Abstract
Background/Purpose
Because of the spread of novel coronavirus disease 2019 (COVID-2019), preventive COVID-19 infection behaviors become important for individuals, especially those who are vulnerable. The present study proposes a model to explain the preventive COVID-19 infection behaviors among people with mental illness in Taiwan.
Methods
A cross-sectional design was carried out and 414 patients with mental illness (230 males [55.6%]; mean age = 46.32 [SD = 10.86]) agreed to participate in the study. All the participants completed the Preventive COVID-19 Infection Behaviors Scale, Self-Stigma Scale-Short, Believing COVID-19 Information Scale, Fear of COVID-19 Scale, and Depression Anxiety Stress Scale-21. Regression models and structural equation modeling (SEM) were applied to examine the factors associated with preventive COVID-19 infection behaviors.
Results
Both regression models and SEM showed that trust in COVID-19 information sources (standardized coefficient [β] = 0.211 in regression; β = 0.194 in SEM) and fear of COVID-19 (β = −0.128 in regression; β = −0.223 in SEM) significantly explained preventive behaviors among individuals with mental illness. The SEM further showed that fear of COVID-19 was significantly explained by trust in COVID-19 information sources (β = 0.220) and self-stigma (β = 0.454).
Conclusion
Based on the results, healthcare providers should help individuals with mental illness reduce self-stigma and fear of COVID-19 which would consequently improve their preventive COVID-19 infection behaviors. Moreover, improving trust in COVID-19 information sources for individuals with mental illness may be another method to improve their preventive behaviors.
Keywords: COVID-19, Fear, Preventive behavior, Psychological distress, Self-stigma
Introduction
With the spread of novel coronavirus disease 2019 (COVID-19) worldwide, health behaviors – especially preventive behaviors by individuals – has become crucial. More specifically, with the awareness and practice of preventive behaviors, the transmission rate of infectious disease can be reduced.1, 2, 3 Shaw et al.2 described how the governments' actions and citizens' behaviors are associated with the inhibition of COVID-19 infection among different East Asian countries. In brief, preventive behaviors can be classified into community level (often implemented by authorized policies) and individual level (often practiced by person based on their beliefs).1 , 2 For instance, spatial distancing has been implemented in many countries to avoid the possibility of infection transmission.4 Such policies appear to be effective because COVID-19 infection rates were lower in countries that applied early preventive policies such as quarantine and closure of non-essential shops and schools.2 , 5 However, reliance on government action alone is insufficient to totally control COVID-19 infection and the World Health Organization (WHO)6 proposed a number of personal preventive behaviors for individuals to engage in to control COVID-19 infection. Therefore, understanding the factors that associated with individuals’ preventive behaviors is an important topic during the COVID-19 pandemic.
After reviewing the literature, the present authors identified three factors that are associated with preventive COVID-19 infection behaviors (i.e., trust in COVID-19 information sources, fear of COVID-19, and psychological distress). Trust in COVID-19 information sources is important because different sources (e.g., social media platforms) are usually used to disseminate how to practice preventive behaviors7 , 8 and trust in such information may increase individuals' good practice in preventive behaviors. Although misconceptions concerning COVID-19 have been found in social media,9 many authorities have used different methods to prevent such misinformation (e.g., penalties for those who distribute false information). Taiwan (where the present study was carried out) has effectively prevented such misinformation.8 Nevertheless, some accurate COVID-19 information (e.g., the death rate and numbers of confirmed cases) may trigger an individual's fear of COVID-19 and induce psychological distress.10 Therefore, trust in COVID-19 information sources may improve individuals' prevention behaviors but jeopardize their mental health, including the increase in the fear of COVID-19 and psychological distress.
Several theories, including the Health Belief Model,11 the Fear Drive Model,12 and the Protection Motivation Theory,13 manipulate fear to facilitate an individual in practicing preventive behaviors to avoid infection. However, extreme fear (for individuals who cannot handle the fear they perceive) may lead to irrational thinking14 and subsequently inhibit practicing preventive behaviors. Moreover, fear of COVID-19 may induce individuals to perform inappropriate behaviors, such as panic purchase, discrimination, and even suicide.15, 16, 17 Indeed, a meta-analysis showed that when individuals cannot control fear, they defensively resist preventive behaviors.18 Therefore, individuals with mental illness may have difficulties in controlling fear and resist engaging in preventive COVID-19 infection behavior. Apart from the potential negative association between fear of COVID-19 and preventive COVID-19 infection behavior, fear of COVID-19 has been found to be associated with psychological distress in studies carried out in different countries.19, 20, 21 Therefore, it is likely that psychological distress also has a negative association with preventive COVID-19 infection behaviors.
Although trust in COVID-19 information sources, fear of COVID-19, and psychological distress have been identified among the general population during the COVID-19 pandemic, it is not known how these factors influence vulnerable populations. Therefore, the present study specifically investigated a vulnerable population (i.e., individuals with mental illness). Such individuals are an especially vulnerable group during the current pandemic. For example, they may not have ability to distinguish good from bad COVID-19 information,22 and they may have more difficulties than general population in handling their mood.22
Moreover, individuals with mental illness often have self-stigma issues that prevent them from performing health behaviors such as treatment compliance.23 Individuals with mental illness and self-stigma are reluctant to adhere to treatment because they have high levels of psychological distress and lower levels of self-esteem.24 , 25 Therefore, it is possible that individuals with mental illness may not want to perform preventive COVID-19 infection behaviors if they have self-stigma issues. However, to the best of the present authors’ knowledge, there is no empirical evidence for healthcare providers to understand the role of self-stigma for individuals with mental illness during COVID-19 pandemic. Consequently, understanding how self-stigma associated with preventive COVID-19 infection behaviors is of great importance. In addition, self-stigma may positively associate with fear of COVID-19 and psychological distress among individuals with mental illness.
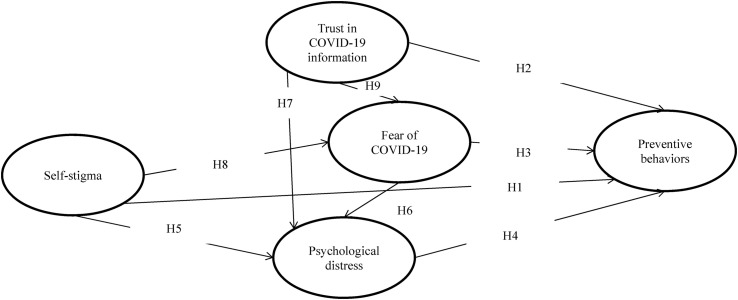
The present study investigated the potential factors explaining preventive COVID-19 infection behaviors among individuals with mental illness in Taiwan. The following hypotheses were formulated based on the aforementioned literature: H1 – self-stigma will be negatively associated with preventive COVID-19 infection behaviors; H2 – trust in COVID-19 information sources will be positively associated with preventive COVID-19 infection behaviors; H3 – fear of COVID-19 will be negatively associated with preventive COVID-19 infection behaviors; H4 – psychological distress will be negatively associated with preventive COVID-19 infection behaviors; H5 self-stigma will be positively associated with psychological distress; H6 – trust in COVID-19 information sources will be positively associated with psychological distress; H7 – fear of COVID-19 will be positively associated with psychological distress; H8 – self-stigma will be positively associated with fear of COVID-19; and H9 – trust in COVID-19 information sources will be positively associated with fear of COVID-19 (Fig. 1 ).
Figure 1.
Proposed model that explains preventive behaviors among individuals with mental illness.
Methods
Study design, participants, and recruitment procedure
The present study adopted a cross-sectional design and commenced after the Taiwan government had already tightened the regulations for many hospitals and clinics to avoid unnecessary contact between different personnel, including medical staff, patients, and outside visitors. Moreover, during this period, the Taiwan government implemented policies in controlling COVID-19 misinformation on social media to eliminate the public panic toward COVID-19 pandemic. The study protocol was approved by the Institute of Review Board (IRB) of the Jianan Psychiatric Center (JPC), Ministry of Health and Welfare (IRB numbers: 20-004). The JPC is located in Tainan, a city of southern Taiwan, and is the sole teaching center providing psychiatric service in this area. Moreover, the psychiatric treatment network of the JPC extends to the entire southern Taiwan region, which indicates its capacity in providing mental health service to more than three million residents who were living in the region. Furthermore, the JPC provides different program services (e.g., daycare programs, outpatient services, and inpatient rehabilitation programs) to thousands of individuals with mental illness.
Following the regulations proposed by the Taiwan government, the JPC adopted dynamic measures that requested every employee to check for fever and declare infection-related information (including health condition, contact, and travel history) before entering the JPC. The data collection period was between March 23 and June 30 (2020) with eligible participants being recruited from the inpatient rehabilitation programs, daycare, and outpatient units. The inclusion criteria of the present study's participants included: (i) having at least one major diagnosis of mental disorder made by one experienced psychiatrist according to the criteria from the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5); (ii) being aged 20 years or above; (iii) having a relatively stable condition as confirmed by a psychiatrist; and (iv) having sufficient cognition to understand the study purpose, provide written informed consent, and complete the measures. The exclusion criteria included having: (i) any neurological disease history; (ii) any severe and unstable medical disease, such as cancer; (iii) any head injury history; and (iv) been an inpatient because inpatients' preventive behaviors were monitored by JPC staff. A total of 414 participants took part in the study.
Measures
Preventive COVID-19 Infection Behaviors Scale (PCIBS)
Considering the five preventive behaviors recommended by the WHO,6 the five-item PCIBS was developed using a five-point Likert scale to quantify how an individual regularly performs preventive behaviors. More specifically, the five-point Likert scale scores from 1 (almost never) to 5 (almost always) with a higher PCIBS score indicating a higher frequency in performing preventive behaviors. “I stay home more when I feel unwell” is an example item in the PCIBS. The PCIBS has demonstrated moderate correlations with psychological distress in a recent study, and reported satisfactory concurrent validity.26 The present study's data showed that the PCIBS had very good internal consistency (α = .77).
Self-Stigma Scale-Short (SSS–S)
Considering stereotypes, emotional responses, and behaviors induced by self-endorsed misconception of mental illness, the nine-item SSS-S was developed using a four-point Likert scale to assess self-stigma. More specifically, the four-point Likert scale scores from 1 (strongly disagree) to 4 (strongly agree) with a higher SSS-S score indicating a greater level of self-stigma. “I feel uncomfortable because I have a mental illness” is an example item in the SSS-S. The SSS-S has demonstrated satisfactory psychometric properties, including internal consistency and construct validity, in samples of Taiwanese individuals with mental illness.27 , 28 The present study showed that the SSS-S had excellent internal consistency (α = .95).
Believing COVID-19 Information Scale (BCIS)
Considering commonly used social media among Taiwanese individuals,6 the six-item BCIS was developed using a five-point Likert scale to assess the extent that an individual trusts COVID-19 information they have obtained. More specifically, the five-point Likert scale scores from 1 (strongly disbelieve) to 5 (strongly believe) with a higher BCIS score indicating a greater level of believing in the information of COVID-19. “How much do you believe in the COVID-19 information in Facebook” is an example item in the BCIS. The present study's data showed that the BCIS had excellent internal consistency (α = .87).
Fear of COVID-19 scale (FCV–19S)
Considering fear symptoms, the seven-item FCV-19S was developed using a five-point Likert scale to assess how an individual fears COVID-19. More specifically, the five-point Likert scale scores from 1 (strongly disagree) to 5 (strongly agree) with a higher FCV-19S score indicating a higher level of fear toward COVID-19. “I cannot sleep because I'm worrying about getting coronavirus-19” is an example item in the FCV-19S. The FCV-19S has demonstrated very good psychometric properties, including internal consistency and construct validity, in a large sample of general Iranian population.29 Moreover, the Chinese FCV-19S was found to be psychometrically sound recently6 , 30 The present study's data showed that the FCV-19S had excellent internal consistency (α = .92).
Depression Anxiety Stress Scale-21 (DASS-21)
Considering the symptoms of different types of psychological distress, the 21-item DASS-21 was developed using a four-point Likert scale to assess how an individual suffers from depression (seven items), anxiety (seven items), and stress (seven items). More specifically, the four-point Likert scale scores from 0 (never) to 3 (almost always) with higher DASS-21 total scores indicating a greater level of psychological distress. “I felt that I was close to panic” is an example item in the DASS-21. The DASS-21 has demonstrated satisfactory psychometric properties, including internal consistency and construct validity, in Korean samples with and without mental illness.31 The present study's data showed that the DASS-21 had excellent internal consistency (α = .96).
Background information
Background information of the participants was obtained from self-reports, including age, gender, educational year, and marital status. Moreover, diagnoses of the participants’ mental illness were retrieved from their medical records.
Data analysis
In addition to the descriptive statistics that illustrate the participants’ characteristics, Pearson correlation was carried out to understand the associations between the studied variables. Following this, two regression models were constructed to understand the factors that could explain preventive COVID-19 infection behaviors among individuals with mental illness. More specifically, the first regression model only included controlled variables (age, gender, and years of education) to explain preventive behaviors. The second regression model (based on the first one) added the independent variables of self-stigma, trust in COVID-19 information sources, fear of COVID-19, and psychological distress. Finally, a path model with latent constructs was proposed using structural equation modeling (SEM) to further understand the factors associated with the preventive COVID-19 infection behaviors (Fig. 1). More specifically, the model was aligned with the hypotheses that (i) self-stigma explained fear of COVID-19, psychological distress, and preventive behavior; (ii) trust in COVID-19 information sources explained fear of COVID-19, psychological distress, and preventive behavior; (iii) fear of COVID-19 explained psychological distress and preventive behavior; and (iv) psychological distress explained preventive behavior.
In the SEM model, all the studied variables (self-stigma, trust in COVID-19 information sources, fear of COVID-19, psychological distress, and preventive behaviors) were treated as latent constructs. Moreover, age, gender, and year of education were controlled in the SEM model. The SEM model was estimated using maximum likelihood method and missing data were handled using full information maximum likelihood method. Additionally, fit indices were used to examine whether the SEM model is supported: comparative fit index (CFI) > .9; Tucker–Lewis index (TLI) > .9, root mean square error of approximation (RMSEA) < .08; and standardized root mean square residual (SRMR) < .08 were thus adopted to indicate good fit.32 , 33 Given that there were five missing values (∼1.2%) in the present study, full information maximum likelihood method was applied to impute the missing information. All the data analyses were performed using IBM SPSS Statistics for Windows, Version 24.0 (IBM corp., Armonk, NY), except for the SEM model, which was analyzed using lavaan package in the R software.
Results
Among the 414 participants, more than half were males (n = 230; 55.6%), the majority were single (n = 208; 50.2%), and the most common major diagnosis was schizophrenia (n = 197; 47.6%). The mean age of the participants was 46.32 (SD = 10.86) years and their mean years of education was 10.89 years (SD = 3.25). Table 1 also presents the participants’ scores on each measure. Moreover, the associations between the studied variables are presented in Table 2 , where significantly moderate associations were observed between self-stigma, fear of COVID-19, and psychological distress (r = .339 to .494; all p-values < .001). Furthermore, trust in COVID-19 information sources was significantly correlated with fear of COVID-19 (r = .215; p < .001) and preventive behavior (r = .176; p < .001).
Table 1.
Participants’ characteristics (N = 414).
| n (%) | Mean (SD) | Range | |
|---|---|---|---|
| Gender | 414 (100.0) | ||
| Male | 230 (55.6) | ||
| Female | 184 (44.4) | ||
| Marital status | 414 (100.0) | ||
| Married | 130 (31.4) | ||
| Single | 208 (50.2) | ||
| Others | 76 (18.3) | ||
| Age (year) | 414 (100.0) | 46.32 (10.86) | 20–74 |
| Major Diagnosis | 414 (100.0) | ||
| Schizophrenia | 197 (47.6) | ||
| Bipolar disorder | 35 (8.5) | ||
| Major depression disorder | 34 (8.2) | ||
| Substance use | 141 (34.1) | ||
| Anxiety | 7 (1.7) | ||
| Years of education | 414 (100.0) | 10.89 (3.25) | 0–18 |
| Self-stigma score | 409 (98.8)a | 2.14 (0.81) | 1–4 |
| Fear of COVID-19 | 413 (99.8)a | 2.34 (1.00) | 1–5 |
| Trust in COVID-19 information | 413 (99.8)a | 3.31 (0.62) | 1–5 |
| Preventive behavior | 413 (99.8)a | 3.61 (0.92) | 1–5 |
| Psychological distress | 411 (99.3)a | 14.88 (4.96) | 0–63 |
With missing values.
Table 2.
Correlations between studied variables.
|
r (p-value) |
||||||||
|---|---|---|---|---|---|---|---|---|
| Age | Gender | Educationa | Self-stigma | Trustb | Fearc | Distress | Behavior | |
| Age | ||||||||
| Gender | −.002 (.96) | – | ||||||
| Educationa | −.275 (<.001) | .022 (.66) | – | |||||
| Self-stigma | −.112 (.024) | −.016 (.75) | .077 (.12) | – | ||||
| Beliefb | −.005 (.92) | −.084 (.09) | .045 (.37) | .047 (.35) | – | |||
| Fearc | −.003 (.95) | .006 (.90) | −.037 (.45) | .415 (<.001) | .215 (<.001) | –` | ||
| Distress | −.021 (.67) | −.148 (.003) | .019 (.70) | .494 (<.001) | .026 (.60) | .339 (<.001) | – | |
| Behavior | .101 (.04) | −.135 (.006) | −.008 (.88) | −.059 (.23) | .176 (<.001) | −.097 (.048) | −.018 (.72) | – |
Years of education.
Trust in COVID-19 information.
Fear of COVID-19.
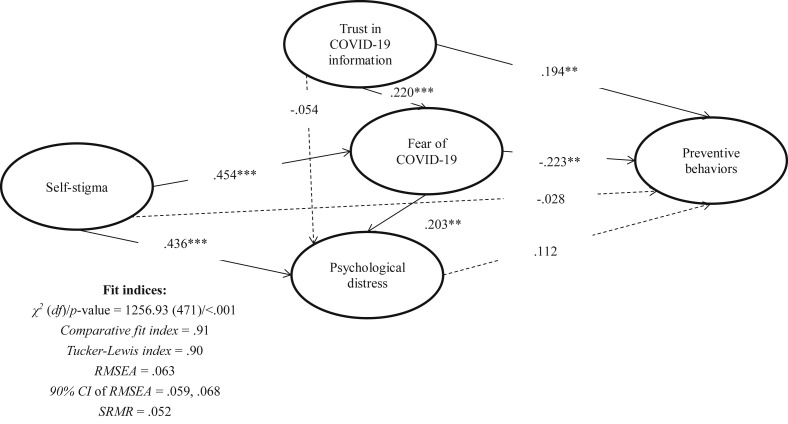
The regression models showed that trust in COVID-19 information sources (standardized coefficient [β] = .211; p < .001) and fear of COVID-19 (β = −.140; p < .01) were the most relevant factors explaining COVID-19 preventive behaviors among individuals with mental illness (Table 3 ). Similar findings are shown in the SEM model, which had satisfactory model fit (CFI = .91; TLI = .90; RMSEA = .063; SRMR = .052), that preventive behaviors were significantly explained by trust in COVID-19 information sources (β = .194; p < .01) and fear of COVID-19 (β = −.223; p < .01). Moreover, a scrutinized observation in the SEM model (Fig. 2 ) indicates that psychological distress was significantly explained by fear of COVID-19 (β = .203; p < .01) and self-stigma (β = .436; p < .001); fear of COVID-19 was significantly explained by trust in COVID-19 information sources (β = .220; p < .001) and self-stigma (β = .454; p < .001). In summary, H2, H3, H5, H6, H8, and H9 were supported. The three remaining hypotheses (H1, H4, and H7) were not supported.
Table 3.
Regression models explaining preventive behaviors among individuals with mental illness.
|
B (SE)/β (95% CI) |
||
|---|---|---|
| Model 1 | Model 2 | |
| Demographics | ||
| Age | 0.009 (0.004)/.110 (0.002, 0.018)∗ | 0.009 (0.004)/.104 (0.0004, 0.017)∗ |
| Gender (Ref: female) | −0.250 (0.090)/-.136 (−0.427, −0.073)∗∗ | −0.194 (0.090)/-.105 (−0.370, −0.017)∗ |
| Years of education | 0.006 (0.014)/.023 (−0.022, 0.035) | 0.002 (0.014)/.007 (−0.026, 0.030) |
| Psychological variables | ||
| Self-stigma | −0.048 (0.066)/-.043 (−0.177, 0.081) | |
| Trust in COVID-19 information | 0.313 (0.073)/.211 (0.170, 0.457)∗∗∗ | |
| Fear of COVID-19 | −0.128 (0.050)/-.140 (−0.227, −0.029)∗∗ | |
| Psychological distress |
0.005 (0.003)/.082 (−0.002, 0.012) |
|
|
Model fit | ||
| F-value (p-value) | 4.10 (.007) | 5.14 (<.001) |
| R2(Adjusted R2) | .029 (.022) | .082 (.066) |
∗p < .05; ∗∗p < .01; ∗∗∗p < .001.
Figure 2.
Proposed model with standardized coefficients in explaining preventive behaviors among individuals with mental illness. Solid lines indicate significant paths; dashed lines indicate nonsignificant paths. Age, gender, and years of education are controlled in the model. ∗p < .05; ∗∗p < .01; ∗∗∗p < .001. RMSEA = root mean square error of approximation; SRMR = standardized root mean square residual.
Discussion
Engaging in preventive behaviors is important for inhibiting the COVID-19 transmission rate.2 The present study proposed a model specifically for individuals with mental illness to understand relevant factors associated with their preventive COVID-19 behaviors. Among the nine hypotheses made in the proposed model, six were supported (H2, H3, H5, H6, H8, and H9) and three were not (H1, H4, and H7). More specifically, greater trust in COVID-19 information sources and less fear of COVID-19 explained more preventive behaviors; higher levels of self-stigma and greater trust in COVID-19 information sources explained more psychological distress; and higher levels of self-stigma and greater trust in COVID-19 information sources explained more fear of COVID-19.
Individuals living with mental illness who had a greater level of trust in COVID-19 information engaged in more preventive COVID-19 infection behaviors. A previous study also showed that higher trust in health information sources concerning cigarette was associated with healthier behavior.34 Trust in information sources is an important part of evaluation for monitoring in how individuals perceive risk and cope with stress differently during the COVID-19 pandemic.35 Individuals with lower socioeconomic status have been found to trust less legitimate sources such as television, social media, or friends more than healthcare professionals.36 Although the Taiwanese government fined and banned individuals disseminating misinformation regarding COVID-19 (from the beginning of the outbreak in February 2020) and legislated that COVID-19 messages on social media had to be accurate, it is still possible that individuals living with mental illness received false information from informal sources. Given the positive association between trust in information sources and COVID-19 preventive behavior, more instructions on how individuals can easily protect themselves from getting infected should be disseminated via various channels.
The present study showed that higher trust in COVID-19 information sources was associated with increased fear of COVID-19 among individuals living with mental illness. Higher trust in COVID-19 information sources may indicate higher exposure and acceptance of COVID-19 information. It is likely that the more individuals living with mental illness are exposed to COVID-19 information, the more fear generated because their lack of understanding of such a new health issue with no effective treatment. This finding is consistent with the Heuristic-Systematic Model, which highlights that individuals with prior knowledge about a topic have lower impact of fear arousal from fear appeals messages of health campaigns.37 Public health campaigns or governments should balance the fact that fear may be an unexpected consequence resulted from providing COVID-19 messages daily via multiple channels. For individuals who do not have resources to filter out useful information or to evaluate their personal risk, additional reassurance for their safety or interpretation of messages from the government on social media and broadcast media may help individuals lower the fear.
As hypothesized, the present study found that more fear of COVID-19 was associated with less preventive COVID-19 infection behaviors but more psychological distress. Fear may promote individuals to engage in preventive behaviors because fear of COVID-19 may motivate individuals to engage in behaviors that prevent them from infection.11, 12, 13, 14 Indeed, Harper et al.38 found that FCV-19S scores were positively correlated with behavior change in preventive COVID-19 infection behaviors. However, evidence from Harper et al.’s study38 was on the general population and therefore their findings may not be replicable for individuals with mental illness. More specifically, the relationship between fear and behaviors is complex14 as other evidence has shown that fear may lead to irrational behaviors.15 , 17 Because individuals with mental illness usually suffer from poor mood control and cognitive impairment,39 , 40 they may have difficulties in practicing preventive behaviors if they perceive unbearable fear. This finding also concurs with the meta-analysis findings from Witte and Allen18 who reported that individuals experiencing difficulties with fear control are less likely to engage in recommended behaviors. In addition, they may have increased psychological distress associated with the fear of COVID-19, like prior research has found in general populations.10
Although self-stigma was not associated with COVID-19 preventive behaviors in the present study, self-stigma was associated with fear of COVID-19 and psychological distress. A possible reason for the nonsignificant association between self-stigma and preventive behaviors is that self-stigma does not directly associate with preventive behaviors. Rather, the association between self-stigma and preventive behaviors was via fear of COVID-19. Indeed, self-stigma was found to be highly associated with fear of COVID-19, and fear of COVID-19 was associated with COVID-19 preventive behaviors. When individuals with mental illness have self-stigma, they may feel incompetence and are afraid of disclosing their illness identity.23 Therefore, individuals with mental illness may have an elevated fear of COVID-19 because they may disclose their mental illness identity if they are affected by COVID-19. That is, they have to visit a physician for COVID-19 treatment and discuss their mental illness. Another explanation is that individuals with mental illness who have self-stigma may worry that healthcare providers may provide poorer quality service and/or have more negative attitudes to them compared with people with no mental illness if they have COVID-19. More specifically, one route for individuals with mental illness to develop self-stigma is through uncomfortable previous experiences (e.g., being laughed and/or not being respected).27 Such experiences may also induce their fear of COVID-19. Moreover, the association between self-stigma and psychological distress found in the present study concurs with prior findings.24 , 25
There are some limitations in the present study. First, the study adopted a cross-sectional design and as such the findings are unable to determine any causal relationship, although the model proposes potential directions among the studied variables. Second, all the measures used in the present study were self-report (or with the assistance of an assistant researcher). Therefore, the associations found in the present study might be influenced by common variance bias. Moreover, other biases such as recall bias and social desirability bias might exit using self-report methods. Nevertheless, using self-reports in the present study had the benefits of low-cost and rapid data collection that can respond in a timely fashion to the need of reaction toward COVID-19 during the pandemic. However, future studies may consider using other types of measurement method (e.g., actually observing preventive behaviors) to corroborate the present study's findings. Third, the participants were in stable condition during the study period. Therefore, the present study's findings may not be generalized to those with a severe mental illness. Fourth, the participants were recruited solely from one institution in Taiwan. Given that different countries have implemented different policies to respond to the threat and infection of COVID-19, individuals with mental illness may receive different levels of COVID-19 information and have different levels of trust in the information. Therefore, the present study's findings may not be replicate to other countries due to the different policies and cultures.
Conclusions
The present study proposed a model to understand preventive COVID-19 infection behaviors among a sample of individuals with mental illness in Taiwan. The results showed that trust in COVID-19 information sources and fear of COVID-19 were significant factors explaining preventive behaviors via different factors. More trust in COVID-19 information sources was associated with more COVID-19 preventive behaviors, while more fear of COVID-19 was associated with less COVID-19 preventive behaviors. Additionally, higher levels of self-stigma and greater trust in COVID-19 information sources were associated with stronger fear of COVID-19. Therefore, healthcare providers may want to reduce self-stigma and fear of COVID-19 among individuals with mental illness to improve the likelihood of engaging in preventive COVID-19 infection behaviors. Moreover, improving trust in COVID-19 information sources for individuals with mental illness may be another method to improve their COVID-19 preventive behaviors.
Funding source declaration
This Project was supported by grants from the Ministry of Health and Welfare, Executive Yuen, Taiwan (MOHW-10961 and MOHW-10962) and partially supported by the following grants funded by the Ministry of Science and Technology, Executive Yuen, Taiwan (MOST 108-2314-B-695-001). The funder had no role in the study design, data analysis, or preparation of this manuscript.
Declaration of Competing Interest
The authors have no conflicts of interest relevant to this article.
References
- 1.Mao L. Evaluating the combined effectiveness of influenza control strategies and human preventive behavior. PloS One. 2011;6:e24706. doi: 10.1371/journal.pone.0024706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shaw R., Kim Y-k, Hua J. Governance, technology and citizen behavior in pandemic: lessons from COVID-19 in East Asia. Prog Disaster Sci. 2020;6:100090. doi: 10.1016/j.pdisas.2020.100090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sim S.W., Moey K.S., Tan N.C. The use of facemasks to prevent respiratory infection: a literature review in the context of the Health Belief Model. Singapore Med J. 2014;55:160–167. doi: 10.11622/smedj.2014037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abel T., McQueen D. The COVID-19 pandemic calls for spatial distancing and social closeness: not for social distancing! Int J Public Health. 2020;65:231. doi: 10.1007/s00038-020-01366-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang C.J., Ng C.Y., Brook R.H. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. J Am Med Assoc. 2020 doi: 10.1001/jama.2020.3151. Advance online publication. [DOI] [PubMed] [Google Scholar]
- 6.Chang K.-C., Hou W.-L., Pakpour A.H., Lin C.-Y., Griffiths M.D. Psychometric testing of three COVID-19-related scales among people with mental illness. Int J Ment Health Addict. 2020 doi: 10.1007/s11469-020-00361-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Basch C.H., Hillyer G.C., Meleo-Erwin Z.C., Jaime C., Mohlman J., Basch C.E. Preventive behaviors conveyed on YouTube to mitigate transmission of COVID-19: cross-sectional study. JMIR Public Health Surveill. 2020;6:e18807. doi: 10.2196/18807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duffy C. How health officials and social media are teaming up to fight the coronavirus "infodemic". 2020. https://www.cnn.com/2020/03/01/tech/coronavirus-social-media-reliable-sources/index.html Available from:
- 9.Geldsetzer P. Knowledge and perceptions of COVID-19 among the general public in the United States and the United Kingdom: a cross-sectional online survey. Ann Intern Med. 2020 doi: 10.7326/M20-0912. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Green E.C., Murphy E. Health belief model. In: Dingwall R., Quah S., editors. Cockerham WC. Illness, Behavior, and Society; 2014. (The Wiley Blackwell encyclopedia of health). [DOI] [Google Scholar]
- 12.Leventhal H., Safer M.A., Panagis D.M. The impact of communications on the self-regulation of health beliefs, decisions, and behavior. Health Educ Q. 1983;10:3–29. doi: 10.1177/109019818301000101. [DOI] [PubMed] [Google Scholar]
- 13.Rogers R.W. A protection motivation theory of fear appeals and attitude change. J Psychol. 1975;91:93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- 14.Pakpour A.H., Griffiths M.D. The fear of COVID-19 and its role in preventive behaviors. J Concurrent Disord. 2020;2:58–63. [Google Scholar]
- 15.Bhuiyan A.I., Sakib N., Pakpour A.H., Griffiths M.D., Mamun M.A. COVID-19-related suicides in Bangladesh due to lockdown and economic factors: case study evidence. Int J Ment Health Addict. 2020 doi: 10.1007/s11469-020-00307-y. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin C.-Y. Social reaction toward the 2019 novel coronavirus (COVID-19) Soc Health Behav. 2020;3:1–2. doi: 10.4103/SHB.SHB_11_20. [DOI] [Google Scholar]
- 17.Taylor S., Landry C., Paluszek M., Fergus T.A., Mckay D., Asmundson G.J.G. Development and initial validation of the COVID stress scales. J Anxiety Disord. 2020 doi: 10.1016/j.janxdis.2020.102232. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Witte K., Allen M. A meta-analysis of fear appeals: implications for effective public health campaigns. Health Educ Behav. 2000;27:591–615. doi: 10.1177/109019810002700506. [DOI] [PubMed] [Google Scholar]
- 19.Sakib N., Mamun M.A., Bhuiyan A.K.M.I., Hossain S., Mamun F.A., Hosen I. Psychometric validation of the bangla fear of COVID-19 scale: confirmatory factor analysis and rasch analysis. Int J Ment Health Addict. 2020 doi: 10.1007/s11469-020-00289-x. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Satici B., Gocet-Tekin E., Deniz M.E., Satici S.A. Adaptation of the Fear of COVID-19 Scale: its association with psychological distress and life satisfaction in Turkey. Int J Ment Health Addict. 2020 doi: 10.1007/s11469-020-00294-0. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Soraci P., Ferrari A., Abbiati F.A., Del Fante E., De Pace R., Urso A. Validation and psychometric evaluation of the Italian version of the Fear of COVID-19 Scale. Int J Ment Health Addict. 2020 doi: 10.1007/s11469-020-00277-1. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fung K.M.T., Tsang H.W.H., Corrigan P.W. Self-stigma of people with schizophrenia as predictor of their adherence to psychosocial treatment. Psychiatr Rehabil J. 2008;32:95–104. doi: 10.2975/32.2.2008.95.104. [DOI] [PubMed] [Google Scholar]
- 24.Huang W.-Y., Chen S.-P., Pakpour A.H., Lin C.-Y. The mediation role of self-esteem for self-stigma on quality of life for people with schizophrenia: a retrospectively longitudinal study. J Pac Rim Psychol. 2018;12:e10. doi: 10.1017/prp.2017.18. [DOI] [Google Scholar]
- 25.Lin C.-Y., Chang C.-C., Wu T.-H., Wang J.-D. Dynamic changes of self-stigma, quality of life, somatic complaints, and depression among people with schizophrenia: a pilot study applying kernel smoothers. Stigma Health. 2016;1:29–43. doi: 10.1037/sah0000014. [DOI] [Google Scholar]
- 26.Ahorsu D.K., Imani V., Lin C.-Y., Timpka T., Broström A., Updegraff J.A. Associations between fear of COVID-19, mental health, and preventive behaviours across pregnant women and husbands: an actor-partner interdependence modelling. Int J Ment Health Addict. 2020 doi: 10.1007/s11469-020-00270-8. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chang C.-C., Lin C.-Y., Gronholm P.C., Wu T.-H. Cross-validation of two commonly used self-stigma measures, Taiwan versions of the Internalized Stigma Mental Illness Scale and Self-Stigma Scale-Short, for people with mental illness. Assessment. 2018;25:777–792. doi: 10.1177/1073191116658547. [DOI] [PubMed] [Google Scholar]
- 28.Wu T.-H., Chang C.-C., Chen C.-Y., Wang J.-D., Lin C.-Y. Further psychometric evaluation of the Self-Stigma Scale-Short: measurement invariance across mental illness and gender. PloS One. 2015;10:e0117592. doi: 10.1371/journal.pone.0117592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ahorsu D.K., Lin C.-Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. Fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict. 2020 doi: 10.1007/s11469-020-00270-8. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pakpour A.H., Griffiths M.D., Chang K.-C., Chen Y.-P., Kuo Y.-J., Lin C.-Y. Brain Behav Immun; 2020. Assessing the fear of COVID-19 among different populations: a response to Ransing et al. (2020) Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee E.H., Moon S.H., Cho M.S., Park E.S., Kim S.Y., Han J.S. The 21-item and 12-item versions of the depression anxiety stress scales: psychometric evaluation in a Korean population. Asian Nurs Res. 2019;13:30–37. doi: 10.1016/j.anr.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 32.Lin Y.-C., Fung X.C.C., Tsai M.-C., Strong C., Hsieh Y.-P., Lin C.-Y. Insufficient physical activity and overweight: does caregiver screen-viewing matter? J Child Fam Stud. 2019;28:286–297. doi: 10.1007/s10826-018-1247-5. [DOI] [Google Scholar]
- 33.Yam C.-W., Pakpour A.H., Griffiths M.D., Yau W.-Y., Lo C.-L.M., Ng J.M.T. Psychometric testing of three Chinese online-related addictive behavior instruments among Hong Kong university students. Psychiatr Q. 2019;90:117–128. doi: 10.1007/s11126-018-9610-7. [DOI] [PubMed] [Google Scholar]
- 34.Rutten L.J.F., Blake K., Hesse B.W., Ackerson L.K. Isolated and skeptical: social engagement and trust in information sources among smokers. J Cancer Educ. 2011;26:465–473. doi: 10.1007/s13187-011-0201-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Betsch C. How behavioural science data helps mitigate the COVID-19 crisis. Nat Hum Behav. 2020;4:438. doi: 10.1038/s41562-020-0866-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen X., Hay J.L., Waters E.A., Kiviniemi M., Biddle C., Schofield E. Health literacy and use and trust in health information. J Health Commun. 2018;23:724–734. doi: 10.1080/10810730.2018.1511658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Averbeck J.M., Jones A., Robertson K. Prior knowledge and health messages: an examination of affect as heuristics and information as systematic processing for fear appeals. South Commun J. 2011;76:35–54. doi: 10.1080/10417940902951824. [DOI] [Google Scholar]
- 38.Harper C.A., Satchell L.P., Fido D., Latzman R.D. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Ment Health Addict. 2020 doi: 10.1007/s11469-020-00281-5. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goyal A.K., Bansal A., Saini J. Nature walk decrease the depression by instigating positive mood. Soc Health Behav. 2018;1:62–66. doi: 10.4103/SHB.SHB_26_18. [DOI] [Google Scholar]
- 40.Millan M., Agid Y., Brüne M., Bullmore E.T., Carter C.S., Clayton N.S. Cognitive dysfunction in psychiatric disorders: characteristics, causes and the quest for improved therapy. Nat Rev Drug Discov. 2012;11:141–168. doi: 10.1038/nrd3628. [DOI] [PubMed] [Google Scholar]