Abstract
Objectives
Lung ultrasonographic (LUS) imaging may play an important role in the management of patients with COVID-19–associated lung injury, particularly in some special populations. However, data regarding the prognostic role of the LUS in nursing home residents, one of the populations most affected by COVID-19, are not still available.
Design
Retrospective.
Settings and Participants
Nursing home residents affected by COVID-19 were followed up with an LUS from April 8 to May 14, 2020, in Chioggia, Venice.
Methods
COVID-19 was diagnosed through a nasopharyngeal swab. LUS results were scored using a 12-zone method. For each of the 12 zones (2 posterior, 2 anterior, 2 lateral, for both left and right lungs), the possible score ranged from 0 to 3 (1 = presence of B lines, separated, with <50% of space from the pleural line; 2 = presence of B lines, separated, with >50% of space from the pleural line; 3 = lung thickening with tissuelike aspect). The total score ranged from 0 to 36. Mortality was assessed using administrative data. Data regarding accuracy (and related parameters) were reported.
Results
Among 175 nursing home residents, 48 (mean age: 84.1 years; mainly female) were affected by COVID-19. Twelve died during the follow-up period. The mean LUS score was 3. The area under the curve of LUS in predicting mortality was 0.603 [95% confidence interval (CI): 0.419-0.787], and it increased to 0.725 (95% CI: 0.41-0.99) after including follow-up LUS controls. Taking an LUS score ≥4 as exposure variable and mortality as outcome, the sensitivity was 58.33% and specificity 63.89%, with a positive likelihood ratio of 1.62 and a negative of 0.65.
Conclusions and Implications
LUS is able to significantly predict mortality in nursing home residents affected by COVID-19, suggesting that this simple tool can be routinely used in this setting instead of more invasive techniques available only in hospital.
Keywords: Ultrasonography, lung, COVID-19, nursing home
Lung ultrasonographic (LUS) evaluation might inform clinical decision making for patients affected by Coronavirus disease 2019 (COVID-19), in particular, the management of the associated respiratory failure and lung injury that are common in these patients, even when they are asymptomatic.1
LUS is a practical and easy-to-perform procedure, being noninvasive, radiation-free, and portable. Therefore, LUS might be used for several scenarios, including the initial bedside screening of low-risk patients, the diagnosis of suspected cases in the emergency department setting, the prognostic stratification, and the monitoring of the changes in pneumonia during therapy.2 For all these characteristics, LUS seems to be the ideal tool for some special populations, for example, pregnant women and children.3 Given this background, LUS could be an ideal tool for the early identification of COVID-19 pneumonia in people affected by dementia or those highly disabled and/or bedridden, such as people residing in nursing homes.4 In this regard, the spread of the COVID-19 epidemic in nursing homes is of one the most important public health issues: it has been estimated that at least one-third of all the deaths due to COVID-19 infection occurred in nursing homes.5
Despite this background, to our knowledge, data regarding the prognostic role of LUS in nursing home residents are not still available. Therefore, with this research, we aimed to investigate the prognostic role of LUS in predicting mortality in a large nursing home placed in Chioggia, Northern Italy.
Materials and Methods
Participants
The nursing home “Felice Fortunato Casson” is situated in Chioggia, Italy, about 40 km from Venice. The nursing home can host a maximum of 175 residents. On March 29, in response to the growing awareness of COVID-19 in nursing homes, the Veneto Region advised periodical screening assessment of residents with portable serological tests or nasopharyngeal swabs every 10 days. After the first case was diagnosed in our nursing home on March 29, 2020, the emergency department chief (A.T.) began screening the residents with periodical LUS and clinical assessments (2 days in a week). The period this study refers to was from April 8 to May 14, 2020.
All data analyzed here were collected as part of routine diagnosis and treatment. In agreement with the current Italian law (Gazzetta Ufficiale della Repubblica Italiana, Serie Generale n. 76 del 31-03-2008), we informed our local Ethical Committee of this observational research regarding normal critical practice by sending a formal letter. Informed consent was collected orally for reasons of hygiene.
COVID-19 Diagnosis
A nasopharyngeal swab test with a reverse transcriptase polymerase chain reaction assay (Copan UTM System, Copan, Italy) for the identification of SARS-CoV-2 was administered to all nursing home residents.
Lung Ultrasonographic Assessment
Only persons testing positive on the nasopharyngeal swab test for COVID-19 had an LUS examination, made within 3 days from the positive test results.
Briefly, the histopathologic appearance of initial COVID-19 pneumonia is characterized by alveolar damage, while the inflammatory component is patchy and mild.6 Reparative processes with pneumocytic hyperplasia and interstitial thickening may sometimes occur.6 The advanced phases report gravitational consolidations with the presence of hemorrhagic necrosis, alveolar congestion, edema, flaking, and fibrosis.6 These pathologic findings can give specific lung patterns at the LUS that highly correlate with histopathologic findings.7
LUS examination was made according to standard procedures, with the appropriate protective gear worn by the operators.8 LUS is normally performed in supine patients.8 LUS was already used in other studies related to COVID-19 research, using a 12-zone method: 2 zones for the anterior vision, 2 for lateral, and 2 for posterior for both the left and right lungs.1 For each zone, the possible score may range from 0 to 3: 0 = normal pattern; 1 = presence of B lines separated with less than 50% of space from the pleural line (with or without thickening); 2 = presence of B lines separated with more than 50% of space from the pleural line (with or without thickening); 3 = lung thickening with tissuelike aspect. The presence of pleural effusion was also evaluated and reported in the diagnosis. The obtained score may range from 0 to 36. Only 1 operator (A.T.) performed all the examinations. In addition, follow-up measurements were made in 32 of 48 participants affected by COVID-19, after a mean of 15 days from the first examination.
Mortality
Vital status was assessed during the follow-up period using administrative data.
Statistical Analysis
After verifying the normality of the continuous variables, data were reported as mean ± standard deviation (continuous data) and numbers (percentages). The accuracy of the LUS score in predicting mortality was evaluated with the 5-fold cross-validated area under the receiver operating characteristic curve (AUC), with 95% confidence intervals (CIs). We also reported the data regarding sensitivity, specificity, and positive and negative likelihood ratios for all the cutoff points identified by the LUS score. In order to decide the best point in terms of accuracy, the Youden index9 (ie, the sum of sensitivity and specificity less 1) was calculated. We also adjusted the area under the curve using the values of the follow-up tests where available.
Threshold of statistical significance was set to 5%. All statistical analyses were performed with Stata software version 14.1 (Stata Corp LP, College Station, TX).
Results
Among the 175 residents of the nursing home in Chioggia, 50 (28.6%) were affected by COVID-19 diagnosis. Of them, for 2 residents data regarding LUS were not available. Therefore, 48 residents affected by COVID-19 were finally included in this research.
The 48 nursing home residents were aged a mean of 84.1 ± 9.8 years (range: 56-101 years), and 81.3% were female. Briefly, these residents were mainly affected by dementia and were bedridden. Of them, 12 residents died during the follow-up period, at a lethality rate of 25%.
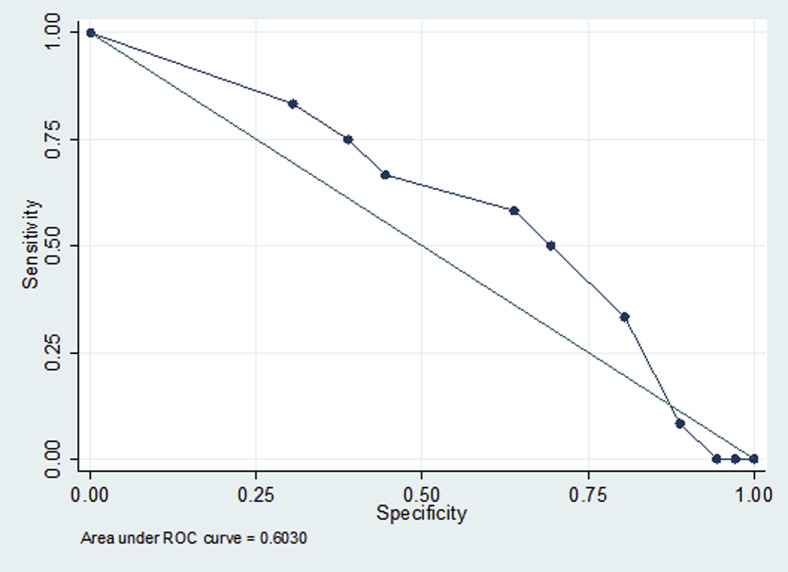
The mean LUS score was 3 (range: 0-11). Figure 1 shows the AUC, taking the LUS score as exposure and mortality as outcome. The AUC was 0.603 (95% CI: 0.419-0.787) and, after adding the follow-up LUS controls, was 0.725 (95% CI: 0.41-0.99). In Table 1 , we report the values of some accuracy parameters of the LUS score in predicting mortality. Among all the scores considered, the best was a score ≥4, for which the sensitivity in predicting mortality was 58.33%, specificity 63.89%, the positive likelihood ratio 1.62, and the negative 0.65. However, we did not find any significant difference in mortality risk in residents with an LUS score ≥4 vs <4 in predicting mortality (7/20 vs 5/28; chi-square test, Fisher exact test = 0.28).
Fig. 1.
Receiver operating characteristic (ROC) curve.
Table 1.
Sensitivity, Specificity, and Positive and Negative Likelihood Ratios for Predetermined LUS Cutoffs in Predicting Mortality
| Cutoffs | Sensitivity | Specificity | Correctly Classified | LR+ | LR– |
|---|---|---|---|---|---|
| ≥0 | 100 | 0 | 25 | 1 | - |
| ≥1 | 83.3 | 30.6 | 43.8 | 1.2 | 0.50 |
| ≥2 | 75.0 | 38.9 | 47.9 | 1.23 | 0.64 |
| ≥3 | 66.7 | 44.4 | 50.0 | 1.20 | 0.75 |
| ≥4 | 58.3 | 63.9 | 62.5 | 1.62 | 0.65 |
| ≥5 | 50.0 | 69.4 | 64.6 | 1.63 | 0.72 |
| ≥6 | 33.3 | 80.6 | 68.8 | 1.71 | 0.83 |
| ≥7 | 8.3 | 88.9 | 68.8 | 0.75 | 1.03 |
| ≥9 | 0.0 | 94.4 | 70.8 | 0 | 1.03 |
| ≥11 | 0 | 97.2 | 72.9 | 0 | 1.03 |
LR+, positive likelihood ratio; LR–, negative likelihood ratio.
Bold values indicate lung ultrasound scores ≥4, which were the most predictive in mortality among all the cutoff points considered, based on Youden's index.
We ran a similar analysis taking as exposure the oxygen saturation at the time of the LUS examination. This parameter ranged from 88% to 98%. In this case, the AUC was 0.501 (95% CI: 0.382-0.699), indicating that oxygen saturation is poorly indicative of mortality in this cohort.
Discussion
In this study including 48 nursing home older residents affected by COVID-19, we found LUS to be fairly accurate in predicting mortality, indicating that LUS examination can be used in this special population, often characterized by dementia and sudden death and, consequently, difficult to transport to hospital. To our knowledge, this is the first report in this population that seems to suffer more than all others from the COVID-19 epidemic.
In the research regarding COVID-19, the use of LUS was justified in other populations for whom the use of radiographic tests can be problematic, such as in patients recovering in the intensive care unit, children, or pregnant women. In a seminal and provocative letter, Buonsenso et al10 suggested using LUS instead of a stethoscope, which was not at all useful in viral pneumonias. Other studies have substantially confirmed that LUS has good agreement with the histopathologic findings typical of COVID-19 pneumonia and therefore with other radiographic tools.1 , 11 , 12 However, our study has 2 novel aspects that we would like to discuss.
In another study, some Italian authors reported that 67% had abnormal LUS findings, with the most common patterns represented by multiple subpleural consolidations and diffuse B-lines, often bilateral. Therefore, a diagnosis of suspect COVID-19 pneumonia was made in only half of the patients. However, our study was the first trying to associate LUS examination with mortality, thereby suggesting a potential prognostic role for this tool. In this regard, we believe that our findings are of importance because they further confirm the reliability of LUS in COVID-19, particularly if frequently repeated during the follow-up period. When we compared our data regarding LUS to the oxygen saturation, we observed that LUS is more accurate than oxygen saturation and this fact, in our opinion, probably reflects the course of COVID-19 pneumonia that often can start as mild/moderate pneumonia with precipitous clinical drops, often requiring intubation and leading to death.13 The second novel aspect is that our work may open the possibility to use LUS not only in the hospital but also at home and in the nursing home. We would like to remember that in Italy several patients affected by COVID-19 were and are treated at their homes.14 Consequently, to have a portable device that allows to easily establish the diagnosis and determine the severity of pneumonia of COVID-19 could be of importance in the near future, for treating patients affected by this condition without hospitalization.
The findings of our study must be interpreted within its limitations. First, the sample size included was small, and future larger studies are needed to confirm these findings. Second, our investigation did not consider other negative (eg, the presence of comorbidities and polypharmacology) or positive (eg, the use of therapy against COVID-19) factors in the association between LUS score and mortality. Finally, our study should be considered exploratory because the area under the curve was less than 0.70 (a common cutoff for considering a tool to have clinical value) and that the values for sensitivity/specificity for a score ≥4 are probably too low for definitively indicating LUS as a screening tool for people affected by COVID-19.
Conclusions and Implications
LUS is able to significantly predict mortality in nursing home residents affected by COVID-19, suggesting that this simple tool can be routinely used in this setting instead of the more invasive techniques available only in hospitals. Future larger studies are needed to confirm our findings.
Footnotes
The authors declare no conflicts of interest.
References
- 1.Smith M., Hayward S., Innes S., Miller A. Point-of-care lung ultrasound in patients with COVID-19—A narrative review. Anaesthesia. 2020;75:1096–1104. doi: 10.1111/anae.15082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dong D., Tang Z., Wang S. The role of imaging in the detection and management of COVID-19: A review. IEEE Rev Biomed Eng. 2020 Apr 27 doi: 10.1109/RBME.2020.2990959. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Moro F., Buonsenso D., Moruzzi M. How to perform lung ultrasound in pregnant women with suspected COVID-19. Ultrasound Obstet Gynecol. 2020;55:593–598. doi: 10.1002/uog.22028. [DOI] [PubMed] [Google Scholar]
- 4.Nouvenne A., Ticinesi A., Parise A. Point-of-care chest ultrasonography as a diagnostic resource for COVID-19 outbreak in nursing homes. J Am Med Dir Assoc. 2020;21:919–923. doi: 10.1016/j.jamda.2020.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnett M.L., Grabowski D.C. 2020. Nursing homes are ground zero for COVID-19 pandemic. Paper presented at: JAMA Health Forum. [DOI] [PubMed] [Google Scholar]
- 6.Tian S., Hu W., Niu L. Pulmonary pathology of early phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J Thorac Oncol. 2020;15:700–704. doi: 10.1016/j.jtho.2020.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Sloun R.J., Demi L. Localizing B-lines in lung ultrasonography by weakly-supervised deep learning, in-vivo results. IEEE J Biomed Health Inform. 2020;24:957–964. doi: 10.1109/JBHI.2019.2936151. [DOI] [PubMed] [Google Scholar]
- 8.Bouhemad B., Zhang M., Lu Q., Rouby J.J. Clinical review: Bedside lung ultrasound in critical care practice. Crit Care. 2007;11:205. doi: 10.1186/cc5668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hilden J., Glasziou P. Regret graphs, diagnostic uncertainty and Youden's Index. Stat Med. 1996;15:969–986. doi: 10.1002/(SICI)1097-0258(19960530)15:10<969::AID-SIM211>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 10.Buonsenso D., Pata D., Chiaretti A. COVID-19 outbreak: Less stethoscope, more ultrasound. Lancet Respir Med. 2020;8:e27. doi: 10.1016/S2213-2600(20)30120-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soldati G., Smargiassi A., Inchingolo R. Is there a role for lung ultrasound during the COVID-19 pandemic? J Ultrasound Med. 2020;39:1459–1462. doi: 10.1002/jum.15284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peng Q.Y., Wang X.T., Zhang L.N. Chinese Critical Care Ultrasound Study Group. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019-2020 epidemic. Intensive Care Unit. 2020;46:849–850. doi: 10.1007/s00134-020-05996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berlin D.A., Gulick R.M., Martinez F.J. Severe COVID-19. N Engl J Med. 2020 May 15 doi: 10.1056/NEJMcp2009575. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020;323:1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]