We applaud the proposal of Piliego et al1 to use lung ultrasound as a bedside test for triage of COVID-19 patients and for subsequent management of clinical workload and level of care in the scenario of a hospital overloaded with SARS-CoV-2 pandemic patients.2 We describe an expanded role for ultrasound (US). Preliminary reports from the Italian outbreak2 prompted us to adopt some variations on our standard clinical protocols and to implement or upgrade techniques we already use in our critical care practice before SARS-CoV-2 pandemic. We propose the following corona virus disease ultrasound (COVID-US) alphabet (figure 1).
Figure 1.
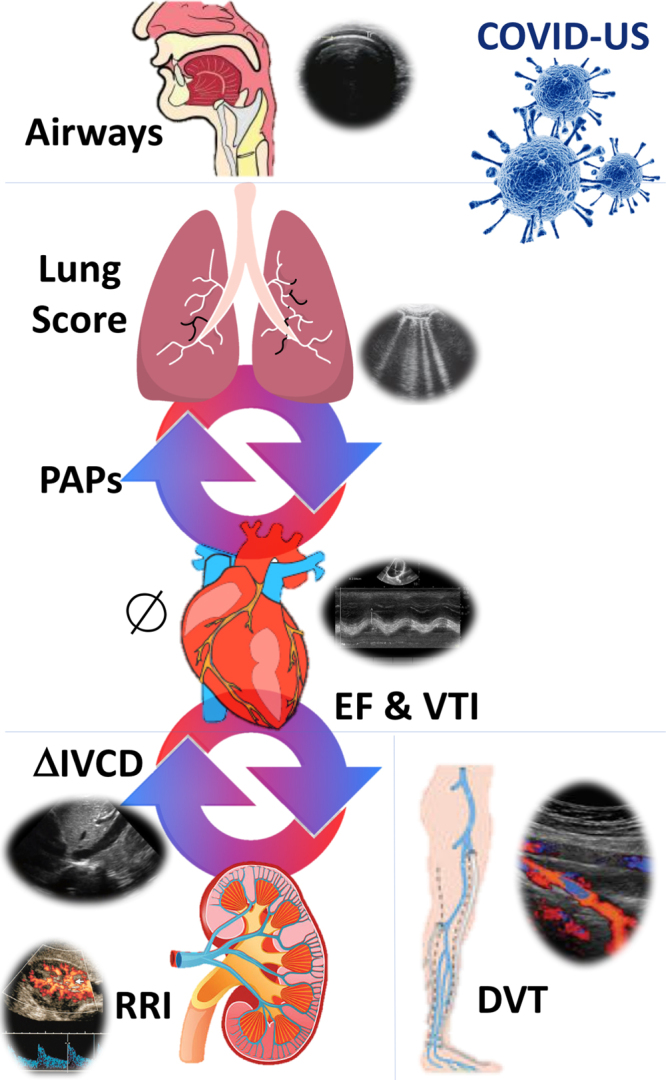
COVID-US applications for monitoring of COVID-19 ICU patients (see text for details).
- C: cardiac evaluation
- Cardiac chambers diameters and kinesis;
- Pericardium (effusion, tamponade);
- PAP;
- EF%
- IVCD;
- O: Outputs
- RRI
- VTI
- V: Ventilation
- B-lines patterns;
- B-lines spatial distribution
- Hyperinflation and recruitment response
- Lung score
- Search for pneumothorax/effusion
- I: intubation
- Prediction of difficult laryngoscopy/intubation
- Endotracheal intubation confirmation
D: Doppler and Deep venous thromboembolism/Pulmonary embolism
The study of cardiac function, diameters and kinesis, including pericardium, is performed bedside at admission and at times when there are significant hemodynamic changes during the ICU stay. Cardiac evaluation includes determination of ejection fraction (EF%), pulmonary artery pressure (PAPs), aortic velocity-time integral (VTI) at apical fifth chamber Eff Ao as a more comprehensive parameter than sole stroke volume variation (SVV%),3 inferior vena cava diameter variations differential (IVCD%)4 with respiratory cycle and renal resistive index (RRI).3 Comparative observation of preload parameters (DIVCD%) with contractile (EF%) and ejective function (VTI) and perfusion indexes such as RRI, allow us to tailor hemodynamic and ventilator therapy based on the specific physio-pathological picture of the single patient and to exclude pulmonary embolism.
Hemodynamic management of COVID-19 patients is particularly challenging because cardio-pulmonary interactions in mechanically ventilated patients. COVID-19 patients show specific lung abnormality patterns, including lesser effect on pulmonary compliance, increase in pulmonary vascular resistance with consequences to the right ventricle, inferior vena cava and renal function and on left ventricle and systemic perfusion. In this setting US is useful in decisions regarding pharmacological choices, fluid administration, ventilator adjustments together with metabolic indexes (ie blood lactate) and the whole clinical picture. In this perspective RRI, though not as well-established as EF or VTI, is added to US hemodynamic evaluation with emphasis on evaluation of “effective” organ perfusion,4 and as added decisional support for administration of vasoactive drugs, diuretics or renal vasodilators,5 for renal replacement therapy, including Cyto-Sorb® (CytoSorbents Corp, Monmouth Junction, NJ, USA) for cytokine storm control.
Similarly, choice of best PEEP is based not only on PaO2/FiO2 ratio and driving pressure evaluation, but also on its hemodynamic effects and kidney repercussions. In a 22 patients sample we observed 9% (2 cases) of ex-novo kidney failure, compared with 22.2% in New York6 experience.
Ventilation was regularly assessed by US between 3 and 4 times in 24 hours, to follow evolutional trends of COVID-19 specific US lung findings,7 to score the amount of B-lines and titrate ventilation accordingly. Response to recruitment maneuver with PEEP escalation was evaluated with US, addressing the need for high (recruiters) or low (non –recruiters) PEEP settings and the decision for early/late/no prone positioning.2 A potential US application that we have not yet adopted, is the assessment of respiratory fatigue through respiratory muscle evaluation, with implications for decision to intubate after the NIV trial2 and extubation readiness assessment.
In our practice we also use US for preintubation airway evaluation, given the aerosolization risk associated with the performance of conventional tests (measuring interincisor distance, determining Mallampati score),8 intubation confirmation when end-tidal CO2 is not immediately available,2 diagnosis of intubation-related complications (pneumothorax, pneumomediastinum, airway trauma) and for lung and ventilation assessment.7
Finally, evaluation of right cardiac chamber diameters and lung windows, and eventual integration with lower limbs US, is used to monitor thromboembolic phenomena as part of routine coagulative evaluation (thromboelastography/thromboelastometry), given the high thrombotic risk associated with COVID-197.
We believe that our approach has two important novelties. First of all, it is not only lung US, but integrated US, involving cardiac and pulmonary evaluation, fluid repletion status and perfusion, airway evaluation and thrombosis screening. The second point is that COVID-US approach is not only a diagnostic tool, but also an integrated monitoring approach following patient’s evolution and a step-by-step clinical and therapeutic decisional support. US applications in COVID-19 patients are promising, though they deserve larger studies and robust data to be validated and adopted in clinical practice. We propose a simple, patient-tailored, bedside approach to COVID-19 patients that reflects the multi-organ involvement of SARS-CoV-2.
Acknowledgments
(the Authors wish to thank all health care providers involved in critical care of COVID-19 patients.)
Footnotes
Conflicts of interest/Competing interests (Massimiliano Sorbello has received paid consultancy from Teleflex Medical, Verathon Medical and DEAS Italia, is a patent co-owner (no royalties) of DEAS Italia and has received lecture grants and travel reimbursements from MSD Italia, MSD USA. Antonio Anile, Giacomo Castiglione, Chiara Zangara, Chiara Calabrò, Mauro Vaccaro declare no other competing interests).
Availability of data and material (data available in electronic patients charts in San Marco Hospital ICU, Catania, Italy)
Authors’ contributions (Antonio Anile: This author helped with the idea and critical appraisal; Giacomo Castiglione: This author helped with the final review; Chiara Zangara: This author worked on database preparation, Chiara Calabrò: This author worked on literature check;, Mauro Vaccaro: This author worked on database access; Massimiliano Sorbello: This author wrote the original text and participated editing.)
REFERENCES
- 1.Piliego C, Strumia A, Stone MB, Pascarella G. The ultrasound guided triage: a new tool for prehospital management of COVID-19 pandemic. Anesth Analg. 2020DOI: 10.1213/ANE.0000000000004920 [epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sorbello M, El-Boghdadly K, Di Giacinto I; on behalf of The Società Italiana di Anestesia Analgesia Rianimazione e Terapia Intensiva (SIAARTI) Airway Research Group, and The European Airway Management Society. The Italian coronavirus disease 2019 outbreak: experiences and recommendations from clinical practice. Anaesthesia. 2020;75:724–732. [DOI] [PubMed] [Google Scholar]
- 3.Anile A, Ferrario S, Campanello L, Orban MA, Castiglione G. Renal resistive index: a new reversible tool for the early diagnosis and evaluation of organ perfusion in critically ill patients: a case report. Ultrasound J. 2019;11:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Corradi F, Brusasco C, Paparo F, et al. Renal doppler resistive index as a marker of oxygen supply and demand mismatch in postoperative cardiac surgery patients. Biomed Res Int. 2015;2015:763940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sorbello M, Morello G, Paratore A, et al. Fenoldopam vs dopamine as a nephroprotective strategy during living donor kidney transplantation: preliminary data. Transplant Proc. 2007;39:1794–1796. [DOI] [PubMed] [Google Scholar]
- 6.Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323:2052–2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Convissar DL, Gibson LE, Berra L, Bittner EA, Chang MG. Application of lung ultrasound during the COVID-19 pandemic: a narrative review. Anesth Analg. 2020;131:345–350.doi: 10.1213/ANE.0000000000004929. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Falcetta S, Cavallo S, Gabbanelli V, et al. Evaluation of two neck ultrasound measurements as predictors of difficult direct laryngoscopy: a prospective observational study. Eur J Anaesthesiol. 2018;35:605–612. [DOI] [PubMed] [Google Scholar]


