Abstract
Background
Pathology relating to mandibular wisdom teeth is a frequent presentation to oral and maxillofacial surgeons, and surgical removal of mandibular wisdom teeth is a common operation. The indications for surgical removal of these teeth are alleviation of local pain, swelling and trismus, and also the prevention of spread of infection that may occasionally threaten life. Surgery is commonly associated with short‐term postoperative pain, swelling and trismus. Less frequently, infection, dry socket (alveolar osteitis) and trigeminal nerve injuries may occur. This review focuses on the optimal methods in order to improve patient experience and minimise postoperative morbidity.
Objectives
To compare the relative benefits and risks of different techniques for surgical removal of mandibular wisdom teeth.
Search methods
Cochrane Oral Health’s Information Specialist searched the following databases: Cochrane Oral Health Trials Register (to 8 July 2019), the Cochrane Central Register of Controlled Trials (CENTRAL) (the Cochrane Library; 2019, Issue 6), MEDLINE Ovid (1946 to 8 July 2019), and Embase Ovid (1980 to 8 July 2019). We searched ClinicalTrials.gov and the World Health Organization International Clinical Trials Registry Platform for ongoing trials. We placed no restrictions on the language or date of publication.
Selection criteria
Randomised controlled trials comparing different surgical techniques for the removal of mandibular wisdom teeth.
Data collection and analysis
Three review authors were involved in assessing the relevance of identified studies, evaluated the risk of bias in included studies and extracted data. We used risk ratios (RRs) for dichotomous data in parallel‐group trials (or Peto odds ratios if the event rate was low), odds ratios (ORs) for dichotomous data in cross‐over or split‐mouth studies, and mean differences (MDs) for continuous data. We took into account the pairing of the split‐mouth studies in our analyses, and combined parallel‐group and split‐mouth studies using the generic inverse‐variance method. We used the fixed‐effect model for three studies or fewer, and random‐effects model for more than three studies.
Main results
We included 62 trials with 4643 participants. Several of the trials excluded individuals who were not in excellent health. We assessed 33 of the studies (53%) as being at high risk of bias and 29 as unclear. We report results for our primary outcomes below. Comparisons of different suturing techniques and of drain versus no drain did not report any of our primary outcomes. No studies provided useable data for any of our primary outcomes in relation to coronectomy.
There is insufficient evidence to determine whether envelope or triangular flap designs led to more alveolar osteitis (OR 0.33, 95% confidence interval (CI) 0.09 to 1.23; 5 studies; low‐certainty evidence), wound infection (OR 0.29, 95% CI 0.04 to 2.06; 2 studies; low‐certainty evidence), or permanent altered tongue sensation (Peto OR 4.48, 95% CI 0.07 to 286.49; 1 study; very low‐certainty evidence). In terms of other adverse effects, two studies reported wound dehiscence at up to 30 days after surgery, but found no difference in risk between interventions.
There is insufficient evidence to determine whether the use of a lingual retractor affected the risk of permanent altered sensation compared to not using one (Peto OR 0.14, 95% CI 0.00 to 6.82; 1 study; very low‐certainty evidence). None of our other primary outcomes were reported by studies included in this comparison.
There is insufficient evidence to determine whether lingual split with chisel is better than a surgical hand‐piece for bone removal in terms of wound infection (OR 1.00, 95% CI 0.31 to 3.21; 1 study; very low‐certainty evidence). Alveolar osteitis, permanent altered sensation, and other adverse effects were not reported.
There is insufficient evidence to determine whether there is any difference in alveolar osteitis according to irrigation method (mechanical versus manual: RR 0.33, 95% CI 0.01 to 8.09; 1 study) or irrigation volume (high versus low; RR 0.52, 95% CI 0.27 to 1.02; 1 study), or whether there is any difference in postoperative infection according to irrigation method (mechanical versus manual: RR 0.50, 95% CI 0.05 to 5.43; 1 study) or irrigation volume (low versus high; RR 0.17, 95% CI 0.02 to 1.37; 1 study) (all very low‐certainty evidence). These studies did not report permanent altered sensation and adverse effects.
There is insufficient evidence to determine whether primary or secondary wound closure led to more alveolar osteitis (RR 0.99, 95% CI 0.41 to 2.40; 3 studies; low‐certainty evidence), wound infection (RR 4.77, 95% CI 0.24 to 96.34; 1 study; very low‐certainty evidence), or adverse effects (bleeding) (RR 0.41, 95% CI 0.11 to 1.47; 1 study; very low‐certainty evidence). These studies did not report permanent sensation changes.
Placing platelet rich plasma (PRP) or platelet rich fibrin (PRF) in sockets may reduce the incidence of alveolar osteitis (OR 0.39, 95% CI 0.22 to 0.67; 2 studies), but the evidence is of low certainty. Our other primary outcomes were not reported.
Authors' conclusions
In this 2020 update, we added 27 new studies to the original 35 in the 2014 review. Unfortunately, even with the addition of these studies, we have been unable to draw many meaningful conclusions. The small number of trials evaluating each comparison and reporting our primary outcomes, along with methodological biases in the included trials, means that the body of evidence for each of the nine comparisons evaluated is of low or very low certainty.
Participant populations in the trials may not be representative of the general population, or even the population undergoing third molar surgery. Many trials excluded individuals who were not in good health, and several excluded those with active infection or who had deep impactions of their third molars.
Consequently, we are unable to make firm recommendations to surgeons to inform their techniques for removal of mandibular third molars. The evidence is uncertain, though we note that there is some limited evidence that placing PRP or PRF in sockets may reduce the incidence of dry socket. The evidence provided in this review may be used as a guide for surgeons when selecting and refining their surgical techniques. Ongoing studies may allow us to provide more definitive conclusions in the future.
Plain language summary
Comparing different surgical techniques used to remove wisdom teeth from the lower jaw
Background
The removal of wisdom teeth is a common operation, but it can cause short‐ and long‐term side effects. People may have their wisdom teeth removed if they are causing pain or infection, or if they are damaging other teeth or not breaking through the gum properly. Surgery has a risk of complications. One of the most common is dry socket (also known as alveolar osteitis). This is when a blood clot fails to form in the socket that the tooth has come out of, or the clot is disturbed before the socket has properly healed. Because the bones and nerves underlying the socket are exposed, it can be a very painful condition.
Review question
We aimed to find out the benefits and harms of different surgical techniques used to remove wisdom teeth from the lower jaw, specifically how surgeons can reduce the risk of complications following surgery. We considered the most important outcomes to be: dry socket, wound infection, long‐term damage to the nerves supplying sensation to the tongue and skin of the lower lip and chin, and problems such as excessive bleeding or a broken jaw.
Study characteristics
We searched for relevant studies up to 8 July 2019. We included 62 studies with 4643 participants. Many studies excluded people who were not in excellent health so the participants in the trials may not be truly representative.
Key results
The available evidence is inconclusive.
It is unclear if the position of the cut into the gum makes any difference to the outcomes.
It is unclear whether it is possible to avoid damaging a nerve to the tongue by using a surgical instrument called a lingual retractor.
It is unclear as to whether the type of surgical tool (a chisel or a rotating drill) used to remove bone from the jaw makes a difference to the likelihood of the wound becoming infected.
It is unclear if the amount and method of delivering saltwater to clean the tooth socket after the extraction makes any difference to the outcomes.
It is unclear whether different methods to stitch the gum after the tooth is removed makes any difference to the outcomes.
Placing products that are derived from the patient’s own blood into the tooth socket may help to reduce the occurrence of dry socket (a condition that causes intense pain a few days after extraction).
Another three surgical approaches were tested in the studies, but they did not measure the important outcomes.
Certainty of the evidence
None of the included studies were at low risk of bias. All of the studies were quite small. The quality of the studies varied, with most having flaws that could have biased their results. In addition, some of the results were very imprecise, with variation between them that could not be explained. For these reasons, we consider the available evidence to be uncertain. Future research may be able to provide dental surgeons and patients with clearer conclusions than those listed above.
Summary of findings
Background
Description of the condition
Surgical removal of mandibular third molars (lower wisdom teeth) is one of the most common operations undertaken in oral and maxillofacial surgery. It is difficult to find accurate figures for the number of people undergoing such procedures; however, it is estimated that the UK National Health Service funds the removal of third molars of approximately 152,000 people per year in England alone (McArdle 2012; McArdle 2018a). Mandibular third molars are also removed in private practice in the UK, as elsewhere in the world, but national systems for this data collection are less developed.
There are many indications for third molar removal, but the most common reason is recurrent infection around the tooth as it attempts to erupt but is impacted against bone or soft tissues (pericoronitis); a recent retrospective study of 1431 extracted third molars found that 49% of these were removed due to pericoronitis (McArdle 2012; McArdle 2018b). Other indications include unrestorable caries, caries in the adjacent tooth (Toedtling 2016), pulpal and periapical pathology, fracture of the tooth, and cyst development, amongst others. Most commonly, the benefits of surgical removal of a wisdom tooth include alleviation of the symptoms and signs of pericoronitis and its potential consequences. The symptoms of pericoronitis are pain, foul taste, swelling of the associated soft tissues about the tooth but also of the face, and restricted mouth opening (trismus). Local infection may spread and be associated with lymphadenopathy, pyrexia, and malaise. More rarely, swelling may threaten airway patency and life. Surgery is frequently associated with postoperative pain, swelling, and restricted mouth opening (trismus). Less common complications include infection, including alveolar osteitis (dry socket), trigeminal nerve injuries (inferior alveolar, lingual, and mylohyoid nerves) and, rarely, fracture of the mandible.
People requiring surgical removal of wisdom teeth are frequently anxious about anticipated postoperative pain, which may be severe. Such is the predictability of postoperative pain that this type of surgery is used as a model of pain for the clinical evaluation of novel analgesics (Bailey 2013; Moore 2015). The severity of pain usually peaks within several hours after surgery and may last for several days or more. Facial swelling may also alarm patients and typically peaks at around one or two days before subsiding over the subsequent days. Restricted mouth opening results from inflammation of the muscles that move the jaw and may be considered initially as having a protective function by encouraging the patient to rest the surgical site and permit healing. However, it may lead to difficulty in eating and functioning if it persists for more than a few days.
Alveolar osteitis (dry socket) has a reported incidence of 1% to 2.9% (Goldberg 1985; Muhonen 1997). Other studies have investigated the role of smoking and complexity of the extraction on the incidence of dry socket (Parthasarathi 2011). The socket has exposed bone, which is extremely painful and sensitive to touch. This condition can be difficult to manage and usually causes pain for up to two weeks. Less commonly an infection presents with pus in the surgical site and may be associated with signs such as lymphadenopathy or raised body temperature. This infection may also spread to the surrounding tissue spaces. Damage to the branches of the trigeminal nerve may arise because of their proximity to the mandibular third molar and consequent physical damage during surgery. Sensory disturbance may be temporary or permanent, and is usually described as temporary if recovery of normal sensation occurs within four to six months (Mason 1988). The degree and description of altered sensation is variable and includes reduced sensation (hypoaesthesia), abnormal sensation (paraesthesia), and unpleasant painful sensation (dysaesthesia) (Jones 1992), and pain on touching (mechanical allodynia). The incidence of temporary and permanent nerve damage following the surgical removal of third molar teeth varies considerably between reports and may be related to a number of factors including the difficulty of surgery, surgical technique, and the skill of the surgeon. The incidence of temporary lingual (tongue) nerve disturbance has been reported to be 0%, Chiapasco 1993, to 15%, Rood 1983, and that of permanent disturbance to be 0%, Schultze‐Mosgau 1993, to 2%, Rood 1992. Inferior alveolar nerve damage has been reported to ocur in about 5% (temporary) and 0.2% (permanent) of patients (Smith 1997), and this affects the sensation of the skin of the lower lip and chin. In a study of 4338 mandibular third molar extractions, 0.35% experienced inferior alveolar nerve deficit and 0.69% experienced lingual nerve deficit; of these, 0.002% and 0.003% experienced inferior alveolar nerve or lingual nerve deficit after six months, respectively (Cheung 2010). Fracture of the mandible may occur during the surgery or postoperatively. The incidence of this rare complication is estimated to be about 1 in 28,000 operations (Libersa 2002). Whilst this complication may be managed very effectively with techniques such as reduction and fixation with mini plates, the patient may experience significantly increased pain and swelling along with the need for hospitalisation. In the UK National Health Service, outcome data on these complications is being analysed, with Patient Reported Outcome Measures (PROMs) and Patient Reported Experience Measures (PREMs) being used to assess the quality and safety of healthcare providers in relation to third molar surgery. In parts of the world without national health or reporting systems, it is not possible to collect accurate outcome data.
Description of the intervention
Various techniques have been developed to permit the successful removal of the third molar whilst minimising complication rates.
Surgical flap design
A surgical incision and soft‐tissue mucoperiosteal flap is typically raised to permit access to the wisdom tooth for removal. Various modifications to the design of the flap have been advocated in order to offer advantage and improve the outcome for the patient. Examples include envelope, triangular, comma‐shaped, bayonet flaps, and further variations of these (Chen 2017).
Lingual nerve protection
A mucoperiosteal flap is usually raised on the buccal aspect of the tooth to be removed, but the practice of also raising a lingual flap to improve access and protect the lingual nerve varies according to differing opinions and cultural and historic views. When bone is being removed buccally only, there is no danger to the lingual nerve that lies in close proximity to the wisdom tooth on its lingual aspect. However, the lingual nerve is at risk of physical injury from the bur when distolingual bone is removed. Distolingual bone may need to be removed to permit tooth removal according to its type of impaction and typically for distolingually impacted teeth. An instrument may be placed between the bone to be removed and the lingual flap enclosing the nerve to protect it from physical injury during bone removal. This ‘lingual nerve protection’ has been the tradition in the UK and in some other parts of the world, but less so in the USA (Pell 1933). Whilst the intention of placing a barrier instrument is to prevent permanent lingual nerve injury, some surgeons believe that it is preferable not to place an instrument for nerve protection, as there is the potential to cause a temporary nerve injury (Renton 2001). However, in this situation, it is imperative not to remove bone distal to the tooth and only bone on the buccal aspect. The type of instrument to be used for lingual nerve protection has also been the subject of investigation, as some prefer to use a wider instrument to ensure more effective nerve protection, although this may be more invasive to place (Greenwood 1994).
Bone removal techniques
Bone removal may be carried out using drills, chisels or, more recently, a novel technique using piezoelectric surgery (Degerliyurt 2009). The choice of surgical technique has been implicated in the incidence of nerve damage as well as the severity of pain and swelling. The most common technique using a chisel is the 'lingual split bone technique', in which a section of distolingual bone about the wisdom tooth is fractured off to facilitate the removal of the impacted tooth, especially distoangular impacted teeth. This technique, in which the socket is saucerized, was originally developed to reduce infection at a time when this was common and fatalities were not unknown. It was later modified when the surgical drill was introduced (Ward 1956).
Wound irrigation techniques
Some surgeons have advocated using mechanical methods of irrigating the surgical wound on removal of the tooth rather than doing this manually. Similarly, it has been thought that larger volumes of irrigant are preferable for outcomes because ensuring removal of more bony debris may reduce the incidence of infection.
Wound closure
The amount of wound closure, whether complete, partial, or left open, has been the subject of debate, with proponents of each claiming a difference in postoperative pain and swelling (Bello 2011; Osunde 2012).
Suturing techniques
Suture technique may also have an impact on healing and surgical outcomes relating to third molar surgery (Waite 2006)
Surgical drains
Some surgeons have recommended placing a surgical drain to reduce the size of haematoma as well as postoperative complications (Osunde 2011b), although in many countries this practice is rarely used in the absence of a collection of pus. An alternative to the use of surgical drains is to allow drainage by not completely closing the surgical wound over the socket.
Use of autologous blood concentrates
Platelet‐rich fibrin (PRF) is a second‐generation platelet concentrate that was initially developed by a team based in France for use in oral and maxillofacial surgery (Dohan 2006). PRF is a product of centrifuged blood. Anticoagulant is unnecessary as activation of clotting of the sample is encouraged. This process produces fibrinogen as the end product of the coagulation cascade; circulating thrombin transforms this into fibrin. This fibrin clot can then be separated from the sample, and the clot will contain platelets within a fibrin mesh. Resistant autologous fibrin membranes can be derived from this mesh by driving the serum from the blood clot. PRF is considered to be a healing biomaterial that appears to accelerate physiologic healing (Choukroun 2006). A recent systematic review on the use of PRF in soft‐tissue wound healing concluded that the material has a positive effect on healing in a variety of soft‐tissue defects (Miron 2017). Commercially available fibrin sealants mimic the final part of the coagulation cascade (fibrinogen is converted to fibrin) in wounds; they are often used instead of sutures to encourage wound healing. These sealants have been shown to reduce postoperative bleeding from dental extraction sockets in patients who are anticoagulated with warfarin (Bodner 1998). The technique required the drawing of blood from the patient and the use of appropriate equipment to prepare the PRF/PRP, which may add significant cost.
Root retention techniques/coronectomy
If a wisdom tooth has a particularly intimate relationship with the inferior alveolar nerve, then injury is more likely on tooth removal, and some have advocated leaving a part of the tooth root in place to reduce this risk rather than removing the whole tooth. Retaining a small part of the root or root apex to reduce the risk of nerve injury has been common practice for many decades, but recently some surgeons have recommended leaving all of the tooth root in place in a technique known as coronectomy (Renton 2012). There has been discussion regarding the fate of the retained roots after coronectomy (Pedersen 2018). It is thought that the majority of root migration occurs within the first 6 to 12 months postoperatively (Leung 2018), but there has been concern about the potential for later pain and infection. Coronectomy may not be successful in that the root may be mobilised during the procedure (Jowett 2016).
How the intervention might work
Wisdom tooth removal is a frequently performed procedure. There is debate about the best way to remove wisdom teeth. It is important to review the evidence base for these surgical techniques in order to provide the best experience for patients and to minimise complication rates.
Why it is important to do this review
Cochrane Oral Health undertook an extensive prioritisation exercise in 2014 to identify a core portfolio of high‐priority reviews (Worthington 2015); this review was identified as a priority by the oral and maxillofacial surgery expert panel (Cochrane Oral Health priority reviews).
Research suggests that wisdom tooth removal has an immediate negative impact on patients' working and social lives. In one study, patients took an average of 1.6 days off work, with over one‐third of patients stating that the surgery had affected their performance at work (Colorado‐Bonnin 2006); participation in social activities, sports, and other hobbies is also negatively affected (Conrad 1999). For some patients, quality of life (QoL) is reduced for one to two weeks after surgery (Savin 1997), and it is considered a major event for large numbers of patients (Van Wijk 2007). A recent study emphasised the emotional impacts of third molar surgery and noted its effects on QoL in relation to anxiety and worry in particular (Beech 2017). The detrimental effects on QoL may be present for considerably longer for those who suffer nerve injury (Hillerup 2007). It is important to summarise and present the current evidence base for third molar surgical techniques so that every effort is made to reduce postoperative morbidity and improve the patient experience for this commonly performed surgical procedure.
Objectives
To compare the relative benefits and risks of different techniques for the surgical removal of mandibular wisdom teeth.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) comparing surgical techniques for the removal of mandibular wisdom teeth.
Types of participants
People requiring the surgical removal of mandibular wisdom teeth. We excluded studies with participants who required surgical removal of a maxillary third molar tooth at the same operation unless the maxillary third molar was erupted and removed as a simple extraction with an elevator or forceps, or both. The reason for this is that it would not be clear which operation led to the reported outcome (e.g. pain, swelling, restricted mouth opening). We also excluded participants requiring removal of a mandibular wisdom tooth with only elevators or forceps without elevating a flap.
Types of interventions
Different surgical techniques to remove mandibular wisdom teeth, including surgical flap design, lingual nerve protection, root retention techniques, bone removal technique, wound irrigation technique, suturing techniques, wound closure, the use of surgical drains, and the use of plasma rich protein/plasma rich fibrin (PRF/PRP).
Types of outcome measures
Primary outcomes
Alveolar osteitis (seven days).
Infection: wounds becoming infected (presence of pus) (seven days).
Permanent altered tongue, chin, or lip sensation (more than six months).
Adverse effects, such as reactionary bleeding or fracture of the mandible (up to 30 days).
Secondary outcomes
Temporary altered tongue sensation (only the time point closest to one‐month postoperatively was used).
Temporary altered chin skin or lower lip sensation (only the time point closest to one‐month postoperatively was used).
Postoperative pain (only the time point closest to one‐day postoperatively was used).
Swelling (only the time point closest to one‐week postoperatively was used).
Trismus (restricted mouth opening) (only the time point closest to one‐week postoperatively was used).
We did not include studies solely looking at periodontal outcomes relating to the second permanent molar.
Search methods for identification of studies
Electronic searches
Cochrane Oral Health's Information Specialist conducted systematic searches in the following databases for RCTs and controlled clinical trials. There were no language, publication year, or publication status restrictions.
Cochrane Oral Health Trials Register (searched 8 July 2019) (Appendix 1).
Cochrane Central Register of Controlled Trials (CENTRAL; 2019, Issue 6) in the Cochrane Library (searched 8 July 2019) (Appendix 2).
MEDLINE Ovid (1946 to 8 July 2019) (Appendix 3).
Embase Ovid (1980 to 8 July 2019) (Appendix 4).
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, they were combined with subject strategy adaptations of the Highly Sensitive Search Strategy designed by Cochrane for identifying RCTs and controlled clinical trials as described in Chapter 6 of the Cochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2011).
Searching other resources
Cochrane Oral Health’s information specialist searched the following trial registries for ongoing studies:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 8 July 2019) (Appendix 5);
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 8 July 2019) (Appendix 6).
We wrote to authors of the RCTs identified and personal contacts in order to identify unpublished or ongoing studies. We checked the bibliographies of papers and review articles for any further studies.
We checked that none of the studies included in this review was retracted due to error or fraud.
We did not perform a separate search for adverse effects of interventions used, considering only adverse effects described in the included studies.
Data collection and analysis
Selection of studies
We exported the results of the database searches for this 2020 update into Covidence (Covidence). Three review authors (WK, NS and EB) independently scanned the titles and abstracts (when available). We designed the search to be sensitive and to include controlled clinical trials; these were filtered out early in the selection process if they were not randomised. For studies that appeared to meet the inclusion criteria, or for which there were insufficient data in the title and abstract to make a clear decision, we obtained the full study report, which two review authors (WK, NS) independently assessed to establish whether the studies met the inclusion criteria or not. Any disagreements were resolved by discussion; we planned to consult a third review author (EB) if required. This was necessary in a small number of cases.
All studies meeting the inclusion criteria underwent a validity assessment in Covidence and data extraction by EB, WK, and NS. We recorded any studies excluded at this or subsequent stages, with reasons for their exclusion, in the Characteristics of excluded studies tables.
Data extraction and management
In the 2020 update, two review authors (WK, NS) independently extracted study data using specially designed data extraction forms. We piloted the data extraction forms on several papers and modified the forms as required before use. Any disagreements were discussed and a third review author (EB) was consulted where necessary. We contacted authors for clarification or missing information whenever possible.
For each trial, we recorded the following data:
year of publication, country of origin, source of study funding, design of the trial (split‐mouth or parallel group);
details of the participants including demographic characteristics, source of recruitment, and criteria for inclusion and exclusion;
details about the type of surgical intervention, and the control intervention;
details of the outcomes reported, including method of assessment and time intervals.
We also noted whether or not an a priori calculation had been undertaken for sample size.
Assessment of risk of bias in included studies
We undertook assessment of risk of bias in Covidence (Covidence), following the Cochrane 'Risk of bias' tool as described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). The tool addresses the following domains: sequence generation; allocation sequence concealment; blinding of participants, surgeons, and assessors; incomplete outcome data; selective outcome reporting; and other bias. Blinding of participants was straightforward in some studies as participants were under a general anaesthetic.
We recorded each piece of information extracted for the 'Risk of bias' tool, together with the precise source of this information. The review authors were not blinded to the names of the authors, institutions, journal, or results of a study. Two review authors performed 'Risk of bias' assessment independently. Any disagreements were resolved by consensus, with the assistance of a third review author.
We tabulated the risk of bias for each included study (see Characteristics of included studies), along with a judgement of low, high, or unclear risk of bias for each domain. 'Risk of bias' summaries are presented in Figure 1 and Figure 2.
1.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Overall risk of bias for each trial
After taking into account the additional information provided by the authors of the trials, we grouped the studies into the following categories.
Low risk of bias (plausible bias unlikely to seriously alter the results) if all criteria were met.
Unclear risk of bias (plausible bias that raises some doubt about the results) if one or more criteria were partly met or there was insufficient information to know if they were met (for example, if study authors had made some attempt to conceal the allocation of participants, to blind the assessors, or to give an explanation for withdrawals, but these attempts were not judged to be ideal).
High risk of bias (plausible bias that seriously weakens confidence in the results) if one or more criteria were not met as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Measures of treatment effect
In parallel trials, for dichotomous outcomes, we expressed the estimate of effect of an intervention as risk ratios (RRs) together with 95% confidence intervals (CIs). We used Peto odds ratios (ORs) when the event rate was very low. For continuous outcomes, we used means and standard deviations (SDs) to summarise the data for each trial employing mean differences (MDs) and 95% CIs. For data analysis from cross‐over or split‐mouth trials, we took into account the pairing of the data using generic inverse‐variance (GIV) outcome type in Review Manager 5 (RevMan; Stedman 2011). We estimated OR for dichotomous data produced by cross‐over and split‐mouth designed studies, after obtaining the log OR and its standard error (SE), using approved Cochrane methods (Becker‐Balagtas methods detailed in Curtin 2002, and assuming an intraclass correlation (ICC) of 0.5 to account for pairing). We estimated MDs, accompanied by 95% CI for relevant continuous outcome data, via GIV in Review Manager 5 by utilising SEs, and deriving these from SDs where SEs were unavailable (again, using standardised Cochrane methods as outlined in Chapter 7 of the Cochrane Handbook for Systematic Reviews of Interventions) (Higgins 2011).
Unit of analysis issues
Study participants had either one or two mandibular wisdom teeth, and these were frequently presented as independent data, so the CIs were slightly narrower than they should be, and P values slightly less. If we were unable to obtain data taking the clustering of the teeth within participants into account, we used these data but were careful about the interpretation. As expected, many of these trials were split‐mouth studies, where the teeth in each participant were surgically removed by different methods (either during the same operation, or at different times). We analysed the data from split mouth‐studies according to methods outlined in the Measures of treatment effect section.
Dealing with missing data
Data from split‐mouth studies are frequently presented omitting the 'paired' relationship of the data. We made estimates of the SE for the continuous outcomes assuming a correlation coefficient of 0.5, and methods for the dichotomous data are outlined in the Measures of treatment effect section. We estimated missing SDs using the methods outlined in Chapter 7 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Some published data related to pain, swelling, and maximum mouth opening could not be used in this review for reasons that are explained in Table 10, Table 11, and Table 12. We contacted trial authors to obtain the raw data for these studies, but no additional unpublished data could be obtained.
1. Unuseable published data related to pain at 24 hours.
| Studies | Comparison | Subgroup | Reasons |
| Rabi 2017 | Flap design | Triangular vs envelope flap | Pain assessed on a visual scale from no pain to severe pain. |
| Şimşek Kaya 2019 | Flap design | Enveloped flap vs modified triangular flap | Standard deviations were not provided. |
| Basheer 2017 | Bone removal techniques | Piezoelectric vs rotary osteotomy technique | Pain assessed on a visual scale from no pain to severe pain. |
| Mantovani 2014 | Bone removal techniques | Piezoelectric (ultrsound) device vs traditional surgery with bur | Pain assessed at day 2 |
| Acar 2017 | Suturing techniques | Horiztonal mattress vs simple interrupted suturing | Unable to calculate MD and SE from data available |
| Gogulanathan 2015 | Suturing techniques | Fibrin sealant vs conventional suturing | Not VAS ‐ numerical scale used |
| Kumar 2016 | Surgical drain | Tube drain vs none | Pain assessed on a visual scale from no pain to severe pain. |
| Dutta 2016 | Wound closure with autologous platelet concentrates | PRF vs none vs PRF + hydroxyapatite | Pain assessed on 6‐point scale. |
| Kumar 2015 | Wound closure autologous with platelet concentrates | Plasma rich fibrin vs none | Data presented as mild, slight, severe. |
| Unsal 2018 | Wound closure autologous with platelet concentrates | PRF vs none | A verbal rating scale was used to evaluate postoperative pain level, which comprised 6 pain severity descriptors: none, mild, moderate, severe, very severe, and excruciating. Not possible to convert this to VAS data |
| Uyanik 2015 | Wound closure autologous with platelet concentrates | Plasma rich fibrin vs none | Data presented as a sum of 7 days. |
MD: mean difference; PRF: platelet rich fibrin; SE: standard error; VAS: visual analogue scale; vs: versus.
2. Unuseable published data related to swelling at 7 days.
| Studies | Comparison | Subgroup | Reasons |
| Şimşek Kaya 2019 | Flap design | Modified triangular flap vs envelope | Presented as % of change from baseline. Data could not be used. Authors were contacted to obtain raw data but no reply received. |
| Mobilio 2017 | Flap design | Envelope flap vs triangular flap | To assess swelling, the average percentage value was obtained from 5 distances (in mm) through 6 facial points (angle of the mandible to tragus, to eye outer canthus, to labial commissure, to nasal border, and to soft pogonion). |
| Arakji 2016 | Bone removal techniques | Conventional techniques vs piezoelectric surgery | Swelling data were presented by taking the mean of the distance of more than 1 measurement, and the raw data were not provided. |
| Basheer 2017 | Bone removal techniques | Piezoelectric vs rotary osteotomy technique | Mean of different measurements |
| Bhati 2017 | Bone removal techniques | Piezoelectric vs rotary osteotomy technique | Mean of multiple measurements |
| Mantovani 2014 | Bone removal techniques | Piezoelectric surgery vs conventional | Overall swelling or oedema (E) was calculated and expressed as E = [Σdi2/4]0.5, where Σdi is the sum of the 4 facial reference measurements (G‐T, G‐C, G‐S, G‐P). |
| Mistry 2016 | Bone removal techniques | Piezoelectric vs rotary osteotomy technique | Distance between extraoral and intraoral reference points was measured with divider to assess the swelling. |
| Piersanti 2014 | Bone removal techniques | Conventional techniques vs piezoelectric surgery | Swelling data were presented by taking the mean of the distance of more than 1 measurement, and the raw data were not provided. |
| Acar 2017 | Suturing techniques | Horizontal mattress suturing vs simple interrupted suturing | Postoperative swelling was evaluated by measuring the changes of the 5 distances on the face of the participants preoperatively and postoperatively. |
| Gogulanathan 2015 | Suturing techniques | Fibrin sealant vs conventional suturing | Swelling raw data were not provided. |
| Kumar 2016 | Surgical drain | Tube drain vs none | Means of horizontal and vertical measurements |
| Pachipulusu 2018 | Primary vs secondary wound closure | Primary vs secondary closure of the surgical wound | Swelling data presented as a percentage of the differences between pre‐op and post‐op measurements. |
| Kumar 2015 | Wound closure with autologous platelet concentrates | PRF vs none | Swelling data were presented as a percentage of the differences between pre‐ and postoperative measurement. |
| Uyanik 2015 | Wound closure with autologous platelet concentrates | PRF or a combination of PRF and piezoelectric surgery vs conventional rotatory osteotomy | Swelling data presented as a percentage of the differences between pre‐op and post‐op measurements. |
| Dutta 2016 | Wound closure with autologous platelet concentrates | PRF vs none vs PRF+ hydroxyapatite | Mean of 3 measurements |
| Kapse 2019 | Wound closure with autologous platelet concentrates | PRF vs none | Swelling data presented as a percentage of the differences between pre‐op and post‐op measurements. |
PRF: platelet rich fibrin; vs: versus.
3. Unuseable published data related to maximum mouth opening at 7 days.
| Studies | Comparisons | Subgroup | Reasons |
| Şimşek Kaya 2019 | Flap design | Modified triangular flap vs envelope | Trismus data were presented as a percentage of the differences between measurements. |
| Acar 2017 | Suturing techniques | Horiztonal mattress vs simple interrupted suturing | Unable to calculate MD and SE from data available |
| Kumar 2015 | Wound closure with autologous platelet concentrates | PRF vs none | Trismus data were presented as a percentage of the differences between pre‐ and postoperative measurements. |
| Uyanik 2015 | Wound closure with autologous platelet concentrates | PRF or a combination of PRF and piezoelectric surgery vs conventional rotatory osteotomy | Trismus data were presented as a percentage of the differences between measurements. |
PRF: platelet rich fibrin; vs: versus.
Assessment of heterogeneity
There were insufficient studies in any one comparison to investigate heterogeneity. Had there been sufficient studies, we would have test statistical heterogeneity by the Chi2 test and I2 statistic. The Chi2 test resulting in P < 0.10 is interpreted as indicating statistically significant heterogeneity. We would have used the I2 statistic to assess and quantify the possible magnitude of inconsistency (i.e. heterogeneity) across studies.
Assessment of reporting biases
We assessed possible reporting biases on two levels: within‐study and between‐study. Within‐study selective outcome reporting was examined as a part of the overall 'Risk of bias' assessment (see Assessment of risk of bias in included studies). We compared outcomes listed in the methods section of a publication against the reported results. Where we found indications of reporting bias, we contacted the study authors for clarification if needed. We planned that if there were at least 10 studies included in a meta‐analysis in the review, we would generate a funnel plot of effect estimates against their SEs to assess a possible between‐study reporting bias. Had we found asymmetry of the funnel plot by inspection which was confirmed by statistical tests, we would have considered possible explanations and taken these into account in the interpretation of the overall estimates of treatment effects.
Data synthesis
We undertook meta‐analysis only if there were studies of similar comparisons reporting the same outcome measures. We combined RRs for dichotomous data, unless: a) the event rate was very low and Peto ORs were used, or b) split‐mouth/cross‐over studies were included in the meta‐analysis, in which case OR employing GIV was used (using the Becker‐Balagtas method, as described in the Measures of treatment effect section). We used MDs for continuous data. If we required pooling of data from a cross‐over/split‐mouth study with continuous data from a parallel‐group study, the parallel group data was converted into the same format (MD, SE) as split‐mouth designed study data for use in GIV. We used the random‐effects model meta‐analyses where there were at least four studies; otherwise, we used the fixed‐effect model.
Subgroup analysis and investigation of heterogeneity
Where possible, we planned to undertake subgroup analyses with respect to the different surgical techniques and different numbers of operators or types of operator. No trials included in the review had relevant data available. We would have assessed clinical heterogeneity by examining the types of participants and interventions for all outcomes in each study if sufficient numbers of studies had been included within the same comparison.
Sensitivity analysis
We planned to undertake sensitivity analyses to examine the effect of allocation concealment and blinded outcome assessment on the overall estimates of effect, but there were no studies at overall risk of bias. In addition, we planned to examine the effect of including unpublished studies, but we did not identify any.
Summary of findings and assessment of the certainty of the evidence
We generated 'Summary of findings' tables for the following outcomes: alveolar osteitis; infection; permanent (more than six months) altered tongue, chin skin or lower lip sensation; temporary altered tongue, chin skin or lower lip sensation; postoperative pain; swelling; and restricted mouth opening. We assessed the certainty of the body of evidence by considering the overall risk of bias of the included studies, directness of the evidence, inconsistency of the results, precision of the estimates, risk of publication bias, magnitude of the effect, and whether or not there was evidence of a dose response. We categorised the certainty of the body of evidence for each comparison and primary outcome as high, moderate, low, or very low. These judgements were made using the GRADE software package (GRADEpro GDT).
Results
Description of studies
Results of the search
In addition to the studies included in the 2014 Cochrane Review search, after removal of duplicates we identified 1561 new references from the updated searches, which covered the time period to 8 July 2019. At least two review authors, independently and in duplicate, assessed the titles and abstracts of the new references, using a Covidence database. We discarded a total of 1456 references at this stage as they were irrelevant to this review (Figure 3).
3.
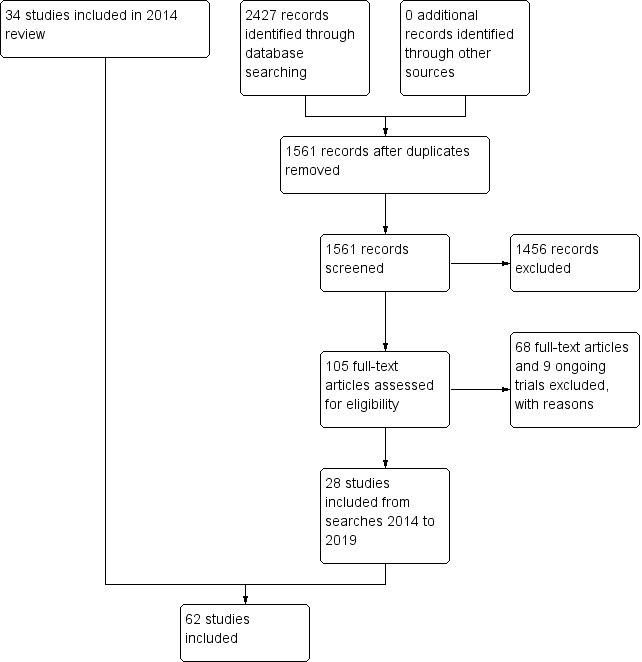
Study flow diagram.
We obtained full‐text copies of the remaining 105 articles. Each of these papers was assessed by at least two review authors, and 68 studies were excluded. From the search update, an additional 28 references (to 28 studies) met the inclusion criteria for this review (Figure 3). The remaining trials are ongoing (ChiCTR‐ICR‐15006182; IRCT2014052017781N1; IRCT2014052717863N2; IRCT2015050722139N1; IRCT201506191760N42; ISRCTN16849867; NCT02495207; NCT02831374; NCT02942108).
Included studies
In addition to the 34 trials included in the review first published in July 2014, we included a further 27 studies in this 2020 review update.
Characteristics of the trial setting and investigators
Of the 62 included studies, 16 were conducted in India (Basheer 2017; Bhati 2017; Danda 2010; Dutta 2016; Gogulanathan 2015; Kapse 2019; Kumar 2015; Kumar 2016; Mistry 2016; Nageshwar 2002; Pachipulusu 2018; Praveen 2007; Rabi 2017; Sandhu 2010; Singh 2018; Srinivas 2006), 11 in Turkey (Acar 2017; Erdogan 2011; Gulsen 2017; Koyuncu 2013; Koyuncu 2015; Mocan 1996; Ozgul 2015; Saglam 2003; Şimşek Kaya 2019; Topcu 2019; Unsal 2018), 6 in Italy (Barone 2010; Mantovani 2014; Mobilio 2017; Pasqualini 2005; Piersanti 2014; Rullo 2013), 5 in Iran (Eshghpour 2014; Haraji 2010; Hashemi 2012; Mohajerani 2018; Refo'a 2011), 4 in Brazil (Briguglio 2011; Cerqueira 2004; Gomes 2005; Xavier 2008), 4 in Nigeria (Bello 2011; Chukwuneke 2008; Osunde 2011a; Osunde 2012), 3 in the UK (Absi 1993; Greenwood 1994; Renton 2005), 3 in the USA (Butler 1977; de Brabander 1988; Sweet 1976), 2 in New Zealand (Goldsmith 2012; Kirk 2007), and 1 in each of Thailand (Rakprasitkul 1997), Spain (Gargallo‐Albiol 2000), China (Leung 2009), South Africa (Roode 2010), Jordon (Baqain 2012), Cyprus (Uyanik 2015), Pakistan (Shad 2015), and Lebanon (Arakji 2016). All of the included studies took place in hospital settings, and no commercial sponsorships were reported or identified in the published reports, although one study did receive financial support from the British Association of Oral and Maxillofacial Surgeons (Renton 2005).
Twenty‐four of 62 included studies were of parallel‐group design, where some participants were randomly allocated to the experimental group and others were randomly allocated to the control group (Barone 2010; Basheer 2017; Bello 2011; Briguglio 2011; Chukwuneke 2008; de Brabander 1988; Dutta 2016; Gargallo‐Albiol 2000; Koyuncu 2013; Kumar 2015; Leung 2009; Mobilio 2017; Mocan 1996; Nageshwar 2002; Osunde 2011a; Osunde 2012; Pachipulusu 2018; Pasqualini 2005; Praveen 2007; Rabi 2017; Refo'a 2011; Renton 2005; Shad 2015; Singh 2018). The remaining 38 studies were of split‐mouth design, where participants had one mandibular third molar randomly allocated to the experimental intervention and the third molar on the opposite side allocated to the control group.
In 23 of the 38 split‐mouth studies, both mandibular third molars were extracted during the same operating session, with each side of the mouth allocated to either experimental or control treatment (Absi 1993; Arakji 2016; Butler 1977; Cerqueira 2004; Danda 2010; Eshghpour 2014; Gomes 2005; Greenwood 1994; Gulsen 2017; Haraji 2010; Hashemi 2012; Kapse 2019; Kirk 2007; Kumar 2016; Mantovani 2014; Mohajerani 2018; Ozgul 2015; Roode 2010; Saglam 2003; Sandhu 2010; Srinivas 2006; Sweet 1976; Xavier 2008). In two of these studies, maxillary third molars were also extracted in the same session (Absi 1993; Butler 1977). In the 23 split‐mouth studies where both mandibular third molars were extracted in a single session, we considered that the outcome of trismus if provided (on the seventh postoperative day) was not applicable since it was not possible to determine which side of the mouth was causing any difference in mouth opening. We considered that it was possible to ascribe differences in the outcomes of pain and swelling to the specific side of the mouth. We took the pairing of the data into account in the analysis.
In 14 of the remaining 15 split‐mouth studies, there was an interval of one week (Unsal 2018), two weeks (Baqain 2012; Mistry 2016; Topcu 2019), three weeks (Erdogan 2011; Gogulanathan 2015; Goldsmith 2012; Uyanik 2015), four weeks (or close to one month) (Acar 2017; Piersanti 2014; Rullo 2013; Şimşek Kaya 2019; Singh 2018), six weeks (Koyuncu 2015), or two months between the two extractions (Rakprasitkul 1997), which meant that pain and swelling had generally resolved prior to the extraction of the second tooth. However, the data in these studies were paired, and this was accounted for in the analysis of the data from these studies. In one split‐mouth study, no information was reported regarding the time interval between the two surgeries (Bhati 2017).
Characteristics of the participants
The included studies involved a total of 4643 participants, with individual studies recruiting between 10 and 380 participants (mean of 75 participants per study). In most of the included studies, participants were systemically healthy and without any indication of infection or inflammation surrounding the mandibular third molars. In one study, all participants had chronic pericoronitis (Baqain 2012).
In the majority of included studies (38 of the 62 studies), the mean age of participants was between 20 and 29 years. In 16 studies, the inclusion criteria specified an age range of approximately 18 to 50 years, but in the majority of these studies the mean age of participants was not reported (Basheer 2017; Briguglio 2011; Butler 1977; Chukwuneke 2008; Dutta 2016; Goldsmith 2012; Kapse 2019; Koyuncu 2015; Kumar 2016; Mohajerani 2018; Ozgul 2015; Pachipulusu 2018; Pasqualini 2005; Şimşek Kaya 2019; Srinivas 2006; Sweet 1976; Uyanik 2015; Xavier 2008). Two studies included participants with a mean age of 19 years (Haraji 2010; Roode 2010); two studies involved participants in their 30s (Barone 2010; Praveen 2007); and in two studies the age of participants was not reported (Gomes 2005; Greenwood 1994).
Characteristics of the interventions
The majority of included studies used a local anaesthetic. In four studies, all the procedures were done under general anaesthetic (Absi 1993; Greenwood 1994; Roode 2010; Sweet 1976); two studies used intravenous sedation in addition to local anaesthesia (Butler 1977; Kirk 2007); and three studies used either general anaesthetic or local anaesthetic in the same trial (Gomes 2005; Leung 2009; Renton 2005). The choice of anaesthetic was unclear in Mohajerani 2018 and Singh 2018; however, it is likely that local anaesthetic was used.
The studies covered a wide range of interventions and comparisons, which we have combined into nine groups that follow the steps of the surgical removal of third molars.
1. Surgical flap type
Fourteen included studies evaluated different types of incision or types of flap. The incision was described slightly differently in each of the trials. We have grouped similar comparisons together where possible.
Eleven trials compared triangular flaps of slightly different designs with an envelope or modified envelope flap (Baqain 2012; Briguglio 2011; Erdogan 2011; Haraji 2010; Kirk 2007; Koyuncu 2013; Mobilio 2017; Mohajerani 2018; Rabi 2017; Sandhu 2010; Şimşek Kaya 2019).
One trial compared a modified triangular flap with an alternative single incision flap (Roode 2010).
One trial compared the envelope flap with a pedicle flap (Goldsmith 2012).
One trial compared the modified envelope flap with a buccal comma‐shaped incision (Nageshwar 2002).
Triangular flap versus envelope or modified envelope flap (11 trials)
Seven trials compared a modified triangular flap with an envelope flap design (Haraji 2010; Kirk 2007; Koyuncu 2013; Mobilio 2017; Mohajerani 2018; Rabi 2017; Şimşek Kaya 2019). The modified triangular flap involved an incision from the distobuccal edge of the second molar dropping at a slight oblique angle and curving forward into the mandibular vestibule, and a second part was a relieving incision from the ramus to the distobuccal aspect of the second molar. The envelope flap involved a sulcular incision from the first to the second mandibular molar and a distal relieving incision along the external oblique ridge to the ramus. The Kirk 2007 study used a split‐mouth design in 32 participants who underwent surgery under local anaesthesia and intravenous conscious sedation. The Haraji 2010 study used a split‐mouth design in 17 participants who underwent surgery under local anaesthesia alone. Participants in Koyuncu 2013, Mobilio 2017, and Rabi 2017 underwent surgery under local anaesthesia.
The Baqain 2012, Briguglio 2011, and Erdogan 2011 studies compared a standard triangular flap with an envelope flap. The triangular flap technique was as described above in the modified triangular flap design but without the curving forward of the buccal oblique incision. The envelope flap design was the same as described in the Kirk 2007 and Haraji 2010 studies, except that the Briguglio 2011 study described a modified envelope design in which the incision finished at the mesial aspect of the second molar rather than continuing to the first molar. We determined that these minor modifications were of little clinical significance compared to the differences between triangular and envelope flaps and so grouped all five of these studies together. The Briguglio 2011 study compared two different minor modifications of an envelope flap with a triangular flap in 45 participants who underwent surgery under local anaesthesia. The Erdogan 2011 study used a split‐mouth design in 20 participants who underwent surgery under local anaesthesia with an interval of three weeks between one side and the other. The Baqain 2012 study used a split‐mouth design under local anaesthesia in 19 participants. Sandhu 2010 compared the bayonet flap with an envelope flap. This study used a split‐mouth cross‐over design in 20 participants who underwent surgery under local anaesthesia. For the bayonet flap, the incision was made as per a triangular flap but followed around the second molar sulcus until its buccal midpoint with the envelope flap. More specifically, the bayonet flap design incision started on the ascending ramus, following the centre of the third molar shelf to the disto‐buccal surface of the second molar and was then extended as a sulcular incision up to the midpoint of the buccal sulcus of the second molar, followed by an oblique vestibular extension. On further analysis, we decided that the 'bayonet flap' is technically a form of triangular flap.
'Long' and 'short' triangular flaps
In order to make best use of the data from the trials evaluating the flap design, we decided to group the 11 trials into two categories:
triangular flap (short) versus envelope (control) (Baqain 2012; Haraji 2010; Kirk 2007; Koyuncu 2013; Mohajerani 2018; Şimşek Kaya 2019);
triangular flap (long) versus envelope (control) (Briguglio 2011; Erdogan 2011; Mobilio 2017; Rabi 2017; Sandhu 2010).
A 'short' triangular flap consists of a two‐sided triangular flap that begins from the ramus of the mandible, extending to the disto‐buccal crown edge of the second molar, with a relieving (vertical or oblique) incision to the mucogingival line. A minor difference was detected in the intervention group of Mohajerani 2018 whereby the mesial incision is slightly distal to the second molar, therefore leaving a small strip of gingivae. A 'long' triangular flap featured relieving incisions that were placed anterior to the middle of the lower second molar (i.e. extending to the mesio‐buccal edge of the second molar, or the disto‐buccal edge of the first molar). The incision from the ramus was similar to that described for the 'short' triangular flap.
The other three trials each made slightly different comparisons. Goldsmith 2012 compared a pedicle flap with an envelope flap; Roode 2010 compared the modified triangular flap with a single incision flap; and Nageshwar 2002 compared a modified envelope incision with a comma incision.
Antibiotics were prescribed postoperatively to participants in the trials by Şimşek Kaya 2019 (amoxicillin 1000 mg twice a day for five days); Mohajerani 2018 (amoxicillin 500 mg three times per day for seven days); Rabi 2017 (amoxicillin 500 mg three times per day for three days); Koyuncu 2013 (amoxicillin 500 mg three times per day for seven days); and Haraji 2010 (oral cefalexin 500 mg four times per day for five days). Antibiotics were given preoperatively in the trials by Briguglio 2011 (1 g amoxicillin), Erdogan 2011 (penicillin), and Sandhu 2010 (intravenous amoxicillin with clavulanic acid). In the Nageshwar 2002 trial, antibiotics were "prescribed as indicated".
Pedicle flap versus envelope flap (one trial)
Goldsmith 2012 compared a pedicle flap design with the envelope flap. For the pedicle flap, an incision distal to the third molar was extended approximately 1 cm and then curved towards the buccal sulcus allowing for rotation of the flap and primary closure over sound bone. Prior to closure, the gingival papilla distal to the second molar was removed and the apex of the pedicle de‐epithelialised. A lingual flap was raised in the subperiosteal plane irrespective of flap design and the lingual nerve protected using a Howarth retractor. This study used a split‐mouth cross‐over design in 52 participants who underwent surgery under local anaesthesia and intravenous conscious sedation.
Modified triangular flap versus alternative single incision flap (one trial)
Roode 2010 compared the modified triangular flap as described above with a newly described alternative design using only a single straight incision about 15 mm in length and beginning 5 mm distal of the second molar and running mesio‐buccally towards the sulcus adjacent to the second molar. Thirty‐three participants underwent surgery under general anaesthesia in this split‐mouth study.
Buccal comma‐shaped incision versus modified envelope flap (one trial)
Nageshwar 2002 compared a newly described buccal comma‐shaped incision with the modified envelope flap described above. Before starting the comma‐shaped incision, the buccal vestibule below the adjacent second molar was stretched down as far as possible with the index finger or thumb of the hand not holding the scalpel to stretch the buccinator beyond its origin on the mandible. Starting from a point at the depth of this stretched vestibule reflection posterior to the distal aspect of the preceding second molar, the incision was made in an anterior direction. The incision was made to a point below the second molar, from where it was smoothly curved up to meet the gingival crest at the disto‐buccal line angle of the second molar. The incision was continued around as a crevicular incision around the distal aspect of the second molar. This study used a parallel‐group design in 100 participants who underwent surgery under local anaesthesia.
2. Lingual nerve protection
An instrument may be placed between distolingual bone to be removed to enable elevation of an impacted tooth and a lingual mucoperiosteal flap enclosing the nerve. The intention is to thereby protect the lingual nerve from physical injury during bone removal. Whilst the intention is to prevent permanent lingual nerve injury, some surgeons have advocated using no lingual nerve protection because instrument placement may be associated with temporary nerve injury.
There were four studies in this group, of which three compared the use of a retractor with no retractor (Gargallo‐Albiol 2000; Gomes 2005; Shad 2015), and one compared two types of retractor (Greenwood 1994).
Lingual nerve retractor versus no retractor (three trials)
Three studies compared the surgical removal of wisdom teeth with or without the use of a retractor for protection of the lingual nerve (Gargallo‐Albiol 2000; Gomes 2005; Shad 2015). In one of these studies, the surgery was undertaken under local anaesthesia alone at the University of Barcelona, Spain, and the type of retractor used was not specified (Gargallo‐Albiol 2000). In Gomes 2005, the surgery was undertaken under local anaesthesia or general anaesthesia with local anaesthesia at the University of Pernambuco, Camaragibe, Brazil, and a Free's elevator was used. In the trial by Shad 2015, surgery was performed under local anaesthetic, and the authors did not describe the type of retractor used to retract the lingual flap.
Broad retractor versus conventional (Howarth) lingual flap retractor (one trial)
Greenwood 1994 compared the use a wider retractor with a conventional Howarth periosteal elevator for protection of the lingual nerve within the lingual flap. All participants in this study underwent surgery under day‐case general anaesthesia.
3. Bone removal techniques
Thirteen studies reported comparisons of different bone removal surgical techniques for the removal of mandibular wisdom teeth.
Bone removal with lingual split with chisel versus bur (three trials)
Distolingual bone obstructing the surgical removal of an impacted wisdom tooth may be removed with a chisel and surgical mallet in a 'distal split' technique or by using a surgical bur. Three studies compared these different surgical techniques (Absi 1993; Mocan 1996; Praveen 2007). The lingual split technique involves making a vertical cut in the buccal bone with a mono bevel chisel distal to the second molar. A second horizontal cut is made to join the first posteriorly. The bone removed allows access to the mesio‐buccal aspect of the impacted tooth and permits a point of application with an elevator. The bevel of the chisel is then turned lingually and a 'lingual split' is made, removing a disto‐lingual piece of bone, which allows the tooth to be elevated. The depth is controlled by angling the chisel between vertical and 45° buccolingual during removal of the lingual cortex. When bone is removed with a bur, a rose‐head bur or similar bur is electrically powered, usually at a speed of 40,000 revolutions per minute (rpm), and irrigation is used. In the Absi 1993, Mocan 1996, and Praveen 2007 studies, the lingual nerve was protected by a Howarth's periosteal elevator.
The Absi 1993 study used a split‐mouth cross‐over design in 52 participants who underwent surgery under general anaesthesia. The Mocan 1996 study used a parallel‐group design in 20 participants who underwent surgery under local anaesthesia. The Praveen 2007 study used a parallel‐group design in 90 participants who underwent surgery under local anaesthesia.
Bone removal with ultrasonic tools versus surgical bur (10 trials)
Ten studies compared the use of ultrasonic surgery with traditional rotary instruments (drill and surgical bur) for bone removal in lower third molar surgery (Arakji 2016; Barone 2010; Basheer 2017; Bhati 2017; Mantovani 2014; Mistry 2016; Piersanti 2014; Rullo 2013; Topcu 2019; Uyanik 2015). Surgical fissure burs were used to section the teeth, where necessary, in both the control and experimental groups. All surgery was carried out by the same surgeon, under local anaesthesia.
Barone 2010 had a parallel‐group design and evaluated 26 participants who underwent surgery under local anaesthesia. Rullo 2013 had a split‐mouth cross‐over design and evaluated 52 participants who underwent surgery under local anaesthesia. Six studies had a split‐mouth design: Mantovani 2014 (125 participants); Piersanti 2014 (10 participants); Uyanik 2015 (20 participants); Arakji 2016 (20 participants); Mistry 2016 (30 participants); and Bhati 2017 (30 participants). In Topcu 2019, also a split‐mouth trial design, no teeth required sectioning. In Basheer 2017, 30 participants were randomised to two parallel arms.
When updating this review, we found new studies in which piezoelectric surgery/ultrasonic was compared with rotary burs (Arakji 2016; Basheer 2017; Bhati 2017; Mantovani 2014; Mistry 2016; Piersanti 2014; Topcu 2019; Uyanik 2015). This indicates that piezoelectric surgery/ultrasonic is an area of active research in the oral surgery community. However, data from Mantovani 2014 and Uyanik 2015 could not be combined with other studies as they were not presented in useable format (Table 10; Table 11; Table 12).
4. Wound irrigation techniques
Two studies were conducted and reported during the 1970s.
Mechanical versus manual surgical wound irrigation (one trial)
Sweet 1976 compared two different modes of application of postsurgical lavage: an electrically driven, mechanical irrigator (Water Pik Model 47, 120 volt, 60 cycle) at a preset pressure of 45 pound‐force per square inch (psi) versus a conventional hand syringe (50‐millilitre disposable syringe with a 15‐gauge needle). Both used the same volume (350 mL) of sterile saline, and the sockets were irrigated immediately after extraction.
Different manual irrigation volumes (one trial)
A single study compared the use of 175 mL sterile saline after an extraction with a much smaller volume of "no more than 25 ml" sterile saline in a split‐mouth trial (Butler 1977). There were 211 participants, each having bilateral mandibular wisdom teeth removed under intravenous conscious sedation by the same operator.
5. Primary versus secondary wound closure
Primary versus secondary closure of surgical wound (nine trials)
Wound closure techniques may consist of total closure in which the mucoperiosteum is hermetically sealed and healing occurs by primary intention, or partial closure in which a window exists or is created to allow healing by secondary intention. With the latter technique, some sutures may be required or no sutures depending on the flap design. Eight included studies evaluated primary versus secondary wound closure techniques (Bello 2011; Danda 2010; Hashemi 2012; Osunde 2011a; Osunde 2012; Pachipulusu 2018; Pasqualini 2005; Refo'a 2011; Xavier 2008).
In the Pasqualini 2005 study, primary closure was obtained after repositioning the flap and suturing hermetically, and secondary closure by removing a wedge of mucosa distal to the second molar and by suturing. This study used a parallel‐group design in 200 participants who underwent surgery under local anaesthesia. In the Xavier 2008 study, primary closure was obtained after repositioning the flap and suturing completely, and secondary closure by placing sutures for partial wound closure. This study used a parallel‐group design in 40 participants who underwent surgery under local anaesthesia. In the Danda 2010 study, primary closure was obtained using two sutures on the distal arm of the incision, and secondary closure by removing a wedge of mucosa distal to the second molar and by placing a single suture on the mesial arm of the incision and another on the distal arm. This study used a split‐mouth cross‐over design in 93 participants who underwent surgery under local anaesthesia. In the Bello 2011 study, primary closure was obtained after repositioning the flap and suturing completely with five sutures, and secondary closure by leaving a window in the wound and placing four sutures. This study used a parallel‐group design in 82 participants who underwent surgery under local anaesthesia. In the Osunde 2011a study, primary closure was obtained after repositioning the flap and suturing completely with multiple sutures, and secondary closure by leaving a window in the wound and placing a single suture in the distal relieving incision. This study used a parallel‐group design in 50 participants who underwent surgery under local anaesthesia. In the Refo'a 2011 study, primary closure was obtained after repositioning the flap and suturing completely, and secondary closure by leaving open the distal extension to the second molar but suturing the other parts of the flap. This study used a parallel‐group design in 32 participants who underwent surgery under local anaesthesia. In the Hashemi 2012 study, primary closure was obtained after repositioning the flap and suturing completely with three sutures, and secondary closure by placing no sutures. This study used a split‐mouth design in 30 participants who underwent surgery under local anaesthesia. In the Osunde 2012 study, primary closure was obtained after repositioning the flap and suturing completely with multiple sutures, and secondary closure by placing no sutures. This study used a parallel‐group design in 80 participants who underwent surgery under local anaesthesia. In the Pachipulusu 2018 study, a parallel‐group RCT with 30 participants in each group, the technique used was similar to that used by Pasqualini 2005 and Danda 2010.
6. Suturing techniques
Two studies reported comparisons of suturing techniques (two trials).
Primary closure: horizontal mattress versus single interrupted (one trial)
Acar 2017 included 30 participants in a split‐mouth study with a four‐week interval between the two surgeries; pain, swelling and trismus were considered in the postsurgery phase. We were not able to use data from this study in analysis (see Table 10; Table 11; Table 12).
Suturing versus fibrin sealant (one trial)
In Gogulanathan 2015, 30 participants were included in a split‐mouth trial in which fibrin sealant compared with conventional suturing and procedures were carried out under local anaesthesia.
7. Surgical drain versus no drain
Eight studies reported comparisons of surgical drain techniques.
Seven studies compared a tube drain with no drain (Cerqueira 2004; Chukwuneke 2008; Koyuncu 2015; Kumar 2016; Rakprasitkul 1997; Saglam 2003; Srinivas 2006), and one study compared the use of a gauze drain with no drain (de Brabander 1988).
In de Brabander 1988, a simple drain made of Vaseline‐coated gauze was placed into the socket, which was compared with using no drain in a parallel‐group study.
8. Wound closure with autologous platelet concentrates
Eight trials reported the comparisons of wound closure with the use of blood products (platelet rich fibrin (PRF) and platelet rich plasma (PRP)).
Platelet rich plasma versus none (one trial)
Dutta 2016 included 40 participants in four parallel groups. The PRP group included 10 participants, in which the extraction socket was filled with PRP before closure of the sockets. Extraction of mandibular third molars was performed under local anaesthesia using standard techniques.
Platelet rich fibrin versus none (seven trials)
In Eshghpour 2014, 78 participants were included in a split‐mouth trial comparing the placement of PRF with no blood products in the extraction socket. In Ozgul 2015, 56 participants were included in multicentre split‐mouth trials. Dutta 2016 included 40 participants in four parallel groups. The PRF group included only 10 of the 40 participants, in which the extraction socket was filled with PRF before closure. The other groups had 10 participants and were control, PRP, and hydroxyapatite. In Gulsen 2017, 30 participants were included in a split‐mouth study; the socket on the intervention side was filled with three pieces of PRF membrane following extraction of the tooth. Kapse 2019 included 30 participants in a split‐mouth study, with PRF placed in the socket on one side following the surgical extraction. Primary closure of the socket was then completed. In the study by Unsal 2018, 50 participants took part in a split‐mouth study, with PRF placed on the experimental side. The type of wound closure was not mentioned.
Data from two further included studies could not be used in data analysis, as the outcome data were presented in unuseable formats (these are summarised in Table 10; Table 11; Table 12) (Kumar 2015; Uyanik 2015). Kumar 2015 included 31 participants in a parallel trial, in which 16 participants in the intervention group (PRF placed into the extraction socket followed by flap approximation) were evaluated against 15 participants in the control group where no blood products were placed. In Uyanik 2015, 20 participants were included in a split‐mouth trial. Ten of the participants received PRF; the PRF was placed in the socket after extraction and compared against no blood product in the control group.
9. Root retention techniques
There were no trials of partial root retention versus whole root retention (coronectomy). There were two trials that assessed the comparison of coronectomy versus complete tooth removal, but we did not consider the data from these studies to be sufficiently reliable for inclusion in the analysis (Leung 2009; Renton 2005). Coronectomy involved transection of the tooth 3 to 4 mm below the enamel of the crown into the dentine. The pulp was then left in place after the crown had been levered off, and received no treatment other than a saline rinse and the re‐apposition of the muco‐periosteal flap. Coronectomy is designed to leave the apices of lower third molars intact if they are in immediate proximity to the inferior alveolar nerve as predicted by radiographic features. In both studies, participants were chosen due to radiographic signs of a close proximity of the tooth to the inferior alveolar nerve using plain radiographs (orthopantomograph).
We did include one new study in this update that involved 30 participants in a parallel‐group RCT comparing coronectomy with complete tooth removal (Singh 2018). The technique in this study was very similar to that described in the studies by Leung 2009 and Renton 2005. Participants were chosen based on the high‐risk signs seen on plain radiographs as described in Rood 1990. One participant had a cone‐beam computed tomography (CT) scan to further assess the anatomical relationship between the third molar and the inferior dental canal. Fifteen participants had a coronectomy, and 15 had complete tooth removal.
Characteristics of outcome measures
Primary outcome measures
Alveolar osteitis was reported by 22 studies (Baqain 2012; Bello 2011; Bhati 2017; Butler 1977; Danda 2010; de Brabander 1988; Dutta 2016; Eshghpour 2014; Goldsmith 2012; Haraji 2010; Hashemi 2012; Kirk 2007; Koyuncu 2013; Leung 2009; Mocan 1996; Mohajerani 2018; Pasqualini 2005; Refo'a 2011; Renton 2005; Şimşek Kaya 2019; Sweet 1976; Unsal 2018).
Wounds becoming infected (presence of pus) was reported by 10 studies (Absi 1993; Baqain 2012; Bello 2011; Briguglio 2011; Goldsmith 2012; Hashemi 2012; Refo'a 2011; Roode 2010; Sandhu 2010; Sweet 1976).
Permanent (more than six months) altered tongue sensation was reported by two studies (Briguglio 2011; Shad 2015).
Permanent (more than six months) altered chin skin or lower lip sensation was reported by two studies (Leung 2009; Renton 2005).
Adverse effects such as fracture of the mandible were not reported in any study.
In split‐mouth studies where the two interventions were delivered during the same surgical session and the outcome of alveolar osteitis was reported, we assumed events were unilateral, unless otherwise stated (Danda 2010; Haraji 2010; Kirk 2007). We received confirmation that alveolar osteitis was unilateral in four studies (Goldsmith 2012; Roode 2010; Sandhu 2010; Sweet 1976).
Likewise in Baqain 2012 and Sandhu 2010, we assumed that wound dehiscence was unilateral, but we were unable to confirm this.
Secondary outcome measures
Temporary altered tongue sensation (only the time point closer to one‐month postoperatively was used) (Absi 1993; Gargallo‐Albiol 2000; Gomes 2005; Greenwood 1994; Leung 2009; Mocan 1996; Praveen 2007; Shad 2015).
Temporary altered chin skin or lower lip sensation (only the time point closer to one‐month postoperatively was used) (Absi 1993; Leung 2009; Mocan 1996; Renton 2005).
Postoperative pain (24 hours postextraction) (Absi 1993; Acar 2017; Arakji 2016; Baqain 2012; Basheer 2017; Bello 2011; Bhati 2017; Briguglio 2011; Cerqueira 2004; Chukwuneke 2008; Dutta 2016; Gogulanathan 2015; Goldsmith 2012; Gulsen 2017; Hashemi 2012; Kapse 2019; Kirk 2007; Koyuncu 2013; Koyuncu 2015; Kumar 2015; Kumar 2016; Mantovani 2014; Mistry 2016; Mobilio 2017; Nageshwar 2002; Osunde 2011a; Osunde 2012; Ozgul 2015; Pachipulusu 2018; Pasqualini 2005; Piersanti 2014; Praveen 2007; Rabi 2017; Rakprasitkul 1997; Rullo 2013; Saglam 2003; Sandhu 2010; Şimşek Kaya 2019; Srinivas 2006; Topcu 2019; Unsal 2018; Uyanik 2015; Xavier 2008).
Swelling (one‐week postextraction) (Absi 1993; Acar 2017; Arakji 2016; Baqain 2012; Basheer 2017; Bello 2011; Bhati 2017; Briguglio 2011; Cerqueira 2004; Chukwuneke 2008; Danda 2010; Dutta 2016; Gogulanathan 2015; Goldsmith 2012; Gulsen 2017; Hashemi 2012; Kapse 2019; Kumar 2015; Kumar 2016; Mantovani 2014; Mistry 2016; Mobilio 2017; Nageshwar 2002; Osunde 2011a; Osunde 2012; Ozgul 2015; Pachipulusu 2018; Pasqualini 2005; Piersanti 2014; Praveen 2007; Rakprasitkul 1997; Roode 2010; Saglam 2003; Sandhu 2010; Şimşek Kaya 2019; Singh 2018; Srinivas 2006; Sweet 1976; Uyanik 2015; Xavier 2008). Some studies included data where swelling was measured from the angle of the mouth to the tragus of the ear in millimetres, whilst other studies used methods including proportional swelling based on preoperative and postoperative measurements (see Characteristics of included studies).
Restricted mouth opening (one‐week postextraction) (Absi 1993; Acar 2017; Arakji 2016; Baqain 2012; Basheer 2017; Bello 2011; Bhati 2017; Briguglio 2011; Cerqueira 2004; Chukwuneke 2008; Erdogan 2011; Gogulanathan 2015; Kirk 2007; Koyuncu 2013; Koyuncu 2015; Kumar 2015; Kumar 2016; Mistry 2016; Nageshwar 2002; Osunde 2011a; Osunde 2012; Pachipulusu 2018; Rabi 2017; Rakprasitkul 1997; Saglam 2003; Sandhu 2010; Şimşek Kaya 2019; Singh 2018; Srinivas 2006; Uyanik 2015; Xavier 2008).
In split‐mouth studies where a different intervention was used on each side of the mouth during the same surgical session, we considered that outcomes of pain and trismus, or the presence or absence of swelling, could not be reliably ascribed to an intervention, so we did not use these data (Cerqueira 2004; Hashemi 2012; Saglam 2003; Srinivas 2006; Sweet 1976). In split‐mouth studies where the sides of the mouth were treated in two separate sessions at least two weeks apart, we used the pain and trismus outcome data that were reported.
We were unable to use data from some included studies because they were presented in unuseable format; summaries of these data can be found in Table 10; Table 11; Table 12.
Excluded studies
We excluded a total of 67 studies (70 references) after full‐text assessment by at least two review authors. Reasons for exclusion for each study are described in Characteristics of excluded studies. In general, the reasons for exclusion were: study found not be to an RCT after review of the full published reports; study design unclear, and attempts to contact the authors for clarification were unsuccessful; full‐report publication was not found, and the abstract contained insufficient information to assess eligibility; the study was confounded due to two or more concurrent interventions; the study involved the surgical removal of both maxillary and mandibular third molars at the same time; the study participants did not have a flap raised, and the extraction was a non‐surgical procedure; the outcome reported in the study was periodontal indices in the months following surgery, which is not an outcome of interest in this review; in three studies the intervention was germectomy rather than third molar extraction.
Risk of bias in included studies
See Figure 1.
Allocation
Sequence generation
Twenty three studies (37%) clearly described the methods used to generate the randomised sequence and were assessed as at low risk of bias for this domain (Arakji 2016; Baqain 2012; Barone 2010; Bello 2011; Briguglio 2011; Erdogan 2011; Gogulanathan 2015; Goldsmith 2012; Greenwood 1994; Kumar 2015; Kumar 2016; Leung 2009; Mantovani 2014; Nageshwar 2002; Pasqualini 2005; Refo'a 2011; Renton 2005; Roode 2010; Rullo 2013; Sandhu 2010; Shad 2015; Şimşek Kaya 2019; Sweet 1976). The remaining 39 studies did not report details concerning the methods of randomisation and were therefore assessed as at unclear risk of bias for this domain.
Allocation concealment
Sixteen studies (24%) described adequate concealment of allocation and were assessed as at low risk of bias for this domain ( Absi 1993; Barone 2010; Bello 2011; Briguglio 2011; de Brabander 1988; Gogulanathan 2015; Goldsmith 2012; Greenwood 1994; Kumar 2015; Leung 2009; Mantovani 2014; Pasqualini 2005; Refo'a 2011; Renton 2005; Sandhu 2010; Şimşek Kaya 2019). The remaining studies provided insufficient information to enable a clear judgement and were therefore assessed as at unclear risk of bias for this domain.
Blinding
It is important to note that participant blinding was unrealistic in many of these studies due to the surgery being carried out under local anaesthetic or with only light sedation. We considered that the blinding of outcome assessment was both possible and important to reduce the risk of detection bias. Where trials were described as double‐blind, we interpreted this as meaning that both the participant and outcome assessor were blinded to the allocated intervention. Where the person assessing the outcomes was the same surgeon who performed the procedure, or where blinded outcome assessment was not mentioned, we considered the risk of detection bias to be high.
In 27 studies (44%), participants were blinded to the allocated intervention or it was considered that lack of participant blinding was not associated with a risk of bias due to the nature of the intervention. We assessed these trials as at low risk of performance bias (Absi 1993; Barone 2010; Bello 2011; Briguglio 2011; Butler 1977; Erdogan 2011; Goldsmith 2012; Greenwood 1994; Haraji 2010; Hashemi 2012; Kirk 2007; Koyuncu 2013; Leung 2009; Mocan 1996; Mohajerani 2018; Nageshwar 2002; Osunde 2011a; Osunde 2012; Pasqualini 2005; Rabi 2017; Refo'a 2011; Renton 2005; Roode 2010; Saglam 2003; Sandhu 2010; Sweet 1976; Xavier 2008). We assessed the risk of performance bias in 10 trials as high due to the lack of participant blinding and self‐assessment by participants of pain outcomes (Cerqueira 2004; Chukwuneke 2008; Danda 2010; de Brabander 1988; Gargallo‐Albiol 2000; Koyuncu 2015; Kumar 2015; Rakprasitkul 1997; Srinivas 2006; Uyanik 2015). In the remaining trials, participant blinding was assessed as at unclear risk of bias.
Twenty‐three studies (37%) clearly described blinded outcome assessment (or provided information upon request) and were assessed as at low risk of bias for this domain (Absi 1993; Briguglio 2011; Erdogan 2011; Eshghpour 2014; Goldsmith 2012; Gomes 2005; Greenwood 1994; Haraji 2010; Kapse 2019; Koyuncu 2013; Koyuncu 2015; Mantovani 2014; Mobilio 2017; Mohajerani 2018; Nageshwar 2002; Osunde 2011a; Osunde 2012; Ozgul 2015; Pasqualini 2005; Sandhu 2010; Şimşek Kaya 2019; Sweet 1976; Xavier 2008). In 20 studies, there was insufficient information to determine whether outcome assessors were blinded, and these studies were assessed as at unclear risk of bias for this domain (Acar 2017; Arakji 2016; Barone 2010; Basheer 2017; Bello 2011; Bhati 2017; Chukwuneke 2008; de Brabander 1988; Dutta 2016; Gogulanathan 2015; Gulsen 2017; Kumar 2015; Kumar 2016; Mistry 2016; Pachipulusu 2018; Shad 2015; Singh 2018; Topcu 2019; Unsal 2018; Uyanik 2015). We assessed the remaining 19 studies as at high risk of bias for this domain because outcome assessors were not blinded to the allocated interventions.
Incomplete outcome data
In 50 studies (81%), outcome data were complete or the numbers lost were less than 10% in split‐mouth studies, so we assessed the risk of attrition bias as low. Ten studies did not clearly report the number of participants included in the outcome assessment and were therefore assessed as at unclear risk of attrition bias (Danda 2010; de Brabander 1988; Haraji 2010; Mocan 1996; Mohajerani 2018; Osunde 2011a; Ozgul 2015; Praveen 2007; Refo'a 2011; Rullo 2013). In Leung 2009, 9% of teeth in the coronectomy group were excluded from the outcome assessments due to "failed coronectomy". The authors supplied some of these missing data, but we assessed the risk of attrition bias as unclear in this study. In Renton 2005, the numbers of teeth included in the outcome assessment varied due to the exclusion of the "failed coronectomy group" despite a planned intention‐to‐treat analysis, and there was a significant loss to follow‐up that was not explained. We considered the risk of attrition bias in this study to be high.
Selective reporting
We assessed the risk of reporting bias as low in 48 studies (77%), as the outcomes prespecified in the methods sections were reported in full, or this information was supplied by study authors.
In two studies, outcomes were reported incompletely, that is as graphs without numerical data and estimates of variance (Mocan 1996; Refo'a 2011), and in a further two studies (Haraji 2010; Hashemi 2012), some outcomes were not reported, and it appeared likely that the paired nature of the data had not been accounted for in the analysis. Based on the published report, it seems likely that attempts were made to measure swelling and trismus in Rullo 2013, but these outcomes were not reported in full because the measures were "not reproducible". In Renton 2005 and Leung 2009, outcomes were not reported for each randomised group of participants; instead the denominator was teeth, and the effects of paired teeth were not accounted for in the analysis. We assessed these seven studies as at high risk of reporting bias. There was insufficient information presented In the remaining seven studies on which to base a judgement, therefore we assessed these studies as at unclear risk of reporting bias (Butler 1977; Goldsmith 2012; Gomes 2005; Nageshwar 2002; Osunde 2011a; Praveen 2007; Xavier 2008).
Other potential sources of bias
We identified other sources of bias in nine studies in this review (15%). In Butler 1977, the irrigation fluid was delivered by either a mechanical irrigation device or by hand, a confounding factor that could have introduced bias. Also, several participants in this study underwent concurrent extraction of maxillary third molars. It was likely that multiple tooth extraction carried a higher risk of alveolar osteitis, and should therefore be considered as a confounding factor in an unknown number of participants in each group. In Greenwood 1994, the method of bone removal was not standardised: "the tooth was then removed employing either drill or chisel for bone removal, according to the operator's personal preference". The bone removal technique could possibly have confounded the results, and it was not recorded how many in each group had bone removal by each technique. Mocan 1996 had a small sample size, with 10 participants in each group, and a different distribution of impactions in the two intervention groups at baseline. The study report by Rullo 2013 contained contradictory information in the text and the tables. The Basheer 2017 study only included male participants, therefore the results are limited to this study population. In Dutta 2016, there was a potential source of other bias due to inconsistencies in the methodology, namely the surgical approach: the method states "a triangular flap using ward‐I or ward‐II incision or an envelope flap was raised". In Mistry 2016, the carry‐over effect was not analysed, and the grouping of participants was reported to be randomised (piezoelectric surgery versus conventional technique); however, it was not mentioned if the side that was chosen for the test/control was randomised. In Briguglio 2011, some participants had unilateral extractions, whilst others had bilateral extractions. This could have influenced outcomes such as pain perception and trismus. In the study by Gulsen 2017, the authors noted that "Bilateral removal of the third molar was performed in a single appointment. For the study side, the sockets were filled with PRF, whereas for the control side, the sockets were left empty". We felt that as both procedures were carried out at the same time in this split‐mouth study, this could have affected participant perception of pain. We assessed these studies as being at high risk of other bias. We assessed 30 studies (48%) as at low risk of other bias (Acar 2017; Baqain 2012; Barone 2010; Bello 2011; Cerqueira 2004; Danda 2010; Erdogan 2011; Eshghpour 2014; Gargallo‐Albiol 2000; Goldsmith 2012; Hashemi 2012; Kapse 2019; Kirk 2007; Koyuncu 2013; Kumar 2015; Mantovani 2014; Mohajerani 2018; Nageshwar 2002; Osunde 2011a; Osunde 2012; Pasqualini 2005; Praveen 2007; Refo'a 2011; Roode 2010; Saglam 2003; Sandhu 2010; Shad 2015; Şimşek Kaya 2019; Srinivas 2006; Sweet 1976). In the other studies, the risk of other bias was unclear.
Overall risk of bias
None of the studies included in this review was assessed as at low risk of bias across all domains. In half of the studies (31 studies, 50%), at least one domain was assessed as at high risk of bias (Baqain 2012; Barone 2010; Basheer 2017; Briguglio 2011; Butler 1977; Cerqueira 2004; Chukwuneke 2008; Danda 2010; Dutta 2016; Gargallo‐Albiol 2000; Greenwood 1994; Gulsen 2017; Haraji 2010; Hashemi 2012; Kirk 2007; Koyuncu 2015; Kumar 2015; Leung 2009; Mistry 2016; Mocan 1996; Piersanti 2014; Praveen 2007; Rakprasitkul 1997; Refo'a 2011; Renton 2005; Roode 2010; Rullo 2013; Saglam 2003; Sandhu 2010; Srinivas 2006; Uyanik 2015). In the other 31 studies, the overall risk of bias was unclear.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9
Summary of findings 1. Choice of surgical flap type for the removal of mandibular wisdom teeth.
| Triangular flap compared with envelope flap for the removal of mandibular wisdom teeth | ||||||
|
Population: adults with mandibular third molars requiring removal Setting: oral surgery Intervention: triangular flap1 Comparison: envelope flap | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Envelope flap | Triangular flap | |||||
|
Alveolar osteitis (1‐week follow‐up) |
132 per 10002 | 48 per 1000 (19 to 73) | OR 0.33 (0.09 to 1.23) | 187 (5 studies) | ⊕⊕⊝⊝ low3 | Triangular (short) vs envelope. Insufficient evidence to claim either is better |
|
Wound infection (1‐week follow‐up) |
46 per 10002 | 14 per 1000 (2 to 90) | OR 0.29 (0.04 to 2.06) | 65 (2 studies) | ⊕⊕⊝⊝ low4 | Triangular (long) vs envelope. Insufficient evidence to claim either is better |
|
Permanent altered tongue, chin, or lip sensation (more than 6 months) |
20 per 1000 2 | 90 per 1000 (1 to 1000) | Peto OR 4.48 (0.07 to 286.49) | 45 (1 study) | ⊕⊝⊝⊝ verylow5 | Triangular (long) vs envelope. Insufficient evidence to claim either is better |
|
Adverse effects ‐ reactionary bleeding (up to 30 days) |
Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OD: odds ratio | ||||||
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1A further four studies evaluated other flap design comparisons but did not report outcome data suitable for inclusion in meta‐analysis. The narrative results of these studies are reported in Effects of interventions. 2Incidence estimated by median of envelope flap group. 3Certainty of evidence downgraded twice due to studies at high or unclear risk of bias and high heterogeneity and imprecision. 4Certainty of evidence downgraded twice due to studies at high or unclear risk of bias and imprecision. 5Certainty of evidence downgraded three times due to single small study at high risk of bias with imprecision.
Summary of findings 2. Lingual nerve protection during the removal of mandibular wisdom teeth.
| Retractor compared with no retractor during the removal of mandibular wisdom teeth | ||||||
|
Patopulation: adults with mandibular third molars requiring removal Setting: oral surgery Intervention: lingual retractor placed (subperiosteal or Free's) Comparison: no retractor | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| No retractor | Retractor | |||||
|
Alveolar osteitis (1‐week follow‐up) |
Not reported | |||||
|
Wound infection (1‐week follow‐up) |
Not reported | |||||
|
Permanent altered tongue, chin, or lip sensation (more than 6 months) |
5 per 10001 | 1 per 1000 (0 to 33) | Peto OR 0.14 (0.00 to 6.82) | 380 (1 study) |
⊕⊝⊝⊝ verylow2 | Insufficient evidence to claim either is better |
|
Adverse effects ‐ reactionary bleeding (up to 30 days) |
Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio | ||||||
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Assumed risk based on control group. 2Downgraded three times due to single study, unclear risk of bias, low event rates, and imprecision of estimate.
Summary of findings 3. Bone removal techniques for the removal of mandibular wisdom teeth.
| Bone removal techniques for the removal of mandibular wisdom teeth | ||||||
| Population: adults with mandibular third molars requiring removal Setting: oral surgery Intervention: bone removal techniques Comparison: conventional technique | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Bone removal with bur | Intervention bone removal technique | |||||
|
Alveolar osteitis (1‐week follow‐up) |
Not reported | |||||
|
Wound infection (1‐week follow‐up) |
58 per 10001 | 58 per 1000 (19 to 165) |
OR 1.00 (0.31 to 3.21) | 52 (1 study) |
⊕⊝⊝⊝ verylow2 | The intervention used lingual split with chisel. Insufficient evidence to claim either is better |
|
Permanent altered tongue, chin, or lip sensation (more than 6 months) |
Not reported | |||||
|
Adverse effects ‐ reactionary bleeding (up to 30 days) |
Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio | ||||||
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1From study control group. 2Certainty of evidence downgraded three times due to single study at high risk of bias with a small number of events and imprecision.
Summary of findings 4. Wound irrigation techniques (A compared to B) for the removal of mandibular wisdom teeth.
| Irrigation techniques (A compared to B) following the removal of mandibular wisdom teeth | ||||||
| Population: adults with mandibular third molars requiring removal Setting: oral surgery Intervention: irrigation technique A Comparison: irrigation technique B | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Irrigation technique B | Irrigation technique A | |||||
| Manual irrigation (low volume) | Mechanical irrigation (high volume) | |||||
|
Alveolar osteitis (up to 1‐week follow‐up) |
10 per 10001 | 3 per 1000 (0 to 81) | RR 0.33 (0.01 to 8.09) | 99 (1 study) | ⊕⊝⊝⊝ verylow2 | Single split‐mouth study. Insufficient evidence to claim either is better |
|
Wound infection (up to 1‐week follow‐up) |
20 per 10001 | 10 per 1000 (10 to 109) | RR 0.5 (0.05 to 5.43) | 99 (1 study) | ⊕⊝⊝⊝ verylow2 | Insufficient evidence to claim either is better |
|
Permanent altered tongue, chin, or lip sensation (more than 6 months) |
Not reported | |||||
|
Adverse effects (up to 30 days) |
Not reported | |||||
| Mechanical irrigation (low volume versus high volume) | ||||||
|
Low volume (approximately 25 mL) |
High volume (approximately 175 mL) |
|||||
|
Alveolar osteitis (up to 1‐week follow‐up) |
10 per 10001 | 5 per 1000 (3 to 10) | RR 0.52 (0.27 to 1.02) | 211 (1 study) | ⊕⊝⊝⊝ very low2 | Insufficient evidence to claim either is better |
|
Wound infection (up to 1‐week follow‐up) |
28 per 10001 | 5 per 1000 (1 to 38) | RR 0.17 (0.02 to 1.37) | 211 (1 study) | ⊕⊝⊝⊝ very low2 | Insufficient evidence to claim either is better |
|
Permanent altered tongue, chin, or lip sensation (more than 6 months) |
Not reported | |||||
|
Adverse effects (up to 30 days) |
Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio | ||||||
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Asssumed risk from the single study. 2Certainty of evidence downgraded three times due to single study at either high or unclear risk of bias and imprecision.
Summary of findings 5. Primary versus secondary wound closure after the removal of mandibular wisdom teeth.
| Primary versus secondary wound closure after the removal of mandibular wisdom teeth | ||||||
|
Population: adults with mandibular third molars requiring removal
Setting: oral surgery
Intervention: primary (complete) wound closure Comparison: secondary (partial) wound closure | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Secondary wound closure | Primary wound closure | |||||
| Alveolar osteitis (up to 1‐week follow‐up) | 43 per 10001 | 43 per 1000 (18 to 103) | RR 0.99 (0.41 to 2.40) | 375 (3 studies) |
⊕⊕⊝⊝ low2 | Insufficient evidence to claim either is better |
| Wound infection (up to 1‐week follow‐up) | 50 per 10003 | 13 per 1000 | RR 4.77 (0.24 to 96.34) | 82 (1 study) |
⊕⊝⊝⊝ verylow4 | Insufficient evidence to claim either is better |
|
Permanent altered tongue, chin, or lip sensation (more than 6 months) |
Not reported | |||||
|
Adverse effects ‐ reactionary bleeding (up to 30 days) |
175 per 10001 | 72 per 1000 (19 to 257) | RR 0.41 (0.11 to 1.47) | 82 (1 study) | ⊕⊝⊝⊝ very low4 | Insufficient evidence to claim either is better |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio | ||||||
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Medium event rate for control group used. 2Certainty of evidence downgraded twice due to studies at unclear or high risk of bias and imprecision in estimate. 3Event rate of 5% assumed. 4Certainty of evidence downgraded three times due to single study with imprecision.
Summary of findings 6. Suturing techniques after the removal of mandibular wisdom teeth.
| Horizontal mattress compared with conventional suturing after the removal of mandibular wisdom teeth | |||||
|
Population: adults with mandibular third molars requiring removal Settings: oral surgery Intervention: horizontal mattress/fibrin sealant Comparison: conventional suturing | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
|
Alveolar osteitis (up to 1‐week follow‐up) |
Not reported | ||||
|
Wound infection (up to 1‐week follow‐up) |
Not reported | ||||
|
Permanent altered tongue, chin, or lip sensation (more than 6 months) |
Not reported | ||||
|
Adverse effects ‐ reactionary bleeding (up to 30 days) |
Not reported | ||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval | |||||
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||||
Summary of findings 7. Surgical drain versus no drain after the removal of mandibular wisdom teeth.
| Drain versus no drain after the removal of mandibular wisdom teeth | |||||
|
Population: adults with mandibular third molars requiring removal
Setting: oral surgery
Intervention: drain (tube drain or gauze drain) Comparison: no drain | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| No drain | Drain | ||||
|
Alveolar osteitis (up to 1‐week follow‐up) |
Not reported | ||||
|
Wound infection (up to 1‐week follow‐up) |
Not reported | ||||
|
Permanent altered tongue, chin, or lip sensation (more than 6 months) |
Not reported | ||||
|
Adverse effects ‐ reactionary bleeding (up to 30 days) |
Not reported | ||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval | |||||
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||||
Summary of findings 8. Wound closure with the use of autologous platelet concentrates versus conventional method after the removal of mandibular wisdom teeth.
| Wound closure with blood product compared to conventional method after the removal of mandibular wisdom teeth | ||||||
|
Population: adults with mandibular third molars requiring removal Setting: oral surgery Intervention: wound closure with blood products (PRF) Comparison: conventional method | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| None | PRP/PRF | |||||
|
Alveolar osteitis (up to 1‐week follow‐up) |
205 per 1000 | 91 per 1000 (54 to 147) | OR 0.39 (0.22 to 0.67) |
128 (2 studies) |
⊕⊕⊝⊝ low1 | Favours PRF |
|
Wound infection (up to 1‐week follow‐up) |
Not reported | |||||
|
Permanent altered tongue, chin, or lip sensation (more than 6 months) |
Not reported | |||||
|
Adverse effects ‐ reactionary bleeding (up to 30 days) |
Not reported | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; PRP: platelet rich plasma; PRF: platelet rich fibrin | ||||||
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1Certainty of evidence downgraded two levels because both studies were small, with one at high risk of bias and one unclear.
Summary of findings 9. Coronectomy versus complete extraction of mandibular wisdom teeth.
| Coronectomy versus complete extraction of mandibular wisdom teeth | |||||
|
Population: adults with mandibular third molars requiring removal Setting: oral surgery Intervention: coronectomy Comparison: complete extraction | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Certainty of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Complete extraction | Coronectomy | ||||
|
Alveolar osteitis (up to 1‐week follow‐up) |
Not reported | ||||
|
Wound infection (up to 1‐week follow‐up) |
Not reported | ||||
|
Permanent altered tongue, chin, or lip sensation (more than 6 months) |
Not reported | ||||
|
Adverse effects ‐ reactionary bleeding (up to 30 days) |
Not reported | ||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval | |||||
|
GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||||
See Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9.
1. Surgical flap type
Thirteen of the 14 included studies that compared different flap designs had data that could be used in the review. Five of these studies were at high risk of bias (Baqain 2012; Haraji 2010; Kirk 2007; Roode 2010; Sandhu 2010); the risk of bias was unclear in the remaining eight studies (Briguglio 2011; Erdogan 2011; Goldsmith 2012; Mobilio 2017; Mohajerani 2018; Nageshwar 2002; Rabi 2017; Şimşek Kaya 2019). As discussed in Included studies, 11 studies compared a triangular flap design with an envelope flap, and we pooled the outcome data into ‘short’ and ‘long’ triangular flap types versus envelope flap.
The remaining three studies in this group each made a slightly different comparison, so we reported data as separate subgroups.
The primary outcomes for this comparison are described in Table 1. None of the studies measured our secondary outcomes of temporary altered tongue sensation or temporary altered chin skin or lower lip sensation.
Alveolar osteitis
Five studies compared a short triangular flap with a type of envelope flap and found no evidence of a difference in risk of alveolar osteitis: odds ratio (OR) 0.33, 95% confidence interval (CI) 0.09 to 1.23, P = 0.10, I2 = 80%, 187 participants (Analysis 1.1) (Haraji 2010; Kirk 2007; Koyuncu 2013; Mohajerani 2018; Şimşek Kaya 2019). A further study with 20 participants made the same comparison and recorded no cases of alveolar osteitis in either group (Baqain 2012).
1.1. Analysis.

Comparison 1: Surgical flap type (A versus B), Outcome 1: Alveolar osteitis (7 days)
In a study with 52 evaluated participants (Goldsmith 2012), a pedicle flap design (similar to a triangular flap) was compared to an envelope flap. The incidence of alveolar osteitis in this study was higher in the envelope flap group: OR 0.08, 95% CI 0.01 to 0.97 (Analysis 1.1). Only Briguglio 2011 had data for the comparison of long triangular flap versus envelope flap. There was no evidence of a difference in alveolar osteitis between the flap designs: OR 0.37, 95% CI 0.02 to 8.31, P = 0.53, 45 participants (Analysis 1.1).
None of the other studies evaluating flap design reported the outcome of alveolar osteitis.
Wound infection (seven days)
Four studies evaluating different flap designs reported the outcome of postoperative infection (Briguglio 2011; Goldsmith 2012; Roode 2010; Sandhu 2010). There was no evidence of a difference between long triangular flap and envelope flap: OR 0.29, 95% CI 0.04 to 2.06, P = 0.22, I2 = 0%, 2 studies, 65 participants (Analysis 1.2). Nor was there evidence from single small studies for a difference between pedicle versus envelope flap or reverse‐L versus alternative single incision flap (Analysis 1.2).
1.2. Analysis.

Comparison 1: Surgical flap type (A versus B), Outcome 2: Wound infection (7 days)
Permanent (longer than six months) altered tongue or chin or lower lip sensation
One study (45 participants) reported this outcome and found no apparent difference in the number of cases of altered tongue sensation persisting for longer than six months between the triangular flap group and the envelope flap group (Analysis 1.3) (Briguglio 2011).
1.3. Analysis.

Comparison 1: Surgical flap type (A versus B), Outcome 3: Permanent altered tongue sensation (> 6 months)
Adverse effects
Only two studies reported any other adverse effects due to the surgery. Two studies reported wound dehiscence at up to 30 days (Baqain 2012; Sandhu 2010); neither study found a statistically significant difference between the groups (Analysis 1.4).
1.4. Analysis.

Comparison 1: Surgical flap type (A versus B), Outcome 4: Adverse effects ‐ wound dehiscence (up to 30 days)
Pain (after 24 hours)
One study (45 participants) reported no difference between the two different flap types with regard to the proportion of participants reporting pain 24 hours after surgery (Analysis 1.5) (Briguglio 2011).
1.5. Analysis.

Comparison 1: Surgical flap type (A versus B), Outcome 5: Pain present at 24 hours (yes/no)
Four studies reported mean pain scores for each group at 24 hours postsurgery (based on a 0‐to‐10 visual analogue scale (VAS)) for the comparison short triangular flap versus envelope flap (Baqain 2012; Kirk 2007; Koyuncu 2013; Şimşek Kaya 2019)). The pooled data demonstrated a mean difference (MD) of −0.84, 95% CI −1.65 to −0.03, P < 0.001, I2 = 77%, 161 participants) (Analysis 1.6). These results favoured the short triangular flap; however, the difference is small on a 0‐to‐10 VAS. Two other single‐study comparisons (comma‐shaped incision versus modified envelope (100 participants), and reverse‐L flap versus single incision (33 participants)) also favoured a flap design not of the envelope variety. A further study (25 participants) comparing a long triangular flap design with an envelope flap design showed no evidence of a difference between the flap types (Analysis 1.6).
1.6. Analysis.

Comparison 1: Surgical flap type (A versus B), Outcome 6: Mean pain at 24 hours (0 to 10 VAS)
Swelling (after seven days)
One study evaluated the binary outcome of swelling or no swelling (Briguglio 2011). The results do not clearly favour either flap design (long triangular flap versus envelope flap) (Analysis 1.7).
1.7. Analysis.

Comparison 1: Surgical flap type (A versus B), Outcome 7: Swelling present (after 1 week) (yes/no)
Seven studies evaluated mean swelling at seven days based on measurements of facial swelling. For the comparison of short triangular flap versus envelope flap, the triangular design was favoured: MD 0.60, 95% CI 0.25 to 0.95, P < 0.001, I2 = 0%, 2 studies, 99 participants. The long triangular flap was also favoured over the envelope flap based on data from two studies: MD 0.68, 95% CI 0.18 to 1.18, P = 0.007, I2 = 0%, 40 participants. One other single‐study comparison (100 participants) also favoured the non‐envelope flap design (comma‐shaped incision versus modified envelope). A further two studies (40 participants) failed to find any difference between the two flap designs (pedicle flap versus envelope flap, and reverse‐L flap versus single incision) (Analysis 1.8).
1.8. Analysis.

Comparison 1: Surgical flap type (A versus B), Outcome 8: Mean swelling (after 1 week)
Trismus (after seven days)
One study found no difference in the proportion of participants in each group with trismus seven days after surgery (Analysis 1.9) (Briguglio 2011).
1.9. Analysis.

Comparison 1: Surgical flap type (A versus B), Outcome 9: Trismus (after 1 week) (yes/no)
Five studies reported mean maximum mouth opening in each group (Baqain 2012; Erdogan 2011; Koyuncu 2013; Nageshwar 2002; Rabi 2017). We pooled data from two studies (158 participants) for the comparison short triangular flap versus envelope flap (Baqain 2012; Koyuncu 2013). The envelope flap was found to be superior, with a standardised mean difference of 0.67, 95% CI 0.30 to 1.04, P < 0.001 (Analysis 1.10). In Analysis 1.11, we evaluated maximum mouth opening at one‐week postoperative using mean difference data. Nageshwar 2002 was the only study to evaluate a comma‐shaped incision versus a modified envelope flap; data for this study of 100 participants indicated that the comma‐shaped incision had greater mouth opening (Analysis 1.11). Two studies assessed a long triangular flap versus an envelope flap (Erdogan 2011; Rabi 2017); pooled data showed that the envelope flap was favoured: MD 1.22, 95% CI 0.33 to 2.11, P = 0.007.
1.10. Analysis.

Comparison 1: Surgical flap type (A versus B), Outcome 10: Maximum mouth opening (after 1 week) (SMD)
1.11. Analysis.

Comparison 1: Surgical flap type (A versus B), Outcome 11: Maximum mouth opening (after 1 week) (MD)
2. Lingual nerve protection
Three studies evaluated the use of retractors for lingual nerve protection compared to no retractor (Gargallo‐Albiol 2000; Gomes 2005; Shad 2015), and one study assessed the direct comparison of two different retractors (Greenwood 1994).
None of these studies measured the outcomes of alveolar osteitis, infection, pain, swelling, trismus, or other adverse effects.
Permanent (longer than six months) altered tongue or chin or lower lip sensation
In one study of 380 participants there was no evidence of a difference in permanent altered sensation when comparing the use of a retractor with no retractor: Peto OR 0.14, 95% CI 0.00 to 6.82; very low‐certainty evidence (Analysis 2.1).
2.1. Analysis.

Comparison 2: Lingual nerve protection versus no protection, Outcome 1: Permanent altered sensation (up to 6 months)
Temporary (approximately one‐month postoperation) altered tongue or chin or lower lip sensation
Meta‐analysis of three studies (735 cases) found that the incidence of temporary lingual nerve damage was higher in the cohort in which retraction was placed: OR 4.18, 95% CI 1.75 to 9.98 (Analysis 2.2).
2.2. Analysis.

Comparison 2: Lingual nerve protection versus no protection, Outcome 2: Temporary altered sensation (up to 1 month)
Greenwood 1994 found more cases of temporary altered sensation for the Howarth's retractor for lingual nerve protection compared to the Broad retractor, based on very low‐certainty evidence: OR 12.96, 95% CI 2.26 to 74.46, 150 participants; data not shown.
3. Bone removal techniques
Thirteen included studies evaluated different bone removal techniques (Absi 1993; Arakji 2016; Barone 2010; Basheer 2017; Bhati 2017; Mantovani 2014; Mistry 2016; Mocan 1996; Piersanti 2014; Praveen 2007; Rullo 2013; Topcu 2019; Uyanik 2015). Five studies were at unclear risk of bias (Absi 1993; Arakji 2016; Barone 2010; Bhati 2017; Mantovani 2014), whilst the remaining studies were assessed as at high risk of bias.
Four of the studies did not contribute to the analysis. Rullo 2013 was a split‐mouth study of 52 participants that compared a piezoelectric bone removal device used in the removal of a mandibular third molar from one side of the mouth with the use of conventional rotative instruments used in a separate session to remove the other mandibular third molar. The data were not reported for each randomised group, but were analysed according to whether the procedure was simple or complex. We were unsuccessful in obtaining useable data from the authors of this study. The study by Mocan 1996 randomly allocated 20 participants to either lingual split or buccal bone removal. However, no data were reported for each group for the outcomes of pain, swelling, or trismus, and we were unable to obtain these data from the authors. Data were not useable from Mantovani 2014 or Uyanik 2015 (reasons are presented in Table 10; Table 11; Table 12).
Of the studies contributing data, Arakji 2016, Basheer 2017, Bhati 2017, Mistry 2016, Piersanti 2014 and Topcu 2019 compared piezoelectric bone removal with conventional rotary bone removal using a surgical handpiece, Barone 2010 compared ultrasonic versus bur, and Absi 1993 and Praveen 2007 compared chisel versus bur.
None of the studies measured our primary outcomes of alveolar osteitis, permanent altered tongue or chin or lower lip sensation or adverse effects.
Wound infection
Absi 1993 was the only study in this group that reported incidence of infection, and found no evidence of a difference between the lingual split with chisel and lingual split using a surgical handpiece. There were three unilateral infections in each group in this split‐mouth study of 52 participants, in which most of the participants (83%) also had maxillary third molars removed during the same treatment session (Analysis 3.1).
3.1. Analysis.

Comparison 3: Bone removal techniques, Outcome 1: Wound infection (7 days)
Temporary (approximately one‐month postoperation) altered tongue or chin or lower lip sensation
Likewise, Absi 1993 was the only study that reported data for the outcome of altered tongue or chin sensation within the first month following surgery. There was no evidence of a difference in these outcomes from this single split‐mouth study of 52 participants (Analysis 3.2; Analysis 3.3).
3.2. Analysis.

Comparison 3: Bone removal techniques, Outcome 2: Temporary alteration of tongue sensation (< 1 month)
3.3. Analysis.

Comparison 3: Bone removal techniques, Outcome 3: Temporary alteration of chin sensation (< 1 month)
Pain (after 24 hours)
Two studies reported data for the outcome of pain after 24 hours: Barone 2010 (26 participants) and Praveen 2007 (90 participants). Praveen 2007 conducted a three‐arm parallel‐group study and found reduced pain (measured on a 0‐to‐10 VAS) in the lingual split with bur group compared to the lingual split with a chisel group, but no difference between lingual split (either bur or chisel) and a "simplified bone removal technique" (Analysis 3.4).
3.4. Analysis.

Comparison 3: Bone removal techniques, Outcome 4: Pain at 24 hours (0‐to‐10 VAS)
The split‐mouth studies by Arakji 2016, Bhati 2017, Mistry 2016, Piersanti 2014, and Topcu 2019 compared piezoelectric bone removal with conventional rotary bone removal using a surgical hand‐piece and measured pain. Meta‐analysis of data from these studies showed that pain at 24 hours on a 0‐to‐10 VAS was reduced in the piezoelectric surgery cohort: MD 1.93, 95% CI 0.77 to 3.08 (Analysis 3.5).
3.5. Analysis.

Comparison 3: Bone removal techniques, Outcome 5: Mean pain at 24 hours (0‐to‐10 VAS)
Swelling (after seven days)
Two studies reported data for the outcome of swelling after seven days: Barone 2010 (26 participants) and Praveen 2007 (90 participants). Praveen 2007 asked participants to rate swelling on a "swelling scale" and found no apparent difference in swelling associated with the lingual split with bur group compared to the lingual split with chisel group (Analysis 3.6), and no apparent difference in swelling between lingual split (either bur or chisel) and a "simplified bone removal technique". There was evidence of significantly reduced swelling for bone removal using ultrasound compared with use of a bur in Barone 2010: MD 0.37, 95% CI 0.20 to 0.54, P < 0.001 (Analysis 3.6). The evidence for all these findings is of very low certainty and should be interpreted with caution until the single trial evaluating each comparison has been independently replicated.
3.6. Analysis.

Comparison 3: Bone removal techniques, Outcome 6: Swelling (after 7 days)
Trismus (after seven days)
The studies by Arakji 2016, Basheer 2017, Bhati 2017, and Mistry 2016 compared piezoelectric bone removal with conventional rotary bone removal using a surgical hand‐piece and measured trismus. Meta‐analysis of these four trials demonstrated an improvement in postoperative trismus at seven days when piezoelectric surgery was used in comparison with conventional bone removal techniques: MD 2.68 mm, 95% CI 0.54 to 4.81 (Analysis 3.7).
3.7. Analysis.

Comparison 3: Bone removal techniques, Outcome 7: Maximum mouth opening (after 7 days)
Barone 2010 found no significant evidence of a difference in maximum mouth opening between the group who had bone removal using ultrasound compared to those participants in which bone was removed with a bur (Analysis 3.8).
3.8. Analysis.

Comparison 3: Bone removal techniques, Outcome 8: Maximum mouth opening (after 7 days)
Given the small number of studies, the different comparisons evaluated, the variable outcomes reported, and the paucity of useful data, we were not able to draw any conclusions regarding bone removal in third molar surgery.
4. Wound irrigation techniques
The two studies of irrigation techniques included in this review were both conducted in the 1970s (Butler 1977; Sweet 1976). Both were split‐mouth studies, which we assessed as being at high and unclear risk of bias, respectively. Butler 1977 (211 participants) compared high‐volume with low‐volume saline irrigation, and Sweet 1976 (99 participants) compared mechanical irrigation with manual irrigation, with both groups receiving a high volume of irrigant.
These studies only measured two of our primary outcomes and none of our secondary outcomes.
Alveolar osteitis
Both studies reported on alveolar osteitis, and neither found a statistically significant difference between groups: mechanical versus manual irrigation: RR 0.33, 95% CI 0.01 to 8.09; high versus low volume: RR 0.52, 95% CI 0.27 to 1.02 (Analysis 4.1).
4.1. Analysis.

Comparison 4: Wound irrigation techniques (A versus B), Outcome 1: Alveolar osteitis (7 days)
Wound infection
Likewise, neither study showed a statistically significant difference between groups for the outcome postoperative infection: mechanical versus manual irrigation: RR 0.50, 95% CI 0.05 to 5.43; low versus high volume: RR 0.17, 95% CI 0.02 to 1.37 (Analysis 4.2).
4.2. Analysis.

Comparison 4: Wound irrigation techniques (A versus B), Outcome 2: Wound infection (7 days)
Neither study reported outcome data measured at the time points of interest for the other outcomes of this review.
5. Primary versus secondary wound closure
Nine included studies compared primary versus secondary wound closure techniques (Bello 2011; Danda 2010; Hashemi 2012; Osunde 2011a; Osunde 2012; Pachipulusu 2018; Pasqualini 2005; Refo'a 2011; Xavier 2008). Of these, three were split‐mouth studies (Danda 2010; Hashemi 2012; Xavier 2008). We assessed three studies as at high risk of bias (Danda 2010; Hashemi 2012; Refo'a 2011), and the remaining studies as at unclear risk of bias.
None of the studies measured the outcomes of permanent or temporary altered tongue or chin or lower lip sensation.
Alveolar osteitis
Four studies reported the outcome of alveolar osteitis (Bello 2011; Danda 2010; Hashemi 2012; Pasqualini 2005). Hashemi 2012 reported no alveolar osteitis in either group, and pooled data from the other three trials showed no evidence of a difference in the incidence of alveolar osteitis: risk ratio 0.99, 95% CI 0.41 to 2.40, P = 0.98, with no heterogeneity (Analysis 5.1).
5.1. Analysis.

Comparison 5: Primary versus secondary wound closure, Outcome 1: Alveolar osteitis (7 days)
Wound infection
Two studies also reported the outcome of postoperative infection (Bello 2011; Hashemi 2012). Hashemi 2012 reported no infections in either group, and Bello 2011 showed no statistically significant difference between the primary and secondary wound closure groups: RR 4.77, 95% CI 0.24 to 96.34 (Analysis 5.2).
5.2. Analysis.

Comparison 5: Primary versus secondary wound closure, Outcome 2: Wound infection (7 days)
Adverse effects
One study reported the adverse effect of reactionary bleeding and reported no statistically significant difference in the number of participants with bleeding between groups (Analysis 5.3) (Bello 2011).
5.3. Analysis.

Comparison 5: Primary versus secondary wound closure, Outcome 3: Adverse effects ‐ reactionary bleeding
Pasqualini 2005 reported wound dehiscence in 33 of the 100 participants who had primary wound closure. In an e‐mail communication, Dr Pasqualini reported "the parameter 'wound dehiscence' is only descriptive of the primary closure group and no comparison or inference should be done with the secondary closure group, where the mucosal dehiscence was systematically created by the surgeon. Lastly, despite the more favourable trend in pain and swelling scores, I would underline the more difficult cleaning of the wound (in the secondary closure group) in the weeks following suture removal, compared to those cases of primary closure where no dehiscence occurred, as a drawback of the secondary closure".
Pain (after 24 hours)
Five parallel‐group studies (474 participants) reported the outcome of mean pain on a 0‐to‐10 VAS in each group after 24 hours (Bello 2011; Osunde 2011a; Osunde 2012; Pachipulusu 2018; Pasqualini 2005). There was evidence of a reduction in pain favouring the secondary closure group: MD 0.94, 95% CI 0.50 to 1.38, P < 0.001, I2 = 87% (Analysis 5.4). There was substantial heterogeneity amongst these studies which was likely due to differences in the type of incision used and whether the secondary closure group had some or no sutures.
5.4. Analysis.

Comparison 5: Primary versus secondary wound closure, Outcome 4: Pain at 24 hours (0‐to‐10 VAS)
Swelling (after seven days)
Seven studies (557 participants) reported data for mean swelling in each group (Bello 2011; Danda 2010; Hashemi 2012; Osunde 2011a; Osunde 2012; Pasqualini 2005; Xavier 2008). Meta‐analysis of these data showed a reduction in swelling favouring the secondary closure group: MD mm 0.33, 95% CI 0.09 to 0.57, P = 0.007, I2 = 89% (Analysis 5.5). The substantial heterogeneity in this estimate was likely due to differences in both study design (three split‐mouth studies and five parallel‐group studies) and the incision shape and number of sutures used to close the wound in the secondary closure groups.
5.5. Analysis.

Comparison 5: Primary versus secondary wound closure, Outcome 5: Swelling (after 7 days)
Trismus (after seven days)
Four parallel‐group studies (274 participants) reported the outcome of mean maximum mouth opening in each group after seven postoperative days (Bello 2011; Osunde 2011a; Osunde 2012; Pachipulusu 2018). Meta‐analysis of these data showed no evidence of a greater maximum mouth opening for either group: MD −0.29, 95% CI −0.90 to 0.32, P = 0.003, I2 = 79% (Analysis 5.6).
5.6. Analysis.

Comparison 5: Primary versus secondary wound closure, Outcome 6: Maximum mouth opening (after 7 days)
6. Suturing techniques
Two studies compared different suturing techniques (Acar 2017; Gogulanathan 2015). Acar 2017 used a split‐mouth/cross‐over design to evaluate the use of horizontal mattress suturing versus simple interrupted suturing, with a wash‐out period of four weeks between the two surgeries. The data could not be used, but the study reported that there was no evidence of differences in the techniques for pain, swelling or trismus (P > 0.05). Another split‐mouth study, Gogulanathan 2015, compared fibrin sealant with conventional suturing for wound closure in 30 participants and measured trismus.
Trismus (after seven days)
A small improvement in maximal mouth opening was found at seven days postoperation when using fibrin sealant in comparison to conventional sutures: MD 3.50 mm, 95% CI 2.69 to 4.31 (Analysis 6.1). These data should be interpreted with caution as they are based on only one study, which we judged to be at unclear risk of bias.
6.1. Analysis.

Comparison 6: Suturing techniques, Outcome 1: Maximum mouth opening
7. Surgical drain versus no drain
Seven included studies evaluated the use of a surgical drain following surgical extraction of mandibular third molars: six studies compared a tube drain with no drain (Cerqueira 2004; Chukwuneke 2008; Koyuncu 2015; Kumar 2016; Rakprasitkul 1997; Saglam 2003; Srinivas 2006), and one study compared the use of a gauze drain with no drain (de Brabander 1988). Three of these studies used a parallel‐group design (Chukwuneke 2008; de Brabander 1988; Koyuncu 2015), and four used a split‐mouth design in which one side of the mouth was randomly allocated a surgical drain and the other was not. One split‐mouth study performed the surgery in two sessions with a two‐month period between surgeries (Rakprasitkul 1997), whilst the other three split‐mouth studies allocated a drain randomly to one side of the mouth following bilateral extraction of mandibular third molars during the same session. We assessed two studies as at unclear risk of bias (de Brabander 1988; Kumar 2016), and the other five studies as at high risk of bias.
None of the studies evaluating surgical drains measured the outcomes of alveolar osteitis, infection, permanent or temporary altered tongue or chin or lower lip sensation, or adverse effects.
Pain (after 24 hours)
Four studies evaluating the use of surgical drains reported the outcome of pain (Cerqueira 2004; Chukwuneke 2008; Koyuncu 2015; Srinivas 2006). Three of these studies used a split‐mouth design in which both mandibular third molars were extracted in the same operating session and a drain was inserted on one randomly chosen side (Cerqueira 2004; Koyuncu 2015; Srinivas 2006). We considered that pain experienced by these participants could not be reliably attributed to the use of a drain or not, and so did not use pain data from split‐mouth studies in which participants received both interventions during a single operative session.
Meta analysis of Chukwuneke 2008, a parallel‐group study, and Koyuncu 2015, a split‐mouth study, showed no evidence of a difference between groups in pain at 24 hours (Analysis 7.1).
7.1. Analysis.

Comparison 7: Surgical drain versus no drain, Outcome 1: Pain at 24 hours (0‐to‐10 VAS)
Swelling (after seven days)
All of the studies evaluating surgical drains reported the outcome of postoperative swelling.
One study evaluating a gauze drain used a "u‐formed calliper" to measure the thickness of the cheek (de Brabander 1988). This study found no statistically significant difference in swelling between the two groups: MD 0.18, 95% CI −0.06 to 0.42, P = 0.32 (data not shown).
The other five studies, all of which evaluated tube drains, took the sum of a horizontal and vertical measurement across the cheek and expressed swelling as the percentage difference compared to the preoperative measure. Meta‐analysis of data from these five studies showed a reduction in swelling with the use of a drain: MD −0.90, 95% CI −1.62 to −0.19, P = 0.01, I2 = 88% (Analysis 7.2). The considerable heterogeneity in this meta‐analysis may be due in part to differences in the design of both the drains and the studies.
7.2. Analysis.

Comparison 7: Surgical drain versus no drain, Outcome 2: Swelling at 7 days
Trismus (after seven days)
The effect of the use of a surgical drain on trismus was assessed by comparing mean maximal mouth opening one week after surgery in each group. Seven included studies reported this outcome (Cerqueira 2004; Chukwuneke 2008; Koyuncu 2015; Kumar 2016; Rakprasitkul 1997; Saglam 2003; Srinivas 2006). However, it was our assessment that this outcome cannot be reliably attributed to intervention or control in split‐mouth studies where both mandibular molars are extracted in the same operative session, therefore maximum mouth opening data from Cerqueira 2004, Saglam 2003, and Srinivas 2006 were not used in this review.
We combined data from the four remaining studies in a meta‐analysis, which showed that maximum mouth opening was greater in those participants who had received a surgical drain: MD 3.11 mm, 95% CI 2.20 to 4.02, P < 0.001, I2 = 20% (Analysis 7.3).
7.3. Analysis.

Comparison 7: Surgical drain versus no drain, Outcome 3: Maximum mouth opening at 7 days
8. Wound closure with autologous platelet concentrates
This comparison was new in this 2020 version of the review. We looked at trials comparing the use of the blood products platelet rich plasma (PRP) and platelet rich fibrin (PRF) in sockets following the surgical removal of third molars (for further details on these novel techniques see Description of the intervention). We included four studies in this comparison (Dutta 2016; Eshghpour 2014; Gulsen 2017; Ozgul 2015).
None of the studies measured wound infection, permanent or temporary altered tongue, chin skin or lower lip sensation, adverse effects or trismus.
Alveolar osteitis (seven days)
The trials by Eshghpour 2014 and Unsal 2018 demonstrated a reduction in the incidence of alveolar osteitis at seven days when PRF was used in comparison to no addition to the socket after extraction: OR 0.39, 95% CI 0.22 to 0.67 (Analysis 8.1). This finding was based on data from two split‐mouth studies with a total of 128 participants; one study was at high risk of bias, and the other at unclear risk of bias.
8.1. Analysis.

Comparison 8: Wound closure with blood products versus none, Outcome 1: Alveolar osteitis (7 days) split‐ mouth studies (OR/BB)
Pain at 24 hours
Three studies evaluated reported pain (using a 0‐to‐10 VAS) at 24 hours postoperatively for the comparison of PRF versus no blood products in the socket at extraction (Gulsen 2017; Kapse 2019; Ozgul 2015). There was no evidence that PRF was better or worse than no blood products for reducing pain: MD ‐0.13, 95% CI ‐0.59 to 0.34 (Analysis 8.2). There was evidence of substantial heterogeneity (P = 0.02, I2 = 74%).
8.2. Analysis.

Comparison 8: Wound closure with blood products versus none, Outcome 2: Mean pain at 24 hours (0‐to‐10 VAS)
Swelling at seven days
Two studies evaluated swelling at seven days postoperatively for the comparison of PRF in the extraction socket versus no blood products postextraction (Gulsen 2017; Ozgul 2015). Meta‐analysis showed no evidence of a difference between the two groups: MD 0.11, 95% CI −0.12 to 0.35 (Analysis 8.3).
8.3. Analysis.

Comparison 8: Wound closure with blood products versus none, Outcome 3: Swelling at 7 days
9. Coronectomy versus complete tooth removal
We did not include data from two older studies evaluating this comparison as we judged them to be unreliable. We identified one new parallel‐group RCT with a small sample size (30 participants, 15 participants per group) (Singh 2018). It measured only two of our outcomes.
Swelling (after seven days)
There was no evidence of a difference in swelling at day 7 between coronectomy and total tooth removal: MD −0.18, 95% CI −0.63 to 0.27 (Analysis 9.1).
9.1. Analysis.

Comparison 9: Coronectomy versus odontectomy, Outcome 1: Swelling at day 7
Trismus (after seven days)
There was also no evidence of a difference in maximal mouth opening at day 7 between coronectomy and total tooth removal: MD −2.94, 95% CI −8.20 to 2.32 (Analysis 9.2).
9.2. Analysis.

Comparison 9: Coronectomy versus odontectomy, Outcome 2: Maximum mouth opening at day 7
Two trials included in this review set out to compare extraction of mandibular third molars with a coronectomy procedure in which only the top part of the impacted third molar was removed (Leung 2009; Renton 2005). We assessed both studies as at high risk of bias due to high attrition in the coronectomy group and unit of analysis errors. Both studies included participants whose preoperative radiographs indicated proximity of the third molar root(s) to the inferior alveolar nerve. Some participants contributed two teeth to the study and some only one.
In both studies, in some of the third molars (9.4% and 38% in Leung 2009 and Renton 2005, respectively) randomly allocated to the coronectomy, the roots were inadvertently mobilised and were therefore completely removed. Also, the analysis in both studies did not take account of the pairing of the data (two teeth from a single participant were incorrectly assumed to have the same independence as two teeth from two different participants). We considered the data from these studies as not sufficiently reliable to include in the review.
However, both studies suggested that in participants where third molar roots were very close to the nerve canal, it was likely that coronectomy was associated with a reduction in nerve damage and no increase in alveolar osteitis, infection, or pain in the short term.
The adverse effect of migration of the root segments occurred following coronectomy in 13% of those evaluated at 13 months in the Renton 2005 study, but extraction was not required. The proportion of participants with root migration at 12 months was 24% in Leung 2009, and two participants in the coronectomy group experienced root exposure. The mean follow‐up was less than one year in Leung 2009 and only two years in Renton 2005, so that neither study was long enough to reliably assess whether there were any long‐term adverse effects associated with coronectomy.
Discussion
Summary of main results
See Table 1; Table 2; Table 3; Table 4; Table 5; Table 7; Table 8; Table 9.
The evidence included in this review is sourced from 62 RCTs evaluating different aspects of the surgical removal of mandibular third molars. However, due to the number of different comparisons evaluated and the overall poor quality of the research, these trials provide low‐ to very low‐certainty evidence, which means that further research may change the estimates and the confidence intervals presented. The overall results for the primary outcomes for the nine categories are summarised below.
There is insufficient evidence to determine whether envelope or triangular flap designs lead to more alveolar osteitis, wound infection, or permanent altered tongue, chin, or lip sensation. None of the studies in this comparison reported adverse effects.
There is insufficient evidence to determine whether the use of a lingual retractor increases or decreases the risk of permanent altered sensation, or makes no difference. No other primary outcomes were reported by the studies included in this comparison.
There is insufficient evidence regarding lingual split with chisel compared with a surgical hand‐piece for bone removal in terms of wound infection. None of the studies in this comparison reported on alveolar osteitis, permanent altered sensation, or adverse effects.
There is insufficient evidence from single studies on irrigation method (manual versus mechanical or irrigation volume) to determine whether either intervention in the two comparisons leads to more alveolar osteitis. There was also no evidence of a difference in postoperative infection for these two comparisons. None of the studies in this comparison reported on permanent altered sensation or adverse effects.
There is insufficient evidence to determine whether primary or secondary wound closure leads to more alveolar osteitis, wound infection, or adverse effects (bleeding). None of the studies in this comparison reported on permanent sensation changes.
We were unable to draw any conclusions about suturing techniques, as the included studies did not report on any of our primary outcomes.
We were unable to draw any conclusions about the use of a surgical drain versus no drain, as the included studies did not report on any of our primary outcomes.
Placing PRP or PRF in sockets may reduce the incidence of dry socket, but the evidence is of low certainty. Our other primary outcomes were not reported.
No studies provided useable data for any of the primary outcomes in relation to coronectomy.
Overall completeness and applicability of evidence
The 62 trials included in this review describe comparisons related to nine aspects of the surgical procedures for extracting impacted mandibular third molars: type of surgical flap raised, use of retractor, techniques for bone removal, wound irrigation, wound closure, wound drainage, use of platelet‐related products, and complete or incomplete tooth removal. There were only one or two trials evaluating a given aspect of the surgery or a specific comparison. Also, many of the included trials reported only some of the primary and secondary outcomes of interest to this review. None of the trials reported the primary outcome fracture of the mandible.
More than half of the RCTs included in this review used a split‐mouth design in which one tooth was allocated to the intervention and the other to control. Whilst this design may be efficient, if both teeth are treated in the same operative session (as was the case for most of these trials), it may be difficult to attribute outcomes such as pain or trismus to the intervention or the control. Furthermore, the paired nature of the outcome data from split‐mouth trials should be recognised in the analysis, and it was not always clear in the published papers whether this had been done. However, we recognise that it may also be undesirable to require participants to undergo two separate procedures, some weeks apart, in order to ascertain the effect of the intervention on these outcomes.
Seven of the included trials were conducted before the year 2000. It is unclear to what extent trials undertaken more than 20 years ago remain relevant to contemporary practice.
Quality of the evidence
Using the GRADE approach, we judged the body of evidence for each of the comparisons and outcomes in this review to be of low or very low certainty. This was because most of the comparisons were based on a small number of trials and participants, and half of the trials were at high risk of bias, with the other half being at unclear risk of bias. It is worth noting that the first included study was published in 1976 and the most recent in 2019. The frequency of observed risk of bias appears to have decreased over time.
Potential biases in the review process
We used contemporary methodology and comprehensive search strategies covering multiple databases. We made some assumptions in the analysis of the split‐mouth trials when data were not reported, as we believed this would introduce less bias than omitting the data from these trials. We used more up‐to‐date methods for assessment of risk of bias and the certainty of the evidence than we had specified in our original protocol, but we do not consider that this would have resulted in any bias. We used Covidence software to screen and assess abstracts and full‐text papers for the 2020 update (Covidence).
Agreements and disagreements with other studies or reviews
A systematic review on primary versus secondary wound closure has been published, and the results do not support a preference for either approach (Carrasco‐Labra 2012), which is in agreement with our review.
Another systematic review compared coronectomy versus total removal, and included four trials (two RCTs and two controlled clinical trials) (Long 2012). The authors concluded that coronectomy is preferable to total removal of a wisdom tooth. We were unable to extract these data and so could not confirm or refute this finding.
Lingual split with chisel versus bur for bone removal was the focus of another systematic review that included five studies (Steel 2012). The tentative conclusions of this review were that there was no difference between interventions in postoperative pain and swelling, and some evidence of less trismus for the lingual split technique. This was similar to the findings of our review, although we did not find a difference for trismus.
A further systematic review looked at lingual flap retraction and prevention of lingual nerve damage associated with third molar surgery (Pichler 2001). The authors included eight studies, of which seven were prospective clinical series and one was described as an RCT (Robinson 1996). We excluded the latter from our Cochrane Review due to the high number of protocol violations resulting in unquantifiable biases. The authors of Pichler 2001 concluded that the use of a lingual nerve retractor during third molar surgery is associated with an increased incidence of temporary nerve damage, and was neither protective nor detrimental with respect to the incidence of permanent nerve damage. We agree with their findings of an increased incidence of temporary nerve damage. We do not agree that use of lingual nerve protection is either protective or detrimental in terms of incidence of permanent nerve damage; one study included in our review found that there was a higher incidence of permanent (greater than six months) altered tongue sensation in the group in which a lingual retractor was not used.
A recent review paper compared the postoperative outcomes of envelope and triangular flaps for third molar surgery (Zhu 2020). This review paper references the 2014 version of our review and includes many of the same studies, but also includes studies with other designs. Their conclusions were very similar to those of this review: "the evidence at present is not sufficient to suggest the use of either flap design. Therefore, future multicenter and large scale randomized clinical trials are required to validate our findings".
Authors' conclusions
Implications for practice.
We included 62 trials in this updated review (an additional 27 since the original 2014 review). The comparisons in the trials related to nine broad aspects of the surgical procedures for impacted mandibular third molar removal: type of surgical flap raised, use of retractor for lingual nerve protection, techniques for bone removal, wound irrigation, wound closure, wound drainage, use of platelet‐related products, and complete or incomplete tooth removal. The certainty of the body of evidence for each of these comparisons was low or very low due to the small number of trials and participants and the high or unclear risk of bias in the trials. No trials were found to be at low risk of bias across all of the domains described.
This review provides a description and analysis of the relevant randomised controlled trial evidence, so that surgeons can make informed choices when adopting new techniques, or continuing with established techniques. It is not possible to recommend changes to surgical practice. The evidence is uncertain, though we note that there is some limited evidence that placing platelet rich plasma or platelet rich fibrin in sockets may reduce the incidence of dry socket.
Implications for research.
The risk of bias for the included studies was high (50%) or unclear. More consistent use of the CONSORT statement for reporting of randomised controlled clinical trials would increase the value of research.
Detailed reporting of methods, such as generation of allocation sequence, allocation concealment, and numbers and reasons for withdrawals and exclusions.
Blinding of outcome assessment, if possible.
Full reporting of methods used to measure facial swelling.
Reporting of adverse effects of interventions.
Studies of a split‐mouth design may be appropriate for comparing different surgical techniques for third molar removal, but trialists need to consider which outcomes can be accurately measured and analysed. It would be helpful to have a consensus agreement on the criteria for the measurement of facial swelling. There is a need for trials looking at coronectomy versus root retention versus complete tooth removal, with long‐term follow‐up so that any adverse effects such as root migration and root exposure requiring further surgery can be determined. We recognise that such studies would require large numbers of participants and long follow‐up, and that it is difficult to source the funding required for such studies.
What's new
| Date | Event | Description |
|---|---|---|
| 7 July 2020 | New citation required and conclusions have changed | The addition of 27 studies has led to slight changes in our conclusions. |
| 8 July 2019 | New search has been performed | Search updated. This review is an update of the first review, which was published in July 2014. We have added two new authors: Wafa Kashbour (WK) and Neha Shah (NS). |
History
Protocol first published: Issue 3, 2003 Review first published: Issue 7, 2014
| Date | Event | Description |
|---|---|---|
| 12 May 2009 | Amended | Converted to new review format. |
Acknowledgements
This update: we wish to thank Laura MacDonald, Anne Littlewood, Dr Philip Riley, and Professor Anne‐Marie Glenny (Cochrane Oral Health), our peer reviewers Professor Alastair Goss and Professor Anthony Pogrel, and copy editor Lisa Winer.
Previous review: we wish to thank Anne Littlewood (Cochrane Oral Health) for her assistance with literature searching and Philip Riley (Cochrane Oral Health) for his help with the preparation of the review. Our thanks to Niall Quigley for contributing to previous versions of the review and Professor K Thongprasom for her assistance in locating and translating a paper published in the Thai language. We thank Susan Furness and Marco Esposito, authors on the previous version of this review, for their contribution. We also wish to thank Professor Chengge Hua, Chang Liu, and Adrien Boillot for their support in the translation of published papers when needed.
Appendices
Appendix 1. Cochrane Oral Health Trials Register search strategy
Cochrane Oral Health’s Trials Register is available via the Cochrane Register of Studies. For information on how the register is compiled, see https://oralhealth.cochrane.org/trials. From February 2013, searches of the Cochrane Oral Health Trials Register were undertaken using the Cochrane Register of Studies and the search strategy below:
#1 ("third molar*" or "3rd molar*" or "mandibular molar*" or "maxillary molar*") #2 (wisdom AND (tooth or teeth)) #3 #1 or #2 #4 (extract* or remov* or surg*) #5 (#3 and #4) AND (INREGISTER)
Earlier searches of the Cochrane Oral Health Trials Register for this review were undertaken using the Procite software and the search strategy below:
((molar‐third OR "molar,‐third" OR "molar,‐ third" OR "Molar, Third" OR "third molar*" OR "3rd molar*" OR (wisdom AND (tooth OR teeth)) OR "third mandibular molar*" OR "third maxillary molar*") AND (tooth‐extraction* OR extract* OR remov* OR (tooth‐impacted AND surg*)))
Cochrane Oral Health’s Trials Register is available via the Cochrane Register of Studies. For information on how the register is compiled, see https://oralhealth.cochrane.org/trials
Appendix 2. Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1 MOLAR THIRD single term (MeSH) #2 (wisdom next tooth) #3 (wisdom next teeth) #4 (third near molar*) #5 (#1 or #2 or #3 or #4) #6 TOOTH EXTRACTION single term (MeSH) #7 (extract* near tooth) #8 (extract* near teeth) #9 (extract* near (third next molar*)) #10 (remov* near tooth) #11 (remov* near teeth) #12 (surgical* near remov*) #13 (surgery near remov*) #14 (surgical* near extract*) #15 (surgery near extract*) #16 (#6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15) #17 (#5 and #16)
Appendix 3. MEDLINE Ovid search strategy
1. Molar, Third/ 2. (third adj6 molar$).mp. 3. (wisdom adj tooth).mp. 4. (wisdom adj teeth).mp. 5. or/1‐4 6. Tooth Extraction/ 7. (extract$ adj6 tooth).mp. 8. (extract$ adj6 teeth).mp. 9. (extract$ adj6 (third adj molar$)).mp. 10. (extract$ adj6 (third adj3 molar$)).mp. 11. (remov$ adj6 tooth).mp. 12. (remov$ adj6 teeth).mp. 13. (surgical$ adj3 remov$).mp. 14. (surgery adj3 remov$).mp. 15. (surgical$ adj3 extract$).mp. 16. (surgery adj3 extract$).mp. 17. or/6‐16 18. 5 and 17
This subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity‐maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of the Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011].
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 4. Embase Ovid search strategy
1. Molar, Third/ 2. (third adj6 molar$).mp. 3. (wisdom adj tooth).mp. 4. (wisdom adj teeth).mp. 5. or/1‐4 6. Tooth Extraction/ 7. (extract$ adj6 tooth).mp. 8. (extract$ adj6 teeth).mp. 9. (extract$ adj6 (third adj molar$)).mp. 10. (extract$ adj6 (third adj3 molar$)).mp. 11. (remov$ adj6 tooth).mp. 12. (remov$ adj6 teeth).mp. 13. (surgical$ adj3 remov$).mp. 14. (surgery adj3 remov$).mp. 15. (surgical$ adj3 extract$).mp. 16. (surgery adj3 extract$).mp. 17. or/6‐16 18. 5 and 17
The above subject search was linked to adapted version of the Cochrane Embase Project filter for identifying RCTs in Embase Ovid (see www.cochranelibrary.com/help/central-creation-details.html for information):
1. Randomized controlled trial/ 2. Controlled clinical study/ 3. Random$.ti,ab. 4. randomization/ 5. intermethod comparison/ 6. placebo.ti,ab. 7. (compare or compared or comparison).ti. 8. ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 9. (open adj label).ti,ab. 10. ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 11. double blind procedure/ 12. parallel group$1.ti,ab. 13. (crossover or cross over).ti,ab. 14. ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 15. (assigned or allocated).ti,ab. 16. (controlled adj7 (study or design or trial)).ti,ab. 17. (volunteer or volunteers).ti,ab. 18. trial.ti. 19. or/1‐18 20. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 21. 19 not 20
Appendix 5. US National Institutes of Health Trials Register ClinicalTrials.gov search strategy
(surgery and ("third molar" or "3rd molar" or "wisdom tooth" or "wisdom teeth"))
Appendix 6. WHO International Clinical Trials Registry Platform search strategy
Advanced search:
Title: "third molar" Intervention: surgery
Data and analyses
Comparison 1. Surgical flap type (A versus B).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Alveolar osteitis (7 days) | 7 | Odds Ratio (IV, Random, 95% CI) | Subtotals only | |
| 1.1.1 Triangular flap (short) versus envelope flap | 5 | 187 | Odds Ratio (IV, Random, 95% CI) | 0.33 [0.09, 1.23] |
| 1.1.2 Pedicle flap versus envelope flap | 1 | 52 | Odds Ratio (IV, Random, 95% CI) | 0.08 [0.01, 0.97] |
| 1.1.3 Triangular flap (long) versus envelope flap | 1 | 45 | Odds Ratio (IV, Random, 95% CI) | 0.37 [0.02, 8.31] |
| 1.2 Wound infection (7 days) | 4 | Odds Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1.2.1 Triangular flap (long) versus envelope flap | 2 | 65 | Odds Ratio (IV, Fixed, 95% CI) | 0.29 [0.04, 2.06] |
| 1.2.2 Pedicle flap versus envelope flap | 1 | 52 | Odds Ratio (IV, Fixed, 95% CI) | 5.30 [0.47, 59.36] |
| 1.2.3 Reverse‐L versus alternative single incision flap | 1 | 33 | Odds Ratio (IV, Fixed, 95% CI) | 3.18 [0.56, 17.98] |
| 1.3 Permanent altered tongue sensation (> 6 months) | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 1.3.1 Triangular flap (long) versus envelope flap | 1 | 45 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 4.48 [0.07, 286.49] |
| 1.4 Adverse effects ‐ wound dehiscence (up to 30 days) | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 1.4.1 Triangular flap (short) versus envelope flap | 1 | 19 | Risk Ratio (IV, Fixed, 95% CI) | 1.00 [0.16, 6.38] |
| 1.4.2 Triangular flap (long) versus envelope flap | 1 | 20 | Risk Ratio (IV, Fixed, 95% CI) | 0.14 [0.02, 1.06] |
| 1.5 Pain present at 24 hours (yes/no) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.5.1 Triangular flap (long) versus envelope flap | 1 | 45 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.27, 5.70] |
| 1.6 Mean pain at 24 hours (0 to 10 VAS) | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.6.1 Triangular flap (short) versus envelope flap | 4 | 161 | Mean Difference (IV, Random, 95% CI) | ‐0.84 [‐1.65, ‐0.03] |
| 1.6.2 Comma‐shaped incision versus modified envelope flap | 1 | 100 | Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐1.37, ‐0.99] |
| 1.6.3 Reverse‐L flap versus alternative single incision flap | 1 | 33 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐1.41, ‐0.19] |
| 1.6.4 Triangular flap (long) versus envelope flap | 1 | 25 | Mean Difference (IV, Random, 95% CI) | ‐0.83 [‐2.92, 1.26] |
| 1.7 Swelling present (after 1 week) (yes/no) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.7.1 Triangular flap (long) versus envelope flap | 1 | 45 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.05, 1.21] |
| 1.8 Mean swelling (after 1 week) | 7 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.8.1 Triangular flap (short) versus envelope flap | 2 | 99 | Mean Difference (IV, Fixed, 95% CI) | 0.60 [0.25, 0.95] |
| 1.8.2 Pedicle flap versus envelope flap | 1 | 52 | Mean Difference (IV, Fixed, 95% CI) | 0.21 [‐0.09, 0.51] |
| 1.8.3 Comma‐shaped incision versus modified envelope flap | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | ‐2.38 [‐2.81, ‐1.95] |
| 1.8.4 Reverse‐L flap versus alternative single incision flap | 1 | 33 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.22, 0.62] |
| 1.8.5 Triangular flap (long) versus envelope flap | 2 | 40 | Mean Difference (IV, Fixed, 95% CI) | 0.68 [0.18, 1.18] |
| 1.9 Trismus (after 1 week) (yes/no) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.9.1 Triangular flap (long) versus envelope flap | 1 | 45 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.00 [0.24, 16.36] |
| 1.10 Maximum mouth opening (after 1 week) (SMD) | 2 | 158 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.67 [‐1.04, ‐0.30] |
| 1.10.1 Triangular flap (short) versus envelope flap | 2 | 158 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.67 [‐1.04, ‐0.30] |
| 1.11 Maximum mouth opening (after 1 week) (MD) | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.11.1 Comma‐shaped incision versus modified envelope flap | 1 | 100 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [0.07, 2.33] |
| 1.11.2 Triangular flap (long) versus envelope flap | 2 | 65 | Mean Difference (IV, Fixed, 95% CI) | ‐1.22 [‐2.11, ‐0.33] |
Comparison 2. Lingual nerve protection versus no protection.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Permanent altered sensation (up to 6 months) | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Subtotals only | |
| 2.1.1 Lingual flap and reflection versus no lingual flap | 1 | 380 | Peto Odds Ratio (Peto, Fixed, 95% CI) | 0.14 [0.00, 6.82] |
| 2.2 Temporary altered sensation (up to 1 month) | 3 | 735 | Odds Ratio (IV, Fixed, 95% CI) | 4.18 [1.75, 9.98] |
| 2.2.1 Subperiosteal lingual nerve protection versus none | 1 | 300 | Odds Ratio (IV, Fixed, 95% CI) | 3.39 [0.35, 32.97] |
| 2.2.2 Free's retractor lingual nerve protection versus none | 1 | 55 | Odds Ratio (IV, Fixed, 95% CI) | 12.09 [1.03, 142.26] |
| 2.2.3 Lingual flap and reflection versus no lingual flap | 1 | 380 | Odds Ratio (IV, Fixed, 95% CI) | 3.64 [1.31, 10.08] |
Comparison 3. Bone removal techniques.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Wound infection (7 days) | 1 | Odds Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.1.1 Lingual split chisel versus lingual split bur | 1 | 52 | Odds Ratio (IV, Fixed, 95% CI) | 1.00 [0.31, 3.21] |
| 3.2 Temporary alteration of tongue sensation (< 1 month) | 1 | Odds Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.2.1 Lingual split chisel versus lingual split bur | 1 | 52 | Odds Ratio (IV, Fixed, 95% CI) | 3.06 [0.27, 34.48] |
| 3.3 Temporary alteration of chin sensation (< 1 month) | 1 | Odds Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 3.3.1 Lingual split chisel versus lingual split bur | 1 | 52 | Odds Ratio (IV, Fixed, 95% CI) | 0.24 [0.04, 1.31] |
| 3.4 Pain at 24 hours (0‐to‐10 VAS) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.4.1 Lingual split chisel versus lingual split bur | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | 0.50 [0.08, 0.92] |
| 3.4.2 Ultrasound versus bur | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐1.32, 0.92] |
| 3.4.3 Lingual split (bur or chisel) versus simplified bone removal | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | ‐0.15 [‐0.43, 0.13] |
| 3.5 Mean pain at 24 hours (0‐to‐10 VAS) | 5 | 111 | Mean Difference (IV, Random, 95% CI) | ‐1.93 [‐3.08, ‐0.77] |
| 3.5.1 Piezoelectric surgery versus conventional | 5 | 111 | Mean Difference (IV, Random, 95% CI) | ‐1.93 [‐3.08, ‐0.77] |
| 3.6 Swelling (after 7 days) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.6.1 Lingual split chisel versus lingual split bur | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.33, 0.13] |
| 3.6.2 Ultrasound versus bur | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | 0.37 [0.20, 0.54] |
| 3.6.3 Lingual split (bur or chisel) versus simplified bone removal | 1 | 90 | Mean Difference (IV, Fixed, 95% CI) | 0.15 [‐0.01, 0.31] |
| 3.7 Maximum mouth opening (after 7 days) | 4 | 110 | Mean Difference (IV, Random, 95% CI) | 2.68 [0.54, 4.81] |
| 3.7.1 Piezoelectric surgery versus conventional ‐ split‐mouth | 4 | 110 | Mean Difference (IV, Random, 95% CI) | 2.68 [0.54, 4.81] |
| 3.8 Maximum mouth opening (after 7 days) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 3.8.1 Ultrasound versus bur | 1 | 26 | Mean Difference (IV, Fixed, 95% CI) | 2.90 [‐0.27, 6.07] |
Comparison 4. Wound irrigation techniques (A versus B).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Alveolar osteitis (7 days) | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1.1 Mechanical versus manual surgical wound irrigation | 1 | 99 | Risk Ratio (IV, Fixed, 95% CI) | 0.33 [0.01, 8.09] |
| 4.1.2 High‐volume versus low‐volume wound irrigation | 1 | 211 | Risk Ratio (IV, Fixed, 95% CI) | 0.52 [0.27, 1.02] |
| 4.2 Wound infection (7 days) | 2 | Risk Ratio (IV, Fixed, 95% CI) | Subtotals only | |
| 4.2.1 Mechanical versus manual surgical wound irrigation | 1 | 99 | Risk Ratio (IV, Fixed, 95% CI) | 0.50 [0.05, 5.43] |
| 4.2.2 High‐volume versus low‐volume wound irrigation | 1 | 211 | Risk Ratio (IV, Fixed, 95% CI) | 0.17 [0.02, 1.37] |
Comparison 5. Primary versus secondary wound closure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Alveolar osteitis (7 days) | 3 | 375 | Risk Ratio (IV, Fixed, 95% CI) | 0.99 [0.41, 2.40] |
| 5.2 Wound infection (7 days) | 1 | 82 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.77 [0.24, 96.34] |
| 5.3 Adverse effects ‐ reactionary bleeding | 1 | 82 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.11, 1.47] |
| 5.4 Pain at 24 hours (0‐to‐10 VAS) | 5 | 474 | Mean Difference (IV, Random, 95% CI) | 0.94 [0.50, 1.38] |
| 5.5 Swelling (after 7 days) | 7 | 557 | Mean Difference (IV, Random, 95% CI) | 0.33 [0.09, 0.57] |
| 5.6 Maximum mouth opening (after 7 days) | 4 | 274 | Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.90, 0.32] |
Comparison 6. Suturing techniques.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Maximum mouth opening | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 3.50 [2.69, 4.31] |
| 6.1.1 Fibrin sealant versus conventional suturing | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 3.50 [2.69, 4.31] |
Comparison 7. Surgical drain versus no drain.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Pain at 24 hours (0‐to‐10 VAS) | 2 | 180 | Mean Difference (IV, Fixed, 95% CI) | ‐0.19 [‐0.49, 0.12] |
| 7.2 Swelling at 7 days | 5 | 203 | Mean Difference (IV, Random, 95% CI) | ‐0.90 [‐1.62, ‐0.19] |
| 7.3 Maximum mouth opening at 7 days | 4 | 234 | Mean Difference (IV, Random, 95% CI) | 3.11 [2.20, 4.02] |
Comparison 8. Wound closure with blood products versus none.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Alveolar osteitis (7 days) split‐ mouth studies (OR/BB) | 2 | 128 | Odds Ratio (IV, Fixed, 95% CI) | 0.39 [0.22, 0.67] |
| 8.1.1 Platelet rich fibrin versus none | 2 | 128 | Odds Ratio (IV, Fixed, 95% CI) | 0.39 [0.22, 0.67] |
| 8.2 Mean pain at 24 hours (0‐to‐10 VAS) | 3 | 116 | Mean Difference (IV, Fixed, 95% CI) | ‐0.13 [‐0.59, 0.34] |
| 8.2.1 Platelet rich fibrin versus none | 3 | 116 | Mean Difference (IV, Fixed, 95% CI) | ‐0.13 [‐0.59, 0.34] |
| 8.3 Swelling at 7 days | 2 | 86 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.12, 0.35] |
| 8.3.1 Platelet rich fibrin versus none | 2 | 86 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.12, 0.35] |
Comparison 9. Coronectomy versus odontectomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Swelling at day 7 | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐0.18 [‐0.63, 0.27] |
| 9.2 Maximum mouth opening at day 7 | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | ‐2.94 [‐8.20, 2.32] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Absi 1993.
| Study characteristics | ||
| Methods | Study design: RCT (split‐mouth) Conducted in: Department of Oral Surgery, University Dental School, Cardiff, Wales, UK |
|
| Participants | Inclusion criteria: 52 consecutive healthy patients scheduled for surgery entered the trial after assessment with dental panoramic radiograph. All had similarly impacted bilateral lower third molars. Exclusion criteria: patients were excluded if they had pericoronitis in the 6 weeks before surgery, or if they were allergic to any of the drugs in the standard regimen Age: mean 22 years Number randomised: 52 Number evaluated: 52 |
|
| Interventions | Lingual split with chisel versus bur for bone removal under general anaesthesia Group A (n = 52 teeth): lingual split with chisel for bone removal Group B (n = 52 teeth): lingual split with bur for bone removal Follow‐up: 4 weeks All procedures were carried out under general anaesthetic. 43/52 participants had maxillary third molars extracted in same session. |
|
| Outcomes | Questionnaire assessment of lingual and inferior alveolar nerve function, swelling and pain were measured by a 4‐point scale at 6 h, 24 h, 48 h, and 7 days after the procedure. Participants also asked to indicate which side they felt was more swollen at these intervals. Infection was assessed by the presence of dry sockets or purulence or both. | |
| Notes | Sample size calculation: not reported Email sent to author (12 February 2003). Unpublished data supplied. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...the method for a particular side and the third molar removed first were selected randomly" After contacting author, method of randomisation disclosed as "nurse blindly selecting a piece of paper on which was written either 'left' or 'right' from a bag in which were placed equal numbers of pieces of paper with 'left' and 'right' written on them". |
| Allocation concealment (selection bias) | Low risk | The operator was blinded to the above randomisation procedure. Comment: allocation concealed |
| Blinding (performance bias and detection bias) patient | Low risk | Quote: "...the trial was single‐blind to the patient as far as the surgical method was concerned" Comment: as the procedures were carried out under general anaesthetic, it can be assumed that the participants were blinded to which side received which intervention |
| Blinding (performance bias and detection bias) assessor | Low risk | Outcome assessors (the participants) were blinded for pain, swelling, and sensory disturbances. "on day 7... the wounds were examined by an independent observer" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts |
| Selective reporting (reporting bias) | Low risk | The author was unable to specify which group (and indeed which socket ‐ upper or lower) received an acute abscess, despite direct correspondence on the matter. |
| Other bias | Unclear risk | In 43 of the 52 participants, maxillary third molars were also extracted; however, we contacted the author, who assured us that none of these were surgical. Author notes: "higher complication rates might have been found if this information had been supplemented by clinical assessments", noting the limitations of subjective assessment |
Acar 2017.
| Study characteristics | ||
| Methods | Study design: RCT; split‐mouth/cross‐over Conducted in: Turkey |
|
| Participants | Inclusion criteria: each participant had fairly symmetrically positioned, bone retained asymptomatic and class III B surgical difficulty grade (scales of Pell–Gregory and Winter) mandibular third molars Exclusion criteria: patients with any systemic disease, pregnancy, poor oral hygiene, or aged Age: above 18 years Number randomised: 30 participants/60 teeth; 4‐week interval between the 2 surgeries |
|
| Interventions | Horizontal mattress suturing versus simple interrupted suturing Group A: (30 teeth) 3 simple interrupted sutures on 1 side Group B: (30 teeth) 2 horizontal mattress sutures on the other side (both achieving primary closure) Preoperatively: 0.2% chlorhexidine mouth rinse for 30 seconds. Then, 2 mL and 1 mL of articaine with 1:200,000 epinephrine were administered to sustain local anaesthesia of the inferior alveolar nerve and buccal nerve, respectively. | |
| Outcomes | Pain (0‐to‐100‐millimetre VAS) Trismus (interincisal distance) Swelling (mean of 5 measurements) |
|
| Notes | "The recorded data were analysed using the Statistical Package for Social Sciences (version 23.0; SPSS, IBM Corp, Armonk, NY). The Shapiro–Wilk test was used to test the normal distribution of individual parameters. Non‐parametric distributed data (pain, trismus, and swelling) were tested with the Mann–Whitney U test for differences in parameters between the groups. Wound healing was evaluated with Pearson correlation test for assessment of statistically significant differences. A value of P < 0.05 was accepted as statistically significant." Sample size calculation: reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The type of suturing technique was randomly selected for each side" Comment: no further details are given on the method of randomisation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details are given on any attempts to conceal the allocations |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: not described, and the participant consent process was also not discussed |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Quote: "These data were collected by another surgeon" Comment: it is not specified if the other surgeon was blinded to the allocations |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts reported. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | None identified |
Arakji 2016.
| Study characteristics | ||
| Methods | Study design: RCT (split‐mouth) Conducted in: Beirut, Lebanon, Faculty of Dentistry |
|
| Participants | Inclusion criteria: male patients having bilateral mandibular mesioangular impacted third molars (Pell and Gregory class II, position B) Exclusion criteria: heavy smokers (≥ 25 cigarettes), uncontrolled systemic conditions, pathologies, and infection related to the site of surgery Age: 18 to 35 Number randomised: 20 Number evaluated: 20 |
|
| Interventions | Comparison: conventional techniques versus piezosurgery for bone removal Group A (n = 20 teeth) control site (conventional surgical hand‐piece, 35,000 rpm) Group B (n = 20 teeth) study site (piezosurgery, frequency was adjusted between 28 and 36 kHz and the microvibration amplitude between 30 and 60 micrometres/s) (Of note, conventional surgical handpiece was used to section the teeth in both control and test sites.) Preoperative chlorhexidine mouthwash was used by all participants. All operations were undertaken by the same surgeon under local anaesthesia consisting of 2% lidocaine hydrochloride with 1:80,000 adrenaline. Both sites were prepared with 5% povidone iodine solution. |
|
| Outcomes | Pain (VAS), trismus (IID measurement), and swelling (measured by tape length). These were evaluated on days 1, 7, and 14 postoperation. Bone density evaluated by the use of IOPA radiograph at baseline, 3, 6 months postoperation using ImageJ software. Marginal bone height along the distal aspect using cone beam computed tomography (CS 9300, Carestream, USA), which was taken immediately, 3 and 6 months postoperation |
|
| Notes | Test and control sites were compared regarding the study clinical and radiographic variables using paired t‐test. Significance level was set at the 5% level. Statistical analysis was performed using SPSS version 20.0. Sample size calculation: reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quotes: "Sites were randomly selected by tossing a coin" Comment: coin‐tossing method was used |
| Allocation concealment (selection bias) | Unclear risk | Comment: unclear who performed the allocation and whether it was concealed from operator |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: participants were treated under local anaesthetic only, therefore it is possible that they were aware of which side had the intervention due to the differences in noise levels between the piezosurgery and conventional rotary instruments |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Comment: it is not clear who carried out the postoperative assessments |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All 20 participants completed the study period up to 6 months. |
| Selective reporting (reporting bias) | Low risk | Planned outcomes were reported. |
| Other bias | Unclear risk | It remains unclear how participants were recruited to the study, and it is also unclear why all the participants were male. |
Baqain 2012.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: Jordan University Hospital, Amman, Jordan |
|
| Participants | Inclusion criteria: symmetrically impacted mandibular third molars, with comparable positioning and angulation, no acute local inflammation or pathology Exclusion criteria: systemic diseases, pregnancy, lactation, smokers, medications that would influence the surgical procedure or wound healing Age: mean 21.4 ± 2.3, 18 to 26 years Number randomised: 20 Number evaluated: 19 |
|
| Interventions | Buccal envelope flap versus triangular flap Group A (n = 19 teeth): sulcular incision from first to second mandibular molar with distal incision along mandibular ramus Group B (n = 19 teeth): incision commenced distally from the mandibular ramus to the disto‐buccal aspect of the second molar, then a sulcular incision near mesio‐buccal edge of M2 was made extending to its distal surface, finally a relieving incision from disto‐buccal aspect of M2 curving forward into mandibular vestibule Follow‐up: 14 days, 2‐week interval between the 2 sides All procedures were carried out by the same surgeon, using the same instruments (rotary and irrigation devices and materials) under sedation with intravenous midazolam and local anaesthetic. |
|
| Outcomes | Pain (VAS 1 to 10), swelling, trismus, periodontal examination of adjacent M2, alveolar osteitis, wound infection at 2, 7, and 14 days | |
| Notes | Sample size calculation: not reported Although alveolar osteitis was one of the outcome measures, no cases of postoperative infection or dry socket occurred in either group. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...randomly assigned using electronic randomization tables with patients numbered according to the order in which they presented for surgery" |
| Allocation concealment (selection bias) | Unclear risk | Unclear who performed the allocation and whether it was concealed from operator |
| Blinding (performance bias and detection bias) patient | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) assessor | High risk | Not mentioned; assessment probably performed by operator |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One randomised participant did not have second procedure. This is unlikely to have introduced bias. |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported in full. |
| Other bias | Low risk | No other sources of bias identified. |
Barone 2010.
| Study characteristics | ||
| Methods | Study design: RCT (parallel group) Conducted in: Versilia Hospital, Lido di Camaiore, Italy |
|
| Participants | Inclusion criteria: people referred for lower third molar extraction at Versilia Hospital who were systemically healthy Exclusion criteria: people with a history of systemic diseases that would contraindicate surgery, pregnant and lactating women, people in whom there was no need to raise the mucoperiosteal flap to remove the third molar, and people who smoked more than 10 cigarettes per day Age: mean 31.2 years Number randomised: 26 Number evaluated: 26 |
|
| Interventions | Ultrasound versus rotary instruments for bone removal Group A (n = 13): surgical removal of lower third molar using ultrasonic bone surgery under local anaesthesia Group B (n = 13): surgical removal of lower third molar using traditional rotary instruments under local anaesthesia (Rotary instruments were used for sectioning of teeth where necessary.) All procedures performed under local anaesthetic. Follow‐up: at days 1, 3, 5, and 7 |
|
| Outcomes | Surgical time (start of first incision to last suture) Pain (0‐to‐10 VAS) at days 1, 3, 5, and 7 Trismus (interincisal distance measured using callipers) at days 1, 3, 5, and 7 Cheek swelling (measured with a standard calliper from the lingual aspect of the midportion of the crown of the first mandibular molar to the tangent of the cheek's skin) at days 1, 3, 5, and 7 |
|
| Notes | Sample size calculation: not reported At baseline (parallel groups only) groups were comparable with regard to type of impaction. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "An independent evaluator allocated the patients into the test and control groups according to a computer‐generated randomisation list" |
| Allocation concealment (selection bias) | Low risk | Allocation was performed by an independent evaluator. |
| Blinding (performance bias and detection bias) patient | Unclear risk | All surgery performed on participants under local anaesthetic only, therefore blinding not possible |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Unclear who carried out the postoperative assessments |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants evaluated. |
| Selective reporting (reporting bias) | Low risk | Pain, swelling, trismus, analgesic consumption planned and recorded. |
| Other bias | Low risk | Groups appeared to be similar at baseline. |
Basheer 2017.
| Study characteristics | ||
| Methods | Study design: parallel RCT Conducted in: India |
|
| Participants | Inclusion criteria: healthy patients above 20 years of age. Individuals having vertical, mesioangular, horizontal mandibular third molar impactions based on radiographic interpretation Exclusion criteria: patients with systemic disease that could influence healing, patients who do not provide consent, patients on antibiotics in the past 6 weeks or who require antibiotic prophylaxis before extraction, and patients who had acute local infection involving the impacted teeth Age: above 20 years old Number evaluated: 30 participants/30 teeth |
|
| Interventions | Piezoelectric versus rotary osteotomy technique for bone removal Group I: piezoelectric osteotomy technique (frequency of 25 to 29 kHz with a microvibration of 60 to 200 mm/s was used with a boosted working mode) Group II: rotary osteotomy technique (35,000 rpm) All participants underwent surgical removal of impacted mandibular third molars under 2% lidocaine with 1:200,000 adrenaline, with inferior alveolar, lingual, and long buccal nerve blocks administered. Postoperatively, all participants received amoxicillin 500 mg 3 times a day and diclofenac sodium 50 mg 3 times a day for 3 days. Postoperative instructions were given, and the sutures were removed on the seventh day. |
|
| Outcomes | Pain VAS (no pain to severe pain) Trismus (interincisal distance) Swelling Other outcomes: time taken for the procedure; patient satisfaction |
|
| Notes | Descriptive analysis was done. Results are explained as mean ± standard deviation (min to max) and also as number (%): 5% was considered as level of significance with 95% confidence interval. Quantitative data were analysed using unpaired t‐test, and qualitative data were analysed using Fisher’s exact test. Sample size calculation: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "individuals were randomly allocated to study groups" Comment: method of randomisation was not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: methods of concealment were not discussed |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: it is unclear if the participants were blinded as they consented to the procedure |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Comment: blinding is not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no reported dropouts. |
| Selective reporting (reporting bias) | Low risk | All of the outcomes were reported. |
| Other bias | High risk | Quote "to standardize our results, it was conducted on 30 male individuals having their age ranging from 25 to 33 years, in order to remove the gender factor that may play a role in postoperative complications due to hormonal changes that may occur in females" Comment: this study only included males, therefore the results are limited to this study population |
Bello 2011.
| Study characteristics | ||
| Methods | Study design: RCT parallel group Conducted in: Department of Oral and Maxillofacial Surgery, National Hospital, Abuja, Nigeria Number of centres: 1 Recruitment period: not stated |
|
| Participants | Inclusion criteria: patients referred for extraction of 1 or 2 impacted mandibular third molars Exclusion criteria: patients with acute pericoronal infection, systemic diseases, or bleeding disorder, patients receiving steroid therapy or contraceptives, and smokers were excluded. Patients whose extraction procedure took more than 35 minutes were also excluded. Number randomised: unclear Number evaluated: 82 |
|
| Interventions | Partial versus complete wound closure Group A (n = 40): partial wound closure was achieved using 4 interrupted sutures leaving a window communicating with the oral cavity Group B (n = 42): complete wound closure was achieved using 5 interrupted sutures that sealed off communication with the oral cavity All procedures done under local anaesthetic by the same surgeon. All participants received pre‐emptive antibiotics (amoxicillin and metronidazole) for 5 days and diclofenac for pain and inflammation for 3 days. |
|
| Outcomes | Pain (VAS 0 to 10) reported daily for 7 days. Maximal interincisal distance (as % of baseline value) and swelling (difference from baseline) were evaluated on days 2, 5, and 7. Numbers of postoperative complications (dry socket, infection, and secondary haemorrhage) were also noted. | |
| Notes | Sample size calculation: not reported E‐mail sent 12 March 2012 requesting further information about the methods used. Reply received 21 March 2012 with unpublished data. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomly allocated" Comment: allocated by drawing lots to either partial or total (e‐mail correspondence) |
| Allocation concealment (selection bias) | Low risk | A paper was drawn by the assistant and shown to the surgeon prior to suturing (e‐mail correspondence). |
| Blinding (performance bias and detection bias) patient | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Assessment done using a "clean proforma", but it is possible that the assessor knew which group the participant was in. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 90 patients were screened for inclusion but unclear how many were randomised. Patients were excluded when the procedure took more than 35 minutes (n = 3). 8 patients did not return for follow‐up assessment, 5 and 3 in each group. |
| Selective reporting (reporting bias) | Low risk | Planned outcomes of pain, trismus, swelling, and complications reported. |
| Other bias | Low risk | No other sources of bias identified. This study excluded patients whose surgeries exceeded 35 minutes; the reason for this was not explained. |
Bhati 2017.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: India |
|
| Participants | Inclusion criteria: patients requiring bilateral surgical removal of impacted mandibular third molars and willing to take part in the study Exclusion criteria:
Age: 27.43 ± 5.27 years Number evaluated: 30 participants/60 teeth |
|
| Interventions | Piezoelectric versus rotary osteotomy technique for bone removal Test group: piezosurgery Control group: conventional rotary hand‐piece (35,000 rpm) Lidocaine 2% with 1:200,000 adrenaline was used for inferior alveolar nerve block along with long buccal nerve block and lingual nerve block. All participants routinely received postoperative dose of oral antibiotics in the form of capsule ampicillin 250 mg plus cloxacillin 250 mg and tablet metronidazole 400 mg 3 times daily for 5 days, and analgesics in a combination of tablet ibuprofen 400 mg and paracetamol 325 mg 3 times daily for 3 days. Participants were recalled on the first, third, and seventh postoperative days for follow‐up. |
|
| Outcomes | Pain VAS (0 to 10) Swelling (this was achieved using a 3‐0 silk suture to measure the distance between the angle of lower jaw (G), and each of 4 facial reference point‐linear distances to tragus, lateral canthus, alar, and pogonion were recorded) Trismus (interincisal distances) Paraesthesia: evaluated by light touch (cotton wisp) and 2‐point discrimination Dry socket (Blum criteria) |
|
| Notes | Sample size calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: method of randomisation unclear |
| Allocation concealment (selection bias) | Unclear risk | Comment: concealment methods not described |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: participants signed an informed consent agreement, but details discussed are unclear |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Comment: unclear who carried out outcome measurements |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no dropouts mentioned |
| Selective reporting (reporting bias) | Low risk | Comment: all planned outcomes reported |
| Other bias | Unclear risk | Comment: split‐mouth study. No mention of when the extraction on the contralateral side took place. No analysis of any carry‐over effect |
Briguglio 2011.
| Study characteristics | ||
| Methods | Study design: parallel‐group RCT Conducted in: Brazil (but researchers based in Italy) |
|
| Participants | Inclusion criteria: patients between the ages of 18 and 41 requiring extraction of mandibular third molars. Those with moderate impaction mesio‐angularly with a tilt degree more than 25° in relation to the second molar. Only impacted third molars with distil periodontal defects at the second molar with PPD ≥ 7 mm and CAL ≥ 6 mm were selected. Exclusion criteria: systemic disease, pregnancy, smoking, and medication (unspecified) Age: 18 to 45 years Number randomised: 45 Number evaluated: 45 |
|
| Interventions | Laskin triangular flap versus Thibault and Parant modified envelope flap versus Laskin envelope flap Group A (n = 15): Laskin triangular flap Group B (n = 15): Thibault and Parant modified envelope flap Group C (n = 15): Laskin envelope flap All participants had a preoperative dental hygiene check, and procedures were performed under local anaesthetic. All participants given 1 g amoxicillin + sulbactam preoperation, and all used CHX mouthwash pre‐ and postoperation. |
|
| Outcomes | Short‐term complications (pain swelling and infection) and PPD and CAL at 3, 6, 12, and 24 months | |
| Notes | Sample size calculation: not reported Gaetano Isola provided additional data on short‐term complications by e‐mail 7 March 2012. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: whilst the technique used in each case was randomly selected, the authors do not specify any further details on this allocation process |
| Allocation concealment (selection bias) | Unclear risk | Comment: no details of the allocation concealment provided |
| Blinding (performance bias and detection bias) patient | Unclear risk | Quote: "A clot of PRF, which was produced in a 10 ml tube, was enough to fill the socket of each patient." Comment: it is unclear if all participants had blood samples taken, or whether samples were only taken from participants in the PRF group. This could be a source of bias. |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "all measurements were assessed by the same person (not the operating surgeon)" Comment: the assessor was blind to the allocations |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: all randomised participants were included until the end of the study |
| Selective reporting (reporting bias) | Low risk | All planned outcomes were reported on. |
| Other bias | High risk | Comment: some participants had unilateral extractions, whilst others had bilateral extractions. This could have influenced outcomes such as pain perception and trismus. |
Butler 1977.
| Study characteristics | ||
| Methods | Study design: RCT (split‐mouth) Conducted in: Bethesda, Maryland, USA |
|
| Participants | Inclusion criteria: patients with bilaterally symmetrical impactions with regard to depth and angulation. Partial or complete impactions were also accepted. Exclusion criteria: patients with evidence of acute infection or severe pericoronitis around the wisdom teeth were excluded from the study Number randomised: 211 Number evaluated: 211 participants/422 teeth |
|
| Interventions | High‐volume irrigation versus low‐volume irrigation Group A (n = 211): postextraction irrigation with 175 mL sterile saline under IV sedation Group B (n = 211): postextraction irrigation with 25 mL sterile saline under IV sedation Follow‐up: at 4, 5, or 6 days All procedures performed under intravenous sedation. |
|
| Outcomes | Presence of alveolar osteitis at recall 4 to 6 days later | |
| Notes | Sample size calculation: not reported In 32 cases a mechanical irrigation device was used for irrigation in the higher‐volume site. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "a random selection technique was used" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Unclear risk | As participants were sedated, they were highly unlikely to be aware of which volume of irrigant they received and where. However, this may be confounded by the 32 cases in which a mechanical irrigating device was used (see below). |
| Blinding (performance bias and detection bias) assessor | High risk | No mention of assessor blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdrawals |
| Selective reporting (reporting bias) | Unclear risk | The authors state that "patients were examined on the fourth, fifth, or sixth postoperative day for evidence of localised osteitis". However, they go on to mention that most "infections" occurred between the seventh and 10th postoperative days. The outcome of infection was not mentioned at the outset, regardless of the fact of a non‐significant result. |
| Other bias | High risk | Quote: "...most patients also had one or two maxillary third molars removed, but these operations were not included in the investigation" Comment: multiple extraction sites may influence the presence of alveolar osteitis and therefore should be considered as a confounding factor In 32 cases a mechanical irrigating device was used to provide the higher volume of irrigant, thus also confounding the results. |
Cerqueira 2004.
| Study characteristics | ||
| Methods | Study design: RCT split‐mouth Conducted in: Pernambuco, Brazil Number of centres: 1 Recruitment period: not stated |
|
| Participants | Inclusion criteria: patients aged 14 to 30 years, with bilateral impacted third molars in similar positions on each side of the mouth Exclusion criteria: patients using medications that could interfere with healing or those with systemic disease Number invited: 5 patients underwent surgery "with the purpose of calibration", and a further 12 were excluded because they "proved to be unsuitable" Number randomised: 53 Number evaluated: 53 |
|
| Interventions | Drain versus no drain Group A (n = 53): 1 side of the mouth, chosen at random, had a silicon tube drain inserted into the buccal fold. Drain in situ for 4 days Group B (n = 53): on the opposing side the wound was sutured with no drain All participants received preoperative antibiotic prophylaxis (amoxicillin) and postoperative cetoprophen for 4 days. All procedures performed under local anaesthesia. |
|
| Outcomes | Pain (0‐to‐10 VAS), maximal mouth opening, swelling (% of preoperative) on postoperative days 1, 3, 7, and 15 | |
| Notes | Sample size calculation: not reported E‐mail sent to Dr Vasconcelos at belmiroc@terra.com.br on 6 March 2012 requesting further information. No reply received. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The choice of treatment "was made randomly". |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Unclear risk | Not mentioned and probably not possible |
| Blinding (performance bias and detection bias) assessor | High risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All 53 participants were evaluated. |
| Selective reporting (reporting bias) | Low risk | Planned outcomes of pain, swelling, and trismus reported. |
| Other bias | Low risk | No other sources of bias identified. |
Chukwuneke 2008.
| Study characteristics | ||
| Methods | Study design: parallel‐group, single‐blind RCT Conducted in: oral surgery department of University of Nigeria Teaching Hospital, Enugu, Nigeria |
|
| Participants | Inclusion criteria: patients who were willing to come for their follow‐up appointments, who were free from pain or any other inflammatory symptoms (swelling, hyperaemia, TMD), had impacted lower wisdom teeth, were not on medication that could interfere with healing, and did not smoke or have any systemic disease Exclusion criteria: pregnant or lactating females were excluded from the study Number randomised: 100 Number evaluated: 100 |
|
| Interventions | Rubber tube (Penrose) drain versus no drain Group A (n = 50): sutures plus Penrose rubber drain placement for 72 h Group B (n = 50): sutures only postoperatively All participants received 2 g amoxicillin preoperatively, and procedures were performed under local anaesthesia. Follow‐up: 24 h, 72 h, and 5 days |
|
| Outcomes | Pain (0‐to‐10 VAS), swelling (horizontal and vertical guide with tape and reference points), and trismus (interincisal callipers). Evaluated at 24 h, 72 h, and 5 days postoperatively | |
| Notes | Sample size calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...a prospective, randomised, single‐blind experimental study was undertaken" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | High risk | Participants could not have been blinded to the treatment group they were in, as they would have been aware of the presence of the Penrose rubber drain in their mouths. This is evidenced in the photographs. |
| Blinding (performance bias and detection bias) assessor | Unclear risk | There is no mention of assessor blinding other than "a prospective, randomised, single‐blind experimental study was undertaken". However, it is not clear to whom this single‐blinding refers. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdrawals |
| Selective reporting (reporting bias) | Low risk | All planned outcomes reported on. |
| Other bias | Unclear risk | The study accepted all impactions, but there was no report of measures to account for possible differing degrees of difficulty with the extractions. Whilst appropriate randomisation should result in groups with similar proportions of high‐risk patients, no baseline characteristics were reported in this trial. It is unclear whether these biases were avoided. |
Danda 2010.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: India Number of centres: 1 Recruitment period: May 2005 to March 2008 |
|
| Participants | Inclusion criteria: patients requiring removal of bilateral impacted third molars, for prophylactic or therapeutic reasons. Partial or complete bony impaction Exclusion criteria: patients with medical problems that would contraindicate oral surgery, bone pathology, immunocompromised patients, and those with soft‐tissue impaction of mandibular third molars Number randomised: 93 Number evaluated: 93 |
|
| Interventions | Primary versus secondary closure Group A (n = 93): primary closure (2 sutures on distal arm and 1 on mesial arm of incision) Group B (n = 93): secondary closure (wedge of mucosa removed distil to second molar, then 1 suture on mesial and another on distil arm of the incision) All procedures performed under local anaesthesia. |
|
| Outcomes | Pain and swelling measure on a VAS (0 to 4) daily for 7 days. Alveolar osteitis and nerve damage also reported. | |
| Notes | Sample size calculation: not reported E‐mail sent to Dr Danda (anilomfs@gmail.com) on 6 March 2012 requesting further information. No reply received. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information regarding the method used to select the side of the mouth for each procedure |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) assessor | High risk | Participants assessed the outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No mention of dropouts, but it is unlikely that all randomised participants were included in outcomes. |
| Selective reporting (reporting bias) | Low risk | All planned outcomes reported. |
| Other bias | Low risk | No other sources of bias identified. |
de Brabander 1988.
| Study characteristics | ||
| Methods | Study design: RCT (parallel) Conducted in: Eastman Dental Center, New York, USA |
|
| Participants | Inclusion criteria: unilateral wisdom tooth needing extraction Exclusion criteria: patients with clinical signs of pericoronitis, or those whose surgery took longer than 20 minutes from the first incision Number randomised: 21 Number evaluated: 21 |
|
| Interventions | Gauze drain versus no drain Group A (n = 11): postextraction placement of a Vaseline‐coated gauze drain partially submerged into the socket, sutured in place Group B (n = 10): postextraction removal of a wedge of tissue distal to the second molar before closure Surgery was performed under local anaesthetic. Follow‐up: 2 and 7 days |
|
| Outcomes | Pain (0‐to‐10 VAS), swelling (examiner VAS, and comparisons with preoperative calliper measurements), trismus (interincisal distance), dry socket | |
| Notes | Sample size calculation: not reported Baseline characteristics of groups not reported. Letter sent to author (May 2003). Reply that no additional data were available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...made on a randomised basis by an individual other than the surgeon performing the procedure"; "the operator did not know whether a drain would be inserted until the time of closure" |
| Allocation concealment (selection bias) | Low risk | Quote: "The decision on whether a drain should be inserted was made on a randomised basis by an individual other than the surgeon performing the procedure" Comment: unclear if was this concealed from the surgeon |
| Blinding (performance bias and detection bias) patient | Unclear risk | Quote: "...the patients were not informed of the potential advantages or disadvantages of the drain", though participants still likely to detect presence of drain in operation site, therefore blinding of participants not possible |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Subsequently, pain assessments by the participants using a VAS were not blinded either: "...the patients were routinely examined by an examiner who was not the surgeon and not aware of the treatment given", therefore assessor was blinded for swelling, trismus, and dry socket. Unclear when drain was removed and whether examiner could have determined whether a drain had been placed |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No withdrawals mentioned, but numbers evaluated not stated. Only means per group were reported. |
| Selective reporting (reporting bias) | Low risk | Although the authors only mention dry socket in the results section, it should be noted that the investigators were looking for dry socket at the outset, regardless of the fact that there was no incidence of this outcome in either group. |
| Other bias | Unclear risk | An exclusion criterion precludes any cases that took longer than 20 minutes from the first incision to removal of the tooth. The authors do not mention whether more participants were included in the study beforehand but subsequently had to withdraw because of lengthy surgery; these participants were not accounted for in the text, if indeed there were any. |
Dutta 2016.
| Study characteristics | ||
| Methods | Study design: parallel RCT Conducted in: India |
|
| Participants | Inclusion criteria
Exclusion criteria
Number evaluated: 40 participants/40 teeth |
|
| Interventions | A randomised comparative prospective study of platelet‐rich plasma (PRP), platelet‐rich fibrin (PRF), and hydroxyapatite (HA) as a graft material for mandibular third molar extraction socket healing Participants were randomly distributed into 4 groups of 10 participants. Control: extraction socket closed without any graft material PRP‐treated group: extraction socket filled with PRP before closure of the sockets PRF‐treated group: extraction socket filled with PRF before closure of the socket HA‐treated group: extraction socket filled with HA before closure of the socket Extraction of mandibular third molars was done under local anaesthesia using the standard technique. A triangular flap using ward‐I or ward‐II incision or an envelope flap was raised. |
|
| Outcomes | Swelling: mean of 3 measurements Pain: VAS based on 6‐point facial Wong‐Baker Scale (cannot be used in data analysis due to lack of clarity) Dry socket: Blum's method Soft tissue healing Radiographic (IOPA) assessment |
|
| Notes | Sample size calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the method of randomisation is not described |
| Allocation concealment (selection bias) | Unclear risk | Concealment methods are not described. |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: the participants gave their consent to the procedure, but details are not provided as to how much information they were given. It is also unclear whether the participants in the control and HA groups also had their blood taken (if they were blinded to the group allocation, not having blood taken would indicate what remaining groups they were in). |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Comment: it is unclear who measured the outcome variables |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts were mentioned. |
| Selective reporting (reporting bias) | Low risk | All planned outcomes were reported. |
| Other bias | High risk | Comment: there is a potential source of bias due to inconsistencies in the methodology, namely the surgical approach. The methods state "a triangular flap using Ward‐I or Ward‐II incision or an envelope flap was raised". |
Erdogan 2011.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: Adana, Turkey Number of centres: 1 Recruitment period: January 2008 to June 2009 |
|
| Participants | Inclusion criteria: participants were aged 20 to 32 years with bilateral symmetrically impacted mandibular third molars. Participants were free of systemic disease and had no history of pericoronal infection or recent anti‐inflammatory drug use. Included teeth were all class I or II and position A or B according to Pell and Gregory classification. Exclusion criteria: deeply impacted cases were not included in the study Age: mean 23.9 ± 4.3, 20 to 32 years Number randomised: 20 Number evaluated: 20 |
|
| Interventions | Envelope flap versus triangular flap Group A (n = 20): sulcular incision extending from the lateral border of the mandibular ramus to the second premolar with no releasing vertical incision Group B (n = 20): buccal releasing incision positioned on the mesial aspect of the second molar All participants had preoperative single dose of oral penicillin and rinsed with CHX. All surgical procedures were performed by the same surgeon under local anaesthetic, and incisions were closed with secondary wound closure. Second extraction was performed after 3 weeks. |
|
| Outcomes | Operating time, mouth opening, VAS (0 to 10) pain (resting and chewing), analgesic consumption | |
| Notes | No sample size calculation reported. Probably underpowered. E‐mail sent 25 March 2013, and reply from authors provided additional information. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quotes: "...selected randomly to have their first operations on the left side…. For the first extraction the flap design was chosen randomly" "A coin toss was used to determine the flap type and surgical site at the day of the first surgery" (e‐mail communication) |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Coin toss was conducted by junior surgeon, and an experienced surgeon performed the surgery" (e‐mail communication) |
| Blinding (performance bias and detection bias) patient | Low risk | Double‐blind |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "A blinded surgeon who was not aware of the flap design, conducted the measurements" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data reported for all 40 procedures on all 20 participants. |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported. |
| Other bias | Low risk | No other sources of bias identified. |
Eshghpour 2014.
| Study characteristics | ||
| Methods | Study design: double‐blinded, randomised clinical trial, split‐mouth technique Conducted in: Iran |
|
| Participants | Inclusion criteria: 18 to 35 years of age, have American Society of Anesthesiologists physical status I or II; have bilateral mandibular third molars; have the same difficulty level of bilateral third molars based on the Pederson classification Exclusion criteria: pericoronitis of the mandibular third molar(s), received antibiotic regimen during the previous 2 weeks, had a smoking habit, was lactating or pregnant, was using oral contraceptives, had any lesions found on the panoramic radiograph, had any complications during extractions, or had received more than 2 anaesthetic cartridges during surgery Number randomised: 85 Number evaluated: 78 (bilateral impacted teeth) (33 male and 45 female; mean age 25.09 years) |
|
| Interventions | Comparison: placement of PRF versus none in the extracted socket PRF was placed in 1 of the sockets, and the other socket received no treatment. Group A intervention (n = 78) Group B control (n = 78) Note: postoperative prescriptions were amoxicillin (500 mg 3 times daily, n = 21) and paracetamol (500 mg 3 times daily, for a maximum of 3 days) |
|
| Outcomes | Alveolar osteitis at days 2 and 7 Based on the c2 analysis, the frequency of alveolar osteitis had a significant association with the application of PRF. Sockets that received PRF after extraction had a statistically significant decreased risk of developing alveolar osteitis compared with non‐PRF sockets (risk ratio 0.44, 95% confidence interval 0.148 to 0.989; P = 0.042). |
|
| Notes | Descriptive statistics (frequency, mean, and standard deviation) were determined for each variable. Data analysis was performed with c2 and t tests using SPSS 11.5 (SPSS Inc, Chicago, IL), with a confidence interval of 95%. Sample size calculation: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "PRF was randomly inserted into one of the sockets" Comment: coin toss technique was used to decide which side received intervention or control |
| Allocation concealment (selection bias) | Unclear risk | Comment: not clear whether randomisation of participants was done by someone different from the person who recruited participants |
| Blinding (performance bias and detection bias) patient | Unclear risk | Quote: an operator blinded to the surgery performed the PRF insertion and suturing. Hence, the participants and the surgeon were blind to the side in which PRF had been inserted. Comment: all participants had blood taken and PRF placed. However, a new surgeon coming in to work on one side of the mouth would reveal which side the PRF went into. |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "the randomisation data were kept unknown by another investigator until the end of the study" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "eighty‐five patients met the inclusion criteria and entered the study; however, 6 patients received more than 2 anesthetic cartridges and 1 female patient had used oral contraceptives during the first postoperative week (as emergency birth control). Therefore, 78 patients (33 male and 45 female; mean age, 25.09 Æ 4.25 yr) completed the study" Comment: 85 participants were recruited, and the outcomes of 78 were reported. Justification for this was provided. |
| Selective reporting (reporting bias) | Low risk | Planned outcomes were reported. |
| Other bias | Low risk | No other sources of bias identified. |
Gargallo‐Albiol 2000.
| Study characteristics | ||
| Methods | Study design: RCT (parallel group) Conducted in: Department of Oral Surgery, Odontology, University of Barcelona, Spain |
|
| Participants | Inclusion criteria: 300 consecutive patients who needed 1 lower impacted wisdom tooth extracted Exclusion criteria: if the tooth did not need to be sectioned during the procedure, then it was excluded from the study Age: mean 27.4 years Number randomised: 300 Number evaluated: 300 |
|
| Interventions | Lingual nerve protection (subperiosteal retractor) versus none Group A (n = 142): lower third molar removed with subperiosteal insertion of retractor for lingual nerve protection Group B (n = 158): lower third molar removed without lingual nerve protection All molars removed under local anaesthetic. Follow‐up: days 7, 21, and 60 |
|
| Outcomes | Verbal self‐assessment and mechanosensory testing of lingual nerve function | |
| Notes | Sample size calculation: not reported The author notes that the low incidence of sensory disturbance in this study may be related to the fact that the procedures were performed under local anaesthetic. Previous studies may indicate that procedures performed under general anaesthetic are associated with higher levels of sensory disturbances, but as the author rightly points out: "the choice of general anaesthesia [...] may also be related to the degree of difficulty when removing the third molar". Baseline comparability: information about the comparability of the groups at baseline not reported Letter sent to author who replied that no additional data were available. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...patients were strictly randomised" Comment: method of sequence generation not stated |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Unclear risk | Participant blinding is not mentioned, but it is likely that participants were aware of whether or not a retractor was used. |
| Blinding (performance bias and detection bias) assessor | High risk | Quote: "...lingual nerve function was tested at one week [...] and was carried out by the same surgeon who performed the procedure" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdrawals mentioned, results reported as percentage and appear to include all randomised participants. This was confirmed by correspondence with author. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported on. |
| Other bias | Low risk | No other sources of bias identified. |
Gogulanathan 2015.
| Study characteristics | ||
| Methods | Study design: RCT split‐mouth method Conducted in: India |
|
| Participants | Inclusion criteria: over 18 years of age; ASA 1 (American Society of Anesthesiology) patient with no systemic diseases or conditions; patient requiring surgical removal of bilaterally impacted mandibular third molars; bilateral impactions with a relatively similar classification and degree of difficulty, based on the Pell and Gregory system; patient agreement to the surgical procedure and clinical trial, providing informed consent Exclusion criteria: presence of systemic diseases; presence of bleeding disorders; patients on antiplatelet or anticoagulant therapy; pregnant or nursing mothers; patients with a known history of allergy to lidocaine; patient not consenting to the procedure or study Number randomised: 30 participants/60 teeth Number evaluated: 30 participants |
|
| Interventions | Fibrin sealant versus conventional suturing using 3–0 black silk Group A (n = 30): fibrin sealant Group B (n = 30): primary closure by suturing Using a split‐mouth study design, wound closure following extraction was done using fibrin sealant on the study side and primary closure suturing on the control side. Procedure was carried out under local anaesthetic. |
|
| Outcomes | Primary outcome measures were (1) the time taken to achieve wound closure and haemostasis and (2) postoperative mouth opening, pain, and swelling. | |
| Notes | As this was a split‐mouth study, the paired t‐test was used to compare the mean values between the control and experimental groups. The paired t‐test was also applied for comparisons between time points. The level of significance was fixed as a = 0.05 (2‐ tailed). IBM SPSS Statistics for Windows, version 20.0 (IBM Corp, Armonk, NY, USA) was used for the data analysis. Sample size calculation: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The patient pool was sequentially numbered 1–30. Lots were drawn, one for each patient, from sealed envelopes that contained combinations of the agent (fibrin sealant/suturing) and the side to be operated (right/left)" Comment: sequentially numbered, sealed envelopes were used |
| Allocation concealment (selection bias) | Low risk | Comment: sealed envelopes were used |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: it is unclear if participants were blinded to the procedure. This is not stated specifically; it is possible the participant would be aware of the presence (or absence) of sutures in mouth. |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Comment: unclear if the assessor was different to the operating surgeon |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "no patients discontinued the trial or were lost to follow‐up" Comment: all participants were analysed |
| Selective reporting (reporting bias) | Low risk | All planned outcomes were reported. |
| Other bias | Unclear risk | This was a cross‐over trial. The order of the receiving of treatments was randomised. There is potential bias from a carry‐over effect; carry‐over effect was not evaluated. |
Goldsmith 2012.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: University of Otago, New Zealand |
|
| Participants | Inclusion criteria: patients aged 16 to 40, American Society of Anesthesiologists Physical Status classification I or II, with bilateral symmetrically impacted partially erupted mandibular third molars, no associated pathology, no medical conditions that might alter wound healing potential Exclusion criteria: history of abuse of midazolam, allergy to any of the medications to be used, pregnancy, present or previous radiotherapy to third molar region of lower jaw, long‐term steroid or bisphosphonate use, bone disorder or fibrous dysplasia Number randomised: 57 Number evaluated: 52 (42 for pain outcome) |
|
| Interventions | Envelope flap versus pedicle flap Group A (n = 52 teeth): incision placed in the buccal gingival sulcus from the mesio‐buccal line angle of the first molar to the most distal visible aspect of the third molar. The relieving incision then extended up the external oblique ridge. Group B (n = 52 teeth): pedicle flap design involved the same initial incision, in the buccal gingival sulcus, but distil to the third molar the incision was extended approximately 1 cm and then curved towards the buccal sulcus allowing for rotation of the flap and primary closure over sound bone Follow‐up: 7 days 3 weeks between procedures. All procedures were carried out by the same surgeon under sedation with midazolam and local anaesthetic. All participants received standard pain relief medication regimen (ibuprofen/paracetamol plus codeine phosphate if required) and 0.2% CHX mouth rinse to be used 3 times daily for 5 days. |
|
| Outcomes | Alveolar osteitis, wound infection, pain, swelling, trismus, wound dehiscence on days 2 and 7 (envelope flap only) | |
| Notes | Sample size calculation: stated that sample size was determined by a power calculation using previously collected data Funding: New Zealand Dental Research Foundation and University of Otago Fuller Scholarship E‐mail from authors 22 August 2013 provided additional information. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomly allocated into one of two groups using the Logan envelope technique.... In one group the first procedure was carried out using the envelope flap design... both flap designs were randomly allocated to left or right side of each participants lower jaw again using Logan envelope technique" E‐mail from author: "...a larger envelope contained smaller pieces of paper that had the type of flap to be assigned to a patient, on the day of the procedure the surgeon's assistant would 'blindly' pick out a piece of paper and the surgeon would then use that type of flap. The same was done for assigning which side of the mouth would be operated on" |
| Allocation concealment (selection bias) | Low risk | Allocation concealed from operator. |
| Blinding (performance bias and detection bias) patient | Low risk | E‐mail from author: "Patients were not aware of what type of flap they received nor were the clinicians who did the follow‐up clinical outcomes" |
| Blinding (performance bias and detection bias) assessor | Low risk | E‐mail from author: "Patients were not aware of what type of flap they received nor were the clinicians who did the follow up clinical outcomes" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 10 participants excluded from pain evaluation due to missing data, but unlikely to result in bias in split‐mouth study. |
| Selective reporting (reporting bias) | Unclear risk | Trismus outcome data not reported. |
| Other bias | Low risk | No other sources of bias identified. |
Gomes 2005.
| Study characteristics | ||
| Methods | Study design: RCT (split‐mouth) Conducted in: Department of Oral and Maxillofacial Surgery, University of Pernambuco, Camaragibe, Brazil |
|
| Participants | Inclusion criteria: patients with bilateral mandibular impacted third molars, and all procedures had to be performed by the same operator Exclusion criteria: patients with medical problems that could contraindicate the procedure were excluded, as were any procedures in which complete fractures of the lingual cortex were likely Age: not stated Number randomised: 55 Number evaluated: 55 |
|
| Interventions | Lingual nerve protection (Free's retractor) versus none Group A (n = 55 teeth): lingual flap with Free's retractor Group B (n = 55 teeth): without lingual flap Procedures under local anaesthesia or general anaesthesia with local anaesthesia. 1 surgeon Follow‐up: 3 months |
|
| Outcomes | Pin‐prick test to confirm nerve injury at 1 and 7 days postoperatively | |
| Notes | Sample size calculation: not reported The authors note in the discussion that the lingual bone plate was preserved in all cases, and that this was responsible for a higher degree of difficulty during the procedure, "especially in deeper impactions". This may affect the homogeneity of the study. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...all patients were randomly allotted" Comment: method of sequence generation not reported |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Unclear risk | Blinding not mentioned. Participants who underwent general anaesthetic are likely to have been unaware of the procedure they received, but those with only local anaesthetic may have been aware of the procedure used. |
| Blinding (performance bias and detection bias) assessor | Low risk | Assessor was blinded. Quote: "An oral and maxillofacial surgeon who knew the proposal of the study but did not know which side was an experimental or a control group performed this evaluation" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdrawals |
| Selective reporting (reporting bias) | Unclear risk | Single outcome of nerve injury reported. |
| Other bias | Unclear risk | The authors note in the discussion that the lingual bone plate was preserved in all cases, and that this was responsible for a higher degree of difficulty during the procedure, "especially in deeper impactions". |
Greenwood 1994.
| Study characteristics | ||
| Methods | Study design: RCT (split‐mouth) Conducted in: Department of Oral and Maxillofacial Surgery, The University of Manchester, UK |
|
| Participants | Inclusion criteria: "150 patients undergoing third molar removal under general anaesthesia were entered into the study. Cases were selected so that the left and right sides were close to identical for tooth position and degree of difficulty" Exclusion criteria: none described Age: not stated Number randomised: 150 Number evaluated: 150 |
|
| Interventions | Howarth's elevator versus broad retractor for lingual nerve protection Group A (n = 150): lingual flap retraction with Howarth's elevator Group B (n = 150): lingual flap retraction using broad retractor All procedures performed under general anaesthesia, all required bone removal with either drill or chisel. Operators had varying experience, from house officers to consultant. Both extractions for each participant were completed by the same operator. Follow‐up: 1 month |
|
| Outcomes | Verbal self‐assessment of lingual nerve function, immediately and at 10 and 30 days postoperatively | |
| Notes | Sample size calculation: not reported E‐mail sent 15 January 2003, and reply received 20 January 2003 with unpublished data. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Left and right sides were then allocated at random..." Comment: we contacted the author who provided the following further information: "the randomisation code was computer generated" |
| Allocation concealment (selection bias) | Low risk | In the same letter, the author notes that "the allocation was concealed until surgery". |
| Blinding (performance bias and detection bias) patient | Low risk | All procedures were performed under general anaesthetic, so it can be assumed that the participants were blinded as to which side received the broader retractor; however, this is not specified in the paper. |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "...the nurse and surgeon assessors were blinded" (from private correspondence) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdrawals |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported on. |
| Other bias | High risk | The method of bone removal was not standardised: "the tooth was then removed employing either drill or chisel for bone removal, according to the operator's personal preference". Bone removal technique may possibly have confounded the results, and it was not recorded how many in each group had bone removal by each technique. Howarth's elevator was used to raise the initial flap for both sides, and then the broad retractor was introduced to 1 side. |
Gulsen 2017.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: Turkey |
|
| Participants | Inclusion criteria: fit study requirements including follow‐ups and informed consent; healthy without significant medical diseases or a history of bleeding problems; symmetrical impacted third molars with same level of surgical difficulty, requiring the same surgical technique to be performed; third molars in Class I, Level B position (according to Pell and Gregory) and in vertical positions according to Winter. Exclusion criteria: pregnant and lactating women; signs of pericoronitis; chronic use of medications such as antihistamines, non‐steroidal anti‐inflammatory drugs, steroids, and antidepressants, which would complicate the evaluation of their postoperative response. Age: between 17 to 27 years Number randomised: 30 participants/60 teeth |
|
| Interventions | PRF versus none Intervention group (n = 30): on the intervention side, the socket was filled with 3 pieces of PRF membrane, and the flap was primarily closed with 3–0 silk sutures Control group (n = 30): none |
|
| Outcomes | Facial swelling was determined by measuring distances from gonion ‐ commissura labiorum, tragus – commissura labiorum and tragus – lateral canthus. Pain evaluated with a VAS, with endpoints of 0 (no pain) to 100 (worst pain). |
|
| Notes | Infection was noted in 3 participants who did not have PRF. Sample size calculation: not reported Infection was not stated as an intended outcome, but was reported (infection not defined in the paper). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "study sides and control sides randomly selected" Comment: method of randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: concealment methods not described. It is not mentioned how the side of the intervention was selected and whether it was concealed or not. |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: participants were informed of the nature of the surgical and experimental procedures. The side in which the PRF was inserted into may have been known to the participant, but this is unclear. |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Quote: "For standardization all measurements were performed by the same surgeon (UG)." Comment: measurements were all done by the same surgeon (UG), but it is not described if "UG" was also the operating surgeon |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts reported. |
| Selective reporting (reporting bias) | Low risk | All planned outcomes were reported, and infection incidence was also reported, although not as a primary outcome variable. |
| Other bias | High risk | Quote: "Bilateral removal of the third molar was performed in a single appointment. For the study side, the sockets were filled with PRF, whereas for the control side, the sockets were left empty." Comment: in this split‐mouth study, both procedures were carried out at the same time. This may have affected the participant perception of pain. |
Haraji 2010.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: Iran Number of centres: 1 Recruitment period: not stated |
|
| Participants | Inclusion criteria: patients with bilaterally impacted third molars with similar difficulty index Exclusion criteria: pre‐existing medical conditions, oral contraceptive use, systemic or neurological conditions, pregnancy, pericoronitis or pathological conditions associated with third molars Age: mean 19.94 ± 1.5 years Number randomised: 17 Number evaluated: unclear |
|
| Interventions | Buccal envelope versus modified triangular flap Group A (n = 17): buccal envelope flap Group B (n = 17): modified triangular flap All participants received local anaesthetic, oral cefalexin 500 mg 6 hourly for 5 days, and 500 mg acetaminophen codeine postoperatively. |
|
| Outcomes | Alveolar osteitis and "healing scores" | |
| Notes | Sample size calculation: not reported E‐mail sent to Dr.a.Haraji@Dentaliau.ir on 12 March 2012 requesting further information. No reply received. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "allocated randomly" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Low risk | Double‐blinded |
| Blinding (performance bias and detection bias) assessor | Low risk | Double‐blinded. Paper does not state who conducted outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Outcomes reported as percentage only with no indication of how many participants were evaluated. |
| Selective reporting (reporting bias) | High risk | Alveolar osteitis reported as percentage in each group and P value, no indication if paired data taken into account in analysis. Suggestion that a number of participants had bilateral osteitis. Pain and healing not reported. |
| Other bias | Unclear risk | 41.7% control group rate of alveolar osteitis is very high, and it seems unlikely that a different flap design would have been solely responsible for the lower rate in the intervention group. Co‐intervention or aseptic conditions for surgery |
Hashemi 2012.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: Tehran, Iran Number of centres: 1 (Tehran University Hospital) Recruitment period: September 2008 to January 2010 |
|
| Participants | Inclusion criteria: bilateral bony mandibular third molars that were fairly similar in terms of angulation, degree of impaction, and estimated difficulty of removal Exclusion criteria: presence of any medical problem that would contraindicate extraction, pathological lesion near teeth to be extracted Number randomised: 30 Number evaluated: 30 |
|
| Interventions | No sutures versus multiple sutures for wound closure Group A (n = 30 teeth) Group B (n = 30 teeth) Follow‐up: 7 days All procedures were carried out by a single surgeon under local anaesthetic. |
|
| Outcomes | Pain (0‐to‐5 VAS) and swelling on days 1, 3, and 7 | |
| Notes | Sample size calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...one of the two impacted mandibular third molars in each patient was randomly allocated" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | No mention of who conducted the randomisation and whether it was concealed from the surgeon. |
| Blinding (performance bias and detection bias) patient | Unclear risk | Not possible |
| Blinding (performance bias and detection bias) assessor | High risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | It appears that all the randomised participants were included in the outcome valuation. |
| Selective reporting (reporting bias) | High risk | Planned outcomes reported, but it is unclear if paired nature of data was taken into account. |
| Other bias | Low risk | No other sources of bias identified. |
Kapse 2019.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: India |
|
| Participants | Inclusion criteria: patients with normal haematologic profiles, no systemic illness, good oral hygiene, and surgical site free of active infection Exclusion criteria: use of tobacco or alcohol during the study period and unwillingness to attend the long‐term follow‐up programme Age: 18 to 40 years Number randomised: 30 participants/60 sites Number evaluated: 30 participants/60 sites |
|
| Interventions | Platelet‐rich fibrin in extraction socket versus none Group A: test group (n = 30 site) PRF placed in the extraction socket Group B: control (n = 30 site) The time interval between extractions of M3 in a participant was 30 days. All procedures were performed under local anaesthesia, braided, black silk suture was used. |
|
| Outcomes | Pain (0‐to‐10 VAS), swelling, and bone healing (radiographical assessment) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: participants were randomly assigned numbers and were categorised into groups |
| Allocation concealment (selection bias) | Unclear risk | Comment: method of concealment of the allocations was not clearly stated |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: it is not explicitly stated |
| Blinding (performance bias and detection bias) assessor | Low risk | Comment: all of the evaluations were carried out by investigators other than the operating surgeon |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no dropouts |
| Selective reporting (reporting bias) | Low risk | All planned outcomes were reported. |
| Other bias | Low risk | No other sources of bias identified. |
Kirk 2007.
| Study characteristics | ||
| Methods | Study design: RCT (split‐mouth) Conducted in: New Zealand Defence Force, Taranaki Base Hospital |
|
| Participants | Inclusion criteria: patients with bilateral, symmetrically impacted lower wisdom teeth Exclusion criteria: patients were excluded if they had a pre‐existing medical condition, or were taking medication that would influence the ability to undergo surgery or alter wound healing. Patients were also excluded if they had any discernible active pathology associated with the third molars, or if the impactions were such that surgical time and trauma would be excessive and mask the possible influence of flap design. Age: mean 24.2 years Number randomised: 35 Number evaluated: 32 |
|
| Interventions | Modified triangular flap versus envelope flap Group A (n = 32): modified triangular flap (on randomly selected side of mouth) Group B (n = 32): envelope flap (on the other side) Both lower 8s removed at same visit, and all procedures performed under intravenous sedation by same surgical operator and dental assistant. Follow‐up: days 2 and 7 |
|
| Outcomes | Pain (0‐to‐10 VAS), alveolar osteitis, infection, trismus, swelling (measured by evaluation of laser scans of the participants' cheeks) | |
| Notes | Sample size calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...the flap design and side of mouth were randomly assigned for each patient" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Unclear risk | It is likely that participants were unaware of which flap they received, but blinding was not specified. |
| Blinding (performance bias and detection bias) assessor | High risk | Not mentioned whether or not assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3 withdrawals, 1 prior to first surgery and 2 before the second surgery. These later two were excluded from the outcome data, but they are unlikely to have introduced bias. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported on. |
| Other bias | Low risk | No other sources of bias identified. |
Koyuncu 2013.
| Study characteristics | ||
| Methods | Study design: a randomised single‐blind clinical trial, parallel Conducted in: Turkey |
|
| Participants | Inclusion criteria: patients with no history of medical illness or medication that could influence the course of postoperative wound healing or alter their wound healing after surgery were selected Exclusion criteria: patients were excluded from randomisation if they had a pre‐existing abscess or cellulitis, acute pericoronitis, or pre‐existing conditions associated with their third molars. Those who required antibiotics for some other reason (such as prophylaxis for endocarditis) were also excluded, as were those who had been given radiotherapy. Immunocompromised patients, pregnant women, those already taking antimicrobials, and those with systemic diseases, such as diabetes, cancer, or renal failure, were excluded. Age: 18 to 29 Number randomised: 80 Number evaluated: 80 |
|
| Interventions | Envelope flap type versus modified triangular flap type Group A (40 participants): envelope flap type Group B (40 participants): modified triangular flap type All operations were done under local anaesthesia (inferior alveolar block, 2 mL 2% lidocaine with 1:80,000 epinephrine). A primary wound closure was carried out in all cases. All participants were given amoxicillin (500 mg/8 h) for 7 days and diclofenac potassium (50 mg/12 h) for pain after surgery. Postoperative instructions for the participants included soft diet and oral hygiene with 0.2% chlorhexidine mouth rinse. Sutures were removed 7 days after surgery. | |
| Outcomes | Primary outcome: any postoperative complication; alveolar osteitis classified as present or absent Secondary outcomes: postoperative side effects (including pain, swelling, and trismus assessed during the postoperative time periods)
|
|
| Notes | This study was mentioned in the previous review update, but was not published at that time. Sample size calculation: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "investigators designed and implemented a randomized single‐blind clinical trial. The flap design was randomly assigned for each patient" Comment: unclear how the participants were recruited and randomised |
| Allocation concealment (selection bias) | Unclear risk | Comment: concealment approaches were not described |
| Blinding (performance bias and detection bias) patient | Low risk | Comment: unclear as it was not described. However, it is unlikely that the participant would have known which flap they had unless they were explicitly told. |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "The surgeon that had operated on the patients was never involved in the preoperative or postoperative assessment" Comment: assessor blinding was appropriate |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: outcomes were reported for all participants (n = 80). 100 participants were initially recruited; the reason for the final number (80) was explained appropriately (they did not meet the inclusion criteria). |
| Selective reporting (reporting bias) | Low risk | All intended outcomes were reported. |
| Other bias | Low risk | No other sources of bias identified. |
Koyuncu 2015.
| Study characteristics | ||
| Methods | Study design: prospective RCT, single‐blind, parallel Conducted in: Turkey |
|
| Participants | Inclusion criteria: bilateral vertically symmetrical impacted third molars on panoramic radiographs. All impacted mandibular third molars had to be in a comparable position bilaterally and carry the same degree of surgical difficulty requiring the same technique. All teeth were fully covered by mucosa and bone. All participants were non‐smokers, periodontally healthy, and well‐educated about their daily oral hygiene. Exclusion criteria: history of medical illness or medication that could influence the course of postoperative wound healing or alter wound healing after extraction. Also excluded were patients who had any pathological lesion in the area of the impacted third molar. The periods between the incision and insertion of the last suture were recorded, and if the operating time differed by more than 5 minutes between the 2 sides, the patient was withdrawn from the study. Age: 18 to 29 years Number randomised: 40 Number evaluated: 40 |
|
| Interventions | Effect of tube drainage versus conventional suturing on postoperative discomfort after extraction Group experimental: a tube drain (n = 40 teeth): an infant feeding tube 3 cm long and 2.67 mm in diameter (8 Ch) (Bıc¸akcılar, Istanbul, Turkey) was inserted in the buccal incision line between the first and second molar. The tube drain was sutured to the vestibular mucosa to prevent it from coming out or becoming lost in the wound. Group B control: no drain (n = 40): a 3‐cornered mucoperiosteal flap was raised to expose the third molar. Bone was removed under constant irrigation with sterile 0.9% saline on the occlusal and buccal aspect of the third molar with rotating instruments of diminishing size. After extraction, potential nests of the dental follicle were removed. Primary wound closure with atraumatic silk sutures without tension (Medico Co. Ltd, China) was used on the side that had no drain. |
|
| Outcomes | Pain (VAS) from zero (no pain) to 10 (worst pain imaginable) daily for 7 days Degree of swelling (mm) at days 2 and 7 Maximum mouth opening at days 2 and 7 A quality of life questionnaire was used; all participants returned the questionnaires on day 7 |
|
| Notes | Sample size calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "groups by random selection in a cross‐over pattern. The trial was randomised, prospective, and single‐blind." Comment: method of randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: concealment methods not described |
| Blinding (performance bias and detection bias) patient | High risk | Comment: "a single blinded study". It is unlikely that participants could be blinded with this study design. |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "The surgeon who had operated on the patients was not involved in either the preoperative or the postoperative assessment" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcomes reported for all participants. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Unclear risk | Carry‐over effect not evaluated. |
Kumar 2015.
| Study characteristics | ||
| Methods | Study design: parallel RCT Conducted in: India |
|
| Participants | Inclusion criteria: healthy patients 19 to 35 years old, mesioangular or horizontal mandibular third molar impaction, and a preoperative platelet count higher than 150,000/mm3 Exclusion criteria: patients in whom the second molar was missing or was indicated for extraction, patients with any underlying systemic disease or compromised immunity, and pregnant or lactating women Age: mean 26.1 years Number randomised: 31 Number evaluated: 31 |
|
| Interventions | Only primary closure versus PRF placed in the socket followed by primary closure Group A intervention (n = 16): the impacted mandibular third molar was surgically removed, and 5 mL of venous blood was drawn and centrifuged at 3000 rpm for 10 minutes to prepare the PRF, which was placed into the extraction socket followed by flap approximation Group B control (n = 15): treated with surgical removal of the impacted mandibular third molar and flap re approximation |
|
| Outcomes | Follow‐up at first day and at 1 and 3 months Clinical evaluations:
Radiographic evaluations: IOPAs and OPGs at 1 and 3 months postoperatively |
|
| Notes | The student t‐test was used to determine a statistical difference between groups in the parameters measured. Proportions were compared by c2 test with Yates correction. Sample size calculation: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomised by the closed‐envelope method and divided into 2 groups" Comment: randomised by closed envelopes |
| Allocation concealment (selection bias) | Low risk | Quote: "patients were randomised by the closed‐envelope method and divided into 2 groups." Comment: concealed envelopes used |
| Blinding (performance bias and detection bias) patient | High risk | Quote: "in the case group, after the tooth was delivered, 5 mL of venous blood was drawn and centrifuged at 3,000 rpm for 10 minutes and PRF was obtained" Comment: the control group did not have blood taken, therefore there is a high chance they would know what group they were in |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdrawals |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported. |
| Other bias | Low risk | No other sources of bias identified. |
Kumar 2016.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: India |
|
| Participants | Inclusion criteria: systemically healthy people between 18 to 50 years with bilaterally completely impacted mandibular third molars indicated for surgical removal Exclusion criteria: medical conditions that can complicate surgical extraction, obesity (body mass index ≥ 30 kg/m2), current smokers, pregnant or lactating females, those taking oral contraceptive drugs, and those under any antibiotic coverage Age: 18 to 50 years Participants: 30 participants/60 teeth |
|
| Interventions | Tube drainage versus no tube Control group (n = 30): primary closure was accomplished using 3‐0 silk suture Experimental group (n = 30): tube drain was sutured by a circumferential suture tethered with the buccal flap through the releasing incision |
|
| Outcomes | Pain scale: no pain‐slight pain‐mild‐severe‐very severe Swelling: mean of horizontal and vertical measurements Maximum interincisal opening in millimetres |
|
| Notes | Sample size calculation: reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "left and right mandibular quadrants of each individual were randomly allocated by means of a tossing coin into two groups, test (with tube drain, n=30) and control (without tube drain, n=30)" Comment: a coin‐tossing technique was used |
| Allocation concealment (selection bias) | Unclear risk | Comment: no concealment methods described |
| Blinding (performance bias and detection bias) patient | Unclear risk | Quote: "The eligible individuals were informed of the nature, possible risks, and benefits of their participation in the study and a written informed consent was obtained from each participant." Comment: it is unclear how much detail was given to participants, but it is likely that they would know which side a tube drain was placed as it was in situ for 3 days |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Comment: blinding of the assessor not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no dropouts mentioned |
| Selective reporting (reporting bias) | Low risk | Comment: planned outcomes reported |
| Other bias | Unclear risk | Quote: "Following the complete resolution of post‐operative sequelae the second surgical procedure of other side with tube drain was carried out in the same patient." Comment: wash‐out period not specified. Any potential carry‐over effect was not analysed. |
Leung 2009.
| Study characteristics | ||
| Methods | Study design: RCT (parallel group) Conducted in: Discipline of Oral and Maxillofacial Surgery, Faculty of Dentistry, The University of Hong Kong, China |
|
| Participants | Inclusion criteria: the wisdom tooth root touched or overlapped with the superior cortical line of the IDN on radiographs. Radiographic signs were used to assess a close relationship with the nerve. Exclusion criteria: wisdom tooth roots did not touch the IDN cortical lines, or if wisdom teeth were associated with apical pathology or cystic or neoplastic lesions. Patients were also excluded if they had any of the following:
Number randomised: 231 Number evaluated: 231 |
|
| Interventions | Coronectomy versus complete tooth removal Group A (n = 171 teeth): underwent coronectomy Group B (n = 178 teeth): underwent conventional extraction Failed coronectomy (n = 16 teeth) Surgical residents undertook treatment under general anaesthesia in 50.3% of test participants and 48.3% of participants in the control group, intravenous sedation with local anaesthesia in 3.5% of test participants and 5.6% in the control group. Local anaesthesia was used in 46.2% of the test participants and 46.1% of the control participants. Follow‐up: postoperatively, assessed at 1 week and at 1, 3, 6, 12, and 24 months. Mean length of follow‐up for all groups was 10.6 months. |
|
| Outcomes | Primary outcome: presence of IDN deficit 1 week postoperatively Secondary outcomes:
|
|
| Notes | Sample size calculation: based on assuming the incidence of IDN deficit in the control group (conventional extraction) and the study group (coronectomy) would be 5% and 0%, respectively. If these assumptions were correct, 152 participants per group would be sufficient to detect a statistical difference, with a 2‐sided type 1 error of 5% and a power of 80%. Baseline comparability: "There were no statistical differences between the 2 groups in terms of age and sex of the patients; eruption status, pattern and depth of impaction, and root shape of the wisdom teeth; the type of anaesthesia used; or the presence and type of radiographic signs" Any other issues: withdrawals clearly stated There was a unit of analysis problem, as participants were randomised, but data are presented at the tooth level. There were 231 participants and 349 teeth. This means the confidence intervals will be narrower than they should be as the teeth are clustered within participants. E‐mail sent to author (30 September 2011). Unpublished data supplied. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A house officer not participating in the study generated a randomisation table using a computer program. Patients were assigned to the 1 or 2 groups according to the randomisation table" |
| Allocation concealment (selection bias) | Low risk | The allocation sequence was kept by an assigned nurse and concealed from both the operator and participant until the participant was assigned. |
| Blinding (performance bias and detection bias) patient | Low risk | Comment: all procedures performed under general anaesthetic, and participants will look similar after operation regardless of intervention. Participants unlikely to be aware of which procedure was performed, but only coronectomy group received orthopantomograms at 1 week. |
| Blinding (performance bias and detection bias) assessor | High risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 16/171 wisdom teeth considered as failed coronectomy were excluded from analysis reported in the paper. However, data on these participants were supplied by the authors. |
| Selective reporting (reporting bias) | High risk | Outcomes: neurosensory deficit, infection rate, pain, and root migration planned and reported, but not by randomised person |
| Other bias | Unclear risk | 231 participants contributed 349 teeth to the study. It seems that the analysis did not take account of this. |
Mantovani 2014.
| Study characteristics | ||
| Methods | Study design: RCT, split‐mouth design Conducted in: Italy |
|
| Participants | Inclusion criteria: the third molar in question had to be Class A or B and in position 1, 2, or 3 according to the radiographic classification of Pell and Gregory, 18 based on the spatial relations of the tooth to the ascending ramus of the mandible and to the occlusal plane; the bilateral molars had to be in the same angulation (horizontal, mesioangular, or vertical); the indication for surgery was based on a diagnosis of pericoronitis Exclusion criteria: a clinically significant medical history (e.g. systemic infective disease, cardiovascular disease, liver disease, haematologic disease, bleeding tendency, diabetes, or neoplastic disease), recent anti‐inflammatory treatment, regular use of medications with possible anti‐inflammatory activity (e.g. antihistamines, non‐steroidal anti‐inflammatory drugs, corticosteroids, and antidepressants), women who were pregnant or breastfeeding, current heavy tobacco smokers (> 10 cigarettes daily), patients undergoing orthodontic therapy, and patients unwilling to undergo the data collection procedures Age: mean 24.02 years Number randomised: 125 Number evaluated: 100 (bilateral extraction) |
|
| Interventions | Piezoelectric (ultrasound) device versus traditional surgery using burs Group A (n = 125): included all operations carried out with the bur Group B (n = 125): surgeries carried out with the piezoelectric technique |
|
| Outcomes | The primary outcomes reported were postoperative pain, objective orofacial swelling, and surgical duration; secondary outcomes were gender, age, radiologic position, and possible adverse events (e.g. paraesthesia or infection). Participants were given a questionnaire about their subjective experience of the 2 different surgeries regarding the presence of vibrations and noise, which intervention was more comfortable, if further dental surgery was necessary, and which one they would prefer. Participants also were asked to describe their pain in detail; the symptoms score was obtained using a VAS. The VAS consisted of a 100‐millimetre horizontal line marked from 0 (no pain) to 100 (most severe pain ever experienced). Participants were asked to mark the scale, late in the evening, daily for 6 days after surgery. Clinical assessments were performed at 2, 7, 14, and 28 days after the surgery. Facial measurements were collected at baseline preoperatively and on day 7 after suture removal to evaluate any swelling. |
|
| Notes | Sample size calculation: reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote; "randomization was performed with a table of random numbers" Comment: random number table used |
| Allocation concealment (selection bias) | Low risk | Quote: "by a researcher not involved in the study and who was blinded to the type of procedure" Comment: concealment methods were put in place. Randomisation was done by an independent researcher who was blinded to the type of procedure. |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: not mentioned, but it is possible the participant was aware of the technique used on each side based on noise levels |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "Postsurgical clinical assessments were performed by a single blinded examiner" Comment: the assessor was blinded to the allocation of sides |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "The study sample was derived from 140 patients. Fifteen of these patients did not show periodontal parameters lower than 20% and thus were excluded; 14 patients underwent only 1 intervention and 11 patients did not attend all follow‐up visits. Thus, the final study sample consisted of 100 patients." Comment: the dropouts from the originally recruited 140 participants have been described and justified |
| Selective reporting (reporting bias) | Low risk | Planned outcomes were reported. |
| Other bias | Low risk | No other sources of bias were identified. |
Mistry 2016.
| Study characteristics | ||
| Methods | Study design: RCT, split‐mouth Conducted in: India |
|
| Participants | Inclusion criteria: only those patients having same angulation, same depth from the occlusal surface of the adjacent second molar, and the same ramus relation, i.e. same difficulty index bilaterally as described by Pederson, in whom bony osteotomy was necessary were selected for the study Exclusion criteria: patients having pericoronitis, acute alveolar abscess, oral submucous fibrosis, on antibiotics for any infection, who consumed alcohol or who smoked tobacco and were not willing to give consent for the study were excluded. 30 cases in total were selected for the study. Age: > 18 Number randomised: 30 participants/60 teeth |
|
| Interventions | Piezosurgery versus conventional Group 1 (n = 30): conventional Group 2 (n = 30): piezosurgery |
|
| Outcomes | Pain VAS (0 to 10) Trismus: measured as the distance between the mesial incisal corner of the right upper and lower central incisors with the help of metallic scale. Measurements were recorded in millimetre unit and were noted preoperatively, postoperatively immediately after the surgical procedure, and then on postoperative days 1, 3, 5, 7, and 15 in both groups. Swelling: distances between extra oral and intra oral by the use divider |
|
| Notes | Sample size calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: authors state the grouping was done randomly, however the method of randomisation is not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: concealment methods are not described |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: consent was given by the participant, but it is unclear whether they were informed of the equipment details, etc. |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Comment: blinding of the assessor is not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no dropouts were reported |
| Selective reporting (reporting bias) | Low risk | Comment: all planned outcomes were reported |
| Other bias | High risk | Comment: carry‐over effect was not analysed. The grouping of participants was reported to be randomised (piezo vs conventional technique), however the side that was chosen for the test/control was not described as randomised. |
Mobilio 2017.
| Study characteristics | ||
| Methods | Study design: a randomised prospective study; parallel groups Conducted in: Italy |
|
| Participants | Inclusion criteria: 25 medication‐free, otherwise healthy consecutive patients (18 women and 7 men; mean age: 27.88 ± 9.75 years, age range: 18 to 61 years) scheduled for lower third molar extraction on an ambulatory basis were included in the study Exclusion criteria: age < 18, diagnosed psychiatric disorders, diagnosed neurological diseases, diagnosed impaired communicative or cognitive abilities, contraindications to non‐steroidal anti‐inflammatory drugs or amoxicillin Age: 18 to 61 Number randomised: 25 participants/25 teeth |
|
| Interventions | Comparison: envelope flap versus triangular flap Group A (n = 13): envelope flap Group B (n = 12): triangular flap Mepivacaine (2%) containing 1:100,000 adrenaline was administered as the inferior alveolar, buccal and lingual nerve block. Standard analgesics were prescribed (ketoprofen 80 mg: first dose after 2 hours, second after 8 hours, then 3 times a day for days 2 and 3); 0.12% chlorhexidine mouth rinse was prescribed from day 2 until day 7. A postoperative meeting was scheduled on days 2 and 7 to check swelling and trismus. The sutures were removed during the second appointment. | |
| Outcomes | Pain: 0‐to‐100‐millimetre VAS at day 7 Swelling: 5 distances (in millimetres) through 6 facial points (angle of the mandible to tragus, to eye outer canthus, to labial commissure, to nasal border, and to soft pogonion) were measured, and then the average percentage value was obtained. Trismus (millimetres): to assess trismus (represented by maximum intercisal opening (MIO) reduction), the distance between the incisal edges of the upper and lower central incisors was measured in millimetres 3 times each day. The differences between initial MIO and 2‐day MIO and initial MIO and 7‐day MIO were assumed as trismus on days 2 and 7, respectively. |
|
| Notes | P < 0.05 Sample size calculation: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomly assigned to two groups in terms of flap design: group A (envelope flap) and group B (triangular flap)" Comment: the method of randomisation is not described. |
| Allocation concealment (selection bias) | Unclear risk | Comment: methods of concealment were not described |
| Blinding (performance bias and detection bias) patient | Unclear risk | Quote: "Each patient provided a written informed consent for participation." Comment: participants were consented for the procedure, but it is unclear if the details of the study were revealed to them |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "Swelling and trismus were assessed by the third examiner before and after surgery, on days 0, 2 and 7." Comment: the role of the third examiner is not well described here, but it is indicated that the third examiner was not involved in the randomisation or surgical procedure |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no dropouts were mentioned |
| Selective reporting (reporting bias) | Low risk | Comment: all outcomes are reported |
| Other bias | Unclear risk | Selective reporting (reporting bias) |
Mocan 1996.
| Study characteristics | ||
| Methods | Study design: RCT (parallel) Conducted in: Department of Oral and Maxillofacial Surgery, University of Ankara, Turkey |
|
| Participants | Inclusion criteria: patients with third molars requiring extraction. A criterion for inclusion in the study was that the third molars should be either partially or fully covered by bone, and only unilateral cases were included. Exclusion criteria: patients with complicating systemic disorders were accepted (ASA I and II) Age: mean 21.5 years Number randomised: 20 Number evaluated: 20 |
|
| Interventions | Chisel versus bur for bone removal Group A (n = 10): lingual split with chisel for bone removal Group B (n = 10): buccal approach with bur for bone removal All procedures performed under local anaesthesia. Follow‐up: day 7 |
|
| Outcomes | Analytical stereometric photogrammetrical assessment of swelling, calliper measure of mouth opening, and VAS (0 to 10) self‐assessment of postoperative pain | |
| Notes | Sample size calculation: not reported Baseline comparability: the lingual split group had 4 mesioangular impactions, 2 distoangular impactions, and 4 vertical impactions, whereas the buccal approach group had 3 mesioangular impactions, 0 distoangular impactions, and 7 vertical impactions E‐mail correspondence in 2003; unpublished data were unavailable |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...the patients were divided randomly into groups" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Unclear risk | Participants were not blinded. |
| Blinding (performance bias and detection bias) assessor | High risk | No mention of assessor blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No withdrawals mentioned, but numbers evaluated unclear. |
| Selective reporting (reporting bias) | High risk | Quote: "...no one experienced sensory impairment of the inferior alveolar or lingual nerves" Comment: it was not mentioned at the outset that sensory assessments were being made, and no method of assessment was described. Raw data and standard deviations not reported for primary outcomes and not supplied by authors. |
| Other bias | High risk | Very small sample size, with only 10 participants in each intervention group Different distribution of impactions in the 2 intervention groups at entry Unable to include in meta‐analysis as raw data not available in the paper or after author contact |
Mohajerani 2018.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: Iran, 2016 | |
| Participants | Inclusion criteria: adult patients had indication of impacted wisdom molar removal Exclusion criteria: patients were excluded from the study if any of following conditions were observed
Age: mean 20.1 years (between 17 and 24 years) Number randomised: 31 Number evaluated: 28 |
|
| Interventions | Envelope flap versus modified triangular flap Group A (n = 28 sites): envelope flap Group B (n = 28 sites): modified triangular flap All procedures performed under local anaesthesia. All participants were given amoxicillin (500 mg/8 hours) for 7 days and codeine/paracetamol (10 mg/325 mg) every 6 hours for pain relief. |
|
| Outcomes | Alveolar osteitis; healing degree | |
| Notes | 3 participants were excluded due to poor co‐operation with follow‐up. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the method of randomisation is unspecified |
| Allocation concealment (selection bias) | Unclear risk | Comment: the method of allocation concealment is unclear |
| Blinding (performance bias and detection bias) patient | Low risk | Participants were unlikely to know the differences between procedures. |
| Blinding (performance bias and detection bias) assessor | Low risk | Comment: study is double‐blinded. The surgeon informed the examiner (evaluator) only about the area of surgery and the code of the treatment group designated to that side, and the patient and evaluator were not aware of which side had EF. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: 3 participants were excluded by the research team because of their poor co‐operation |
| Selective reporting (reporting bias) | Low risk | All planned outcomes were reported. |
| Other bias | Low risk | It seems that both surgeries were done on the same day; however, pain and trismus were not considered. |
Nageshwar 2002.
| Study characteristics | ||
| Methods | Study design: parallel‐group RCT Conducted in: India Number of centres: 1 Recruitment period: not stated |
|
| Participants | Inclusion criteria: patients scheduled to undergo surgical removal of impacted mandibular third molars Exclusion criteria: not explicit Age: mean 25.66 ± 4.45 years Number randomised: 100 Number evaluated: 100 (e‐mail from author) |
|
| Interventions | Comma incision versus modified envelope incision Group A (n = 50): new comma incision Group B (n = 50): conventional modified envelope incision All participants had local anaesthesia, conventional methods of bone removal and tooth sectioning as required. All had prescribed antibiotics and analgesics as indicated and CHX mouthwash until suture removal. |
|
| Outcomes | Pain (VAS 0 to 10), swelling, trismus (compared to baseline), and periodontal sequelae measured on days 1, 3, 7, and 14 | |
| Notes | Sample size calculation: not reported E‐mail sent 12 March 2012 requesting further information on randomisation and variance of outcome estimates. Reply with unpublished information received from Dr N Iyer 15 March 2012. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quotes: "...divided at random"; "Table a random numbers was used in sequence" (e‐mail communication) |
| Allocation concealment (selection bias) | Unclear risk | Surgeon allocated each surgical site to 1 of the 2 groups just prior to the procedure (e‐mail communication). |
| Blinding (performance bias and detection bias) patient | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "The person who assessed all the study parameters did not know which kind of incision each patient received" (e‐mail communication) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in the analysis (e‐mail communication). |
| Selective reporting (reporting bias) | Unclear risk | Planned outcomes pain swelling and trismus reported but no estimates of variance provided, so data cannot be used in meta‐analysis. Data supplied by author via e‐mail. |
| Other bias | Low risk | No other sources of bias identified. |
Osunde 2011a.
| Study characteristics | ||
| Methods | Study design: RCT parallel group Conducted in: Department of Dental and Maxillofacial Surgery, Aminu Kano Teaching Hospital, Kano, Nigeria Number of centres: 1 Recruitment period: January to December 2007 |
|
| Participants | Inclusion criteria: patients referred for extraction of impacted lower third molars Exclusion criteria: patients with a perceptible level of pain at time of surgery were excluded Number randomised: unclear Number evaluated: 50 |
|
| Interventions | Partial versus complete wound closure Group A (n = 25): a single 3‐0 silk suture for closing the socket was placed at the distal relieving incision Group B (n = 25): multiple sutures for closing the socket; the sutures were placed at the interdental papilla between the second and third molars and at the distal relieving incision All procedures performed under local anaesthetic. Both treatment groups received oral antibiotics (amoxicillin and metronidazole for 5 days), analgesics (ibuprofen for 3 days), and instructions to use a warm saline mouth rinse. |
|
| Outcomes | Participants assessed at days 1, 2, 3, 5, and 7 postoperatively to evaluate the degree of pain, swelling, and trismus. | |
| Notes | Sample size calculation: not reported E‐mail sent to otdany@yahoo.co.uk on 12 March 2012 requesting additional information on randomisation and participants. No reply received. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...randomized into two groups" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Low risk | Quote: "Double blind" |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "Double blind" Comment: outcomes were assessed by an independent evaluator who was unaware of the treatment group to which participants belonged |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear how many participants were originally randomised to treatment. Patients with perceptible pain at baseline were excluded from the study. |
| Selective reporting (reporting bias) | Unclear risk | Pain, swelling, and trismus reported but not postoperative complications. |
| Other bias | Low risk | No other sources of bias identified. |
Osunde 2012.
| Study characteristics | ||
| Methods | Study design: parallel‐group RCT Conducted in: Benin City, Nigeria Number of centres: 1 (Aminu Kano Teaching Hospital) Recruitment period: not stated |
|
| Participants | Inclusion criteria: patients aged 18 to 38 years with mesioangular, distoangular, horizontal, and vertical impactions with a difficulty index of 3‐8 according to Peterson's criteria. No symptoms of pain, facial swelling, or trismus in 10 days preceding surgery, non‐smokers, no concomitant medications or systemic diseases that could interfere with healing Exclusion criteria: pregnant or lactating females, patients with more than 1 third molar requiring treatment Number of participants randomised: 80 Number of participants evaluated: 80 |
|
| Interventions | No sutures versus multiple sutures for wound closure Group A (n = 40): no sutures Group B (n = 40): multiple sutures using 3/0 silk, placed at the interdental papilla immediately distil to the second molar, the buccal relieving incision, and the distil relieving incision Follow‐up: 7 days All procedures were carried out by the same surgeon and assistant under local anaesthetic. |
|
| Outcomes | Pain (0‐to‐10‐centimetre VAS), trismus, swelling, on days 1, 2, and 7 | |
| Notes | Sample size calculation: not reported E‐mail sent to otdany@yahoo.co.uk on 12 March 2012 requesting additional information on randomisation and participants. No reply received. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Consecutively randomised into two treatment groups" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | No mention of who conducted the random allocation and whether it was concealed from the surgeon |
| Blinding (performance bias and detection bias) patient | Unclear risk | Not possible |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "...the patients were evaluated in a blinded manner by the same independent observer" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants were included in the outcome assessment. |
| Selective reporting (reporting bias) | Low risk | Planned outcomes reported in full. |
| Other bias | Low risk | No other sources of bias identified. |
Ozgul 2015.
| Study characteristics | ||
| Methods | Study design: randomised, multicentre, split‐mouth clinical trial Conducted in: Turkey |
|
| Participants | Inclusion criteria: bilateral, fully impacted third molars that have the same degree of surgical difficulty comparing 1 side with the other; no pre‐existing medical conditions or use of medication that would influence or alter wound healing; no active pathology associated with the third molars; no temporomandibular joint disorder history that would affect pain sensation after surgery Age: 18 to 28 years Number randomised: 56 (23 male, 33 female) Number evaluated: 56 |
|
| Interventions | PRF versus none Group A (n = 56): PRF was placed in the socket Group B (n = 56): control; nothing placed in the socket |
|
| Outcomes | At 24 h, 72 h, and 7 days Evaluation of facial swelling was performed using a horizontal and vertical guide. Pain/comfort was evaluated in the postoperative period using a 0‐to‐100‐millimetre VAS. |
|
| Notes | Sample size calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A coin toss technique was used for the study. |
| Allocation concealment (selection bias) | Unclear risk | Comment: unclear if the person making the allocations was separate to the operator |
| Blinding (performance bias and detection bias) patient | Low risk | Quote: "Patients were blind to the knowledge of PRF placed side" Comment: participants were reported as being blind to the intervention |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "The postoperative evaluations were performed by surgeons that were blinded to the operative procedures, in order to eliminate unwanted bias." Comment: assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: it is not stated if outcomes were measured for all participants. No dropouts are mentioned. |
| Selective reporting (reporting bias) | Low risk | Comment: planned outcomes were reported |
| Other bias | Unclear risk | Comment: the recruitment process is unclear; patients were "selected" |
Pachipulusu 2018.
| Study characteristics | ||
| Methods | Study design: parallel‐arm RCT Conducted in: India |
|
| Participants | Inclusion criteria:
Exclusion criteria:
Age: mean 29.3 years Number randomised: 60 Number evaluated: 60 |
|
| Interventions | Primary versus secondary closure of surgical wound Group A: 30 participants in which primary closure was done after surgical extraction Group B: 30 participants in which secondary closure was done after surgical extraction Suturing was done using round bodied 3–0 black silk or polyglactin 910 (Vicryl). Postoperative instructions were given, and the same course of antibiotics (amoxicillin with clavulanic acid 625 mg 3 times a day) and analgesics (aceclofenac with paracetamol 2 times a day) for 5 days were given for participants in both groups postoperatively after extraction. |
|
| Outcomes | Pain (0‐to‐10 VAS); swelling; trismus; periodontal healing | |
| Notes | Sample calculation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the method of randomisation was not stated |
| Allocation concealment (selection bias) | Unclear risk | Comment: no mention of allocation concealment |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: although it is unlikely that participants would have known which treatment they had received, this is not explicitly stated |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Comment: it is unclear who assessed the participants postoperatively |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no dropouts |
| Selective reporting (reporting bias) | Low risk | Comment: planned outcomes were reported |
| Other bias | Unclear risk | Quote: "using round bodied 3–0 black silk or vicryl, and sutures were removed after 1 week whether it is vicryl or silk" Comment: methodology was not consistent; the same sutures should have been used in the whole of Group A |
Pasqualini 2005.
| Study characteristics | ||
| Methods | Study design: parallel‐group RCT Conducted in: Italy Number of centres: 1 Recruitment period: not stated |
|
| Participants | Inclusion criteria: totally or partially bone‐impacted mandibular third molar with mesial inclination between 25 and 30°, no systemic disease, good general health, age less than 30 years, non‐smoker, no inflammation of the oral cavity, co‐operation with the study and with postoperative follow‐up, and no contraindication to anaesthetics or study drugs Number randomised: 200 Number evaluated: 200 |
|
| Interventions | Primary versus secondary wound closure Group A (n = 100): primary wound closure; "flap repositioned and sutured hermetically" Group B (n = 100): secondary wound closure; "a sedge of mucosa 5‐6 mm was removed from second molar and flap was repositioned and sutured" All procedures performed under local anaesthesia. All participants also received antibiotics (amoxicillin 2 g/day for 5 days and nimesulide 200 mg/day for 3 days) |
|
| Outcomes | Pain and swelling on 0‐to‐4 VAS daily for 7 days | |
| Notes | Sample size calculation: not reported E‐mail sent to Dr Pasqualini (damianox@mac.com) who provided additional information on the methods of this trial 6 March 2012. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quotes: "...randomly divided"; "Randomization was performed using a computer generated random numbers sequence created by an independent research office" (e‐mail from author) |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocations were kept in sealed serially numbered opaque envelopes which were opened in sequence and showed to the surgeon at the moment of surgical closure, with at least one independent witness present (generally a nurse)" (e‐mail from author) |
| Blinding (performance bias and detection bias) patient | Low risk | The participants were not aware of the type of closure (e‐mail from author). |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Quote: "The examiner who assessed the postoperative outcome at 7 and 30 days was not aware of the allocation. However they could have presumed it by looking at the residual wound" (e‐mail from author) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in the outcome evaluation. |
| Selective reporting (reporting bias) | Low risk | Pain, swelling, and infection reported as planned. |
| Other bias | Low risk | Author confirmed that no wound dressings were used in either group. |
Piersanti 2014.
| Study characteristics | ||
| Methods | Study design: randomised clinical trial (split‐mouth, unblinded) Conducted in: Italy |
|
| Participants | Inclusion criteria: had to be 18 to 25 years of age and require removal of the impacted lower third molars with a mucoperiosteal flap and osteoplasty; these 2 teeth in the same patient had to have the same difficulty extraction score, according to the Yuasa Scale Exclusion criteria: teeth affected by acute infections, such as pericoronitis, an acute alveolar abscess, or oral submucous fibrosis at the time of surgery Age: 22.4 ± 2.3 years Number randomised: 10 (6 female, 4 male) Number evaluated: 10 (20 teeth) |
|
| Interventions | Compare the discomfort and surgical outcomes of a piezosurgery device versus rotatory instruments Group A (n = 10): piezosurgery device Group B (n = 10): rotatory instruments |
|
| Outcomes | The primary outcome was a postoperative symptom severity scale known as PoSSe (0 to 100) 1 week after surgery. The scale consists of 7 subscales that investigate the patient’s ability to enjoy food; speak properly; perceive altered sensations, appearance, pain, and sickness; and interference with daily activities. Secondary outcomes included pain (VAS 0 to 10), trismus, and swelling. These variables were evaluated at baseline and 7 days postoperatively. |
|
| Notes | Sample size calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly allocated to have the third molar removed with a conventional rotating handpiece or a piezosurgery unit" Comment: the method of randomisation is not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: concealment approaches were not described |
| Blinding (performance bias and detection bias) patient | Unclear risk | Quote: "All patients were informed about the procedures, postoperative recovery times, and possible complications and signed a detailed consent form." Comment: it is unclear if the participant knew which side was the test side and which was the control |
| Blinding (performance bias and detection bias) assessor | High risk | Comment: it is unclear who the assessor was. It is mentioned that the trial was unblinded, but no further information is given. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: all participants completed the study |
| Selective reporting (reporting bias) | Low risk | Comment: all planned outcomes were reported |
| Other bias | Unclear risk | Comment: the carry‐over effect was not evaluated |
Praveen 2007.
| Study characteristics | ||
| Methods | Study design: parallel‐group RCT Conducted in: India Number of centres: 1 Recruitment period: not stated |
|
| Participants | Inclusion criteria: healthy patients with symptomatic impacted mandibular third molars Exclusion criteria: not explicitly stated Number randomised: 90 Number evaluated: unclear |
|
| Interventions | Lingual split with chisel versus surgical bur versus simplified split bone technique Group A (n = 30): lingual split, bone removed with a 5‐millimetre mono bevelled chisel Group B (n = 30): bone removal with 702 bur at 15,000 rpm Group C (n = 30): "Simplified split bone technique" using chisel from buccal aspect "The lingual nerve was protected by a Howarth's periosteal elevator in all cases." All procedures performed under local anaesthetic. |
|
| Outcomes | Pain, swelling, and sensory disturbances recorded at 6, 24, and 48 hours and on day 7 using VAS | |
| Notes | Sample size calculation: not reported E‐mail sent to Dr Rajesh (rajeshomfs@gmail.com) seeking clarifications on 28 February 2012. No reply received. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The methods for a particular patient were selected randomly" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) assessor | High risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear how many extractions are included in the reported outcomes |
| Selective reporting (reporting bias) | Unclear risk | There appear to be omissions and errors in the reported data, where different aspects are contradictory. |
| Other bias | Low risk | No other sources of bias identified. |
Rabi 2017.
| Study characteristics | ||
| Methods | Study design: parallel‐group RCT Conducted in: India |
|
| Participants | Inclusion criteria: patients without any history of medical illness or taking any medication that could influence the surgical procedure or postoperative wound healing; non‐smokers; and patients with healthy dental and periodontal status Age: 20 to 30 years Participants: 50 Number evaluated: 50 |
|
| Interventions | Triangular versus envelope flap designs
Group 1 (n = 25): triangular flap
Group 2 (n = 25): envelope flap
Triangular flap: the incision was placed distally from the mandibular ramus to the distobuccal aspect of the second molar. This was followed by a sulcular incision that started near the mesiobuccal edge of second molar extending to its distal surface, and a relieving incision from the distobuccal aspect of the second molar, without incising the interdental papilla, at an oblique angle curving forward into the mandibular vestibule. Envelope flap: a sulcular incision was placed from the first mandibular molar to the second mandibular molar, following which a distal incision along the mandibular ramus was placed Anaesthetic: 2% lidocaine with 1:200,000 adrenaline with inferior alveolar, lingual, and long buccal nerve block administered All participants received amoxicillin 500 mg 3 times a day and diclofenac sodium 50 mg 3 times a day for 3 days postoperatively. Postoperative instructions were given, and the sutures were removed on the seventh day. |
|
| Outcomes | Pain: VAS (not continuous 0‐to‐4 scale) (no pain; slight pain; mild pain; severe pain; very severe pain) Trismus: inter incisal distance in millimetres |
|
| Notes | Results of continuous data are depicted as mean ± standard deviation (SD; min–max), and results of categorical measurements are shown as number (%). Significance was assessed at a level of significance of 5%, with 95% confidence interval. Unpaired t‐test was used for analysis of quantitative data, and Fisher's exact test was used for analysis of qualitative data. Sample size calculation: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A total of 50 participants were assessed clinically and were divided randomly into two groups, group I (participants operated by triangular flap) and group II (participants operated by envelope flap), with 25 participants each." Comment: the method of randomisation was not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: methods of concealment were not described |
| Blinding (performance bias and detection bias) patient | Low risk | Comment: not mentioned, but patient unlikely to be aware of differences |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Comment: not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: all enrolled participants were evaluated |
| Selective reporting (reporting bias) | Low risk | Comment: all planned outcomes were reported |
| Other bias | Unclear risk | Comment: no other sources of bias were identified |
Rakprasitkul 1997.
| Study characteristics | ||
| Methods | Study design: RCT (split‐mouth) Conducted in: Oral and Maxillofacial Surgery Department, Faculty of Dentistry, Mahidol University, Bangkok, Thailand |
|
| Participants | Inclusion criteria: healthy patients requiring bilaterally impacted third molars, who would co‐operate with the study and postoperative follow‐up. All teeth were fully covered by mucosa, and partially or completely covered by bone. Exclusion criteria: patients with significant medical diseases or a history of bleeding problems were excluded, as were pregnant women. In addition, patients with any sign of pericoronitis were excluded from the study. Number randomised: 23 Number evaluated: 23 |
|
| Interventions | Tube drain versus no drain Group A (n = 23): surgical drain placement for 3 days Group B (n = 23): simple primary wound closure with no surgical drain placement Surgery performed by the same surgeon on 2 occasions 2 months apart, under local anaesthetic. Follow‐up: day 7 |
|
| Outcomes | Pain (0‐to‐10 VAS), swelling (measured by distance of 2 transecting lines across cheek, and by patient grading), mouth opening (interincisal distance) | |
| Notes | Sample size calculation: not reported E‐mail sent to author (March 2003). Reply that no additional data were available |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...the patients were assigned to test and control groups by random selection" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Unclear risk | Although this is not specified, participants would have been aware of the presence of a surgical drain in their mouths. |
| Blinding (performance bias and detection bias) assessor | High risk | Quote: "...the patients were examined by the same person [surgeon] immediately preoperatively, and on the third and seventh postoperative days" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdrawals |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported on. |
| Other bias | Unclear risk | By having a 2‐month gap between the 2 extractions (1 side then the other), participants' perception of pain may be altered by that previous experience. |
Refo'a 2011.
| Study characteristics | ||
| Methods | Study design: parallel‐group RCT Conducted in: Tehran, Iran Number of centres: 1 Recruitment period: not stated |
|
| Participants | Inclusion criteria: patients aged 20 to 25 years with wholly bone‐impacted mandibular third molar with mesioangular inclination and willing to participate in study Exclusion criteria: systemic medical conditions, smoking, inflammation in the oral cavity, history of drug use Number randomised: 32 Number evaluated: unclear |
|
| Interventions | Primary versus secondary wound closure Group A (n = 16): triangular flap was raised, teeth were extracted and following saline irrigation flaps were repositioned and sutured completely using 0.5‐inch round cutting needle with 3.0 silk suture Group B (n = 16): triangular flap was raised, teeth were extracted and following saline irrigation flaps were repositioned and 5 to 6 mm of distil extension to second molars was kept open, while other parts of the flap were repositioned and sutured All surgical procedures were performed by the same surgeon under local anaesthetic. All participants received amoxicillin and ibuprofen and used CHX mouth rinse twice daily postoperatively. |
|
| Outcomes | Pain VAS (0 to 5), swelling, and trismus after 3 days | |
| Notes | No sample size calculation reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quotes: "...randomly divided into two quantitatively equal groups using a computer generated random number table…. The groups were equalised regarding gender" |
| Allocation concealment (selection bias) | Low risk | The surgeon was unaware of the type of closure until suturing. |
| Blinding (performance bias and detection bias) patient | Unclear risk | Not specifically mentioned |
| Blinding (performance bias and detection bias) assessor | High risk | Blinding of outcome assessment not mentioned. Participants self assessed pain, and it is unclear if lack of blinding would have introduced a risk of bias. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Numbers of participants included in the outcome evaluation not stated. |
| Selective reporting (reporting bias) | High risk | Pain, swelling, and trismus were planned outcomes in the methods section. Data for swelling and trismus not reported, only graph without estimates of variance and P values for difference. |
| Other bias | Low risk | No other sources of bias identified. |
Renton 2005.
| Study characteristics | ||
| Methods | Study design: RCT (parallel/split‐mouth) Conducted in: Department of Oral and Maxillofacial Surgery, Guy's Dental Hospital London, UK |
|
| Participants | Inclusion criteria: patients who required removal of third molars and were judged to be at high risk of injury to the inferior alveolar nerve based on radiographic features Exclusion criteria: patients who were predisposed to local infection, or who had systemic infections, and those with previous or existing defects of the inferior alveolar nerve. Patients with neuromuscular disorders or non‐vital third molars were also excluded. Number randomised: 128 participants, 196 teeth Number evaluated: unclear |
|
| Interventions | Coronectomy versus complete surgical removal Group A (n = 94 teeth): coronectomy ‐ sectioning 3 to 4 mm below the crown, reducing roots with bur and leaving in situ. No treatment to the pulp Group B (n = 102 teeth): complete surgical removal of teeth 60% of teeth were treated under general anaesthesia, 30% under local anaesthesia, and 10% under sedation + local anaesthesia. 3 surgeons performed the procedures. Follow‐up: 2 years |
|
| Outcomes | Verbal assessment and mechanosensory testing of inferior alveolar nerve, dry socket infection or soft‐tissue infection assessed immediately postoperation, on day 3, and after 1 to 2 weeks | |
| Notes | Sample size calculation: not reported Unit of randomisation is teeth. Patients having non‐surgical extraction were excluded. In order to overcome problems related to the study being a mixture of split‐mouth and parallel‐group designs, 1 site per participant was randomly selected. Additional information supplied by author. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...the teeth to be removed were randomised (using a table of random numbers that was concealed from the surgeon)" |
| Allocation concealment (selection bias) | Low risk | Quote: "...the teeth to be removed were randomised (using a table of random numbers that was concealed from the surgeon)" |
| Blinding (performance bias and detection bias) patient | Unclear risk | Blinding of participants not mentioned. Surgeons would have an ethical duty to inform their patients that some of their tooth was remaining in situ. |
| Blinding (performance bias and detection bias) assessor | High risk | Not mentioned whether or not outcome assessors were blinded. Method of pain assessment not discussed. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 128 participants were included, but it is unclear how many participants were in each group. Denominators for outcomes are teeth not people, and participants not analysed in the groups into which they were originally randomised: presence of the failed coronectomy subgroup confounds the intention‐to‐treat analysis. 22 of the 196 teeth were simple elevation extractions, and there does not appear to be any statistical accounting for this. "Of the 58 patients who had coronectomy 47 (81%) attended the department for review within the first 6 months." No reasons given for these failures of follow‐up. No mention of follow‐up in extraction group |
| Selective reporting (reporting bias) | High risk | All prespecified outcomes reported on, but some outcomes not reported for each randomised group. Some data were supplied by the authors, but it is unclear when and how pain was assessed. Pain is reported per tooth, but participants with 2 teeth in the study would be expected to have greater pain. |
| Other bias | Unclear risk | No mention of how pain was assessed or if any statistical tests were done on it. 196 teeth from 128 participants, and it is often unclear which numbers were used in analysis. |
Roode 2010.
| Study characteristics | ||
| Methods | Study design: RCT (split‐mouth) Conducted in: Department of Maxillofacial and Oral Surgery, Faculty of Health Sciences, University of Pretoria, South Africa Number of centres: 1 Recruitment period: not stated |
|
| Participants | Inclusion criteria: no pre‐existing medical conditions or medication use that would influence patient's ability to undergo surgery. Symmetrical, bilateral impacted lower third molars fully covered by mucosa with no discernable active pathology associated Mean age: 19 years; 26 female, 10 male Number randomised: 36 participants, 72 teeth Number evaluated: 33 |
|
| Interventions | Reverse L‐flap versus straight line incision Group A (n = 33): reverse L‐flap method of raising surgical flap for access to impacted tooth Group B (n = 33): alternative surgical flap method, a straight line incision All participants had both types of flap in a single procedure. The side of mouth was randomly allocated. All participants treated under general anaesthesia. Follow‐up: clinical assessment at day 3, questionnaires collected with 7 days of postoperative data compiled by the participant |
|
| Outcomes | Outcomes: duration of procedure, infection incidence reported. Pain and swelling using a VAS (0 to 10) assessed daily (every morning) from the day after surgery to day 7. | |
| Notes | Sample size calculation: not mentioned All procedures performed by the same surgeon. E‐mail sent to authors requesting additional information 2 July 2012. Unpublished data supplied. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The side for the intervention and the control were selected by the "cast of a die". |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Low risk | All procedures carried out under a general anaesthetic. |
| Blinding (performance bias and detection bias) assessor | High risk | Not mentioned whether or not clinical outcome assessors were blinded. Some outcomes participant reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 36 participants were included in the trial, but questionnaires were only returned by 33. Unlikely to introduce bias in this split‐mouth trial |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported, and estimates of variance for outcomes supplied by e‐mail from authors. |
| Other bias | Low risk | No other sources of bias identified. |
Rullo 2013.
| Study characteristics | ||
| Methods | Study design: RCT (split‐mouth), procedures 30 days apart Conducted in: Naples, Italy Number of centres: 1 Recruitment period: not stated |
|
| Participants | Inclusion criteria: (a) the presence in each person of bilateral and symmetrically oriented impacted lower third molars to be extracted for prophylactic reasons; (b) forceps extractions not requiring osteotomy were excluded; (c) no systemic diseases; (d) age > 18 years; (e) non‐smoker; (f) not pregnant; and (g) no allergy to penicillin or other drugs used in the standardised postoperative therapy Exclusion criteria: patients who were taking antibiotics for current infection or who had acute pericoronitis or severe periodontal disease at the time of operation Mean age: 26.2 years, range 18 to 54 years. Male 20, female 32 Number randomised: 52 Number evaluated: 52 |
|
| Interventions | Piezoelectric bone removal versus bur Group A (n = 52): piezoelectric hand‐piece operating with modulated ultrasound with a functional frequency of 25e29 kHz and a digital modulation of 30 kHz. The inserts moved with a linear vibration of between 60 and 210 mm. Group B (n = 52): osteotomies using a conventional rotating drill were carried out with a Stryker tungsten carbide bur mounted on a surgical high‐speed hand‐piece Procedures subgrouped into "simple extractions" and complex extractions. All procedures performed under local anaesthetic, and drain inserted. All participants received amoxicillin (500 mg 3 times daily for 7 days starting day before surgery), ibuprofen 600 mg 3 times daily for 4 days, and CHX mouthwash. Follow‐up: VAS (0 to 10) for pain completed daily for 6 days |
|
| Outcomes | Duration of procedure, pain (100‐point VAS), surgical difficulty (Parant scale), histological analysis of bone biopsy samples | |
| Notes | Sample size calculation: not reported All procedures performed by the same surgeon. E‐mail sent to authors requesting additional information. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quotes: "...the instruments were randomly selected using a coin toss", "instrument sequence was random" |
| Allocation concealment (selection bias) | Unclear risk | Unclear who performed the coin toss and exactly how the first extraction side was chosen |
| Blinding (performance bias and detection bias) patient | Unclear risk | Participants and clinicians could not be blinded to allocated treatments. |
| Blinding (performance bias and detection bias) assessor | High risk | No blinding of outcome assessment undertaken. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear how many procedures were included in the simple and complex subgroups, for each procedure |
| Selective reporting (reporting bias) | High risk | Pain measured and reported. It seems likely that attempts were made to measure swelling and trismus, but these outcomes were not reported because the measures were "not reproducible". |
| Other bias | High risk | The outcomes in the graphs and in the tables are contradictory. |
Saglam 2003.
| Study characteristics | ||
| Methods | Study design: RCT (split‐mouth) Conducted in: Department of Oral and Maxillofacial Surgery, School of Dentistry at Suleyman Demirel University, Isparta, Turkey |
|
| Participants | Inclusion criteria: healthy, co‐operative patients aged 15 to 39 years who had bilateral fully impacted mandibular third molars, partly or completely covered by bone Exclusion criteria: patients with significant medical diseases or history of bleeding problems. Pregnant women and patients with signs of pericoronitis were also excluded. Number randomised: 13 Number evaluated: unclear ‐ no mention of withdrawals, but numbers evaluated not stated |
|
| Interventions | Tube drain versus no drain Group A (n = 13 teeth): small surgical tube drain applied via a stab incision in buccal fold between first and second molars; drain was removed 3 days postoperation Group B (n = 13 teeth): no drain used; flap approximated without tension All procedures performed by 1 surgeon, and all participants received the same antimicrobial and analgesic drugs. Seems likely that procedures performed on 2 separate visits, but timing unclear. All procedures performed under local anaesthetic. Follow‐up: 7 days |
|
| Outcomes | Swelling by measuring distance from commissures to ear lobe and distance from outer canthus of eye to angulus mandibulae. Maximum mouth opening measured between edges of maxillary and mandibular central incisors. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...the teeth were assigned [...] by random selection and in a crossover pattern" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding (performance bias and detection bias) patient | Unclear risk | Not mentioned, and it is not possible to blind participants to the presence of an intraoral surgical drain |
| Blinding (performance bias and detection bias) assessor | High risk | Quote: "...the patients were examined by the same surgeon immediately preoperatively, and on the first, second, third and seventh post‐operative days." Comment: unclear whether the outcome assessor was the surgeon who performed the procedure. Probably obvious whether drain was used |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No mention of withdrawals. It is likely that all 26 were included in evaluation. |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported on. |
| Other bias | Low risk | No other sources of bias identified. |
Sandhu 2010.
| Study characteristics | ||
| Methods | Study design: split‐mouth cross‐over RCT Conducted in: India Number of centres: 1 Recruitment period: not stated |
|
| Participants | Inclusion criteria: patients requiring extraction of bilateral impacted third molars, with no history of medical illness or medication use that could influence wound healing, healthy dental and periodontal status at the time of surgery. Attempt was made to include those with teeth of comparable position and expected difficulty during extraction. Exclusion criteria: not explicitly stated Age: mean 25 years Number randomised: 20 (40 teeth) Number evaluated: 20 |
|
| Interventions | Bayonet flap versus envelope flap Group A (n = 20): bayonet flap raised Group B (n = 20): envelope flap raised Minimum of 1 month between procedures All procedures performed under local anaesthetic. All participants given prophylactic intravenous amoxicillin/clavulanic acid, ibuprofen tablet, and CHX mouth rinse prior to surgery, and ibuprofen and CHX mouth rinses in the postoperative period. |
|
| Outcomes | Pain (0‐to‐10 VAS), facial swelling, trismus, wound dehiscence evaluated on days 1, 3, 7, 14, and 30 | |
| Notes | Sample size calculation: not reported E‐mail sent 26 March 2012 requesting further information. Reply received 31 March 2012 with unpublished data. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quotes: "...randomized by systematic allocation"; "Both the type of flap used and the side operated were randomized by tossing a coin which was carried out by the surgeon, and communicated to the evaluator after the surgical procedure for recording" (e‐mail communication) |
| Allocation concealment (selection bias) | High risk | Coin toss done by operating surgeon (e‐mail communication). |
| Blinding (performance bias and detection bias) patient | Low risk | Quote: "...both patients and evaluator were blinded to the flap groups" |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "...both patients and evaluator were blinded to the flap groups" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in the outcome evaluations. |
| Selective reporting (reporting bias) | Low risk | All planned outcomes reported. |
| Other bias | Low risk | No other sources of bias identified. |
Shad 2015.
| Study characteristics | ||
| Methods | Study design: RCT, parallel Conducted in: Lahore, Pakistan |
|
| Participants | Inclusion criteria: patients who were clinically and radiographically diagnosed as having impacted mandibular third molar were included in the study Exclusion criteria: patients with medically compromised conditions that affect wound healing, e.g. diabetes mellitus, anaemia, patients on steroid therapy, and unco‐operative patients who were not willing to come for follow‐up Age: 18 to 38 years; mean 25.58 years (SD ± 5.11) Number randomised: 380 participants Number evaluated: 380 participants |
|
| Interventions | Reflection and retraction of lingual flap (+ buccal flap) versus no lingual reflection and retraction (buccal flap only) Group A (n = 190): reflection and retraction of lingual flap in addition to buccal flap Group B (n = 190): no lingual flap procedure was performed (buccal flap only) Participants were operated under local anaesthesia through regional block of inferior alveolar, lingual, and buccal nerves. |
|
| Outcomes | Sensory disturbance was evaluated on seventh postoperative day. Lingual nerve function was assessed by light touch, pin prick, 2 point discrimination, and taste. Lingual nerve was labelled injured if there was absence of any of the above mentioned sensations. Lingual nerve damage occurred in 8.94% in Group A in which lingual flap retraction was performed but damage was reversible. In Group B, 2.63% lingual nerve damage was observed, and nature of damage was permanent. The difference was statistically significant (P = 0.008). |
|
| Notes | Comparison was made with Chi2. P ≤ 0.05 was considered significant. Sample size calculation: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Comment: blocked randomisation was used |
| Allocation concealment (selection bias) | Unclear risk | Comment: it remains unclear who recruited participants and who carried out the randomisation |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: the procedure was explained to the participant, but the details of what was explained are unclear |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Comment: it is unclear whether the person measuring the outcomes was different to the surgeons |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: all outcome data for all participants were reported |
| Selective reporting (reporting bias) | Low risk | Comment: all intended outcomes were reported |
| Other bias | Low risk | Comment: no other sources of bias were identified |
Singh 2018.
| Study characteristics | ||
| Methods | Study design: parallel arms Conducted in: India |
|
| Participants | Inclusion criteria: impacted mandibular third molar, patients between 18 and 40 years old, with recurrent pericoronitis, vital tooth with no periapical infection, vertical, mesio, or disto angular impaction Exclusion criteria: allergic to local anaesthesia, presence of infection and swelling, medically compromised patients, mobile teeth, and patients with horizontal impacted tooth Age: mean 24.9 +/‐ 3.933 years Number randomised: 30 Number evaluated: 30 |
|
| Interventions | Coronectomy versus odontectomy Group 1 (n = 15): coronectomy Group 2 (n = 15): odontectomy All procedures performed under local anaesthetic. Postoperative antibiotics were given: ampicillin 250 mg, cloxacillin 250 mg, metronidazole 400 mg 3 times a day for 5 days, paracetamol 325 mg 3 times a day for 3 days |
|
| Outcomes | Pain (100‐millimetre VAS), swelling (facial measurements pre‐ and postoperation), nerve paraesthesia, trismus, postoperative infection, wound dehiscence, pocket depth, and root migration (by measuring fixed points on OPG radiographs) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the method of randomisation was not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Comment: allocation concealment is not mentioned |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: it is unclear whether participants knew which treatment they received |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Comment: not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no dropouts |
| Selective reporting (reporting bias) | Low risk | Comment: all planned outcomes were reported |
| Other bias | Unclear risk | It is unclear why 1 participant had cone beam tomography and the other participants did not, in this "randomised prospective study". |
Srinivas 2006.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: Bangalore, India Number of centres: 1 Recruitment period: not stated |
|
| Participants | Inclusion criteria: patients aged 15 to 39 years willing to participate in the study. No significant medical history, non‐smokers, non‐alcoholics with bilateral and symmetrically positioned impacted lower third molars that were completely covered by mucosa/partially or completely covered by bone Exclusion criteria: none stated Number randomised: 14 Number evaluated: 14 |
|
| Interventions | Tube drain versus no drain Group A (n = 14): mucoperiosteal flap raised following envelope incision, flap was reflected and bone removed with a bur. Tooth was removed and socket was irrigated with saline. Small surgical drain was placed via stab incision in buccal fold between first and second molar and closed. Tube was removed on postoperative day 3. Group B (n = 14): mucoperiosteal flap raised following envelope incision, flap was reflected and bone removed with a bur. Tooth was removed and socket was irrigated with saline. Flap was approximated, closed with interrupted 3‐0 silk sutures. All surgical procedures were performed by the same surgeon under local anaesthetic. Second extraction was performed after 2 months. |
|
| Outcomes | Pain (present/absent), swelling (vertical/horizontal measurements), trismus (MMO) | |
| Notes | No sample size calculation reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly chosen" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) assessor | High risk | Not mentioned. Likely that the same operator performed the procedures and assessed the outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in outcomes. |
| Selective reporting (reporting bias) | Low risk | All planned outcomes reported. |
| Other bias | Low risk | No other sources of bias identified. |
Sweet 1976.
| Study characteristics | ||
| Methods | Study design: RCT (split‐mouth) Conducted in: United States Public Health Service Hospital, New York, USA |
|
| Participants | Inclusion criteria: male patients from 17 to 27 years of age, who were in good health, and who required bilateral, similarly impacted wisdom teeth extracted. Medical health was ascertained by a "complete physical examination by a physician, normal hospital screening tests, a resident's admission examination, and a complete medical history". In addition, "only patients with soft‐tissue or osseous‐tissue impactions which were asymptomatic were accepted for the study". Exclusion criteria: "patients with a preoperative infection or pericoronitis were eliminated from the study" Number of participants randomised: 103 men, 206 teeth Number of participants evaluated: 99; no withdrawals, but 4 patients with infection excluded from other outcome assessments |
|
| Interventions | Mechanical irrigation versus manual irrigation Group A (n = 103 teeth): postextraction mechanical lavage (350 mL sterile saline) Group B (n = 103 teeth): conventional manual syringe lavage (350 mL sterile saline) Procedures performed under general anaesthetic, both teeth extracted in same session by same surgeon. Follow‐up: days 3 and 5 |
|
| Outcomes | Alveolar osteitis, infection, pain (4‐point scale), swelling (4‐point scale) | |
| Notes | Sample size calculation: not reported 4 participants who presented with alveolar osteitis or infection were excluded from other outcome assessments. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The type of irrigation [...] was predetermined by random selection technique, with the use of random sampling numbers, before the study was begun" |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Low risk | Blinding not mentioned, but it is likely that participants were unaware of lavage volume as they were sedated with pentobarbital. |
| Blinding (performance bias and detection bias) assessor | Low risk | Quotes: "These examinations were made by a dental surgeon who was not involved with the operation"; "the surgical sites were observed by a dental surgeon who was not involved with the operation, and who was unaware of the irrigation methods used" Comment: assessor blinding successful |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No withdrawals, but 4 participants who had infections were excluded from wound healing outcome. However, in a split‐mouth study this is unlikely to have introduced bias. Quote: "once a patient was treated, he was then counted in the 'treated group', and was not evaluated for any healing results at the 3‐ or 5‐day levels" |
| Selective reporting (reporting bias) | Low risk | All planned outcomes reported. |
| Other bias | Low risk | No other sources of bias identified. |
Topcu 2019.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: Turkey |
|
| Participants | Inclusion criteria: patients with bilateral, comparable impacted lower third molars with a symmetrical position and angulation Exclusion criteria: patients with a history of systemic diseases, alcoholism, drug abuse, and heavy smoking; patients with allergies to local anaesthetics, antibiotics, and anti‐inflammatories; and patients with acute infections at the time of surgery Age: mean 22.38 years Number randomised: 21 participants (42 sites) Number evaluated: 21 |
|
| Interventions | Piezoelectric surgery versus conventional osteotomy Group 1 (n = 21): piezoelectric surgery (n = 21 impacted molars) Group 2 (n = 21): conventional osteotomy technique (n = 21 teeth) The second operation for the extraction of the contralateral impacted lower third molar was scheduled for 2 weeks after the first operation. All surgeries were conducted under local anaesthetic. All participants were instructed to take 500 mg of paracetamol 4 times a day postoperatively. |
|
| Outcomes | Neurosensory deficit and paraesthesia, pain (0‐to‐10 VAS), anxiety (State Trait Anxiety Inventory), operation time | |
| Notes | 2‐week interval between the 2 surgeries Paraesthesia was zero in both groups. 1 participant reported buzzing sound in the ear, which relieved at the follow‐up period. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: method of randomisation was not described. Recruitment details are not specified. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The osteotomy technique (piezoelectric surgery or conventional rotatory handpiece) was randomly allocated to be performed on the left or right side" Comment: it is unclear how or if the allocation was concealed |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: it is not explicitly stated whether the participants were blinded or not |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Comment: no mention of who carried out the postoperative measurements |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no dropout |
| Selective reporting (reporting bias) | Low risk | Comment: all planned outcomes were reported |
| Other bias | Unclear risk | Quote: "The second operation for the extraction of the contralateral impacted lower third molar was scheduled 2 weeks after the first operation." Comment: a wash‐out period of 2 weeks may not be sufficient depending on healing from the first procedure |
Unsal 2018.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: Turkey |
|
| Participants | Inclusion criteria: (a) the presence of bilateral, symmetrically oriented, partially erupted lower third molars requiring extraction for prophylactic reasons; (b) the absence of pathology associated with the third molars; (c) no pre‐existing systemic diseases; and
(d) no chronic opioid use Exclusion criteria: patients who had no second molars and pregnant or lactating women were excluded Age: mean 23.96 Number randomised: 50 Number evaluated: 50 |
|
| Interventions | PRF versus none Group A (n = 50): PRF was placed in the socket Group B (n = 50): control; nothing was placed in the opposite socket Postoperative prescriptions were paracetamol (500 mg) 3 times per day and 0.2% chlorhexidine mouthwash 3 times per day for 7 days. |
|
| Outcomes | Pain (verbal rating scale 0 to 10); alveolar osteitis | |
| Notes | Only 7 days between the 2 surgeries | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: the method of randomisation was not stated |
| Allocation concealment (selection bias) | Unclear risk | Comment: no mention of allocation concealment |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: although it is unlikely that participants knew which side had which intervention, this is not explicitly stated |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Comment: it is unclear who assessed the participants postoperatively |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no withdrawal |
| Selective reporting (reporting bias) | Low risk | Comment: all planned outcomes were reported |
| Other bias | Unclear risk | Quote: "...using round bodied 3–0 black silk or vicryl, and sutures were removed after 1 week whether it is vicryl or silk." Comment: methodology was not consistent, the same sutures should have been used in the whole of Group A |
Uyanik 2015.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: Nicosia, Cyprus |
|
| Participants | Inclusion criteria: (a) the presence of bilateral, symmetrically oriented, impacted lower third molars requiring extraction for prophylactic reasons; (b) the absence of systemic diseases; (c) no chronic opioid use; (d) age > 18 years; (e) non‐smoker and non‐alcoholic; (f ) not pregnant; and (g) no allergy to penicillin or other drugs Exclusion criteria: patients taking antibiotics for a current infection, or who had acute pericoronitis or severe periodontal disease at the time of the operation and if tooth needed sectioning during the surgery Age: 19 to 31 Number randomised: 20 (10 female/10 male) Number evaluated: 20 (40 wisdom teeth) |
|
| Interventions | PRF or a combination of PRF and piezosurgery versus conventional rotatory osteotomy Group A (n = 10 participants/20 teeth): traditional surgery was performed on 1 side (Group 1, n = 10); traditional surgery was performed and PRF was administered to the extracted socket on the other side of same participant (Group 2, n = 10) Group B (n = 10 participants/20 teeth): piezosurgery was used for osteotomy and PRF was administered on 1 side (Group 3, n = 10); traditional surgery was performed on the other side of same participant (Group 4, n = 10) |
|
| Outcomes | Variables assessed were pain, the number of analgesics taken, trismus, and cheek swelling at baseline and on postoperative days 1, 2, 3, and 7. Pain VAS (0 to 10) Trismus (measurement of interincisal distances). |
|
| Notes | Sample size calculation: not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "the selection of processes of which technique to use first on each participant was randomly selected." |
| Allocation concealment (selection bias) | Unclear risk | Comment: concealment approaches were not described, and it is unclear how the randomisation was achieved |
| Blinding (performance bias and detection bias) patient | High risk | Quote: "all of the participants were informed regarding the surgical procedure, postoperative time and possible complications." Comment: the extent to which the surgical procedure was described is unclear. All participants had PRF in 1 of their extraction sites; however, as the control and experimental extractions were done on separate occasions, unless the participant had blood samples taken on both occasions they would have guessed which side had PRF. |
| Blinding (performance bias and detection bias) assessor | Unclear risk | Quote: "all of the examinations were undertaken at approximately the same time of day and by the same surgeon; measurements were always obtained by the same individual, both preoperatively and postoperatively." Comment: it is unclear if this was the operating surgeon |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: all participants included in data evaluation, no dropout |
| Selective reporting (reporting bias) | Low risk | Comment: all planned outcomes were reported |
| Other bias | Unclear risk | Comment: carry‐over effect was not evaluated |
Xavier 2008.
| Study characteristics | ||
| Methods | Study design: RCT (split‐mouth) Conducted in: Recife, Brazil Recruitment period: May to September 2004 |
|
| Participants | Inclusion criteria: participants consecutively enrolled between May and September 2004 for surgical extraction of bilateral impacted lower third molars. Both wisdom teeth had to be in similar position according to Pell and Gregory classification. Exclusion criteria: history of significant systemic pathology, or use of any medication that could interfere with the repair process Number of participants randomised: 20 Number of participants evaluated: 20 |
|
| Interventions | Partial wound closure versus complete wound closure Group A (n = 20 teeth): sutures on attached gum only Group B (n = 20 teeth): complete suture was performed on free and attached gums Procedures performed under local anaesthetic, both teeth extracted in same session by same surgeon. Follow‐up: days 3, 7, and 15, and 3 months |
|
| Outcomes | Pain, swelling, trismus at 7 days, probing depth 3 months postoperation | |
| Notes | Sample size calculation: not reported E‐mail sent 29 March 2012 requesting further information. No reply received. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "2 groups were established on randomised basis (by allotment)" Comment: method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) patient | Low risk | Double‐blinded |
| Blinding (performance bias and detection bias) assessor | Low risk | Double‐blinded; assumed that both participants and clinical outcome assessor blinded to treatment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in outcome evaluation. |
| Selective reporting (reporting bias) | Unclear risk | All planned outcomes reported. |
| Other bias | Unclear risk | No other sources of bias identified. |
Şimşek Kaya 2019.
| Study characteristics | ||
| Methods | Study design: split‐mouth RCT Conducted in: Turkey |
|
| Participants | Inclusion criteria: patients for surgical removal of bilaterally impacted mandibular third molars (with the ability to understand verbal and written instructions) were included in study. Additional inclusion criteria were American Society of Anesthesiologists (ASA) physical status class I (indicating a normally healthy patient), no medication use, asymptomatic bilateral symmetrically impacted mandibular third molars with mesioangular (Winter classification) 18 class II B impaction (Pell and Gregory classification) 19 and healthy dental and periodontal status with no local inflammation or pathology at the time of surgery. Exclusion criteria: patients with allergies or contraindications to the anaesthetics employed, with local inflammation or pathology in the oral cavity, with poor oral hygiene, ASA > 1, pregnant or lactating women, or women regularly using oral contraceptives were excluded Age: 18 to 40 years Number randomised: 30 Number evaluated: 30 |
|
| Interventions | Envelope flap versus modified triangular flap techniques Group A: modified triangular flap techniques Group B: envelope flap A minimum of 1 month was allowed to elapse between the 2 procedures. In the postoperative period, amoxicillin (1000 mg, 2 x 1/day), ibuprofen (400 mg, 3 × 1/day), and 0.2% chlorhexidine gluconate (30 mL, 2 × 1/day) were prescribed to all participants for 5, 7, and 5 days, respectively. |
|
| Outcomes | Pain (0‐to‐10‐centimetre scale), swelling, trismus, alveolar osteitis (Blum's criteria), wound dehiscence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Treatment modalities for each patient were determined by a nurse not involved in the study using the lottery method" |
| Allocation concealment (selection bias) | Low risk | Quote: "The treatment allocation sequence was concealed using sequentially numbered, opaque, sealed envelopes. Allocation concealment was intended to prevent selection bias and to protect the assignment sequence until the first procedure." "The treatment allocation sequence was concealed using sequentially numbered, opaque, sealed envelopes. Allocation concealment was intended to prevent selection bias" |
| Blinding (performance bias and detection bias) patient | Unclear risk | Comment: it is not explicitly stated that the participants were blinded as to which intervention they received, but it seems unlikely that they would have been aware of the type of intervention |
| Blinding (performance bias and detection bias) assessor | Low risk | Quote: "One author, responsible for calculation and calibration and not involved in the selection and intervention of participants (GYY), performed all the measurements." Comment: of note, the authors state that the operator and dental assistant who performed the surgical intervention could not be blinded due to the nature of the interventions |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: no withdrawal |
| Selective reporting (reporting bias) | Low risk | Comment: all prespecified outcomes were reported on |
| Other bias | Low risk | Comment: no other sources of bias identified |
CAL: clinical attachment level; CHX: chlorhexidine; IDN: inferior dental nerve; IID: interincisal distance; IND: inferior dental nerve; IOPA: intra‐oral periapical; MMO: maximum mouth opening; OPG: orthopantomogram; PPD: probing pocket depth; PRF: platelet rich fibrin; RCT: randomised controlled trial; SD: standard deviation; TMD: temporomandibular disorder; rmp: revolutions per minute; VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abu‐Serriah 2004 | Most study participants had both maxillary and mandibular third molars extracted in the same procedure. Also, bur group participants were irrigated with saline and those in the laser group were irrigated with water. This was thought to be a confounding factor. |
| Afat 2018 | Not a surgical technique |
| Akota 1998 | Surgical drain used in 1 group was coated with chlortetracycline ointment. It was thought that the antibiotic confounded the effect of the drain. |
| Al‐Moraissi 2016 | It is a review not an RCT. |
| Alqahtani 2017 | No data could be used from this study. |
| Ayad 1995 | Unclear study design ‐ both parallel‐group and split‐mouth study. Also, wisdom teeth in the maxilla were included. |
| Bilginaylar 2016 | Ineligible trial design |
| Cetinkaya 2009 | Primary outcome measures of this review not reported. Trial looks at effects on periodontal disease. |
| Chang 2015 | Ineligible surgical technique |
| Chen 2016 | Ineligible outcomes |
| Chossegros 2002 | Study describes germectomy not extraction of third molars. |
| Clauser 1994 | Not all participants had incision and flap raised. Some third molars were removed using an elevator. |
| Cortell‐Ballester 2015 | Ineligible outcomes |
| de Carvalho 2015 | Ineligible outcomes |
| Desai 2014 | Ineligible outcomes |
| Ding 2000 | No mention of incision or flap being raised |
| Dubois 1982 | Split‐mouth trial, but allocation of 1 side of face to treatment was not randomised |
| Dutta 2015 | Ineligible outcomes |
| Egbor 2014 | The use of white head varnish is not a surgical technique. |
| Elo 2016 | Data could not be used as there were no raw data. |
| Eshghpour 2018 | Not a surgical technique |
| Finne 1981 | Study describes germectomy not extraction of third molars. |
| Gao 2011 | Ineligible outcomes |
| Gawai 2015 | Not an RCT |
| Gay‐Escoda 2015 | Data presented in graph/figures only. |
| Gazivoda 2015 | Ineligible comparison ‐ synthetic suture materials |
| Genu 2008 | Unclear whether study was truly randomised; appeared to have 2 interventions, and there was confounding of the effects. Unable to contact authors to obtain further information |
| Gonzalez 2001 | Abstract only; insufficient information to include. No subsequent publication identified. |
| Goyal 2012 | Allocation by alternation |
| Guo 2012 | Not an RCT |
| He 2015 | Not available in English. Study was sent to a translator, but insufficient data or information to make an assessment. We contacted the study authors but received no reply. |
| Holland 1984 | Comparison is between 2 types of wound closure, but 1 incision also had a dressing, which acted as a confounder. |
| Jain 2016 | Ineligible technique |
| Jakse 2002 | Not an RCT |
| Jiang 2015 | A review, not an RCT |
| Kerdvongbundit 1989 | Unable to locate a copy of this paper. There is no abstract, and based on title it is unclear whether this was a randomised trial. |
| Korkmaz 2015 | Inappropriate techniques |
| Li 2012 | Systematic review |
| Li 2014 | Ineligible techniques; we contacted the authors but received no reply. |
| Ma 2015 | Ineligible outcomes |
| Martin 2015 | Systematic review |
| Mavrodi 2015 | Inappropriate techniques |
| Oyri 2016 | Not an RCT |
| Quee 1985 | Trial of the effect of flap design on subsequent periodontal health. Not relevant to this review |
| Robinson 1996 | The study compared removal of wisdom teeth with or without lingual flap retraction. Prior to operation the operator was aware of allocation. The authors found significant differences in the grades of surgical difficulty between the 2 groups. On investigation some of the operators had deviated from the protocol. In an unknown number of easier surgical cases, the lingual flap was not raised when it should have been. We are unable to quantify the bias caused by this protocol violation. |
| Rosa 2002 | Not an RCT |
| Sala‐Perez 2016 | Ineligible techniques |
| Salentijn 2011 | Ineligible techniques |
| Sener 2015 | Not evaluating a surgical technique |
| Shevel 2001 | This study included both mandibular and maxillary molar teeth. The removal of the maxillary teeth may affect pain and swelling, so we could not use the data for the mandibular teeth. |
| Sivolella 2011 | Study describes germectomy not extraction of third molars. |
| Smith 2000 | Not an RCT |
| Sortino 2008 | Not an RCT |
| Strukmeier 1980 | Probably not RCT after translation from German |
| Suarez‐Cunqueiro 2003 | This study is confounded by the surgical removal of unerupted maxillary third molars. |
| Suddhasthira 1991 | Paper in Thai language. Sent to translator. Not an RCT |
| Sun 2009 | Not available in English |
| Sweet 1978 | Contradiction on state of teeth. They are described as all being impacted, and then some are described as being erupted. We are also unsure whether the same surgical technique was used bilaterally. |
| Tabrizi 2014 | Ineligible techniques |
| Tan 2015 | Ineligible techniques |
| Torres‐Lagares 2006a | Ineligible techniques |
| Torres‐Lagares 2006b | Intervention is postsurgical use of chlorhexidine gel to prevent infection. Not a surgical intervention |
| Tuffin 1990 | Design fault. This study compared irrigation of the socket at the end of surgery with bupivacaine versus no irrigation. Apart from the planned interventions, the participants were also treated by chisel or drill technique, with 16 treated by drill but only 1 of them in the control group and the other 15 being in the treatment group. We felt this could be a confounding factor. |
| Yang 2015 | Ineligible techniques |
| Yolcu 2015 | Ineligible techniques |
| Zhang 1997 | No mention of incision or flap being raised |
| Zhou 2016 | Ineligible intervention |
RCT: randomised controlled trial
Characteristics of studies awaiting classification [ordered by study ID]
Kumar 2013.
| Methods | RCT cross‐over design |
| Participants | 20 participants |
| Interventions | Standard incision versus comma‐shaped incision and its influence on postoperative complications in surgical removal of impacted third molar |
| Outcomes | Postoperative complications |
| Notes | Categorical data ‐ need to dichotomise and ask authors for paired data. Email sent to author 19 February 2018 ‐ no reply received. |
Ozveri Koyuncu 2013.
| Methods | RCT parallel group |
| Participants | 36 participants |
| Interventions | 3‐cornered flap versus modified triangular flap |
| Outcomes | Dehiscence, pain, swelling, mouth opening |
| Notes | Author contacted about study design and missing data but no reply received. |
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
ChiCTR‐ICR‐15006182.
| Study name | Posterior‐triangle flap: a new flap design for impacted mandibular third molars |
| Methods | Interventional study, parallel RCT |
| Participants | 180 participants with impacted mandibular third molars. 18 to 30 years old |
| Interventions | Triangular flap versus envelope flap versus posterior triangular flap |
| Outcomes | Operation time; postoperative pain; mouth opening; swelling; periodontal index; tongue paraesthesia |
| Starting date | 5 February 2015 |
| Contact information | Chengge Hua, Sichuan, China. huachengke@scu.edu.cn |
| Notes | Objectives: this prospective study compared posterior‐triangle flap to envelope flap and triangular flap in extraction of impacted mandibular third molars, and assessed how the interventions affect operation time, and postoperative complications such as pain, swelling, trismus, periodontal healing, as well as inferior alveolar and lingual nerve injure. To evaluate whether posterior‐triangle flap is a better way for mandibular third molar extraction |
IRCT2014052017781N1.
| Study name | Compare of influence different two suture techniques on periodontal health of the mandibular second molars after extraction of impact third molar |
| Methods | Non‐blinded parallel RCT |
| Participants | Target sample size: 13. 20 to 25 years old |
| Interventions | 2 suture techniques |
| Outcomes | Not specified |
| Starting date | 31 December 2013, 1392/10/10 |
| Contact information | Fouzieh Vahidnia, Ahvaz University of Medical Sciences, Iran Email: vahidnia.f@ajums.ac.ir |
| Notes |
IRCT2014052717863N2.
| Study name | The effect of two types of envelope and modified triangular flap in the prevention of dry socket after mandibular third molar surgery |
| Methods | Double‐blinded parallel RCT |
| Participants | Target sample size: 60 |
| Interventions | 2 surgical flaps |
| Outcomes | Dry socket |
| Starting date | 13 March 2013 |
| Contact information | Sahebe Talebi Banizi, Shahid Sadoughi University of Medical Sciences, Iran (Islamic Republic of) Email: addresssahebetalebi@ssu.ac.ir |
| Notes |
IRCT2015050722139N1.
| Study name | Tissue adhesives for surgical wound closures |
| Methods | Single‐blind RCT |
| Participants | Target sample size: 12 |
| Interventions | Using tissue adhesive 2 ethyl‐cyanoacrylate (EPIGLU, Meyer‐Haake Co., Germany) for wound closure in intervention group. Adhesive was used according to package insert. |
| Outcomes | Pain, bleeding, wound healing, patient comfort |
| Starting date | September 2014 |
| Contact information | Benika Abbasi, Jundishapur University of Medical Sciences Email: Abbasi.b@ajums.ac.ir |
| Notes |
IRCT201506191760N42.
| Study name | The effect of releasing (relaxing) incision on the postoperative complication of mandibular third molar surgery |
| Methods | Single‐blinded parallel RCT |
| Participants | Target sample size: 20 |
| Interventions | Surgical flaps |
| Outcomes | Complications after surgery; pain; lockjaw; ecchymosis; duration of surgery |
| Starting date | 6 July 2015 |
| Contact information | Nargess Gholizadeh Pasha Fatemehzahra Infertility Reproductive Health Research Center, Babol University of Medical Sciences, Iran (Islamic Republic of) Email addresszahra@mubabol.ac.ir |
| Notes |
ISRCTN16849867.
| Study name | Platelet rich fibrin effects on third molar surgery |
| Methods | RCT |
| Participants | 17 to 27 |
| Interventions | Platelet rich fibrin |
| Outcomes | Swelling; pain |
| Starting date | 6 March 2017 |
| Contact information | Dr Mehmet Fatih Şentürk mehmetsenturk@sdu.edu.tr |
| Notes |
NCT02495207.
| Study name | A comparison between conventional surgery and piezosurgery |
| Methods | Parallel RCT |
| Participants | 15 participants |
| Interventions | Piezosurgery |
| Outcomes | Primary outcome measures: levels of heat shock protein 70 (time frame: 5 minutes before third molar removal with the last removed layer of bone). This will be measured using ELISA (enzyme‐linked immunosorbent assay) methodology. Secondary outcome measures: percentage of viable bone cells (time frame: this variable will be measured from the specimens taken within the first 15 minutes of bone cutting to remove third molars). Percentage of viable bone cells will be calculated based on the counts of viable bone cells observed under the microscope. |
| Starting date | 19 June 2015 |
| Contact information | Department of Oral and Maxillofacial Surgery, University of Damascus Dental School/ Damascus, Damascus, Syrian Arab Republic |
| Notes | Official title: A histo‐immunological comparative study of bone cutting by conventional surgery and piezosurgery on the secretion of heat shock protein 70 (HSP70) and on the bone cells clinicaltrials.gov/ct2/show/NCT02495207 |
NCT02831374.
| Study name | Effectiveness of platelet rich plasma in wound healing |
| Methods | Randomised parallel assignment |
| Participants | 40 participants |
| Interventions | PRP gel |
| Outcomes | Primary outcome measures
|
| Starting date | October 2015 |
| Contact information | No contacts or locations provided. |
| Notes |
NCT02942108.
| Study name | Piezoelectric vibrations and tissue, cellular and molecular mechanisms of oral wound healing after third molar surgery |
| Methods | Interventional (clinical trial) |
| Participants | 40 participants |
| Interventions | Randomised cross‐over/piezosurgery |
| Outcomes | Primary outcome measures:
|
| Starting date | October 2016 |
| Contact information | Bozidar M Brkovic, DDS, PhD |
| Notes | 2nd Principal Investigator Marija S Milic, DDS, PhD |
PRP: platelet rich plasma; PRF: platelet rich fibrin; RCT: randomised controlled trial
Differences between protocol and review
Changes between original review (2014) and 2020 update: we excluded studies that evaluated "synthetic products" as wound closure techniques. This is because there were varieties of products used with no clear information about their manufacturing and contents. We updated GRADE assessments from 'quality' to 'certainty'.
Changes between protocol (2003) and original review (2014): during the preparation of the review we decided to exclude studies of germectomy as this procedure is fundamentally different from the extraction of impacted mandibular third molars. We also excluded studies looking at 'periodontal outcomes relating to the second permanent molar from the review', although this was not specified in the protocol. There were some changes to the prespecified outcomes and prioritisation of outcomes. New methods were applied for: quality assessment, inclusion of 'Summary of findings' tables and GRADE quality assessment.
Contributions of authors
Conceiving, designing and co‐ordination of the review: PC Screening search results and retrieval of papers against inclusion criteria: WK, NS, EB (PC, ME in previous versions) 'Risk of bias' assessment and data extraction: WK, NS, EB (PC, ME, TR, Susan Furness (SF) in previous versions) Writing to authors for additional information: WK (PC, EB in previous versions) Data management for the review and entering data into Review Manager 5: WK, HW (SF, EB in previous versions) Analysis and interpretation of data: HW, PC, EB, SF, TR, WK, NS Writing the review: WK, NS, EB, PC (SF in previous review) Providing general advice on the review: HW, PC, TR (PC, ME, TR in previous review)
Sources of support
Internal sources
School of Dentistry, The University of Manchester, UK
The Sahlgrenska Academy at Goteborg University, Sweden
GKTDI, King's College, London, UK
-
MAHSC, UK
Cochrane Oral Health is supported by the Manchester Academic Health Sciences Centre (MAHSC) and the NIHR Manchester Biomedical Research Centre.
External sources
Swedish Medical Research Council (9495), Sweden
-
Cochrane Oral Health Global Alliance, UK
The production of Cochrane Oral Health reviews has been supported financially by our Global Alliance since 2011 (oralhealth.cochrane.org/partnerships-alliances). Contributors in the last two years have been the American Association of Public Health Dentistry, USA; AS‐Akademie, Germany; the British Association for the Study of Community Dentistry, UK; the British Society of Paediatric Dentistry, UK; the Canadian Dental Hygienists Association, Canada; the Centre for Dental Education and Research at All India Institute of Medical Sciences, India; the National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; and Swiss Society of Endodontology, Switzerland.
-
National Institute for Health Research (NIHR), UK
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Oral Health. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Evidence Synthesis Programme, the NIHR, NHS, or the Department of Health and Social Care.
Declarations of interest
Edmund Bailey: none known Wafa Kashbour: none known Neha Shah: none known Helen V Worthington: none known. Tara F Renton: I am an author of a study included in this review; however, I was not involved in 'Risk of bias' assessment of this study. Paul Coulthard: none known
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Absi 1993 {published and unpublished data}
- Absi EG, Shepherd JP. A comparison of morbidity following the removal of lower third molars by lingual split and surgical bur methods. International Journal of Oral and Maxillofacial Surgery 1993;22(3):149-53. [DOI] [PubMed] [Google Scholar]
Acar 2017 {published data only}
- Acar AH, Kazancioglu HO, Erdem NF, Asutay F. Is horizontal mattress suturing more effective than simple interrupted suturing on postoperative complications and primary wound healing after impacted mandibular third molar surgery? Journal of Craniofacial Surgery 2017;28(7):e657-61. [DOI] [PubMed] [Google Scholar]
Arakji 2016 {unpublished data only}
- Arakji H, Shokry M, Aboelsaad N. Comparison of piezosurgery and conventional rotary instruments for removal of impacted mandibular third molars: a randomized controlled clinical and radiographic trial. International Journal of Dentistry 2016;2016:8169356. [DOI: 10.1155/2016/8169356] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baqain 2012 {published data only}
Barone 2010 {published data only}
Basheer 2017 {published data only}
- Basheer SA, Govind RJ, Daniel A, Sam G, Adarsh VJ, Rao A. Comparative study of piezoelectric and rotary osteotomy technique for third molar impaction. Journal of Contemporary Dental Practice 2017;18(1):60-4. [DOI] [PubMed] [Google Scholar]
Bello 2011 {published and unpublished data}
- Bello SA, Olaitan AA, Ladeinde AL. A randomized comparison of the effect of partial and total wound closure techniques on postoperative morbidity after mandibular third molar surgery. Journal of Oral and Maxillofacial Surgery 2011;69:e24-30. [DOI] [PubMed] [Google Scholar]
Bhati 2017 {published data only}
- Bhati B, Kukreja P, Kumar S, Rathi VC, Singh K, Bansal S. Piezosurgery versus rotatory osteotomy in mandibular impacted third molar extraction. Annals of Maxillofacial Surgery 2017;7(1):5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Briguglio 2011 {published and unpublished data}
- Briguglio F, Zenobio EG, Isola G, Briguglio R, Briguglio E, Farronato D, et al. Complications in surgical removal of impacted mandibular third molars in relation to flap design: clinical and statistical evaluations. Quintessence International 2011;42(6):445-53. [PubMed]
Butler 1977 {published data only}
- Butler DP, Sweet JB. Effect of lavage on the incidence of localized osteitis in mandibular third molar extraction sites. Oral Surgery 1977;44(1):14-20. [DOI] [PubMed] [Google Scholar]
Cerqueira 2004 {published data only}
- Cerqueira PR, Vasconcelos BC, Bessa-Nogueira RV. Comparative study of the effect of a tube drain in impacted lower third molar surgery. Journal of Oral and Maxillofacial Surgery 2004;62(1):57-61. [DOI] [PubMed] [Google Scholar]
Chukwuneke 2008 {published data only}
- Chukwuneke FN, Oji C, Saheeb DB. A comparative study of the effect of using a rubber drain on postoperative discomfort following lower third molar surgery. International Journal of Oral and Maxillofacial Surgery 2008;37(4):341-4. [DOI] [PubMed] [Google Scholar]
Danda 2010 {published data only}
- Danda AK, Krishna Tatiparthi M, Narayanan V, Siddareddi A. Influence of primary and secondary closure of surgical wound after impacted mandibular third molar removal on postoperative pain and swelling - a comparative and split mouth study. Journal of Oral and Maxillofacial Surgery 2010;68(2):309-12. [DOI] [PubMed] [Google Scholar]
de Brabander 1988 {published data only}
- Brabander EC, Cattaneo G. The effect of surgical drain together with a secondary closure technique on postoperative trismus, swelling and pain after mandibular third molar surgery. International Journal of Oral and Maxillofacial Surgery 1998;17(2):119-21. [DOI] [PubMed] [Google Scholar]
Dutta 2016 {published data only}
- Dutta SR, Passi D, Singh P, Sharma S, Singh M, Srivastava D. A randomized comparative prospective study of platelet-rich plasma, platelet-rich fibrin, and hydroxyapatite as a graft material for mandibular third molar extraction socket healing. National Journal of Maxillofacial Surgery 2016;7(1):45-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Erdogan 2011 {published and unpublished data}
- Erdogan O, Tatli U, Ustun Y, Damlar I. Influence of two different flap designs on the sequelae of mandibular third molar surgery. Oral and Maxillofacial Surgery 2011;15(3):147-52. [DOI] [PubMed] [Google Scholar]
Eshghpour 2014 {published data only}
- Eshghpour M, Dastmalchi P, Nekooei AH, Nejat A. Effect of platelet-rich fibrin on frequency of alveolar osteitis following mandibular third molar surgery: a double-blinded randomized clinical trial. Journal of Oral and Maxillofacial Surgery 2014;72(8):1463-7. [DOI] [PubMed] [Google Scholar]
Gargallo‐Albiol 2000 {published data only}
- Gargallo-Albiol J, Buenechea-Imaz R, Gay-Escoda C. Lingual nerve protection during surgical removal of lower third molars. A prospective randomised study. International Journal Oral and Maxillofacial Surgery 2000;29(4):268-71. [PubMed] [Google Scholar]
Gogulanathan 2015 {published data only}
- Gogulanathan M, Elavenil P, Gnanam A, Raja VB. Evaluation of fibrin sealant as a wound closure agent in mandibular third molar surgery - a prospective, randomized controlled clinical trial. International Journal of Oral and Maxillofacial Surgery 2015;44(7):871-5. [DOI] [PubMed] [Google Scholar]
Goldsmith 2012 {published and unpublished data}
- Goldsmith SM, De Silva RK, Tong DC, Love RM. Influence of a pedicle flap design on acute postoperative sequelae after lower third molar removal. International Journal of Oral and Maxillofacial Surgery 2012;41(3):371-5. [DOI] [PubMed] [Google Scholar]
Gomes 2005 {published data only}
- Gomes ACA, Vasconcelos BC, Oliveira e Silva ED, da Silva LC. Lingual nerve damage after mandibular third molar surgery: a randomised clinical trial. Journal of Oral and Maxillofacial Surgery 2005;63(10):1443-6. [DOI] [PubMed] [Google Scholar]
Greenwood 1994 {published and unpublished data}
- Greenwood M, Langton SG, Rood JP. A comparison of broad and narrow retractors for lingual nerve protection during lower third molar surgery. British Journal of Oral and Maxillofacial Surgery 1994;32(2):114-7. [DOI] [PubMed] [Google Scholar]
Gulsen 2017 {published data only}
- Gulsen U, Senturk MF. Effect of platelet rich fibrin on edema and pain following third molar surgery: a split mouth control study. BMC Oral Health 2017;17(1):79-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISRCTN16849867. Platelet rich fibrin effects on third molar surgery. IRCTN Registry. [DOI: 10.1186/ISRCTN16849867] [DOI]
Haraji 2010 {published data only}
- Haraji A, Motamedi MH, Rezvani F. Can flap design influence the incidence of alveolar osteitis following removal of impacted mandibular third molars? General Dentistry 2010;58(5):e187-9. [PubMed]
Hashemi 2012 {published data only}
- Hashemi HM, Beshkar M, Aghajani R. The effect of sutureless wound closure on postoperative pain and swelling after impacted mandibular third molar surgery. British Journal of Oral and Maxillofacial Surgery 2012;50(3):256-8. [DOI] [PubMed] [Google Scholar]
Kapse 2019 {published data only}
- Kapse S, Surana S, Satish M, Hussain SE, Vyas S, Thakur D. Autologous platelet-rich fibrin: can it secure a better healing? Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 2019;127:8-18. [DOI] [PubMed] [Google Scholar]
Kirk 2007 {published data only}
- Kirk DG, Liston PN, Tong DC, Love RM. Influence of two different flap designs on incidence of pain, swelling, trismus, and alveolar osteitis in the week following third molar surgery. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2007;104(1):e1-6. [DOI] [PubMed] [Google Scholar]
Koyuncu 2013 {published data only}
- Koyuncu BO, Cetingul E. Short-term clinical outcomes of two different flap techniques in impacted mandibular third molar surgery. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 2013;116(3):e179-84. [DOI] [PubMed] [Google Scholar]
Koyuncu 2015 {published data only}
- Koyuncu BO, Zeytinoglu M, Tetik A, Gomel MM. Effect of tube drainage compared with conventional suturing on postoperative discomfort after extraction of impacted mandibular third molars. British Journal of Oral & Maxillofacial Surgery 2015;53(1):63-7. [DOI] [PubMed] [Google Scholar]
Kumar 2015 {published data only}
- Kumar N, Prasad K, Ramanujam L, Ranganath R, Dexith J, Chauhan A. Evaluation of treatment outcome after impacted mandibular third molar surgery with the use of autologous platelet-rich fibrin: a randomized controlled clinical study. Journal of Oral and Maxillofacial Surgery 2015;73(6):1042-9. [DOI] [PubMed] [Google Scholar]
Kumar 2016 {published data only}
- Kumar YR, Mohanty S, Verma M, Kaur RR, Bhatia P, Kumar VR, et al. Platelet-rich fibrin: the benefits. Journal of Clinical and Diagnostic Research 2016;54(1):57-61. [DOI] [PubMed] [Google Scholar]
Leung 2009 {published and unpublished data}
- Leung YY, Cheung LK. Can coronectomy of wisdom teeth reduce the incidence of inferior dental nerve injury? Annals of the Royal Australasian College of Dental Surgeons 2008;19:50-1. [PubMed]
- Leung YY, Cheung LK. Coronectomy as the treatment of choice in wisdom teeth showing radiographic signs of close proximity to inferior dental nerve. Annals of the Royal Australasian College of Dental Surgeons 2010;20:93-4. [PubMed]
- Leung YY, Cheung LK. Safety of coronectomy versus excision of wisdom teeth: a randomized controlled trial. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2009;108(6):821-7. [DOI] [PubMed]
Mantovani 2014 {published data only}
- Mantovani E, Arduino PG, Schierano G, Ferrero L, Gallesio G, Mozzati M, et al. A split-mouth randomized clinical trial to evaluate the performance of piezosurgery compared with traditional technique in lower wisdom tooth removal. Journal of Oral and Maxillofacial Surgery 2014;72(10):1890-7. [DOI] [PubMed] [Google Scholar]
Mistry 2016 {published data only}
- Mistry FK, Hegde ND, Hegde MN. Postsurgical consequences in lower third molar surgical extraction using micromotor and piezosurgery. Annals of Maxillofacial Surgery 2016;6(2):251-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mobilio 2017 {published data only}
- Mobilio N, Vecchiatini R, Vasquez M, Calura G, Catapano S. Effect of flap design and duration of surgery on acute postoperative symptoms and signs after extraction of lower third molars: a randomized prospective study. Journal of Dental Research Dental Clinics Dental Prospects 2017;11(3):156-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mocan 1996 {published and unpublished data}
- Mocan A, Kisnisci R, Ucok C. Stereophotogrammetric and clinical evaluation of morbidity after removal of lower third molars by two different surgical techniques. Journal of Oral and Maxillofacial Surgery 1996;54(2):171-5. [DOI] [PubMed] [Google Scholar]
Mohajerani 2018 {published data only}
- Mohajerani H, Esmaeelinejad M, Jafari M, Amini E, Sharabiany SP. Comparison of envelope and modified triangular flaps on incidence of dry socket after surgical removal of impacted mandibular third molars: a double-blind, split-mouth study. Journal of Contemporary Dental Practice 2018;19(7):836-41. [PubMed] [Google Scholar]
Nageshwar 2002 {published and unpublished data}
- Nageshwar N. Comma incision for impacted mandibular third molars. Journal of Oral and Maxillofacial Surgery 2002;60(12):1506-9. [DOI] [PubMed] [Google Scholar]
Osunde 2011a {published data only}
- Osunde OD, Saheeb BD, Adebola RA. Comparative study of effect of single and multiple suture techniques on inflammatory complications after third molar surgery. Journal of Oral and Maxillofacial Surgery 2011;69:971-6. [DOI] [PubMed] [Google Scholar]
Osunde 2012 {published data only}
Ozgul 2015 {published data only}
- Ozgul O, Senses F, Er N, Tekin U, Tuz HH, Alkan A, et al. Efficacy of platelet rich fibrin in the reduction of the pain and swelling after impacted third molar surgery: randomized multicenter split-mouth clinical trial. Head & Face Medicine 2015;11:37-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pachipulusu 2018 {published data only}
- Pachipulusu PV, Manjula S. Comparative study of primary and secondary closure of the surgical wound after removal of impacted mandibular third molars. Oral and Maxillofacial Surgery 2018;2018(22):261–6. [DOI] [PubMed] [Google Scholar]
Pasqualini 2005 {published and unpublished data}
- Pasqualini D, Cocero N, Castella A, Mela L, Bracco P. Primary and secondary closure of the surgical wound after removal of impacted mandibular third molars: a comparative study. International Journal of Oral and Maxillofacial Surgery 2005;34(1):52-7. [DOI] [PubMed] [Google Scholar]
Piersanti 2014 {published data only}
- Piersanti L, Dilorenzo M, Monaco G, Marchetti C. Piezosurgery or conventional rotatory instruments for inferior third molar extractions? Journal of Oral and Maxillofacial Surgery 2014;72(9):1647-52. [DOI] [PubMed] [Google Scholar]
Praveen 2007 {published data only}
- Praveen G, Rajesh P, Neelakandan RS, Nandagopal CM. Comparison of morbidity following the removal of mandibular third molar by lingual split, surgical bur and simplified split bone technique. Indian Journal of Dental Research 2007;18(1):15-8. [DOI] [PubMed] [Google Scholar]
Rabi 2017 {published data only}
- Rabi A, Haris PMM, Panickal DM, Ahamed S, Pulikkottil VJ, Haris KTM. Comparative evaluation of two different flap designs and postoperative outcome in the surgical removal of impacted mandibular third molar. Journal of Contemporary Dental Practice 2017;18(9):807-11. [DOI] [PubMed] [Google Scholar]
Rakprasitkul 1997 {published data only}
- Rakprasitkul S, Pairuchvej V. Mandibular third molar surgery with primary closure with a drain. International Journal of Oral and Maxillofacial Surgery 1997;26(3):187-90. [DOI] [PubMed] [Google Scholar]
Refo'a 2011 {published data only}
- Refo'a Y, Ouatik N, Golchin F, Mahboobi N. Comparing primary and secondary wound healing discomfort after mandibular third molar surgery: a randomized, double-blind clinical trial. General Dentistry 2011;59(4):310-3. [PubMed]
Renton 2005 {published data only}
- Renton T, Hankins M, Sproate C, McGurk M. A randomised controlled clinical trial to compare the incidence of injury to the inferior alveolar nerve as a result of coronectomy and removal of mandibular third molars. British Journal of Oral and Maxillofacial Surgery 2005;43(1):7-12. [DOI] [PubMed] [Google Scholar]
Roode 2010 {published and unpublished data}
- Roode GJ, Butow K. An alternative surgical flap design for impacted third molars: a comparison of two different surgical techniques. South African Dental Association Journal 2010;65(6):246, 248-51. [PubMed] [Google Scholar]
Rullo 2013 {published data only}
- Rullo R, Addabbo F, Papaccio G, D'Aquino R, Festa VM. Piezoelectric device vs. conventional rotative instruments in impacted third molar surgery: relationships between surgical difficulty and postoperative pain with histological evaluations. Journal of Cranio-Maxillo-Facial Surgery 2013;41(2):e33-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Saglam 2003 {published data only}
- Saglam AA. Effects of tube drain with primary closure techniques on postoperative trismus and swelling after removal of fully impacted mandibular third molars. Quintessence International 2003;34(2):143-7. [PubMed] [Google Scholar]
Sandhu 2010 {published and unpublished data}
- Sandhu A, Sandhu S, Kaur T. Comparison of two different flap designs in the surgical removal of bilateral impacted mandibular third molars. International Journal of Oral and Maxillofacial Surgery 2010;39(11):1091-6. [DOI] [PubMed] [Google Scholar]
Shad 2015 {published data only}
- Shad S, Shah SM, Alamgir, Abbasi MM. Frequency of lingual nerve injury in mandibular third molar extraction: a comparison of two surgical techniques. Journal of Ayub Medical College, Abbottabad 2015;27(3):580-3. [PubMed] [Google Scholar]
Şimşek Kaya 2019 {published data only}
- Şimşek Kaya G, Yapıcı Yavuz G, Saruhan N. The influence of flap design on sequelae and quality of life following surgical removal of impacted mandibular third molars: a split-mouth randomized clinical trial. Journal of Oral Rehabilitation 2019;00:1-8. [DOI] [PubMed] [Google Scholar]
Singh 2018 {published data only}
- Singh K, Kumar S, Singh S, Mishra V, Sharma PK, Singh D. Impacted mandibular third molar: comparison of coronectomy with odontectomy. Indian Journal of Dental Research 2018;29(5):605-10. [DOI] [PubMed] [Google Scholar]
Srinivas 2006 {published data only}
- Srinivas DR. Effect of Surgical Tube Drain With Primary Closure Technique After Removal of Impacted Mandibular Third Molars - a Clinical Study (Dissertation). Karnataka, Bangalore, India: Rajiv Gandhi University of Health Sciences, 2006. [Google Scholar]
Sweet 1976 {published data only}
- Sweet JB, Butler MS, Drager JL. Effects of lavage techniques with third molar surgery. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology 1976;41(2):152-68. [DOI] [PubMed] [Google Scholar]
Topcu 2019 {published data only}
- Topcu SIK, Palancioglu A, Yaltirik M, Koray M. Piezoelectric surgery versus conventional osteotomy in impacted lower third molar extraction: evaluation of perioperative anxiety, pain, and paresthesia. Journal of Oral and Maxillofacial Surgery 2019;77:471-7. [DOI] [PubMed] [Google Scholar]
Unsal 2018 {published data only}
- Unsal H, Erbasar GNH. Evaluation of the effect of platelet-rich fibrin on the alveolar osteitis incidence and periodontal probing depth after extracting partially erupted mandibular third molars extraction. Nigerian Journal of Clinical Practice 2018;21(2):201-5. [DOI] [PubMed] [Google Scholar]
Uyanik 2015 {published data only}
- Uyanik LO, Bilginaylar K, Etikan I. Effects of platelet-rich fibrin and piezosurgery on impacted mandibular third molar surgery outcomes. Head & Face Medicine 2015;11:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Xavier 2008 {published data only}
- Xavier RL, Vasconcelos BC, Caubi AF, Porto GG, Maurette MA. Passive drainage through the vestibular oblique incision in impacted inferior third molar surgery: a preliminary study. Acta Odontologica Latinoamericana 2008;21(1):57-63. [PubMed]
References to studies excluded from this review
Abu‐Serriah 2004 {published data only}
- Abu-Serriah M, Critchlow H, Whitters CJ, Ayoub A. Removal of partially erupted third molars using an Erbium (Er):YAG laser: a randomised controlled clinical trial. British Journal of Oral and Maxillofacial Surgery 2004;42(3):203-8. [DOI] [PubMed] [Google Scholar]
Afat 2018 {published data only}
- Afat IM, Akdogan ET, Gonul O. Effects of leukocyte- and platelet-rich fibrin alone and combined with hyaluronic acid on pain, edema, and trismus after surgical extraction of impacted mandibular third molars. Journal of Oral and Maxillofacial Surgery 2018;76(5):926-32. [DOI] [PubMed] [Google Scholar]
Akota 1998 {published data only}
- Akota I, Alvsaker B, Bjørnland T. The effect of locally applied gauze drain impregnated with chlortetracycline ointment in mandibular third-molar surgery. Acta Odontologica Scandinavica 1998;56(1):25-9. [DOI] [PubMed] [Google Scholar]
Al‐Moraissi 2016 {published data only}
- Al-Moraissi EA, Elmansi YA, Al-Sharaee YA, Alrmali AE, Alkhutari AS. Does the piezoelectric surgical technique produce fewer postoperative sequelae after lower third molar surgery than conventional rotary instruments? A systematic review and meta analysis. International Journal of Oral and Maxillofacial Surgery 2016;45(3):383-91. [DOI] [PubMed] [Google Scholar]
Alqahtani 2017 {published data only}
- Alqahtani NA, Khaleelahmed S, Desai F. Evaluation of two flap designs on the mandibular second molar after third molar extractions. Journal of Oral and Maxillofacial Pathology 2017;21(2):317-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ayad 1995 {published data only}
- Ayad W, Jöhren P, Dieckmann J. Results of a comparative prospective randomized study of surgical removal of mandibular wisdom teeth with and without rubber drainage. Fortschritte der Kiefer- und Gesichts-chirurgie 1995;40:134-6. [PubMed] [Google Scholar]
Bilginaylar 2016 {published and unpublished data}
- Bilginaylar K, Uyanik LO. Evaluation of the effects of platelet-rich fibrin and piezosurgery on surgical outcomes after removal of impacted mandibular third molars. British Journal of Oral & Maxillofacial Surgery 2016;54(10):e99. [DOI: 10.1016/j.bjoms.2016.03.016] [DOI] [PubMed] [Google Scholar]
Cetinkaya 2009 {published data only}
- Cetinkaya BO, Sumer M, Tutkun F, Sandikci EO, Misir F. Influence of different suturing techniques on periodontal health of the adjacent second molars after extraction of impacted mandibular third molars. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2009;108(2):156-61. [DOI] [PubMed] [Google Scholar]
Chang 2015 {published data only}
- Chang HH, Lee MS, Hsu YC, Tsai SJ, Lin CP. Comparison of clinical parameters and environmental noise levels between regular surgery and piezosurgery for extraction of impacted third molars. Journal of the Formosan Medical Association 2015;114(10):929-35. [DOI] [PubMed] [Google Scholar]
Chen 2016 {published data only}
- Chen YW, Lee CT, Hum L, Chuang SK. Effect of flap design on periodontal healing after impacted third molar extraction: a systematic review and meta-analysis. International Journal of Oral and Maxillofacial Surgery 2016;46(3):363-72. [DOI] [PubMed] [Google Scholar]
Chossegros 2002 {published data only}
- Chossegros C, Guyot L, Cheynet F, Belloni D, Blanc JL. Is lingual nerve protection necessary for lower third molar germectomy? A prospective study of 300 procedures. International Journal of Oral and Maxillofacial Surgery 2002;31(6):620-4. [DOI] [PubMed] [Google Scholar]
- Thierry G, Chossegros C, Paris J, Guyot L, Cheynet F, Belloni D, et al. Should the lingual nerve be protected during germectomies? A prospective study of 300 procedures [Faut-il protéger le nerf lingual au cours des germectomies? Etude prospective à propos de 300 interventions]. Revue de Stomatologie et de Chirurgie Maxillo-Faciale 2001;102(6):299-303. [PubMed] [Google Scholar]
Clauser 1994 {published data only}
- Clauser C, Barone R. Effect of incision and flap reflection on postoperative pain after the removal of partially impacted mandibular third molars. Quintessence International 1994;25(12):845-9. [PubMed] [Google Scholar]
Cortell‐Ballester 2015 {published data only}
- Cortell-Ballester I, Figueiredo R, Valmaseda-Castellon E, Gay-Escoda C. Effects of collagen resorbable membrane placement after the surgical extraction of impacted lower third molars. Journal of Oral and Maxillofacial Surgery 2015;73(8):1457-64. [DOI] [PubMed] [Google Scholar]
de Carvalho 2015 {published data only}
- Carvalho RW, do Egito Vasconcelos BC. High weight standard and removal of third molars: a prospective randomised study. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 2015;120(5):554-61. [DOI] [PubMed] [Google Scholar]
Desai 2014 {published data only}
- Desai A, Patel R, Desai K, Vachhani NB, Shah KA, Sureja R. Comparison of two incision designs for surgical removal of impacted mandibular third molar: a randomised comparative clinical study. Contemporary Clinical Dentistry 2014;5(2):170-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ding 2000 {published data only}
- Ding L, Lu Q. The comparative study of high-speed air turbine handpiece and traditional chisel applying in extraction of impacted mandibular third molars. Chinese Journal of Stomatology 2000;20(3):133-4. [Google Scholar]
Dubois 1982 {published data only}
- Dubois DD, Pizer ME, Chinnis RJ. Comparison of primary and secondary closure techniques after removal of impacted mandibular third molars. Journal of Oral and Maxillofacial Surgery 1982;40(10):631-4. [DOI] [PubMed] [Google Scholar]
Dutta 2015 {published data only}
- Dutta SR, Singh P, Passi D, Patter P. Mandibular third molar extraction wound healing with and without platelet rich plasma: a comparative prospective study. Journal of Maxillofacial and Oral Surgery 2015;14(3):808-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Egbor 2014 {published data only}
- Egbor PE, Saheeb BD. A prospective randomized clinical study of the influence of primary closure or dressing on post-operative morbidity after mandibular third molar surgery. Nigerian Journal of Surgery 2014;20(2):59-63. [www.ajol.info/index.php/njs/article/view/106844/96760] [DOI] [PMC free article] [PubMed] [Google Scholar]
Elo 2016 {published data only}
- Elo JA, Sun HH, Dong F, Tandon R, Singh HM. Novel incision design and primary flap closure reduces the incidence of alveolar osteitis and infection in impacted mandibular third molar surgery. Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology 2016;122(2):124-33. [DOI] [PubMed] [Google Scholar]
Eshghpour 2018 {published data only}
- Eshghpour M, Danaeifar N, Kermani H, Nejat AH. Does intra-alveolar application of chlorhexidine gel in combination with platelet-rich fibrin have an advantage over application of platelet-rich fibrin in decreasing alveolar osteitis after mandibular third molar surgery? A double-blinded randomized clinical trial. Journal of Oral and Maxillofacial Surgery 2018;76(5):939.e1-7. [DOI] [PubMed] [Google Scholar]
Finne 1981 {published data only}
Gao 2011 {published data only}
- Gao Y, Jiang A, Li B, Yang L. Comparison of piezosurgery and chisel osteotomy in the extraction of mandibular impacted third molars. Huaxi Kongqiang Yixue Zazhi [West China Journal of Stomatology] 2011;29(4):372-4. [PubMed] [Google Scholar]
Gawai 2015 {published data only}
- Gawai KT, Sobhana CR. Clinical evaluation of use of platelet rich plasma in bone healing. Journal of Maxillofacial and Oral Surgery 2015;14(1):67-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gay‐Escoda 2015 {published data only}
- Gay-Escoda C, Gomez-Santos L, Sanchez-Torres A, Herraez-Vilas JM. Effect of the suture technique on postoperative pain, swelling and trismus after removal of lower third molars: a randomized clinical trial. Medicina Oral, Patologia Oral y Cirugia Bucal 2015;20(3):e372-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gazivoda 2015 {published data only}
- Gazivoda D, Pelemis D, Vujaskovic G. A clinical study on the influence of suturing material on oral wound healing. Journal of Maxillofacial and Oral Surgery 2015;72(9):765-9. [DOI] [PubMed] [Google Scholar]
Genu 2008 {published data only}
- Genu PR, Vasconcelos BCE. Influence of the tooth section technique in alveolar nerve damage after surgery of impacted lower third molars. International Journal of Oral and Maxillofacial Surgery 2008;37(10):923-8. [DOI] [PubMed] [Google Scholar]
Gonzalez 2001 {published data only}
- Gonzalez MT, Medina AS, Mendoza AS, Milina RP, Sanchez FN, Canacho LS. Comparative study of surgery (scalpel vs electro surgery) of impacted inferior third molars (Abstract FDI World Dental Congress). International Dental Journal 2001;51(5):380. [Google Scholar]
Goyal 2012 {published data only}
- Goyal M, Marya K, Jhamb A, Chawla S, Sonoo PR, Singh V. Comparative evaluation of surgical outcome after removal of impacted mandibular third molars using a Piezotome or a conventional handpiece: a prospective study. British Journal of Oral and Maxillofacial Surgery 2012;50(6):556-61. [DOI] [PubMed] [Google Scholar]
Guo 2012 {published data only}
- Guo ZZ, Zhang H, Li Y, Li X, Liu Y, Wang Y, et al. Comparative study of complications among routine method, high speed turbine handpiece and piezosurgery device after extraction of impacted wisdom teeth. Shanghai Journal of Stomatology 2012;21(2):208-10. [PubMed] [Google Scholar]
He 2015 {published data only}
- He JQ, Ouyang KX, Zhang QB, Zhou M, Yang ZN, Piao ZG. Comparison of two different flap designs in removal of impacted wisdom tooth. Shanghai Kou Qiang Yi Xue 2015;24(2):224-7. [PubMed] [Google Scholar]
Holland 1984 {published data only}
- Holland CS, Hindle MO. The influence of closure or dressing of third molar sockets on post-operative swelling and pain. British Journal of Oral and Maxillofacial Surgery 1984;22(1):65-71. [DOI] [PubMed] [Google Scholar]
Jain 2016 {published data only}
- Jain N, Thomas S, Prabhu S, Jain S, Pathak AD, Pillai A, et al. Influence of tooth sectioning technique and various risk factors in reducing the IAN injury following surgical removal of an impacted mandibular third molar. Oral and Maxillofacial Surgery 2016;20(2):149-56. [DOI] [PubMed] [Google Scholar]
Jakse 2002 {published data only}
- Jakse N, Bankaoglu V, Eskici A, Pertl C. Wound healing without complications after removal of lower wisdom teeth using a modified incision. Deutsche Zahnarztliche Zeitschrift 2001;56 Suppl:S8-9. [Google Scholar]
- Jakse N, Bankaoglu V, Wimmer G, Eskici A, Pertl C. Primary wound healing after lower third molar surgery: evaluation of 2 different flap designs. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2002;93(1):7-12. [DOI] [PubMed] [Google Scholar]
Jiang 2015 {published data only}
- Jiang Q, Qiu Y, Yang C, Yang J, Chen M, Zhang Z. Piezoelectric versus conventional rotary techniques for impacted third molar extraction: a meta-analysis of randomized controlled trials. Medicine 2015;94(41):e1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kerdvongbundit 1989 {published data only}
- Kerdvongbundit V, Sirirat M, Vechakarnvithaya A. The effect of two flap designs for the removal of the impacted mandibular third molar on the periodontal status of the mandibular second molar. Mahidol Dental Journal 1989;9(3):141-50.
Korkmaz 2015 {published data only}
- Korkmaz YT, Mollaoglu N, Ozmeric N. Does laterally rotated flap design influence the short-term periodontal status of second molars and postoperative discomfort after partially impacted third molar surgery? Journal of Oral and Maxillofacial Surgery 2015;73(6):1031-41. [DOI] [PubMed] [Google Scholar]
Li 2012 {published data only}
- Li S, Li C, Wu Y, Pan J, Zhao H, Li L. Drainage for the control of complications after extraction of impacted mandibular third molar: a systematic review. Huaxi Kongqiang Yixue Zazhi [West China Journal of Stomatology] 2012;30(6):615-9. [PubMed] [Google Scholar]
Li 2014 {published data only}
- Li D, Wei Z, Zhang W, Li Z. Crown cutting mode selection in extracting the mandible third molar by dental drilling system. Chinese Journal of Stomatology 2014;49(9):521-4. [PubMed] [Google Scholar]
Ma 2015 {published data only}
- Ma Z, Xu G, Yang C, Xie Q, Shen Y, Zhang S. Efficacy of the technique of piezoelectric corticotomy for orthodontic traction of impacted mandibular third molars. British Journal of Oral and Maxillofacial Surgery 2015;53(4):326-31. [DOI] [PubMed] [Google Scholar]
Martin 2015 {published data only}
- Martin A, Perinetti G, Costantinides F, Maglione M. Coronectomy as a surgical approach to impacted mandibular third molars: a systematic review. Head & Face Medicine 2015;11(1):9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mavrodi 2015 {published data only}
- Mavrodi A, Ohanyan A, Kechagias N, Tsekos A, Vahtsevanos K. Influence of two different surgical techniques on the difficulty of impacted lower third molar extraction and their post-operative complications. Medicina Oral, Patologia Oral y Cirugia Bucal 2015;20(5):e640-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Oyri 2016 {published data only}
- Oyri H, Bjornland T, Barkvoll P, Jensen JL. Mandibular third molar surgery in 396 patients at a Norwegian university clinic: morbidity recorded after 1 week utilizing an e-infrastructure for clinical research. Acta Odontologica Scandinavica 2016;74(2):148-54. [DOI] [PubMed] [Google Scholar]
Quee 1985 {published data only}
Robinson 1996 {published data only}
- Robinson PP, Smith KG. Lingual nerve damage during lower third molar removal: a comparison of two surgical methods. British Dental Journal 1996;180(12):456-61. [DOI] [PubMed] [Google Scholar]
Rosa 2002 {published data only}
- Rosa AL, Carneiro MG, Lavrador MA, Novaes AB Jr. Influence of flap design on periodontal healing of second molars after extraction of impacted mandibular third molars. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2002;93(4):404-7. [DOI] [PubMed] [Google Scholar]
Sala‐Perez 2016 {published data only}
- Sala-Perez S, Lopez-Ramirez M, Quinteros-Borgarello M, Valmaseda-Castellon E, Gay-Escoda C. Antibacterial suture vs silk for the surgical removal of impacted lower third molars. A randomized clinical study. Medicina Oral, Patologia Oral y Cirugia Bucal 2016;21(1):e95-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
Salentijn 2011 {published data only}
- Salentijn EG, Forouzanfar T. Effect of ice compression on pain after mandibular third molar surgery: a single blind randomized controlled trial. International Journal of Oral and Maxillofacial Surgery 2011;40(10):1100. [DOI] [PubMed] [Google Scholar]
Sener 2015 {published data only}
- Sener I, Metin M, Bereket C, Tek M, Arici S, Alkan A. Effects of different local haemostatic agents on facial swelling after the third molar surgery. Journal of Experimental and Clinical Medicine 2015;32(1):7-11. [Google Scholar]
Shevel 2001 {published data only}
- Shevel E, Koepp WG, Butow K-W. A subjective assessment of pain and swelling following the surgical removal of impacted third molar teeth using different surgical techniques. South African Dental Journal 2001;56(5):238-41. [PubMed] [Google Scholar]
Sivolella 2011 {published data only}
- Sivolella S, Berengo M, Bressan E, Di Fiore A, Stellini E. Osteotomy for lower third molar germectomy: randomized prospective crossover clinical study comparing piezosurgery and conventional rotatory osteotomy. Journal of Oral and Maxillofacial Surgery 2011;69:e15-23. [DOI] [PubMed] [Google Scholar]
Smith 2000 {published data only}
- Smith K. Lingual nerve protection during the removal of lower third molars not necessary. Evidence-Based Dentistry 2000;2(4):92. [Google Scholar]
Sortino 2008 {published data only}
Strukmeier 1980 {published data only}
- Strukmeier A, Pape HD. Comparative studies on the vestibular and lingual osteotomy in the removal of lower wisdom teeth [Vergleichende untersuchungen zur vestibularen und lingualen osteotomie bei der entfernung unterer weisheitszahne]. Deutsche Zahnarztlische Zeitschrift 1980;35:124-7. [PubMed] [Google Scholar]
Suarez‐Cunqueiro 2003 {published data only}
- Suarez-Cunqueiro MM, Gutwald R, Richman J, Otero-Cepeda XL, Schmelzeisen R. Marginal flap versus paramarginal flap in impacted third molar surgery: a prospective study. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2003;95(4):403-8. [DOI] [PubMed] [Google Scholar]
Suddhasthira 1991 {published data only}
- Suddhasthira T, Chaiwat S, Sattapongsda P. The comparative study of primary and secondary closure techniques after removal of impacted lower third molars. Thai Journal of Oral Maxillofacial Surgery 1991;5:67-73. [Google Scholar]
Sun 2009 {published data only}
- Sun G, Dang H, Zhao YG, Zhang YD, Qian J, Cui H. Comparative study of extraction of impacted wisdom teeth assisted by micro-dynamic systems and turbines. China Journal of Oral & Maxillofacial Surgery 2009;7(5):468-9. [Google Scholar]
Sweet 1978 {published data only}
- Sweet JB, Butler B. Predisposing and operative factors: effect on the incidence of localized osteitis in mandibular third-molar surgery. Oral Surgery 1978;46(2):206-15. [DOI] [PubMed] [Google Scholar]
Tabrizi 2014 {published data only}
- Tabrizi R, Khorshidi H, Shahidi S, Gholami M, Kalbasi S, Khayati A. Use of lincomycin-impregnated demineralized freeze-dried bone allograft in the periodontal defect after third molar surgery. Journal of Oral and Maxillofacial Surgery 2014;72(5):850-7. [DOI] [PubMed] [Google Scholar]
Tan 2015 {published data only}
- Tan S, Lynham A. Efficacy of cold saline irrigation on reducing post operative complications of third molar extraction. International Journal of Oral and Maxillofacial Surgery 2015;44:e150. [Google Scholar]
Torres‐Lagares 2006a {published data only}
- Torres-Lagares D, Infante-Cossio P, Gutierrez-Perez JL, Romero-Ruiz MM, Garcia-Calderon M, Serrera-Figallo MA. Intra-alveolar chlorhexidine gel for the prevention of dry socket in mandibular third molar surgery. A pilot study [Gel de Clorhexidina intra-alveolar en la prevención de la alveolitis tras la extracción de terceros molares inferiores. Estudio piloto]. Medicina Oral, Patología Oral y Cirugía Bucal 2006;11(2):113-8. [PubMed] [Google Scholar]
Torres‐Lagares 2006b {published data only}
- Torres-Lagares D, Gutierrez-Perez JL, Infante-Cossio P, Garcia-Calderon M, Romero-Ruiz MM, Serrera-Figallo MA. Randomized, double-blind study on effectiveness of intra-alveolar chlorhexidine gel in reducing the incidence of alveolar osteitis in mandibular third molar surgery. International Journal of Oral and Maxillofacial Surgery 2006;35(4):348-51. [DOI] [PubMed] [Google Scholar]
Tuffin 1990 {published data only}
- Tuffin JR, Cunliffe DR, Begg R, Shaw SR. Does bupivacaine irrigation of third molar sockets reduce postoperative pain? A double blind controlled trial. British Journal of Oral and Maxillofacial Surgery 1990;28(2):96-8. [DOI] [PubMed] [Google Scholar]
Yang 2015 {published data only}
- Yang YY, Du SN, Lv ZK. Evaluation of the results of high-speed handpiece and minimally invasive extraction in impacted mandibular third molar extraction. Shanghai Journal of Stomatology 2015;24(4):489-92. [PubMed] [Google Scholar]
Yolcu 2015 {published data only}
- Yolcu U, Acar AH. Comparison of a new flap design with the routinely used triangular flap design in third molar surgery. International Journal of Oral and Maxillofacial Surgery 2015;44(11):1390-7. [DOI] [PubMed] [Google Scholar]
Zhang 1997 {published data only}
- Zhang BX, Wang EG, Shu ZQ, Huang LZ, Shi H. Removal of wisdom teeth by using microwave heat coagulator. Journal of PLA Medical College 1997;25(1):44-6.
Zhou 2016 {published data only}
- Zhou J, Hu B, Liu Y, Yang Z, Song J. The efficacy of intra-alveolar 0.2% chlorhexidine gel on alveolar osteitis: a meta-analysis. Oral Diseases 2016;23(5):598-608. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Kumar 2013 {published data only}
- Kumar SB, Sarumathi T, Veerabahu M, Raman U. Study of comparison of flap designs - comma incision versus standard incision in impacted third molar surgery. Journal of Clinical and Diagnostic Research 2013;7(7):1514-8. [DOI: 10.7860/JCDR/2013/6200.3135] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ozveri Koyuncu 2013 {published data only}
- Özverí Koyuncu B, Zeytínoğlu M, Çetíngül E. Comparison of 2 different flap techniques in the surgical removal of bilateral impacted mandibular third molars. Turkish Journal of Medical Sciences 2013;43:891-8. [Google Scholar]
References to ongoing studies
ChiCTR‐ICR‐15006182 {published data only}
- ChiCTR-ICR-15006182. Posterior-triangle flap: a new flap design for impacted mandibular third molars. www.chictr.org.cn/showprojen.aspx?proj=10696.
IRCT2014052017781N1 {published data only}
- IRCT2014052017781N1. Compare of influence different two suture techniques on periodontal health of the mandibular second molars after extraction of impact third molar. Iranian Registry of Clinical Trials 2014.
IRCT2014052717863N2 {published data only}
- IRCT2014052717863N2. Evaluation of side effects of two types of flap after impacted mandibular third molar surgery. Iranian Registry of Clinical Trials 2014.
IRCT2015050722139N1 {published data only}
- IRCT2015050722139N1. Tissue adhesives for surgical wound closures. Iranian Registry of Clinical Trials 2015.
IRCT201506191760N42 {published data only}
- IRCT201506191760N42. The effect of releasing (relaxing) incision on the postoperative complication of mandibular third molar surgery. Iranian Registry of Clinical Trials 2015.
ISRCTN16849867 {published data only}
- ISRCTN16849867. Platelet rich fibrin effects on third molar surgery. IRCTN Registry. [DOI: 10.1186/ISRCTN16849867] [DOI]
NCT02495207 {published data only}
- NCT02495207. A comparison between conventional surgery and piezosurgery. ClinicalTrials.gov 2016.
NCT02831374 {published data only}
- NCT02831374. Effectiveness of platelet rich plasma in wound healing. ClinicalTrials.gov 2016.
NCT02942108 {published data only}
- NCT02942108. Piezoelectric vibrations and tissue, cellular and molecular mechanisms of oral wound healing after third molar surgery. ClinicalTrials.gov 2016.
Additional references
Bailey 2013
- Bailey E, Worthington HV, Wijk A, Yates JM, Coulthard P, Afzal Z. Ibuprofen and/or paracetamol (acetaminophen) for pain relief after surgical removal of lower wisdom teeth. Cochrane Database of Systematic Reviews 2013, Issue 12. Art. No: CD004624. [DOI: 10.1002/14651858.CD004624.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Beech 2017
- Beech AN, Haworth S, Knepil GJ. Measurement of generic compared with disease-specific quality of life after removal of mandibular third molars: a patient-centred evaluation. British Journal of Oral Maxillofacial Surgery 2017;55(3):274-80. [DOI] [PubMed] [Google Scholar]
Bodner 1998
- Bodner L, Weinstein JM, Baumgarten AK. Efficacy of fibrin sealant in patients on various levels of oral anticoagulant undergoing oral surgery. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 1998;86(4):421-4. [DOI] [PubMed] [Google Scholar]
Carrasco‐Labra 2012
- Carrasco-Labra A, Brignardello-Petersen R, Yanine N, Araya I, Guyatt G. Secondary versus primary closure techniques for the prevention of postoperative complications following removal of impacted mandibular third molars: a systematic review and meta-analysis of randomized controlled trials. Journal of Oral and Maxillofacial Surgery 2012;70(8):e441-57. [DOI] [PubMed] [Google Scholar]
Chen 2017
- Chen Y-W, Lee C-T, Hum L, Chuang S-K. Effect of flap design on periodontal healing after impacted third molar extraction: a systematic review and meta-analysis. International Journal of Oral and Maxillofacial Surgery 2017;46(3):363-72. [DOI] [PubMed] [Google Scholar]
Cheung 2010
- Cheung LK, Leung YY, Chow LK, Wong MC, Chan EK, Fok YH. Incidence of neurosensory deficits and recovery after lower third molar surgery: a prospective clinical study of 4338 cases. International Journal of Oral and Maxillofacial Surgery 2010;39(4):320-6. [DOI] [PubMed] [Google Scholar]
Chiapasco 1993
- Chiapasco M, De Cicco L, Marrone G. Side effects and complications associated with third molar surgery. Oral Surgery, Oral Medicine, and Oral Pathology 1993;76:412-20. [DOI] [PubMed] [Google Scholar]
Choukroun 2006
- Choukroun J, Diss A, Simonpieri MO, Girard C, Schoeffler SL, Dohan AJ, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV: clinical effects on tissue healing. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2006;101(3):e56-60. [DOI] [PubMed] [Google Scholar]
Colorado‐Bonnin 2006
- Colorado-Bonnin M, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C. Quality of life following lower third molar removal. International Journal of Oral and Maxillofacial Surgery 2006;35(4):343-7. [DOI] [PubMed] [Google Scholar]
Conrad 1999
- Conrad SM, Blakey GH, Shugars DA, Marciani RD, Phillips C, White RP Jr. Patients' perception of recovery after third molar surgery. Journal of Oral and Maxillofacial Surgery 1999;57(11):1288-94. [DOI] [PubMed] [Google Scholar]
Covidence [Computer program]
- Veritas Health Innovation Covidence. Version accessed 1 April 2018. Melbourne, Australia: Veritas Health Innovation. Available at covidence.org.
Curtin 2002
- Curtin F, Elbourne D, Altman DG. Meta-analysis combining parallel and cross-over clinical trials. II: Binary outcomes. Statistics in Medicine 2002;21(15):2145-59. [DOI] [PubMed] [Google Scholar]
Degerliyurt 2009
- Degerliyurt K, Akar V, Denizci S, Yucel E. Bone lid technique with piezosurgery to preserve inferior alveolar nerve. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 2009;108(6):e1-5. [DOI] [PubMed] [Google Scholar]
Dohan 2006
- Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2006;101(3):e37-44. [DOI] [PubMed] [Google Scholar]
Goldberg 1985
- Goldberg MH, Nemarich AN, Marco WP Jr. Complications after mandibular third molar surgery: a statistical analysis of 500 consecutive procedures in private practice. Journal of the American Dental Association 1985;111(2):277-9. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime) GRADEpro GDT. Version accessed 1 May 2019. Hamilton (ON): McMaster University (developed by Evidence Prime).
Higgins 2011
- Higgins JPT, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hillerup 2007
- Hillerup S. Iatrogenic injury to oral branches of the trigeminal nerve: records of 449 cases. Clinical Oral Investigation 2007;11(2):133-42. [DOI] [PubMed] [Google Scholar]
Jones 1992
- Jones RH. Microsurgical repair of nerves injures during third molar surgery. Australian Dental Journal 1992;37:253-61. [DOI] [PubMed] [Google Scholar]
Jowett 2016
- Jowett A, Mansoor J, Coulthard P. The coronectomy technique for lower third molars: past and present. Oral Surgery 2016;9:150-4. [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Leung 2018
- Leung YY, Cheung KY. Root migration pattern after third molar coronectomy: a long-term analysis. International Journal of Oral and Maxillofacial Surgery 2018;47(6):802-8. [DOI] [PubMed] [Google Scholar]
Libersa 2002
- Libersa P, Roze D, Cachart T, Libersa JC. Immediate and late mandibular fractures after third molar removal. Journal of Oral and Maxillofacial Surgery 2002;60(2):163-5. [DOI] [PubMed] [Google Scholar]
Long 2012
- Long H, Zhou Y, Liao L, Pyakurel U, Wang Y, Lai W. Coronectomy vs. total removal for third molar extraction: a systematic review. Journal of Dental Research 2012;91(7):659-65. [DOI] [PubMed] [Google Scholar]
Mason 1988
- Mason DA. Lingual nerve damage following lower third molar surgery. International Journal of Oral and Maxillofacial Surgery 1988;17:290-4. [DOI] [PubMed] [Google Scholar]
McArdle 2012
- McArdle LW, Renton T. The effects of NICE guidelines on the management of third molar teeth. British Dental Journal 2012;213(5):E8. [PMID: ] [DOI] [PubMed] [Google Scholar]
McArdle 2018a
- McArdle LW, Patel N, Jones J, McDonald F. The mesially impacted mandibular third molar: the incidence and consequences of distal cervical caries in the mandibular second molar. Surgeon 2018;16(2):67-73. [DOI] [PubMed] [Google Scholar]
McArdle 2018b
- McArdle LW, Andiappan M, Khan I, Jones J, McDonald F. Diseases associated with mandibular third molar teeth. British Dental Journal 2018;224(6):434-40. [DOI] [PubMed] [Google Scholar]
Miron 2017
- Miron RJ, Fujioka-Kobayashi M, Bishara M, Zhang Y, Hernandez M, Choukroun J. Platelet-rich fibrin and soft tissue wound healing: a systematic review. Tissue Engineering. Part B, Reviews 2017;23(1):83-99. [DOI] [PubMed] [Google Scholar]
Moore 2015
- Moore RA, Derry S, Wiffen PJ, Straube S, Aldington DJ. Overview review: Comparative efficacy of oral ibuprofen and paracetamol (acetaminophen) across acute and chronic pain conditions. European Journal of Pain 2015;19(9):1213-23. [DOI] [PubMed] [Google Scholar]
Muhonen 1997
- Muhonen A, Venta I, Ylipaavalniemi P. Factors predisposing to postoperative complications related to wisdom tooth surgery among university students. Journal of the American College of Health 1997;46(1):39-42. [DOI] [PubMed] [Google Scholar]
Osunde 2011b
- Osunde OD, Adebola RA, Omeje UK. Management of inflammatory complications in third molar surgery: a review of the literature. African Health Sciences 2011;11(3):530-7. [PMC free article] [PubMed] [Google Scholar]
Parthasarathi 2011
- Parthasarathi K, Smith A, Chandu A. Factors affecting incidence of dry socket: a prospective community-based study. Journal of Oral and Maxillofacial Surgery 2011;69(7):1880-4. [DOI] [PubMed] [Google Scholar]
Pedersen 2018
- Pedersen MH, Bak J, Matzen LH, Hartlev J, Bindslev J, Schou S, et al. Coronectomy of mandibular third molars: a clinical and radiological study of 231 cases with a mean follow-up period of 5.7 years. International Journal of Oral and Maxillofacial Surgery 2018;47(12):1596-603. [DOI] [PubMed] [Google Scholar]
Pell 1933
- Pell GJ, Gregory GT. Impacted mandibular third molars: classification and modified technique for removal. Dental Digest 1933;39:330-8. [Google Scholar]
Pichler 2001
- Pichler JW, Ross Beirne O. Lingual flap retraction and prevention of lingual nerve damage associated with third molar surgery: a systematic review of the literature. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 2001;91:395-401. [DOI] [PubMed] [Google Scholar]
Renton 2001
- Renton T, McGurk M. Evaluation of factors predictive of lingual nerve injury in third molar surgery. British Journal of Oral and Maxillofacial Surgery 2001;39(6):423-8. [DOI] [PubMed] [Google Scholar]
Renton 2012
- Renton T. Notes on coronectomy. British Dental Journal 2012;212(7):323. [DOI] [PubMed] [Google Scholar]
RevMan [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.4. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2020.
Rood 1983
- Rood JP. Lingual split technique. Damage to inferior alveolar and lingual nerves during removal of impacted third molars. British Dental Journal 1983;154:402-3. [DOI] [PubMed] [Google Scholar]
Rood 1990
- Rood JP, Shehab BN. The radiological prediction of inferior alveolar nerve injury during third molar surgery. British Journal of Oral and Maxillofacial Surgery 1990;28(1):20-5. [DOI] [PubMed] [Google Scholar]
Rood 1992
- Rood JP. Permanent damage to inferior alveolar and lingual nerves during the removal of impacted mandibular third molars. Comparison of two methods of bone removal. British Dental Journal 1992;172:108-10. [DOI] [PubMed] [Google Scholar]
Savin 1997
- Savin J, Ogden GR. Third molar surgery - a preliminary report on aspects affecting quality of life in the early postoperative period. British Journal of Oral and Maxillofacial Surgery 1997;35(4):246-53. [DOI] [PubMed] [Google Scholar]
Schultze‐Mosgau 1993
- Schultze-Mosgau S, Reich RH. Assessment of inferior alveolar and lingual nerve disturbances after dentoalveolar surgery, and recovery of sensitivity. International Journal of Oral and Maxillofacial Surgery 1993;22:214-7. [DOI] [PubMed] [Google Scholar]
Smith 1997
- Smith AC, Barry S, Chiong A. Inferior alveolar nerve damage following removal of mandibular third molar teeth. A prospective study using panoramic radiography. Australian Dental Journal 1997;42:149-52. [DOI] [PubMed] [Google Scholar]
Stedman 2011
- Stedman MR, Curtin F, Elbourne DR, Kesselheim AS, Brookhart MA. Meta-analyses involving cross-over trials: methodological issues. International Journal of Epidemiology 2011;40(6):1732-4. [DOI] [PubMed] [Google Scholar]
Steel 2012
- Steel B. Lingual split versus surgical bur technique in the extraction of impacted mandibular third molars: a systematic review. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics 2012;114(3):294-302. [PMID: ] [DOI] [PubMed] [Google Scholar]
Toedtling 2016
- Toedtling V, Coulthard P, Thackray GJ. Distal caries of the second molar in the presence of a mandibular third molar - a prevention protocol. British Dental Journal 2016;221(6):297. [DOI] [PubMed] [Google Scholar]
Van Wijk 2007
- Wijk A, Kieffer JM, Lindeboom JH. Effect of third molar surgery on oral health-related quality of life in the first postoperative week using Dutch version of Oral Health Impact Profile. Journal of Oral and Maxillofacial Surgery 2009;67(5):1026-31. [DOI] [PubMed] [Google Scholar]
Waite 2006
- Waite PD, Cherala S. Surgical outcomes for suture-less surgery in 366 impacted third molar patients. Journal of Oral and Maxillofacial Surgery 2006;64(4):669-73. [DOI] [PubMed] [Google Scholar]
Ward 1956
- Ward TG. The split bone technique for removal of lower third molars. British Dental Journal 1956;101:297-304. [Google Scholar]
Worthington 2015
- Worthington H, Clarkson J, Weldon J. Priority oral health research identification for clinical decision-making. Evidence-Based Dentistry 2015;16(3):69-71. [DOI] [PubMed] [Google Scholar]
Zhu 2020
- Zhu J, Yuan X, Yan L, Li T, Guang M, Zhang Y. Comparison of postoperative outcomes between envelope and triangular flaps after mandibular third molar surgery: a systematic review and meta-analysis. Journal of Oral and Maxillofacial Surgery 2020;78:515-27. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Coulthard 2003
- Coulthard P, Esposito M, Renton TF, Worthington HV. Surgical techniques for the removal of mandibular wisdom teeth. Cochrane Database of Systematic Reviews 2003, Issue 3. Art. No: CD004345. [DOI: 10.1002/14651858.CD004345] [DOI] [PubMed] [Google Scholar]
Coulthard 2014
- Coulthard P, Bailey E, Esposito M, Furness S, Renton TF, Worthington HV. Surgical techniques for the removal of mandibular wisdom teeth. Cochrane Database of Systematic Reviews 2014, Issue 7. Art. No: CD004345. [DOI: 10.1002/14651858.CD004345.pub2] [DOI] [PubMed] [Google Scholar]


