Abstract
Background
Ocular injury is a preventable cause of blindness, yet it remains a significant disabling health problem that affects all age groups. Injuries may occur in the home, in the workplace, during recreational activities or as a result of road crashes. Types of injuries vary from closed globe (contusion or lamellar laceration) to an open globe injury, which includes penetration and even perforation of the globe. To date, the main strategy to prevent these injuries has been to educate people to identify high‐risk situations and to take correct action to avoid danger.
Objectives
To assess the evidence for the effectiveness of educational interventions for the prevention of eye injuries.
Search methods
We searched the Cochrane Injuries and the Cochrane Eyes & Vision Group Specialised Registers, CENTRAL (The Cochrane Library 2008, Issue 3), MEDLINE, EMBASE, Current Controlled Trials metaRegister (now includes National Research Register), AgeInfo, HMIC Health Management Information Consortium, WHOLIS (World Health Organization Library Information System), LILACS (Latin American and Caribbean Health Sciences), MEDCARIB (Caribbean Health Sciences Literature), ISI Web of Science: (Science Citation Index Expanded (SCI‐EXPANDED), Social Sciences Citation Index (SSCI) Conference Proceedings Citation Index‐Science (CPCI‐S)), ERIC, ZETOC and SPORTdiscus. We also checked reference lists of relevant papers and contacted study authors in an effort to identify published, unpublished and ongoing trials. Searches were last updated in August 2008.
Selection criteria
We included any randomised controlled trials (RCTs) and controlled before‐and‐after studies which evaluated any educational intervention aimed at preventing eye injuries.
Data collection and analysis
Four authors independently screened the electronic search results and data extracted. Three authors entered data into RevMan 5. As we judged there to be substantial heterogeneity between participants and interventions, we did not pool the studies' results, but have reviewed the results narratively.
Main results
We included two RCTs and three controlled before‐and‐after studies in this review. One study reported eye injuries as an outcome and four studies reported change in behaviour or knowledge.
Authors' conclusions
The included studies do not provide reliable evidence that educational interventions are effective in preventing eye injuries. There is a need for well‐conducted RCTs with adequate allocation concealment and masking (blinding). Studies should have a longer follow‐up time and more studies need to be conducted in low and middle‐income countries.
Keywords: Humans; Health Behavior; Accidents, Occupational; Accidents, Occupational/prevention & control; Athletic Injuries; Athletic Injuries/prevention & control; Eye Injuries; Eye Injuries/prevention & control; Eye Injuries, Penetrating; Eye Injuries, Penetrating/prevention & control; ; /methods; Wounds, Nonpenetrating; Wounds, Nonpenetrating/prevention & control
Plain language summary
Educational interventions for preventing eye injuries
Eye injuries are a preventable cause of blindness, yet remain a significant disabling health problem that affects all age groups. Despite health and safety requirements and widespread legislation, injuries can still occur at home, in the workplace, during recreational activities or as a result of road crashes.
The authors of this review searched for randomised controlled trials and controlled before‐and‐after studies looking at the effectiveness of educational interventions, such as written materials, video or audio tapes, for the prevention of eye injuries. The authors found five studies involving different types of people, using various educational interventions and based in different countries, that met the inclusion criteria. Due to the low quality of the studies identified, the authors concluded that there is no reliable evidence that educational interventions are effective in preventing eye injuries.
The review authors recommend that further high quality randomised controlled trials, with longer follow‐up periods are conducted. More trials should be based in low and middle‐income countries in order to carry out a comparison with those in high‐income countries.
Background
Description of the condition
Ocular injury is a preventable cause of blindness, and yet it remains a significant disabling health problem that affects all age groups. Injuries may occur in the home, in the workplace, during recreational activities or as a result of road crashes. Types of injuries vary from closed globe (contusion or lamellar laceration) to an open globe injury, which includes rupture, penetration, and perforation of the globe. To date, the main strategy to prevent these injuries has been to educate people to identify high‐risk situations and to take correct action to avoid danger.
Information from the World Health Organization (WHO) suggests that over 55 million eye injuries occur each year (Negrel 1998). They report that about 1.6 million people go blind from these injuries, 2.3 million suffer from bilateral low vision and 19 million remain with unilateral blindness or low vision. Data from the United States Eye Injury Register (USEIR) have identified that over 57% of the injuries occur in people under 30 years of age. In children under three years old, injury remains the main cause of eyeball loss (enucleation).
A population‐based survey (Krisnainah 2006) and the USEIR have established that males are more likely to sustain eye injury. Data from the USEIR indicate that over 40% of injuries occur within the home environment. In contrast, data from studies conducted in some developing countries, specifically India and Nepal, identify the mainly‐agricultural work environment (Khatry 2004; Krisnainah 2006) as a higher risk situation. The Birmingham Eye Trauma Terminology (BETT) (Kuhn 2004) has been endorsed as a comprehensive and standardised classification that attempts to address ambiguity in the description of eye injuries. The BETT classification defines all eye injuries as open or closed globe injuries. In the US it has been found that 31% of injuries occur from blunt objects and result in varying degrees of contusion (from 'black eye' to severe intraocular tearing) and, occasionally, rupture of the globe, or blow out fracture of the floor of the orbit. Sharp objects contribute to about 18% of injuries (USEIR). Penetrating injuries and perforating injuries often carry a poor prognosis. The management of each case varies, and is dependent on how far and where the sharp object entered the eye. Intraocular foreign bodies can cause structural damage as well as be toxic to the tissues. These materials vary from plastics and glass to metal, and even plant matter, which can induce an infection. Burns to the eye remain an ophthalmic emergency where the outcome depends upon the concentration and pH of the burning agent. Alkalis are a particular challenge as they penetrate the ocular tissues and cause irreversible damage.
In the UK almost half of all eye emergencies are due to trauma (MacEwen 1999), though injuries within the UK workplace have decreased significantly due to better awareness and the use of eye protection in industrial settings (Canavan 1980). Similarly, eye injuries due to road traffic crashes have decreased in countries where there is widespread use of seat belts and laminated windscreens (Vernon 1984).
Evidence suggests that some population groups are at a greater risk because of increased exposure to hazards that lead to ocular injuries (Negrel 1998). Inability to detect or avoid the risk contributes to higher incidence, particularly in low and middle‐income countries. Worker safety measures in industrialised nations has led to a significant reduction in injuries but these are costly and not universally applied. The key preventive strategy therefore remains with behaviour change of individuals through educational interventions to recognise risks and avoid exposure where possible.
How the intervention might work
Behavioural change may prevent many ocular injuries. Educational interventions have been proposed as a potentially effective approach to assist in bringing about such a change; these may be implemented in conjunction with new or existing legislation/regulations. Lipscomb 2000 has identified that interventions to prevent ocular injuries have been effective when used in conjunction with policy changes in both industrial and agricultural settings. Educational interventions can range from simple printed information such as leaflets, announcements on the radio or television, to intensive safety workshops. These interventions can also range from costing very little to being quite expensive to implement.
Cost and type of intervention will also have a bearing on low and middle‐income countries. A written intervention such as a leaflet or advertisement in a newspaper, whilst effectively cheaper and easier to circulate than holding an intensive workshop, may be limited to those who are literate. Broadcasting on the radio or television might be more effective, but will only reach those who are able to afford electronic equipment. Additionally, educational messages need to be tailored to meet the requirements of the exposed population.
In low and middle‐income countries, the environmental factors, farming techniques, and lack of safety regulation in industrial settings leads to a high burden of injury. The behaviour of an individual is influenced by their own awareness as well as the social and legislative norms held in the community. Therefore to bring about a change in behaviour changes are necessary at multiple levels, and an educational intervention is the most applicable pathway.
Why it is important to do this review
We were unable to identify any evidence that shows the effectiveness of educational interventions for the prevention of eye injuries. Previous reviews Lipscomb 2000 highlight the uncertainty surrounding the effectiveness of educational interventions to prevent eye injuries by bringing about the required behavioural change ‐ with or without legislation. Evidence of the effects of interventions will provide vital information in identifying the most suitable educational method(s) to help bring about a 'cultural' change in behaviour to prevent ocular injuries.
Objectives
To assess the evidence for the effectiveness of educational interventions for the prevention of eye injuries.
Methods
Criteria for considering studies for this review
Types of studies
The following study designs were eligible (definitions from Higgins 2005):
Randomised controlled trials (RCTs) (defined as an experiment in which investigators randomly allocate eligible participants into an intervention group (arm), each of which receives one or more of the interventions that are being compared. The results are assessed by comparing outcomes between the arms).
Cluster‐randomised controlled trials (defined as a trial in which clusters of individuals (for example, clinics, families, geographical areas), rather than individuals themselves, are randomised to different arms).
Controlled before‐and‐after studies (CBAs) (a non‐randomised study design where a control population of similar characteristics and performance as the intervention group is identified. Data are collected before and after the intervention in both the control and intervention groups).
Types of participants
People of any age.
Types of interventions
Any educational intervention specifically aimed at reducing the occurrence or risk of eye injuries, or both. These may be based on written materials, video or audiotapes delivered on an individual basis (for example, one‐to‐one counselling), in a group setting (for example, classes) and/or population‐wide (for example, mass marketing campaigns).
We included educational interventions irrespective of the setting in which they were delivered. For example, we anticipated that eligible interventions may be home‐based, school‐based, work‐based or recreation‐based. Studies of educational interventions that were administered in a multi‐component programme involving other ineligible interventions, were only considered if outcomes attributable to the educational intervention were distinguished and/or the education component was the primary intervention (we referred to the trial's reported objectives to determine if education was the primary intervention of interest).
Types of outcome measures
Primary outcomes
Eye injuries of any severity.
Secondary outcomes
Change in behaviour.
Change in knowledge.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases:
Cochrane Eyes & Vision Group Specialised Register (6 August 2008);
Cochrane Injuries Group Specialised Register (6 August 2008);
CENTRAL (The Cochrane Library 2008, Issue 3);
MEDLINE (1966 to July (week 4) 2008);
EMBASE (1980 to July 2008);
ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) (1970 to July 2008), Social Sciences Citation Index (SSCI) (1970 to July 2008), Conference Proceedings Citation Index‐ Science (CPCI‐S) (1990 to July 2008);
HMIC Health Management Information Consortium (1979 to March 2007);
National Research Register (now searched as part of Current Controlled Trials metaRegister);
Current Controlled Trials metaRegister (to July 2008);
ERIC (to July 2008);
Zetoc (to July 2008);
SPORTdiscus (to July 2008);
WHOLIS (World Health Organization Library Information System) (searched 31 March 2007);
LILACS (Latin American and Caribbean Health Sciences) (searched 31 March 2007); and
MEDCARIB (Caribbean Health Sciences Literature) (searched 31 March 2007).
The search strategies are reported in detail in Appendix 1.
Searching other resources
We conducted an Internet search for relevant information. We also searched the Internet for relevant conferences and examined the conference abstracts. We sought further, potentially relevant, published or unpublished studies by checking reference lists of relevant papers and literature reviews and by communicating with trial authors.
None of the searches were restricted by language or publication status.
Data collection and analysis
Selection of studies
All four authors independently assessed the titles and abstracts of citations identified from the electronic database searches for eligibility. We obtained the full text of studies that definitely, or possibly, met the pre‐defined inclusion criteria. The reasons for excluding any study for which a full text copy was obtained is documented in the 'Characteristics of excluded studies' table. Any disagreements were resolved by discussion within the review team.
Data extraction and management
The review authors split up into two pairs and then each person in the pair extracted the following information independently onto a standardised form developed and assessed beforehand. The following data were extracted:
study design;
study setting;
details of participants;
details of interventions;
outcomes.
Each author within the pair then checked the other's data extraction before three of the authors entered the data in to RevMan 5 (RevMan 2008). Where information was missing or unclear, we contacted the trial authors.
Assessment of risk of bias in included studies
We independently assessed the risk of bias in the included studies, resolving any disagreements by discussion. We used the Cochrane Collaboration's tool for assessing risk of bias presented in Higgins 2008, which we adapted to incorporate additional domains used in the tool by the Effective Public Health Practice Project (Thomas 2003), which is a tool designed to assess the methodological quality of both randomised and non‐randomised study designs.
The following domains were assessed for each study:
sequence generation;
allocation concealment;
masking (blinding);
incomplete outcome data;
selective reporting;
confounders;
intervention compliance;
data collection methods;
duration of follow up.
We completed a 'Risk of bias' table for each study, incorporating a description of the study's performance against each of the above domains and our overall judgement of the risk of bias for each entry as follows:
'Yes' indicates low risk of bias;
'Unclear' indicates unclear or unknown risk of bias;
'No' indicates high risk of bias.
Measures of treatment effect
For dichotomous outcomes we calculated rate ratios and 95% confidence intervals. The rate ratio is the ratio of event rates post and pre intervention in the intervention area divided by the corresponding post to pre intervention event ratio in the control area. Provided that any changes in the population at risk are the same in both control and intervention areas, the rate ratio gives the reduction in the event rate in the intervention area compared to that in the control area. For example, a rate ratio of 0.8 corresponds to a 20% reduction in events compared to that predicted from the rates in the control area. For injury outcome data the standard errors for logarithms of rate ratios and hence 95% confidence intervals for rate ratios were calculated assuming that the number of events in each area in each period followed a Poisson Distribution.
For continuous outcomes we calculated the weighted mean difference (WMD) and 95% confidence intervals.
For studies which presented an appropriate summary effect estimate in the report, we have reported this estimate in the Results section.
Dealing with missing data
We contacted the trial investigators for missing data.
Assessment of heterogeneity
We planned to use the Chi2 test to assess the presence of statistical heterogeneity and the I2 statistic to assess the impact of heterogeneity (a value greater than 50% may be considered substantial heterogeneity). We looked for clinical heterogeneity by examination of the study details. We had also planned to examine the funnel plot for other sources of heterogeneity.
Data synthesis
If no substantial statistical or clinical heterogeneity was detected we planned to combine the results in a meta‐analysis using a random‐effects model. If there had been fewer than three trials and no heterogeneity was detected, we planned to use the fixed‐effect model. However as we judged there to be substantial clinical heterogeneity we did not combine the study results and instead summarised the information narratively.
Subgroup analysis and investigation of heterogeneity
If there had been enough data, we planned to perform the following subgroup analyses:
age (children < 18 years of age, adults > 18 years of age);
severity of injury;
setting (work‐based injury, home‐based injury, recreation‐based injury, school‐based);
education only versus education combined with supportive legislation.
Sensitivity analysis
We planned to conduct sensitivity analyses to determine the impact of exclusion of studies with higher risk of bias (randomised versus non‐randomised studies), unpublished data and industry‐funded studies.
Results
Description of studies
Results of the search
The electronic database searches covered all available years and were carried out between April 2007 and July 2008. We identified a total of 799 citations, of which 36 were judged to be potentially eligible based on title and/or abstract. After discussion between all four authors, full text copies were obtained for 24 of these papers. After all four authors had reviewed the full text copies, a total of 12 completed studies were judged to be potentially eligible. From these 12 we included five studies (Adler‐Grinberg 1985; Eime 2005; Forst 2004; Hathaway 1992; Smith 1978) and excluded seven (Benton 1978; Bezan 1988; Danis 2000; Eime 2004; Forst 2006; Mancini 2005; Murthy 1994).
Included studies
See the 'Characteristics of included studies' table for further details of the five studies that were included in this review.
Study design
Forst 2004; Hathaway 1992 and Smith 1978 were controlled before‐and‐after studies. Two studies were randomised; Eime 2005 was a cluster‐randomised trial in different geographical locations and Adler‐Grinberg 1985 was a randomised study with age‐matched controls.
Study objectives
Adler‐Grinberg 1985: To address ‘preventable blindness’ caused by eye injuries. School‐aged children were taught about eye health and safety by the use of an NSPC‐designed teaching unit, aimed at preventing blindness. The study assessed the effectiveness of the program afterwards by examining the students' knowledge, attitudes and self‐reported behaviour regarding eye health and safety to see if the aims of the programme were met.
Eime 2005: To prevent eye injuries in squash players by the use of appropriate eyewear (i.e. that have standards‐approved protective polycarbonate lenses). The study evaluated the implementation of a health education and eyewear promotion strategy, the Protective Eyewear Promotion (PEP) strategy. The use of appropriate eyewear in squash players was assessed before and after the intervention by comparing the player’s eyewear behaviour to see whether the objectives of the study were met.
Forst 2004: To reduce work‐related eye injury and illness among Latino migrant and seasonal workers by the use of a ‘Promotor de salud’ (or Community Health Worker) to provide training and protective eyewear. Pre and post‐intervention questionnaires were used to examine whether the aims of the study were met.
Hathaway 1992: To examine factors influencing user‐compliance with warning signs in a racquetball court. It tested (i) cost of compliance (by making it either easy or more difficult to comply by either providing eye protection or not); and (ii) inclusion of specific consequence information, such as number of eye injuries in racquet sport players per year, on warning signs (or not). Players were observed to find out if the aims of the study were met.
Smith 1978: To use behaviour modification techniques to improve worker safety behaviour. The shipyard environment under examination had a high incidence of eye injury, therefore the wearing of safety glasses by ship‐fitters to prevent eye injury was selected as the behaviour to be modified. The study tested the effectiveness of training supervisors in the fundamentals of behaviour modification in order to increase the use of safety glasses by employees. Eye accident rates before and after the intervention were examined to see if the aims of the study were met.
Setting
Four of the studies were based in the USA. Adler‐Grinberg 1985 was set in schools in California, Georgia and Ohio. Eime 2005 was conducted in squash venues in Melbourne, Australia. Forst 2004 was set in 34 farms in Michigan and Illinois. Hathaway 1992 was set on the racquet ball courts at Washington State University and Smith 1978 was based at a US shipyard.
Participants
Adler‐Grinberg 1985 involved school children from the 2nd/3rd/5th/6th grades of an elementary school. Eime 2005 involved predominantly male squash players of mixed abilities. Forst 2004 involved predominantly male, adult, Latino farm workers who had volunteered to participate in the study. Hathaway 1992 involved predominantly male racquet ball players who did not wear prescription eyewear and did not bring their own protective eye wear. Smith 1978 involved crews of ship‐fitters.
Sample sizes
Adler‐Grinberg 1985: 2440 school children; 26 schools, 102 classes (unit of analysis). Eime 2005: Pre‐intervention: (n = 266 protective eyewear promotion (PEP); n = 170 control), post‐intervention: (n = 379 PEP; n = 232 control). Forst 2004: Total sample size of 786 (83 later excluded due to irregularities in data collection). Hathaway 1992: Total sample size of 420, only data from the target population (266) are presented. Smith 1978: 44 crews; five experimental, 39 control (crew sizes not reported).
Interventions
Experimental group 2nd/3rd graders (n = 30): Short film about the basic principles in eye health and safety through song. There were five sessions which were approximately 20 minutes long.
5th/6th graders (n = 21): Filmstrip presenting the basic facts about the eye. The instructional package also consisted of a poster illustrating the structure of the eye, four tests and a sticker that describes basic first aid procedures for eye emergencies.
There were five sessions which were 40 to 60 minutes each.
Control group 2nd/3rd graders (n = 29), 5th/6th graders (n = 22): No intervention, usual practice.
Players at the randomly selected venues either had protected eyewear promotion (PEP) (intervention) or no promotion, the usual safety practice of the venue (control).
Pre‐intervention: n = 266 PEP; n = 170 control. Post‐intervention: n = 379 PEP; n = 232 control.
Forst 2004 had three study groups:
Intervention group 1 (n = 256) ‐ Community health workers (CHWs) provided protective eye wear and training to farm workers. Each farm worker received at least one individual training session and at least one group session.
Intervention group 2 (n = 298) ‐ CHWs provided eyewear without training.
Control group (n = 149) ‐ Eyewear distributed to farm workers, no CHW present and no training.
Players were exposed to three different situations:
no warning;
warning;
warning + information (information consisted of a list of five facts related to racquet ball and eye injuries).
High or low compliance cost was added to the situation.
Low compliance cost = eye protection available (four pairs of eye protection placed next to the door of each court)
High compliance cost = no eye protection available (no eye protection placed next to the door of each court)
Intervention group (n = 177)
(n = 41) low‐cost compliance + warning;
(n = 49) low‐cost compliance + warning + information;
(n = 47) high‐cost compliance + warning;
(n = 40) high‐cost compliance + warning + information.
Control group (n = 89)
(n = 36) low‐cost compliance + no warning or information;
(n = 53) high‐cost compliance + no warning or information.
Supervisors of five crews given five to 10 hours of classroom‐based safety education spread over one week.
Intervention group (n = 5 ship‐fitting crew supervisors) supervisors were trained in fundamentals of behaviour modification:
observing worker behaviour (specifically in the use of safety equipment);
recording worker behaviour;
giving praise for wearing safety equipment. Each supervisor then received five to 10 hours of classroom training over one week.
Control group (n = 39 ship‐fitting crews). Supervisors did not receive behaviour modification training or safety education.
The main target of the behaviour modification was the wearing of safety glasses by ship‐fitters.
Outcomes
Adler‐Grinberg 1985: The primary outcome was not collected in this study. Data on knowledge and behaviour were measured by questionnaires to students, teachers and parents. Eime 2005: The primary outcome was not collected in this study. Data were collected on knowledge (use of protective eyewear) and behaviour (use of appropriate protective eyewear). Forst 2004: Data were collected on the occurrence of eye injuries, behaviour (observation of use of safety glasses by study team and self‐reported use of safety glasses) and knowledge of eye injuries. Hathaway 1992: Data were reported in a 2 x 3 table as target sample compliance rates for cost of compliance and warning information. Smith 1978: Data were reported as average eye accident rates before and after treatment in the experimental and control groups.
Excluded studies
Seven studies were not eligible for inclusion in this review and reasons for exclusion are listed in the 'Characteristics of excluded studies' table.
Risk of bias in included studies
For an overview of the risk of bias, please see Figure 1 and Figure 2. For more detailed information on each study and risk of bias domain, please refer to the 'Risk of bias in included studies' table.
1.
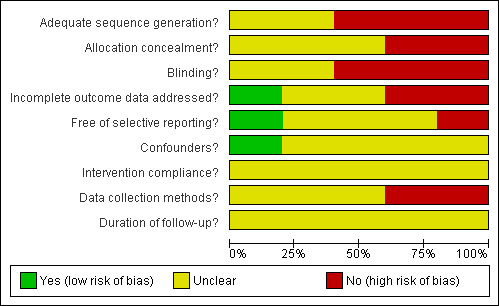
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
2.
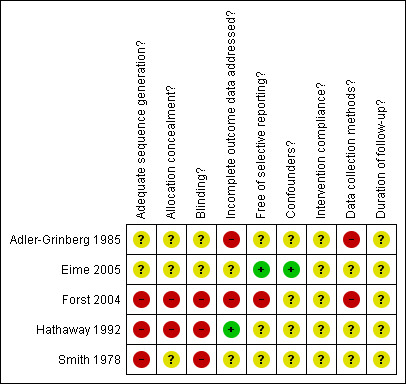
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Allocation
Adequate sequence generation
Three studies were assessed as having high risk of bias (Forst 2004; Hathaway 1992; Smith 1978) and two were assessed as unclear (Adler‐Grinberg 1985; Eime 2005) due to the lack of information on sequence generation provided in the study report.
Allocation concealment
Forst 2004 and Hathaway 1992 were assessed as having high risk of bias for allocation concealment and Adler‐Grinberg 1985; Eime 2005 and Smith 1978 were assessed as unclear as this information was not reported.
Blinding
Three trials were assessed as having high risk of bias for masking (blinding) (Forst 2004; Hathaway 1992; Smith 1978) and two trials were assessed as unclear (Adler‐Grinberg 1985; Eime 2005) due to lack of reporting of this information.
Incomplete outcome data
Eime 2005 and Smith 1978 were assessed as unclear as we were unable to establish whether data were missing. Adler‐Grinberg 1985 and Forst 2004 were assessed as high risk of bias. The latter due to unreported data, which was confirmed by the author. Hathaway 1992 was assessed as low risk of bias.
Selective reporting
Eime 2005 was assessed as having a low risk of bias for this parameter as all outcomes were reported. Forst 2004 was assessed as high risk of bias due to selective reporting, Adler‐Grinberg 1985; Hathaway 1992; and Smith 1978 were assessed as unclear due to a lack of this information in the study reports.
Other potential sources of bias
Confounders
Four studies were assessed as unclear for risk of bias due to confounders. Eime 2005 did account for potential player specific confounders.
Intervention compliance
All five studies were assessed as unclear for risk of bias due to intervention compliance.
Data collection methods
Adler‐Grinberg 1985 and Forst 2004 were assessed as having high risk of bias on the basis of information provided about methods. The rest of the studies were assessed as unclear due to lack of information provided.
Duration of follow up
All five studies were assessed as unclear for risk of bias due to duration of follow up.
Effects of interventions
Primary outcome: eye injuries
Two studies (Forst 2004; Smith 1978) collected data on eye injuries. However, injury outcome data were not reported in Forst 2004 as the study author judged that the surveillance of eye injuries was 'inadequate'.
Smith 1978 reported injury rates per 100 employees for the before and after periods in the intervention and control groups. For the experimental group, injury rates in the before and after periods were 11.8 and 4.32 per 100 employees (7.48% decrease), respectively. For the control group, injury rates in the before and after periods were 5.82 and 4.66 per 100 employees (1.16% decrease), respectively. The review authors calculated a rate ratio of 0.45 (95% CI 0.09 to 2.36), indicating a 55% decrease in injuries in the experimental group relative to the control, although this finding is not statistically significant (‐55%, 95% CI ‐91% to +136%).
Secondary outcome: behaviour
Four studies reported behaviour outcome data (Adler‐Grinberg 1985; Eime 2005; Forst 2004; Hathaway 1992).
Adler‐Grinberg 1985assessed the effects on behaviour by a questionnaire administered to parents and teachers of children in the experimental group. No behaviour outcome data are reported for the control group. Of the 72% of parents who responded, 30% said they had noticed some positive changes in their child's knowledge, awareness or behaviour related to eye‐care practices. Of the 71% of teachers who responded, 71% responded 'good' when asked if students were incorporating safety skills into their practices; 21% responded 'fair' and 9% responded 'excellent'.
Eime 2005 assessed behaviour through a pre and post‐survey of the use of protective eyewear by squash players. Amongst players in the experimental group, between the before and after periods those using appropriate eyewear increased from 8.0% to 13.8%, using inappropriate eyewear fell from 9.5% to 7.4% and using no eyewear decreased from 82.4% to 78.8%. Amongst players in the control group, between the before and after periods those using appropriate eyewear increased from 7.1% to 9.6%, using inappropriate eyewear increased from 5.9% to 7.7% and using no eyewear decreased from 87.0% to 82.8%.
The study authors calculated the odds ratio and 95% confidence interval, using multivariate analysis to adjust for potential player specific confounders. The analysis found that players in the intervention group had 1.8 times greater odds (95% CI 0.9 to 3.5) than control players of using appropriate eyewear.
Forst 2004 measured the self‐reported and observed use of safety glasses by farm workers.
The self‐reported use of safety glasses was measured using the question 'I always use safety glasses when working in agriculture' to workers gave a rating between 1 (strongly agree) and 5 (strongly disagree). The rating improved (P<0.0001) in all study groups between the before and after periods. In group 1 (received training and protective eyewear by community health workers) the average change between the two periods was ‐1.48, in group 2 (received eyewear but no training from CHWs) the average change was ‐0.71, and in group 3 (received eyewear with no CHWs present or training) the average change was ‐0.96.
The observed use of safety glasses also improved in all three study groups. Between the before and after periods, in group 1 the use of safety glasses increased from 1.1% to 36% (24/67); in group 2 use increased from 0% (0/198) to 5.2% (9/172); and in group 3 use increased from 0% (0/107) to 14% (11/76). The review authors calculated the rate ratio comparing use of glasses in the education group (group 1) with the two no education groups (group 2 and 3); RR was 2.02 (95% CI 0.07 to 62.30), indicating that glasses use amongst workers in the experimental group was two times greater than in the control group.
Hathaway 1992: collected data on the observed use of safety glasses by racquetball players. Percentage of players in each study group wearing appropriate glasses was:
Education group 1 ‐ low‐cost compliance + warning (23%);
Education group 2 ‐ low‐cost compliance + warning + information (60%);
Education group 3 ‐ high‐cost compliance + warning (0%);
Education group 4 ‐ high‐cost compliance + warning + information (0%);
Control group 1 ‐ low‐cost compliance + no warning or information (25%);
Control group 2 ‐ high‐cost compliance + no warning or information (0%).
Secondary outcome: knowledge
Three studies reported knowledge outcome data (Adler‐Grinberg 1985; Eime 2005; Forst 2004).
Adler‐Grinberg 1985measured knowledge by tests administered to the school children and a questionnaire to the teachers, before and after the intervention.
For the children in the second and third grades; in the experimental group the mean (SD) test score increased from 37.76 (5.00) to 41.15 (4.32), an average change of 3.39 (1.90); in the control group the mean (SD) test score increased from 37.70 (5.15) to 38.66 (4.65), an average change of 0.96 (1.69).
For the children in the fifth and sixth grades; in the experimental group the mean (SD) test score increased from 45.94 (2.29) to 52.78 (3.33), an average change of 6.84 (4.04); in the control group the mean (SD) test score increased from 44.74 (2.03) to 44.95 (2.88), an average change of 0.21 (1.93).
The review authors combined data for both groups of children in the intervention and control group to provide overall data for one experimental and one control group, and calculated the weighted mean difference (WMD) of change in knowledge. The WMD was 4.17 (95% CI 3.11 to 5.23), indicating a statistically significant improvement in knowledge amongst the intervention children compared to the control children.
Of the 71% of teachers in the experimental group who completed the questionnaire, 79% answered 'yes' to students having increased their knowledge about eye safety as a result of the programme. There are no corresponding data for the control group.
Eime 2005 measured players' knowledge of which eyewear provided adequate protection, before and after the intervention (polycarbonate lens are the only type of eyewear to provide adequate protection). The study reported the results as odd ratios and 95% confidence intervals calculated by multivariate analysis (to adjust for potential player specific confounders), which describe the difference in effect of the education between the before and after periods, compared with the control group.
Polycarbonate lens ‐ 0.74 (95% CI 0.39 to 1.36), P=0.32.
Open eye guards ‐ 0.51 (95% CI 0.26 to 1.10), P=0.05.
Don't know ‐ 1.72 (95% CI 0.89 to 3.30), P=0.10.
Industrial eyewear ‐ 1.00 (95% CI 0.46 to 2.21), P=0.99.
Prescription glasses ‐ 0.70 (95% CI 0.18 to 2.71), P=0.61.
Contact lenses ‐ 0.89 (95% CI 0.30 to 2.66), P=0.84.
Forst 2004 used a questionnaire to assess risk perception and knowledge. No figures are presented in the report however the study authors describe that the results indicated that the knowledge of participants in group 1 improved between the before and after periods, and neither group 2 or group 3 showed an overall improvement.
Discussion
Summary of main results
The results from the five included studies do not provide reliable evidence that educational interventions are effective in preventing eye injuries. Two of the studies reported data on the primary outcome, eye injuries, which found a reduction associated with the intervention given in that study. However, methodological weaknesses in these studies, such as allocation concealment and their susceptibility to bias, means that their findings should be viewed with caution.
Overall completeness and applicability of evidence
Although we included five studies in this review, there are a number of issues that need to be addressed when considering it as a useful source of evidence.
Overall, the low quality study designs, variation in educational campaigns, lack of uniformity of the occupations and activities studied (farming to sports activities) and range of age groups (primary school children to adults) makes it difficult to evaluate the evidence presented.
The educational interventions used were different for each study even where the settings were similar such as the sports activities (squash and racquetball) or the labour intensive industries (farm workers and ship‐fitters). For Adler‐Grinberg 1985, audio or visual aids were used in combination with other tests and worksheets. The length of the training was for five sessions of 20 minutes each or five sessions of 40 minutes to an hour each. There was also emphasis on classroom activities to reinforce the concepts that were shown/heard in the presentations. For Eime 2005 which was set in squash venues, the emphasis was on visual materials such as posters, pamphlets and stickers as well as offering incentives. Hathaway 1992, the other sports study based on racquetball players, used written materials in the form of warning signs and offered the use of protective gear. Forst 2004 used personnel in the form of community health workers to train the farm workers. The farm workers were expected to have at least two training sessions which included enlarged photographs, presentations, and other written materials that demonstrated eye injuries and hazards. Each farm worker was also fitted with safety glasses. Smith 1978 looked at ship‐fitters and trained the supervisors by giving them five to 10 hours of classroom training over a period of one week. Incentives such as praising workers who wore safety glasses were used to help the ship‐fitters modify their behaviour.
All five studies were conducted in high‐income countries (four in the USA and one in Australia); we found no eligible studies from low or middle‐income countries. Studies conducted in low and middle‐income countries may be affected by a lack of health and safety awareness or legislation and the level of technology and safety features of machines etc., which may have implications for eye injury rates.
The studies cover a broad time frame from 1978 to 2005. Additional data that may have been collected when the trial was conducted was generally not available. Findings from the older studies may not be applicable or appropriate today due to advancement of technology and changing methods in industry. Despite extensive searches we did not identify any planned or ongoing studies. This suggests that although eye injuries may be a health burden in many countries, this is not reflected in the level of research in this area.
The included reviews also had short follow‐up times. Behaviour changes were in most cases measured immediately after the intervention, which raised concerns about the sustainability of the change over time. Follow‐up times should be sufficient to gauge whether a change in outcome is caused by random fluctuation or if there really is an effect from the intervention over time.
The studies tend to focus on self‐reported injury rates or subjective changes in behaviour which are difficult to evaluate. The value of questionnaires and interviews, in this instance, is also unclear.
Quality of the evidence
The methodological quality of the studies was poor overall. Due to a lack of reporting or unclear information provided, we were not able to assess the overall risk of bias for each study. Only two randomised controlled trials were found. Only one study reported on eye injuries as an outcome so no conclusions could be drawn. None of the studies in this review measured the effect of the intervention through data collected in emergency departments. Self‐reporting of eye injuries or observation of behaviour is much more difficult to equate and therefore not as objective. The range of settings and interventions were not conducive to a successful comparison of the studies. Pre and post‐test measurements of knowledge or attitude do not necessarily give a suitable indicator of behaviour change.
Potential biases in the review process
This systematic review addresses a focused research question using predefined inclusion criteria and methodology to select and appraise eligible studies. As with all systematic reviews, the possibility of publication bias should be considered as a potential threat to validity. Identification of research for systematic reviews of public health interventions tends to require more complex searching than for reviews of medical interventions. The multi‐disciplinary nature of the research means that it is more widely scattered, with much published in the grey literature (Jackson 2005). In recognition of this, the search strategy for this systematic review involved searching multiple electronic databases from a range of disciplines (including two specific databases of grey literature). Reference lists of relevant studies and contact with experts in the field were employed as methods to identify all potentially eligible published and unpublished studies. The searching was not limited to studies in English. With such a comprehensive search strategy, the chance of having missed an important study should be low and issues of publication bias should be minimal.
The findings of this systematic review are limited by the overall poor methodological quality of the included studies; poorly designed and executed studies are susceptible to bias and can lead to either an over or under estimate of effect.
Several studies were conducted over a decade ago, so their relevance and generalisability to the present situation is questionable. An additional limitation is the lack research from low and middle‐income countries.
Possible bias is introduced when the study is conducted and reported by those who are involved. For example in Smith 1978, crews reported compliance to safety methods and eye injury rates to supervisors.
Lack of follow up is a potential form of bias and none of the included studies were followed up for a reasonable period of time after the intervention had been given.
Agreements and disagreements with other studies or reviews
The results of this review support and echo the recommendations made by Lipscomb 2000 in a review evaluating the effectiveness of interventions to prevent work‐related eye injuries. Lipscomb reviewed all studies (irrespective of study design) which were set in the construction, manufacturing and agricultural industries. The primary outcome was eye injury rates.
Lipscomb also noted in the review that not much recent scientific research had been done. In her review, four out of the seven studies she included were published before 1980 and the most recent was published in 1993. Few studies have been carried out since; this review identified only two eligible studies (Eime 2005; Forst 2004) since Lipscomb's review was published.
Along with the dearth of recent literature published on this topic, Lipscomb also concluded that "much of the information we do have comes from descriptions of safety programs that have not been rigorously evaluated. Carefully designed controlled trials would allow us to more clearly understand the effects of different interventions in different work environments". Her statement clearly reflects the findings of this review.
Authors' conclusions
Implications for practice.
This review found no evidence to support the idea that educational interventions help to prevent eye injuries. Although there is no evidence of harm, it fails to confirm whether educational interventions bring about a sustained decline in ocular injury rates and outcomes. One of the studies included in the review does show that educational interventions can bring about change in knowledge which leads to change in behaviour but it is unclear how this could translate to a change in injury rate or have a sustained effect on behaviour.
The review does highlight the variety of educational tools available, but their effectiveness and replicability for different population groups and environments is inconclusive. It is also not possible to conclude on the impact of educational effectiveness by age, gender, occupation or environment.
Implications for research.
Future research in this area should concentrate on well‐conducted randomised trials with adequate allocation concealment and masking (blinding). Studies should have a longer follow‐up time to better understand the sustainability of behaviour change through an educational intervention. Exposure to risks varies by age, gender, profession and environmental safety factors and which must be evaluated before and after an intervention.
Appropriate studies need to be carried out in low and middle‐income countries where poor conditions/work environments and lack of appropriate legislation dictate a greater risk of injury. These studies must also evaluate the cost to individuals and the practical implications of employing interventions that aim to influence behaviour and prevent ocular injuries.
Studies should look at eye injury rates as the primary outcome. Secondary outcomes, such as behaviour changes and effectiveness of the educational tool, should be collected independently of those taking part. Statistically feasible methods (judgement analysis) and interrupted time series over several years could be applied.
History
Protocol first published: Issue 2, 2007 Review first published: Issue 4, 2009
| Date | Event | Description |
|---|---|---|
| 1 May 2008 | Amended | Converted to new review format. |
Notes
This review is a collaborative project between the Cochrane Eyes & Vision and Injuries Review Groups.
Acknowledgements
Linda Forst, MD, MPH, MS Michael J Smith PhD Joanne Elliott, Trials Search Co‐ordinator, Cochrane Bone, Joint and Muscle Trauma Group
Appendices
Appendix 1. Search strategy
Cochrane Injuries Group and Cochrane Eyes & Vision Group Specialised Register (searched 6 August 2008) (eye or eyes or ocular) and (injury or injuries or trauma*) and (educat* or aware* or teach* or health‐promot*)
MEDLINE 1950 to July (week 4) 2008 1. exp eye/ 2. exp accident prevention/ 3. accidents occupational/pc [Prevention & Control] 4. 2 or 3 5. 1 and 4 6. eye injuries/pc [Prevention & Control] 7. eye burns/pc [Prevention & Control] 8. exp eye protective devices/ 9. (5 or 6 or 7) and 8 10. ((eye or eyes or ocular or orbit$ or retina$ or globe) adj3 (injur$ or trauma$ or contusion$ or rupture$ or burn$ or damag$)).ab,ti. 11. ((eye or eyes or ocular or intra?ocular) adj3 (foreign adj1 (body or bodies or substance$ or object$))).ab,ti. 12. retina/in [Injuries] 13. ((safety or health or eye$) adj5 (train$ or instruct$ or demonstrat$ or educat$ or aware$ or teach$ or inform$ or promot$)).ab,ti. 14. education.fs. 15. exp Education/ 16. exp Health Education/ 17. exp Health Promotion/ 18. exp risk reduction behavior/ 19. 5 or 6 or 7 or 9 or 10 or 11 or 12 20. or/13‐18 21. 19 and 20
EMBASE 1980 to July 2008 1. exp Retina Injury/ 2. exp Retina Tear/ 3. exp eye/ 4. exp accident prevention/ 5. accidents occupational/pc [Prevention & Control] 6. 4 or 5 7. 3 and 6 8. eye injuries/pc [Prevention & Control] 9. eye burns/pc [Prevention & Control] 10. exp eye protective devices/ 11. (7 or 8 or 9) and 10 12. ((eye or eyes or ocular or orbit$ or retina$ or globe) adj3 (injur$ or trauma$ or contusion$ or rupture$ or burn$ or damag$)).ab,ti. 13. ((eye or eyes or ocular or intraocular) adj3 (foreign adj1 (body or bodies or substance$ or object$))).ab,ti. 14. ((safety or health or eye$) adj5 (train$ or instruct$ or demonstrat$ or educat$ or aware$ or teach$ or inform$ or promot$)).ab,ti. 15. exp Education/ 16. exp Health Education/ 17. exp Health Promotion/ 18. exp risk reduction behavior/ 19. 1 or 2 or 7 or 8 or 9 or 11 or 12 or 13 20. 14 or 15 or 16 or 17 or 18 21. 19 and 20
The Cochrane Library to Issue 3, 2008 #1 MeSH descriptor Accident Prevention explode all trees #2 MeSH descriptor Accidents, Occupational explode all trees #3 (#1 OR #2) #4 MeSH descriptor Eye explode all trees #5 (#3 AND #4) #6 MeSH descriptor Eye Injuries explode all trees #7 MeSH descriptor Eye Burns explode all trees #8 (#5 OR #6 OR #7) #9 MeSH descriptor Eye Protective Devices explode all trees #10 (#8 AND #9) #11 ((eye or eyes or ocular or orbit* or retina* or globe) near3 (injur* or trauma* or contusion* or rupture* or burn* or damag*)) #12 eye or eyes or ocular or intra‐ocular #13 foreign near3 (body or bodies or substance* or object*) #14 (#12 AND #13) #15 MeSH descriptor Retina explode all trees with qualifier: IN #16 ((safety or health or eye*) near5 (train* or instruct* or demonstrat* or educat* or aware* or teach* or inform* or promot*)) #17 MeSH descriptor Education explode all trees #18 MeSH descriptor Health Education explode all trees #19 MeSH descriptor Health Promotion explode all trees #20 MeSH descriptor Risk Reduction Behavior explode all trees #21 (#16 OR #17 OR #18 OR #19 OR #20) #22 (#8 OR #10 OR #11 OR #14 OR #15) #23 (#21 AND #22)
National Research Register (searched 19 April 2007); (now searched as part of Current Controlled Trials metaRegister) #1((eye or eyes or ocular or orbit* or retina* or globe) and (injur* or trauma* or contusion* or rupture* or burn* or damag*)) #2((safety or health or eye*) and (promot* or train* or instruct* or demonstrat* or educat* or aware* or teach* or inform*)) #3#1 and #2
Current Controlled Trials meta Register (searched 6 August 2008) (eye or eyes or ocular) and (injury or injuries or trauma*) and (educat* or aware* or teach* or health‐promot*)
AgeInfo (Centre for Policy on Ageing) (searched 6 August 2008) (eye* or retina* or ocular or orbit or globe) and (injury or injuries or trauma* or contusion* or rupture* or burn* or damag*)
Indian Medlars/PakMediNet (searched 6 August 2008) (eye or eyes or ocular or orbit$ or retina$ or globe) and (injur$ or trauma$ or contusion$ or rupture$ or burn$ or "foreign body" or substance$ or “foreign object” or damag$) and (safety or promot$ or train$ or instruct$ or demonstrat$ or educat$ or aware$ or teach$ or inform$)
LILACS (Latin American and Caribbean Health Sciences), WHOLIS (World Health Organization Library Information System), MEDCARIB (Caribbean Health Sciences Literature) (searched 31 March 2007) 1. eye or eyes or ocular or orbit$ or retina$ or globe 2. injur$ or trauma$ or contusion$ or rupture$ or burn$ or "foreign body" or substance$ or “foreign object” or damag$ 3. safety or promot$ or train$ or instruct$ or demonstrat$ or educat$ or aware$ or teach$ or inform$ 4. 1 and 2 and 3
Web of Science (SCI, SSCI) (searched 6 August 2008) TS=(eye* or eyes or ocular) AND TS=(injur* or trauma* or wound* or contusion* or burn* or rupture* or damag*) AND TS=(educat* or aware* or safety or "health promotion" or inform*) AND TS=(evaluat* or trial* or study or studies or program*)
ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) (1970 to July 2008), Social Sciences Citation Index (SSCI) (1970 to July 2008), Conference Proceedings Citation Index‐ Science (CPCI‐S) (1990 to July 2008 TS=(eye* or eyes or ocular) AND TS=(injur* or trauma* or wound* or contusion* or burn* or rupture* or damag*) AND TS=(educat* or aware* or safety or "health promotion" or inform*) AND TS=(evaluat* or trial* or study or studies or program*)
ERIC (Education Resource Information Centre) (searched 6 August 2008) 1. eye* or eyes or ocular or orbit or retina* or globe 2. injur* or trauma* or wound* or contusion* or burn* or rupture* or damag* 3. educat* or aware* or safety or "health promotion" or inform*
HMIC Health Management Information Consortium 1979 to 2007 (searched 31 March 2007) 1. exp eye/ 2. exp accident prevention/ 3. exp industrial injuries/ 4. 2 or 3 5. 1 and 4 6. ((eye or eyes or ocular or orbit$ or retina$ or globe) adj3 (injur$ or trauma$ or contusion$ or rupture$ or burn$ or damag*)).ab,ti. 7. ((eye or eyes or ocular or intra?ocular) adj3 (foreign adj1 (body or bodies or substance$ or object$))).ab,ti. 8. ((safety or health or eye$) adj5 (train$ or instruct$ or demonstrat$ or educat$ or aware$ or teach$ or inform$ or promot$)).ab,ti. 9. 5 or 6 or 7 or 8 10. exp Education/ 11. exp Health Education/ 12. exp Health Promotion/ 13. 10 or 11 or 12 14. 9 and 13
ZETOC (searched 6 August 2008) Eye* + injur* + educat* Eye* + trauma* + educat* Eye* + damag* + educat* Ocular + injur* + educat* Ocular + trauma* + educat* Ocular + damag* + educat*
SPORTdiscus (searched 15 August 2008) 1. Eye/ 2. (safe$ or health$).tw. 3. and/1‐2 4. (train$ or instruct$ or demonstrat$ or educat$ or aware$ or teach$ or inform$ or promot$).tw. 5. and/3‐4
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Adler‐Grinberg 1985.
| Methods | Study design: Cluster‐randomised, age‐match controlled | |
| Participants | Setting: Schools in 3 US states: California, Georgia, Ohio. Elementary public school students (n = 2440) in 102 classrooms from 26 voluntary schools. Students were from the second, third, fifth and sixth grade classes. | |
| Interventions | Unit of analysis: Classrooms
Intervention: 2nd/3rd graders watched an 8‐minute film called "The Eyes Have It" which introduced them to the basic principles of eye health and safety through song. Seven printed worksheets which generated classroom activities reinforced the concepts of the film. The students had 5 sessions which were approximately 20 minutes long. 2nd graders (n = 15), 3rd graders (n = 15) Control: No control, classes carried on as normal. 2nd graders (n = 14), 3rd graders (n = 15) Intervention: 5th/6th graders (n = 21) watched a filmstrip called "The Magic of Sight" with a 13‐minute audiocassette that presented the basic facts about the eye. The instructional package also consisted of a poster illustrating the structure of the eye, 4 tests and a sticker that describes basic first aid procedures for eye emergencies. The students had 5 sessions which were 40 to 60 minutes each. Control: No control, classes carried on as normal. 5th graders (n = 12), 6th graders (n = 10) |
|
| Outcomes | Knowledge and attitudes related to eye health and safety: measured by questionnaire given to students Knowledge and attitudes related to eye health and safety: measured by questionnaire given to teachers involved in the programme Knowledge, attitudes and observed behaviour related to eye health and safety: measured by questionnaire given to parents of students involved |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Although schools were randomly assigned to experimental and control groups, there is no mention of how this was done |
| Allocation concealment? | Unclear risk | There is no mention of how this was done |
| Blinding? All outcomes | Unclear risk | There is very little information to judge whether the students, teachers, parents or outcome assessors were unaware of the intervention assigned. Teachers were aware of the programme as they were teaching it but parents had not been notified of their child's participation in the programme. |
| Incomplete outcome data addressed? All outcomes | High risk | There is no mention of drop‐outs or participants excluded from the intervention. There is no mention of what happened to students who did not complete the whole educational package, i.e. they missed a lesson or more than 1 lesson. 29% of teachers in the experimental group and 28% of parents in the control group did not respond to the post‐intervention questionnaire. |
| Free of selective reporting? | Unclear risk | ‐ |
| Confounders? | Unclear risk | ‐ |
| Intervention compliance? | Unclear risk | Not reported |
| Data collection methods? | High risk | Data were collected by questionnaires given to students, teachers involved in teaching the educational package and parents of students involved in the study. For the teachers and parents, the questionnaires were given on a voluntary basis. |
| Duration of follow‐up? | Unclear risk | For all students (experimental and control), it was 1 day after the programme. For teachers and parents of the experimental group, the questionnaires were given 'following the presentation of the educational unit'. |
Eime 2005.
| Methods | Study design: Cluster‐randomised Date: 2002‐2003. 4‐month trial. | |
| Participants | Setting: Squash venues in northwest and southeast Melbourne, Australia. Eight squash venues (4 from each geographical location). Median age: 37 to 39 years. Predominantly male. | |
| Interventions | Intervention: Protective eyewear promotion (PEP). The promotion involved informing and educating both squash venue operators and players of the risk of eye injury and of wearing appropriate eyewear as well as providing eyewear to players to try out and purchase. Educational pamphlets and task specific posters and stickers were also displayed near the registration desk, squash courts and in the changing room. Control: Usual safety practice Pre‐intervention: (n = 266 PEP; n = 170 control), post‐intervention: (n = 379 PEP; n = 232 control) |
|
| Outcomes | Behaviour ‐ use of protective eyewear measured by post‐intervention survey. The PEP venue managers completed record forms to report the borrowing/loan and sales of eyewear during the trial. Knowledge ‐ measured by post‐intervention survey |
|
| Notes | With the exception of Standards Approved polycarbonate eyewear, all other types of eyewear were considered inappropriate as they did not provide adequate eye protection | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "Two squash associations of different geographical locations. One in the northwest region of Melbourne and the other in the southeast region, were randomly allocated to one of two groups: PEP (to receive the intervention) and control (without the intervention". "Four PEP and four control venues were randomly selected from the list of public squash venues in the two separate playing associations". |
| Allocation concealment? | Unclear risk | Not reported |
| Blinding? All outcomes | Unclear risk | Not reported |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Although missing values (participants) are reported in Table 1, no reasons are given for the losses. |
| Free of selective reporting? | Low risk | ‐ |
| Confounders? | Low risk | The authors did adjust for "years played, grade of competition, hours usually played per week, and sex". |
| Intervention compliance? | Unclear risk | ‐ |
| Data collection methods? | Unclear risk | ‐ |
| Duration of follow‐up? | Unclear risk | ‐ |
Forst 2004.
| Methods | Study design: Controlled before‐and‐after Date: 2001 | |
| Participants | Setting: Farms in Southeastern Michigan, USA. Latino farm workers (n = 703) from 34 farms, predominantly male. Volunteered to participate in study. | |
| Interventions | Three study groups; 2 intervention, 1 control Intervention group 1 ‐ Community health workers (CHWs) provided protective eyewear and training to farm workers ‐ at least 1 individual training session for each farm worker and at least 1 group session (n = 256) Intervention group 2 ‐ CHWs provided eyewear without training (n = 298) Control group ‐ Eyewear distributed to farm workers, no CHW present and no training (n = 149) In all 3 groups farm workers received safety glasses and cords with information sheet on preventing eye injuries and illnesses in agriculture |
|
| Outcomes | Eye injuries ‐ reported by participants to study team Behaviour ‐ observation of use of safety glasses by study team, self‐reported use of safety glasses Knowledge of eye injuries ‐ measured by questionnaire |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | Controlled before‐and‐after study |
| Allocation concealment? | High risk | Farms were divided into groups based on where the CHW worked, the housing of the participants (in an effort to avoid contamination) and equalising the participants numbers in the intervention groups |
| Blinding? All outcomes | High risk | It is unclear whether members of the study team who observed the use of safety glasses were masked (blind) to allocation Due to nature of intervention, participants and CHWs could not have been masked |
| Incomplete outcome data addressed? All outcomes | High risk | Data for 83 participants were excluded as one CHW admitted completing the self‐reported outcome forms herself |
| Free of selective reporting? | High risk | Outcome data not reported for the eye injuries and knowledge outcomes |
| Confounders? | Unclear risk | None reported |
| Intervention compliance? | Unclear risk | Not reported |
| Data collection methods? | High risk | Data on injuries and knowledge were collected by self‐report questionnaire Observations by the study team were used to obtain data on behaviour |
| Duration of follow‐up? | Unclear risk | Ranged from 4 to 12 weeks |
Hathaway 1992.
| Methods | Study design: Controlled before‐and‐after Date: 1992 | |
| Participants | Setting: Racquet ball courts at the Washington State University. Target population of 266 racquet ball players taken from a total sample size of 420 (339 males and 81 females). Target population were those who did not wear prescription eyewear and did not bring protective eyewear with them. | |
| Interventions | Players were exposed to 3 different situations:
High or low compliance cost was added to the situation
|
|
| Outcomes | Percentages of those who wear eye protection are presented for each group | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | Controlled before‐and‐after study |
| Allocation concealment? | High risk | Allocation was according to when racquet ball players attended the courts |
| Blinding? All outcomes | High risk | Data collected by observation therefore masking not possible |
| Incomplete outcome data addressed? All outcomes | Low risk | All data for numbers reported is supplied |
| Free of selective reporting? | Unclear risk | ‐ |
| Confounders? | Unclear risk | None detected |
| Intervention compliance? | Unclear risk | Not reported |
| Data collection methods? | Unclear risk | Data were collected by observation |
| Duration of follow‐up? | Unclear risk | Not reported |
Smith 1978.
| Methods | Study design: Cluster‐controlled before‐and‐after Date: 1970s | |
| Participants | Setting: Large (20,000 workforce) shipyard in USA. 44 ship‐fitter crews. | |
| Interventions | Intervention group: 5 supervisors from 5 ship‐fitter crews given 5 to 10 hours classroom‐based safety training over the course of 1 week. Also included training in fundamental behaviour modification which included: observing worker behaviour, recording worker behaviour, giving praise for wearing safety equipment (with a focus on wearing safety glasses). Control group: 39 ship‐fitter crews. Neither supervisors nor crews given any safety training. |
|
| Outcomes | Average eye accident rates were recorded from each group for the periods before and after the intervention | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | Cluster before‐and‐after study |
| Allocation concealment? | Unclear risk | There is no description of how the groups were chosen |
| Blinding? All outcomes | High risk | Data collected by observation therefore masking not possible |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Crew numbers not stated so not clear data is incomplete |
| Free of selective reporting? | Unclear risk | Use of safety equipment discussed but not reported |
| Confounders? | Unclear risk | None reported |
| Intervention compliance? | Unclear risk | Compliance is not discussed |
| Data collection methods? | Unclear risk | Eye injury rates were recorded before and after intervention |
| Duration of follow‐up? | Unclear risk | Not reported |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Benton 1978 | No control group |
| Bezan 1988 | Survey, no control group |
| Danis 2000 | Non‐randomised cohort study |
| Eime 2004 | Interview survey, no control group |
| Forst 2006 | Cohort study, no control group, observational |
| Mancini 2005 | No distinct control group |
| Murthy 1994 | Uncontrolled before and after study |
Differences between protocol and review
The assessment of methodological quality used in earlier versions of this review and the protocol has been replaced with an assessment of the risk of bias. This amendment is in response to a change in the Cochrane Collaboration's methodological guidance.
Contributions of authors
KB, KK, DP and AS jointly devised the review concept and wrote the protocol. KB designed the search strategy. KB, KK, DP and AS screened the search results and extracted data from the included trials. KB, KK and AS entered data in to RevMan 5. KB, KK, DP and AS wrote the review.
Sources of support
Internal sources
London School of Hygiene & Tropical Medicine, UK.
External sources
No sources of support supplied
Declarations of interest
None known.
New
References
References to studies included in this review
Adler‐Grinberg 1985 {published data only}
- Adler‐Grinberg D, Lovato C, Nussenblatt H, Davis‐Poirier R. Evaluation of the NSPB elementary school teaching unit on eye health. Journal of the American Optometric Association 1985;56(11):882‐6. [PubMed] [Google Scholar]
Eime 2005 {published data only}
- Eime R, Finch C, Wolfe R, Owen N, McCarty C. The effectiveness of a squash eyewear promotion strategy. British Journal of Sports Medicine 2005;39:681‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Forst 2004 {published data only}
- Forst L, Lacey S, Chen HY, Jimenez R, Bauer S, Skinner S, et al. Effectiveness of community health workers for promoting use of safety eyewear by Latino farm workers. American Journal of Industrial Medicine 2004;46:607‐13. [DOI] [PubMed] [Google Scholar]
Hathaway 1992 {published data only}
- Hathaway JA, Dingus TA. The effects of compliance cost and specific consequence information on the use of safety equipment. Accident Analysis & Prevention 1992;24(6):577‐84. [DOI] [PubMed] [Google Scholar]
Smith 1978 {published data only (unpublished sought but not used)}
- Smith MJ, Anger WK, Uslan SS. Behavioral modification applied to occupational safety. Journal of Safety Research 1978;10(2):87‐8. [Google Scholar]
References to studies excluded from this review
Benton 1978 {published data only}
- Benton V H, Truelove N. "Adopt‐a‐school" a program of eye care for children. Sight‐Saving Review 1978;48(2):77‐80. [PubMed] [Google Scholar]
Bezan 1988 {published data only}
- Bezan D, Bezan K. Prevention of eye injuries in the dental office. Journal of the American Optometric Association 1988;59(12):929‐34. [PubMed] [Google Scholar]
Danis 2000 {published data only}
- Danis R P, Hu K, Bell M. Acceptability of baseball face guards and reduction of oculofacial injury in receptive youth league players. Injury Prevention 2000;6(3):232‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eime 2004 {published data only}
- Eime R, Finch C, Owen N, Gifford S, Vear P. Knowledge, beliefs and attitudes of squash venue operators relating to use of protective eyewear. Injury Control & Safety Promotion 2004;11(1):47‐53. [DOI] [PubMed] [Google Scholar]
Forst 2006 {published data only}
- Forst L, Noth IM, Lacey S, Bauer S, Skinner S, Petrea R, et al. Barriers and benefits of protective eyewear use by Latino farm workers. Journal of Agromedicine 2006;11(2):11‐7. [DOI] [PubMed] [Google Scholar]
Mancini 2005 {published data only}
- Mancini G, Baldasseroni A, Laffi G, Curti S, Mattioli S, Violante FS. Prevention of work related eye injuries: long term assessment of the effectiveness of a multicomponent intervention among metal workers. Occupational and Environmental Medicine 2005;62:830‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murthy 1994 {published data only}
- Murthy GV, Verma L, Ahuja S. Evaluation of an innovative school eye health educational mode. Indian Pediatrics 1994;31(5):553‐7. [PubMed] [Google Scholar]
Additional references
Canavan 1980
- Canavan YM, O'Flaherty MJ, Archer DB, Elwood JH. A 10‐year survey of eye injuries in Northern Ireland 1967‐76. British Journal of Ophthalmology 1980;64(8):618‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2005
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5 [updated May 2005]. http://www.cochrane.org/resources/handbook/hbook.htm (accessed July 2006).
Khatry 2004
- Khatry SK, Lewis AE, Schein OD, Thapa MD, Pradhan EK, Katz J. The epidemiology of ocular trauma in rural Nepal. British Journal of Ophthalmology 2004;88(4):456‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Krisnainah 2006
- Krishnaiah S, Nirmalan PK, Shamanna BR, Srinivas M, Rao GN, Thomas R. Ocular trauma in a rural population of southern India: the Andhra Pradesh Eye Disease Study. Ophthalmology 2006;113(7):1159‐64. [DOI] [PubMed] [Google Scholar]
Kuhn 2004
- Kuhn F, Morris R, Witherspoon CD, Mester V. The Birmingham Eye Trauma Terminology system (BETT). Journal Français d'Ophtalmologie 2004;27(2):206‐10. [DOI] [PubMed] [Google Scholar]
Lipscomb 2000
- Lipscomb HJ. Effectiveness of interventions to prevent work‐related eye injuries. American Journal of Preventive Medicine 2000;18(4S):27‐32. [DOI] [PubMed] [Google Scholar]
MacEwen 1999
- MacEwen CJ. Ocular injuries. Journal of the Royal College of Surgeons of Edinburgh 1999;44(5):317‐23. [PubMed] [Google Scholar]
Negrel 1998
- Negrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiology 1998;5(3):143‐69. [DOI] [PubMed] [Google Scholar]
RevMan 2008 [Computer program]
- The Nordic Cochrane Centre. The Cochrane Collaboration. Review Manager (RevMan). Version 5.0. Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration, 2008.
Thomas 2003
- Thomas H. Quality assessment tool for quantitative studies. Effective Public Health Practice Project (http://www.myhamilton.ca/myhamilton/CityandGovernment/HealthandSocialServices/Research/EPHPP/) 2003. Accessed 3 August 2009.
USEIR
- US Eye Injury Register. www.useironline.org. Accessed 3 August 2009.
Vernon 1984
- Vernon SA, Yorston DB. Incidence of ocular injuries from road traffic accidents after introduction of seat belt legislation. Journal of the Royal Society of Medicine 1984;77(3):198‐200. [DOI] [PMC free article] [PubMed] [Google Scholar]


