Abstract
Background
A burn wound is a complex and evolving injury, with both local and systemic consequences. Burn treatments include a variety of dressings, as well as newer strategies, such as negative pressure wound therapy (NPWT), which, by means of a suction force that drains excess fluids from the burn, tries to promote the wound healing process and minimise progression of the burn wound.
Objectives
To assess the effectiveness of NPWT for people with partial‐thickness burns.
Search methods
We searched the Cochrane Wounds Group Specialised Register (searched 04 September 2014); The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2014, Issue 8).
Selection criteria
All randomised controlled trials (RCTs) and controlled clinical trials (CCTs) that evaluated the safety and effectiveness of NPWT for partial‐thickness burns.
Data collection and analysis
Two review authors used standardised forms, and extracted the data independently. We assessed each trial for risk of bias, and resolved differences by discussion.
Main results
One RCT, that was an interim report, satisfied the inclusion criteria. We undertook a narrative synthesis of results, as the absence of data and poor reporting precluded us from carrying out any formal statistical analysis. The trial was at high risk of bias.
Authors' conclusions
There was not enough evidence available to permit any conclusions to be drawn regarding the use of NPWT for treatment of partial‐thickness burn wounds.
Keywords: Humans, Negative‐Pressure Wound Therapy, Wound Healing, Burns, Burns/pathology, Burns/therapy, Occlusive Dressings, Randomized Controlled Trials as Topic, Suction, Suction/instrumentation, Suction/methods
Plain language summary
Negative pressure wound therapy (NPWT) for treating partial‐thickness burns
Negative pressure wound therapy (NPWT) is the application of negative pressure (a vacuum) across a wound with the aim of managing the wounds and promoting healing. Alternative names for NPWT include topical negative pressure (TNP) therapy, vacuum‐assisted closure (VAC) and sealed surface wound suction. In the case of burns, NPWT is used to help the drainage of excess fluid and increase localised blood flow. It has been suggested that the action of NPWT may result in the burn being supplied with increased oxygen and nutrition which could promote healing.We could identify only one clinical trial that tried to address whether NPWT is effective in treating partial‐thickness burns, and its results have not yet been published in full. Consequently, there is a lack of trial evidence available, and we could not determine whether NPWT is effective in treating partial‐thickness burns. Much more research needs to be done in this area to find out whether NPWT is helpful.
Background
Description of the condition
Burn injuries are a considerable source of morbidity and mortality. Every year in the USA alone, approximately two million people are burned, up to 80,000 are hospitalised as a result of burns and more than 6500 people die from their injuries (Brigham 1996). A skin burn is defined as damage to the skin caused by heat or caustic chemicals. Heat causes the most immediate and obvious injury. Excessive heat causes rapid protein denaturation and cell damage, and thus initiates a complex and evolving injury, with both local and systemic (whole body) consequences ‐ the latter manifesting once the burn area is greater than 20% of the body surface area (BSA) (Sheridan 2002).
Locally, the burn wound tends to extend during the acute (first) phase of the injury as a result of microvascular changes, profound activation of white cells and platelets, and the development of oedema (build up of fluid). Many small vessels are coagulated by the application of heat, while others will thrombose (block) later and develop tissue dehydration (Boykin 1980). The systemic response to burning is characterised by interstitial oedema in distant organs, i.e. the swelling of any organ or tissue due to accumulation of excess lymph fluid (between cells), and is secondary to a combination of wound‐released mediators and hypoproteinaemia (abnormally small amounts of protein in the circulating blood plasma) (Demling 1979; Youn 1992).
Burn wounds are often classified by depth: superficial (first‐degree burn), partial‐thickness (second‐degree burn) or full‐thickness (third‐degree burn). Often, the depth of injury is diagnosed by the anatomic thickness of the skin involved (i.e. the epidermis (outermost thin layer), stratum corneum (outer layer) and the dermis (deepest layer)) and based on either clinical observation, or objective assessment, or both. Clinical evaluation often relies on features of the burn wound's appearance, such as blanching, capillary return, presence and degree of fixed capillary staining, and evaluation of retained light touch and pinprick sensation. Objective assessment tools such as laser doppler flowmetry, laser doppler imaging or indocyanine green video angiography, may be used to measure blood flow into the tissue and, therefore, depth of burn injury (Demling 2005).
First‐degree, or superficial, burns are confined exclusively to the epidermis or outer surface of the skin, and generally are not significant injuries, as they heal rapidly and spontaneously. Second‐degree, or partial‐thickness, burns involve varying amounts of the dermis. These may become deeper, and heal with variable amounts of scarring, the degree of which depends partly on the depth of the burn.
The superficial partial‐thickness burn is a sub‐category of partial‐thickness burns. This type of burn extends through the epidermis into the papillary (superficial) layer of the dermis. These wounds become erythematous, i.e. the skin reddens because the dermal tissue has become inflamed. One hallmark of the superficial partial‐thickness burn is blanching followed by rapid capillary refill when pressure is applied to the reddened area and subsequently released (Demling 2005; Johnson 2003). Thin‐walled, fluid‐filled blisters develop within minutes of the injury. As these blisters break, the exposed nerve endings transmit superficial pain, light touch and temperature, making these wounds extremely painful. The wound is moist because the characteristic waterproofing of the epidermis has been lost, allowing body fluid to leak onto the wound surface. Also, moderate oedema is usually present, due to the involvement of the dermal blood vessels in this type of injury (Demling 2005; Johnson 2003).
Deep partial‐thickness burns extend downward into the reticular (deeper) layer of the dermis and present as mixed red or waxy white. Areas of redness will continue to blanch when pressure is applied, but capillary refill may be absent, or sluggish, when pressure is released. Blisters are usually absent; however, the exposed surface of the wound is wet or moist, in a similar way to superficial partial‐thickness burns. Oedema is marked, and sensation is altered in areas of a deep partial‐thickness burn (Demling 2005; Johnson 2003).
Description of the intervention
Since the biology of wound healing has become better understood, many strategies have been developed to try to manipulate this wound healing process (Banwell 1999), and to minimise the progression of burn wounds by involving deeper tissue in the acute phase. These strategies range from use of a variety of skin substitutes and dressings, such as polyurethane films and hydrocolloids (Wasiak 2005), to the use of more complex and experimental techniques, such as hyperbaric oxygen therapy (Villanueva 2004), application of growth factors and cytokine biology (Atiyeh 2005). One way of manipulating the wound environment with a view to promoting healing is to apply negative pressure wound therapy (NPWT) across the wound surface via a dressing (Ubbink 2008). There are a number of terms to describe the treatment of a wound with NPWT including: subatmospheric pressure, vacuum‐sealing technique, sealed surface wound suction, vacuum assisted closure (VAC), negative pressure therapy or dressing, foam suction dressing, vacuum compression, vacuum pack technique, negative pressure dressing and foam suction dressing (Banwell 2004a). For the purposes of this review, all variations of this intervention will be referred to as NPWT. In NPWT a dressing is applied to a burn and a negative pressure (vacuum) applied though it, with tissue fluid being collected into a canister. NPWT was developed in the 1990s, and its uptake by the healthcare systems of developed countries has been dramatic. A US Department of Health report estimated that Medicare payments for NPWT pumps and associated equipment increased between 2001 and 2007 from USD 24 million to USD 164 million (an increase of almost 600%) (Department of Health and Human Services 2009).
How the intervention might work
Negative pressure is purported to induce an interstitial gradient shift which can cause a reduction in oedema, and a secondary increase in dermal perfusion, thus aiding in the removal of blood or serous fluid (Banwell 2004a). It is also postulated that the ability of NPWT to produce a mechanical stress or force that has a direct effect in cellular activity, and, in particular, the development of new blood vessels, may also contribute to a decrease in burn wound progression. The maintenance of a moist environment that provides optimal conditions for epithelialisation and the prevention of tissue desiccation is also potentially advantageous (Banwell 1999; Banwell 2004a; Pham 2003).
Why it is important to do this review
NPWT is an expensive, yet widely used, health technology. The US Food and Drug Administration approved the use of at least one NPWT system for use on partial‐thickness burns in 2003, and subsequently its use in burn wound management has been described by a number of clinicians (Kamolz 2004; Moisidis 2004; Schrank 2004). Yet it is unclear what evidence of the effectiveness of NPWT for treatment of partial‐thickness burns is available to guide both clinical and policy decision making. We plan to summarise the evidence to determine whether NPWT is safe, effective and beneficial to those patients with partial‐thickness burns.
Objectives
To compare the effects of NPWT with standard care or other adjuvant therapies in the healing of partial‐thickness burns in adults.
Methods
Criteria for considering studies for this review
Types of studies
We included all randomised controlled trials (RCTs) and controlled clinical trials (CCTs) that evaluated the effectiveness of NPWT for partial‐thickness burns, irrespective of publication status or language.
Types of participants
We included studies recruiting adults aged 18 years, or over, with a partial‐thickness burn, the severity of which could be determined either by clinical evaluation or objective assessment, or both. Clinical evaluation relied on burn wound appearance, blanching, capillary return, presence and degree of fixed capillary staining and evaluation of retained light touch and pinprick sensation. Objective assessment involved the measurement of tissue perfusion by methods such as laser doppler flowmetry, laser doppler imaging or indocyanine green video angiography.
Types of interventions
Studies were eligible if they compared NPWT with standard burn wound therapies in the treatment of partial‐thickness burns. Studies involving any mode of delivery of NPWT were eligible, including commercially available devices (such as VAC Pump, KCI Texas, USA), wall suction or surgical drainage bottles, as well as negative pressure cycles that vary in degree, application (including continuous and/or intermittent pressure cycles) and duration.
Types of outcome measures
Studies were eligible for inclusion if they reported any of the following outcome measures:
Primary outcomes
time to complete healing;
rate of change in wound area;
proportion of wound completely healed within the trial period.
Secondary outcomes
incidence of wound infection;
adverse events;
measures of satisfaction or patient preference;
quality of life.
Search methods for identification of studies
Electronic searches
The search methods section of the third update of this review can be found in Appendix 1
For the fourth update we conducted a streamlined search:
The Cochrane Wounds Group Specialised Register, comprising references identified from comprehensive electronic database searches, handsearches of relevant journals and abstract books of conference proceedings (searched 04 September 2014);
The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2014, Issue 8)
The following search strategy was used in The Cochrane Central Register of Controlled Trials (CENTRAL): #1 MeSH descriptor Negative‐Pressure Wound Therapy explode all trees #2 MeSH descriptor Suction explode all trees #3 MeSH descriptor Vacuum explode all trees #4 ("negative pressure" or negative‐pressure or TNP):ti,ab,kw #5 (sub‐atmospheric or subatmospheric):ti,ab,kw #6 ((seal* NEXT surface*) or (seal* NEXT aspirat*)):ti,ab,kw #7 (wound NEAR/3 suction*):ti,ab,kw #8 (wound NEAR/3 drainage):ti,ab,kw #9 ((foam NEXT suction) or (suction NEXT dressing*)):ti,ab,kw #10 ((vacuum NEXT therapy) or (vacuum NEXT dressing*) or (vacuum NEXT seal*) or (vacuum NEXT assist*) or (vacuum NEAR closure) or (vacuum NEXT compression) or (vacuum NEXT pack*) or (vacuum NEXT drainage) or VAC):ti,ab,kw #11 ("vacuum assisted closure technique" or VAC):ti,ab,kw #12 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11) #13 MeSH descriptor Burns explode all trees #14 (burn or burns or burned):ti,ab,kw #15 (#13 OR #14) #16(#12 AND #15)
The search strategies for Ovid MEDLINE, Ovid EMBASE and Ovid CINAHL can be found in Appendix 2, Appendix 3 and Appendix 4, respectively. The Ovid MEDLINE search was combined with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximizing version (2008 revision); Ovid format (Lefebvre 2011). The EMBASE and CINAHL searches were combined with the trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN) (SIGN 2012). We did not apply language restrictions.
Searching other resources
For the original review we contacted authors of relevant studies to request details of unpublished or ongoing investigations and checked citations of retrieved studies for further trials. This process was not repeated for the updates. No new studies were identified for this update, so there were no additional reference lists to check.
Data collection and analysis
Selection of studies
Two review authors independently scanned records retrieved by the searches to exclude obviously irrelevant studies, and to identify trials that met the inclusion criteria. They retrieved, and independently reviewed, full text articles for the purpose of applying inclusion criteria. In all instances, differences of opinion were resolved by discussion.
Data extraction and management
The review authors extracted data independently from the studies using standardised forms. Data extracted included country of origin, health care setting, study design, baseline characteristics of participants by treatment group, inclusion and exclusion criteria, details of intervention and comparison, outcome measures and results. When missing or incomplete data were encountered, we contacted study authors with a request for information. All differences of opinion were resolved by discussion among the review authors.
Assessment of risk of bias in included studies
We undertook a quality assessment considering the adequacy of the randomisation and allocation concealment process, whether intention to treat (ITT) analysis was performed, the level of blinding and whether the follow‐up was complete. For this update the Cochrane Collaboration tool for assessing risk of bias was applied to included studies (Higgins 2011). This tool addresses six specific domains; namely sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting and other issues (e.g. extreme baseline imbalance) (see Appendix 5 for the criteria on which risk of bias judgements were made). A risk of bias table was completed for the eligible study. The review authors independently assessed the studies and any disagreements were resolved by discussion.
Assessment of heterogeneity
We planned to consider both clinical and statistical heterogeneity. Wherever appropriate, we planned to pool data using meta‐analysis (conducted using RevMan 5.1 (RevMan 2011)), that is where studies appeared similar in terms of wound type, intervention type, duration and outcome type. We planned to assess statistical heterogeneity using the chi² test (a significance level of P less than 0.1 was considered to indicate heterogeneity) and the I² estimate (Higgins 2003). The I² estimate examines the percentage of total variation across studies due to heterogeneity rather than to chance. Values of I² over 50 per cent indicate a high level of heterogeneity. In the absence of clinical heterogeneity and in the presence of statistical heterogeneity (I² over 50 per cent), we anticipated using a random‐effects model, however, we would not pool studies when heterogeneity was very high (I² over 75 per cent). Where there was no clinical or statistical heterogeneity we envisaged using a fixed‐effect model.
Data synthesis
Where possible, we planned to present the outcome results for each trial with 95% confidence intervals (CI). We planned to report estimates for dichotomous outcomes (e.g. burns healed during a particular time period) as risk ratios (RR). We decided to use the RR rather than odds ratio (OR), since ORs (when interpreted as RR) can give an inflated impression of the effect size when event rates are high, as is the case for many trials reporting healing (Deeks 2002). We planned to report outcomes relating to continuous data (e.g. percentage change in ulcer area) as mean differences (MD) and overall effect size (with 95% CI). Where a study reported time‐to‐healing data (the probability of healing over a consecutive time period) we planned to report and plot these data (where possible) using hazard ratio estimates. If studies reported time‐to‐event data (e.g. time to healing), did not report hazard ratios, or reported these data incorrectly as a continuous variable, then, where feasible, we planned to estimate this using other reported outcomes, such as the numbers of events, through the application of available statistical methods (Tierney 2007).
Where statistical data synthesis was not possible we planned to present a narrative synthesis.
Results
Description of studies
The searches for this fourth review retrieved seven references, none of which met the inclusion criteria for this review. We did not obtain any citations as full text. The searches for the third review update retrieved 27 references, none of which met the inclusion criteria.
The original searches for this review identified 60 references, of these 10 potentially relevant articles obtained as full text, with nine being excluded because they were either case reports, case series or narrative reviews (Adamkova 2005; Banwell 2004b; Haslik 2004; Moisidis 2004; Molnar 2004b; Nugent 2005; Schintler 2005), or did not address primary outcome measures (Kamolz 2004; Schrank 2004) (see Characteristics of excluded studies). We did not find additional studies when we examined citations of retrieved studies.
One study was included which formed the basis of this review (Molnar 2004a) ‐ this is a conference abstract reporting interim data. At the time of the original review we contacted the authors of this abstract, who stated that the abstract results were preliminary data that would be publishable in the foreseeable future (personal communication), as well as providing further details of the study population. In 2014, the author was contacted again, but, as yet, no further information has been received.
The included abstract (Molnar 2004a) reported that participants with bilateral thermal hand burns (treated for less than 24 hours post injury) had one hand randomised to receive NPWT (125 mmHg pressure) applied for 48 hours, whilst the other hand was treated with silver sulphadiazine (SSD). The study used a commercially available device (VAC Pump, KCI Inc, Texas, United States) to apply the negative pressure. All participants served as their own control. The trial reported outcome data at day 30 of a 60‐day study period. Outcome measures assessed were reported as: rate of burn healing by use of a Sigma Scan (Systat Software Inc, California, United States), volume of hand as determined by fluid displacement, range of motion, grip and pinch strength. The abstract did not clearly state how many people had been randomised, but reported that it presented results for the first 23 participants. Additional information supplied via personal communication with the author noted that the mean age of these 23 participants was 46 years and the total burn surface area (TBSA) ranged from five per cent to 40 per cent, with mean TBSA at 16 per cent.
Risk of bias in included studies
A full study report has not been identified, therefore the risk of bias assessment for Molnar 2004a was based on the conference abstract alone (see Characteristics of included studies). The study is described as "prospective, randomised, controlled, blinded, multi‐center and web‐based", however, the exact method of sequence generation was not specified in the abstract, and allocation concealment was also not reported. Due to the nature of NPWT, it is unlikely that the patients or treatment provider could have been blinded to the intervention. Molnar 2004a reported that, at strategic time points, a blinded principal investigator was used to determine the area of the burns to determine their rate of healing (personal communication with the author). Since the study was an interim report, judging risk of bias for 'incomplete outcome data' was not possible; no attrition was reported at this point in the trial. Burn wound progression and hand function were pre‐specified as outcomes in the abstract, both of which were reported (see risk of bias Figure 1).
1.
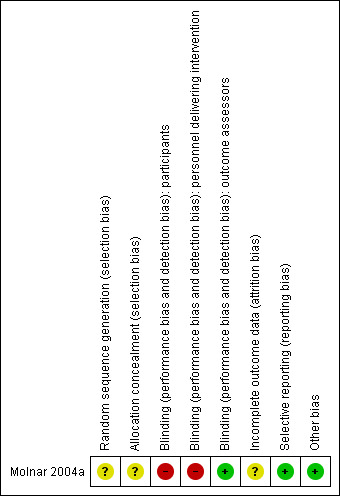
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Effects of interventions
Due to missing data, poor reporting or both, a formal statistical analysis was not possible. A series of outcome measures such as the reduction in hand oedema, the volume of fluid displaced, and grip and pinch strength were reported by Molnar 2004a, although these were not considered by our review. As a result we focused on the following outcome measures:
Primary outcomes
Time to complete healing
No data were reported for this outcome.
Rate of change in wound area
Molnar 2004a reported a significant difference in burn size at day three (P < 0.09) and day five (P < 0.04), but not at day 14. From the abstract it is not clear which group was favoured in the day 3 and 5 analysis. No data were presented beyond P values.
Proportion of wounds completely healed within the trial period
No data were reported for this outcome.
Secondary outcomes
Incidence of wound infection
No data were reported for this outcome.
Adverse events
Molnar 2004a reported that there were no discernable complications with NPWT treatment of the acute burns.
Measures of satisfaction or patient preference
No data were reported for this outcome.
Quality of life measures
No data were reported for this outcome.
Discussion
This systematic review summarises the best available evidence relating to safety and effectiveness of NPWT in adults with partial‐thickness burns. After an extensive search of the literature, only one RCT was found, which was an interim report judged to be at high risk of bias.
There is currently an absence of evidence regarding the use of NPWT for burn wounds, despite the theoretical considerations that may support the concept. Our results highlighted the need for high‐level, good‐quality research into the safety and effectiveness of NPWT in adults with partial‐thickness burns. The trial by Molnar 2004a was methodologically weak and poorly reported. There was no description of the randomisation process, and no mention of the degree of comparability of burn injury to both hands at baseline. Other weaknesses included: the absence of reporting on clinically relevant outcomes, such as rate of healing, time to complete healing, rate of change in wound area, and proportion of the wound completely healed within the trial period; lack of clarity regarding the definition and reduction of oedema formation; and the ongoing use of SSD as a comparator, as it is not only known to be toxic to regenerating epithelial cells (Wasiak 2005), but may place patients at increased risk of developing complications such as neutropenia (a lack of white blood cells), erythema multiforme (a rash usually resulting from a drug reaction), crystals in the urine and methaemoglobinaemia (oxidation of more than 1% of the haemoglobin in blood to the ferric state) (Subrahmanyam 1998).
The small sample size and preliminary analysis of only 23 patients precludes the drawing of any conclusions regarding the nature or frequency of adverse events.
Authors' conclusions
Implications for practice.
No data from completed RCTs on NPWT for partial‐thickness burn injury are available, which means that conclusions cannot be drawn on the merits ‐ or otherwise ‐ of this treatment.
Implications for research.
This systematic review highlights the need for good quality research into the safety and effectiveness of NPWT in partial‐thickness burns. Suggestions adapted from Ubbink 2008 indicate that future research needs include:
Well‐designed, adequately‐powered, multi‐centred RCTs to evaluate the contribution of NPWT in the treatment of partial thickness burns.
RCTs of NPWT in which the comparison intervention represents current standard practice for partial‐thickness burns based on the best available evidence.
RCTs to evaluate the effects of NPWT on healing times, cost, quality of life, pain and comfort, and to determine whether there is an optimum NPWT regime for partial‐thickness burns.
Economic evaluations to determine whether the costs of NPWT justify its potential benefits in those with burn injury.
What's new
| Date | Event | Description |
|---|---|---|
| 4 September 2014 | New search has been performed | New search, no new studies identified. |
| 4 September 2014 | New citation required but conclusions have not changed | New author team, conclusions remain unchanged. |
History
Protocol first published: Issue 4, 2006 Review first published: Issue 3, 2007
| Date | Event | Description |
|---|---|---|
| 18 May 2012 | New search has been performed | Third update, new search, no new studies identified, risk of bias assessment added, terminology updated. |
| 18 May 2012 | New search has been performed | New author team, new search, no new studies identified, conclusions remain unchanged. |
| 15 January 2009 | New search has been performed | New searches, no new studies included, conclusions remain unchanged |
| 8 August 2008 | Amended | Converted to new review format. |
| 27 April 2007 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
The authors would like to thank Sally Bell‐Syer for her ongoing support and commitment, and acknowledge the Wounds Group Editors (Nicky Cullum, Andrea Nelson and Gill Worthy) and referees (Susanne Hempel, Tom Potokar and Durhane Wong‐Rieger) for their comments on both the protocol and review. The first update of this review was copy edited by Helena Mullineaux and Nancy Owens. This update was copy edited by Elizabeth Royle.
The authors would like to acknowledge the contribution of Jason Wasiak and Heather Cleland who drafted the protocol, undertook study selection and wrote the original version of the review (Wasiak 2007). They did not wish to be involved in the current and future updates of this review.
Appendices
Appendix 1. Search methods ‐ second update 2010
Electronic searches
For the third update we modified the previous search string and searched the following electronic databases:
Cochrane Wounds Group Specialised Register (searched 18 May 2012);
The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2012, Issue 5);
Ovid MEDLINE (2010 to May Week 2 2012);
Ovid MEDLINE (In‐Process & Other Non‐Indexed Citations 17 May 2012);
Ovid EMBASE (2010 to 2012 Week 19);
EBSCO CINAHL (2010 to 16 May 2012).
The following search strategy was used in The Cochrane Central Register of Controlled Trials (CENTRAL): #1 MeSH descriptor Negative‐Pressure Wound Therapy explode all trees #2 MeSH descriptor Suction explode all trees #3 MeSH descriptor Vacuum explode all trees #4 ("negative pressure" or negative‐pressure or TNP):ti,ab,kw #5 (sub‐atmospheric or subatmospheric):ti,ab,kw #6 ((seal* NEXT surface*) or (seal* NEXT aspirat*)):ti,ab,kw #7 (wound NEAR/3 suction*):ti,ab,kw #8 (wound NEAR/3 drainage):ti,ab,kw #9 ((foam NEXT suction) or (suction NEXT dressing*)):ti,ab,kw #10 ((vacuum NEXT therapy) or (vacuum NEXT dressing*) or (vacuum NEXT seal*) or (vacuum NEXT assist*) or (vacuum NEAR closure) or (vacuum NEXT compression) or (vacuum NEXT pack*) or (vacuum NEXT drainage) or VAC):ti,ab,kw #11 ("vacuum assisted closure technique" or VAC):ti,ab,kw #12 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11) #13 MeSH descriptor Burns explode all trees #14 (burn or burns or burned):ti,ab,kw #15 (#13 OR #14) #16(#12 AND #15)
The search strategies for Ovid MEDLINE, Ovid EMBASE and Ovid CINAHL can be found in Appendix 3, Appendix 4 and Appendix 5 respectively. The Ovid MEDLINE search was combined with the Cochrane Highly Sensitive Search Strategy for identifying randomised trials in MEDLINE: sensitivity‐ and precision‐maximizing version (2008 revision); Ovid format (Lefebvre 2009). The EMBASE and CINAHL searches were combined with the trial filters developed by the Scottish Intercollegiate Guidelines Network (SIGN) (SIGN 2010). We applied no language restrictions.
Searching other resources
For the original review we contacted authors of relevant studies to request details of unpublished or ongoing investigations and checked citations of retrieved studies for further trials. We did not repeat this exercise for the updates.
Appendix 2. Ovid MEDLINE search strategy
1 exp Suction/ 2 exp Vacuum/ 3 (negative pressure or negative‐pressure or TNP).mp. 4 (sub‐atmospheric or subatmospheric).mp. 5 ((seal$ adj surface$) or (seal$ adj aspirat$)).mp. 6 (wound adj5 suction$).mp. 7 (wound adj5 drainage).mp. 8 ((foam adj suction) or (suction adj dressing$)).mp. 9 ((vacuum adj therapy) or (vacuum adj dressing$) or (vacuum adj seal$) or (vacuum adj closure) or (vacuum adj compression) or (vacuum adj pack$) or (vacuum adj drainage) or (suction$ adj drainage)).mp. 10 or/1‐9 11 exp Burns/ 12 (burn or burns or burned).ti,ab. 13 or/11‐12
Appendix 3. Ovid EMBASE search strategy
1 exp suction drainage/ 2 exp vacuum assisted closure/ 3 (negative pressure or negative‐pressure or TNP).mp. 4 (sub‐atmospheric or subatmospheric).mp. 5 ((seal$ adj surface$) or (seal$ adj aspirat$)).mp. 6 (wound adj5 suction$).mp. 7 (wound adj5 drainage).mp. 8 ((foam adj suction) or (suction adj dressing$)).mp. 9 ((vacuum adj therapy) or (vacuum adj dressing$) or (vacuum adj seal$) or (vacuum adj closure) or (vacuum adj compression) or (vacuum adj pack$) or (vacuum adj drainage) or (suction$ adj drainage)).mp. 10 or/1‐9 11 exp Burns/ 12 (burn or burns or burned).ti,ab. 13 or/11‐12 14 10 and 13
Appendix 4. EBSCO CINAHL search strategy
1 exp Suction/ 2 exp Vacuum/ 3 (negative pressure or negative‐pressure or TNP).mp. 4 (sub‐atmospheric or subatmospheric).mp. 5 ((seal$ adj surface$) or (seal$ adj aspirat$)).mp. 6 (wound adj5 suction$).mp. 7 (wound adj5 drainage).mp. 8 ((foam adj suction) or (suction adj dressing$)).mp. 9 ((vacuum adj therapy) or (vacuum adj dressing$) or (vacuum adj seal$) or (vacuum adj closure) or (vacuum adj compression) or (vacuum adj pack$) or (vacuum adj drainage) or (suction$ adj drainage)).mp. 10 or/1‐9 11 exp Burns/ 12 (burn or burns or burned).ti,ab. 13 or/11‐12 (9111) 14 10 and 13
Appendix 5. Judgement criteria for risk of bias assessments
1. Was the allocation sequence randomly generated?
Low risk of bias
The investigators describe a random component in the sequence generation process such as: referring to a random number table; using a computer random number generator; coin tossing; shuffling cards or envelopes; throwing dice; drawing of lots.
High risk of bias
The investigators describe a non‐random component in the sequence generation process. Usually, the description would involve some systematic, non‐random approach, for example: sequence generated by odd or even date of birth; sequence generated by some rule based on date (or day) of admission; sequence generated by some rule based on hospital or clinic record number.
Unclear
Insufficient information about the sequence generation process provided to permit judgement of low or high risk of bias.
2. Was the treatment allocation adequately concealed?
Low risk of bias
Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation (including telephone, web‐based and pharmacy‐controlled randomisation); sequentially‐numbered drug containers of identical appearance; sequentially‐numbered, opaque, sealed envelopes.
High risk of bias
Participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, when allocation based on use of: an open random allocation schedule (e.g. a list of random numbers); assignment envelopes without appropriate safeguards (e.g. if envelopes unsealed, non‐opaque, or not sequentially numbered); alternation or rotation; date of birth; case record number; any other explicitly unconcealed procedure.
Unclear
Insufficient information provided to permit judgement of low or high risk of bias. This is usually the case in instances where the method of concealment is not described, or not described in sufficient detail to allow a definite judgement to be made, for example when the use of assignment envelopes is described, but it is not clear whether envelopes were sequentially numbered, opaque and sealed.
3. Blinding ‐ was knowledge of the allocated interventions adequately prevented during the study?
Low risk of bias
Any one of the following:
No blinding, but the review authors judge that the outcome and the outcome measurement are not likely to be influenced by lack of blinding.
Blinding of participants and key study personnel ensured, and unlikely that the blinding could have been broken.
Either participants or some key study personnel were not blinded, but outcome assessment was blinded and the non‐blinding of others is unlikely to introduce bias.
High risk of bias
Any one of the following:
No blinding, or incomplete blinding, and the outcome or outcome measurement is likely to be influenced by lack of blinding.
Blinding of key study participants and personnel attempted, but likely that the blinding could have been broken.
Either participants or some key study personnel were not blinded, and the non‐blinding of others is likely to introduce bias.
Unclear
Any one of the following:
Insufficient information to permit judgement of low or high risk of bias.
The study did not address this outcome.
4. Were incomplete outcome data adequately addressed?
Low risk of bias
Any one of the following:
No missing outcome data.
Reasons for missing outcome data unlikely to be related to true outcome (for survival data, censoring unlikely to be introducing bias).
Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups.
For dichotomous outcome data, the proportion of missing outcomes compared with observed event risk is not enough to have a clinically relevant impact on the intervention effect estimate.
For continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes not enough to have a clinically relevant impact on observed effect size.
Missing data have been imputed using appropriate methods.
High risk of bias
Any one of the following:
Reason for missing outcome data likely to be related to true outcome, with either imbalance in numbers or reasons for missing data across intervention groups.
For dichotomous outcome data, the proportion of missing outcomes compared with observed event risk is enough to induce clinically relevant bias in intervention effect estimate.
For continuous outcome data, plausible effect size (difference in means or standardised difference in means) among missing outcomes is enough to induce clinically relevant bias in observed effect size.
‘As‐treated’ analysis done with substantial departure of the intervention received from that assigned at randomisation.
Potentially inappropriate application of simple imputation.
Unclear
Any one of the following:
Insufficient reporting of attrition/exclusions to permit judgement of low or high risk of bias to be made (e.g. number randomised not stated, no reasons for missing data provided).
The study did not address this outcome.
5. Are reports of the study free of suggestion of selective outcome reporting?
Low risk of bias
Any of the following:
The study protocol is available and all of the study’s pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way.
The study protocol is not available, but it is clear that the published reports include all expected outcomes, including those that were pre‐specified (convincing text of this nature may be uncommon).
High risk of bias
Any one of the following:
Not all of the study’s pre‐specified primary outcomes have been reported.
One or more primary outcomes is reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not pre‐specified.
One or more reported primary outcomes were not pre‐specified (unless clear justification for their reporting is provided, such as an unexpected adverse effect).
One or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis.
The study report fails to include results for a key outcome that would be expected to have been reported for such a study.
Unclear
Insufficient information to permit judgement of low or high risk of bias to be made. It is likely that the majority of studies will fall into this category.
6. Other sources of potential bias
Low risk of bias
The study appears to be free of other sources of bias.
High risk of bias
There is at least one important risk of bias. For example, the study:
had a potential source of bias related to the specific study design used; or
has been claimed to have been fraudulent; or
had some other problem.
Unclear
There may be a risk of bias, but there is either:
insufficient information to assess whether an important risk of bias exists; or
insufficient rationale or evidence that an identified problem will introduce bias.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Molnar 2004a.
| Methods | RCT: "the study design was prospective, randomised, controlled, blinded, multi‐center and web‐based". | |
| Participants | 23 patients (age range 20‐70 years, mean 46 years; TBSA 5%‐40%, mean TBSA 16%) with bilateral hand burns treated within 24 h of burn injury. | |
| Interventions | NPWT (125 mmHg pressure) applied for 48 h or silver sulfadiazine (SSD). | |
| Outcomes | Rate of burn healing, volume of hand as determined by fluid displacement, range of motion, grip and pinch strength. | |
| Notes | Only conference abstract available, which was an interim report on first 23 patients recruited. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not specified, although participants were reported as "randomised" to either the treatment or control group. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) participants | High risk | Not possible due to nature of intervention. |
| Blinding (performance bias and detection bias) personnel delivering intervention | High risk | Not possible due to nature of intervention. |
| Blinding (performance bias and detection bias) outcome assessors | Low risk | Blinding of principal investigator used to determine rate of burn healing (personal communication with study author, information not available in abstract). |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Interim report only; no attrition reported at this point in trial. |
| Selective reporting (reporting bias) | Low risk | All pre‐specified outcomes presented in interim report. |
| Other bias | Low risk | No other concerns. |
Abbreviations
h = hour(s) NPWT = negative pressure wound therapy SSD = silver sulfadiazine TBSA: total burn surface area
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adamkova 2005 | Not a randomised controlled trial. |
| Banwell 2004b | Not a randomised controlled trial. |
| Haslik 2004 | Not a randomised controlled trial. |
| Kamolz 2004 | Did not address a pre‐specified primary outcome measure. |
| Moisidis 2004 | No separate data on burns. |
| Molnar 2004b | Not a randomised controlled trial. |
| Nugent 2005 | Not a randomised controlled trial. |
| Schintler 2005 | Not a randomised controlled trial. |
| Schrank 2004 | Did not address a pre‐specified primary outcome measure. |
Contributions of authors
Jo Dumville: literature searching, study selection, risk of bias assessment, writing and updating review. Christopher Munson: literature searching, study selection, drafting written submission of review update. Janice Christie: literature searching, writing and updating review.
Contributions of editorial base
Nicky Cullum: edited the review, advised on methodology, interpretation and review content. Approved the final review and review update prior to submission. Sally Bell‐Syer: co‐ordinated the editorial process. Advised on methodology, interpretation and content. Edited the review and the updated review, checked the search results for the update and actioned feedback from the copy editors. Amanda Briant: ran the searches for the update.
Sources of support
Internal sources
No sources of support supplied
External sources
The National Institute for Health Research (NIHR) is the sole funder of the Cochrane Wounds Group, UK.
Declarations of interest
None known.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Molnar 2004a {published data only}
- Molnar JA, Heimbach DM, Tredget EE, Hickerson WL, Still JM, Luterman A, et al. Prospective randomized controlled mulitcenter trial applying subatmospheric pressure to acute hand burns: an interim report. 2nd World Union of Wound Healing Societies' Meeting July 18‐23; Paris, France. 2004.
References to studies excluded from this review
Adamkova 2005 {published data only}
- Adamkova M, Tymonova J, Zamecnikova I, Kadlcik M, Klosova H. First experience with the use of vacuum assisted closure in the treatment of skin defects at the burn center. Acta Chirurgiae Plasticae 2005;47(1):24‐7. [PubMed] [Google Scholar]
Banwell 2004b {published data only}
- Banwell PE. Topical negative pressure wound therapy: advances in burn wound management. Ostomy/Wound Management 2004;50(11A Suppl):9S‐14S. [PubMed] [Google Scholar]
Haslik 2004 {published data only}
- Haslik W, Kamolz LP, Andel H, Meissl G, Frey M. The use of subatmospheric pressure to prevent burn wound progression: first experiences in burn wound treatment. Zentralblatt fur Chirurgie 2004;129(Suppl 1):S62‐3. [DOI] [PubMed] [Google Scholar]
Kamolz 2004 {published data only}
- Kamolz LP, Andel H, Haslik W, Winter W, Meissl G, Frey M. Use of subatmospheric pressure therapy to prevent burn wound progression in human: first experiences. Burns 2004;30(3):253‐8. [DOI] [PubMed] [Google Scholar]
Moisidis 2004 {published data only}
- Moisidis E, Heath T, Boorer C, Ho K, Deva AK. A prospective, blinded, randomized, controlled clinical trial of topical negative pressure use in skin grafting. Plastic and Reconstructive Surgery 2004;114(4):917‐22. [DOI] [PubMed] [Google Scholar]
Molnar 2004b {published data only}
- Molnar JA. Applications of negative pressure wound therapy to thermal injury. Ostomy/Wound Management 2004;50(4A Suppl):17S‐19S. [PubMed] [Google Scholar]
- Molnar JA. The science behind negative pressure wound therapy. Ostomy/Wound Management 2004;50(4A Suppl):2S‐5S. [PubMed] [Google Scholar]
Nugent 2005 {published data only}
- Nugent N, Lannon D, O'Donnell M. Vacuum‐assisted closure ‐ a management option for the burns patient with exposed bone. Burns 2005;31(3):390‐3. [DOI] [PubMed] [Google Scholar]
Schintler 2005 {published data only}
- Schintler M, Marschitz I, Trop M. The use of topical negative pressure in a paediatric patient with extensive burns. Burns 2005;31(8):1050‐3. [DOI] [PubMed] [Google Scholar]
Schrank 2004 {published data only}
- Schrank C, Mayr M, Overesch M, Molnar J, Henkel V, Donnersmarck G, et al. Results of vacuum therapy (v.a.c.) of superficial and deep dermal burns. Zentralblatt fur Chirurgie 2004;129(Suppl 1):S59‐61. [DOI] [PubMed] [Google Scholar]
Additional references
Atiyeh 2005
- Atiyeh BS, Gunn SW, Hayek SN. State of the art in burn treatment. World Journal of Surgery 2005;29(2):131‐48. [DOI] [PubMed] [Google Scholar]
Banwell 1999
- Banwell PE. Topical negative pressure therapy in wound care. Journal of Wound Care 1999;8(2):79‐84. [DOI] [PubMed] [Google Scholar]
Banwell 2004a
- Banwell PE, Musgrave M. Topical negative pressure therapy: mechanisms and indications. International Wound Journal 2004;1(2):95‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boykin 1980
- Boykin JV, Eriksson E, Pittman RN. In vivo microcirculation of a scald burn and the progression of postburn dermal ischemia. Plastic and Reconstructive Surgery 1980;66(2):191‐8. [DOI] [PubMed] [Google Scholar]
Brigham 1996
- Brigham PA, McLoughlin E. Burn incidence and medical care use in the United States: Estimates, trends, and data sources. Journal of Burn Care Rehabilitation 1996;17(2):95‐107. [DOI] [PubMed] [Google Scholar]
Deeks 2002
- Deeks JJ. Issues in the selection of a summary statistic for meta‐analysis of clinical trials with binary outcomes. Statistics in Medicine 2002;21(1):575‐600. [DOI] [PubMed] [Google Scholar]
Demling 1979
- Demling RH, Niehaus G, Perea A, Will JA. Effect of burn‐induced hypoproteinemia on pulmonary transvascular fluid filtration rate. Surgery 1979;85(3):39‐43. [PubMed] [Google Scholar]
Demling 2005
- Demling RH, DeSanti L. Managing the burn wound. http://www.burnsurgery.org/Modules/BurnWound%201/index.htm (accessed 11 Jan 2006).
Department of Health and Human Services 2009
- Department of Health and Human Services. Comparison of prices for negative pressure wound therapy pumps. oig.hhs.gov/oei/reports/oei‐02‐07‐00660.pdf. OEI‐02‐07‐00660 2009.
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, on behalf of the Cochrane Statistical Methods Group and the Cochrane Bias Methods Group (Editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Johnson 2003
- Johnson MR, Richard R. Partial thickness burns: identification and management. Advances in Skin and Wound Care 2003;16(4):178‐87. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J, on behalf of the Cochrane Information Retrieval Methods Group. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Pham 2003
- Pham CT, Middleton P, Maddern G. Vacuum‐assisted closure for the management of wounds: an accelerated systematic review. Australian Safety & Efficacy Register of New Interventional Procedures – Surgical (ASERNIPS‐S) 2003;Report No.37:1‐53. [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre. Review Manager (RevMan) Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, issue 2011.
Sheridan 2002
- Sheridan RL. Burns. Critical Care Medicine 2002;30(11):S500‐S514. [DOI] [PubMed] [Google Scholar]
SIGN 2012
- Scottish Intercollegiate Guidelines Network (SIGN). Search filters. Available from http://www.sign.ac.uk/methodology/filters.html#random (accessed 23 August 2012).
Subrahmanyam 1998
- Subrahmanyam M. A prospective randomised clinical and histological study of superficial burn wound healing with honey and silver sulfadiazine. Burns 1998;24(2):157‐61. [DOI] [PubMed] [Google Scholar]
Tierney 2007
- Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time‐to‐event data into meta‐analysis. Trials 2007;7(8):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ubbink 2008
- Ubbink DT, Westerbos SJ, Evans D, Land L, Vermeulen H. Topical negative pressure for treating chronic wounds. Cochrane Database of Systematic Reviews 2008, Issue 3. [DOI: 10.1002/14651858.CD001898.pub2] [DOI] [PubMed] [Google Scholar]
Villanueva 2004
- Villanueva E, Bennett MH, Wasiak J, Lehm JP. Hyperbaric oxygen therapy for thermal burns. Cochrane Database of Systematic Reviews 2004, Issue 2. [DOI: 10.1002/14651858.CD004727.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wasiak 2005
- Wasiak J, Cleland HJ. Burns (minor thermal). Clinical Evidence. BMJ Publishing Group Ltd, 2005. [PubMed] [Google Scholar]
Youn 1992
- Youn YK, LaLonde C, Demling R. The role of mediators in the response to thermal injury. World Journal of Surgery 1992;16(1):30‐6. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Dumville 2012
- Dumville JC, Munson C. Negative pressure wound therapy for partial‐thickness burns.. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD006215.pub3.] [DOI] [PubMed] [Google Scholar]
Wasiak 2007
- Wasiak J, Cleland H. Topical negative pressure (TNP) for partial thickness burns. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD006215.pub2] [DOI] [PubMed] [Google Scholar]


