Abstract
Background
Risks of stillbirth or neonatal death increase as gestation continues beyond term (around 40 weeks' gestation). It is unclear whether a policy of labour induction can reduce these risks. This Cochrane Review is an update of a review that was originally published in 2006 and subsequently updated in 2012 and 2018.
Objectives
To assess the effects of a policy of labour induction at or beyond 37 weeks' gestation compared with a policy of awaiting spontaneous labour indefinitely (or until a later gestational age, or until a maternal or fetal indication for induction of labour arises) on pregnancy outcomes for the infant and the mother.
Search methods
For this update, we searched Cochrane Pregnancy and Childbirth’s Trials Register, ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform (ICTRP) (17 July 2019), and reference lists of retrieved studies.
Selection criteria
Randomised controlled trials (RCTs) conducted in pregnant women at or beyond 37 weeks, comparing a policy of labour induction with a policy of awaiting spontaneous onset of labour (expectant management). We also included trials published in abstract form only. Cluster‐RCTs, quasi‐RCTs and trials using a cross‐over design were not eligible for inclusion in this review.
We included pregnant women at or beyond 37 weeks' gestation. Since risk factors at this stage of pregnancy would normally require intervention, only trials including women at low risk for complications, as defined by trialists, were eligible. The trials of induction of labour in women with prelabour rupture of membranes at or beyond term were not considered in this review but are considered in a separate Cochrane Review.
Data collection and analysis
Two review authors independently assessed trials for inclusion, assessed risk of bias and extracted data. Data were checked for accuracy. We assessed the certainty of evidence using the GRADE approach.
Main results
In this updated review, we included 34 RCTs (reporting on over 21,000 women and infants) mostly conducted in high‐income settings. The trials compared a policy to induce labour usually after 41 completed weeks of gestation (> 287 days) with waiting for labour to start and/or waiting for a period before inducing labour. The trials were generally at low to moderate risk of bias.
Compared with a policy of expectant management, a policy of labour induction was associated with fewer (all‐cause) perinatal deaths (risk ratio (RR) 0.31, 95% confidence interval (CI) 0.15 to 0.64; 22 trials, 18,795 infants; high‐certainty evidence). There were four perinatal deaths in the labour induction policy group compared with 25 perinatal deaths in the expectant management group. The number needed to treat for an additional beneficial outcome (NNTB) with induction of labour, in order to prevent one perinatal death, was 544 (95% CI 441 to 1042). There were also fewer stillbirths in the induction group (RR 0.30, 95% CI 0.12 to 0.75; 22 trials, 18,795 infants; high‐certainty evidence); two in the induction policy group and 16 in the expectant management group.
For women in the policy of induction arms of trials, there were probably fewer caesarean sections compared with expectant management (RR 0.90, 95% CI 0.85 to 0.95; 31 trials, 21,030 women; moderate‐certainty evidence); and probably little or no difference in operative vaginal births with induction (RR 1.03, 95% CI 0.96 to 1.10; 22 trials, 18,584 women; moderate‐certainty evidence). Induction may make little or difference to perineal trauma (severe perineal tear: RR 1.04, 95% CI 0.85 to 1.26; 5 trials; 11,589 women; low‐certainty evidence). Induction probably makes little or no difference to postpartum haemorrhage (RR 1.02, 95% CI 0.91 to 1.15, 9 trials; 12,609 women; moderate‐certainty evidence), or breastfeeding at discharge (RR 1.00, 95% CI 0.96 to 1.04; 2 trials, 7487 women; moderate‐certainty evidence). Very low certainty evidence means that we are uncertain about the effect of induction or expectant management on the length of maternal hospital stay (average mean difference (MD) ‐0.19 days, 95% CI ‐0.56 to 0.18; 7 trials; 4120 women; Tau² = 0.20; I² = 94%).
Rates of neonatal intensive care unit (NICU) admission were lower (RR 0.88, 95% CI 0.80 to 0.96; 17 trials, 17,826 infants; high‐certainty evidence), and probably fewer babies had Apgar scores less than seven at five minutes in the induction groups compared with expectant management (RR 0.73, 95% CI 0.56 to 0.96; 20 trials, 18,345 infants; moderate‐certainty evidence).
Induction or expectant management may make little or no difference for neonatal encephalopathy (RR 0.69, 95% CI 0.37 to 1.31; 2 trials, 8851 infants; low‐certainty evidence, and probably makes little or no difference for neonatal trauma (RR 0.97, 95% CI 0.63 to 1.49; 5 trials, 13,106 infants; moderate‐certainty evidence) for induction compared with expectant management. Neurodevelopment at childhood follow‐up and postnatal depression were not reported by any trials.
In subgroup analyses, no differences were seen for timing of induction (< 40 versus 40‐41 versus ≥ 41 weeks' gestation), by parity (primiparous versus multiparous) or state of cervix for any of the main outcomes (perinatal death, stillbirth, NICU admission, caesarean section, operative vaginal birth, or perineal trauma).
Authors' conclusions
There is a clear reduction in perinatal death with a policy of labour induction at or beyond 37 weeks compared with expectant management, though absolute rates are small (0.4 versus 3 deaths per 1000). There were also lower caesarean rates without increasing rates of operative vaginal births and there were fewer NICU admissions with a policy of induction. Most of the important outcomes assessed using GRADE had high‐ or moderate‐certainty ratings.
While existing trials have not yet reported on childhood neurodevelopment, this is an important area for future research.
The optimal timing of offering induction of labour to women at or beyond 37 weeks' gestation needs further investigation, as does further exploration of risk profiles of women and their values and preferences. Offering women tailored counselling may help them make an informed choice between induction of labour for pregnancies, particularly those continuing beyond 41 weeks ‐ or waiting for labour to start and/or waiting before inducing labour.
Plain language summary
Induction of labour in women with normal pregnancies at or beyond 37 weeks
Does a policy of inducing labour at or beyond 37 weeks' gestation reduce risks for babies and their mothers when compared with a policy of waiting until a later gestational age, or until there is an indication for induction of labour?
This review was originally published in 2006 and subsequently updated in 2012 and 2018.
What is the issue?
The average pregnancy lasts 40 weeks from the start of the woman's last menstrual period. Pregnancies continuing beyond 42 weeks are described as 'post‐term' or 'postdate' and a woman and her clinician may decide to bring the birth on by induction. Factors associated with post‐term birth include obesity, first baby and the mother being more than 30 years old.
Why is this important?
Prolonged gestation may increase risks for babies, including a greater risk of death (before or shortly after birth). However, inducing labour may also have risks for mothers and their babies, especially if the women’s cervix is not ready to go into labour. Current tests cannot predict the risks for babies or their mother, as such, and many hospitals have policies for how long pregnancies should be allowed to continue.
What evidence did we find?
We searched for evidence (17 July 2019) and identified 34 randomised controlled trials based in 16 different countries and involving > 21,500 women (mostly with low risk of complications). The trials compared a policy of inducing labour usually after 41 completed weeks of gestation (> 287 days) with a policy of waiting (expectant management).
A policy of labour induction was associated with fewer perinatal deaths (22 trials, 18,795 infants). Four perinatal deaths occurred in the labour induction policy group compared with 25 perinatal deaths in the expectant management group. Fewer stillbirths occurred in the induction group (22 trials, 18,795 infants), with two in the induction policy group and 16 in the expectant management group.
Women in the induction arms of the trials were probably less likely to have a caesarean section compared with expectant management (31 trials, 21,030 women) and there was probably little or no difference in assisted vaginal births (22 trials, 18,584 women).
Fewer babies went into the neonatal intensive care unit (NICU) in the policy of labour induction group (17 trials, 17,826 infants; high‐certainty evidence). A simple test of the baby’s health (Apgar score) at five minutes was probably more favourable in the induction groups compared with expectant management (20 trials, 18,345 infants).
A policy of induction may make little or no difference to the women experiencing perineal trauma and probably makes little or no difference to the number of women having a postpartum haemorrhage, or breastfeeding at discharge. We are uncertain about the effect of induction or expectant management on the length of maternal hospital stay due to very low‐certainty evidence.
For newborn babies, the number with trauma or encephalopathy were similar in the induction and expectant management groups (moderate and low‐certainty evidence respectively). Neurodevelopment at childhood follow‐up and postnatal depression were not reported in any of the trials. Only three trials reported some measure of maternal satisfaction.
What does this mean?
A policy of labour induction compared with expectant management is associated with fewer deaths of babies and probably fewer caesarean sections; with probably little or no difference in assisted vaginal births. The best timing of when to offer induction of labour to women at or beyond 37 weeks' gestation warrants further investigation, as does further exploration of risk profiles of women and their values and preferences. Discussing the risks of labour induction, including benefits and harms, may help women make an informed choice between induction of labour for pregnancies, particularly those continuing beyond 41 weeks, or waiting for labour to start and/or waiting before inducing labour. Women's understanding of induction, the procedures, their risks and benefits, is important in influencing their choices and satisfaction.
Summary of findings
Summary of findings 1. Labour induction versus expectant management (infant/child outcomes).
| Induction of labour for improving birth outcomes for women at or beyond 37 weeks gestation | ||||||
| Population: pregnant women at or beyond 37 weeks gestation Setting: Austria, Canada, China, India, Finland, Malaysia, Netherlands, Norway, Russia, Spain, Sweden, Thailand, Tunisia, Turkey, UK and USA Intervention: labour induction Comparison: expectant management | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with expectant management | Risk with labour induction | |||||
| Perinatal death (intrauterine deaths plus neonatal deaths in the first week of life) | Study population | RR 0.31 (0.15 to 0.64) | 18,795 (22 RCTs) | ⊕⊕⊕⊕ HIGH1 | Exact day of death not reported for all of the nine neonatal deaths but all were likely to have occurred in the first week of life (see Table 2) | |
| 3 per 1000 | 0.4 per 1000 (0.1 to 1.9) |
|||||
| Stillbirth | Study population | RR 0.30 (0.12 to 0.75) | 18,795 (22 RCTs) | ⊕⊕⊕⊕ HIGH1 | ||
| 2 per 1000 | 1 per 1000 (0.15 to 1.5) | |||||
| Admission to neonatal intensive care unit | Study population | RR 0.88 (0.80 to 0.96) | 17,826 (17 RCTs) | ⊕⊕⊕⊕ HIGH1 | ||
| 95 per 1000 | 83 per 1000 (80 to 91) | |||||
| Neonatal encephalopathy | Study population | RR 0.69 (0.37 to 1.31) | 8,851 (2 RCTs) |
⊕⊕⊝⊝ LOW 2 |
||
| 5 per 1000 | 3 per 1000 (2 to 7) |
|||||
| Apgar score less than 7 at 5 minutes | Study population | RR 0.73 (0.56 to 0.96) | 18,345 (20 RCTs) | ⊕⊕⊕⊝ MODERATE3 | ||
| 13 per 1000 | 10 per 1000 (7 to 12) | |||||
| Neonatal (birth) trauma | Study population | RR 0.97 (0.63 to 1.49) | 13,106 (5 RCTs) | ⊕⊕⊕⊝ MODERATE4 | ||
| 7 per 1000 | 7 per 1000 (5 to 12) | |||||
| Neurodevelopment at childhood follow‐up | Study population | ‐ | (0 RCTs) | ‐ | No RCTs reported data for this outcome. | |
| see comment | see comment | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1Not downgraded (larger studies (> 1000 participants) are generally at low risk of bias, although some smaller studies have unclear risk of selection bias); not downgraded for lack of blinding as unlikely to have influenced objective outcomes.
2Downgraded 2 levels for very serious concerns regarding imprecision (wide confidence intervals crossing the line of no effect).
3Downgraded 1 level for serious concerns regarding indirectness, with three studies reporting Apgar scores with more stringent cutoffs than < 5 at 7 minutes (see graph footnotes).
4Downgraded 1 level for serious concerns regarding imprecision, with wide confidence intervals crossing line of no effect.
5. Causes of death (stillbirths and livebirth deaths).
| Study | Cause of death | |
| Intervention Group | Control Group (Expectant management) | |
| Augensen 1987 | No deaths | No deaths |
| Bergsjo 1989 | 1. Severe malformations (Livebirth) GA at birth and timing of death after birth not reported, but assumed to be early |
1. Malformation (Livebirth) GA at birth and timing of death after birth not reported, but assumed to be early 2. Pneumonia (Livebirth) GA at birth and timing of death after birth not reported, but assumed to be early |
| Chanrachkul 2003 | No deaths | No deaths |
| Cole 1975 | No deaths | 1. Congenital heart condition (Stillbirth) GA at detection of death not reported |
| Dyson 1987 | No deaths | 1. Meconium aspiration and persistent fetal circulation (Livebirth) GA at birth was 43 + 4 and timing of death after birth was early but not reported in days |
| Egarter 1989 | No deaths | 1. Cord complication (Stillbirth) GA at detection of fetal death was 40 + 3 weeks |
| Gelisen 2005 | No deaths | 1. Intrauterine fetal death (Stillbirth) GA at death 41 + 5 weeks |
| Grobman 2018 | Antepartum stillbirth: 1 Intrapartum stillbirth: 0 Neonatal death: 1 | Antepartum stillbirth: 1 Intrapartum stillbirth: 0 Neonatal death: 2 early deaths (no other information; time of death not reported) |
| Hannah 1992 | No deaths | 1. Hypoxic ischaemic encephalopathy (Stillbirth) GA at detection of death not reported in days 2. Massive aspiration of meconium (Stillbirth) GA at detection of death not reported |
| Heimstad 2007 | No deaths | 1. Birth asphyxia secondary to a true knot in the umbilical cord (Livebirth) Birth at 294 days GA; death at 2 days of age |
| Henry 1969 | No deaths | 1. Stillbirth in a woman with an abnormal glucose tolerance test (Stillbirth) GA at detection of death not reported 2. Neonatal death from meconium inhalation in a woman with a positive amnioscopy who refused surgical induction of labour (Livebirth) GA at detection of death not reported, but presumed early |
| Herabutya 1992 | No deaths | 1. Congenital anomaly (Livebirth) Birth at 43 weeks; death at 3 days of age |
| James 2001 | No deaths | No deaths |
| Keulen 2019 | One fetal death: “The stillbirth in the induction group was in a 30 year old multiparous woman who was randomised at 40 weeks+5 days and scheduled for induction at 41 weeks+1 day. She had reduced fetal movements at 40 weeks+6 days, and fetal death was diagnosed at consultation. She delivered a neonate weighing 3595 g (20th to 50th centiles). Investigations, including a postmortem examination, did not explain the stillbirth.” | 2 fetal deaths: "stillbirth was diagnosed in a 36 year old nulliparous woman at 41 weeks+3 days, when she was admitted to hospital in labour. She delivered a neonate weighing 2945 g (5th to 10th centiles). Investigations, including placental examination, did not explain the stillbirth, and the parents declined a postmortem examination. The second stillbirth in the expectant management group was diagnosed in a 32 year old multiparous woman at 41 weeks+4 days during a regular consultation in secondary care for impending post‐term pregnancy. She delivered a neonate weighing 3715 g (20th to 50th centiles). No postmortem examination was performed, but the placenta showed signs of chorioamnionitis.” |
| Martin 1978 | No deaths reported | 1 (Stillbirth) Stillbirth after induction of labour at 42 weeks for postmaturity and meconium |
| Martin 1989 | No deaths | No deaths |
| NICHHD 1994 | No deaths | No deaths |
| Sargunam 2019 | No deaths reported | No deaths reported |
| Sahraoui 2005 | No deaths | 1 (Intrauterine fetal death) (Stillbirth) Death detected at 42 weeks' GA |
| Sande 1983 | No deaths | No deaths |
| Suikkari 1983 | No deaths | No deaths |
| Walker 2016 | No deaths | No deaths |
| Wennerholm 2019 | No deaths | 6 (5 stillbirths; 1 early neonatal death) One stillborn baby had cardiovascular malformations not considered to be lethal and there were no explanations for the deaths of the other four stillbirths; Cause of the early neonatal death was hypoxic ischaemic encephalopathy in a large for gestational age neonate. |
GA:gestational age
Summary of findings 2. Labour induction versus expectant management (maternal outcomes).
| Induction of labour for improving birth outcomes for women at or beyond term | ||||||
| Population: pregnant women at or beyond 37 weeks gestation Setting: Austria, Canada, China, Finland, France, India, Malaysia, Netherlands, Norway, Spain, Sweden, Russia, Thailand, Tunisia, Turkey, UK, and USA Intervention: labour induction Comparison: expectant management | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with expectant management | Risk with labour induction | |||||
| Caesarean section | Study population | RR 0.90 (0.85 to 0.95) | 21,030 (31 RCTs) | ⊕⊕⊕⊝ MODERATE1 | ||
| 186 per 1000 | 167 per 1000 (158 to 177) | |||||
| Operative vaginal birth (forceps or ventouse) | Study population | RR 1.03 (0.96 to 1.10) | 18,584 (22 RCTs) | ⊕⊕⊕⊝ MODERATE1 | ||
| 136 per 1000 | 140 per 1000 (131 to 150) | |||||
| Perineal trauma (severe perineal tear) | Study population | RR 1.04 (0.85 to 1.26) | 11,589 (5 RCTs) | ⊕⊕⊝⊝ LOW1,2 | ||
| 31 per 1000 | 33 per 1000 (26 to 39) | |||||
| Postpartum haemorrhage | Study population | RR 1.02 (0.91 to 1.15) | 12,609 (9 RCTs) | ⊕⊕⊕⊝ MODERATE3 | variously defined | |
| 79 per 1000 | 81 per 1000 (73 to 91) | |||||
| Breastfeeding at discharge | Study population | RR 1.00 (0.96 to 1.04) |
7487 (2 RCTs) |
⊕⊕⊕⊝ MODERATE4 | ||
| 505 per 1000 | 505 per 1000 (485 to 525) |
|||||
| Postnatal depression | Study population | ‐ | (0 RCTs) | ‐ | No RCTs reported data for this outcome. | |
| see comment | see comment | |||||
| Length of maternal hospital stay (days) | ‐ | ‐ | Average MD 0.19 days shorter for women who were induced (0.56 days shorter to 0.18 days longer) | 4120 (7 RCTs) | ⊕⊝⊝⊝ VERY LOW5 |
|
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1Downgraded 1 level for serious concerns regarding unclear allocation concealment methods for many of the 31 trials included for this outcome. 2Downgraded 1 level for serious concerns regarding imprecision with wde confidence intervals crossing the line of no effect, signalling some uncertainty about direction of effect.
3Downgraded 1 level for serious concerns regarding indirectness with postpartum haemorrhage defined in different ways for several of the trials.
4Downgraded 1 level for indirectness with one of the two studies reporting breastfeeding 4‐8 weeks after discharge (not at discharge).
5Downgraded 1 level for serious concerns regarding selection bias, with 4 of 5 trials having with unclear allocation concealment; and downgraded 2 levels for very serious concerns regarding inconsistency, with very high statistical heterogeneity (I² = 94%).
Background
Description of the condition
Pregnancies continuing beyond 294 days (420 weeks) are described as being 'post‐term' or 'postdate' (Roos 2010). In 2017 in the USA, 5.8% of pregnancies progressed to 41+ weeks (Martin 2018), dropping from around 10% a decade or so earlier (Olesen 2003; Zeitlin 2007). However the definition of term pregnancy is less clear, with increasing calls for term to be redefined as close to 40 completed weeks as possible (University of Sydney 2020).
While the aetiology of post‐term birth is not well elucidated (Mandruzzato 2010), risk factors such as obesity, nulliparity and maternal age greater than 30 years have been associated with an increased risk of post‐term birth (Arrowsmith 2011; Caughey 2009; Heslehurst 2017; Roos 2010). Placental senescence may play a role in the pathophysiology of post‐term birth (Mandruzzato 2010), and genetic/epigenetic factors have also been implicated (Schierding 2014).
In a systematic review of 15 million pregnancies from high‐income countries, the risk of stillbirth increased with gestational age, from 0.11 per 1000 births at 37 weeks' gestation to 3.18 per 1000 births at 42 weeks' gestation; and risk of neonatal death was nearly doubled for pregnancies continuing beyond 41 weeks, compared with 38‐41 weeks' gestation (Muglu 2019). In a large retrospective cohort study from the United States, involving 5.4 million pregnancies of low‐risk, parous women at 39 to 41 weeks' gestation, overall risks of a composite adverse neonatal outcome (any of: Apgar score less than five at five minutes, assisted ventilation for longer than six hours, neonatal seizure or neonatal mortality) and a composite adverse maternal outcome (any of: intensive care unit admission, blood transfusion, uterine rupture, or unplanned hysterectomy) increased from 39 through to 41 weeks (Chen 2019). These findings are important in that, even in settings where early booking allows accurate assessment of gestational age and antenatal services are accessible for most women, post‐term pregnancy still constitutes a high‐risk situation, especially for the baby.
The obstetric problems associated with post‐term pregnancy include induction of labour with an unfavourable cervix, caesarean section, prolonged labour, postpartum haemorrhage and traumatic birth. It is likely that some of these unwanted outcomes result from intervening when the uterus and cervix are not ready for labour (Caughey 2004).
Description of the intervention
Induction of labour is widely practised to try and prevent outcomes such as caesarean section, prolonged labour, postpartum haemorrhage and traumatic birth (Caughey 2004), and to improve health outcomes for women and their infants. Rates of induction of labour have increased over recent decades, with between and within country variations (Coates 2020; Marconi 2019). In the USA in 2017, one in four births (25.7%) was induced (Martin 2018). In Australia, the induction rate rose from 25% in 2007 to 33% in 2017 (AIHW 2019). For post‐term pregnancies, one in every two births may be induced (e.g. 52% induction rate for gestations ≥ 41 weeks as reported by Wolff 2016).
Variation in rates of post‐term births suggests that different policies and practices for managing post‐term pregnancies (especially timing of inductions) are used in Europe (Zeitlin 2007), and elsewhere. There is concern about increasing caesarean rates, despite induction rates also rising (Keirse 2010).
Earlier versions of this review included interventions involving monitoring, such as early pregnancy ultrasound, that may have an effect on the outcomes of pregnancies for women at or beyond 37 weeks. This topic is addressed in the Cochrane Review 'Ultrasound for fetal assessment in early pregnancy' (Whitworth 2015). In this update, we evaluated the effects of timing of labour induction at or beyond 37 weeks compared with expectant management (which may include various intensities and forms of monitoring).
How the intervention might work
Methods of induction of labour aim to induce cervical ripening and/or the onset of uterine contractions, and primarily include pharmacological methods (such as prostaglandins and oxytocin) and mechanical methods (such as the Foley catheter, double balloon catheter and artificial rupture of amniotic membranes: 'amniotomy'). Prostaglandins (misoprostol: prostaglandin E1 ‐ with oral, buccal/sublingual or vaginal administration; and dinoprostone: prostaglandin E2 ‐ available as vaginal gels or pessaries) are commonly used when the cervix is not favourable. When the cervix is favourable, oxytocin is usually used. The Foley catheter and/or amniotomy may be used alone, or in association with oxytocin, or misoprostol (Marconi 2019).
Why it is important to do this review
Determining the threshold for induction of post‐term pregnancies has been described as 'the 41 week to 42 week dilemma' (Keulen 2018), with many clinical practice guidelines now recommending a policy of induction at 41 weeks rather than a policy of waiting to induce at 42 weeks if spontaneous labour has not occurred (ACOG 2014; New Zealand Guideline Development Panel 2019; NICE 2008; SOGC 2017; WHO 2018). As there are no agreed standards for the timing of induction of labour, with guidance varying considerably internationally and nationally, debate continues (Coates 2020). Much uncertainty surrounds the optimal timing for induction, with clinical practice, and research studies in some settings, demonstrating trends towards earlier gestations at induction (Coates 2020).
It is important to assess whether improved outcomes such as reduced perinatal death and fewer caesarean sections can be achieved without negative impacts of being born too early, by choosing a window of timing for induction, and to determine optimal gestational thresholds, which may differ according to individual characteristics of women (Alavifard 2019).
Objectives
To assess the effects of a policy of labour induction at or beyond 37 weeks' gestation compared with a policy of awaiting spontaneous labour indefinitely (or until a later gestational age, or until a maternal or fetal indication for induction of labour arises) on pregnancy outcomes for the infant and the mother.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials. We included trials presented only as abstracts as well as trials published in full‐text manuscript format.
Cluster‐randomised trials, quasi‐randomised trials and cross‐over trials were not eligible for inclusion in this review.
Types of participants
We included pregnant women at or beyond 37 weeks. Since a risk factor at this stage of pregnancy would normally require an intervention, only trials including women at low risk for complications were eligible. We accepted the trialists' definition of 'low risk'. The trials of induction of labour exclusively in women with prelabour rupture of membranes at or beyond term were not considered in this review (and are considered in the Cochrane Review 'Planned early birth versus expectant management (waiting) for prelabour rupture of membranes at term (37 weeks or more)' (Middleton 2017), although some women participating in the eligible trials in this review may have had ruptured membranes.
Types of interventions
The intervention evaluated in this review is a policy of labour induction at a predetermined gestational age at or beyond 37 weeks. This policy is compared with 'expectant management' until an indication for birth arises. The trial protocols differ according to:
gestational age used in the induction of labour policy;
actual method of labour induction (prostaglandins, misoprostol, +/‐ oxytocin);
protocol used (dosage of any drugs, timing, frequency of use and mode of administration);
expectant management protocols (intensity of fetal well‐being assessment and fetal monitoring techniques used).
Types of outcome measures
Primary outcomes
Perinatal death (defined as intrauterine death plus neonatal death in the first week of life)
Secondary outcomes
For the infant/child
Stillbirth
Neonatal death within first week
Birth asphyxia (as defined by trialists)
Admission to neonatal intensive care unit
Neonatal convulsions
Neonatal encephalopathy
Use of anticonvulsants
Meconium aspiration syndrome
Pneumonia
Apgar score less than seven at five minutes
Birthweight
Birthweight > 4000 g
Neonatal trauma
Neurodevelopment at childhood follow‐up
For the mother
Mode of birth (caesarean section)
Operative vaginal birth (forceps or ventouse)
Analgesia used
Perineal trauma
Prolonged labour (cut‐off used by the trialists was used)
Postpartum haemorrhage (cut‐off used by the trialists was used)
Anxiety before birth
Other measures of satisfaction with the approach
Breastfeeding at discharge
Postnatal depression
Health services use
Length of maternal postnatal stay
Length of neonatal postnatal stay
Length of labour
Cost‐related analyses are described in the Discussion.
Search methods for identification of studies
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Electronic searches
We searched Cochrane Pregnancy and Childbirth’s Trials Register by contacting their Information Specialist (17 July 2019).
The Register is a database containing over 25,000 reports of controlled trials in the field of pregnancy and childbirth. It represents over 30 years of searching. For full current search methods used to populate Pregnancy and Childbirth’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link.
Briefly, Cochrane Pregnancy and Childbirth’s Trials Register is maintained by the Information Specialist and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
monthly searches of CINAHL (EBSCO);
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Search results are screened by two people and the full text of all relevant trial reports identified through the searching activities described above is reviewed. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth review topic (or topics), and is then added to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set that has been fully accounted for in the relevant review sections (Included studies; Excluded studies; Studies awaiting classification; Ongoing studies).
In addition, we searched ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform (ICTRP) for unpublished, planned and ongoing trial reports (17 July 2019) (see: Appendix 1 for search methods used).
Searching other resources
We searched the reference lists of retrieved studies. We did not apply any language or date restrictions.
Data collection and analysis
For methods used in the previous versions of this review, seeGülmezoglu 2012; and Middleton 2018.
For this update, the following methods were used for assessing the reports that were identified as a result of the updated search. Where required, information pertaining to the previously included studies was updated according to methods outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Selection of studies
Two review authors independently assessed for inclusion all the potential studies identified as a result of the search strategy. We resolved any disagreement through discussion or, if required, we consulted the third review author.
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted the third review author. Data were entered into Review Manager software (RevMan 2014), and checked for accuracy.
When information regarding any of the above was unclear, we planned to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreement was resolved by discussion or by involving the third review author.
(1) Allocation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether the intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding was unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blinded outcome assessment as:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we planned to re‐include missing data in the analyses which we undertook.
We assessed methods as:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it is clear that all of the study’s prespecified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study’s prespecified outcomes have been reported; one or more reported primary outcomes were not prespecified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Handbook (Higgins 2011). With reference to (1) to (6) above, we assessed the likely magnitude and direction of the bias and whether we considered it was likely to have impacted on the findings. We explored the impact of the level of bias through undertaking sensitivity analyses ‐ seeSensitivity analysis.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio with 95% confidence intervals.
Continuous data
For continuous data, we used the mean difference. We planned to use the standardised mean difference to combine trials that measured the same outcome, but used different methods.
Unit of analysis issues
Cluster‐randomised trials
Cluster‐randomised trials were not eligible for inclusion.
Cross‐over trials
Cross‐over trials were not eligible for inclusion.
Multiple pregnancies
We did not identify any eligible studies that reported multiple pregnancies separately. If studies with multiple pregnancies are reported separately in trials included in future updates of this review, we will adjust for clustering in the analyses wherever possible, and use the inverse variance method for adjusted analyses, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), and in Yelland 2011.
Multi‐armed trials
Where we included studies with multiple arms, we created single pairwise comparisons, by including only the groups relevant to this review, or by combining groups. In Gelisen 2005, we combined the three induction arms for the relevant analyses.
Dealing with missing data
For included studies, we noted levels of attrition. In future updates, if more eligible studies are included, we will explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analyses.
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We regarded heterogeneity as substantial if an I² was greater than 30% and either the Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity. Where we identified substantial heterogeneity (above 30%), we aimed to explore it using prespecified subgroup analyses.
Assessment of reporting biases
Where there were 10 or more studies in the meta‐analyses, we investigated reporting biases (such as publication bias) using funnel plots. We assessed funnel plot asymmetry visually. If asymmetry was suggested by a visual assessment, we planned to perform exploratory analyses to investigate it.
Data synthesis
We carried out statistical analysis using the Review Manager software (RevMan 2014). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: i.e. where studies were examining the same intervention, and the studies' populations and methods were judged sufficiently similar. The denominators used for neonatal outcomes were the whole randomised population (without the stillbirths removed).
Where there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or where substantial statistical heterogeneity was detected, we used random‐effects meta‐analysis to produce an overall summary if an average treatment effect across trials was considered clinically meaningful. The random‐effects summary has been treated as the average of the range of possible treatment effects and we have discussed the clinical implications of treatment effects differing between trials. If the average treatment effect was not clinically meaningful, we decided that we would not combine trials. Where we used random‐effects analyses, the results have been presented as the average treatment effect with 95% confidence intervals, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
Where we identified substantial heterogeneity, we planned to investigate it using subgroup and sensitivity analyses. We planned to consider whether an overall summary was meaningful, and if it was, we used random‐effects analysis to produce it.
We carried out the following subgroup analyses.
-
Gestational age by week of gestation when induction was intended in the intervention arm
in this update, we have presented the main groups as gestational ages < 40 weeks, 40‐41 weeks, and > 41 completed weeks (> 287 days).
Parity (nulliparous versus mixed parity (primi‐ and multiparous versus not stated).
State of the cervix (favourable versus unfavourable versus unknown or mixed status).
We were unable to conduct subgroup analyses by method of induction, due to wide variation in reporting of dosage, timing, frequency and mode of administration.
Where possible, we used the following outcomes in subgroup analyses.
For the infant/child
Perinatal death, defined as intrauterine deaths plus neonatal deaths in the first week of life
Stillbirth
Admission to neonatal intensive care unit
For the mother
Mode of birth (caesarean section)
Operative vaginal birth (forceps or ventouse)
Perineal trauma
We assessed subgroup differences by interaction tests available within RevMan (RevMan 2014). We reported the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value.
Sensitivity analysis
We carried out sensitivity analyses to explore the effect of trial risk of bias assessed by concealment of allocation, high attrition rates, or both, with studies at high risk of bias being excluded from the analyses in order to assess whether this made any difference to the overall result. We used the following outcomes in our sensitivity analyses. If enough data becomes available in future updates, we will explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analyses.
For the infant/child
Perinatal death, defined as intrauterine deaths plus neonatal deaths in the first week of life
Stillbirth
Admission to neonatal intensive care unit
For the mother
Mode of birth (caesarean section)
Operative vaginal birth (forceps or ventouse)
Perineal trauma
Assessment of the certainty of the evidence using the GRADE approach
For this update, we used the GRADE approach as outlined in the GRADE handbook, in order to assess the certainty of the body of evidence relating to the following outcomes.
For the infant/child
Perinatal death, defined as intrauterine deaths plus neonatal deaths in the first week of life
Stillbirth
Admission to neonatal intensive care unit
Neonatal encephalopathy
Apgar score less than seven at five minutes
Neonatal trauma
Neurodevelopment at childhood follow‐up
For the mother
Mode of birth (caesarean section)
Operative vaginal birth (forceps or ventouse)
Perineal trauma (e.g. severe perineal tear)
Postpartum haemorrhage (cut‐off reported by the trialists was used)
Breastfeeding at discharge
Postnatal depression
Length of maternal postnatal stay
We used the GRADEpro Guideline Development Tool to import data from Review Manager 5.3 (RevMan 2014), in order to create ’Summary of findings’ tables, comparing a policy of labour induction versus expectant management. A summary of the intervention effect and a measure of certainty for each of the above outcomes was produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the certainty of the body of evidence for each outcome. The evidence can be downgraded from 'high certainty' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Results
Description of studies
Results of the search
See Figure 1.
1.
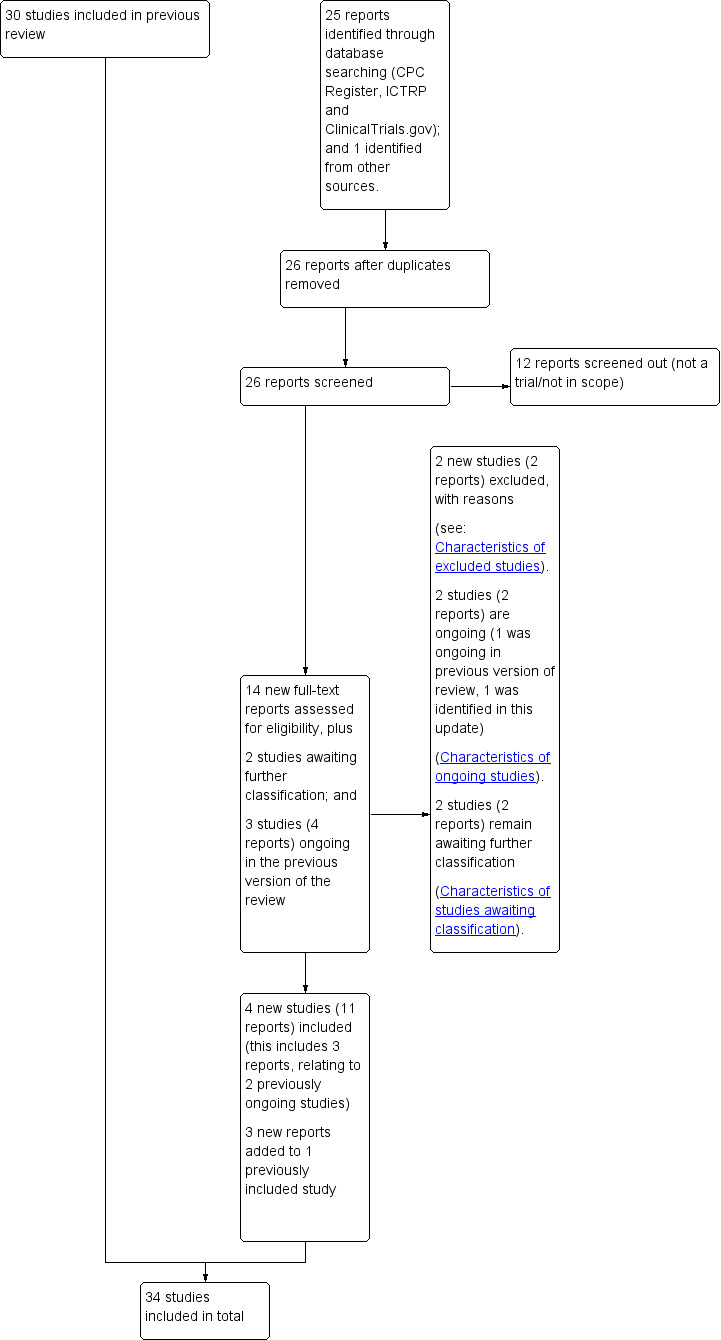
Study flow diagram.
For this update, we assessed 14 new trial reports, and re‐assessed three ongoing studies, Wennerholm 2019 (classified as Elden 2016 in the previous version of this review); Grobman 2018 (classified as NCT01990612 in the previous version of this review); ISRCTN15646866; and re‐assessed two studies which were previously awaiting further classification (Benito Reyes 2010; ISRCTN74323479)).
We included four new studies (11 reports) (Baev 2017; Grobman 2018; Sargunam 2019; Wennerholm 2019), excluded two new studies (two reports) (PACTR201805002872322; CTRI/2018/09/015719), and listed one new study as ongoing (one report) (ISRCTN83219789). Three of the new reports related to an already included study (Keulen 2019 (Kortekaas 2014 in the previous version of this review)). Two of the previously ongoing studies related to trial protocols for two newly included studies (Grobman 2018; Wennerholm 2019); and one of the previously ongoing studies (ISRCTN15646866) remains ongoing. Benito Reyes 2010 and ISRCTN74323479 remain awaiting classification (requiring an English translation, and further details, to assess eligibility respectively).
Therefore, 34 studies are included in this update (69 reports), two studies are ongoing (two reports), 66 studies are excluded (77 reports), and two studies (two reports) await further classification.
Included studies
Settings
Of the 34 included trials:
seven were conducted in the USA (Dyson 1987; Grobman 2018; Martin 1989; Miller 2015; NICHHD 1994; Nielsen 2005; Witter 1987);
four in the UK (Scotland; England; Ireland) (Cole 1975; Henry 1969; Martin 1978; Walker 2016);
three in China (Bergsjo 1989; Cohn 1992; Roach 1997);
three in Norway (Augensen 1987; Heimstad 2007; Sande 1983);
three in Sweden (Brane 2014; Tylleskar 1979; Wennerholm 2019);
two in India (Chakravarti 2000; James 2001);
two in Thailand (Chanrachkul 2003; Herabutya 1992);
one in Tunisia (Sahraoui 2005);
one in Turkey (Gelisen 2005);
one in Canada (Hannah 1992);
one in France (Breart 1982);
one in Austria (Egarter 1989);
one in Spain (Ocon 1997);
one in the Netherlands (Keulen 2019);
one in Malaysia (Sargunam 2019);
one in Finland (Suikkari 1983); and
one in Russia (Baev 2017).
Date trials published/conducted
Four trials were published in or before the 1970s (Cole 1975; Henry 1969; Martin 1978; Tylleskar 1979)
Nine trials were published in the 1980s (Augensen 1987; Bergsjo 1989; Breart 1982; Dyson 1987; Egarter 1989; Martin 1989; Sande 1983; Suikkari 1983; Witter 1987)
Six trials were published in the 1990s (Cohn 1992; Hannah 1992; Herabutya 1992; NICHHD 1994; Ocon 1997; Roach 1997)
Seven trials were published in the 2000s (Chakravarti 2000; Chanrachkul 2003; Gelisen 2005; Heimstad 2007; James 2001; Nielsen 2005; Sahraoui 2005)
Eight trials were published in the 2010s (Baev 2017; Brane 2014; Grobman 2018; Keulen 2019; Miller 2015; Sargunam 2019; Walker 2016; Wennerholm 2019).
Over half the total participants (12,074) were recruited from trials published in the last seven years.
Cervix status
Ten trials did not mention cervix status as an inclusion criterion (Bergsjo 1989; Breart 1982; Chakravarti 2000; Cohn 1992; Cole 1975; Henry 1969; James 2001; Roach 1997; Suikkari 1983; Witter 1987). Ten trials included women with unfavourable cervix (Baev 2017; Dyson 1987; Gelisen 2005; Hannah 1992; Herabutya 1992; Martin 1989; Miller 2015; NICHHD 1994; Ocon 1997; Sahraoui 2005), and five with favourable cervical status (Chanrachkul 2003; Egarter 1989; Nielsen 2005; Sande 1983; Tylleskar 1979). Nine trials included women with mixed cervical status (Augensen 1987 (35% of women with unfavourable cervix); Brane 2014; Grobman 2018; Heimstad 2007; Keulen 2019; Martin 1978; Sargunam 2019; Walker 2016; Wennerholm 2019).
Interventions
All trials were conducted in hospitals with various intensities of fetal monitoring both in the induction and expectant management groups (seeCharacteristics of included studies).
Timing of induction ‐ induction group
The information on timing of induction in each trial is outlined in Table 4.
1. Gestational age, at baseline and at induction.
| Study | At baseline/enrolment (all participants) |
At induction (intervention group participants only) Mean [SD] unless otherwise indicated |
| Augensen 1987 | 41 weeks (290‐297 days) | 294.8 days (category: ≥ 41 weeks) |
| Baev 2017 | 40+6 weeks (283‐289 days) | 285.35 [0.93] days (category: 40‐41 weeks) |
| Bergsjo 1989 | 42 weeks+ (294+ days) | 294+ days, mean NR (category: ≥ 41 weeks) |
| Brane 2014 | between 37+0 and 41+6 weeks | 282 [5.9] days (category: 40‐41 weeks) |
| Breart 1982 | 37 to 39 weeks (259‐273 days) | 259‐273 days, mean NR (category: < 40 weeks) |
| Chakravarti 2000 | < 41 weeks (< 290 days) | < 290 days, mean NR (category: 40‐41 weeks) |
| Chanrachkul 2003 | 41+3 weeks (290 days) | 290.4 [1.4] days (category: ≥ 41 weeks) |
| Cohn 1992 | 42+0 weeks (294 days) | 294+ days (category: ≥ 41 weeks) |
| Cole 1975 | 39 to 40 weeks (273‐280 days) | 273‐280 days, mean NR (category: < 40 weeks) |
| Dyson 1987 | 41 weeks+ (287 days+) | 296.3 [2.6] days (category: ≥ 41 weeks) |
| Egarter 1989 | 40 weeks (280 days) | 280 days (category: 40 to 41 weeks ) |
| Gelisen 2005 | 41 weeks+ 0‐1 | 286‐288 days (category: ≥ 41 weeks) |
| Grobman 2018 | 380 weeks to 386 (268‐274 days) | 390 weeks to 394 weeks (273‐279 days) (category: < 40 weeks) |
| Hannah 1992 | 41 weeks+ (287 days+) | 287 days+ mean NR (authors stated that women were induced within 4 days of enrolment, and that 88% of women were 41 weeks GA, (287‐293 days GA), no further details) (category: ≥ 41 weeks) |
| Heimstad 2007 | 406 weeks (286 days) | Mean 289 [0.7] days (category: ≥ 41 weeks) |
| Henry 1969 | 41 weeks+ (287 days+) | 287+ days, mean NR (category: ≥ 41 weeks) |
| Herabutya 1992 | 42 weeks+ (294 days+) | 294+ days, mean NR (category: ≥ 41 weeks) |
| James 2001 | 41 weeks (287 days) | 287+ days, mean NR (category: ≥ 41 weeks) |
| Keulen 2019 | 405 to 410 weeks (285‐287 days) | 287 to 288 days, mean NR (category: ≥ 41 weeks) |
| Martin 1978 | 371 to 376 weeks (260‐266 days) | 273 days (category: < 40 weeks) |
| Martin 1989 | 41 weeks (287 days) | 287+ days, mean NR (category: ≥ 41 weeks) |
| Miller 2015 | 380 to 386 (266 to 272 days) | 390 to 396 weeks (273‐279 days), mean NR (category: < 40 weeks) |
| NICHHD 1994 | 41 weeks+ (at least 287 days) | 287 days to < 301 days, mean NR (category: ≥ 41 weeks) |
| Nielsen 2005 | 390 to 396 weeks (273‐279 days) | Within a week after enrolment, therefore between 39 and 40 weeks (274 to 280 days) (mean time between enrolment and induction of labour 3.7 days) (category: < 40 weeks) |
| Ocon 1997 | Unclear (due to incomplete translation of paper) | 42 completed weeks (category: ≥ 41 weeks) |
| Roach 1997 | 410 to 416 weeks (287 to 293 days) | 42 completed weeks (category: ≥ 41 weeks) |
| Sahraoui 2005 | 410 to 416 weeks (287‐293 days) | 287‐293 days, mean NR (category: ≥ 41 weeks) |
| Sande 1983 | 400 and 406 weeks | 280 to 286 days (category: 40 to 41 weeks) |
| Sargunam 2019 | ≥ 39 weeks (≥ 273 days) | ≥ 273 days (category: < 40 weeks) |
| Suikkari 1983 | 10 days or more post‐date | 287+ days (category: ≥ 41 weeks) |
| Tylleskar 1979 | At least 37 weeks (259+ days) | 40 weeks, EDD +/‐ 2 days (category: 40 to 41 weeks) |
| Walker 2016 | 360 to 396 weeks (252‐279 days) | 390 to 396 weeks (273‐279 days) (category: < 40 weeks) |
| Wennerholm 2019 | 406 to 411 weeks (286 to 288 days) | 288.7 [1.1] weeks (category: ≥ 41 weeks) |
| Witter 1987 | 41 weeks (293 to 298 days) | 42 weeks (293‐298 days) (category: ≥ 41 weeks) |
EDD: estimated due date GA: gestational age NR: not reported SD: standard deviation
We have categorised timing of induction in the intervention arm into three groups:
induced at < 40 weeks: eight trials (Breart 1982; Cole 1975; Grobman 2018; Martin 1978; Miller 2015; Nielsen 2005; Sargunam 2019; Walker 2016);
induced between 40 to 41 weeks: six trials (Baev 2017; Brane 2014; Chakravarti 2000; Egarter 1989; Sande 1983; Tylleskar 1979);
induced at ≥ 41 weeks: 20 trials (Augensen 1987; Bergsjo 1989; Chanrachkul 2003; Cohn 1992; Dyson 1987; Gelisen 2005; Hannah 1992; Heimstad 2007; Henry 1969; Herabutya 1992; James 2001; Keulen 2019; Martin 1989; NICHHD 1994; Ocon 1997; Roach 1997; Sahraoui 2005; Suikkari 1983; Wennerholm 2019; Witter 1987).
Parity
Most of the 34 included trials included a mixture of primiparous and multiparous women:
primiparous women: six trials (Brane 2014; Chakravarti 2000; Grobman 2018; Miller 2015; Sargunam 2019; Walker 2016);
primiparous and multiparous women: 22 trials (Augensen 1987; Baev 2017; Bergsjo 1989; Breart 1982; Chanrachkul 2003; Cole 1975; Dyson 1987; Egarter 1989; Gelisen 2005; Hannah 1992; Heimstad 2007; Henry 1969; Herabutya 1992; Keulen 2019; Martin 1978; NICHHD 1994; Nielsen 2005; Sahraoui 2005; Sande 1983; Suikkari 1983; Tylleskar 1979; Wennerholm 2019);
not stated/unclear: six trials (Cohn 1992; James 2001; Martin 1989; Ocon 1997; Roach 1997; Witter 1987).
See Characteristics of included studies table and Table 5 for further details.
2. Parity.
| Primiparous | Mixed (primi‐ and multiparous) | Not stated/not available |
| Brane 2014 | Augensen 1987 | Cohn 1992 |
| Chakravarti 2000 | Baev 2017 | James 2001 |
| Grobman 2018 | Bergsjo 1989 | Martin 1989 |
| Miller 2015 | Breart 1982 | Ocon 1997 |
| Sargunam 2019 | Chanrachkul 2003 | Roach 1997 |
| Walker 2016 | Cole 1975 | Witter 1987 |
| Dyson 1987 | ||
| Egarter 1989 | ||
| Gelisen 2005 | ||
| Hannah 1992 | ||
| Heimstad 2007 | ||
| Henry 1969 | ||
| Herabutya 1992 | ||
| Keulen 2019 | ||
| Martin 1978 | ||
| NICHHD 1994 | ||
| Nielsen 2005 | ||
| Sahraoui 2005 | ||
| Sande 1983 | ||
| Suikkari 1983 | ||
| Tylleskar 1979 | ||
| Wennerholm 2019 (perinatal deaths reported by parity) |
Method of induction ‐ induction group
Labour induction was by oxytocin with or without artificial rupture of membranes in most trials. In trials recruiting women with an unfavourable cervix, priming with prostaglandins was often undertaken before induction.
Of the 34 included trials:
two trials did not report the method used (Chakravarti 2000; Cohn 1992);
27 trials used oxytocin infusion in some or all women in their intervention group (Augensen 1987; Baev 2017; Bergsjo 1989; Brane 2014; Breart 1982; Chanrachkul 2003; Cole 1975; Dyson 1987; Gelisen 2005; Grobman 2018; Hannah 1992; Heimstad 2007; Henry 1969; Herabutya 1992; James 2001; Keulen 2019; Martin 1989; Miller 2015; NICHHD 1994; Nielsen 2005; Sande 1983; Sargunam 2019; Suikkari 1983; Tylleskar 1979; Walker 2016; Wennerholm 2019; Witter 1987). Of those trials, only one used oxytocin as the sole method of induction (Augensen 1987). Twenty trials used artificial rupture of membranes (AROM) where indicated, as well as oxytocin infusion (when possible) (Baev 2017; Bergsjo 1989; Brane 2014; Breart 1982; Chanrachkul 2003; Cole 1975; Grobman 2018; Heimstad 2007; Henry 1969; Herabutya 1992; James 2001; Keulen 2019; Miller 2015; Nielsen 2005; Sande 1983; Sargunam 2019; Suikkari 1983; Tylleskar 1979; Walker 2016; Witter 1987);
none of the included trials used AROM as the sole method of induction;
13 trials used intravaginal prostaglandin E2 for some or all women in the intervention group (in either gel or pessary form) (Baev 2017; Brane 2014; Dyson 1987; Egarter 1989; Hannah 1992; Herabutya 1992; Keulen 2019; NICHHD 1994; Ocon 1997; Roach 1997; Sahraoui 2005; Walker 2016; Wennerholm 2019). Four trials used prostaglandin E2 as the sole method of induction (Egarter 1989; Ocon 1997; Roach 1997; Sahraoui 2005) and eight trials used a combination of prostaglandin and oxytocin +/‐ AROM (Baev 2017; Brane 2014; Dyson 1987; Hannah 1992; Herabutya 1992; Keulen 2019; NICHHD 1994; Walker 2016);
six trials used vaginal misoprostol in some or all women in the intervention group (Gelisen 2005; Heimstad 2007; Keulen 2019; Miller 2015; Sargunam 2019; Wennerholm 2019), and one used vaginal mifepristone in all women in the intervention group (Baev 2017);
in Keulen 2019, cervical priming was according to local protocol, which included prostaglandin E2, misoprostol, Foley catheter, double balloon catheter or a combination; and in Grobman 2018, the method of cervical priming (where indicated) was left to the discretion of the woman’s obstetric provider;
two trials had more than one intervention group (Gelisen 2005; NICHHD 1994), although the placebo priming and oxytocin arm in NICHHD 1994 was not included in this review. The Gelisen 2005 trial had three labour induction arms with misoprostol, oxytocin and Foley catheter.
Expectant management group protocols
For the majority of trials, expectant management protocols included various combinations of fetal heart rate monitoring, ultrasound for amniotic fluid measurements and, in earlier studies, biochemical tests.
No gestational age limit for induction in the expectant management groups was imposed or reported in 10 of the trials (Brane 2014; Cohn 1992; Dyson 1987; Henry 1969; James 2001; Ocon 1997; Roach 1997; Sargunam 2019; Suikkari 1983; Witter 1987). In the remaining 24 trials, women were induced at the following times (unless they went into spontaneous labour earlier) in the expectant management groups.
405 to 422 weeks (Grobman 2018)
41 weeks (Cole 1975)
41 to 42 weeks (Walker 2016)
42 weeks (Baev 2017; Breart 1982; Chakravarti 2000; Egarter 1989; Gelisen 2005; Keulen 2019; Martin 1978; Miller 2015; Nielsen 2005; Sahraoui 2005; Sande 1983; Tylleskar 1979; Wennerholm 2019)
42 to 43 weeks (Augensen 1987; Heimstad 2007)
43 weeks (Bergsjo 1989; Martin 1989)
44 weeks (Chanrachkul 2003; Hannah 1992; Herabutya 1992; NICHHD 1994)
See Characteristics of included studies for further details.
Setting of induction is reported in Table 6.
3. Induction setting (start and waiting).
| STUDY | START (hospital or home: and type of unit (obstetric or midwife‐led)) | WAITING (hospital or home) |
| Augensen 1987 | Hospital "Women in group 1 (immediate induction) were then referred to the delivery department for induction" |
Not reported |
| Baev 2017 | Hospital | Not reported |
| Bergsjo 1989 | Hospital | Hospital (not explicitly stated that women in the induction group stayed in hospital after induction started). However authors reported that two women in the induction group (who waited up until a week for induction) stayed in hospital after randomisation, due to transport/distance issues). This suggests that some women waited at home. |
| Brane 2014 | Hospital (Swedish delivery unit) | Hospital |
| Breart 1982 | Unclear (in French) | Unclear (in French) |
| Chakravarti 2000 | Not reported | Not reported |
| Chanrachkul 2003 | Hospital | Hospital |
| Cohn 1992 | Not reported | Not reported |
| Cole 1975 | Hospital | Not reported |
| Dyson 1987 | Hospital | Home and hospital: women who did not have a regular contractile pattern 45 minutes after induction gel was administered were allowed to go home; those who did were admitted to the hospital. |
| Egarter 1989 | Not reported | Not reported |
| Gelisen 2005 | Hospital | Hospital |
| Grobman 2018 | Not reported (A specific induction protocol was not mandated for women who underwent induction in either group). |
Not reported |
| Hannah 1992 | Hospital (community and tertiary) | Not reported, only reported that when induction was started, women were treated as outpatients in the hospital |
| Heimstad 2007 | Hospital | Not reported |
| Henry 1969 | Hospital | Not reported |
| Herabutya 1992 | Hospital | Home and hospital or either: women with a Bishop score > 6 stayed in hospital after the induction was performed, and sent to birthing ward; while those with a lower Bishop score were asked to go home and come in the next morning |
| James 2001 | Hospital | Not reported |
| Keulen 2019 | Primary care midwifery practices (n = 123) and hospitals (n = 45) (in the Netherlands, care is provided for women with normal risk pregnancies by midwives, and for pregnancies at increased risk by obstetricians or gynaecologists) | "all women in the 41 week induction group received obstetrician led intrapartum secondary care" |
| Martin 1978 | Hospital | Hospital |
| Martin 1989 | Hospital | Hospital |
| Miller 2015 | Hospital | Hospital |
| NICHHD 1994 | Hospital | Hospital |
| Nielsen 2005 | Hospital | Not reported |
| Ocon 1997 | Unclear (in Spanish) | Unclear (in Spanish) |
| Roach 1997 | Hospital | Not reported |
| Sahraoui 2005 | Not reported | Not reported |
| Sande 1983 | Not reported | Not reported |
| Sargunam 2019 | Hospital Not stated by authors, however implied by the trial inclusion criteria: "persistent contractions after overnight hospitalisation > 8 h" |
Not reported |
| Suikkari 1983 | Hospital | Not reported |
| Tylleskar 1979 | "Two health clinics" | Health clinic where labour was induced |
| Walker 2016 | Not reported: "In the induction group, local policies for induction of labor were followed". | Not reported |
| Wennerholm 2019 | Not reported | Not reported |
| Witter 1987 | Hospital | Not reported |
Outcomes
The primary outcome of perinatal death was reported in 22 of the 34 included trials. Caesarean section was reported in 31 trials. Operative vaginal birth (forceps or ventouse) was reported in 22 trials. Apgar score less than seven at five minutes, birthweight and admission to neonatal intensive care unit, were reported in 20, 18 and 17 trials, respectively. Other outcomes, such as many of the adverse pregnancy and neonatal outcomes, were reported in fewer than half of the included trials. Only three trials reported on maternal satisfaction and only two reported on breastfeeding. No trials reported on maternal anxiety or depression.
Funding
Twelve of the 34 included trials reported their funding sources as follows: Karolinska Institute Foundations and Funds (Brane 2014); Ramathibodi Hospital Research Grants (Chanrachkul 2003; Herabutya 1992); Community Service Program of Kaiser Foundation Hospitals (Dyson 1987); Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grobman 2018); Medical Research Council of Canada (Hannah 1992); and Upjohn Company of Canada supplied the prostaglandin gel for this study; ZonMW: The Netherlands Organisation for Health Research and Development (Keulen 2019); Vicksburg Hospital Medical Foundation (Martin 1989); National Institute of Child Health and Human Development, NIH, USA (NICHHD 1994); University of Malaya (Sargunam 2019); other Research for Patient Benefit Programme of the National Institute for Health Research (Walker 2016); Swedish Government and county councils, Health Technology Centre at Sahlgrenska University Hospital, Foundation of the Health and Medical care committee of the Region of Vastra Gotaland, Sweden, Hjalmar Svensson Foundation, Foundation Mary von Sydow, born Wijk donation fund, Uppsala‐Orebro regional research council, region Orebro County research committee, ALF agreement in Stockholm, Centre for Clinical Research Dalama‐Uppsala University, Sweden (Wennerholm 2019).
One trial (Baev 2017) reported receiving no funding.
Twenty‐one of the 34 included trials did not report their funding sources.
Declarations of interest
Walker 2016 declared relevant interests on the part of one author, Dr Smith: "Dr. Smith reports receiving fees for serving on an advisory board from Roche Diagnostics, consulting fees from GlaxoSmithKline, equipment loans from Roche Diagnostics and General Electric, travel support from Roche Diagnostics and Chiesi, and grant support from GlaxoSmithKline and Action Medical Research, and being named as an inventor on a pending patent (PCT/EP2014/062602) filed by GlaxoSmithKline related to retosiban as a preventive treatment for preterm labour in women with increased uterine stretch". Grobman 2018 declared interests for one author: "Dr. Silver reports receiving consulting fees from Gestavision". The authors of these studies reported no other relevant potential conflict of interest. Keulen 2019 also declared interests from one author "BWM is supported by a National Health and Medical Research Council practitioner fellowship (GNT1082548) and reports consultancy for ObsEva, Merck, and Guerbet".
Baev 2017, Miller 2015 and Wennerholm 2019 declared no conflicts of interest.
None of the remaining 28 studies reported any declarations of interest.
Excluded studies
Most of the excluded trials were comparisons of different methods of labour induction (17 trials: Ascher‐Walsh 2000; De Aquino 2003; Evans 1983; Kipikasa 2005; Lee 1997; Lemancewicz 1999; Magann 1999; Mancuso 1998; Meydanli 2003; Misra 1994; Müller 1995; Papageorgiou 1992; Rijnders 2011; Satin 1991; Stenlund 1999; Su 1996; Surbek 1997) or cervical ripening protocols (28 trials: Bell 1993; Berghella 1996; Boulvain 1998; Buttino 1990; Damania 1992; Dare 2002; Doany 1997; Elliott 1984; El‐Torkey 1992; Giacalone 1998; Hage 1993; Ingemarsson 1987; Jenssen 1977; Kadar 1990; Klopper 1969; Lien 1998; Lyons 2001; Magann 1998; Newman 1997; Rayburn 1988; Rayburn 1999; Roberts 1986; Sawai 1991; Sawai 1994; Williams 1990; Wing 2000; Wong 2002; Ziaei 2003). Nine studies were not randomised trials (Amano 1999; Cardozo 1986; Garry 2000; Heden 1991; Hernandez‐Castro 2008; Iqbal 2004; Katz 1983; Knox 1979; Ohel 1996), in two trials pregnancies were not considered low risk (PACTR201805002872322; CTRI/2018/09/015719), and there were a variety of reasons for excluding the remaining 10 studies (Alcalay 1996; Conway 2000; Dunn 1989; Frass 2011; Gregson 2015; Imsuwan 1999; Neri 2014; Nicholson 2008; Paul 1988; Suzuki 1999). More details are provided in the Characteristics of excluded studies tables.
Risk of bias in included studies
Three trials (Chakravarti 2000; Cohn 1992; Suikkari 1983), were available only as abstracts and despite extensive searches we could not locate full publications of the studies, which limited our assessment of their risk of bias.
We judged the majority of included trials to be at low to moderate risk of bias (Figure 2; Figure 3), largely due to a lack of clear reporting.
2.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
We judged 18 trials (Augensen 1987; Baev 2017; Bergsjo 1989; Chanrachkul 2003; Dyson 1987; Grobman 2018; Heimstad 2007; James 2001; Keulen 2019; Martin 1978; Miller 2015; NICHHD 1994; Nielsen 2005; Sahraoui 2005; Sargunam 2019; Walker 2016; Wennerholm 2019; Witter 1987), to be at low risk of selection bias, reporting some form of adequate random sequencing such as a computer‐generated sequence or a list of random numbers. We judged the remaining 16 trials to be at unclear risk of selection bias, as they did not report how a random sequence was generated (Brane 2014; Breart 1982; Chakravarti 2000; Cohn 1992; Cole 1975; Egarter 1989; Gelisen 2005; Hannah 1992; Henry 1969; Herabutya 1992; Martin 1989; Ocon 1997; Roach 1997; Sande 1983; Suikkari 1983; Tylleskar 1979).
Of the 34 included trials, only 11 reported a method of allocation concealment likely to have a low risk of bias ‐ either central randomisation or sequentially numbered sealed opaque envelopes (Baev 2017; Grobman 2018; Hannah 1992; Heimstad 2007; Keulen 2019; Miller 2015; NICHHD 1994; Nielsen 2005; Sargunam 2019; Walker 2016; Wennerholm 2019). Eight trials reported that they used an envelope system with an unclear risk of bias (Brane 2014; Breart 1982; Dyson 1987; Gelisen 2005; James 2001; Martin 1989; Roach 1997; Witter 1987), one trial reported a partial third party system also with unclear risk of bias (Augensen 1987), and 14 trials did not report a method for concealing allocation and were rated as being at unclear risk of bias (Bergsjo 1989; Chakravarti 2000; Chanrachkul 2003; Cohn 1992; Cole 1975; Egarter 1989; Henry 1969; Herabutya 1992; Martin 1978; Ocon 1997; Sahraoui 2005; Sande 1983; Suikkari 1983; Tylleskar 1979).
Blinding
Performance bias
Given the nature of the intervention (induction of labour) and comparison (expectant management), it was not possible or not likely for women or clinicians to be blinded to the treatment group in any of the 34 trials, and thus risk of performance bias was judged to be high for 33 trials and unclear in Sargunam 2019. For the more objective outcomes such as perinatal death, this lack of blinding is unlikely to be a major source of bias.
Detection bias
It would have been possible for outcome assessment to have been undertaken by someone blinded to allocation groups, however, for the vast majority of studies (29), blinding, or lack of blinding, of outcome assessors was not explicitly stated. Keulen 2019 was assessed to be at low risk of detection bias, stating that "The statistician who performed the analyses was blinded to the allocation of the participants and performed the analysis according to a predefined analysis plan" and another trial (Martin 1978) reported blinded outcome assessment (also rated as low risk of bias). One study indicated partial blinding of outcome assessment (Hannah 1992), with an adjudication of abnormal neonatal outcomes undertaken by a neonatologist who was unaware of the mothers' group assignments (rated as unclear risk of bias). Grobman 2018 reported that assessment of neonatal primary outcomes "requiring review" were blinded, however, did not provide information regarding blinding of other outcome assessment (rated as unclear risk of bias). Wennerholm 2019 explicitly reported on the absence of blinding for outcome assessors (caregivers) and was thus rated as high risk of bias.
As above, measurement of objective outcomes such as perinatal death is unlikely to be influenced by lack of blinding.
Incomplete outcome data
We considered the majority of trials (24) (Augensen 1987; Baev 2017; Bergsjo 1989; Breart 1982; Chanrachkul 2003; Dyson 1987; Gelisen 2005; Grobman 2018; Hannah 1992; Heimstad 2007; Henry 1969; Herabutya 1992; James 2001; Keulen 2019; Martin 1989; Miller 2015; NICHHD 1994; Nielsen 2005; Ocon 1997; Roach 1997; Sahraoui 2005; Walker 2016; Wennerholm 2019; Witter 1987) to be at low risk of attrition bias, with minimal/no losses to follow‐up or exclusions. We judged seven trials to be at unclear risk of attrition bias (Brane 2014; Chakravarti 2000; Cohn 1992; Cole 1975; Egarter 1989; Sargunam 2019; Suikkari 1983), commonly due to some post‐randomisation exclusions and/or missing data, or due to insufficient information to determine losses or exclusions (due to publication in abstract form only).
We judged three trials to be at high risk of attrition bias. In both Martin 1978 and Tylleskar 1979, between 25% and 30% of the women randomised were excluded post‐randomisation due to going into labour prior to their planned date of induction (for women in the induction group), due to obstetric abnormalities or failure to go into spontaneous labour before 42 weeks (women in the expectant management group of Martin 1978), going into labour prior to their expected delivery date (women in the expectant management group of Tylleskar 1979). In Sande 1983, a per protocol analysis was performed, where women were not analysed in the group to which they were randomised, rather according to whether they had their labour induced, or delivered spontaneously.
Selective reporting
Only five trials (Grobman 2018; Keulen 2019; Sargunam 2019; Walker 2016; Wennerholm 2019) were judged to be at low risk of reporting bias, with outcomes reported as prespecified in the published protocol. We judged 23 trials (Baev 2017; Brane 2014; Breart 1982; Chakravarti 2000; Chanrachkul 2003; Cohn 1992; Cole 1975; Dyson 1987; Gelisen 2005; Hannah 1992; Heimstad 2007; Henry 1969; Herabutya 1992; James 2001; Martin 1978; Miller 2015; NICHHD 1994; Nielsen 2005; Ocon 1997; Roach 1997; Sahraoui 2005; Suikkari 1983; Witter 1987) to be at unclear risk of reporting bias, largely due to insufficient information to assess selective reporting (i.e. no access to trial protocols and limited detail reported in manuscript methods). We considered six trials (Augensen 1987; Bergsjo 1989; Egarter 1989; Martin 1989; Sande 1983; Tylleskar 1979), to be at high risk of reporting bias, predominately due to the incomplete reporting of outcomes data (such as in text or figures only, with statements such as "no significant difference between groups" made) such that outcome data could not be included in review meta‐analyses.
Other potential sources of bias
Most of the trials (25) (Augensen 1987; Baev 2017; Bergsjo 1989; Brane 2014; Breart 1982; Chanrachkul 2003; Cole 1975; Dyson 1987; Gelisen 2005; Grobman 2018; Hannah 1992; Heimstad 2007; Henry 1969; Herabutya 1992; James 2001; Martin 1989; Miller 2015; NICHHD 1994; Ocon 1997; Roach 1997; Sahraoui 2005; Sargunam 2019; Walker 2016; Wennerholm 2019; Witter 1987), appeared to be free of other potential sources of bias. We judged the other nine trials to be at unclear risk of bias, five trials due to limited reporting (abstract only or limited methodological detail provided) (Chakravarti 2000; Cohn 1992; Martin 1978; Suikkari 1983; Tylleskar 1979); one trial each for imbalance in the numbers of women randomised to each group (Egarter 1989), baseline characteristic imbalance (Nielsen 2005), lack of reporting of baseline characteristics (Sande 1983), and the systematically different care and assessment of neonates between groups (with the induction group receiving obstetrician‐led intrapartum secondary care, and a high proportion of the expectant management group receiving midwifery‐led primary care at both the start of labour and time of birth (Keulen 2019).
Effects of interventions
Labour induction versus expectant management (all trials)
Primary outcome
Perinatal death
Fewer perinatal deaths occurred in the labour induction groups than in the expectant management groups: four perinatal deaths occurred in the induction group compared with 25 in the expectant group: risk ratio (RR) 0.31, 95% confidence interval (CI) 0.15 to 0.64; 22 trials; 18,795 infants; high‐certainty evidence; Analysis 1.1.
1.1. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 1: Perinatal death
Interaction tests failed to demonstrate differences between the timing of induction subgroups for perinatal deaths (Chi² = 0.62, P = 0.73, I² = 0%; Analysis 2.1); parity (Chi² = 0.08, P = 0.77, I² = 0%; Analysis 3.1); or for subgroups according to state of cervix (Chi² = 0.01, P = 0.99, I² = 0%; Analysis 4.1). Rates of perinatal death by gestation are also presented in Table 7.
2.1. Analysis.

Comparison 2: Labour induction versus expectant management (subgroup analysis by gestational age at induction), Outcome 1: Perinatal death
3.1. Analysis.

Comparison 3: Labour induction versus expectant management (subgroup analysis by parity), Outcome 1: Perinatal death
4.1. Analysis.

Comparison 4: Labour induction versus expectant management (subgroup analysis by status of cervix), Outcome 1: Perinatal death
4. Rates of perinatal death by gestation.
| Week | IOL | Expectant | ||
| rate/1000 | rate/1000 | |||
| 37 | 0 | 0 | 0 | 0 |
| 38 | 0/111 | 0 | 1/117 | 8.5 |
| 39 | 2/3455 | 0.6 | 4/3443 | 1.2 |
| 40‐41 | 0/380 | 0 | 1/380 | 2.6 |
| ≥ 42 | 2/5472 | 0.37 | 19/5437 | 3.5 |
IOL:induction of labour
Two trials reported perinatal death by parity ‐ Keulen 2019 reported three stillbirths (one in a nulliparous woman and one in a multiparous woman in the expectant management group; and one in a multiparous woman in the induction group); and in Wennerholm 2019 all six perinatal deaths (five stillbirths and one neonatal death) occurring in the expectant management group in nulliparous women.
Some trials (e.g. Hannah 1992), excluded perinatal deaths due to congenital anomalies while other trials included these. If the three deaths reported to be due to congenital anomalies in other trials were excluded, there were then a total of three deaths in the labour induction group and 23 in the expectant management group. This made little difference to the overall result (RR 0.30, 95% CI 0.14 to 0.64).
Table 2 details, where known, the respective causes of death (stillbirths and neonatal deaths) for 19 babies, including the stillbirth reported in Martin 1978 (where it was not clear if there were any neonatal deaths).
The number needed to treat for an additional beneficial outcome (NNTB) with a policy of induction of labour in order to prevent one perinatal death was 544 (95% CI 441 to 1042).
Twelve trials, (Baev 2017; Brane 2014; Breart 1982; Chakravarti 2000; Cohn 1992; Miller 2015; Nielsen 2005; Ocon 1997; Roach 1997; Sargunam 2019; Tylleskar 1979; Witter 1987), did not report on perinatal deaths.
Sensitivity analyses
Only 10 of the 34 trials were judged to be of low risk of bias, defined as adequate allocation concealment and low attrition (Baev 2017; Grobman 2018; Hannah 1992; Heimstad 2007; Keulen 2019; Miller 2015; NICHHD 1994; Nielsen 2005; Walker 2016; Wennerholm 2019). We have presented each of the sensitivity analyses under each of the relevant prespecified outcomes.
Perinatal death ‐ sensitivity analysis: RR 0.29, 95% CI 0.10 to 0.83; seven trials, 15,539 infants. There were three perinatal deaths in the induction group and 14 perinatal deaths in the expectant management group. This sensitivity analysis was similar to the overall analysis (RR 0.31, 95% CI 0.15 to 0.64), favouring induction over expectant management.
Secondary outcomes for the infant/child
Stillbirth
Eighteen of the 25 perinatal deaths were stillbirths. Two stillbirths occurred in the induction group and 16 stillbirths occurred in the expectant management group (RR 0.30, 95% CI 0.12 to 0.75; 22 trials; 18,795 infants; high‐certainty evidence; Analysis 1.2). Interaction tests failed to demonstrate differences between the timing of induction subgroups (Chi² = 0.49, P = 0.78, I² = 0%; Analysis 2.2) or for subgroups according to by parity (Chi² = 0.13, P = 0.72, I² = 0%; Analysis 3.2) or state of cervix (Chi² = 0.01, P = 0.99, I² = 0%; Analysis 4.2) for the outcome of stillbirth.
1.2. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 2: Stillbirth
2.2. Analysis.

Comparison 2: Labour induction versus expectant management (subgroup analysis by gestational age at induction), Outcome 2: Stillbirth
3.2. Analysis.

Comparison 3: Labour induction versus expectant management (subgroup analysis by parity), Outcome 2: Stillbirth
4.2. Analysis.

Comparison 4: Labour induction versus expectant management (subgroup analysis by status of cervix), Outcome 2: Stillbirth
Sensitivity analyses
Stillbirth ‐ sensitivity analysis: RR 0.27, 95% CI 0.08 to 0.98; seven trials, 15,539 infants, with two stillbirths in the induction group and 10 stillbirths in the expectant management group. This sensitivity analysis was similar to the overall analysis (RR 0.30, 95% CI 0.12 to 0.75), favouring induction over expectant management.
Neonatal death
There were 11 live birth deaths ‐ two of these were in the induction group and nine were in the expectant management groups (RR 0.39, 95% CI 0.13 to 1.14; 21 trials; 18,611 infants; Analysis 1.3).
1.3. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 3: Neonatal death
Birth asphyxia
Rates of birth asphyxia were not clearly different between the induction and expectant management groups (RR 1.66, 95% CI 0.61 to 4.55: four trials; 1456 infants; Analysis 1.4).
1.4. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 4: Birth asphyxia
Admission to neonatal intensive care unit (NICU)
Rates of NICU admissions were lower when labour induction was compared with expectant management (RR 0.88, 95% CI 0.80 to 0.96; 17 trials; 17,826 infants; high‐certainty evidence; Analysis 1.5).
1.5. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 5: Admission to neonatal intensive care unit
Interaction tests failed to demonstrate differences between the timing of induction subgroups (Chi² = 1.67, P = 0.43, I² = 0%; Analysis 2.3) or for subgroups according to parity (Chi² = 2.03, P = 0.36, I² = 1.4%; Analysis 3.3) or state of cervix (Chi² = 0.81, P = 0.67, I² = 0%; Analysis 4.3) for the outcome of NICU admission.
2.3. Analysis.

Comparison 2: Labour induction versus expectant management (subgroup analysis by gestational age at induction), Outcome 3: Admission to neonatal intensive care unit
3.3. Analysis.

Comparison 3: Labour induction versus expectant management (subgroup analysis by parity), Outcome 3: Admission to neonatal intensive care unit
4.3. Analysis.

Comparison 4: Labour induction versus expectant management (subgroup analysis by status of cervix), Outcome 3: Admission to neonatal intensive care unit
Sensitivity analyses
Admission to the NICU ‐ sensitivity analysis: RR 0.87, 95% CI 0.79 to 0.96; nine trials, 15,709 infants. This was very similar to the overall analysis (RR 0.88, 95% CI 0.80 to 0.96).
Neonatal convulsions
There were no clear differences in instances of neonatal convulsions when labour induction was compared with expectant management (average RR 1.01, 95% CI 0.15 to 6.67; Tau² = 2.25; Chi² = 7.96, P = 0.05; I² = 62%; 5 trials, 13,216 infants; Analysis 1.6). The heterogeneity may be due to Grobman 2018 (who reported seizures).
1.6. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 6: Neonatal convulsions
Neonatal encephalopathy (HIE)
Two trials reported neonatal encephalopathy (HIE), indicating little or no difference between the induction and expectant groups (RR 0.69, 95% CI 0.37 to 1.31; 8851 infants; low‐certainty evidence; Analysis 1.7).
1.7. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 7: Neonatal encephalopathy (HIE)
Use of anticonvulsants
No clear differences between induction and expectant groups were evident for use of anticonvulsants in a single trial (RR 0.34, 95% CI 0.01 to 8.17; 349 infants; Analysis 1.8).
1.8. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 8: Use of anticonvulsants
Meconium aspiration syndrome
There was a 25% relative reduction in the risk of meconium aspiration syndrome in the induction groups compared with the expectant management groups (RR 0.75, 95% CI 0.62 to 0.92; 13 trials; 16,622 infants; Analysis 1.9).
1.9. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 9: Meconium aspiration syndrome
Pneumonia
In two trials, there was a possibly decreased incidence of pneumonia in the induction group compared with the expectant management group (RR 0.54, 95% CI 0.27 to 1.06; 8851 infants; Analysis 1.10).
1.10. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 10: Pneumonia
Apgar score less than seven at five minutes
Probably fewer babies had Apgar scores less than seven at five minutes in the induction groups compared with the expectant management groups (RR 0.73, 95% CI 0.56 to 0.96; 20 trials; 18,345 infants; moderate‐certainty evidence; Analysis 1.11). Several trials reported different cut‐offs for Apgar scores but omission of these results made little difference to the overall result.
1.11. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 11: Apgar score less than 7 at 5 minutes
Birthweight (g)
On average, infants born to mothers in the induction group had lower birthweights than those born to mothers in the expectant management group (mean difference (MD) ‐59.38 g, 95% CI ‐77.03 to ‐41.73; 18 trials; 8817 infants; Analysis 1.12).
1.12. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 12: Birthweight (g)
Grobman 2018 reported birthweights as median and interquartile ranges (IQR), also showing lower birthweights in the induction group (median 3330 g IQR 3040 to 3565) compared with the expectant management group (median 3380 g IQR 3110 to 3650); P < 0.001.
Birthweight greater than 4000 g
There was a 28% relative reduction in the rate of macrosomia (greater than 4000 g) in the labour induction groups (average RR 0.72, 95% CI 0.54 to 0.96; 8 trials; 5593 infants; Tau² = 0.09; Chi² = 20.84, P = 0.004; I² = 66%; Analysis 1.13) (Hannah 1992 used a cutoff‐of 4500 g rather than 4000 g for this outcome). Removal of Gelisen 2005 from the analysis for this outcome (which still observed a substantial beneficial effect, with 23/300 macrosomic infants born to women in the induction group, versus 74/300 infants to women in the expectant management group), eliminated the observed heterogeneity.
1.13. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 13: Birthweight > 4000 g
Neonatal (birth) trauma
Meta‐analysis of data from five trials suggests that induction makes little or no differencein rates of birth trauma in newborns and expectant management (RR 0.97, 95% CI 0.63 to 1.49; 13,106 infants; moderate‐quality evidence; Analysis 1.14).
1.14. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 14: Neonatal (birth) trauma
Unreported outcomes
No trials reported on neurodevelopment at childhood follow‐up (although Bergsjo 1989 reported no signs of neurological impairment in children at two years of age).
Secondary outcomes for the mother
Caesarean section
There were probably fewer caesarean sections (a relative reduction of 10%) in the induction groups compared with the expectant management groups on meta‐analysis of data from 31 trials (RR 0.90, 95% CI 0.85 to 0.95; 21,030 women; moderate‐certainty evidence; Analysis 1.15). This equates to a reduction of nearly 2% (from a rate of 18.6% in the expectant management group to 16.7% in the induction group). Subgroup interaction tests did not show clear differences according to timing of induction (Chi² = 3.70, P = 0.16, I² = 45.9%; Analysis 2.4), by parity (Chi² = 1.84, P = 0.40, I² = 0%; Analysis 3.4) or by state of cervix (Chi² = 1.60, P = 0.45, I² = 0%; Analysis 4.4) for this outcome.
1.15. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 15: Caesarean section
2.4. Analysis.

Comparison 2: Labour induction versus expectant management (subgroup analysis by gestational age at induction), Outcome 4: Caesarean section
3.4. Analysis.

Comparison 3: Labour induction versus expectant management (subgroup analysis by parity), Outcome 4: Caesarean section
4.4. Analysis.

Comparison 4: Labour induction versus expectant management (subgroup analysis by status of cervix), Outcome 4: Caesarean section
Sensitivity analyses
Caesarean section sensitivity analysis: RR 0.90, 95% CI 0.84 to 0.96; 10 trials, 16,075 women. These results are very similar to the overall analysis (RR 0.90, 95% CI 0.85 to 0.95).
Operative vaginal birth (forceps or ventouse)
Rates of operative vaginal birth showed little or no difference between the policy of labour induction and expectant management groups (RR 1.03, 95% CI 0.96 to 1.10; 22 trials, 18,584 women; moderate‐certainty evidence; Analysis 1.16). This equates to an increase of 0.4% (from a rate of 13.6% in the expectant management group to 14% in the induction group). Subgroup interaction tests did not show clear differences according to timing of induction (Chi² = 1.14, P = 0.57, I² = 0%; Analysis 2.5), parity (Chi² = 1.62, P = 0.44, I² = 0%; Analysis 3.5) or by state of cervix (Chi² = 0.73, P = 0.70, I² = 0%; Analysis 4.5) for this outcome.
1.16. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 16: Operative vaginal birth (forceps or ventouse)
2.5. Analysis.

Comparison 2: Labour induction versus expectant management (subgroup analysis by gestational age at induction), Outcome 5: Operative vaginal birth (forceps or ventouse)
3.5. Analysis.

Comparison 3: Labour induction versus expectant management (subgroup analysis by parity), Outcome 5: Operative vaginal birth (forceps or ventouse)
4.5. Analysis.

Comparison 4: Labour induction versus expectant management (subgroup analysis by status of cervix), Outcome 5: Operative vaginal birth (forceps or ventouse)
Sensitivity analyses
Operative vaginal birth sensitivity analysis: RR 0.99, 95% CI 0.92 to 1.07; 8 trials, 15,565 women. This was similar to the overall analysis (RR 1.03, 95% CI 0.96 to 1.10).
Analgesia used
There was little or no difference in the use of epidural/regional analgesia between induction and expectant management groups (average RR 1.09, 95% CI 0.99 to 1.20; 8 trials, 4579 women; Tau² = 0.01; Chi² = 24.41, P = 0.001; I² = 71%) (Analysis 1.17). A possible increased use of analgesia (variously defined) was observed with labour induction, compared with expectant management (average RR 1.11, 95% CI 1.05 to 1.18; 4 trials, 2352 women) (Analysis 1.17).
1.17. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 17: Analgesia used
Perineal trauma
Probably little or no difference in perineal trauma, assessed as severe perineal tear, was seen between induction and expectant management (RR 1.04, 95% 0.85 to 1.26; 5 trials; 11,589 women; low‐certainty evidence (Analysis 1.18). For episiotomy (RR 0.96, 95% CI 0.84 to 1.11; 2 trials; 1747 women; and obstetrical and sphincter injuries (RR 0.81, 95% CI 0.51 to 1.31; 2 trials; 1698 women) there were probably little or no differences between induction and expectant management (Analysis 1.18).
1.18. Analysis.
Comparison 1: Labour induction versus expectant management (all trials), Outcome 18: Perineal trauma
Interaction tests, performed for perineal trauma (assessed as severe perineal tear), failed to detect any differences for subgroups by timing of induction (Chi² = 1,89, P = 0.17, I² = 47.2% Analysis 2.6), by parity (Chi² = 1.89, P = 0.17, I² = 47.2%; Analysis 3.6) or by state of cervix (tests for subgroup differences: not applicable) for this outcome.
2.6. Analysis.

Comparison 2: Labour induction versus expectant management (subgroup analysis by gestational age at induction), Outcome 6: Perineal trauma
3.6. Analysis.

Comparison 3: Labour induction versus expectant management (subgroup analysis by parity), Outcome 6: Perineal trauma (severe perineal tear)
Sensitivity analyses
Sensitivity analysis for perineal trauma (severe perineal tear): all five trials reporting this outcome were judged to not be at high risk of bias and so the sensitivity analysis is the same as the overall analysis.
Prolonged labour
The outcome of prolonged labour was reported in several different ways by four trials with 1009 women, with none of the four comparisons showing clear differences between the induction and expectant management groups (Analysis 1.19).
1.19. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 19: Prolonged labour
Postpartum haemorrhage
There was probably no or little difference in rates of postpartum haemorrhage (variously defined) for induction and expectant management groups (RR 1.02, 95% CI 0.91 to 1.15; 9 trials, 12,609 women; moderate‐certainty evidence; Analysis 1.20).
1.20. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 20: Postpartum haemorrhage
Breastfeeding
There was probably no or little differences between induction and expectant groupsfor breastfeeding (at discharge in one trial; and at four to eight weeks after discharge in the other trial) (RR 1.00, 95% CI 0.96 to 1.04; 7487 infants; moderate‐certainty evidence ‐ Analysis 1.21).
1.21. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 21: Breastfeeding
Maternal satisfaction
In one trial of 496 women, more women in the induction group said that they would choose the same arm in a future trial compared with women in the expectant management group (RR 1.93, 95% CI 1.62 to 2.30), but in two other trials, similar numbers of women indicated that they preferred the group they had been allocated to (RR 0.99, 95% CI 0.88 to 1.13; 493 women; Analysis 1.22). Sargunam 2019 also reported little or no difference in satisfaction with pregnancy outcomes between groups (RR 0.92 95% CI 0.80 to 1.06; 308 women; Analysis 1.22). Walker 2016 reported little or no difference in Childbirth Experience Questionnaire scores (four‐point scale; higher scores indicate higher satisfaction) between women in the induction or expectant management groups (MD 0.07, 95% CI ‐0.02 to 0.16; 619 women; Analysis 1.23).
1.22. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 22: Maternal satisfaction
1.23. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 23: Maternal satisfaction
Grobman 2018 also reported slightly higher scores on the Labor Agentry Scale, indicating greater perceived control during childbirth in the induction group; and also reported that women in the induction group reported less pain than women in the expectant management group.
Unreported outcomes
No trials reported on anxiety before birth or postnatal depression.
Secondary outcomes relating to health service use
Length of maternal postnatal stay (days)
It is very uncertain whether there is any difference between induction or expectant management for duration of maternal hospital stay (average MD ‐0.19 days, 95% CI ‐0.56 to 0.18; 7 trials; 4120 women; very low‐quality evidence; Analysis 1.24). There was very substantial heterogeneity (Tau² = 0.20; Chi² = 104.20, P < 0.00001; I² = 94%) between the trials for this outcome.
1.24. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 24: Length of maternal hospital stay (days)
Length of maternal postnatal stay (days, categories)
One trial of 6091 women reported five maternal postnatal stay categories (Grobman 2018) indicating slightly more women in the induction group stayed two days and slightly fewer women in the induction group stayed 3 or 4 days (Analysis 1.25).
1.25. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 25: Length of maternal (postnatal) stay (categories)
Length of neonatal hospital stay (days)
In one trial of 302 babies, there was a slightly shorter mean hospital stay for the induction group compared with the expectant management group (MD ‐0.30 days, 95% CI ‐0.61 to 0.01; Analysis 1.26).
1.26. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 26: Length of neonatal hospital stay (days)
Length of neonatal postnatal stay (days, categories)
One trial of 6091 infants reported length of neonatal postnatal stay as five categories, which we collapsed into ≤ 2 days and ≥ 3 days. Infants in the induction group were more likely to stay ≤ 2 days than those in the expectant group (RR 1.05, 95% CI 1.02 to 1.08) and correspondingly less likely to stay ≥ 3 days (RR 0.86, 95% CI 0.79 to 0.94) (Analysis 1.27).
1.27. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 27: Length of neonatal (postnatal) stay (categories)
Length of labour (hours)
Overall, length of labour was shorter for women undergoing induction compared with expectant management (average MD ‐1.08 hours, 95% CI ‐1.67 to ‐0.50; 12 trials; 4025 women; Tau² = 0.84; Chi² = 46.70, P < 0.0001; I² = 72%; Analysis 1.28).
1.28. Analysis.

Comparison 1: Labour induction versus expectant management (all trials), Outcome 28: Length of labour (hours)
Funnel plots
We assessed funnel plots for the outcomes: perinatal death (Figure 4), stillbirth (Figure 5), neonatal death (Figure 6), admission to NICU (Figure 7), meconium aspiration syndrome (Figure 8), Apgar score less than seven at five minutes (Figure 9), birthweight (Figure 10), caesarean section (Figure 11), operative vaginal birth (Figure 12), postpartum haemorrhage (Figure 13) and length of labour (Figure 14).
4.

Funnel plot of comparison: 1 Labour induction versus expectant management (all trials), outcome: 1.1 Perinatal death.
5.

Funnel plot of comparison: 1 Labour induction versus expectant management (all trials), outcome: 1.2 Stillbirth.
6.

Funnel plot of comparison: 1 Labour induction versus expectant management (all trials), outcome: 1.3 Neonatal death.
7.

Funnel plot of comparison: 1 Labour induction versus expectant management (all trials), outcome: 1.5 Admission to neonatal intensive care unit.
8.

Funnel plot of comparison: 1 Labour induction versus expectant management (all trials), outcome: 1.9 Meconium aspiration syndrome.
9.

Funnel plot of comparison: 1 Labour induction versus expectant management (all trials), outcome: 1.11 Apgar score less than 7 at 5 minutes.
10.

Funnel plot of comparison: 1 Labour induction versus expectant management (all trials), outcome: 1.12 Birthweight (g).
11.

Funnel plot of comparison: 1 Labour induction versus expectant management (all trials), outcome: 1.15 Caesarean section.
12.

Funnel plot of comparison: 1 Labour induction versus expectant management (all trials), outcome: 1.16 Operative vaginal birth (forceps or ventouse).
13.

Funnel plot of comparison: 1 Labour induction versus expectant management (all trials), outcome: 1.20 Postpartum haemorrhage.
14.
Funnel plot of comparison: 1 Labour induction versus expectant management (all trials), outcome: 1.28 Length of labour (hours).
Some visual asymmetry may be apparent for meconium aspiration syndrome (Figure 8); birthweight (Figure 10) and postpartum haemorrhage (Figure 13). Funnel plots for perinatal death (Figure 4), stillbirth (Figure 5), and neonatal death (Figure 6) were difficult to visually interpret.
Discussion
Summary of main results
In this updated review, we included 34 randomised controlled trials (reporting on 21,563 women).
We included pregnant women at or beyond 37 weeks' gestation. Since a risk factor at this stage of pregnancy would normally require an intervention, only trials including women at low risk for complications were eligible. We accepted the trialists' definition of 'low risk'. The trials of induction of labour in women with prelabour rupture of membranes at or beyond 37 weeks were not considered in this review.
A policy of labour induction reduced perinatal deaths (with four perinatal deaths in the labour induction policy group compared with 25 perinatal deaths in the expectant management group) (high‐certainty evidence). When restricted to a policy of induction at later gestational ages (> 41 weeks), there were two and 13 perinatal deaths, respectively. While subgroup interaction tests did not have sufficient power to assess whether perinatal mortality differed by week of gestation, the rate of perinatal deaths in the expectant management compared to the induction group for gestational age > 42 weeks, 3.5 deaths per 1000, was higher than the rate of perinatal deaths for gestational age 40 to 41 weeks (2.6 deaths per 1000) and 39 weeks (1.2 deaths per 1000); see Table 7.
Although some trials excluded deaths from congenital anomalies, other trials did not exclude these deaths. When the three deaths reported to be due to congenital anomalies were excluded, the overall findings remained very similar. Induction of labour also reduced stillbirth compared with expectant management (two versus 16 in the expectant management group), (high‐certainty evidence).
A policy of labour induction probably reduced caesarean section compared with expectant management (moderate‐certainty evidence) and probably had no or little impact on operative vaginal birth compared with expectant management (moderate‐certainty evidence). Induction of labour also reduced neonatal intensive care unit admission (high‐certainty evidence), and probably reduced the occurrence of Apgar scores less than seven at five minutes (moderate‐certainty evidence), compared with expectant management. Induction of labour probably made no or little difference for neonatal trauma, postpartum haemorrhage and breastfeeding compared with expectant management (moderate‐certainty evidence); and may lead to no or little difference in neonatal encephalopathy and perineal trauma (low‐certainty evidence). The effect of labour induction compared with expectant management on length of maternal hospital stay was uncertain (very low‐certainty evidence). Neurodevelopment at childhood follow‐up and postnatal depression were not reported by any of the included trials.
No clear differences by timing of induction (< 40 weeks versus 40 to 41 weeks versus > 41 weeks), cervical status (favourable versus unfavourable versus mixed), or parity (nulliparous versus multiparous versus mixed) were apparent in subgroup analyses for the main outcomes of this review.
For the sensitivity analyses, all six prespecified outcomes demonstrated results in the same direction as the main analyses and there was little material difference in the overall result.
This review evaluates trials where a policy of induction has been compared with a policy of waiting. However, women scheduled to be induced may not have ended up being induced; and women allocated to wait may have ended up being induced (Keirse 2010). For example, about one‐third of the women randomised to the induction policy group in the Hannah trial were not induced; and about one‐third of the women randomised to waiting or expectant management were induced (Hannah 1992).
Overall completeness and applicability of evidence
The body of evidence for this review is now quite extensive, including 34 trials and over 20,000 women. This has been sufficient to detect a difference in perinatal death between the induction and expectant management groups. The decrease seen in caesarean section with a policy of induction has been previously questioned by some authors (Keirse 2010; Mandruzzato 2010). They have suggested that the women in the large Hannah 1992 trial who were induced in the policy of induction group (66% of this group), may have had a more effective cervical ripening regimen (prostaglandin) than the women who were induced in the expectant management group (33% of this group), and that more women in the expectant management group had a caesarean section for fetal distress (8.3% versus 5.7% in the induction group) (Keirse 2010;Mandruzzato 2010). Since review results for caesarean section were similar when the Hannah 1992 trial was omitted, this is not likely to have been the reason for the effect observed.
The trials included in this review employed a wide range and combinations of induction methods (see Characteristics of included studies), and it was not possible to assess differences in outcomes by method of induction through conducting subgroup analyses. Trials were conducted in different countries and consequently this review reflects a range of strategies for both induction of labour, and expectant management, across trials.
Some women with post‐term pregnancies have described this period of unexpected waiting as being in a state of limbo, with increasingly negative feelings as the pregnancy continues, which could be addressed with more information and support from their healthcare professionals (Wessberg 2017). Our review highlighted the lack of information measured and reported by randomised trials to date, with only five (Grobman 2018; Heimstad 2007; Martin 1978; Sargunam 2019; Walker 2016) of the 34 included studies reporting some measure of maternal satisfaction. A recent systematic review of qualitative evidence included five studies addressing women's experiences and perceptions of induction of labour for uncomplicated post‐term pregnancy, highlighting the importance of women's understanding of induction in influencing their choices, decision‐making, and thus satisfaction ‐ and emphasised the need for "in‐depth and clear unbiased individualized information and education on alternatives and details of procedures as well as risks and benefits" (Akuamoah‐Boateng 2018).
As noted above, the randomised trials conducted to date have not provided data regarding longer‐term neurodevelopmental outcomes for children, and cohort studies have shown inconsistent results as to whether post‐term birth has a negative, positive or null impact on childhood development. A large cohort study from Denmark has suggested that more children born at 41 weeks' gestation or later achieved developmental milestones compared with children born at earlier term gestations (39 to 40 weeks) (Olesen 2015). A further large cohort study from Australia demonstrated elevated risks of poor child development at school age with early (at < 39 weeks' gestation) planned birth compared with birth at later gestations (Bentley 2016).
Assessment of intervention cost‐effectiveness was beyond the scope of our review, however, three of the included trials have reported data related to costs. In the Hannah 1992 trial, the mean cost of a woman undergoing induction for a post‐term pregnancy was $193 lower than for a woman managed expectantly, due mainly to the costs of additional monitoring and the significantly higher rates of caesarean section among women assigned to expectant management. Walker 2017 reported that induction of labour at 39 weeks, specifically for nulliparous women aged 35 years and over, is associated with a mean cost saving of £263 and a small additional gain in QALYs (without considering QALY gains from stillbirth prevention). A health utilisation study (based on the Grobman 2018 trial) (Grobman 2020) found that while low risk nulliparous women, assigned to induction of labour at 390 to 394 weeks spent more time on the labour and delivery suite (thus using more resources specific to induction), they had fewer antenatal visits and tests, fewer intrapartum interventions, and shorter postnatal stays, compared with women assigned to expectant management; and concluded "that the health outcome advantages associated with induction of labour are gained without incurring uniformly greater health care resource use".
Quality of the evidence
Included trials were generally at low to moderate risk of bias. Aspects of methodological quality were unclear for many of the included trials (Figure 2; Figure 3).
Most of the outcomes assessed using GRADE had a rating of high‐ or moderate‐certainty evidence (see Table 1; Table 3) ‐ with downgrading decisions generally due to study limitations such as risk of selection bias, or imprecise effect estimates. Postpartum haemorrhage was downgraded to moderate due to indirectedness.
However, for the majority of outcomes assessed using GRADE, statistical heterogeneity was mostly low, countering claims (e.g. Davey 2016), that some of the trials had unreliable results due to being outdated or flawed. One outcome (length of maternal stay) was downgraded to very low‐certainty evidence (due to inconsistency) and two outcomes (neonatal encephalopathy and perineal trauma (severe perineal tear)) were downgraded for imprecision.
Potential biases in the review process
Due to the rigorous methods used (comprehensive searching, double screening and data extraction, and careful appraisal and analysis), biases are likely to be low.
As mentioned above, there have been several criticisms of trials and reviews on this topic. Wood 2014 and colleagues point out that the decision to perform a caesarean section is often subjective, and anxiety from medical staff about the dangers of a prolonged pregnancy may be a factor in determining when to carry out a caesarean, as could factors such as fetal distress or fetal size. They also make the observation, whatever the reason(s) may be, that this does not change the fact that induction has shown reduced risk of caesarean section in clinical trials of induction of labour versus expectant management in women with intact membranes.
We investigated reporting biases (such as publication bias) using funnel plots for prespecified outcomes, with a small number demonstrating some asymmetry. This could indicate possible reporting bias, with the smaller published trials reporting exaggerated intervention effect estimates, and there remains the possibility that further small trials (including those reporting smaller effect estimates) remain unpublished.
Agreements and disagreements with other studies or reviews
Both observational studies and systematic reviews of randomised controlled trials of timing of induction have shown mixed findings for important outcomes including perinatal death and caesarean section rates (Davey 2016).
Wood 2014 is the most comparable systematic review and meta‐analysis in terms of included studies, though they only reported a single outcome, caesarean section. Across 27 trials in women between 37 and 42 weeks' gestation, they found a similar reduction with a policy of induction as our review. The Mishanina 2014 systematic review and meta‐analysis of induction versus expectant management at any gestational age also found a reduction in caesarean birth for inductions from 37 weeks onwards (but not if induction was at less than 37 weeks), along with an overall reduction in fetal death with induction. The recent Saccone 2019 systematic review and meta‐analysis, included only seven trials (7598 women) in women with uncomplicated singleton pregnancies at term (defined as 390 to 406 weeks) ‐ all seven trials were included in our review. While the authors did not demonstrate reductions in the risks of caesarean section or perinatal death as we have, they stated that they recognised the review was not powered for these outcomes. The Sotiriadis 2019 systematic review and meta‐analysis including women with singleton uncomplicated pregnancies, randomised between 390 and 396 weeks) ‐ a 'subset' of the Saccone 2019 review. Sotiriadis 2019 did demonstrate a reduction in caesarean section as was observed in our review. The difference in findings between Saccone 2019 and Sotiriadis 2019 appear to be largely attributable to the high rate of caesarean section in the induction group in the Miller 2015 trial (25/82 in induction group versus 14/79 in expectant group) (included in Saccone 2019 but not Sotiriadis 2019), which randomised women with an unfavourable cervix at 380 to 386 weeks.
Recent mathematical modelling (Monte Carlo microsimulation) has revealed similar findings to our review, however specifically in relation to nulliparous women at 39 weeks with uncomplicated, singleton, vertex pregnancies (Sinkey 2018). Maternal and neonatal risks (including caesarean section, maternal morbidity, stillbirth, neonatal death and neonatal morbidity) were lower with induction of labour, as compared with expectant management, including induction at 41 weeks if a woman has still not given birth (Sinkey 2018). The Keulen 2018 review was conducted specifically to focus on studies of comparisons of induction within the 41 to 42 weeks' gestation timeframe, to assess the outcomes of perinatal mortality, meconium aspiration syndrome and caesarean section. Only four trials were considered to have comparisons relevant to this timing of induction, and the authors concluded that evidence for the recommendation to induce labour at 41 weeks instead of 42 weeks for improved perinatal outcomes was lacking (Keulen 2018).
While a major concern surrounding elective induction at > 37 weeks, particularly in first pregnancies, has been increased risk of caesarean section (Davey 2016), such studies have been largely observational in nature, and increasingly, there is evidence to the contrary (Souter 2019). In a recent scoping review of clinical indications for induction, 15 studies related to induction of labour for post‐term pregnancy (> 40 weeks) were identified; this included the previous version of our review (Middleton 2018), the Keulen 2018 review, the Keulen 2019 trial, and 12 observational studies (one prospective cohort, nine retrospective cohorts, and two secondary analyses of cohort studies) (Coates 2020). Based on the totality of evidence, the authors concluded that induction of labour beyond 41 to 42 weeks was associated with reductions in perinatal death and caesarean section, though recognising the high NNT for perinatal death.
While the subgroup interaction tests for our main outcomes (perinatal death, stillbirth, admission to NICU, caesarean section, operative vaginal birth, perinatal trauma) did not demonstrate any clear differential effects of induction based on gestational age (< 40 weeks, 40 to 41 weeks, > 41 weeks), over 72% of perinatal deaths reported were in the > 41 week subgroup.
In addition to factors explored in our review's subgroup analysis (gestational age, parity, cervical status), there are various other factors that are likely to impact outcomes following induction (and may explain some discrepancies observed between studies), such as indications for caesarean section, and maternal age. For example, in an Australian retrospective cohort study (17,647 women), among nulliparous women, induction of labour at 38 to 39 weeks was shown to be associated with an increased risk of caesarean section in young women (< 25 years of age), but not associated with caesarean section for slow progress (De Vries 2019). Conversely, induction of labour at 38 to 39 weeks was associated with an increased risk of caesarean section for suspected fetal compromise among nulliparous women < 30 years (De Vries 2019). In a retrospective registry‐based study from Denmark, Finland, Iceland, Norway and Sweden (involving 3,398,586 births), advanced maternal age was associated with an increased risk of caesarean section among women undergoing induction of labour at term with singleton pregnancies without previous caesarean sections; with the absolute risk being three to five times higher across five‐year age groups in nulliparous relative to multiparous women (Bergholt 2020). It is important, however, to distinguish between different methodological approaches where comparing labour induction to spontaneous onset of labour in a retrospective cohort (instead of a prospective assessment of expectant management of pregnancy) which may lead to exaggerated estimates of the risk of caesarean birth, for example (Danilack 2016). Moreover, in our review, there did not appear to be any differential effect of caesarean section by baseline rates of studies.
Many of the current relevant clinical practice guidelines recommend offering women induction of labour after 41 completed weeks of gestation (ACOG 2014; New Zealand Guideline Development Panel 2019; NICE 2008; SOGC 2017; WHO 2018). The most recent WHO guidelines provide a recommendation for induction of labour for women who are known with certainty to have reached 41 weeks; they highlight that the guidance does not apply to settings where gestational age cannot be reliably established and the importance of discussing the potential need for induction with women in advance to provide opportunity for women to understand benefits and possible risks (WHO 2018). These guidelines were based on the previous version of this review (Middleton 2018), in which the evidence for some critical outcomes (including perinatal death, stillbirth, admission to the neonatal intensive care) were judged to be of lower certainty than this update which incorporates new evidence of higher certainty.
Authors' conclusions
Implications for practice.
The main message from this review is that a policy of induction of labour at or beyond term is associated with fewer perinatal deaths, including stillbirths (although the absolute risk reduction is small), with a reduced risk of caesarean section and little or no difference in operative vaginal birth. If women are offered the option of labour induction, it may be helpful for health professionals to provide information and resources about the absolute and relative risks of perinatal death at different gestational age time points. Recognising that women's assessments, circumstances, values and preferences may differ, ideally use of these resources would be tailored accordingly. If a woman chooses to wait for spontaneous labour onset, it may be prudent to have regular fetal monitoring, as longitudinal epidemiological studies suggest increased risk of perinatal death by increasing gestational age.
Implications for research.
The optimal timing of offering induction of labour to women at or beyond 37 weeks' gestation needs further investigation, as does further exploration of risk profiles of women and their values and preferences. While existing trials have not yet reported on childhood neurodevelopment, this is an important area for future research.
Feedback
Marowitz, 14 April 2011
Summary
Both my students and myself are unable to understand the following sentence in text for ‘Effects of the intervention':
"Women induced at 37 to 40 completed weeks were more likely to have a caesarean section with expectant management than those in the labour induction group (RR 0.58; 95% CI 0.34 to 0.99)."
Are there errors in the wording of this sentence?
[Comment submitted by Amy Marowitz, April 2011]
Reply
Thank you for your feedback. We have corrected the error.
Contributors
A Metin Gülmezoglu
Keulen et al, 1 August 2020
Summary
With great interest we have read the recently published updated review by Middleton et al on Induction of labour at or beyond 37 weeks (1). However, as authors of the included INDEX trial (2) we would like to comment on several points in this review.
1. Categorisation of groups
Timing of induction has been categorised in the intervention arm into three groups: induction at < 40 weeks, induction between 40 to 41 weeks and induction at > 41 weeks. With this categorisation 410 weeks is not included in one of the groups. In our trial, but also in the Wennerholm et al. trial (3) (a total of 4561 women), induction at 410 weeks or 411 weeks was compared with expectant management. We suggest to change the category of induction at > 41 weeks into ≥ 41 weeks.
2. Detection bias
In the risk of bias assessment paragraph of the Cochrane review is written: “Keulen 2019 and Wennerholm 2019 explicitly reported on the absence of blinding for outcome assessors (caregivers) and were thus both rated as high risk of bias.” Caregivers were aware of group assignments because of the nature of the intervention of the included trials. It is not possible to blind caregivers, therefore this kind of bias applies to all included trials (no blinding of patients or personnel). However, this does not concern detection bias. In our trial the outcome assessor was a statistician who was blinded for the allocation, as is described explicitly in our publication and trial protocol. (quote from the statistical paragraph in our article: ‘The statistician who performed the analyses was blinded to the allocation of the participants and performed the analysis according to a predefined analysis plan.’)
3. Reporting bias
In this section is written: “Keulen 2019; to be at unclear risk of reporting bias, largely due to insufficient information to assess selective reporting (i.e. no access to trial protocols and limited detail reported in manuscript methods).”
Our trial protocol is published (4) and we had a predefined analysis plan as we have reported in our article. Therefore we wonder what kind of information is missing.
4. Induction setting (start and waiting)
In Table 3 the induction setting is described. However, this is not correct for our induction group as induction took always place in obstetrician led care in the hospital (start and waiting) as is described as such in our article (quote 1: ‘Women allocated to induction were scheduled for the procedure at 41 weeks+0 days‐41 weeks+1 day’ and quote 2: ‘all women in the 41 week induction group received obstetrician led intrapartum secondary care’. We assumed it a matter of course that a scheduled induction procedure (start and waiting) was done in a hospital setting since that was the mainstream procedure at the time of inclusion.
5. Causes of death (stillbirths and livebirth deaths)
In table 5 it is reported that the causes of perinatal death are not described in our publication. However, we gave a full description of the cases in our paper:
(Quote) “Three perinatal deaths (stillbirths) occurred: one in the induction group and two in the expectant management group. There were no neonatal deaths. The stillbirth in the induction group was in a 30 year old multiparous woman who was randomised at 40 weeks+5 days and scheduled for induction at 41 weeks+1 day. She had reduced fetal movements at 40 weeks+6 days, and fetal death was diagnosed at consultation. She delivered a neonate weighing 3595 g (20th to 50th centiles). Investigations, including a postmortem examination, did not explain the stillbirth. In the expectant management group, stillbirth was diagnosed in a 36 year old nulliparous woman at 41 weeks+3 days, when she was admitted to hospital in labour. She delivered a neonate weighing 2945 g (5th to 10th centiles). Investigations, including placental examination, did not explain the stillbirth, and the parents declined a postmortem examination. The second stillbirth in the expectant management group was diagnosed in a 32 year old multiparous woman at 41 weeks+4 days during a regular consultation in secondary care for impending post‐term pregnancy. She delivered a neonate weighing 3715 g (20th to 50th centiles). No postmortem examination was performed, but the placenta showed signs of chorioamnionitis.”
Also, in the paragraph describing the primary outcome perinatal death, it was reported that Wennerholm et al. (2019) was the only trial reporting perinatal death by parity, though as is shown in the above copy‐paste of our article, we clarified the parity for the cases of perinatal mortality in the article.
6. General remarks
Finally, we have two general remarks:
In Table 4 (Rates of perinatal death by gestation) the last group is called > 42, while this should be > 41 weeks (or to be totally correct ≥ 41 weeks).
The rate of meconium aspiration syndrome of the Sahraoui et al. trial is not reported in the original publication but the incidence of meconium stained amniotic fluid. (quote from original article: ‘un liquide amniotique teinté ou méconial était plus fréquemment rentcontré dans le groupe “surveillance”(44%) que dans le group “Prépidil (25,3%) (p=0.013)’ ). Because this concerns relatively high numbers (33 versus 19) this may affect the RR (Analyis 1.9) and funnel plot (figure 8) of meconium aspiration syndrome. (5)
Since the Cochrane review is the source for many caregivers and guideline developers who rely on the judgement of the quality of the included studies, we hope for a rapid processing of our comments.
Yours sincerely, on behalf of the INDEX‐team
Judit Keulen (first author), Esteriek de Miranda (project leader), Joris van der Post (guarantor)
References:
Middleton P, Shepherd E, Morris J, Crowther CA, Gomersall JC. Induction of labour at or beyond 37 weeks' gestation. Cochrane Database Syst Rev. 2020;7:CD004945.
Keulen JK, Bruinsma A, Kortekaas JC, van Dillen J, Bossuyt PM, Oudijk MA, et al. Induction of labour at 41 weeks versus expectant management until 42 weeks (INDEX): multicentre, randomised non‐inferiority trial. BMJ. 2019;364:l344.
Wennerholm UB, Saltvedt S, Wessberg A, Alkmark M, Bergh C, Wendel SB, et al. Induction of labour at 41 weeks versus expectant management and induction of labour at 42 weeks (SWEdish Post‐term Induction Study, SWEPIS): multicentre, open label, randomised, superiority trial. BMJ. 2019;367:l6131.
Kortekaas JC, Bruinsma A, Keulen JK, van Dillen J, Oudijk MA, Zwart JJ, et al. Effects of induction of labour versus expectant management in women with impending post‐term pregnancies: the 41 week ‐ 42 week dilemma. BMC pregnancy and childbirth. 2014;14:350.
Keulen JKJ, Bruinsma A, Kortekaas JC, van Dillen J, van der Post JAM, de Miranda E. Timing induction of labour at 41 or 42 weeks? A closer look at time frames of comparison: A review. Midwifery. 2018;66:111‐8.
Reply
1. Categorisation of groups
Timing of induction has been categorised in the intervention arm into three groups: induction at < 40 weeks, induction between 40 to 41 weeks and induction at > 41 weeks. With this categorisation 410 weeks is not included in one of the groups. In our trial, but also in the Wennerholm et al. trial (3) (a total of 4561 women), induction at 410 weeks or 411 weeks was compared with expectant management. We suggest to change the category of induction at > 41 weeks into ≥ 41 weeks.
Response:
Changed as requested, this has not impacted on the results.
2. Detection bias
In the risk of bias assessment paragraph of the Cochrane review is written: “Keulen 2019 and Wennerholm 2019 explicitly reported on the absence of blinding for outcome assessors (caregivers) and were thus both rated as high risk of bias.” Caregivers were aware of group assignments because of the nature of the intervention of the included trials. It is not possible to blind caregivers, therefore this kind of bias applies to all included trials (no blinding of patients or personnel). However, this does not concern detection bias. In our trial the outcome assessor was a statistician who was blinded for the allocation, as is described explicitly in our publication and trial protocol. (quote from the statistical paragraph in our article: ‘The statistician who performed the analyses was blinded to the allocation of the participants and performed the analysis according to a predefined analysis plan.’)
Response:
Changed to low risk of bias (and results text changed accordingly).
3. Reporting bias
In this section is written: “Keulen 2019; to be at unclear risk of reporting bias, largely due to insufficient information to assess selective reporting (i.e. no access to trial protocols and limited detail reported in manuscript methods).”
Our trial protocol is published (4) and we had a predefined analysis plan as we have reported in our article. Therefore we wonder what kind of information is missing.
Response:
Changed to low risk of bias (and results text changed accordingly); we note that your paper on women’s preferences has now been published.
4. Induction setting (start and waiting)
In Table 3 the induction setting is described. However, this is not correct for our induction group as induction took always place in obstetrician led care in the hospital (start and waiting) as is described as such in our article (quote 1: ‘Women allocated to induction were scheduled for the procedure at 41 weeks+0 days‐41 weeks+1 day’ and quote 2: ‘all women in the 41 week induction group received obstetrician led intrapartum secondary care’. We assumed it a matter of course that a scheduled induction procedure (start and waiting) was done in a hospital setting since that was the mainstream procedure at the time of inclusion.
Response:
Changed to ‘all women in the 41 week induction group received obstetrician led intrapartum secondary care’.
5. Causes of death (stillbirths and livebirth deaths)
In table 5 it is reported that the causes of perinatal death are not described in our publication. However, we gave a full description of the cases in our paper:
(Quote) “Three perinatal deaths (stillbirths) occurred: one in the induction group and two in the expectant management group. There were no neonatal deaths. The stillbirth in the induction group was in a 30 year old multiparous woman who was randomised at 40 weeks+5 days and scheduled for induction at 41 weeks+1 day. She had reduced fetal movements at 40 weeks+6 days, and fetal death was diagnosed at consultation. She delivered a neonate weighing 3595 g (20th to 50th centiles). Investigations, including a postmortem examination, did not explain the stillbirth. In the expectant management group, stillbirth was diagnosed in a 36 year old nulliparous woman at 41 weeks+3 days, when she was admitted to hospital in labour. She delivered a neonate weighing 2945 g (5th to 10th centiles). Investigations, including placental examination, did not explain the stillbirth, and the parents declined a postmortem examination. The second stillbirth in the expectant management group was diagnosed in a 32 year old multiparous woman at 41 weeks+4 days during a regular consultation in secondary care for impending post‐term pregnancy. She delivered a neonate weighing 3715 g (20th to 50th centiles). No postmortem examination was performed, but the placenta showed signs of chorioamnionitis.”
Also, in the paragraph describing the primary outcome perinatal death, it was reported that Wennerholm et al. (2019) was the only trial reporting perinatal death by parity, though as is shown in the above copy‐paste of our article, we clarified the parity for the cases of perinatal mortality in the article.
Response:
Changed to: “The stillbirth in the induction group was in a 30 year old multiparous woman who was randomised at 40 weeks+5 days and scheduled for induction at 41 weeks+1 day. She had reduced fetal movements at 40 weeks+6 days, and fetal death was diagnosed at consultation. She delivered a neonate weighing 3595 g (20th to 50th centiles). Investigations, including a postmortem examination, did not explain the stillbirth.”
In the expectant management group, stillbirth was diagnosed in a 36 year old nulliparous woman at 41 weeks+3 days, when she was admitted to hospital in labour. She delivered a neonate weighing 2945 g (5th to 10th centiles). Investigations, including placental examination, did not explain the stillbirth, and the parents declined a postmortem examination. The second stillbirth in the expectant management group was diagnosed in a 32 year old multiparous woman at 41 weeks+4 days during a regular consultation in secondary care for impending post‐term pregnancy. She delivered a neonate weighing 3715 g (20th to 50th centiles). No postmortem examination was performed, but the placenta showed signs of chorioamnionitis.”
Regarding the feedback paragraph about describing the primary outcome perinatal death, we have added Keulen text on parity to this paragraph.
General remarks
Finally, we have two general remarks:
In Table 4 (Rates of perinatal death by gestation) the last group is called > 42, while this should be > 41 weeks (or to be totally correct ≥ 41 weeks).
Response:
Changed to ≥ 41 weeks
The rate of meconium aspiration syndrome of the Sahraoui et al. trial is not reported in the original publication but the incidence of meconium stained amniotic fluid. (quote from original article: ‘un liquide amniotique teinté ou méconial était plus fréquemment rentcontré dans le groupe “surveillance”(44%) que dans le group “Prépidil (25,3%) (p=0.013)’ ). Because this concerns relatively high numbers (33 versus 19) this may affect the RR (Analyis 1.9) and funnel plot (figure 8) of meconium aspiration syndrome. (5)
Response:
While we acknowledge that the definition has some ambiguity, we have retained the data from Sahraoui. Though the magnitude differs somewhat, the overall finding remains similar.
Contributors
Philippa Middleton, Emily Shepherd, Jonathan Morris, Caroline Crowther, Judith Gomersall, 7 August 2020.
What's new
| Date | Event | Description |
|---|---|---|
| 24 August 2020 | Amended | Review amended in relation to feedback. |
| 24 August 2020 | Feedback has been incorporated | Added comments from Judit Keulen, 1 August 2020 and responses from the authors dated 7 August 2020 ‐ see Feedback 2 |
History
Protocol first published: Issue 4, 2004 Review first published: Issue 4, 2006
| Date | Event | Description |
|---|---|---|
| 27 March 2020 | New citation required and conclusions have changed | Operative vaginal birth now shows little or no difference with a policy of induction (moderate‐certainty evidence). The four new trials have nearly doubled the number of participants to over 21,000, with a concomitant increase in GRADE certainty for perinatal mortality and neonatal intensive care unit admission from moderate to high. |
| 17 July 2019 | New search has been performed | Search updated. Four new included trials added, two new ongoing trials added. |
| 28 December 2017 | New search has been performed | Search updated and eight additional trials included (Brane 2014; Cohn 1992; Keulen 2019; Martin 1978; Miller 2015; Sande 1983; Tylleskar 1979; Walker 2016). We have updated the methods in line with the standard methods used by Cochrane Pregnancy and Childbirth and we now use GRADE to assess the quality of the body of evidence. For this update, the overall conclusions have not changed. However, there is moderate certainty evidence to suggest that induction was associated with fewer stillbirths and fewer babies with low Apgar scores. |
| 9 October 2017 | New citation required but conclusions have not changed | Conclusions not changed. |
| 31 March 2012 | New search has been performed | Search updated ‐ no new trials identified. Trial reports that were previously awaiting classification have now been incorporated into the review. We have added three new included trials (Heimstad 2007; Nielsen 2005; Sahraoui 2005), three new excluded trials (Hernandez‐Castro 2008; Imsuwan 1999; Nicholson 2008) and one ongoing trial (Rijnders 2007). This updated review is now comprised of 22 included studies (reporting on 9383 women); 64 excluded studies and one ongoing study. Results are now presented as 37‐39 weeks; 39‐40 weeks; < 41 weeks, 41 weeks and > 41 weeks. A new author joined the team to help prepare this update. |
| 31 March 2012 | New citation required and conclusions have changed | Whilst the overall conclusions have not changed, there is now evidence to show that induction of labour at or beyond term is associated with a lower rate of caesarean section. |
| 6 July 2011 | Amended | Error corrected in response to feedback from Amy Marowitz (Feedback). |
| 6 July 2011 | Feedback has been incorporated | Feedback from Amy Marowitz added. |
| 14 July 2009 | Amended | Search updated. Eight reports of five trials added to Studies awaiting classification (Heimstad 2007a; Hernandez‐Castro 2008a; Imsuwan 1999a; Nicholson 2008a; Rijnders 2007a). |
| 3 September 2008 | Amended | Converted to new review format. |
| 28 February 2007 | Amended | The Implications for research section has been amended to include the uncertainty about timing of labour induction beyond term, which was unintentionally left out during the revision process. |
| 21 August 2006 | New citation required but conclusions have not changed | This version has been re‐written, including a new protocol which now limits the scope to labour induction |
| 30 June 2006 | New search has been performed | The previous version of this review included studies up to 1997 and included 21 labour induction trials (Gülmezoglu 2006). This version has been re‐written, including a new protocol which now limits the scope to labour induction, and includes 19 trials. Thirteen of the 21 trials included in the previous version are included in this version. The remaining eight trials were excluded because of alternate allocation (Cardozo 1986; Heden 1991; Katz 1983), a high proportion of postrandomization exclusion (greater than 30% in Martin 1978a and greater than 24% in Tylleskar 1979a), cervical ripening with breast stimulation (Elliott 1984; Kadar 1990), and analysis by intervention received (i.e. groups switched, Sande 1983a). Six trials published since the publication of the previous version have been included in this update (Chakravarti 2000; Chanrachkul 2003; Gelisen 2005; James 2001; Ocon 1997; Roach 1997). |
Acknowledgements
We acknowledge the support from Cochrane Pregnancy and Childbirth editorial team in Liverpool and the Australian and New Zealand Satellite of Cochrane Pregnancy and Childbirth.
We thank Therese Dowswell from Cochrane Pregnancy and Childbirth who provided support for the 2018 update. Therese assisted with data extraction, and the production of 'Summary of findings' tables.
We would like to acknowledge the contribution of Machiko Suganuma who assisted with data extraction for the 2018 update.
We would like to acknowledge the contribution of A Metin Gulmezoglu who initiated, led and assisted in the review preparation until 2016 and Emer Van Ryswyk for her contribution to a previous version of this review (Gülmezoglu 2012).
As part of the pre‐publication editorial process, this review has been commented on by three peers (an editor and two referees who are external to the editorial team), a member of our international panel of consumers and our Group's Statistical Adviser. The authors are grateful to the following peer reviewers for their time and comments: Jim Thornton, Professor of Obstetrics and Gynaecology, University of Nottingham, UK; Rory Windrom, Department of Obstetrics and Gynaecology, University of Toronto, Canada.
This project was supported by the National Institute for Health Research (NIHR), via Cochrane programme grant funding, and Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service or the Department of Health.
This review is supported by funding from the UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Sexual and Reproductive Health and Research, World Health Organization to Cochrane Pregnancy and Childbirth (University of Liverpool). HRP supports and co‐ordinates research on a global scale, synthesises research through systematic reviews of literature, builds research capacity in low‐ and middle‐income countries and develops dissemination tools to make efficient use of ever‐increasing research information. In addition to its co‐sponsors, the International Planned Parenthood Federation (IPPF) and UNAIDS are both members of HRP’s governing body.
Appendices
Appendix 1. Search methods used for ICTRP and ClinicalTrials.gov
ICTRP
Each line was run separately
induction AND expectant
induction AND wait(ing)
post‐term
postterm
postdate(s)
post‐date(s)
term AND pregnancy and expectant
ClinicalTrials.gov
Each combination of terms was run separately.
Advanced search ‐ Intervention studies
pregnancy, prolonged AND (expectant OR wait OR waiting OR monitor)
post‐term pregnancy AND (expectant OR wait OR waiting OR monitor)
expectant AND labor
postterm OR post‐term
postdates OR post‐dates
Data and analyses
Comparison 1. Labour induction versus expectant management (all trials).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Perinatal death | 22 | 18795 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.15, 0.64] |
| 1.2 Stillbirth | 22 | 18795 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.12, 0.75] |
| 1.3 Neonatal death | 21 | 18611 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.13, 1.14] |
| 1.4 Birth asphyxia | 4 | 1456 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.66 [0.61, 4.55] |
| 1.5 Admission to neonatal intensive care unit | 17 | 17826 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.80, 0.96] |
| 1.6 Neonatal convulsions | 5 | 13216 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.15, 6.67] |
| 1.7 Neonatal encephalopathy (HIE) | 2 | 8851 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.37, 1.31] |
| 1.8 Use of anticonvulsants | 1 | 349 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.01, 8.17] |
| 1.9 Meconium aspiration syndrome | 13 | 16622 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.62, 0.92] |
| 1.10 Pneumonia | 2 | 8851 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.27, 1.06] |
| 1.11 Apgar score less than 7 at 5 minutes | 20 | 18345 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.56, 0.96] |
| 1.12 Birthweight (g) | 18 | 8817 | Mean Difference (IV, Fixed, 95% CI) | ‐59.38 [‐77.03, ‐41.73] |
| 1.13 Birthweight > 4000 g | 8 | 5593 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.54, 0.96] |
| 1.14 Neonatal (birth) trauma | 5 | 13106 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.63, 1.49] |
| 1.15 Caesarean section | 31 | 21030 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.85, 0.95] |
| 1.16 Operative vaginal birth (forceps or ventouse) | 22 | 18584 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.96, 1.10] |
| 1.17 Analgesia used | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.17.1 Epidural/regional | 8 | 4579 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.99, 1.20] |
| 1.17.2 Other | 4 | 2352 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [1.05, 1.18] |
| 1.18 Perineal trauma | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.18.1 Severe perineal tear | 5 | 11589 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.85, 1.26] |
| 1.18.2 Episiotomy | 2 | 1747 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.84, 1.11] |
| 1.18.3 Obstetrical anal sphincter injuries | 2 | 1698 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.51, 1.31] |
| 1.19 Prolonged labour | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.19.1 First stage | 2 | 648 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.49, 1.20] |
| 1.19.2 Second stage | 1 | 508 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.36, 1.22] |
| 1.19.3 Third stage | 1 | 249 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.02 [0.12, 73.52] |
| 1.19.4 No definition | 1 | 112 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.01, 8.30] |
| 1.20 Postpartum haemorrhage | 9 | 12609 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.91, 1.15] |
| 1.21 Breastfeeding | 2 | 7487 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.96, 1.04] |
| 1.22 Maternal satisfaction | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.22.1 Hoping to be randomised to the same trial arm as they had been in this study | 1 | 496 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.93 [1.62, 2.30] |
| 1.22.2 Preferred/satisfied with their allocation | 2 | 493 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.88, 1.13] |
| 1.22.3 Satisfaction with pregnancy outcome | 1 | 308 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.80, 1.06] |
| 1.23 Maternal satisfaction | 1 | 619 | Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.02, 0.16] |
| 1.24 Length of maternal hospital stay (days) | 7 | 4120 | Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.56, 0.18] |
| 1.25 Length of maternal (postnatal) stay (categories) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.25.1 < 2 days | 1 | 6096 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.87, 1.17] |
| 1.25.2 2 days | 1 | 6096 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [1.01, 1.08] |
| 1.25.3 3 days | 1 | 6096 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.77, 0.99] |
| 1.25.4 4 days | 1 | 6096 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.62, 0.97] |
| 1.25.5 > 4 days | 1 | 6096 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.48, 1.82] |
| 1.26 Length of neonatal hospital stay (days) | 1 | 302 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐0.61, 0.01] |
| 1.27 Length of neonatal (postnatal) stay (categories) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.27.1 ≤ 2 days | 1 | 6091 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [1.02, 1.08] |
| 1.27.2 ≥ 3 days | 1 | 6091 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.79, 0.94] |
| 1.28 Length of labour (hours) | 12 | 4025 | Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.67, ‐0.50] |
Comparison 2. Labour induction versus expectant management (subgroup analysis by gestational age at induction).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Perinatal death | 22 | 18795 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.15, 0.64] |
| 2.1.1 < 40 weeks | 4 | 7126 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.13, 2.01] |
| 2.1.2 40 to 41 weeks | 3 | 760 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.01, 7.45] |
| 2.1.3 ≥ 41 weeks | 15 | 10909 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.11, 0.64] |
| 2.2 Stillbirth | 22 | 18795 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.12, 0.75] |
| 2.2.1 < 40 weeks | 4 | 7126 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.09, 2.76] |
| 2.2.2 40 to 41 weeks | 3 | 760 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.01, 7.45] |
| 2.2.3 ≥ 41 weeks | 15 | 10909 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.08, 0.78] |
| 2.3 Admission to neonatal intensive care unit | 17 | 17826 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.80, 0.96] |
| 2.3.1 < 40 weeks | 5 | 7409 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.79, 1.02] |
| 2.3.2 40 to 41 weeks | 3 | 527 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.68 [0.53, 5.29] |
| 2.3.3 ≥ 41 weeks | 9 | 9890 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.74, 0.96] |
| 2.4 Caesarean section | 31 | 21030 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.85, 0.95] |
| 2.4.1 < 40 weeks | 8 | 8537 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.80, 0.95] |
| 2.4.2 40 to 41 weeks | 6 | 1189 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.88, 1.43] |
| 2.4.3 ≥ 41 weeks | 17 | 11304 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.83, 0.97] |
| 2.5 Operative vaginal birth (forceps or ventouse) | 22 | 18584 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.96, 1.10] |
| 2.5.1 < 40 weeks | 7 | 8376 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.93, 1.16] |
| 2.5.2 40 to 41 weeks | 4 | 707 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.82, 3.29] |
| 2.5.3 ≥ 41 weeks | 11 | 9501 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.92, 1.11] |
| 2.6 Perineal trauma | 5 | 11589 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.85, 1.26] |
| 2.6.1 < 40 weeks | 2 | 6714 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.90, 1.55] |
| 2.6.2 40 to 41 weeks | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 2.6.3 ≥ 41 weeks | 3 | 4875 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.66, 1.19] |
Comparison 3. Labour induction versus expectant management (subgroup analysis by parity).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Perinatal death | 22 | 18795 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.15, 0.64] |
| 3.1.1 Nulliparous | 3 | 8229 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.06, 1.05] |
| 3.1.2 Mixed (primi‐ and multiparous) | 18 | 10470 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.14, 0.78] |
| 3.1.3 Not stated | 2 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 3.2 Stillbirth | 22 | 18795 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.12, 0.74] |
| 3.2.1 Nulliparous | 3 | 8229 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.04, 1.35] |
| 3.2.2 Mixed (primi‐ and multiparous) | 18 | 10470 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.12, 0.97] |
| 3.2.3 Not stated | 2 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 3.3 Admission to neonatal intensive care unit | 17 | 17826 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.80, 0.96] |
| 3.3.1 Nulliparous | 5 | 7312 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.79, 1.03] |
| 3.3.2 Mixed (primi‐ and multiparous) | 10 | 10200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.73, 0.95] |
| 3.3.3 Not stated | 2 | 314 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [0.70, 2.06] |
| 3.4 Caesarean section | 31 | 21030 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.85, 0.95] |
| 3.4.1 Nulliparous | 6 | 7543 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.81, 0.97] |
| 3.4.2 Mixed (primi‐ and multiparous) | 20 | 12877 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.83, 0.97] |
| 3.4.3 Not stated | 5 | 610 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.81, 1.56] |
| 3.5 Operative vaginal birth (forceps or ventouse) | 22 | 18584 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.96, 1.10] |
| 3.5.1 Nulliparous | 4 | 7151 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.84, 1.09] |
| 3.5.2 Mixed (primi‐ and multiparous) | 15 | 11224 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.97, 1.15] |
| 3.5.3 Not stated | 3 | 209 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.58, 2.06] |
| 3.6 Perineal trauma (severe perineal tear) | 5 | 11589 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.85, 1.26] |
| 3.6.1 Nulliparous | 2 | 6714 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.90, 1.55] |
| 3.6.2 Mixed (primi‐ and multiparous) | 3 | 4875 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.66, 1.19] |
Comparison 4. Labour induction versus expectant management (subgroup analysis by status of cervix).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Perinatal death | 22 | 18795 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.15, 0.64] |
| 4.1.1 Favourable cervix | 3 | 760 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.01, 7.45] |
| 4.1.2 Unfavourable cervix | 7 | 4938 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.07, 1.17] |
| 4.1.3 Unknown/mixed state of cervix | 12 | 13097 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.13, 0.77] |
| 4.2 Stillbirth | 22 | 18795 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.12, 0.75] |
| 4.2.1 Favourable cervix | 3 | 760 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.01, 7.45] |
| 4.2.2 Unfavourable cervix | 7 | 4938 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.05, 1.66] |
| 4.2.3 Unknown/mixed state of cervix | 12 | 13097 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.31 [0.10, 0.95] |
| 4.3 Admission to neonatal intensive care unit | 17 | 17826 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.80, 0.96] |
| 4.3.1 Favourable cervix | 2 | 475 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.02 [0.12, 73.52] |
| 4.3.2 Unfavourable cervix | 6 | 4529 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.77, 1.05] |
| 4.3.3 Unknown/mixed state of cervix | 9 | 12822 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.77, 0.97] |
| 4.4 Caesarean section | 31 | 21030 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.85, 0.95] |
| 4.4.1 Favourable cervix | 4 | 906 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.76, 1.65] |
| 4.4.2 Unfavourable cervix | 10 | 5361 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.83, 1.01] |
| 4.4.3 Unknown/mixed state of cervix | 17 | 14763 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.82, 0.95] |
| 4.5 Operative vaginal birth (forceps or ventouse) | 22 | 18584 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.96, 1.10] |
| 4.5.1 Favourable cervix | 3 | 655 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.42, 1.82] |
| 4.5.2 Unfavourable cervix | 5 | 3799 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.95, 1.18] |
| 4.5.3 Unknown/mixed state of cervix | 14 | 14130 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.92, 1.11] |
| 4.6 Perineal trauma | 5 | 11589 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.85, 1.26] |
| 4.6.1 Unknown/mixed state of cervix | 5 | 11589 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.85, 1.26] |
4.6. Analysis.

Comparison 4: Labour induction versus expectant management (subgroup analysis by status of cervix), Outcome 6: Perineal trauma
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Augensen 1987.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 409
Setting: Bergen, Norway Study date: 1981‐84 (no further details) Inclusion criteria
Exclusion criteria
State of cervix: mixed (about 35% in each group had unripe cervix) |
|
| Interventions |
Induction group (n = 214): immediate induction with oxytocin (5 IU increased in a stepwise manner). GA at intervention 41+ weeks (290‐297 days) versus EM group (n = 195): NST every 3‐4 days, IOL after 7 days |
|
| Outcomes |
Mother: caesarean section; assisted vaginal birth; length of labour; length of hospital stay Baby: perinatal death; birthweight; neonatal jaundice; meconium‐stained amniotic fluid; NICU admission |
|
| Notes |
Funding: not reported Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | List of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was unclear given that it was not undertaken by a staff member or team member clearly uninvolved in the trial. It was reported that the midwife undertook allocation using a random number list, and this list was inaccessible to the participating physicians. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4/214 in the IOL group went into labour before IOL but data for these women have been included in the IOL group for analyses. No apparent losses to follow‐up or exclusions. |
| Selective reporting (reporting bias) | High risk | No outcomes were prespecified in the methods; some outcomes reported incompletely in text, e.g. "There was no significant difference between the groups in the use of analgesia, sedatives, and epidural anaesthesia". |
| Other bias | Low risk | Appears to be free of other bias. |
Baev 2017.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 156 Setting: Tertiary referral hospital, Moscow, Russia Study date: study conducted January 2014‐15 Inclusion criteria
Exclusion criteria
State of cervix: unfavourable at trial entry (Bishop score < 8 at enrolment) |
|
| Interventions |
Induction group (n = 78): mifepristone for cervical ripening and IOL (200 mg orally at the time of enrolment and, if applicable, second dose after 24 hours). If after 72 hours the Bishop score had not changed, induction was considered 'failed'; if the Bishop score was 6‐7, dinoprostone (PGE2, gel, into the cervical canal) (0.5 mg initially, followed by a second and third dose at 6 and 12 hours if required). When Bishop score was ≥ 8, women were transferred to the labour ward for AROM. If after 4 hours there were no uterine contractions, IV oxytocin was given (starting at an incremental dose of 3 mU/minute) versus EM group (n = 78): routine appointments except examination of Bishop score after 24 and 48 hours; evaluation for maternal and fetal well‐being (including CTG). IOL at 42 weeks' gestation if birth had not yet occurred. |
|
| Outcomes |
Mother: caesarean section; assisted vaginal birth (vacuum extraction, forceps delivery); analgesia used (regional analgesia); postpartum haemorrhage; perineal trauma (episiotomy, perineal laceration 1‐2 degree); prolonged labour (protracted active phase); length of labour Baby: birthweight; Apgar score (less than or equal to 7 at 5 minutes); NICU admission |
|
| Notes |
Funding: none declared Declarations of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers organised into permuted blocks of 4 |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque envelopes sealed by independent staff member |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants and personnel was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Trialists reported that 74/78 (95%) of intervention group women allocated were included in analyses (1 woman lost to follow‐up, intervention discontinued in 2 women due to PROM, 1 woman dropped out due to skin rash reaction to drug). 75/78 (96%) of control group women analysed (3 women lost to follow‐up). |
| Selective reporting (reporting bias) | Unclear risk | Could not determine without access to protocol. Perinatal death, stillbirth or neonatal death not reported (and not specified in list of exclusions) |
| Other bias | Low risk | Appeared to be free of other bias, however, unclear why intrapartum characteristics were available only for 70 women in each group |
Bergsjo 1989.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 188 Setting: Wuhan, Hubei province, China Study date: study conducted 1 July 1982 to January 1985 (enrolment ended early 1984) Inclusion criteria
Exclusion criteria
State of cervix: not mentioned |
|
| Interventions |
Induction group (n = 94): stripping of membranes followed by oxytocin infusion and AROM if cervix sufficiently dilated. GA for intervention: 42 completed weeks (294 days) versus EM group (n = 94): no intervention for 1 week, IOL at 43 weeks. |
|
| Outcomes |
Mother: operative vaginal birth; duration of labour; caesarean section; breastfeeding (timing of recording of this outcome in relation to birth or discharge time was not specified) Baby: perinatal death; meconium aspiration syndrome |
|
| Notes |
Funding: not reported Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | List of random numbers |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 8/94 in IOL group went into labour before IOL but were kept in the allocated group. No apparent losses to follow‐up or exclusions |
| Selective reporting (reporting bias) | High risk | Most prespecified outcomes were reported; however, limited information was provided for some outcomes (e.g. combined maternal complications) and neonatal outcomes, e.g. "Maternal complications, including protracted labour, cervical edema, cervical laceration, postpartum hemorrhage and unspecified postpartum morbidity accounted to about 15% in both groups, with no significant differences;" and "About 90 mothers in each group were breastfeeding." |
| Other bias | Low risk | Appeared to be free of other bias |
Brane 2014.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 138
Setting: Stockholm, Sweden Study conducted: women recruited June 2007 to May 2012 Inclusion criteria
Exclusion criteria
State of cervix: Bishop score at presentation ranged from 1‐8 in induction group and 2‐9 in EM group. |
|
| Interventions |
Induction group (n = 71): 5 hours after medication to promote 'therapeutic rest' IOL performed, with method dependent on state of cervix: intravaginal PGE2 or transcervical catheter +/‐ AROM if cervical dilation permitted; followed by IV oxytocin (augmented every 20‐30 minutes) if no progress after AROM versus EM group (n = 67): spontaneous labour awaited as long as possible; IOL if women wanted, or if the obstetrician/midwife considered suitable |
|
| Outcomes |
Mother: mode of birth; experience of birth; duration of labour; labour analgesia; oxytocin for augmentation; birth presentation; postpartum haemorrhage; sphincter tears Baby: Apgar score < 7 at 5 minutes; cord artery metabolic acidosis; birthweight; head circumference; admission to NICU |
|
| Notes | Women in both groups given medication to promote 'therapeutic rest' (1 g paracetamol, 10 mg zolpidem, 10 mg morphine). During active phase of labour (cervical dilation ≥ 4 cm or ROM) women monitored according to local protocol; slow progress (arrest of dilation for 2‐3 hours) was treated with AROM or oxytocin Funding: Karolinska Institute Foundations and Funds Declaration of interests: The authors reported no conflicts of interest. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The randomization was performed in blocks of 5–10 in each group." Method of sequence generation not reported |
| Allocation concealment (selection bias) | Unclear risk | "A sealed envelope containing coded protocols for the respective groups… was opened by the midwife." No further detail provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Some attrition and missing data, particularly for the women’s views questionnaire. Most of the sample were included in the analyses for the primary outcome (65/71, and 64/67 in main analysis for mode of birth). The reasons for missing data for some clinical outcomes were not reported. |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol to confidently assess selective reporting. Perinatal death not reported |
| Other bias | Low risk | Appeared to be free of other bias |
Breart 1982.
| Study characteristics | ||
| Methods | RCT (1:2 randomisation) | |
| Participants | Number of women randomised: 716
Setting: Paris, France Study conducted: not reported Inclusion criteria: GA: 37‐39 weeks (259‐273 days) Exclusion criteria: high risk, contraindication for IOL State of cervix: not mentioned Parity: mixed (60% nulliparous) |
|
| Interventions |
Induction group (n = 235): oxytocin and AROM at GA 37‐39 weeks versus EM group (n = 481): FHR checking and amnioscopy every 2‐3 days |
|
| Outcomes | Mother: duration of labour; mode of birth Baby: morbidity (Apgar scores, resuscitation) | |
| Notes |
Funding: not reported Declaration of interests: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | It was reported that a closed envelope system was used for allocation concealment, although no further detail was available. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 202/235 in the induction group and 173/481 in the expectant group followed the trial protocol; trial results were reported for all 716 women and their babies. |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol to confidently assess selective reporting. Perinatal death was not reported. |
| Other bias | Low risk | Appeared to be free of other bias |
Chakravarti 2000.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 231
Setting: Calcutta, India Study date: not reported Inclusion criteria
State of cervix: not mentioned |
|
| Interventions |
Induction group (n = 117): IOL, no details of the method are available.
versus EM group (n = 114 randomised): daily fetal movement counts, biophysical profile and ultrasound; IOL after 1 week. |
|
| Outcomes | Only caesarean section rates were adequately reported in the abstract. | |
| Notes | Reported as conference abstract. Only data for caesarean included in meta‐analysis. Funding: not reported Declaration of interests: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Appeared that blinding was not feasible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to determine |
| Selective reporting (reporting bias) | Unclear risk | No outcomes were prespecified in the methods (conference abstract). Insufficient information to determine |
| Other bias | Unclear risk | Unable to identify other bias based on the abstract |
Chanrachkul 2003.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 249
Setting: Bangkok, Thailand Study date: study conducted October 1998 to May 2000 Inclusion criteria
Exclusion criteria
State of cervix: favourable (Bishop score 6 or more) |
|
| Interventions |
Induction group (n = 124): AROM + oxytocin (if uterine contractions inadequate after 2 hours); versus EM group (n = 125): spontaneous labour awaited unless 1) non‐reactive NST or 2) amniotic fluid index < 5 cm or 3) medical or obstetric indication for birth or 4) reaching 44 completed weeks. |
|
| Outcomes | Mother: prolonged labour; modes of birth and their indications; death; postpartum haemorrhage Baby: perinatal death, birthweight; birth asphyxia, NICU admission, birthweight > 4000 g; Apgar < 7 at 5 minutes | |
| Notes |
Funding: Ramathibodi Hospital Research Grant 2/2542 Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was carried out using computer‐generated numbers. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 woman (in IOL group) excluded after randomisation because of misclassification (breech presentation). No apparent losses to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | While prespecified outcomes (in the methods) were reported, no access to trial protocol to further assess selective reporting. |
| Other bias | Low risk | Appeared to be free of other bias |
Cohn 1992.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 248
Setting: Hong Kong, China Study date: not mentioned but abstract published in 1992 Inclusion criteria
Exclusion criteria
State of cervix: Not reported |
|
| Interventions |
Induction group (n = not reported): induction versus EM group (n = not reported): women were seen twice weekly. |
|
| Outcomes |
Mother: length of stay in hospital; analgesia; caesarean birth; meconium‐stained liquor Baby: neonatal admission for meconium aspiration; birthweight; Apgar scores; umbilical cord vein pH |
|
| Notes | Abstract only. No data included in meta‐analyses Funding: not reported Declaration of interests: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | " A prospective randomised study". The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information on losses to follow‐up or exclusions |
| Selective reporting (reporting bias) | Unclear risk | Abstract only |
| Other bias | Unclear risk | Abstract only. Baseline characteristics were not described. |
Cole 1975.
| Study characteristics | ||
| Methods | Randomly allocated, no further details available | |
| Participants | Number of women randomised: 228
Setting: Glasgow, Scotland Study date: not reported Inclusion criteria
State of cervix: not reported |
|
| Interventions |
Induction group (n = 111): IOL with AROM + oxytocin
versus EM group (n = 117): no intervention until 41 weeks, thereafter IOL |
|
| Outcomes |
Mother: length of labour; mode of birth (including operative versus non operative); analgesia requirements; postpartum blood loss Baby: perinatal deaths; meconium staining; Apgar scores; birthweight; neonatal jaundice |
|
| Notes |
Funding: not reported Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 7/118 and 2/119 in the intervention and control groups excluded after randomisation because of misclassification as low risk |
| Selective reporting (reporting bias) | Unclear risk | No outcomes were prespecified in the methods; no access to trial protocol to further assess selective reporting |
| Other bias | Low risk | Appeared to be free of other bias |
Dyson 1987.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 302
Setting: Kaiser Permanente Medical Care Hospital in California, USA Study date: study conducted 11 January 1983 to 3 December 1985 Inclusion criteria
Exclusion criteria
State of cervix: unfavourable (Bishop score < 6) |
|
| Interventions |
Induction group (n = 152): PE2 gel (initially 3 mg but later reduced to 0.5 mg). If no labour in 24 hours, repeat PE2 and oxytocin if needed versus EM group (n = 150): NST twice weekly, pelvic examination and amniotic fluid determination weekly between 41‐42 weeks and twice weekly afterwards |
|
| Outcomes |
Mother: length of hospital stay; caesarean section; length of labour Baby: perinatal death; 1 minute Apgar score < 7; 5 minute Apgar score < 7; meconium‐stained amniotic fluid; meconium aspiration syndrome; post‐maturity syndrome; fetal distress; birthweight; birthweight > 4000 g; infant hospital stay length |
|
| Notes |
Funding: Community Service Program of Kaiser Foundation Hospitals Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A table of random numbers was used. |
| Allocation concealment (selection bias) | Unclear risk | The authors reported " using a series of consecutively numbered, sealed envelopes..." for allocation concealment, but no mention was made of envelope opaqueness. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses to follow‐up or exclusions |
| Selective reporting (reporting bias) | Unclear risk | No outcomes were prespecified in the methods; no access to trial protocol to further assess selective reporting |
| Other bias | Low risk | Appeared to be free of other bias |
Egarter 1989.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 345
Setting: Vienna, Austria Study date: not reported Inclusion criteria
Exclusion criteria
State of cervix: favourable (Modified Bishop score > 4) |
|
| Interventions |
Induction group (n = 180): vaginal PE2 (3 mg) tablets repeated 6 and 24 hours later if no active labour versus EM group (n = 165): spontaneous labour awaited until 42 weeks. NST monitoring every 2‐3 days |
|
| Outcomes |
Mother: birth interval (onset of contractions to birth in hours); rate and indication for operative birth; length of labour; analgesia requirements; caesarean section Baby: birthweight; length of baby at birth; incidence of meconium‐stained amniotic fluid; Apgar scores; results of umbilical cord pH determination; perinatal death |
|
| Notes |
Funding: not reported Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 8/180 women in the induction group refused to be induced; and 3/165 women in the expectant group requested induction; and these 11 women were excluded from analysis post‐randomisation. |
| Selective reporting (reporting bias) | High risk | No outcomes were prespecified in the methods, limited information was provided for some outcomes, e.g. "The incidence of prolonged labor was not different in both groups... both groups required analgesic treatment in 35%... Birthweight and length, the incidence of meconium‐stained amniotic fluid, of low Apgar scores, and the results of pH determination were not different between the two groups." |
| Other bias | Unclear risk | Some imbalance in the numbers randomised to each group (180 versus 165) |
Gelisen 2005.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 600
Setting: teaching hospital in Ankara, Turkey; Study date: not reported Inclusion criteria
Exclusion criteria
State of cervix: unfavourable ‐ Bishop score < 5 Just under half the women were nulliparous. |
|
| Interventions |
Induction group: labour induction (3 methods*) (1) vaginal administration of 50 mg misoprostol (n = 100) (2) oxytocin induction (n = 100), and (3) transcervical insertion of a Foley balloon (n = 100) versus EM group: spontaneous follow‐up with twice‐weekly nonstress testing and amniotic fluid measurement and once‐weekly biophysical scoring (n = 300); 24% of women were induced after 42 completed weeks. *the 3 induction arms were combined for analyses |
|
| Outcomes | Mother: oligohydramnios; pre‐eclampsia; tachysystole; hyperstimulation; vaginal birth; caesarean (emergent abdominal birth for worrying FHR); failed IOL Baby: perinatal death; shoulder dystocia; meconium stained amniotic fluid; meconium aspiration syndrome; fetal anomaly; low Apgar scores (< 7 at 5 minutes); umbilical artery pH < 7.16; NICU admission; fetal macrosomia; birthweight; birthweight > 4000 g; length of hospital stay | |
| Notes |
Funding: not reported Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was by sealed, opaque envelopes but there was no mention of numbering and sequential opening of the envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding: "Staff members in charge of labor were not blinded to the type of medication used for induction". |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses to follow‐up or exclusions |
| Selective reporting (reporting bias) | Unclear risk | While prespecified outcomes (in the methods) were reported, no access to trial protocol to further assess selective reporting |
| Other bias | Low risk | Appeared to be free of other bias |
Grobman 2018.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 6106 Setting: 41 hospitals participating in the Maternal‐Fetal Medicine Units Network of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, USA Study date: women recruited March 2014 through August 2017 Inclusion criteria
Exclusion criteria
State of cervix: favourable and unfavourable (at the time of randomisation, 63% of the participants had an unfavourable modified Bishop score (i.e. a score < 5)) |
|
| Interventions |
Induction group (n = 3062): women were assigned to undergo IOL at 390 weeks to 394 weeks; with no specific induction protocol mandated. Supplementary Appendix for the manuscript indicated that oxytocin was used, and for women with an unfavourable cervix, cervical ripening was used (actual method left to the discretion of the woman's obstetric provider), in conjunction with or followed by oxytocin; mechanical ripening using a Foley catheter without saline infusion and without concurrent oxytocin was permitted; although not mandated, it was suggested that women should be allowed at least 12 hours in the latent phase after completion of any ripening, ROM, and use of oxytocin before the induction was considered 'failed' (and subsequent caesarean birth) versus EM group (n = 3044): women were asked to forgo elective birth before 405 weeks and to have birth initiated no later than 422 weeks. A specific induction protocol was not mandated for women who underwent induction in either group. |
|
| Outcomes |
Mother: caesarean section; operative vaginal birth; perineal trauma (third‐ or fourth‐degree perineal laceration); postpartum haemorrhage; breastfeeding (at 4‐8 weeks after birth); length of maternal hospital stay (days, categories including < 2, 2, 3, 4, > 4) Baby: perinatal death (antenatal stillbirth and neonatal death); stillbirth; neonatal death; admission to NICU (intermediate or intensive care unit); neonatal convulsions (seizures); neonatal hypoxic‐ischaemic encephalopathy; pneumonia (confirmed); meconium aspiration syndrome; Apgar score (≤ 3 at 5 minutes); length of neonatal hospital stay (days, categories including < 2, 2, 3, 4, > 4) |
|
| Notes |
Funding: Eunice Kennedy Shriver National Institute of Child Health and Human Development. Declarations of interest: "Dr. Silver reports receiving consulting fees from Gestavision. No other potential conflict of interest rel avant to this article was reported." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Prepared by an independent data coordinating centre, using the simple urn method, with stratification according to clinical site |
| Allocation concealment (selection bias) | Low risk | Randomisation sequence prepared by an independent data coordinating centre, and an internet‐based randomisation system was used. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | For neonatal primary outcomes requiring review, "Reviewers were unaware of the trial‐group assignments". Unclear whether any other outcomes were assessed blind, though discussion reported that "because masking was not feasible, ascertainment bias is possible". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3059/3062 women assigned to induction were included in analyses (1 lost to follow‐up; 2 withdrew consent); 3037/3044 women assigned to control included in analyses (2 lost to follow‐up; 5 withdrew consent) |
| Selective reporting (reporting bias) | Low risk | Comprehensive range of outcomes specified in protocol and reported |
| Other bias | Low risk | Note: authors noted report that 184/3059 women (6%) in the induction group, and 140/3037 (4.6%) women in the control group did not birth 'per protocol'. |
Hannah 1992.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 3418 enrolled (data available for 3407 women only)
Setting: 22 hospitals across Canada Study date: study conducted between November 1985 and December 1990 Inclusion criteria
Exclusion criteria
State of cervix: unfavourable at trial entry (first ripening and then IOL in the intervention group) |
|
| Interventions |
Induction group (n = 1701): up to 3 x 0.5 mg doses of PGE2 gel administered intracervically (if NST was normal and cervix unfavourable at time of induction = 77% of women), followed by either AROM or IV oxytocin infusion, or both versus EM group (n = 1706): daily fetal movement counting, NST and amniotic fluid measurement 2‐3 times per week. If either the NST or amniotic fluid volume assessment was abnormal, or other complications developed, labour was induced (28% of women induced in the expectant group received some form of PE2 (not gel)). |
|
| Outcomes | Mother: caesarean section; operative vaginal birth Baby: perinatal death (stillbirth or neonatal death before discharge excluding deaths caused by lethal congenital anomalies); birthweight > 4000 g; Apgar score < 7 at 5 minutes; asphyxial encephalopathy (seizures, alterations in levels of consciousness or tone, or a need for tube feeding during the first 48 hours of life), respiratory distress (oxygen requirement > 40% and respiratory rate > 60 breaths/minute, both within 12 hours after birth and persisting for more than 24 hours, or assisted ventilation for more than 24 hours): meconium aspiration syndrome; neonatal trauma; NICU admission | |
| Notes | Most women (89%) were enrolled at 410 to 416 weeks' gestation (3% before 41 weeks and 8% at or beyond 42 weeks), of whom 86.2% in the induced group and 63.6% in the expectant group gave birth before 42 weeks' gestation. In the induction group, 31% of women were not induced and in the EM group, 34% of women were induced. Funding: Medical Research Council of Canada: MA‐8472; Upjohn Company of Canada supplied the prostaglandin gel. Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Low risk | Randomisation was carried out at a site separate from the trial ("centrally controlled at McMaster University"). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The study was partially blinded; an adjudication of abnormal neonatal outcomes was undertaken by a neonatologist who was unaware of the mothers' group assignments. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3418 women enrolled (data available for 3407 women); 7 women whose babies had lethal congenital anomalies were excluded after randomisation from the analysis of perinatal and neonatal outcomes ‐ induction group (1 woman) and EM group (6 women). |
| Selective reporting (reporting bias) | Unclear risk | Prespecified outcomes (from the methods) were reported; some results reported incompletely in text, e.g. "The frequency of postpartum maternal morbidity (hemorrhage, sepsis, endometritis) did not differ between the two groups (data not shown)". No access to trial protocol to further assess selective reporting |
| Other bias | Low risk | Appeared to be free of other bias; although methods of induction differed between the induction group and the women requiring induction in the EM group. |
Heimstad 2007.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 508
Setting: St. Olavs University Hospital, Trondheim, Norway Study date: women randomised between September 2002 and July 2004 Inclusion criteria
State of cervix: all stages included |
|
| Interventions |
Inductiongroup (n = 254): if cervix favourable (Bishop score ≥ 6) AROM + oxytocin, if not (Bishop score < 6) 50 µg misoprostol vaginally versus EM group (n = 254): twice‐weekly ultrasound and CTG, labour induction after 300 days of pregnancy |
|
| Outcomes | Mother: prolonged labour; mode of birth; perineal trauma; maternal satisfaction; postpartum haemorrhage Baby: perinatal death; neonatal morbidity, for which a score was tallied (by evaluating the degree of deviation from the potential of a perfect outcome for each newborn as defined by the authors); neonatal trauma; birthweight; birthweight > 4000 g, NICU admission, birth asphyxia, meconium aspiration syndrome, Apgar < 7 at 5 minutes | |
| Notes |
Funding: not reported Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computerised randomisation using blocks of 16 with no stratification |
| Allocation concealment (selection bias) | Low risk | Central allocation ‐ clinical trials office |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No women were lost to follow‐up for clinical outcomes; 8 women did not complete the inclusion questionnaire; for the post‐birth telephone survey, 12 women were lost to follow‐up (4 in induction group and 8 in EM group). |
| Selective reporting (reporting bias) | Unclear risk | While all prespecified outcomes (in the methods) were reported, with no access to trial protocol, it was not possible to further assess selective reporting. |
| Other bias | Low risk | Appeared to be free of other bias |
Henry 1969.
| Study characteristics | ||
| Methods | RCT with inadequately reported randomisation methods | |
| Participants | Number of women randomised: 112
Setting: Birmingham, UK Study date: not reported Inclusion criteria (not well specified)
Exclusion criteria
State of cervix: Not mentioned as a criterion |
|
| Interventions |
Induction group (n = 55): AROM and oxytocin ("surgical" group)
versus EM group (n = 57): weekly amnioscopy |
|
| Outcomes |
Mother: number of days past term; prolonged labour; mode of birth Baby: perinatal death; birthweight |
|
| Notes | 4 women in expectant group and 1 in induction group were randomised before 41 weeks. Funding: not reported Declaration of interests: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses to follow‐up or exclusions |
| Selective reporting (reporting bias) | Unclear risk | No outcomes were prespecified in the methods; no access to trial protocol to further assess selective reporting |
| Other bias | Low risk | Appeared to be free of other bias |
Herabutya 1992.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 108
Setting: Bangkok, Thailand Study date: study conducted July 1987 to January 1991 Inclusion criteria
Exclusion criteria
State of cervix: unfavourable cervix (Bishop score 6 or less) |
|
| Interventions |
Induction group (n = 57): PGE2 intracervical, repeated after 6 hours, AROM and oxytocin on day 2 according to contractions versus EM group (n = 51): a) NST between 42 and 43 completed weeks. 2) NST between 43 and 44 completed weeks; women underwent IOL if there were abnormalities in antepartum fetal testing as non‐reactive NST, or variable decelerations on NST or if Bishop score > 6 on reaching 44 completed weeks' gestation |
|
| Outcomes |
Mother: length of first stage of labour; mode of birth; cephalopelvic disproportion; fetal distress Baby: birthweight; meconium staining; Apgar score < 7 at 1 minute; Apgar score < 7 at 5 minutes; intubation required; admission to special care baby unit; perinatal death |
|
| Notes |
Funding: Ramathibodi Hospital Research Fund Grant 1988 Declaration of interests: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses to follow‐up or exclusions |
| Selective reporting (reporting bias) | Unclear risk | No outcomes were prespecified in the methods; no access to trial protocol to further assess selective reporting |
| Other bias | Low risk | Appeared to be free of other bias |
James 2001.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 74 Setting: Vellore, India Study date: not reported Inclusion criteria
Exclusion criteria
State of cervix: not mentioned as a criterion |
|
| Interventions |
Induction group (n = 37): Bishop < 5: cervical ripening with extra‐amniotically placed 16F Foley catheter with 20 mL of saline Bishop > 5: stripping of membranes Then, 12 hours later, IOL by AROM and oxytocin infusion versus EM group (n = 37): daily fetal movement counts; biophysical profile every second day |
|
| Outcomes |
Mother: mode of birth and indications; duration of labour; mean hospital stay Baby: meconium staining of amniotic fluid; meconium aspiration; Apgar scores < 7 (at 1 and 5 min); need for neonatal intubation; birthweight; birthweight > 4000 g; signs of post‐maturity; perinatal deaths; abnormal electronic fetal trace monitoring |
|
| Notes |
Funding: not reported Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A table of random numbers was used. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was unclear since "... a series of consecutively numbered, sealed envelopes..." was used but no mention was made of opaqueness of the envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up or post‐randomisation exclusion |
| Selective reporting (reporting bias) | Unclear risk | All of the outcomes mentioned in the methods section were reported on in the results section; mean duration of labour was reported with no measure of variance. No access to trial protocol to further assess selective reporting |
| Other bias | Low risk | Appeared to be free of other bias |
Keulen 2019.
| Study characteristics | ||
| Methods | Multicentre RCT (non‐inferiority trial) | |
| Participants | Number of women randomised: 1815 randomised Setting: 123 primary care midwifery practices and 45 hospitals (secondary care) equally distributed across the Netherlands Study date: study conducted 2012‐16 Inclusion criteria:
Exclusion criteria:
State of cervix: mixed ‐ in both groups three‐quarters of the women had a Bishop score < 6 at study entry |
|
| Interventions |
Induction group (n = 907): Women were scheduled for induction at 410 weeks to 411 weeks. All women were primed or induced, or both according to local protocols. Women with a Bishop score < 6 received cervical priming with PGE1 (misoprostol, oral or vaginal), PGE2 (dinoprostone), Foley catheter or double balloon catheter, or a combination of these until AROM could be performed. AROM was followed by IV oxytocin if required. versus EM group (n = 908): women awaited spontaneous onset of labour until 420 weeks in their initial care setting (primary or secondary), with monitoring according to local protocol. which typically involved a combination of CTG, and sonographic assessment of amniotic fluid in secondary care at 41‐42 weeks. Women with ongoing pregnancies were scheduled for induction at 420 weeks in secondary care, following a similar induction protocol to the intervention group. |
|
| Outcomes |
Mother: caesarean section; operative vaginal birth; analgesia used (reports on pain treatment during labour, and specifically on remifentanil, pethidine/promethazine/other opiates, epidural anaesthesia, other); perineal trauma (episiotomy (without tear), obstetrica anal sphincter injuries, third‐degree tear, fourth‐degree tear, episiotomy and third‐degree tear, episiotomy and fourth‐degree tear); postpartum haemorrhage (≥ 1000 mL); Baby: perinatal death; stillbirth; neonatal death; NICU admission; meconium aspiration syndrome; Apgar score < 7 at 5 minutes; birthweight |
|
| Notes |
Funding: grant from the Netherlands Organisation for Health Research and Development ZonMw (grant No 171202008) Declarations of interest: "BWM is supported by a National Health and Medical Research Council practitioner fellowship (GNT1082548) and reports consultancy for ObsEva, Merck, and Guerbet; no support from any other organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Web‐based program (ALEA) using randomly permuted block sizes of 4 and 2, stratified by centre |
| Allocation concealment (selection bias) | Low risk | Central (web‐based) randomisation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Women and staff were aware of assignments. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | ‘"he statistician who performed the analyses was blinded to the allocation of the participants and performed the analysis according to a predefined analysis plan." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 900/907 women allocated to induction were analysed in ITT analyses (7 were excluded – 1 withdrew consent, and 6 were not eligible); 901/908 women allocated to EM were analysed in ITT analyses (7 were excluded due to ineligibility). |
| Selective reporting (reporting bias) | Low risk | Wide range of outcomes reported, as specified in published protocol. |
| Other bias | Unclear risk | "Since in our trial all women in the 41 week induction group received obstetrician led intrapartum secondary care whereas in the expectant management group until 42 weeks 68.7% of the women received midwifery led primary care at start of labour and 34.3% at time of birth, it could be suggested that our study is prone to performance bias (different care) and measurement bias (different assessment of neonates)." |
Martin 1978.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 264 "admitted to this trial"
Setting: Royal Maternity Hospital, Northern Ireland, UK Study date: not reported Inclusion criteria
Exclusion criteria
State of cervix: not clearly reported; assumed to be mixed (Bishop score recorded). |
|
| Interventions |
Induction group (n = 131 admitted; 92 analysed): IOL at 39 weeks' GA. Women were admitted for fasting at 8:30 am; their forewaters were punctured soon after and Bishop score and cervical dilatation recorded. IV oxytocin commenced at 2.5 mU/minute and doubled every 30 minute until satisfactory uterine response achieved; dose varied to maintain adequate contractions. All women continuously monitored with internal tocography and fetal scalp electrode. versus EM group (n = 133 admitted; 92 analysed): await spontaneous labour until 42 weeks, unless IOL required earlier for medical reasons. Women had, if necessary, augmentation of labour by puncture of the forewaters or IV oxytocin; when possible, they were also monitored. |
|
| Outcomes |
Mother: mode of birth (assisted birth; caesarean birth); induction to birth interval; unexplained postpartum pyrexia; analgesia demand; type 1 and 2 diabetes; meconium staining of the amniotic fluid; duration of gestation; attitudes towards management Baby: Apgar scores at 1 and 5 minutes; Dubowitz scores < 45; stillbirth; hyperbilirubinaemia |
|
| Notes |
Funding: not reported Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "A prospective randomized controlled trial"; "allocated using random number tables." |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “All monitor records were examined blind at completion of the trial.” |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 184/264 women followed up (30% loss to follow‐up). 264 women eligible, 34 excluded: induction group: obstetric abnormality (8 women); refusal (10 women); defaulter (6 women); spontaneous labour before attending clinic (1 woman). EM group: obstetric reasons (9); leaving 230 women in the trial (106 in planned birth, 124 in EM group) Of the 106 women in the induction group, 13 went into spontaneous labour before the date of admission and 1 was excluded due to medical reasons – therefore 92 women were induced and analysed. Of the 124 women in the EM group, a further 32 were excluded due to obstetric abnormalities or failure to go into spontaneous labour before 42 weeks – therefore only 92 were analysed. |
| Selective reporting (reporting bias) | Unclear risk | Some results reported incompletely, e.g.: “There was no difference with respect to the distribution of Apgar scores…at five minutes.” |
| Other bias | Unclear risk | Groups appeared comparable at baseline however analyses excluded 30% of women admitted to the trial. Limited methodological detail provided to further assess other bias |
Martin 1989.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 22
Setting: Jackson, USA Study date: women recruited 1 July 1987 to 31 January 1988 Inclusion criteria
Exclusion criteria
State of cervix: unripe (Bishop score 5 or less) included |
|
| Interventions |
Induction group (n =12): laminaria tents followed by oxytocin versus EM group (n = 10): weekly ultrasound for amniotic fluid assessment and NST |
|
| Outcomes |
Mother: mode of birth; length of labour; type of analgesia; length of hospital stay; labour‐associated morbidity Baby: birthweight; Apgar score; perinatal deaths; neonatal course; meconium staining |
|
| Notes |
Funding: Vicksburg Hospital Medical Foundation Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Allocation in sealed envelopes but no mention of opaqueness, numbering and sequential opening of envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses to follow‐up or exclusions. |
| Selective reporting (reporting bias) | High risk | No outcomes were prespecified in the methods; a number of outcomes reported without measures of variance (e.g. birthweight, length of labour, hospital stay), and thus these outcomes could not be used in the meta‐analyses. No access to protocol to further assess selective reporting |
| Other bias | Low risk | Appeared to be free of other bias |
Miller 2015.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 162
Setting: Military tertiary care medical centre, USA Study date: women randomly assigned March 2010 to February 2014 Inclusion criteria
Exclusion criteria
State of cervix: modified Bishop score ≤ 5 |
|
| Interventions |
Induction group (n = 82): IOL ≤ 1 week of randomisation; not before 39 weeks' GA Where possible, IOL by Foley catheter (single balloon, 60 mL water), taped in place until expulsion or 12 hours. After Foley catheter, oxytocin (2 mIU per min, increasing every 20 minute to 36 mIU per minute max) until adequate contractions. If Foley catheter placement not possible, IOL by misoprostol 25 µg vaginally, repeated every 4 hours; AROM after 3 cm dilation; oxytocin administered after last if adequate contractions not observed with misoprostol versus EM group (n = 80): scheduled for routine appointments and birthed for obstetric indications no later than 42 weeks' GA |
|
| Outcomes |
Mother: caesarean birth; mode of birth; number of visits after randomisation; unscheduled clinic or triage visits; number of antepartum fetal testing appointments; GA at admission; Bishop score at admission; admission diagnosis; indication for operative birth; use of regional anaesthesia; chorioamnionitis; EBL; blood transfusion; endomyometritis; labour and birth length of stay; postpartum stay Baby: meconium‐stained amniotic fluid; NICU admission; birthweight; SGA; LGA; Apgar score < 5 at 5 minutes |
|
| Notes |
Funding: not reported Declarations of interest: the authors declared that they had no financial conflicts of interest. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of random numbers in permuted blocks of 4 |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed by the use of opaque, sealed, sequentially numbered envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding: "blinding of health care providers to the indication for delivery was deemed impractical." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low loss to follow‐up following randomisation (82/82 and 79/80 women included in the analyses) |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol to assess selective reporting. Perinatal death not reported |
| Other bias | Low risk | Appeared to be free of other bias |
NICHHD 1994.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 440
Setting: University hospitals in the USA Study date: Women screened December 1987 to July 1989 Inclusion criteria
Exclusion criteria
State of cervix: unfavourable (Bishop score 6 or less) |
|
| Interventions |
Induction group (n = 174): cervical priming with PGE2 gel followed 12 hours later with oxytocin versus EM group (n = 175): weekly cervix assessments, twice weekly NST and amniotic fluid volume assessment A total of 265 women were randomised to the intervention arm; however, 91 of these women were randomised to placebo gel with oxytocin 12 hours later and these women have not been included in this review. |
|
| Outcomes | Mother: time to birth from randomisation; maternal infection; need for transfusion; uterine hyperactivity; mode of birth; maternal death Baby: mechanical ventilation; nerve injury; seizures; babies with ≽1 adverse outcome; perinatal death; birthweight; Apgar score < 4 at 5 minutes; late decelerations in labour; meconium in amniotic fluid; meconium in aspiration pneumonia | |
| Notes | The initial sample size intended was 2800. However, after 18 months and 440 participants, the study was stopped, since the incidence of adverse outcome was only 1.1% and therefore a sample size of 5600 would be required to adequately test the hypothesis proposed. Funding: National Institute of Child Health and Human Development, NIH, USA Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence generation was performed using a computer‐generated randomisation scheme stratified by site and GA. |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed by using central allocation by a data co‐ordinating centre. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses to follow‐up or exclusions |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcomes (in methods) were reported; no access to trial protocol to further assess selective reporting |
| Other bias | Low risk | Appeared to be free of other bias |
Nielsen 2005.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 226
Setting: Army Medical Center, Tacoma, Washington, USA Study date: enrolled September 1999 to December 2002 Inclusion criteria
Exclusion criteria
State of cervix: favourable (≥ 5 for nulliparous and ≥ 4 for multiparous women) |
|
| Interventions |
Induction group (n = 116): AROM, oxytocin or both versus EM group (n = 110): weekly follow‐up until 42 weeks. Labour induced after 42 weeks. Weekly monitoring with CTG and ultrasound, increased to twice a week after 41 weeks. |
|
| Outcomes |
Mother: randomisation to birth interval; admission to birth interval; Indication for admission; epidural analgesia; mode of birth; EBL; length of labour; chorioamnionitis; postpartum days Baby: birthweight; admission to NICU; Apgar score < 7 at 5 minutes |
|
| Notes | The study was discontinued after recruitment of 226 women (target of 600) due to slow recruitment and no observed difference in the 2 groups. Funding: not reported Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was generated using a computer‐generated list. |
| Allocation concealment (selection bias) | Low risk | Allocation concealment was achieved using sequentially numbered, opaque, sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses to follow‐up or exclusions. 23/116 (19.8%) in induction group went into spontaneous labour, 10/110 (9.1%) in the EM group required labour induction and results for these women were analysed according to which group they were randomised. |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol to confidently assess selective reporting. Perinatal death not reported |
| Other bias | Unclear risk | Baseline imbalance for Bishop score "The only significant difference noted was EM patients had a more favorable Bishop score on admission than IND patients (7.2 + 2.1 versus 8.6 + 2.0, P < 0.0001)." |
Ocon 1997.
| Study characteristics | ||
| Methods | RCT (partially translated). | |
| Participants | Number of women randomised: 113
Setting: Gran Canaria, Spain Study date: not reported Inclusion criteria
Exclusion criteria
State of cervix: unfavourable (Bishop score < 5) |
|
| Interventions |
Induction group (n = 57): intracervical PGE2 gel (0.5 mg); unclear whether further intervention occurred (full translation not available) versus EM group (n = 56): monitoring by NST, biophysical profile and amnioscopy |
|
| Outcomes | Mother: time to birth; mode of birth Baby: meconium staining; NICU admission; birthweight > 4000 g; Apgar score < 7 at 5 minutes (other outcomes may have been present, but were not reported in the translation) | |
| Notes |
Funding: not reported Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not reported according to the translation. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not reported according to the translation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses to follow‐up or exclusions |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol to confidently assess selective reporting. Perinatal deaths appeared not to have been reported according to the translation, although this has not been verified by a second translation. |
| Other bias | Low risk | Appeared to be free of other bias |
Roach 1997.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 201
Setting: Hong Kong, China Study date: not reported Inclusion criteria
Exclusion criteria
State of cervix: not mentioned as a criterion |
|
| Interventions |
Induction group (n = 96): PGE2 pessaries 6‐hourly if necessary versus EM group (n = 105): serial monitoring with NST (x 2) and amniotic fluid index measurements (x 1) weekly |
|
| Outcomes |
Mother: spontaneous labour; caesarean section; fetal distress in labour Baby: birthweight; Apgar score < 7 (1 minute/5 minutes); cord blood pH; admission to NICU; meconium below the vocal cords |
|
| Notes |
Funding: not reported Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generation was not reported. |
| Allocation concealment (selection bias) | Unclear risk | Allocation in a series of identical envelopes but no mention of sealed envelopes, opaqueness and sequential numbered envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses to follow‐up or exclusions. 17/96 (18%) in the induction group went into spontaneous labour and 12/105 (11%) in the EM group were induced and the results for these women were included in the analyses. |
| Selective reporting (reporting bias) | Unclear risk | Very few outcomes reported; "We did not address perinatal mortality in this study." No access to trial protocol to further assess selective reporting |
| Other bias | Low risk | Appeared to be free of other bias |
Sahraoui 2005.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 150
Setting: Sousse, Tunisie (Tunisia) Study date: not reported Inclusion criteria
Exclusion criteria
State of cervix: cervix unripe (Bishop score < 4) |
|
| Interventions |
Induction group (n = 75): PGE2 gel intracervically (daily cervical ripening by PGE2 gel, maximum 3 gels) versus EM group (n = 75): CTG every second day until 42 completed weeks. After that, PGE2 gel if no spontaneous labour |
|
| Outcomes |
Mother: duration of labour; mode of birth; GA at birth; duration of mother’s hospital stay (hours); need for augmentation of labour using synthetic oxytocin (Recours aux ocytociques); effect of Bishop score on admission on duration of labour (Effet du score de Bishop à l’admission sur la durée (duration) du travail (labour); progress in labour; time between final dose of PE2 gel and birth Baby: duration of infant’s hospital stay (hours); total cost of care; admission to neonatal unit; stained amniotic fluid; Apgar score at 1 minute; perinatal death; stillbirth; neonatal death; macrosomia; signs of post‐maturity; need for resuscitation at birth; number of doses of gel administered |
|
| Notes | This article is in French. Funding: not reported Declaration of interests: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by computer |
| Allocation concealment (selection bias) | Unclear risk | Article in French. Appeared not to have been reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No apparent losses to follow‐up or exclusions |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol to confidently assess selective reporting |
| Other bias | Low risk | Appeared to be free of other bias |
Sande 1983.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 166
Setting: Ulleval Hospital, Norway Study date: not reported Inclusion criteria
Exclusion criteria
State of cervix: Bishop score ≥ 5 |
|
| Interventions |
Induction group (n = 76): IOL on the following morning after randomisation; IV oxytocin (10 units in 1 L 5% glucose) immediately following AROM. Women were monitored by CTG versus EM group (n = 90): waited for spontaneous labour to occur, following the normal procedure for the department (labour was induced after 42 weeks) |
|
| Outcomes |
Mother: duration of first and second stages of labour; pain relief; mode of birth (caesarean birth; vacuum; forceps; spontaneous birth); postpartum bleeding; induction to birth interval Baby: liveborn; neonatal death; birthweight; Apgar scores at 1 and 5 minutes; morbidity (transfer to NICU; paediatric examination of 1st and 5th day) |
|
| Notes | Only data for perinatal death, stillbirth and neonatal death included in meta‐analyses | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generated was not reported. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Per protocol analysis performed. Of the 76 women randomised to the induction group, 23 birthed spontaneously before induction In the EM group, 15 of the 90 women passed 42 weeks and had their labour induced. Therefore, there were a total of 68 women who had their labour induced, and 98 birthed spontaneously (results analysed as such, not as per randomisation). |
| Selective reporting (reporting bias) | High risk | A number of outcomes such as birthweight, postpartum bleeding, and neonatal morbidity were reported incompletely in the text, e.g. “no differences” and “ns.” |
| Other bias | Unclear risk | No information by randomisation group |
Sargunam 2019.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 318
Setting: University hospital in Malaysia Study date: recruitment 5 June 2015 to 10 November 2017 Inclusion criteria: GA: ≥ 39 weeks* (≥ 273 days); prolonged latent phase of labour (defined as an overnight hospitalisation of at least 8 hours), persistent contractions of at least 1 in 30 minutes, cervical dilation ≤ 3 cm and intact membranes, nulliparous (no prior pregnancy > 20 weeks), a singleton fetus, cephalic presentation, reassuring FHR tracing Exclusion criteria: known fetal abnormalities, estimated fetal weight ≥ 4 kg or ≤ 2 kg (clinical assessment for small or large for GA, if either suspected then ultrasound EFW), contraindications to EM (e.g. pregnancy‐induced hypertension, suspected abruption), previous uterine surgery (e.g. myomectomy or hysterotomy), known prostaglandin allergy or contraindication to vaginal birth State of cervix: mixed, mean Bishop Score 4.3 [1.6] intervention group; 4.1 [1.4] comparator Parity: nulliparous |
|
| Interventions |
Induction group (n = 158): immediate IOL (with vaginal dinoprostone or amniotomy or oxytocin as appropriate) EM group (n = 160): await labour for at least 24 hours unless indicated intervention as directed by care provider |
|
| Outcomes |
Mother: caesarean; vaginal birth (including instrumental versus spontaneous); labour duration outcomes (intervention to active phase of labour i.e. cervical dilation ≥ 5 cm and time to birth); epidural analgesia needed, intrapartum oxytocin, titrated oxytocin infusion or vaginal dinoprostone pessary (nonreassuring fetal heart tracing concurrent with uterine tachysystole ≥ 6 contractions in 10 minutes), postpartum haemorrhage (blood loss ≥ 500 mL), women's satisfaction (Likert response) to allocated intervention, during birth and baby outcomes ‐ obtained before hospital discharge Baby: 5 minute Apgar score < 7; cord artery acidosis (pH ≤ 7 and base excess ≤ ‐8 mmol/L; birthweight; admission to NICU; indications for admission |
|
| Notes | *ISRCTN protocol stated 39‐41 weeks GA; also registered as Malaysian National Medical Research Register NMRR‐15.16‐23,886 Funding: "This study was internally funded by University of Malaya research grant (BK078‐2015)". Declaration of interests: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "computer generated random sequence using random.org" |
| Allocation concealment (selection bias) | Low risk | Web‐based/central randomisation and by an investigator who was not involved in the trial. Participants were randomised by opening the lowest numbered, sealed, opaque envelope remaining. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported ‐ unlikely considering the type of interventions compared |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported ‐ unlikely for most outcomes assessed |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "318 women were randomized (158 to labor induction and 160 to expectant management). Due to criteria infringements, we excluded nine women allocated to labor induction due to 1) labor induction refusal (four women), 2) membranes already ruptured (three women) and 3) pre‐induction non‐reassuring FHR tracing (two women) and one women assigned to expectant management due to membranes already ruptured". Assessed as unclear due to differential attrition in the 2 groups: 9/158 versus 1/160 |
| Selective reporting (reporting bias) | Low risk | Outcomes specified in prospectively registered protocol reported |
| Other bias | Low risk | Data reported on key characteristics of participants, indicating few differences between groups |
Suikkari 1983.
| Study characteristics | ||
| Methods | Randomised trial, no further details | |
| Participants | Number of women randomised: 119
Setting: Lappenranta, Finland Study date: recruitment October 1980 to December 1981 Inclusion criteria
Exclusion criteria
State of cervix: not used as a criterion |
|
| Interventions |
Induction group (n = 66): oxytocin alone or with AROM depending on the cervix versus EM group (n = 53): obstetric examination, NST, biochemical tests and amniotic fluid determination every 3 days |
|
| Outcomes | Mother: mode of birth (reported only as operative); duration of labour; mean blood loss during labour; maternal death Baby: mean birthweight; Apgar scores; perinatal death; stillbirth; neonatal death | |
| Notes | The study was available as an abstract only. Funding: not reported Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generated was not reported. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to determine losses to follow‐up or exclusions |
| Selective reporting (reporting bias) | Unclear risk | No outcomes were prespecified (abstract). |
| Other bias | Unclear risk | Unable to identify other bias based on the abstract; some degree of imbalance in numbers randomised to each group (66 and 53). |
Tylleskar 1979.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 112
Setting: Linköping and Motala, Sweden Study date: not reported Inclusion criteria
Exclusion criteria
State of cervix: primipara with pelvic score of at least 5 points and engaged head; multipara with pelvic score at least 4 points |
|
| Interventions |
Induction group (n = 57): after AROM, an open‐ended saline‐filled catheter was inserted for measurement of intraamniotic pressure and a scalp electrode applied for continuous recording of FHR. IV oxytocin (using Cardiff Infusion System Mark II) was started 15 minutes later at 1 mU/minute, increased continuously until the intensity of contractions was at least 33 mm Hg, with a frequency of at least 1 contraction every 150 seconds; the infusion rate doubled every 12.5 minutes. versus EM group (n = 55): women were asked to come to the delivery ward as soon as labour started; external CTG recordings were made until definite labour activity was demonstrated. AROM was performed, a catheter and scalp electrode applied when for primipara the cervix was at least 50% effaced and dilated more than 2 cm, and for multipara when the cervix was dilated to 3 cm. If the pregnancy lasted more than 14 days beyond the estimated time of birth labour was induced using IV oxytocin. |
|
| Outcomes |
Mother: duration of labour; uterine activity at 6 cm cervical dilatation; total amount of oxytocin used; FHR patterns (early decelerations; late decelerations; bradycardia); amount of bleeding during the third stage of labour; mode of birth (vacuum extraction); placental retention; maternal pH at birth; analgesia (pudendal block, nitrous oxide, pethidine/atarax); women's experiences of the birth Baby: birthweight; birth asphyxia; Apgar score at 1 and 5 minutes; baby pH; lowest weight in first week; haemoglobin and haematocrit in umbilical vein and day 2; bilirubin levels day 1‐3; 4 dimensions of the Brazelton Scale |
|
| Notes |
Funding: not reported Declaration of interests: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The method of sequence generated was not reported. |
| Allocation concealment (selection bias) | Unclear risk | The method of allocation concealment was not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 112 women were randomised. 13/57 in the induction group and 12/55 in the EM group went into labour before the expected due date and were excluded. 3 further women were excluded – 1 in the EM group birthed rapidly and data collection was not possible; 1 woman in each group had a caesarean due to feto‐pelvic disproportion. Thus 43/57 in the induction group and 41/55 in the EM group were analysed; overall 84/112 (75%). |
| Selective reporting (reporting bias) | High risk | Results for a number of outcomes are reported incompletely, e.g. "Nor were there any differences in maternal pH at delivery"; "Analgesia in the form of pudendal block or nitrous oxide was given in the same frequency in the two groups;" and "An analysis of the questionnaire with respect to the patients experiences of the delivery indicate a positive attitude... No statistical differences between groups were found." |
| Other bias | Unclear risk | Limited methodological detail provided. The only baseline characteristics reported were age, pelvic score and number of previous pregnancies, and only for women analysed. |
Walker 2016.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 619
Setting: 39 National Health Service hospitals, UK Study date: women recruited August 2012 to March 2015 Inclusion criteria
Exclusion criteria
State of cervix: not clearly reported (mixed) |
|
| Interventions |
Induction group (n = 305): IOL between 390 and 396 weeks, with method dependent on local protocol and cervical ripeness (most participating units used prostaglandin ripening followed, if necessary, by AROM and oxytocin). Prostaglandin tablet regimen (n = 49), prostaglandin gel regimen (n = 63), prostaglandin slow release pessary (N = 158), AROM (n = 129), oxytocin (n = 137) (women could have > 1 intervention) versus EM group (n = 314): waiting for spontaneous onset of labour, unless a situation developed necessitating birth by IOL or caesarean. Women underwent IOL between 41‐42 weeks (7‐14 days after due date) depending on preference and physician's usual practice; if a woman declined induction at 42 weeks, she could undergo a scan to determine fetal growth and amniotic fluid volume daily or every other day, CTG and monitoring according to usual practice. |
|
| Outcomes |
Mother: caesarean; method of birth; onset of labour; indication for induction; method of induction; indication for caesarean; intrapartum and postpartum complications (e.g. systemic infection, need for blood transfusion); mother’s expectations and experience of childbirth; analgesia; perineal trauma; postpartum haemorrhage Baby: live or stillbirth; birthweight; admission to NICU; birth trauma; 2 composite outcomes for serious neonatal complications (direct trauma and hypoxia); Apgar < 7 at 5 minutes |
|
| Notes | Staff were encouraged to use the same methods of IOL in the induction group and the EM group who were subsequently induced. Funding: Grant (PB‐PG‐0610‐22275) from the Research for Patient Benefit Programme of the National Institute for Health Research Declarations of interest: Dr. Smith reported receiving fees for serving on an advisory board from Roche Diagnostics, consulting fees from GlaxoSmithKline, equipment loans from Roche Diagnostics and General Electric, travel support from Roche Diagnostics and Chiesi, and grant support from GlaxoSmithKline and Action Medical Research, and being named as an inventor on a pending patent (PCT/EP2014/062602) filed by GlaxoSmithKline related to retosiban as a preventive treatment for preterm labour in women with increased uterine stretch. No other potential conflict of interest relevant to this article was reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 1:1 ratio using a computer‐generated code with the use of permuted blocks of randomly varying size generated by a clinical trials unit. Stratified by trial centre and maternal age |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed by using central allocation by the Clinical Trials Unit |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not feasible. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Analysis included all but 1/619 women; 83% completed childbirth experience questionnaires |
| Selective reporting (reporting bias) | Low risk | Trial protocol published |
| Other bias | Low risk | Appeared to be free of other bias |
Wennerholm 2019.
| Study characteristics | ||
| Methods | Multicentre RCT: ISRCTN26113652 | |
| Participants | 2760* healthy women ≥ 18 years old with a singleton pregnancy in cephalic presentation at 41+0 weeks Setting: 14 hospitals in Sweden. Study date: recruitment 20 May 2016 to 13 October 2018. Trial undertaken within the Swedish Network for National Clinical Studies within Obstetrics and Gynaecology (SNAKS) Inclusion criteria: women 18 years or older, able to understand oral and written information, cephalic presentation at 40 + 6 to 41 + 1 weeks according to ultrasound based dating in first or second trimesteror for pregnancies after assisted reproduction according to day of oocyte retrieval Exclusion criteria: previous caesarean section or other uterine surgery, pregestational or insulin dependent diabetes, hypertensive disorder of pregnancy, known oligohydramnios (amniotic fluid index < 50 mm or deepest vertical pocket < 20 mm), or small for gestational age fetus (estimated fetal weight ≤ 2 standard deviations according to the sex and gestational age specific to Swedish reference), diagnosed fetal anomaly, contraindication to vaginal birth, and any other maternal condition affecting the progress of the pregnancy to 42 weeks. Parity: 55% nulliparous State of cervix: mixed |
|
| Interventions |
Induction group (n = 1381): labour induction at 41 weeks' gestation (early induction); randomisation was done between 40+6 weeks and 41+1 weeks. Labour was induced within 24 hours of randomisation (same or next day). Expectant group (n = 1379): EM and induction at 42 weeks' gestation (late induction). Labour was induced at 42 weeks+0 to 42 weeks+1. IOL was carried out in the same way in both groups: Amniotomy was performed if the fetal head was well engaged and the cervix was ripe (Bishop score ≥ 6 for primiparous women and ≥ 5 for multiparous women), followed by oxytocin infusion after 1‐2 hours without spontaneous regular contractions. If the fetal head was not engaged and the cervix was less ripe, any of the following methods was used according to local routines: mechanical dilation with a Foley‐like catheter, prostaglandin E1 (misoprostol, oral or vaginal), prostaglandin E2 (dinoprostone, vaginal). |
|
| Outcomes |
Primary outcome: composite of stillbirth, neonatal death and neonatal morbidity (defined as at least 1 of the following variables: Apgar score < 7 at 5 minutes, metabolic acidosis defined as pH < 7.05 and base deficit > 12 mmol/L in umbilical artery or pH < 7.00 in umbilical artery, HIE I‐III, intracranial haemorrhage, neonatal convulsions, meconium aspiration syndrome, mechanical ventilation, obstetric brachial plexus injury) Mother: use of epidural anaesthesia, caesarean, operative vaginal birth, duration of labour (from onset of regular contractions to birth), chorioamnionitis, shoulder dystocia, third‐ or fourth‐degree perineal tear, postpartum haemorrhage (> 1000 mL), wound infection, urinary tract infection, endometritis, sepsis, and breastfeeding at discharge from hospital and at 4 weeks postpartum; cervical tear, uterine rupture, hypertensive disorders of pregnancy (pre‐eclampsia, gestational hypertension, eclampsia), venous thromboembolism, duration of stay in hospital, ICU admission, mortality with 42 days. Baby: components of composite; admission to NICU, Apgar score < 4 at 5 minutes, birthweight, macrosomia (≥ 4500 g), neonatal jaundice, therapeutic hypothermia, pneumonia, or sepsis: neonatal hypoglycaemia, birth trauma (fracture of long bone, clavicle or skull, other neurological injury, retinal haemorrhage, or facial nerve palsy), SGA and LGA. |
|
| Notes |
Funding: Swedish Government and county councils, Health Technology Centre at Sahlgrenska University Hospital, Foundation of the Health and Medical Care committee of the Region of Vastra Gotaland, Sweden, Hjalmar Svensson Foundation, Foundation Mary von Sydow, born Wijk donation fund, Uppsala‐Orebro regional research council, region Orebro County research committee, ALF agreement in Stockholm, Centre for Clinical Research Dalama‐Uppsala University, Sweden. The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The researchers were independent of the funders. All authors declared no support from any organisation for the submitted work; no financial relationship with any organisation that might have an interest in the submitted work in the previous three years, no other relationships or activities that could appear to have influenced the submitted work. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Central online randomisation by dynamic allocation (actively minimises the imbalance between groups, by using centre and parity as variables) |
| Allocation concealment (selection bias) | Low risk | As above |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind women or staff |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not feasible to blind women or staff |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2/1383 women in the intervention group withdrew consent before intervention. |
| Selective reporting (reporting bias) | Low risk | Protocol published; extensive range of outcomes reported (with individual components of composite reported separately) |
| Other bias | Low risk | Baseline characteristics similar |
Witter 1987.
| Study characteristics | ||
| Methods | RCT | |
| Participants | Number of women randomised: 200
Setting: Baltimore, USA Study date: not reported Inclusion criteria
Exclusion criteria No additional criteria reported State of cervix: not mentioned |
|
| Interventions |
Induction group (n = 103): oxytocin infusion with AROM when possible
versus EM group (n = 97): Estriol measurements 2‐3/week. In both groups women initiated fetal movement counting. If reduced fetal movements, FHR and estriol testing were undertaken at 41 completed weeks. |
|
| Outcomes | Mother: GA at birth; length of hospital stay; urinary estriol/creatinine ratio; maternal complications; endometritis; pre‐eclampsia; PROM; caesarean section + indications Baby: birthweight; biparietal diameter; placental weight; Dubowitz score (assesses infant GA); SGA/AGA/LGA; fetal distress; meconium staining; infant complications; Apgar scores (< 7 at 5 minutes); fetal anomalies; post‐mature infants; meconium aspiration | |
| Notes |
Funding: not reported Declarations of interest: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation sequence was generated using a computer‐generated random number table. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment was achieved using sequentially labelled sealed envelopes, but there was no mention of opaqueness. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Appeared that blinding was not feasible |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinded outcome assessment was not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3/103 women and 2/97 women in the induction and EM groups dropped out of the study; 35/103 women and 39/97 in the induction and EM groups birthing prior to 42 completed weeks (and were included); all were included in the analyses. |
| Selective reporting (reporting bias) | Unclear risk | No detailed outcomes were prespecified in the methods; perinatal death was not reported. No access to trial protocol to further assess selective reporting |
| Other bias | Low risk | Appeared to be free of other bias |
AGA: appropriate for gestational age; AROM: artificial rupture of membranes/amniotomy; CTG: cardiotocography; EBL: estimated blood loss; EFW: estimation of fetal weight; EM: expectant management; FHR: fetal heart rate; GA: gestational age; HIE: hypoxic ischaemic encelopathy; HIV: human immunodeficiency virus; IOL: induction of labour; IND: induction; ITT: intention to treat; IU: international units; IUFD: intrauterine fetal death IUGR: intrauterine fetal growth restriction IV: intravenous; IVF: in‐vitro fertilisation; LGA: large‐for‐gestational age; LMP: last menstrual period mIU: milli‐international units; mU: milli‐units; NICU: neonatal intensive care unit; NST: nonstress test; PGE2 (and PE2): prostaglandin E2; PROM: premature rupture of membranes; RCT: randomised controlled trial; ROM: rupture of membranes; SGA: small‐for‐gestational age
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alcalay 1996 | PROM at term |
| Amano 1999 | Alternate allocation trial |
| Ascher‐Walsh 2000 | Compared 2 forms of IOL |
| Bell 1993 | Trial of cervical ripening not IOL |
| Berghella 1996 | Membrane stripping to decrease the need for formal IOL |
| Boulvain 1998 | Membrane stripping to decrease the need for formal IOL |
| Buttino 1990 | Trial of cervical ripening not IOL |
| Cardozo 1986 | Alternate allocation trial |
| Conway 2000 | Trial of active versus expectant management in women with oligohydramnios |
| CTRI/2018/09/015719 | High‐risk pregnancy (women with previous caesarean) included in this trial |
| Damania 1992 | Trial of cervical ripening (2 methods) not IOL |
| Dare 2002 | Trial of cervical ripening not IOL |
| De Aquino 2003 | Compares 2 forms of IOL |
| Doany 1997 | Trial of cervical ripening not IOL |
| Dunn 1989 | Intervention not a policy to induce labour compared with expectant management |
| El‐Torkey 1992 | Trial of cervical ripening not IOL |
| Elliott 1984 | Trial of nipple stimulation as a method of cervical ripening. No commitment to delivery within a given time or protocol |
| Evans 1983 | Compares 2 forms of IOL |
| Frass 2011 | Trial where all women were judged to be at risk (severe pre‐eclampsia) |
| Garry 2000 | Alternate allocation trial |
| Giacalone 1998 | Trial of cervical ripening not IOL |
| Gregson 2015 | Assessing effectiveness of acupuncture for IOL (role of acupuncture not established) |
| Hage 1993 | Trial of cervical ripening not IOL |
| Heden 1991 | Alternate allocation trial |
| Hernandez‐Castro 2008 | Not a RCT |
| Imsuwan 1999 | This is a RCT evaluating the effectiveness of weekly membrane sweeping in labour initiation for women at 41 completed weeks. It is not evaluating a policy of stopping the pregnancy at 41 weeks |
| Ingemarsson 1987 | Trial of cervical ripening not IOL |
| Iqbal 2004 | Alternate allocation trial |
| Jenssen 1977 | Trial of cervical ripening not IOL |
| Kadar 1990 | Trial of nipple stimulation as a method of cervical ripening. No commitment to delivery within a given time or protocol |
| Katz 1983 | Alternate allocation trial |
| Kipikasa 2005 | Comparing alternate methods for IOL |
| Klopper 1969 | Trial of cervical ripening not IOL |
| Knox 1979 | Quasi‐randomised (last digit of hospital number) |
| Lee 1997 | Compares 2 forms of IOL |
| Lemancewicz 1999 | Compares 2 forms of IOL |
| Lien 1998 | Trial of cervical ripening not IOL |
| Lyons 2001 | Trial of cervical ripening not IOL |
| Magann 1998 | Trial of cervical ripening not IOL |
| Magann 1999 | Compares 2 forms of IOL |
| Mancuso 1998 | Compares 2 forms of IOL |
| Meydanli 2003 | Compares 2 forms of IOL |
| Misra 1994 | Compares 2 forms of IOL |
| Müller 1995 | Compares 2 forms of IOL |
| Neri 2014 | Assessing effectiveness of acupressure for IOL (role of acupuressure not established) |
| Newman 1997 | Trial of cervical ripening not IOL |
| Nicholson 2008 | Trial where all women were judged to be at risk |
| Ohel 1996 | Alternate allocation |
| PACTR201805002872322 | Not low risk pregnancies |
| Papageorgiou 1992 | Compared 2 forms of IOL |
| Paul 1988 | Protocol for RCT only ‐ no results |
| Rayburn 1988 | Trial of cervical ripening not IOL |
| Rayburn 1999 | Trial of cervical ripening not IOL |
| Rijnders 2011 | Compared 2 alternative management strategies for IOL |
| Roberts 1986 | Trial of cervical ripening not IOL |
| Satin 1991 | Compared 2 forms of IOL |
| Sawai 1991 | Trial of cervical ripening not IOL |
| Sawai 1994 | Trial of cervical ripening not IOL |
| Stenlund 1999 | Mifepristone versus placebo for IOL, but all women given PGE2 if necessary after 48 hours |
| Su 1996 | Both groups induced within 2 days with alternative methods |
| Surbek 1997 | Compared 2 forms of IOL |
| Suzuki 1999 | Immediate IOL versus expectant management in twin pregnancies |
| Williams 1990 | Trial of cervical ripening not IOL |
| Wing 2000 | Trial of cervical ripening not IOL |
| Wong 2002 | Trial of cervical ripening not IOL |
| Ziaei 2003 | Trial of cervical ripening not IOL |
IOL: induction of labour PGE2: prostaglandin E2 PROM: premature rupture of membranes RCT: randomised controlled trial
Characteristics of studies awaiting classification [ordered by study ID]
Benito Reyes 2010.
| Methods | Quote: "prospective study" |
| Participants | 200 |
| Interventions | Elective induction versus expectant management |
| Outcomes | Caesarean section |
| Notes |
ISRCTN74323479.
| Methods | RCT (ISRCTN74323479) |
| Participants | 100 pregnant primiparous women who have not laboured at or beyond 41 weeks' gestation with cervical length > 3 cm |
| Interventions | Mifepristone versus standard care |
| Outcomes | Length of time from induction to onset of labour |
| Notes |
Characteristics of ongoing studies [ordered by study ID]
ISRCTN15646866.
| Study name | Induction of labour at 39 weeks or beyond in multiparous women with a favourable cervix (ISRCTN15646866) |
| Methods | RCT |
| Participants | 160 pregnant women ≥ 39 weeks' gestation, with at least 1 previous vaginal birth |
| Interventions | 1) induction of labour at 39 weeks 2) expectant management with recommendation to induce at 41 weeks if woman has not given birth |
| Outcomes | Time of giving birth; maternal satisfaction |
| Starting date | 30 September 2016 |
| Contact information | Dr Aida Othman, Dept Obstetrics & Gynaecology, University Malaya Medical Centre, Kuala Lumpur, 59100, Malaysia |
| Notes |
ISRCTN83219789.
| Study name | The Finnish randomised controlled multicentre trial on optimal timing of labor induction in nulliparous women with post‐term pregnancy (ISRCTN83219789) |
| Methods | RCT |
| Participants | Nulliparous pregnant women (n = 600) |
| Interventions | 1) induction at 41 + 0 weeks 2) induction at 41 + 5 to 42 + 1 weeks, according to hospital policy |
| Outcomes | Caesarean section |
| Starting date | March 2018 |
| Contact information | Associate Professor Leena Rahkonen, Department of Obstetrics and Gynecology, Helsinki University Hospital, Haartmaninkatu 2, Helsinki 00029 HUS, Finland Tel: +358 504 271248, E‐mail: leena.rahkonen@hus.fi |
| Notes |
CPAP: continuous positive airway pressure GW: gestational weeks HIE: Hypoxic ischaemic encephalopathy IVH: intraventricular haemorrhage RCT: Randomised controlled trial
Differences between protocol and review
2020 update of the review
The title has been changed to 'Induction of labour at or beyond 37 weeks' gestation' to reflect increasing debate about how 'term' should be defined.
The subgroup analyses by gestational age are now reported by induction at < 40 weeks; 40 to 41 weeks; and > 41 weeks.
We have included an additional subgroup analysis based on parity.
2018 update of the review
We have updated the methods in line with those in the standard template used by Cochrane Pregnancy and Childbirth.
We have omitted the outcome of vaginal birth as it is the obverse of caesarean section.
We have used the GRADE approach to assess the quality of the body of evidence and we have included ’Summary of findings’ tables.
We have added three new infant secondary outcomes (birthweight; birthweight > 4000 g; neonatal trauma), which were reported as non‐prespecified, but important, outcomes in the previous version of this review, in our main outcomes list.
The secondary infant outcome 'Perinatal death (stillbirth, newborn deaths within first week)' (which is the same as the primary outcome) has been changed to two separate outcomes, 'Stillbirth' and 'Neonatal death within the first week'.
The subgroup analyses by gestational age are now reported by induction at < 41 weeks; and at ≥ 41 weeks.
We have added in an additional search of ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform (ICTRP).
In the previous (Gülmezoglu 2012) update of this review:
The subgroup analyses by gestational age were reported by induction at 39 to 40 weeks; at 41 weeks; and at > 41 weeks.
The methods were updated to reflect the latest Cochrane Handbook for Systematic Reviews of Interventions version (Higgins 2011).
Contributions of authors
For this updated review, Philippa Middleton (PM), Emily Shepherd (ES) and Judith Gomersall (JG) applied the selection criteria, extracted data for included studies, assessed risk of bias, carried out GRADE assessments and prepared SoF tables. All five authors (PM, ES, JG, Jonathan Morris, Caroline Crowther) contributed to drafting and editing of this update.
Sources of support
Internal sources
Robinson Research Institute, The University of Adelaide, Adelaide, Australia
Women and Kids, South Australian Health and Medical Research Institute (SAHMRI), Adelaide, Australia
Liggins Institute, The University of Auckland, Auckland, New Zealand
External sources
-
NHMRC: National Health and Medical Research Council, Australia
Funding for the Cochrane Pregnancy and Childbirth Australian and New Zealand Satellite
-
NIHR: National Institute for Health Research, UK
NIHR Cochrane Programme Grant Project: 13/89/05 – Pregnancy and childbirth systematic reviews to support clinical guidelines
-
UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Sexual and Reproductive Health and Research, World Health Organization, Switzerland
This review is supported by funding to Cochrane Pregnancy and Childbirth (University of Liverpool)
Declarations of interest
Philippa Middleton: none known.
Caroline A Crowther: none known.
Jonathan Morris: none known.
Emily Shepherd: none known.
Judith Gomersall: none known.
Edited (no change to conclusions)
References
References to studies included in this review
Augensen 1987 {published data only}
- *.Augensen K, Bergsjo P, Eikeland T, Ashvik K, Carlsen J. Randomized comparison of early versus late induction of labour in post-term pregnancy. BMJ 1987;294:1192-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augensen K, Bergsjo P, Eikeland T, Askvik K, Carlsen J. Induction of labour in prolonged pregnancy. A prospective randomized study. In: Jaehrig K, Woraschk H-J, Roepke F , editors(s). 10th European Congress of Perinatal Medicine; 1986 Aug 12-16; Leipzig, Germany. 1986.
Baev 2017 {published data only}
- *.Baev O, Rumyantseva V, Tysyachnyu O. Randomized trial of labour preinduction with mifepristone versus expectant management. International Journal of Gynecology and Obstetrics 2018;143(S3):277. [Google Scholar]
- Baev OR, Rumyantseva VP, Tysyachnyu OV, Kozlova OA, Sukhikh GT. Outcomes of mifepristone usage for cervical ripening and induction of labour in full-term pregnancy. Randomized controlled trial. European Journal of Obstetrics Gynecology and Reproductive Biology 2017;217:144-9. [DOI] [PubMed] [Google Scholar]
Bergsjo 1989 {published data only}
- Bergsjo P, Huang GD, Yu SQ, Gao Z, Bakketeig LS. Comparison of induced vs non-induced labor in post-term pregnancy. Acta Obstetricia et Gynecologica Scandinavica 1989;68:683-7. [DOI] [PubMed] [Google Scholar]
Brane 2014 {published data only}
- Brane E, Olsson A, Andolf E. A randomized controlled trial on early induction compared to expectant management of nulliparous women with prolonged latent phases. Acta Obstetricia Et Gynecologica Scandinavica 2014;93:1042-9. [DOI] [PubMed] [Google Scholar]
Breart 1982 {published data only}
- Breart G, Goujard J, Maillard F, Chavigny C, Rumeau-Rouquette C, Sureau C. Comparison of two obstetrical policies with regard to artificial induction of labour at term. A randomised trial. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 1982;11:107-12. [PubMed] [Google Scholar]
Chakravarti 2000 {published data only}
- Chakravarti S, Goenka B. Conservative policy of induction of labor in uncomplicated postdated pregnancies. In: XVI FIGO World Congress of Obstetrics & Gynecology; 2000 Sept 3-8; Washington DC, USA (Book 3). 2000:62.
Chanrachkul 2003 {published data only}
- Chanrachkul B, Herabutya Y. Postterm with favorable cervix: is induction necessary? European Journal of Obstetrics & Gynecology and Reproductive Biology 2003;106:154-7. [DOI] [PubMed] [Google Scholar]
Cohn 1992 {published data only}
- Cohn M, Rogers M. Post maturity; a randomised study in a Hong Kong population. In: 26th British Congress of Obstetrics and Gynaecology; 1992 July 7-10; Manchester, UK. 1992:306.
Cole 1975 {published data only}
- *.Cole RA, Howie PW, MacNaughton MC. Elective induction of labour. A randomised prospective trial. Lancet 1975;1:767-70. [DOI] [PubMed] [Google Scholar]
- Engleman SR, Hilland MA, Howie PW, McIlwaine GM, McNay MB. An analysis of the economic implications of elective induction of labour at term. Community Medicine 1979;1:191-8. [DOI] [PubMed] [Google Scholar]
Dyson 1987 {published data only}
- *.Dyson D, Miller PD, Armstrong MA. Management of prolonged pregnancy: induction of labour versus antepartum testing. American Journal of Obstetrics and Gynecology 1987;156:928-34. [DOI] [PubMed] [Google Scholar]
- Dyson DC, Miller P, Miller M. Management of prolonged pregnancy - induction versus antepartum fetal testing. In: 6th Annual Meeting of the Society of Perinatal Obstetricians; 1986 Jan 30-Feb 1; San Antonio, Texas, USA. 1986:205.
Egarter 1989 {published data only}
- *.Egarter CH, Kofler E, Fitz R, Husslein P. Is induction of labour indicated in prolonged pregnancy? Results of a prospective randomised trial. Gynecologic and Obstetric Investigation 1989;27:6-9. [DOI] [PubMed] [Google Scholar]
- Husslein P, Egarter C, Sevelda P, Genger H, Salzer H, Kofler E. Induction of labour with Prostaglandin E2 vaginal tablets - a revival of elective induction? Results of a prospective randomised trial [Geburtseinleitung mit 3mg Prostaglandin E2-vaginaltabletten: eine renaissance der programmierten geburt?]. Geburtshilfe und Frauenheilkunde 1986;46:83-7. [DOI] [PubMed] [Google Scholar]
Gelisen 2005 {published data only}
- Gelisen O, Caliskan E, Dilbaz S, Ozdas E, Dilbaz B, Ozdas E, et al. Induction of labor with three different techniques at 41 weeks of gestation or spontaneous follow-up until 42 weeks in women with definitely unfavorable cervical scores. European Journal of Obstetrics & Gynecology and Reproductive Biology 2005;120(2):164-9. [DOI] [PubMed] [Google Scholar]
Grobman 2018 {published data only}
- El-Sayed YY. 23: factors associated with adverse outcomes in nulliparas at 39 weeks with induction or expectant management. American Journal of Obstetrics and Gynecology 2019;220(1):S20. [Google Scholar]
- Grobman WA, Grecio Sandoval MA, Reddy UM, Tital ATN, Silver RM, Mallett G, et al. Health resource utilization of labor induction versus expectant management. American Journal of Obstetrics and Gynecology 2020;222(4):369.e1-369.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Grobman WA, Rice MM, Reddy UM, Tita ATN, Silver RM, Mallett G, et al. Labor induction versus expectant management in low-risk nulliparous women. New England Journal of Medicine 2018;379(6):513-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grobman WA. 2: resource utilization among low-risk nulliparas randomized to elective induction at 39 weeks or expectant management. American Journal of Obstetrics and Gynecology 2019;220(1):S2-S3. [Google Scholar]
- NCT01990612. A randomised trial of induction versus expectant management (ARRIVE). clinicaltrials.gov/ct2/show/NCT01990612 (first received 21 November 2013).
Hannah 1992 {published data only}
- Farquharson D, Hannah ME, Hannah WJ, Hewson SA, Willan A, Young D, et al. The Canadian multicentre postterm pregnancy trial (CMPPT): outcome in the induction group based on method of induction. In: 49th Annual Clinical Meeting of the Society of Obstetricians and Gynaecologists of Canada; 1993 June 22-26; Ottawa, Ontario, Canada. 1993:15.
- Goeree R, Hannah M, Hewson S, Canadian Postterm Pregnancy Trial Group. Cost-effectiveness of induction of labour versus serial antenatal monitoring in the Canadian multicentre postterm pregnancy trial. Canadian Medical Association Journal 1995;152:1445-50. [PMC free article] [PubMed] [Google Scholar]
- Hannah M, Canadian MG. The Canadian Multicentre Postterm Pregnancy trial. International Journal of Gynecology & Obstetrics 1994;46:31. [Google Scholar]
- *.Hannah ME, Hannah WJ, Hellman J, Hewson S, Milner R, Willan A. Induction of labour as compared with serial antenatal monitoring in post-term pregnancy. A randomized controlled trial. New England Journal of Medicine 1992;326:1587-92. [DOI] [PubMed] [Google Scholar]
- Hannah ME, Huh C, Hewson SA, Hannah WJ. Postterm pregnancy: putting the merits of a policy of induction into perspective. Birth 1996;23(1):13-9. [DOI] [PubMed] [Google Scholar]
Heimstad 2007 {published data only}
- Heimstad R, Romundstad PR, Hyett J, Mattsson LA, Salvesen KA. Women's experiences and attitudes towards expectant management and induction of labor for post-term pregnancy. Acta Obstetricia et Gynecologica Scandinavica 2007;86(8):950-6. [DOI] [PubMed] [Google Scholar]
- Heimstad R, Skogvoli E, Mattsson L, Johansen OJ, Eik-Nes SH, Romundstad PR, et al. Induction of labour or serial antenatal fetal monitoring in post-term pregnancy. A randomised controlled trial. In: 36th Nordic Congress of Obstetrics and Gynecology; 2008 June 14-17; Reykjavik, Iceland. 2008:84. [DOI] [PubMed]
- *.Heimstad R, Skogvoll E, Mattsson LA, Johansen OJ, Eik-Nes SH, Salvesen KA. Induction of labor or serial antenatal fetal monitoring in postterm pregnancy: a randomized controlled trial. Obstetrics & Gynecology 2007;109(3):609-17. [DOI] [PubMed] [Google Scholar]
- NCT00385229. Post term pregnancy - induction of labor or monitoring of pregnancy. clinicaltrials.gov/show/NCT00385229 (first received 9 October 2006).
Henry 1969 {published data only}
- Henry GR. A controlled trial of surgical induction of labour and amnioscopy in the management of prolonged pregnancy. Journal of Obstetrics and Gynaecology of the British Commonwealth 1969;76:795-8. [DOI] [PubMed] [Google Scholar]
Herabutya 1992 {published data only}
- Herabutya Y, Prasertsawat PO, Tongyai T, Isarangura N, Ayudthya N. Prolonged pregnancy: the management dilemma. International Journal of Gynecology & Obstetrics 1992;37:253-8. [DOI] [PubMed] [Google Scholar]
James 2001 {published data only}
- James C, George SS, Gaunekar N, Seshadri L. Management of prolonged pregnancy: a randomized trial of induction of labour and antepartum foetal monitoring. National Medical Journal of India 2001;14:270-3. [PubMed] [Google Scholar]
Keulen 2019 {published data only}
- Bruinsma A, Keulen J, Bakker J, Van De Post J, De Miranda E, Kortekaas J, et al. Induction of labor at 41 weeks or expectant management until 42 weeks - preliminary results of the INDEX trial. American Journal of Obstetrics and Gynecology 2017;216(1 Suppl):S27-S28, Abstract no: 40. [Google Scholar]
- Bruinsma A, Keulen J, Kortekaas J, Dillen J, Oudijk M, Bakker J, et al. Induction of labour at 41 weeks or expectant management until 42 weeks in obstetrical low risk women (the INDEX trial). BJOG 2017;124:15. [Google Scholar]
- *.Keulen JK, Bruinsma A, Kortekaas JC, Van Dillen J, Bossuyt PM, Oudijk MA, et al. Induction of labour at 41 weeks versus expectant management until 42 weeks (INDEX): multicentre, randomised non-inferiority trial. BMJ 2019;20(364):1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kortekaas J, Van Dillen J, Vandenbussche F, Bruinsma A, Keulen J, Oudijk M, et al. Induction of labour at 41 weeks versus expectant management until 42 weeks (index-trial). International Journal of Gynecology and Obstetrics 2018;143:256.
- Kortekaas JC, Bruinsma A, Keulen JKJ, Van Dillen J, Oudijk MA, Zwart JJ, et al. Effects of induction of labour versus expectant management in women with impending post-term pregnancies: the 41 week - 42 week dilemma. BMC Pregnancy and Childbirth 2014;14(1):350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mol B. Costs and effects of induction of labour at 41 weeks compared to waiting for spontaneous labour until 42 weeks. trialregister.nl/trialreg/admin/rctview.asp?TC=3431 (first received 12 May 2012).
Martin 1978 {published data only}
- Martin DH, Thompson W, Pinkerton JHM, Watson JD. A randomised controlled trial of selective planned delivery. British Journal of Obstetrics and Gynaecology 1978;85:109-13. [DOI] [PubMed] [Google Scholar]
Martin 1989 {published data only}
- Martin JN, Sessums JK, Howard P, Martin RW, Morrison JC. Alternative approaches to the management of gravidas with prolonged post-term postdate pregnancies. Journal of the Mississippi State Association 1989;30:105-11. [PubMed] [Google Scholar]
Miller 2015 {published data only}
- *.Miller NR, Cypher RL, Foglia LM, Pates JA, Nielsen PE. Elective induction of labor compared with expectant management of nulliparous women at 39 weeks of gestation: a randomized controlled trial. Obstetrics and Gynecology 2015;126(6):1258-64. [DOI] [PubMed] [Google Scholar]
- Miller NR, Cypher RL, Foglia LM, Pates JA, Nielsen PE. Elective induction of nulliparous labor at 39 weeks of gestation: a randomized clinical trial. Obstetrics and Gynecology 2014;123(5 Suppl):72S. [DOI] [PubMed] [Google Scholar]
- NCT01076062. Elective induction of nulliparous labor. clinicaltrials.gov/ct2/show/NCT01076062 (first received 25 February 2010).
NICHHD 1994 {published data only}
- Medearis AL. Postterm pregnancy: active labor induction (PGE2 gel) not associated with improved outcomes compared to expectant management. A preliminary report. In: 10th Annual Meeting of Society of Perinatal Obstetricians; 1990 January 23-27; Houston, Texas, USA. 1990:17.
- *.National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. A clinical trial of induction of labor versus expectant management in postterm pregnancy. American Journal of Obstetrics and Gynecology 1994;170:716-23. [PubMed] [Google Scholar]
Nielsen 2005 {published data only}
- Nielsen PE, Howard BC, Hill CC, Larson PL, Holland RH, Smith PN. Comparison of elective induction of labor with favorable Bishop scores versus expectant management: a randomized clinical trial. Journal of Maternal-Fetal & Neonatal Medicine 2005;18(1):59-64. [DOI] [PubMed] [Google Scholar]
Ocon 1997 {published data only}
- Ocon L, Hurtado R, Coteron JJ, Zubiria A, Ramirez O, Garcia JA. Prolonged pregnancy: procedure guidelines [Gestacion prolongada: pautas de actuacion]. Progresos de Obstetricia y Ginecologia 1997;40:101-6. [Google Scholar]
Roach 1997 {published data only}
- Roach VJ, Rogers MS. Pregnancy outcome beyond 41 weeks gestation. International Journal of Gynecology & Obstetrics 1997;59:19-24. [DOI] [PubMed] [Google Scholar]
Sahraoui 2005 {published data only}
- Sahraoui W, Hajji S, Bibi M, Nouira M, Essaidi H, Khair H. Management of pregnancies beyond forty-one week's gestation with an unfavorable cervix [Prise en charge obstetricale des grossesses prolongees au-dela de 41 semaines d'amenorrhee avec un score de Bishop defavorable]. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 2005;34(5):454-62. [DOI] [PubMed] [Google Scholar]
Sande 1983 {published data only}
- Sande HA, Tuveng J, Fonstelien T. A prospective randomized study of induction of labor. International Journal of Gynecology & Obstetrics 1983;21:333-6. [DOI] [PubMed] [Google Scholar]
Sargunam 2019 {published data only}ISRCTN14099170
- Sargunam PN, Bak LLM, Tan PC, Vallikkannu N, Azmi MAN, Zaidi SN, et al. Induction of labor compared to expectant management of term nulliparas with a latent phase of labor of more than 8 hours: a randomized trial. BMC Pregnancy and Childbirth 2019;19:493. [DOI: 10.1186/s12884-019-2602-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Suikkari 1983 {published data only}
- Suikkari AM, Jalkanen M, Heiskala H, Koskela O. Prolonged pregnancy: induction or observation. Acta Obstetricia et Gynecologica Scandinavica Supplement 1983;116:58. [Google Scholar]
Tylleskar 1979 {published data only}
- Leijon I, Finnstrom O, Hedenskog S, Ryden G, Tylleskar J. Spontaneous labor and elective induction - a prospective randomized study. II Bilirubin levels in the neonatal period. Acta Obstetricia et Gynecologica Scandinavica 1980;59:103-6. [DOI] [PubMed] [Google Scholar]
- Leijon I, Finnstrom O, Hedenskog S, Ryden G, Tylleskar J. Spontaneous labour and elective induction - a prospective randomised study. Behavioural assessment and neurological examination in the newborn period. Acta Paediatrica Scandinavica 1979;68:553-60. [DOI] [PubMed] [Google Scholar]
- Tylleskar J, Finnstrom O, Hedenskog S, Leijon I, Ryden G. Spontaneous delivery-elective induction for convenience, a comparative study. In: 6th European Congress of Perinatal Medicine; 1978 Aug 29-Sept 1; Vienna, Austria. 1978:345.
- *.Tylleskar J, Finnstrom O, Leijon I, Hedenskog S, Ryden G. Spontaneous labor and elective induction - a prospective randomized study. Effects on mother and fetus. Acta Obstetricia et Gynecologica Scandinavica 1979;58:513-8. [DOI] [PubMed] [Google Scholar]
Walker 2016 {published data only}ISRCTN11517275
- ISRCTN11517275. Induction of labour versus expectant management for women over 35 years. isrctn.com/ISRCTN11517275 (first received 23 August 2012).
- Walker K, Bugg G, Macpherson M, McCormick C, Wildsmith C, Smith G, et al. The 35/39 trial: a multi-centre prospective randomised controlled trial of induction of labour versus expectant management for nulliparous women over 35 years of age. International Journal of Gynecology and Obstetrics 2015;131(Suppl 5):E221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker KF, Bugg G, Macpherson M, McCormick C, Wildsmith C, Smith G, et al. Induction of labour versus expectant management for nulliparous women over 35 years of age: a multi-centre prospective, randomised controlled trial. BMC Pregnancy and Childbirth 2012;12:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker KF, Bugg G, Macpherson M, McCormick C, Wildsmith C, Smith G, et al. Induction of labour versus expectant management for nulliparous women over 35 years of age: protocol for a multicentre prospective, randomised controlled trial. BJOG 2013;120(Suppl s1):495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker KF, Bugg GJ, Macpherson M, McCormick C, Wildsmith C, Smith GC, et al. The 35/39 trial: a multicentre prospective randomised controlled trial of induction of labour versus expectant management for nulliparous women over 35 years of age. BJOG 2015;122(Suppl S2):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Walker KF, Bugg J, Macpherson M, McCormick C, Grace N, Wildsmith C, et al. Randomized trial of labor induction in women 35 years of age or older. New England Journal of Medicine 2016;374(9):813-22. [DOI] [PubMed] [Google Scholar]
- Walker KF, Dritsaki M, Bugg G, Macpherson M, McCormick C, Grace N, et al. Labour induction near term for women aged 35 or over: an economic evaluation. BJOG 2017;124(6):929-34. [DOI] [PubMed] [Google Scholar]
Wennerholm 2019 {published data only}ISRCTN26113652
- Elden H, Hagberg H, Wessberg A, Sengpiel V, Herbst A, Bullarbo M, et al. Study protocol of SWEPIS a Swedish multicentre register based randomised controlled trial to compare induction of labour at 41 completed gestational weeks versus expectant management and induction at 42 completed gestational weeks. BMC Pregnancy and Childbirth 2016;16:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISRCTN26113652. Induction of labor at 41 completed gestational weeks versus expectant management and induction at 42 completed gestational weeks. isrctn.com/ISRCTN26113652 (first received 21 March 2015).
- *.Wennerholm UB, Saltvedt S, Wessberg A, Alkmark M, Bergh C, Wendel SB, et al. Induction of labour at 41 weeks versus expectant management and induction of labour at 42 weeks (SWEdish Post-term Induction Study, SWEPIS): multicentre, open label, randomised, superiority trial. BMJ 2019;367:I6131. [DOI] [PMC free article] [PubMed] [Google Scholar]
Witter 1987 {published data only}
- Witter FR, Weitz CM. A randomised trial of induction at 42 weeks of gestation vs expectant management for postdates pregnancies. American Journal of Perinatology 1987;4:206-11. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Alcalay 1996 {published data only}
- Alcalay M, Hourvitz A, Reichman B, Luski A, Quint J, Barkai G, et al. Prelabour rupture of membranes at term: early induction of labour vs expectant management. European Journal of Obstetrics & Gynecology and Reproductive Biology 1996;70:129-33. [DOI] [PubMed] [Google Scholar]
Amano 1999 {published data only}
- Amano K, Saito K, Shoda T, Tani A, Yoshihara H, Nishijima M. Elective induction of labour at 39 weeks of gestation: a prospective randomized trial. Journal of Obstetrics and Gynaecology Research 1999;25:33-7. [DOI] [PubMed] [Google Scholar]
Ascher‐Walsh 2000 {published data only}
- Ascher-Walsh C, Burke B, Baxi L. Outpatient management of prolonged pregnancy with misoprostol (MP): a randomized, double-blind placebo controlled study, prelim. data. American Journal of Obstetrics and Gynecology 2000;182(1 Pt 2):S20. [Google Scholar]
Bell 1993 {published data only}
- Bell RJ, Permezel M, MacLennan A, Hughes C, Healy D, Brennecke S. A randomized, double-blind controlled trial of the safety of vaginal recombinant human relaxin for cervical ripening. Obstetrics & Gynecology 1993;82:328-33. [PubMed] [Google Scholar]
Berghella 1996 {published data only}
- Berghella V, Mickens R. Stripping of membranes as a safe method to reduce prolonged pregnancies. In: XIV World Congress of Gynecology and Obstetrics (FIGO);1994 Sept 26-30; Montreal, Canada. 1994:PO34.16.
- *.Berghella V, Rogers RA, Lescale K. Stripping of membranes as a safe method to reduce prolonged pregnancies. Obstetrics & Gynecology 1996;87:927-31. [DOI] [PubMed] [Google Scholar]
Boulvain 1998 {published data only}
- Boulvain M, Fraser WD, Marcoux S, Fontaine J-Y, Bazin S, Pinault J-J, et al. Does sweeping of the membranes reduce the need for formal induction of labour? A randomised controlled trial. British Journal of Obstetrics and Gynaecology 1998;105:34-40. [DOI] [PubMed] [Google Scholar]
Buttino 1990 {published data only}
- Buttino L, Garite T. Intracervical prostaglandin in postdate pregnancy. Journal of Reproductive Medicine 1990;35(2):155-8. [PubMed] [Google Scholar]
Cardozo 1986 {published data only}
- *.Cardozo L, Fysh J, Pearce JM. Prolonged pregnancy: the management debate. BMJ 1986;293:1059-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardozo L, Pearce JM, Fysh J. Conservative management of post-maturity. Journal of Obstetrics and Gynaecology of the British Commonwealth 1983;4:69-72. [Google Scholar]
- Pearce JM, Cardozo L. Prolonged pregnancy: results of supplemental analysis. BMJ 1988;297:715-7. [Google Scholar]
Conway 2000 {published data only}
- Conway DL, Groth S, Adkins WB, Langer O. Management of isolated oligohydramnios in the term pregnancy: a randomized clinical trial. American Journal of Obstetrics and Gynecology 2000;182:S21. [Google Scholar]
CTRI/2018/09/015719 {published data only}
- CTRI/2018/09/015719. Comparison of induction of labour versus expectant management at 40 weeks on rates of successful vaginal birth in women with previous one caesarean section: A Randomized Controlled Trial and a pilot study. www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=27789 (first received 14 September 2018).
Damania 1992 {published data only}
- Damania KK, Natu U, Mhatre PN, Mataliya M, Mehta AC, Daftary SN. Evaluation of two methods employed for cervical ripening. Journal of Postgraduate Medicine 1992;38(2):58-9. [PubMed] [Google Scholar]
Dare 2002 {published data only}
- Dare FO, Oboro VO. The role of membrane stripping in prevention of post-term pregnancy: a randomised clinical trial in Ile-Ife, Nigeria. Journal of Obstetrics and Gynaecology 2002;22(3):283-6. [DOI] [PubMed] [Google Scholar]
De Aquino 2003 {published data only}
- De Aquino MMA, Cecatti JG. Misoprostol versus oxytocin for labour induction in term and post-term pregnancy: randomized controlled trial. Sao Paulo Medical Journal 2003;121:102-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Doany 1997 {published data only}
- *.Doany W, McCarty J. Outpatient management of the uncomplicated postdate pregnancy with intravaginal prostaglandin E2 gel and membrane stripping. Journal of Maternal-Fetal Medicine 1997;6:71-8. [DOI] [PubMed] [Google Scholar]
- Doany W. Outpatient management of postdate pregnancy with intravaginal prostaglandin E2 and membrane stripping. American Journal of Obstetrics and Gynecology 1997;174(1 Pt 2):351. [DOI] [PubMed] [Google Scholar]
Dunn 1989 {published data only}
- Dunn PA, Rogers D, Halford K. Transcutaneous electrical nerve stimulation at acupuncture points in the induction of uterine contractions. Obstetrics & Gynecology 1989;73:286-90. [PubMed] [Google Scholar]
Elliott 1984 {published data only}
- Elliott JP, Flaherty JF. The use of breast stimulation to prevent postdate pregnancy. American Journal of Obstetrics and Gynecology 1984;149:628-32. [DOI] [PubMed] [Google Scholar]
El‐Torkey 1992 {published data only}
- El-Torkey M, Grant JM. Sweeping of the membranes is an effective method of induction of labour in prolonged pregnancy: a report of a randomized trial. British Journal of Obstetrics and Gynaecology 1992;99:455-8. [DOI] [PubMed] [Google Scholar]
Evans 1983 {published data only}
- Evans MI, Dougan MB, Moawad AH, Evans WJ, Bryant-Greenwood GD, Greenwood FC. Ripening of the human cervix with porcine ovarian relaxin. American Journal of Obstetrics and Gynecology 1983;147:410-4. [DOI] [PubMed] [Google Scholar]
Frass 2011 {published data only}
- Frass KA, Shuaib AA, Al-Harazi AH. Misoprostol for induction of labor in women with severe preeclampsia at or near term. Saudi Medical Journal 2011;32(7):679-84. [PubMed] [Google Scholar]
Garry 2000 {published data only}
- Garry D, Figueroa R, Guillaume J, Cucco V. Use of castor oil in pregnancies at term. Alternative Therapies 2000;6(1):77-9. [PubMed] [Google Scholar]
Giacalone 1998 {published data only}
- Giacalone PL, Targosz V, Laffargue F, Boog G, Faure JM. Cervical ripening with mifepristone before labor induction. Obstetrics & Gynecology 1998;92(4 Pt 1):487-92. [DOI] [PubMed] [Google Scholar]
Gregson 2015 {published data only}
- Gregson S, Tiran D, Absalom J, Older L, Bassett P. Acupressure for inducing labour for nulliparous women with post-dates pregnancy. Complementary Therapies in Clinical Practice 2015;21(4):257-61. [DOI] [PubMed] [Google Scholar]
Hage 1993 {published data only}
- Hage P, Shawi J, Zarou D, Fleisher J. Double blind randomized trial to evaluate the role of outpatient use of PGE2 in cervical ripening. American Journal of Obstetrics and Gynecology 1993;168:430. [Google Scholar]
Heden 1991 {published data only}
- Heden L, Ingemarsson I, Ahlstrom H, Solum T. Induction of labor versus conservative management in prolonged pregnancy: controlled study. International Journal of Feto-Maternal Medicine 1991;4(4):148-52. [Google Scholar]
Hernandez‐Castro 2008 {published data only}
- Hernandez-Castro F, Alvarez-Chavez LD, Martinez-Gaytan V, Cortes-Flores R. Ambulatory treatment of prolonged pregnancy with prostaglandin E2 gel [Embarazo de 41 semanas o mayor. Manejo ambulatorio con gel de prostaglandina E2]. Revista Medica del Instituto Mexicano del Seguro Social 2008;46(2):191-4. [PubMed] [Google Scholar]
Imsuwan 1999 {published data only}
- Imsuwan Y, Tanapat Y. Reduction of pregnancy with gestational age more than 41 weeks by membrane stripping to induce labor: a randomized controlled clinical trial. Thai Journal of Obstetrics and Gynaecology 1999;11(4):267. [Google Scholar]
Ingemarsson 1987 {published data only}
- Ingemarsson I, Heden L, Montan S, Sjoberg NO. Personal communication 1987.
Iqbal 2004 {published data only}
- Iqbal S. Management of prolonged pregnancy. Journal of the College of Physicians & Surgeons, Pakistan 2004;14(5):274-7. [PubMed] [Google Scholar]
Jenssen 1977 {published data only}
- Jenssen H, Wright PB. The effect of dexamethasone therapy in prolonged pregnancy. Acta Obstetricia et Gynecologica Scandinavica 1977;56:467-73. [DOI] [PubMed] [Google Scholar]
Kadar 1990 {published data only}
- Kadar N, Tapp A, Wong A. The influence of nipple stimulation at term on the duration of pregnancy. Journal of Perinatology 1990;10(2):164-6. [PubMed] [Google Scholar]
Katz 1983 {published data only}
- Katz Z, Yemini M, Lancet M, Mogilner BM, Ben-Hur H, Caspi B. Non-aggressive management of post-date pregnancies. European Journal of Obstetrics & Gynecology and Reproductive Biology 1983;15:71-9. [DOI] [PubMed] [Google Scholar]
Kipikasa 2005 {published data only}
- Kipikasa JH, Adair CD, Williamson J, Breen JM, Medford LK, Sanchez-Ramos L. Use of misoprostol on an outpatient basis for postdate pregnancy. International Journal of Gynecology & Obstetrics 2005;88:108-11. [DOI] [PubMed] [Google Scholar]
Klopper 1969 {published data only}
- Klopper AI, Dennis KJ, Farr V. Effect of intra-amniotic oestriol sulphate on uterine contractions. BMJ 1969;786(2):786-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Knox 1979 {published data only}
- Knox GE, Huddleston JF, Flowers CE. Management of prolonged pregnancy: results of a prospective randomized trial. American Journal of Obstetrics and Gynecology 1979;134:376-84. [DOI] [PubMed] [Google Scholar]
Lee 1997 {published data only}
- Lee HY. A randomised double-blind study of vaginal misoprostol vs dinoprostone for cervical ripening and labour induction in prolonged pregnancy. Singapore Medical Journal 1997;38(7):292-4. [PubMed] [Google Scholar]
Lemancewicz 1999 {published data only}
- Lemancewicz A, Urban R, Skotnicki MZ, Karpiuk A, Urban J. Uterine and fetal Doppler flow changes after misoprostol and oxytocin therapy for induction of labor in post-term pregnancies. International Journal of Gynecology & Obstetrics 1999;67:139-45. [DOI] [PubMed] [Google Scholar]
Lien 1998 {published data only}
- Lien JM, Morgan MA, Garite TJ, Kennedy KA, Sassoon DA, Freeman RK. Antepartum cervical ripening: applying prostaglandin E2 gel in conjunction with scheduled nonstress tests in postdate pregnancies. American Journal of Obstetrics and Gynecology 1998;179:453-8. [DOI] [PubMed] [Google Scholar]
Lyons 2001 {published data only}
- Lyons C, Rumney P, Huang W, Morrison E, Thomas S, Nageotte M, et al. Outpatient cervical ripening with oral misoprostol post-term: induction rates decreased. American Journal of Obstetrics and Gynecology 2001;184(1):S116. [Google Scholar]
Magann 1998 {published data only}
- Magann EF, Chauhan SP, Nevils BG, McNamara MF, Kinsella MJ, Morrison JC. Management of pregnancies beyond forty-one weeks' gestation with an unfavorable cervix. American Journal of Obstetrics and Gynecology 1998;178:1279-87. [DOI] [PubMed] [Google Scholar]
Magann 1999 {published data only}
- Magann EF, Chauhan SP, McNamara MF, Bass JD, Estes CM, Morrison JC. Membrane sweeping versus dinoprostone vaginal insert in the management of pregnancies beyond 41 weeks with an unfavorable cervix. Journal of Perinatology 1999;19(2):88-91. [DOI] [PubMed] [Google Scholar]
Mancuso 1998 {published data only}
- Mancuso S, Ferrazzani S, De Carolis S, Carducci B, De Santis L, Caruso A. Term and postterm low-risk pregnancies: management schemes for the reduction of high rates of cesarean section. Minerva Ginecologica 1998;48:95-8. [PubMed] [Google Scholar]
Meydanli 2003 {published data only}
- Meydanli MM, Caliskan E, Burak F, Narin MA, Atmaca R. Labor induction post-term with 25 micrograms vs. 50 micrograms of intravaginal misoprostol. International Journal of Gynecology & Obstetrics 2003;81:249-55. [DOI] [PubMed] [Google Scholar]
Misra 1994 {published data only}
- Misra M, Vavre S. Labour induction with intracervical prostaglandin E2 gel and intravenous oxytocin in women with a very unfavourable cervix. Australia and New Zealand Journal of Obstetrics and Gynaecology 1994;34(5):511-5. [Google Scholar]
Müller 1995 {published data only}
- Müller T, Rempen A. Comparison of 0,5 mg PG-E2-Intracervical-gel versus 3 mg PG-E2-vaginal tablet for the induction of labour [Geburtseinleitung mit prostaglandinen: 0,5 mg PG-E2-intrazervikalgel versus 3 mg PG-E2-vaginaltablette]. Zeitschrift fur Geburtshilfe und Neonatologie 1995;199:30-4. [PubMed] [Google Scholar]
Neri 2014 {published data only}
- Neri I, Monari F, Salvioli C, Facchinetti F. Acupuncture in post-date pregnancy: a pilot study. Journal of Maternal-Fetal & Neonatal Medicine 2014;27(9):874-8. [DOI] [PubMed] [Google Scholar]
Newman 1997 {published data only}
- Newman M, Newman R. Multiple-dose PGE2 cervical ripening on an outpatient basis: safety and efficacy. American Journal of Obstetrics and Gynecology 1997;176:S112. [Google Scholar]
Nicholson 2008 {published data only}
- NCT00598260. Active management of risk in pregnancy at term to reduce rate of cesarean deliveries (AMOR IPAT). https://clinicaltrials.gov/ct2/show/NCT00598260?cond=active+management+of+risk+in+pregnancy&draw=2&rank=1 (first received 21 January 2008).
- Nicholson J, Caughey A, Parry S, Rosen S, Evans A, Macones G. Prospective randomized trial of the active management of risk in pregnancy at term: improved birth outcomes from prostaglandin-assisted preventive labor induction. American Journal of Obstetrics and Gynecology 2007;197(6 Suppl 1):S37, Abstract no: 84. [Google Scholar]
- *.Nicholson JM, Parry S, Caughey AB, Rosen S, Keen A, Macones GA. The impact of the active management of risk in pregnancy at term on birth outcomes: a randomized clinical trial. American Journal of Obstetrics & Gynecology 2008;198(5):511.e1-511.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ohel 1996 {published data only}
- Ohel G, Rahav D, Rothbart H, Ruach M. Randomised trial of outpatient induction of labor with vaginal PGE2 at 40-41 weeks of gestation versus expectant management. Archives of Gynecology and Obstetrics 1996;258:109-12. [DOI] [PubMed] [Google Scholar]
PACTR201805002872322 {published data only}
- PACTR201805002872322. Repeat induction versus expectant management after failed primary labor induction at term: a randomised clinical trial at Kenyatta National Hospital. pactr.samrc.ac.za/TrialDisplay.aspx?TrialID=2872 (first received 15 December 2017).
Papageorgiou 1992 {published data only}
- Papageorgiou I, Tsionou C, Minaretzis D, Michalas S, Aravantinos D. Labor characteristics of uncomplicated prolonged pregnancies after induction with intracervical prostaglandin E2 gel versus intravenous oxytocin. Gynecologic and Obstetric Investigation 1992;34:92-6. [DOI] [PubMed] [Google Scholar]
Paul 1988 {published data only}
- Paul R, Romero R. Clinical trial of induction versus expectant management in postterm pregnancy. Personal communication 1988.
Rayburn 1988 {published data only}
- Rayburn W, Gosen R, Ramadei C, Woods R, Scott J. Outpatient cervical ripening with prostaglandin E2 gel in uncomplicated postdate pregnancies. American Journal of Obstetrics and Gynecology 1988;158:1417-23. [DOI] [PubMed] [Google Scholar]
Rayburn 1999 {published data only}
- Rayburn WF, Gittens LN, Lucas MJ, Gall SA, Martin ME. Weekly administration of prostaglandin E2 gel compared with expectant management in women with previous cesareans. Obstetrics & Gynecology 1999;94:250-4. [DOI] [PubMed] [Google Scholar]
Rijnders 2011 {published data only}ISRCTN47736435
- ISRCTN47736435. Costs and effects of amniotomy at home for induction of post term pregnancy. isrctn.com/ISRCTN47736435 (first received: 9 January 2006).
- *.Rijnders MEB. A randomised controlled trial of amniotomy at home for induction between 292 and 294 days gestation. In: Interventions in Midwife Led Care in the Netherlands to Achieve Optimal Birth Outcomes: Effects and Women's Experiences. Amsterdam: University of Amsterdam, 2011. [ISRCTN47736435] [Google Scholar]
- Rijnders MEB. Costs and effects of amniotomy at home for induction of post term pregnancy. trialregister.nl/trialreg/admin/rctview.asp?TC=504 (first received 13 December 2005).
Roberts 1986 {published data only}
- Roberts WE, North DH, Speed JE, Martin JN, Palmer SM, Morrison JC. Comparative study of prostaglandin, laminaria, and minidose oxytocin for ripening of the unfavorable cervix prior to induction of labor. Journal of Perinatology 1986;6:16-9. [Google Scholar]
Satin 1991 {published data only}
- *.Satin AJ, Hankins GDV, Yeomans ER. A prospective study of two dosing regimens of oxytocin for the induction of labor in patients with unfavorable cervices. American Journal of Obstetrics and Gynecology 1991;165:980-4. [DOI] [PubMed] [Google Scholar]
- Satin AJ, Hankins GDV, Yeomans ER. A randomized study of two dosing regimens of oxytocin for the induction of patients with an unfavorable cervix. American Journal of Obstetrics and Gynecology 1991;164:307. [DOI] [PubMed] [Google Scholar]
Sawai 1991 {published data only}
- Sawai SK, Williams MC, O'Brien WF, Angel JL, Mastrogiannis DS, Johnson L. Sequential outpatient application of intravaginal prostaglandin E2 gel in the management of postdates pregnancies. Obstetrics & Gynecology 1991;78:19-23. [PubMed] [Google Scholar]
Sawai 1994 {published data only}
- *.Sawai SK, O'Brien WF, Mastrogiannis DS, Krammer J, Mastry MG, Porter GW. Patient-administered outpatient intravaginal prostaglandin E2 suppositories in post-date pregnancies: a double-blind, randomized, placebo-controlled study. Obstetrics & Gynecology 1994;84(5):807-10. [PubMed] [Google Scholar]
- Sawai SK, O'Brien WF, Mastrogiannis MS, Mastry MG, Porter GW, Johnson L. Outpatient prostaglandin E2 suppositories in postdates pregnancies. American Journal of Obstetrics and Gynecology 1992;166(1 Pt 2):400. [Google Scholar]
Stenlund 1999 {published data only}
- Stenlund PM, Bygdeman M, Ekman G. Induction of labor with mifepristone (RU 486). A randomized double-blind study in post-term pregnant women with unripe cervices. Acta Obstetricia et Gynecologica Scandinavica Supplement 1994;73(161):FP50. [PubMed] [Google Scholar]
- *.Stenlund PM, Ekman G, Aedo AR, Bygdeman M. Induction of labor with mifepristone: a randomized, double-blind study versus placebo. Acta Obstetrica et Gynecologica Scandinavica 1999;78:793-8. [PubMed] [Google Scholar]
Su 1996 {published data only}
- Su H, Li E, Weng L. Clinical observation on mifepristone for induction of term labor. Chinese Journal of Obstetrics & Gynecology 1996;31:676-80. [PubMed] [Google Scholar]
Surbek 1997 {published data only}
- Surbek DV, Boesiger H, Hoesli L, Pavu N, Holzgreve W. Cervical priming and labor induction with intravaginal misoprostol versus PGE2: a double-blind randomized trial. American Journal of Obstetrics and Gynecology 1997;176(1 Pt 2):S112. [DOI] [PubMed] [Google Scholar]
Suzuki 1999 {published data only}
- Suzuki S, Otsubo Y, Sawa R, Yoneyama Y, Araki T. Clinical trial of induction of labor versus expectant management in twin pregnancy. Gynecologic and Obstetric Investigation 1999;49:24-7. [DOI] [PubMed] [Google Scholar]
Williams 1990 {published data only}
- Williams MG, O'Brien WF, Sawai SK, Knuppel RA. Outpatient cervical ripening in the postdates pregnancy. In: 10th Annual Meeting of Society of Perinatal Obstetricians; 1990 January 23-27; Houston, Texas, USA. 1990:533.
Wing 2000 {published data only}
- Wing DA, Fassett MJ, Mishell DR. Mifepristone for preinduction cervical ripening beyond 41 weeks' gestation: a randomized controlled trial. Obstetrics & Gynecology 2000;96(4):543-8. [DOI] [PubMed] [Google Scholar]
Wong 2002 {published data only}
- Wong SF, Hui SK, Choi H, Ho LC. Does sweeping of membranes beyond 40 weeks reduce the need for formal induction of labour? BJOG 2002;109:632-6. [DOI] [PubMed] [Google Scholar]
Ziaei 2003 {published data only}
- Ziaei S, Rosebehani N, Kazeminejad A, Zafarghandi S. The effects of intramuscular administration of corticosteroids on the induction of parturition. Journal of Perinatal Medicine 2003;31:134-9. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Benito Reyes 2010 {published data only}
- Benito Reyes V, Hurtado Mendoza R, Rodriguez Rodriguez F, Reyes Suarez D, Alvarez Leon EE, Garcia Hernandez JA. Elective termination versus expectant management in prolonged pregnancy: a prospective study of 200 pregnant women [Finalizacion electiva versus manejo expectante en el control de la gestacion prolongada: estudio prospectivo de 200 gestantes]. Progresos de Obstetricia y Ginecologia 2010;53(11):446-53. [Google Scholar]
ISRCTN74323479 {published data only}ISRCTN74323479
- ISRCTN74323479. What shall we do with the postdates woman who is not in labour? isrctn.com/ISRCTN74323479 (first received 12 September 2003).
References to ongoing studies
ISRCTN15646866 {published data only}ISRCTN15646866
- ISRCTN15646866. Induction of labour at 39 weeks or beyond in multiparous women with a favourable cervix. isrctn.com/ISRCTN15646866 (first received 27 January 2017).
ISRCTN83219789 {published data only}ISRCTN83219789
- ISRCTN83219789. The Finnish randomised controlled multicentre trial on optimal timing of labor induction in nulliparous women with post-term pregnancy. www.isrctn.com/ISRCTN83219789 (first received 20 July 2017).
Additional references
ACOG 2014
- ACOG. Management of late-term and postterm pregnancies practice bulletin 146. Obstetrics and Gynecology 2014;124(2 Pt 1):390-6. [DOI] [PubMed] [Google Scholar]
AIHW 2019
- Australian Institute of Health and Welfare. Australia’s Mothers and Babies 2017 —in brief. Perinatal statistics series no. 35. Cat. no. PER 100. Canberra: AIHW, 2019. [Google Scholar]
Akuamoah‐Boateng 2018
- Akuamoah-Boateng J, Spencer R. Woman-centered care: Women's experiences and perceptions of induction of labor for uncomplicated post-term pregnancy: a systematic review of qualitative evidence. Midwifery 2018;67:46-56. [DOI] [PubMed] [Google Scholar]
Alavifard 2019
- Alavifard S, Meier K, Shulman Y, Tomlinson G, D'Souza R. Derivation and validation of a model predicting the likelihood of vaginal birth following labour induction. BMC Pregnancy and Childbirth 2019;19(1):130. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arrowsmith 2011
- Arrowsmith S, Wray S, Quenby S. Maternal obesity and labour complications following induction of labour in prolonged pregnancy. BJOG 2011;118(5):578-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bentley 2016
- Bentley JP, Roberts CL, Bowen JR, Martin AJ, Morris JM, Nassar N. Planned birth before 39 weeks and child development: a population-based study. Pediatrics 2016;138(6):pii: e20162002. [DOI] [PubMed] [Google Scholar]
Bergholt 2020
- Bergholt T, Skjeldestad FE, Pyykönen A, Rasmussen SC, Tapper AM, Bjarnadóttir RI. Maternal age and risk of cesarean section in women with induced labor at term - a Nordic register-based study. Acta Obstetricia et Gynecologica Scandinavica 2020;99(2):283-9. [DOI] [PubMed] [Google Scholar]
Caughey 2004
- Caughey AB, Musci TJ. Complications of term pregnancy beyond 37 weeks of gestation. Obstetrics and Gynecology 2004;103(1):57-62. [DOI: 10.1097/01AOG.0000109216.24211] [DOI] [PubMed] [Google Scholar]
Caughey 2009
- Caughey AB, Sundaram V, Kaimal AJ, Gienger A, Cheng YW, McDonald KM, et al. Systematic review: elective induction of labor versus expectant management of pregnancy. Annals of Internal Medicine 2009;151:252-63. [DOI] [PubMed] [Google Scholar]
Chen 2019
- Chen HY, Grobman WA, Blackwell SC, Chauhan SP. Neonatal and maternal adverse outcomes among low-risk parous women at 39-41 weeks of gestation. Obstetrics and Gynecology 2019;134(2):288-94. [DOI] [PubMed] [Google Scholar]
Coates 2020
- Coates D, Makris A, Catling C, Henry A, Scarf V, Watts N, et al. A systematic scoping review of clinical indications for induction of labour. PLOS One 2020;15(1):e0228196. [DOI] [PMC free article] [PubMed] [Google Scholar]
Danilack 2016
- Danilack VA, Triche EW, Dore DD, Muri JH, Phipps MG, Savitz DA. Comparing expectant management and spontaneous labor approaches in studying the effect of labor induction on cesarean delivery. Annals Epidemiology 2016;26(6):405-11. [DOI] [PubMed] [Google Scholar]
Davey 2016
- Davey MA, King J. Caesarean section following induction of labour in uncomplicated first births - a population-based cross-sectional analysis of 42,950 births. BMC Pregnancy and Childbirth 2016;16:92. [DOI: 10.1186/s12884-016-0869-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
De Vries 2019
- De Vries BS, McGeechan K, Barratt A, Tooher J, Wong E, Phipps H. The association between induction of labour at 38 to 39 weeks pregnancy and indication for caesarean delivery: an observational study. Australian & New Zealand Journal of Obstetrics & Gynaecology 2019;59(6):791-8. [DOI] [PubMed] [Google Scholar]
Elden 2016
- Elden H, Hagberg H, Wessberg A, Sengpiel V, Herbst A, Bullarbo M, et al. Study protocol of SWEPIS a Swedish multicentre register based randomised controlled trial to compare induction of labour at 41 completed gestational weeks versus expectant management and induction at 42 completed gestational weeks. BMC Pregnancy and Childbirth 2016;16:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grobman 2020
- Grobman WA, Grecio Sandoval MA, Reddy UM, Tital ATN, Silver RM, Mallett G, et al. Health resource utilization of labor induction versus expectant management. American Journal of Obstetrics and Gynecology 2020;222(4):369.e1-369.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Heslehurst 2017
- Heslehurst N, Vieira R, Hayes L, Crowe L, Jones D, Robalino S, et al. Maternal body mass index and post-term birth: a systematic review and meta-analysis. Obesity Reviews 2017;18(3):293-308. [DOI: 10.111/obr.12489] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Keirse 2010
- Keirse MJNC. Elective induction, selective deduction,and cesarean section. Birth 2010;37(3):252-6. [DOI] [PubMed] [Google Scholar]
Keulen 2018
- Keulen JKJ, Bruinsma A, Kortekaas JC, Van Dillen J, Van der Post JAM, De Miranda E. Timing induction of labour at 41 or 42 weeks? A closer look at time frames of comparison: a review. Midwifery 2018;66:111-8. [DOI] [PubMed] [Google Scholar]
Kortekaas 2014
- Kortekaas JC, Bruinsma A, Keulen JKJ, Van Dillen J, Oudijk MA, Zwart JJ, et al. Effects of induction of labour versus expectant management in women with impending post-term pregnancies: the 41 week - 42 week dilemma. BMC Pregnancy and Childbirth 2014;14(1):350. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mandruzzato 2010
- Mandruzzato G, Alfirevic Z, Chervenak F, Gruenebaum A, Heimstad R, Heinonen S, et al. Guidelines for the management of postterm pregnancy. Journal of Perinatal Medicine 2010;38:111-9. [DOI] [PubMed] [Google Scholar]
Marconi 2019
- Marconi AM. Recent advances in the induction of labor. F1000 Research 2019;8:1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martin 2018
- Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2017. National Vital Statistics Report 2018;67(1):1-55. [PubMed] [Google Scholar]
Middleton 2017
- Middleton P, Shepherd E, Flenady V, McBain RD, Crowther CA. Planned early birth versus expectant management (waiting) for prelabour rupture of membranes at term (37 weeks or more). Cochrane Database of Systematic Reviews 2017, Issue 1. Art. No: CD005302. [DOI: 10.1002/14651858.CD005302.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mishanina 2014
- Mishanina E, Rogozinska E, Thatthi T, Uddin-Khan R, Khan K, Meads C. Use of labour induction and risk of cesarean delivery: a systematic review and meta-analysis. Canadian Medical Association Journal 2014;186(9):665-73. [DOI: 10.1503/cmaj.130925] [DOI] [PMC free article] [PubMed] [Google Scholar]
Muglu 2019
- Muglu J, Rather H, Arroyo-Manzano D, Bhattacharya S, Balchin I, Khalil A, et al. Risks of stillbirth and neonatal death with advancing gestation at term: a systematic review and meta-analysis of cohort studies of 15 million pregnancies. PLOS Medicine 2019;16(7):e1002838. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT01990612
- NCT01990612. A randomized trial of induction versus expectant management (ARRIVE). clinicaltrials.gov/ct2/show/record/NCT01990612 (first received 21 November 2013). [NCT01990612]
New Zealand Guideline Development Panel 2019
- New Zealand Guideline Development Panel. Induction of Labour in New Zealand: a Clinical Practice Guideline [draft]. Auckland: NZCOM, RANZCOG, RACP, 2019. [Google Scholar]
NICE 2008
- National Institute for Health and Clinical Excellence. Induction of labour clinical guideline. guidance.nice.org.uk/CG70/Guidance/pdf/English (accessed 27 June 2017).
Olesen 2003
- Olesen AW, Westergaard JG, Olsen J. Perinatal and maternal complications related to postterm delivery: a national register-based study, 1978-1993. American Journal of Obstetrics and Gynecology 2003;189:222-7. [DOI] [PubMed] [Google Scholar]
Olesen 2015
- Olesen AW, Olsen J, Zhu JL. Developmental milestones in children born post-term in the Danish National Birth Cohort: a main research article. BJOG 2015;122(10):1331-9. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, the Cochrane Collaboration, 2014.
Roos 2010
- Roos N, Sahlin L, Ekman-Ordeberg G, Kilere H, Stephansson O. Maternal risk factors for postterm pregnancy and cesarean delivery following labour induction. Acta Obstetricia et Gynecologica Scandinavica 2010;89:1003-10. [DOI] [PubMed] [Google Scholar]
Saccone 2019
- Saccone G, Della Corte L, Maruotti GM, Quist-Nelson J, Raffone A, De Vivo V. Induction of labor at full-term in pregnant women with uncomplicated singleton pregnancy: a systematic review and meta-analysis of randomized trials. Acta Obstetricia et Gynecologica Scandinavica 2019;98(8):958-66. [DOI] [PubMed] [Google Scholar]
Schierding 2014
- Schierding W, O'Sullivan JM, Derraik JGB, Cutfield WS. Genes and post-term birth: late for delivery. BMC Research Notes 2014;7:720. [DOI: 10.1186/1756-0500-7-720] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sinkey 2018
- Sinkey RG, Lacevic J, Reljic T, Hozo I, Gibson KS, Odibo AO. Elective induction of labor at 39 weeks among nulliparous women: the impact on maternal and neonatal risk. PLOS One 2018;13(4):e0193169. [DOI] [PMC free article] [PubMed] [Google Scholar]
SOGC 2017
- Delaney M, Roggensack A, Society of Obstetricians and Gynaecologists of Canada (SOGC). No. 214 - Guidelines for the management of pregnancy at 41 + 0 to 42 + 0 weeks. Journal of Obstetrics and Gynaecology Canada 2017;39(8):e164-e174. [DOI] [PubMed] [Google Scholar]
Sotiriadis 2019
- Sotiriadis A, Petousis S, Thilaganathan B, Figueras F, Martins WP, Odibo AO. Maternal and perinatal outcomes after elective induction of labor at 39 weeks in uncomplicated singleton pregnancy: a meta-analysis. Ultrasound in Obstetrics & Gynecology 2019;53(1):26-35. [DOI] [PubMed] [Google Scholar]
Souter 2019
- Souter V, Painter I, Sitcov K, Caughey AB. Maternal and newborn outcomes with elective induction of labor at term. American Journal of Obstetrics and Gynecology 2019;220(3):273.e1-11. [DOI] [PubMed] [Google Scholar]
University of Sydney 2020
- University of Sydney, Sydney Health Partners, Australian Preterm Birth Prevention Alliance. Every week counts. www.everyweekcounts.com.au/ (accessed 26 March 2020).
Walker 2017
- Walker KF, Dritsaki M, Bugg G, Macpherson M, McCormick C, Grace N, et al. Labour induction near term for women aged 35 or over: an economic evaluation. BJOG 2017;124(6):929-34. [DOI] [PubMed] [Google Scholar]
Wessberg 2017
- Wessberg A, Lundgren I, Elden H. Being in limbo: women's lived experiences of pregnancy at 41 weeks of gestation and beyond - a phenomenological study. BMC Pregnancy and Childbirth 2017;17(1):162. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whitworth 2015
- Whitworth M, Bricker L, Mullan C. Ultrasound for fetal assessment in early pregnancy. Cochrane Database of Systematic Reviews 2015, Issue 7. Art. No: CD007058. [DOI: 10.1002/14651858.CD007058.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2018
- WHO. WHO Recommendations: Induction of Labour at or beyond Term. Geneva: World Health Organization, 2018. [PubMed] [Google Scholar]
Wolff 2016
- Wolff SL, Lorentzen I, Kaltoft AP, Schmidt H, Jeppesen MM, Maimburg RD. Has perinatal outcome improved after introduction of a guideline in favour of routine induction and increased surveillance prior to 42 weeks of gestation?: A cross-sectional population-based registry study. Sexual and Reproductive Healthcare 2016;10:19-24. [DOI: 10.1016/j.srhc.2016.03.002] [DOI] [PubMed] [Google Scholar]
Wood 2014
- Wood S, Cooper S, Ross S. Does induction of labour increase the risk of caesarean section? A systematic review and meta-analysis of trials in women with intact membranes. BJOG 2014;121(6):674-85. [DOI: 10.1111/1471-0528] [DOI] [PubMed] [Google Scholar]
Zeitlin 2007
- Zeitlin J, Blondel B, Alexander S, Bréart G, PERISTAT Group. Variation in rates of postterm birth in Europe: reality or artefact? BJOG 2007;114:1097-103. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Gülmezoglu 2004
- Gülmezoglu AM, Crowther CA. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database of Systematic Reviews 2004, Issue 4. Art. No: CD004945. [DOI: 10.1002/14651858.CD004945] [DOI] [PubMed] [Google Scholar]
Gülmezoglu 2006
- Gülmezoglu AM, Crowther CA, Middleton P. Interventions for preventing or improving the outcome of delivery at or beyond term. Cochrane Database of Systematic Reviews 2006, Issue 4. Art. No: CD004945. [DOI: 10.1002/14651858.CD004945.pub2] [DOI] [Google Scholar]
Gülmezoglu 2012
- Gülmezoglu AM, Crowther CA, Middleton P, Heatley E. Induction of labour for improving birth outcomes for women at or beyond term. Cochrane Database of Systematic Reviews 2012, Issue 6. Art. No: CD004945. [DOI: 10.1002/14651858.CD004945.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Middleton 2018
- Middleton P, Shepherd E, Morris J, Crowther CA, Gomersall JC. Induction of labour at or beyond 37 weeks gestation. Cochrane Database of Systematic Reviews 2018, Issue 5. Art. No: CD004945. [DOI: 10.1002/14651858.CD004945.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]


