Abstract
Introduction
The COVID-19 pandemic has put significant stress on healthcare systems globally. This study focuses on emergency general surgery services at a major trauma centre and teaching hospital. We aimed to identify whether the number of patients and the severity of their presentation has significantly changed since the implementation of a national lockdown.
Materials and methods
This study is a retrospective review of acute referrals (from general practice and accident and emergency) to the emergency general surgery team over a 14-day period before (group 1) and during (group 2) lockdown.
Results
A total of 151 patients were reviewed by the general surgical team in group 1 and 75 in group 2 (a 50.3% reduction). The number of days with symptoms prior to presentation was significantly shorter in group 1 compared with group 2 (3 vs 4, p = 0.04). There was no significant difference in the National Early Warning Score, white blood cell count, lymphocytes and C-reactive protein on admission between the two groups of patients. There were significantly fewer patients admitted after lockdown compared with pre-lockdown (66% vs 48%, p = 0.01). Length of hospital stay was significantly shorter during lockdown compared with pre-lockdown (5 days vs 4 days, p = 0.04).
Conclusion
Fewer patients were referred and admitted during lockdown compared with pre-lockdown, and the length of stay was also significantly reduced. There was also a delay in presentation to hospital, although these patients were not more unwell based on the scoring criteria used within this study.
Keywords: COVID-19; Coronavirus, Pandemic, General surgery, Emergency service
Introduction
The World Health Organization declared COVID-19 a global pandemic on the 11 March 2020.1 The zoonotic disease was first detected in Wuhan, China, in December 2019 with substantial person-to-person transmission rapidly spreading worldwide, causing major public health and governance concerns. As of 4 June 2020, COVID-19 confirmed cases were 6,602,996 worldwide with 388,500 deaths.2
After the initial detection in China, Italy was first hit in Europe and the subsequent impact has been unprecedented.3,4 Countries have been strongly advised to implement a containment strategy alongside accelerating efforts to control the disease and these have been in the form of a national lockdown. With cases rapidly increasing in the UK in March 2020, the government took emergency measures on disease prevention and imposed a national lockdown on the 23 March 2020, causing a sharp shock to the British economy and social norms. This was deemed the safest action in view of the absence of an established treatment or vaccine and very little data on the pathophysiology and course of COVID-19.
The pandemic has caused a surge in healthcare demands and has commanded significant restructuring of the general surgical department involving cancellation of non-urgent procedures, centralisation of colorectal cancer procedures and conversion of outpatient clinics to telephone clinics. The need to care for patients with acute surgical presentations continues, however.4
The primary aim of this study was to identify the impact of the COVID-19 lockdown on the number of patients attending the surgical assessment unit with general surgery emergencies. The secondary aim was to assess the severity of their presentation before and after lockdown implementation. Our aim was to compare two cohorts, one attending before lockdown (group 1) and the second attending during lockdown (group 2).
We hypothesised that there would be fewer patients in the group 2 cohort, with a delayed presentation to hospital (translating to a longer duration of symptoms prior to presentation and worsened surrogate markers of disease severity such as inflammatory markers and patient observations). We also expected that more conservative (non-surgical) measures would be taken to treat them safely during the COVID-19 pandemic.
Material and methods
Study setting
This was a single-site retrospective review of acute general surgical referrals accepted at a 1,300 hospital bed level one trauma centre in South West London, a site which provides cover for a patient population of approximately 2.6 million.5 We compared two cohorts of patients attending inclusive of the period 30 March to 12 April 2019 (group 1) and those attending between 30 March and 12 April 2020 (patients accepted during a period of national lockdown, group 2).
Referrals were made to the general surgical registrar either directly from the community by an allied health professional or via referral from accident and emergency following initial triage and assessment by an emergency department doctor. All patients were 18 years of age or above. Existing inpatients under a separate clinical speciality referred for a general surgical opinion but without formal admission under the general surgical team were excluded.
The general surgical team also attend all trauma calls with significant bleeding (a ‘code red’) and penetrating or blunt abdominal trauma. Patients with urological or gynaecological complaints and head or chest trauma are not routinely reviewed or admitted by the general surgical team. All ‘on-call’ general surgery patients are reviewed either in the emergency department or the surgical assessment unit.
The referrals made during the timeframes set out above were retrospectively collected using on-call general surgery handover lists (updated daily by the on-call surgical registrar). The data points were collected using online patient records via the hospital electronic patient record and the picture archiving and communication system. Data collection and analysis was performed by authors RP, AJH and KD.
The demographic details collected for each patient were age and sex. The severity of presentation was assessed using clinical parameters which included presenting complaint, duration of symptoms before presentation, National Early Warning Score (NEWS)2 on admission,6 and inflammatory markers white blood cell count (WBC), C-reactive protein (CRP) and lymphocyte count.
Further data points were ultrasound, computed tomography (CT) of the abdomen and pelvis, CT diagnosis including evidence of hollow visceral perforation, overall diagnosis, conservative or surgical management, treatment details, antibiotic administration (oral and/or intravenous) and duration of stay.
Data analysis
The unpaired t-test or Mann–Whitney U test was performed to compare continuous variables. The two-tailed Fisher’s exact test was used to compare categorical variables. Data was collected using an Excel spreadsheet and statistics were performed with Stats Direct software.
Results
There were 151 patients seen by the general surgical team pre-lockdown (group 1) and 75 seen during lockdown (group 2), which equates to a 50.3% reduction. There was no significant difference in age (p = 0.82) or sex (p = 0.38) between the two groups (Table 1).
Table 1.
Demographics for patients in each group
| Group 1 | Group 2 | |
|---|---|---|
| Patients (n) | 151 | 75 |
| Mean age (years) | 50 | 49 |
| Median (IQR) | 47 (34–67) | 47 (32–63) |
| Sex, n (%): | ||
| Male | 73 (48) | 41 (55) |
| Female | 78 (52) | 34 (45) |
| Computed tomography, n (%) | 65 (43) | 33 (44) |
| Ultrasound, n (%) | 24 (16) | 6 (8) |
IQR, interquartile range.
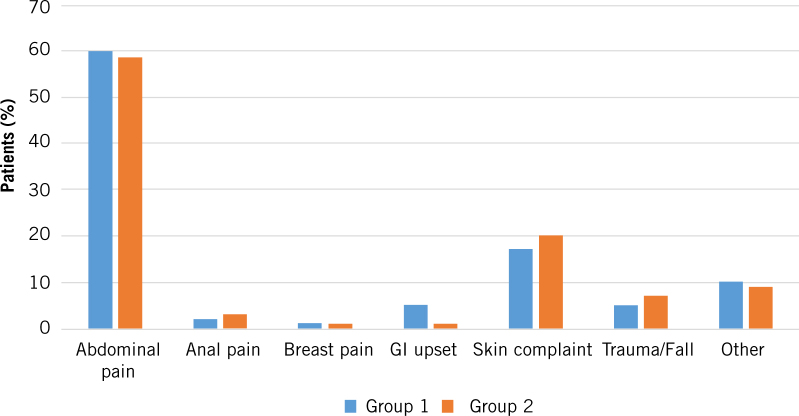
The number of days with symptoms prior to presentation was significantly shorter in group 1 compared with group 2 (p = 0.04; Table 2). Although there was no statistical significance between group 1 and 2 for NEWS2 on admission, more patients in group 2 were admitted with a NEWS2 of 3 or greater (18.9% vs 6.0%) (Fig 1). No patients in group 1 presented with a NEWS2 of greater than 6, while a total of five presented with NEWS2 ranging between 7 and 12 in group 2 (8.0%). There was no significant difference in the WBC, Lymphocytes and CRP on admission between the two groups of patients (Table 2).
Table 2.
Length of symptoms prior to admission and salient blood tests on admission for the two groups
| Feature on admission | Group 1 mean (median; IQR) |
Group 2 mean (median; IQR) |
2-sided p-value |
|---|---|---|---|
| Length of symptoms | 3 (1.5; 1–3) | 4 (2); 1 – 5) | 0.04 |
| NEWS2 | 1 (1; 1 – 1) | 1.5 (1; 0–2) | 0.15 |
| WBC | 10.8 (10; 7.7–12.8) | 10 (9.6; 7.3–12.8) | 0.72 |
| Lymphocytes | 1.6 (1.6; 1–2.2) | 1.8 (1.6; 0.9–2.2) | 0.61 |
| CRP | 48 (19; 5–64) | 53 (18.5; 4.9–53) | 0.59 |
CRP, C-reactive protein; IQR, interquartile range; NEWS2, National Early Warning Score; WBC, white blood cell count.
Figure 1.
The National Early Warning Score 2 for group 1 (mean 1, median 1, interquartile range 1–1) and group 2 (mean 1.5, median 1, interquartile range 0–2) presented as a box and whisker plot
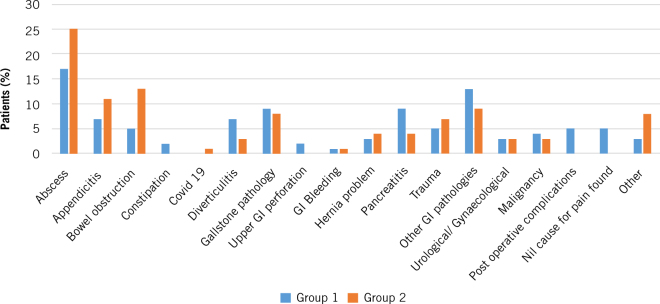
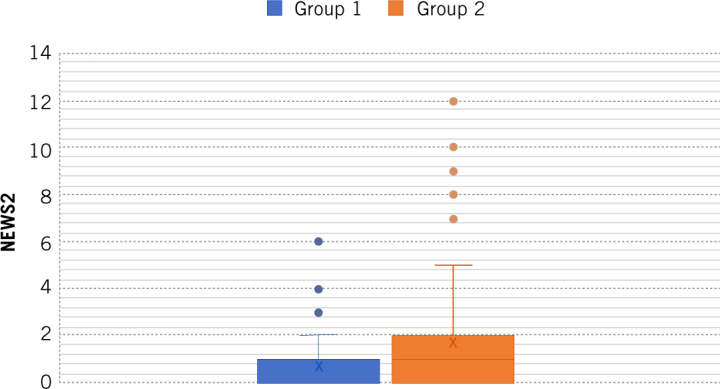
The presenting complaint and diagnoses are outlined in Figures 2 and 3. The primary presenting complaint was abdominal pain (60% of group 1 vs 59% of group 2). Other common surgical presentations remained similar between the two groups, as did the incidence of abdominoperineal trauma. Pre-lockdown there were eight cases where there was no cause of abdominal pain identified; there were no such cases in group 2. The percentage of patients with bowel obstruction increased from 5% in group 1 to 13% in group 2 (Fig 3).
Figure 2.
The percentage of patients with each type of presenting complaint in each group
Figure 3.
The percentage of patients with each type of diagnosis in each group
There was no significant difference in the proportion of patients undergoing CT (p = 0.12) or ultrasound (p = 0.09; Table 1) nor any significant difference in the proportion of patients diagnosed with a perforation on CT (3, 1%, in group 1 vs 6, 4%, in group 2; p = 0.92).
There were significantly fewer patients admitted during lockdown compared with pre-lockdown (66% of patients in group 1 compared with 48% of patients in group 2; p = 0.01; Table 3). Length of stay was significantly shorter during lockdown compared with pre-lockdown (p = 0.04; Table 3).
Table 3.
The features of admission for the two groups
| Feature | Group 1 | Group 2 |
|---|---|---|
| Overnight admission, n (%) | 99 (66) | 36 (48) |
| Length of admission for all patients | ||
| Mean (days) | 3 | 2 |
| Median (IQR) | 2 (0–4) | 0 (0–3) |
| Length of admission for patients who had any overnight stay | ||
| Mean (days) | 5 | 4 |
| Median (IQR) | 3 (2–5) | 3 (1–6) |
| Treatment, n (%): | ||
| Conservative | 113 (75) | 54 (72) |
| Surgical | 38 (25) | 20 (27) |
| Self-discharged | 0 | 1 |
| Mainstay of treatment, n (%): | ||
| Conservative | ||
| Antibiotics | 35 | 19 |
| Symptomatic relief (eg analgesia, antiemetics, PPI) | 51 | 20 |
| Medical management | 0 | 1 (infliximab) |
| Supportive care (transfusion, cardiovascular support) | 18 | 3 |
| Drip and suck ± gastrografin | 4 | 4 |
| Interventional | 1 | 2 |
| Palliative | 0 | 5 |
| Surgical | ||
| Appendicectomy | 8 (laparoscopic) | 3 (open) |
| Incision and drainage or wound debridement | 14 | 13 (6 LA) |
| Hernia repair | 2 (open) | 1 (open) |
| Defunctioning loop colostomy | 1 (laparoscopic) | 1 (trephine) |
| Laparotomy | 5 | 2 |
| Othera | 4 | 0 |
| Antibiotics | 66 (44%) (41 IV) | 50 (67%) (18 IV) |
a In group 1: 1 diagnostic laparoscopy and drainage of tubo-ovarian abscess, 1 rectal prolapse repair, 1 EUA and removal of foreign body and 1 EUA with anal dilation.
EUA, examination under anaesthetic; IQR, interquartile range; IV, intravenous; LA, local anaesthesia, PPI, proton pump inhibitor.
There was no significant difference in the proportion of patients undergoing surgical treatment in each group (either in all patients, p = 0.65, or in just those patients admitted, p = 0.84; Table 3). More patients received antibiotics in group 2 (67%) compared with group 1 (44%; p = 0.001; Table 3). In group 2, one of five patients treated conservatively for appendicitis and one of three patients treated conservatively for cholecystitis were readmitted (both were still treated conservatively). Of those undergoing surgery, 2 patients of 20 were readmitted (1 wound infection post open appendicectomy and 1 perianal pain following incision and drainage of a perianal abscess).
There were five patients in each group who died within 14 days of presentation (3% in group 1 and 7% in group 2).
Discussion
This study has shown that fewer patients were seen and significantly fewer patients admitted during lockdown compared with pre-lockdown, and the length of stay was also significantly reduced. There was also a delay in presentation to hospital and an increase in the proportion of patients receiving antibiotics. These findings are in keeping with our hypotheses.
The COVID-19 pandemic first hit the UK in January 2020 and, since then, cases have risen rapidly requiring unprecedented changes to surgical care and rapid restructuration of the services provided for surgical patients. The NHS took adaptive measures at a speed never seen before to deal with this 21st-century crisis. Its primary aim was to increase capacity for the influx of COVID-19 patients. Data from Italy and China were used to draw up new national guidelines for the delivery of safe surgical care.4
Within the general surgery department, every aspect of the patient pathway from outpatient clinic referrals to performing curative cancer surgery has been modified to minimise the spread of disease. Outpatient clinics have dramatically decreased to minimise the risk of cross-infection of COVID-19 and new referrals, including suspected gastrointestinal cancer referrals, which have been triaged via telephone clinics straight to the most appropriate and available diagnostic tests.6 Endoscopic procedures have been limited due to potential aerosolisation of digestive tract fluids; viral RNA has been detected in saliva and stools, suggesting an alternative oral–faecal route of transmission.7–9
Elective non-cancerous surgery has been cancelled, first to reallocate staff, particularly anaesthetists, to help with the COVID-19 emergency and second to free up theatres with invaluable ventilators for the sickest affected patients. Colorectal cancer patients are now categorised on their clinic urgency using a proposed system of prioritisation for cancer patients requiring surgery outlined by NHS England. These cases are now to be performed at ‘clean’, COVID-19-free local cancer hubs.9,10 Emergency general surgery is an essential service that continues to run at full capacity and is the focus of this study.
First, looking at the number of patients reviewed by general surgery, the number of patients with general surgical complaints decreased by 50.3% from 151 (group 1) to 75 (group 2). Over the course of lockdown, patients have evidently avoided visiting the hospital in fear of contracting COVID-19 and of not wanting to ‘overburden’ an already stretched service. With the UK government emphasising that ‘the single most important action you can take is to stay at home in order to protect the NHS and save lives’ may have been misleading to the general public to think that they may not leave their homes at any cost and put greater pressure on the already overstretched NHS.11 It is likely that many have feared becoming ill and have suffered with symptoms of life-threatening illnesses such as myocardial infarctions or cerebrovascular accidents at home.
Hospital cases of COVID-19 were rising exponentially in March, leading up to the expected ‘peak’ of the disease on the Easter weekend (10–12 April 2020), creating a hotspot for viral transmission. Symptoms such as abdominal pain must have been managed at home and general practitioners have played an important role here in attempting to manage patients in the community and treating acute conditions such as acute cholecystitis with antibiotics and regular telephone reviews. The NHS helpline 111 has also provided advice for patients at home. On review of all emergency presentations, the number of accident and emergency attendances and emergency admissions in the UK have dropped by 29.4% and 23.0%, respectively, in March 2020 compared with March 2019.12
Second, we expected patients to present with a delayed presentation during the COVID-19 crisis and potentially more acutely unwell. Patients in group 2, as anticipated, waited significantly longer than group 1 to present to the hospital with their ‘emergency’ symptoms (p = 0.04). Again, reasons for a delayed presentation could be as aforementioned, avoiding COVID-19 hotspots and a fever, considered a cardinal sign of COVID-19, is also a sign of acute inflammatory surgical conditions such as appendicitis, acute cholecystitis, diverticulitis and pancreatitis. Clear guidance has been given by the government that if a person is found to have a fever they should self-isolate.13 The confusion of which condition – viral or acute surgical – the fever is attributed to could easily lead to a delay in presentation.
Although a small but significant delay in presentation was seen, the patients were not more ‘unwell’ as measured by NEWS2 and inflammatory markers. However, as illustrated in Figure 1, there were more patients in group 2 admitted with a NEWS2 of 2 or greater and no patients in group 1 presented with a NEWS2 of greater than 6, while a total of five presented with NEWS2 ranging between 7 and 12 in group 2. The mortality rate in group 2 was twice as high as in group 1 (7% in group 2 and 3% in group 1).
Making the decision to perform emergency surgery in this current environment is a significant one requiring considerable planning and senior involvement. Each patient is handled as COVID-19 positive unless proven otherwise and should have pulmonary imaging prior to their emergency surgery.14 Guidelines for the management of appendicitis and acute cholecystitis, both traditionally treated surgically, have radically changed. Laparoscopic gastrointestinal tract surgery in a patient with COVID-19 is considered a higher risk due to the potential aerosolisation of the SARS-CoV-2 virus, with the CO2 circulation within the abdominal cavity increasing dissemination of aerosols and therefore facilitates viral spread.4 The majority of patients presenting with appendicitis in group 2 were treated with antibiotics (62.5%). The remaining patients admitted who were not responding to intravenous antibiotics and demonstrating signs of perforated appendicitis were treated surgically with an open procedure as per national guidelines.14
The literature states that the recurrence of uncomplicated appendicitis can be up to 27% when treated conservatively. However, treatment with antibiotics may be the safest option during these unprecedented times.15,16 Likewise, all patients presenting with acute cholecystitis during the lockdown period (group 2) were treated with antibiotics deviating from best practice guidelines of a laparoscopic cholecystectomy within one week of diagnosis.17 In practice, patients admitted with acute cholecystitis pre-lockdown (group 1) were discharged home and booked on to a semi-elective list for a laparoscopic cholecystectomy within 10 days of initial presentation.
There were significantly fewer patients admitted under the general surgical team during lockdown compared with pre-lockdown (66% of patients compared with 48% of patients; p = 0.01). Patients who were symptomatic but deemed clinically stable by their reviewing senior clinician were discharged home with a form of treatment such as antibiotics and clear safety-netting advice. It was considered safer to discharge these carefully reviewed patients to protect them and not run the risk of contracting the virus on admission to surgical wards for treatment that they could otherwise receive at home. This is also reflected as a significantly reduced length of stay in group 2 (p = 0.04).
This is a short time interval representative of the early phase of the lockdown period. As peoples’ attitudes and behaviours adapt and the prolonged effects of a reduction of services and delays to essential surgery are seen, the pattern and severity of presentations are also likely to change.
Limitations
Data collected are dependent on accurate documentation and certain data points such as length of symptoms are wholly dependent on recollection and may be subject to recall bias. Management of the patients including investigations such as CT and treatment plans may be subjective to the reviewing surgeon.
Conclusion
The rapid diffusion of the novel coronavirus has threatened healthcare systems globally. Although the focus will be on treating the COVID-19 pandemic, patients will continue to need emergency surgical care. This study has shown that the national lockdown has reduced the number of patients using emergency general surgery services and patients have attended with a delayed presentation. Management of general surgery emergencies has, however, radically changed to a more conservative approach to minimise the risk of cross-infection of patients and to free up capacity for patients with COVID-19.
Further work is required to identify the long-term outcomes of patients comparing those treated conservatively during the COVID-19 outbreak with those managed surgically. Patients discharged with treatments could be followed up for readmissions and morbidity. Studying this population would help with risk stratification and identifying the cohort of patients suitable for telephone follow-up.
References
- 1.World Health Organization Director-General’s opening remarks at the media briefing on COVID-19 – 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (cited June 2020).
- 2.Worldometer Coronavirus cases https://www.worldometers.info/coronavirus/ (cited June 2020).
- 3.Spinelli A, Pellion G. COVID-19 pandemic: perspectives on an unfolding crisis. Br J Surg 2020; : 785–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Di Saverio S, Pata F, Gallo G, et al. Coronavirus pandemic and colorectal surgery: practical advice based on the Italian experience. Colorectal Dis 2020. March 31 [Epub ahead of print.] [DOI] [PubMed] [Google Scholar]
- 5.St George’s University Hospitals NHS Foundation Trust. Major trauma centre. https://www.stgeorges.nhs.uk/service/emergency-department/major-trauma-centre/ (cited June 2020).
- 6.Royal College of Physicians National Early Warning Score (NEWS) 2. https://www.rcplondon.ac.uk/projects/outputs/national-early-warning-score-news-2 (cited June 2020).
- 7.To KK-W, Tsang OT-Y, Chik-Yan Yip C et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis 2020. February 12; ciaa149 DOI: 10.1093/cid/ciaa149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Young BE, Ong SWX, Kalimuddin S et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA 2020; : 1488–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang J, Wang S, Xue Y. Fecal specimen diagnosis 2019 novel coronavirus-infected pneumonia. J Med Virol 2020; : 680–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Health Service Clinical Guide for the Management of Noncoronavirus Patients Requiring Acute Treatment: Cancer. Specialty guides for patient management during the coronavirus pandemic. https://www.england.nhs.uk/coronavirus/secondary-care/other-resources/specialty-guides/#cancer (cited June 2020).
- 11.Coronavirus: stay at home, protect the NHS, save lives. gov.uk https://www.gov.uk/government/publications/coronavirus-covid-19-information-leaflet/coronavirus-stay-at-home-protect-the-nhs-save-lives-web-version (cited June 2020).
- 12.NHS England A&E Attendances and Emergency Admissions. https://www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/ (cited June 2020).
- 13.Public Health England Coronavirus (COVID-19): What is social distancing? https://publichealthmatters.blog.gov.uk/2020/03/04/coronavirus-covid-19-what-is-social-distancing/ (cited June 2020).
- 14.Royal College of Surgeons of England Updated Intercollegiate General Surgery Guidance on COVID-19. Guidance for surgeons working during the pandemic. https://www.rcseng.ac.uk/coronavirus/joint-guidance-for-surgeons-v2/ (cited June 2020).
- 15.Salminen P, Paajanen H, Rautio T et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA 2015; : 2340–2348. [DOI] [PubMed] [Google Scholar]
- 16.Sippola S, Haijanen J, Viinikainen L et al. Quality of life and patient satisfaction at 7-year follow-up of antibiotic therapy vs appendectomy for uncomplicated acute appendicitis: a secondary analysis of a randomized clinical trial. JAMA Surg 2020. February 19; e196028 . [Epub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Institute for Health and Care Excellence Gallstone Disease: Diagnosis and Management. Clinical Guideline CG188 London: NICE; 2014. [Google Scholar]