Abstract
Background
Retinitis pigmentosa (RP) comprises a group of hereditary eye diseases characterized by progressive degeneration of retinal photoreceptors. It results in severe visual loss that may lead to blindness. Symptoms may become manifest during childhood or adulthood which include poor night vision (nyctalopia) and constriction of peripheral vision (visual field loss). Visual field loss is progressive and affects central vision later in the disease course. The worldwide prevalence of RP is approximately 1 in 4000, with 100,000 individuals affected in the USA. At this time, there is no proven therapy for RP.
Objectives
The objective of this review was to synthesize the best available evidence regarding the effectiveness and safety of vitamin A and fish oils (docosahexaenoic acid (DHA)) in preventing the progression of RP.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL), which contains the Cochrane Eyes and Vision Trials Register (2020, Issue 2); Ovid MEDLINE; Embase.com; PubMed; Latin American and Caribbean Health Sciences Literature Database (LILACS); ClinicalTrials.gov; the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP); and OpenGrey. We did not use any date or language restrictions in the electronic searches for trials. We last searched the electronic databases on 7 February 2020.
Selection criteria
We included randomized controlled trials that enrolled participants of any age diagnosed with any degree of severity or type of RP, and evaluated the effectiveness of vitamin A, fish oils (DHA), or both compared to placebo, vitamins (other than vitamin A), or no therapy, as a treatment for RP. We excluded cluster‐randomized trials and cross‐over trials.
Data collection and analysis
We prespecified the following outcomes: mean change from baseline visual field, mean change from baseline electroretinogram (ERG) amplitudes, and anatomic changes as measured by optical coherence tomography (OCT), at one‐year follow‐up, and mean change in visual acuity, at five‐year follow‐up. Two review authors independently extracted data and evaluated risk of bias for all included trials. We also contacted study investigators for further information when necessary.
Main results
In addition to three trials from the previous version of this review, we included a total of four trials with 944 participants aged 4 to 55 years. Two trials included only participants with X‐linked RP and the other two included participants with RP of all forms of genetic predisposition. Two trials evaluated the effect of DHA alone; one trial evaluated vitamin A alone; and one trial evaluated DHA and vitamin A versus vitamin A alone. Two trials recruited participants from the USA, and the other two recruited from the USA and Canada. All trials were at low risk of bias for most domains. We did not perform meta‐analysis due to clinical heterogeneity.
Four trials assessed visual field sensitivity. Investigators found no evidence of a difference in mean values between the groups. However, one trial found that the annual rate of change of visual field sensitivity over four years favored the DHA group in foveal (−0.02 ± 0.55 (standard error (SE)) dB versus −0.47 ± 0.03 dB, P = 0.039), macular (−0.42 ± 0.05 dB versus −0.85 ± 0.03 dB, P = 0.031), peripheral (−0.39 ± 0.02 versus −0.86 ± 0.02 dB, P < 0.001), and total visual field sensitivity (−0.39 ± 0.02 versus −0.86 ± 0.02 dB, P < 0.001). The certainty of the evidence was very low.
The four trials evaluated visual acuity (LogMAR scale) at a follow‐up of four to six years. In one trial (208 participants), investigators found no evidence of a difference between the two groups, as both groups lost 0.7 letters of the Early Treatment Diabetic Retinopathy Study (ETDRS) visual acuity per year. In another trial (41 participants), DHA showed no evidence of effect on visual acuity (mean difference −0.01 logMAR units (95% confidence interval −0.14 to 0.12; one letter difference between the two groups; very low‐certainty evidence). In the third trial (60 participants), annual change in mean number of letters correct was −0.8 (DHA) and 1.4 letters (placebo), with no evidence of between‐group difference. In the fourth trial (572 participants), which evaluated (vitamin A + vitamin E trace) compared with (vitamin A trace + vitamin E trace), decline in ETDRS visual acuity was 1.1 versus 0.9 letters per year, respectively.
All four trials reported electroretinography (ERG). Investigators of two trials found no evidence of a difference between the DHA and placebo group in yearly rates of change in 31 Hz cone ERG amplitude (mean ± SE) (−0.028 ± 0.001 log μV versus −0.022 ± 0.002 log μV; P = 0.30); rod ERG amplitude (mean ± SE) (−0.010 ± 0.001 log μV versus −0.023 ± 0.001 log μV; P = 0.27); and maximal ERG amplitude (mean ± SE) (−0.042 ± 0.001 log μV versus −0.036 ± 0.001 log μV; P = 0.65). In another trial, a slight difference (6.1% versus 7.1%) in decline of ERG per year favored vitamin A (P = 0.01). The certainty of the evidence was very low.
One trial (51 participants) that assessed optical coherence tomography found no evidence of a difference in ellipsoid zone constriction (P = 0.87) over two years, with very low‐certainty evidence. The other three trials did not report this outcome.
Only one trial reported adverse events, which found that 27/60 participants experienced 42 treatment‐related emergent adverse events (22 in DHA group, 20 in placebo group). The certainty of evidence was very low. The rest of the trials reported no adverse events, and no study reported any evidence of benefit of vitamin supplementation on the progression of visual acuity loss.
Authors' conclusions
Based on the results of four studies, it is uncertain if there is a benefit of treatment with vitamin A or DHA, or both for people with RP. Future trials should also take into account the changes observed in ERG amplitudes and other outcome measures from trials included in this review.
Plain language summary
Use of vitamin A and fish oils for retinitis pigmentosa
What is the aim of this review? The aim of this Cochrane Review was to determine whether vitamin A and fish oils work in delaying the continued worsening of vision in people with an inherited condition of the eyes that causes loss of vision (retinitis pigmentosa) and whether these treatments are safe.
Key messages We are uncertain whether giving vitamin A or fish oil, or both to people with retinitis pigmentosa delays the continued worsening of vision, as the certainty of the evidence was very low. More research is needed, in particular information about whether vitamin A and/or fish oil with or without other vitamin supplements may affect clinical outcomes.
What was studied in the review? Retinitis pigmentosa is a group of inherited eye disorders that cause a gradual, yet progressive, loss of vision. People with this eye disorder have difficulty seeing in low‐light conditions, problems with vision out of the corner of the eye, and in most cases, gradually become visually impaired. Vitamin A or fish oils, or both have been proposed as having possible benefit in helping delay the progression of vision loss in this group of people.
What are the main results of the review? We found four studies that were conducted in the USA and Canada, including a total of 944 participants between the ages of 4 and 55 years. The participants were given vitamin A or fish oil, or both because of their inherited eye disorder and were followed for four years. People who were given vitamin A or fish oil, or both, were compared with those who were not given vitamin A or fish oil. Participants in the vitamin A and/or fish oil group were given different doses of vitamin A or fish oil for differing lengths of time. Participants in the no‐vitamin A and/or fish oil group were given pills that did not include vitamin A or fish oil (placebo pills); other treatments thought to prevent progression of vision loss such as multivitamins with or without traces of vitamin A; or no treatment at all.
The review shows that whether vitamin A or fish oil, or both, makes any difference in delaying the progression of visual loss is uncertain.
How up‐to‐date is this review? We searched for studies that had been published up to 7 February 2020.
Summary of findings
Summary of findings 1. Vitamin A and fish oils (docosahexaenoic acid) compared to placebo, vitamins (including vitamin A), or no therapy for retinitis pigmentosa.
| Vitamin A and fish oils (docosahexaenoic acid) compared to placebo, vitamins (including vitamin A), or no therapy for retinitis pigmentosa | |||||
| Patient or population: retinitis pigmentosa Setting: eye hospital Intervention: vitamin A and fish oils (docosahexaenoic acid) Comparison: placebo, vitamins (including vitamin A), or no therapy | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | |
| Risk with placebo, vitamins (including vitamin A), or no therapy | Risk with vitamin A and fish oils (DHA) | ||||
| Visual field sensitivity (visual field) assessed with: measured in decibels (dB) follow‐up: range 4 years to 6 years | Investigators in all 4 trials found no difference in mean values between DHA and placebo groups. However, in 1 trial, the annual rate of change over 4 years showed benefit in favor of the DHA group compared to the placebo group in foveal (−0.02 ± 0.55 (standard error) dB versus −0.47 ± 0.03 dB, P = 0.039), macular (−0.42 ± 0.05 dB versus −0.85 ± 0.03 dB, P = 0.031), peripheral (−0.39 ± 0.02 versus −0.86 ± 0.02 dB, P < 0.001), and total visual field sensitivity (−0.39 ± 0.02 versus −0.86 ± 0.02 dB, P < 0.001). | 881 (4 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | ||
| Visual acuity
change in logMAR visual acuity, may be reported as ETDRS follow‐up: range 4 years to 6 years |
In 1 trial (208 participants), investigators found no difference between the 2 groups, as both groups lost 0.7 letters of ETDRS visual acuity per year. In another trial (41 participants), when compared to placebo, DHA showed no effect on change from baseline visual acuity (mean difference −0.01 logMAR units, 95% CI −0.14 to 0.12), representing less than 1 letter difference between the 2 groups. Data from investigators of the third study (60 participants) found that annual change in mean number of letters correct was −0.8 in DHA group and 1.4 letters in placebo group, with no between‐group difference observed. The fourth trial (572 participants) compared (vitamin A + vitamin E trace) to (vitamin A trace + vitamin E trace) and found that decline in ETDRS visual acuity was 1.1 letters per year in the (vitamin A + vitamin E trace) group and 0.9 letters per year in the control group (vitamin A trace + vitamin E trace), with no evidence of a difference between groups. |
881 (4 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | ||
| Electroretinography (ERG)
assessed with: log mean change in ERG amplitude (rod response, mixed response, and cone response) follow‐up: 4 years |
All 4 trials examined the treatment effect associated with DHA on ERG amplitudes, and 1 trial examined the effect of vitamin A on ERG. 1 study reported that the vitamin A group had, on average, a slower rate of decline of retinal function than the group not receiving this dosage. In a post hoc analysis in another trial, investigators observed an 8.3% decline in ERG per year in the vitamin A group versus 10% decline per year in non‐vitamin A group; P < 0.001, although the clinical relevance of this difference was minimal. When the analysis included all randomized participants in this trial, the decline in ERG was 6.1% per year in vitamin A group versus 7.1% per year in non‐vitamin A group; P = 0.01. | 881 (4 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | ||
| Optical coherence tomography (OCT) assessed with: Change from baseline in tomographic features follow‐up: mean 2 years | No evidence of a difference was seen in ellipsoid zone constriction (P = 0.87) over 2 years. | 51 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | ||
| Adverse effects: as reported by studies | 1 trial reported that 27/60 participants experienced 42 treatment‐related emergent adverse events (22 in DHA group, 20 in placebo group), while the remaining studies reported no adverse events. | 944 (4 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; DHA: docosahexaenoic acid; ETDRS: Early Treatment Diabetic Retinopathy Study; RCT: randomized controlled trial | |||||
| GRADE Working Group grades of evidence High certainty: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: We are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: Our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: We have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | |||||
1Downgraded one level for risk of bias, due to potential attrition and reporting bias. 2Downgraded one level for inconsistency, due to clinical heterogeneity. 3Downgraded one level for imprecision, based on small number of studies.
Background
Description of the condition
The term 'retinitis pigmentosa' (RP) comprises a diverse group of diseases characterized by progressive degeneration of the retinal photoreceptors (light‐sensing cells) and the adjacent retinal pigment epithelium. RP may occur as part of a syndrome, including abnormalities of other organs, or in a non‐syndromic form in which the clinical manifestations are restricted to the eye (65% of all cases in the USA) (Daiger 2007). RP is often associated with other ocular abnormalities in addition to retinal degeneration, such as cataract (clouding of the lens of the eye) or cystoid macular edema (swelling of the central retina). The worldwide prevalence of RP is approximately 1 in 4000, with 100,000 people affected in the USA (Hartong 2006).
RP is a genetic condition, and its inheritance pattern may be autosomal dominant (30%), autosomal recessive (20%), X‐linked (15%), mitochondrial (5%), or sporadic (30%). At least 50 separate gene defects have been reported to be associated with RP (Daiger 2007).
Depending on the specific genetic variant, symptoms may manifest during childhood or adulthood. The initial symptoms are typically poor night vision (nyctalopia) and constriction of peripheral vision (visual field loss). This field loss is progressive, and usually central vision is not reduced until late in the disease course.
The natural course of RP involves an approximate 4% to 12% annual loss of visual field (Berson 1985). In addition to the visual field loss, deterioration of visual acuity and full‐field electroretinogram (ERG) changes are observed. Visual acuity loss occurs more gradually compared to visual field loss and is more severe if the central retina (macula) is affected (Flynn 2001; Holopigian 1996). On average, a decline in visual acuity of one line is observed over five years for individuals without macular lesions, compared to a loss of three to four lines in those with macular involvement (Flynn 2001).
The diagnosis of RP is made on clinical examination. Typical findings include abnormal pigmented changes in the peripheral retina (known as bone spicules, because of their similarity to the microscopic appearance of bone), pallor (paleness) of the optic disc (or optic nerve head, part of the optic nerve), and attenuation (narrowing) of the retinal blood vessels. Cataract and cystoid macular edema may also be noted.
Peripheral vision is measured with visual field testing, frequently with a static Humphrey perimeter (automated threshold perimeter) or kinetic Goldmann perimeter. Full‐field ERG provides additional quantitative measurement of disease progression. RP patients have reduced rod (elicited by dark‐adapted flash) and cone (elicited by single flash) response amplitudes and a delay in timing from stimulus to peak rod‐ or cone‐isolated responses (Berson 1969). It has been estimated that people with RP lose approximately 17% of remaining ERG amplitude per year (Berson 1985). Changes in the ERG are generally observed before clinical detection of changes in visual field and visual acuity.
Studies have documented microscopic changes in the retinal layers using a newer, non‐invasive clinical test known as optical coherence tomography (OCT) (Walia 2007; Witkin 2006). Witkin 2006 reported that the foveal photoreceptor outer segment/pigment epithelial thickness was significantly lower in eyes with RP than in controls. Oishi 2009 correlated findings from OCT with changes in visual acuity: patients without integrity of the inner segment‐outer segment junction of the photoreceptors had greater loss of visual acuity than patients with a more normal tomographic appearance.
Description of the intervention
Certain ophthalmic conditions associated with RP can be treated successfully. For example, cataract surgery may be performed for RP‐associated cataract, and various medications may be effective in the treatment of RP‐associated cystoid macular edema. However, there is no proven treatment that slows or delays the progressive retinal degeneration.
Treatments that have been studied include oral supplementation with vitamin A (retinyl palmitate), the omega‐3 long‐chain polyunsaturated fatty acid docosahexaenoic acid (DHA), or both (Birch 2005; Hodge 2005).
How the intervention might work
Mechanisms through which vitamin A and DHA might modify the disease process in RP have not yet been fully explained. However, vitamin A has been reported to have an important role in the function of retinal photoreceptors (Berson 1982; Dowling 1960). Rhodopsin is a pigment located in retinal rods that allows the rods to detect small amounts of light. Rhodopsin, along with other pigments in the retina, stores vitamin A compounds; vitamin A is important for rhodopsin formation and the visual cycle.
Similarly, DHA is found within photoreceptor cell membranes, and some authors have suggested that it has a functional role (Chen 1996).
Why it is important to do this review
RP is an uncommon but clinically important disease. It is progressive, potentially blinding, and has no proven treatment. Vitamin A and fish oils have been proposed as having some therapeutic potential in some of the clinical trials conducted. The most recent version of this review was published seven years ago (Rayapudi 2013), thus an update was needed to evaluate both earlier and more recent evidence on the relative safety and effectiveness of vitamin A and fish oils (DHA) in preventing the progression of RP.
Objectives
The objective of this review was to synthesize the best available evidence regarding the effectiveness and safety of vitamin A and fish oils (docosahexaenoic acid (DHA)) in preventing the progression of RP.
Methods
Criteria for considering studies for this review
Types of studies
We included randomized controlled trials (RCTs) of any design, including parallel and factorial. We did not include cross‐over trials or cluster‐randomized trials, as these designs could not address our question of interest.
We excluded studies that used quasi‐random allocation methods such as alternation, case‐record numbers, dates of birth, or days of the week for randomizing participants to a group. Although trials with quasi‐random allocation methods may provide data that support findings from RCTs, they are susceptible to selection bias and confounding.
Types of participants
We included trials that enrolled participants of any age diagnosed with any degree of severity or type of RP. If trials included participants with varying severity or stage of disease, we extracted baseline characteristics to explore disease severity as a source of variability across trials (see Subgroup analysis and investigation of heterogeneity).
Types of interventions
We included trials evaluating the effectiveness of vitamin A (administered as vitamin A1, retinyl palmitate, 11‐cis retinol, retinol, tretinoin, or all‐trans‐retinol), fish oils (administered as docosahexaenoic acid (DHA), omega‐3 fatty acids or eicosapentaenoic acid, fish‐liver oils and cod‐liver oil) or both, for any duration, as a treatment for RP.
We included trials when the following interventions and comparisons were used in studies.
1. For which participants received the following interventions:
only fish oils or only vitamin A;
fish oils along with any (one or more than one) type of other vitamin(s);
vitamin A along with any (one or more than one) type of vitamin(s).
We included trials in which participants receiving the above‐mentioned interventions were compared to participants receiving placebo, vitamins (other than vitamin A), or no therapy.
2. For which participants received the following interventions:
both fish oils and vitamin A;
both vitamin A and fish oils in combination with other vitamins.
We included trials in which participants receiving the above‐mentioned interventions were compared to participants receiving placebo, vitamins (including vitamin A), or no therapy.
Types of outcome measures
Primary outcomes
Mean change in visual field sensitivity (measured in decibels (dB)) at one‐year follow‐up. We also prespecified that we would analyze this outcome at other follow‐up times using available data (i.e. two, three, four, and five years). We planned that if the investigators could not provide mean change values, we would report the proportion of participants with visual field loss for these trials.
Visual field can be measured using different instruments, such as the Humphrey Field Analyzer and Goldmann perimeter. We described the methods used to measure visual field (by instrument, manual versus automated, threshold versus kinetic perimetry) and programs used to analyze automated threshold perimetry (e.g. 30‐2, 30/60‐1) in the Characteristics of included studies table.
Secondary outcomes
Visual acuity: in the protocol for this systematic review, we specified the change in logMAR visual acuity at five‐year follow‐up. We examined data at other follow‐up times (one, two, three, and four years' follow‐up) as well, as these were reported in the included trials.
Electroretinography (ERG): we analyzed the log mean change in ERG amplitude (rod response, mixed response, and cone response) at one year. We also examined this outcome at other follow‐up times (two, three, four, and five years). When ERG findings were reported in other ways, we summarized the available data.
Optical coherence tomography (OCT): analysis of this variable included the change from baseline in tomographic features, especially the junction between the photoreceptor outer segments and inner segments, at one year and at other times of follow‐up as available.
Adverse effects (severe, minor)
We summarized any adverse outcomes reported in the included trials. Specific adverse events of interest were systemic complications such as liver injury, elevated blood lipid levels, increased intracranial pressure, bone changes, teratogenicity (association with birth defects), and ocular complications such as loss of six or more lines of visual acuity at one‐year follow‐up.
Quality of life measures
We planned to report any quality of life measures associated with patient satisfaction, subjective visual improvement, and any other vision‐related quality of life measures assessed by questionnaires or other methods that were reported in the trials.
Follow‐up
We included trials with follow‐up of one year or longer in the review. Where possible, we planned to conduct meta‐analysis for trials with similar lengths of follow‐up.
Search methods for identification of studies
Electronic searches
The Cochrane Eyes and Vision Information Specialist searched the following electronic databases for RCTs and controlled clinical trials. There were no language or publication year restrictions. We last searched the electronic databases on 7 February 2020.
Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 2) (which contains the Cochrane Eyes and Vision Trials Register) in the Cochrane Library (searched 7 February 2020) (Appendix 1).
MEDLINE Ovid (1946 to 7 February 2020) (Appendix 2).
Embase.com (1947 to 7 February 2020) (Appendix 3).
PubMed (1948 to 7 February 2020) (Appendix 4).
Latin American and Caribbean Health Sciences Literature database (LILACS) (1982 to 7 February 2020) (Appendix 5).
metaRegister of Controlled Trials (mRCT) (www.isrctn.com/; last searched 20 August 2013) (Appendix 6).
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov/; searched 7 February 2020) (Appendix 7).
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/en/; searched 7 February 2020) (Appendix 8).
OpenGrey (www.opengrey.eu/; searched 7 February 2020) (Appendix 9).
Searching other resources
We handsearched the reference lists of the publications from studies eligible for inclusion in the review for information about other possible trials. We used the Web of Science database to identify additional studies that cited the included trials. We also searched abstracts from the annual meetings of the Association for Research in Vision and Ophthalmology (ARVO) and the American Academy of Ophthalmology (AAO) electronically.
We did not contact individuals or organizations to identify trials for this review.
Data collection and analysis
Selection of studies
Two review authors, working independently, assessed the titles and abstracts identified by the searches. Each review author classified the citations as 'definitely include,' 'possibly include (unsure),' and 'definitely exclude.' We obtained the full‐text publications of listings classified as definitely include and possibly include (unsure) to determine whether they were from studies that met the inclusion criteria, and then reclassified them as 'include,' 'exclude,' or 'awaiting classification.' We scanned the reference lists of the included studies manually to identify additional relevant citations. For studies categorized as 'awaiting classification' by both review authors, we requested additional information from the study investigators for clarification.
Review authors were not masked to any trial details in this process. Disagreements were resolved through discussion. We tabulated excluded trials along with reasons for exclusion.
Data extraction and management
Two review authors, working independently, extracted data from the publications of all included studies using data extraction forms developed by Cochrane Eyes and Vision and pilot‐tested specifically for this review. Any discrepancies were resolved through discussion.
We extracted the following information from each study.
Methods: method of randomization, allocation concealment, masking (blinding), number randomized to each trial arm, exclusions after randomization, losses to follow‐up, and unusual study design features.
Participants: country where participants were enrolled, age, sex, and inclusion/exclusion criteria.
Interventions: details of test intervention and comparison intervention (control) including dose and frequency of administration and duration of intervention.
Outcomes: visual field (primary outcome), visual acuity (secondary outcome), ERG measurements (secondary outcome), adverse events, any other outcomes assessed, and percentage of participants for whom no outcome data were reported.
Follow‐up and analysis: length of follow‐up, reasons stated for dropouts or withdrawal, compliance, and methods for analysis.
Others: additional details (such as funding sources) and publication year.
When any of the above data were missing from publications of a trial, we attempted to contact the study investigators for further information. If we did not receive a response within two months (after three emailed messages and one telephone contact), we proceeded without the missing information.
One author (SAA) entered data into the Review Manager 5 software (Review Manager 2014), and the second review author (SGS) verified the data entered against data extracted from the publications.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias of the included studies according to the following criteria as described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017). We graded each of the six 'Risk of bias' domains as low, high, or unclear (indicating either uncertainty or a lack of information). We provided a description for each judgement of bias.
Adequate sequence generation (selection bias): we categorized a study as being at low risk if the sequence was generated using a computer program or a random‐numbers table. We categorized all other methods as high risk or unclear risk.
Allocation concealment (selection bias): we categorized a study as being at low risk if the participants or the investigators enrolling the participants could not determine the assignments (e.g. use of central allocation, sequentially numbered, opaque, sealed envelopes). We categorized all other methods as being at high risk or unclear risk.
Masking of participants: we assessed whether the methods used to mask participants were adequate. When adequate methods to mask knowledge of the assigned intervention were used and described, such as similar‐looking pills administered at similar times of the day, we categorized the study as being at low risk of bias. We categorized all other methods as being at high risk or unclear risk.
Masking of care providers: we assessed whether the methods used to mask physicians and other care providers were adequate. When adequate methods to mask knowledge of the assigned intervention were used and described in specific language indicating masking, we categorized a study as being at low risk of bias. We categorized all other methods as being at high risk or unclear risk.
Masking of outcome assessors: we assessed whether the methods used to mask outcome assessors with regard to the treatment arm were adequate. When adequate methods to mask knowledge of the assigned intervention were used and described, such as analyzing each assessment (such as visual field) without access to prior tests, we categorized a study as being at low risk of bias. We categorized all other methods as being at high risk or unclear risk.
Incomplete outcome data: we assessed included trials for exclusions after randomization and losses to follow‐up along with the reasons for missing outcome data to determine the risk of bias. We categorized a study as being at low risk of bias when there were no missing outcome data, or the reasons for missing outcome data were not related to the true outcome; the reasons for missing data were similar across groups; or the missing data had been imputed using appropriate methods. We categorized all other reasons for missing outcome data as being at high risk or unclear risk.
Measures of treatment effect
We planned to use risk ratios (RR) (i.e. RR and 95% confidence intervals (CI)) as the measure of effect for dichotomous outcomes (proportion of participants with new visual field defects, visual acuity data reported as dichotomous outcomes, and proportion of participants with adverse events). We calculated a mean difference (MD) for continuous outcomes (mean change in visual field, logMAR visual acuity, and mean change in ERG amplitude).
We decided a priori that wherever visual acuity data were reported as a dichotomous outcome, we would attempt to contact the investigators for mean change values. If no additional data were available, we would analyze visual acuity as a dichotomous outcome (such as proportion of participants losing two or more lines of visual acuity) using the data in the trial report.
We planned to summarize the electroretinogram either as a continuous outcome or a dichotomous outcome based on the available data. We analyzed the mean change in ERG amplitude as a continuous outcome. We planned to analyze the proportion of participants with non‐detectable ERG patterns in response to high‐frequency flickers (30 or 31 Hz) as a dichotomous outcome.
Unit of analysis issues
Since participants in the included trials were given systemic treatment, the unit of analysis was the individual. We planned that when data were available for both eyes of an individual, we would perform an analysis for the average of the two eyes for continuous outcomes. For vision‐related dichotomous outcomes (e.g. visual acuity), we would use the eye as the unit of analysis.
Dealing with missing data
We contacted the study investigators for further information on trials with publications that did not report outcomes on all randomized participants. We planned that if they did not respond after three emailed messages and telephone contacts, initiated within two months, we would assess the study on the basis of the available information. One author responded, but was unable to provide any additional data or information that was missing from the publication. We attempted to extract data on standard deviations for the change from baseline if a P value or a CI was reported, using the methods described in Section 16.1.3 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We did not attempt to impute the standard deviations using possible values of correlation coefficients. We conducted analyses by the intention‐to‐treat principle, with all participants analyzed in the group to which they had been randomized, to the extent permitted by the methods described here. If the data in the publication or the trial investigators were unable to provide data to permit an intention‐to‐treat analysis, we conducted analysis on the available number of participants in the publication.
Assessment of heterogeneity
We assessed clinical and methodological heterogeneity by examining the characteristics of the included studies and by visual examination of the forest plots; we used the I2 statistic and Chi2 test to assess statistical heterogeneity.
Assessment of reporting biases
Had there been a sufficient number of included trials, we would have used a funnel plot to identify evidence of publication bias. We did not have access to the trial protocols to assess selective outcome reporting.
Data synthesis
We prespecified in the protocol for this review that if we found substantial heterogeneity across studies, either because of clinical heterogeneity (variability in types of participants, interventions, follow‐up, etc.) or statistical heterogeneity (I2 values greater than 50%, statistically significant Chi2 test for heterogeneity), we would not attempt a meta‐analysis but would present an estimate of effect and associated 95% CI for each individual trial. We would conduct a fixed‐effect meta‐analysis if there was little variation between trials, if we had two or three trials and there was no clinical heterogeneity and minimal statistical heterogeneity (as indicated by I2 values); we would conduct a random‐effects meta‐analysis when there was no clinical heterogeneity but there was moderate statistical heterogeneity (I2 values of 30% to 50%).
Subgroup analysis and investigation of heterogeneity
Had we found substantial heterogeneity, we would have explored the reasons for this heterogeneity by examining details from the trials including types of participants (baseline characteristics including severity of the disease, genetic profile, and syndromic or non‐syndromic RP), interventions (frequency and dose), duration of follow‐up, methodological characteristics such as losses to follow‐up, reasons for losses to follow‐up, and outcome measurement methods. We provided a qualitative analysis and summary of the variability across included trials. If the included trials provided sufficient data, we would conduct a subgroup analysis based on whether participants had syndromic or non‐syndromic RP.
Sensitivity analysis
We planned to conduct sensitivity analyses to assess the impact of excluding studies with poor methodological quality (high risk of bias for all or a large majority of 'Risk of bias' domains) and industry‐funded studies, however we did not perform this due to the few number of included studies.
Summary of findings and assessment of the certainty of the evidence
We summarized the main findings for each comparison of interest, including strengths and limitations of evidence, for primary, secondary, and adverse outcomes, using the GRADE approach (GRADEpro 2014). We assessed the quality of evidence for each outcome as 'high,' 'moderate,' 'low,' or 'very low' according to the following criteria as described in Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2011a; Schünemann 2011b).
High risk of bias among included studies.
Indirectness of evidence.
Unexplained heterogeneity or inconsistency of results.
Imprecision of results (i.e. wide confidence intervals).
High probability of publication bias.
We presented a 'Summary of findings' table for each comparison of interest where data were available. The comparisons include either only fish oils or only vitamin A, or both; fish oils along with any (one or more than one) type of other vitamin(s); vitamin A along with any (one or more than one) type of vitamin(s); or both vitamin A and fish oils in combination with other vitamins compared with placebo, vitamins (other than vitamin A), or no therapy. We included the following outcomes at one year or other follow‐up times in the Table 1.
Mean change in visual field sensitivity
Visual acuity
Electroretinography (ERG)
Optical coherence tomography (OCT)
Adverse events.
Results
Description of studies
Results of the search
The search in the previous version of the review conducted in August 2013, excluded seven studies with reasons and included three trials (Rayapudi 2013). Through an updated electronic search on 20 November 2018, we retrieved a total of 2028 titles and abstracts. After removing duplicate records, we reviewed 1287 titles and abstracts for eligibility, excluding 1267 of these records. We screened 20 full‐text reports, excluded 14 with reasons, classified one as ongoing study and one new RCT (Hoffman 2014) added in this update. In a top‐up search conducted on 7 February 2020, we identified 1821 records, screening 239 records after removal of duplicates. We retrieved two full‐text reports and further excluded one report with reasons, classifying one record as an ongoing trial (Figure 1). Overall, we included four RCTs, excluded 22 studies (22 records), assessed two studies (two records) as ongoing trials. We did not identify any additional studies through searching the reference lists of the included studies or the Web of Science database.
1.
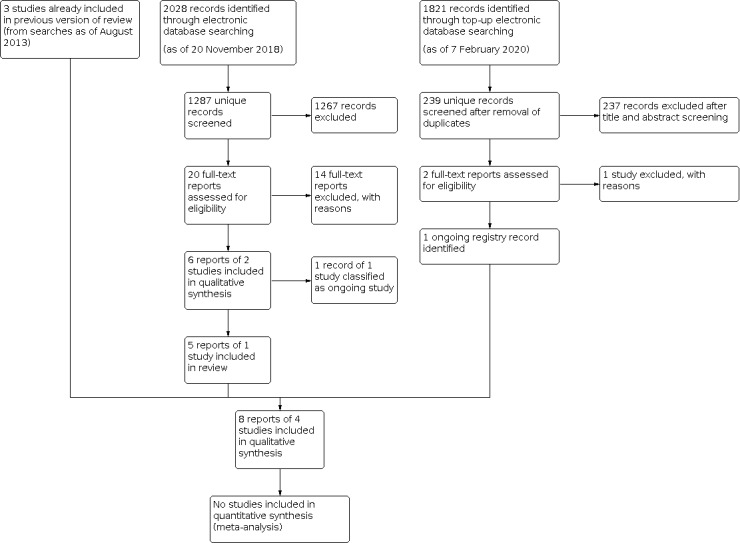
Results from searching for studies for inclusion in the review.
Included studies
Detailed characteristics of each included trial are presented in the Characteristics of included studies table and Table 2. Table 2 summarizes the study design, baseline characteristics of the participants, and interventions across the included trials.
1. Summary of included trials.
| Study ID | Berson 1993 | Berson 2004a | Hoffman 2004 | Hoffman 2014 |
| Design | 2x2 factorial design | Parallel | Parallel | Parallel |
| Genetic profile of participants | Autosomal dominant | Autosomal dominant | Not included | Not included |
| Autosomal recessive | Autosomal recessive | Not included | Not included | |
| X‐linked | X‐linked | X‐linked | X‐linked | |
| Dominant with mutation | Dominant with mutation | Not included | Not included | |
| Isolate | Isolate | Not included | Not included | |
| Undetermined | Undetermined | Not included | Not included | |
| Age range | 18 to 49 years | 18 to 55 years | 4 to 38 years | 7 to 32 years |
| Gender (% female) | Men and women (38%) | Men and women (49%) | Only males (0%) | Only males (0%) |
| Number randomized | 601 | 221 | 44 | 78 |
| Intervention(s) | Vitamin A + vitamin E
trace = 146 Vitamin A + vitamin E = 151 Vitamin A trace + vitamin E trace =149 Vitamin A trace + vitamin E = 155 |
DHA + vitamin A = 105 (number analyzed) DHA placebo + vitamin A = 103 (number analyzed) |
DHA = 23 DHA placebo = 21 |
DHA = 41 DHA placebo = 37 |
| Dose | Vitamin A = 15,000 IU/d Vitamin A trace = 75 IU/d Vitamin E = 400 IU/d Vitamin E trace = 3 IU/d |
DHA, 1200 mg/d Vitamin A, 1500 IU/d |
DHA, 400 mg/d | DHA, 600 to 3600 mg/d (30 mg/kg/d) |
| Primary outcome | Cone ERG amplitude | Visual field (total point score for 30‐2 HFA) | Cone ERG amplitude | Cone ERG amplitude |
| Other outcomes | Rod ERG, visual acuity, visual field | Cone ERG, visual acuity, visual field (total point score for 30‐2 and 30/60‐1 programs combined) | Rod ERG, visual acuity, visual field, dark adaptation | Rod and maximal ERG amplitudes, cone ERG implicit times, visual acuity, final dark‐adapted threshold, shape discrimination threshold, foveal VFS, macular VFS, peripheral VFS, total VFS, ellipsoid zone transitional sensitivity |
| Length of follow‐up | 4 to 6 years | 4 years | 4 years | 4 years |
DHA: docosahexaenoic acid ERG: electroretinogram HFA: Humphrey Field Analyzer IU: international units VFS: visual field sensitivity
Study design and setting
Two trials recruited participants from the USA (Berson 2004a; Hoffman 2004), and the other two (Berson 1993, Hoffman 2014) recruited participants from the USA and Canada. Three studies were RCTs with a parallel‐group design, and one employed a factorial design (Berson 1993). Participants were primarily recruited from eye registries and clinical centers supported by the Foundation Fighting Blindness (FFB). Hoffman 2004 recruited participants from the Southwest Eye Registry and from the clinical centers supported by FFB, and Hoffman 2014 recruited from the Southwest Eye Registry, the FFB database, and referrals from US and Canadian ophthalmologists. Berson 1993 and Berson 2004a recruited participants from the Baltimore Eye Registry, the centers supported by FFB, and the contacts of private ophthalmologists.
Types of participants
A total of 944 participants were enrolled, and 881 were analyzed. The trials varied in size from 44 participants (Hoffman 2004) to 601 participants (Berson 1993). The age of participants in the included trials ranged from 4 to 55 years. Hoffman 2004 and Hoffman 2014 included children and participants of a younger age range (4 to 38 years and 7 to 31 years, respectively) than the other two trials. Two trials included both male and female participants (Berson 1993; Berson 2004a), while the other two trials enrolled only male participants (Hoffman 2004; Hoffman 2014). In all four trials, RP was diagnosed in all participants by an ophthalmologist. None of trials reported RP according to specific subtypes or subdiagnosis and treatment response.
People with atypical forms of retinitis pigmentosa (such as unilateral RP, sector RP, paravenous RP) and most syndromic forms of RP (Bardet‐Biedl syndrome, Bassen‐Kornzweig syndrome, Refsum disease, Usher's syndrome type 1) were not included in any of the four trials. However, two trials included people with some syndromic forms of RP (including Usher's syndrome type 2 (RP associated with partial hearing loss)) (Berson 1993; Berson 2004a). Participants with all levels of genetic predisposition were included in these two trials (autosomal dominant, autosomal recessive, X‐linked, dominant with mutation, isolate and undetermined), while the other two trials included only participants with X‐linked RP (Hoffman 2004; Hoffman 2014).
Different instruments were used to measure visual field in the included trials, resulting in different measures of baseline values. Kinetic perimetry was used in Berson 1993, whereas static perimetry was used in the remaining three trials. Guidelines for converting results between kinetic and static perimeters have been reported by Anderson and colleagues (Anderson 1989). Participants enrolled in Berson 2004a had a baseline Humphrey Field Analyzer (HFA) 30‐2 program total point score ≥ 250 dB, using size V test light, whereas those enrolled in Berson 1993 had a central visual field diameter of ≥ 8 degrees (Goldman V‐4‐e). In Hoffman 2014, participants had an HFA 30‐2 program with spot size V, except participants with fields > 30 degrees, who used program 30/60‐2. A baseline visual field result was not specified in Hoffman 2004.
Visual acuity was measured using Early Treatment Diabetic Retinopathy Study (ETDRS) charts in all four trials. Participants enrolled in Berson 1993 and Berson 2004a were required to have a baseline minimum visual acuity of 20/100 (Snellen equivalent), but a baseline visual acuity minimum was not specified in the remaining trials.
Two trials included participants with greater than 0.68 µV of cone ERG (Berson 2004a; Hoffman 2004), and one trial included participants with greater than 0.64 µV of cone ERG (Hoffman 2014). The remaining trial included participants with cone ERG of at least 12 µV (Berson 1993). The percentages of participants with a measurable rod response at baseline were 61% (366/601), 55% (114/208), and 50% (22/44) in Berson 1993, Berson 2004a, and Hoffman 2004, respectively. In all studies but Hoffman 2014, response amplitude to cone ERG of less than 2 µV was narrowband amplified in order to reliably distinguish responses greater than 0.05 µV from noise.
We identified clinical heterogeneity among participants in the included trials regarding several aspects including age of the participants, genetic predisposition, gender, and baseline severity. Participants in Hoffman 2004 and Hoffman 2014 were younger than those in Berson 1993 and Berson 2004a; the mean ages were: 16 ± 9 years (Hoffman 2004); 14.9 ± 1.1 (placebo) and 16.1 ± 1.4 (DHA) years (Hoffman 2014); 32.5 ± 0.7 years (Berson 1993); and 37.8 ± 0.90 years (Berson 2004a). The baseline severity of RP varied among the trials as described above for baseline values of ERG, visual field, and visual acuity. We were unable to extract data for the outcomes specified in the protocol for this review based on the genetic profile of participants.
Types of interventions
The trials included in this review evaluated different interventions. Docosahexanoic acid (DHA) only was administered in two trials (Hoffman 2004; Hoffman 2014). Vitamin A (along with vitamin E for some participants) was administered in Berson 1993. Both DHA and vitamin A were administered in Berson 2004a. Doses also varied between trials. Hoffman 2004 administered 400 mg of DHA per day, whereas Berson 2004a administered 1200 mg of DHA per day. In Hoffman 2014, 30 mg/kg/d of DHA was administered, ranging from 600 mg to 3600 mg of DHA per day. Vitamin A was administered at a dose of 15,000 international units (IU) in both trials in which it was used (Berson 1993; Berson 2004a). Interventions (vitamin A and DHA) were administered orally in the form of gelatin capsules for a minimum period of four years. However, in Berson 1993, 43% of participants received the test or control intervention for six years.
Comparison intervention: DHA was compared to placebo in Hoffman 2004 and Hoffman 2014; DHA + vitamin A was compared to vitamin A alone in Berson 2004a; and vitamin A was compared to trace vitamins group (vitamin A trace + vitamin E trace) in Berson 1993.
Excellent compliance was documented in Berson 1993 (94% of capsules were consumed in any given year by 88% of participants) and Berson 2004a (92% of DHA capsules and 94% of vitamin A capsules were consumed over all four years). In Hoffman 2014, mean adherence to protocol was 89.4% in the DHA group and 84.6% in the placebo group by capsule count monitoring. Hoffman 2004 reported poor compliance in 5 of 44 participants (11.4%), using analysis of red blood cell levels of DHA.
Types of outcomes
Our primary outcome measure, visual field sensitivity, was analyzed as primary outcome in Berson 2004a, and as a secondary outcome measure in the three other trials (Berson 1993; Hoffman 2004; Hoffman 2014), in which annual change in full field cone ERG amplitude was the primary outcome measure. How each of the visual outcomes in the included trials was analyzed is shown in Table 3.
2. Summary of analysis of visual outcomes (visual field and visual acuity) in included trials.
| Outcome | Berson 1993 | Berson 2004a | Hoffman 2004 | Hoffman 2014 | |
| Visual field | Instrument used | Goldmann perimeter (V‐4‐e white test light) | HFA 30‐2 program | 640 HFA, program 30‐2 | 640 HFA, program 30‐2; program 30/60‐2 was used for participants with fields > 30 degrees |
| Effect measure | Per cent decline per year of remaining visual field area | Mean annual rate of loss of field sensitivity | Mean change in defect in Humphrey spot size III field from baseline at 4 years | Annual rate of change in foveal, macular, peripheral, and total visual field sensitivity for 4 years | |
| Method used for estimation | Longitudinal regression analysis | Longitudinal regression analysis | Mean change from baseline | Mean change from baseline | |
| Estimate | Vitamin A + vitamin E
trace = 5.6% Vitamin A + vitamin E = 6.2% Vitamin A trace + vitamin E trace = 5.9% Vitamin A trace + vitamin E = 6.3% |
DHA + vitamin A = 36.95 ± 3.36 dB/year Control + vitamin A = 37.68 ± 3.36 dB/year |
DHA = 2.4 ± 3.66 dB (0.24 logMAR) Placebo = 1.4 ± 1.32 dB (0.14 logMAR) | Mean change ± SE Foveal VFS: DHA = −0.02 ± 0.05 Placebo = −0.47 ± 0.03 Macular VFS: DHA = −0.42 ± 0.05 Placebo = −0.85 ± 0.03 Peripheral VFS: DHA = −0.39 ± 0.02 Placebo = −0.86 ± 0.02 Total VFS: DHA = −0.39 ± 0.02 Placebo = −0.86 ± 0.02 |
|
| Data interpretation | No significant vitamin A or vitamin E main effects or interaction effects were observed. |
No significant difference | No significant difference | Significantly reduced in favor of DHA group | |
| Visual acuity | Instrument used | ETDRS chart | ETDRS chart | ETDRS chart | Electronic ETDRS |
| Effect measure | Number of ETDRS letters lost per year |
Annual rate of decline of ETDRS visual acuity over 4 years | Mean group difference in logMAR visual acuity between years 0 and 4 for the average of both eyes | Annual rate of change in letters correct between years 0 and 4 for the average of both eyes | |
| Method used for estimation | Longitudinal regression analysis | Longitudinal regression analysis | Mean change from logMAR baseline visual acuity | Mean change from baseline | |
| Estimate | Vitamin A + vitamin E
trace = 1.1 letters/year Vitamin A + vitamin E = 0.7 letters/year Vitamin A trace + vitamin E trace = 0.9 letters/year Vitamin A trace + vitamin E = 0.9 letters/year |
DHA + vitamin A = 0.71 + 0.12
letters/year Control + vitamin A = 0.68 + 0.12 letters/year |
DHA = 0.05 ± 0.23 log
units (logMAR) Placebo = 0.06 ± 0.2 log units (logMAR) |
DHA = −0.8 ± 0.8 Placebo = 1.43 ± 1.1 P = 0.19 |
|
| Data interpretation | No significant difference | No significant difference | No significant difference | No significant difference |
DHA: docosahexaenoic acid ETDRS: Early Treatment Diabetic Retinopathy Study HFA: Humphrey Field Analyzer RCT: randomized controlled trial VFS: visual field sensitivity
Excluded studies
We excluded a total of 22 records; reasons for their exclusion are shown in the Characteristics of excluded studies table.
Ongoing studies and studies awaiting classification
We identified two ongoing studies (see Characteristics of ongoing studies). No trial was classified as awaiting classification.
Risk of bias in included studies
We evaluated the risk of bias for all of the included trials using the six prespecified domains described in the Assessment of risk of bias in included studies section. We categorized blinding of outcome assessors and incomplete outcome data reporting into three criteria for primary and secondary outcomes, and so recorded a total of 12 criteria in the Characteristics of included studies and Figure 2. We found Berson 1993, Hoffman 2004, and Berson 2004a to have a low overall risk of bias. Summary of 'Risk of bias' assessment is shown in Figure 2.
2.

Risk of bias summary: review authors' judgements about each risk of bias domain for each included study.
Allocation
In three trials the random sequence was generated adequately by using computer‐generated random numbers (Berson 1993; Berson 2004a; Hoffman 2014). Hoffman 2004 used a cluster‐RCT strategy, as relatives were randomized together to the same intervention to eliminate a potential for mixing of capsules. In the Methods, we stated that we intended to exclude cluster‐randomized trials, and although Hoffman 2004 mentioned that the relatives were randomized to same intervention using a cluster‐RCT strategy, the strategy was not clearly and adequately described, and it was not clear how many relatives were randomized or what percent of randomized individuals were randomized using a cluster‐RCT strategy. In addition, upon our assessment, we found that individuals were randomized to treatment groups. We therefore did not consider Hoffman 2004 to be a cluster‐randomized trial, and so decided to include it.
Allocation was implemented using a centralized system in Berson 1993 and Berson 2004a, which implies that personnel enrolling participants could not determine the next assignment. It was unclear whether there was adequate allocation concealment in the remaining two trials.
Blinding
All four included trials masked all personnel (participants, investigator, caregiver, outcome assessors) adequately. The outcome assessors were masked to both primary (visual field) and secondary (visual acuity and ERG) outcomes.
Incomplete outcome data
In Hoffman 2004, 44/44 participants completed three years of follow‐up, and 41/44 participants completed four years of follow‐up. Three people missed visits over the entire span of study. The trialists imputed data for missed visits using the 'last observation carried forward' method and performed intention‐to‐treat analysis. In Berson 2004a and Berson 1993, the trialists imputed missed measurements using multiple imputation methods. All trials accounted for incomplete outcome data adequately. In Hoffman 2014, 12/41 (29.3%) participants in the DHA group and 15/37 (40.5%) participants in the placebo group who were randomized were not included in the final analysis at four years of follow‐up. We assessed this study as at high risk of bias for incomplete outcome data.
Selective reporting
In one study (Hoffman 2014), the outcome loss of peripheral visual fields, which was listed in the ClinicalTrials.gov registration, was not described in the publication, therefore we assessed this study as at high risk of bias for selective outcome reporting. We did not have access to protocols or to other information that would have allowed us to assess selective reporting in the remaining three trials.
Other potential sources of bias
We did not assess the potential for publication bias using a funnel plot or other means, given that we identified only four trials that were eligible for inclusion.
Effects of interventions
See: Table 1
All of the included trials reported visual field, visual acuity, and ERG as either a primary outcome or secondary outcome. One trial performed OCT (Hoffman 2014).
We elected not to conduct a meta‐analysis because of clinical heterogeneity in the types of participants included and differences in the intervention and comparison groups studied (as described in earlier sections of this review) across the included trials. In addition, we were unable to extract data from the included trials on outcomes prespecified in the protocol for this review. Although the outcomes measured in all four trials included visual field, ERG amplitude, and visual acuity, they were analyzed and reported in ways that did not allow quantitative synthesis and comparison of data. We were thus unable to report a summary effect of interventions in terms of the outcomes prespecified in the protocol. We have presented a narrative summary of evidence reported in included studies below.
Table 3 and Table 4 illustrate the variability across the included trials in defining the outcome variable and its analysis for visual field, visual acuity, and ERG amplitude.
3. Summary of analysis of electroretinogram in included studies.
| Berson 1993 | Berson 2004a | Hoffman 2004 | Hoffman 2014 | |||||
|
Effect
measure and estimate |
Rate of decline of remaining 30 Hz ERG amplitude per year | Vitamin A + vitamin E trace = 6.1% Vitamin A + vitamin E = 6.3% Vitamin A trace + vitamin E trace = 7.1% Vitamin A trace + vitamin E = 7.9% |
Annual rate of decline of 30 Hz ERG amplitude, loge % decline | DHA + vitamin A = 0.10 ± 0.01 Control + vitamin A = 0.11 ± 0.01 |
The mean (±1 SD) change in log cone ERG amplitude by 4th year | DHA = −0.199 ± 0.172 log μV Placebo = −0.266 ± 0.173 log μV |
Annual rate of change in log cone ERG amplitude for 4 years | Mean ± SE DHA = −0.028 ± 0.001 log μV Placebo = −0.022 ± 0.002 log μV DHA = −0.94 ± 1.00 μV Placebo = −0.95 ± 1.00 μV |
| Percentage of participants with less than 50% decline in 30 Hz ERG amplitude relative to baseline at year 6 (high amplitude cohort) | Vitamin A + vitamin E trace = 62% Vitamin A + vitamin E = 50% Vitamin A trace + vitamin E trace = 48% Vitamin A trace + vitamin E = 27% |
Mean annual rate of decline of remaining 30 Hz ERG function | DHA + vitamin A = 9.92% Control + vitamin A = 10.49% |
Mean change from baseline after 4 years in log cone ERG amplitude (text) and for all years of follow‐up | "A repeated‐measures ANOVA showed a significant main effect of year(<.0001), with the population as a whole showing significant progression. The main effect of group was not significant (P=.16), and the interaction between group and year was not significant (P=.61)." | Annual rate of change in rod ERG amplitude for 4 years | Mean ± SE DHA = −0.010 ± 0.001 log μV Placebo = −0.023 ± 0.001 log μV DHA = −0.98 ± 1.00 μV Placebo = −0.95 ± 1.00 μV |
|
| Mean change from baseline for each year of follow‐up (for high‐amplitude cohort) | Data in figure only | ‐ | ‐ | ‐ | ‐ | Annual rate of change in maximal ERG amplitude for 4 years | Mean ± SE DHA = −0.042 ± 0.001 log μV Placebo = −0.036 ± 0.001 log μV DHA = −0.91 ± 1.00 μV Placebo = −0.92 ± 1.00 μV |
|
| Method used for estimation | Longitudinal regression analysis Survival analysis Mean change analysis |
Longitudinal regression analysis | Subtracting the mean baseline log amplitude from the mean follow‐up log amplitude | Repeated‐measures mixed‐model regression analysis | ||||
| Data interpretation | The vitamin A group had, on average, a slower rate of decline of retinal function than the 2 groups not receiving this dosage. | No significant difference | No significant difference | No significant difference | ||||
ANOVA: analysis of variance DHA: docosahexaenoic acid ERG: electroretinogram SD: standard deviation SE: standard error
Visual field (4 studies involving 881 participants)
Three trials examined the treatment effect associated with DHA (Berson 2004a; Hoffman 2004; Hoffman 2014), and one trial examined the effect of vitamin A on visual field (Berson 1993), although they reported different measurement parameters. All studies measured visual field either as a primary outcome, Berson 2004a, or secondary outcome (Berson 1993; Hoffman 2004; Hoffman 2014). One trial reported that the annual rate of visual field loss over four years was significantly smaller in the DHA group compared to the placebo group (Hoffman 2014), while the other three trials found no evidence of difference in rates of loss of visual field over four years between the treatment and control groups.
The primary outcome measure reported in Berson 2004a (208 participants) was the measurement of static perimetric sensitivities (total point score, i.e. overall assessment) on the HFA 30‐2 program with size V target. There was no evidence of difference in the mean annual rates of decline of visual field sensitivity between the intervention group (participants receiving DHA and vitamin A, 36.95 ± 3.36 dB per year) and the control group (participants receiving placebo and vitamin A, 37.68 ± 3.36 dB per year, P = 0.88). The investigators reported the combined total point score on the HFA 30‐2 and 30/60‐1 programs as a secondary outcome measure. Again, there were no evidence of a difference in the mean annual rates of decline between the intervention group (57.21 ± 4.90 dB per year) and the control group (59.59 ± 4.90 dB per year, P = 0.73). However, in a separate publication (Berson 2004b), the investigators reported a post hoc subgroup analysis (participants taking vitamin A prior to entry into the trial compared to those not taking vitamin A prior to entry into the trial). They concluded that among participants not taking vitamin A prior to entry into the trial, the mean annual rates of decline of central and total field sensitivity may be lower in the intervention group (30 participants; DHA + vitamin A) than in the control group (35 participants; placebo + vitamin A) in the first and second years of follow‐up, but not in the third and fourth years of follow‐up (data not shown).
Hoffman 2014 (60 participants) assessed visual field sensitivity by using HFA 30‐2 program with spot size V, and program 30/60‐2 for those who had field more than 30 degrees. The investigators reported that although there was no difference in mean values between the DHA and placebo groups, the annual rate of change over four years probably favors the DHA versus placebo group in foveal (−0.02 ± 0.05 (standard error (SE)) dB versus −0.47 ± 0.03 dB, P = 0.039), macular (−0.42 ± 0.05 dB versus −0.85 ± 0.03 dB, P = 0.031), peripheral (−0.39 ± 0.02 versus −0.86 ± 0.02 dB, P < 0.001), and total visual field sensitivity (−0.39 ± 0.02 versus −0.86 ± 0.02 dB, P < 0.001).
In contrast, Hoffman 2004 reported the focal assessment of change, presented in mean field defect (average of all differences from mean normal) using the HFA 30‐2 program with size III target and the 30/60‐2 program for participants with sufficient peripheral function. There was no evidence of a difference between the intervention (DHA, 2.4 ± 3.66 dB over four years) and control group (placebo, 1.4 ± 1.32 dB over four years); P = 0.29.
In Berson 1993 (572 participants), the percentage decline in the residual visual field (on kinetic Goldmann perimetry) was 5.6% in the intervention group (vitamin A + vitamin E trace) and 5.9% in the control group (vitamin A trace + vitamin E trace), with no difference between the two groups. We graded the certainty of evidence for this outcome in all four studies as very low, downgrading for risk of bias, inconsistency, and imprecision.
Visual acuity (4 studies involving 881 participants)
Visual acuity was assessed as a secondary outcome using the ETDRS charts in all trials included in this review. Three trials examined the effect of DHA on visual acuity (Berson 2004a; Hoffman 2004; Hoffman 2014), and one trial examined the effect of vitamin A on visual acuity (Berson 1993). All of the included studies showed no difference in rates of loss of visual acuity over four years between the intervention and comparison groups.
Berson 2004a (208 participants) reported the ETDRS visual acuity as number of letters per year. Both the (DHA and vitamin A) and (placebo and vitamin A) groups lost 0.7 letters of ETDRS visual acuity per year.
In Hoffman 2004 (41 participants), the mean change from baseline visual acuity after four years' follow‐up was 0.05 logMAR units (95% confidence interval (CI) −0.04 to 0.14) (i.e. 2.5 letters) among participants treated with DHA, and 0.06 logMAR units (95% CI −0.02 to 0.14) among participants treated with placebo, with no evidence of a difference between the two groups (mean difference −0.01 logMAR units, 95% CI −0.14 to 0.12) (i.e. less than one letter difference).
In Hoffman 2014 (60 participants), annual change in mean number of letters correct was −0.8 in the DHA group and 1.4 letters in the placebo group, with no evidence of a between‐group difference observed (P = 0.19).
In Berson 1993 (572 participants), decline in ETDRS visual acuity was 1.1 letters per year in the intervention group (vitamin A + vitamin E trace) and 0.9 letters per year in the control group (vitamin A trace + vitamin E trace), with no evidence of a difference between the groups.
We assessed the certainty of the evidence across all four studies as very low, downgrading for risk of bias, inconsistency, and imprecision.
Electroretinography (4 studies involving 881 participants)
Three trials examined the treatment effect associated with DHA on ERG amplitudes (Berson 2004a; Hoffman 2004; Hoffman 2014), and one trial examined the effect of vitamin A (Berson 1993). Both rod and cone ERG amplitudes were measured in all four trials. The results varied across the four trials.
In Berson 2004a (208 participants), the effect of vitamin A and DHA on cone ERG amplitude was reported in terms of mean rate of decline of remaining 30 Hz ERG amplitude per year of follow‐up. Over four years, analysis of 30 Hz cone ERGs showed that the mean annual rates of decline of remaining function were 9.92% in the group receiving DHA and vitamin A, and 10.49% in the group receiving only vitamin A, with no difference between the two groups (P = 0.64).
In Hoffman 2004 (41 participants), the average difference in change from baseline in cone ERG amplitude between DHA and placebo after four years' follow‐up was 0.07 log μV (95% CI −0.04 to 0.17). In calculating the sample size for Hoffman 2004, the trial was powered to detect an anticipated change of 0.085 log units per year in cone ERG amplitude. The observed decline in cone ERG amplitude in the control group was only 0.066 log units per year. This trial may thus have not been adequately powered to detect the prespecified treatment effect. In a subgroup analysis of Hoffman 2004, investigators reported that there may be an effect of DHA on rod ERG amplitude (P = 0.04), but not on cone ERG amplitude in children under 12 years of age (P = 0.86). Conversely, the investigators found that there may also be an effect of DHA on cone ERG amplitude (P = 0.04) but not on rod ERG amplitude among children 12 years or older.
In Hoffman 2014 (60 participants), 31 Hz cone ERG amplitude, rod and maximal ERG amplitude, and cone ERG implicit time were assessed annually up to four years. There was no evidence of a difference with respect to yearly rates of change between the DHA and placebo group in 31 Hz cone ERG amplitude (mean ± SE) (−0.028 ± 0.001 log μV versus −0.022 ± 0.002 log μV; P = 0.30), rod ERG amplitude (mean ± SE) (−0.010 ± 0.001 log μV versus −0.023 ± 0.001 log μV; P = 0.27), maximal ERG amplitude (mean ± SE) (−0.042 ± 0.001 log μV versus −0.036 ± 0.001 log μV; P = 0.65), and cone ERG implicit time (mean ± SE) (no change over four years (data not reported) versus 0.12 ± 0.02; P = 0.77) over four years of follow‐up. We judged the certainty of the evidence for this outcome across all four studies as very low, downgrading for risk of bias, inconsistency, and imprecision.
Berson 1993 (572 participants) reported an effect of vitamin A on the mean change in log ERG amplitude from baseline (P = 0.01). A previous cohort study had estimated a decline of 17% of remaining cone ERG amplitude per year among patients with RP (Berson 1985), and the Berson 1993 trial was designed using this assumption for sample size calculation. The 1985 trial report described that participants with measurable cone ERG amplitude (≥ 0.68 μV) at baseline showed a decline of 10% per year (in the trace group), whereas participants in the trace group with < 0.68 μV cone ERG amplitude did not show any measurable rate of decline in cone ERG amplitude. The Berson 1993 authors inferred from these observations that the effects of the intervention might be detected only in participants who had minimum cone ERG amplitude of 0.68 μV at baseline. Accordingly, Berson 1993 reported a post hoc subgroup analysis that included only participants who had high cone ERG amplitude at baseline. The findings from this subgroup analysis indicated that daily supplementation with 15,000 IU vitamin A may reduce the annual rate of loss of remaining cone ERG amplitude compared to people not receiving this dose of vitamin A (8.3% decline per year in the vitamin A group versus 10% decline per year in the non‐vitamin A group; P < 0.001), although the clinical relevance of this difference is questionable (Berson 1993). A probable effect was also observed for this outcome when the analysis included all randomized participants in this trial (6.1% decline per year in the vitamin A group versus 7.1% decline per year in the non‐vitamin A group; P = 0.01). These findings from subgroup analyses have not been replicated or substantiated by findings in any of the remaining trials. We rated the certainty of the evidence for this outcome across all four trials as very low, downgrading for risk of bias, inconsistency, and imprecision.
Optical coherence tomography (1 study involving 51 participants)
Optical coherence tomography data were available over two years in Hoffman 2014 (51 participants). No evidence of a difference was seen in ellipsoid zone constriction (P = 0.87) over two years. We assessed the certainty of the evidence as very low, downgrading for risk of bias, inconsistency, and imprecision.
Adverse effects (4 studies involving 944 participants)
Hoffman 2014 (60 participants) reported that 27 participants (34.6%) experienced 42 treatment‐related or possibly related treatment‐emergent adverse events (22 in the DHA group, 20 in the placebo group) during four years of treatment. No severe treatment‐emergent adverse events were observed in this study. No toxicity or adverse events were reported in the other three trials. We rated the certainty of the evidence across all four studies as very low, downgrading for risk of bias, inconsistency, and imprecision.
Discussion
Summary of main results
We did not find clear evidence for the benefit of treatment with vitamin A or DHA, or both, for people with RP for the outcomes prespecified in our protocol, with the exception of one subgroup in Berson 1993, in which participants with high cone amplitude at baseline appeared to have had a reduced rate of loss of remaining cone function compared to non‐supplemented controls. The findings from this subgroup analysis have not been replicated in other RCTs. Where data were available for the mean change in visual field, visual acuity, and cone ERG amplitude after four years of follow‐up in adult participants with X‐linked RP (Hoffman 2004), there was no statistically significant benefit. Berson 1993 described a statistically significant protective effect of vitamin A on the annual mean change in cone ERG amplitude.
Despite testing visual fields with two different visual field instruments, different automated strategies and outcome measures, there was no demonstrable effect of therapy on visual field outcome. Berson 1993 initially performed kinetic Goldmann visual fields with V‐4‐e white test light on a 601 participants aged 18 to 49 years. Comparing treatment groups and controls, there was no treatment effect on visual field area; however, the authors noted a positive trend correlating visual field area and change in 30 Hz ERG amplitude, suggesting that participants receiving vitamin A had a slower rate of decline in visual field area over the four years of treatment.
In a follow‐up study in 2004 (Berson 2004a), the investigators studied central and peripheral visual field changes using the Humphrey Field Analyzer (HFA). They assessed central field with the HFA 30‐2 program and total field with the combined HFA 30‐2 and 30/60‐1 programs over three to four years. A size V target was used centrally and peripherally using the FASTPAC test. There was significant visual field loss over all the points measured in the treatment and the control groups: centrally (37 to 38 dB per year to the HFA 30‐2 program condition) combined with overall visual field loss (57 to 60 dB to the HFA 30‐2/30/60‐1 programs combined). The trialists reported: “these total point score declines summarize about 0.5 dB and 0.4 dB per year, respectively, for an average location in the visual field.”
Hoffman 2004 studied visual fields in 21 participants in the treatment group and 23 controls using the HFA. A 30‐2 static program with spot size III was used to assess 74 locations within the central 30 degrees. Participants who had retained peripheral function were also tested at 72 locations with the 30/60‐2 program. As the trialists reported, “The visual field parameter selected for evaluation was the mean field defect (average of all differences from mean normal; dB),” and the mean defect changed by 1.4 ± 1.32 dB in the placebo (control) group compared with 2.4 ± 3.66 dB in the treatment group. The authors expressed concern about the young age of participants doing visual field testing at the beginning of the study.
Hoffman 2014, the most recent study, included 78 participants aged 7 to 31 years (41 in the DHA group and 37 in the placebo group). Visual field sensitivity was assessed by using HFA program 30‐2 with spot size V, and program 30/60‐2 for those who had field more than 30 degrees. Trialists reported that although mean values were not significantly different between the DHA and placebo groups, annual rate of change over four years showed a statistically significant difference in favor of the DHA group in foveal (DHA −0.02 ± 0.55 (SE) dB, placebo −0.47 ± 0.03 dB, P = 0.039), macular (DHA −0.42 ± 0.05 dB, placebo −0.85 ± 0.03 dB, P = 0.031), peripheral (DHA −0.39 ± 0.02, placebo −0.86 ± 0.02 dB, P < 0.001), and total visual field sensitivity (DHA −0.39 ± 0.02, placebo −0.86 ± 0.02 dB, P < 0.001). The authors also reported that 27 participants (34.6%) experienced 42 (22 in DHA group, 20 in placebo group) treatment‐related or possibly related treatment‐emergent adverse events during four years of treatment.
Overall completeness and applicability of evidence
Small, non‐randomized pilot studies (e.g. Tcherkes 1950 and Dagnelie 2000) have reported evidence of effectiveness of vitamins in the treatment of RP, but the four well‐designed, well‐executed RCTs included in this review did not, either individually or collectively. However, one of the four studies found that annual rate of change over four years showed a statistically significant difference in favor of the DHA group in foveal and total visual field sensitivity. The available data do not indicate a significant beneficial effect of DHA or vitamin A on progression of loss of visual acuity and visual field. Furthermore, there was no evidence that the effects of vitamin A or combination of vitamin A and DHA differed according to the genetic profile of the participants, as assessed in Berson 1993 and Berson 2004a.
The trials included in this review enrolled participants with common forms of RP. None of the trials included participants with atypical forms of RP (e.g. paravenous retinitis pigmentosa, clumped pigmentary retinal degeneration, sector retinitis pigmentosa, or unilateral retinitis pigmentosa); most syndromic forms of RP (Refsum disease, Bardet‐Biedl syndrome, Usher's syndrome type 1 (i.e. retinitis pigmentosa with profound congenital deafness)); or RP associated with hereditary abetalipoproteinemia (i.e. Bassen‐Kornzweig syndrome). In addition, none of the included trials involved pregnant women, people with weight and height under the 5th percentile for a given age and sex, those with liver malfunction, those over 55 years of age, and people with a more advanced stage of the disease (visual acuity < 20/100, central visual field diameter < 8 degrees, or people with 30 Hz cone ERG amplitude of < 0.5 μV in response to 0.5 Hz white light or < 0.12 μV in response to 30 Hz white flickering light).
Quality of the evidence
We determined that three included trials had a low risk of bias for the domains assessed (Berson 1993; Berson 2004a; Hoffman 2004). We assessed Hoffman 2014 as at high risk of bias for incomplete outcome data and selective outcome reporting due to substantial losses to follow‐up and because one outcome, loss of peripheral visual fields, was listed in the ClinicalTrials.gov registration but not reported in the publication.
The results described in the trials are valid. However, we were unable to extract sufficient data on the outcomes specified in our protocol from the results described in the trial reports. The included trials appear to have been well designed and conducted. However, the conclusions drawn from the data that supplemental vitamin A or vitamin A along with DHA slows the progression of RP were based on the findings through ERG measurements rather than visual field or visual acuity.
Potential biases in the review process
The descriptions of potential biases in the review process pertain to the current status of availability of data. We will revise our findings based on response from trial authors regarding data on outcomes. We were unable to extract data from the text, tables, or figures for the outcomes specified in the protocol for this review. In one case, the mean cone ERG amplitude was available for both treatment groups from a figure, but we could not extract the standard error for the difference in mean change from baseline between the groups. Communicating with authors should not introduce selection bias into the review (Borly 2001), and may result in the availability of more data for assessment, since we are working with a small number of included trials and are unlikely to be able to conduct a meta‐analysis.
Because only four trials met inclusion criteria for this review, heterogeneity of the compared interventions was allowed. Specifically, the comparisons were as follows: vitamin A, vitamin E, vitamin A plus vitamin E, and trace amounts of both vitamins (Berson 1993); vitamin A plus DHA versus vitamin A plus control capsules (Berson 2004a); DHA versus placebo capsules (Hoffman 2004); and DHA plus a multivitamin versus a placebo plus a multivitamin (Hoffman 2014). Consequently, two trials compared DHA with placebo (Hoffman 2004; Hoffman 2014); one trial compared vitamin A plus DHA with vitamin A alone (Berson 2004a); and one trial compared vitamin A with vitamin E (Berson 1993). We judged this heterogeneity to be an acceptable trade‐off to permit the inclusion of as many relevant trials as possible. In addition, results were not combined in the analyses.
Agreements and disagreements with other studies or reviews
This review is generally in agreement with other published reviews and comments. For example, Dr Edward Norton, a member of the Data Safety and Monitoring Committee for Berson 1993, published his opinion that the data did not demonstrate a significant beneficial effect for vitamin A (Norton 1993). Similarly, Massof 2010 reviewed three RCTs, including Berson 1993 and Berson 2004a, and concluded that the results did not prove that these interventions slowed the rate of progression of RP.
Authors' conclusions
Implications for practice.
Based on the results of four randomized controlled trials, there is no clear evidence for the benefit of treatment with vitamin A or docosahexaenoic acid (extracted from fish oil), or both, for individuals with retinitis pigmentosa (RP), in terms of mean change in visual field and electroretinogram amplitudes after one year, and mean change in visual acuity at five years' follow‐up. Consequently, there is inadequate data at present to recommend the use of these two interventions for individuals with RP. Although the exclusion criteria across the included trials were extensive, thus limiting the applicability of evidence to many individuals with RP, it is unlikely that future trials would include patients that meet these criteria. The findings from the trials included in this systematic review should therefore be carefully considered in the management of patients that meet these exclusion criteria.
Systemic side effects or toxicity for long‐term supplementation of high‐dose vitamin A is unknown.
Implications for research.
The design and reporting of future trials on individuals with RP should consider outcomes relevant to various stakeholders (e.g. patients, physicians, and family members) as well as those specified in this systematic review. Some of the included trials included unplanned subgroup analysis that suggested differential effects based on previous vitamin A exposure, so investigators should consider examining this issue in future randomized controlled trials. Future trials on the effects of vitamin A and fish oils for RP should take into account the changes observed in electroretinogram amplitudes and other outcome measures from trials included in this review, in addition to previous cohort studies, when calculating sample sizes in order to ensure adequate power to detect clinically and statistically meaningful difference between treatment arms.
What's new
| Date | Event | Description |
|---|---|---|
| 7 January 2022 | Review declared as stable | This review is no longer being updated as the intervention is no longer used. |
History
Protocol first published: Issue 3, 2010 Review first published: Issue 12, 2013
| Date | Event | Description |
|---|---|---|
| 15 June 2020 | New search has been performed | Issue 6 2020: An updated search yielded results from one new study. The overall finding that whether giving vitamin A or fish oil, or both to people with retinitis pigmentosa delays the continued worsening of vision remains uncertain. |
| 15 June 2020 | New citation required but conclusions have not changed | Issue 6 2020: One new study (Hoffman 2014) and two new ongoing studies (CTRI/2016/01/006497NCT00004827) added. |
Acknowledgements
We thank Iris Gordon, the Information Specialist for the Cochrane Eyes and Vision (CEV), for her help in developing and conducting the electronic searches. We thank Ann‐Margret Ervin, PhD, for her critical comments on earlier versions of this protocol. We acknowledge the assistance provided by Kay Dickersin, MA, PhD, at the Cochrane Eyes and Vision US Project, funded by Grant 1 U01 EY020522‐01, National Eye Institute, National Institutes of Health, USA, in developing the protocol for this review.
This review update was managed by CEV@US and was signed off for publication by Tianjing Li and Richard Wormald.
Appendices
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor: [Retinitis Pigmentosa] explode all trees #2 (retini* or retina* or retinopath*) near pigment* #3 ((tapetoretina* or tapeto retina*) near (degener* or dystroph*)) #4 rod near cone near dystroph* #5 MeSH descriptor: [Tangier Disease] explode all trees #6 tangier near disease* #7 {or #1‐#6} #8 MeSH descriptor: [Vitamin A] explode all trees #9 "vitamin a" or "aquasol a" or "vitamin a1" or "a vitamin" or "vit a" or "A 313" or "all‐trans‐retinyl alcohol" or "Anti‐Infective Vitamin" or "Antixerophthalmic Vitamin" or "Arovit" or "Avibon" or "Avitol" or "Axerol" or "Axerophthol" or "Axerophtholum" or "Biosterol" or "Biovit‐A" or "Chocola A" or "Del‐VI‐A" or "Ido A 50" or "Idrurto A" or "Lard Factor" or "Ledovit A" or "Micelle A" or "Mulsal A Megadosis" or "Oleovitamin A" or "Ophthalamin" or "Palmitate‐1‐14C" or "Rinocusi Vitaminico" or "viatmin a" or "Vitaminoftalmina" or "Vitaminum A" or "Viva‐Drops" or "Vogan" #10 MeSH descriptor: [Retinoids] explode all trees #11 retino* or retinyl palmitate* #12 MeSH descriptor: [beta Carotene] explode all trees #13 beta carotene* or betacarotene* or Carotaben or "Max Caro" or MaxCaro or Solatene or Vetoron or BellaCarotin or Provatene or "b‐tene" or "beta carotin" or betatene or lurotin or solvin or "b Carotene" or "B‐Caro‐T" or BETACRTN or Caroguard or Lumitene or "Provitamin A" #14 MeSH descriptor: [Fish Oils] explode all trees #15 (oil* near (fish* or "cod liver" or halibut or squid or krill or mackerel or menhaden or salmon or seal or "shark liver" or seafood)) #16 EPA or EFA or MaxEPA or ameu or efamed or epax or feniko or himega or "k 85" or "lachs 550" or lipitac or olemar or optimepa or pikasol or promega or superepa or "sea omega" #17 MeSH descriptor: [Fatty Acids, Omega‐3] explode all trees #18 omega3 or "omega 3" or n3 fatty acid* or n 3 fatty acid* or "n3 PUFA" or "n 3 PUFA" or n3 polyunsaturated fatty acid* or n 3 polyunsaturated fatty acid* or n3 Oil* or n 3 oil* or "bilantin omega" or "conchol 36" or "eicosa e" or eicosapen or epaisdin or epanova or "omega forte" or sakana #19 MeSH descriptor: [Docosahexaenoic Acids] explode all trees #20 docosahex* or dhasco or DHA or DPA #21 MeSH descriptor: [Eicosapentaenoic Acid] explode all trees #22 eicosapen* or timnodonic or icosapent* #23 {or #8‐#22} #24 #7 and #23
Appendix 2. MEDLINE Ovid search strategy
1. Randomized Controlled Trial.pt. 2. Controlled Clinical Trial.pt. 3. (randomized or randomised).ab,ti. 4. placebo.ab,ti. 5. drug therapy.fs. 6. randomly.ab,ti. 7. trial.ab,ti. 8. groups.ab,ti. 9. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 10. exp animals/ not humans.sh. 11. 9 not 10 12. exp Retinitis Pigmentosa/ 13. ((retini* or retina* or retinopath*) adj2 pigment*).tw. 14. ((tapetoretina* or tapeto retina*) adj2 (degener* or dystroph*)).tw. 15. (rod adj2 cone adj2 dystroph*).tw. 16. exp Tangier Disease/ 17. (tangier adj2 disease*).tw. 18. or/12‐17 19. exp Vitamin A/ 20. ("vitamin a" or "aquasol a" or "vitamin a1" or "a vitamin" or "vit a" or "A 313" or "all‐trans‐retinyl alcohol" or "Anti‐Infective Vitamin" or "Antixerophthalmic Vitamin" or "Arovit" or "Avibon" or "Avitol" or "Axerol" or "Axerophthol" or "Axerophtholum" or "Biosterol" or "Biovit‐A" or "Chocola A" or "Del‐VI‐A" or "Ido A 50" or "Idrurto A" or "Lard Factor" or "Ledovit A" or "Micelle A" or "Mulsal A Megadosis" or "Oleovitamin A" or "Ophthalamin" or "Palmitate‐1‐14C" or "Rinocusi Vitaminico" or "viatmin a" or "Vitaminoftalmina" or "Vitaminum A" or "Viva‐Drops" or "Vogan").tw. 21. exp Retinoids/ 22. (retino* or retinyl palmitate*).tw. 23. exp beta Carotene/ 24. (beta carotene* or betacarotene* or Carotaben or "Max Caro" or MaxCaro or Solatene or Vetoron or BellaCarotin or Provatene or "b‐tene" or "beta carotin" or betatene or lurotin or solvin or "b Carotene" or "B‐Caro‐T" or BETACRTN or Caroguard or Lumitene or "Provitamin A").tw. 25. exp Fish Oils/ 26. (oil* adj3 (fish* or "cod liver" or halibut or squid or krill or mackerel or menhaden or salmon or seal or "shark liver" or seafood)).tw. 27. (EPA or EFA or MaxEPA or ameu or efamed or epax or feniko or himega or "k 85" or "lachs 550" or lipitac or olemar or optimepa or pikasol or promega or superepa or "sea omega").tw. 28. exp Fatty Acids, Omega‐3/ 29. (omega3 or "omega 3" or n3 fatty acid* or n 3 fatty acid* or "n3 PUFA" or "n 3 PUFA" or n3 polyunsaturated fatty acid* or n 3 polyunsaturated fatty acid* or n3 Oil* or n 3 oil* or "bilantin omega" or "conchol 36" or "eicosa e" or eicosapen or epaisdin or epanova or "omega forte" or sakana).tw. 30. exp Docosahexaenoic Acids/ 31. (docosahex* or dhasco or DHA or DPA).tw. 32. exp Eicosapentaenoic Acid/ 33. (eicosapen* or timnodonic or icosapent*).tw. 34. or/19‐33 35. 18 and 34 36. 11 and 35
The search filter for trials at the beginning of the MEDLINE strategy is from the published paper by Glanville 2006.
Appendix 3. Embase.com search strategy
#1 'randomized controlled trial'/exp #2 'randomization'/exp #3 'double blind procedure'/exp #4 'single blind procedure'/exp #5 random*:ab,ti #6 #1 OR #2 OR #3 OR #4 OR #5 #7 'animal'/exp OR 'animal experiment'/exp #8 'human'/exp #9 #7 AND #8 #10 #7 NOT #9 #11 #6 NOT #10 #12 'clinical trial'/exp #13 (clin* NEAR/3 trial*):ab,ti #14 ((singl* OR doubl* OR trebl* OR tripl*) NEAR/3 (blind* OR mask*)):ab,ti #15 'placebo'/exp #16 placebo*:ab,ti #17 random*:ab,ti #18 'experimental design'/exp #19 'crossover procedure'/exp #20 'control group'/exp #21 'latin square design'/exp #22 #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 #23 #22 NOT #10 #24 #23 NOT #11 #25 'comparative study'/exp #26 'evaluation'/exp #27 'prospective study'/exp #28 control*:ab,ti OR prospectiv*:ab,ti OR volunteer*:ab,ti #29 #25 OR #26 OR #27 OR #28 #30 #29 NOT #10 #31 #30 NOT (#11 OR #23) #32 #11 OR #24 OR #31 #33 'retinitis pigmentosa'/exp #34 ((retini* OR retina* OR retinopath*) NEAR/2 pigment*):ab,ti #35 ((tapetoretina* OR 'tapeto retina*') NEAR/2 (degener* OR dystroph*)):ab,ti #36 (rod NEAR/2 cone NEAR/2 dystroph*):ab,ti #37 'tangier disease'/exp #38 (tangier NEAR/2 disease*):ab,ti #39 #33 OR #34 OR #35 OR #36 OR #37 OR #38 #40 'retinol'/exp #41 ("vitamin a" OR "aquasol a" OR "vitamin a1" OR "a vitamin" OR "vit a" OR "A 313" OR "all‐trans‐retinyl alcohol" OR "Anti‐Infective Vitamin" OR "Antixerophthalmic Vitamin" OR "Arovit" OR "Avibon" OR "Avitol" OR "Axerol" OR "Axerophthol" OR "Axerophtholum" OR "Biosterol" OR "Biovit‐A" OR "Chocola A" OR "Del‐VI‐A" OR "Ido A 50" OR "Idrurto A" OR "Lard Factor" OR "Ledovit A" OR "Micelle A" OR "Mulsal A Megadosis" OR "Oleovitamin A" OR "Ophthalamin" OR "Palmitate‐1‐14C" OR "Rinocusi Vitaminico" OR "viatmin a" OR "Vitaminoftalmina" OR "Vitaminum A" OR "Viva‐Drops" OR "Vogan"):ab,ti,tn #42 'retinoid'/exp #43 retino*:ab,ti,tn OR 'retinyl palmitate*':ab,ti,tn #44 'beta carotene'/exp #45 'beta carotene*':ab,ti,tn OR betacarotene*:ab,ti,tn OR carotaben:ab,ti,tn OR 'max caro':ab,ti,tn OR maxcaro:ab,ti,tn OR solatene:ab,ti,tn OR vetoron:ab,ti,tn OR 'bellacarotin':ab,ti,tn OR provatene:ab,ti,tn OR 'b‐tene':ab,ti,tn OR 'beta carotin':ab,ti,tn OR betatene:ab,ti,tn OR lurotin:ab,ti,tn OR solvin:ab,ti,tn OR "b Carotene":ab,ti,tn OR "B‐Caro‐T":ab,ti,tn OR BETACRTN:ab,ti,tn OR Caroguard:ab,ti,tn OR Lumitene:ab,ti,tn OR "Provitamin A":ab,ti,tn) #46 'fish oil'/exp #47 (oil* NEAR/3 (fish* OR 'cod liver*' OR halibut OR squid OR krill OR mackerel OR menhaden OR salmon OR seal OR 'shark liver*' OR seafood)):ab,ti,tn #48 epa:ab,ti,tn OR efa:ab,ti,tn OR maxepa:ab,ti,tn OR ameu:ab,ti,tn OR efamed:ab,ti,tn OR epax:ab,ti,tn OR feniko:ab,ti,tn OR himega:ab,ti,tn OR 'k 85':ab,ti,tn OR 'lachs 550':ab,ti,tn OR lipitac:ab,ti,tn OR olemar:ab,ti,tn OR optimepa:ab,ti,tn OR pikasol:ab,ti,tn OR promega:ab,ti,tn OR superepa:ab,ti,tn OR "sea omega":ab,ti,tn #49 'omega 3 fatty acid'/exp #50 omega3:ab,ti,tn OR 'omega 3':ab,ti,tn OR 'n3 fatty acid*':ab,ti,tn OR 'n 3 fatty acid*':ab,ti,tn OR 'n3 pufa':ab,ti,tn OR 'n 3 pufa':ab,ti,tn OR 'n3 polyunsaturated fatty acid*':ab,ti,tn OR 'n 3 polyunsaturated fatty acid*':ab,ti,tn OR 'n3 oil*':ab,ti,tn OR 'n 3 oil*':ab,ti,tn OR 'bilantin omega':ab,ti,tn OR 'conchol 36':ab,ti,tn OR 'eicosa e':ab,ti,tn OR eicosapen:ab,ti,tn OR epaisdin:ab,ti,tn OR epanova:ab,ti,tn OR 'omega forte':ab,ti,tn OR sakana:ab,ti,tn #51 'docosahexaenoic acid'/exp #52 docosahex*:ab,ti,tn OR dhasco:ab,ti,tn OR dha:ab,ti,tn OR dpa:ab,ti,tn #53 'icosapentaenoic acid'/exp #54 eicosapen*:ab,ti,tn OR timnodonic:ab,ti,tn OR icosapent*:ab,ti,tn #55 #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50 OR #51 OR #52 OR #53 OR #54 #56 #39 AND #55 #57 #32 AND #56
Appendix 4. PubMed search strategy
1. ((randomized controlled trial[pt]) OR (controlled clinical trial[pt]) OR (randomised[tiab] OR randomized[tiab]) OR (placebo[tiab]) OR (drug therapy[sh]) OR (randomly[tiab]) OR (trial[tiab]) OR (groups[tiab])) NOT (animals[mh] NOT humans[mh]) 2. ((retini*[tw] OR retina*[tw] OR retinopath*[tw]) AND pigment*[tw]) 3. (tapetoretina*[tw] OR tapeto retina*[tw]) AND (degener*[tw] OR dystroph*[tw]) 4. (rod[tw] AND cone[tw] AND dystroph*[tw]) 5. (tangier[tw] AND disease*[tw]) 6. #2 OR #3 OR #4 OR #5 7. "vitamin a"[tw] OR "aquasol a"[tw] OR "vitamin a1"[tw] OR "a vitamin"[tw] OR "vit a"[tw] OR "A 313"[tw] OR "all‐trans‐retinyl alcohol"[tw] OR "Anti‐Infective Vitamin"[tw] OR "Antixerophthalmic Vitamin"[tw] OR "Arovit"[tw] OR "Avibon"[tw] OR "Avitol"[tw] OR "Axerol"[tw] OR "Axerophthol"[tw] OR "Axerophtholum"[tw] OR "Biosterol"[tw] OR "Biovit‐A"[tw] OR "Chocola A"[tw] OR "Del‐VI‐A"[tw] OR "Ido A 50"[tw] OR "Idrurto A"[tw] OR "Lard Factor"[tw] OR "Ledovit A"[tw] OR "Micelle A"[tw] OR "Mulsal A Megadosis"[tw] OR "Oleovitamin A"[tw] OR "Ophthalamin"[tw] OR "Palmitate‐1‐14C"[tw] OR "Rinocusi Vitaminico"[tw] OR "viatmin a"[tw] OR "Vitaminoftalmina"[tw] OR "Vitaminum A"[tw] OR "Viva‐Drops"[tw] OR "Vogan"[tw] 8. retino*[tw] OR retinyl palmitate*[tw] 9. beta carotene*[tw] OR betacarotene*[tw] OR carotaben[tw] OR "max caro"[tw] OR maxcaro[tw] OR solatene[tw] OR vetoron[tw] OR bellacarotin[tw] OR provatene[tw] OR "b‐tene"[tw] OR "beta carotin"[tw] OR betatene[tw] OR lurotin[tw] OR solvin[tw] OR "b Carotene"[tw] OR "B‐Caro‐T"[tw] OR BETACRTN[tw] OR Caroguard[tw] OR Lumitene[tw] OR "Provitamin A"[tw] 10. (oil*[tw] AND (fish*[tw] OR cod liver*[tw] OR halibut[tw] OR squid[tw] OR krill[tw] OR mackerel[tw] OR menhaden[tw] OR salmon[tw] OR seal[tw] OR shark liver*[tw] OR seafood[tw])) 11. epa[tw] OR efa[tw] OR maxepa[tw] OR ameu[tw] OR efamed[tw] OR epax[tw] OR feniko[tw] OR himega[tw] OR "k 85"[tw] OR "lachs 550"[tw] OR lipitac[tw] OR olemar[tw] OR optimepa[tw] OR pikasol[tw] OR promega[tw] OR superepa[tw] OR "sea omega"[tw] 12. omega3[tw] OR "omega 3"[tw] OR n3 fatty acid*[tw] OR n 3 fatty acid*[tw] OR "n3 pufa"[tw] OR "n 3 pufa"[tw] OR n3 polyunsaturated fatty acid*[tw] OR n 3 polyunsaturated fatty acid*[tw] OR n3 oil*[tw] OR n 3 oil*[tw] OR "bilantin omega"[tw] OR "conchol 36"[tw] OR "eicosa e"[tw] OR eicosapen[tw] OR epaisdin[tw] OR epanova[tw] OR "omega forte"[tw] OR sakana[tw] 13. docosahex*[tw] OR dhasco[tw] OR dha[tw] OR dpa[tw] 14. eicosapen*[tw] OR timnodonic[tw] OR icosapent*[tw] 15. #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 16. #6 AND #15 17. #1 AND #16 18. Medline[sb] 19. #17 NOT #18
Appendix 5. LILACS search strategy
(MH:C11.270.684$ OR MH:C11.768.585.658.500$ OR MH:C16.320.290.684$ OR (Retini$ AND Pigment$) OR (Retina$ AND Pigment$) OR (Retinopath$ AND Pigment$) OR (tapetoretina$ AND degener$) OR (tapetoretina$ AND dystroph$) OR (tapeto retina$ AND degener$) OR (tapeto retina$ AND dystroph$) OR (rod AND cone AND dystroph$) OR MH:C10.668.829.800.875$ OR MH:C16.320.565.398.500.330.750$ OR MH:C18.452.584.500.875.330.750$ OR MH:C18.452.648.398.500.330.750$ OR "Tangier Disease" OR "Enfermedad de Tangier" OR "Doença de Tangier") AND ((MH:D02.455.326.271.665.202.495.818$ OR MH:D02.455.426.392.368.367.379.249.700.860$ OR MH:D02.455.849.131.495.818$ OR MH:D23.767.261.700.860$ OR "vitamin a" OR "aquasol a" OR "vitamin a1" OR "a vitamin" OR "vit a" OR "A 313" OR "all‐trans‐retinyl alcohol" OR "Anti‐Infective Vitamin" OR "Antixerophthalmic Vitamin" OR "Arovit" OR "Avibon" OR "Avitol" OR "Axerol" OR "Axerophthol" OR "Axerophtholum" OR "Biosterol" OR "Biovit‐A" OR "Chocola A" OR "Del‐VI‐A" OR "Ido A 50" OR "Idrurto A" OR "Lard Factor" OR "Ledovit A" OR "Micelle A" OR "Mulsal A Megadosis" OR "Oleovitamin A" OR "Ophthalamin" OR "Palmitate‐1‐14C" OR "Rinocusi Vitaminico" OR "viatmin a" OR "Vitaminoftalmina" OR "Vitaminum A" OR "Viva‐Drops" OR "Vogan" OR MH:D02.455.326.271.665.202.495$ OR MH:D02.455.426.392.368.367.379.249.700$ OR MH:D02.455.849.131.495$ OR MH:D23.767.261.700$ OR retino$ OR (retinyl palmitate$) OR MH:D02.455.326.271.665.202.123$ OR MH:D02.455.426.392.368.367.379.249.050$ OR MH:D02.455.849.131.123$ OR MH:D23.767.261.050$ OR (beta caroten$) OR betacarotene* OR Carotaben OR "Max Caro" OR MaxCaro OR Solatene OR Vetoron OR BellaCarotin OR Provatene OR "b‐tene" OR "beta carotin" OR betatene OR lurotin OR solvin OR MH: D10.627.430$ OR (oil$ AND (fish$ OR "cod liver" OR halibut OR squid OR krill OR mackerel OR menhaden OR salmon OR seal OR "shark liver" OR seafood)) OR EPA OR EFA OR MaxEPA OR ameu OR efamed OR epax OR feniko OR himega OR "k 85" OR "lachs 550" OR lipitac OR olemar OR optimepa OR pikasol OR promega OR superepa OR "sea omega" OR "Aceites de Pescado" OR "Óleos de Peixe" OR MH:D10.212.302.380.410$ OR MH:D10.251.355.337$ OR MH:D10.627.430.450$ OR omega3 OR "omega 3" OR (n3 fatty acid$) OR (n 3 fatty acid$) OR "n3 PUFA" OR "n 3 PUFA" OR (n3 polyunsaturated fatty acid$) OR (n 3 polyunsaturated fatty acid$) OR (n3 oil$) OR (n 3 oil$) OR "bilantin omega" OR "conchol 36" OR "eicosa e" OR eicosapen OR epaisdin OR epanova OR "omega forte" OR sakana OR Docosahex$ OR dhasco OR DHA OR DPA OR "Docosa Hexaenoicos"OR eicosapen$ OR timnodonic OR icosapent$))
Appendix 6. metaRegister of Controlled Trials search strategy
(Retinitis Pigmentosa) AND (fish oil OR omga 3 OR docsahexaenoic OR eicosapentaenoic OR vitamin A OR Retino OR carotene)
Appendix 7. ClinicalTrials.gov search strategy
(Retinitis Pigmentosa) AND (Vitamin A OR Retinoids OR beta Carotene OR fish oils OR Omega‐3 Fatty Acids)
Appendix 8. WHO ITCRP search strategy
Retinitis Pigmentosa AND Vitamin A OR Retinitis Pigmentosa AND Retinoids OR Retinitis Pigmentosa AND Retinol OR Retinitis Pigmentosa AND beta Carotene OR Retinitis Pigmentosa AND fish oils OR Retinitis Pigmentosa AND Omega‐3 Fatty Acids OR Retinitis Pigmentosa AND Docosahexaenoic OR Retinitis Pigmentosa AND Eicosapentaenoic
Appendix 9. OpenGrey search strategy
(Retinitis Pigmentosa) AND (Vitamin A OR Retinoids OR beta Carotene OR fish oils OR Omega‐3 Fatty Acids)
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Berson 1993.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes |
Notes: the trial was originally planned to allow for 4 years of follow‐up for each participant. However, due to slow recruitment (required 3 years), follow‐up was continued on all participants until the last randomized participants had completed their 4th year of follow‐up. The DSMB recommended cessation of this protocol in September 1991 because by then all participants had completed their 4th year of follow‐up, and additional follow‐up data would probably not lead to conclusions that would be substantially more precise. The smaller sample sizes at year 5 (n = 472) and year 6 (n = 261) reflect the fact that the study was stopped after the last 4‐year follow‐up visit. The mean duration of follow‐up was 5.2 years for all randomized participants. Trial registration number: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | “A separate set of randomization assignments was maintained for each stratum based on a computer‐generated set of random numbers to facilitate the above randomization” (p 764) |
| Allocation concealment (selection bias) | Low risk | “Each bottle contained 100 capsules labeled with a lot number and instructions for storage at room temperature but not labeled as to content.” (p 763) |
| Blinding of Participants | Low risk | “Patients did not know the contents of the supplements under study or their group assignment and also agreed not to know the course of their retinal degeneration until the end of the study” (p 764) |
| Blinding of Caregivers | Low risk | “All members of the staff in contact with the patients, including the principal investigator (E.L.B.), were masked as to the treatment group assignment of each patient.” (p 764) |
| Blinding outcome assessors for primary outcome (visual field) | Low risk | “All members of the staff in contact with the patients, were masked as to the treatment group assignment of each patient. Each ocular examination and ERG was performed without review of previous records” (p 764) |
| Blinding outcome assessors for secondary outcome (visual acuity) | Low risk | “All members of the staff in contact with the patients were masked as to the treatment group assignment of each patient. Each ocular examination and ERG was performed without review of previous records” (p 764) |
| Blinding outcome assessors for secondary outcome (ERG) | Low risk | “Each ocular examination and ERG was performed without review of previous records.” (p 764) |
| Incomplete outcome data addressed for primary outcome (visual field) | Low risk | “Only 5% (29/601) of patients failed to complete this study; four of these patients died and 25 patients declined to continue participation, most after the fourth year.” (p 770) |
| Incomplete outcome data addressed for secondary outcome (visual acuity) | Low risk | “Only 5% (29/601) of patients failed to complete this study; four of these patients died and 25 patients declined to continue participation, most after the fourth year.” (p 770) |
| Incomplete outcome data addressed for secondary outcome (ERG) | Low risk | “Only 5% (29/601) of patients failed to complete this study; four of these patients died and 25 patients declined to continue participation, most after the fourth year.” (p 770) |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement, as the study protocol is not available |
| Other bias | Low risk | We did not detect other bias. |
Berson 2004a.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
Each participant received either 6 capsules/day each containing 500 mg of fatty acids (200 mg of which was DHA, for a total of 1200 mg/d of DHA), or 6 placebo capsules/day containing 500 mg of fatty acids with no DHA, for 4 years. Vitamin A was administered as retinyl palmitate. |
|
| Outcomes |
|
|
| Notes |
Trial registration number: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A separate set of randomization assignments was maintained for each stratum based on a computer generated set of random numbers" (p 1299) |
| Allocation concealment (selection bias) | Low risk | ". . . computer generated set of random numbers that was available only to a programmer who provided assignment information to the data manager (C.W.D.) on a case‐by‐case basis. Group assignment was implemented by the data manager" (p 1299) |
| Blinding of Participants | Low risk | "Patients did not know the contents of the supplement under study or their treatment group assignment and also agreed not to know the course of their retinal degeneration until the end of the study" (p 1299) |
| Blinding of Caregivers | Low risk | "All members of the staff in contact with the patients, including the principal investigator (E.L.B.), were masked with regard to each patient’s treatment group assignment" (p 1299) |
| Blinding outcome assessors for primary outcome (visual field) | Low risk | "Each ocular examination was performed without review of previous records" (p 1299) |
| Blinding outcome assessors for secondary outcome (visual acuity) | Low risk | "Treatment group assignments and plasma DHA and RBC PE DHA levels were placed in records separate from that used for ocular examinations as part of masking those in contact with the patients" (p 1299) |
| Blinding outcome assessors for secondary outcome (ERG) | Low risk | "Treatment group assignments and plasma DHA and RBC PE DHA levels were placed in records separate from that used for ocular examinations as part of masking those in contact with the patients" (p 1299) |
| Incomplete outcome data addressed for primary outcome (visual field) | Low risk | "Two hundred eight of these patients (221) completed all 4 annual follow‐up visits. Analyses performed on patients with partial follow‐up, but with missing values left as missing and after using multiple imputation methods to account for missing data among patients with incomplete followup" (p 1301) |
| Incomplete outcome data addressed for secondary outcome (visual acuity) | Low risk | "Two hundred eight of these patients (221) completed all 4 annual follow‐up visits. Analyses performed on patients with partial follow‐up, but with missing values left as missing and after using multiple imputation methods to account for missing data among patients with incomplete followup" (p 1301) |
| Incomplete outcome data addressed for secondary outcome (ERG) | Low risk | "Two hundred eight of these patients (221) completed all 4 annual follow‐up visits. Analyses performed on patients with partial follow‐up, but with missing values left as missing and after using multiple imputation methods to account for missing data among patients with incomplete followup" (p 1301) |
| Selective reporting (reporting bias) | Unclear risk | Study protocol is not available. |
| Other bias | Low risk | We did not detect other bias. |
Hoffman 2004.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
Each participant received 2 capsules/day each containing 500 mg of fatty acids (200 mg of which was DHA, for a total of 400 mg/d of DHA), or 2 placebo capsules/day containing 500 mg of fatty acids with no DHA, administered for 4 years. |
|
| Outcomes |
|
|
| Notes |
Trial registration number: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Placebo and + DHA assignments were made following a block randomization schedule (10/block).” (p 705) Method used for random sequence generation is unclear. |
| Allocation concealment (selection bias) | Low risk | “Relatives were randomized together to eliminate a potential for mixing of capsules; there were five sib‐pairs in each cohort” (p 705) |
| Blinding of Participants | Low risk | “All medications were labeled either A or B by the manufacturer. Both study oils were encapsulated with ethyl vanillin‐flavored gelatin; thus, smell and taste of the capsules were identical.” (p 705) |
| Blinding of Caregivers | Low risk | “Martek retained the code and divulged group assignment to the Data and Safety Monitoring Committee when requested to or to a patient’s physician in case of a medical emergency.” (p 705) |
| Blinding outcome assessors for primary outcome (visual field) | Low risk | “The randomization code was not available to study personnel conducting visual function assessments until after completion of testing.” (p 705) |
| Blinding outcome assessors for secondary outcome (visual acuity) | Low risk | “The randomization code was not available to study personnel conducting visual function assessments until after completion of testing.” (p 705) |
| Blinding outcome assessors for secondary outcome (ERG) | Low risk | “The randomization code was not available to study personnel conducting visual function assessments until after completion of testing.” (p 705) |
| Incomplete outcome data addressed for primary outcome (visual field) | Low risk | “Of the 44 patients enrolled, all completed 3 years; 41 patients completed 4 years. . . test results from the previous year were used in place of an occasional missing value” (pp 706, 709) |
| Incomplete outcome data addressed for secondary outcome (visual acuity) | Low risk | “Of the 44 patients enrolled, all completed 3 years; 41 patients completed 4 years. . . test results from the previous year were used in place of an occasional missing value” (pp 706, 709) |
| Incomplete outcome data addressed for secondary outcome (ERG) | Low risk | “Of the 44 patients enrolled, all completed 3 years; 41 patients completed 4 years. . . test results from the previous year were used in place of an occasional missing value” (pp 706, 709) |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information to permit judgement as the study protocol is not available |
| Other bias | Low risk | We did not detect other bias. |
Hoffman 2014.
| Study characteristics | ||
| Methods |
|
|
| Participants |
|
|
| Interventions |
|
|
| Outcomes |
|
|
| Notes |
Trial registration number: NCT00100230 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants (ages 7–31 years) meeting entry criteria were assigned to DHA (n = 41) or placebo (n = 37) using a computer‐generated randomization schedule with varying block sizes" (p 4) |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding of Participants | Low risk | "The DHA and placebo capsules were indistinguishable based on appearance, smell, or taste and contained vitamins E and C as antioxidants (12.5 mg each) and food‐grade orange extract as flavoring (5.9 mg)." (p 4) |
| Blinding of Caregivers | Low risk | "All testing personnel were masked to treatment assignment."; "The DHA and placebo capsules were indistinguishable based on appearance, smell, or taste and contained vitamins E and C as antioxidants (12.5 mg each) and food‐grade orange extract as flavoring (5.9 mg)." (p 4) |
| Blinding outcome assessors for primary outcome (visual field) | Low risk | "All testing personnel were masked to treatment assignment." (p 4) |
| Blinding outcome assessors for secondary outcome (visual acuity) | Low risk | "All testing personnel were masked to treatment assignment." (p 4) |
| Blinding outcome assessors for secondary outcome (ERG) | Low risk | "All testing personnel were masked to treatment assignment." (p 4) |
| Incomplete outcome data addressed for primary outcome (visual field) | High risk | 22 of 37 participants in placebo group and 29 of 41 participants in the DHA group completed 4‐year follow‐up; attrition and reasons for attrition were described; "A lower than expected event rate and an underpowered trial due to participant dropout were primary trial limitations." (p 9) |
| Incomplete outcome data addressed for secondary outcome (visual acuity) | High risk | 22 of 37 participants in placebo group and 29 of 41 participants in the DHA group completed 4‐year follow‐up; attrition and reasons for attrition were described; "A lower than expected event rate and an underpowered trial due to participant dropout were primary trial limitations." (p 9) |
| Incomplete outcome data addressed for secondary outcome (ERG) | High risk | 22 of 37 participants in placebo group and 29 of 41 participants in the DHA group completed 4‐year follow‐up; attrition and reasons for attrition were described; "A lower than expected event rate and an underpowered trial due to participant dropout were primary trial limitations." (p 9) |
| Selective reporting (reporting bias) | High risk | Third outcome listed in the ClinicalTrials.gov registration (loss of peripheral visual fields) was not described in the publication. |
| Other bias | Low risk | We did not detect other bias. |
±: plus or minus/with or without >: more/greater than ≥: more/greater than or equal to <: less than DHA: docosahexaenoic acid DSMB: Data and Safety Monitoring Board EDTRS: Early Treatment Diabetic Retinopathy Study ERG: electroretinogram HFA: Humphrey Field Analyzer IU: international units no.: number RBC: red blood cells RCT: randomized controlled trial RP: retinitis pigmentosa SD: standard deviation SE: standard error TEAEs: treatment‐emergent adverse events VFS: visual field sensitivity
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bergsma 1977 | Not randomized. A cohort of RP patients followed prospectively before and after administration of vitamin A without a control group. |
| Berson 2010 | Vitamin A was given to all participants. Not able to justify the effectiveness of vitamin A |
| Berson 2012 | Re‐analysis of 3 RCTs |
| Dagnelie 2000 | Not randomized. A cohort of RP patients and patients with related retinal degenerations followed prospectively before and after administration of lutein. No control group |
| Fex 1996 | Uncontrolled trial, did not examine the outcome of interest to this review |
| Johnson 2008 | Not the population of interest, healthy women not retinitis pigmentosa |
| JPRN UMIN000005510 | Single‐arm study |
| Massof 2010 | Not an RCT, letter |
| McCafferty 2017 | Not the population of interest |
| NCT00004345 | Not an RCT |
| NCT00346333 | Not an intervention of interest, all participants received vitamin A |
| NCT01256697 | Cross‐over trial |
| NCT01543906 | Single‐arm study |
| NCT01680510 | Cross‐over design |
| NCT02018692 | Not a comparator of interest |
| Norton 1993 | Not a comparator of interest |
| Pierce 2017 | Re‐analysis of 3 RCTs |
| Sibulesky 1999 | Secondary analysis assessing the safety of long‐term vitamin A supplementation for RP in an RCT (Berson 1993) |
| Tcherkes 1950 | Not randomized. A cohort of RP patients followed prospectively before and after administration of vitamin A. No control group |
| Wheaton 2003 | Secondary analysis assessing the safety of long‐term DHA supplementation for X‐linked RP in an RCT |
| Wittes 2011 | Not an RCT, letter |
| Zhao 2019 | Not an RCT, review article |
DHA: docosahexaenoic acid RCT: randomized controlled trial RP: retinitis pigmentosa
Characteristics of ongoing studies [ordered by study ID]
CTRI/2016/01/006497.
| Study name | A Ayurvedic treatment of retinitis pigmentosa compared with modern treatment |
| Methods | Randomized parallel‐group design |
| Participants |
Inclusion criteria: individuals aged 16 to 50 years, who are: willing to participant in the present study; show symptoms of night blindness, markedly reduced dark adaptation, progressive visual field loss, double vision, etc.; have bony corpuscles, have fundus retinal vessels narrowing especially arteriolar narrowing; have vitreous changes such as cells, opacities and pigments; macular changes; such as edema atrophic changes, pigment clumping, etc. Exclusion criteria: individuals aged age < 16 or > 50 years, individuals not willing for present study, or are extremely debilitating and not able to withstand treatment procedures, or have vision less than 6/60 or any lenticular changes, individuals with total blindness and other known systemic pathology will be excluded from study. |
| Interventions |
Intervention 1: 1) Snehayukta Virechana, followed by 2) oral medication along with nasya and tarpana Intervention 2: 1) Snehayukta Virechana include, deepana and pachana by trikatu churna for 3 to 5 days, snehapana by plain cow ghrita till the samyak Snigdha Lakshana appear, external snehana with bala taila followed by swedana once a day for 3 days, virechana with triphala kwath and eranda taila samsarjana Krama for 3 to 7 days. (Acc. to type of Shuddhi), followed by 2) bhrinaraja taila Nasya 7 days → tarpana with goghrita for 7 days. 1 such course of nasya and tarpana in a month for 3 months. 3) The oral medicine will be started after samsarjana krama till completion of the therapy. Comparator intervention: 1) capsule Aquasol A (vitamin A) 50,000 IU once daily for 1 month 2) tablet Complamina retard once daily for 3 months |
| Outcomes |
Primary outcomes:
Secondary outcome:
Maximum follow‐up: 6 months |
| Starting date | February 2015 Estimated end date: not reported |
| Contact information | www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=12218 |
| Notes |
NCT00004827.
| Study name | Study of docosahexaenoic acid (DHA) supplementation in patients with X‐linked retinitis pigmentosa |
| Methods | Randomized parallel‐group design |
| Participants |
Inclusion criteria: 46 children and adults with early stage X‐linked retinitis pigmentosa, with sufficient cone function determined by recordable ERG (30 Hz amplitude; greater than 0.32 microvolts); visual fields greater than 20 degrees; sufficient rod function (greater than 3.0 microvolts amplitude); media clarity sufficient for fundus photography; with no concurrent use of anticoagulant medication; no chronic metabolic disease that could interfere with fatty acid metabolism; and no bleeding of clinical significance Exclusion criteria: not reported |
| Interventions |
Intervention: 2 gel capsules per day of docosahexaenoic acid (DHA)‐enriched oil Comparator intervention: 2 gel capsules per day of placebo |
| Outcomes |
Primary outcome: retardation of progression of visual function loss Secondary outcome: not reported Maximum follow‐up: 3 years |
| Starting date | March 1996 Estimated end date: 25 March 2015 |
| Contact information | clinicaltrials.gov/ct2/show/record/NCT00004827 |
| Notes |
ERG: electroretinogram IU: international units
Differences between protocol and review
In the protocol, we stated that we would record visual acuity data at six months. However, when writing the full review, we found that none of the four included trials reported visual acuity data at six‐month intervals.
We stated in the inclusion criteria in the protocol that when both fish oil and vitamin A were included in one group, we would not include a comparison to vitamin A, which would lead to the exclusion of studies comparing fish oil + vitamin A versus vitamin A. However, our original intention also included seeking evidence on the effectiveness of fish oil, therefore we modified this criterion in the review to include such studies.
Contributions of authors
SGS and PC conceived and designed the review. SGS co‐ordinated the review. SGS, AEK and SAA screened search results, organized the retrieval of papers, screened the retrieved papers against the inclusion criteria, appraised the quality of papers, abstracted data, contacted study investigators for additional information, obtained data from unpublished studies, entered data into Review Manager 5, and analyzed and interpreted the data. SAA provided a methodological perspective of support, and SGS, AEK and PC provided a clinical perspective of support. SGS, XW, AEK and SAA wrote the review. AEK and PC provided substantial critical comments. SGS and PC secured funding for the review. SGS is the guarantor for the review.
Sources of support
Internal sources
-
National Institutes of Health, USA
Stephen G Schwartz is supported by NIH 5R01EY012118‐13 and partially supported by NIH Center Core Grant P30‐EY014801
-
Research to Prevent Blindness, New York, NY, USA
Stephen G Schwartz is partially supported by an unrestricted grant to the University of Miami from Research to Prevent Blindness
-
Department of Defense, USA
Stephen G Schwartz is partially supported by DOD Grant #W81XWH‐09‐1‐0675
External sources
-
National Eye Institute, National Institutes of Health, USA
Grant 1 U01 EY020522‐01
-
National Institute for Health Research (NIHR), UK
Richard Wormald, Co‐ordinating Editor for the Cochrane Eyes and Vision (CEV) acknowledges financial support for his CEV research sessions from the Department of Health through the award made by the National Institute for Health Research to Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology for a Specialist Biomedical Research Centre for Ophthalmology.
This review update was supported by the NIHR, via Cochrane Infrastructure funding to the CEV UK editorial base.
The views expressed in this publication are those of the authors and not necessarily those of the NIHR, NHS, or the Department of Health.
Declarations of interest
Stephen G Schwartz: Dr Schwartz has within the past three years received consulting fees from Welch Allyn, which are unrelated to this work. Xue Wang: None known. Pamela Chavis: None known. Ajay Kuriyan: None known. Samuel A Abariga: None known.
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Berson 1993 {published data only}
- Berson EL, Rosner B, Sandberg MA, Hayes KC, Nicholson BW, Weigel-DiFranco C, et al. A randomized trial of vitamin A and vitamin E supplementation for retinitis pigmentosa. Archives of Ophthalmology 1993;111(6):761-72. [DOI] [PubMed] [Google Scholar]
Berson 2004a {published data only}
- Berson EL, Rosner B, Sandberg MA, Hayes KC, Weigel-DiFranco C, Moser A, et al. Clinical trial of Docosahexaenoic acid in patients with retinitis pigmentosa receiving vitamin A treatment. Archives of Ophthalmology 2004;122(9):1297-305. [DOI] [PubMed] [Google Scholar]
- Berson EL, Rosner B, Sandberg MA, Weigel-DiFranco C, Moser A, Brockhurst RJ, et al. Further evaluation of docosahexaenoic acid in patients with retinitis pigmentosa receiving vitamin A treatment: subgroup analyses. Archives of Ophthalmology 2004;122(9):1306-14. [DOI] [PubMed] [Google Scholar]
Hoffman 2004 {published data only}
- Hoffman DR, Locke KG, Wheaton DH, Fish GE, Spencer R, Birch DG. A randomized, placebo-controlled clinical trial of docosahexaenoic acid supplementation for X-linked retinitis pigmentosa. American Journal of Ophthalmology 2004;137(4):704-18. [DOI] [PubMed] [Google Scholar]
Hoffman 2014 {published data only}
- Hoffman DR, Hughbanks-Wheaton DK, Pearson NS, Fish GE, Spencer R, Takacs A, et al. Four-year placebo-controlled trial of docosahexaenoic acid in X-linked retinitis pigmentosa (DHAX trial): a randomized clinical trial. JAMA Ophthalmology 2014;132(7):866-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman DR, Hughbanks-Wheaton DK, Spencer R, Fish GE, Pearson NS, Wang YZ, et al. Docosahexaenoic acid slows visual field progression in x-linked retinitis pigmentosa: ancillary outcomes of the DHAX trial. Investigative Ophthalmology and Visual Science 2015;56(11):6646-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman DR, Wheaton DKH, Spencer R, Fish G, Pearson NS, Wang YZ, et al. Ancillary outcomes of the DHAX trial: docosahexaenoic acid (DHA) supplementation in x-linked retinitis pigmentosa (XLRP). Investigative Ophthalmology and Visual Science 2015;56:ARVO E-abstract 3803. [DOI] [PMC free article] [PubMed]
- Wheaton DKH, Birch DG, Fish GE, Spencer R, Pearson NS, Takacs A, et al. Safety assessment of high dose docosahexaenoic acid (DHA) supplementation in a 4-year randomized clinical trial in X-linked retinitis pigmentosa (XLRP). Investigative Ophthalmology and Visual Science 2014;55:ARVO E-abstract 1391. [DOI] [PMC free article] [PubMed]
References to studies excluded from this review
Bergsma 1977 {published data only}
- Bergsma DR, Wolf ML. A therapeutic trial of vitamin A in patients with pigmentary retinal degenerations: a negative study. Advances in Experimental Medicine and Biology 1977;77:197-209. [DOI] [PubMed] [Google Scholar]
Berson 2010 {published data only}
- Berson EL, Rosner B, Sandberg MA, Weigel-DiFranco C, Brockhurst RJ, Hayes KC, et al. Clinical trial of lutein in patients with retinitis pigmentosa receiving vitamin A. Archives of Ophthalmology 2010;128(4):403-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berson 2012 {published data only}
- Berson EL, Rosner B, Sandberg MA, Weigel-DiFranco C, Willett WC. ω-3 intake and visual acuity in patients with retinitis pigmentosa receiving vitamin A. Archives of Ophthalmology 2012;130(6):707-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dagnelie 2000 {published data only}
- Dagnelie G, Zorge IS, McDonald TM. Lutein improves visual function in some patients with retinal degeneration: a pilot study via the Internet. Optometry 2000;71(3):147-64. [PubMed] [Google Scholar]
Fex 1996 {published data only}
- Fex GA, Andreasson S, Ehinger B. Serum retinoids in retinitis pigmentosa patients treated with vitamin A. Graefe's Archive for Clinical and Experimental Ophthalmology 1996;234(Suppl 1):S18-21. [DOI] [PubMed] [Google Scholar]
Johnson 2008 {published data only}
- Johnson EJ, Chung HY, Caldarella SM, Snodderly DM. The influence of supplemental lutein and docosahexaenoic acid on serum, lipoproteins, and macular pigmentation. American Journal of Clinical Nutrition 2008;87(5):1521-9. [DOI] [PubMed] [Google Scholar]
JPRN UMIN000005510 {published data only}
- JPRN-UMIN000005510. Trial for retinitis pigmentosa with oral 9-cis beta-carotene. https://upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000006532 (first received 1 May 2011).
Massof 2010 {published data only}
- Massof RW, Fishman GA. How strong is the evidence that nutritional supplements slow the progression of retinitis pigmentosa? Archives of Ophthalmology 2010;128(4):493-5. [DOI] [PubMed] [Google Scholar]
McCafferty 2017 {published data only}
- McCafferty S, Harris A, Kew C, Kassm T, Lane L, Levine J, et al. Pseudophakic cystoid macular edema prevention and risk factors; prospective study with adjunctive once daily topical nepafenac 0.3% versus placebo. BMC Ophthalmology 2017;17(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT00004345 {published data only}
- NCT00004345. Study of dietary N-3 fatty acids in patients with retinitis pigmentosa and Usher Syndrome. clinicaltrials.gov/ct2/show/NCT00004345 (first received 19 October 1999).
NCT00346333 {unpublished data only}
- NCT00346333. Clinical trial of lutein for patients with retinitis pigmentosa receiving vitamin A. clinicaltrials.gov/ct2/show/NCT00346333 (first received 29 June 2006).
NCT01256697 {published data only}
- NCT01256697. The effect of oral administration of 9-cis rich powder of the alga Dunaliella bardawil on visual functions in patients with retinitis pigmentosa. clinicaltrials.gov/ct2/show/NCT01256697 (first received 8 December 2010).
NCT01543906 {published data only}
- NCT01543906. Oral QLT091001 in retinitis pigmentosa (RP) subjects with an autosomal dominant mutation in retinal pigment epithelial 65 protein (RPE65). clinicaltrials.gov/ct2/show/NCT01543906 (first received 5 March 2012).
NCT01680510 {published data only}
- NCT01680510. The effect of oral administration of 9-cis β carotene rich powder of the alga Dunaliella bardawil. clinicaltrials.gov/ct2/show/NCT01680510 (first received 7 September 2012).
NCT02018692 {published data only}
- NCT02018692. The effect of oral administration of 9-cis rich powder of the alga Dunaliella bardawil on visual functions in adolescent patients with retinitis pigmentosa. https://clinicaltrials.gov/ct2/show/NCT02018692 (first received 17 December 2013).
Norton 1993 {published data only}
- Norton EW. A randomized trial of vitamin A and vitamin E supplementation for retinitis pigmentosa. Archives of Ophthalmology 1993;111(11):1460-5. [DOI] [PubMed] [Google Scholar]
Pierce 2017 {published data only}
- Pierce EA, Bujakowska KM, Place E, Navarro-Gomez D, Maher M, Weigel-Dfranco C, et al. The effect of vitamin A on progression of retinitis pigmentosa is not determined by the underlying genetic cause of disease. Investigative Ophthalmology and Visual Science 2017;58(8):2011. [Google Scholar]
Sibulesky 1999 {published data only}
- Sibulesky L, Hayes KC, Pronczuk A, Weigel-DiFranco C, Rosner B, Berson EL. Safety of <7500 RE (<25000 IU) vitamin A daily in adults with retinitis pigmentosa. American Journal of Clinical Nutrition 1999;69(4):656-63. [DOI] [PubMed] [Google Scholar]
Tcherkes 1950 {published data only}
- Tcherkes LA, Averbach DM, Iakovleva SP. Use of vitamin A in retinitis pigmentosa. Vjestnik Oftalmologyi 1950;29(1):33-40. [Google Scholar]
Wheaton 2003 {published data only}
- Wheaton DH, Hoffman DR, Locke KG, Watkins RB, Birch DG. Biological safety assessment of docosahexaenoic acid supplementation in a randomized clinical trial for X-linked retinitis pigmentosa. Archives of Ophthalmology 2003;121(9):1269-78. [DOI] [PubMed] [Google Scholar]
Wittes 2011 {published data only}
- Wittes J, Gorin MB, Mayne ST, McCarthy CS, Sternberg PJ, Wall M. Letter from the DSMC regarding a clinical trial of lutein in patients with retinitis pigmentosa. Archives of Ophthalmology 2011;129(5):675-6. [DOI] [PubMed] [Google Scholar]
Zhao 2019 {published data only}
- Zhao Y, Feng K, Liu R, Pan J, Zhang L, Lu X. Vitamins and mineral supplements for retinitis pigmentosa. Journal of Ophthalmology 2019;2019:8524607. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
CTRI/2016/01/006497 {published data only}
- CTRI/2016/01/006497. A ayurvedic treatment of retinitis pigmentosa compared with modern treatment. www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=12218 (first received 22 February 2015).
NCT00004827 {published data only}
- NCT00004827. Study of Docosahexaenoic Acid (DHA) supplementation in patients with X-Linked retinitis pigmentosa. clinicaltrials.gov/ct2/show/NCT00004827 (first received 25 February 2000).
Additional references
Anderson 1989
- Anderson DR, Feuer WJ, Alward WL, Skuta GL. Threshold equivalence between perimeters. American Journal of Ophthalmology 1989;107(5):493-505. [DOI] [PubMed] [Google Scholar]
Berson 1969
- Berson EL, Gouras P, Hoff M. Temporal aspects of the electroretinogram. Archives of Ophthalmology 1969;81(2):207-14. [DOI] [PubMed] [Google Scholar]
Berson 1982
- Berson EL. Nutrition and retinal degenerations: vitamin A, taurine, ornithine, and phytanic acid. Retina 1982;2(4):236-55. [PubMed] [Google Scholar]
Berson 1985
- Berson EL, Sandberg MA, Rosner B, Birch DG, Hanson AH. Natural course of retinitis pigmentosa over a three-year interval. American Journal of Ophthalmology 1985;99(3):240-51. [DOI] [PubMed] [Google Scholar]
Berson 2004b
- Berson EL, Rosner B, Sandberg MA, Weigel-DiFranco C, Moser A, Brockhurst RJ, et al. Further evaluation of docosahexaenoic acid in patients with retinitis pigmentosa receiving vitamin A treatment: subgroup analyses. Archives of Ophthalmology 2004;122(9):1306-14. [DOI] [PubMed] [Google Scholar]
Birch 2005
- Birch DG. A randomized placebo-controlled clinical trial of docosahexaenoic acid (DHA) supplementation for X-linked retinitis pigmentosa. Retina 2005;25(Suppl 8):S52-4. [DOI] [PubMed] [Google Scholar]
Borly 2001
- Borly L, Wille-Jorgensen P, Rasmussen MS, Andersen BR. Problems with retrieving original data: is it a selection bias? In: 9th Annual Cochrane Colloquium; 2001 Oct 9-13; Lyon, France. 2001.
Chen 1996
- Chen Y, Houghton LA, Brenna JT, Noy N. Docosahexaenoic acid modulates the interactions of the interphotoreceptor retinoid-binding protein with 11-cis-retinal. Journal of Biological Chemistry 1996;271(34):20507-15. [DOI] [PubMed] [Google Scholar]
Daiger 2007
- Daiger SP, Bowne SJ, Sullivan LS. Perspective on genes and mutations causing retinitis pigmentosa. Archives of Ophthalmology 2007;125(2):151-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dowling 1960
- Dowling JE, Wald G. The biological function of vitamin A acid. Proceedings of the National Academy of Sciences 1960;46(5):587-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
Flynn 2001
- Flynn MF, Fishman GA, Anderson RJ, Roberts DK. Retrospective longitudinal study of visual acuity change in patients with retinitis pigmentosa. Retina 2001;21(6):639-46. [DOI] [PubMed] [Google Scholar]
Glanville 2006
- Glanville JM, Lefebvre C, Miles JN, Camosso-Stefinovic J. How to identify randomized controlled trials in MEDLINE: ten years on. Journal of the Medical Library Association 2006;94(2):130-6. [PMC free article] [PubMed] [Google Scholar]
GRADEpro 2014 [Computer program]
- GRADE Working Group, McMaster University GRADEpro GDT. Version accessed prior to 7 June 2017. Hamilton (ON): GRADE Working Group, McMaster University, 2014.
Hartong 2006
- Hartong DT, Berson EL, Dryja TP. Retinitis pigmentosa. Lancet 2006;368(9549):1795-809. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Deeks JJ, Altman DG, editor(s). Chapter 16: Special topics in statistics. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2017
- Higgins JPT, Altman DG, Sterne JAC, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Churchill R, Chandler J, Cumpston MS, editor(s). Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017). Cochrane, 2017. Available from www.training.cochrane.org/handbook.
Hodge 2005
- Hodge W, Barnes D, Schachter HM, Pan Y, Lowcock EC, Zhang L, et al. Effects of omega-3 fatty acids on eye health. Evidence Report: Technology Assessment (Summary) 2005;117:1-6. [PMC free article] [PubMed] [Google Scholar]
Holopigian 1996
- Holopigian K, Greenstein V, Seiple W, Carr RE. Rates of change differ among measures of visual function in patients with retinitis pigmentosa. Ophthalmology 1996;103(3):398-405. [DOI] [PubMed] [Google Scholar]
Oishi 2009
- Oishi A, Nakamura H, Tatsumi I, Sasahara M, Kojima H, Kurimoto M, et al. Optical coherence tomographic pattern and focal electroretinogram in patients with retinitis pigmentosa. Eye 2009;23(2):299-303. [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan 5). Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Schünemann 2011a
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and ‘Summary of findings' tables. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Schünemann 2011b
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Walia 2007
- Walia S, Fishman GA, Edward DP, Lindemann M. Retinal nerve fiber layer defects in RP patients. Investigative Ophthalmology and Visual Science 2007;48(10):4748-52. [DOI] [PubMed] [Google Scholar]
Witkin 2006
- Witkin AJ, Ko TH, Fujimoto JG, Chan A, Drexler W, Schuman JS, et al. Ultra-high resolution optical coherence tomography assessment of photoreceptors in retinitis pigmentosa and related diseases. American Journal of Ophthalmology 2006;142(6):945-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Rayapudi 2010
- Rayapudi S, Schwartz SG, Chavis P. Vitamin A and fish oils for retinitis pigmentosa. Cochrane Database of Systematic Reviews 2010, Issue 3. Art. No: CD008428. [DOI: 10.1002/14651858.CD008428] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rayapudi 2013
- Rayapudi S, Schwartz SG, Wang X, Chavis P. Vitamin A and fish oils for retinitis pigmentosa. Cochrane Database of Systematic Reviews 2013, Issue 12. Art. No: CD008428. [DOI: 10.1002/14651858.CD008428.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


