pers comm]) Study start/end date: study carried out in March of the first year of medical school; exact study dates not specified Funding source: grant from the Arnold P Gold Foundation Declaration of interest: The authors report no conflict of interest Ethical approval needed/obtained for study: approved by the SUNYDownstate IRB Comments by authors: checklist of Items for Reporting Trials of Nonpharmacologic Treatments in appendix Miscellaneous outcomes by the review authors: information received from authors: "We had: 30 controls 29 treatment at the start of the study. By the end, because of attrition of one individual from each arm we had 29 controls, 28 study subjects = 57 participants total analyzed" Correspondence: Mert Erogul; Department of Emergency Medicine, SUNY Downstate School of Medicine, 155 Lafayette Ave #1a, Brooklyn, NY 11238; erogul1@gmail.com |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The selection process involved using a random number generator to select students who had been numbered according to their alphabetical order in the class." Quote: "After this random allocation, students were asked by email to consent to participate in the group to which they had been assigned. A proportion of students declined to participate (as indicated below), and were replaced by other students selected at random in a similar fashion from the remaining members of the class on a rolling basis until a complement of 30 control and 29 study participants was achieved." Quote: "There were no significant differences with respect to age, sex, PSS, SCS and RS scores at baseline." Judgement comment: The investigators describe a random component in the sequence‐generation process (random‐number generator). However, after 22 participants refused to participate in allocated intervention after randomisation, they were replaced by other students selected at random from class "in a similar fashion". It is not clear how the second random selection was performed; verified baseline comparability of groups for sociodemographic characteristics (age, gender) and outcomes of interest on the basis of analysis |
| Allocation concealment (selection bias) | Unclear risk | Quote: "This process blindly allocated thirty students to control and thirty to intervention." Quote: "After this random allocation, students were asked by email to consent to participate in the group to which they had been assigned. A proportion of students declined to participate (as indicated below), and were replaced by other students selected at random in a similar fashion from the remaining members of the class on a rolling basis until a complement of 30 control and 29 study participants was achieved." Judgement comment: participants and investigators enrolling participants could probably not foresee assignment during computer‐based allocation (exact method not described); but insufficient information about allocation concealment for allocation of participants who replaced the ones who refused to participate in allocated group |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "un‐blinded randomized controlled study" Judgement comment: blinding of participants and personnel not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; but due to performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "After this random allocation, students were asked by email to consent to participate in the group to which they had been assigned. A proportion of students declined to participate (as indicated below), and were replaced by other students selected at random in a similar fashion from the remaining members of the class on a rolling basis until a complement of 30 control and 29 study participants was achieved." Quote: "One study participant dropped out during the first week for scholastic reasons and his data were not used." Judgement comment: information received from authors: “We had: 30 controls, 29 treatment at the start of the study. By the end, because of attrition of one individual from each arm we had 29 controls and 28 study subjects = 57 participants total analyzed”; reasons for missing data unlikely to be related to true outcome with relative balance in missing data between groups (12 in CG refused to participate in allocated group after randomisation vs 10 in IG); participants who dropped out were replaced by other students in the class; 2 dropouts during intervention phase (IG: 1, CG: 1); per‐protocol analysis analysis (only participants who took part in allocated intervention) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Galante 2018.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): To detect a change in Clinical Outcomes in Routine Evaluation Outcome Measure (CORE‐OM) score of SD 0.3 at a P value < 0.05 with 90% power, 550 students were estimated to be needed, allowing for 20% loss to follow‐up.; 59% attendance rate at half or more course sessions could have represented a constraint on statistical power, but the study was designed to accommodate this Imputation of missing data: multiple imputation for primary outcome; for primary outcome psychological distress (and outcome grades): per‐protocol analysis (with participants in IG who completed at least 4 mindfulness course sessions and excluding individuals in CG who engaged in meditation elsewhere during the follow‐up period preceding outcome measurement) AND intention‐to‐treat analysis (see also appendix) |
|
| Participants |
Country: UK
Setting: University of Cambridge (courses run during university terms)
Age: range = 17 ‐ ≥ 31 years; see information from authors: only 1 participant aged 17 years
Sample size (randomised): 616
Sex: 388 women, 228 men
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: psychological distress (CORE‐OM): IG: 1.01 (0.54); CG: 0.97 (0.51) Population description: students (undergraduate and postgraduate) at University of Cambridge Method of recruitment: recruitment from students at University of Cambridge; method of recruitment not specified Inclusion criteria: 1) current undergraduate or postgraduate students (aged ≥ 18 years) at the University of Cambridge; 2) students who believed they could attend at least 7 of the 8 sessions of the mindfulness course Exclusion criteria: 1) currently experiencing severe periods of anxiety or depression; 2) a severe mental illness, such as hypomania or psychotic episodes; 3) recent bereavement or major loss; 4) any other serious mental or physical health problem that would affect their ability to engage with the course Attrition (withdrawals and exclusions): lost to follow‐up: post‐intervention: 135 (IG: 52, CG: 83); examination period: 175 (IG: 76, CG: 99); 5 (2%) (all in CG) withdrew from study Reasons for missing data: reasons for missing data (lost to follow‐up) at post‐intervention and examination period not specified; withdrawals from study in CG: in final year, could not undertake Mindfulness Skills for Students (MSS) course in following year |
|
| Interventions |
Intervention: TAU (mental health support as usual) + MSS intervention (mindfulness‐based intervention to increase resilience) (n = 309)
Control: TAU (mental health support as usual) (n = 307)
|
|
| Outcomes |
Outcomes collected and reported: most outcomes only assessed in examination period
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) examination period (post‐intervention; stressor exposure) Adverse events: no participants with adverse reactions related to self‐harm, suicidality, or harm to others; number of adverse events triggered by surpassing CORE‐OM risk subscales cut‐off scores: 1) pre‐intervention: IG: 15, CG: 11; 2) post‐intervention: IG: 13, CG: 13; 3) examination term: IG: 7, CG: 12; for all outcome time points: IG: 20; CG: n25 |
|
| Notes |
Contact with authors: We contacted the authors for the subgroup outcome data (means and SDs for all outcomes) of students in the fields of 'Clinical medicine' and 'Humanities and social sciences'; response received from authors (Galante 2019 [pers comm]); but subgroup data could not be sent while the review was written up Study start/end date: 28 September 2015 – 1 January 2015 Funding source: University of Cambridge and National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care East of England; study funded by the University of Cambridge Vice‐Chancellor’s Endowment Fund, the University Counselling Service, and the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care East of England hosted by the Cambridgeshire and Peterborough National Health Service Foundation Trust Declaration of interest: no competing interests declared Ethical approval needed/obtained for study: approved by Cambridge Psychology Research Ethics Committee on 25 August 25, 2015 (number PRE.2015.060); independent data monitoring and ethics committee is set up and study is co‐produced with students and university officers to increase validity of results Comments by study authors: registered with the Australia and New Zealand Clinical Trials Registry, number ACTRN12615001160527 Miscellaneous outcomes by the review authors: information received from authors: only 1 participant aged 17 years Correspondence: Dr Julieta Galante; Department of Psychiatry, University of Cambridge, Douglas House, Cambridge CB2 8AH, UK; mjg231@cam.ac.uk |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "participants were randomly assigned (1:1), via remote survey software (Qualtrics) using computer‐generated random numbers (simple random isation), to receive either mindfulness training with the Mindfulness Skills for Students (MSS) course plus mental health support as usual, or mental health support as usual alone." Quote: "Baseline characteristics were similar between groups (table 1)." Judgement comment: The investigators describe a random component in the sequence‐generation process (computer random‐number generator).; insufficient information about comparability of groups at baseline for sociodemographic variables (statistical (non)significance not reported); baseline comparability for outcome variables unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of 'Low risk' or 'High risk'; study management team informed of participants' allocation AFTER baseline assessment and allocation process concealed; but method of allocation is not described and unclear if researchers in study management team were also responsible for participant enrolment |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Quote: "Each participant was informed of their allocation automatically after completion of the baseline questionnaire." Quote: "Concurrently, members of the study management team were also informed automatically of participants’ allocation" Quote: "Due to the nature of the intervention, participants were aware of group allocation for the duration of the study." Judgement comment: no blinding of participants and personnel (face‐to‐face intervention), but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "Each participant was informed of their allocation automatically after completion of the baseline questionnaire." Quote: "Concurrently, members of the study management team were also informed automatically of participants’ allocation" Quote: "Due to the nature of the intervention, participants were aware of group allocation for the duration of the study." Judgement comment: no blinding of participants and personnel (face‐to‐face intervention), and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: assessment of objective outcome via smartphone app; blinding of outcome assessment unclear, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Low risk | Quote: "Data collection was remote and automatic using the web‐based Qualtrics software to ensure masking of outcome assessors." Judgement comment: blinding of outcome assessment ensured, and unlikely that the blinding could have been broken |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "we randomly assigned 616 students to the MSS group (n=309) or the support as usual group (n=307; figure 2)." Quote: "Five (2%) people, all in the support as usual group, withdrew from the study; three of four in their final year said this was because they could not undertake the MSS course the following year." Quote: "Multiple imputation addressed missing data (appendix pp 3, 4)." Quote: "The primary analysis was by intention to treat." Judgement comment: reasons for missing data likely to be related to true outcome with imbalance in missing data between groups (see Figure 2; lost to follow‐up: post‐intervention: IG: 52; CG: 83; examination period questionnaire: IG: 76; CG: 99); for primary outcome and grades: per‐protocol analysis (with participants in IG who completed at least 4 mindfulness course sessions and excluding individuals in CG who engaged in meditation elsewhere during the follow‐up period preceding outcome measurement) AND multiple imputation and intention‐to‐treat analysis (see also appendix) |
| Selective reporting (reporting bias) | High risk | Quote: "This trial is registered with the Australia and New Zealand Clinical Trials Registry, number ACTRN12615001160527." Judgement comment: trial registration (ACTRN12615001160527) and study protocol (Galante 2016) available; some prespecified (secondary) outcomes were not reported (e.g. mental health services use); some reported (secondary) outcomes were not prespecified (e.g. inability to sit examinations/intermissions of study); prespecified 1‐year follow‐up not reported here |
Geschwind 2015.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
|
| Participants |
Country: Belgium Setting: laboratory (sound‐attenuated and dimmed experimental room) Age: mean = 19.35 (SD = 1.98) years Sample size (randomised): 50, including 37 psychology students Sex: 50 women Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: healthy women Method of recruitment: recruited from psychology students at University of Leuven (n = 37) + healthy volunteers (n = 13) Inclusion criteria: not specified Exclusion criteria: 1) being pregnant; 2) having respiratory or cardiovascular diseases, neurologic diseases (e.g. epilepsy), or any other minor or major illness, including chronic pain; 3) uncorrected hearing problems; 4) pain at the dominant hand or wrist Attrition (withdrawals and exclusions): for positive and negative affect: 8 missing at follow‐up; unclear for other outcomes Reasons for missing data: not specified |
|
| Interventions |
Intervention: positive affect induction (BPS) (n = 25)
Control: attention control (Typical Day) (n = 25)
|
|
| Outcomes |
Outcomes collected and reported:
Positive and negative affect (modified Differential Emotions Scale; mDES) also assessed before/after affect induction, but not stated as dependent variables Time points measured and reported: 1) pre‐intervention, during acquisition phase (pain‐US expectancy, fear of movement‐related pain; rated after every 4th block in acquisition phase); 2) pre‐intervention (before affect induction phase; mDES); 3) post‐intervention (after affect induction phase; mDES); 4) post‐intervention, during test of generalisation (pain‐US expectancy, fear of movement‐related pain; rated before each movement); 5) post‐intervention, during transfer‐of‐acquisition phase (pain‐US expectancy, fear of movement‐related pain every other block); 6) 20‐minute follow‐up (mDES; after test of generalisation, approximately 20 minutes after affect induction) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted authors to ask for the subgroup (summary outcome) data for psychology students, but they had not responded at the time of writing Study start/end date: not specified Funding source: Ann Meulders (AM) is a postdoctoral researcher of the Research Foundation Flanders (FWO‐Vlaanderen), Belgium (12E33714 N). The participation of Nicole Geschwind was made possible by the Center for Excellence on Generalization research, Katholieke Universiteit (KU) Leuven, Belgium (GRIP*TT; KU Leuven grant PF/10/005). The study was also supported by the Odysseus Grant ‘‘The Psychology of Pain and Disability Research Program’’ funded by the Research Foundation Flanders (FWO‐Vlaanderen), Belgium to Johan WS Vlaeyen (G090208N) and by an EFIC‐Grunenthal Research Grant (E‐G‐G ID: 169518451) to AM. Declaration of interest: The authors report no conflict of interest Ethical approval needed/obtained for study: approved by the Ethical Committee of the Faculty of Psychology and Educational Sciences of the University of Leuven (registration number: S‐54568) and the Medical Ethical Committee of the University Hospital of the University of Leuven (registration number: ML8513) Comments by authors: supplementary data related to this article can be found at dx.doi.org/10.1016/j.jpain.2014.12.003 Miscellaneous outcomes by the review authors: not relevant Correspondence: Nicole Geschwind, Department of Clinical Psychological Science, Maastricht University, Maastricht, The Netherlands; Corresponding author: Ann Meulders PhD, Department of Psychology, University of Leuven, Tiensestraat 102, Box 3726, 3000 Leuven, Belgium; ann.meulders@ppw.kuleuven.be |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Participants were randomly allocated to either the PA induction group (n = 25) or the control group (n = 25), stratified by hand preference (left/right)." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; verified baseline comparability (see Supplementary Table S1) between groups in sociodemographic characteristic (age), variables related to pain‐US (physical stimulus intensity, duration of pain‐US) and positive affect before affect induction phase; significant difference in self‐reported stimulus intensity at calibration; baseline comparability for outcome variables (self‐reported fear of movement‐related pain, pain‐US expectancy) that were also assessed in acquisition phase before affect induction unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants unclear; blinding of study personnel probably not done (experimenter who provides the intervention next to laboratory of participants, verbal communication and observation possible) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Unclear risk | Judgement comment: insufficient information about blinding of outcome assessment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Participants were randomly allocated to either the PA induction group (n = 25) or the control group (n = 25)" Quote: "FU measures were available only in a subset of 42 participants." Judgement comment: see supplementary material 1 (Increase PA after affect induction phase (post‐test)) for results for positive affect, 50 analysed; insufficient reporting of attrition/exclusions to permit judgement of ‘Low risk’ or ‘High risk’ (e.g. unclear how many participants were analysed for single outcomes) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Goldstein 2019.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified in conference abstract/poster or abstract of manuscript under review Imputation of missing data: no imputation of missing data; per‐protocol analysis (i.e. only participants who completed workshops) and available‐case analysis (i.e. only participants for whom outcomes were obtained) |
|
| Participants |
Country: USA Setting: undergraduate students; training setting not specified Age: mean = 20.77 (SD = 3.36) years Sample size (randomised): 92 Sex: 36 women, 9 men (in analysed sample) Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: undergraduate students (including health profession students) Method of recruitment: not specified Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): pre‐intervention (assessment not completed): 3 (IG: 1, CG: 2); further withdrawals during workshops: 20 (IG: 9, CG: 11); post‐intervention (further lost to follow‐up): 9 (IG: 4, CG: 5); 3‐month follow‐up (further lost to follow‐up): 15 (IG: 7, CG: 8) Reasons for missing data: not specified |
|
| Interventions |
Intervention: ‘Your Enlightened Side’ (YESplus) (n = 47)
Control: attention control: ‘Wisdom On Wellness’ (WOW) (n = 45)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 3‐month follow‐up (3 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for information on whether fostering resilience was a primary aim of the study (see miscellaneous outcomes). Since the authors gave feedback that health profession students were also included (Goldstein 2019 [pers comm]), we asked for the outcome data for this subgroup. We received no response to this inquiry. Study start/end date: not specified in conference abstract/poster or abstract of manuscript under review Funding source: research funded by a Mind and Life Institute Varela Award and National Science Foundation Graduate Research Fellowship Declaration of interest: not specified in conference abstract/poster or abstract of manuscript under review Ethical approval needed/obtained for study: not specified in conference abstract/poster or abstract of manuscript under review Comments by study authors: not relevant Miscellaneous outcomes by the review authors: conference abstract; presented at 2019 33rd Annual Meeting of the Associated Professional Sleep Societies, San Antonio, TX; manuscript under review according to authors; Information received from authors concerning study aims: “It aimed to improve well‐being, as measured by various domains including depression, anxiety, perceived stress, self‐esteem, sleep, life satisfaction, and cardiac stress metrics which could be considered correlates or potential mechanisms of resilience. Given that it was a longitudinal design focusing on students, with a 3‐month follow‐up period, we anticipated the participants to experience natural stress associated with being a student and interpret the results as reflecting increased resilience.” corresponding poster and paper of manuscript under review sent by authors Correspondence: Michael R Goldstein; Department of Psychology, Psychophysiology Research Laboratory; University of Arizona, Tucson, AZ, USA; mgoldstein@email.arizona.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "89 students (age 20.9±3.1 years, 73% female, 86% undergraduate) with general distress complaints were randomly assigned to undergo one of two stress‐management workshops." Quote (paper abstract; paper under review): "In this study, students were randomized to one of two psychosocial stress‐management interventions." Judgement comment: based on conference abstract, poster and paper abstract of manuscript under review, insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; verified baseline comparability of groups for sociodemographic characteristics (gender, age, ethnicity, race, student status, GPA; all Ps > 0.377); baseline comparability for outcome variables not specified |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: based on conference abstract, poster and paper abstract of manuscript under review, insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Judgement comment: based on conference abstract, poster and paper abstract of manuscript under review, blinding of participants and personnel probably not done (face‐to‐face group intervention), but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: based on conference abstract, poster and paper abstract of manuscript under review, blinding of participants and personnel probably not done (face‐to‐face group intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: based on conference abstract, poster and paper abstract of manuscript under review, insufficient information about blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement: based on conference abstract, poster and paper abstract of manuscript under review, insufficient information about blinding of outcome assessment; but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "89 students (age 20.9±3.1 years, 73% female, 86% undergraduate) with general distress complaints were randomly assigned to undergo one of two stress‐management workshops." Quote (Paper abstract of manuscript under review): "Forty‐five students completed all time‐points and were used for analysis" Judgement comment: based on conference abstract, poster and paper abstract of manuscript under review, reasons for missing data likely to be related to true outcome with imbalance in missing data between groups: (Pre‐intervention: IG: 1, CG: 2; further withdrawals during workshop: IG: 9, CG: 11; Post‐intervention (further lost to follow‐up): IG: 4, CG: 5; 3‐month follow‐up (further lost to follow‐up): IG: 7, CG: 8); per‐protocol analysis (i.e. only participants who completed workshops) and available‐case analysis (i.e. only participants for whom outcomes were obtained) |
| Selective reporting (reporting bias) | Unclear risk | Judgement comment: no study protocol or trial registration available; based on conference abstract, poster and paper abstract of manuscript under review, insufficient information to permit judgement of 'Low risk' or 'High risk' |
Houston 2017.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: no imputation of missing data; available‐case analysis (only participants for whom outcomes were obtained independent of compliance with intervention) |
|
| Participants |
Country: USASetting: universityAge: range = 18 ‐ 23 yearsSample size (randomised): 129 including 38 college students in healthcare professionsSex: 93 women, 36 menComorbidity (mean (SD) of respective measures in indicated, if available) at baseline: anxiety (GAD‐7): IG: 2.18 (0.81), CG: 2.08 (0.73); depression (CES‐D): IG: 1.85 (0.52), CG: 1.82 (0.52); stress (items on stressful experiences): IG: 2.94 (0.49), CG: 2.91 (0.57) Population description: college undergraduate students Inclusion criteria: no inclusion criteria (universal application of RCI) Exclusion criteria: no exclusion criteria Attrition (withdrawals and exclusions): post‐intervention: 10 did not complete assessment (IG: 6, CG: 4); 9 of 64 participants in IG not present at session 3 of RCI, but did complete the assessment Reasons for missing data: not specified |
|
| Interventions |
Intervention: RCI (n = 64)
Control: no intervention (n = 65) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors to ask for the subgroup outcome data for college students in health professions (Houston 2019 [pers comm]). Study start/end date: implemented during the spring 2015 semester; exact study dates not specified Funding source: supported by the US Substance Abuse and Mental Health Services Administration (SAMHSA) through the Disaster and Community Crisis Center (DCC; http://dcc. missouri.edu) at the University of Missouri, a partner in the National Child Traumatic Stress Network (NCTSN) Declaration of interest: The authors have no conflicts of interest to report Ethical approval needed/obtained for study: approved by the University of Missouri IRB Miscellaneous outcomes by the review authors: subgroup data for college students in health professions sent from authors Correspondence: J Brian Houston, PhD; Disaster and Community Crisis Center, Department of Communication, University of Missouri, 204 Switzler Hall, Columbia, MO 65211, USA; houstonjb@missouri.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "65 were randomly assigned to the control group and 64 were randomly assigned to the intervention group using blocked randomization." Quote: "Group randomization was conducted immediately prior to the Week 1 sessions using blocked randomization with 4 units in each block." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; no information about comparability of groups at baseline or respective analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: reasons for missing data unlikely to be related to true outcome with relative balance in missing data between groups (IG: 6 at post‐intervention; CG: 4); no reasons for missing data stated for each group; available‐case analysis (only participants for whom outcomes were obtained independent of compliance with intervention) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
ISRCTN64217625.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified in trial registration Imputation of missing data: not specified |
|
| Participants |
Country: UK Setting: University of Brighton and Oxford‐Brookes University Age: not specified Sample size (randomised): 50 targeted Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: student paramedics who do not have post‐traumatic stress disorder or depression Inclusion criteria: student paramedics who do not have post‐traumatic stress disorder or depression (adults) Exclusion criteria: student paramedics who are suffering from PTSD or major depression Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: Mind's resilience intervention plus a new internet‐based top‐up session (n = not specified)
Control: active control (Mind's resilience intervention) (n = not specified)
|
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Secondary outcome
Outcomes reported not specified Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 6‐month follow‐up (6 months post‐intervention); time points reported not specified Adverse events: not specified |
|
| Notes |
Correspondence required: We contacted the authors to see whether the trial was completed and published and if the authors could provide the summary outcome data for the 2 groups (Wild 2018 [pers comm]). Study start/end date: January 2016 – October 2016 Funding source: University of Oxford; Mind, the mental health charity (UK) Declaration of interest: not specified in trial registration Ethical approval needed/obtained for study: approved by University of Oxford Central University Research Ethics Committee, 07 December 2015, ref: MS‐IDREC‐C1‐2015‐059 Comments by authors: not relevant Miscellaneous outcomes by the review authors: information received from authors: trial completed but unpublished Correspondence: primary contact: Dr Jennifer Wild; Department of Experimental Psychology, University of Oxford, South Parks Road, Oxford, OX1 3UD, United Kingdom; Jennifer.wild@psy.ox.ac.uk |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (see trial registration): "Participants will be randomly allocated to one of the following: 1. Six sessions of standard group‐based resilience training, 2. Six sessions of standard group‐based resilience training plus a one hour internet‐based top‐up training" Judgement comment: based on trial registration, insufficient information about random‐sequence generation to permit judgement of 'Low risk' or 'High risk'; for baseline comparability, no judgement possible based on trial registration |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: based on trial registration, insufficient information about allocation concealment to permit judgement of 'Low risk' or 'High risk' |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Judgement comment: based on trial registration, blinding of participants and personnel probably not done (face‐to‐face intervention), but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement: based on trial registration, blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: based on trial registration, insufficient information about blinding of outcome assessment, but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: based on trial registration, insufficient information about blinding of outcome assessment; but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: no judgement possible based on trial registration |
| Selective reporting (reporting bias) | Unclear risk | Judgement comment: no judgement possible based on trial registration |
Kelleher 2018.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified in conference abstract Imputation of missing data: not specified |
|
| Participants |
Country: USASetting: not specifiedAge: not specifiedSample size (randomised): not specifiedSex: not specifiedComorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: first semester baccalaureate nursing students (BSNs) Method of recruitment: recruited from first semester BSNs in Fall 2012; RCT repeated for Spring 2013 first semester BSNs Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: Brief MBSR programme (n randomised not specified)
Control: wait‐list control (n randomised not specified)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (at 4 weeks); 3) 1‐month follow‐up (at 8 weeks; i.e. 4 weeks post‐intervention); all time points reported except for 1) pre‐intervention Adverse events: not specified |
|
| Notes | Contact with authors: We contacted the authors to see if the study was already published (Kelleher 2019 [pers comm]).Study start/end date: not specified Funding source: not specified Declaration of interest: not specifiedEthical approval needed/obtained for study: not specifiedComments by study authors: not relevantMiscellaneous outcomes by the review authors: information received from authors: results have not been published yet; quantitative data was not available from the study authors Correspondence: Catherine Kelleher; University of Maryland, School of Nursing; kelleher@umaryland.edu | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (see conference abstract): "A randomized intervention pilot evaluated impact of a brief MBSR program for Fall 2012 first semester baccalaureate students in nursing (BSNs) and was repeated for Spring 2013 first semester BSNs." Judgement comment: based on conference abstract, insufficient information about random‐sequence generation to permit judgement of 'Low risk' or 'High risk'; for baseline comparability, no judgement possible based on conference abstract |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: based on conference abstract, insufficient information about allocation concealment to permit judgement of 'Low risk' or 'High risk' |
| Blinding of participants and personnel (performance bias) Objective outcomes | Low risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention), but the review authors judge that the outcome is not likely to be influenced by lack of blinding |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Objective outcomes | Low risk | Judgement comment: based on conference abstract, insufficient information about blinding of outcome assessment (electronic surveys), but the review authors judge that the outcome measurement is not likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: based on conference abstract, insufficient information about blinding of outcome assessment; but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: no judgement possible based on conference abstract |
| Selective reporting (reporting bias) | Unclear risk | Judgement comment: no judgement possible based on conference abstract |
Kötter 2016.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): With 39 students per group, the trial would have been powered to detect medium‐to‐large effect sizes (d = 0.65) for the difference in Perceived Medical School Stress German version (PMSS‐D) (SD 7.8), using a 2‐tailed test, α = 0.05 and an 80% power level. This number was determined using G*Power. In order to allow for a 10% dropout, the target sample size for the trial was 43 students per group (intervention groups 1 and 2 and control group 3) Imputation of missing data: missing values substituted following rules provided in handbooks for instruments; incomplete data sets were excluded; missing data from responses (IG: n = 5, CG: n = 7) imputed through last‐observation‐carried forward method of imputation (conservative method chosen due to equal dropout in IG and CG); per‐protocol analysis and intention‐to‐treat analysis (with 105 participants); as per‐protocol analysis yielded very similar results, only intention‐to‐treat analysis reported |
|
| Participants |
Country: Germany
Setting: medical students registered for first medical examination at the University of Lübeck; training setting not specified
Age: mean = 24.2 (SD = 2.6) years
Sample size (randomised): 1) randomisation (treatment (group 1 or 2) vs control group): 129; 2) randomisation to group 1 or 2 (only participants assigned to treatment group): 67
Sex: 70 women, 35 men (of 105 participants)
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: depression (HADS‐D; range = 0 ‐ 21) after randomisation 1 as well as after psychoeducative seminar: IG (coaching group): 3.88 (2.87), CG: 4.05 (3.72); anxiety (HADS‐D; range = 0 ‐ 21): IG (coaching group): 7.87 (3.39), 7.55 (4.30); perceived stress (PMSS‐D): IG (coaching group): 29.60 (6.57), CG: 28.74 (6.90) Population description: medical students Inclusion criteria: 1) registration for the first medical examination (“Physikum”) by mid‐July 2014 at University of Lübeck Exclusion criteria: after randomisation 1 (to treatments vs control group): 1) participants who did not do a test necessary to fulfil the exam admission requirements Attrition (withdrawals and exclusions):
Reasons for missing data: for losses to follow‐up: no reasons specified; for 1 withdrawal in IG1: refused to participate in 2. coaching session; for missing data from responses: not specified |
|
| Interventions |
Intervention 1: psycho‐educative seminar + individual coaching (after 1) 24 exclusions due to not passing test necessary to fulfil exam admission requirements and 2) randomisation: 34)
Intervention 2: psycho‐educative seminar (after 24 exclusions due to not passing test necessary to fulfil exam admission requirements and 2. randomisation: n = 33)
IG1 and IG2 were combined in analysis, thus: IG (coaching group): n = 67, CG: n = 38 Control: no intervention (after 24 exclusions due to not passing test necessary to fulfil exam admission requirements: n = 38)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) during intervention, after psycho‐educative seminar in groups 1 and 2, but before examination preparation phase and coaching (t1); 2) post‐intervention (after seminar and coaching, but directly before examination; t2) Adverse events: not specified in this report; qualitative analyses to ask about adverse events (results will be published separately) |
|
| Notes | Contact with authors: no correspondence requiredStudy start/end date: recruitment in 2014; see trial registration: July – September 2014Funding source: support and funding by Lübeck Medical School, especially Jürgen WestermannDeclaration of interest: 1 author is certified wingwave® coach and acted as 1 of the coaches in the study; authors declare no additional conflicts of interestEthical approval needed/obtained for study: approved by the Ethics Committee of the University of Lübeck (File reference 14‐098)Comments by study authors: registered with the German Clinical Trials Register (DRKS00006349); study acronym: LUST_wingwave; due to unexpected shortfall in the sample size (24 students did not pass a test necessary to fulfil the examination admission requirements, Figure 1), decision to combine both intervention groups for the quantitative analysesMiscellaneous outcomes by the review authors: not relevantCorrespondence: Thomas Kötter; Institute of Social Medicine and Epidemiology, University of Lübeck, Ratzeburger Allee 160, 23562 Lübeck, Germany; Tel +49 451 500 5874; Fax +49 451 500 5455; thomas.koetter@uksh.de | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After preliminary enrolment, we randomly allocated participants to the treatment (groups 1 and 2) or control group (group 3) using a computer‐generated random numbers table (randomization 1)." Quote: "In a second step, the participants in the treatment group were randomly allocated to treatment groups 1 and 2 (randomization 2)." Quote: "Table 1 displays baseline characteristics for all participants included. Overall, 35 male and 70 female students (M =24.2 years, SD =2.6) with an age range between 19 and 32 years participated in this study (66% of the whole class). The study participants were 0.5 years younger and the percentage of females was higher when compared to the whole class. We had a lower percentage of male participants in the coaching group and participants in this group were 0.5 years older (Table 1)." Judgement comment: The investigators describe a random component in the sequence‐generation process (computer‐generated random numbers table) for randomisation 1 (treatment in group 1 or 2 vs control group); insufficient information about random‐sequence generation for randomisation 2 (to group 1 or 2); verified comparability between groups at assessment t1 (i.e. after randomisation 1 and psychoeducative seminar, but before coaching in group 1) for outcome variables (see Table 2; all Ps > 0.42); insufficient information about comparability of groups in sociodemographic characteristics (e.g. smaller percentage of male participants in CG, but statistical (non)significance not specified); insufficient information about baseline comparability BEFORE psycho‐educative seminar |
| Allocation concealment (selection bias) | Unclear risk | Quote: "By inviting those participants in the treatment group to participate in the psychoeducative seminar (described earlier), the students were immediately informed of their allocation to either control or treatment group. In a second step, the participants in the treatment group were randomly allocated to treatment groups 1 and 2 (randomization 2). This allocation was concealed by means of sealed, opaque envelopes until the end of the psychoeducative seminar and the t1 survey." Judgement comment: insufficient information about allocation concealment for randomisation 1 (treatment (group 1 or 2) vs control group); for randomisation 2, participants and investigators enrolling participants could probably not foresee assignment (sealed, opaque envelopes) |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "By inviting those participants in the treatment group to participate in the psychoeducative seminar (described earlier), the students were immediately informed of their allocation to either control or treatment group. In a second step, the participants in the treatment group were randomly allocated to treatment groups 1 and 2 (randomization 2). This allocation was concealed by means of sealed, opaque envelopes until the end of the psychoeducative seminar and the t1 survey. The participants, coaches, and the involved researcher were not blinded hereafter." Judgement comment: 1) no blinding of participants and personnel (for allocation to treatment (group 1 or 2) or control group after randomisation 1 nor for allocation to treatment group 1 or 2 after randomisation; and 2) the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Quote: "Also, as group allocation was not concealed; t1 measures were completed after randomization; and the students, coaches, and investigators were not blinded, the differences between the groups at both t1 and t2 might have been influenced by a certain amount of frustration in the control group in not having received coaching." Judgement comment: probably no blinding of outcome assessment (e.g. group allocation after randomisation 1 not concealed and study personnel/participants were not blinded) and the outcome measurement is likely to be influenced by lack of blinding; unclear blinding for t2 assessment (web surveys); but due to performance bias (no blinding of participants), the review authors judge that the participants' responses at t2 assessment to questionnaires may also be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "We substituted missing values following the rules provided in the handbooks for the instruments, that is, through interpolation where tolerable. We then excluded incomplete data sets." Quote: "Data were missing from the responses of five students in the intervention group and seven in the control group, respectively. The last‐observation‐carried‐forward method of imputation was chosen because this is a conservative method used in instances in which there is an equal dropout rate in the intervention and the control group." Quote: "Intention‐to‐treat and per‐protocol analyses yielded very similar results and we therefore present only the former." Judgement comment: reasons for missing data unlikely to be related to true outcome with relative balance in missing data between groups (lost to follow‐up: IG1: 2; IG2: 1, CG: 1; missing data from responses: IG: 5, CG: 7); no reasons for missing data specified for each group; per‐protocol analysis and intention‐to‐treat analysis after last‐observation‐carried‐forward method of imputation (see Table 2) |
| Selective reporting (reporting bias) | High risk | Quote: "The trial was approved by the Ethics Committee of the University of Lübeck (File reference 14‐098) and registered with the German Clinical Trials Register (DRKS00006349)" Judgement comment: trial registration available (DRKS00006349) and all of the study’s prespecified (primary and secondary) outcomes have been reported in the prespecified way; but according to trial registration 3 assessments (t1 before coaching/examination preparation phase; t2 after individual coaching and directly before the examination; t3 after the examination "Physikum"), but only t1 and t2 reported |
Mathad 2017.
| Study characteristics | ||
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): A priori computation of sample size using G* Power version 3.1.9.2, revealed 64 participants were required with an effect size 0.347 at an α value of 0.05 and with an actual power of 0.80 Imputation of missing data: no imputation of missing data; per‐protocol analysis (only participants who did not drop out from IG or CG; i.e. 80 participants analysed according to authors) | |
| Participants |
Country: India
Setting: nursing students; training setting not specified
Age: mean = 19.5 (SD = 1.28) years
Sample size (randomised): 100
Sex: all women
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: nursing students (1st and 2nd year General Nursing and Midwifery (GNM) and 1st to 3rd year Bachelor of Scence Nusing (BSc Nursing)) Inclusion criteria: 1) female students aged between 17 and 30 years; 2) willing to learn yoga Exclusion criteria: 1) students diagnosed with severe neurological or psychiatric illness; 2) students receiving treatment for hormonal imbalance; 3) who recently underwent surgical intervention; 4) students regularly practising yoga Attrition (withdrawals and exclusions): 20 dropouts (IG: 10, CG: 10) Reasons for missing data: for 20 dropouts: 5: sick (IG: 3, CG: 2); 2: could not attend due to personal reasons (IG); 7: were not willing (to attend) (IG: 3, CG: 4); 3: excluded during data analysis (IG: 2, CG: 1); 1 started treatment for hypothyroidism (CG); 2: discontinued the course (CG) |
|
| Interventions |
Intervention: yoga intervention (n = 50)
Control: wait‐list control (n = 50)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the number of participants aged ≥ 18 years in the final sample and if they could provide the subgroup data for these participants (Mathad 2019 [pers comm]) Study start/end date: May 2015 – July 2015 Funding source: not specified Declaration of interest: no financial or other competing interests Ethical approval needed/obtained for study: approval of Institutional Ethics Committee was obtained for this study {RES/IEC‐SVYASA/59/2015} Comments by study authors: not relevant Miscellaneous outcomes by the review authors: information received from authors: "Data was analysed for 80 participants who were 18 years and above", i.e. no participants < 18 years in final (analysed) sample Correspondence: Ms Monali Devaraj Mathad; Research Scholar, Department of Division of Yoga and Humanities, S‐VYASA University, #19, Eknath Bhavan, Gavipuram Circle, Kempe Gowda Nagar, Bengaluru‐560019, Karnataka, India; mathad.kwr@gmail.com |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After screening, students were randomly allocated into two groups." Quote: "Meanwhile, normality test (Shapiro‐Wilk) ensured that there is no significant difference between yoga and WLC groups at baseline for all the variables." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; verified baseline comparability for several sociodemographic characteristics (age, gender, marital status, residence); baseline comparability for other sociodemographic variables (class/batch; religion, mother tongue) (i.e. statistical (non‐)significance) not specified; no significant baseline differences in outcome variables (see Table 4; all Ps > 0.18) |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "100 students were recruited, 50 participants in each group and there were 10 dropouts in each group. Finally, for analysis there were 80 students left." Judgement comment: reasons for missing data unlikely to be related to true outcome with relative balance in number and reasons for missing data between groups (IG: 10 dropouts; CG: 10 dropouts; e.g. IG: 3 not willing to attend vs 4 in CG; IG: 2 excluded during data analysis vs 1 in CG; IG: 2 could not attend intervention due to personal reasons vs 2 in CG who discontinued the course); per‐protocol analysis (i.e. only participants who did not drop out from IG or CG) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Mejia‐Downs 2016.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: imputation of missing data not specified; all randomised participants were analysed (n = 43) |
|
| Participants |
Country: USA Setting: university Age: adults (see Population description; age not specified) Sample size (randomised): 43 Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: perceived stress (PSS‐10): IG: 13.59 (5.01), CG: 13.90 (4.56) Population description: health professional students/doctor of physical therapy students Inclusion criteria: current enrolment in Doctor of Physical Therapy programme at either Indiana University or the University of Indianapolis Exclusion criteria: no exclusion criteria specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: resilience curriculum (n = 22)
Control: wait‐list control (n = 21) |
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Secondary outcome
Other outcome
Time points measured and reported: 1) pre‐intervention (in first 2 weeks of semester); 2) 2‐week follow‐up (4‐week intervention after 2‐week pre‐intervention assessment; follow‐up at week 8 after baseline, i.e. 2 weeks post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted authors for the summary outcome data for the outcomes (Mejia‐Downs 2018 [pers comm]). Study start/end date: see trial registration: September 2015 – January 2016 Funding source: University of Indianapolis Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by authors: register number: NCT02541240 Miscellaneous outcomes by the review authors: dissertation; information received from authors: study completed but not yet published; result tables for RCT provided from published dissertation Correspondence: principal investigator: Anne M Mejia‐Downs, PT, MPH; University of Indianapolis; adowns@uindy.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (see trial registration): "The study involves curriculum development and evaluation by randomized controlled trial. Participants will be randomized to the intervention group to receive a Resilience Curriculum or to a wait‐list control group" Judgement comment: insufficient information about random‐sequence generation (in trial registration and results sent from authors) to permit judgement of 'Low risk' or 'high risk'; no significant baseline differences between groups in resilience and positive affect, not described for other variables |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information (in trial registration and results sent from authors) about allocation concealment to permit judgement of 'Low risk' or 'high risk' |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention), and the outcome is likely to be related to true outcome |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment (in trial registration and results sent from authors); but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: results sent from authors; all 43 randomised participants were analysed; but unclear if there were any missing data that were imputed |
| Selective reporting (reporting bias) | Low risk | Judgement comment: trial registration (NCT02541240) available and all of the study’s prespecified (primary and secondary) outcomes that are of interest in the review have been reported in the prespecified way |
Miu 2016.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: no imputation of missing data; available‐case analysis (only participants for whom outcomes were obtained at baseline and follow‐up assessment) |
|
| Participants |
Country: USASetting: laboratory at Emory UniversityAge: age not specified (university students)Sample size (randomised): 123Sex: 81 women, 26 menComorbidity (mean (SD) of respective measures in indicated, if available) at baseline: depressive symptoms (BDI‐II): IG: 8.41, CG: 8.29; many participants with minimal number of depressive symptoms (8.35 (6.89)); considerable number of participants who reported mild depression (20%) and moderate depression (9%) with range of 0 ‐ 31; i.e. no clinical sample, but adequate range of depression symptoms; severe mental disorders (e.g. bipolar disorder, schizophrenia) as exclusion criterion: none of participants met this criterion Population description: university students from psychology department Inclusion criteria: not specified Exclusion criteria: severe mental disorders, such as bipolar disorder and schizophrenia Attrition (withdrawals and exclusions): in total: 16 excluded from analysis: 11 lost to follow‐up (i.e. did not complete follow‐up assessment); 5 excluded Reasons for missing data: for 11 losses to follow‐up: not specified; 1 outlier excluded; 4 excluded due to being non‐freshmen Adverse events: not specified |
|
| Interventions |
Intervention: mindset intervention (n = 61)
Control: attention control (n = 62)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention (initial visit); 2) 1‐month follow‐up (2. visit; i.e. 1 month after initial visit; 1 month post‐intervention); 3) participants with complete data at both time points, invited to participate in voluntary 3‐month follow‐up (3. visit; i.e. 3 months after initial visit, 3 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the SDs for the outcomes reported in Table 3, but received no response to 2 inquiries Study start/end date: not specifiedFunding source: not specifiedDeclaration of interest: not specifiedEthical approval needed/obtained for study: not specifiedComments by study authors: not relevant Miscellaneous outcomes by the review authors: dissertationCorrespondence: Adriana S Miu; Advisor: Marshall Duke, PhD; Duke: Department of Psychology; Emory University; psymd@emory.edu; 36 Eagle Row, Emory University, Atlanta, GA 30322; Phone: 404‐727‐7453 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "After participants completed baseline questionnaires of mindsets, depression, and attributions, within the same session, they were randomly assigned on Qualtrics (Qualtrics, Provo, UT) to either the changeability mindset intervention or the control condition, as detailed below." Quote: "Randomization Check. Randomization of the mindset intervention was effective except for baseline differences in mindsets (see Table 1)." Quote: "There were no significant baseline differences on covariates between participants in intervention and control groups, such as sex (X 2 = 1.96, p =.162), race/ ethnicity (X 2 = 2.53, p =.639), socioeconomic class (X 2 = 5.94, p =.204), grades (t = ‐1.75, p = .084), and locus of control (t = .84, p = .400)." Quote: "Regarding variables of interest, there were no significant baseline differences in depressive symptoms (t = ‐.09, p = .932), and stable attributions (t = .40, p = .687), between treatment and control groups, except for baseline mindset beliefs, t = ‐2.33, p = .022." Quote: "At baseline prior to the intervention, participants who received the intervention had a more changeability mindset (M = 2.95, SD = 1.07) compared to participants who were randomized to the control condition (M = 2.50, SD = .90)." Judgement comment: investigators describe a random component in the sequence‐generation process (Qualtrics software); verified baseline comparability of groups for sociodemographic characteristics (sex, race/ethnicity, socioeconomic class, grades, locus of control; all Ps > 0.16) and most outcome variables (depressive symptoms, stable attributions) except for mindset belief (P = 0.022) with IG having a more changeability mindset compared to CG |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ (method of concealment is not described in sufficient detail) |
| Blinding of participants and personnel (performance bias) Subjective outcomes | Low risk | Quote: "Research assistants and researchers were blind to condition, as treatment randomization was conducted through Qualtrics." Quote: "a double‐blind randomized mindset intervention was conducted to reduce depressive symptoms one month post‐intervention." Judgement comment: intervention provided in the laboratory (participants in both groups read articles and are asked to write narratives); blinding of participants and intervention providers probably ensured (double‐blind study), and unlikely that the blinding could have been broken |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Low risk | Judgement comment: blinding of outcome assessment probably ensured, and unlikely that the blinding could have been broken (online surveys; e‐mail/link to online survey provided by researcher; see performance bias: research assistants and researchers were blind to condition) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Eleven participants did not complete the one‐month follow‐up study and four participants were not freshmen and therefore excluded (see Table 2 for baseline differences between dropouts and full sample)." Judgement comment: reasons for missing data likely to be related to true outcome with imbalance in missing data between groups (61 randomised to IG vs 62 to CG; in total: 16 exclusions (11 lost to follow‐up, 1 outlier, 4 non‐freshmen): IG: 12 exclusions, CG: 4); available‐case analysis (only participants for whom outcomes were obtained at baseline and follow‐up assessment) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified (T3 assessment optional) |
Mueller 2018.
| Study characteristics | ||
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): power not specified; study limitation: sample size was restricted to a group of 36 physical therapy students in 1 programme Imputation of missing data: information received from authors: per‐protocol analysis with Time 2 and Time 3 following the completion of the intervention by both groups | |
| Participants |
Country: USA
Setting: online, self‐guided intervention
Age: mean = 26.83 (SD = 3.31) years
Sample size (randomised): 37
Sex: 25% women, 75% men
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: entry‐level doctor of physical therapy (DPT) students Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): 1 withdrawal in IG (immediate group) Reasons for missing data: for 1 withdrawal in IG: pregnancy‐related delay in internships |
|
| Interventions |
Intervention: “Called to Care” curriculum (immediate group) (n = 19)
Control: wait‐list control (n = 18)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (after completion of intervention and 1. internship); 3) 10‐week follow‐up in IG (i.e. 10 weeks post‐intervention and after 2. internship) and post‐intervention in CG; for review only 1) and 2) relevant as the wait‐list control had also received the intervention at 3) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for information about the number of participants analysed for the outcomes reported in Table 2 and 3 (i.e. per‐protocol analysis with 36 participants at T2 and T3 and without 1 withdrawal). We also asked for more details about the intervention content (Mueller 2019 [pers comm]). Study start/end date: not specified; Called to Care curriculum provided to all participants at the end of spring 2015 semester Funding source: The authors report no funding or conflicts of interest related to this study Declaration of interest: no funding or conflicts of interest related to this study reported Ethical approval needed/obtained for study: approved by the Northern Arizona University IRB (case 729441‐1) Comments by study authors: not relevant Miscellaneous outcomes by the review authors: additional information about intervention content and number of participants analysed received from authors Correspondence: Dr Karen Mueller; Department of Physical Therapy and Athletic Training, Northern Arizona University, 208 E Pine Knoll Dr, PO Box 15105, Flagstaff, AZ 86011, USA; Karen.mueller@nau.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "participants were randomly assigned (via a blinded shuffle of cards) to an immediate intervention group or a delayed intervention group. The deck included only the numbered cards (to ensure an even 50/50 split) and group assignment based on evens or odds." Quote: "There were no significant differences in age or gender distribution, and no significant differences between the baseline outcome measures of the immediate and delayed intervention groups, suggesting that the randomization worked appropriately." Judgement comment: investigators describe a random component in the sequence‐generation process (shuffling cards); verified baseline comparability of groups for sociodemographic characteristics (all Ps > 0.055) and outcomes of interest on the basis of analysis (see Table 1; Ps > 0.213) |
| Allocation concealment (selection bias) | Unclear risk | Quote: "randomly assigned (via a blinded shuffle of cards) to an immediate intervention group or a delayed intervention group." Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ ("blinded shuffle of cards"; method of allocation concealment is not described in sufficient detail) |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "The participants were informed of their designation into the immediate or delayed intervention group." Judgement comment: online, self‐guided intervention; no blinding of participants and probably no blinding of personnel (monitored discussion board postings); the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment to permit judgment of ‘Low risk’ or ‘High risk’ (in part electronic assessments); but due to performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "37 students volunteered to participate in the Called to Care study. Of the 37 students, 1 withdrew from the project due to a pregnancy‐ related delay in her internships. Thirty‐six students completed the project." Quote: "FIGURE 1. Study design flowchart." Judgement comment: reasons for missing data unlikely to be related to true outcome (only 1 withdrawal in IG due to pregnancy); information received from authors: "We did perform a per‐protocol analysis with T2 and T3 following the completion of the intervention by both groups." |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Peng 2014.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individualsPower (power & sample size calculation, level of power achieved): not specifiedImputation of missing data: not specified |
|
| Participants |
Country: ChinaSetting: medical students of Third Military Medical University; training setting not specifiedAge: mean = 19.78 (SD = 0.77); range = 18 ‐ 22 yearsSample size (randomised): 60; 30 divided into high‐resilience group (SD above average score of CD‐RISC (CD‐RISC)); n = 30, divided into low‐resilience group (SD below average score of CD‐RISC)Sex: 18 women, 42 menComorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specifiedPopulation description: medical students Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: Penn Resilience Program (PRP) (in total: n = 30; n = 15 of high‐resilience group, n = 15 of low‐resilience group)
Control: wait‐list control (in total: n = 30; 15 of high‐resilience group, 15 of low‐resilience group) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the second full text, but received no response to 2 inquiries. Study start/end date: not specifiedFunding source: This study was financially supported by National Natural Science Foundation of China Granted to Min Li (No. 31170994) and Project of Military Research Foundation of PLA of China to Min Li (Grants 12XLZ212 and CWS11J049).Declaration of interest: not specifiedEthical approval needed/obtained for study: approved by the Ethics Committee of the Third Military Medical UniversityComments by study authors: not relevantMiscellaneous outcomes by the review authors: 2 reports; full text for 2. report not availableCorrespondence: Li Peng; corresponding author: Min Li; Department of Military Psychology, School of Psychology, The Third Military Medical University, No. 30, Gaotanyan Road, Shapingba District, Chongqing 400038, China, Tel.: +86 23 68752267; fax: +86 23 68752360; limin52267@tmmu.edu.cn (M. Li) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "the students were divided into high‐resilience and low‐resilience groups, with each group consisting of 30 students. Half of the students from each group were then divided into the experimental group and received PRP training. The remaining students were divided into the control group and were told to wait for resilience training." Quote: "From them, 30 students with high resilience and 30 with low resilience were obtained. These students were further randomly assigned into experimental group to receive resilience training (n = 15), and control group without training (n = 15)." Quote: "No significant differences in resilience, positive emotion, negative emotion, cognitive appraisal, and expression inhibition scores were found between the control and experimental groups (P > .05) (see Table 2)." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; verified baseline comparability of groups for outcome variables on the basis of analysis (see Table 2; all Ps > 0.28 in high‐resilience participants or all Ps > 0.30 in low‐resilience individuals), baseline comparability for sociodemographic characteristics (e.g. age, gender) not specified |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit a judgement of low risk or high risk |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement: insufficient reporting of attrition/exclusions to permit judgement of 'Low risk' or 'High risk' (probably 30 randomised in each group were also analysed; but unclear if there were any missing data and if missing data were imputed) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Porter 2008.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified; according to publication maybe lack of statistical power Imputation of missing data: no imputation of missing data; available‐case analysis (only participants for whom outcomes were obtained at both time points) |
|
| Participants |
Country: Canada Setting: college programme for paramedic students Age: mean = 21.69 (SD = 1.92); range = 19 ‐ 28 years Sample size (randomised): 29 Sex: 11 women, 18 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: depression (SCL‐90‐R): IG: 1.08 (0.42); CG: 1.57 (0.65); Anxiety (SCSL‐90‐R): IG: 0.73 (0.49); CG: 0.93 (0.51); Global Severity Index (SCL‐90‐R): IG: 0.85 (0.33); CG: 1.09 (0.52); Burnout‐emotional exhaustion (MBI): IG:17.09 (6.72); CG: 20.64 (10.20); Burnout‐depersonalisation (MBI): IG: 8.82 (4.88); CG: 9.45 (3.86); Burnout‐personal accomplishment (MBI): IG: 34.64 (8.32); CG: 32.73 (8.36) Population description: paramedic students in the final year of a 2‐year college paramedic programme Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): 6 participants dropped out of the study before post‐intervention assessment (IG: 3/15 (20%); CG: 3/14 (21.4%)); n = 1 participant did not complete WAYS measure Reasons for missing data: not specified |
|
| Interventions |
Intervention: psycho‐educational group (n = 15)
Control: no intervention (n = 14) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) 2‐month follow‐up (2‐months post‐intervention; 6‐month interval between 2 assessments) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted authors for the number of dropouts and the number of participants analysed for each group at pre‐ and post‐intervention assessment (Porter 2018 [pers comm]). Study start/end date: recruitment start in fall 2007; exact study dates not specified Funding source: funding for this research provided by Fanshawe College Research Initiatives Fund Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by authors: not relevant Miscellaneous outcomes by the review authors: not relevant Correspondence: Shirley Porter; Fanshawe College, Student Success Centre, 1001 Fanshawe College Blvd., F2010, P.O. Box 7005, London, Ontario, Canada N5Y 5R6; saporter@fanshawec.ca |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Fourteen participants (8 women) were randomly assigned to be part of the control group, and fifteen participants (5 women) were randomly assigned to be part of the treatment group." Quote: "Ages ranged from 20 to 25 in the control group (M = 21.82, SD = 1.72), and from 19 to 28 in the treatment group (M = 21.58, SD = 2.31). This age difference was not statistically significant." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; verified baseline comparability for sociodemographic variable age; baseline comparability for other sociodemographic characteristics and outcomes of interest unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Six participants dropped out of the study before post‐test measures were collected. Three of these individuals (all men) were in the control group, and three of these individuals were in the treatment group (2 women)." Quote: "The final sample was, therefore, comprised of 23 individuals, 11 in the control group (8 women), and 12 in the treatment group (3 women)." Judgement comment: reasons for missing data unlikely to be related to true outcome with balance in missing data between groups (IG: n = 3; CG: n = 3); for burnout, attitudes toward emotional expression, peer support and ways of coping subscales: 1 additional missing participant; reasons for missing data not reported; available‐case analysis (only participants for whom outcomes were obtained at both time points) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Recabarren 2019.
| Study characteristics | ||
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): To determine the optimal sample size, the trialists performed an a priori power analysis using G∗Power and computed an expected medium effect size based on the meta‐analysis of Regehr 2013 for an ANOVA (analysis of variance) with 2 measurement points, 2 groups and between and within factors interaction; sample size of 54 obtained; in addition, drop‐out rate of 15% estimated based on the results of similar intervention programme, leading to an adequate sample size of 64 participants Imputation of missing data: per‐protocol analysis and available‐case analysis (i.e. including only data from participants who participated in at least 5/8 intervention sessions and who answered the post‐treatment measures) + intention‐to‐treat analysis (i.e. including all 64 randomised participants who completed pre‐treatment assessment; including also non‐completing participants and those with missing outcomes); missing data at post‐intervention dealt by using LOCF method | |
| Participants |
Country: Switzerland
Setting: university students; training setting not specified
Age: mean = 21.35 (SD = 2.53); only psychology students (n = 51): mean = 21.02 (SD = 2. 47); range: 18 ‐34 years Sample size (randomised): 64, including 51 psychology students Sex: 56 women, 8 men (total sample); only psychology students (n = 51): 46 women, 5 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline:
Population description: university students (majority psychology students) Inclusion criteria: see also trial registration: 1) being older than 18 years old; 2) having a good understanding of French or German; 3) being a student at the University Fribourg; 4) for the other parts of the study: being right‐handed Exclusion criteria: 1) presence of an endocrinological condition, history or presence of a neurological disorder or brain injury; 2) use of psychotropic drugs; 3) presence of a mental disorder; 4) participating in another psychological intervention or any type of therapy or coaching and participating in the longitudinal part of this study; 5) for the other parts of the study: general MRI exclusion criteria, i.e. presence of claustrophobia, being pregnant (tested with a pregnancy test), metal in the body (pacemakers, aneurysm's clips, metallic prosthesis, cochlear implant…) Attrition (withdrawals and exclusions): 1 withdrawal in IG (did not begin intervention) Reasons for missing data: not specified |
|
| Interventions |
Intervention: multidimensional stress intervention/prevention programme (n = 32)
Control: wait‐list control (n = 32)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention (maximum of 2 weeks before start of intervention); 2) post‐intervention (maximum of 2 weeks after end of the intervention); according to trial registration also assessments at 3‐month and 6‐month follow‐up (i.e. 3 and 6 months post‐intervention) in certain cohorts Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the subgroup outcome data (i.e. means, SDs and number of participants analysed) for all outcomes for psychology students (Recabarren 2019 [pers comm]). Study start/end date: data collection between March 2015 – March 2017 (see also trial registration) Funding source: supported by the research pool of the University of Fribourg (grant number 578) Declaration of interest: research conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest Ethical approval needed/obtained for study: accepted by the Ethics Committee of the Cantons of Vaud and Fribourg (Protocol 261/14) Comments by study authors: registered in the research register of the University of Fribourg FUTURA (Project number 6239; http://admin.unifr.ch/futura/content/ projects/6239) as well as in the Clinicaltrial Register (clinicaltrials.gov.NCT03861013) Miscellaneous outcomes by the review authors: subgroup data for psychology students were sent by the authors Correspondence: Romina Evelyn Recabarren; Division of Clinical and Health Psychology, IReach Lab, Department of Psychology, University of Fribourg, Fribourg, Switzerland; rominaevelyn.recabarren@unifr.ch |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "After that, participants were randomly distributed in the intervention or the wait‐list control group. The randomization was done using a free available software, i.e., www. randomization.com" Quote: "No significant differences were found in the sociodemographic variables between the participants of the wait‐list control group and of the intervention groups (all p >0.05) [age: t (62) = −0.393, p = 0.696; sex: X 2 (1) = 0.571, p = 0.450; socioeconomic position: Cramer’s V = 0.135, p = 0.769; studies (psychology and other): X 2 (1) = 0.097, p = 0.756]." Judgement comment: The investigators describe a random component in the sequence‐generation process (randomisation software); verified baseline comparability of groups for some sociodemographic characteristics (age, sex, socioeconomic position, studies); baseline comparability for other sociodemographic variables (e.g. marital status) and outcomes of interest not specified on the basis of analysis |
| Allocation concealment (selection bias) | Unclear risk | Quote: "After that, participants were randomly distributed in the intervention or the wait‐list control group. The randomization was done using a free available software, i.e., www. randomization.com and was archived in an electronic document saved separately." Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ (method of concealment is not described in sufficient detail: "archived in electronic document saved separately"; unclear if random‐sequence allocation was concealed from personnel and/or participants) |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "After randomization had been done and due to the design of the study, investigators and participants were not blinded about group allocation." Judgement comment: no blinding of participants and personnel (face‐to‐face intervention), and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: blinding of interviewers for structure diagnostic interview on psychopathological disorders at baseline ensured; insufficient information about blinding of outcome assessment (online questionnaires); but due to performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "We analyzed our data using the per‐protocol (PP) approach (108). In that respect, we calculated the ANOVA analyses but only with data from participants who participated in at least five of the eight intervention sessions and who answered the post‐treatment measures. Considering the completion of post‐ treatment measures and according to the dependent variable considered, the sample of post‐treatment participants for the PP‐analyses varies from 56 to 60." Quote: "To increase the confidence of our results, we performed the same analyses considering an intention‐to‐treat approach (ITT). In the ITT analyses, all randomized participants who completed the pre‐treatment assessment (T1) were taken into account, including non‐completing participants and those with missing outcomes. Missing data at post‐treatment assessment (T2) were dealt by using the last observation carried forward method (LOCF), which in this case correspond to the pre‐ treatment measure (T1) (108). A total of 64 participants were taken account for these analyses." Judgement comment: unclear if reasons for missing data are related to true outcome (e.g. number of missing data not reported for each group); per‐protocol analysis with participants who participated in at least 5/8 intervention sessions and available‐case analysis (i.e. participants who provided post‐treatment measures) with varying number of participants analysed for each outcome (n = 56 to 60); but also intention‐to‐treat analysis with all randomised participants (n = 64) using LOCF method |
| Selective reporting (reporting bias) | High risk | Quote: "This study was registered in the research register of the University of Fribourg FUTURA (Project number 6239; http://admin.unifr.ch/futura/content/ projects/6239) as well as in the Clinicaltrial Register (clinicaltrials.gov.NCT03861013)." Judgement comment: trial registration available (NCT03861013); not all of the study’s prespecified primary and secondary outcomes have been reported; PRESPECIFIED: Primary outcomes: depression, anxiety (trait/state), sense of coherence, burnout, social anxiety, quality of life, difficulties in emotion regulation, perceived stress, self‐efficacy, mindfulness skills, mental health problems, self‐compassion, perceived social support, reward responsiveness, self‐esteem, reactions after traumatic events, childhood trauma, post‐traumatic stress, cannabis abuse, coping, life orientation/optimism, smartphone addiction, internet addiction, changes in participant's progress through the course of the therapy; Secondary outcomes: ambulatory assessment, answer to reward task, cortisol levels in daily life and laboratory task; Other outcomes: socio‐economic position index, information about relatives, handedness, nicotine dependence, psychotherapy alliance, quality of the group relationship, academic success, change in psychopathological disorders; REPORTED: mental health problems, depression, anxiety (trait/state), social anxiety, changes in participant's progress through the course of the therapy, quality of life, self‐efficacy, sense of coherence, self‐compassion, perceived social support |
Sahranavard 2018.
| Study characteristics | ||
| Methods | Study design: RCTStudy grouping: parallel groupUnit of randomisation: individualsPower (power & sample size calculation, level of power achieved): power achieved in 1‐way covariate analysis in MANCOVA (multivariate analysis of covariance) indicates adequacy of sample size (anxiety sensitivity: 0.97; hope: 0.82; positive and negative affect: 0.57; anxiety: 1.00; hardiness: 0.82; self‐efficacy: 0.92)Imputation of missing data: not specified | |
| Participants |
Country: Iran
Setting: female students from Birjand University of Medical Science; training setting not specified
Age: mean = 22.00 (SD = 1.11); range = 20 ‐ 24 years
Sample size (randomised): 30
Sex: 30 women
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: anxiety symptoms (BAI): IG: 13.40 (6.16); CG: 13.46 (5.16) Population description: female medical students of Birjand University of Medical Sciences Method of recruitment: recruited at Birjand University of Medical Sciences in Iran; method of recruitment not specified (selected by available sampling) Inclusion criteria: 1) having the BDI score higher than 16; 2) living in the dormitory; and 3) being informed and satisfied; according to Sahranavard 2018, also participants with higher than average score on the BAI Exclusion criteria: 1) unsatisfied students; 2) being graduates; 3) those who did not live in the dormitory; and 4) having BDI < 16; according to Sahranavard 2018, also students with lower than average score on the BAI Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: stress‐management‐based cognitive‐behavioural group treatment (n = 15)
Control: wait‐list control (n = 15) |
|
| Outcomes |
Outcomes collected and reported:
Depression (BDI) no outcome measure, but only assessed at baseline Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (1 week after training) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for any withdrawals/exclusions from the study and the number of participants analysed. We also asked for the post‐intervention means and SDs for positive and negative affect separately and whether the CBT group included 6 or 10 sessions. We received no response to 2 inquiries Study start/end date: not specifiedFunding source: no specific funding for this work; nil financial support and sponsorshipDeclaration of interest: no conflicts of interest disclosedEthical approval needed/obtained for study: approved by the Research Ethics Committee of the Birjand University of Medical Sciences (Birjand, Iran)Comments by study authors: not relevant Miscellaneous outcomes by the review authors:Sahranavard 2018 and Sahranavard 2019 are 2 reports of the same study (n = 30 randomised) with different outcomes reportedCorrespondence: Dr Sara Sahranavard; Department of Psychology, Faculty of Medicine, Birjand University of Medical Science; Social Determinants of Health Research Center, Faculty of Health, Birjand University of Medical Sciences, Tehran, Iran; sahranavard_sara@yahoo.com; alesaleh70@yahoo.com |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A sample of 30 participants were selected through the available sampling method and randomly assigned into experimental (CBT) and control groups (each group, 15 female student)." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; verified baseline comparability of groups for sociodemographic characteristic age (unclear for other sociodemographic variables); baseline comparability for outcome variables unclear (i.e. statistical significance not specified) |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: insufficient reporting of attrition/exclusions to permit judgement of ‘Low risk’ or ‘High risk’ (n = 15 randomised to each group; but unclear if there were any missing data or if potential missing data were imputed; number of participants analysed in each group not stated) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Samouei 2015.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: not exactly specified (based on full text unclear if individual or cluster‐randomisation)Power (power & sample size calculation, level of power achieved): not specifiedImputation of missing data: not specified |
|
| Participants |
Country: IranSetting: students of Isfahan University of Medical Sciences; training setting probably university (since training sessions held at same day as other university classes)Age: not specifiedSample size (randomised): not specifiedSex: not specifiedComorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: students of Isfahan University of Medical Sciences Method of recruitment: recruited from students of Isfahan University of Medical Sciences (Department of Management and Medical Informatics and Department of Rehabilitation Sciences); 5 study groups selected from majors of audiology, speech therapy, orthopaedics, physiotherapy, healthcare management, and medical librarianship; method of recruitment not specified Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
|
| Interventions |
Intervention: mindfulness training (n = not specified)
Control: active control (n = not specified)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) 3‐month follow‐up (i.e. 3 months after last session); only 2) reported Adverse events: not specified |
|
| Notes | Contact with authors: We contacted the authors for the number of participants randomised to each group. We also asked if there were any missing data (e.g. withdrawals or exclusions) in the 2 groups, the number of participants analysed, respectively, and if the study used cluster randomisation, but received no response to 2 inquiries. Study start/end date: study conducted in 2013Funding source: financial support and sponsorship: nilDeclaration of interest: There are no conflicts of interest.Ethical approval needed/obtained for study: not specifiedComments by study authors: not relevantMiscellaneous outcomes by the review authors: not relevantCorrespondence: Miss Rahele Samouei, PhD Student of Health Management in Disasters; Social Determinants of Health Research Center, Isfahan University of Medical Sciences, Isfahan, Iran; Samouei@mail.mui.ac.ir | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Therefore, cluster sampling method was employed by simultaneous selection of five groups of students from two departments to four majors whom were then randomly divided to study and control groups." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; no information about comparability of groups in sociodemographic characteristics or outcome variables at baseline or respective analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Judgement comment: insufficient reporting of attrition/exclusions to permit judgement of ‘Low risk’ or ‘High risk’ (e.g. number randomised to each group not stated; unclear if there were any missing data and if missing data were imputed, for example; number of participants analysed in each group not specified) |
| Selective reporting (reporting bias) | High risk | Judgement comment: no study protocol or trial registration available, but not all of the study’s prespecified outcomes have been reported (FFMQ values at post‐intervention not reported) |
Smeets 2014.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: unclear if available‐case analysis (with n = 49 as indicated in text) or if missing data were imputed to perform intention‐to‐treat analysis |
|
| Participants |
Country: Netherlands Setting: mid‐sized European University Age: mean = 19.96 (SD = 1.33) years Sample size (randomised): 52 Sex: 52 women Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: female psychology students entering first or second year of college Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): only CG: 3/25 (12%) did not complete post‐test assessment and were excluded from analysis (according to text; but see also Table 2 in the report) Reasons for missing data: not specified |
|
| Interventions |
Intervention: self‐compassion (SC) intervention (n = 27)
Control: attention control (time management control intervention) (n = 25)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention (1 week before intervention); and 2) post‐intervention (1 week after intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted authors to ask if missing data had been imputed to perform intention‐to‐treat analysis (according to text: n = 49 analysed due to exclusions; Table 2: n = 52 analysed), but they had not responded at the time of writing this review Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: approved by the local committee for research ethics Comments by authors: not relevant Miscellaneous outcomes by the review authors: not relevant Correspondence: Elke Smeets; Department of Clinical Psychological Science, Maastricht University, P.O. Box 616, 6200 MD Maastricht, The Netherlands; elke.smeets@maastrichtuniversity.nl |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "All participants were randomly assigned to either the self‐compassion intervention group (N = 27) or the time management control group (N = 25) by means of an Internet‐based randomization program (www.randomizer.org)." Quote: "Analyses of variance procedures (ANOVAs) were employed to examine whether there were significant differences between the self‐compassion intervention group and the time management control group on study measures at pretest. ANOVA’s revealed no significant differences between groups on any of the pretest or demographic measures (all Fs < 2.54, all ps < .05)." Judgement comment: The investigators describe a random component in the sequence‐generation process (internet‐based randomisation); verified baseline comparability of groups for sociodemographic characteristics and outcomes on the basis of analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "The initial sample comprised 52 female psychology students" Quote: "Three control participants did not complete posttest measurements and were excluded from analyses, leaving a final sample size of 49 participants (N = 27 in the intervention group, and N = 22 in the control group)." Judgement comment: reasons for missing outcome data likely to be related to true outcome, with (slight) imbalance in numbers of missing data between groups (IG: n = 0; CG: n = 3); reasons for missing data not reported; unclear if available case analysis (with n = 49 as indicated in text) or if missing data were imputed to perform intent‐to‐treat analysis (see Table 2) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Stephens 2012.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): preferred sample size (n = 111) was predetermined by a power analysis using the G*Power 3.1 software (Faul 2007) with medium effect size (0.30), α = 0.05, power = 0.80, 2 groups, and 3 measurements; loss of statistical power by missing of 17% of 210 total measurements (measurements each for 70 participants) Imputation of missing data: for missing data points in items: missing value imputation methods using the expectation maximisation (EM) approach (according to authors, imputed values rounded to the nearest whole number) and computation of maximum likelihood estimation (as though there were no missing data) |
|
| Participants |
Country: USA Setting: state‐supported universities Age: mean = 20.9 (SD = 0.95); range = 19 ‐ 23 years Sample size (randomised): 70 Sex: 62 women, 8 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: perceived stress (PSS): IG: 20.23 (6.37), CG: 20.37 (5.89) Population description: baccalaureate nursing students enrolled full‐time and in clinical nursing course at 2 university colleges of nursing Inclusion criteria: 1) full‐time status at 1 of the 2 universities; 2) enrolled in a clinical course; 3) between the ages of 19 ‐ 23; 4) currently have an active mobile phone account; 5) currently have the ability to send/receive text messages; and 6) have Twitter account or be willing to establish one prior to beginning of the study Exclusion criteria: not specified Attrition (withdrawals and exclusions): post‐intervention: 6 did not complete data collection (IG: 3/35 (8.6%); CG: 3/35 (8.6%)); 1‐month follow‐up: 8 did not complete data collection (IG: 3/35 (8.6%); CG: 5/35 (14.3%)); 1 student not completing time 2 (T2) completed time 3 (T3) assessment Reasons for missing data: dropped out of nursing programme (n = 2); never took time to set up Twitter account (n = 1); reasons for other missing data not specified |
|
| Interventions |
Intervention: educational intervention by Twitter to enhance resilience (n = 35)
Control: attention control (same number of tweets received) (n = 35) CONTROL
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (within 1 week following last tweet; and 3) 1‐month follow‐up (1 month post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the number of participants analysed in each group at each time point (Stephens 2018 [pers comm]). Study start/end date: not specified Funding source: research grant from Gamma Chi Chapter of Sigma Theta Tau International Declaration of interest: not specified Ethical approval needed/obtained for study: verbal approval obtained from the appropriate administrative personnel at both universities early in the planning process; IRB approval was granted by both institutions prior to the recruitment of participants and any data collection Comments by authors: not relevant Miscellaneous outcomes by the review authors: dissertation Correspondence: Teresa Maggard Stephens; now: East Tennessee State University; now: Stephenstl@etsu.ed |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A computerized random number generator (www.randomizer.org) was used to randomly select half the participating students at each institution as the experimental group and half as the attention placebo control group." Quote: "An independent samples t‐test was used to determine if there were statistically significant differences between the experimental and control groups on age. Results indicate there were no statistically significant differences, t(68) = .47, p = .49." Quote: "According to the chi‐square analysis, there were no statistically significant differences between control and experimental groups on race, χ²(1, N =70) = 1.01, p = .31; and there were no statistically significant differences between control and experimental groups on gender, χ²(1, N = 70) = .56, p = .45." Judgement comment: investigators describe a random component in the sequence‐generation process (computer random‐number generator); verified baseline comparability of groups for some sociodemographic characteristics (age, gender, race); baseline comparability for other sociodemographic characteristics (e.g. high school education, employment, health behaviours, sources of financial/emotional support) and outcome variables (see Table 24, statistical (non)significance) unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: no blinding of study personnel (intervention is provided by Twitter by only 1 researcher who also performs outcome assessment); blinding of participants unclear; outcomes are likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: no blinding of outcome assessment (outcome assessment by the same researcher who provides the intervention by Twitter) and the outcome measurement is likely to be influenced by lack of blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All 70 participants completed T1 data collection." Quote: "A total of six students did not participate in T2 data collection, three from the experimental group (8.6%) and three from the control group (8.6%)." Quote: "A total of eight students did not participate in T3 data collection, three from the experimental group (8.6%) and five from the control group (14.2%)." Quote: "Nine items (Time 2) and one item (Time 3) were determined to be missing at random and were replaced via missing value imputation methods using the expectation maximization (EM) approach." Quote: "The EM method was used to compute missing values for the appropriate scale at the specified time for the missing items. Imputed values were rounded to the nearest whole number and the maximum likelihood estimation was computed as though there were no missing data." Quote: "According to Krueger and Tian (2004), MLM can be used to describe nonlinear relationships across time in a longitudinal dataset with multiple missing data points. This method was chosen over the repeated measures analysis of variance (RM ANOVA) because the MLM can accommodate flexible time schedules, missing data points and because of its emphasis on patterns of change." Quote: "In this study, six participants did not complete the data collection at Time 2 (three from the control group and three from the experimental group), and eight participants did not complete the data collection at Time 3 (three from the experimental group and five from the control group). Two participants did not complete the data collection because they dropped out of the nursing program and another student stated she never took the time to set up her Twitter account. The other students did not give a reason for not completing the data collection." Judgement comment: information received from authors on number of participants analysed in each group and imputation methods: "Each group contained 35 participants (total n=70). For the missing data: I used the expectation maximization (EM) approach. The EM method was used to compute missing values for the appropriate scale at the specified time for the missing items. Imputed values were rounded to the nearest whole number and the maximum likelihood estimation was computed as though there were no missing data."; reasons for missing data unlikely to be related to true outcome (relative balance in missing data between groups: T1: none missing; T2: IG: n = 3, CG: n = 3; T3: IG: n = 3; CG: n = 5); for missing values in single items: missing value imputation methods using the expectation maximization (EM) approach and computation of maximum likelihood estimation |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Venieris 2017.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): A priori power analysis using G*Power 3.17 determined that 171 participants (n = 57 participants per group) were necessary to detect an effect size of 0.4 at a significance level of 0.05 and a power of 0.80. Imputation of missing data: no imputation of missing data; per‐protocol analysis (i.e. only participants who missed fewer than 3 daily assignments consecutively or overall in 2 IGs) and available‐case analysis (only participants who took pre‐test and post‐test surveys) |
|
| Participants |
Country: USA
Setting: graduate students from various disciplines at large, public university in the Southwest; training setting: self‐guided online intervention
Age: mean = 28.4 (SD = 6.21); range = 20 ‐ 53 years
Sample size (randomised): 234
Sex: 133 women, 97 men, 3 transgender, 1 other
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: graduate students from various disciplines at large public university in the Southwest Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions):
Reasons for missing data: not specified |
|
| Interventions |
Intervention 1 (relevant for review): positive psychology intervention (PPI) (n = 78)
Intervention 2: informative stress intervention (n = 78)
Control: wait‐list control (n = 78)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; and 3) 3‐month follow‐up (3 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the subgroup data (means and SDs for all outcomes) for graduate students in Health & Wellness and Social & Behavioral Sciences (Yeghnazar 2019 [pers comm]). Subgroup data were not available until writing of the review Study start/end date: June – September 2016 (recruitment in Spring 2016; intervention period from 1 June 2016 to 21 June 2016; 3‐month follow‐up in September 2016) Funding source: study financially supported by the Graduate and Professional Student Association (GPSA) Declaration of interest: not specified Ethical approval needed/obtained for study: IRB approval (ASU IRB STUDY00004364) Comments by study authors: not relevant Miscellaneous outcomes by the review authors: dissertation Correspondence: Pauline Venieris; now: Pauline Yeghnazar Peck (www.therapywithpauline.com/contact); pauline.yeghnazar@gmail.com; chair of dissertation: Prof Richard Kinnier; Counseling and Counseling Psychology Department; Arizona State University, EDB 446G Counseling and Counseling Psychology TEMPE, Arizona State University; kinnier@asu.edu |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The 234 participating students were randomly assigned to the three conditions (PPI, informative stress, and wait list) using an online random assignment generator." Quote: "There were no significant differences between the three groups at pre‐test. No significant differences were found between the treatment groups on any of the covariates, ensuring that the sample sorted evenly into the three treatment groups on the variables used in these analyses." Judgement comment: The investigators describe a random component in the sequence‐generation process (online random assignment generator).; verified baseline comparability of groups for sociodemographic characteristics (all Ps > 0.172) and outcome variables (GSIR, SHI, RSA; all Ps > 0.119) on the basis of analysis (see Appendix P, Table 1) |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | Unclear risk | Quote: "While not specifically told about the number and nature of the three treatment conditions, the form stated that they may or may not be asked to participate in different activities (e.g., exercising, journaling). They were informed that while this was a mostly online study, that they may be asked to attend one of the four campus locations twice throughout the three‐week period. " Quote: "Each group, which consisted of 85 students, was emailed separately to inform them of the study start date (June 1, 2016) and to review what they would be asked to do." Judgement comment: blinding of participants probably ensured (participants not specifically told about number/nature of 3 conditions; only informed that they may or may not be asked to participate in different activities, e.g. exercising, journalling); insufficient information about blinding of study personnel (interventions delivered by online educational system) |
| Blinding of outcome assessment (detection bias) Subjective outcomes | Unclear risk | Judgement comment: insufficient information about blinding of outcome assessment to permit judgement of ‘Low risk’ or ‘High risk’ (online surveys) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Most of the students who dropped out of the study were in the treatment conditions, suggesting that those groups were most impacted by the timing of this study." Quote: "At the three‐month follow‐up, 117 students participated (27% attrition from post‐test and 50% attrition from pre‐test), and were included in the follow‐up analyses" Quote: "At the end of the three‐week period, 160 students completed the post‐test (32% attrition) and were included in the post‐test analyses." Quote: "Thus, 234 participants began the study on the first day." Quote: "Complete participation for the control group meant taking pre‐test and post‐test surveys." Quote: "Complete participation for the experimental and comparison groups meant taking pre‐test and post‐test surveys as well as completing the daily activities for 21 days (and not missing more than 3 days consecutively or overall)." Judgement comment: reasons for missing data likely to be related to true outcome with imbalance in missing data between groups (lost to follow‐up: post‐intervention: IG1: 28, IG2: 38; CG: 8; follow‐up: IG1: 13 further lost to follow‐up; CG: 33 further lost to follow‐up; see Appendix E, Table 1); reasons for missing data not provided (for each group); probably per‐protocol analysis (i.e. only participants who missed fewer than 3 daily assignments consecutively or overall in 2 IGs) and available‐case analysis (only participants who took pre‐test and post‐test surveys) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified (see Appendix Q, Table 2) |
Victor 2018.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): Sample size was calculated a priori using the software G* Power using an expected effect of d = 0.30 and was set to n = 54 participants in total. Based on the assumption of 40% dropouts and exclusions, 30 participants per group or n = 90 in total were sought Imputation of missing data: per‐protocol analysis (i.e. only participants who completed the intervention) and available‐case analysis (i.e. only participants for whom outcomes were obtained and who completed post‐test assessments) AND intention‐to‐treat analysis (ITT) based on 85 participants; last observation carried forward (LOCF) for 5 participants with missing post‐test assessments; 4 participants with missing pretest assessments could not be considered in ITT analysis |
|
| Participants |
Country: Germany
Setting: intervention offered at psychiatric outpatient department of university Witten/Herdecke
Age: mean = 22.85 (SD = 2.49) years
Sample size (randomised): 89; exclusion of 24 students not fulfilling the inclusion criteria AFTER the intervention period due to ethical reasons; including 43 psychology students (28 in 2 groups relevant for this review)
Sex: 42 women, 15 men
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: all participants with Global Severity Index (GSI) value in the Brief Symptom Inventory‐18 (BSI‐18) ≥ 4 (above cut‐off for symptom burden); BSI‐18 GSI: IG 9.95 (5.56), CG1: 11.22 (6.08), CG2: 12.74 (8.35) Population description: university students (including psychology students) Inclusion criteria: symptom burden in the Brief Symptom Inventory (BSI‐18) GSI ≥ 4 at pretest (i.e. above cut‐off estimated in non‐clinical sample in global GSI (M = 3.87); see Spitzer et al 2011) Exclusion criteria: 1) psychosis; and 2) suicidality Attrition (withdrawals and exclusions):
Reasons for missing data:
|
|
| Interventions |
Intervention: Personal Model of Resilience (PRM) (n randomised not stated; n = after exclusion of 24 students not fulfilling the criteria: 22)
Control 1: attention control (ABC model)(relevant for this review) (n randomised not stated; n = after exclusion of 24 students not fulfilling the criteria: 19)
Control 2: wait‐list control (n randomised not stated; n = after exclusion of 24 students not fulfilling the criteria: 24)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) 3‐week follow‐up (3 weeks post‐intervention) Adverse events: no systematic assessment of adverse events; but no negative effects mentioned by participants in verbal feedback |
|
| Notes |
Contact with authors: We contacted the authors for subgroup outcome data of psychology students (i.e. means and SDs for all outcomes reported in Table 2 with the number of participants analysed) (Victor 2019 [pers comm]). Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: study was positively evaluated by the IRB of the university Witten/Herdecke Comments by study authors: not relevant Miscellaneous outcomes by the review authors: article in German (translated); subgroup outcome data for psychology students sent from authors Correspondence: Dr Philipp Victor; Department of Psychology and Psychotherapy, University Witten/Herdecke, Alfred‐Herrhausen‐Straße 44, 58448 Witten; philipp.victor@uni‐wh.de |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Die Intervention (PRM) wurde im randomisierten kontrollierten Prä‐Post‐Design mit einer aktiven KVT‐Vergleichsintervention (ABC) und einer Wartekontrollgruppe (WKG) evaluiert." ["The intervention (PRM) was evaluated in a randomised controlled pre‐post design with an active CBT control condition (ABC) and a waitlist control group (WKG)."] Quote: "Teilnehmende wurden auf Basis einer zufallsgenerierten Liste in Reihenfolge ihrer Teilnahme‐zusage einer Bedingung zugeordnet."; ["Based on a randomly generated list, participants were assigned to conditions in order of their confirmation to participate in the study."] Quote: "Vor Beginn der Intervention bzw. der Wartezeit unterschieden sich die drei Gruppen in ANOVAs auf keiner Evaluationsdimension."; ["Before the beginning of the intervention or the waiting period, the three groups did not differ in any dimension of evaluation in ANOVAs."] Quote: "Zwischen den Interventionsgruppen bestanden Prä keine signifikanten Unterschiede in Alter, Geschlecht, vorangegangener psychotherapeutischer Behandlung, Studiengang, Semesteranzahl (Tabelle 1) oder einem der eingesetzten Messinstrumente (Tabelle 2)."; ["At pretest, there were no significant differences between the groups in age, gender, previous psychotherapeutic treatment, studies or number of semesters (Table 1) or any of the used assessment instruments (Table 2)."] Judgement comment: investigators describe a random component in the sequence‐generation process (random list); verified baseline comparability of groups for sociodemographic characteristics (age, gender, previous treatment, studies, semester; all Ps > 0.21) and outcomes of interest on the basis of analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment (online survey); but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Abbildung 1. CONSORT Flussdiagramm. Persönliches Resilienzmodell (PRM), ABC‐Modell (ABC), Wartekon‐ trollgruppe (WKG)."; ["Figure 1. CONSORT Flow chart. Personal model of resilience (PRM), ABC model (ABC), waitlist control (WKG)."] Quote: "89 Studierende interessierten sich für die Studie und wurden den drei Bedingungen PRM, ABC oder WKG zugelost. 85 begannen die erste Online‐Messung und stimmten Teilnahme und Datenauswertung zu. 4 brachen bereits nach der Randomisierung ab, 3 davon in der WKG."; ["89 students were interested in the study and were randomized to the three conditions PRM, ABC and WKG. 85 began the first online assessment and consented to participate in the study and the data processing. 4 withdrew after randomization, 3 of them in the WKG."] Quote: "61 Studierende wiesen Prä eine Symptombelastung von BSI‐18 GSI ≥ 4 auf; 57 nahmen an der Post‐Messung teil und wurden in die Analyse einbezogen (Completer)."; ["At pretest, 61 students had a symptom burden of ≥ 4 in the BSI‐18 GSI (‐‐> were included in the study); 57 took part in the posttest assessment and were considered in the analysis (completers)"] Quote: "Dropouts wurden mit Completern hinsichtlich demographischer und testpsychologischer Kennwerte verglichen. Eine Intention‐to‐treat‐Analyse wurde mittels ANCOVAs analog der oben beschriebenen Systematik für die Gesamtstichprobe durchgeführt; bei fehlenden Post‐Messungen wurde jeweils der Prä‐Wert fortgeschrieben (LOCF)."; ["Dropouts were compared with completers concerning demographic and psychological measures. Analogous to the description above, an intention‐to‐treat analysis using ANCOVAs was performed for the total sample; in case of missing posttest values, the corresponding pretest value was used (LOCF)."] Judgement comment: reasons for missing data likely to be related to true outcome with (slight) imbalance in missing data between groups (PRM: 2 withdrew from the intervention due to lack of time; ABC: 1 withdrew after randomisation (reasons unknown); WKG: 3 withdrew after the randomisation, 2 did not complete post‐test assessment); per‐protocol analysis (i.e. only participants who completed the respective intervention; "completers") and available case analysis (only participants for whom outcomes were obtained at post‐test) + intent‐to‐treat analysis (with last observation carried forward method) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Waddell 2005.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
|
| Participants |
Country: Canada Setting: baccalaureate nursing program in an urban university Age: range = 20‐40 years Sample size (randomised): 25 Sex: not specified for total sample Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: students from the second and third years of a basic baccalaureate nursing program Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): after phase 1: n = 5 dropouts (IG: 4/14 (28.6%); CG: 1/11 (9.1%)) Reasons for missing data: academic and family life demands (n = 5) |
|
| Interventions |
Intervention: career planning and development programme (n = 14)
Control: no intervention (n = 11). Participants in CG offered CPD program at completion of phase 2; at that time, they also received career planning and development book with student career planning and development workbook folder
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention (pre‐test of phase 1); 2) during intervention (within 2 weeks after intervention in phase 1); 3) during intervention (pre‐test of phase 2); and ) 1‐month follow‐up (1‐month after intervention in phase 2, i.e. 1 month after total intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: no correspondence required Study start/end date: phase 1: during fall 1999/2000 academic year; phase 2: 2000/2001 academic year Funding source: not exactly specified; probably also by scholarship of Gail J Donner and Mary M Wheeler (donnewheeler) Declaration of interest: not specified Ethical approval needed/obtained for study: approved by the university ethics review board at the study site Comments by authors: not relevant Miscellaneous outcomes by the review authors: not relevant Correspondence: Janice Waddell, RN, PhD; Department of Nursing, Ryerson University, 350 Victoria Street, Toronto, Ontario M5B 2K3, Canada; jwaddell@ryerson.ca |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "All participants in Phase One were invited to continue their involvement in Phase Two, with the understanding that participants would remain in the group (intervention/control) to which they were originally randomly assigned." Quote: "The self‐selected participants from the initial randomized group were then randomly assigned to control or intervention groups." Quote: "No significant differences in career planning activities and career decision‐making were found between the control and intervention groups before the career planning and development program intervention was introduced." Judgement comment: insufficient information about random sequence generation to permit judgment of ‘Low risk’ or ‘High risk’; verified baseline comparability of groups for outcomes of interest on the basis of analysis; baseline comparability for sociodemographic characteristics unclear |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgment of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (large part of intervention is face‐to‐face) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; however, due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "All participants in Phase One were invited to continue their involvement in Phase Two, with the understanding that participants would remain in the group (intervention/control) to which they were originally randomly assigned. Of the 25 original participants, 5 students dropped out of the study citing academic and family life demands. The remaining 20 participants (10 in each group) requested to continue their study involvement for the 2000/2001 academic year." Quote: "After the end of the project and the academic term, however, 5 of the 10 (3 third‐year and 2 fourth‐year students) intervention group participants" Quote: "All Phase One and Two participants completed and returned their questionnaires." Judgement comment: reasons for missing data unlikely to be related to true outcome (imbalance in missing data between groups: after phase 1: n = 5 dropouts in total; IG: n = 4; CG: n = 1; but see reasons for missing data: family and academic life demands); not clearly specified how many participants were analysed (phase 2 post‐test) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified |
Waddell 2015.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: no imputation of missing data; not specified if attrition from intervention or lost to assessments; probably per‐protocol analysis (only participants who took part in allocated intervention) and available‐case analysis (only participants for whom outcomes were obtained) |
|
| Participants |
Country: Canada Setting: collaborative baccalaureate nursing degree programme at academic sites (2 colleges, 1 university site) Age: range = 18 ‐ 22 years Sample size (randomised): 142 (recruited in 2 cohorts in year 1, n = 120, and beginning of year 3, n = 22) Sex: not specified; most of analysed sample was female Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: nursing students in a collaborative baccalaureate degree program Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): probably attrition of n = 70 participants over study course (not specified which group) Reasons for missing data: CG: probably information about assignment to control group; IG: probably due to time commitment; most students withdrew in year 2,which is considered by students and faculty to be most demanding and difficult |
|
| Interventions |
Intervention: career planning and development (CPD) programme (n not specified; for 72 participants analysed: n = 33)
Control: TAU (standard undergraduate curriculum group) (n not specified; for 72 participants analysed: n = 39)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention (year 2 of baccalaureate programme, prior to randomisation); 2) during intervention, year 3 of baccalaureate programme; 3) post‐intervention, year 4 of baccalaureate programme; and 4) 12‐month follow‐up (12 months post‐intervention/after baccalaureate programme); 4) presented in 2nd report Adverse events: not specified |
|
| Notes |
Contact with authors: We contacted the authors for the number of participants randomised to each group and whether there were 70 missing, but they had not responded at the time of writing this review Study start/end date: not specified Funding source: funding support by Social Sciences and Humanities Council Declaration of interest: not specified Ethical approval needed/obtained for study: research ethics board approval Comments by authors: not relevant Miscellaneous outcomes by the review authors: Waddell 2015 is the first of 3 reports on this study; besides this 1st report on the undergraduate student outcomes of the programme, 2nd paper will examine graduate nurses’ experiences at 12 months post‐graduation, 3rd paper will explore faculty outcomes for those participating in the programme Correspondence: Janice Waddell; Department of Nursing, Ryerson University, 350 Victoria Street, Toronto, Ontario M5B 2K3, Canada; jwaddell@ryerson.ca |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Eligible students who consented to participate were randomly assigned by means of a random numbers chart with allocation concealment, to one of two conditions: (a) a 4‐year CPD group (intervention) or (b) a 4‐year standard undergraduate curriculum group (control)." Quote: "There were no significant group differences in terms of marital status (majority were single), number of children (majority were childless), registration with the Registered Nurses Association of Ontario (majority were not members), or employment status. Finally, there were no significant group differences in terms of previous CPD training/ involvement outside of this study (most respondents reported no previous engagement in CPD activities)." Quote: "Mean career scores, including total scores (p = 0.002) and subscale scores, were higher for all intervention participants except at Time 1 (when baseline scores for the initial 142 participants were gathered prior to randomization where there were no significant between group differences)." Judgement comment: investigators describe a random component in the sequence‐generation process (random‐numbers chart); verified baseline comparability of groups for sociodemographic characteristics and outcome variables on the basis of analysis (mean career scores refers to total score of CPD activities and self‐efficacy as well as subscales in Table 1) |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Eligible students who consented to participate were randomly assigned by means of a random numbers chart with allocation concealment, to one of two conditions: (a) a 4‐year CPD group (intervention) or (b) a 4‐year standard undergraduate curriculum group (control)." Judgement comment: insufficient information about allocation concealment to permit judgement of 'Low risk' or 'High risk'; unclear if random‐sequence generation was concealed from personnel or participants, or both; exact method not described |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "A large number of those randomized into the control group dropped out of the study after completing the pre‐study measures and being informed of their assignment to the control group." Judgement comment: no blinding of participants and personnel (face‐to‐face intervention; CG participants were informed of being in the control group) and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; but due to performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "One hundred and twenty students in their first year in the program consented to participate (Cohort # 1). Due to participant attrition in Year 2 of the program, a second recruitment phase was undertaken as the Year 2 cohort was beginning the third year of their program." Quote: "A final sample size, after accounting for attrition, was an additional 22 participants (Cohort # 2) for a total of 142 participants entering the third year of the program." Quote: "The final sample for quantitative data analysis consisted of 50 participants from Cohort #1 (Intervention = 29, Control = 21) and 22 participants from Cohort #2 (Intervention = 4, Control = 18) for a total of 72 participants, 33 of whom were in the intervention group and 39 in the control group." Quote: "large number of those randomized into the control group dropped out of the study after completing the pre‐study measures and being informed of their assignment to the control group." Quote: "The time commitment involved may have been a major factor that contributed to attrition in the intervention group. These participants were required to attend one 3‐hour CPD workshop per term, per program year. The majority of students who withdrew from the study during its first year were in Year 2, which is considered by students and faculty to be the most demanding and difficult, as students’ clinical hours increase to 11 per week in addition to five classroom or online courses per term." Judgement comment: insufficient information about attrition/exclusions (number of participants randomised to each group not stated; number of attrition per group not specified; not specified if attrition from intervention or lost to assessments); probably per‐protocol analysis (only participants who took part in allocated intervention) and available‐case analysis (only participants for whom outcomes were obtained) since only 72 participants were analysed |
| Selective reporting (reporting bias) | Unclear risk | Judgement comment: no study protocol available; published report seems to include all expected outcomes, including those that were prespecified; unclear if Time 4 refers to 12‐month follow‐up since not further specified in text |
Wang 2012.
| Study characteristics | ||
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified Imputation of missing data: no imputation of missing data; per‐protocol analysis (only participants who took part in intervention) |
|
| Participants |
Country: China Setting: students from medical university; setting of training not specified Age: mean = 20.45 (SD = 0.97) years Sample size (randomised): 70 Sex: 40 women, 28 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: Symptom Checklist (SCL‐90) subscales: somatisation: IG: 1.58 (0.41), CG: 1.55 (0.38); obsessive‐compulsive: IG: 2.72 (0.38), CG: 2.55 (0.48); interpersonal sensitivity: IG: 2.32 (0.51), CG: 2.17 (0.46); depression: IG: 2.06 (0.42), CG: 2.10 (0.52); anxiety: IG: 2.00 (0.38), CG: 2.02 (0.43); hostility: IG: 1.81 (0.47), CG: 1.84 (0.51); phobic anxiety: IG: 1.84 (0.63), CG: 1.71 (0.46); paranoid ideation: IG: 1.79 (0.42), CG: 1.90 (0.41); psychoticism: IG: 1.78 (0.32), CG: 1.82 (0.28); other symptoms: IG: 1.95 (0.53), CG: 1.83 (0.47); Global Severity Index: IG: 179.70 (19.70), CG: 176.70 (23.00) Population description: students (freshman and sophomores) with mental crisis from medical university Inclusion criteria: participants with psychoticism factor > 2.2 in SCL‐90 Exclusion criteria: not specified Attrition (withdrawals and exclusions): 2 dropouts (did not participate); unclear which group Reasons for missing data: not specified |
|
| Interventions |
Intervention: positive psychology‐oriented group counselling (n = not specified; of 68 analysed participants: n = 33)
Control: not specified (n = not specified; of 68 analysed participants: n = 35) |
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention (1 week before start of intervention); 2) post‐intervention ; and 3) 3‐month follow‐up (3 months post‐intervention) Adverse events: not specified |
|
| Notes |
Contact with authors: no correspondence required Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by authors: not relevant Miscellaneous outcomes by the review authors: article in Chinese (translated) Correspondence: Zhe Wang; School of Nursing, Southern Medical University, Guangzhou 510515, China |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "在检出的本科生中,遵循自愿招募的原则,经简 短访谈后纳入团体。 鉴于团体干预的适应性,排除症 状自评量表中精神病性因子大于 2.2 的成员,最终选 取大一、大二学生 70 名,随机分配到试验组和对照组" ["In view of the adaptability of group intervention, members with a psychotic factor greater than 2.2 in the self‐rating scale of the exclusion syndrome were selected, and 70 freshmen and sophomores were selected and randomly assigned to the experimental group and the control group."] Quote: "全程有效参与干预的学生共 68 名,其中试验组 33 名, 男 12 名,女 21 名,年 龄(20.4±1.09)岁,对 照 组 35 名,男 16 名,女 19 名,年龄 20.5±0.85)岁,两组间年 龄、性别、专业等基本情况经分析差异无统计学意义P>0.05)" ["A total of 68 students participated in the intervention, including 33 experimental groups, 12 males and 21 females, aged (20.4±1.09) years old, 35 in the control group, 16 males and 19 females, aged 20.5±0.85). At the age of the two groups, the differences in age, gender, and specialty between the two groups were not statistically significant (P>0.05)"] Quote: "3.1 两组间测量指标的基线比较 干预前两组各 项指标平衡,均无统计学意义(P>0.05)" ["3.1 Baseline comparison of measured indicators between the two groups. There was no statistically significant difference between the two groups before the intervention (P>0.05).] Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’; verified baseline comparability of groups for sociodemographic characteristics and outcomes of interest on the basis of analysis |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Judgement comment: blinding of participants and personnel probably not done (face‐to‐face intervention) and outcome is likely be related to true outcome |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Judgement comment: insufficient information about blinding of outcome assessment; but due to potential performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Judgement comment: number of participants randomised to each group not specified, unclear in which group dropout of 2 occurred; per‐protocol analysis (only participants who participated in the study) |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
Warnecke 2011.
| Study characteristics | ||
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): target sample size for the trial was 42 students per group (control and intervention); This number is based on data from a previous study of university students, which found a mean pre‐test PSS score of 18.11 (SD 6.19). These data are consistent with findings from the small unpublished pilot trial undertaken in our cohort last year. The trial was powered to detect a 4‐point difference (SD 0.6) in PSS score, using a 2‐tailed test, α = 0.05 and power = 0.80, and allowing for a 10% dropout rate. The cohort from which we recruited our participants numbered 194 students Imputation of missing data: no imputation of missing data specified (missing data treated as absent and were not assigned a score; no participants excluded from analysis); according to authors intention‐to‐treat analysis; based on outcome data received from authors (24 analysed in IG, 32 analysed in CG): available‐case analysis | |
| Participants |
Country: Australia
Setting: guided mindfulness practice using CD; home setting
Age: mean = 23.92 (SD = 3.2) years
Sample size (randomised): 66
Sex: 42 women, 24 men
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline:
Population description: medical students Inclusion criteria: medical students in the final 2 years of their degree course Exclusion criteria: individuals with potentially significant psychological distress in need of immediate assessment and management (K10 questionnaire score ≥ 30) Attrition (withdrawals and exclusions): 1 withdrawal in IG after trial start (withdrew before data collection and did not receive allocated intervention); lost to follow‐up: post‐intervention: 9 (IG: 7, CG: 2); 2‐month follow‐up (only in IG): 5 Reasons for missing data: no reasons specified; participants lost to follow‐up failed to respond to correspondence |
|
| Interventions |
Intervention: guided mindfulness practice (brief self‐guided mindfulness of breath practice) (n = 32)
Control: TAU (n = 34)
|
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (end of 8‐week intervention); and 3) 2‐month follow‐up (i.e. 2 months post‐intervention or 4 months after baseline) ONLY in IG Adverse events: no reported adverse effects of intervention |
|
| Notes | Contact with authors: We contacted the authors for the post‐intervention means and SDs for both primary and secondary outcomes in both groups with the number of participants analysed, respectively. We also asked if missing data had been imputed (Warnecke 2019 [pers comm]). Study start/end date: June 2009 (recruitment) – October 2009 Funding source: supported by a seeding grant awarded by the Australian and New Zealand Association for Health Professional Educators (ANZAHPE) Declaration of interest: none Ethical approval needed/obtained for study: approval from the University of Tasmania Human Research Ethics Committee (H0010500) Comments by study authors: not relevant Miscellaneous outcomes by the review authors: post‐intervention means and SDs for outcomes received from author Correspondence: Dr Emma Warnecke; School of Medicine, University of Tasmania; emma.warnecke@utas.edu.au; Private Bag 34, Hobart, Tasmania 7001, Australia; Tel: 00 61 3 6226 4757; Fax: 00 61 3 6226 4894 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: We carried out a multicentre, single‐blinded, randomised controlled trial"
Quote: "Eligible participants were randomised centrally, using block randomisation with block sizes of two, to the intervention arm or the usual care control arm." Quote: "There were no statistically significant differences between the two arms at baseline in either demographics or baseline outcome scores." Judgement comment: insufficient information about random‐sequence generation to permit judgement of ‘Low risk’ or ‘High risk’ (method of random sequence generation is not described); verified baseline comparability of groups for sociodemographic characteristics and outcomes of interest on the basis of analysis (all Ps > 0.12) |
| Allocation concealment (selection bias) | Unclear risk | Judgement comment: insufficient information about allocation concealment to permit judgement of ‘Low risk’ or ‘High risk’ (i.e. method of allocation concealment during randomisation procedure is not described, only blinding of intervention specified) |
| Blinding of participants and personnel (performance bias) Subjective outcomes | High risk | Quote: "We conducted a multicentre, single‐blinded, randomised controlled trial (RCT) with intention‐to‐treat analysis." Quote: "Randomisation was not blinded to the individual participant because of the nature of the intervention." Quote: "Participant packs were prepared centrally. All packs contained a CD cover so that trial packs in the two arms of the study looked identical. The purpose of this was to conceal allocation." Quote: "Participants were specifically advised not to inform others about which group they were in and not to discuss the intervention. Participants were also advised not to give the intervention to anyone else." Judgement comment: single‐blind study; no blinding of participants and the outcome is likely to be influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) Subjective outcomes | High risk | Quote: "Both the research assistant who scored and entered data and the statistician who analysed the results were blinded to group allocation." Judgement comment: insufficient information about blinding of outcome assessment; research assistants who scored and entered as well as analysed the data were blinded to group allocation; but unclear if blinded research assistant also performed the outcome assessment (i.e. distributed the questionnaires); due to performance bias (no blinding of participants), the review authors judge that the participants' responses to questionnaires may be affected by the lack of blinding (i.e. knowledge and beliefs about intervention they received) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: "Figure 1 Progress of participants through the trial"
Quote: "One participant withdrew from the trial after it began. This participant had been allocated to the intervention arm, but withdrew before any data had been collected. Baseline data (T1) were collected for all 65 remaining participants." Quote: "We conducted a multicentre, single‐blinded, randomised controlled trial (RCT) with intention‐to‐treat analysis." Quote: "Given the difference in dropout rates between the intervention and control arms, data were analysed to look for any statistical difference in those who did not complete T2 data. We found no statistically significant difference in age, sex or baseline scores for perceived stress, depression, anxiety or stress in participants who dropped out of the trial, suggesting that they left at random." Quote: "Results were analysed on an intention‐to‐treat basis. Missing data were treated as absent and were not assigned a score. No participants were excluded from the analysis." Judgement comment: reasons for missing data unlikely to be related to true outcome (imbalance in missing data between groups: IG: 1 withdrawal, 7 lost to follow‐up vs CG: 0 withdrawal, 2 lost to follow‐up; but see additional analysis with no significant difference in demographic and outcome variables between completers and non‐completers suggesting random loss); according to authors, intention‐to‐treat analysis; but missing data were treated as absent and not assigned a score; based on outcome data received from authors (24 analysed in IG, 32 analysed in CG): available‐case analysis |
| Selective reporting (reporting bias) | Low risk | Judgement comment: no study protocol or trial registration available but it is clear that the published reports include all expected outcomes, including those that were prespecified |
α: alpha, significance level; ASQ: Attributional Style Questionnaire; BAI: Beck Anxiety Inventory; BDI‐II: Beck Depression Inventory; BPS: best possible self; Brief‐COPE: Brief Coping Orientation to Problems Experience Scale; BSN: Baccalaureate nursing students; BRS: Brief Resilience Scale; BSI: Brief Symptom Inventory; CBT: cognitive behavioural therapy; CD: compact disc; CDMSES‐SF: Career Decision‐Making Self‐Efficacy Scale ‐ Short Form; d: delta (Cohen's d, effect size); CD‐RISC: Connor‐Davidson Resilience Scale; CES‐D: Center for Epidemiology Studies Depression Scale; CFS: Coping Flexibility Scale; CG: control group; CORE‐OM: Clinical Outcomes in Routine Evaluation ‐ Outcome Measure; CPAM: Career Planning Activities Measure; CPD: career planning and development; DASS: Depression, Anxiety and Stress Scale; ERS: Emotion Regulation Scale; FFMQ: Five Facets Mindfulness Questionnaire; GAD‐7: Generalised Anxiety Disorder scale; GPA: grade point average; Grit: grit as "perseverance and passion for long‐term goals (i.e. working strenuously toward challenges, maintaining effort and interest over years despite failure, adversity, and plateaus in progress"; Duckworth 2007, p 1087‐8); GSEQ: General Self‐Efficacy Questionnaire; GSI: Global Severity Index; GSI‐R: Graduate Stress Inventory ‐ Revised; HADS‐D: Hospital Anxiety and Depression Scale ‐ German version; IG: intervention group; IRB: Institutional Review Board; ITPQ: Implicit Personality Theory Questionnaire; ITT: intention‐to‐treat analysis; JSEHPS: Jefferson Scale of Empathy ‐ Health Professions ‐ Students version; K10: Kessler Psychological Distress Scale; KIMS‐E: Kentucky Inventory of Mindfulness Skills; LOCF: last observation carried forward; LSAS‐SR: Liebowitz Social Anxiety Scale ‐ Self‐report; MASQ: Mood and Anxiety Symptom Questionnaire; MAST: Maastricht Acute Stress Test; MBI: Maslach Burnout Inventory; MBSR: Mindfulness‐Based Stress Reduction; mDES: Modified Differential Emotion Scale; MSC: Brief Mindfulness‐based Compassion; MSS: Mindfulness Skills for Students; n = sample size (e.g. in respective group), NHS: National Health Service; NURSE: Nurture nurse, Use resources, foster Resilience, Stress and Environment management; OQ‐45.2: Outcome Questionnaire; PANAS: Positive and Negative Affect Schedule; PCQ: Psychological Capital Questionnaire; PMSS‐D: Perceived Medical School Stress Scale ‐ German version; PRP: Penn Resilience Program; PSQI: Pittsburgh Sleep Quality Index; PSS: Perceived Stress Scale; PTSD: post‐traumatic stress disorder; RCI: Resilience and Coping Intervention; RCT: randomised controlled trial; RS: Resilience Scale; RSA: Resilience Scale for Adults; RSES: Rosenberg Self‐Esteem Scale; SCL90‐R: Symptom Check List ‐ Revised; SCL‐27‐plus: Symptom Checklist‐27 plus; SCS: Self‐Compassion Scale; SD: standard deviation; SPS: Social Provision Scale; STAI: State‐Trait Anxiety Inventory; SWLS: Satisfaction With Life Scale; US: unconditioned stimulus; USB: universal serial bus; UWES‐17: Utrecht Work Engagement Scale; vs: versus; WEMWS: Warwick‐Edinburgh Mental Well‐being Scale; WHOQOL: World Health Organization Quality of Life Scale; WOC: Ways of Coping Questionnaire.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| ACTRN12617000300370 | Study withdrawn/terminated prematurely |
| Brady 2016 | Ineligible intervention |
| De la Fuente 2018 | Ineligible intervention |
| De Vibe 2013 | Ineligible intervention |
| Duan 2019 | Ineligible intervention |
| Dvořáková 2017 | Ineligible intervention |
| Esch 2013 | Ineligible intervention |
| Huennekens 2018 | Ineligible intervention |
| Pogrebtsova 2018 | Ineligible intervention |
| Sampl 2017 | Ineligible intervention |
| Song 2015 | Ineligible intervention |
| Van Dijk 2015 | Ineligible intervention |
| Victor 2017 | Ineligible study design |
Characteristics of studies awaiting classification [ordered by study ID]
Arch 2014.
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified for total study Imputation of missing data: not specified; probably available‐case analysis (only participants who completed TSST |
| Participants |
Country: USA Setting: laboratory Age: mean = 19.53 years (analysed sample) Sample size (randomised): not specified; probably 107 Sex: 105 women Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: no exact values for state anxiety specified Population description: undergraduate women Method of recruitment: not specified Inclusion criteria: 1) reported no use of oral contraception or other prescription medication; 2) fluent in English; 3) non‐smokers; 4) non‐drug users; 5) physically healthy (no reported fever or illnesses, no diseases or conditions that may impact stress responses such as endocrine disorders, autoimmune disorders, cardiovascular or respiratory conditions, etc.) Exclusion criteria: 1) drinking caffeinated or alcoholic beverages in the 3 hours prior to the TSST; 2) exercising in the 3 hours prior to the TSST; 3) consuming anything other than water for the hour prior; 4) using any drugs or medications for 24 hours prior Attrition (withdrawals and exclusions): 3 exclusions from salivary biomarker analyses; 1 withdrew; 1 was withdrawn Reasons for missing data: 2 withdrawals: 1 refused to do TSST, i in high distress at baseline (i.e. pale, shaking, appearing physical unwell); 3 exclusions from salivary biomarker analyses due to technical problems |
| Interventions |
Intervention: self‐compassion training (n randomised not specified)
Control 1: attention control (placebo; n randomised not specified)
Control 2: no intervention (n randomised not specified)
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported:
Adverse events: not specified |
| Notes |
Contact with authors: We contacted the study authors for the number of participants randomised in total (N = 107?) and to each group, as well as the means and SDs for all outcomes at each measurement point with the number of participants analysed, respectively. In another inquiry, we asked whether healthcare students were included in the sample. We received the response that the "majors of the undergraduate female subjects in the study had not been asked; however, they were recruited from an Intro Psychology class and the corresponding author was sure that a decent portion went on to be psychology majors, although she had no way of knowing which ones" (quote; Arch 2019 [pers comm]). Study start/end date: not specified Funding source: 1 author supported with startup funds from the University of Colorado Boulder; 1 author partially supported by National Institutes of Health (NIH) grant (CA126971) Declaration of interest: All study authors declare that they have no conflicts of interest Ethical approval needed/obtained for study: human participants IRB approval Comments by study authors: not relevant Miscellaneous outcomes by the review authors: according to the study authors, undergraduates were recruited from introductory psychology classes; but it is unclear if the final sample included participants who were psychology major students Correspondence: Joanna J Arch, PhD; Department of Psychology and Neuroscience, University of Colorado Boulder, 345 UCB Muenzinger, Boulder, CO, 80309‐0345 USA; Joanna.Arch@Colorado.edu; telephone: 303‐492‐4634 |
Baeza‐Velasco 2020.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Bauman 2014.
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): findings demonstrate that the intervention lacked power to produce statistically significant group differences; relatively small sample size of 41 students, with only 19 students in the intervention group and 22 students assigned to control group, limited the statistical significance of the findings Imputation of missing data: no imputation of missing data; available‐case analysis (only participants for whom outcomes were obtained at pretest and 2 post‐tests, i.e. without 4 participants without missing data at 2‐week follow‐up) |
| Participants | Country: USA Setting: students at private, faith‐based liberal arts institution on the West coast; setting of training not specified Age: range = 18 – 24 years; 18 years: 16 (39%), 19 years: 14 (34.1%), 20 years: 7 (17.1%), 21 years: 1 (2.4%), 22 years: 1 (2.4%), 23 years: 1 (2.4%), 24 years: 1 (2.4%) Sample size (randomised): not specified, probably 41 Sex: 31 women, 10 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: traditionally‐aged undergraduate students (18 to 24 years) at a private, faith‐based liberal arts institution on the West coast Method of recruitment: students enrolled in the following undergraduate courses during the Fall 2013 semester: Foundations of Psychology (for psychology majors), Introduction to Psychology (for non‐psychology majors), and Introductory Statistics Inclusion criteria: 1) students enrolled in following undergraduate courses during Fall 2013 semester: Foundations of Psychology (for psychology majors), Introduction to Psychology (for non‐psychology majors), Introductory Statistics; 2) students enrolled in these courses required to obtain 4 credit hours of research participation as part of course curriculum Exclusion criteria: not specified Attrition (withdrawals and exclusions): 4 cases excluded at 2‐week follow‐up (post‐test 2) Reasons for missing data: missing data from that post‐test |
| Interventions |
Intervention: Psychological Capital (PsyCap) intervention "Navigating the College Experience" (n randomised not specified; in analysed sample: n = 19)
Control: wait‐list control (n randomised not specified; in analysed sample: n = 22)
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (1 day after the conclusion of the treatment group’s participation in the PsyCap intervention; post‐test 1); 3) 2‐week follow‐up (2 weeks after the intervention; post‐test 2); 4) post‐intervention in CG after their participation in 2‐week intervention (post‐test 3, only in CG) Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors for the number of participants randomised (41 or more since 4 exclusions?) in total and to each group as well as the amount of missing data in each group. We also asked whether an available‐case analysis post‐test had been performed. In a second inquiry, we also asked whether healthcare students were included in the sample. The author responded and expressed her openness to provide the data (Bauman 2019 [pers comm]). However, the response did not include the information on whether healthcare students were included in the final sample; data have not so far been received Study start/end date: not specified; recruitment during Fall 2013 semester Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: approval from Azusa Pacific University’s IRB upon submission of the research design and instruments Comments by study authors: not relevant Miscellaneous outcomes by the review authors: dissertation; recruitment at psychology courses, but unclear if final sample included participants who were psychology major students Correspondence: Leslie Vaccarello Bauman; dissertation committee chair: Laurie A. Schreiner, PhD; School of Behavioral and Applied Sciences, Department of Higher Education, Azusa Pacific University, Duke 502; lschreiner@apu.edu; Phone (626) 815‐5349; Fax (626) 815‐5408 |
Beadel 2016.
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: no imputation of missing data; probably per‐protocol analysis (see flow chart; without 33 exclusions in both groups and without 7 participants who discontinued intervention; n = 50 analysed) |
| Participants | Country: USA Setting: recruitment from college; training and CO2 breathing challenge in laboratory Age: not specified Sample size (randomised): 90 Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: college students Inclusion criteria: college students scoring 27,5 or higher on the ASI Exclusion criteria: 1) serious, unstable illnesses, including type I and type II diabetes mellitus, hepatic, renal, gastroenterologic, respiratory, cardiovascular, endocrinologic, neurologic, immunologic, or haematologic disease; 2) 1 or more past seizures without a clear and resolved aetiology; 3) a concussion or other head trauma within the past month; 4) current or past episodes of psychosis; 5) currently taking antidepressants or a non‐psychotropic medication with psychotropic effects (e.g. beta‐adrenergic blockers), unless the dosage has been stable for a minimum of 1 month prior to the study; 6) self‐reported confirmation or possibility of pregnancy; 7) no benzodiazepine medication for at least 48 hours prior to final session of the study (CO2 breathing challenge) Attrition (withdrawals and exclusions): 7 withdrawals from interventions (IG: 2, CG: 5); 5 lost to follow‐up (IG: 2, CG: 3); 33 exclusions (IG: 14, CG:19) Reasons for missing data: 33 exclusions (did not meet ASI cut‐off at study session 1); PDSS not usable to assess outcomes (administered at baseline, post‐training and follow‐up, but due to skip pattern in the measure, only 16 completed full measure at all time points); reasons for losses to follow‐up or withdrawals from intervention not specified |
| Interventions |
Intervention: Cognitive Bias Modification‐Interpretation (CBM‐I) (Ambiguous Scenario Training) (n = 45)
Control: attention control (sham version); neutral version of CBM (n = 45)
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 2‐month follow‐up (2 months after final laboratory session) Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors for the number of participants analysed in each group at post‐test and follow‐up as well as means and SDs for SUDS at the beginning and at the end of CO2 breathing challenge in both conditions. In a second inquiry, we also asked if healthcare students were included in the sample. We received the response from the authors that "all of the participants were college undergraduates enrolled in a participant pool from introductory psychology courses, but there were no additional information about whether of the participants may have been health professionals, though this is unlikely" (Beadel 2019 [pers comm]). Study start/end date: not specified Funding source: funded by a Templeton Science of Prospection Award to Bethany Teachman Declaration of interest: Jessica R. Beadel, Andrew Mathews, Bethany A. Teachman declares that they have no conflict of interest Ethical approval needed/obtained for study: not specified Comments by study authors: not relevant Miscellaneous outcomes by the review authors: according to authors, college undergraduates enrolled in participant pool from introductory psychology courses; unclear if any health professionals (though unlikely) Correspondence: Jessica R. Beadel, University of Virginia, P.O. Box 400400, Charlottesville, VA 22904, USA; jrb2mx@virginia.edu |
Chen 2018b.
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified in conference abstract Imputation of missing data: not specified |
| Participants | Country: China Setting: not specified Age: not specified Sample size (randomised): 40 Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: students with depression Population description: urban college students with depression Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: cognitive coping group training and psychological intervention (n randomised not specified)
Control: TAU (normal training; n randomised not specified)
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 6‐month follow‐up; only pre‐intervention difference reported Adverse events: not specified |
| Notes |
Contact with authors: We were not able to contact the study authors on whether the intervention focused on resilience and if healthcare students were included in the final sample, since we identified no contact data (e‐mail address) of the authors. Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by study authors: not relevant Miscellaneous outcomes by the review authors: several eligibility criteria of this review unclear (inclusion of healthcare students, focus on resilience) Correspondence: Chen C.Y.; Wuhan University of Technology, Wuhan, 430070, China and Zhongnan University of Economics and Law, Wuhan, 430073, China; no e‐mail address identified |
Clark 2019.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Crane 2020.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Despeaux 2019.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
DRKS00011265.
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified in trial registration Imputation of missing data: not specified |
| Participants |
Country: Germany, Austria, Switzerland
Setting: online intervention
Age: not specified
Sample size (randomised): 264 targeted
Sex: not specified
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified
Population description: college students with significant minor resilience
Inclusion criteria: 1) student status; 2) significant minor resilience (1 SD below average); 3) internet access, consent; 4) sex: both; 5) age: no minimum or maximum age limit
Exclusion criteria: 1) individuals who have been diagnosed with a mental disorder within the past 12 months; 2) individuals who are on a waiting list for a psychotherapy, are currently in treatment or have experienced psychotherapeutic treatment in the last 12 months; 3) current or life‐longing psychotic or bipolar disorder; 4) individuals with high suicide risk Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: StudiCare: Resilienz (n randomised not specified)
Control: wait‐list control (n randomised not specified)
|
| Outcomes |
Outcomes collected and reported: Primary outcome:
Secondary outcomes:
Outcomes reported not specified Time points measured and reported: post‐intervention (8 weeks after randomisation); time points reported not specified Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors to ask whether the trial also included healthcare students, but received no response Study start/end date: date of first enrolment: 24 March 2017; end date not specified Funding source: primary sponsor: BARMER GEK (Hauptverwaltung, Produktentwicklung, Versorgungsmanagement, Prävention); European Union Declaration of interest: not specified Ethical approval needed/obtained for study: approved by Ethics Committee of Friedrich‐Alexander‐University Erlangen‐Nürnberg Comments by study authors: website, studicare.com; secondary trial registration: ISRCTN13856522 (Spanish partner study) Miscellaneous outcomes by the review authors: based on trial registration, recruiting; unclear if trial also includes healthcare students Correspondence: Dr Daniel Ebert, Nägelsbachstraße 25a, 91052 Erlangen, Germany; Daniel.Eber@fau.de; phone +49 9131 8567567 |
DRKS00013765.
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified in trial registration Imputation of missing data: not specified |
| Participants |
Country: Germany, Austria, Switzerland
Setting: online intervention
Age: not specified
Sample size (randomised): 260 targeted
Sex: not specified
Comorbidity (mean (SD) of respective measures in indicated, if available): not specified
Population description: resilient college students
Inclusion criteria: 1) student status; 2) internet access; 3) consent; 4) sex: both; 5) age: no minimum or maximum age limit
Exclusion criteria: 1) individuals with significant minor resilience (1 SD below average); 2) individuals who have been diagnosed with a mental disorder within the past 12 months; 3) individuals who are on a waiting list for a psychotherapy, are currently in treatment or have experienced psychotherapeutic treatment in the last 12 months; 4) current or lifelong psychotic or bipolar disorder; 5) individuals with high suicide risk Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: StudiCare: Resilienz UP (n randomised not specified)
Control: wait‐list control (n randomised not specified)
|
| Outcomes |
Outcomes collected and reported: Primary outcome:
Secondary outcomes:
Outcomes reported not specified Time points measured and reported: post‐intervention (8 weeks after randomisation); time points reported not specified Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors to ask whether the trial also included healthcare students, but received no response Study start/end date: date of first enrolment: 15 March 2018; end date not specified Funding source: primary sponsor: BARMER GEK (Hauptverwaltung, Produktentwicklung, Versorgungsmanagement, Prävention); European Union Declaration of interest: not specified Ethical approval needed/obtained for study: approved by Ethics Committee of Friedrich‐Alexander‐University Erlangen‐Nürnberg Comments by study authors: website, studicare.com Miscellaneous outcomes by the review authors: based on trial registration, recruiting; unclear if trial also includes healthcare students Correspondence: Dr Daniel Ebert, Nägelsbachstraße 25a, 91052 Erlangen, Germany; Daniel.Eber@fau.de; phone +49 9131 8567567 |
Enrique 2019.
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): Taking a conservative approach, they expect a small effect size for well‐being outcomes (d = 0.2), based on a meta‐analysis of RCTs on positive psychology interventions; taking an equally conservative approach, at the minimum they anticipate a similar effect size for resilience outcomes. Therefore, given a small expected effect size of 0.2 for resilience and well‐being outcomes and recent guidelines for estimating sample size for pilot RCTs designed with 90% power and 2‐sided 5% significance, based on a non‐central t‐distribution approach, a sample size of 75 was determined (25 per arm) Imputation of missing data: not specified, but all analyses will be based on the intention‐to‐treat principle according to study protocol |
| Participants | Country: Ireland Setting: internet‐delivered intervention Age: not specified in trial registration or study protocol Sample size (randomised): 75 Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified, but see exclusion criteria: students with psychotic or bipolar disorder, at risk of suicide and currently in psychological treatment excluded Population description: undergraduate and postgraduate college students Inclusion criteria: 1) above 18 years of age; 2) registered student at the university Exclusion criteria: 1) individuals with psychotic or bipolar disorder; 2) individuals at risk of suicide; 3) individuals currently in psychological treatment Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention 1: internet‐delivered intervention for resilience with human support (Space for Resilience; n planned = 25)
Intervention 2: internet‐delivered intervention for resilience with automated support (Space for Resilience; n planned = 25)
Control: wait‐list control (n planned = 25) |
| Outcomes |
Outcomes collected and reported: Primary outcome:
Secondary outcomes:
Other measures:
Outcomes reported not specified Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; time points reported not specified Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors for information about the inclusion of healthcare students, but received no response Study start/end date: see trial registration: October 2018 to May 2019 Funding source: funded by joint resources provided from SilverCloud Health and Student Counselling Service, Trinity College Dublin Declaration of interest: 4 authors are employees of SilverCloud Health, 2 of them are members of the e‐mental health research group, School of Psychology, Trinity College Dublin Ethical approval needed/obtained for study: approved by the research ethics committee at the School of Psychology, Trinity College Dublin (Approval ID: SPREC112018‐12; 27th November 2018) Comments by study authors: trial registration: ISRCTN11866034 Miscellaneous outcomes by the review authors: according to trial registration: no longer recruiting, overall trial status: completed, unpublished trial (last update in April 2019); inclusion of healthcare students unclear Correspondence: A. Enrique; E‐Mental Research group, School of Psychology, Trinity College Dublin, Ireland and Clinical Research & Innovation, SilverCloud Health, Dublin, Ireland; corresponding author: D. Richards; E‐Mental Research group, School of Psychology, Trinity College Dublin; Ireland; derek.richards@tcd.ie |
Flett 2020.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Games 2020.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Gerson 2013 (study 1).
| Methods | Study design: RCT, according to authors; but (systematic) non‐random approach: alternation Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): A power analysis using the G*Power 3 program indicated that power was low for a medium effect size with 28 participants (f2 = 0.32 for a multiple linear regression with 3 predictors and f = 0.25 for an analysis of covariance); preliminary study (findings should be interpreted cautiously given number of variables and very small sample size) Imputation of missing data: not specified; per‐protocol analysis (only participants who completed treatment in both groups) |
| Participants | Country: USA Setting: university, psychology lab Age: mean = 19.9 (SD = 2.17) years; range = 18 ‐ 26 years Sample size (randomised): 33 Sex: 20 women, 13 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: depression (BDI‐II)): IG: 7.88 (3.50), CG: 14.00 (7.94) Population description: undergraduates at a small, private university in southern California Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): attrition of 5 participants (IG: 1, CG: 4) Reasons for missing data: not specified |
| Interventions |
Intervention: Program for Accelerated Thriving and Health (PATH) (n = 16)
Control: wait‐list control (n = 17)
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 3‐week follow‐up (follow‐up only for IG; post‐intervention for CG which also receives intervention after waiting period) Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors for the means and SDs for the outcomes in both groups at each of the 3 time points and received the response that data for study 1 appeared to be corrupted (Gerson 2018b [pers comm]). We also asked for the potential inclusion of healthcare students in the sample, but received no response to this inquiry Study start/end date: not specified Funding source: supported in part by a Summer Undergraduate Research Fellowship provided by the Office for Undergraduate Research of California Lutheran University Declaration of interest: not specified Ethical approval needed/obtained for study: approved by the university’s IRB Comments by study authors: not relevant Miscellaneous outcomes by the review authors: for study 1, unclear if psychology students were included in the study Correspondence: Marylie W. Gerson; Department of Psychology, California Lutheran University, 60 W. Olsen Road, mail code 3800, Thousand Oaks, CA 91360, USA; mgerson@callutheran.edu |
Gerson 2013 (study 2).
| Methods |
Study design:RCT
Study grouping: parallel group
Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): Although power with a sample of 63 approached a moderate level for a multiple linear regression analysis with 3 predictors (f2 = .70), it was still low for an analysis of covariance (f = .50), so caution should be used in interpreting findings Imputation of missing data: not specified; form of per‐protocol analysis (only participants who took part in treatment in general; participants who only attended 1st session were also considered) |
| Participants | Country: USA Setting: university, psychology lab Age: mean = 21.58 (SD = 3.88); range = 17 ‐ 50 years Sample size (randomised): not exactly specified; 63 finally analysed; probably 73 randomised Sex: 52 women, 12 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: depressive symptoms at baseline not specified Population description: undergraduates Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): 9 dropouts (IG: 5, CG: 4); 1 exclusion (IG) Reasons for missing data: not specified |
| Interventions |
Intervention: Program for Accelerated Thriving and Health (PATH) (n = 36)
Control: attention control (equivalent in every way to IG except for content; n = 37)
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors for the number of participants randomised (N = 73?) in total and to each group as well as for the means and SDs for the outcomes in both groups at each time point (Gerson 2018a [pers comm]). In a second inquiry, we also asked if healthcare students were included in the sample and whether subgroup data could be provided, but received no response Study start/end date: not specified (held at start of new school year) Funding source: supported in part by a Summer Undergraduate Research Fellowship provided by the Office for Undergraduate Research of California Lutheran University Declaration of interest: not specified Ethical approval needed/obtained for study: approved by the university’s IRB Comments by study authors: not relevant Report ID (e.g. duplicate publications, follow‐up studies): not relevant Miscellaneous outcomes by the review authors: means, SDs and sample sizes for both groups at pre‐ and posttest for resilience and depression provided by authors; unclear if psychology students were included in the study Correspondence: Marylie W. Gerson; Department of Psychology, California Lutheran University, 60 W. Olsen Road, mail code 3800, Thousand Oaks, CA 91360, USA; mgerson@callutheran.edu |
Harrer 2018.
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): The sample size allowed the detection of effect sizes of d = 0.41 with a power (1− β) of 0.80 with α of.05 and was based on a meta‐analysis on internet‐based interventions for college students, which reported an SMD of 0.73 for stress but lower effects for depression outcomes (SMD = 0.43). A sample size of 150 was therefore chosen to detect significant changes for secondary outcomes in this study such as depression Imputation of missing data: Analyses based on the intention‐to‐treat (ITT) principle were conducted, with missing data imputed using a Markov chain Monte Carlo multivariate imputation algorithm with 100 estimations per missing and all variables set as predictors for imputation. Imputed datasets were then aggregated to obtain 1 imputed dataset; completer analysis + ITT analysis |
| Participants |
Country: Germany
Setting: internet‐ and app‐based intervention
Age: mean = 24.1 (SD = 4.1) years
Sample size (randomised): 150
Sex: 112 women, 38 men
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: depression (CES‐D; 0 ‐ 45) : IG: 24.31 (9.06), CG: 23.97 (8.63); anxiety (Spielberger STAI; 6 ‐ 24): IG: 16.05 (3.37), CG: 15.77 (4.22); emotional exhaustion (MBI; 5 ‐ 30): IG: 21.63 (4.49), CG: 22.27 (4.31); 106 participants (76.8%) indicated that they were first‐time help‐seekers; 77.3% (IG: 58/75; CG: 58/75) showed clinically relevant depressive symptoms at baseline
Population description: college students at German‐speaking universities with elevated levels of stress (PSS‐4 ≥ 8)
Inclusion criteria: 1) elevated levels of perceived stress (PSS‐4 ≥ 8; representing a level of stress one SD = 2.92 above the mean of 4.49 in a large student sample); 2) enrolment in a German‐speaking university at the beginning of the training; 3) age ≥ 18 years; 4) internet access; 5) willingness to provide self‐report data at all assessment points; 6) informed consent
Exclusion criteria: 1) self‐reported diagnosis of dissociative symptoms or psychosis in the past; 2) considerable risk for suicide (BDI item 9 > 1; “I feel I would be better off dead” or “I would kill myself if I had the chance”) Attrition (withdrawals and exclusions): post‐intervention: 11 lost to assessment (all in IG, 14.7%); all participants in CG (n = 75) provided data; follow‐up: 45 lost to assessment (IG: 35/46.7%, CG: 10/13.3%) Reasons for missing data: not specified for 56 lost to assessment/follow‐up at different assessments |
| Interventions |
Intervention: TAU + StudiCare Stress (n = 75)
Control: TAU + wait‐list control (n = 75)
|
| Outcomes |
Outcomes collected and reported: Primary outcome:
Secondary outcomes: Mental health:
Risk and protective factors:
College‐related outcomes:
Additional measures:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention; 3) 5‐week follow‐up (at 3 months after randomisation; i.e. 5 weeks after end of 7‐week intervention); treatment credibility and expectancies only measured at pre‐intervention Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors for information on whether the intervention focused on fostering resilience and if healthcare students were included in the sample, but received no response Study start/end date: 9 May 2016 (start of recruitment) ‐ 30 January 2017 (follow‐ups completed) Funding source: partly funded by BARMER (major healthcare insurance company in Germany) Declaration of interest: Daniel David Ebert (DDE) reports to have received consultancy fees or served in the scientific advisory board from several companies such as Minddistrict, Lantern, Schön Kliniken, and German health insurance companies (BARMER, Techniker Krankenkasse). DDE and Mathias Harrer are also stakeholders of the Institute for health trainings online (GET.ON), which aims to implement scientific findings related to digital health interventions into routine care. Harald Baumeister reports to have received consultancy fees and fees for lectures or workshops from chambers of psychotherapists and training institutes for psychotherapists. In the past 3 years, Ronald C Kessler (RCK) received support for his epidemiological studies from Sanofi Aventis, was a consultant for Johnson & Johnson Wellness and Prevention, Sage Pharmaceuticals, Shire, Takeda, and served on an advisory board for the Johnson & Johnson Services Inc, and Lake Nona Life Project. RCK is a co‐owner of DataStat, Inc, a market research firm that carries out health care research. Ethical approval needed/obtained for study: approved by the University of Erlangen‐Nuremberg ethics committee (Erlangen, Germany; 322_15 B) Comments by study authors: study carried out as part of the WHO World Mental Health International College Student project; trial registration number: German Clinical Trial Register DRKS00010212; website, studicare.com Miscellaneous outcomes by the review authors: According to the feedback from the authors in another trial (DRKS00011800) using an intervention (StudiCare Fernstudierende) that is adapted from the intervention investigated here (StudiCare Stress), the intervention also aims to foster health‐promoting factors (secondary outcomes), such as resilience and the reduction of perceived stress; but unclear if healthcare students were included in the final sample Correspondence: Mathias Harrer, BSc; Clinical Psychology and Psychotherapy; Friedrich‐Alexander‐University Erlangen‐Nuremberg, Nägelsbachstraße 25a, Erlangen, 91052, Germany; mathias.harrer@fau.de; Phone: 49 1708237654 |
Heath 2020.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Herrero 2019.
| Methods | Study design: RCT Study grouping: parallel Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): So far, there are no data about the effect sizes that can be obtained in Internet‐based interventions for the prevention of depression or other common mental health disorders mainly focusing on promoting resilience. However, previous studies on online interventions have shown effect sizes of between 0.36 and 0.50 for the reduction of symptoms of depression and between 0.32 and 0.42 for the reduction of symptoms of anxiety. At least similar effects on improving resilience are expected. Adopting a conservative approach, the sample size is based on the smallest effect size detected in previous studies (Cohen's d = 0.32), a significance level of 0.05, a power of 0.80, and a dropout rate of 30%, on the primary outcome measure (CD‐RISC). The planned sample size of 464 participants is sufficient to detect a small effect size (Cohen's d = 0.32). Covariate adjustment for relevant baseline prognostic factors will further increase the power. To ensure recruitment feasibility, 5 universities (with an estimated number of 170,000 students) will take part in the trial Imputation of missing data: according to study protocol, intention‐to‐treat and per‐protocol analysis; to assess the effect of missing data on the primary analysis the primary outcome will be reanalysed after a multiple imputation strategy (developed within blinded data review) was applied to the data; ITT sample comprises all randomised participants who provided the primary outcome measure within the initially assigned study arm |
| Participants | Country: Spain, Germany, Switzerland Setting: internet‐based programme Age: not specified in study protocol and conference abstract Sample size (randomised): 464 (planned) Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: university students with low levels of resilience Inclusion criteria: 1) university students with a score of 1 SD below the mean of the sample on the CD‐ RISC‐25; 2) adequate knowledge to understand and read Spanish or German; 3) access to the internet, and the ability to use a computer Exclusion criteria: 1) university students with a history of a common mental health disorder in the past 12 months; 2) university students who are on a waiting list for psychotherapy or are currently or have been in psychotherapeutic treatment within the past 12 months; 3) individuals with a current psychotic or bipolar disorder or a history of one; 4) individuals at risk for suicide Attrition (withdrawals and exclusions): not specified in study protocol and conference abstract Reasons for missing data: not specified in study protocol and conference abstract |
| Interventions |
Intervention: unguided internet‐based intervention CORE (Cultivating our Resilience; also named as ICare‐R in conference abstract Botella 2016 (n = 232 planned)
Control: TAU (n = 232 planned)
|
| Outcomes |
Outcomes collected and reported: Primary outcome:
Secondary outcomes:
Other measures:
Outcomes reported not specified Time points measured and reported: 1) pre‐intervention; 2) during intervention (4 weeks); 3) post‐intervention (8 weeks); 4) 4‐month follow‐up (at 6 months/24 weeks, i.e. 6 weeks after 8‐week intervention); 5) 10‐month follow‐up (at 12 months/48 weeks, i.e. 40 weeks after 8‐week intervention); resilience at screening, pre‐intervention, post‐intervention and follow‐ups; depression, anxiety, PANAS and perceived stress at all time points but screening; personality and CEQ only at pre‐intervention; self‐esteem, alcohol at pre‐, mid‐, and post‐intervention; well‐being, self‐compassion, CSRI, EOS at pre‐ and post‐intervention and follow‐ups; therapeutic alliance at mid‐ and post‐intervention; treatment satisfaction only at post‐intervention; time points reported not specified Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors for the study status and received the response that data could not yet be accessed until the recruitment was finished (Herrero 2018 [pers comm]). Study start/end date: see trial registration: September 2015 ‐ July 2019 Funding source: Tfunding from the European Union's Horizon 2020 Research and Innovation Programme under grant agreement No 634757 Declaration of interest: no competing interests declared Ethical approval needed/obtained for study: approved by local ethical commissions in each country Comments by study authors: trial registration number ISRCTN13856522; study is part of the European research project: Integrating Technology into Mental Health Care Delivery in Europe (ICare, No 634757; http://www.icare‐ online.eu) Miscellaneous outcomes by the review authors: see trial registration: recruitment status: no longer recruiting, overall trial status, completed (last update: March 2020); information received from authors: at the end of project, analysis is currently started, first publication expected to be ready by the end of 2019; unclear if final sample included healthcare students Correspondence: Cristina Botella; Universitat Jaume I, Av. Vicent Sos Banyat s/n, Castellón 12071, Spain; botella@uji.es |
ISRCTN17156687.
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified in trial registration Imputation of missing data: not specified |
| Participants | Country: Finland Setting: smartphone‐delivered intervention Age: range = 18 ‐ 40 years (see inclusion criteria) Sample size (randomised): 120 targeted Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: Finnish university students with diagnosed depression Method of recruitment: recruited through the Finnish Student Health Service’s centres in 4 Finnish cities; Tampere, Turku, Jyväskylä and Helsinki; patients with depression from Finnish Student Health Service (YTHS) Inclusion criteria: 1) diagnosis of a depressive disorder (ICD‐10 (International Classification of Diseases‐10): diagnoses F32 or F33) at the time of enrolment; 2) willingness to commit to the 8‐week online therapy programme; 3) no prior established mindfulness practice/meditation experience; 4) aged 18 ‐ 40 years; 5) living in Finland; 6) has a smartphone with iOS or Android mobile operating system; 7) access to mobile internet Exclusion criteria: 1) previous suicide attempts; 2) severe suicidal ideation; 3) other serious mental disorders such as psychosis or severe personality disorders; 4) active substance abuse; 5) ongoing psychotherapy Attrition (withdrawals and exclusions): not specified in trial registration Reasons for missing data: not specified in trial registration |
| Interventions |
Intervention: TAU (regular treatment for depression) + Ascend therapy programme (n = 60 planned)
Control: TAU (n = 60 planned)
|
| Outcomes |
Outcomes collected and reported: Primary outcome:
Secondary outcomes:
Outcomes reported not specified Time points measured and reported: 1) pre‐intervention; 2) 2 weeks; 3) 4 weeks 4) 6 weeks; 5) 8 weeks; 6) 3 months; 7) 6 months post‐intervention; user‐friendliness of mobile phone application only measured at 8 weeks; time points reported not specified Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors to ask if the trial also included healthcare students, but received no response Study start/end date: 1 April 2018 ‐ 31 December 2019 Funding source: Meru Health Inc.; Lifeline Ventures Inc. Declaration of interest: not specified Ethical approval needed/obtained for study: Ethics Committee of the Tampere University Central Hospital Comments by study authors: not relevant Miscellaneous outcomes by the review authors: recruitment status: not longer recruiting; overall trial status: completed (last updated: September 2019); unclear if healthcare students included in final sample Correspondence: Dr Anu Raevuori; Meru Health; Lapinlahdenkatu 16, Helsinki 00180, Finland |
Jackson 2019.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Kanekar 2010.
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): A sample size of 25 students in each group was reached considering an alpha of 0.05, power of 0.70 and estimated effect size of 0.70; study accounted for attrition of 5 participants and hence the sample size was increased to 30 per group; some of the limitations of the study: small sample size (considerable dropout of 21) Imputation of missing data: no imputation of missing data reported; unclear how many participants dropped out of the intervention and how many did not complete the questionnaires; probably available‐case analysis (only participants for whom outcomes were obtained) and per‐protocol analysis (only participants who completed allocated intervention) |
| Participants | Country: USA Setting: large research‐1 university in Ohio Age: mean = 24.67 (SD = 2.68); range = 21 ‐ 33 years Sample size (randomised): 60 Sex: 5 women, 34 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: No‐one in the study population ever had mental illness and the group was mentally healthy Population description: international students of Asian Indian origin enrolled full‐time at large Research‐I university in Ohio Inclusion criteria: 1) student had to be an Indian citizen by birth; 2) student must have lived for at least 15 years in India immediately prior to entering the USA Exclusion criteria: not specified Attrition (withdrawals and exclusions): high dropout rate (n = 21 dropouts) Reasons for missing data: not specified; reasons can be conjectured to be time commitment to the study, participant interest in the study, length of survey instrument |
| Interventions |
Intervention: internet‐based intervention to enhance social support, hardiness, and acculturation (n = 30)
Control: attention control (general health awareness and wellness intervention; n = 30)
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors about the inclusion of healthcare students in the sample. We received the response from the authors that "health‐related international students were not specifically targeted by the study and there could have been some health professionals in the sample; the sample was composed of international students from diverse departments across the university campus" (Kanekar 2019 [pers comm]). Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: IRB approval at the University of Ohio (June 2007) Comments by study authors: not relevant Miscellaneous outcomes by the review authors: according to authors, there could have been some health professionals in the final sample, but unclear how many and which participants Correspondence: Prof. Manoj Sharma, PhD; Health Promotion and Education, University of Cincinnati, P.O. Box 210068 Cincinnati, OH 45221‐0068; manoj.sharma@uc.edu; manoj.sharma@jsums.edu |
Kon 2019.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Liu 2016.
| Methods | Study design: randomisation unclear based on full text Study grouping: not specified Unit of randomisation: not specified Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
| Participants | Country: not specified Setting: training setting not specified Age: not specified Sample size (randomised): not specified Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: college students (who want to improve the mental ability, interpersonal skill, with good mental state instead of obvious psychological disorder) Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: positive group psychology counselling (n randomised not specified)
Control: no intervention (n randomised not specified) |
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
| Notes |
Contact with authors: We were not able to contact the authors to ask for the study design (randomisation) and the potential inclusion of healthcare students, since we had no contact data (e‐mail address) of the authors Study start/end date: not specified Funding source: Funds Project: 2015 Heilongjiang Province Philosophy and Social Science Planning Project Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by study authors: Lian Liu, female, the Han nationality, master, research direction: Psychological health education Miscellaneous outcomes by the review authors: several eligibility criteria of this review unclear for this study (randomisation; inclusion of healthcare students) Correspondence: Lian Liu; Heihe University; Heihe, China |
Liu 2019.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
NCT02867657.
| Methods | Study design: RCT Study grouping: parallel Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified in trial registration Imputation of missing data: not specified |
| Participants |
Country: Denmark
Setting: training setting not specified
Age: not specified
Sample size (randomised): 72 (estimated enrolment)
Sex: not specified
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified
Population description: bachelor students at Danish Universities and University Colleges
Inclusion criteria: 1) age 18 years and older (adult, older adult); 2) bachelor student at a Danish Universities or University Colleges; 3) a score of 16 or above on the PSS Exclusion criteria: 1) smoking; 2) psychiatric diagnosis (depression, anxiety, adjustment disorder, post‐traumatic stress disorder, personality disorder, psychosis); 3) untreated ADHD, autism, abuse and risk of suicide Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: mindfulness in nature (n randomised not specified)
Control 1: attention control: mindfulness indoor (n randomised not specified)
Control 2: wait‐list control (n randomised not specified)
|
| Outcomes |
Outcomes collected and reported: Primary outcomes:
Secondary outcomes:
Outcomes reported not specified Time points measured and reported: 1) post‐intervention (at end of 5‐day retreat); time points reported not specified Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors for the trial status and the potential inclusion of healthcare students, but received no response Study start/end date: June 2016 ‐ November 2018 (estimated completion date according to trial registration) Funding source: VIA University College Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by study authors: not relevant Miscellaneous outcomes by the review authors: unclear if healthcare students were included; trial status unclear Correspondence: Jesper Dahlgaard, PhD; VIA University College, Aarhus, Denmark, DK‐8200; jesd@via.dk; phone: +45 8755 2992 |
NCT03669016.
| Methods | Study design: RCT Study grouping: parallel Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
| Participants |
Country: Finland
Setting: face‐to‐face training: training setting not specified; internet‐based training: online
Age: not specified
Sample size (randomised): 120 (estimated enrolment)
Sex: not specified
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified
Population description: undergraduate students of Faculty of Medicine
Inclusion criteria: 1) all undergraduate students of Faculty of Medicine, University of Helsinki who have started their studies in year 2009 or later
Exclusion criteria: 1) students who can not participate fully in the intervention (self‐evaluated); 2) students who have severe mental problems (like anxiety or depression) when the study starts; 3) students who have had a great loss or trauma in near past, or some other mental or physical health problem that could make participation difficult. This is evaluated based on how the students answer the following measures in the baseline questionnaire: answers to the CORE‐OM questionnaire, answers to the questions where students evaluate themselves for anxiety, depression, mental health. If students say they have some other mental disorder, they are not accepted into the study Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention 1: Face‐to‐face group‐based mindfulness (n randomised not specified)
Intervention 2: Internet‐based mindfulness training (n randomised not specified)
Control: no intervention (n randomised not specified)
|
| Outcomes |
Outcomes collected and reported: Primary outcome:
Secondary outcomes:
Outcomes reported not specified Time points measured and reported: 1) pre‐intervention (3 weeks before the intervention starts); 2) post‐intervention; 3) 4 months follow‐up; for students’ possibilities to influence their own studies, participants’ own evaluation of their mental health, previous experiences in practising mindfulness and/or meditation: only pre‐intervention; for amount and quality of independent mindfulness practice: only post‐intervention and 4 months follow‐up; time points reported not specified Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors to ask whether the primary focus of the intervention was on fostering resilience or if resilience was only measured as a secondary outcome, but received no response from the authors Study start/end date: August 2018 ‐ April 2019 Funding source: sponsor: University of Helsinki Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by study authors: not relevant Miscellaneous outcomes by the review authors: recruitment status according to trial registration: recruiting (last updated in September 2018); unclear if fostering resilience was primary focus; resilience is only mentioned once under secondary outcomes Correspondence: principal investigator: Saara Repo, PhD; University of Helsinki, Finland; saara.repo@helsinki.fi; phone: +358405189456 |
NCT03903978.
| Methods | Study design: RCT Study grouping: parallel Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified in trial registration Imputation of missing data: not specified |
| Participants |
Country: Spain, Argentina and Mexico
Setting: web‐based intervention
Age: not specified
Sample size (randomised): 324 (estimated enrolment)
Sex: not specified
Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified
Population description: Spanish‐speaking university students
Inclusion criteria: 1) age: 18 ‐ 60 years; 2) university students with a SD score below the sample mean on the CD‐RISC‐25; 3) adequate knowledge to understand and read Spanish and/or be Spanish‐speaking; 4) internet access and computer skills Exclusion criteria: 1) university students who are on a waiting list for psychotherapy or who are or have been undergoing psychotherapy in the last 12 months; 2) individuals with a current or past psychotic or bipolar disorder; 3) individuals at risk of suicide Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: Unguided web‐based resilience intervention (CORE; n = 108 planned)
Control 1: active control; Healthy lifestyle psycho‐educational programme; HLP; n = 108 planned)
Control 2: wait‐list control (n = 108 planned)
|
| Outcomes |
Outcomes collected and reported: Primary outcome:
Secondary outcomes:
Other outcomes:
Outcomes reported not specified Time points measured: 1) pre‐intervention; 2) post‐intervention; 3) 6‐month follow‐up; 4) 12‐month follow‐up; time points reported not specified Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors to ask if the trial also included healthcare students, but only received the response from the authors that they were starting the analysis for the project (Herrero 2019 [pers comm]). Study start/end date: November 2018 ‐ November 2020 (estimated study completion data) Funding source: Universitat Jaume I Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by study authors: not relevant Miscellaneous outcomes by the review authors: unclear if healthcare students were also included in the trial; trial status according to trial registration: enrolling by invitation; last updated in April 2019 Correspondence: study director: Cristina Botella, PhD; University Jaume I, Castellon, Spain |
NCT04064372.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
NCT04416074.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Noormohamadi 2019.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Oman 2008.
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): To obtain greater statistical power, the trialists focus on comparing the effects of receiving either 1 of the intervention groups against outcomes from a control group; relatively small sample size and correspondingly reduced statistical power for assessing precise changes over time, or differences in treatment effect that may be associated with covariates Imputation of missing data: OMAN 2008: not specified; intention‐to‐treat analysis according to authors, with 44 participants (i.e. including 1 participant who did not participate in assessment at post‐test); but per‐protocol analysis (without 3 who dropped out before intervention or after Session 1); SHAPIRO 2011: LOCF for missing data on several variables at post‐intervention (for 1) and 12‐month follow‐up (for 3); but also per‐protocol analysis (without 2 dropouts in MBSR before intervention) |
| Participants | Country: USA Setting: undergraduates recruited from catholic university; setting of training not specified Age: range = 18 ‐ 24 years Sample size (randomised): 47 Sex: 35 women, 9 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: undergraduate students at a small private university in California (e.g. recruitment in psychology department classrooms) Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): 3 dropouts after randomisation/before intervention (MBSR: 2) or after Session 1 (EPP: 1); post‐intervention: 1 lost to follow‐up/did not complete assessment; Shapiro 2011: 12‐month follow‐up: 3 (MBSR: 1, CG: 2) with missing data on several variables Reasons for missing data: for 3 dropouts after randomisation/before intervention or after Session 1: death of a parent (n = 1 in EPP), had overextended himself (n = 1 in MBSR), no reason reported (n = 1 in MBSR); reasons for participants lost to follow‐up/with missing data in assessments (see also Shapiro 2011) not specified |
| Interventions |
Intervention 1: Meditation Management of Stress – MBSR; n = 16; exchange between 2 intervention groups after randomisation due to scheduling conflicts: MBSR: n = 17)
Intervention 2: Meditation Management of Stress – Easwaran’s Eight‐Point Program (EPP; n = 16; exchange between MBSR and EPP after randomisation due to scheduling conflicts: EPP: n = 15)
2 intervention groups were combined in statistical analysis Control: wait‐list control (n = 15)
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (after 8‐week interventions); 3) 2‐month follow‐up (2 months post‐intervention); 4) 12‐month follow‐up (12 months post‐intervention) (only in Shapiro 2011) Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors to ask for the means and SDs for the treatment group (MBSR and EPP combined) for each outcome at each time point and whether the 12‐month follow‐up had been conducted for the combined IG and not only for MBSR (as reported in Shapiro 2011). We also asked whether healthcare students were included in the final sample, but received no response to our inquiries Study start/end date: recruitment in fall 2004; exact study dates not specified Funding source: Metanexus Institute (grant: “Learning from Spiritual Examples: Measures & Intervention”), John Templeton Foundation, Academic Council of Learned Societies, Contemplative Mind in Society, Fetzer Institute, Santa Clara University Internal Grants for Research, and the Spirituality and Health Institute, Santa Clara University Declaration of interest: not specified Ethical approval needed/obtained for study: approval from the IRBs of the overall administering organisation and the university Comments by study authors: not relevant Miscellaneous outcomes by the review authors: Shapiro 2011 reported part of data of study described in Oman 2008; follow‐up study with 12‐month follow‐up; interventions MBSR and EEP analysed in combined manner in Oman 2008; unclear if psychology students were included in the study Correspondence: Dr Doug Oman, School of Public Health, University of California, 50 University Hall #7360, University of California, Berkeley, CA 94720‐7360, USA; DougOman@post.Harvard.edu; Shauna L. Shapiro, Department of Counseling Psychology, Santa Clara University, , El Camino Real, Santa Clara University, Santa Clara, CA 95053; slshapiro@scu.edu |
Palma‐Gómez 2020.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Roghanchi 2013.
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): small sample size (n = 24) as main limitation; achieved power not specified Imputation of missing data: not specified |
| Participants | Country: Iran Setting: university Age: mean = 21.53 (SD = 1.86); range = 19 ‐ 24 years Sample size (randomised): 24 Sex: 16 women, 8 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: first year undergraduate students admitted into the counselling centre at Razi University, Iran Method of recruitment: not specified Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: Rational emotive behaviour therapy (REBT) and art therapy (engraving on copper) (n = 12)
Control: wait‐list control (n = 12)
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) post‐intervention Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors for the SDs for both outcomes at both time points and if there had been any missing data. We also asked if healthcare students had been included in the final sample, but received no response Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by study authors: not relevant Miscellaneous outcomes by the review authors: unclear if healthcare students were included in the study Correspondence: Mahmoud Roghanchi, PhD; School of Social Science, Razi University, Kermanshah, Iran and School of Educational Studies, Universiti Sains Malaysia, 11800 USM, Penang, Malaysia; mahmoudroghanchi@yahoo.com |
Seligman 2007.
| Methods | Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: not specified; available‐case analysis (only participants for whom outcomes were obtained) |
| Participants | Country: USA Setting: recruited from college; training setting in part probably University of Pennsylvania for classroom‐based workshops, also web‐based materials and e‐mail coaching Age: not specified Sample size (randomised): 240 Sex: 156 women, 84 men Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: depression (BDI): IG: 9.8 (5), CG: 10.4 (5.7); all participants with BDI score 9 ‐ 24 (mild to moderate depressive symptoms); anxiety (BAI): IG: 10 (5.7), CG: 11.8 (7.6) Population description: first‐year undergraduates at the University of Pennsylvania Inclusion criteria: 1) at risk for depression by virtue of scoring between 9 and 24 on the BDI, which are considered mild to moderate levels of depressive symptoms; 2) read and sign the voluntary consent form Exclusion criteria: BDI score above 24 (as these individuals were more likely to be in a current major depressive episode, and the purpose of the study was to prevent depression, not to treat current depression; 1.5% above 24) Attrition (withdrawals and exclusions): 13 lost to follow‐up: pre‐intervention (IG: 11, CG: 2); post‐intervention: no further loss to follow‐up; 6 further losses at 1‐ follow‐up (IG: 4, CG: 2); 9 further losses at 2‐ follow‐up (IG: 6, CG: 3); over total study course: 28 lost to follow‐up (IG: 21: CG: 7); attrition rate often exceeds 5.4% Reasons for missing data: too busy; studying abroad for 1 or 2 semesters |
| Interventions |
Intervention: cognitive‐behavioral workshop along with web‐based materials and e‐mail coaching (n = 113)
Control: no intervention (n = 127)
|
| Outcomes |
Outcomes collected and reported:
Time points measured and reported: 1) pre‐intervention; 2) 2. assessment (end of fall semester in which 8‐week workshop took place); 3) 1. follow‐up (early in spring semester after intervention took place in fall semester); 4) 2. follow‐up (late in spring semester after intervention took place in fall semester) Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors for how many weeks/months after the end of the intervention the 2. assessment and the 1. follow‐up took place (Schulman 2018 [pers comm]). We also asked whether healthcare students were included in the study, but received no response to this inquiry Study start/end date: mid‐ to late‐September (year not indicated) to end of spring semester (second follow‐up assessment); but planned to track participants 3 years Funding source: supported by grant MH63430 from the National Institute of Mental Health and by grant MH52270 from the National Institute of Mental Health Declaration of interest: The Penn Resilience Training for College Students is owned by the University of Pennsylvania. The University of Pennsylvania has licensed this program to Adaptiv Learning Systems. Dr Martin Seligman owns stock in Adaptiv and could profit from the sale of this program. The other researchers who collaborated on this project do not have a financial relationship with Adaptiv Ethical approval needed/obtained for study: not specified Comments by study authors: workshop manual developer and trainer of workshop leaders: Dr Karen Reivich; study is replication study of Seligman 1999 Miscellaneous outcomes by the review authors: unclear if healthcare students were included in the study Correspondence: Martin EP Seligman; University of Pennsylvania; 3720 Walnut Street, Solomon Labs, Philadelphia, PA 19104, USA; seligman@psych.upenn.edu |
Tollefson 2018.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Xu 2019.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Result from top‐up search in June 2020; will be incorporated into the review at the next update |
Ye 2016.
| Methods | Study design: not specified in title (full text not available) Study grouping: not specified Unit of randomisation: not specified Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
| Participants | Country: not specified Setting: not specified Age: not specified Sample size (randomised): not specified Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: undergraduate nursing interns Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: emotional resilience training (n not specified)
Control: not specified if there was a potential control group |
| Outcomes | Outcomes collected and reported: not specified Time points measured and reported: not specified Adverse events: not specified |
| Notes |
Contact with authors: We were not able to contact the study authors on whether the study was a RCT comparing the emotional resilience training with a comparator, since we had no contact details for the authors Study start/end date: not specified Funding source: not specified Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by study authors: not relevant Miscellaneous outcomes by the review authors: neither abstract nor full text available for this study; based on title, the study design is unclear for this study Correspondence: no contact data found |
Zhang 2018.
| Methods | Study design: unclear based on conference abstract; cluster random‐sampling method to select students that are divided into high‐resilience and low‐resilience groups using college students' Resilience Scale (HARA); based on conference abstract, unclear if RCT and if wisdom education was compared to control Study grouping: not specified Unit of randomisation: not specified Power (power & sample size calculation, level of power achieved): not specified Imputation of missing data: not specified |
| Participants | Country: not specified Setting: not specified Age: not specified Sample size (randomised): 200 selected; 20 in low‐resilience and high‐resilience groups, respectively Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: male and female college students Inclusion criteria: not specified Exclusion criteria: not specified Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: wisdom education (n not specified; unclear if RCT)
Control: not specified in conference abstract if there was a control group |
| Outcomes | Outcomes collected and reported: outcomes collected not further specified (adjustment of short‐term and long‐term psychological changes in frustration situation); probably resilience (college students' Resilience Scale, HARA); outcomes reported: positive regulation of wisdom education on adjustment of short‐term psychological changes; adjustment of college students' long‐term psychological changes exists in both positive and negative aspects of regulation Time points measured and reported: not specified Adverse events: not specified |
| Notes |
Contact with authors: We contacted the authors to ask whether the study fulfilled several of our eligibility criteria, but received no response to 2 inquiries Study start/end date: not specified Funding source: supported by project of Guizhou Normal University ‐ Construction and Application of Internet + Wisdom Campus Based on Big Data (No. 11904/0517041) Declaration of interest: not specified Ethical approval needed/obtained for study: not specified Comments by study authors: not relevant Miscellaneous outcomes by the review authors: several eligibility criteria of this review unclear for this study (RCT, inclusion of healthcare students) Correspondence: Hao Zhang; School of Education Science, Guizhou Normal University, Guiyang, 550001, China and Education Policy and Law Research Center, Guizhou, Normal University, Guiyang, 550001, China; 13885167180@163.com |
α = alpha, significance level; ACT: Acceptance and Commitment Therapy; ASI: Anxiety Sensitivity Inventory; ASQ: Attributional Style Questionnaire; AUDIT: Alcohol Use Disorders Identification Test; β: statistical power; BAI: Beck Anxiety Inventory; BDI: Beck Depression Inventory; BRS: Brief Resilience Scale; CBM: cognitive bias modification; CBM‐I: cognitive bias modification‐interpretation; CBT: cognitive behavioural therapy; CD‐RISC: Connor‐Davidson Resilience Scale; CEQ: Credibility and Expectancy Questionnaire; CES‐D: Center for Epidemiology Studies Depression Scale; CG: control group; CORE: Cultivating Our Resilience; d: delta (Cohen's d, effect size); ECG: electrocardiograph; EOS: Enjoyment Orientation Scale; EPP: Easwaran’s Eight‐Point Program; f or f2: Cohen's f or f2 (effect size); FFMQ: Five‐Facet Mindfulness Questionnaire; FMI: Freiburg Mindfulness Index; GAD‐7: Generalised Anxiety Disorder Scale; IG: intervention group; IRB: Institutional Review Board; ISEL: Interpersonal Support Evaluation List; ISI: Insomnia Severity Index; ITT: intention‐to‐treat analysis; LOCF: last observation carried forward; MBI: Maslach Burnout Inventory; MBRS: mindfulness‐based stress reduction; n: sample size (e.g. in respective group); PANAS: Positive and Negative Affect Schedule; PATH: Program for Accelerated Thriving and Health; PCQ: Psychological Capital Questionnaire; PDSS: Panic Disorder Severity Scale; PHQ‐9: Patient Health Questionnaire; PSS: Perceived Stress Scale; PsyCap: psychological capital; PWB: psychological well‐being; RCT: randomised controlled trial; REBT: rational emotive behaviour therapy; RRT: recognition ratings task; RS: Resilience Scale; RSES: Rosenberg Self‐Esteem Scale; SCS: Self‐Compassion Scale; SD: standard deviation; SMD: standardised mean difference; SMS: short message service; STAI: State‐Trait Anxiety Inventory; SUDS: Subjective Unit of Distress Scale; SWLS: Satisfaction with Life Scale; t: t value; TAU: treatment as usual; TSST: Tier Social Stress Test; WEMWS: Warwick‐Edinburgh Mental Well‐being Scale
Characteristics of ongoing studies [ordered by study ID]
Harrer 2019.
| Study name |
Public title: Online‐based self‐help stress management program for distance‐learning students with feedback on demand Scientific title: Online‐based self‐help stress management program for distance‐learning students with feedback on demand ‐ StudiCare |
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): The trialists aim to include 200 participants, allowing for a between‐trial arm group comparison against a statistically relevant effect size threshold of d = 0.40, a power (1 − β) of 80%, and an α of 0.05 (2‐tailed) for the intention‐to‐treat (ITT) analysis. A recent meta‐analytic review for internet‐based stress interventions reported effect sizes of d = 0.64 for perceived stress in guided interventions but considerably smaller effect sizes for unguided programmes (d = 0.34 for depression, d = 0.32 for anxiety). Results for internet‐based interventions addressing psychological distress in tertiary education are mixed, ranging from non‐significant findings to moderate‐sized effects in favour of the respective intervention. Thus, the trialists are aiming for an effect size of d = 0.40. Imputation of missing data: Analyses based on the ITT principle will be conducted, with missing data imputed using a Markov chain Monte Carlo multivariate imputation algorithm with 100 estimations per missing; complete‐case analysis and ITT analysis planned |
| Participants |
Country: Germany, Austria, Switzerland (recruitment) Setting: internet‐based intervention Age: not specified in trial registration or study protocol Sample size (randomised): 200 targeted Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: students of a large German distance university with elevated levels of depression (CES‐D score ≥ 16) Inclusion criteria: (see trial registration and study protocol; Harrer 2019): 1) distinct level of perceived study‐related stress: experience elevated levels of depression measured by a score ≥ 16 on the German version of the CES‐D 20‐item version (Allgemeine Depressionsskala (ADS), indicating subthreshold to full‐blown symptoms of depression during the last 2 weeks); 2) enrolled in a bachelor’s or master’s degree programme at a large German distance‐learning tertiary education facility (FernUniversität in Hagen) by the beginning of the intervention; 3) motivation to participate in an online intervention targeting stress reduction; 4) are at least 18 years old; 5) have internet access; 6) willingness to provide a valid e‐mail address and telephone number to the study team; 7) declare willingness to provide self‐report data at all 3 assessment points (online surveys of 45 minutes duration each); 8) give informed consent Exclusion criteria: (see trial registration and study protocol; Harrer 2019): 1) CES‐D score < 16; 2) self‐reported dissociative symptoms or psychosis, currently or in the past; 3) considerable risk for suicide as indicated by a score > 1 on item 9 of the German version of the BDI‐II; “I feel I would be better off dead” or “I would kill myself if I had the chance”; 4) currently undergoing treatment; 5) not enrolled at distance‐learning university; 6) no internet; 7) not willing to sign informed consent Attrition (withdrawals and exclusions): not specified in trial registration or study protocol Reasons for missing data: not specified in trial registration or study protocol |
| Interventions |
Intervention: TAU + StudiCare Fernstudierende (n = 100 planned)
Control: TAU + attention control (n = 100 planned)
For more details, see also study protocol |
| Outcomes |
Outcomes collected and reported: Primary outcome:
Secondary outcomes: Mental health:
Academic outcomes:
Risk and protective factors:
Health literacy and help‐seeking intentions:
Health economic measures:
Additional measures:
According to trial registration also assessed:
Further variables (e.g. suicidal ideation, self‐reported history of psychosis/dissociative symptoms, help‐seeking intentions, internet therapy experience, e‐health literary, reasons for participation, intervention credibility and expectations, sociodemographic characteristics, personality traits) only assessed at baseline (see study protocol, Harrer 2019) Outcomes reported not specified Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (i.e. 7 weeks after randomisation); 3) 5‐week follow‐up (i.e. 3 months after randomisation); time points reported not specified Adverse events: not specified |
| Starting date | Study start/end date: June 2017 (date of first enrolment); end date not specified |
| Contact information |
Principal investigator: Dr Jennifer Apolinário‐Hagen Address: FernUniversität Hagen, Universitätsstr. 33, 58097 Hagen, Germany Email: jennifer.apolinario‐hagen@fernuni‐hagen.de, stress.hagen@studicare.de Telephone: 02331 987 – 2272 |
| Notes |
Contact with authors: We contacted the authors for information on trial status, focus of the intervention on resilience and inclusion of healthcare students (Apolinário‐Hagen 2019 [pers comm]) Funding source: funded through internal research funds of the Fern Universität in Hagen (see study protocol) Declaration of interest: see study protocol. David Ebert is a stakeholder of the Institute for Online Health Trainings, which aims to transfer scientific knowledge related to the present research into routine health care. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest Ethical approval needed/obtained for study: approved by the University of Erlangen‐Nuremberg ethics committee (Erlangen, Germany; 33_17 Bc) Comments by study authors: trial registration number: DRKS00011800 (assigned 27 February 2017) Miscellaneous outcomes by the review authors: according to trial registration, recruitment and follow‐up are both complete (last update in February 2020) |
NL7623.
| Study name |
Public title: DEcrease STress through RESilience training for Students Scientific title: DEcrease STress through RESilience training for Students |
| Methods |
Study design: hybrid design: longitudinal observational cohort with nested RCT Study grouping: parallel group (IG vs CG); sequential multiple assignment Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): not specified in trial registration Imputation of missing data: not specified |
| Participants |
Country: The Netherlands Setting: not specified Age: not specified Sample size (randomised): 706 targeted Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: students at the Erasmus University Medical Centre Rotterdam, aged 16 years and older, who provide informed consent and have a score of 14 or higher on the PSS‐10 Method of recruitment: not specified Inclusion criteria: eligible for longitudinal cohort study: 1) all medical students, research master students, PhD students, nanobiology and clinical technology students at the Erasmus University Medical Centre (Erasmus MC) Rotterdam; 2) aged 16 years or older; 3) who give informed consent; within observational cohort, students fulfilling the following criteria are included in the nested RCT: 1) participation in the cohort study; 2) score of 14 or higher on the PSS‐10 Exclusion criteria: A student who meets any of the following criteria will be excluded from participation in the RCT, but can participate in the cohort study: 1) not insured for health care (for care provided in The Netherlands); 2) diagnosis of, or previously treated for, psychosis or mania; 3) response to at least 1 question on the Four‐Dimensional Symptom Questionnaire (4DSQ) items 33 or 46 is “often” or “very often or constantly" Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: multiple behavioural interventions (n randomised not specified)
Control: active control (n randomised not specified)
|
| Outcomes |
Outcomes collected and reported: Primary outcome
Secondary outcomes
Outcomes reported not specified Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (before and after each 8‐week intervention period); 3) 1‐year follow‐up; 4) 2‐year follow‐up;time points reported not specified Adverse events: not specified |
| Starting date | Study start/end date: February 2019 ‐ September 2023 |
| Contact information |
Principal investigator: Prof. Myriam Hunink Address: Erasmus University Medical Center Rotterdam, Rotterdam, The Netherlands Email: m.hunink@erasmusmc.nl Telephone: +31107043489 |
| Notes |
Contact with authors: no correspondence required Funding source: Erasmus MC, Studie Voorschot Middelen Declaration of interest: not specified in trial registration Ethical approval needed/obtained for study: not specified in trial registration Comments by study authors: website, destress.info Miscellaneous outcomes by the review authors:trialregister.nl/trial/7623 (trial register number assigned 22 March 2019); according to trial registration, the recruitment status is 'recruiting' |
Wild 2018.
| Study name |
Public title: A study of resilience training for student paramedics Scientific title: Preventing PTSD, depression, and associated health problems in student paramedics: a randomised controlled trial of internet‐delivered cognitive training for resilience (iCT‐R) |
| Methods |
Study design: RCT Study grouping: parallel group Unit of randomisation: individuals Power (power sample size calculation, level of power achieved): Setting power at 80%, α = 0.05 and hypothesising a reduction of relative risk of 50% gives an Odds Ratio of 0.429, which requires a total sample size of 304 to show a risk reduction of 50% between internet‐delivered cognitive training for resilience (iCT‐R) and the alternative intervention. Thus, each condition would require 152 participants. Since we have a third condition (standard practice), the total sample size required would be 456. Allowing for a 20% rate of attrition, we will require a total sample size of 570 Imputation of missing data: potential method of imputation not specified; data analysis will be intention‐to‐treat; all participants who have been randomised will be included in analyses, including those who drop out |
| Participants |
Country: UK Setting: online interventions Age: not specified in trial registration or study protocol Sample size (randomised): 570 targeted Sex: not specified Comorbidity (mean (SD) of respective measures in indicated, if available) at baseline: not specified Population description: student paramedics Inclusion criteria: see trial registration and study protocol (Wild 2018): 1) aged 18 and above (until 65 years); 2) training to be paramedics and in years 1, 2 or 3 of student paramedic training; 3) access to internet; 4) willing to be randomly allocated Exclusion criteria: see trial registration and study protocol (Wild 2018): 1) current symptoms of PTSD or MD, including suicidal ideation, requiring treatment (participants excluded if symptoms are interfering with their lives and they would like treatment; (score ≥ 10 on PHQ‐9); score on PHQ‐9 suicidal ideation item ≥ 1; Post‐traumatic Stress Disorder Checklist for Diagnostic and Statistical Manual of Mental Disorders, 5th edition (PCL‐5): ≥ 33) Attrition (withdrawals and exclusions): not specified Reasons for missing data: not specified |
| Interventions |
Intervention: iCT‐R: n randomised not specified)
Control 1: attention control mind‐online resilience intervention (already available intervention; n randomised not specified)
Control 2: TAU/wait‐list control (n randomised not specified)
|
| Outcomes |
Outcomes collected and reported: Primary outcome:
Secondary outcomes:
Tertiary outcomes (see study protocol Wild 2018):
Outcomes reported not specified Time points measured and reported: 1) pre‐intervention; 2) post‐intervention (i.e. 6 weeks); 3) 6‐month follow‐up (i.e. 6 months after intervention); 4) 1‐year follow‐up (i.e. 1 year after intervention); 5) 2‐year follow‐up (i.e. 2 years after intervention); diagnoses of PTSD and MD: all outcomes except 6‐month follow‐up; PTSD and MD symptomatology: all time points; secondary and tertiary outcomes: all time points except 6‐month follow‐up except for demographics (only pre‐intervention, 1‐year and 2‐year follow‐up); time points reported not specified Adverse events: not specified |
| Starting date | Study start/end date: January 2016; ‐January 2021 |
| Contact information |
Principal investigator: Dr Jennifer Wild Address: Department of Experimental Psychology; University of Oxford; Oxford Centre for Anxiety Disorders and Trauma, Oxford OX1 1TW, United Kingdom Email: jennifer.wild@psy.ox.ac.uk Telephone: +44 1865 618 612 |
| Notes |
Contact with authors: no correspondence required Funding source:
Declaration of interest: see study protocol (Wild 2018): Jennifer Wild, Anke Ehlers and their team have developed iCT‐R. They do not receive any income from this work Ethical approval needed/obtained for study: Ethical approval of the research protocol was gained from The Medical Sciences Inter‐Divisional Research Ethics Committee at the University of Oxford, 17 August 2017, ref: R44116/RE001 Comments by study authors: trial registration number ISRCTN16493616 (assigned 9 October 2017) Miscellaneous outcomes by the review authors: according to trial registration, the study is no longer recruiting but the overall trial status is ongoing; intention to publish September 2021 (last updated October 2017) |
Abbreviations common to all tables:
α: significance level; β: statistical power; BADS: Behavioural Activation for Depression Scale; BASS: Beliefs About Stress Scales; BDI: Beck Depression Inventory; BMI: body mass index; BRS: Brief Resilience Scale; CD‐RISC: Connor‐Davidson Resilience Scale; CEQ: Capability and Expectancy Questionnaire; CES‐D: Center for Epidemiology Studies‐ Depression; CG: control group; d: delta (Cohen's d, effect size); IG: intervention group; GAD‐7: Generalised Anxiety Disorder scale; GHQ: General Health Questionnaire; iCT‐R: internet‐delivered cognitive training for resilience; ISI: Insomnia Severity Index; ITT: intention‐to‐treat analysis; MBI: Maslach Burnout Inventory; MBSR: mindfulness‐based stress reduction; MD: major depression; n: sample size (e.g. in respective study group); OBI: Oldenburg Burnout Inventory; PCL‐5: Post‐traumatic stress disorder Check List for Diagnostic and Statistical Manual of Mental Disorders, 5th Edition; PHQ: Patient Health Questionnaire; PSS: Perceived Stress Scale; PSS: Presenteeism Scale for Students; PTSD: post‐traumatic stress disorder; RCT: randomised controlled trial; RIQ: Response to Intrusions Scale; RRS: Ruminative Response Scale; RS: Resilience Scale; RSES: Rosenburg Self‐Esteem Scale; SCS: Self‐Compassion Scale; SD: standard deviation; SMS: short message service; STAI: State‐Trait Anxiety Inventory; TAU: Treatment as usual; VAS: Visual Analogue Scales; vs: versus; WEMWS: Warwick‐Edinburgh Mental Well‐being Scale
Differences between protocol and review
We describe all modifications to the methods specified in the protocol (Helmreich 2017) in the following section.
-
Title
We changed the title of the review due to the post hoc restriction to healthcare students (see Types of participants).
-
Due to the post hoc restriction to healthcare students, we adapted the Background sections (Description of the condition; Description of the intervention; How the intervention might work; Why it is important to do this review) for this target group, e.g. by adding current references concerning previous systematic reviews in this population.
-
Description of the intervention
We modified the first sentence of this section to illustrate that we refer to resilience intervention research in general.
To be consistent, we limited the number of references for each psychotherapeutic method to one reference.
-
How the intervention might work
We changed the order of appearance of the different psychotherapeutic approaches in order to present theoretical approaches that are associated with cognitive‐behavioural therapy (CBT), such as stress inoculation and problem‐solving therapy, immediately after CBT before discussing other theoretical approaches.
Instead of performing a subgroup analysis on the target group of training, we had planned to conduct a subgroup analysis on training intensity, and added arguments for whether participants could benefit differently from differing training intensities. However, we were not able to perform this subgroup analysis due to the limited number of studies (see Table 2).
To derive the planned subgroup analysis for the theoretical foundation, we modified the section by describing the recent results of Joyce 2018, who analysed the impact of theoretical foundations of resilience intervention for the first time. At the time of writing the protocol (Helmreich 2017), this systematic review had not been published.
-
Why it is important to do this review
Compared to the protocol (Helmreich 2017), we presented the need for doing this review by integrating the results of recently‐published systematic reviews in clinical and non‐clinical adult populations (e.g. Joyce 2018).
-
We modified the objectives of the review by referring them to healthcare students, due to the post hoc restriction to this population.
-
Post hoc change 1: Initially, we planned to include clinical and non‐clinical populations (e.g. patients, employees, students, military) in this review (see Helmreich 2017). Based on a broad search strategy in October 2016, we identified 251 studies and 18 ongoing studies evaluating resilience‐training programmes in a variety of target groups. To be able to manage the large number of studies with many divergent target groups, we decided to de‐scope the review based on the populations investigated. This also allowed us to perform top‐up searches (i.e. for the period October 2016 to the present) that were specific to the respective target groups. We took the decision to de‐scope the review for two main reasons. First, using the database of 269 studies found by searches in October 2016, the review that we had originally planned might have been trumped by the publication of studies since this time point. Studies published since 2016, for example, using innovative delivery formats or different therapy methods from earlier studies, might have affected the results of subgroup analyses in the review (e.g. concerning delivery format). We also expected a substantial number of new studies fulfilling the eligibility criteria of the review for the period from the end of 2016 to 2019. Especially since 2015, there has been a significant growth in publications in the field; for example, by searching additional sources (e.g. reference lists, trial registers) or through study protocols published until October 2016, we identified 26 RCTs published in 2017 and 2018, plus 16 completed studies that had not yet been published (e.g. manuscripts in preparation or under review). Second, the RCTs identified were spread across a large number of comparisons (e.g. different target groups, theoretical foundations of interventions or control groups), which might have over‐scoped the review and resulted in substantial heterogeneity had all 269 studies been included. Based on the number of studies identified for the healthcare sector (including healthcare professionals like physicians, healthcare students like medical students, and employees associated with the healthcare sector such as human service professionals) in October 2016, we therefore decided to focus on RCTs in these populations. In June 2019, we performed top‐up searches broadly focusing on the healthcare sector, in order to guarantee a review of high credibility, which synthesised the latest evidence on the efficacy of psychological resilience interventions in this group at the time of publication.
Post hoc change 2: Based on the top‐up searches in June 2019, we identified 31 studies and eight ongoing studies that had been performed in healthcare professionals, healthcare students, and employees associated with the healthcare sector. Combined with the original search, we found a total of 80 RCTs and nine ongoing studies in this population. During the process of writing up this publication, we made further decisions about the eligibility criteria of this review for the Types of participants. We further separated the pool of 80 RCTs into two groups: 1) healthcare professionals (i.e. with completed training), and 2) healthcare students. Based on the evidence from the two searches, the first group of healthcare professionals, which is considered in another publication (Kunzler 2020), includes physicians, nurses, hospital personnel, and allied healthcare staff (e.g. psychologists, social workers) who are not always employed in direct medical care. We also considered studies with mixed samples where one of the named groups was included as a subgroup (total: 44 RCTs and five ongoing studies). The current (second) review refers to psychological interventions to foster resilience in healthcare students (total: 30 RCTs and three ongoing studies). We took the decision to split the review for the following empirical reasons: first, when summarising the 80 RCTs in an initial review draft we identified a substantial amount of heterogeneity for these studies that could only be partially explained by the planned subgroup analyses (see Table 2). Similarly, during internal peer review, the question arose about whether the research question for such a review (i.e. including healthcare professionals, students, and different employees associated with the healthcare sector) was too broad and the studies too heterogeneous to combine in the same review. We therefore decided to split the review into two publications, one for qualified workers and one for students, in order to create two very focused reviews that are based on sufficiently homogeneous studies, are up‐to‐date, and provide a concise summary of the evidence for the reviews' readers. A second rationale behind the decision to split the data referred to the stressor exposure in the two groups of healthcare professionals and healthcare students: Students and qualified staff have different stressor exposures and responsibilities, which might moderate the effect of resilience training. While healthcare professionals are exposed to stressors such as shift work, medical decision‐making or hierarchies, students are confronted with different kinds of stressors, e.g. exams, challenging subjects. A split between these two groups therefore seemed reasonable. Based on both searches, we identified six studies in employees widely associated with the healthcare sector, whose samples were too heterogeneous (e.g. human service professionals, nurse managers) to combine them with healthcare professionals (e.g. physicians, nurses) and who are mostly employed in clinical practice and patient care. It had also been critically questioned whether these employees can actually be viewed as frontline healthcare staff and should be included in a review of this target group. We therefore decided to omit this group of studies.
Based on these two post hoc changes, which had been discussed with the Cochrane Developmental, Psychosocial and Learning Problem (CDPLP) Editorial Team and the Cochrane Editorial and Methods Department, we adapted the Types of participants section accordingly, by writing that the current review considered healthcare students, i.e. students in training for health professions delivering direct medical care (e.g. medical students, nursing students, paramedic students) and for allied health professions as distinct from medical care (e.g. psychology students, social work students, counselling students, physical therapy students, occupational therapy students, speech therapy students, medical assistant students, medical technician students). Since we also identified several eligible studies in mixed samples, we stated that we would consider these mixed samples in the review and also included them in meta‐analyses, provided that the data for healthcare students could be obtained separately through the study authors.
-
We stated in the protocol that we planned also to include broader, health‐promoting interventions (e.g. well‐being therapy) (Helmreich 2017), but in the full review included only studies that explicitly defined the aim of fostering resilience, hardiness or post‐traumatic growth by using one or more of these terms in the publications. We made this modification on the basis of a post‐protocol amendment in consultation with the CDPLP Editorial Team. During the initial process of data extraction, we realised that it was not feasible to consider all health‐promoting interventions that aim to foster resilience in a broader sense (e.g. mental health, well‐being, psychological adaptation in a population with stressor exposure) without including the terms resilience, hardiness or post‐traumatic growth for the following reasons. First, it appeared very difficult to decide between which of the very large number of interventions should be included in the review and which should not, since the relationship of the interventions to the concept of resilience was not made explicit in those interventions. This would have left the review authors having to make many assumptions, with no objective criteria, resulting in reduced traceability of selection criteria and potentially low inter‐rater reliability on completion of screening. Second, since the objective of the review was to synthesise the current evidence on the efficacy of resilience training, including broader interventions, could have biased the review’s conclusions, as fostering resilience was not explicitly formulated as an aim in any of those interventions.
-
Based on a suggestion during internal peer review, we added adverse events as a primary outcome of this review, and marked it with an asterisk for inclusion in the 'Summary of findings' table.
-
We planned to perform searches in October 2016 for a review on psychological resilience interventions in clinical and non‐clinical populations. However, due to post hoc adaptation of the inclusion criteria, we based the search process for the review on a two‐step approach with searches performed in October 2016 and top‐up searches in June 2019.
We expanded the description of the search process by adding details of the use of the Cochrane Highly Sensitive Search Strategy for MEDLINE and Embase, as specified in the Cochrane Handbook (Lefebvre 2019), in order to present the search strategy in sufficient detail.
We searched the Web of Science Core Collection databases simultaneously rather than individually (Science Citation Index; Social Science Citation Index; Conference Proceedings Citation Index ‐ Social Science & Humanities; Conference Proceedings Citation Index ‐ Science), since our institutional access to this database only offered this possibility.
-
We judged the feasibility of selection criteria after 500 instead of 50 studies screened, due to the large number of records yielded by the searches for this review.
-
Assessment of risk of bias in included studies
We described our decision that the achieved baseline comparability between study conditions was part of selection bias (random‐sequence generation) in addition to the standard 'Risk of bias' domains in the Cochrane Handbook (Higgins 2011a). We had extracted this additional information from the included studies and judged it to be interesting for the readers of this review.
-
Continuous data: In the protocol we said we would calculate SMD effect sizes because resilience‐training studies are likely to use different measures for resilience and related constructs (Helmreich 2017). In the review, we added a sentence on the actual variation in the measurement scales between the included studies and referred to Table 3 and Table 4, which report the outcome scales used. We added information on how we interpreted the magnitude of effect sizes (SMDs) for continuous outcomes in the review.
-
Repeated observations on participants: We explained when we judged 'post‐test' in intervention studies as 'post‐intervention assessment' and considered them in the respective meta‐analyses. Assessments at more than one week after the end of training were declared as post‐test by some study authors, although interim events between the end of the intervention and the assessment might affect the effects measured. However, we wished to differentiate between such assessments and 'real' post‐tests with greater proximity to the end of training (i.e. within one week after the intervention ended)
-
We supplemented the procedure of dealing with missing data in the review by explaining how we would handle missing (summary outcome) data in studies of mixed samples. We added this information because we also considered studies with mixed samples in the review (see point 4).
We added a sentence about how we dealt with missing/incomplete summary outcome data, as well as missing outcome data due to attrition.
-
We added a sentence explaining that we discuss the similarities and differences between the included studies (e.g. in terms of study characteristics) in the Results and Discussion section of the review.
We further described the conventions used to interpret I2 values based on the suggestions in the Cochrane Handbook (Deeks 2019), in order be more transparent.
We added a sentence explaining that we calculated the 95% prediction intervals from random‐effects meta‐analyses to present the extent of between‐study variation according to the Cochrane Handbook (Deeks 2019).
-
Assessment of reporting biases
We stated in the protocol that we would assess potential publication bias by drawing and inspecting funnel plots, provided at least 10 studies were included in the meta‐analysis (Helmreich 2017). However, despite the limited number of studies per outcome (fewer than 10 studies), we chose to assess reporting bias for the primary outcomes at post‐test, in order to consider possible publication bias when rating the certainty of the evidence. We added this information to the review. We also stated that we did not assess reporting bias for the remaining outcomes at the other time points.
We inspected contour‐enhanced funnel plots for the primary outcomes, as they offer more graphical possibilities to detect publication bias than traditional funnel plots.
-
For several studies in the review that provided no means and SDs, but provided alternative data to calculate SMDs and the respective standard error, we described the procedure for combining these with other studies using the generic invariance method in Review Manager 5. This information had been missing from the protocol (Helmreich 2017).
We expanded the description of dealing with scales for depression and burnout, as well as scales for general well‐being or quality of life and work‐related measures in the same study, because several included studies met these criteria.
We did not conduct a planned network meta‐analysis, due to the insufficient evidence base in the review.
-
Summary of findings
We added information about the inclusion of the primary outcomes at post‐test in the ‘Summary of findings’ table. We took the decision to restrict the outcomes reported in the 'Summary of findings' table to those assessed at post‐test as a result of feedback received at internal peer review. Adverse events are now included in this table (see Types of outcome measures and point 6 in this section).
We replaced the term 'quality of the evidence' with 'certainty of the evidence' throughout the review, in order to be consistent with current guidelines and preferences in the literature (Hultcrantz 2017).
We provided further details for the downgrading of studies for each of the five GRADE criteria (study limitations, indirectness, inconsistency, imprecision, publication bias).
We also explained how we interpreted effect sizes and rated the certainty of the evidence, as this information had been missing from the protocol (Helmreich 2017).
-
Subgroup analysis and investigation of heterogeneity
We omitted the preplanned sensitivity analysis on 'target group in resilience interventions', due to the review's revised focused on healthcare students only.
We added a post hoc analysis of training intensity; low‐intensity training included interventions with a total duration of five hours or less or three sessions or fewer (if no duration in hours or minutes was indicated); moderate intensity to training that included more than five hours to 12 hours or less, or more than three sessions to 12 sessions or fewer; and high intensity to programmes of more than 12 hours or more than 12 sessions. We added this subgroup analysis post hoc, due to the restriction to healthcare students (see point 2c).
We added a subgroup for mobile‐based delivery format to the preplanned analysis on delivery format, given the evidence found in this review.
We changed ‘multimodal intervention’ to ‘combined intervention’ to the preplanned analysis on theoretical foundation, to refer to resilience interventions that were based on two or more explicit theoretical foundations, such as CBT and ACT or CBT and mindfulness. We also added coaching, positive psychology and nonspecific resilience training. Non‐specific training programmes included resilience interventions fostering one or several resilience factors, but without specifying any explicit theoretical foundation or where the underlying framework could not be assigned to a definite theoretical foundation. We changed from 'multimodal' to 'combined intervention' in order to be consistent with other subgroup analyses (compare combined setting, combined delivery). We added the subgroups based on the evidence found in this review.
Lastly, we added active and attention control to the preplanned analysis on comparator group, in order to distinguish between these groups. Attention‐control groups referred to an alternative treatment that mimicked the amount of time and attention received (e.g. by the trainer) in the intervention group. We used the term ‘active control’ for alternative treatment (no standard care; for example, treatment developed specifically for the treatment study) but that did not control for the amount of time and attention in the intervention group, and was not attention control in a narrow sense. We made these changes following the evidence found in this review.
-
We provided more detail on the planned sensitivity analysis based on risk of bias (i.e. restriction to studies at low and unclear risk of attrition, as well as at low and unclear risk of reporting bias, respectively), as this information had been missing from the protocol (Helmreich 2017). See Table 2.
Contributions of authors
Angela Kunzler: protocol writing, study selection, data extraction and assimilation, 'Risk of bias' assessment, GRADE assessment, statistical analysis and review writing. Angela Kunzler has overall responsibility for the review and is the guarantor for the review. Isabella Helmreich: protocol writing, study selection, data extraction, 'Risk of bias' assessment, GRADE assessment, review writing. Jochem König: protocol writing, expert statistical support, statistical analysis and review writing. Andrea Chmitorz: protocol writing, review writing, arbiter. Michèle Wessa: protocol writing and review writing. Harald Binder: protocol writing, expert statistical support, statistical analysis and review writing. Klaus Lieb: overall supervision of the review, protocol writing, review writing, arbiter.
All review authors agreed on this version before publication.
Sources of support
Internal sources
-
Leibniz Institute for Resilience Research (LIR) gGmbH, Wallstraße 7/7a, 55122 Mainz, Germany
Home institution of AMK, IH, MW and KL; support provided in the form of salary and resources.
-
Institute of Medical Biostatistics, Epidemiology and Informatics (IMBEI), University Medical Center of the Johannes Gutenberg University Mainz, Germany
Home institution of JK; support provided in the form of salary and resources.
-
Institute of Medical Biometry and Statistics, Faculty of Medicine and Medical Center, University of Freiburg, Germany
Home institution of HB; support provided in the form of salary and resources.
External sources
-
Funding provided by the Ministry of Science (MWWK) of the State Rhineland‐Palatinate, Germany
Support provided in the form of resources.
Declarations of interest
Angela Kunzler: none known. Isabella Helmreich is a board‐certified cognitive‐behaviour therapist. Jochem König: none known. Andrea Chmitorz is a board‐certified cognitive‐behaviour therapist. Michèle Wessa is a board‐certified cognitive‐behaviour therapist. Harald Binder: none known. Klaus Lieb (KL) is a board‐certified cognitive‐behaviour therapist with a special interest in schema therapy, and an Editor with Cochrane Developmental, Psychosocial and Learning Problems. KL received funding for this review from the Ministry of Science (MWWK) of the State Rhineland‐Palatinate, Germany.
New
References
References to studies included in this review
Akbari 2017 {published data only}
- Akbari B. Effectiveness of training psychological resilience on aggression and happiness among students. Journal of Holistic Nursing and Midwifery 2017;27(1):1-7. [DOI: 10.18869/acadpub.hnmj.27.1.1] [DOI] [Google Scholar]
Anderson 2017 {published data only}
- Anderson GS, Vaughan AD, Mills S. Building personal resilience in paramedic students. Journal of Community Safety & Well-being 2017;2(2):51-4. [DOI: 10.35502/jcswb.44] [DOI] [Google Scholar]
Barry 2019 {published and unpublished data}
- Barry KM, Woods M, Martin A, Stirling C, Warnecke E. A randomized controlled trial of the effects of mindfulness practice on doctoral candidate psychological status. Journal of American College Health 2019;67(4):299-307. [DOI: 10.1080/07448481.2018.1515760] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chen 2018a {published data only}
- Chen L, Kelleher C. Comparative impact of brief mindfulness-based compassion and mindfulness-based stress reduction programs on stress management and grades of first semester nursing students. Global Advances In Health and Medicine 2018;7:174. [DOI: 10.1177/2164956118773837] [3562] [DOI] [Google Scholar]
Delaney 2016 {published data only}
- Delaney C, Barrere C, Robertson S, Zahourek R, Diaz D, Lachapelle L. Pilot testing of the NURSE stress management intervention. Journal of Holistic Nursing 2016;34(4):369-89. [DOI: 10.1177/0898010115622295] [PMID: ] [DOI] [PubMed] [Google Scholar]
Erogul 2014 {published and unpublished data}
- Erogul M, Singer G, McIntyre T, Stefanov DG. Abridged mindfulness intervention to support wellness in first-year medical students. Teaching and Learning in Medicine 2014;26(4):350-6. [DOI: 10.1080/10401334.2014.945025] [PMID: ] [DOI] [PubMed] [Google Scholar]
Galante 2018 {published data only}
- Galante J, Dufour G, Vainre M, Wagner AP, Stochl J, Benton A, et al. A mindfulness-based intervention to increase resilience to stress in university students (the Mindful Student Study): a pragmatic randomised controlled trial. Lancet. Public Health 2018;3(2):e72-81. [DOI: 10.1016/S2468-2667(17)30231-1] [PMC5813792] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galante J, Dufour G, Vainre M, Wagner AP, Stochl J, Benton A, et al. Effectiveness of providing university students with a mindfulness-based intervention to increase resilience to stress: a pragmatic randomised controlled trial. Early Intervention in Psychiatry 2018;12(Suppl 1):96. [DOI: 10.1111/eip.12723] [Oral 16, Talk 5] [DOI] [Google Scholar]
Geschwind 2015 {published data only}
- Geschwind N, Meulders M, Peters ML, Vlaeyen JW, Meulders A. Can experimentally induced positive affect attenuate generalization of fear of movement-related pain? Journal of Pain 2015;16(3):258-69. [DOI: 10.1016/j.jpain.2014.12.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Goldstein 2019 {published and unpublished data}
- Goldstein MR. Improvements in sleep disturbance following yogic breathing-based stress-management intervention compared to cognitively based intervention in college students. Sleep 2019;42(Suppl 1):A394-5. [DOI: 10.1093/sleep/zsz067.977] [0980] [DOI] [Google Scholar]
Houston 2017 {published and unpublished data}
- First J, First NL, Houston B. Resilience and Coping Intervention (RCI): a group intervention to foster college student resilience. Social Work with Groups 2018;41(3):198-210. [DOI: 10.1080/01609513.2016.1272032] [DOI] [Google Scholar]
- Houston JB, First J, Spialek ML, Sorenson ME, Mills-Sandoval T, Lockett M, et al. Randomized controlled trial of the resilience and coping intervention (RCI) with undergraduate university students. Journal of American College Health 2017;65(1):1-9. [DOI: 10.1080/07448481.2016.1227826] [PMID: ] [DOI] [PubMed] [Google Scholar]
ISRCTN64217625 {published data only}
- ISRCTN64217625. An evaluation of resilience interventions for emergency workers [An evaluation of resilience interventions for emergency workers: a randomised controlled trial]. www.isrctn.com/ISRCTN64217625 (first received 5 February 2016).
Kelleher 2018 {published data only}
- Kelleher C, Chen L. Impact of a brief mindfulness-based stress reduction program for first semester nursing students. Global Advances In Health and Medicine 2018;7:172. [DOI: 10.1177/2164956118773837] [3555] [DOI] [Google Scholar]
Kötter 2016 {published data only}
- Kötter T, Niebuhr F. Resource-oriented coaching for reduction of examination-related stress in medical students: an exploratory randomized controlled trial. Advances in Medical Education and Practice 2016;7:497-504. [DOI: 10.2147/AMEP.S110424] [PMC5003014] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mathad 2017 {published data only}
- Mathad MD, Pradhan B, Sasidharan RK. Effect of yoga on psychological functioning of nursing students: a randomized wait list control trial. Journal of Clinical and Diagnostic Research 2017;11(5):KC01-5. [DOI: 10.7860/JCDR/2017/26517.9833] [PMC5483709] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mejia‐Downs 2016 {unpublished data only}
- Mejia-Downs AM. An Intervention Enhances Resilience in Physical Therapy Students [PhD thesis]. Provo (UT): Rocky Mountain University of Health Professions, 2016. [Google Scholar]
Miu 2016 {published data only}
- Miu AS. The Effects of Mindsets on Depression [PhD thesis]. Atlanta (GA): Emory University, 2016. [Google Scholar]
Mueller 2018 {published data only}
- Mueller K, Prins R, De Heer HD. An online intervention increases empathy, resilience, and work engagement among physical therapy students. Journal of Allied Health 2018;47(3):196-203. [PMID: ] [PubMed] [Google Scholar]
Peng 2014 {published data only}
- Peng L, Li M, Jiang X, Zuo X, Miao Y, Yu Y, et al. Effects of resilience training on positive and negative emotion and emotion regulation strategies in military medical students with different resilience. Journal of Third Military Medical University 2014;36(5):470-2. [en.cnki.com.cn/Article_en/CJFDTOTAL-DSDX201405015.htm] [Google Scholar]
- Peng L, Li M, Zuo X, Miao Y, Chen L, Yu Y, et al. Application of the Pennsylvania resilience training program on medical students. Personality and Individual Differences 2014;61-2:47-51. [DOI: 10.1016/j.paid.2014.01.006] [DOI] [Google Scholar]
Porter 2008 {published and unpublished data}
- Porter S, Johnson A. Increasing paramedic students' resiliency to stress: assessing correlates and the impact of intervention. College Quarterly 2008;11(3):1-13. [files.eric.ed.gov/fulltext/EJ830648.pdf] [Google Scholar]
Recabarren 2019 {published and unpublished data}
- NCT03861013. Reward under stress: effects of a multidimensional stress prevention program in university students [Reward under stress: psychobiological mechanisms of resilience to stress]. clinicaltrials.gov/ct2/show/NCT03861013 (first received 23 December 2018).
- Recabarren RE, Gaillard C, Guillod M, Martin-Soelch C. Short-term effects of a multidimensional stress prevention program on quality of life, well-being and psychological resources. A randomized controlled trial. Frontiers in Psychiatry 2019;10:88. [DOI: 10.3389/fpsyt.2019.00088] [PMC6422882] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sahranavard 2018 {published data only}
- Sahranavard S, Esmaeili A, Dastjerdi R, Salehiniya H. The effectiveness of stress-management-based cognitive-behavioral treatments on anxiety sensitivity, positive and negative affect and hope. BioMedicine 2018;8(4):10-7. [DOI: 10.1051/bmdcn/2018080423] [PMC6254097] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahranavard S, Esmaeili A, Salehiniya H, Behdani S. The effectiveness of group training of cognitive behavioral therapy-based stress management on anxiety, hardiness and self-efficacy in female medical students. Journal of Education and Health Promotion 2019;8:49. [DOI: 10.4103/jehp.jehp_327_18] [PMC6432834] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Samouei 2015 {published data only}
- Samouei R, Ghasemim F. Role of mindfulness training on psychological capital of Isfahan University of Medical Sciences students. International Journal of Educational & Psychological Researches 2015;1(4):293–7. [DOI: 10.4103/2395-2296.163936] [DOI] [Google Scholar]
Smeets 2014 {published data only (unpublished sought but not used)}
- Smeets E, Neff K, Alberts H, Peters M. Meeting suffering with kindness: effects of a brief self-compassion intervention for female college students. Journal of Clinical Psychology 2014;70(9):794-807. [DOI: 10.1002/jclp.22076] [PMID: ] [DOI] [PubMed] [Google Scholar]
Stephens 2012 {unpublished data only}
- Stephens TL. Increasing Resilience in Adolescent Nursing Students [PhD thesis]. Knoxville (TN): University of Tennessee, 2012. [Google Scholar]
Venieris 2017 {published data only}
- Venieris P. The Happiness Project: A Randomized Control Trial of an Online Positive Psychology Intervention for Graduate Students [PhD thesis]. Tempe (AZ): Arizona State University, 2017. [Google Scholar]
Victor 2018 {published and unpublished data}
- Victor P, Dikloo AS, Schwert P, Willutzki U. Resilienz- vs problemorientierte beratung von studierenden: eine randomisierte kontrollierte studie. Zeitschrift für Klinische Psychologie und Psychotherapie 2018;47(4):241-51. [DOI: 10.1026/1616-3443/a000496] [DOI] [Google Scholar]
Waddell 2005 {published data only}
- Waddell J, Bauer M. Career planning and development for students: building a career in a professional practice discipline. Canadian Journal of Career Development 2005;4(2):4-13. [cjcdonline.ca/wp-content/uploads/2014/11/Career-Planning-and-Development-for-Students.pdf] [Google Scholar]
Waddell 2015 {published data only (unpublished sought but not used)}
- Waddell J, Spalding K, Canizares G, Navarro J, Connell M, Jancar S, et al. Integrating a career planning and development program into the baccalaureate nursing curriculum: part I. Impact on students' career resilience. International Journal of Nursing Education Scholarship 2015;12:162-73. [DOI: 10.1515/ijnes-2014-0035] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wang 2012 {published data only}
- Wang Z, Wang H-Z, Zhai H-M. Effects of positive-psychology-based group counseling on college students with mental crisis. Journal of Nursing 2012;19(11):4-7. [en.cnki.com.cn/Article_en/CJFDTOTAL-NFHL201211003.htm] [Google Scholar]
Warnecke 2011 {published and unpublished data}
- Warnecke E, Quinn S, Ogden K, Towle N, Nelson MR. A randomised controlled trial of the effects of mindfulness practice on medical student stress levels. Medical Education 2011;45(4):381-8. [DOI: 10.1111/j.1365-2923.2010.03877.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
ACTRN12617000300370 {published data only}
- ACTRN12617000300370. The effect of mobile mindfulness meditation on distress in two cohorts: incoming university students and university staff [A randomised, controlled trial to evaluate the effectiveness of a mobile mindfulness meditation tool at reducing distress, and improving wellness, resilience, and mindfulness in two cohorts: incoming university students and university staff]. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=372301 (first received 17 February 2017).
Brady 2016 {published data only}
- Brady ST, Reeves SL, Garcia J, Purdie-Vaughns V, Cook JE, Taborsky-Barba S, et al. The psychology of the affirmed learner: spontaneous self-affirmation in the face of stress. Journal of Educational Psychology 2016;108(3):353-73. [DOI: 10.1037/edu0000091] [DOI] [Google Scholar]
De la Fuente 2018 {published data only}
- De la Fuente J, Mañas I, Franco C, Cangas AJ, Soriano E. Differential effect of level of self-regulation and mindfulness training on coping strategies used by university students. International Journal of Environmental Research and Public Health 2018;15(10):E2230. [DOI: 10.3390/ijerph15102230] [PMC6210926] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
De Vibe 2013 {published data only}
- De Vibe M, Solhaug I, Rosenvinge JH, Tyssen R, Hanley A, Garland E. Six-year positive effects of a mindfulness-based intervention on mindfulness, coping and well-being in medical and psychology students: results from a randomized controlled trial. PLOS One 2018;13(4):e0196053. [DOI: 10.1371/journal.pone.0196053] [PMC5916495] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Vibe M, Solhaug I, Tyssen R, Friborg O, Rosenvinge JH, Sørlie T, et al. Mindfulness training for stress management: a randomised controlled study of medical and psychology students. BMC Medical Education 2013;13:107. [DOI: 10.1186/1472-6920-13-107] [PMC3751423] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Duan 2019 {published data only}
- Duan W, Bu H. Randomized trial investigating of a single-session character-strength-based cognitive intervention on freshman's adaptability. Research on Social Work Practice 2019;29(1):82-92. [DOI: 10.1177/1049731517699525] [DOI] [Google Scholar]
Dvořáková 2017 {published data only}
- Dvořáková K, Kishida M, Li J, Elavsky S, Broderick PC, Agrusti MR, et al. Promoting healthy transition to college through mindfulness training with first-year college students: pilot randomized controlled trial. Journal of American College Health 2017;65(4):259-67. [DOI: 10.1080/07448481.2017.1278605] [PMC5810370] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Esch 2013 {published data only}
- Esch T, Sonntag U, Esch SM, Thees S. Stress management and mind-body medicine: a randomized controlled longitudinal evaluation of students' health and effects of a behavioral group intervention at a middle-size German university (SM-MESH). Forschende Komplementärmedizin 2013;20(2):129-37. [DOI: 10.1159/000350671] [PMID: ] [DOI] [PubMed] [Google Scholar]
Huennekens 2018 {published data only}
- Huennekens AO. Comparing the Effectiveness of Christian and Secular Mindfulness-Based Stress Reduction: A Randomized Controlled Trial [PhD thesis]. Mobile (AL): University of South Alabama, 2018. [Google Scholar]
Pogrebtsova 2018 {published data only}
- Pogrebtsova E, Craig J, Chris A, O'Shea D, González-Morales MG. Exploring daily affective changes in university students with a mindful positive reappraisal intervention: a daily diary randomized controlled trial. Stress and Health 2018;34(1):46-58. [DOI: 10.1002/smi.2759] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sampl 2017 {published data only}
- Sampl J, Maran T, Furtner MR. A randomized controlled pilot intervention study of a mindfulness-based self-leadership training (MBSLT) on stress and performance. Mindfulness 2017;8(5):1393-407. [DOI: 10.1007/s12671-017-0715-0] [PMC5605596] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Song 2015 {published data only}
- Song Y, Lindquist R. Effects of mindfulness-based stress reduction on depression, anxiety, stress and mindfulness in Korean nursing students. Nurse Education Today 2015;35(1):86-90. [DOI: 10.1016/j.nedt.2014.06.010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Dijk 2015 {published data only}
- Van Dijk I, Lucassen PL, Akkermans RP, Van Engelen BG, Van Weel C, Speckens AE. Effects of mindfulness-based stress reduction on the mental health of clinical clerkship students: a cluster-randomized controlled trial. Academic Medicine 2017;92(7):1012-21. [DOI: 10.1097/ACM.0000000000001546] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Van Dijk I, Lucassen PL, Speckens AE. Mindfulness training for medical students in their clinical clerkships: two cross-sectional studies exploring interest and participation. BMC Medical Education 2015;15:24. [DOI: 10.1186/s12909-015-0302-9] [PMC4348100] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Victor 2017 {published data only}
- Victor PP, Teismann T, Willutzki U. A pilot evaluation of a strengths-based CBT intervention module with college students. Behavioural and Cognitive Psychotherapy 2017;45(4):427-31. [DOI: 10.1017/s1352465816000552] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Arch 2014 {published data only}
- Arch JJ, Brown KW, Dean DJ, Landy LN, Brown KD, Laudenslager ML. Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Psychoneuroendocrinology 2014;42:49–58. [DOI: 10.1016/j.psyneuen.2013.12.018] [PMC3985278] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baeza‐Velasco 2020 {published data only}
- Baeza-Velasco C, Genty C, Jaussent I, Benramdane M, Courtet P, Olié E. Study protocol of a multicenter randomized controlled trial of mindfulness-based intervention versus relaxation to reduce emotional exhaustion in medical students in France: the "Must prevent" study. BMC Psychiatry 2020;20(1):115. [DOI: 10.1186/s12888-020-02529-9] [PMC7066837] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bauman 2014 {published data only}
- Bauman LV. The Impact of a Psychological Capital Intervention on College Student Well-Being [PhD thesis]. Azusa (CA): Azusa Pacific University, 2014. [Google Scholar]
Beadel 2016 {published data only}
- Beadel JR, Mathews A, Teachman BA. Cognitive bias modification to enhance resilience to a panic challenge. Cognitive Therapy and Research 2016;40(6):799–812. [DOI: 10.1007/s10608-016-9791-z] [DOI] [Google Scholar]
Chen 2018b {published data only}
- Chen CY. A study of group intervention on depression in urban college students. Basic & Clinical Pharmacology & Toxicology 2018;122(Suppl 2):17-18. [DOI: 10.1111/bcpt.12968] [HHME17-TH04] [DOI] [Google Scholar]
Clark 2019 {published data only}
- Clark CM, Gorton KL. Cognitive rehearsal, HeartMath, and simulation: an intervention to build resilience and address incivility. Journal of Nursing Education 2019;58(12):690-7. [DOI: 10.3928/01484834-20191120-03] [PMID: ] [DOI] [PubMed] [Google Scholar]
Crane 2020 {published data only}
- Crane MF, Kangas M, Karin E, Searle B, Chen D. Leveraging the experience of stressors: the role of adaptive systematic self-reflection. Anxiety, Stress & Coping 2020;33(3):231-47. [DOI: 10.1080/10615806.2020.1732359] [PMID: ] [DOI] [PubMed] [Google Scholar]
Despeaux 2019 {published data only}
- Despeaux KE, Lating JM, Everly GS Jr, Sherman MF, Kirkhart MW. A randomized controlled trial assessing the efficacy of group Psychological First Aid. Journal of Nervous and Nental Disease 2019;207(8):626-32. [DOI: 10.1097/NMD.0000000000001029] [PMID: ] [DOI] [PubMed] [Google Scholar]
DRKS00011265 {published data only}
- DRKS00011265. Efficacy and cost efficacy of an internetbased, unguided self-help intervention (StudiCare: Resilienz) for improving resilience in students. www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00011265 (first received 18 January 2017).
DRKS00013765 {published data only}
- DRKS00013765. Efficacy and cost efficacy of an internetbased, unguided selfhelp intervention (StudiCare: Resilienz) for improving resilience in resilient students. www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00013765 (first received 10 April 2018).
Enrique 2019 {published data only}ISRCTN11866034
- Enrique A, Mooney O, Salamana-Sanabria A, Lee CT, Farrell S, Richards D. Assessing the efficacy and acceptability of an internet-delivered intervention for resilience among college students: a pilot randomised control trial protocol. Internet Interventions 2019;17:100254. [DOI: 10.1016/j.invent.2019.100254] [PMC6603299] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISRCTN11866034. Assessment of the effectiveness and acceptability of an online intervention for adapting well in the face of adversity, trauma, tragedy, threats or significant sources of stress [Assessing the efficacy and acceptability of an Internet-delivered intervention for resilience: a pilot study for a randomised control trial]. www.isrctn.com/ISRCTN11866034 (first received 3 February 2019).
Flett 2020 {published data only}
- Flett JAM, Conner TS, Riordan BC, Patterson T, Hayne H. App-based mindfulness meditation for psychological distress and adjustment to college in incoming university students: a pragmatic, randomised, waitlist-controlled trial. Psychology & Health 2020 Feb 12 [Epub ahead of print]. [DOI: 10.1080/08870446.2019.1711089] [DOI] [PubMed]
Games 2020 {published data only}
- Games N, Thompson CL, Barrett P. A randomised controlled trial of the Adult Resilience Program: a universal prevention program. International Journal of Psychology 2020;55(S1):78-87. [DOI: 10.1002/ijop.12587] [DOI] [PubMed] [Google Scholar]
Gerson 2013 (study 1) {published data only}
- Gerson MW, Fernandez N. PATH: a program to build resilience and thriving in undergraduates. Journal of Applied Social Psychology 2013;43(11):2169-84. [DOI: 10.1111/jasp.12168] [DOI] [Google Scholar]
Gerson 2013 (study 2) {published data only}
- Gerson MW, Fernandez N. PATH: a program to build resilience and thriving in undergraduates. Journal of Applied Social Psychology 2013;43(11):2169-84. [DOI: 10.1111/jasp.12168] [DOI] [Google Scholar]
Harrer 2018 {published data only}
- DRKS00010212. Online based self-help stress management program for students with feedback on demand. www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00010212 (first received 12 May 2016).
- Harrer M, Adam SH, Fleischmann RJ, Baumeister H, Auerbach R, Bruffaerts R, et al. Effectiveness of an internet- and app-based intervention for college students with elevated stress: randomized controlled trial. Journal of Medical Internet Research 2018;20(4):e136. [DOI: 10.2196/jmir.9293] [PMC5938594] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Heath 2020 {published data only}
- Heath J, Walmsley LA, Aker RM, Ferrin S, Stone D, Norton JC. CPR to the rescue! An interprofessional pilot program: cultivating practices for resilience (CPR) camp. Clinical Nurse Specialist 2020;34(2):63-9. [DOI: 10.1097/NUR.0000000000000506] [PMID: ] [DOI] [PubMed] [Google Scholar]
Herrero 2019 {published data only}
- Botella C, Baños R, Ebert D, Berger T, Schaub M, Garcia-Palacios A, et al. ICARE-R: an internet-based intervention for promoting resilience in freshmen university students. Cyber Therapy & Rehabilitation 2016;9(1):46-7. [www.cybertherapyandrehabilitation.com/2017/03/full-issue-91-2/] [Google Scholar]
- Herrero R, Mira A, Cormo G, Etchemendy E, Baños R, Garciá-Palacios A, et al. An internet based intervention for improving resilience and coping strategies in university students: study protocol for a randomized controlled trial. Internet Interventions 2019;16:43-51. [DOI: 10.1016/j.invent.2018.03.005] [PMC6364440] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
ISRCTN17156687 {published data only}ISRCTN17156687
- ISRCTN17156687. Study of a smartphone-delivered, therapist-supported mindfulness-based therapy program for depression in Finnish university students [Randomized controlled study of a smartphone-delivered, therapist-supported, mindfulness-based intervention for depression in Finnish university students]. www.isrctn.com/ISRCTN17156687 (first received 24 June 2018).
Jackson 2019 {published data only}
- Jackson AC. The Efficacy of Coaching Interventions for Undergraduates to Increase Positive Coping Behavior: A Quantitative Quasi-Experiment [PhD thesis]. Portland (OR): Concordia University, 2019. [Google Scholar]
Kanekar 2010 {published data only}
- Kanekar A, Sharma M, Atri A. Enhancing social support, hardiness, and acculturation to improve mental health among Asian Indian international students. International Quarterly of Community Health Education 2010;30(1):55-68. [DOI: 10.2190/IQ.30.1.e] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kon 2019 {published data only}
- Kon RH, Flickinger TE, Schorling J, May N, Owens JE, Harrison M, et al. Flourishing in the clerkship year: a longitudinal curriculum introducing skills to reduce burnout and foster resilience in medical students. Journal of General Internal Medicine 2019;34(2):S809. [DOI: 10.1007/s11606-019-05007-5] [DOI] [Google Scholar]
Liu 2016 {published data only}
- Liu L, Zhang X, Song L. Research on the intervention of positive group psychology counseling on the resilience of college students. Advances in Social Science, Education and Humanities Research 2016;40:53-5. [DOI: 10.2991/icelaic-16.2017.13] [DOI] [Google Scholar]
Liu 2019 {published data only}
- Liu JJW, Reed M, Vickers K. Reframing the individual stress response: Balancing our knowledge of stress to improve responsivity to stressors. Stress & Health 2019;35(5):607-16. [DOI: 10.1002/smi.2893] [DOI] [PubMed] [Google Scholar]
NCT02867657 {published data only}
- NCT02867657. Bringing the practice of mindfulness into nature - preventing mental fatigue in healthcare professionals [Enhancement of presence, compassion and resilience bringing the practice of mindfulness into nature - preventing mental fatigue in healthcare professionals]. clinicaltrials.gov/ct2/show/NCT02867657 (first received 10 August 2016).
NCT03669016 {published data only}
- NCT03669016. MIndfulness for students (Mindfulstud) [Mindfulness for students]. clinicaltrials.gov/ct2/show/NCT03669016 (first received 31 August 2018).
NCT03903978 {published data only}
- NCT03903978. Efficacy and effectiveness of a self-applied online program to promote resilience and coping skills in college students [Efficacy and effectiveness of a self-applied online program to promote resilience and coping skills in university students in three Spanish-speaking countries: study protocol for a randomized controlled trial]. clinicaltrials.gov/show/nct03903978 (first received 18 September 2018).
NCT04064372 {published data only}
- NCT04064372. Mindful response to adversity: a brief stress resilience training [Mindful response to adversity: a brief stress resilience training for improving mental health in students]. clinicaltrials.gov/ct2/show/NCT04064372 (first received 1 January 2019).
NCT04416074 {published data only}
- NCT04416074. An online 5-week professional identity group psychotherapy [An online 5-week professional identity group psychotherapy for nursing student during clinical rotation practice]. clinicaltrials.gov/ct2/show/NCT04416074 (first received 30 May 2020).
Noormohamadi 2019 {published data only}
- Noormohamadi SM, Arefi M, Afshaini K, Kakabaraee K. The effect of rational-emotive behavior therapy on anxiety and resilience in students. International Journal of Adolescent Medicine and Health 2019 Jun 8 [Epub ahead of print]. [DOI: 10.1515/ijamh-2019-0099] [ijamh.ahead-of-print/ijamh-2019-0099/ijamh-2019-0099.xml] [PMID: ] [DOI] [PubMed]
Oman 2008 {published data only}
- Oman D, Shapiro SL, Thoresen CE, Plante TG, Flinders T. Meditation lowers stress and supports forgiveness among college students: a randomized controlled trial. Journal of American College Health 2008;56(5):569-78. [DOI: 10.3200/JACH.56.5.569-578] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Shapiro SL, Brown KW, Thoresen C, Plante TG. The moderation of mindfulness-based stress reduction effects by trait mindfulness: results from a randomized controlled trial. Journal of Clinical Psychology 2011;67(3):267-77. [DOI: 10.1002/jclp.20761] [PMID: ] [DOI] [PubMed] [Google Scholar]
Palma‐Gómez 2020 {published data only}
- Palma-Gómez A, Herrero R, Baños R, García-Palacios A, Castañeiras C, Fernandez GL, et al. Efficacy of a self-applied online program to promote resilience and coping skills in university students in four Spanish-speaking countries: study protocol for a randomized controlled trial. BMC Psychiatry 2020;20(1):148. [DOI: 10.1186/s12888-020-02536-w] [PMC7133009] [PMID: 32248795 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Roghanchi 2013 {published data only}
- Roghanchi M, Mohamad AR, Mey SC, Momeni KM, Golmohamadian M. The effect of integrating rational emotive behavior therapy and art therapy on self-esteem and resilience. The Arts in Psychotherapy 2013;40(2):179-84. [DOI: 10.1016/j.aip.2012.12.006] [DOI] [Google Scholar]
Seligman 2007 {published data only}
- Seligman ME, Schulman P, Tryon AM. Group prevention of depression and anxiety symptoms. Behaviour Research and Therapy 2007;45(6):1111-26. [DOI: 10.1016/j.brat.2006.09.010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tollefson 2018 {published data only}
- Tollefson M, Kite B, Matuszewicz E, Dore A, Heiss C. Effectiveness of student-led stress reduction activities in the undergraduate classroom on perceived student stress. College Student Journal 2018;52(4):505-15. [www.ingentaconnect.com/content/prin/csj/2018/00000052/00000004/art00010;jsessionid=7big1jsg068pt.x-ic-live-03] [Google Scholar]
Xu 2019 {published data only}
- Xu YY, Wu T, Yu YJ, Li M. A randomized controlled trial of well-being therapy to promote adaptation and alleviate emotional distress among medical freshmen. BMC Medical Education 2019;19(1):182. [DOI: 10.1186/s12909-019-1616-9] [PMC6547604] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ye 2016 {published data only}
- Ye YS, Zhang ZX, Ye L, Bao CY. Impact of emotional resilience training upon psychological safety of undergraduate nursing interns. Chinese Journal of Modern Nursing 2016;22(18):2633-6. [No DOI or other object identifier available] [Google Scholar]
Zhang 2018 {published data only}
- Zhang H. Influence of wisdom education on psychological resilience of college students in frustration situation. Indian Journal of Pharmaceutical Sciences 2018;80(Suppl 1):50-1. [Poster 130] [www.ijpsonline.com/supplementary-files/supplement-to-issue-1-jan-feb.pdf] [Google Scholar]
References to ongoing studies
Harrer 2019 {published and unpublished data}
- DRKS00011800. Online based self-help stress management program for distance-learning students with feedback on demand [Online based self-help stress management program for distance-learning students with feedback on demand - StudiCare]. who.int/trialsearch/Trial2.aspx?TrialID=DRKS00011800 (first received 27 February 2017).
- Harrer M, Apolinário-Hagen J, Fritsche L, Drüge M, Krings L, Beck K, et al. Internet- and app-based stress intervention for distance-learning students with depressive symptoms: protocol of a randomized controlled trial. Frontiers in Psychiatry 2019;10:361. [DOI: 10.3389/fpsyt.2019.00361] [PMC6537513] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
NL7623 {published data only}
- NL7623. DEcrease STress through RESilience training for Students. who.int/trialsearch/Trial2.aspx?TrialID=NL7623 (first received 22 March 2019).
Wild 2018 {published data only}ISRCTN16493616
- ISRCTN16493616. A study of resilience training for student paramedics [Preventing PTSD, depression, and associated health problems in student paramedics: a randomised controlled trial of internet-delivered cognitive training for resilience (iCT-R)]. isrctn.com/ISRCTN16493616 (first received 1 October 2017).
- Wild J, El-Salahi S, Tyson G, Lorenz H, Pariante CM, Danese A, et al. Preventing PTSD, depression and associated health problems in student paramedics: protocol for PREVENT-PTSD, a randomised controlled trial of supported online cognitive training for resilience versus alternative online training and standard practice. BMJ Open 2018;8(12):e022292. [DOI: 10.1136/bmjopen-2018-022292] [PMC6318590] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Abbott 2009
- Abbott J-A, Klein B, Hamilton C, Rosenthal A. The impact of online resilience training for sales managers on wellbeing and performance. E-Journal of Applied Psychology 2009;5(1):89-95. [DOI: 10.7790/ejap.v5i1.145] [DOI] [Google Scholar]
Abel 2002a
- Abel MH. Humor, stress, and coping strategies. Humor: International Journal of Humor Research 2002;15(4):365–81. [DOI: 10.1515/humr.15.4.365] [DOI] [Google Scholar]
Abel 2002b
- Abel MH, Maxwell D. Humor and affective consequences of a stressful task. Journal of Social and Clinical Psychology 2002;21(2):165-90. [DOI: 10.1521/jscp.21.2.165.22516] [DOI] [Google Scholar]
Achor 2012
- Achor S. Positive intelligence; January-February 2012. Available at hbr.org/2012/01/positive-intelligence#.
Achor 2014
- Achor S. Happily orange after; Feburary 2014. Available at trainingmag.com/trgmag-article/happily-orange-after/.
Adams 2012
- Adams N. Skinner’s Walden Two: an anticipation of positive psychology. Review of General Psychology 2012;16(1):1–9. [DOI: 10.1037/a0026439] [DOI] [Google Scholar]
Ahern 2004
- Ahern J, Galea S, Fernandez WG, Koci B, Waldman R, Vlahov D. Gender, social support, and posttraumatic stress in postwar Kosovo. Journal of Nervous and Mental Disease 2004;192(11):762-70. [DOI: 10.1097/01.nmd.0000144695.02982.41] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ahmad 2010
- Ahmad S, Feder A, Lee EJ, Wang Y, Southwick SM, Schlackman E, et al. Earthquake impact in a remote South Asian population: psychosocial factors and posttraumatic symptoms. Journal of Traumatic Stress 2010;23(3):408-12. [DOI: 10.1002/jts.20535] [PMID: ] [DOI] [PubMed] [Google Scholar]
Al‐Yagon 2009
- Al-Yagon M, Margalit M. Positive and negative affect among mothers of children with intellectual disabilities. British Journal of Developmental Disabilities 2009;55 Pt 2(109):109-27. [DOI: 10.1179/096979509799103070] [DOI] [Google Scholar]
Alessandri 2007
- Alessandri G, Vecchio GM, Steca P, Caprara MG, Caprara GV. A revised version of Kremen and Block's Ego Resiliency Scale in an Italian sample. TPM - Testing, Psychometrics, Methodology in Applied Psychology 2007;14(3-4):165-83. [www.tpmap.org/wp-content/uploads/2014/11/14.3.4.pdf] [Google Scholar]
Alexander 2001
- Alexander DA, Klein S. Ambulance personnel and critical incidents: impact of accident and emergency work on mental health and emotional well-being. British Journal of Psychiatry 2001;178(1):76-81. [DOI: 10.1192/bjp.178.1.76] [PMID: ] [DOI] [PubMed] [Google Scholar]
Alim 2008
- Alim TN, Feder A, Graves RE, Wang Y, Weaver J, Westphal M, et al. Trauma, resilience, and recovery in a high-risk African-American population. American Journal of Psychiatry 2008;165(12):1566-75. [DOI: 10.1176/appi.ajp.2008.07121939] [PMID: ] [DOI] [PubMed] [Google Scholar]
Alipour 1993
- Alipour A, Noorbala A. Survey elementary of the validity and reliability of Oxford Happiness Inventory in Tehran University students. Journal of Thought and Behavior 1993;5(2):55-64. [No DOI or other object identifier available] [Google Scholar]
Allart 2013
- Allart P, Soubeyran P, Cousson-Gélie F. Are psychosocial factors associated with quality of life in patients with haematological cancer? A critical review of the literature. Psycho-oncology 2013;22(2):241-9. [DOI: 10.1002/pon.3026] [PMID: ] [DOI] [PubMed] [Google Scholar]
Andrew 2008
- Andrew ME, McCanlies EC, Burchfiel CM, Charles LE, Hartley TA, Fekedulegn D, et al. Hardiness and psychological distress in a cohort of police officers. International Journal of Emergency Mental Health 2008;10(2):137-47. [PMID: ] [PubMed] [Google Scholar]
Aniţei 2012
- Aniţei M, Chraif M, Chiriac G. Resilience to stress evidence-based improvements in integrative psychotherapy working groups. Procedia - Social and Behavioral Sciences 2012;33:1042-6. [DOI: 10.1016/j.sbspro.2012.01.281] [DOI] [Google Scholar]
Ano 2005
- Ano GG, Vasconcelles EB. Religious coping and psychological adjustment to stress: a meta-analysis. Journal of Clinical Psychology 2005;61(4):461-80. [DOI: 10.1002/jclp.20049] [PMID: ] [DOI] [PubMed] [Google Scholar]
Antonovsky 1979
- Antonovsky A. Health, Stress and Coping: New Perspectives on Mental and Physical Well-being. San Francisco (CA): Jossey-Bass, 1979. [Google Scholar]
Apolinário‐Hagen 2019 [pers comm]
- Apolinário-Hagen J. Trial status, focus of intervention and inclusion of healthcare students [personal communication]. Email to: A Kunzler 30 August 2019.
Arch 2019 [pers comm]
- Arch J. Potential inclusion of healthcare students [personal communication]. Email to: A Kunzler 16 September 2019.
Arnetz 1985
- Arnetz BB, Fjellner B, Eneroth P, Kallner A. Stress and psoriasis: psychoendocrine and metabolic reactions in psoriatic patients during standardized stressor exposure. Psychosomatic Medicine 1985;47(6):528–41. [DOI: 10.1097/00006842-198511000-00003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Aronson 1999
- Aronson E. The power of self-persuasion. American Psychologist 1999;54(11):875–84. [DOI: 10.1037/h0088188] [DOI] [Google Scholar]
Atal 2016
- Atal S, Cheng C. Socioeconomic health disparities revisited: coping flexibility enhances health-related quality of life for individuals low in socioeconomic status. Health and Quality of Life Outcomes 2016;14:7. [DOI: 10.1186/s12955-016-0410-1] [PMC4709869] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Atri 2007a
- Atri A. Role of Social Support, Hardiness and Acculturation as Predictors of Mental Health Among the International Students of Asian Indian Origin in Ohio [MS thesis]. Cincinnati (OH): University of Cincinnati, 2007. [DOI] [PubMed] [Google Scholar]
Atri 2007b
- Atri A, Sharma M, Cottrell R. Role of social support, hardiness, and acculturation as predictors of mental health among international students of Asian Indian origin. International Quarterly of Community Health Education 2007;27(1):59-73. [DOI: 10.2190/IQ.27.1.e] [PMID: ] [DOI] [PubMed] [Google Scholar]
Azad 2015
- Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ, et al. Sleep disturbances among medical students: a global perspective. Journal of Clinical Sleep Medicine 2015;11(1):69–74. [DOI: 10.5664/jcsm.4370] [PMC4265662] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bailey 2013
- Bailey A, Sharma M, Jubin M. The mediating role of social support, cognitive appraisal, and quality health care in black mothers' stress-resilience process following loss to gun violence. Violence and Victims 2013;28(2):233-47. [DOI: 10.1891/0886-6708.11-00151] [PMID: ] [DOI] [PubMed] [Google Scholar]
Balduzzi 2019
- Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evidence-Based Mental Health 2019;22(4):153–60. [DOI: 10.1136/ebmental-2019-300117] [DOI] [PMC free article] [PubMed] [Google Scholar]
Barry 2003
- Barry LC, Guo Z, Kerns RD, Duong BD, Reid MC. Functional self-efficacy and pain-related disability among older veterans with chronic pain in a primary care setting. Pain 2003;104(1-2):131-7. [DOI: 10.1016/S0304-3959(02)00471-2] [PMID: ] [DOI] [PubMed] [Google Scholar]
Barry 2019 [pers comm]
- Barry K. Subgroup outcome data of doctoral candidates in health professions [personal communication]. Email to: A Kunzler 3 September 2019.
Bartone 1989
- Bartone PT, Ursano RJ, Wright KM, Ingraham LH. The impact of a military air disaster on the health of assistance workers: a prospective study. Journal of Nervous and Mental Disease 1989;177(6):317-28. [DOI: 10.1097/00005053-198906000-00001] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bauer 2018
- Bauer A, Newbury-Birch D, Robalino S, Ferguson J, Wigham S. Is prevention better than cure? A systematic review of the effectiveness of well-being interventions for military personnel adjusting to civilian life. PLOS One 2018;13(5):e0190144. [DOI: 10.1371/journal.pone.0190144] [PMC5931793] [PROSPERO Registration number: CRD42015026341] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bauer‐Wu 2005
- Bauer-Wu S, Farran CJ. Meaning in life and psycho-spiritual functioning: a comparison of breast cancer survivors and healthy women. Journal of Holistic Nursing 2005;23(2):172-90. [DOI: 10.1177/0898010105275927] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bauman 2019 [pers comm]
- Bauman L. Openness to provide the data [personal communication]. Email to: A Kunzler 21 February 2019.
Beadel 2019 [pers comm]
- Beadel J. Potential inclusion of healthcare students [personal communication]. Email to: A Kunzler 29 September 2019.
Beck 1961
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry 1961;4(6):561-71. [DOI: 10.1001/archpsyc.1961.01710120031004] [PMID: ] [DOI] [PubMed] [Google Scholar]
Beck 1964
- Beck AT. Thinking and depression. II. Theory and therapy. Archives of General Psychiatry 1964;10(6):561-71. [DOI: 10.1001/archpsyc.1964.01720240015003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Beck 1976
- Beck AT. Cognitive Therapy and the Emotional Disorders. New York (NY): International Universities Press, 1976. [Google Scholar]
Beck 1987
- Beck AT, Steer RA. BDI: Beck Depression Inventory, Manual. San Antonio (TX): Psychological Corporation, 1987. [Google Scholar]
Beck 1993
- Beck AT, Steer RA. BAI: Beck Anxiety Inventory, Manual. San Antonio (TX): Psychological Corporation, 1993. [Google Scholar]
Beck 1996
- Beck AT, Steer RA, Brown GK. BDI-2: Beck Depression Inventory, Manual. San Antonio (TX): Psychological Corporation, 1996. [Google Scholar]
Beck 2011
- Beck JS. Cognitive Behavior Therapy: Basics and Beyond. 2nd edition. New York (NY): Guilford Press, 2011. [Google Scholar]
Bekki 2013
- Bekki JM, Smith ML, Bernstein BL, Harrison C. Effects of an online personal resilience training program for women in STEM doctoral programs. Journal of Women and Minorities in Science and Engineering 2013;19(1):17-35. [DOI: 10.1615/JWomenMinorScienEng.2013005351] [DOI] [Google Scholar]
Belingheri 2020
Bengel 2009
- Bengel J, Meinders-Lücking F, Rottmann N. Schutzfaktoren bei Kindern und Jugendlichen: Stand der Forschung zu Psychosozialen Schutzfaktoren für Gesundheit. Köln: BzgA, 2009. [Google Scholar]
Bengel 2012
- Bengel J, Lyssenko L. Resilienz und Psychologische Schutzfaktoren im Erwachsenenalter: Stand der Forschung zu psychologischen Schutzfaktoren von Gesundheit im Erwachsenenalter. Köln: BzgA, 2012. [Google Scholar]
Benjamin 2011
- Benjamin CL, Puleo CM, Settipani CA, Brodman DM, Edmunds JM, Cummings CM, et al. History of cognitive-behavioral therapy in youth. Child and Adolescent Psychiatric Clinics of North America 2011;20(2):179-89. [DOI: 10.1016/j.chc.2011.01.011] [PMC3077930] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Berk 2009
- Berk M, Parker G. The elephant on the couch: side-effects of psychotherapy. Australian and New Zealand Journal of Psychiatry 2009;43(9):787–94. [DOI: 10.1080/00048670903107559] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bernas 2000
- Bernas KH, Major DA. Contributors to stress resistance: testing a model of women's work-family conflict. Psychology of Women Quarterly 2000;24(2):170-8. [DOI: 10.1111/j.1471-6402.2000.tb00198.x] [DOI] [Google Scholar]
Besser 2014
- Besser A, Weinberg M, Zeigler-Hill V, Neria Y. Acute symptoms of posttraumatic stress and dissociative experiences among female Israeli civilians exposed to war: the roles of intrapersonal and interpersonal sources of resilience. Journal of Clinical Psychology 2014;70(12):1227-39. [DOI: 10.1002/jclp.22083] [PMID: ] [DOI] [PubMed] [Google Scholar]
Betz 1996
- Betz NE, Klein KL, Taylor KM. Evaluation of a short form of the Career Decision-Making Self-Efficacy Scale. Journal of Career Assessment 1996;4(1):47–57. [DOI: 10.1177/106907279600400103] [DOI] [Google Scholar]
Bjørkløf 2013
- Bjørkløf GH, Engedal K, Selbæk G, Kouwenhoven SE, Helvik AS. Coping and depression in old age: a literature review. Dementia and Geriatric Cognitive Disorders 2013;35(3-4):121-54. [DOI: 10.1159/000346633] [PMID: ] [DOI] [PubMed] [Google Scholar]
Blackburn 2015
- Blackburn L, Owens GP. The effect of self efficacy and meaning in life on posttraumatic stress disorder and depression severity among veterans. Journal of Clinical Psychology 2015;71(3):219-28. [DOI: 10.1002/jclp.22133] [PMID: ] [DOI] [PubMed] [Google Scholar]
Block 1996
- Block J, Kremen AM. IQ and ego-resiliency: conceptual and empirical connections and separateness. Journal of Personality and Social Psychology 1996;70(2):349-61. [DOI: 10.1037//0022-3514.70.2.349] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bonanno 2004
- Bonanno GA, Papa A, Lalande K, Westphal M, Coifman K. The importance of being flexible: the ability to both enhance and suppress emotional expression predicts long-term adjustment. Psychological Science 2004;15(7):482-7. [DOI: 10.1111/j.0956-7976.2004.00705.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bonanno 2011
- Bonanno GA, Pat-Horenczyk R, Noll J. Coping flexibility and trauma: the Perceived Ability to Cope With Trauma (PACT) scale. Psychological Trauma: Theory, Research, Practice, and Policy 2011;3(2):117-29. [DOI: 10.1037/a0020921] [DOI] [Google Scholar]
Bonanno 2013
- Bonanno GA, Diminich ED. Annual Research Review: positive adjustment to adversity--trajectories of minimal-impact resilience and emergent resilience. Journal of Child Psychology and Psychiatry 2013;54(4):378-401. [DOI: 10.1111/jcpp.12021] [PMC3606676] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bonanno 2015
- Bonanno GA, Romero SA, Klein SI. The temporal elements of psychological resilience: an integrative framework for the study of individuals, families, and communities. Psychological Inquiry 2015;26(2):139–69. [DOI: 10.1080/1047840X.2015.992677] [DOI] [Google Scholar]
Bookwala 2014
- Bookwala J. Spouse health status, depressed affect, and resilience in mid and late life: a longitudinal study. Developmental Psychology 2014;50(4):1241-9. [DOI: 10.1037/a0035124] [PMID: ] [DOI] [PubMed] [Google Scholar]
Brandt 1981
- Brandt PA, Weinert C. The PRQ--a social support measure. Nursing Research 1981;30(5):277-80. [PMID: ] [PubMed] [Google Scholar]
Bromley 2006
- Bromley E, Johnson JG, Cohen P. Personality strengths in adolescence and decreased risk of developing mental health problems in early adulthood. Comprehensive Psychiatry 2006;47(4):315-24. [DOI: 10.1016/j.comppsych.2005.11.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Brooks 2003
- Brooks MV. Health-related hardiness and chronic illness: a synthesis of current research. Nursing Forum 2003;38(3):11-20. [DOI: 10.1111/j.0029-6473.2003.00011.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Buddeberg‐Fischer 2006
- Buddeberg-Fischer B, Herta KD. Formal mentoring programmes for medical students and doctors--a review of the Medline literature. Medical Teacher 2006;28(3):248-57. [DOI: 10.1080/01421590500313043] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bunevicius 2008
- Bunevicius A, Katkute A, Bunevicius RS. Symptoms of anxiety and depression in medical students and in humanities students: relationship with big-five personality dimensions and vulnerability to stress. International Journal of Social Psychiatry 2008;54(6):494–501. [DOI: 10.1177/0020764008090843] [PMID: ] [DOI] [PubMed] [Google Scholar]
Burton 2012
- Burton CL, Yan OH, Pat-Horenczyk R, Chan IS, Ho S, Bonanno GA. Coping flexibility and complicated grief: a comparison of American and Chinese samples. Depression and Anxiety 2012;29(1):16-22. [DOI: 10.1002/da.20888] [PMC3242921] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Butler 2009
- Butler LD, Koopman C, Azarow J, Blasey CM, Magdalene JC, DiMiceli S, et al. Psychosocial predictors of resilience after the September 11, 2001 terrorist attacks. Journal of Nervous and Mental Disease 2009;197(4):266-73. [DOI: 10.1097/NMD.0b013e31819d9334] [PMID: ] [DOI] [PubMed] [Google Scholar]
Caldwell 2005
- Caldwell DM, Ades AE, Higgins JP. Simultaneous comparison of multiple treatments combining direct and indirect evidence. BMJ 2005;331(7521):897-900. [DOI: 10.1136/bmj.331.7521.897] [PMC1255806] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell‐Sills 2007
- Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): validation of a 10-item measure of resilience. Journal of Traumatic Stress 2007;20(6):1019-28. [DOI: 10.1002/jts.20271] [PMID: ] [DOI] [PubMed] [Google Scholar]
Carver 1997
- Carver CS. You want to measure coping but your protocol's too long: consider the brief COPE. International Journal of Behavioral Medicine 1997;4(1):92-100. [DOI: 10.1207/s15327558ijbm0401_6] [PMID: ] [DOI] [PubMed] [Google Scholar]
Carver 1998
- Carver CS. Resilience and thriving: issues, models, and linkages. Journal of Social Issues 1998;54(2):245–66. [DOI: 10.1111/0022-4537.641998064] [DOI] [Google Scholar]
Carver 2010
- Carver CS, Scheier MF, Segerstrom SC. Optimism. Clinical Psychology Review 2010;30(7):879-89. [DOI: 10.1016/j.cpr.2010.01.006] [NIHMS174994] [PMC4161121] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Casale 2013
- Casale M, Wild L. Effects and processes linking social support to caregiver health among HIV/AIDS-affected carer-child dyads: a critical review of the empirical evidence. AIDS and Behavior 2013;17(5):1591-611. [DOI: 10.1007/s10461-012-0275-1] [PMID: ] [DOI] [PubMed] [Google Scholar]
Castro 2015
- Castro A, García-Palacios A, García-Campayo J, Mayoral F, Botella C, García-Herrera JM, et al. Efficacy of low-intensity psychological intervention applied by ICTs for the treatment of depression in primary care: a controlled trial. BMC Psychiatry 2015;15:106. [DOI: 10.1186/s12888-015-0475-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cecil 2014
- Cecil J, McHale C, Hart J, Laidlaw A. Behaviour and burnout in medical students. Medical Education Online 2014;19:25209. [DOI: 10.3402/meo.v19.25209] [PMC4145104] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chaimani 2019
- Chaimani A, Caldwell DM, Li T, Higgins JP, Salanti G. Chapter 11: Undertaking network meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Chan 2013a
- Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Annals of Internal Medicine 2013;158(3):200-7. [DOI: 10.7326/0003-4819-158-3-201302050-00583] [PMC5114123] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chan 2013b
- Chan AW, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. [DOI: 10.1136/bmj.e7586] [PMC3541470] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chang 2012
- Chang E, Eddins-Folensbee F, Coverdale J. Survey of the prevalence of burnout, stress, depression, and the use of supports by medical students at one school. Academic Psychiatry 2012;36(3):177–82. [DOI: 10.1176/appi.ap.11040079] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chen 2004
- Chen G, Goddard TG, Casper WJ. Examination of the relationships among general and work-specific self-evaluations, work-related control beliefs, and job attitudes. Applied Psychology: An International Review 2004;53(3):349-70. [DOI: 10.1111/j.1464-0597.2004.00175.x] [DOI] [Google Scholar]
Cheng 2014
- Cheng C, Lau HP, Chan MP. Coping flexibility and psychological adjustment to stressful life changes: a meta-analytic review. Psychological Bulletin 2014;140(6):1582-607. [DOI: 10.1037/a0037913] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chesney 2003
- Chesney MA, Chambers DB, Taylor JM, Johnson LM, Folkman S. Coping effectiveness training for men living with HIV: results from a randomized clinical trial testing a group-based intervention. Psychosomatic Medicine 2003;65(6):1038-46. [DOI: 10.1097/01.psy.0000097344.78697.ed] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chiang 2012
- Chiang YM, Chang Y. Stress, depression, and intention to leave among nurses in different medical units: implications for healthcare management/nursing practice. Health Policy 2012;108(2-3):149-57. [DOI: 10.1016/j.healthpol.2012.08.027] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chmitorz 2018
- Chmitorz A, Kunzler A, Helmreich I, Tüscher O, Kalisch R, Kubiak T, et al. Intervention studies to foster resilience - a systematic review and proposal for a resilience framework in future intervention studies. Clinical Psychology Review 2018;59:78-100. [DOI: 10.1016/j.cpr.2017.11.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cicchetti 2012
- Cicchetti D, Rogosch FA. Gene × environment interaction and resilience: effects of child maltreatment and serotonin, corticotropin releasing hormone, dopamine, and oxytocin genes. Development and Psychopathology 2012;24(2):411-27. [DOI: 10.1017/S0954579412000077] [PMC3684053] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cochrane Community 2020
- Glossary. community.cochrane.org/glossary (accessed 15 June 2020).
Cohen 1983a
- Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology 1983;13(2):99-125. [DOI: 10.1111/j.1559-1816.1983.tb02325.x] [DOI] [Google Scholar]
Cohen 1983b
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior 1983;24(4):385-96. [DOI: 10.2307/2136404] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cohen 1988a
- Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan, S, Oskamp, S, editors(s). The Social Psychology of Health: Claremont Symposium on Applied Social Psychology. Newbury Park (CA): Sage Publications Inc, 1988:31-67. [Google Scholar]
Cohen 1988b
- Cohen J. Statistical Power Analysis in the Behavioral Sciences. 2nd edition. Hillsdale (NJ): Lawrence Erlbaum Associates, Inc, 1988. [Google Scholar]
Cohen 2003
- Cohen O, Savaya R. Sense of coherence and adjustment to divorce among Muslim Arab citizens of Israel. European Journal of Personality 2003;17(4):309-26. [DOI: 10.1002/per.493] [DOI] [Google Scholar]
Cohen 2006
- Cohen S, Alper CM, Doyle WJ, Treanor JJ, Turner RB. Positive emotional style predicts resistance to illness after experimental exposure to rhinovirus or influenza a virus. Psychosomatic Medicine 2006;68(6):809-15. [DOI: 10.1097/01.psy.0000245867.92364.3c] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cohen 2012
- Cohen S, Janicki-Deverts D. Who's stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. Journal of Applied Social Psychology 2012;42(6):1320–34. [DOI: 10.1111/j.1559-1816.2012.00900.x] [DOI] [Google Scholar]
Colloca 2008
- Colloca L, Sigaudo M, Benedetti F. The role of learning in nocebo and placebo effects. Pain 2008;136(1-2):211-8. [DOI: 10.1016/j.pain.2008.02.006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Compton 2008
- Compton MT, Carrera J, Frank E. Stress and depressive symptoms/dysphoria among US medical students: results from a large, nationally representative survey. Journal of Nervous and Mental Disease 2008;196(12):891-7. [DOI: 10.1097/NMD.0b013e3181924d03] [PMID: 19077856 ] [DOI] [PubMed] [Google Scholar]
Connor 2003
- Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety 2003;18(2):76-82. [DOI: 10.1002/da.10113] [PMID: ] [DOI] [PubMed] [Google Scholar]
Connor 2006
- Connor KM, Zhang W. Resilience: determinants, measurement, and treatment responsiveness. CNS Spectrums 2006;11(Suppl S12):5-12. [DOI: 10.1017/S1092852900025797] [DOI] [PubMed] [Google Scholar]
CRD 2009
- Centre for Reviews and Dissemination (CRD). Systematic Reviews: CRD's Guidance for Undertaking Reviews in Health Care. York (NYS): Univesity of York, 2009. [Google Scholar]
Cruz 2016
- Cruz JP, Colet PC, Qubeilat H, Al-Otaibi J, Coronel EI, Suminta RC. Religiosity and health-related quality of life: a cross-sectional study on Filipino Christian hemodialysis patients. Journal of Religion and Health 2016;55(3):895-908. [DOI: 10.1007/s10943-015-0103-9] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cuijpers 2017
- Cuijpers P, Kleiboer A, Karyotaki E, Riper H. Internet and mobile interventions for depression: opportunities and challenges. Depression and Anxiety 2017;34(7):596-602. [DOI: 10.1002/da.22641] [PMID: 28471479 ] [DOI] [PubMed] [Google Scholar]
Cushway 1996
- Cushway D, Tyler PA, Nolan P. Development of a stress scale for mental health professionals. British Journal of Clinical Psychology 1996;35(2):279-95. [DOI: 10.1111/j.2044-8260.1996.tb01182.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cutrona 1987
- Cutrona CE, Russell DW. The provisions of social relationships and adaptation to stress. In: Jones WH, Perlman D, editors(s). Advances in Personal Relationships. Vol. 1. Greenwich (CT): JAI Press, 1987:37-67. [Google Scholar]
Dawson 2019
- Dawson AF, Brown WW, Anderson J, Datta B, Donald JN, Hong K, et al. Mindfulness-based interventions for university students: a systematic review and meta-analysis of randomised controlled trials. Applied Psychololgy. Health and Well Being 2019 Nov 19 [Epub ahead of print]. [DOI: 10.1111/aphw.12188] [PMID: ] [DOI] [PubMed]
Deady 2017
- Deady M, Choi I, Calvo RA, Glozier N, Christensen H, Harvey SB. eHealth interventions for the prevention of depression and anxiety in the general population: a systematic review and meta-analysis. BMC Psychiatry 2017;17(1):310. [DOI: 10.1186/s12888-017-1473-1] [PMC5576307 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2019
- Deeks JJ, Higgins JP, Altman DG (editors). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Demerouti 2010
- Demerouti E, Mostert K, Bakker AB. Burnout and work engagement: a thorough investigation of the independency of both constructs. Journal of Occupational Health Psychology 2010;15(3):209-22. [DOI: 10.1037/a0019408] [PMID: ] [DOI] [PubMed] [Google Scholar]
Derogatis 1994
- Derogatis LR. SCL-90-R Symptom Checklist-90-R: Administration, Scoring, & Procedures Manual. 3rd edition. Minneapolis (MN): National Computer Systems Inc, 1994. [Google Scholar]
DeRoon‐Cassini 2010
- DeRoon-Cassini TA, Mancini AD, Rusch MD, Bonanno G. Psychopathology and resilience following traumatic injury: a latent growth mixture model analysis. Rehabilitation Psychology 2010;55(1):1-11. [DOI: 10.1037/a0018601] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dias 2010
- Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Statistics in Medicine 2010;29(7-8):932-44. [DOI: 10.1002/sim.3767] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dias 2015
- Dias R, Santos RL, Sousa MF, Nogueira MM, Torres B, Belfort T, et al. Resilience of caregivers of people with dementia: a systematic review of biological and psychosocial determinants. Trends in Psychiatry and Psychotherapy 2015;37(1):12-9. [DOI: 10.1590/2237-6089-2014-0032] [PMID: ] [DOI] [PubMed] [Google Scholar]
Diener 1985
- Diener E, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. Journal of Personality Assessment 1985;49(1):71-5. [DOI: 10.1207/s15327752jpa4901_13] [PMID: ] [DOI] [PubMed] [Google Scholar]
Do 2008
- Do AM, Rupert AV, Wolford G. Evaluations of pleasurable experiences: the peak-end rule. Psychonomic Bulletin & Review 2008;15(1):96-8. [DOI: 10.3758/pbr.15.1.96] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dobkin 2013
- Dobkin PL, Hutchinson TA. Teaching mindfulness in medical school: where are we now and where are we going? Medical Education 2013;47(8):768-79. [DOI: 10.1111/medu.12200] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dolan 2006
- Dolan CA, Adler AB. Military hardiness as a buffer of psychological health on return from deployment. Military Medicine 2006;171(2):93-8. [DOI: 10.7205/milmed.171.2.93] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dolbier 2000
- Dolbier CL, Steinhardt MA. The development and validation of the Sense of Support Scale. Behavioral Medicine 2000;25(4):169-79. [DOI: 10.1080/08964280009595746] [PMID: ] [DOI] [PubMed] [Google Scholar]
Donner 1998
- Donner GJ. Taking control of your future: the time is now. In: Donner GJ, Wheeler MM, editors(s). Taking Control of Your Career and Your Future: For Nurses by Nurses. Ottawa (ON): Canadian Nurses Association, 1998:3-11. [Google Scholar]
Downs 1998
- Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health 1998;52(6):377–84. [DOI: 10.1136/jech.52.6.377] [PMC1756728] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Duckworth 2007
- Duckworth AL, Peterson C, Matthews MD, Kelly DR. Grit: perseverance and passion for long-term goals. Journal of Personality and Social Psychology 2007;92(6):1087-101. [DOI: 10.1037/0022-3514.92.6.1087] [PMID: ] [DOI] [PubMed] [Google Scholar]
Duits 1997
- Duits AA, Boeke S, Taams MA, Passchier J, Erdman RA. Prediction of quality of life after coronary artery bypass graft surgery: a review and evaluation of multiple, recent studies. Psychosomatic Medicine 1997;59(3):257-68. [DOI: 10.1097/00006842-199705000-00009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dyrbye 2006
- Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among US and Canadian medical students. Academic Medicine 2006;81(4):354–73. [DOI: 10.1097/00001888-200604000-00009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dyrbye 2009
- Dyrbye LN, Thomas MR, Harper W, Massie FS Jr, Power DV, Eacker A, et al. The learning environment and medical student burnout: a multicentre study. Medical Education 2009;43(3):274-82. [DOI: 10.1111/j.1365-2923.2008.03282.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dyrbye 2010
- Dyrbye LN, Power DV, Massie FS, Eacker A, Harper W, Thomas MR, et al. Factors associated with resilience to and recovery from burnout: a prospective, multi-institutional study of US medical students. Medical Education 2010;44(10):1016-26. [DOI: 10.1111/j.1365-2923.2010.03754.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dyrbye 2011
- Dyrbye LN, Harper W, Durning SJ, Moutier C, Thomas MR, Massie FS Jr, et al. Patterns of distress in US medical students. Medical Teacher 2011;33(10):834-9. [DOI: 10.3109/0142159X.2010.531158] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dyrbye 2016
- Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Medical Education 2016;50(1):132-49. [DOI: 10.1111/medu.12927] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dörfel 2008
- Dörfel D, Rabe S, Karl A. Coping strategies in daily life as protective and risk factors for post traumatic stress in motor vehicle accident survivors. Journal of Loss and Trauma 2008;13(5):422-40. [DOI: 10.1080/15325020701742136] [DOI] [Google Scholar]
Earvolino‐Ramirez 2007
- Earvolino-Ramirez M. Resilience: a concept analysis. Nursing Forum 2007;42(2):73-82. [DOI: 10.1111/j.1744-6198.2007.00070.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Edwards 2010
- Edwards D, Burnard P, Bennett K, Hebden U. A longitudinal study of stress and self-esteem in student nurses. Nurse Education Today 2010;30(1):78-84. [DOI: 10.1016/j.nedt.2009.06.008] [PMID: ] [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629-34. [DOI: 10.1136/bmj.315.7109.629] [PMC2127453] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Eley 2014
- Eley DS, Stallman H. Where does medical education stand in nurturing the 3Rs in medical students: responsibility, resilience and resolve? Medical Teacher 2014;36(10):835-7. [DOI: 10.3109/0142159X.2014.917159] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ellis 1957
- Ellis A. Rational psychotherapy and individual psychology. Journal of Individual Psychology 1957;13:38-44. [pdfs.semanticscholar.org/552c/e878498ce8e8c2b57ff62144538f1ac3d84c.pdf] [Google Scholar]
Ellis 1975
- Ellis A, Harper RA. A New Guide to Rational Living. Chatsworth (CA): Wilshire Book Company, 1975. [Google Scholar]
Ellis 1991
- Ellis A. The revised ABC’s of rational-emotive therapy (RET). Journal of Rational-Emotive and Cognitive-Behavior Therapy 1991;9(3):139–72. [DOI: 10.1007/BF01061227] [DOI] [Google Scholar]
Enck 2008
- Enck P, Benedetti F, Schedlowski M. New insights into the placebo and nocebo responses. Neuron 2008;59(2):195–206. [DOI: 10.1016/j.neuron.2008.06.030] [PMID: ] [DOI] [PubMed] [Google Scholar]
Eriksson 2006
- Eriksson M, Lindström B. Antonovsky's Sense Of Coherence scale and the relation with health: a systematic review. Journal of Epidemiology and Community Health 2006;60(5):376-81. [DOI: 10.1136/jech.2005.041616] [PMC2563977] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Erogul 2018 [pers comm]
- Erogul M. Number of participants randomised and analysed in total and each group at each time point [personal communication]. Email to: A Kunzler 26 May 2018.
Eschleman 2010
- Eschleman KJ, Bowling NA, Alarcon GM. A meta-analytic examination of hardiness. International Journal of Stress Management 2010;17(4):277-307. [DOI: 10.1037/a0020476.supp] [DOI] [Google Scholar]
Evans 2000
- Evans C, Mellor-Clark J, Margison F, Barkham M, Audin K, Connell J, et al. CORE: Clinical Outcomes in Routine Evaluation. Journal of Mental Health 2000;9(3):247–55. [DOI: 10.1080/jmh.9.3.247.255] [DOI] [Google Scholar]
Evans 2004
- Evans W, Kelly B. Pre-registration diploma student nurse stress and coping measures. Nurse Education Today 2004;24:473–82. [DOI: 10.1016/j.nedt.2004.05.004] [DOI] [PubMed] [Google Scholar]
Farber 2000
- Farber EW, Schwartz JA, Schaper PE, Moonen DJ, McDaniel JS. Resilience factors associated with adaptation to HIV disease. Psychosomatics 2000;41(2):140-6. [DOI: 10.1176/appi.psy.41.2.140] [PMID: ] [DOI] [PubMed] [Google Scholar]
Farber 2003
- Farber EW, Mirsalimi H, Williams KA, McDaniel JS. Meaning of illness and psychological adjustment to HIV/AIDS. Psychosomatics 2003;44(6):485-91. [DOI: 10.1176/appi.psy.44.6.485] [PMID: ] [DOI] [PubMed] [Google Scholar]
Farchi 2010
- Farchi M, Gidron Y. The effects of "psychological inoculation" versus ventilation on the mental resilience of Israeli citizens under continuous war stress. Journal of Nervous and Mental Disease 2010;198(5):382-4. [DOI: 10.1097/NMD.0b013e3181da4b67] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fares 2016
- Fares J, Al Tabosh H, Saadeddin Z, El Mouhayyar C, Aridi H. Stress, burnout and coping strategies in preclinical medical students. North American Journal of Medical Sciences 2016;8(2):75-81. [DOI: 10.4103/1947-2714.177299] [PMC4791902] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Faul 2007
- Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods 2007;39(2):175-91. [DOI: 10.3758/BF03193146] [PMID: ] [DOI] [PubMed] [Google Scholar]
Feder 2011
- Feder A, Charney D, Collins K. Neurobiology of resilience. In: Southwick SM, Litz BT, Charney D, Friedman MJ, editors(s). Resilience and Mental Health: Challenges Across the Lifespan. Cambridge (UK): Cambridge University Press, 2011:1-29. [Google Scholar]
Feder 2013
- Feder A, Ahmad S, Lee EJ, Morgan JE, Singh R, Smith BW, et al. Coping and PTSD symptoms in Pakistani earthquake survivors: purpose in life, religious coping and social support. Journal of Affective Disorders 2013;147(1-3):156-63. [DOI: 10.1016/j.jad.2012.10.027] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fernández‐Lansac 2012
- Fernández-Lansac V, Crespo López M, Cáceres R, Rodríguez-Poyo M. Resilience in caregivers of patients with dementia: a preliminary study. Revista Española de Geriatría y Gerontología 2012;47(3):102-9. [DOI: 10.1016/j.regg.2011.11.004] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ferring 1996
- Ferring D, Filipp SH. Measurement of self-esteem: findings on reliability, validity, and stability of the Rosenberg scale [Messung des selbstwertgefühls: befunde zu reliabilität, validität und stabilität der Rosenberg skala]. Diagnostica 1996;42(3):284–92. [psycnet.apa.org/record/1996-94139-005] [Google Scholar]
First 2018
- First J, First NL, Houston JB. Resilience and Coping Intervention (RCI): a group intervention to foster college student resilience. Social Work with Groups 2018;41(3):198-210. [DOI: 10.1080/01609513.2016.1272032] [DOI] [Google Scholar]
Fletcher 2013
- Fletcher D, Sarkar M. Psychological resilience: a review and critique of definitions, concepts, and theory. European Psychologist 2013;18(1):12-23. [DOI: 10.1027/1016-9040/a000124] [DOI] [Google Scholar]
Folkman 1988
- Folkman S, Lazarus RS. Manual for the Ways of Coping Questionnaire. Palo Alto (CA): Consulting Psychologists Press Inc, 1988. [Google Scholar]
Forgeard 2012
- Forgeard MJ, Seligman ME. Seeing the glass half full: a review of the causes and consequences of optimism. Pratiques Psychologiques 2012;18(2):107-20. [DOI: 10.1016/j.prps.2012.02.002] [DOI] [Google Scholar]
Forstmeier 2009
- Forstmeier S, Kuwert P, Spitzer C, Freyberger HJ, Maercker A. Posttraumatic growth, social acknowledgment as survivors, and sense of coherence in former German child soldiers of World War II. American Journal of Geriatric Psychiatry 2009;17(12):1030-9. [DOI: 10.1097/JGP.0b013e3181ab8b36] [PMID: ] [DOI] [PubMed] [Google Scholar]
Foster 2015
- Foster K, McCloughen A, Delgado C, Kefalas C, Harkness E. Emotional intelligence education in pre-registration nursing programmes: an integrative review. Nurse Education Today 2015;35(3):510–7. [DOI: 10.1016/j.nedt.2014.11.009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Foster 2018
- Foster K, Fethney J, Kozlowski D, Fois R, Reza F, McCloughen A. Emotional intelligence and perceived stress of Australian pre-registration healthcare students: a multi-disciplinary cross-sectional study. Nurse Education Today 2018;66:51-6. [DOI: 10.1016/j.nedt.2018.04.001] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fredrickson 2003
- Fredrickson BL, Tugade MM, Waugh CE, Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. Journal of Personality and Social Psychology 2003;84(2):365–76. [DOI: 10.1037//0022-3514.84.2.365] [NIHMS141511] [PMC2755263] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fredrickson 2008
- Fredrickson BL, Cohn MA, Coffey KA, Pek J, Finkel SM. Open hearts build lives: Positive emotions, induced through loving-kindness meditation, build consequential personal resources. Journal of Personality and Social Psychology 2008;95(5):1045–62. [DOI: 10.1037/a0013262] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Frei 2010
- Frei E, Stamm M, Buddeberg-Fischer B. Mentoring programs for medical students—a review of the PubMed literature 2000–2008. BMC Medical Education 2010;10:32. [DOI: 10.1186/1472-6920-10-32] [PMC2881011] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fresco 2006
- Fresco DM, Alloy LB, Reilly–Harrington N. Association of attributional style for negative and positive events and the occurrence of life events with depression and anxiety. Journal of Social and Clinical Psychology 2006;25(10):1140-59. [DOI: 10.1521/jscp.2006.25.10.1140] [DOI] [Google Scholar]
Friborg 2003
- Friborg O, Hjemdal O, Rosenvinge JH, Martinussen M. A new rating scale for adult resilience: what are the central protective resources behind healthy adjustment? International Journal of Methods in Psychiatric Research 2003;12(2):65-76. [DOI: 10.1002/mpr.143] [PMC6878238] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Friborg 2005
- Friborg O, Barlaug D, Martinussen M, Rosenvinge JH, Hjemdal O. Resilience in relation to personality and intelligence. International Journal of Methods in Psychiatric Research 2005;14(1):29-42. [DOI: 10.1002/mpr.15] [PMC6878482] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Frommberger 1999
- Frommberger U, Stieglitz RD, Straub S, Nyberg E, Schlickewei W, Kuner E, et al. The concept of "sense of coherence" and the development of posttraumatic stress disorder in traffic accident victims. Journal of Psychosomatic Research 1999;46(4):343-8. [DOI: 10.1016/S0022-3999(98)00117-2] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fuller‐Iglesias 2008
- Fuller-Iglesias H, Sellars B, Antonucci TC. Resilience in old age: social relations as a protective factor. Research in Human Development 2008;5(3):181-93. [DOI: 10.1080/15427600802274043] [DOI] [Google Scholar]
Gable 2006
- Gable SL, Gonzaga GC, Strachman A. Will you be there for me when things go right? Supportive responses to positive event disclosures. Journal of Personality and Social Psychology 2006;91(5):904-17. [DOI: 10.1037/0022-3514.91.5.904] [PMID: ] [DOI] [PubMed] [Google Scholar]
Galante 2019 [pers comm]
- Galante J. Subgroup data for students in health professions [personal communication]. Email to: A Kunzler 6 August 2019.
Galatzer‐Levy 2012
- Galatzer-Levy IR, Burton CL, Bonanno GA. Coping flexibility, potentially traumatic life events, and resilience: a prospective study of college student adjustment. Journal of Social and Clinical Psychology 2012;31(6):542-67. [DOI: 10.1521/jscp.2012.31.6.542] [DOI] [Google Scholar]
Gao 2019
- Gao L, Peranson J, Nyhof-Young J, Kapoor E, Rezmovitz J. The role of "improv" in health professional learning: a scoping review. Medical Teacher 2019;41(5):561-8. [DOI: 10.1080/0142159X.2018.1505033] [PMID: ] [DOI] [PubMed] [Google Scholar]
García‐Herrera 2011
- García-Herrera JM, Nogueras-Morillas V, Muñoz-Cobos F, Morales-Asensio JM. Guía de Práctica Clínica para el Tratamiento de la Depresión en Atención Primaria [Clinical Practice Guide on the Treatment of Depression in Primary Care]. Distrito Sanitario Málaga UGC Salud Mental Hospital Regional Universitario “Carlos Haya”. Málaga: GAEDAP, 2011. [Google Scholar]
Gazzaz 2018
- Gazzaz ZJ, Baig M, Al Alhendi BS, Al Suliman MM, Al Alhendi AS, Al-Grad MS, et al. Perceived stress, reasons for and sources of stress among medical students at Rabigh Medical College, King Abdulaziz University, Jeddah, Saudi Arabia. BMC Medical Education 2018;18(1):29. [DOI: 10.1186/s12909-018-1133-2] [PMC5824476] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gerson 2018a [pers comm]
- Gerson M. Means and SDs for both groups [personal communication]. Email to: A Kunzler 13 August 2018.
Gerson 2018b [pers comm]
- Gerson M. Means and SDs for study 1 not available [personal communication]. Email to: A Kunzler 13 August 2018.
Geschwind 2010
- Geschwind N, Peeters F, Jacobs N, Delespaul P, Derom C, Thiery E, et al. Meeting risk with resilience: high daily life reward experience preserves mental health. Acta Psychiatrica Scandinavica 2010;122(2):129-38. [DOI: 10.1111/j.1600-0447.2009.01525.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Geschwind 2011
- Geschwind N, Peeters F, Drukker M, Van Os J, Wichers M. Mindfulness training increases momentary positive emotions and reward experience in adults vulnerable to depression: a randomized controlled trial. Journal of Consulting and Clinical Psychology 2011;79(5):618-28. [DOI: 10.1037/a0024595] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gilmartin 2017
- Gilmartin H, Goyal A, Hamati MC, Mann J, Saint S, Chopra V. Brief mindfulness practices for healthcare providers - a systematic literature review. American Journal of Medicine 2017;130(10):1219.e1-17. [DOI: 10.1016/j.amjmed.2017.05.041] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gloria 2016
- Gloria CT, Steinhardt MA. Relationships among positive emotions, coping, resilience and mental health. Stress & Health 2016;32(2):145-56. [DOI: 10.1002/smi.2589] [PMID: ] [DOI] [PubMed] [Google Scholar]
Goldstein 2019 [pers comm]
- Goldstein M. Information about resilience as primary aim of the study and inclusion of students in health professions [personal communication]. Email to: A Kunzler 1 August 2019.
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime) GRADEpro GDT. McMaster University (developed by Evidence Prime), accessed 4 May 2020. Available at www.gradepro.org.
Griffiths 2019
- Griffiths A, Royse D, Murphy A, Starks S. Self-care practice in social work education: a systematic review of interventions. Journal of Social Work Education 2019;55(1):102-14. [DOI: 10.1080/10437797.2018.1491358] [DOI] [Google Scholar]
Grolimund 2008
- Grolimund F. Effektiv Denken - Effektiv Lernen. Morrisville (NC): Lulu Press, 2008. [Google Scholar]
Grossman 2004
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: a meta-analysis. Journal of Psychosomatic Research 2004;57(1):35-43. [DOI: 10.1016/S0022-3999(03)00573-7] [PMID: ] [DOI] [PubMed] [Google Scholar]
Grote 2007
- Grote NK, Bledsoe SE, Larkin J, Lemay EP Jr, Brown C. Stress exposure and depression in disadvantage women: the protective effects of optimism and perceived control. Social Work Research 2007;31(1):19-33. [DOI: 10.1093/swr/31.1.19] [DOI] [Google Scholar]
Guardino 2014
- Guardino CM, Schetter CD. Coping during pregnancy: a systematic review and recommendations. Health Psychology Review 2014;8(1):70-94. [DOI: 10.1080/17437199.2012.752659] [PMC3904449] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Guest 2015
- Guest R, Craig A, Nicholson Perry K, Tran Y, Ephraums C, Hales A, et al. Resilience following spinal cord injury: a prospective controlled study investigating the influence of the provision of group cognitive behavior therapy during inpatient rehabilitation. Rehabilitation Psychology 2015;60(4):311-21. [DOI: 10.1037/rep0000052] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011a
- Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso-Coello P, et al. GRADE guidelines: 4. Rating the quality of evidence--study limitations (risk of bias). Journal of Clinical Epidemiology 2011;64(4):407-15. [DOI: 10.1016/j.jclinepi.2010.07.017] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011b
- Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, et al. GRADE guidelines: 5. Rating the quality of evidence--publication bias. Journal of Clinical Epidemiology 2011;64(12):1277-82. [DOI: 10.1016/j.jclinepi.2011.01.011] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011c
- Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence--imprecision. Journal of Clinical Epidemiology 2011;64(12):1283-93. [DOI: 10.1016/j.jclinepi.2011.01.012] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011d
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence--inconsistency. Journal of Clinical Epidemiology 2011;64(12):1294-1302. [DOI: 10.1016/j.jclinepi.2011.03.017] [PMID: ] [DOI] [PubMed] [Google Scholar]
Guyatt 2011e
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 8. Rating the quality of evidence--indirectness. Journal of Clinical Epidemiology 2011;64(12):1303-10. [DOI: 10.1016/j.jclinepi.2011.04.014] [PMID: ] [DOI] [PubMed] [Google Scholar]
Haase 2004
- Haase JE. The adolescent resilience model as a guide to interventions. Journal of Pediatric Oncology Nursing 2004;21(5):289-99. [DOI: 10.1177/1043454204267922] [DOI] [PubMed] [Google Scholar]
Haglund 2007
- Haglund ME, Nestadt PS, Cooper NS, Southwick SM, Charney DS. Psychobiological mechanisms of resilience: relevance to prevention and treatment of stress-related psychopathology. Development and Psychopathology 2007;19(3):889-920. [DOI: 10.1017/S0954579407000430] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hamshire 2019
- Hamshire C, Jack K, Forsyth R, Langan AM, Harris WE. The wicked problem of healthcare student attrition. Nursing Inquiry 2019;26(3):e12294. [DOI: 10.1111/nin.12294] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hartley 2008
- Hartley SM, Vance DE, Elliott TR, Cuckler JM, Berry JW. Hope, self-efficacy, and functional recovery after knee and hip replacement surgery. Rehabilitation Psychology 2008;53(4):521-9. [DOI: 10.1037/a0013121] [DOI] [Google Scholar]
Harvey 2003
- Harvey MR, Liang B, Harney PA, Koenen K, Tummala-Narra P, Lebowitz L. A multidimensional approach to the assessment of trauma impact, recovery and resiliency: initial psychometric findings. Journal of Aggression, Maltreatment & Trauma 2003;6(2):87-109. [DOI: 10.1300/J146v06n02_05] [DOI] [Google Scholar]
Hasson 2005
- Hasson D, Arnetz BB. Validation and findings comparing VAS vs Likert scales for psychosocial measurements. International Electronic Journal Health Education 2005;8:178–92. [files.eric.ed.gov/fulltext/EJ794094.pdf] [Google Scholar]
Hautzinger 2006
- Hautzinger M, Keller F, Kühner C. BDI-II: Beck Depressions Inventar - Revision, Manual. 2nd edition. Frankfurt: Harcourt Test Services, 2006. [Google Scholar]
Hayes 2004
- Hayes SC, Follette VM, Linehan MM. Mindfulness and Acceptance: Expanding the Cognitive-Behavioral Tradition. New York (NY): Guilford Press, 2004. [Google Scholar]
Hayes 2006
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: model, processes and outcomes. Behaviour Research and Therapy 2006;44(1):1-25. [DOI: 10.1016/j.brat.2005.06.006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hayter 2014
- Hayter MR, Dorstyn DS. Resilience, self-esteem and self-compassion in adults with spina bifida. Spinal Cord 2014;52(2):167-71. [DOI: 10.1038/sc.2013.152] [PMID: ] [DOI] [PubMed] [Google Scholar]
Heber 2017
- Heber E, Ebert DD, Lehr D, Cuijpers P, Berking M, Nobis S, et al. The benefit of web- and computer-based interventions for stress: a systematic review and meta-analysis. Journal of Medical Internet Research 2017;19(2):e32. [DOI: 10.2196/jmir.5774] [PMC5336602 ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hebert 2007
- Hebert RS, Dang Q, Schulz R. Religious beliefs and practices are associated with better mental health in family caregivers of patients with dementia: findings from the REACH study. American Journal of Geriatric Psychiatry 2007;15(4):292-300. [DOI: 10.1097/01.JGP.0000247160.11769.ab] [PMID: ] [DOI] [PubMed] [Google Scholar]
Heinen 2017
- Heinen I, Bullinger M, Kocalevent RD. Perceived stress in first year medical students - associations with personal resources and emotional distress. BMC Medical Education 2017;17(1):4. [DOI: 10.1186/s12909-016-0841-8] [PMC5216588] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Helgeson 2006
- Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit finding and growth. Journal of Consulting and Clinical Psychology 2006;74(5):797-816. [DOI: 10.1037/0022-006X.74.5.797] [PMID: ] [DOI] [PubMed] [Google Scholar]
Henderson 1996
- Henderson N, Milstein MM. Resiliency in Schools: Making it Happen for Students and Educators. Thousand Oaks (CA): Corwin Press, 1996. [Google Scholar]
Hernandez 2013
- Hernandez M, Barrio C, Yamada AM. Hope and burden among Latino families of adults with schizophrenia. Family Process 2013;52(4):697-708. [DOI: 10.1111/famp.12042] [PMC5032651] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Heron 2010
- Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. British Journal of Health Psychology 2010;15(Pt 1):1-39. [DOI: 10.1348/135910709X466063] [19646331] [PMID: PMC2800172 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Herrero 2018 [pers comm]
- Herrero R. Trial status and data [personal communication]. Email to: A Kunzler 12 February 2018.
Herrero 2019 [pers comm]
- Herrero R. Trial status and analysis [personal communication]. Email to: A Kunzler 30 July 2019.
Herrmann‐Lingen 2011
- Herrmann-Lingen C, Buss U, Snaith RP. Hospital Anxiety and Depression Scale – Deutsche Version (HADS-D). Bern: Huber, 2011. [Google Scholar]
Higgins 2011a
- Higgins JP, Altman DG, Sterne JA, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [DOI: 10.1136/bmj.d5928] [PMC3196245] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2019a
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Higgins 2019b
- Higgins JP, Li T, Deeks JJ (editors). Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Higgins 2019c
- Higgins JP, Eldridge S, Li T (editors). Chapter 23: Including variants on randomized trials. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Hill 2018
- Hill MR, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Medical Education Online 2018;23(1):1530558. [DOI: 10.1080/10872981.2018.1530558] [30286698] [PMID: PMC6179084 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hills 2002
- Hills P, Argyle M. The Oxford Happiness Questionnaire: a compact scale for the measurement of psychological well-being. Personality and Individual Differences 2002;33(7):1073–82. [DOI: 10.1016/S0191-8869(01)00213-6] [DOI] [Google Scholar]
Hjemdal 2001
- Hjemdal O, Friborg O, Martinussen M, Rosenvinge JH. Preliminary results from the development and validation of a Norwegian scale for measuring adult resilience [Mestring og psykologisk motstandsdyktighet hos voksne: utvikling og foreløpig validering av et nytt instrument]. Tidsskrift for Norsk Psykologforening 2001;38(4):310-7. [psycnet.apa.org/record/2001-17289-001] [Google Scholar]
Ho 2010
- Ho SM, Ho JW, Bonanno GA, Chu AT, Chan EM. Hopefulness predicts resilience after hereditary colorectal cancer genetic testing: a prospective outcome trajectories study. BMC Cancer 2010;10:279. [DOI: 10.1186/1471-2407-10-279] [PMC2891641] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hodges 2008
- Hodges HF, Keeley AC, Troyan PJ. Professional resilience in baccalaureate-prepared acute care nurses: first steps. Nursing Education Perspectives 2008;29(2):80-9. [DOI: 10.1097/00024776-200803000-00008] [PMID: ] [DOI] [PubMed] [Google Scholar]
Houston 2019 [pers comm]
- Houston B. Subgroup data for university students in health professions [personal communication]. Email to: A Kunzler 19 September 2019.
Hu 2008
- Hu Y-Q, Gan Y-Q. Development and psychometric validity of the Resilience Scale for Chinese Adolescents. Acta Psychologica Sinica 2008;40(8):902-12. [DOI: 10.3724/SP.J.1041.2008.00902] [DOI] [Google Scholar]
Hu 2015
- Hu T, Zhang D, Wang J. A meta-analysis of the trait resilience and mental health. Personality and Individual Differences 2015;76:18-27. [DOI: 10.1016/j.paid.2014.11.039] [DOI] [Google Scholar]
Hultcrantz 2017
- Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, et al. The GRADE Working Group clarifies the construct of certainty of evidence. Journal of Clinical Epidemiology 2017;87:4-13. [DOI: 10.1016/j.jclinepi.2017.05.006] [PMC6542664] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hurtes 2001
- Hurtes KP, Allen LR. Measuring resiliency in youth: the Resiliency Attitudes and Skills Profile. Therapeutic Recreation Journal 2001;35(4):333-47. [b32aefb8453f58c579cdc2faddb56ca5.pdf] [Google Scholar]
Hystad 2011
- Hystad SW, Eid J, Brevik JI. Effects of psychological hardiness, job demands, and job control on sickness absence: a prospective study. Journal of Occupational Health Psychology 2011;16(3):265-78. [DOI: 10.1037/a0022904] [PMID: ] [DOI] [PubMed] [Google Scholar]
Iacoviello 2014
- Iacoviello BM, Charney DS. Psychosocial facets of resilience: implications for preventing posttrauma psychopathology, treating trauma survivors, and enhancing community resilience. European Journal of Psychotraumatology 2014;5(1):23970. [DOI: 10.3402/ejpt.v5.23970] [PMC4185137] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jackson 2007
- Jackson D, Firtko A, Edenborough M. Personal resilience as a strategy for surviving and thriving in the face of workplace adversity: a literature review. Journal of Advanced Nursing 2007;60(1):1-9. [DOI: 10.1111/j.1365-2648.2007.04412.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Jackson 2014
- Jackson T, Wang Y, Wang Y, Fan H. Self-efficacy and chronic pain outcomes: a meta-analytic review. Journal of Pain 2014;15(8):800-14. [DOI: 10.1016/j.jpain.2014.05.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Jacob 2013
- Jacob T, Itzchak EB, Raz O. Stress among healthcare students--a cross disciplinary perspective. Physiotherapy Theory and Practice 2013;29(5):401-12. [DOI: 10.3109/09593985.2012.734011] [PMID: ] [DOI] [PubMed] [Google Scholar]
Jameson 2014
- Jameson PR. The effects of a hardiness educational intervention on hardiness and perceived stress of junior baccalaureate nursing students. Nurse Education Today 2014;34(4):603–7. [DOI: 10.1016/j.nedt.2013.06.019] [PMID: ] [DOI] [PubMed] [Google Scholar]
Jeffries 2007
- Jeffries PR. Simulation in Nursing Education: From Conceptualization to Evaluation. New York (NY): National League for Nursing, 2007. [Google Scholar]
Jennings 2013
- Jennings PA, Frank JL, Snowberg KE, Coccia MA, Greenberg MT. Improving classroom learning environments by Cultivating Awareness and Resilience in Education (CARE): results of a randomized controlled trial. School Psychology Quarterly 2013;28(4):374-90. [DOI: 10.1037/spq0000035] [PMID: ] [DOI] [PubMed] [Google Scholar]
Johnson 2009
- Johnson RJ, Canetti D, Palmieri PA, Galea S, Varley J, Hobfoll SE. A prospective study of risk and resilience factors associated with posttraumatic stress symptoms and depression symptoms among Jews and Arabs exposed to repeated acts of terrorism in Israel. Psychological Trauma: Theory, Research, Practice, and Policy 2009;1(4):291-311. [DOI: 10.1037/a0017586] [DOI] [Google Scholar]
Johnson 2010
- Johnson J, Gooding PA, Wood AM, Tarrier N. Resilience as positive coping appraisals: testing the schematic appraisals model of suicide (SAMS). Behaviour Research and Therapy 2010;48(3):179-86. [DOI: 10.1016/j.brat.2009.10.007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Johnson 2015
- Johnson AJ, Tottenham N. Regulatory skill as a resilience factor for adults with a history of foster care: a pilot study. Developmental Psychobiology 2015;57(1):1-16. [DOI: 10.1002/dev.21227] [PMC4302248] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnston 2015
- Johnston MC, Porteous T, Crilly MA, Burton CD, Elliott A, Iversen L, et al. Physical disease and resilient outcomes: a systematic review of resilience definitions and study methods. Psychosomatics 2015;56(2):168-80. [DOI: 10.1016/j.psym.2014.10.005] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jones 2000
- Jones MC, Johnston DW. Reducing distress in first level and student nurses: a review of the applied stress management literature. Journal of Advanced Nursing 2000;32(1):66–74. [DOI: 10.1046/j.1365-2648.2000.01421.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Joseph 1992
- Joseph S, Andrews B, Williams R, Yule W. Crisis support and psychiatric symptomatology in adult survivors of the Jupiter cruise ship disaster. British Journal of Clinical Psychology 1992;31(1):63-73. [DOI: 10.1111/j.2044-8260.1992.tb00968.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Joyce 2018
- Joyce S, Shand F, Tighe J, Laurent SJ, Bryant RA, Harvey SB. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018;8(6):e017858. [DOI: 10.1136/bmjopen-2017-017858] [PMC6009510] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Judkins 2005a
- Judkins S, Rind R. Hardiness, job satisfaction, and stress among home health nurses. Home Health Care Management & Practice 2005;17(2):113-8. [DOI: 10.1177/1084822304270020] [DOI] [Google Scholar]
Judkins 2005b
- Judkins S, Arris L, Keener E. Program evaluation in graduate nursing education: hardiness as a predictor of success among nursing administration students. Journal of Professional Nursing 2005;21(5):314–21. [DOI: 10.1016/j.profnurs.2005.07.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kabat‐Zinn 1990
- Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of your Body and Mind to Face Stress, Pain, and Illness. New York (NY): Delacourte Press, 1990. [Google Scholar]
Kahneman 1993
- Kahneman D, Fredrickson BL, Schreiber CA, Redelmeier DA. When more pain is preferred to less: adding a better end. Psychological Science 1993;4(6):401–5. [DOI: 10.1111/j.1467-9280.1993.tb00589.x] [DOI] [Google Scholar]
Kalisch 2015
- Kalisch R, Müller MB, Tüscher O. A conceptual framework for the neurobiological study of resilience. Behavioral and Brain Sciences 2015;38:e92. [DOI: 10.1017/S0140525X1400082X] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kalisch 2017
- Kalisch R, Baker DG, Basten U, Boks MP, Bonanno GA, Brummelman E, et al. The resilience framework as a strategy to combat stress-related disorders. Nature Human Behaviour 2017;1(11):784-90. [DOI: 10.1038/s41562-017-0200-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kanekar 2019 [pers comm]
- Kanekar A. Potential inclusion of healthcare students. Email to: A Kunzler 15 September 2019.
Karstoft 2015
- Karstoft KI, Armour C, Elklit A, Solomon Z. The role of locus of control and coping style in predicting longitudinal PTSD-trajectories after combat exposure. Journal of Anxiety Disorders 2015;32:89-94. [DOI: 10.1016/j.janxdis.2015.03.007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kasen 2014
- Kasen S, Wickramaratne P, Gameroff MJ. Religiosity and longitudinal change in psychosocial functioning in adult offspring of depressed parents at high risk for major depression. Depression and Anxiety 2014;31(1):63-71. [DOI: 10.1002/da.22131] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kaspersen 2003
- Kaspersen M, Matthiesen SB, Götestam KG. Social network as a moderator in the relation between trauma exposure and trauma reaction: a survey among UN soldiers and relief workers. Scandinavian Journal of Psychology 2003;44(5):415-23. [DOI: 10.1046/j.1467-9450.2003.00362.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kelleher 2019 [pers comm]
- Kelleher C. Information about whether trial was already published [personal communication]. Email to: A Kunzler 1 August 2019.
Kent 2011
- Kent M, Davis MC, Stark SL, Stewart LA. A resilience-oriented treatment for posttraumatic stress disorder: results of a preliminary randomized clinical trial. Journal of Traumatic Stress 2011;24(5):591-5. [DOI: 10.1002/jts.20685] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kent 2014
- Kent M, Davis MC, Reich JW. The Resilience Handbook: Approaches to Stress and Trauma. New York (NY): Routledge, 2014. [Google Scholar]
Kiamarthi 1998
- Kiamarthi A, Najarian B, Mehrabi Zadeh Honarmand M. Construction and validation of a scale to measure the psychological hardiness. Journal of Psychology 1998;3:271-84. [No DOI or other object identifier available] [Google Scholar]
Kilic 2013
- Kilic SA, Dorstyn DS, Guiver NG. Examining factors that contribute to the process of resilience following spinal cord injury. Spinal Cord 2013;51(7):553-7. [DOI: 10.1038/sc.2013.25] [PMID: ] [DOI] [PubMed] [Google Scholar]
King 1998
- King LA, King DW, Fairbank JA, Keane TM, Adams GA. Resilience-recovery factors in post-traumatic stress disorder among female and male Vietnam veterans: hardiness, postwar social support, and additional stressful life events. Journal of Personality and Social Psychology 1998;74(2):420-34. [DOI: 10.1037//0022-3514.74.2.420] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kivimäki 2005
- Kivimäki M, Vahtera J, Elovainio M, Helenius H, Singh-Manoux A, Pentti J. Optimism and pessimism as predictors of change in health after death or onset of severe illness in family. Health Psychology 2005;24(4):413-21. [DOI: 10.1037/0278-6133.24.4.413] [PMID: ] [DOI] [PubMed] [Google Scholar]
Klohnen 1996
- Klohnen EC. Conceptual analysis and measurement of the construct of ego-resiliency. Journal of Personality and Social Psychology 1996;70(5):1067-79. [DOI: 10.1037//0022-3514.70.5.1067] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kneebone 2003
- Kneebone II, Martin PR. Coping and caregivers of people with dementia. British Journal of Health Psychology 2003;8(Part 1):1-17. [DOI: 10.1348/135910703762879174] [PMID: ] [DOI] [PubMed] [Google Scholar]
Koenen 2003
- Koenen KC, Stellman JM, Stellman SD, Sommer JF Jr. Risk factors for course of posttraumatic stress disorder among Vietnam veterans: a 14-year follow-up of American Legionnaires. Journal of Consulting and Clinical Psychology 2003;71(6):980-6. [DOI: 10.1037/0022-006X.71.6.980] [PMID: ] [DOI] [PubMed] [Google Scholar]
Koenig 2007
- Koenig HG. Religion and remission of depression in medical inpatients with heart failure/pulmonary disease. Journal of Nervous and Mental Disease 2007;195(5):389-95. [DOI: 10.1097/NMD.0b013e31802f58e3] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kok 2013
- Kok BE, Coffey KA, Cohn MA, Catalino LI, Vacharkulksemsuk T, Algoe SB, et al. How positive emotions build physical health: perceived positive social connections account for the upward spiral between positive emotions and vagal tone. Psychological Science 2013;24(7):1123–32. [DOI: 10.1177/0956797612470827] [PMID: ] [DOI] [PubMed] [Google Scholar]
Korpershoek 2011
- Korpershoek C, Van der Bijl J, Hafsteinsdóttir TB. Self-efficacy and its influence on recovery of patients with stroke: a systematic review. Journal of Advanced Nursing 2011;67(9):1876-94. [DOI: 10.1111/j.1365-2648.2011.05659.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Krahn 2013
- Krahn U, Binder H, König J. A graphical tool for locating inconsistency in network meta-analyses. BMC Medical Research Methodology 2013;13:35. [DOI: 10.1186/1471-2288-13-35] [PMC3644268] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Krahn 2014
- Krahn U, Binder H, König J. Visualizing inconsistency in network meta-analysis by independent path decomposition. BMC Medical Research Methodology 2014;14:131. [DOI: 10.1186/1471-2288-14-131] [PMC4279676] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Krause 2007
- Krause N. Evaluating the stress-buffering function of meaning in life among older people. Journal of Aging and Health 2007;19(5):792-812. [DOI: 10.1177/0898264307304390] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kuehner 2017
- Kuehner C. Why is depression more common among women than among men? Lancet. Psychiatry 2017;4(2):146-58. [DOI: 10.1016/S2215-0366(16)30263-2] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kuiper 1992
- Kuiper NA, Martin RA, Dance KA. Sense of humour and enhanced quality of life. Personality and Individual Differences 1992;13(12):1273-83. [DOI: 10.1016/0191-8869(92)90169-P] [DOI] [Google Scholar]
Kuiper 2012
- Kuiper NA. Humor and resiliency: towards a process model of coping and growth. Europe’s Journal of Psychology 2012;8(3):475-91. [DOI: 10.5964/ejop.v8i3.464] [DOI] [Google Scholar]
Kumpfer 1999
- Kumpfer KL. Factors and processes contributing to resilience: the resilience framework. In: Glantz MD, Johnson JL, editors(s). Resilience and Development: Positive Life Adaptations. New York (NY): Kluwer Academic Publishers, 1999:179-224. [Google Scholar]
Kunttu 2017
- Kunttu K, Pesonen T, Saari J. Research Publications of the Finnish Student Health Service 48. Student Health Survey 2016: A National Survey Among Finnish University Students. Helsinki: Finnish Student Health Service, 2017. [www.yths.fi/app/uploads/2020/03/KOTT_2016_ENG.pdf] [Google Scholar]
Kunzler 2018
- Kunzler AM, Chmitorz A, Bagusat C, Kaluza AJ, Hoffmann I, Schäfer M, et al. Construct validity and population-based norms of the German Brief Resilience Scale (BRS). European Journal of Health Psychology 2018;25(3):107-17. [DOI: 10.1027/2512-8442/a000016] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kunzler 2020
- Kunzler AM, Helmreich I, Chmitorz A, König J, Binder H, Wessa M, et al. Psychological interventions to foster resilience in healthcare professionals. Cochrane Database of Systematic Reviews 2020, Issue 7. Art. No: CD012527. [DOI: 10.1002/14651858.CD012527.pub2] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kvillemo 2014
- Kvillemo P, Bränström R. Coping with breast cancer: a meta-analysis. PLOS One 2014;9(11):e112733. [DOI: 10.1371/journal.pone.0112733] [PMC4244095] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
König 2013
- König J, Krahn U, Binder H. Visualizing the flow of evidence in network meta-analysis and characterizing mixed treatment comparisons. Statistics in Medicine 2013;32(30):5414-29. [DOI: 10.1002/sim.6001] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kötter 2013
- Kötter T, Voltmer E. Measurement of specific medical school stress: translation of the “perceived medical school stress instrument” to the German language [Stressbelastung von medizinstudierenden messen: übersetzung des "Perceived Medical School Stress Instruments" in die deutsche sprache]. GMS Zeitschrift für Medizinische Ausbildung 2013;30(2):Doc22. [DOI: 10.3205/zma000865] [PMC3671318] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kötter 2017
- Kötter T, Wagner J, Brüheim L, Voltmer E. Perceived medical school stress of undergraduate medical students predicts academic performance: an observational study. BMC Medical Education 2017;17(1):256. [DOI: 10.1186/s12909-017-1091-0] [PMC5732510] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Landy 1991
- Landy FJ, Rastegary H, Thayer J, Colvin C. Time urgency: the construct and its measurement. Journal of Applied Psychology 1991;76(5):644-57. [DOI: 10.1037/0021-9010.76.5.644] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lawler 1992
- Lawler KA, Schmied LA. A prospective study of women's health: the effects of stress, hardiness, locus of control, type A behavior, and physiological reactivity. Women & Health 1992;19(1):27-41. [DOI: 10.1300/J013v19n01_02] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lazarus 1987
- Lazarus RS, Folkman S. Transactional theory and research on emotions and coping. European Journal of Personality 1987;1(3):141-69. [DOI: 10.1002/per.2410010304] [DOI] [Google Scholar]
Lechner 2007
- Lechner L, Bolman C, Van Dalen A. Definite involuntary childlessness: associations between coping, social support and psychological distress. Human Reproduction 2007;22(1):288-94. [DOI: 10.1093/humrep/del327] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lee 2013
- Lee JH, Nam SK, Kim A-R, Kim B, Lee MY, Lee SM. Resilience: a meta-analytic approach. Journal of Counseling & Development 2013;91(3):269-79. [DOI: 10.1002/j.1556-6676.2013.00095.x] [DOI] [Google Scholar]
Lefebvre 2019
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Leppin 2014
- Leppin AL, Bora PR, Tilburt JC, Gionfriddo MR, Zeballos-Palacios C, Dulohery MM, et al. The efficacy of resiliency training programs: a systematic review and meta-analysis of randomized trials. PLOS One 2014;9(10):e111420. [DOI: 10.1371/journal.pone.0111420] [ PROSPERO #CRD42014007185] [PMC4210242] [PMID: 25347713] [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2011
- Li T, Puhan MA, Vedula SS, Singh S, Dickersin K, Ad Hoc Network Meta-analysis Methods Meeting Working Group. Network meta-analysis-highly attractive but more methodological research is needed. BMC Medicine 2011;9:79. [DOI: 10.1186/1741-7015-9-79] [PMC3159133] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2017
- Li SH, Graham BM. Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? The potential role of sex hormones. Lancet. Psychiatry 2017;4(1):73-82. [DOI: 10.1016/S2215-0366(16)30358-3] [PMID: ] [DOI] [PubMed] [Google Scholar]
Li 2019
- Li T, Higgins JP, Deeks JJ (editors). Chapter 5: Collecting data. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Liebenberg 2012
- Liebenberg L, Ungar M, Van de Vijver F. Validation of the Child and Youth Resilience Measure - 28 (CYRM-28) among Canadian youth. Research on Social Work Practice 2012;22(2):219-26. [DOI: 10.1177/1049731511428619] [DOI] [Google Scholar]
Liebenberg 2013
- Liebenberg L, Ungar M, LeBlanc JC. The CYRM-12: a brief measure of resilience. Canadian Journal of Public Health 2013;104(2):e131-5. [DOI: 10.1007/BF03405676] [PMC6974279] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Liebmann 2004
- Liebmann M. Art Therapy for Groups. New York: Brunner-Routledge, 2004. [Google Scholar]
Linde 2016
- Linde K, Rücker G, Schneider A, Kriston L. Questionable assumptions hampered interpretation of a network meta-analysis of primary care depression treatments. Journal of Clinical Epidemiology 2016;71:86-96. [DOI: 10.1016/j.jclinepi.2015.10.010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lo 2018
- Lo K, Waterland J, Todd P, Gupta T, Bearman M, Hassed C, et al. Group interventions to promote mental health in health professional education: a systematic review and meta-analysis of randomised controlled trials. Advances in Health Sciences Education: Theory and Practice 2018;23(2):413-47. [DOI: 10.1007/s10459-017-9770-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
Locke 2007
- Locke DE, Decker PA, Sloan JA, Brown PD, Malec JF, Clark MM, et al. Validation of single-item linear analog scale assessment of quality of life in neuro-oncology patients. Journal of Pain and Symptom Management 2007;34(6):628-38. [DOI: 10.1016/j.jpainsymman.2007.01.016] [PMC2732111] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Loprinzi 2011
- Loprinzi CE, Prasad K, Schroeder DR, Sood A. Stress management and resilience training (SMART) program to decrease stress and enhance resilience among breast cancer survivors: a pilot randomized clinical trial. Clinical Breast Cancer 2011;11(6):364-8. [DOI: 10.1016/j.clbc.2011.06.008] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lovell 2018
- Lovell B. What do we know about coaching in medical education? A literature review. Medical Education 2018;52(4):376-90. [DOI: 10.1111/medu.13482] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lovibond 1993
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scale. Sydney (NSW): University of New South Wales, 1993. [Google Scholar]
Lovibond 1995
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. Sydney (NSW): Psychology Foundation of Australia, 1995. [Google Scholar]
Lowery 2005
- Lowery K, Stokes MA. Role of peer support and emotional expression on posttraumatic stress disorder in student paramedics. Journal of Traumatic Stress 2005;18(2):171-9. [DOI: 10.1002/jts.20016] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lu 2006
- Lu G, Ades AE. Assessing evidence inconsistency in mixed treatment comparisons. Journal of the American Statistical Association 2006;101(474):447-59. [DOI: 10.1198/016214505000001302] [DOI] [Google Scholar]
Lumley 2002
- Lumley T. Network meta-analysis for indirect treatment comparisons. Statistics in Medicine 2002;21(16):2313-24. [DOI: 10.1002/sim.1201] [PMID: ] [DOI] [PubMed] [Google Scholar]
Luo 2015
- Luo T, Cheng X, Xiong Y. Relationship among resilience, coping style and mental health of newly recruited workers born after 1990 in manufacturing industry of Shenzhen City. Journal of Hygiene Research 2015;44(2):252-6. [PMID: ] [PubMed] [Google Scholar]
Luszczynska 2009
- Luszczynska A, Benight CC, Cieslak R. Self-efficacy and health-related outcomes of collective trauma: a systematic review. European Psychologist 2009;14(1):51-62. [DOI: 10.1027/1016-9040.14.1.51] [DOI] [Google Scholar]
Luthans 2004
- Luthans F, Luthans KW, Luthans BC. Positive psychological capital: beyond human and social capital. Business Horizons 2004;47(1):45–50. [DOI: 10.1016/j.bushor.2003.11.007] [DOI] [Google Scholar]
Luthans 2006
- Luthans F, Avey JB, Avolio BJ, Norman SM, Combs GJ. Psychological capital development: toward a micro-intervention. Journal of Organizational Behavior 2006;27(3):387-93. [DOI: 10.1002/job.373] [DOI] [Google Scholar]
Luthans 2007
- Luthans F, Avolio B, Avey JB, Norman SM. Postive psychological capital: measurement and relationship with performance and job satisfaction. Personnel Psychology 2007;60(3):541-72. [DOI: 10.1111/j.1744-6570.2007.00083.x] [DOI] [Google Scholar]
Luthans 2010
- Luthans F, Avey JB, Avolio BJ, Peterson SJ. The development and resulting performance impact of positive psychological capital. Human Resource Development Quarterly 2010;21(1):41-67. [DOI: 10.1002/hrdq.20034] [DOI] [Google Scholar]
Luthar 2000
- Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Development 2000;71(3):543-62. [DOI: 10.1111/1467-8624.00164] [NIHMS21559] [PMC1885202] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lyon 2001
- Lyon DE, Younger JB. Purpose in life and depressive symptoms in persons living with HIV disease. Journal of Nursing Scholarship 2001;33(2):129-33. [DOI: 10.1111/j.1547-5069.2001.00129.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Macedo 2014
- Macedo T, Wilheim L, Gonçalves R, Coutinho ES, Vilete L, Figueira I, et al. Building resilience for future adversity: a systematic review of interventions in non-clinical samples of adults. BMC Psychiatry 2014;14:227. [DOI: 10.1186/s12888-014-0227-6] [PMC4149241] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Maddi 1987
- Maddi SR. Hardiness training at Illinois Bell Telephone. In: Opatz JP, editors(s). Health Promotion Evaluation. Stephens Point (WI): National Wellness Institute, 1987:101-15. [Google Scholar]
Maddi 1998
- Maddi SR, Kahn S, Maddi KL. The effectiveness of hardiness training. Consulting Psychology Journal: Practice and Research 1998;50(2):78-86. [DOI: 10.1037/1061-4087.50.2.78] [DOI] [Google Scholar]
Maddi 2001
- Maddi SR, Khoshaba DM. HardiSurvey III-R: Test Development and Internet Instruction Manual. Irvine (CA): Hardiness Institute, 2001. [Google Scholar]
Maddi 2009
- Maddi SR, Harvey RH, Khoshaba DM, Fazel M, Resurreccion N. Hardiness training facilitates performance in college. Journal of Positive Psychology 2009;4(6):566-77. [DOI: 10.1080/17439760903157133] [DOI] [Google Scholar]
Madsen 2010
- Madsen MD, Abell N. Trauma Resilience Scale: validation of protective factors associated with adaptation following violence. Research on Social Work Practice 2010;20(2):223-33. [DOI: 10.1177/1049731509347853] [DOI] [Google Scholar]
Mancini 2009
- Mancini AD, Bonanno GA. Predictors and parameters of resilience to loss: toward an individual differences model. Journal of Personality 2009;77(6):1805-32. [DOI: 10.1111/j.1467-6494.2009.00601.x] [PMC4224188] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mao 2019
- Mao Y, Zhang N, Liu J, Zhu B, He R, Wang X. A systematic review of depression and anxiety in medical students in China. BMC Medical Education 2019;19:327. [DOI: 10.1186/s12909-019-1744-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Martin‐Krumm 2003
- Martin-Krumm CP, Sarrazin PG, Peterson C, Famose J-P. Explanatory style and resilience after sports failure. Personality and Individual Differences 2003;35(7):1685-95. [DOI: 10.1016/S0191-8869(02)00390-2] [DOI] [Google Scholar]
Marty 2010
- Marty MA, Segal DL, Coolidge FL. Relationships among dispositional coping strategies, suicidal ideation, and protective factors against suicide in older adults. Aging & Mental Health 2010;14(8):1015-23. [DOI: 10.1080/13607863.2010.501068] [PMID: ] [DOI] [PubMed] [Google Scholar]
Maslach 1996
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd edition. Palo Alto (CA): Consulting Psychologist Press, 1996. [Google Scholar]
Maslach 1997
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. In: Zalaquett CP, Wood RJ, editors(s). Evaluating Stress: A Book of Resources. Lanham (MD): Scarecrow Press Inc, 1997:191-218. [Google Scholar]
Massey 2019
- Massey CN, Feig EH, Duque-Serrano L, Wexler D, Moskowitz JT, Huffman JC. Well-being interventions for individuals with diabetes: a systematic review. Diabetes Research and Clinical Practice 2019;147:118-33. [DOI: 10.1016/j.diabres.2018.11.014] [PMC6370485] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Masten 2001
- Masten AS. Ordinary magic: resilience processes in development. Amercian Psychologist 2001;56(3):227-38. [DOI: 10.1037//0003-066x.56.3.227] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mathad 2019 [pers comm]
- Mathad M. Number of participants aged ≥ 18 years in final sample [personal communication]. Email to: A Kunzler 7 September 2019.
Mathews 2000
- Mathews A, Mackintosh B. Induced emotional interpretation bias and anxiety. Journal of Abnormal Psychology 2000;109(4):602–15. [PMID: ] [PubMed] [Google Scholar]
McAllister 2009
- McAllister M, McKinnon J. The importance of teaching and learning resilience in the health disciplines: a critical review of the literature. Nurse Education Today 2009;29(4):371-9. [DOI: 10.1016/j.nedt.2008.10.011] [PMID: ] [DOI] [PubMed] [Google Scholar]
McCann 2013
- McCann CM, Beddoe E, McCormick K, Huggard P, Kedge S, Adamson C, et al. Resilience in the health professions: a review of recent literature. International Journal of Wellbeing 2013;3(1):60-81. [DOI: 10.5502/ijw.v3i1.4] [DOI] [Google Scholar]
McGowan 2016
- McGowan JE, Murray K. Exploring resilience in nursing and midwifery students: a literature review. Journal of Advanced Nursing 2016;72(10):2272-83. [DOI: 10.1111/jan.12960] [PMID: ] [DOI] [PubMed] [Google Scholar]
McIntosh 2012
- McIntosh RC, Rosselli M. Stress and coping in women living with HIV: a meta-analytic review. AIDS and Behavior 2012;16(8):2144-59. [DOI: 10.1007/s10461-012-0166-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
McLarnon 2013
- McLarnon MJ, Rothstein MG. Development and initial validation of the Workplace Resilience Inventory. Journal of Personnel Psychology 2013;12(2):63-73. [DOI: 10.1027/1866-5888/a000084] [DOI] [Google Scholar]
Meichenbaum 2007
- Meichenbaum D. Stress inoculation training: a preventative and treatment approach. In: Lehrer PM, Woolfolk RL, Sime WS, editors(s). Principles and Practice of Stress Management. 3rd edition. New York (NY): Guilford Press, 2007:497-518. [Google Scholar]
Mejia‐Downs 2018 [pers comm]
- Mejia-Downs AM. Summary outcome data for the outcomes [personal communication]. Email to: A Kunzler 6 December 2018.
Michael 2003
- Michael ST, Crowther MR, Schmid B, Allen RS. Widowhood and spirituality: coping responses to bereavement. Journal of Women & Aging 2003;15(2-3):145-65; discussion 185-7. [DOI: 10.1300/J074v15n02_09] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mills 2012
- Mills EJ, Ioannidis JP, Thorlund K, Schünemann HJ, Puhan MA, Guyatt GH. How to use an article reporting a multiple treatment comparison meta-analysis. JAMA 2012;308(12):1246-53. [DOI: 10.1001/2012.jama.11228] [PMID: ] [DOI] [PubMed] [Google Scholar]
Milne 2016
- Milne T, Creedy DK, West R. Integrated systematic review on educational strategies that promote academic success and resilience in undergraduate indigenous students. Nurse Education Today 2016;36:387-94. [DOI: 10.1016/j.nedt.2015.10.008] [PMID: ] [DOI] [PubMed] [Google Scholar]
Milte 2015
- Milte CM, Luszcz MA, Ratcliffe J, Masters S, Crotty M. Influence of health locus of control on recovery of function in recently hospitalized frail older adults. Geriatrics & Gerontology International 2015;15(3):341-9. [DOI: 10.1111/ggi.12281] [PMID: ] [DOI] [PubMed] [Google Scholar]
Min 2013
- Min JA, Yu JJ, Lee CU, Chae JH. Cognitive emotion regulation strategies contributing to resilience in patients with depression and/or anxiety disorders. Comprehensive Psychiatry 2013;54(8):1190-7. [DOI: 10.1016/j.comppsych.2013.05.008] [PMID: ] [DOI] [PubMed] [Google Scholar]
Miu 2015
- Miu AS, Yeager DS. Preventing symptoms of depression by teaching adolescents that people can change: effects of a brief incremental theory of personality intervention at 9-month follow-Up. Clinical Psychological Science 2015;3(5):726–43. [DOI: 10.1177/2167702614548317] [DOI] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [DOI: 10.1136/bmj.b2535] [PMC2714657] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mohr 2014
- Mohr DC, Ho J, Hart TL, Baron KG, Berendsen M, Beckner V, et al. Control condition design and implementation features in controlled trials: a meta-analysis of trials evaluating psychotherapy for depression. Translational Behavioral Medicine 2014;4(4):407-23. [DOI: 10.1007/s13142-014-0262-3] [PMC4286544] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moritz 2019
- Moritz S, Nestoriuc Y, Rief W, Klein JP, Jelinek L, Peth J. It can't hurt, right? Adverse effects of psychotherapy in patients with depression. European Archives of Psychiatry and Clinical Neuroscience 2019;269(5):577-86. [DOI: 10.1007/s00406-018-0931-1] [PMID: ] [DOI] [PubMed] [Google Scholar]
Morris 2013
- Morris MC, Rao U. Psychobiology of PTSD in the acute aftermath of trauma: integrating research on coping, HPA function and sympathetic nervous system activity. Asian Journal of Psychiatry 2013;6(1):3-21. [DOI: 10.1016/j.ajp.2012.07.012] [PMC3565157] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moskowitz 2009
- Moskowitz JT, Hult JR, Bussolari C, Acree M. What works in coping with HIV? A meta-analysis with implications for coping with serious illness. Psychological Bulletin 2009;135(1):121-41. [DOI: 10.1037/a0014210] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mueller 2019 [pers comm]
- Mueller MK. Number of participants analysed for outcomes reported in Table 2 and 3 and details about intervention content [personal communication]. Email to: A Kunzler 5 September 2019.
Myhren 2010
- Myhren H, Ekeberg O, Tøien K, Karlsson S, Stokland O. Posttraumatic stress, anxiety and depression symptoms in patients during the first year post intensive care unit discharge. Critical Care 2010;14(1):R14. [DOI: 10.1186/cc8870] [PMC2875529] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nagarathna 2008
- Nagarathna R, Nagendra HR. Integrated Approach of Yoga Therapy for Positive Health. Bangalore (KA): Swami Vivekananda Yoga Prakashana, 2008. [Google Scholar]
Natvik 2011
- Natvik S, Bjorvatn B, Moen BE, Magerøy N, Sivertsen B, Pallesen S. Personality factors related to shift work tolerance in two- and three-shift workers. Applied Ergonomics 2011;42(5):719-24. [DOI: 10.1016/j.apergo.2010.11.006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nazroo 1998
- Nazroo JY, Edwards AC, Brown GW. Gender differences in the prevalence of depression: artefact, alternative disorders, biology or roles? Sociology of Health & Illness 1998;20(3):312-30. [DOI: 10.1111/1467-9566.00104] [DOI] [Google Scholar]
NCVC 2005
- National Center for Victims of Crime. Reach in. Reach out. Finding your resilience. members.victimsofcrime.org/docs/2006%20Kit/resilience-brochure-(web-ready).pdf 2005.
Neff 2003a
- Neff KD. The development and validation of a scale to measure self-compassion. Self and Identity 2003;2(3):223–250. [DOI: 10.1080/15298860309027] [DOI] [Google Scholar]
Neff 2003b
- Neff KD. Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self and Identity 2003;2(2):85–101. [DOI: 10.1080/15298860309032] [DOI] [Google Scholar]
Neumann 2011
- Neumann M, Edelhäuser F, Tauschel D, Fischer MR, Wirtz M, Woopen C, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Academic Medicine 2011;86(8):996-1009. [DOI: 10.1097/ACM.0b013e318221e615] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nezu 1988
- Nezu AM, Nezu CM, Blissett SE. Sense of humor as a moderator of the relation between stressful events and psychological distress: a prospective analysis. Journal of Personality and Social Psychology 1988;54(3):520-5. [DOI: 10.1037//0022-3514.54.3.520] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nezu 2013
- Nezu AM, Nezu CM, D' Zurilla TJ. Problem-Solving Therapy. A Treatment Manual. New York (NY): Springer Publishing Company, 2013. [Google Scholar]
NICE 2009
- National Institute for Health and Care Excellence. Depression in Adults: the treatment and management of depression in adults; October 2009. www.nice.org.uk/guidance/cg90/resources/guidance-depression-in-adults-pdf. [PubMed]
Nieuwsma 2012
- Nieuwsma JA, Trivedi RB, Mcduffie J, Kronish I, Benjamin D, Williams JW. Brief psychotherapy for depression: a systematic review and meta-analysis. International Journal of Psychiatry in Medicine 2012;43(2):129–51. [DOI: 10.2190/PM.43.2.c.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Norris 2009
- Norris FH, Tracy M, Galea S. Looking for resilience: understanding the longitudinal trajectories of responses to stress. Social Science & Medicine 2009;68(12):2190-8. [DOI: 10.1016/j.socscimed.2009.03.043] [PMID: ] [DOI] [PubMed] [Google Scholar]
Northouse 2002
- Northouse LL, Mood D, Kershaw T, Schafenacker A, Mellon S, Walker J, et al. Quality of life of women with recurrent breast cancer and their family members. Journal of Clinical Oncology 2002;20(19):4050-64. [DOI: 10.1200/JCO.2002.02.054] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nowack 1989
- Nowack KM. Coping style, cognitive hardiness, and health status. Journal of Behavioral Medicine 1989;12(2):145-58. [DOI: 10.1007/bf00846548] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nowack 1990
- Nowack KM. Initial development of an inventory to assess stress and health risk. American Journal of Health Promotion 1990;4(3):173-80. [DOI: 10.4278/0890-1171-4.3.173] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nowlan 2015
- Nowlan JS, Wuthrich VM, Rapee RM. Positive reappraisal in older adults: a systematic literature review. Aging & Mental Health 2015;19(6):475-84. [DOI: 10.1080/13607863.2014.954528] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nugent 1993
- Nugent WR, Thomas JW. Validation of a clinical measure of self-esteem. Research on Social Work Practice 1993;3(2):191-207. [DOI: 10.1177/104973159300300205] [DOI] [Google Scholar]
Ong 2006
- Ong AD, Bergeman CS, Bisconti TL, Wallace KA. Psychological resilience, positive emotions, and successful adaptation to stress in later life. Journal of Personality and Social Psychology 2006;91(4):730-49. [DOI: 10.1037/0022-3514.91.4.730] [PMID: ] [DOI] [PubMed] [Google Scholar]
Orengo 2001
- Orengo CA, Wei SH, Molinari VA, Hale DD, Kunik ME. Functioning in rheumatoid arthritis: the role of depression and self-efficacy. Clinical Gerontologist 2001;23(3-4):45-56. [DOI: 10.1300/J018v23n03_05] [DOI] [Google Scholar]
Oshio 2002
- Oshio A, Nakaya N, Kaneko H, Nagamine S. Development and validation of an Adolescent Resilience Scale. Japanese Journal of Counseling Science 2002;35:57-65. [www.researchgate.net/publication/284332745_Development_and_validation_of_an_adolescent_resilience_scale] [Google Scholar]
Oshio 2003
- Oshio A, Kaneko H, Nagamine S, Nayaka M. Construct validity of the Adolescent Resilience Scale. Psychological Reports 2003;93(3 Pt 2):1217-22. [DOI: 10.2466/pr0.2003.93.3f.1217] [PMID: ] [DOI] [PubMed] [Google Scholar]
Owens 2009
- Owens GP, Steger MF, Whitesell AA, Herrera CJ. Posttraumatic stress disorder, guilt, depression, and meaning in life among military veterans. Journal of Traumatic Stress 2009;22(6):654-7. [DOI: 10.1002/jts.20460] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ozbay 2007
- Ozbay F, Johnson DC, Dimoulas E, Morgan CA, Charney D 3rd, Southwick SM. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry 2007;4(5):35-40. [PMC2921311] [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Ozer 2003
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychological Bulletin 2003;129(1):52-73. [DOI: 10.1037/0033-2909.129.1.52] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pace 2009
- Pace TW, Negi LT, Adame DD, Cole SP, Sivilli TI, Brown TD, et al. Effect of compassion meditation on neuroendocrine, innate immune and behavioral responses to psychosocial stress. Psychoneuroendocrinology 2009;34(1):87–98. [10.1016/j.psyneuen.2008.08.011] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Padesky 2012
- Padesky CA, Mooney KA. Strengths-based cognitive-behavioural therapy: a four-step model to build resilience. Clinical Psychology & Psychotherapy 2012;19(4):283-90. [DOI: 10.1002/cpp.1795] [PMID: ] [DOI] [PubMed] [Google Scholar]
Page 2005
- Page K. Subjective Wellbeing in the Workplace [BA thesis]. Geelong (VIC): Deakin University, 2005. [Google Scholar]
Page 2019
- Page MJ, Higgins JP, Sterne JA. Chapter 13: Assessing risk of bias due to missing results in a synthesis. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Paige 2015
- Paige JT, Arora S, Fernandez G, Seymour N. Debriefing 101: training faculty to promote learning in simulation-based training. American Journal of Surgery 2015;209(1):126-31. [DOI: 10.1016/j.amjsurg.2014.05.034] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pallavicini 2016
- Pallavicini F, Argenton L, Toniazzi N, Aceti L, Mantovani F. Virtual reality applications for stress management training in the military. Aerospace Medicine and Human Performance 2016;87(12):1021-30. [DOI: 10.3357/AMHP.4596.2016] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pangallo 2015
- Pangallo A, Zibarras L, Lewis R, Flaxman P. Resilience through the lens of interactionism: a systematic review. Psychological Assessment 2015;27(1):1-20. [DOI: 10.1037/pas0000024] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pargament 2000
- Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: development and initial validation of the RCOPE. Journal of Clinical Psychology 2000;56(4):519-43. [DOI: ] [PMID: ] [DOI] [PubMed] [Google Scholar]
Park 2008
- Park CL, Edmondson D, Fenster JR, Blank TO. Meaning making and psychological adjustment following cancer: the mediating roles of growth, life meaning, and restored just-world beliefs. Journal of Consulting and Clinical Psychology 2008;76(5):863-75. [DOI: 10.1037/a0013348] [PMID: ] [DOI] [PubMed] [Google Scholar]
Park 2015
- Park M, Chang ER, You S. Protective role of coping flexibility in PTSD and depressive symptoms following trauma. Personality and Individual Differences 2015;82:102-6. [DOI: 10.1016/j.paid.2015.03.007] [DOI] [Google Scholar]
Paterson 2013
- Paterson C, Jones M, Rattray J, Lauder W. Exploring the relationship between coping, social support and health-related quality of life for prostate cancer survivors: a review of the literature. European Journal of Oncology Nursing 2013;17(6):750-9. [DOI: 10.1016/j.ejon.2013.04.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pesantes 2015
- Pesantes MA, Lazo-Porras M, Abu Dabrh AM, Ávila-Ramírez JR, Caycho M, Villamonte GY, et al. Resilience in vulnerable populations with type 2 diabetes mellitus and hypertension: a systematic review and meta-analysis. Canadian Journal of Cardiology 2015;31(9):1180-8. [DOI: 10.1016/j.cjca.2015.06.003] [PMC4556590] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Peter 2012
- Peter C, Müller R, Cieza A, Geyh S. Psychological resources in spinal cord injury: a systematic literature review. Spinal Cord 2012;50(3):188-201. [DOI: 10.1038/sc.2011.125] [PMID: ] [DOI] [PubMed] [Google Scholar]
Peters 2008
- Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. Journal of Clinical Epidemiology 2008;61(10):991-6. [DOI: 10.1016/j.jclinepi.2007.11.010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Peters 2010
- Peters ML, Flink IK, Boersma K, Linton SJ. Manipulating optimism: can imagining a best possible self be used to increase positive future expectancies? Journal of Positive Psycholology 2010;5(3):204-11. [DOI: 10.1080/17439761003790963] [DOI] [Google Scholar]
Peterson 2000
- Peterson C. The future of optimism. American Psychologist 2000;55(1):44–55. [DOI: 10.1037//0003-066X.55.1.44] [DOI] [PubMed] [Google Scholar]
Petree 2012
- Petree RD, Broome KM, Bennett JB. Exploring and reducing stress in young restaurant workers: results of a randomized field trial. American Journal of Health Promotion 2012;26(4):217-24. [DOI: 10.4278/ajhp.091001-QUAN-321] [PMID: ] [DOI] [PubMed] [Google Scholar]
Petriwskyj 2016
- Petriwskyj A, Parker D, O'Dwyer S, Moyle W, Nucifora N. Interventions to build resilience in family caregivers of people living with dementia: a comprehensive systematic review. JBI Database of Systematic Reviews and Implementation Reports 2016;14(6):238-73. [DOI: 10.11124/JBISRIR-2016-002555] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pezaro 2017
- Pezaro S, Clyne W, Fulton EA. A systematic mixed-methods review of interventions, outcomes and experiences for midwives and student midwives in work-related psychological distress. Midwifery 2017;50:163-73. [DOI: 10.1016/j.midw.2017.04.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Piepho 2012
- Piepho HP, Williams ER, Madden LV. The use of two-way linear mixed models in multitreatment meta-analysis. Biometrics 2012;68(4):1269-77. [DOI: 10.1111/j.1541-0420.2012.01786.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Piepho 2014
- Piepho HP. Network-meta analysis made easy: detection of inconsistency using factorial analysis-of-variance models. BMC Medical Research Methodology 2014;14:61. [DOI: 10.1186/1471-2288-14-61] [PMC4049370] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pietrzak 2013
- Pietrzak RH, Cook JM. Psychological resilience in older US veterans: results from the national health and resilience in veterans study. Depression and Anxiety 2013;30(5):432-43. [DOI: 10.1002/da.22083] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pine 2007
- Pine R, Tart K. Return on investment: benefits and challenges of baccalaureate nurse residency program. Nursing Economics 2007;25(1):13-8. [PMID: ] [PubMed] [Google Scholar]
Pines 2012
- Pines EW, Rauschhuber ML, Norgan GH, Cook JD, Canchola L, Richardson C, et al. Stress resiliency, psychological empowerment and conflict management styles among baccalaureate nursing students. Journal of Advanced Nursing 2012;68(7):1482-93. [DOI: 10.1111/j.1365-2648.2011.05875.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Porter 2018 [pers comm]
- Porter S. Number of dropouts and number of participants analysed in each group at pre- and post-intervention [personal communication]. Email to: A Kunzler 14 May 2018.
Pragodpol 2013
- Pragodpol P, Ryan C. Critical review of factors predicting health-related quality of life in newly diagnosed coronary artery disease patients. Journal of Cardiovascular Nursing 2013;28(3):277-84. [DOI: 10.1097/JCN.0b013e31824af56e] [PMID: ] [DOI] [PubMed] [Google Scholar]
Prati 2009
- Prati G, Pietrantoni L. Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: a meta-analysis. Journal of Loss and Trauma 2009;14(5):364-88. [DOI: 10.1080/15325020902724271] [DOI] [Google Scholar]
Quale 2010
- Quale AJ, Schanke AK. Resilience in the face of coping with a severe physical injury: a study of trajectories of adjustment in a rehabilitation setting. Rehabilitation Psychology 2010;55(1):12-22. [DOI: 10.1037/a0018415] [PMID: ] [DOI] [PubMed] [Google Scholar]
R 3.6.3 2019 [Computer program]
- R Foundation for Statistical Computing R: a language and environment for statistical computing. R Core Team, Version 3.6.3. Vienna: R Foundation for Statistical Computing, 2019. Available at www.R-project.org/.
Radloff 1977
- Radloff LS. The CES-D scale: a self report depression scale for research in the general population. Applied Psychological Measurement 1977;1(3):385-401. [DOI: 10.1177/014662167700100306] [conservancy.umn.edu/bitstream/handle/11299/98561/v01n3p385.pdf?sequence=1] [DOI] [Google Scholar]
Ratanasiripong 2012
- Ratanasiripong P, Ratanasiripong N, Kathalae D. Biofeedback intervention for stress and anxiety among nursing students: a randomized controlled trial. ISRN Nursing 2012;2012:827972. [DOI: 10.5402/2012/827972] [PMC3395228] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Recabarren 2019 [pers comm]
- Recabarren R. Subgroup outcome data for all outcomes for psychology students [personal communication]. Email to: A Kunzler 4 September 2019.
Regehr 2013
- Regehr C, Glancy D, Pitts A. Interventions to reduce stress in university students: a review and meta-analysis. Journal of Affective Disorders 2013;148(1):1–11. [DOI: 10.1016/j.jad.2012.11.026] [PMID: 23246209 ] [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rew 2003
- Rew L, Horner SD. Youth resilience framework for reducing health-risk behaviors in adolescents. Journal of Pediatric Nursing 2003;18(6):379-88. [DOI: 10.1016/S0882-5963(03)00162-3] [PMID: ] [DOI] [PubMed] [Google Scholar]
Reyes 2018
- Reyes AT, Kearney CA, Lee H, Isla K, Estrada J. Interventions for posttraumatic stress with resilience as outcome: an integrative review. Issues in Mental Health Nursing 2018;39(2):166-78. [DOI: 10.1080/01612840.2017.1390801] [PMID: ] [DOI] [PubMed] [Google Scholar]
Robertson 2015
- Robertson IT, Cooper CL, Sarkar M, Curran T. Resilience training in the workplace from 2003 to 2014: a systematic review. Journal of Occupational and Organizational Psychology 2015;88(3):533-62. [DOI: 10.1111/joop.12120] [DOI] [Google Scholar]
Rocha‐Singh 1994
- Rocha-Singh IA. Perceived stress among graduate students: development and validation of the Graduate Stress Inventory. Educational and Psychological Measurement 1994;54(3):714-27. [DOI: 10.1177/0013164494054003018] [DOI] [Google Scholar]
Rogers 2016
- Rogers D. Which educational interventions improve healthcare professionals' resilience? Medical Teacher 2016;38(12):1236-41. [DOI: 10.1080/0142159x.2016.1210111] [DOI] [PubMed] [Google Scholar]
Rose 2013
- Rose RD, Buckey JC Jr, Zbozinek TD, Motivala SJ, Glenn DE, Cartreine JA, et al. A randomized controlled trial of a self-guided, multimedia, stress management and resilience training program. Behaviour Research and Therapy 2013;51(2):106-12. [DOI: 10.1016/j.brat.2012.11.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rosenberg 1965
- Rosenberg M. Society and the Adolescent Self-Image. Princeton (NJ): Princeton University Press, 1965. [Google Scholar]
Rutten 2013
- Rutten BP, Hammels C, Geschwind N, Menne-Lothmann C, Pishva E, Schruers K, et al. Resilience in mental health: linking psychological and neurobiological perspectives. Acta Psychiatrica Scandinavica 2013;128(1):3-20. [DOI: 10.1111/acps.12095] [PMC3746114] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ryan 2014
- Ryan A. ACT and be READY: Evaluation of an ACT-based Resilience Training Program Delivered to People with Diabetes [PhD thesis]. Brisbane (QLD): University of Queensland, 2014. [Google Scholar]
Ryff 1989
- Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology 1989;57(6):1069-81. [DOI: 10.1037/0022-3514.57.6.1069] [DOI] [Google Scholar]
Rücker 2011
- Rücker G, Schwarzer G, Carpenter JR, Binder H, Schumacher M. Treatment-effect estimates adjusted for small-study effects via a limit meta-analysis. Biostatistics 2011;12(1):122-42. [DOI: 10.1093/biostatistics/kxq046] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rücker 2020 [Computer program]
- Netmeta: network meta-analysis using frequentist methods. Rücker G, Schwarzer G, Krahn U, König J, Version 1.2-1. Freiburg: Guido Schwarzer, 2020. Available at CRAN.R-project.org/package=netmeta.
Sadow 1993
- Sadow D, Hopkins B. Resiliency training and empowerment among homeless, substance-abusing veterans: increasing a sense of self-efficacy and internal attribution of control as a result of resiliency training. Research Communications in Psychology, Psychiatry & Behavior 1993;18(3-4):121-34. [psycnet.apa.org/record/1997-71085-001] [Google Scholar]
Sahler 2013
- Sahler OJ, Dolgin MJ, Phipps S, Fairclough DL, Askins MA, Katz ER, et al. Specificity of problem-solving skills training in mothers of children newly diagnosed with cancer: results of a multisite randomized clinical trial. Journal of Clinical Oncology 2013;31(10):1329-35. [DOI: 10.1200/JCO.2011.39.1870] [ClinicalTrials.gov: NCT00234793] [PMC3607672] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Saksvik 2011
- Saksvik IB, Bjorvatn B, Hetland H, Sandal GM, Pallesen S. Individual differences in tolerance to shift work--a systematic review. Sleep Medicine Reviews 2011;15(4):221-35. [DOI: 10.1016/j.smrv.2010.07.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Salamin 2019
- Salamin V, Ray P, Gothuey I, Corzani S, Martin-Soelch C. An internet-based intervention for the relatives of people with mental illnesses: an open pilot trial with two groups. Swiss Journal of Psychology 2019;78(1-2):15-27. [DOI: 10.1024/1421-0185/a000219] [DOI] [Google Scholar]
Salanti 2008
- Salanti G, Higgins JP, Ades AE, Ioannidis JP. Evaluation of networks of randomized trials. Statistical Methods in Medical Research 2008;17(3):279-301. [DOI: 10.1177/0962280207080643] [PMID: ] [DOI] [PubMed] [Google Scholar]
Salsman 2015
- Salsman JM, Pustejovsky JE, Jim HS, Munoz AR, Merluzzi TV, George L, et al. A meta-analytic approach to examining the correlation between religion/spirituality and mental health in cancer. Cancer 2015;121(21):3769-78. [DOI: 10.1002/cncr.29350] [PMC4618157] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sanderson 2017
- Sanderson B, Brewer M. What do we know about student resilience in health professional education? A scoping review of the literature. Nurse Education Today 2017;58:65-71. [DOI: 10.1016/j.nedt.2017.07.018] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sandman 2015
- Sandman N, Valli K, Kronholm E, Revonsuo A, Laatikainen T, Paunio T. Nightmares: risk factors among the Finnish general adult population. Sleep 2015;38(4):507-14. [DOI: 10.5665/sleep.4560] [PMC4355890] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Santen 2010
- Santen SA, Holt DB, Kemp JD, Hemphill RR. Burnout in medical students: examining the prevalence and associated factors. Southern Medical Journal 2010;103(8):758–63. [DOI: 10.1097/SMJ.0b013e3181e6d6d4] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sapienza 2011
- Sapienza JK, Masten AS. Understanding and promoting resilience in children and youth. Current Opinion in Psychiatry 2011;24(4):267-73. [DOI: 10.1097/YCO.0b013e32834776a8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sarkar 2014
- Sarkar M, Fletcher D. Psychological resilience in sport performers: a review of stressors and protective factors. Journal of Sports Sciences 2014;32(15):1419-34. [DOI: 10.1080/02640414.2014.901551] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sattler 2014
- Sattler DN, Boyd B, Kirsch J. Trauma-exposed firefighters: relationships among posttraumatic growth, posttraumatic stress, resource availability, coping and critical incident stress debriefing experience. Stress & Health 2014;30(5):356-65. [DOI: 10.1002/smi.2608] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schachman 2004
- Schachman KA, Lee RK, Lederma RP. Baby boot camp: facilitating maternal role adaptation among military wives. Nursing Research 2004;53(2):107-15. [DOI: 10.1097/00006199-200403000-00006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schaefer 2013
- Schaefer SM, Morozink Boylan J, Van Reekum CM, Lapate RC, Norris CJ, Ryff CD, et al. Purpose in life predicts better emotional recovery from negative stimuli. PLOS One 2013;8(11):e80329. [DOI: 10.1371/journal.pone.0080329] [PMC3827458] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schaufeli 2002
- Schaufeli WB, Salanova M, González-Romá V, Bakker AB. The measurement of engagement and burnout: a two sample confirmatory factor analytic approach. Journal of Happiness Studies 2002;3:71-92. [DOI: 10.1023/A:1015630930326] [DOI] [Google Scholar]
Scheier 1994
- Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a re-evaluation of the Life Orientation Test. Journal of Personality and Social Psychology 1994;67(6):1063-78. [DOI: 10.1037//0022-3514.67.6.1063] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schnyder 2008
- Schnyder U, Wittmann L, Friedrich-Perez J, Hepp U, Moergeli H. Posttraumatic stress disorder following accidental injury: rule or exception in Switzerland? Psychotherapy and Psychosomatics 2008;77(2):111-8. [DOI: 10.1159/000112888] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schulman 2018 [pers comm]
- Schulman P. Time point of 2 assessment [personal communication]. Email to: A Kunzler 25 June 2018.
Schulz 2010
- Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. [DOI: 10.1136/bmj.c332] [PMC2844940] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schumacher 2005
- Schumacher J, Leppert K, Gunzelmann T, Strauss B, Brähler E. Die Resilienzskala – ein fragebogen zur erfassung der psychischen widerstandsfähigkeit als personmerkmal. Zeitschrift für Klinische Psychologie, Psychiatrie und Psychotherapie 2005;53:16–39. [No DOI or other object identifier available] [Google Scholar]
Schumm 2006
- Schumm JA, Briggs-Phillips M, Hobfoll SE. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among inner-city women. Journal of Traumatic Stress 2006;19(6):825-36. [DOI: 10.1002/jts.20159] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schwarzer 1995
- Schwarzer R, Jerusalem M. Generalized Self-Efficacy Scale. In: Weinman J, Wright S, Johnston M, editors(s). Measures in Health Psychology: A User’s Portfolio. Causal and Control Beliefs. 35–7 edition. Windsor (UK): NFER-NELSON, 1995. [Google Scholar]
Schwarzer 2008
- Schwarzer R, Hallum S. Perceived teacher self-efficacy as a predictor of job stress and burnout: mediation analyses. Applied Psychology 2008;57(S1):152-71. [DOI: 10.1111/j.1464-0597.2008.00359.x] [DOI] [Google Scholar]
Schwarzer 2019 [Computer program]
- metasens: Advanced Statistical Methods to Model and Adjust for Bias in Meta-analysis. Schwarzer G, Carpenter JR, Rücker G, Version 0.4-0. Freiburg: Guido Schwarzer, 2019. Available at CRAN.R-project.org/package=metasens. [CRAN.R-project.org/package=metasens]
Schweitzer 1990
- Schweitzer MB, Paulhan I. Manuel pour L’Inventaire D’Anxiété Trait-État (Forme Y). Bordeaux: Laboratoire de Psychologie de la Santé, Université de Bordeaux II, 1990. [Google Scholar]
Schünemann 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A, editor(s). Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (updated October 2013). GRADE Working Group, 2013. Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html.
Schünemann 2019a
- Schünemann HJ, Vist GE, Higgins JP, Santesso N, Deeks JJ, Glasziou P, et al. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Schünemann 2019b
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl EA, Skoetz N, et al. Chapter 14: Completing ‘Summary of findings’ tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). The Cochrane Collaboration, 2019. Available from www.training.cochrane.org/handbook.
Segovia 2012
- Segovia F, Moore JL, Linnville SE, Hoyt RE, Hain RE. Optimism predicts resilience in repatriated prisoners of war: a 37-year longitudinal study. Journal of Traumatic Stress 2012;25(3):330-6. [DOI: 10.1002/jts.21691] [PMID: ] [DOI] [PubMed] [Google Scholar]
Seligman 1999
- Seligman ME, Schulman P, DeRubeis RJ, Hollon SD. The prevention of depression and anxiety. Prevention and Treatment 1999;2(1):Article 8a. [DOI: 10.1037/1522-3736.2.1.28a] [DOI] [Google Scholar]
Seligman 2005
- Seligman MEP, Steen TA, Park N, Peterson C. Positive psychology progress: empirical validation of interventions. American Psychologist 2005;60(5):410-21. [DOI: 10.1037/0003-066X.60.5.410] [PMID: ] [DOI] [PubMed] [Google Scholar]
Senra 2015
- Senra H, Barbosa F, Ferreira P, Vieira CR, Perrin PB, Rogers H, et al. Psychologic adjustment to irreversible vision loss in adults: a systematic review. Ophthalmology 2015;122(4):851-61. [DOI: 10.1016/j.ophtha.2014.10.022] [PMID: ] [DOI] [PubMed] [Google Scholar]
Shand 2015
- Shand LK, Cowlishaw S, Brooker JE, Burney S, Ricciardelli LA. Correlates of post-traumatic stress symptoms and growth in cancer patients: a systematic review and meta-analysis. Psycho-oncology 2015;24(6):624-34. [DOI: 10.1002/pon.3719] [PMID: ] [DOI] [PubMed] [Google Scholar]
Shapiro 2005
- Shapiro SL, Astin JA, Bishop SR, Cordova M. Mindfulness-based stress reduction for health care professionals: results from a randomized trial. International Journal of Stress Management 2005;12(2):164-76. [DOI: 10.1037/1072-5245.12.2.164] [DOI] [Google Scholar]
Sherbourne 1991
- Sherbourne CD, Stewart AL. The MOS social support survey. Social Science & Medicine 1991;32(6):705-14. [DOI: 10.1016/0277-9536(91)90150-b] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sherer 1982
- Sherer M, Maddux JE, Mercandante B, Prentice-Dunn S, Jacobs B, Rogers RW. The Self-efficacy Scale: construction and validation. Psychological Reports 1982;51(2):663-71. [DOI: 10.2466/pr0.1982.51.2.663] [DOI] [Google Scholar]
Shiralkar 2013
- Shiralkar MT, Harris TB, Eddins-Folensbee FF, Coverdale JH. A systematic review of stress-management programs for medical students. Academic Psychiatry 2013;37(3):158-64. [DOI: 10.1176/appi.ap.12010003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Silver 2002
- Silver RC, Holman EA, McIntosh DN, Poulin M, Gil-Rivas V. Nationwide longitudinal study of psychological responses to September 11. JAMA 2002;288(10):1235-44. [DOI: 10.1001/jama.288.10.1235] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sinclair 2004
- Sinclair VG, Wallston KA. The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment 2004;11(1):94-101. [DOI: 10.1177/1073191103258144] [PMID: ] [DOI] [PubMed] [Google Scholar]
Skeffington 2013
- Skeffington PM, Rees CS, Kane R. The primary prevention of PTSD: a systematic review. Journal of Trauma & Dissociation 2013;14(4):404-22. [DOI: 10.1080/15299732.2012.753653] [PMID: ] [DOI] [PubMed] [Google Scholar]
Smith 2007
- Smith C, Hancock H, Blake-Mortimer J, Eckert K. A randomised comparative trial of yoga and relaxation to reduce stress and anxiety. Complementary Therapies in Medicine 2007;15(2):77-83. [DOI: 10.1016/j.ctim.2006.05.001] [PMID: ] [DOI] [PubMed] [Google Scholar]
Smith 2008
- Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The Brief Resilience Scale: assessing the ability to bounce back. International Journal of Behavioral Medicine 2008;15(3):194-200. [DOI: 10.1080/10705500802222972] [PMID: ] [DOI] [PubMed] [Google Scholar]
Smith 2009
- Smith BW, Tooley EM, Montague EQ, Robinson AE, Cosper CJ, Mullins PG. The role of resilience and purpose in life in habituation to heat and cold pain. Journal of Pain 2009;10(5):493-500. [DOI: 10.1016/j.jpain.2008.11.007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Solomon 1988
- Solomon Z, Mikulincer M, Avitzur E. Coping, locus of control, social support, and combat-related posttraumatic stress disorder: a prospective study. Journal of Personality and Social Psychology 1988;55(2):279-85. [DOI: 10.1037//0022-3514.55.2.279] [PMID: ] [DOI] [PubMed] [Google Scholar]
Songprakun 2012
- Songprakun W, McCann TV. Effectiveness of a self-help manual on the promotion of resilience in individuals with depression in Thailand: a randomised controlled trial. BMC Psychiatry 2012;12:12. [DOI: 10.1186/1471-244X-12-12] [Australian New Zealand Clinical Trials Registry: ACTRN12611000905965] [PMC3298500] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sood 2010
- Sood A. Train Your Brain, Engage Your Heart, Transform Your Life: A Two Step Program to Enhance Attention; Decrease Stress; Cultivate Peace, Joy and Resilience; and Practice Presence with Love. A course in Attention & Interpretation Therapy (AIT). Rochester (MN): Morning Dew Publications, 2010. [Google Scholar]
Sood 2011
- Sood A, Prasad K, Schroeder D, Varkey P. Stress management and resilience training among Department of Medicine faculty: a pilot randomized clinical trial. Journal of General Internal Medicine 2011;26(8):858-61. [DOI: 10.1007/s11606-011-1640-x] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sood 2014
- Sood A, Sharma V, Schroeder DR, Gorman B. Stress management and resiliency training (SMART) program among Department of Radiology faculty: a pilot randomized clinical trial. Explore 2014;10(6):358-63. [DOI: 10.1016/j.explore.2014.08.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Southwick 2005
- Southwick SM, Vythilingam M, Charney DS. The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annual Review of Clinical Psychology 2005;1:255-91. [DOI: 10.1146/annurev.clinpsy.1.102803.143948] [PMID: ] [DOI] [PubMed] [Google Scholar]
Southwick 2011
- Southwick SM, Pietrzak RH, White G. Interventions to enhance resilience and resilience-related constructs in adults. In: Southwick SM, Litz BT, Charney DS, Friedman MJ, editors(s). Resilience and Mental Health: Challenges Across the Lifespan. Cambridge: Cambridge University Press, 2011:289-306. [DOI: 10.1017/CBO9780511994791.022] [DOI] [Google Scholar]
Southwick 2012
- Southwick SM, Charney DS (editors). Resilience: The Science of Mastering Life's Greatest Challenges. Cambridge: Cambridge University Press, 2012. [Google Scholar]
Spielberger 1970
- Spielberger CD, Gorsuch RL, Lushene RE. STAI Manual for the State-Trait Anxiety Inventory. Palo Alto (CA): Consulting Psychologists Press, 1970. [Google Scholar]
Spielberger 1983
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto (CA): Consulting Psychologists Press, 1983. [Google Scholar]
Spitzer 1999
- Spitzer RL, Kroenke K, Williams JB, Patient Health Questionnaire Primary Study Group. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA 1999;282(18):1737-44. [DOI: 10.1001/jama.282.18.1737] [PMID: ] [DOI] [PubMed] [Google Scholar]
Spitzer 2006
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine 2006;166(10):1092-7. [DOI: 10.1001/archinte.166.10.1092] [PMID: ] [DOI] [PubMed] [Google Scholar]
Stahl 2010
- Stahl B, Goldstein E. A Mindfulness-Based Stress Reduction Workbook. Oakland (CA): New Harbinger Publications, 2010. [Google Scholar]
Steinhardt 2008
- Steinhardt MA, Dolbier CL. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. Journal of American College Health 2008;56(4):445-53. [DOI: 10.3200/JACH.56.44.445-454] [PMID: ] [DOI] [PubMed] [Google Scholar]
Steinman 2014
- Steinman SA, Teachman BA. Reaching new heights: Comparing interpretation bias modification to exposure therapy for extreme height fear. Journal of Consulting and Clinical Psychology 2014;82(3):404–17. [DOI: 10.1037/a0036023] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stephens 2013
- Stephens TM. Nursing student resilience: a concept clarification. Nursing Forum 2013;48(2):125-33. [DOI: 10.1111/nuf.12015] [PMID: ] [DOI] [PubMed] [Google Scholar]
Stephens 2018 [pers comm]
- Stephens TM. Number of participants analysed at each time point [personal communication]. Email to: A Kunzler 24 July 2018.
Stewart 2011
- Stewart DE, Yuen T. A systematic review of resilience in the physically ill. Psychosomatics 2011;52(3):199-209. [DOI: 10.1016/j.psym.2011.01.036] [PMID: ] [DOI] [PubMed] [Google Scholar]
Storebø 2020
- Storebø OJ, Stoffers-Winterling JM, Völlm BA, Kongerslev MT, Mattivi JT, Jørgensen MS, et al. Psychological therapies for people with borderline personality disorder. Cochrane Database of Systematic Reviews 2020, Issue 5. Art. No: CD012955. [DOI: 10.1002/14651858.CD012955.pub2] [PMC7199382] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Strand 2006
- Strand EB, Zautra AJ, Thoresen M, Ødegård S, Uhlig T, Finset A. Positive affect as a factor of resilience in the pain-negative affect relationship in patients with rheumatoid arthritis. Journal of Psychosomatic Research 2006;60(5):477-84. [DOI: 10.1016/j.jpsychores.2005.08.010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sumer 2005
- Sumer N, Karanci AN, Berument SK, Gunes H. Personal resources, coping self-efficacy, and quake exposure as predictors of psychological distress following the 1999 earthquake in Turkey. Journal of Traumatic Stress 2005;18(4):331-42. [DOI: 10.1002/jts.20032] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tams 2016
- Tams R, Prangnell SJ, Daisley A. Helping families thrive in the face of uncertainty: strengths based approaches to working with families affected by progressive neurological illness. NeuroRehabilitation 2016;38(3):257-70. [DOI: 10.3233/nre-161317] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tan 2016
- Tan KK, Chan SW, Wang W, Vehviläinen-Julkunen K. A salutogenic program to enhance sense of coherence and quality of life for older people in the community: a feasibility randomized controlled trial and process evaluation. Patient Education and Counseling 2016;99(1):108-16. [DOI: 10.1016/j.pec.2015.08.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Taylor 1983
- Taylor KM, Betz NE. Applications of self-efficacy theory to the understanding and treatment of career indecision. Journal of Vocational Behavior 1983;22(1):63-81. [DOI: 10.1016/0001-8791(83)90006-4] [DOI] [Google Scholar]
Tedeschi 1996
- Tedeschi RG, Calhoun LG. The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. Journal of Traumatic Stress 1996;9(3):455-71. [DOI: 10.1007/bf02103658] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tempski 2012
- Tempski P, Martins MA, Paro HB. Teaching and learning resilience: a new agenda in medical education? Medical Education 2012;46(4):345-6. [DOI: 10.1111/j.1365-2923.2011.04207.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Thomas 2016
- Thomas LJ, Revell SH. Resilience in nursing students: an integrative review. Nurse Education Today 2016;36:457-62. [DOI: 10.1016/j.nedt.2015.10.01] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tilden 1990
- Tilden VP, Nelson CA, May BA. The IPR inventory: development and psychometric characteristics. Nursing Research 1990;39(6):337-43. [PMID: ] [PubMed] [Google Scholar]
Townshend 2016
- Townshend K, Jordan Z, Stephenson M, Tsey K. The effectiveness of mindful parenting programs in promoting parents' and children's wellbeing: a systematic review. JBI Database of Systematic Reviews and Implementation Reports 2016;14(3):139-80. [DOI: 10.11124/JBISRIR-2016-2314] [PMID: ] [DOI] [PubMed] [Google Scholar]
Truitt 2012
- Truitt M, Biesecker B, Capone G, Bailey T, Erby L. The role of hope in adaptation to uncertainty: the experience of caregivers of children with Down syndrome. Patient Education and Counseling 2012;87(2):233-8. [DOI: 10.1016/j.pec.2011.08.015] [PMC3816013] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsai 2015
- Tsai J, El-Gabalawy R, Sledge WH, Southwick SM, Pietrzak RH. Post-traumatic growth among veterans in the USA: results from the National Health and Resilience in Veterans Study. Psychological Medicine 2015;45(1):165-79. [DOI: 10.1017/S0033291714001202] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tsai 2016
- Tsai J, Sippel LM, Mota N, Southwick SM, Pietrzak RH. Longitudinal course of posttraumatic growth among US military veterans: results from the National Health and Resilience in Veterans Study. Depression and Anxiety 2016;33(1):9-18. [DOI: 10.1002/da.22371] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tschannen‐Moran 2001
- Tschannen-Moran M, Hoy AW. Teacher efficacy: capturing an elusive construct. Teaching and Teacher Education 2001;17(7):783-805. [DOI: 10.1016/S0742-051X(01)00036-1] [DOI] [Google Scholar]
Tung 2018
- Tung YJ, Lo KK, Ho RC, Tam WS. Prevalence of depression among nursing students: a systematic review and meta-analysis. Nurse Education Today 2018;63:119-29. [DOI: 10.1016/j.nedt.2018.01.009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Turner 2017
- Turner K, McCarthy VL. Stress and anxiety among nursing students: a review of intervention strategies in literature between 2009 and 2015. Nurse Education in Practice 2017;22:21-9. [DOI: 10.1016/j.nepr.2016.11.002] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ungar 2008
- Ungar M, Liebenberg L, Boothroyd R, Kwong WM, Lee TY, Leblanc J, et al. The study of youth resilience across cultures: lessons from a pilot study of measurement development. Research in Human Development 2008;5(3):166-80. [DOI: 10.1080/15427600802274019] [DOI] [Google Scholar]
Van der Kleij 2011
- Van der Kleij R, Molenaar D, Schraagen JM. Making teams more resilient: effects of shared transformational leadership training on resilience. Proceedings of the Human Factors and Ergonomics Society Annual Meeting 2011;55(1):2158-62. [DOI: 10.1177/1071181311551450] [DOI] [Google Scholar]
Van Kessel 2013
- Van Kessel G. The ability of older people to overcome adversity: a review of the resilience concept. Geriatric Nursing 2013;34(2):122-7. [DOI: 10.1016/j.gerinurse.2012.12.011] [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Kessel 2014
- Van Kessel G, MacDougall C, Gibbs L. Resilience-rhetoric to reality: a systematic review of intervention studies after disasters. Disaster Medicine and Public Health Preparedness 2014;8(5):452-60. [DOI: 10.1017/dmp.2014.104] [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Leeuwen 2012
- Van Leeuwen CM, Kraaijeveld S, Lindeman E, Post MW. Associations between psychological factors and quality of life ratings in persons with spinal cord injury: a systematic review. Spinal Cord 2012;50(3):174-87. [DOI: 10.1038/sc.2011.120] [PMID: ] [DOI] [PubMed] [Google Scholar]
Vanhove 2016
- Vanhove AJ, Herian MN, Perez AL, Harms PD, Lester PB. Can resilience be developed at work? A meta-analytic review of resilience-building programme effectiveness. Journal of Occupational and Organizational Psychology 2016;89(2):278-307. [DOI: 10.1111/joop.12123] [DOI] [Google Scholar]
Verma 2011
- Verma R, Balhara YP, Gupta CS. Gender differences in stress response: role of developmental and biological determinants. Industrial Psychiatry Journal 2011;20(1):4-10. [DOI: 10.4103/0972-6748.98407] [PMC3425245] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Victor 2019 [pers comm]
- Victor P. Subgroup outcome data of psychology students [personal communication]. Email to: A Kunzler 28 August 2019.
Viechtbauer 2010
- Viechtbauer W. Conducting meta-analyses in R with the metafor package. Journal of Statistical Software 2010;36(3):1–48. [DOI: 10.18637/jss.v036.i03] [DOI] [Google Scholar]
Visser 2010
- Visser A, Garssen B, Vingerhoets A. Spirituality and well-being in cancer patients: a review. Psycho-oncology 2010;19(6):565-72. [DOI: 10.1002/pon.1626] [PMID: ] [DOI] [PubMed] [Google Scholar]
Waddell 2009
- Waddell J, Donner GJ, Wheeler MM. Building your Nursing Career: A Guide for Students. 3rd edition. Toronto: Mosby/Elsevier, 2009. [Google Scholar]
Wade 2001
- Wade SL, Borawski EA, Taylor HG, Drotar D, Yeates KO, Stancin T. The relationship of caregiver coping to family outcomes during the initial year following pediatric traumatic injury. Journal of Consulting and Clinical Psychology 2001;69(3):406-15. [DOI: 10.1037//0022-006x.69.3.406] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wagnild 1993
- Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. Journal of Nursing Measurement 1993;1(2):165-78. [PMID: ] [PubMed] [Google Scholar]
Wagnild 2009
- Wagnild GM. The Resilience Scale User’s Guide: for the US English Version of the Resilience Scale and the 14-item Resilience Scale (RS-14). Worden (MT): Resilience Center, 2009. [Google Scholar]
Wainwright 2019
- Wainwright E, Wainwright D, Coghill N, Walsh J, Perry R. Resilience and return-to-work pain interventions: systematic review. Occupational Medicine 2019;69(3):163-76. [DOI: 10.1093/occmed/kqz012] [PMID: ] [DOI] [PubMed] [Google Scholar]
Waite 2004
- Waite PJ, Richardson GE. Determining the efficacy of resiliency training in the work site. Journal of Allied Health 2004;33(3):178-83. [PMID: ] [PubMed] [Google Scholar]
Walker 1987
- Walker SN, Sechrist KR, Pender NJ. The Health-Promoting Lifestyle Profile: development and psychometric characteristics. Nursing Research 1987;36(2):76-81. [PMID: ] [PubMed] [Google Scholar]
Walsh 2002
- Walsh K, King M, Jones L, Tookman A, Blizard R. Spiritual beliefs may affect outcome of bereavement: prospective study. BMJ 2002;324(7353):1551. [DOI: 10.1136/bmj.324.7353.1551] [PMC116607] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Walton 2011
- Walton GM, Cohen GL. A brief social-belonging intervention improves academic and health outcomes of minority students. Science 2011;331(6023):1447-51. [DOI: 10.1126/science.1198364] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wang 1999
- Wang XD, Wang XL. Rating Scales for Mental Health. Beijing: Chinese Mental Health Journal Press, 1999. [Google Scholar]
Wang 2014
- Wang F, Liu J, Liu L, Wang F, Ma Z, Gao D, et al. The status and correlates of depression and anxiety among breast-cancer survivors in Eastern China: a population-based, cross-sectional case–control study. BMC Public Health 2014;14:326. [DOI: 10.1186/1471-2458-14-326] [PMC3997219] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ware 1994
- Ware JE, Kosinski M, Keller SD. SF-36 Physical and Mental Health Summary Scales: A User’s Manual. Boston (MA): Health Institute, New England Medical Center, 1994. [Google Scholar]
Warnecke 2019 [pers comm]
- Warnecke E. Post-intervention means and SDs for both primary and secondary outcomes in both groups with number of participants analysed [personal communication]. Email to: A Kunzler 12 September 2019.
Watson 1988
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology 1988;54(6):1063-70. [DOI: 10.1037//0022-3514.54.6.1063] [PMID: ] [DOI] [PubMed] [Google Scholar]
Watson 1994
- Watson D, Clark LA. The PANAS-X: Manual for the Positive and Negative Affect Schedule - Expanded Form. Ames (IA): University of Iowa, 1994. [10.17077/48vt-m4t2] [Google Scholar]
Watson 2008
- Watson J. Nursing: The Philosophy and Science of Caring. Boulder (CO): University Press of Colorado, 2008. [Google Scholar]
Waysman 2001
- Waysman M, Schwarzwald J, Solomon Z. Hardiness: an examination of its relationship with positive and negative long term changes following trauma. Journal of Traumatic Stress 2001;14(3):531-48. [DOI: 10.1023/A:1011112723704] [PMID: ] [DOI] [PubMed] [Google Scholar]
Weiss 2002
- Weiss MJ. Hardiness and social support as predictors of stress in mothers of typical children, children with autism, and children with mental retardation. Autism 2002;6(1):115-30. [DOI: 10.1177/1362361302006001009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Werner 1992
- Werner EE, Smith RS. Overcoming the Odds: High Risk Children from Birth to Adulthood. Ithaca (NY): Cornell University Press, 1992. [Google Scholar]
Werner 2001
- Werner EE, Smith RS. Journeys from Childhood to Midlife: Risk, Resilience and Recovery. Ithaca (NY): Cornell University Press, 2001. [DOI] [PubMed] [Google Scholar]
White 2005
- White IR, Thomas J. Standardized mean differences in individually-randomized and cluster-randomized trials, with applications to meta-analysis. Clinical Trials 2005;2(2):141-51. [DOI: 10.1191/1740774505cn081oa] [PMID: ] [DOI] [PubMed] [Google Scholar]
White 2012a
- White JH, Magin P, Attia J, Sturm J, Carter G, Pollack M. Trajectories of psychological distress after stroke. Annals of Family Medicine 2012;10(5):435-42. [DOI: 10.1370/afm.1374] [PMC3438211] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
White 2012b
- White IR, Barrett JK, Jackson D, Higgins JP. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Research Synthesis Methods 2012;3(2):111-25. [DOI: 10.1002/jrsm.1045] [PMC4433771] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Whiting‐O'Keefe 1984
- Whiting-O'Keefe QE, Henke C, Simborg DW. Choosing the correct unit of analysis in medical care experiments. Medical Care 1984;22(12):1101-14. [DOI: 10.1097/00005650-198412000-00005] [PMID: ] [DOI] [PubMed] [Google Scholar]
WHO 1986
- World Health Organization. Ottawa Charter for Health Promotion. www.euro.who.int/__data/assets/pdf_file/0004/129532/Ottawa_Charter.pdf?ua=1 1986.
WHO 1996
- World Health Organization, Division of Mental Health. WHOQOL-BREF: Introduction, Administration, Scoring and Generic Version of the Assessment. Field Trial Version. apps.who.int/iris/bitstream/handle/10665/63529/WHOQOL-BREF.pdf?sequence=1&isAllowed=y 1996. [www.who.int/iris/handle/10665/63529]
WHO 2004
- World Health Organization. Promoting Mental Health: Concepts, Emerging Evidence, Practice: Summary Report. www.who.int/mental_health/evidence/en/promoting_mhh.pdf 2004.
WHO 2019
- World Health Organization. Gender and women's mental health. Gender disparities and mental health: the facts. www.who.int/mental_health/prevention/genderwomen/en/ (accessed 29 April 2020).
WHOQOL Group 1998
- WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine 1998;28(3):551-8. [DOI: 10.1017/s0033291798006667] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wild 2016
- Wild J. An Evaluation of Mind's Resilience Intervention for Emergency Workers. Oxford: University of Oxford, 2016. [www.mind.org.uk/media/4627959/strand-3.pdf] [Google Scholar]
Wild 2018 [pers comm]
- Wild J. Information if trial was completed and published; inquiry for provision of summary data [personal communication]. Email to: A Kunzler 5 August 2018.
Wilks 2010
- Wilks SE, Spivey CA. Resilience in undergraduate social work students: social support and adjustment to academic stress. Social Work Education 2010;29(3):276-88. [DOI: 10.1080/02615470902912243] [DOI] [Google Scholar]
Williams 1997
- Williams RA. Psychometrics of the Coping Styles Questionnaire (CSQ). Ann Arbo (MI): University of Michigan, 1997. [Google Scholar]
Williams 2011
- Williams M, Penman D. Mindfulness: A Practical Guide to Finding Peace in a Frantic World. London: Piatkus, 2011. [Google Scholar]
Williams 2015
- Williams D, Tricomi G, Gupta J, Janise A. Efficacy of burnout interventions in the medical education pipeline. Academic Psychiatry 2015;39(1):47–54. [DOI: 10.1007/s40596-014-0197-5] [PMID: ] [DOI] [PubMed] [Google Scholar]
Windle 2008
- Windle G, Markland DA, Woods RT. Examination of a theoretical model of psychological resilience in older age. Aging & Mental Health 2008;12(3):285-92. [DOI: 10.1080/13607860802120763] [PMID: ] [DOI] [PubMed] [Google Scholar]
Windle 2011a
- Windle G. What is resilience? A review and concept analysis. Reviews in Clinical Gerontology 2011;21(2):152-69. [DOI: 10.1017/S0959259810000420] [DOI] [Google Scholar]
Windle 2011b
- Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health and Quality of Life Outcomes 2011;9:8. [DOI: 10.1186/1477-7525-9-8] [PMC3042897] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Winger 2016
- Winger JG, Adams RN, Mosher CE. Relations of meaning in life and sense of coherence to distress in cancer patients: a meta-analysis. Psycho-oncology 2016;25(1):2-10. [DOI: 10.1002/pon.3798] [PMC4575247] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Winwood 2013
- Winwood PC, Colon R, McEwen K. A practical measure of workplace resilience: developing the resilience at work scale. Journal of Occupational and Environmental Medicine 2013;55(10):1205-12. [DOI: 10.1097/JOM.0b013e3182a2a60a] [PMID: ] [DOI] [PubMed] [Google Scholar]
Wolfe 2004
- Wolfe F. Fatigue assessments in rheumatoid arthritis: comparative performance of visual analog scales and longer fatigue questionnaires in 7760 patients. Journal of Rheumatology 2004;31(10):1896-902. [PMID: ] [PubMed] [Google Scholar]
Wolpe 1958
- Wolpe J. Psychotherapy by Reciprocal Inhibition. Stanford (CA): Stanford University Press, 1958. [Google Scholar]
Wright 2008
- Wright LJ, Zautra AJ, Going S. Adaptation to early knee osteoarthritis: the role of risk, resilience, and disease severity on pain and physical functioning. Annals of Behavioral Medicine 2008;36(1):70-80. [DOI: 10.1007/s12160-008-9048-5] [PMC2613296] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wright 2019
- Wright B, Richmond Mynett J. Training medical students to manage difficult circumstances - a curriculum for resilience and resourcefulness? BMC Medical Education 2019;19:280. [DOI: 10.1186/s12909-019-1712-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2013
- Wu G, Feder A, Cohen H, Kim JJ, Calderon S, Charney DS, et al. Understanding resilience. Frontiers in Behavioral Neuroscience 2013;7:10. [DOI: 10.3389/fnbeh.2013.00010] [PMC3573269] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Xu 2008
- Xu H. Construction of an Early Warning Index System and Information Evaluation System for College Students' Psychological Crisis [Masters thesis]. BeiBei District (CQ): Southwest University, 2008. [Google Scholar]
Yamada 2014
- Yamada Y, Klugar M, Ivanova K, Oborna I. Psychological distress and academic self-perception among international medical students: the role of peer social support. BMC Medical Education 2014;14:256. [DOI: 10.1186/s12909-014-0256-3] [PMC4251849] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ye 2018
- Ye Y, Hu R, Ni Z, Jiang N, Jiang X. Effects of perceived stress and professional values on clinical performance in practice nursing students: a structural equation modeling approach. Nurse Education Today 2018;71:157-62. [DOI: 10.1016/j.nedt.2018.09.036] [PMID: ] [DOI] [PubMed] [Google Scholar]
Yeager 2011
- Yeager D, Miu AS. Implicit theories of personality predict motivation to use prosocial coping strategies after bullying in high school. In: Frydenberg E, Reevy G, editors(s). Personality, stress and coping: implications for education. Charlotte, NC: Information Age Publications, 2011:47-62. [Google Scholar]
Yeager 2013a
- Yeager DS, Trzesniewski KH, Dweck CS. An implicit theories of personality intervention reduces adolescent aggression in response to victimization and exclusion. Child Development 2013;84(3):970-88. [DOI: 10.1111/cdev.12003] [PMC3660787] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yeager 2013b
- Yeager DS, Miu AS, Powers J, Dweck CS. Implicit theories of personality and attributions of hostile intent: a meta-analysis, an experiment, and a longitudinal intervention. Child Development 2013;84(5):1651-67. [DOI: 10.1111/cdev.12062] [PMID: ] [DOI] [PubMed] [Google Scholar]
Yeghnazar 2019 [pers comm]
- Yeghnazar P. Subgroup data for graduate students in health professions [personal communication]. Email to: A Kunzler 8 August 2019.
Yu 2007
- Yu X, Zhang J. Factor analysis and psychometric evaluation of the Connor-Davidson Resilience Scale (CD-RISC) with Chinese people. Social Behavior and Personality: An International Journal 2007;35(1):19-30. [DOI: 10.2224/sbp.2007.35.1.19] [DOI] [Google Scholar]
Zauszniewski 2010
- Zauszniewski JA, Bekhet AK, Suresky MJ. Resilience in family members of persons with serious mental illness. Nursing Clinics of North America 2010;45(4):613-26. [DOI: 10.1016/j.cnur.2010.06.007] [PMID: ] [DOI] [PubMed] [Google Scholar]
Zautra 2005
- Zautra AJ, Johnson LM, Davis MC. Positive affect as a source of resilience for women in chronic pain. Journal of Consulting and Clinical Psychology 2005;73(2):212-20. [DOI: 10.1037/0022-006X.73.2.212] [NIHMS71708] [PMC2593933] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zigmond 1983
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica 1983;67(6):361–70. [DOI: 10.1111/j.1600-0447.1983.tb09716.x] [6880820] [DOI] [PubMed] [Google Scholar]
Zimet 1988
- Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. Journal of Personality Assessment 1988;52(1):30-41. [DOI: 10.1207/s15327752jpa5201_2] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Helmreich 2017
- Helmreich I, Kunzler A, Chmitorz A, König J, Binder H, Wessa M, et al. Psychological interventions for resilience enhancement in adults. Cochrane Database of Systematic Reviews 2017, Issue 2. Art. No: CD012527. [DOI: 10.1002/14651858.CD012527] [DOI] [PMC free article] [PubMed] [Google Scholar]


