Abstract
Background
Primary angle closure glaucoma (PACG) accounts for 50% of glaucoma blindness worldwide. More than three‐quarters of individuals with PACG reside in Asia. In these populations, PACG often develops insidiously leading to chronically raised intraocular pressure and optic nerve damage, which is often asymptomatic. Non‐contact tests to identify people at risk of angle closure are relatively quick and can be carried out by appropriately trained healthcare professionals or technicians as a triage test. If the test is positive, the person will be referred for further specialist assessment.
Objectives
To determine the diagnostic accuracy of non‐contact tests (limbal anterior chamber depth (LACD) (van Herick test); oblique flashlight test; scanning peripheral anterior chamber depth analyser (SPAC), Scheimpflug photography; anterior segment optical coherence tomography (AS‐OCT), for identifying people with an occludable angle.
Search methods
We searched the following bibliographic databases 3 October 2019: CENTRAL; MEDLINE; Embase; BIOSIS; OpenGrey; ARIF and clinical trials registries. The searches were limited to remove case reports. There were no date or language restrictions in the searches.
Selection criteria
We included prospective and retrospective cross‐sectional, cohort and case‐control studies conducted in any setting that evaluated the accuracy of one or more index tests for identifying people with an occludable angle compared to a gonioscopic reference standard.
Data collection and analysis
Two review authors independently performed data extraction and quality assessment using QUADAS2 for each study. For each test, 2 x 2 tables were constructed and sensitivity and specificity were calculated. When four or more studies provided data at fixed thresholds for each test, we fitted a bivariate model using the METANDI function in STATA to calculate pooled point estimates for sensitivity and specificity. For comparisons between index tests and subgroups, we performed a likelihood ratio test comparing the model with and without the covariate.
Main results
We included 47 studies involving 26,151 participants and analysing data from 23,440. Most studies were conducted in Asia (36, 76.6%). Twenty‐seven studies assessed AS‐OCT (analysing 15,580 participants), 17 studies LACD (7385 participants), nine studies Scheimpflug photography (1616 participants), six studies SPAC (5239 participants) and five studies evaluated the oblique flashlight test (998 participants). Regarding study quality, 36 of the included studies (76.6%) were judged to have a high risk of bias in at least one domain.The use of a case‐control design (13 studies) or inappropriate exclusions (6 studies) raised patient selection concerns in 40.4% of studies and concerns in the index test domain in 59.6% of studies were due to lack of masking or post‐hoc determination of optimal thresholds. Among studies that did not use a case‐control design, 16 studies (20,599 participants) were conducted in a primary care/community setting and 18 studies (2590 participants) in secondary care settings, of which 15 investigated LACD.
Summary estimates were calculated for commonly reported parameters and thresholds for each test; LACD ≤ 25% (16 studies, 7540 eyes): sensitivity 0.83 (95% confidence interval (CI) 0.74, 0.90), specificity 0.88 (95% CI 0.84, 0.92) (moderate‐certainty); flashlight (grade1) (5 studies, 1188 eyes): sensitivity 0.51 (95% CI 0.25, 0.76), specificity 0.92 (95% CI 0.70, 0.98) (low‐certainty); SPAC (≤ 5 and/or S or P) (4 studies, 4677 eyes): sensitivity 0.83 (95% CI 0.70, 0.91), specificity 0.78 (95% CI 0.70, 0.83) (moderate‐certainty); Scheimpflug photography (central ACD) (9 studies, 1698 eyes): sensitivity 0.92 (95% CI 0.84, 0.96), specificity 0.86 (95% CI 0.76, 0.93) (moderate‐certainty); AS‐OCT (subjective opinion of occludability) (13 studies, 9242 eyes): sensitivity 0.85 (95% CI 0.76, 0.91); specificity 0.71 (95% CI 0.62, 0.78) (moderate‐certainty).
For comparisons of sensitivity and specificity between index tests we used LACD (≤ 25%) as the reference category. The flashlight test (grade 1 threshold) showed a statistically significant lower sensitivity than LACD (≤ 25%), whereas AS‐OCT (subjective judgement) had a statistically significant lower specificity. There were no statistically significant differences for the other index test comparisons. A subgroup analysis was conducted for LACD (≤ 25%), comparing community (7 studies, 14.4% prevalence) vs secondary care (7 studies, 42% prevalence) settings. We found no evidence of a statistically significant difference in test performance according to setting.
Performing LACD on 1000 people at risk of angle closure with a prevalence of occludable angles of 10%, LACD would miss about 17 cases out of the 100 with occludable angles and incorrectly classify 108 out of 900 without angle closure.
Authors' conclusions
The finding that LACD performed as well as index tests that use sophisticated imaging technologies, confirms the potential for this test for case‐detection of occludable angles in high‐risk populations. However, methodological issues across studies may have led to our estimates of test accuracy being higher than would be expected in standard clinical practice. There is still a need for high‐quality studies to evaluate the performance of non‐invasive tests for angle assessment in both community‐based and secondary care settings.
Plain language summary
How accurate are screening tests in identifying those at risk of developing primary angle closure glaucoma?
Why is improving the diagnosis of primary angle closure glaucoma important? Glaucoma is a group of eye diseases that cause damage to the optic nerve at the back of the eye. If untreated, glaucoma can lead to blindness. Primary angle closure glaucoma is a type of glaucoma, where the drainage route for the fluid inside the eye (known as the angle) is narrowed or blocked, leading to raised eye pressure and loss of the field of vision. Primary angle closure glaucoma accounts for a quarter of all cases of glaucoma globally and it is more likely to lead to vision loss than the more common form, primary open angle glaucoma.
A variety of non‐invasive tests are available to identify people at risk of primary angle closure glaucoma in a community or non‐specialist clinical setting. Those who test positive are referred for further specialist investigation and possible treatment. Failure to detect this condition (a false negative result) may result in an increased risk of progressive optic nerve damage and blindness. An incorrect diagnosis (a false positive result) could lead to unnecessary and costly investigation.
What is the aim of this review? The aim of this review was to find out how accurate non‐invasive screening tests are in identifying those at risk of developing primary angle closure glaucoma.
What was studied in this review? Five non‐invasive tests were studied. These range from simple tests that require either a pen torch or a widely available piece of clinical equipment known as a slit ‐lamp microscope (oblique flashlight test; limbal anterior chamber depth (LACD)) to more sophisticated imaging equipment (anterior segment optical coherence tomography (AS‐OCT), Scheimpflug photography and scanning peripheral anterior chamber depth analyser (SPAC)) that can scan and measure the dimensions of the drainage angle.
What were the main results in this review? The review included 47 relevant studies, with a total of 26,151 participants. Twenty‐seven studies assessed AS‐OCT, 17 studies assessed LACD, nine studies Scheimpflug photography, six studies SPAC and five studies evaluated the flashlight test.
The overall diagnostic performance of LACD was similar to the more advanced imaging technologies, AS‐OCT, Scheimpflug photography and SPAC, however, the flashlight test showed an inferior performance. Using LACD as an example, if this test was performed on 1000 people, of whom 100 were at risk of primary angle closure, an estimated 83 would be correctly identified and 17 cases would be missed (false negatives). The test would correctly identify 792 of the 900 not at risk of angle closure glaucoma and incorrectly classify 108 (12%), who would be unnecessarily referred (false positives).
How reliable were the results of the studies in this review? Most studies were of low quality due to the way that the participants were recruited or how the tests were performed. This could have led to the tests appearing more accurate than what they really are. We can therefore not be sure that the tests will always produce the reported results.
What are the implications of this review? The studies included in this review were mostly conducted in Asia, which carries the greatest burden of primary angle closure glaucoma. The results of this review have shown that LACD, which is a quick and simple test that can be performed with a minimal amount of training, can identify people at risk of primary angle closure glaucoma, leading to early and appropriate treatment. Although this test could potentially miss approximately one in six of those at risk of the condition and lead to an over referral of 12%, the test could be useful for targeted screening in areas with a high prevalence of the condition.
How up to date is this review? Evidence in this review is current to 3 October 2019.
Summary of findings
Summary of findings 1. Should non‐contact tests be used to diagnose an occludable angle in people at risk of primary angle closure glaucoma?
|
Test (measure and/or threshold) |
N. studies (N. with occludable angles/total analysed) | Accuracy estimates | False positives and false negatives at prevalence 10%: 100 participants with and 900 without occludable angles | False positives and false negatives at prevalence 30%: 300 participants with and 700 without occludable angles | Certainty of evidence for sensitivity and specificity | |||
|
Sensitivity (95%CI) |
Specificity (95%CI) |
False positives (95% CI) | False negatives (95% CI) | False positives (95% CI) | False negatives (95% CI) | |||
|
LACD (cut‐off: ≤25%) |
16 studies (1490/7540) |
0.83 (0.74 to 0.90) |
0.88 (0.84 to 0.92) |
108 (72 to 144) |
17 (10 to 26) |
51 (30 to 78) |
84 (56 to 112) |
Moderatea |
| Oblique flashlight test (grade 1) | 5 studies (298/1188) |
0.51 (0.25 to 0.76) |
0.92 (0.70 to 0.98) |
72 (18 to 270) |
49 (24 to 46) |
56 (14 to 210) |
147 (75 to 228) |
Lowb |
|
SPAC (≤5 and/or S or P) |
4 studies (994/4677) |
0.83 (0.70 to 0.91) |
0.78 (0.70 to 0.83) |
207 (162 to 261) |
17 (10 to 26) |
161 (126 to 203) |
51 (30 to 78) |
Moderatec |
|
Scheimpflug photography (ACD central) |
9 studies (461/1698) |
0.92 (0.84 to 0.96) |
0.86 (0.76 to 0.93) |
126 (63 to 216) |
8 (4 to 16) |
98 (49 to 168) |
24 (12 to 48) |
Moderated |
|
AS‐OCT (subjective assessment) |
13 studies (1850/9239) |
0.85 (0.76 to 0.91) |
0.71 (0.62 to 0.78) |
270 (198 to 351) |
14 (8 to 24) |
210 (154 to 273) |
42 (24 to 72) |
Moderatee |
Certainty of evidence applies to both sensitivity and specificity.
Explanations
a Downgraded one level due to risk of bias: 75% of studies had a high risk of bias in one or more domains. Two studies (13%) used a case‐control design. b Downgraded one level due to risk of bias: 40% of studies with high risk of bias in one or more domains. Downgraded one level due to imprecision. There was also significant unexplained heterogeneity in estimates of sensitivity. c Downgraded one level due to risk of bias: 60% of studies had a high risk of bias in one or more domains. d Downgraded one level due to risk of bias: all studies had a high risk of bias in one or more domains. Five studies (56%) used a case‐control design. e Downgraded one level due to applicability concerns (various subjective cut‐point criteria were used, which may limit the applicability of the results).
Legend
ACD: anterior chamber depth AS‐OCT: anterior segment optical coherence tomography CI: confidence interval LACD: limbal anterior chamber depth SPAC: scanning peripheral anterior chamber depth analyser
Background
Clinical problem
Primary angle closure (PAC) is characterised by appositional or adhesional (synechial) narrowing (and eventually occlusion) of the drainage angle in the anterior chamber of the eye, resulting in elevated intraocular pressure (IOP) and subsequent glaucomatous optic neuropathy, a condition known as primary angle closure glaucoma (PACG). The occlusion of the drainage angle may occur rapidly or slowly. Rapid occlusion results in symptomatic IOP elevation that requires emergency medical treatment (known as acute angle closure). Individuals presenting with acute angle closure, characterised by eye pain, headache, corneal oedema and vascular congestion, are treated initially with topical and oral medications to lower the IOP. This is followed by laser peripheral iridotomy (LPI) as soon as possible after angle closure, usually with prophylactic treatment of the fellow eye (Emanuel 2014). An occlusion that develops insidiously results in chronically raised IOP, which is often asymptomatic. Management for chronic angle closure involves: medical therapy (topical hypotensives); LPI; filtration surgery or a combination of these to lower the IOP and open up the drainage angle. Although LPI remains the first‐line intervention for acute and chronic PAC, there is a growing evidence that clear lens extraction is associated with better clinical and patient‐reported outcomes than LPI and may therefore be a better first‐line treatment option (Azuara‐Blanco 2016; Tanner 2020).
The prevalence of PACG varies across ethnic groups; in European‐derived populations PACG has been estimated to be 0.40% of those aged 40 years and older, compared to 1.09% in Asian populations (Tham 2014). For those aged 70 years and older, the prevalence increases to 0.94% (Day 2012) and 2.32% (Cheng 2014), respectively. Although, globally, open‐angle glaucoma is more common (3%) (Tham 2014), PACG is more likely to result in bilateral blindness (Foster 2001; Quigley 1996; Quigley 2006; Resnikoff 2004).
A classification scheme for PAC designed for use in prevalence surveys and epidemiological research was published by Foster and colleagues (Foster 2002). This identifies three stages in the natural history of angle closure from initial irido‐trabecular contact (ITC) to anterior segment signs of disease (raised IOP, peripheral anterior synechiae (PAS), or both), culminating in glaucomatous optic neuropathy.
Primary angle closure suspect (PACS): an eye in which appositional contact between the peripheral iris and posterior trabecular meshwork is considered in two or more quadrants, in dark room conditions using static gonioscopy.
PAC: an eye with an occludable drainage angle and features indicating that trabecular obstruction by the peripheral iris has occurred, such as PAS, elevated IOP (> 21 mmHg), iris whorling (distortion of the radially orientated iris fibres), “glaucomfleken” lens opacities, or excessive pigment deposition on the trabecular surface. There is no evidence of glaucomatous optic neuropathy or associated glaucomatous field loss.
PACG: signs of PAC, as described above, and evidence of glaucomatous optic neuropathy.
There are various anatomical and demographic risk factors for PAC (Amerasinghe 2008; Lowe 1970). Anatomical risk factors include: a shallow anterior chamber depth (ACD), thickening of the crystalline lens, small corneal diameter and a short axial length (Nolan 2006; Wang 2019). The risk of PACG increases with age (Day 2012; Wang 2019), and the prevalence also varies with ethnicity, with higher rates occurring in Inuit and Asian populations (Clemmesen 1971; Drance 1973; Tham 2014).
The natural history of angle closure disease is not well documented due to the sparsity of long‐term observational data (Alsbirk 1992; Thomas 2003; Wilensky 1993; Yip 2008). A recent large randomised controlled trial, conduced in China (Zhongshan Angle‐closure Prophylaxis Study) (He 2019), carried out LPI in one randomly selected eye of participants with bilateral PACS, with the other eye acting as an untreated control. The primary outcome was incident primary angle closure disease as a composite endpoint of elevated IOP, PAS, or an acute angle‐closure episode during the 72‐month follow‐up period. The rate of developing any angle closure endpoint in this population was very low (less than 1% per year). Although eyes that underwent LPI showed a significant reduction in the risk of developing PAC or an acute attack, the authors concluded that prophylactic treatment is of limited benefit and was unlikely to be cost‐effective. However, in view of differences in the causative mechanism of angle closure between Europeans and East Asians (He 2006), the generalisability of these findings is unclear.
Target condition being diagnosed
For this review we used an occludable angle as the target condition indicative of an anatomical predisposition to angle closure as identified by gonioscopy (Weinreb 2006). In this review we defined an occludable angle as either:
an eye which has appositional contact between the peripheral iris and posterior trabecular meshwork in two or more quadrants (≥180°); or
an eye with, or at risk of, angle closure as judged by an experienced eye care professional using gonioscopy with or without indentation.
Conditions that are similar to the target condition include secondary angle closure glaucoma, such as aqueous misdirection, neovascular glaucoma and ciliary body swelling. The clinical features and management of conditions that cause secondary angle closure glaucoma have been reviewed by Parivadhini 2014 and were not investigated in this review.
Index test(s)
Targeted screening for PAC/PACG has established the effectiveness of measuring anterior chamber dimensions to identify occludable angles (Congdon 1996; Devereux 2000; Kurita 2009). A variety of non‐contact tests are available for the assessment of the ACD, anterior chamber angle (ACA), or both.
Oblique flashlight test
The flashlight test is an accessible method to detect a potentially occludable angle if no other equipment is available. The test can be carried out in a primary‐ or secondary‐care setting and involves shining a pen torch into the eye from the temporal limbus parallel to the iris to assess the ACD. Quantitative grading uses a four‐point scale, based on the proportion of the nasal iris that is in shadow (grade 4 = minimal or no shadow; grade 1 = nasal iris in complete shadow (Van Herick 1969; Vargas 1973;) grade 1 is associated with a high risk of angle closure. Alternatively, qualitative grading can be used to describe the amount of shadow falling on the iris as shallow, medium or deep, and is further described by He 2007.
Limbal anterior chamber depth assessment (van Herick technique)
The van Herick technique is used to assess the ACD at the limbus using a slit lamp biomicroscope (Van Herick 1969). The illumination system is set at 60° from the observation system. A focused vertical slit‐beam is positioned at the limbus and moved just onto the cornea until the beam separates into a corneal section and reflection of the beam onto the iris. An estimate of the thickness of the dark space between the beams (which corresponds to the limbal anterior chamber depth (LACD)) is recorded as a fraction (or percentage) of the corneal section thickness over the central portion of the beam. Van Herick 1969 originally described a four‐point grading scheme, which was extended to a seven‐point scale by Foster 2000, in an effort to improve the precision of the measurement. Van Herick 1969 considered that an eye with a LACD of grade 2 or less (≤ 25%) required gonioscopy and that a grade 1 angle was at a high risk of angle closure. Foster 2000 further subdivided grade 1 into 5% and 15% cut‐off values and also included a 0% grade, which was defined as iridocorneal contact for at least one clock hour within the observed quadrant. The augmented scale was associated with improved test accuracy.
Scanning peripheral anterior chamber depth analyser
Scanning peripheral anterior chamber depth analysis (SPAC) is an objective method for measuring the peripheral and central ACD by automatically taking 21 slit lamp images of the anterior chamber using a 1 mm‐wide slit at 0.4‐mm intervals from the optical axis towards the limbus (Kashiwagi 2006). These measurements are compared to a normative database and converted into a numerical scale ranging from 1 to 12, with 12 representing the deepest ACD. In addition, the instrument provides a categorical grading of the risk of angle closure, S (suspect angle closure), P (potential angle closure), or N (normal). The device has been shown to be reproducible and easy to operate (Kashiwagi 2004).
Scheimpflug photography
The Scheimpflug principle is used to correct perspective distortion in aerial photographs and has been adapted for ocular imaging. The Oculus Pentacam (Oculus, Wetzlar, Germany) device employs this principle using monochromatic blue light at a wavelength of 475 nm. By rotating the apparatus around the optical axis of the eye, a series of radially oriented images is generated in three dimensions around the 360° extent of the anterior segment. Between 12 and 50 real‐time sections from the anterior surface of the cornea to the posterior vertex of the lens are acquired within a two‐second acquisition frame. This generates a set of measurements that provide a detailed description of the biometric configuration of the anterior segment, which includes the ACA, ACD and the anterior chamber volume (ACV). When calculating the ACA, it should be noted that this is not a direct measurement of the ACA, but is extrapolated from the measurements taken by the Pentacam. . Currently there is no consensus on which parameter or cut‐off value to use in the determination of an occludable angle.
Anterior segment‐optical coherence tomography
Anterior segment‐optical coherence tomography (AS‐OCT) allows both qualitative and quantitative analysis of the angle. The technique is based on low‐coherence interferometry whereby the delay and intensity of light reflected from the ocular tissue structures is measured. There are currently several AS‐OCT devices available on the market; depending on the device, they use one of the following methods to obtain clinical data: time domain, spectral domain or the more recent swept source domain method. Spectral and swept source domain methods have a higher scan speed and resolution than time domain methods. A wavelength of 1310 nm is used to image the anterior segment and inbuilt software is used to quantitatively assess in detail angle parameters, which include: the trabeculo‐iris space area (TISA, measured at 500 microns and 750 microns), angle recess area (ARA) and angle opening distance (AOD) at 500 microns and 750 microns (Quek 2011). Qualitative interpretation has been typically defined by contact between the peripheral iris and any part of the angle wall anterior to the scleral spur. There is currently no consensus on which threshold values to use for any of the quantitative parameters mentioned to identify an occludable angle (Smith 2013).
Clinical pathway
A variety of non‐contact devices with varying degrees of sophistication have been developed to evaluate the risk of angle closure. The high prevalence of PAC and the burden of blindness attributable to PACG raises the possibility of using such techniques as triage tests in high‐risk populations who may not have access to eye care services (see Figure 1) (Nolan 2003; Nolan 2006). More commonly, non‐invasive assessment of the dimensions of the anterior chamber, including ACD, angle, or both are part of a standard ophthalmic examination in a primary/community or secondary care setting. If the index test is positive, such individuals are identified as being 'at risk' of PACG and are referred for further assessment, usually to a glaucoma sub‐specialist ophthalmologist. The ophthalmologist will carry out gonioscopy (the reference standard for qualitative and quantitative assessment of the ACA). If an occludable angle is diagnosed, additional tests are then performed to further diagnose the condition as PACS/PAC/PACG. Depending on the clinical presentation, the affected individual may be closely monitored or undergo prophylactic treatment with LPI or lens extraction, possibly in conjunction with IOP‐lowering eye drops.
1.

Clinical Pathway
Role of index test(s)
The reference standard test to detect an occludable angle is gonioscopy; however, this is not routinely performed outside the specialist setting since it is invasive and requires a high level of skill, which may lead to missed diagnoses. Non‐contact tests are relatively quick and can be carried out by appropriately trained healthcare professionals or technicians as a triage test to identify people at risk of angle closure. A systematic review published in 2013 concluded that there was insufficient evidence for non‐contact tests to replace gonioscopy, as they do not provide sufficient information on the ACA anatomy (Smith 2013). It should be noted that in some cases, when gonioscopy fails to visualise the anterior chamber configuration and depth, typically in secondary causes of angle closure, AS‐OCT and Scheimpflug photography can be used to provide objective measurements (Kang 2013). In addition, these techniques can be used to supplement existing clinical documentation by providing objective measurements (Smith 2013).
Alternative test(s)
Tests that use contact methods, such as ultrasound biomicroscopy, have been reviewed by Smith 2013, and were not included in the current review.
Rationale
A systematic review published in 2013 evaluated whether anterior segment imaging (using ultrasound biomicroscopy, optical coherence tomography (OCT), Scheimpflug photography or SPAC aided the diagnosis of PAC (Smith 2013). This review included 79 studies and concluded that although anterior segment imaging provided useful information, none of the tests provided sufficient information about the anatomy of ACA to be considered a substitute for gonioscopy. However, no meta‐analysis of accuracy data was conducted. The current review updates and extends this review by considering the following non‐contact tests of anterior chamber assessment (flashlight test, slit‐lamp techniques for LACD assessment, AS‐OCT, Scheimpflug photography and SPAC).
Objectives
To determine the diagnostic accuracy of non‐contact tests for identifying people with an occludable anterior chamber angle of the eye.
Secondary objectives
To investigate the accuracy of each non‐contact test for detecting the most severe referable condition or PACG (versus PACS or PAC)
To explore potential causes of heterogeneity in diagnostic performance
Methods
Criteria for considering studies for this review
Types of studies
We included all prospective and retrospective cohort studies ('single‐gate' design) and case‐control studies ('two‐gate' design) that evaluated the accuracy of non‐contact tests for diagnosing occludable angles compared to a gonioscopic reference standard. We included studies comparing each method separately, and studies comparing more than one method, to the reference standard in the same population. This included studies in which participants received all the tests or were randomised to receive different tests. We included only studies that provided sufficient data to allow the calculation of sensitivity and specificity.
Non‐contact tests for the detection of occludable angles are mainly of interest in primary‐care settings as a triage test aiming to guide referrals to glaucoma specialists. The tests are also used in non‐specialist secondary care settings. Since the relative accuracy of these tests in these settings is not well known, we included studies investigating these tests in any setting, and planned to assess the effect of this on accuracy in subgroup analyses.
Participants
We included all participants who met the inclusion criteria for studies conducted in any setting, which evaluated any of the index tests against the reference standard. We considered data from both untested asymptomatic populations and other pre‐tested predominantly asymptomatic populations recruited in secondary care.
Index tests
We assessed non‐contact tests including: the oblique flashlight test, LACD using the van Herick technique, SPAC, Scheimpflug photography and AS‐OCT.
Target conditions
An occludable angle, as a referable condition that can include PACS, PAC or PACG, as described above, was the target condition of interest.
As a secondary objective, we also planned to extract data to investigate the accuracy of the test for detecting the most severe referable condition or PACG (versus PAC or PACS).
Reference standards
Gonioscopy was the reference standard for the diagnosis of an occludable angle. We included studies using any of the standard gonioscopic classification schemes and used the authors' definition of an occludable angle, based on the number of quadrants of ITC. When the information was available, we further classified an occludable angle into one of three subgroups PACS, PAC, PACG.
Gonioscopy
Gonioscopy is the acknowledged reference standard for the evaluation of eyes with or at risk of angle closure, and should be performed on both eyes in any individual with suspected angle closure. The technique should be performed under dark‐room conditions and used in the primary position to visualise angle structures, the presence of ITC, PAS, or both (Bhargava 1973). Dynamic assessment is helpful in distinguishing ITC from PAS using a four‐mirror lens, which is applied to the cornea creating pressure with the goniolens. The Shaffer grading system, which records the ACA width in four quadrants, from grade 0 (closed) to grade 4 (wide open), is the most widely adopted ACA classification scheme (Shaffer 1960). Angle morphology can be further described using the Scheie grading system (Scheie 1957). This scheme describes the angle according to the anatomical structures observed (grade IV: Schwalbe’s line not visible; grade III: Schwalbe’s line visible; grade II: anterior trabecular meshwork visible; grade I: visible scleral spur; and grade 0: ciliary body band visible). The Spaeth classification is the most detailed of the three grading systems that allows grading of the geometric angle, iris profile and level of iris insertion (Spaeth 1971).
Search methods for identification of studies
Electronic searches
The Cochrane Eyes and Vision Information Specialist searched the following electronic databases. We imposed no restrictions on language or year of publication.The date of the search was 3 October 2019.
Cochrane Central Register of Controlled Trials (CENTRAL) (which contains the Cochrane Eyes and Vision Trials Register) in the Cochrane Library (searched 3 October 2019) (Appendix 1).
Health Technology Assessment Database (HTAD) in the Cochrane Library (searched 3 October 2019) (Appendix 1).
MEDLINE Ovid (January 1946 to 3 October 2019) (Appendix 2).
Embase Ovid (January 1980 to 3 October 2019) (Appendix 3).
BIOSIS (January 1969 to 3 October 2019) (Appendix 4).
System for Information on Grey Literature in Europe (OpenGrey) (1995 to 3 October 2019) (Appendix 5).
Aggressive Research Intelligence Facility database (ARIF) (www.birmingham.ac.uk/research/activity/mds/projects/HaPS/PHEB/ARIF/index.aspx; searched 3 October 2019. ARIF database last updated June 2018) (Appendix 6).
ISRCTN registry (www.isrctn.com/editAdvancedSearch; searched 3 October 2019) (Appendix 7).
US National Institutes of Health Ongoing Trials Register ‐ ClinicalTrials.gov (www.clinicaltrials.gov; searched 3 October 2019) (Appendix 8).
World Health Organization International Clinical Trials Registry Platform (www.who.int/ictrp; searched 3 October 2019) (Appendix 9).
Searching other resources
We searched the references of included studies for information about further studies. We did not handsearch journals and conference proceedings.
Data collection and analysis
Selection of studies
Two review authors (AJ and IC) independently assessed the titles and abstracts of all studies identified by the electronic searches. We labelled each record at this stage as "definitely relevant", "possibly relevant" or "definitely not relevant". We excluded records labelled as "definitely not relevant" by both review authors. We retrieved full‐text reports of records labelled as "definitely relevant" or "possibly relevant" and the two review authors independently assessed whether these met the inclusion criteria. We resolved any disagreement when present at any stage through discussion. When necessary, we consulted a third review author or contacted the study investigators for more information to determine eligibility.
Data extraction and management
Two review authors (AJ and JL) independently extracted the following data, where possible, from the included studies: the number of true positives (TP), false positives (FP), true negatives (TN) and false negatives (FN) using 2 x 2 contingency tables. From the 2 X 2 tables we calculated sensitivity (the proportion of diseased people correctly diagnosed) and specificity (the proportion of non‐diseased people correctly diagnosed) with 95% confidence intervals (CIs).
One review author entered data into Review Manager 5 (RevMan 5) (Review Manager 2014) and a second review author verified the entered data. We resolved any disagreement when present at any stage through discussion. We contacted study investigators to provide missing information or to clarify data, and we allowed two weeks for a response. If we did not receive a response during this time, we proceeded to use the information available in the published reports. We summarised the characteristics of included studies in a 'Characteristics of included studies' table. The characteristics extracted from each study are shown in Appendix 10. See Appendix 11 for abbreviations.
Assessment of methodological quality
Two review authors (AJ and JL) independently assessed each included study for risk of bias using the QUADAS 2 tool to assess the susceptibility to bias of the included studies, based on guidance presented in Appendix 12 (Whiting 2011). We assessed each study and judged each bias criterion to be at 'high', 'low' or 'unclear' risk of bias (lack of information or uncertainty over the potential for bias). Concerns regarding applicability were rated as 'high', 'low' or 'unclear' concerns.
Statistical analysis and data synthesis
We extracted and analysed the data available at fixed thresholds for each index test, in order to ease the interpretability of our summary measures of accuracy. Our preferred thresholds were:
oblique flashlight test: grades 1 and 2;
LACD using the van Herick technique: grades 1 and 2 (≤ 25%);
SPAC: categorical grading of suspect angle closure or potential angle closure, as provided by the device.
As there is no current consensus regarding thresholds for Scheimpflug photography and AS‐OCT, we extracted these data, when available, from the included studies.
We generated estimates of sensitivity and specificity in forest plots for each index test and also plotted them in receiver operating characteristics (ROC) space in RevMan. When four or more studies provided data at fixed thresholds for each test, we fitted a bivariate model using the METANDI function in STATA to calculate pooled point estimates for sensitivity and specificity. For comparisons between index tests and between subgroups, we performed a likelihood ratio test comparing the model with and without the covariate and assumed that the variances for the random effects for the logit sensitivities and logit specificities were similar. For the investigation of heterogeneity we used the melogit command in STATA to fit models that included particular covariates.
Takwoingi 2013 has showed that direct comparisons conducted within each study are more reliable than indirect comparisons. When direct comparisons were available, we plotted data points and joined the two estimates (one for each test) from each study by a line to show the difference in accuracy between tests. If a sufficient number of such paired studies had been available, we planned to pool them in bivariate meta‐analyses and tested their relative accuracy with a covariate coding for each test using the methods described above.
Since occludable angles are often bilateral, this complication may result in unit of analysis issues. We included studies that evaluated only one eye of each participant or, in participants with two affected eyes, studies that randomly selected only one eye. We also included studies that included both eyes in our review, but we acknowledged the unit of analysis issue when formulating our conclusions (i.e. acknowledging the overestimate of the precision in accuracy).
Investigations of heterogeneity
We investigated any heterogeneity in sensitivity and specificity through visual inspection of forest plots and the degree to which individual study results lie close together on the summary ROC curve. For diagnostic tests with a sufficient number of eligible studies, we planned to formally explore heterogeneity using the following study‐level covariates:
study design (e.g. single‐gate and two‐gate designs);
diagnostic reference thresholds (gonioscopy grading (e.g. number of quadrants occluded));
characteristics of the study population (e.g. high versus low prevalence, ethnicity). The comparison of low versus high prevalence level was based on the study setting. Studies undertaken in secondary care included populations with a higher prevalence, whilst studies conduced in a primary care/community setting included participants with a low prevalence of the target condition.
Sensitivity analyses
We planned to perform a sensitivity analysis to assess the impact of risk of bias on test accuracy by repeating the analysis after removing studies at high risk of bias.
Results
Results of the search
The electronic searches yielded a total of 6719 records (Figure 2). After 2460 duplicate records were removed we screened the remaining 4259 records. We excluded 4094 records at the title and abstract stage and obtained full‐text reports of 165 references for further assessment. We excluded 108 reports of 108 studies (see Characteristics of excluded studies for reasons). We identified 57 reports of 47 studies (see Characteristics of included studies) that met the inclusion criteria, recruiting 26,151 participants and providing data from 23,440 participants for quantitative analysis. Nineteen of the included studies were cohort studies, 15 were cross‐sectional and 13 used a case‐control design. Most studies were conducted in Asia (36, 76.6%), followed by Europe (5, 10.6%), North America (3, 6.4%), South America (2, 4.3%) and Africa (1, 2.1%), and over half the studies (30 studies, 4950 participants) were conducted in a secondary care setting, with the remainder (17 studies, 21,201 participants) in a primary care or community setting. The sample size ranged from 24 to 2052 participants (median 200) with most studies enrolling one eye per person (34, 72.3%).
2.

Study flow diagram.
Twenty‐seven studies assessed AS‐OCT (analysing 15,580 participants), 17 studies LACD (7385 participants), nine studies Scheimpflug photography (1616 participants), six studies SPAC (5239 participants) and five studies evaluated the flashlight (oblique handlight) test (998 participants). Thirty‐three of the studies evaluated a single index test and the remainder evaluated two or more tests on the same population. For the gonioscopic reference standard, 42 studies reported either the number of quadrants or degrees occluded. Thirty‐six (76.6%) studies (analysing 21,840 (93.2%) of participants) used a diagnostic definition 2 or more quadrants occluded, six studies used one or more quadrants occluded, three studies reported on occlusion of the nasal or temporal quadrant only, and one study used the clinicians subjective opinion of occludability. The gonioscopic reference criterion was not reported in one study.
Methodological quality of included studies
A summary of the methodological quality assessment is shown in the risk of bias and applicability graph and summary for each test (Figure 3 and Figure 4). Thirty‐six of the included studies (76.6%) were judged to have a high risk of bias in at least one domain.The risk of bias and applicability concerns are detailed below.
3.
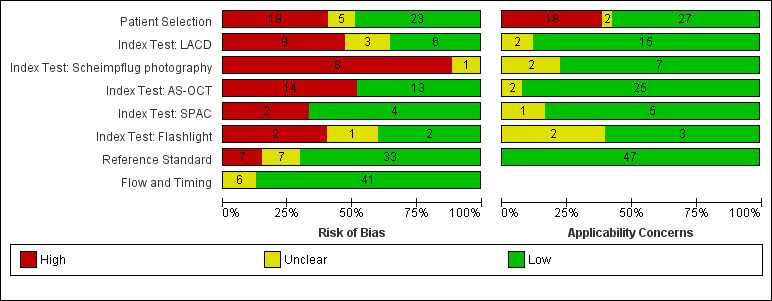
Risk of bias and applicability concerns graph: review authors' judgements about each domain presented as percentages across included studies
4.

Risk of bias and applicability concerns summary: review authors' judgements about each domain for each included study
Patient Selection domain
Nineteen of the included studies (40.4%) were judged to have a high risk of patient selection bias. Thirteen studies adopted a case‐control design that recruited participants with the target condition (cases), and a group of control participants without the target condition. Six studies used inappropriate exclusions e.g. excluding eyes with PAS, high myopia, optic neuropathy, or used age restrictions. Five studies (10.6%) were categorised as having an unclear risk of bias due to poor reporting of recruitment strategy e.g. failure to report exclusion criteria or method of sampling,
The purpose of the index tests is to triage at‐risk populations or in opportunistic case‐detection to identify people at risk of angle closure. The inclusion of participants with a previous diagnosis of the target condition therefore raised applicability concerns, as the spectrum of participants in these studies was not representative of those who would receive the test in practice.
Index test domain
There was a high risk of bias in studies where index test thresholds were not pre‐defined. Optimal cut‐offs were determined post hoc in eight of the nine studies that evaluated Scheimpflug photography, approximately half for AS‐OCT (14 studies, 52%) and two of the six studies that evaluated SPAC. In the majority of studies, the index test was interpreted without knowledge of the results of the reference standard. However, for LACD, eight studies (47.1%) were judged at high risk of bias since either the same observer performed the index and reference test (6 studies) or the threshold was not pre‐defined (2 studies).
Applicability of the test was generally of low concern across all the index tests, as the tests and testing procedures were clearly described and executed by personal who were sufficiently trained.
Reference standard domain
For the reference standard domain, 33 studies (70.2%) were judged to be at a low risk of bias, seven studies (14.9%) were classified as high risk as gonioscopy was not masked to the index test result, and in seven studies (14.9%) masking was unclear. Concerns regarding applicability were not applicable for this review, since gonioscopy was used as the reference standard for the diagnosis of an occludable angle in all of the included studies.
Flow and Timing domain
For the flow and timing domain, the majority of studies (41, 87.2%) were classified as having a low risk of bias. In these studies, all participants receiving the index test were verified with the reference standard, the number of participants included in the study matched the number in the analysis and there was less than a three‐month interval between the execution of the index and reference tests. There were five studies (10.6%) where the time interval where the time interval between the index and reference test was not reported, and in one study it was unclear whether all participants were included in the analysis.
The overall number of participants/eyes excluded from all the studies due to gonioscopy was negligible (< 0.3%), for LACD, flashlight, SPAC and Scheimpflug photography it was small (0% to 1.9%). The number of eyes/participants excluded from final analysis using AS‐OCT was relatively high (13.9%), due to the non‐interpretation of the data owing to either the clinician or the internal software inability to identify the scleral spur.
Conflict of Interest
Conflict of interest was of high concern in 15 studies, of unclear concern in 10 studies, and of no concern in 22 studies. Conflicts of interest were reported for 13 studies that evaluated AS‐OCT (56.5%), where the authors described receiving financial support from the manufacturer and/or loan of the device. For SPAC, four studies (66%) involved the patent holder of the device who was also a co‐author.
Unit of analysis concerns
Thirteen studies analysed data from both eyes, however seven of these studies corrected for clustering of data (Congdon 1996; Foster 2000; Lavanya 2008; Narayanaswamy 2010; Nolan 2007; Li 2019; Rossi 2012).
Findings
Forty‐seven studies reported sensitivity and specificity values for one or more index tests. Table 2 presents the pooled diagnostic accuracy estimates for index test parameters with four or more studies providing data at fixed thresholds for each test.
1. Accuracy of index test parameters.
| Test |
No. of studies (Number of eyes analysed) |
Se (95% CI) | Sp (95% CI) | P values for differences between [test] and LACD ≤ 25% | |
| Se | Sp | ||||
| LACD | |||||
| 25% or < 25% | 16 (7540) | 0.83 (0.74 to 0.90) | 0.88 (0.84 to 0.92) | Reference | |
| 15% | 5 (3345) | 0.61 (0.36 to 0.81) | 0.93 (0.83 to 0.97) | ||
| 5% | 4 (2920) | 0.42 (0.31 to 0.55) | 0.97 (0.96 to 0.98) | ||
| 0% | 4 (2920) | 0.08 (0.03 to 0.18) | 1.00 (0.99 to 1.00) | ||
| Flashlight | |||||
| Grade One | 5 (1188) | 0.51 (0.25 to 0.76) | 0.92 (0.70 to 0.98) | 0.0181 | 0.5508 |
| SPAC | |||||
| ≤ 5 and/or S or P | 4 (4677) | 0.83 (0.70 to 0.91) | 0.78 (0.70 to 0.83) | 0.9707 | 0.5947 |
| Scheimpflug photography | |||||
| ACD central | 9 (1698) | 0.92 (0.84 to 0.96) | 0.86 (0.76 to 0.93) | 0.0828 | 0.5325 |
| ACA | 6 (1330) | 0.79 (0.64 to 0.89) | 0.88 (0.68 to 0.96) | ||
| ACV | 6 (1474) | 0.87 (0.82 to 0.91) | 0.79 (0.70 to 0.86) | ||
| AS‐OCT | |||||
| Subjective | 13 (9239) | 0.85 (0.76 to 0.91) | 0.71 (0.62 to 0.78) | 0.6632 | 0.0003 |
| ACA | 4 (517) | 0.81 (0.72 to 0.88) | 0.91 (0.84 to 0.95) | ||
| ACD | 4 (530) | 0.89 (0.78 to 0.95) | 0.88 (0.75 to 0.95) | ||
| AOD 500 nasal | 4 (1976) | 0.95 (0.76 to 0.99) | 0.82 (0.72 to 0.89) | ||
| AOD 500 temp. | 4 (1976) | 0.94 (0.75 to 0.99) | 0.81 (0.73 to 0.87) | ||
| AOD 750 temp. | 4 (3758) | 0.93 (0.84 to 0.97) | 0.85 (0.77 to 0.90) | ||
| TISA 500 nasal | 4 (1976) | 0.79 (0.71 to 0.85) | 0.81 (0.73 to 0.86) | ||
| TISA 500 temp. | 4 (1976) | 0.84 (0.77 to 0.89) | 0.81 (0.61 to 0.92) | ||
For the comparison between index tests, we considered LACD < 25% as the reference category and used bivariate models to investigate whether sensitivity and/or specificity differs between the most commonly used test parameters for each index test.
Limbal anterior chamber depth (LACD)
Seventeen studies (recruiting 7385 participants) assessed LACD, with nine studies evaluating a single threshold and the remainder providing data on two or more thresholds. With an increasing LACD cut‐off criterion (0%, ≤ 5%, ≤ 15%, ≤ 25%), there was an increase in sensitivity (0.08 to 0.83) with a corresponding reduction in specificity (1.00 to 0.88). (Table 2). The most commonly used threshold was ≤ 25% (used in 16 studies, 7011 participants (7540 eyes)), which produced pooled sensitivity and specificity estimates of 0.83 (95% CI 0.74 to 0.90) and 0.88 (95% CI 0.84 to 0.92), respectively Figure 5. The certainty of this evidence was moderate due to risk of bias concerns, since the same observer performed the index and the reference test in many studies (see Table 1).
5.

Summary ROC Plot of LACD with thresholds of 0%, ≤5%, ≤15%, ≤ 25% or <25%, ≤40%, >25% to ≤50%. Summary point estimate and confidence region shown for LACD ≤ 25%.
Flashlight Test
Five studies (998 participants) evaluated the flashlight test, three studies evaluated grades 1 and 2, and two studies evaluated only grade 1. Visual inspection of the forest plot at this threshold revealed significant heterogeneity with respect to sensitivity, which ranged from 0.20 to 0.89. A meta‐analysis was conducted for grade 1 (1188 eyes), including all studies, with an estimated pooled sensitivity of 0.51 (95% CI 0.25 to 0.76) and specificity of 0.92 (95% CI 0.70 to 0.98) (Figure 6). The certainty of this evidence was low due to heterogeneity in accuracy estimates among studies and a high risk of bias (Table 1). There were insufficient studies to generate a summary estimate for grade 2.
6.

Summary ROC Plot of the flashlight test with thresholds of grade 1 and grade 2. Summary point estimate and confidence region shown for flashlight grade 1.
SPAC
Six studies (5239 participants) examined SPAC, three studies reported both categorical and numerical grades, two studies presented only the numerical grading and one study described only categorical thresholds. Four studies used both categorical and numerical thresholds Figure 7. The most common numerical grading was a threshold of ≤ 5. For the meta‐analysis, this numerical grade was amalgamated with the combined S and P categorical grade (4 studies, 4677 eyes), to produce a summary estimate of diagnostic performance for ≤ 5 and/or S or P (sensitivity 0.83 (95% CI 0.70 to 0.91); specificity 0.78 (95% CI 0.70 to 0.83)). The certainty of this evidence was moderate (Table 1).
7.

Summary ROC Plot of SPAC with thresholds of S or P, S, ≤ 4, ≤ 5, ≤ 5 and or S or P, ≤ 6, ≤ 6 and or S or P.
Scheimpflug photography
Nine studies (1616 participants) evaluated the diagnostic performance of Scheimpflug photography. Four studies reported all three anterior segment parameters (ACA, ACD and ACV), four studies evaluated two parameters and one study evaluated only ACD Figure 8. Point estimates of summary sensitivity varied between 0.79 and 0.92 across the parameters. Central ACD was the most commonly reported threshold (used in all nine studies, 1698 eyes), which produced a pooled sensitivity estimate of 0.92 (95% CI 0.84 to 0.96) and specificity 0.86 (95% CI 0.76 to 0.93). The certainty of this evidence was moderate due to the case‐control design used in over half of the studies (Table 1).
8.

Summary ROC Plot of Scheimpflug photography with thresholds of ACV, ACD (central), ACA. and ACD (peripheral). Summary point estimate and confidence region shown for ACD (central).
Quantitative parameters reported unique cut‐off values that were derived from the data post‐hoc in eight of the nine studies.
Anterior segment optical coherence tomography (AS‐OCT)
Twenty‐seven studies (15,580 participants) assessed AS‐OCT, 17 studies used the Visante time domain AS‐OCT; four studies used a slit lamp OCT; two studies spectral domain OCT with a lens adapter and four studies utilised swept source OCT. Thirteen unique AS‐OCT parameters were reported; using either quantitative or qualitative thresholds or both. Pooled point estimates of sensitivity and specificity could only be calculated for eight parameters (subjective opinion of occludability, AOD 500 (nasal), AOD 500 (temporal), AOD 750 (temporal), TISA 500 (nasal), TISA 500 (temporal), ACA, ACD) with pooled sensitivities ranging from 0.79 to 0.95 and specificities from 0.71 to 0.88 (Table 2). Subjective judgement of occludability was the most commonly used threshold (used in 13 studies (48.1%), 9,239 eyes), which produced a pooled sensitivity estimate of 0.85 (95% CI 0.76 to 0.91); specificity 0.71 (95% CI 0.62 to 0.78) (Figure 9). The certainly of this evidence was moderate (Table 1).
9.

Summary ROC Plot of AS‐OCT with thresholds of subjective judgement), AOD 500 temporal, AOD 500 nasal, AOD 750 temporal, TISA 500 temporal, TISA 500 nasal, TISA 750 temporal, TISA 750 nasal, ACA angle, ACA area, ACD, ACV, ARA 500 average, ARA 750 average, ARA 750 nasal and LV. Summary point estimate and confidence region shown for AS‐OCT (subjective judgement).
Quantitative parameters reported unique cut‐off values that were derived from the data post‐hoc, which could have led to an overestimation of test performance.
Comparison between tests
The most commonly reported parameter for each index test was compared using LACD (≤ 25%) as the reference category Table 2. Comparisons of sensitivity and specificity were not shown to differ across all the index tests, except for the flashlight test, where a grade 1 threshold had a statistically significant lower sensitivity than LACD, and AS‐OCT (subjective judgement), which had a statistically significant lower specificity.
Direct comparisons between tests in the same studies were available for LACD ≤ 25% versus AS‐OCT (subjective opinion of occludability) in three studies, Figure 10) and for LACD ≤ 25% versus Scheimpflug photography (central ACD) in two studies (Figure 11), with no clear pattern seen. LACD ≤ 25% seemed more accurate than flashlight (grade1) in two studies (Figure 12).
10.

Summary ROC of tests: 4 Direct comparison: LACD ≤ 25% or <25%, 20 Direct comparison: AS‐OCT (subjective judgement).
11.
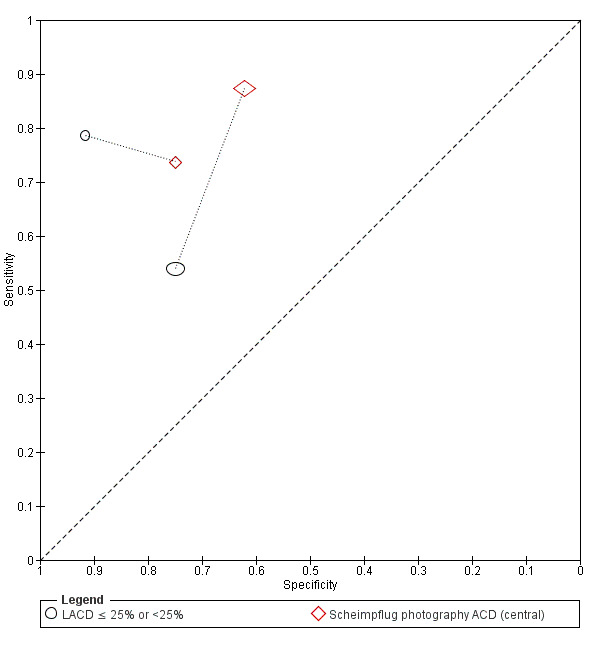
Summary ROC Plot of tests: 4 Direct comparison: LACD ≤ 25% or < 25%, 17 Direct comparison: Scheimpflug photography ACD (central).
12.

Summary ROC Plot of tests: 4 Direct comparison: LACD ≤ 25% or < 25%, 7 Direct comparison: Flashlight grade 1.
Investigation of heterogeneity and subgroup analysis
Among pre‐planned study level covariates, we investigated the effect of the setting by comparing accuracy in 16 studies reporting LACD at a common threshold (≤ 25%) conducted in a primary care/ community setting (seven studies, mean prevalence 14.4%) with that in studies conducted in secondary care (seven studies, mean prevalence 42%) and in case‐control studies (two studies, 520 participants, mean prevalence 79.2%). Case‐control studies were analysed in a different category since prevalence is determined by study design. The sensitivity and specificity were 0.90 (95% CI: 0.75 to 0.97) and 0.82 (95%CI: 0.66 to 0.91) for primary care/community studies, 0.82 (95%CI: 0.67 to 0.91) and 0.91 (95% CI: 0.85 to 0.94) in secondary care studies, and 0.89 (95% CI: 0.64 to 0.97) and 0.86 (95% CI: 0.78 to 0.91) in case‐control studies. We found no evidence of a statistically significant difference in test performance according to setting.
There were insufficient studies to conduct the effect of other pre‐specified covariates including gonioscopic diagnostic reference thresholds. We also planned to perform a sensitivity analysis to assess the impact of risk of bias on test accuracy by repeating the analysis after removing studies at high risk of bias, however nearly all the studies were judged to have at least one domain that was labelled as high/unclear risk of bias or had applicability concern.
Discussion
This systematic review evaluated the diagnostic accuracy of non‐contact tests including: LACD (van Herick test), flashlight, SPAC, Scheimpflug photography and AS‐OCT for detecting individuals at risk of PACG. These tests were evaluated as stand‐alone triage methods that could be used by specialist or non‐specialist healthcare professionals in a primary care or secondary care setting for case‐detection. In the proposed clinical pathway, screen positive cases would be referred for gonioscopic assessment by a glaucoma specialist.
Summary of main results
We analysed data from a total of 23,440 participants in 47 studies reporting the diagnostic accuracy of one or more index tests for the detection of an occludable angle.
The LACD test (van Herick test) was investigated in 17 studies. This test is quick, relatively inexpensive and can be used by non‐glaucoma specialists with a minimal amount of training, Using a cut‐off 25% or less, our pooled estimates found that at 10% prevalence as in a community setting, 17 out of 100 people at risk of angle closure would be missed and not sent to ophthalmic assessment and would potentially be exposed to acute or chronic angle‐closure glaucoma and 108 out of 900 people who are not at risk would be sent to ophthalmic assessment unnecessarily, increasing costs with little or no benefit. These estimates of accuracy, although they are sub‐optimal, can still be suitable for case‐detection in areas where most people do not receive basic ophthalmic care, There were only two case‐control studies in the main analysis on LACD and the certainty of the evidence was moderate, meaning that we are relatively confident in our estimates. A subgroup analysis comparing community (low prevalence) studies versus secondary care (high prevalence) settings found no evidence of a statistically significant difference in diagnostic performance according to setting.
Fifty‐seven per cent of included studies evaluated AS‐OCT. This technology has a number of theoretical advantages, including the rapid and non‐invasive acquisition of high‐resolution images of the complete 360 degrees of the ACA. These images can be interpreted qualitatively or quantitatively. Although the included studies provided data on 13 separate AS‐OCT parameters, the lack of consistency in the thresholds used meant that summary estimates could only be calculated for a minority of parameters (n = 8). The largest number of studies used subjective AS‐OCT assessment of angle width (n = 13) and yielded a similar sensitivity to LACD but a statistically significant lower specificity. This evidence was moderate‐certainty. Only four studies each used objective AS‐OCT test measures and ACD and AOD 500 obtained good sensitivity and specificity. However, given the small number of studies available for each measure, we conclude that more research is needed on AS‐OCT both in community and secondary care settings. This is particularly important as OCT technology continues to develop with ongoing improvements in image resolution. It is likely that the superior resolution of newer devices e.g. swept‐source OCT, may overcome the current problem of scleral spur visualisation, which is an important anatomical landmark for ACA evaluation. Furthermore, machine learning has recently shown potential for automated detection of angle‐closure in AS‐OCT images (Fu 2019).
Scheimpflug photography, which requires a costly device that is rarely used for anterior chamber angle assessment was evaluated in nine studies. The best performing parameter was ACD (central), which had similar sensitivity and specificity estimates to LACD (moderate‐certainty evidence).
Other tests, including the oblique flashlight test and SPAC, were investigated in only five studies each and showed either a low sensitivity or unacceptable specificity, with low‐ and moderate‐certainty evidence, respectively.
Although no firm conclusions can be drawn from indirect comparisons of diagnostic tests, we find no evidence of statistically significant differences between LACD and other objective tests that use costly devices. However, based on this analysis, the flashlight test showed a statistically significant lower sensitivity than LACD. This was also shown in the small number of studies that compared the tests directly.
The majority of studies were conducted in Asia. Pre‐specified thresholds were reported for LACD, flashlight, SPAC and the subjective judgement of occludability using AS‐OCT. However, all the reported thresholds for eight out of the nine studies for Scheimpflug photography and all quantitative AS‐OCT thresholds were calculated post‐hoc and were based on the best performing cut‐points derived from each study population. The heterogeneity of sensitivity and specificity estimates for each test was large and could not be adequately explained. Furthermore, 36 of the 47 included studies (76.6%) were judged to have a high risk of bias in at least one domain, most commonly due to patient selection bias and/or not pre‐defining the index test threshold. However, 38% of included studies recruited participants with a previous diagnosis of an occludable angle, which was mainly attributed to the use of a case‐control design. These designs are known to over‐estimate the performance of diagnostic tests and therefore our estimates of test accuracy could be higher than would be expected in unscreened populations. It is therefore possible that the reported estimates of test performance may differ from what may be expected in a standard clinical setting.
Strengths and weaknesses of the review
Strengths of this systematic review included its methodological rigour, which included the following.
A comprehensive search strategy to identify as many potential studies for inclusion as possible, with no language, clinical setting, study design or publication year restrictions
All titles and abstracts were independently screened by two review authors
Two review authors independently extracted data and conducted a quality assessment of studies (using QUADAS‐2).
We obtained translations of two non‐English studies that met the inclusion criteria and undertook data extraction and conducted 'Risk of bias' assessments
Sufficient studies were available to conduct a meta‐analysis and produce summary estimates of sensitivity and specificity for all five index tests
There were a number of limitations of the review. Comparisons between index tests are best conducted using direct (within study) comparisons, as direct comparisons are considered to be more reliable than indirect comparisons (between studies) (Takwoingi 2013). Since there were insufficient studies that reported more than one test or parameter, comparisons of test accuracy were mostly based on indirect comparisons and therefore subject to between‐study differences in characteristics of participants, diagnostic standards and study design. The majority of studies had a high or unclear risk of bias in at least one domain and substantial heterogeneity was observed between studies. This should be taken into consideration when interpreting the review findings. Finally, there were insufficient studies to compare test performance in populations of different ethnicity or angle closure disease severity, in addition we were unable to conduct the planned sensitivity analysis on the risk of bias, as this may have impacted the applicability of such tests.
Applicability of findings to the review question
Given that the tests could be applied in either primary or secondary care, we did not place any restriction on setting, although in both pathways consecutive undiagnosed participants would be evaluated or triaged. Several included studies recruited participants with a previous diagnosis of an occludable angle, which was mainly attributed to the use of a case‐control design, which may not only overestimate accuracy, but also cause concerns regarding applicability.
Although proportionately more studies were conducted in a secondary care setting and participants were typically recruited from specialist or general ophthalmology clinics, over 80% of participants included in the quantitative analysis were recruited from a primary care or community setting. Participants in these studies included those recruited in large cross‐sectional epidemiological studies, or from community polyclinics that provide primary care services to local populations. In the context of angle closure, patients with suspected occludable angles in such settings would be referred to secondary care for specialist evaluation.
Three‐quarters of the included studies were performed in Asia, which carries the greatest burden of PACG and its associated blindness (Tham 2014). The prevalence of PACG in Asian populations is up to three times higher than in European‐derived groups (Cheng 2014; Day 2012). Consequently, case‐detection of angle closure disease in these populations is more likely to be cost‐effective (Tang 2019).
Non‐contact tests for identifying occludable angles include both subjective (flashlight, LACD) and objective tests (SPAC and Scheimpflug photography). AS‐OCT imaging can be interpreted subjectively or objectively. Subjective tests in the included studies were generally interpreted by ophthalmologists, which could have potentially led to an improved test performance. However, previous studies evaluating LACD have found no difference in performance within and between ophthalmologists and non‐medical healthcare professionals, with moderate inter‐observer agreement for each group (Jindal 2015; Johnson 2018). Similarly, a small study assessing AS‐OCT qualitative judgements by glaucoma specialists also found moderate agreement (Tay 2015).
Angle closure disease represents a spectrum of disorders from angle closure suspect to PACG. Angle closure is defined by the degree of appositional contact between the peripheral iris and trabecular meshwork and the presence or absence of trabecular damage (PAS). Although all studies used gonioscopy as the reference standard, a variety of diagnostic definitions were used. The review allowed for this flexibility in clinical definition and accepted the classification of an occludable angle adopted by the investigators. The term 'occludable angle' could encompass varying degrees of risk of angle closure, clinically it is most important to ascertain whether the angle is potentially occludable and therefore at risk of developing glaucomatous optic neuropathy. The widely accepted classification of occludability is that proposed by the International Society for Geographical and Epidemiological Ophthalmology ISGEO group (Foster 2002) (two more quadrants occluded). Thirty‐six (76.6%) of the included studies (recruiting 24,347 (93.1%) of participants) used a diagnostic definition two or more quadrants occluded, one study used a sub‐specialist ophthalmologist opinion that the angle was occludable and nine studies used a threshold of one or less quadrants occluded. We therefore feel that the majority of angles included represented a referable condition and would be classified as at risk of occludability.
Authors' conclusions
Implications for practice.
Although the incidence of significant angle‐closure disease has recently been shown to be low amongst those with primary angle closure suspect (PACS), identified through community‐based screening (He 2019), it is possible that combined population screening for open‐ and closed‐angle glaucoma could be cost‐effective in high‐risk populations (Tang 2019).
The current reference standard to detect occludable angles is gonioscopy. Whilst this technique offers comprehensive visualisation of the anterior chamber angle (ACA) and adjacent structures, the test is invasive, requires a high degree of skill and is not usually performed outside a specialist ophthalmic setting. Gonioscopy is therefore unsuitable for case‐detection in primary care or non‐specialist secondary care settings. The current review evaluated tests that can be used to evaluate risk of angle closure by measuring anterior chamber dimensions. We found moderate‐certainty evidence that limbal anterior chamber depth (LACD), using a cut‐off of 25% or less, showed an acceptable sensitivity and a sufficient specificity for case‐finding and performed as well as more sophisticated imaging equipment. This finding is particularly important for case‐detection in areas where most people do not receive basic ophthalmic care. LACD is simple to perform and can be learned with relatively little training. The pooled estimates of diagnostic accuracy of LACD should be interpreted with caution since they derive from indirect comparisons
The flashlight test using a grade 1 cut point had a statistically significant lower diagnostic performance than other non‐contact tests and is therefore not recommended for case‐detection. Our evaluation of the diagnostic accuracy of anterior segment optical coherence tomography (AS‐OCT) was limited by the variety of parameters reported and the lack of pre‐specified thresholds.
Implications for research.
There is still a need for high‐quality studies to evaluate the performance of non‐invasive tests for angle assessment. These studies should adopt consecutive or random sampling using pre‐specified thresholds. Furthermore, investigators performing the index test and reference standard should be masked. Moreover, these studies should preferably be conducted in a community or primary care setting and avoid a case‐control design. If adequately funded, a direct comparison of LACD with objective devices to detect occludable angles should be undertaken.
The diagnostic accuracy of index tests to identify angle‐closure in subgroups (PACS, primary angle closure (PAC), primary angle closure glaucoma (PACG)) would also provide useful additional information that would be relevant for the development of care pathways for angle closure.
What's new
| Date | Event | Description |
|---|---|---|
| 31 July 2020 | Amended | Minor edits made to text in the following sections. Abstract/Data collection and analysis: METADAS macro in SAS changed to METANDI function in STATA. Findings/Anterior segment optical coherence tomography (AS OCT): 9.242 eyes corrected to 9,239 eyes. Table 1: Scheimpflug photography: 9 studies (461/1676) corrected to (461/1698) and AS‐OCT 13 studies (1995/9242) corrected to (1850/9239). Table 2: AS‐OCT Subjective 13 (9242) corrected to 13 (9239). |
History
Protocol first published: Issue 2, 2018 Review first published: Issue 5, 2020
Acknowledgements
We thank Iris Gordon (information Specialist, Cochrane Eyes and Vision (CEV)) who created and ran the electronic search strategies, Gemma Rossi for her comments on the protocol, Francesco Oddone for his comments on the review and Anupa Shah, Managing Editor for CEV for her help throughout the editorial process.
Appendices
Appendix 1. The Cochrane Library search strategy
#1 MeSH descriptor: [Glaucoma, Angle‐Closure] this term only #2 angle* near/3 (occlud* or narrow* or width or close* or closure) #3 glaucoma* near/3 (occlud* or narrow* or width or close* or closure) #4 PAC or PACS or PACG or ACG #5 #1 or #2 or #3 or #4 #6 MeSH descriptor: [Anterior Chamber] this term only #7 MeSH descriptor: [Anterior Eye Segment] this term only #8 anterior near/2 (chamber or segment) #9 ACD or ACA #10 #6 or #7 or #8 or #9 #11 MeSH descriptor: [Glaucoma] explode all trees #12 #10 and #11 #13 #5 or #12 #14 MeSH descriptor: [Diagnostic Techniques, Ophthalmological] explode all trees #15 flashlight* or torch #16 MeSH descriptor: [Slit Lamp] this term only #17 MeSH descriptor: [Slit Lamp Microscopy] this term only #18 slit near/2 (lamp or beam) #19 biomicroscope #20 anterior chamber depth* #21 Anterior chamber volume #22 lens volume #23 ACD or LACD or SPAC or ACV #24 Herick #25 Scheimpflug or Pentacam or Sirius or Galilei #26 MeSH descriptor: [Tomography, Optical Coherence] explode all trees #27 optical coherence tomograph* #28 AS‐OCT or Visanti #29 anterior segment imag* #30 angle recess area #31 angle opening distance #32 (angle or area*) near/2 trabec* near/2 iris #33 AOD or TISA #34 #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #33 #35 #13 and #34
Appendix 2. MEDLINE Ovid search strategy
1. Glaucoma, Angle‐Closure/ 2. (angle$ adj3 (occlud$ or narrow$ or width or close$ or closure)).tw. 3. (glaucoma$ adj3 (occlud$ or narrow$ or width or close$ or closure)).tw. 4. (PAC or PACS or PACG or ACG).tw. 5. or/1‐4 6. Anterior Chamber/ 7. Anterior Eye Segment/ 8. (anterior adj2 (chamber or segment)).tw. 9. (ACD or ACA).tw. 10. or/6‐9 11. exp Glaucoma/ 12. 10 and 11 13. 5 or 12 14. Diagnostic Techniques, Ophthalmological/ 15. (flashlight$ or torch).tw. 16. Slit Lamp/ 17. Slit Lamp Microscopy/ 18. (slit adj2 (lamp or beam)).tw. 19. biomicroscope.tw. 20. anterior chamber depth$.tw. 21. (ACD or LACD or SPAC).tw. 22. Herick.tw. 23. (Scheimpflug or Pentacam or Sirius or Galilei).tw. 24. Tomography, Optical Coherence/ 25. optical$ coherence tomograph$.tw. 26. (AS‐OCT or Visanti).tw. 27. anterior segment imag$.tw. 28. angle recess area.tw. 29. angle opening distance.tw. 30. ((angle or area$) adj2 trabec$ adj2 iris).tw. 31. (AOD or TISA).tw. 32. or/14‐31 33. 13 and 32 34. exp case report/ 35. (case adj1 (study or report$)).tw. 36. 34 or 35 37. 33 not 36
Appendix 3. Embase Ovid search strategy
1. closed angle glaucoma/ or glaucomatous optic neuropathy/ or neovascular glaucoma/ or secondary glaucoma/ 2. (angle$ adj3 (occlud$ or narrow$ or width or close$ or closure)).tw. 3. (glaucoma$ adj3 (occlud$ or narrow$ or width or close$ or closure)).tw. 4. (PAC or PACS or PACG or ACG).tw. 5. or/1‐4 6. anterior eye chamber/ 7. anterior eye segment/ 8. (anterior adj2 (chamber or segment)).tw. 9. (ACD or ACA).tw. 10. or/6‐9 11. exp glaucoma/ 12. 10 and 11 13. 5 or 12 14. (flashlight or torch).tw. 15. slit lamp/ 16. (slit adj2 (lamp or beam)).tw. 17. biomicroscope.tw. 18. anterior eye chamber angle/ 19. anterior eye chamber depth/ 20. anterior chamber depth$.tw. 21. Anterior chamber volume.tw. 22. lens volume.tw. 23. (ACD or LACD or SPAC or ACV).tw. 24. Herick.tw. 25. ophthalmic camera/ 26. (Scheimpflug or Pentacam or Sirius or Galilei).tw. 27. optical coherence tomography/ 28. optical$ coherence tomograph$.tw. 29. (AS‐OCT or Visanti).tw. 30. anterior segment imag$.tw. 31. angle recess area.tw. 32. angle opening distance.tw. 33. ((angle or area$) adj2 trabec$ adj2 iris).tw. 34. (AOD or TISA).tw. 35. or/14‐34 36. 13 and 35 37. exp case report/ 38. (case adj1 (study or report$)).tw. 39. or/37‐38 40. 36 not 39
Appendix 4. BIOSIS search strategy
#29 #28 AND #27 #28 TS= (human or humans) #27 #26 AND #10 #26 #25 OR #24 OR #23 OR #22 OR #21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 #25 TS=(AOD or TISA) #24 TS= ((angle or area*) NEAR/2 trabec* NEAR/2 iris) #23 TS= (angle opening distance) #22 TS= (angle recess area) #21 TS= (anterior segment imag*) #20 TS = (AS‐OCT or Visanti) #19 TS= (optical* coherence tomograph*) #18 TS= (Herick or Scheimpflug or Pentacam or Sirius or Galilei) #17 TS= (ACD or LACD or SPAC or ACV) #16 TS= (lens volume) #15 TS= (Anterior chamber volume) #14 TS= (anterior chamber depth) #13 TS=biomicroscope #12 TS=(slit NEAR/2 (lamp or beam)) #11 TS= (flashlight* or torch) #10 #9 OR #4 #9 #8 AND #7 #8 TS= Glaucoma #7 #6 OR #5 #6 TS= (ACD or ACA) #5 TS= (anterior NEAR/2 (chamber or segment)) #4 #3 OR #2 OR #1 #3 TS= (PAC or PACS or PACG or ACG) #2 TS= (glaucoma* NEAR/3 (occlud* or narrow* or width or close* or closure)) #1 TS = (angle* NEAR/3 (occlud* or narrow* or width or close* or closure))
Appendix 5. OpenGrey search strategy
(angle closure glaucoma OR PAC OR PACS OR PACG OR ACG) AND (flashlight OR torch OR Slit Lamp OR biomicroscope OR anterior chamber depth OR ACD OR LACD OR SPAC OR Scheimpflug OR Pentacam OR Optical Coherence Tomography OR Visanti)
Appendix 6. ARIF search strategy
(angle closure glaucoma OR PAC OR PACS OR PACG OR ACG) (All indexed fields) AND (flashlight OR torch OR Slit Lamp OR biomicroscope OR anterior chamber depth OR ACD OR LACD OR SPAC OR Scheimpflug OR Pentacam OR Optical Coherence Tomography OR Visanti) (All indexed fields)
Appendix 7. ISRCTN search strategy
(angle closure glaucoma OR PAC OR PACS OR PACG OR ACG) AND (flashlight OR torch OR Slit Lamp OR biomicroscope OR anterior chamber depth OR ACD OR LACD OR SPAC OR Scheimpflug OR Pentacam OR Optical Coherence Tomography OR Visanti)
Appendix 8. ClinicalTrials.gov search strategy
(angle closure glaucoma OR PAC OR PACS OR PACG OR ACG) AND (flashlight OR torch OR Slit Lamp OR biomicroscope OR anterior chamber depth OR ACD OR LACD OR SPAC OR Scheimpflug OR Pentacam OR Optical Coherence Tomography OR Visanti)
Appendix 9. ICTRP search strategy
angle closure glaucoma OR PAC OR PACS OR PACG OR ACG = Condition AND flashlight OR torch OR Slit Lamp OR biomicroscope OR anterior chamber depth OR ACD OR LACD OR SPAC OR Scheimpflug OR Pentacam OR Optical Coherence Tomography OR Visanti = Intervention
Appendix 10. Data extracted for the Characteristics of Included Studies table
| Study identification | First author, year of publication |
| Clinical features and settings | Previous testing and clinical setting including country where the study was conducted. Presentation at recruitment, prior treatment that would affect the ACD (i.e. peripheral iridotomy, iridoplasty, etc.) |
| Participants | Sample size, age, sex, ethnicity and country |
| Study design | Whether the sample was selected as a single group (consecutive series) or as separate groups with and without the target condition (case‐control). Whether participants were consecutively enrolled in the study and were identified retrospectively or prospectively. Training involved for index tests, both eyes included in the study |
| Target condition | An occludable angle as a referable condition, which includes PACS, PAC and PACG |
| Reference standard | The reference standard test used: gonioscopy for diagnosing an occludable angle; this is acceptable if this is the only target condition in large‐scale screening or primary‐care settings. Gonioscopy combined with tonometry, visual fields investigation and optic disc assessment for distinguishing the relative subgroup of participants with an occludable angle as PACS/PAC/PACG |
| Index tests | Oblique flashlight test: grade recorded LACD using the van Herick technique: van Herick grade, or percentage, or both SPAC: numerical or categorical grade, or both Scheimpflug photography: ACA, ACV and ACD AS‐OCT: model of OCT device, manufacturer and any technical characteristics (e.g. software analyses). TISA, ARA, AOD 500 microns and 750 microns for each parameter |
| Follow up | Numbers of participants lost to follow‐up or who had uninterpretable test results |
| Notes | Source of funding, anything else of relevance |
Appendix 11. List of abbreviations
| ACA ACD ACV AOD ARA AS‐OCT IOP ITC LACD LPI PAC PACG PACS PAS SPAC TISA |
Anterior chamber angle Anterior chamber depth Anterior chamber volume Angle opening distance Angle recess area Anterior segment optical coherence tomography Intraocular pressure Irido‐trabecular contact Limbal anterior chamber depth Laser peripheral iridotomy Primary angle closure Primary angle closure glaucoma Primary angle closure suspect Peripheral anterior synechiae Scanning peripheral anterior chamber analysis Trabeculo‐iris space area |
Appendix 12. Guidance for QUADAS 2 assessment of risk of bias
| DOMAIN | LOW | HIGH | UNCLEAR |
| PARTICIPANT SELECTION | Describe methods of participant selection; describe included participants (prior testing, presentation, intended use of index test and setting) | ||
| Was a consecutive or random sample of participants enrolled? | Consecutive sampling or random sampling of people according to inclusion criteria | Non‐consecutive cohort of referrals (from primary care) or (in screening setting) sampling based on volunteering or referral | Unclear whether consecutive or random sampling used |
| Was a case‐control design avoided? | No selective recruitment of people with or without occludable angles, or nested case‐control designs (systematically and randomly selected from a defined population cohort) | Selection of either cases or controls in a predetermined, non‐random fashion; or enrichment of the cases from a selected population | Unclear selection mechanism |
| Did the study avoid inappropriate exclusions? | Exclusions are detailed and felt to be appropriate (e.g. people with corneal opacities, known ocular malformation or disease causing bulbar derangement) | Inappropriate exclusions are reported (e.g. of people with borderline index test results) | Exclusions are not detailed (pending contact with study authors) |
| Risk of bias: could the selection of participants have introduced bias? | All signalling questions = ‘Yes’ | Any signalling question = ‘No’ | Unclear |
| Concerns regarding applicability: are there concerns that the included participants do not match the review question? | Inclusion of participants without a previous diagnosis of an occludable angle | Inclusion of participants with a previous diagnosis of an occludable angle | Unclear inclusion criteria |
| INDEX TEST | Describe the index test and how it was conducted and interpreted | ||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Test performed “blinded” or “independently and without knowledge of” reference standard results are sufficient and full details of the blinding procedure are not required; or clear temporal pattern to the order of testing that precludes the need for formal blinding | Reference standard results were available to those who conducted or interpreted the index tests | Unclear whether results are interpreted independently |
| If a threshold was used, was it prespecified? | The study authors declare that the selected cut‐off used to dichotomise data was specified a priori; or a protocol is available with this information | A study is classified at higher risk of bias if the authors define the optimal cut‐off post hoc, based on their own study data | No information on pre selection of index test cut‐off values |
| Risk of bias: could the conduct or interpretation of the index test have introduced bias? | All signalling questions = ‘Yes’ | Any signalling question = ‘No’ | Unclear |
| Concerns regarding applicability: are there concerns that the index test, its conduct or interpretation differ from the review question? | Tests used and testing procedure clearly reported and tests executed by personnel with sufficient training | Tests used are not validated or study personnel was insufficiently trained | Unclear execution of the tests or unclear study personnel profile, background and training |
| REFERENCE STANDARD | Describe the reference standard and how it was conducted and interpreted | ||
| Is the reference standard likely to correctly classify the target condition? | Not applicable. Score ‘Yes’ for all studies | ||
| Were the reference standard results interpreted without knowledge of the results of the index test? | Reference standard performed “blinded” or “independently and without knowledge of” index test results are sufficient and full details of the blinding procedure are not required; or clear temporal pattern to the order of testing that precludes the need for formal blinding | Index test results were available to those who conducted the reference standard | Unclear whether results were interpreted independently |
| Risk of bias: could the reference standard, its conduct or its interpretation have introduced bias? | All signalling questions = ‘Yes’ | Any signalling question = ‘No’ | Unclear |
| Concerns regarding applicability: are there concerns that the target condition as defined by the reference standard does not match the review question? | Not applicable. Score ‘Low’ for all studies | ||
| FLOW AND TIMING | Describe any participants who did not receive the index test(s) or reference standard, or either, or who were excluded from the 2 x 2 table (refer to study flow diagram); describe the time interval and any interventions between index test(s) and reference standard | ||
| Was there an appropriate interval between index test(s) and reference standard? | No more than three months between index and reference test execution | More than three months between index and reference test execution | Unclear whether test results were executed within three months |
| Did all participants receive a reference standard? | All participants receiving the index test were verified with the reference standard | Not all participants receiving the index test were verified with the reference standard | Unclear whether all participants receiving the index test were verified with the reference standard |
| Did all participants receive the same reference standard? | Not applicable. Score ‘Yes’ for all studies | ||
| Were all participants included in the analysis? | The number of participants included in the study match the number in analysis | The number of participants included in the study does not match the number in analysis | Insufficient information on whether the number of participants included in the study matches the number in analysis |
| Risk of bias: could the participants' flow through the study have introduced bias? | All signalling questions = ‘Yes’ | Any signalling question = ‘No’ | Unclear |
Data
Presented below are all the data for all of the tests entered into the review.
Tests. Data tables by test.
1. Test.

LACD 0%
2. Test.

LACD ≤ 5%
3. Test.
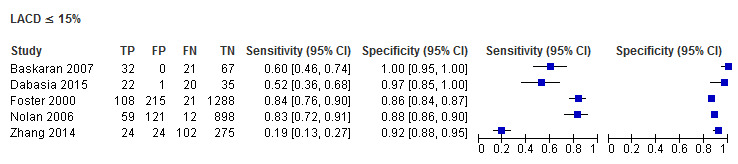
LACD ≤ 15%
4. Test.

LACD ≤ 25% or <25%
5. Test.

LACD ≤ 40%
6. Test.

LACD > 25% to ≤ 50%
7. Test.

Flashlight grade 1
8. Test.

Flashlight grade 2
9. Test.

SPAC S or P
10. Test.

SPAC S
11. Test.

SPAC ≤ 4
12. Test.

SPAC ≤ 5
13. Test.

SPAC ≤ 5 and or S or P
14. Test.

SPAC ≤6
15. Test.
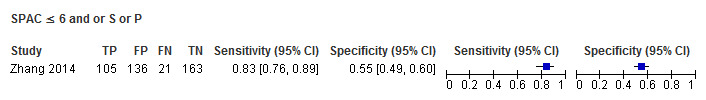
SPAC ≤ 6 and or S or P
16. Test.

Scheimpflug photography ACV
17. Test.

Scheimpflug photography ACD (central)
18. Test.

Scheimpflug photography ACA
19. Test.

Scheimpflug photography ACD (peripheral)
20. Test.

AS‐OCT (subjective judgement)
21. Test.

AS‐OCT AOD 500 temporal
22. Test.

AS‐OCT AOD 500 nasal
23. Test.

AS‐OCT AOD 750 temporal
24. Test.

AS‐OCT AOD 750 nasal
25. Test.

AS‐OCT AOD 500 average
26. Test.

AS‐OCT TISA 500 temporal
27. Test.

AS‐OCT TISA 500 nasal
28. Test.

AS‐OCT TISA 500 average
29. Test.
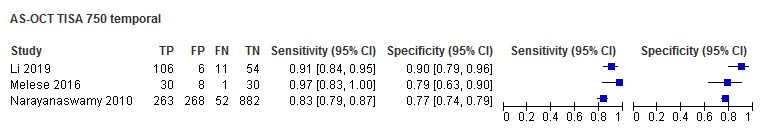
AS‐OCT TISA 750 temporal
30. Test.

AS‐OCT TISA 750 nasal
31. Test.

AS‐OCT TISA 750 average
32. Test.

AS‐OCT ACA
33. Test.

AS‐OCT ACA area
34. Test.

AS‐OCT ACD
35. Test.

AS‐OCT ACV
36. Test.

AS‐OCT ARA 500 average
37. Test.

AS‐OCT ARA 750 nasal
38. Test.

AS‐OCT ARA750 temporal
39. Test.
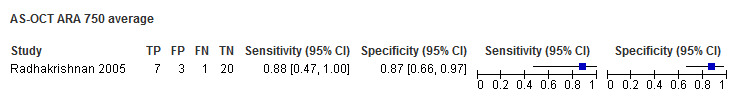
AS‐OCT ARA 750 average
40. Test.

AS‐OCT ITC index ≥35%
41. Test.

AS‐OCT ITC index ≥50%
42. Test.

AS‐OCT ITC index ≥70%
43. Test.

AS‐OCT ITC index ≥75%
44. Test.

AS‐OCT LV
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alonso 2010.
| Study characteristics | |||
| Patient Sampling | Cohort study. Methods of patient sampling and recruitment were not reported. Data from both eyes were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 60 participants, 112 eyes (38 eyes narrow angle and 74 open angle). Age: mean (SD), 51 ± 12, range 21‐72 years. Sex: 32 (53.3%) female. Setting: secondary care. Country: Brazil. Ethnicity: not reported. Exclusions: not reported. |
||
| Index tests | Scheimpflug photography: HR Pentacam, Oculus Inc, Germany, nasal and temporal angles were studied in the horizontal meridian, cut‐off values were derived from the study data for ACA and ACD. | ||
| Target condition and reference standard(s) | Static gonioscopy was performed, an occludable angle was classified using a Shaffer grade of 1 (the number of quadrants/degrees occluded were not reported). | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: no conflict of interest statement provided. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Could the selection of patients have introduced bias? | Unclear risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Andrews 2012.
| Study characteristics | |||
| Patient Sampling | Case‐control study. Cases were primary angle‐closure suspects (PACS), controls were participants with open‐angles who did not meet the PACS criteria. Data from the right eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 442 eyes (370 narrow angle and 72 open angle). Age: mean (SD), 59.8 ± 4.9 years (narrow angle 59.7 0 ± 5.2; controls 60.2 ± 3.2). Sex: 345 (78.0%) female. Setting: secondary care. Country: China. Ethnicity: Chinese. Exclusions: prior intraocular surgery, excessively high risk of acute angle‐closure attack, cataract preventing anterior chamber imaging. |
||
| Index tests |
LACD: graded as a percentage fraction of adjacent corneal thickness at the temporal limbus: >100%, 75%, 40%, 25%, 15%, 5%, and 0%, cut‐off value used ≤ 25%. SPAC: measurements ranged from 1 to 12, cut‐off value used ≤ 6. |
||
| Target condition and reference standard(s) | PACS: participants with pigmented trabecular meshwork not visible in at least two quadrants (≥180 degrees) on gonioscopy (without PAS, glaucomatous optic neuropathy or elevated IOP). | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflicts of interest: Dr Kashiwagi has a Japanese patent on the SPAC (Japanese patent No. 3878164). Dr Friedman currently has the SPAC instrument on loan from Carl Zeiss Meditec. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Ashaye 2003.
| Study characteristics | |||
| Patient Sampling | Cohort study. Cases were newly diagnosed people with primary glaucoma, with both cases and open angle controls were recruited from a secondary care setting from 1996 to 1998. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 490 eyes (40 narrow angle and 450 open angle). Age: mean (SD) 56.8 ± 11.1 years, (glaucoma 57.8 ± 11.5; non‐glaucoma 55.8 ± 10.7). Sex: 214 (43.7%) female. Setting: secondary care. Country: Nigeria. Ethnicity: African. Exclusions: not reported. |
||
| Index tests | LACD: if the peripheral ACD was equal to or greater than the corneal thickness it was recorded as grade 4; half corneal thickness was grade 3; quarter thickness of cornea was noted as grade 2, less than a quarter as grade 1 and no distance between the iris and cornea as grade 0. A cut‐off value of ≤ 25% was used at the temporal limbus. | ||
| Target condition and reference standard(s) | An occludable angle was defined as an angle in which the pigmented trabecular meshwork was not seen in ≥ 270 degrees of the angle circumference by static gonioscopy. | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. The index test and reference standard conducted on the same occasion. | ||
| Comparative | |||
| Notes | From the 450 participants with an open angle, 214 patients had primary open angle glaucoma and 236 had no glaucoma. Conflict of interest: no conflict of interest statement provided. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Could the selection of patients have introduced bias? | Unclear risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | No | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | High risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Baskaran 2007.
| Study characteristics | |||
| Patient Sampling | Cohort study, adult participants were recruited from glaucoma and general ophthalmology clinics. Consecutive participants were enrolled. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 120 eyes (53 narrow angle and 67 open angle). Age: mean (SD) 62.1 ± 11.3, range 30‐90 years. Sex: 68 (56.7%) female. Setting: secondary care. Country: Singapore. Ethnicity: 87 (72.5%) Chinese, 25 (20.8%) Indian, 8 Malay (6.7%). Exclusions: participants with corneal disorders and uveitis were excluded in the control group. People with a history of laser or intraocular surgery were excluded in the narrow angle group. |
||
| Index tests |
LACD: determined at the temporal limbus and graded as categories: 0%, 5%, 15%, 25%, 40%, 75% and ≥ 100%. Cut‐off values analysed were 0%, ≤ 5%, ≤ 15%, ≤ 25% and ≤ 40%. SPAC: SPAC categorical grades used for risk of angle closure. Thresholds used were S, P and the combination of S & P. |
||
| Target condition and reference standard(s) | An occludable angle was defined as the presence of a Shaffer grade of up to 1 (10 degree iridotrabecular angle) for at least 180 degrees on gonioscopy with or without PAS. | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: Dr Kashiwagi has a Japanese patent on SPAC (Japanese patent application no: 2003‐111322). | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Baskaran 2012.
| Study characteristics | |||
| Patient Sampling | Cohort study. Participants above the age of 40 years were recruited from a glaucoma clinic. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 98 eyes (39 narrow angle and 59 open angle). Age: mean (SD) 60.7 ± 12.6 years. Sex: 49 (50%) female. Setting: secondary care. Country: Singapore. Ethnicity: 69 (70%) Chinese. Exclusions: prior intraocular surgery or penetrating eye injury, corneal disorders such as corneal endothelial dystrophy, pterygium or corneal scars that may preclude satisfactory imaging or those on medications that act on the pupil. |
||
| Index tests | AS‐OCT: time domain, Visante; Carl Zeiss Meditec, Dublin, CA, USA. Three AS‐OCT images of each eye were obtained in dark conditions: one image scanning the angle at the nasal and temporal positions, one scanning the superior angle and one scanning the inferior angle. The cut‐off value was a closed angle in two or more quadrants, which was defined as subjective judgement of contact between the iris and angle wall anterior to the scleral spur. | ||
| Target condition and reference standard(s) | The ACA was considered ‘closed’ in that quadrant if the posterior pigmented trabecular meshwork could not be seen in the primary position without indentation on gonioscopy (Scheie grade 3 or 4). The eye was classified as having an occludable angle if there were two or more quadrants (≥ 180 degrees) closed. | ||
| Flow and timing | 98 participants entered the study, 1 was excluded, reason not specified. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: Dr Aung has received research support, travel support and honoraria from Carl Zeiss Meditec, Dublin, CA USA, as well as an instrument loan. Participants who underwent peripheral iridotomy were not excluded. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Baskaran 2013.
| Study characteristics | |||
| Patient Sampling | Cohort study. Phakic participants aged 40 years or older were recruited from glaucoma clinics at an eye hospital between January 2011 and July 2011. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 140 eyes (32 narrow angle and 108 open angle). Age: mean (SD), 59.2 ± 8.9 years, (narrow angle 63.7 ± 8.0; controls 57.8 ± 8.8). Sex: 99 (70.7%) female. Setting: secondary care. Country: Singapore. Ethnicity: 134 (95.7%) Chinese, 2 (1.4%) Malay, 3 (2.1%) Indian and 1 other. Exclusions: participants with corneal disease that precluded imaging of the anterior segment and those with previous uveitis, intraocular surgery, or lid abnormalities were excluded. |
||
| Index tests | AS‐OCT: swept source domain, CASIA SS‐1000, Tomey Corporation, Nagoya, Japan. Each eye was scanned with the 3‐dimensional angle analysis scan. Cut‐off values were derived from the study data using ITC analysis for the “ITC index,” which represents the ratio of ITC (angle closure) in degrees to the total angle visible, as a percentage. | ||
| Target condition and reference standard(s) | The ACA was considered “closed” on gonioscopy in that quadrant if the posterior pigmented trabecular meshwork could not be seen in the primary position without indentation (Modified Shaffer grade 0 to 2). The eye was classified as having an occludable angle if there were 2 or more closed quadrants (≥180 degrees). | ||
| Flow and timing | There were 152 participants, 1 person had a poor‐quality scan, and in 11 people the scleral spur could not be identified, leaving 140 eyes for the final analysis. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Participants who had LPI were not excluded in the recruitment phase. Conflict of interest: authors reported no conflict of interest. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Campbell 2015.
| Study characteristics | |||
| Patient Sampling | Cohort study. Participants aged ≥ 40 years or older with glaucoma or suspect glaucoma were recruited from two community optometry practices. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 80 eyes (12 narrow angle and 68 open angle). Age: mean (SD) 58.9 ± 10.0, range 40‐80 years. Sex: 53 (66%) female. Setting: primary care. Country: UK. Ethnicity: 70 (87.5%) Caucasian, 6 (7.5%) African, 4 (5%) Indian. Exclusions: corneal disorders, recent eye infection, ocular inflammation (within the previous 6 months), previous refractive surgery, peripheral iridotomy or intra‐ocular surgery. |
||
| Index tests |
LACD: original van Herick grading scheme used (grade 1‐4) performed at the nasal and temporal angle. Grade 1 was used as the cut ‐off (< 25%) at either the nasal or the temporal angle. AS‐OCT: spectral domain, Topcon OCT‐2000 (Topcon Europe Medical B.V). Laser wavelength of 840 nm using anterior segment mode via a 3 mm line scan size with the scan count at 32. If any iris contact was visible anterior to the position of the scleral spur for either the nasal or temporal image or both, this was qualitatively classified as 'occludable'. |
||
| Target condition and reference standard(s) | If posterior trabecular meshwork was not visible for ≥ 90 degrees using, or in other words, if one or more quadrants was graded 0–1 on the Shaffer grading scheme. | ||
| Flow and timing | 84 participants were recruited and 83 participants. 4 participants were excluded as they were unable to tolerate gonioscopy, 80 eyes were included in the final analysis for LACD. In 4 cases, the AS‐OCT images were un‐gradable and 76 eyes were analysed for AS‐OCT. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflicts of interest: authors reported no conflict of interest. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | No | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | No | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | High risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Chang 2011.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. Asymptomatic participants aged over 50 years were identified by systematic sampling from a community polyclinic, completing a comprehensive ophthalmic examination at the same visit between December 2005 and June 2006. Data from the right eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 2047 eyes (395 narrow angle and 1652 open angle). Age: mean (SD), 63.2 ± 8.0 years, (narrow angle 65.1 ± 7.8; controls 62.7 ± 8.0). Sex: 1077 (52.6%) female. Setting: community. Country: Singapore. Ethnicity: Chinese. Exclusions: patients with glaucoma, intraocular surgery or corneal disorders preventing anterior‐chamber imaging. |
||
| Index tests |
SPAC: measurements ranged from 1 to 12. Cut‐off values used were a numerical value of 4 and ≤ 5. AS‐OCT: time domain, Visante, Carl Zeiss Meditec AG. Scans were centred on the pupil and taken along the horizontal (nasal‐temporal) and vertical meridians (superior‐inferior) to the peripheral angle. A quadrant was classified as closed when the iris was in contact with the angle wall. Cut‐off values; qualitative; when two or more quadrants were observed as closed, quantitative cut‐offs were derived from the study data using AOD750. |
||
| Target condition and reference standard(s) | An eye was defined as occludable if it had a Shaffer score of 0 or 1 on non‐indentation gonioscopy for at least two quadrants (≥180 degrees), with or without PAS. | ||
| Flow and timing | There were 2102 participants, 55 could not complete all the tests and were excluded from the analysis due to: alignment errors (12), inability to follow instructions (16), refused gonioscopy (4) or other reasons (18), 2047 eyes were included in the final analysis. There was quantitative AS‐OCT data missing from 579 of the eyes analysed and SPAC data were not available on 41 eyes. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: KK has a Japanese patent on the SPAC (Japanese patent no. 3878164). TA has received funding, travel support and honoraria from Carl Zeiss Meditec. DSF has received an instrument loan from Carl Zeiss Meditec. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Choudhari 2019a.
| Study characteristics | |||
| Patient Sampling | Cohort study. Phakic participants aged 40 years or older were recruited from an eye hospital between October and December 2017. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 111 eyes (69 narrow angle and 42 open angle). Age: median 62 IQR (53‐67). Sex: 65 (58.5%) female. Setting: secondary care. Country: India. Ethnicity: Indian. Exclusions: abnormalities that would preclude visualisation of the peripheral ACD, aphakia, pseudophakia, optic neuropathy and strabismus or insufficient cooperation. |
||
| Index tests | LACD: original van Herick grading scheme used (grade 1‐4) performed at the temporal angle. Grades 3 (> 25% to ≤ 50%) and Grade 2 and less (≤ 25%) were used as the cut‐offs. | ||
| Target condition and reference standard(s) | Indentation gonioscopy was performed in a dark room. An occludable angle was defined as the posterior trabecular meshwork not visible in 2 or more quadrants (≥ 180 degrees). | ||
| Flow and timing | There were 150 participants recruited; two participants were excluded due to poor clarity of the peripheral cornea and 37 participants did not report for the study procedures. Data from 111 eyes were used in the final analysis. The index test and reference standard were conducted within 1 month of each other. | ||
| Comparative | |||
| Notes | Conflict of interest: no conflict of interest statement provided. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | No | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Choudhari 2019b.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. Phakic participants aged 40 years or older attending a rural eye clinic were examined between June 2001 and January 2003. Data from the right eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 888 eyes (271 narrow angle and 617 open angle). Age: median 50 IQR (45‐60). Sex: 497 (55.9%) female. Setting: community. Country: India. Ethnicity: Indian. Exclusions: abnormalities that would preclude visualisation of the peripheral ACD, aphakia, pseudophakia, manifest strabismus or insufficient co‐operation. |
||
| Index tests | LACD: original van Herick grading scheme used (grade 1‐4) performed at the temporal angle. Grade 2 or less was used as the cut‐off (≤ 25%). | ||
| Target condition and reference standard(s) | Indentation gonioscopy was performed in dim illumination. An occludable angle was defined as the posterior trabecular meshwork not visible in 2 or more quadrants (≥ 180 degrees). | ||
| Flow and timing | There were no participants that were excluded or had uninterpretable results. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: no conflict of interest statement provided. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | No | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | High risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Congdon 1996.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. Participants, aged 40 years and above, were invited for screening. Data from both eyes were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 562 participants. Age: mean (SD) 59.2 ± 11.8 years. Sex: 312 (55.6%) female. Setting: community. Country: Taiwan. Ethnicity: East Asian. Exclusions: none reported. |
||
| Index tests |
LACD: modified van Herick grading method used; Grades 3 or 4 termed ‘deep’, Grade 2 ‘narrow’; Grade 1 ‘critically narrow’. Cut‐off values were < 25% and > 25% to ≤ 50%. Flashlight: oblique handlight illumination using three grades: critically narrow (nasal shadow > 1/2 the distance from limbus to pupillary axis); narrow (1/4 to 1/2); or deep (< 1/4). Cut‐off values used were critically narrow (grade 1) and narrow (grade 2). |
||
| Target condition and reference standard(s) | The ACA was graded by Zeiss 4‐mirror dynamic gonioscopy. If no trabecular meshwork was seen in 1 or more quadrants (≥ 90 degrees), an overall grade of 'narrow' was given. A grade of ‘critically narrow’ was given to eyes that were ‘closed’ in two or more quadrants (≥ 180 degrees). The authors defined PACG as 'one or both eyes graded as narrow or critically narrow by gonioscopy who had one or more of the following: intraocular pressure (IOP) greater than 18 mmHg, a rise in IOP greater than or equal to 8 mmHg on dark‐prone provocative testing, or past acute attack with an iridectomy already performed. The optic disc and visual field could be normal or abnormal.' | ||
| Flow and timing | 562 participants were recruited, 503 participants were included in the analysis for LACD and 352 for the flashlight test. For the flashlight, the numbers were smaller than the LACD as handlight testing of all participants was started one month after the study had begun. The index test and reference standard were conducted on the same occasion. There were no uninterpretable test results or exclusions reported. | ||
| Comparative | |||
| Notes | Conflict of interest: no conflict of interest statement provided. Van Herick Grade 2 is a modified version of the original van Herick grade. For both van Herick and flashlight grade 1 and grade 2 was compared to a critical narrow and narrow angle respectively on gonioscopy. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Unclear | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Dabasia 2015.
| Study characteristics | |||
| Patient Sampling | Case‐control study. Adult participants were recruited from glaucoma and general ophthalmology clinics. Data from the right eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 78 eyes (42 narrow angle and 36 open angle). Age: median 66 IQR (53‐79), range 30‐83 years. Sex: 44 (56.4%) female. Setting: secondary care. Country: UK. Ethnicity: 44 (56%) White, 27 (35%) South Asian. Exclusions: participants receiving systemic or topical medications known to affect the ACA configuration (e.g. miotics), anomalies of the anterior segment that affect ACA configuration. |
||
| Index tests |
LACD: determined at the temporal limbus. Graded as a percentage fraction of adjacent corneal thickness at the temporal limbus: > 100%, 75%, 40%, 25%, 15%, 5%, and 0%, cut‐off values reported ≤ 25%,15%, 5% and 0%. Scheimpflugphotography: Oculus Pentacam (software version 1.19r11). ACA estimates were obtained along the nasal‐temporal meridian using Scheimpflug horizontal image segment. Cut‐off values were derived from the study data for ACA, ACD and ACV. AS‐OCT: time domain, Visante, Carl Zeiss Meditec AG (software version 2.0.1.88). An ‘anterior segment single’ mode using wide‐field scanning optics was used to provide a cross‐section of the nasal and temporal angles in a single, 16 x 6 mm image frame between the 3 and 9 o’clock positions. Optimal cut‐off were defined using the study data for ACA and ACD. |
||
| Target condition and reference standard(s) | An occludable angle was defined as the posterior trabecular meshwork not visible for ≥ 270 degrees on non‐indentation gonioscopy and with the eye in the primary position | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Cut‐off values were obtained by contacting the author for 0%, ≤ 5% and ≤ 15%. Conflict of interest: authors reported no conflict of interest. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | No | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Foster 2000.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. Conducted in two phases, participants aged 40 years and older were selected for examination in 1995 using a combination of multistage, clustered, simple random, and systematic sampling.The second phase was conducted in 1997 in which local government census data were used to select participants aged 40 years and older evenly distributed between each decade age group. Data from both eyes were included in the analysis. | ||
| Patient characteristics and setting | Sample size:1717 participants analysed, a gonioscopically narrow angle was found in at least one eye of 140 participants and an open angle in 1577 participants. 35 eyes were classified as having PAC, and a further 28 as PACG. Age: mean age not reported, range 40‐93 years. Sex: 974 (56.7%) female. Setting: community Country: Mongolia. Ethnicity: not reported. Exclusions: if it was not possible to allocate a LACD grade for either eye. |
||
| Index tests | LACD: determined at the temporal limbus and graded as categories: 0%, 5%, 15%, 25%, 40%, 75% and ≥100%. Cuts off reported for 0%, ≤ 5%, ≤ 15%, ≤ 25% and ≤ 40%. | ||
| Target condition and reference standard(s) | An occludable angle was defined as an angle in which the trabecular meshwork was not seen in ≥270 degrees of the angle circumference by gonioscopy. PAC was diagnosed in participants with an occludable angle and either raised IOP and/or PAS. PACG was diagnosed in cases with an occludable angle combined with glaucomatous optic neuropathy. | ||
| Flow and timing | 1800 participants were recruited. Uninterpretable results were reported for 17 participants for reference standard and 76 for index test. Data from 1717 participants were included in the final analysis. Index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: authors reported no conflict of interest. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | High risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Gracitelli 2014.
| Study characteristics | |||
| Patient Sampling | Cohort study. Participants with glaucoma or who were glaucoma suspects were enrolled when attending an outpatient clinic. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 45 eyes (9 narrow angle and 36 open angle). Age: mean (SD), 47.1 ± 16.4, range 19‐85 years. Sex: 30 (67.7%) female. Setting: secondary care. Country: Brazil. Ethnicity: not reported. Exclusions: conditions precluding clear visualization of the AC (e.g. pterygium, corneal opacity), congenital anterior segment, abnormalities, eyelid alterations, ocular trauma and intraocular surgery (incisional or laser procedures). |
||
| Index tests | Flashlight: A flashlight beam was directed parallel to the iris from the temporal side. Eyes identified as having a narrow anterior chamber were those in which a nasal iris shadow, formed between the limbus and the pupillary edge, was visualised (grade 1). Cut‐off value grade 1 was used for the analysis. | ||
| Target condition and reference standard(s) | Gonioscopy was performed in a dark room. An occludable angle was defined as the posterior trabecular meshwork not visible in 2 or more quadrants without indentation (≥ 180 degrees). | ||
| Flow and timing | Eyes which were excluded or had uninterpretable test results were not reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: authors reported no conflicts of interest. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Unclear risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Grewal 2011.
| Study characteristics | |||
| Patient Sampling | Cohort study. Participants aged 40 years and older were recruited from an ophthalmology clinic. Data from the right eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 265 eyes (28 narrow angle and 237 open angle). Age: mean (SD), 55.3 ± 5.1 years, (narrow angle 56.2 ± 6.5; controls 58.3 ± 5.7). Sex: 136 (51.3%) female. Setting: secondary care. Country: India. Ethnicity: Indian. Exclusions: history of glaucoma, intraocular surgery, laser treatment, penetrating trauma, and corneal disorders that precluded imaging. |
||
| Index tests |
AS‐OCT: spectral domain, RTVue 100 (Optovue Inc., Fremont, CA, USA, software version 4.0). Anterior segment morphology was assessed with the corneal adaptor module long (CAM‐L), using the angle scan protocol, which captured 1 x 1024 A‐scans in the nasal and temporal quadrants. Optimal cut‐off values were derived from the study data at AOD500 and TISA 500. Scheimpflug photography: Pentacam (Oculus, software version 1.11). Optimal cut‐off values were derived from the study data using ACD and ACV. |
||
| Target condition and reference standard(s) | Static gonioscopy, Shaffer grading system was used and an occludable angle was defined as Shaffer grade 1 or less in all four quadrants (360 degrees). | ||
| Flow and timing | 300 participants were recruited; 35 participants were excluded because of an undetectable scleral spur on AS‐OCT. Data from 265 eyes were included in the final analysis. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: the authors declare no conflict of interest. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
He 2007.
| Study characteristics | |||
| Patient Sampling | Case‐control study. Participants aged 50 and older were enrolled from Liwan District, Guangzhou, using cluster‐random sampling. Data from the right eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 295 eyes (186 narrow angle and 109 open angle). Age: mean (SD), 67.8 ± 9.5 years, (narrow angle 70.0 ± 8.7; controls 64.0 ± 9.6). Sex: 186 (63.0%) female. Setting: primary care. Country: China. Ethnicity: Chinese. Exclusions: participants with abnormalities precluding clear visualisation of the anterior chamber (e.g. pterygium, corneal opacity, iris abnormalities) and participants who underwent surgery that changes the configuration of the anterior segment (e.g. cataract, glaucoma, LPI). |
||
| Index tests | Flashlight: flashlight beam was set parallel to the iris plane from the temporal side. Grading was in reference to the area occupied by the iris shadow on the nasal iris between the limbus and the pupil margin, as follows: shallow, iris shadow reaching the pupil margin;medium, iris shadow reaching middle of the nasal iris; deep, almost no shadow. The cut‐off value of 'shallow' was used (Grade 1). | ||
| Target condition and reference standard(s) | An occludable angle was defined as posterior and usually pigmented trabecular meshwork was not visible in two or more quadrants (≥ 180 degrees) using static gonioscopy. | ||
| Flow and timing | 602 participants entered the study, excluded cases were eyes with aphakia/pseudophakia (44) and angle closure suspects (236) for the right eye, presence of pterygium and cornea abnormalities (22) and gonioscopy data missing (5). 295 eyes were included in the final analysis. There were no uninterpretable results reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: authors reported no conflict of interest. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Hong 2009.
| Study characteristics | |||
| Patient Sampling | Case‐control study. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 73 eyes (41 narrow angle and 32 open angle). Age: mean (SD), 65.2 ± 10.0 years, (narrow angle 67.5 ± 8.0; controls 62.2 ± 11.5). Sex: 50 (68.5%) female. Setting: secondary care. Country: South Korea. Ethnicity: Korean. Exclusions: history of previous ocular trauma or intraocular disease/surgery. |
||
| Index tests |
AS‐OCT: slit‐lamp OCT, Heidelberg Engineering,GmbH, Germany. Angle images were captured using the horizontal linear scan protocol (from 3‐o’clock to 9‐o’clock direction). ACA was measured automatically by the angle at ARA500. Scheimpflug photography: Oculus Inc., Wetzlar, Germany. Angle images were captured using the horizontal linear scan protocol (from 3‐o’clock to 9‐o’clock direction). Optimal cut‐off values were derived from the study data for both index tests for ACA and ACD. |
||
| Target condition and reference standard(s) | An occludable angle was defined as an angle where the trabecular meshwork could not be seen ≥ 270 degrees of the angle circumference by static gonioscopy. | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: authors reported no conflict of interest. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Johnson 2018.
| Study characteristics | |||
| Patient Sampling | Cohort study. Participants aged 50 years or older were selected by inspection of clinical data from visits to the glaucoma clinic between November 2015 and November 2017. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 131 eyes (19 narrow angle and 112 open angle). Age: mean (SD), 62.0 ± 8.7 years. Sex: 58 (44.3%) female. Setting: secondary care. Country: USA. Ethnicity: 110 (84.0%) Black, 8 (6.1%) White (non‐Hispanic), 6 (4.6%) Hispanic (7.1%), 5 (3.8%) Asian, 2 (1.5%) Middle Eastern. Exclusions: pseudophakia, aphakia, previous glaucoma surgery, previous iridotomy or iridectomy, anterior segment dysgenesis, phthisis bulbi and corneal opacities. |
||
| Index tests | LACD: original van Herick grading scheme used (grade 1‐4) performed at the temporal angle. Grade 2 and less was used as the cut‐off (≤ 25%). | ||
| Target condition and reference standard(s) | Static gonioscopy, an angle was defined as occludable when the posterior trabecular meshwork was not visible in 2 or more quadrants (≥ 180 degrees) in dim illumination. | ||
| Flow and timing | 131 participants recruited and there were 2 participants who were excluded from the analysis, reason was not reported. Data from 129 eyes were included in the analysis. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: authors reported no conflict of interest. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | No | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Khor 2010.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. Participants aged 50 years or older were recruited from a non‐ophthalmic community clinic. Data from the right eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 1853 eyes (380 narrow angle and 1473 open angle). Age: mean (SD), 63.4±8.1, range 50‐93 years. Sex: 1103 (52.4%), female. Setting: community. Country: Singapore. Ethnicity: 1883 (89.5%) Chinese, 44 (2.1%) Malay, 154 (7.3%) Indian and 23 (1.1%) other. Exclusions: history of intraocular surgery or penetrating trauma, previous anterior segment laser treatment, or a history of glaucoma. |
||
| Index tests | AS‐OCT: time‐domain, Visante, Carl Zeiss Meditec, Dublin, CA. All four quadrants were examined. A subjective cut‐off was used whereby an occludable was defined by contact between the iris and angle wall anterior to the scleral spur in any quadrant. | ||
| Target condition and reference standard(s) | Static gonioscopy; an occludable angle was defined as the posterior trabecular meshwork not being seen in the primary position without indentation (Scheie grade 3 or 4) in one or more quadrants (≥ 180 degrees). | ||
| Flow and timing | There were 2104 participants originally studied; 251 (11.9%) eyes were uninterpretable as at least one of the quadrants could not be classified due to poor image quality on the AS‐OCT images. Data from 1853 eyes were included in the final analysis.The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: Carl Zeiss Meditec loaned the AS‐OCT for the study. Dr Aung has received financial support and honoraria for travel to conferences from Carl Zeiss Meditec. Patient characteristics: reported ethnicity and gender demographics was based on original 2104 participants recruited. Data reported compared a range of closed angles observed on gonioscopy and AS‐OCT. Data extracted for the review; occludable angle defined on gonioscopy at >= 90 degrees and a closed angle observed on AS‐OCT in one quadrant or more. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Kim 2014.
| Study characteristics | |||
| Patient Sampling | Case‐control study. Study participants were identified by retrospective medical review and then examined between January 2010 and August 2013 in glaucoma and cataract clinics. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 202 eyes, (101 narrow angle and 101 open angle). Age: mean (SD), 64.5 ± 6.2 years. Sex: 110 (54.4%) female. Setting: secondary care. Country: Korea. Ethnicity: Korean. Exclusions: prior intraocular surgery or if AS‐OCT images were of poor quality. |
||
| Index tests | AS‐OCT: time domain, Visante, Carl Zeiss Meditec, Dublin, CA. Mode to capture; one cross‐sectional horizontal scan. Cut‐off values were derived from the study data at examining lens vault and ACD. | ||
| Target condition and reference standard(s) | Static gonioscopy; an occludable angle was defined when the pigmented posterior trabecular meshwork was not visible for 180 degrees or more in the primary position, with PAS and/or raised IOP. | ||
| Flow and timing | There were 124 narrow angles and 112 age‐matched controls. Of the 112 control participants matched, 11 had low‐quality images consequently data from 11 control participants were eliminated. Data from 202 eyes were included in the final analysis. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: authors reported no conflict of interest. All cases had an LPI. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Ko 2015.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. Participants were recruited from participants of the first Shihpai Eye Study visit in 1999 (a community‐based,cross‐sectional survey of vision and eye diseases aged 65 years and older). Only one eye of each participant was included in the analysis. | ||
| Patient characteristics and setting | Sample size: 374 eyes (199 narrow angle and 175 open angle). Age: mean (SD), 77.4 ± 3.8 years, (narrow angle 77.6 ± 4.1; controls 77.2 ± 3.5). Sex: 122 (32.6%) female. Setting: community. Country: Taiwan. Ethnicity: Chinese. Exclusions: participants with secondary angle‐closure, non‐glaucomatous visual field defects or if the eye was was pseudophakic. |
||
| Index tests | LACD: modified van Herick grading: Grade 0 (Iridocorneal contact), Grade 1 (≤1/4), Grade 2 (> 1/4 to ≤ 1/2), Grade 3 (> 1/2 to ≤ 3/4), Grade 4 (> 3/4 but ≤ 3/4) corneal thickness and Grade 5 (> corneal thickness). Cut‐off value of > 25% to ≤ 50% was used. | ||
| Target condition and reference standard(s) | An occludable angle was defined as an angle in which the trabecular meshwork was not seen in ≥ 270 degrees of the angle circumference by gonioscopy. PAC was diagnosed in participants with an occludable angle and either raised IOP and/or PAS. PACG was diagnosed in cases with an occludable angle combined with glaucomatous optic neuropathy. | ||
| Flow and timing | 460 participants were initially recruited, 86 excluded due to: gonioscopy not performed (15), exclusion criteria not met (62), bilateral pseudophakia (3), pseudophakic PACG (6), LPI. There were 374 eyes included in the final analysis. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflicts of interest: authors reported no conflict of interest. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | No | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | High risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Kurita 2009.
| Study characteristics | |||
| Patient Sampling | Cohort study. Participants were referred and consecutively recruited for a detailed examination of the ACA with gonioscopy to confirm a diagnosis between April 1, 2006 and September 31, 2006. Data from both eyes were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 39 participants (72 eyes), a gonioscopically narrow angle was found in 42 eyes in participants with either PACS or PAC, 16 eyes of 9 patients with open angle glaucoma and 14 open angle eyes in normal eyes. Age: mean (SD), 58.4 ± 15.3, range 27‐83 years. Sex: not reported. Setting: secondary care. Country: Tokyo, Japan. Ethnicity: Japanese. Exclusions: pathological changes or history of diseases in the cornea, anterior chamber, iris, or ocular tissues which would affect ACA, history of acute PAC in either eye, history of ocular surgery that would affect anterior chamber or evidence of broad PAS on gonioscopy. |
||
| Index tests | Scheimpflug photography: Pentacam, Oculus Inc, Wetzlar, Germany, cut‐off value was derived from the study data for ACD. | ||
| Target condition and reference standard(s) | Using gonioscopy, an eye having an ACA width of Shaffer’s Grade 2 or less in 3 or more quadrants (≥ 270 degrees) was considered to be occludable. | ||
| Flow and timing | 47 participants (83 eyes) entered the study, four eyes with broad PAS, 3 eyes with nodules in the ACA, 2 eyes with suspected ACA recession suggesting a history of ocular injury, and 2 eyes with significant ocular nystagmus were excluded, 72 eyes were included in the final analysis. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: authors reported no conflict of interest. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Lavanya 2008.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. Participants aged 50 years or older were recruited from a community polyclinic, they were systematically sampled (every fifth patient registered at the polyclinic) and examined between December of 2005 to June of 2006. Data from both eyes were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 2052 participants (422 participants had a narrow angle in at least 1 eye and 1630 participants with an open angle in both eyes). Age: mean (SD), 63.3 ± 8.0 years, (narrow angle 65.5 ± 8.2; controls 62.8 ± 7.9). Sex: 1085 (52.9%) female. Setting: primary care. Country: Singapore. Ethnicity: 1840 (89.7%) Chinese, 43 Malay (2.1%), 146 Indian (7.1%), others (1.1%). Exclusions: history of glaucoma, previous intraocular surgery or penetrating eye injury, and corneal disorders, such as corneal endothelial dystrophy, corneal opacity, or pterygium, preventing ACD measurement. |
||
| Index tests |
SPAC: Cut‐off values used were a numerical grade of ≤ 5, P or S, combination of grade ≤ 5 and/or S or P. AS‐OCT: time domain, Visante, Carl Zeiss Meditec, Dublin, CA, Scans were centered on the pupil and taken along the horizontal (nasal‐temporal angles at 0–180 degrees) and vertical meridians (superior–inferior angles 90–270 degrees). Subjective judgement was used to defined an occludable angle as contact between the iris and any part of angle wall anterior to the scleral spur in ≥ 2 quadrants. |
||
| Target condition and reference standard(s) | An eye was defined as having an occludable angle by gonioscopy, if the posterior pigmented trabecular meshwork was not visible on non‐indentation gonioscopy for ≥ 180 degrees, with or without PAS. | ||
| Flow and timing | There were 2114 participants originally studied, Twelve participants were ineligible because they were pseudophakic in both eyes or were known to have glaucoma, 50 participants could not complete the tests for various reasons: alignment errors (12), inability to follow instructions (16) or focus on the fixation light (4), refused gonioscopy (4) or other reasons (14). Data from 2052 participants were included in the final analysis. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: Dr Kashiwagi has a Japanese patent on the SPAC (Japanese patent No. 3878164). Dr Friedman has been a paid consultant to Carl Zeiss‐Meditec.Dr Foster has received honoraria and travel support from Carl Zeiss Meditec. Dr Aung has received research funding and travel support from Carl Zeiss Meditec. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Li 2019.
| Study characteristics | |||
| Patient Sampling | Case‐control study. Participants aged 18 years and older were recruited. Data from both eyes were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 161 participants, 177 eyes (117 narrow angle and 60 open angle). Age: mean (SD), 57.7 ± 13.3 years, (narrow angle 61.8 ± 9.1 years; controls 49.6 ± 16.3). Sex: 97 (54.8%) female. Setting: secondary care. Country: China. Ethnicity: Chinese. Exclusions: secondary angle closure, history of incisional or laser ocular surgery, history of acute angle closure crisis, high myopia (> 6DS) and presence of other ocular co‐morbidities. |
||
| Index tests | AS‐OCT: swept source CASIA I (Tomey Corporation, Nagoya, Japan). For 3D image reconstruction, a series of 128 radial B‐scans across the anterior chamber were taken. Cut‐off values were derived from the study data for AOD500, AOD750, TISA500, TISA750, ACD and ACV. | ||
| Target condition and reference standard(s) | Static gonioscopy: a participant’s eye was considered to be occludable when the posterior pigmented trabecular meshwork was not visible in 2 or more quadrants (≥180 degrees) in the primary position. | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. It was not reported if the index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: authors reported no conflict of interest. Note: The control group consisted of those with primary open angle glaucoma, ocular hypertension and normal eyes. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | No | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Melese 2016.
| Study characteristics | |||
| Patient Sampling | Case‐control study. Participants were recruited across 3 sites. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 189 participants recruited, however 69 eyes were used for analysis (31 narrow angle and 38 open angle). Age: mean (SD), 54.0 ± 14.1 years, (narrow angle 60.9 ± 9.2; controls 49.1 ± 14.9) of the 189 participants reported. Sex: 132 (70%) female. Setting: secondary care. Country: USA. Ethnicity: 94 (50%) Caucasian, 44 (23%) African origin, 27 (14%) Hispanic, and 24 (13%) Asian. Exclusions: anterior segment abnormalities that could affect the angle parameters, such as significant corneal opacity, lid obstruction or eye movement artefact that could not properly be imaged, medication that may have affected angle anatomy within a month before imaging. |
||
| Index tests | AS‐OCT: swept source CASIA SS‐1000 (Tomey Corporation, Nagoya, Japan). For 3D image reconstruction, the CASIA SS‐1000 obtains a series of 128 cross‐sectional images (512 A‐scans each) across the whole anterior chamber. Cut‐off values were derived from the study data for AOD500, AOD 750, TISA500, TISA750. | ||
| Target condition and reference standard(s) | Using the Spaeth grading system on gonioscopy, eyes were graded as narrow (A or B) based on the deepest structure visible in one quadrant (90 degrees). For angles graded as C where the scleral spur was partially visualized, the classification as occludable or open was based on the clinical decision of whether treatment was required. | ||
| Flow and timing | There were 189 participants recruited, 120 eyes were used for training, therefore 69 eyes were analysed for the study. Eyes which were excluded or had uninterpretable test results were not reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Demographics reported on whole set but not separately for the test set. Open angle eyes included normals, suspect and confirmed primary open angle glaucoma. Conflict of interest: reported financial disclosures considered not to raise any conflict of interest for the study. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Mosler 2015.
| Study characteristics | |||
| Patient Sampling | Cohort study. All patients were recruited following glaucoma consultation at the University Eye Clinic. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 90 eyes (14 narrow angle and 76 open angle). Age: mean (SD), 66.3 (SD not reported). Sex: 52 (57.8%) female. Setting: secondary care. Country: Germany. Ethnicity: Caucasian. Exclusions: medicinal mydrasis, poor image quality and lack of clinical documentation. |
||
| Index tests | AS‐OCT: time domain, Visante, Carl Zeiss Meditec, Dublin, CA, Scans were taken along the horizontal meridians.The cut‐off was an ACA ≤ 20 degrees. | ||
| Target condition and reference standard(s) | Gonioscopy using the Shaffer classification, where an eye with a chamber angle below 20 degrees was considered as occludable in one quadrant (90 degrees). | ||
| Flow and timing | There were 104 participants originally studied, 14 patients were excluded from the evaluation due to poor image quality (5) or lack of documentation of clinical parameters (9). Data from 90 eyes were included in the final analysis. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: authors reported no conflict of interest. It was not reported whether the nasal or temporal quadrant was analysed. All the recruited participants had glaucoma. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | No | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Muto 2019.
| Study characteristics | |||
| Patient Sampling | Case‐control study. Participants with newly diagnosed acute primary angle closure (APAC), PACS and normal age‐matched controls were recruited between January 2010 and July 2017. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 506 eyes (48 narrow angle and 458 open angle). Age: mean (SD), 74.0 ± 7.0 years, (narrow angle 74.1 ± 7.7 years; controls 73.6 ± 6.9). Sex: 280 (55.3%) female. Setting: secondary care. Country: Japan. Ethnicity: Japanese. Exclusions: pseudophakia, previous iridotomy or iridectomy, or those with bilateral acute primary angle closure. |
||
| Index tests | Scheimpflug photography: Oculus Pentacam HR, optimal cut‐off's were derived from the study data for the following parameters; ACA, ACD (central and peripheral) and ACV. | ||
| Target condition and reference standard(s) | Gonioscopy, an occludable angle was defined as having appositional contact between the peripheral iris and the posterior trabecular meshwork in 3 or more quadrants (≥ 270 degrees). | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: authors reported no conflict of interest. Diagnostic thresholds for males and females were reported separately for all the parameters. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Narayanaswamy 2010.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. Participants aged 50 years or older were recruited from a community polyclinic, they were systematically sampled (every fifth patient registered at the polyclinic) and examined from December of 2005 to June of 2006. Data from both eyes were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 1465 participants (315 participants had at least 1 eye with a narrow angle and 1150 participants had an open angle in both eyes). Age: mean (SD), 62.7±7.7, range 50‐93 years. Sex: 793 (54.1%) female. Setting: community. Country: Singapore. Ethnicity: 1318 (90.0%) Chinese, 27 (1.8%) Malay, 102 (7.0%), Indian and 8 (1.2%) others. Exclusions: history of intraocular surgery, evidence of aphakia/pseudophakia, or penetrating trauma in the eye; previous anterior segment laser treatment; history of glaucoma; or corneal disorders such as corneal endothelial dystrophy, corneal opacity, or pterygium. |
||
| Index tests | AS‐OCT: time domain, Visante; Carl Zeiss Meditec Inc. Single‐scan‐mode protocol: one image scanning the angle at the 3‐ and 9‐o’clock positions followed by one scanning the superior angle at 12 o’clock and one scanning the inferior angle at 6 o’clock. Cut‐off values were derived from the study data for AOD500, AOD750, TISA500, TISA750 and ARA750. | ||
| Target condition and reference standard(s) | An eye was defined as having an occludable angle if the posterior pigmented trabecular meshwork was not visible for at least 180 degrees on non‐indentation gonioscopy with the eye in the primary position. | ||
| Flow and timing | There were 2047 participants originally studied, 582 were excluded due to; inability to locate the scleral spur (515), poor image quality (28), or software delineation errors (39). Data from 1465 participants were included in the final analysis. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: Dr Friedman reports having been as a paid consultant to Carl Zeiss Meditec Inc, Dr Foster reports receiving honoraria and travel support from Carl Zeiss Meditec Inc, and Dr Aung reports receiving research funding, honoraria, and travel support from Carl Zeiss Meditec Inc. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Nolan 2006.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. Participants recruited from the electoral register of Tanjong Pagar district residing in 50 area clusters, using a disproportionate, stratified, clustered, random sampling procedure. Data from the right eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 1090 eyes (71 narrow angle and 1019 open angle). Age: Mean not reported, range 40‐81 years. Sex: 593 (54.4%) female. Setting: community. Country: Singapore. Ethnicity: Chinese. Exclusions: none reported. |
||
| Index tests | LACD: at the temporal limbus and graded as percentage categories: 0%, 5%, 15%, 25%, 40%, 75% and ≥100%. Cut‐off values used were 0%, ≤ 5%, ≤ 15% and ≤ 25%. | ||
| Target condition and reference standard(s) | An eye was classified as occludable on gonioscopy if the posterior (usually pigmented) trabecular meshwork was not visible for at least 270 degrees of the angle circumference. | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: authors reported no conflicts of interest. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | No | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | High risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Nolan 2007.
| Study characteristics | |||
| Patient Sampling | Case‐control study. Participants 40 years old or older were recruited from glaucoma clinics at an eye hospital. Both eyes were used in the analysis. | ||
| Patient characteristics and setting | Sample size: 200 participants (99 participants had at least 1 eye with a narrow angle and 101 participants had an open angle in both eyes). Age: median age 62.5, range 40‐86 years. Sex: 123 (60.6%) female. Setting: secondary care. Country: Singapore. Ethnicity: 174 (85.7%) Chinese, 9 (4.4%) Malay, 12 (5.9%) Indian and 8 (3.9%) were of other ethnic origins. Exclusions: eyes of patients with pseudophakia or had previous glaucoma surgery. |
||
| Index tests | AS‐OCT: prototype AS‐OCT (Carl Zeiss Meditec, Dublin, CA). Images of the temporal, inferior, and nasal quadrants were analysed qualitatively. Subjective judgment was used to define an occludable angle on AS‐OCT based on contact between the peripheral iris and any part of the angle wall anterior to the scleral spur in one or more quadrants. | ||
| Target condition and reference standard(s) | An occludable angle was defined when the iris was in contact with the posterior (usually pigmented) trabecular meshwork (Spaeth grade, 0 degrees) in at least 1 quadrant (≥ 90 degrees) using gonioscopy. | ||
| Flow and timing | 203 participants were recruited. In 3 participants, it was not possible to obtain either gonioscopic grading or AS‐OCT images. Data from 200 participants were included in the final analysis. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: technical support and loan of AS‐OCT from Carl Zeiss Meditec, Dublin, California. Demographics: ethnicity and age were reported from the original 203 participants entering the study, open angle cohort included normals and those with primary open angle glaucoma. Study participants included patients who had undergone peripheral iridotomy. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Nongpiur 2011.
| Study characteristics | |||
| Patient Sampling | Case‐control study. Angle closure participants were recruited were those attending a glaucoma clinic and control participants were recruited from an ongoing population‐based study. Data from the right eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 278 eyes (102 narrow angle and 176 open angle). Age: mean (SD), 58.3 ± 9.9 years, (65.3 ± 9.1; controls 54.2 ± 7.9). Sex: 150 (54.0%) female. Setting: secondary care. Country: Singapore. Ethnicity: Chinese. Exclusions: secondary angle closure, corneal abnormalities that would affect imaging, laser iridoplasty or an history of intraocular surgery history. Controls; family history of glaucoma. |
||
| Index tests | AS‐OCT: time domain, Visante, Carl Zeiss Meditec, Dublin, CA, Scans were centered on the pupil and were obtained along the horizontal axis ( 0°–180°) using the standard anterior segment single‐scan protocol. The optimal threshold was derived from the study data examining lens vault. | ||
| Target condition and reference standard(s) | An occludable angle was defined when there was appositional angle closure for 180 degrees or more with PAS on gonioscopy, raised IOP, or both, but with or without glaucomatous optic neuropathy. Those with previous acute primary angle closure were defined as the presence of at least 2 of the following symptoms: ocular or periocular pain, nausea or vomiting or both, and an antecedent history of intermittent blurring of vision with haloes; a presenting IOP of more than 28 mmHg on Goldmann applanation tonometry; and the presence of at least 3 of the following signs: conjunctival injection, corneal epithelial oedema, mid‐dilated un‐reactive pupil, and shallow anterior chamber. | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported.The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | All cases diagnosed with angle closure previously had LPI. Conflict of interest: Tin Aung and Tien Yin Wong received financial Support from Carl Zeiss Meditec. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Okabe 1991.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. Recruited from a glaucoma screening programme in the Gifu prefecture, Japan. Participants were selected randomly between 1988‐1989. Data from both eyes were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 585 participants (1169 eyes; 94 narrow angle and 1075 open angle). Age: mean, male 59.1; female 58.4 years. SD was not reported. Sex: 380 (65.0%) female. Setting: community. Country: Japan. Ethnicity: Japanese. Exclusions: history of glaucoma or trauma and ophthalmic diseases that could influence the angle. |
||
| Index tests | LACD: original van Herick grading used with a cut‐off value of ≤ 25%. | ||
| Target condition and reference standard(s) | An occludable angle was defined on gonioscopy as the mean grade from all four quadrants ≤ 2 using the Shaffer grading system. | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. Not reported when the reference test was conducted with respect to the the index test. | ||
| Comparative | |||
| Notes | Conflict of interest: no conflict of interest statement provided. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Park 2011.
| Study characteristics | |||
| Patient Sampling | Cohort study. Recruited from a glaucoma service from May 2008 to January 2009. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 148 eyes (93 narrow angle and 55 open angle). Age: mean (SD), 65.1 ± 12.0 years, (narrow angle 66.0 ± 10.1; controls 63.5 ± 14.6). Sex: 72 (48.6%) female. Setting: secondary care. Country: Republic of Korea. Ethnicity: not reported. Exclusions: ages of under 40 or over 80 years, refractive errors > 3.00DS, pseudophakia/aphakia, corneal disorders, a history of glaucoma, previous intraocular surgery or penetrating eye injury. Plateau iris configuration and eyes with PAS were also excluded. |
||
| Index tests |
LACD: determined at the nasal and temporal limbus. Original van Herick grading (Grade 1‐4). Grade 0 was defined as no space visible between the corneal slit image and the slit image on the iris. A cut‐off value of < 25% was used at the temporal limbus. AS‐OCT: time domain, Visante, Carl Zeiss Meditec, Dublin, CA. Enhanced anterior segment single’’ protocol (scan length 16 mm; 256 A‐scans, with only only nasal and temporal angle images obtained. Angle closure was defined by subjective judgement as contact between the peripheral iris and the angle wall anterior to the scleral spur at the temporal angle image. |
||
| Target condition and reference standard(s) | Gonioscopy, an occludable angle was determined when the posterior pigmented trabecular meshwork was not visible on non‐indentation gonioscopy for at ≥ 60 degrees (two‐thirds of quadrant) both with and without PAS at either the nasal or temporal quadrant. | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: no conflict of interest statement provided. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | No | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Porporato 2019.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. Participants aged 50 years and older were recruited from a community polyclinic providing primary healthcare services from June to September 2013. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 1857 eyes (139 narrow angle and 1718 open angle). Age: mean (SD), 61.8 ± 6.7 years. Sex: 1179 (63.5%) female. Setting: primary care. Country: Singapore. Ethnicity: 1621 (87.3%) Chinese. Exclusions: no previous glaucoma, laser treatment, intraocular surgery, ocular trauma or poor quality scans. |
||
| Index tests | AS‐OCT: swept source CASIA SS‐1000 (Tomey Corporation, Nagoya, Japan). For 3D image reconstruction, the CASIA SS‐1000 obtains a series of 128 meridional scans, each consisting of 512 A‐scans across the across the anterior chamber. The quantitative cut‐off values used were the inbuilt ITC indices. Subjective grading; an occludable angle on AS‐OCT was defined as contact between the iris and any part of angle wall anterior to the scleral spur in 50% of more in 1 quadrant (45 degrees). | ||
| Target condition and reference standard(s) | Static gonioscopy, an occludable angle was classified where the posterior pigmented trabecular meshwork could not be seen in the primary position in 2 or more (≥180 degrees) quadrants. | ||
| Flow and timing | There were 2038 participants originally studied. 181 participants were excluded where the SS‐OCT images were of poor quality in more than 5 consecutive scans (170) or gonioscopy was refused or had difficulties in performing the reference test (11). Data from 1857 eyes were included in the final analysis. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: Tin Aung has received grant support and honoraria, and is a consultant for Alcon, Novartis, Santen and Allergan. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Radhakrishnan 2005.
| Study characteristics | |||
| Patient Sampling | Case‐control study. Participants were recruited from an secondary care setting. Data from both eyes were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 24 participants, 31 eyes (8 eyes narrow angle and 23 open angle). Age: mean (SD), 42.9 years, SD not reported. Sex: 15 (62.5%) female. Setting: secondary care. Country: USA. Ethnicity: 14 (58.3%) Caucasian. Exclusions: not reported. |
||
| Index tests | AS‐OCT: prototype AS‐OCT (Carl Zeiss Meditec, Dublin, CA). Temporal and nasal AC angles were recorded in lateral gaze. Optimal thresholds were derived from study data on AOD 500, ARA 500, ARA 750, TISA 500 AND TISA 750. | ||
| Target condition and reference standard(s) | An occludable angle was defined as Shaffer grade 1 or lower in all quadrants (360 degrees) on gonioscopy. | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | The number of the reported ethnicity of participants do not match the number analysed. Conflict of interest: Dr Huang has provided research support to Carl Zeiss Meditec Inc, Dublin, Calif, and has received a patent royalty for optical coherence tomography. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Rossi 2012.
| Study characteristics | |||
| Patient Sampling | Case‐control study. Cases 40 years and older, controls 18 years and older were both recruited from an ophthalmology clinic. Data from both eyes were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 34 participants, 64 eyes (28 narrow angle and 36 open angle). Age: mean (SD), 66.7 ± 10.5 years, (66.1 ± 13.2; controls 66.2 ± 7.9). Sex: 23 (67.7%) female. Setting: secondary care. Country: Italy. Ethnicity: Caucasian. Exclusions: no previous laser treatment, no previous filtering surgery or other ocular surgery. |
||
| Index tests | Scheimpflug photography: Oculus Pentacam HR, optimal cut‐off's were derived from the study data for the following parameters; ACD and ACV. | ||
| Target condition and reference standard(s) | An occludable angle was defined by the presence of Shaffer grade 0‐1 in at least 2 quadrants (≥ 180 degrees) on gonioscopy and no evidence of glaucomatous optic neuropathy or visual field defect. | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported.The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: authors reported no conflict of interest. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Sakata 2010.
| Study characteristics | |||
| Patient Sampling | Cohort study. Participants were recruited from a glaucoma clinic from January to June 2007. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 101 participants (30 narrow angle and 71 open angle). Age: mean (SD), 62.4 ± 9.6, range 41‐89 years. Sex: 57 (58%) female. Setting: secondary care. Country: Singapore. Ethnicity: 88 (87%) Chinese, 2 Malay (2%), 7 Indian (7%), 4 others (4%). Exclusions: history of previous intraocular surgery or penetrating trauma, or any cornea opacities or abnormalities that precluded AS‐OCT imaging. |
||
| Index tests |
AS‐OCT: time domain,Visante; (model 1000,software version 1.0, Carl Zeiss Meditec). AS‐OCT: time domain, slit‐lamp OCT device (software version 1.1, Heildelberg Engineering). Scans for both devices examined the ACA of each eye were obtained at the 3 and 9 o’ clock positions (horizontal), and at the 6 and 12 o’clock positions (vertical). ACA was considered ‘closed’ on both devices if there was any contact between the iris and angle wall anterior to the scleral spur in at least two quadrants. |
||
| Target condition and reference standard(s) | An angle was defined as occludable when the posterior trabecular meshwork could not be seen in the primary position without indentation (Scheie grade 3 or 4) in 180 degrees or more using gonioscopy. | ||
| Flow and timing | There were 101 participants originally studied, there were 18 participants excluded where ACA could not be assessed in four quadrants with both AS‐OCT devices. Gonioscopy results were not reported for 3 particpants and data from 80 eyes where used in the final analysis. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | All cases diagnosed with angle closure previously had LPI. Demographics reported are of those recruited and not number analysed. Conflict of interest: Carl Zeiss Meditec and Heidelberg Engineering loaned the respective AS‐OCTs. Dr Aung has received research support and honoraria for travel to conferences from Carl Zeiss Meditec. Dr Wong has received financial support and honoraria for travel to conferences from Carl Zeiss Meditec and Heidelberg Engineering. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Tan 2012.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. Participants aged 50 years and older were recruited from a community polyclinic, they were systematically sampled (every fifth person registered at the polyclinic) and examined between December of 2005 to July of 2006. Data from the right eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 1465 eyes (315 narrow angle and 1150 open angle). Age: mean (SD), 62.7 ± 7.7 years. Sex: 793 (54.1%) female. Setting: community. Country: Singapore. Ethnicity: 1317 (90%) Chinese, 27 Malay (1.8%), 102 Indian (7.0%), others (1.2%). Exclusions: history of glaucoma, previous intraocular surgery or laser treatment, penetrating eye injury or corneal disorders preventing anterior chamber assessment. |
||
| Index tests | AS‐OCT: time domain,Visante, Carl Zeiss Meditec, Dublin, California, USA). Scans were centered on the pupil and taken along the horizontal axis,using the standard anterior segment single‐scan protocol. Optimal thresholds were derived from study's data on ACV. LV and ACA. | ||
| Target condition and reference standard(s) | An occludable angle was defined if the posterior trabecular meshwork was not visible for at least 180 degrees on non‐indentation gonioscopy with the eye in the primary position. | ||
| Flow and timing | There were 2047 participants originally studied, 582 participants were excluded for the following reasons:11 people could not undergo gonioscopy; 62 participants did not complete AS‐OCT examination or had poor quality AS‐OCT images; 42 participants showed software delineation errors; and the scleral spur was not clearly visible on AS‐OCT images in 467 participants. Data from 1465 eyes were used in the final analysis. The index test and reference standard were conducted on the same occasion. |
||
| Comparative | |||
| Notes | Dr Aung has received research support and honoraria for travel to conferences from Carl Zeiss Meditec. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Thomas 1996.
| Study characteristics | |||
| Patient Sampling | Cohort study. Participants were consecutively recruited when they attended an outpatient clinic. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 96 eyes (21 narrow angle and 75 open angle). Age: mean (SD), 45.5 ± 14.9, range 14‐74 years. Sex: 46 (47.9%) female. Setting: secondary care. Country: India. Ethnicity: Indian. Exclusions: acute conditions. |
||
| Index tests |
LACD: original van Herick grading used (grades 1‐ 4). Cut‐off used LACD < 25%. Flashlight: flashlight beam was directed parallel to the iris from the temporal side. The crescent iris shadow thus formed was graded according to the area between the limbus and the pupillary edge that it occupied. Grade 1 was defined as more than half, Grade 2 as half to one‐third; Grade 3 minimal; and Grade 4 as no shadow. Grade 1 and 2 were used as the cut‐offs. |
||
| Target condition and reference standard(s) | Dynamic gonioscopy was performed with the clinician deciding whether the angle was ‘gonioscopically occludable. A Scheie grade 3 or less was considered to be occludable (middle third of the trabecular meshwork visible). | ||
| Flow and timing | 100 participants recruited, 4 participants were excluded as they had acute conditions: phacolytic glaucoma (1), phacomorphic glaucoma (2) and a corneal ulcer (1). There were no uninterpretable test results. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: no conflict of interest statement provided. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | No | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | No | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | No | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | High risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Tun 2017.
| Study characteristics | |||
| Patient Sampling | Cohort study. 202 phakic participants were recruited from a glaucoma clinic. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 202 eyes (50 narrow angle and 152 open angle). Age: mean (SD), 62.3 ± 9.7 years. Sex: 113 (55.9%) female. Setting: secondary care. Country: Singapore. Ethnicity: 170 (84.2%) Chinese. Exclusions: history of intraocular surgery or any corneal abnormalities that would preclude imaging. |
||
| Index tests | AS‐OCT: spectral domain, HD‐OCT Cirrus‐OCT, model 5000; Carl Zeiss Meditec Dublin, California, USA). Subjective judgement was used to defined a closed angle defined as contact between the iris and trabecular meshwork anterior to the scleral spur in that quadrant. If the scleral was not visible but the trabecular meshwork was, any contact between the trabecular meshwork and the iris was also diagnosed as an occludable angle in that quadrant where two or more quadrants were defined as closed. | ||
| Target condition and reference standard(s) | A eye was considered occludable if the posterior trabecular meshwork could not be seen in the primary position without indentation (the Scheie grade 3 or 4) in 2 quadrants (≥ 180 degrees) on gonioscopy. | ||
| Flow and timing | There were 202 participants recruited, and there 10 images excluded from AS‐OCT as the examiner was unable to determinate the trabecular meshwork and scleral spur locations. It is not reported whether participants were from the open or narrow angle group. The index test and reference standard were conducted on the same occasion | ||
| Comparative | |||
| Notes | From the 152 participants with an open angle, 70 participants had primary open angle glaucoma and 64 had no glaucoma. Of the original angle closure eyes, 18 had open angles after LPI and were included also in the open angle group. Dr Aung has received research support and honoraria for travel to conferences from Carl Zeiss Meditec. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Winegarner 2019.
| Study characteristics | |||
| Patient Sampling | Case‐control study. Review of participants with angle closure disease and healthy controls that were examined in a hospital based setting. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 136 eyes (87 narrow angle and 49 open angle). Age: mean (SD), 71.9 ± 8.2 years, range (49‐87). Sex: 84 (61.8%) female. Setting: secondary care. Country: Japan. Ethnicity: Japanese. Exclusions: intraocular diseases, history of intraocular surgery or iridotomy, secondary glaucoma or over the age of 90 years. |
||
| Index tests | Scheimpflug photography: Oculus Pentacam, pre‐specified thresholds (one SD from the mean) were based on the internal normative database for the following parameters; ACA, ACD and ACV. | ||
| Target condition and reference standard(s) | An eye with an occludable angle was defined using gonioscopy, where 3 quadrants (≥ 270 degrees) of the posterior trabecular meshwork could not be seen. | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. It was not reported if the index test and reference standard was conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: Miki A has received funding from pharmaceutical companies. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | No | ||
| Did the study avoid inappropriate exclusions? | No | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Unclear | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Unclear risk | ||
Wirbelauer 2005.
| Study characteristics | |||
| Patient Sampling | Cohort study. Data from both eyes were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 109 participants; (138 eyes, 64 narrow angle and 74 open angle). Age: mean (SD), 66±15 years, range 23‐90 years. Sex: 66 (60.1%) female. Setting: secondary care. Country: Germany. Ethnicity: not reported. Exclusions: not reported. |
||
| Index tests |
LACD: determined at the temporal limbus using the original van Herick grading (grades 1‐4). Cut‐off used LACD ≤ 25%. AS‐OCT 4 Optics AG, Lübeck, Germany. Optimal thresholds were extropolated from the study data for ACA and AOD 500. |
||
| Target condition and reference standard(s) | Gonioscopy; an eye was considered occludable if the ACA was ≤ 20 degrees in the temporal angle (90 degrees). | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: no conflict of interest statement provided. LACD analysis; study compared the temporal LACD to the reference temporal ACA for both eyes. AS‐OCT analysis: study conglomerated both nasal and temporal quadrants for both eyes. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Unclear | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Could the selection of patients have introduced bias? | Unclear risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Unclear | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Unclear risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Wong 2009a.
| Study characteristics | |||
| Patient Sampling | Cohort study. Participants recruited from a glaucoma clinic at a Singapore hospital from January 1 to July 31, 2007. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 188 eyes. Age: mean (SD), 63.3 ± 10.5, range 37‐99 years. Sex: 107 (57.0%) female. Setting: secondary care. Country: Singapore. Ethnicity: 162 (86.2%) Chinese, 8 (4.3% ) Malay, 12 (6.4%) Indian and other 6 (3.2%). Exclusions: participants who had undergone any prior intraocular procedures or had any penetrating eye injuries or corneal disorders, such as corneal endothelial dystrophy, pterygium, or a corneal scar, that may preclude satisfactory imaging. |
||
| Index tests |
SPAC: categorical grades and inbuilt numerical scale ranged from 1 to 12, with 12 representing the deepest ACD. Cut‐off values used: optimal thresholds were derived from study data using either separate or combined categorical and numerical grading. AS‐OCT: slit‐lamp OCT (Heidelberg Engineering, Heidelberg, Germany), image acquisition required imaging of the entire cross‐section of the anterior segment in 1 single‐image frame. Subjective judgement cut‐off: the ACA was considered closed on SL‐OCT imaging if there was contact between the iris and angle wall anterior to the scleral spur in two quadrants or more. |
||
| Target condition and reference standard(s) | Gonioscopy, the eye was considered occludable if the posterior trabecular meshwork could not be seen in the primary position without indentation (Scheie grade 3 or 4) in 2 or more quadrants (≥ 180 degrees). | ||
| Flow and timing | 188 participants recruited, 35 were excluded due to; failure in obtaining SL‐OCT images due to obstructions or motion artefacts (14), SL‐OCT images could not be graded owing to poor definition of the scleral spur (21), leaving 153 for the final analysis. The index test and reference standard were conducted on the same occasion | ||
| Comparative | |||
| Notes | Ethnicity reported on original participants entering the study and not the analysed participants. Defined ACA closure for AS‐OCT and gonioscopy was reported in one or more quadrants, data entry for this review was considered for only 2 quadrants identified as closed for both the reference and index test. Conflict of interest: Dr T. Aung has received grant funding as well as financial support and honoraria for travel to conferences from Carl Zeiss Meditec. Patients who had undergone laser iridotomy were not excluded. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Wong 2009b.
| Study characteristics | |||
| Patient Sampling | Cohort study. Recruited from a glaucoma clinic. Data from one eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 45 eyes (17 narrow angle and 28 open angle). Age: mean (SD), 62.5 ± 9.1 years. Sex: 28 (62.2%) female. Setting: secondary care. Country: Singapore. Ethnicity: 41 (91.1%) Chinese. Exclusions: history of previous intraocular surgery or penetrating trauma or any cornea opacities or abnormalities that precluded angle imaging.. |
||
| Index tests |
AS‐OCT: time domain, Visante; Carl Zeiss Meditec HD‐OCT: spectral domain, Cirrus‐OCT; Carl Zeiss Meditec Dublin, California Subjective cut‐off criteria used for both devices i.e. if there was any contact between the iris and angle wall anterior to the scleral spur in one quadrant. |
||
| Target condition and reference standard(s) | Gonioscopy, an angle was considered occludable if the posterior trabecular meshwork could not be seen in the primary position without indentation (Scheie grade 3 or 4) in at least 90 degrees. | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: Dr Wong has received financial support and honoraria for travel to conferences from Carl Zeiss Meditec and Heidelberg Engineering. Dr Friedman has received an instrument loan and has been a consultant for Carl Zeiss Meditec. Dr T. Aung has received grant funding as well as financial support and honoraria for travel to conferences from Carl Zeiss Meditec. Patients who had undergone peripheral iridotomy were not excluded. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Wu 2011.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. Participants aged 50 years and older who did not have any ophthalmic symptoms were recruited from a community polyclinic, they were systematically sampled (every fifth person registered at the polyclinic) and examined between December of 2005 to June of 2006. Data from the right eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 1922 eyes (317 narrow angle and 1605 open angle). Age: mean (SD), 63.0 ± 7.9 years. Sex: 1007 (52.4%) female. Setting: primary care. Country: Singapore. Ethnicity: 1717 (89.3%) Chinese, 39 Malay (2%), 142 Indian (7.4%), 24 others (1.2%). Exclusions: history of glaucoma, previous intraocular surgery, previous laser treatment, penetrating eye injury, or corneal disorders preventing anterior chamber assessment were excluded. |
||
| Index tests | AS‐OCT: time domain,Visante; Carl Zeiss Meditec, California. Scans were centered on the pupil and were obtained along the horizontal axis (0–180 degrees) using the standard anterior segment single‐scan protocol. The optimal thresholds was derived from the study data examining ACA and ACV. | ||
| Target condition and reference standard(s) | An eye was considered to have occludable angles if the posterior pigmented trabecular meshwork was not visible for at least 180 degrees on non‐indentation gonioscopy with the eye in the primary position. | ||
| Flow and timing | There were 2047 participants originally studied, 125 were excluded from the analysis for the following reasons: 5 participants could not undergo gonioscopy, 63 participants could not complete AS‐OCT examination or had poor quality AS‐OCT images, and 57 participants had Zhongshan Angle Assessment Program software delineation errors.Data from 1922 eyes were used in the final analysis. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: Dr Aung has received research funding, travel support, and honoraria from Carl Zeiss Meditec. Dr Friedman has received an instrument loan from Carl Zeiss Meditec. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Yes | ||
| Could the selection of patients have introduced bias? | Low risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Yu 1995a.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study, 20% random sample taken from a population over 50 years old from the Doumen county of the Guangdong province in November 1995. Data from both eyes were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 200 participants, 390 eyes (72 narrow angle and 318 open angle). Age: not reported. Sex: not reported. Setting: community. Country: China. Ethnicity: Chinese. Exclusions: not reported. |
||
| Index tests | Flashlight: flashlight beam was shown from the temporal side, a cut‐off using 1/4 (grade 2) or <1/4 (grade 1) nasal iris light band ratio were used. | ||
| Target condition and reference standard(s) | Gonioscopy using Shaffer’s chamber angle grading a grade 2 was considered as occludable in the temporal quadrant (90 degrees). | ||
| Flow and timing | There were no uninterpretable test results or exclusions reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflict of interest: no conflict of interest statement provided. | ||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | Yes | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | Unclear | ||
| Could the selection of patients have introduced bias? | Unclear risk | ||
| Are there concerns that the included patients and setting do not match the review question? | Low concern | ||
| DOMAIN 2: Index Test (LACD) | |||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| DOMAIN 2: Index Test (SPAC) | |||
| DOMAIN 2: Index Test (Flashlight) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Unclear | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Unclear | ||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Unclear | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Unclear risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
Zhang 2014.
| Study characteristics | |||
| Patient Sampling | Cross‐sectional study. All participants aged 40 years or older participated in a 5‐year follow‐up examination between August and December 2012. Gonioscopy was performed on participants with a LACD ≤ 40% as well as 1:10 participants registered per day. Data from the right eye were included in the analysis. | ||
| Patient characteristics and setting | Sample size: 425 eyes (126 narrow angle and 299 open angle). Age: mean (SD), 56.9 ± 10.1 years, (narrow angle 60.7 ± 8.1; open angle 55.4 ± 10.4). Sex: 270 (63.5%) female. Setting: community. Country: China. Ethnicity: Chinese. Exclusions: cases that could confound the results of the ACA examinations, and broad PAS (> 3 clock hours) that could influence the ACA configuration. Also if there was pre‐existing ocular surface pathology, history of eye trauma, contact lens wear, previous ocular surgery, use of drops that could influence ACA, inability to fixate on the target, or general physical or mental impairments that precluded participation. |
||
| Index tests |
LACD: determined at the temporal limbus and graded as % categories: 0%, 5%, 15%, 25%, 40%, 75% and ≥ 100%. Cut‐off values used: ≤ 15%, ≤ 25% and ≤ 40%. SPAC: measurements ranged from 1 to 12. Cut‐off values used: ≤ 5 and/or S or P; ≤ 6 and/or S or P and ACD. AS‐OCT: time domain, Visante, Carl Zeiss Meditec AG (software version 1.0). Subjective cut‐off used: an occludable angle on AS‐OCT was defined by contact between the iris and any part of the angle wall anterior to the scleral spur in 2 quadrants. Scheimpflug photography: Pentacam, Oculus Inc, Wetzlar, Germany, optimal cut‐off values were derived form the study data for ACD, ACA and ACV. |
||
| Target condition and reference standard(s) | Dynamic gonioscopic examination: an occludable angle was diagnosed as ≥ 180 degrees of the posterior trabecular meshwork was not visible on static gonioscopy. | ||
| Flow and timing | There were 431 participants originally studied, 6 participants were excluded due to inability to follow instructions or focus on the fixation light, or unwillingness to undergo gonioscopy. Data from 425 eyes were included in the analysis. There were no uninterpretable results reported. The index test and reference standard were conducted on the same occasion. | ||
| Comparative | |||
| Notes | Conflicts of interest: authors reported no conflicts of interest. Gonioscopy was performed on those with an LACD ≤ 40% and for 1 in 10 participants (number 1, 11, 21, etc) registered per day when seen in clinic. |
||
| Methodological quality | |||
| Item | Authors' judgement | Risk of bias | Applicability concerns |
| DOMAIN 1: Patient Selection | |||
| Was a consecutive or random sample of patients enrolled? | No | ||
| Was a case‐control design avoided? | Yes | ||
| Did the study avoid inappropriate exclusions? | No | ||
| Could the selection of patients have introduced bias? | High risk | ||
| Are there concerns that the included patients and setting do not match the review question? | High | ||
| DOMAIN 2: Index Test (LACD) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Scheimpflug photography) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | No | ||
| Could the conduct or interpretation of the index test have introduced bias? | High risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (AS‐OCT) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (SPAC) | |||
| Were the index test results interpreted without knowledge of the results of the reference standard? | Yes | ||
| If a threshold was used, was it pre‐specified? | Yes | ||
| Could the conduct or interpretation of the index test have introduced bias? | Low risk | ||
| Are there concerns that the index test, its conduct, or interpretation differ from the review question? | Low concern | ||
| DOMAIN 2: Index Test (Flashlight) | |||
| DOMAIN 3: Reference Standard | |||
| Is the reference standards likely to correctly classify the target condition? | Yes | ||
| Were the reference standard results interpreted without knowledge of the results of the index tests? | Yes | ||
| Could the reference standard, its conduct, or its interpretation have introduced bias? | Low risk | ||
| Are there concerns that the target condition as defined by the reference standard does not match the question? | Low concern | ||
| DOMAIN 4: Flow and Timing | |||
| Was there an appropriate interval between index test and reference standard? | Yes | ||
| Were all patients included in the analysis? | Yes | ||
| Did all patients receive a reference standard | Yes | ||
| Could the patient flow have introduced bias? | Low risk | ||
ACA: anterior chamber angle; ACD: anterior chamber depth; ACV: anterior chamber volume; AS‐OCT: anterior segment optical coherence tomography; IOP: intraocular pressure; ITC: irido‐trabecular contact; IQR: interquartile range; LACD: limbal anterior chamber depth; LPI: laser peripheral iridotomy; PACG: primary angle closure glaucoma; PACS: primary angle closure suspect; PAS: peripheral anterior synechiae; SD: standard deviation; SPAC: scanning peripheral anterior chamber.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Addepalli 2019 | No diagnostic information regarding index test reported |
| Adegbehingbe 2007 | No diagnostic information regarding index test reported |
| Alsbirk 1973 | Review index test not present |
| Alsbirk 1982 | 2x2 diagnostic table can not be constructed (gonioscopy performed on those identified with a shallow anterior chamber on the index test) |
| Alsbirk 1986 | 2x2 diagnostic table can not be constructed (gonioscopy performed on those identified with a shallow anterior chamber on the index test) |
| Alsbirk 1988 | 2x2 diagnostic table can not be constructed (gonioscopy performed on those identified with a shallow anterior chamber on the index test) |
| Alsbirk 1992 | 2x2 diagnostic table can not be constructed |
| Alsbirk 1994 | 2x2 diagnostic table can not be constructed |
| Annoh 2019 | 2x2 diagnostic table can not be constructed |
| Bai 2005 | 2x2 diagnostic table can not be constructed |
| Baskaran 2015 | Cases were not diagnosed using the reference test |
| Bastawrous 2018 | No diagnostic information regarding index test reported |
| Bhartiya 2013 | 2x2 diagnostic table can not be constructed |
| Bonomi 2000 | 2x2 diagnostic table can not be constructed |
| Bosem 1992 | No diagnostic information regarding index test reported |
| Bourne 2010 | 2x2 diagnostic table can not be constructed (gonioscopy not performed on all participants) |
| Chong 2013 | Correlation study, no threshold specified for index test for 2x2 table |
| Chong 2016 | No diagnostic information regarding index test reported |
| Chuka‐Okosa 2005 | No diagnostic information regarding index test reported |
| Chung 1995 | No diagnostic information regarding index test reported |
| Congdon 1999 | No diagnostic information regarding index test reported |
| Dandona 2001 | Commentary |
| Dawczynski 2007 | No diagnostic information regarding index test reported |
| Drance 1973 | Review index test not present |
| Foo 2011 | No diagnostic information regarding index test reported |
| Foo 2012 | No diagnostic information regarding index test reported |
| Forsius 1991 | Review index test not present |
| Friedman 2008 | 2x2 diagnostic table can not be constructed |
| Guo 2015 | No diagnostic information regarding index test reported |
| Hadziahmetovic 2014 | No diagnostic information regarding index test reported |
| He 2012 | Gonioscopy not the reference standard |
| Kalev‐landoy 2007 | 2x2 diagnostic table can not be constructed (index test not reported for those diagnosed with open angles) |
| Kashiwagi 2006 | Novel algorithm |
| Kashiwagi 2013 | 2x2 diagnostic table can not be constructed |
| Khalil 1975 | Review index test not present |
| Khan 2017 | 2x2 diagnostic table can not be constructed |
| Kim 2012 | Review index test not present |
| Kochupurakal 2016 | 2x2 diagnostic table not possible (No. of diseased/non‐diseased not reported) |
| Leung 2010 | Ethnicities compared, no threshold specified for diagnostic test accuracy |
| Li 2014 | Prevalence study |
| Liu 2011 | 2x2 diagnostic table can not be constructed |
| Lu 1980 | Gonioscopy not the reference standard |
| Mani 2014 | Diagnostic data could not be obtained |
| Matonti 2011 | No diagnostic information regarding index test reported |
| Melese 2015 | Novel algorithm for AS‐OCT |
| Moghimi 2015 | No controls or participants with open angles were examined |
| Moghimi 2017 | No diagnostic information regarding index test reported |
| Moreno‐Montanes 1992 | Review index test not present |
| Narayanaswamy 2013 | Prevalence study, no diagnostic information regarding index test reported |
| Ni 2014 | Novel algorithm for AS‐OCT |
| Niemeyer 2014 | No diagnostic information regarding index test reported |
| Nongpiur 2010 | Novel algorithm for AS‐OCT |
| Nongpiur 2013 | Novel algorithm for AS‐OCT |
| Nongpiur 2014 | Novel algorithm for AS‐OCT |
| Nongpiur 2017 | Study design |
| Nongpiur 2019 | 2x2 diagnostic table can not be constructed |
| Nuriyah 2010 | Gonioscopy not the reference standard |
| Pakravan 2012 | Target condition was not an occludable angle |
| Pei 2019 | 2x2 diagnostic table can not be constructed |
| Pekmezci 2009 | 2x2 diagnostic table not possible (No. of diseased/non‐diseased not reported) |
| Quek 2012 | 2x2 diagnostic table can not be constructed |
| Ren 2005 | No diagnostic information regarding index test reported |
| Rigi 2016 | No diagnostic information regarding index test reported |
| Rojananuangnit 2016 | No diagnostic information regarding index test reported |
| Rueda 2003 | Not diagnostic information available |
| Sah 2007 | Prevalence study, no diagnostic information regarding index test reported |
| Sakata 2007 | Prevalence study, no diagnostic information regarding index test reported |
| Sakata 2008 | Prevalence study, no diagnostic information regarding index test reported |
| Sasikumar 2011 | No diagnostic information regarding index test reported |
| Scalamogna 2002 | Not diagnostic information available |
| Shibata 1992 | No diagnostic information regarding index test reported |
| Shikino 2016 | No diagnostic information regarding index test reported |
| Sihota 2019 | Gonioscopy not performed |
| Sparks 1997 | Gonioscopy not the reference standard |
| Talaspayeva 2015 | No diagnostic information regarding index test reported |
| Tay 2015 | 2x2 diagnostic table can not be constructed |
| Thompson 2018 | 2x2 diagnostic table can not be constructed |
| Tomoyose 2010 | No diagnostic information regarding index test reported |
| Trueba 2010 | Gonioscopy not the reference standard |
| Tun 2013 | No diagnostic information regarding index test reported |
| Vargas 1973 | Gonioscopy not the reference standard |
| Varma 2017 | 2x2 diagnostic table can not be constructed |
| Wang 2013 | No diagnostic information regarding index test reported |
| Wang 2014 | No diagnostic information regarding index test reported |
| Wang 2015 | No diagnostic information regarding index test reported |
| Wong 2015 | No diagnostic data available |
| Xie 2011 | No diagnostic information regarding index test reported |
| Xu 2001 | No diagnostic information regarding index test reported |
| Xu 2004 | No diagnostic information regarding index test reported |
| Xu 2005 | Gonioscopy not the reference standard |
| Xu 2008 | No diagnostic information regarding index test reported |
| Xu 2009 | No diagnostic information regarding index test reported |
| Xu 2011 | No diagnostic information regarding index test reported |
| Xu 2018 | 2x2 diagnostic table can not be constructed |
| Xu 2019a | Deep learning algorithm |
| Xu 2019b | 2x2 diagnostic table can not be constructed |
| Yamamoto 2005 | No diagnostic information regarding index test reported |
| Yamamoto 2009 | 2x2 diagnostic table can not be constructed |
| Ye 1995 | Gonioscopy not the reference standard |
| Ye 1998 | Gonioscopy not performed |
| Yip 2008 | 2x2 diagnostic table can not be constructed |
| Yu 1995b | Gonioscopy not performed |
| Yu 1996 | Gonioscopy not the reference standard |
| Yu 1997 | Health economic review |
| Yuan 2007 | Prevalence study, no diagnostic information regarding index test reported |
| Zhang 2008 | No diagnostic information regarding index test reported |
| Zhang 2010 | No diagnostic information regarding index test reported |
| Zhao 2008 | No diagnostic information regarding index test reported |
AS‐OCT: anterior segment optical coherence tomography.
Contributions of authors
Conceiving the review: JL Drafting of protocol: AJ, JL, IC, GV, EL Assessed studies for inclusion and exclusion: AJ, IC, JL Assessed risk of bias, extracted data, entered data and authored the first draft of the review: AJ, JL Conducted the statistical analysis: EL Commented on the text of the review: AJ, JL, IC, GV, EL
Sources of support
Internal sources
No sources of support supplied
External sources
-
College of Optometrists, UK
Anish Jindal acknowledges support from a PhD studentship from the College of Optometrists and a Doctoral Progress Award from City,University of London
-
National Institute for Health Research (NIHR), UK
Richard Wormald, Co‐ordinating Editor for Cochrane Eyes and Vision (CEV) acknowledges financial support for his CEV research sessions from the Department of Health through the award made by the National Institute for Health Research to Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology for a Specialist Biomedical Research Centre for Ophthalmology.
This review was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the CEV UK editorial base.
The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Declarations of interest
AJ: Received funding for a PhD studentship from the College of Optometrists and a doctoral progress award from City, University of London, there are no conflicts of interest in publishing this review. IC: None known GV: None known ESL: None known JL: Recieved grant income from NIHR, IGA and the College of Optometrists for projects outside the submitted review.
Edited (no change to conclusions)
References
References to studies included in this review
Alonso 2010 {published data only}
- Alonso RS, Ambrosio Junior R, Paranhos Junior A, Sakata LM, Ventura MP. Glaucoma anterior chamber morphometry based on optical Scheimpflug images. Arquivos Brasileiros de Oftalmologia 2010;73(6):497-500. [DOI] [PubMed] [Google Scholar]
Andrews 2012 {published data only}
- Andrews J, Chang DS, Jiang Y, He M, Foster PJ, Munoz B, et al. Comparing approaches to screening for angle closure in older Chinese adults. Eye 2012;26(1):96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ashaye 2003 {published data only}
- Ashaye AO. Use of limbal and central anterior chamber depth measurements in detecting eyes with gonioscopically occludable angles and primary angle closure glaucoma in Ibadan. African Journal of Medicine and Medical Sciences 2003;32(4):413-6. [PubMed] [Google Scholar]
Baskaran 2007 {published data only}
- Baskaran M, Oen FT, Chan YH, Hoh ST, Ho CL, Kashiwagi K, et al. Comparison of the scanning peripheral anterior chamber depth analyzer and the modified van Herick grading system in the assessment of angle closure. Ophthalmology 2007;114(3):501-6. [DOI] [PubMed] [Google Scholar]
Baskaran 2012 {published data only}
- Baskaran M, Aung T, Friedman DS, Tun TA, Perera SA. Comparison of EyeCam and anterior segment optical coherence tomography in detecting angle closure. Acta Ophthalmologica 2012;90(8):e621-5. [DOI] [PubMed] [Google Scholar]
Baskaran 2013 {published data only}
- Baskaran M, Ho SW, Tun TA, How AC, Perera SA, Friedman DS, et al. Assessment of circumferential angle-closure by the iris-trabecular contact index with swept-source optical coherence tomography. Ophthalmology 2013;120(11):2226-31. [DOI] [PubMed] [Google Scholar]
Campbell 2015 {published data only}
- Campbell P, Agarwal R, Redmond T, Lim KS, Evans B. Repeatability and comparison of anterior chamber angle assessment tests. Investigative Ophthalmology and Visual Science 2014;55(13):ARVO E-abstract 933.
- Campbell, P, Redmond T, Agarwal, R, Marshall, LR, Evans BJ. Repeatability and comparison of clinical techniques for anterior chamber angle assessment. Ophthalmic and Physiological Optics 2015;35(2):170-8. [DOI] [PubMed] [Google Scholar]
Chang 2011 {published data only}
- Chang DS, Sakata LM, Aung T, He MG, Lavanya R, Kashiwagi K, et al. Single versus sequential testing with scanning peripheral anterior chamber depth analyser, IOLMaster and anterior segment optical coherence tomography for the detection of narrow angles. British Journal of Ophthalmology 2011;95(10):1410-4. [DOI] [PubMed] [Google Scholar]
Choudhari 2019a {published data only}
- Choudhari NS, Chanda S, Khanna R, Senthil S, Garudadri CS. Diagnostic accuracy of van Herick technique to detect pre-disease states of primary angle closure glaucoma in a resource constraint region. Ophthalmic Epidemiology 2019;26(3):175-82. [DOI] [PubMed] [Google Scholar]
Choudhari 2019b {published data only}
- Choudhari NS, Chandran PA, Rao H, Jonnadula G, Addepalli U, Senthil S, et al. Screening for primary angle closure disease in resource constraint region. Investigative Ophthalmology and Visual Science 2017;58(8):ARVO E-abstract 5612.
- Choudhari NS, George R, Asokan R, Khanna R, Vijaya L, Garudadri CS. Combination of simple diagnostic tests to detect primary angle closure disease in a resource-constrained region. Ophthalmic Epidemiology 2019;26(3):175-82. [DOI] [PubMed] [Google Scholar]
Congdon 1996 {published data only}
- Congdon NG, Quigley HA, Hung PT, Wang TH, Ho TC. Screening techniques for angle-closure glaucoma in rural Taiwan. Acta Ophthalmologica Scandinavica 1996;74(2):113-9. [DOI] [PubMed] [Google Scholar]
Dabasia 2015 {published data only}
- Dabasia P, Murdoch I, Edgar D, Lawrenson J. Case‐finding for angle closure: the diagnostic value of simple tests for estimating limbal and central anterior chamber depth. In: Acta Ophthalmologica. Vol. 94. 14 September 2016.
- Dabasia PL, Edgar DF, Murdoch IE, Lawrenson JG. Non-contact screening methods for the detection of narrow anterior chamber angles. Investigative Ophthalmology and Vision Science 2015;56(6):3929–35. [DOI] [PubMed] [Google Scholar]
Foster 2000 {published data only}
- Foster PJ, Devereux JG, Alsbirk PH, Lee PS, Uranchimeg D, Machin D, et al. Detection of gonioscopically occludable angles and primary angle closure glaucoma by estimation of limbal chamber depth in Asians: modified grading scheme. British Journal of Ophthalmology 2000;84(2):186-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gracitelli 2014 {published data only}
- Gracitelli CP, Landgren B, Graciani FB, Sousa AK, Paranhos A Jr, Prata TS. Ability of non-ophthalmologist doctors to detect eyes with occludable angles using the flashlight test. International Ophthalmology 2014;34(3):557-61. [DOI] [PubMed] [Google Scholar]
Grewal 2011 {published data only}
- Grewal DS, Brar GS, Jain R, Grewal SP. Comparison of Scheimpflug imaging and spectral domain anterior segment optical coherence tomography for detection of narrow anterior chamber angles. Eye 2011;25(5):603-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
He 2007 {published data only}
- He M, Huang W, Friedman DS, Wu C, Zheng Y, Foster PJ. Slit lamp-simulated oblique flashlight test in the detection of narrow angles in Chinese eyes: the Liwan eye study. Investigative Ophthalmology and Visual Science 2007;48(12):5459-63. [DOI] [PubMed] [Google Scholar]
Hong 2009 {published data only}
- Hong S, Yi JH, Kang SY, Seong GJ, Kim CY. Detection of occludable angles with the Pentacam and the anterior segment optical coherence tomography. Yonsei Medical Journal 2009;50(4):525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnson 2018 {published data only}
- Johnson TV, Ramulu PY, Quigley HA, Singman EL. Low sensitivity of the Van Herick method for detecting gonioscopic angle closure independent of observer expertise. American Journal of Ophthalmology 2018;195:63-71. [DOI] [PubMed] [Google Scholar]
Khor 2010 {published data only}
- Khor WB, Sakata LM, Friedman DS, Narayanaswamy A, Lavanya R, Perera SA, et al. Evaluation of scanning protocols for imaging the anterior chamber angle with anterior segment-optical coherence tomography. Journal of Glaucoma 2010;19(6):365-8. [DOI] [PubMed] [Google Scholar]
Kim 2014 {published data only}
- Kim YK, Yoo BW, Kim HC, Aung T, Park KH. Relative lens vault in subjects with angle closure. BMC Ophthalmology 2014;14:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ko 2015 {published data only}
- Ko YC, Liu CJ, Hsu WM, Cheng CY, Kuang TM, Chou P. Determinants and characteristics of angle-closure disease in an elderly Chinese population. Ophthalmic Epidemiology 2015;22(2):109-15. [DOI] [PubMed] [Google Scholar]
Kurita 2009 {published data only}
- Kurita N, Mayama C, Tomidokoro A, Aihara M, Araie M. Potential of the Pentacam in screening for primary angle closure and primary angle closure suspect. Journal of Glaucoma 2009;18(7):506-12. [DOI] [PubMed] [Google Scholar]
Lavanya 2008 {published data only}
- Lavanya R, Foster PJ, Sakata LM, Friedman DS, Kashiwagi K, Wong TY, et al. Screening for narrow angles in the Singapore population: evaluation of new non-contact screening methods. Ophthalmology 2008;115(10):1720-7. [DOI] [PubMed] [Google Scholar]
Li 2019 {published data only}
- Li F, Zhou R, Gao K, Jin L, Zhang X. Volumetric parameters-based differentiation of narrow angle from open angle and classification of angle configurations: an SS-OCT study. British Journal of Ophthalmology 2020;104(1):92-7. [DOI] [PubMed] [Google Scholar]
Melese 2016 {published data only}
- Melese EK, Chan JD, Blieden LS, Chuang AZ, Baker LA, Bell NP, et al. Determination and validation of thresholds of anterior chamber parameters by dedicated anterior segment optical coherence tomography. American Journal of Ophthalmology 2016;169:208-17. [DOI] [PubMed] [Google Scholar]
Mosler 2015 {published data only}
- Mosler MP, Werner JU, Lang GK. Chamber angle assessment in clinical practice - a comparison between optical coherence tomography and gonioscopy. Klinische Monatsblatter fur Augenheilkunde 2015;232(7):874-80. [DOI] [PubMed] [Google Scholar]
Muto 2019 {published data only}
- Muto T, Nishimura T, Sakamoto M, Inomata T, Machida S. Identification of eyes at risk of acute primary angle-closure in elderly Japanese patients. Clinical Ophthalmology 2019;13:859-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
Narayanaswamy 2010 {published data only}
- Narayanaswamy A, Sakata LM, He MG, Friedman DS, Chan YH, Lavanya R, et al. Diagnostic performance of anterior chamber angle measurements for detecting eyes with narrow angles: an anterior segment OCT study. Archives of Ophthalmology 2010;128(10):1321-7. [DOI] [PubMed] [Google Scholar]
Nolan 2006 {published data only}
- Nolan WP, Aung T, Machin D, Khaw PT, Johnson GJ, Seah SK, et al. Detection of narrow angles and established angle closure in Chinese residents of Singapore: potential screening tests. American Journal of Ophthalmology 2006;141(5):896-901. [DOI] [PubMed] [Google Scholar]
Nolan 2007 {published data only}
- Nolan WP, See J, Aung T, Ce Z, Radhakrishnan S, Friedman DS, et al. Detection of patients at risk of angle-closure using anterior segment OCT. Investigative Ophthalmology and Visual Science 2005;46(13):ARVO E-abstract 145.
- Nolan WP, See JL, Chew PT, Friedman DS, Smith SD, Radhakrishnan S, et al. Detection of primary angle closure using anterior segment optical coherence tomography in Asian eyes. Ophthalmology 2007;114(1):33-9. [DOI] [PubMed] [Google Scholar]
Nongpiur 2011 {published data only}
- Nongpiur ME, He M, Amerasinghe N, Friedman DS, Tay WT, Baskaran M, et al. Lens vault, thickness, and position in Chinese subjects with angle closure. Ophthalmology 2011;118(3):474-9. [DOI] [PubMed] [Google Scholar]
Okabe 1991 {published data only}
- Okabe I, Tomita G, Sugiyama K, Taniguchi T. An epidemiological study on the prevalence of the narrow chamber angle in Japanese. Journal of Japanese Ophthalmological Society 1991;95(3):279-87. [PubMed] [Google Scholar]
Park 2011 {published data only}
- Park SB, Sung KR, Kang SY, Jo JW, Lee KS, Kook MS. Assessment of narrow angles by gonioscopy, Van Herick method and anterior segment optical coherence tomography. Japanese Journal of Ophthalmology 2011;55(4):343-50. [DOI] [PubMed] [Google Scholar]
Porporato 2019 {published data only}
- Porporato N, Baskaran M, Tun TA, Sultana R, Tan M, Quah JH, et al. Understanding diagnostic disagreement in angle closure assessment between anterior segment optical coherence tomography and gonioscopy. British Journal of Ophthalmology Sep 6 2019 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Porporato N, Baskaran M, Tun TA, Sultana R, Tan MC, Quah JH, et al. Assessment of circumferential angle closure with swept-source optical coherence tomography: a community based study. American Journal of Ophthalmology 2019;199:133-9. [DOI] [PubMed] [Google Scholar]
- Porporato N, Mani B, Ganguly RS, Tun TA, Tan MC, Quah JH, et al. Assessment of circumferential angle closure with swept-source optical coherence tomography: A community based study. Investigative Ophthalmology and Visual Science 2018;59(9):ARVO E-abstract 5902. [DOI] [PubMed]
- Porporato N, Mani B, Yanwu X, Tun TA, Trikha S, Wong DW, et al. Automated grading of anterior segment swept source OCT images: A validation study for assessment of angle closure. Investigative Ophthalmology and Visual Science 2017;58(8):ARVO E-abstract 2086.
Radhakrishnan 2005 {published data only}
- Goldsmith JA, Radhakrishnan S, Westphal V, Huang D, Dueker DK, Rollins AM, et al. Comparison of optical coherence tomography and ultrasound biomicroscopy in identifying anatomically narrow angles. Investigative Ophthalmology and Visual Science 2002;43(13):ARVO E-abstract 287. [Google Scholar]
- Radhakrishnan S, Goldsmith J, Huang D, Westphal V, Dueker DK, Rollins AM, et al. Comparison of optical coherence tomography and ultrasound biomicroscopy for detection of narrow anterior chamber angles. Archives of Ophthalmology 2005;123(8):1053-9. [DOI] [PubMed] [Google Scholar]
Rossi 2012 {published data only}
- Rossi GC, Scudeller L, Delfino A, Raimondi M, Pezzotta S, Maccarone M, et al. Pentacam sensitivity and specificity in detecting occludable angles. European Journal of Ophthalmology 2012;22(5):701-8. [DOI] [PubMed] [Google Scholar]
Sakata 2010 {published data only}
- Sakata LM, Wong TT, Wong HT, Kumar RS, Htoon HM, Aung HT, et al. Comparison of Visante and slit-lamp anterior segment optical coherence tomography in imaging the anterior chamber angle. Eye 2010;24(4):578-87. [DOI] [PubMed] [Google Scholar]
Tan 2012 {published data only}
- Tan G, Li J, He MG, Sakata LM, Friedman DS, Aung, T. Diagnostic performance of novel morphological parameters for the screening of narrow angles. Proceedings of Singapore Healthcare 2010;19:S241. [Google Scholar]
- Tan GS, He M, Zhao W, Sakata LM, Li J, Nongpiur ME, et al. Determinants of lens vault and association with narrow angles in patients from Singapore. American Journal of Ophthalmology 2012;154(1):39-46. [DOI] [PubMed] [Google Scholar]
Thomas 1996 {published data only}
- Thomas R, George T, Braganza A, Muliyil J. The flashlight test and van Herick's test are poor predictors for occludable angles. Australian and New Zealand Journal of Ophthalmology 1996;24(3):251-6. [DOI] [PubMed] [Google Scholar]
Tun 2017 {published data only}
- Tun TA, Baskaran M, Tan SS, Perera SA, Aung T, Husain R. Evaluation of the anterior segment angle-to-angle scan of cirrus high-definition optical coherence tomography and comparison with gonioscopy and with the visante OCT. Investigative Ophthalmology and Visual Science 2017;58(1):59-64. [DOI] [PubMed] [Google Scholar]
Winegarner 2019 {published data only}
- Winegarner A, Miki A, Kumoi M, Ishida Y, Wakabayashi T, Sakimoto S, et al. Anterior segment Scheimpflug imaging for detecting primary angle closure disease. Graefe's Archive for Clinical and Experimental Ophthalmology 2019;257(1):161-7. [DOI] [PubMed] [Google Scholar]
Wirbelauer 2005 {published data only}
- Wirbelauer C, Karandish A, Haberle H, Pham DT. Non-contact goniometry with optical coherence tomography. Archives of Ophthalmology 2005;123(2):179-85. [DOI] [PubMed] [Google Scholar]
Wong 2009a {published data only}
- Wong HT, Chua JL, Sakata LM, Wong MH, Aung HT, Aung T. Comparison of slitlamp optical coherence tomography and scanning peripheral anterior chamber depth analyzer to evaluate angle closure in Asian eyes. Archives of Ophthalmology 2009;127(5):599-603. [DOI] [PubMed] [Google Scholar]
Wong 2009b {published data only}
- Wong HT, Lim MC, Sakata LM, Aung HT, Amerasinghe N, Friedman DS, et al. High-definition optical coherence tomography imaging of the iridocorneal angle of the eye. Archives of Ophthalmology 2009;127(3):256-60. [DOI] [PubMed] [Google Scholar]
Wu 2011 {published data only}
- Wu RY, Nongpiur ME, He MG, Sakata LM, Friedman DS, Chan YH, et al. Association of narrow angles with anterior chamber area and volume measured with anterior-segment optical coherence tomography. Archives of Ophthalmology 2011;129(5):569-74. [DOI] [PubMed] [Google Scholar]
Yu 1995a {published data only}
- Yu Q, Xu J, Zhu S, Liu, Q. A role of oblique flashlight test in screening for primary angle closure glaucoma. Eye Science 1995;11(4):177-9. [PubMed] [Google Scholar]
Zhang 2014 {published data only}
- Zhang Y, Li S, Wang N. Screening efficiency of scanning peripheral anterior chamber depth analyzer for occludable angle-Handan Eye Study. Chinese Journal of Experimental Ophthalmology 2015;33(3):259-62. [Google Scholar]
- Zhang Y, Li SZ, Li L, Thomas R, Wang NL. The Handan Eye Study: comparison of screening methods for primary angle closure suspects in a rural Chinese population. Ophthalmic Epidemiology 2014;21(4):268-75. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Addepalli 2019 {published data only}
- Addepalli UK, Jonnadula GB, Garudadri CS, Khanna RC, Papas EB. Prevalence of primary glaucoma as diagnosed by study optometrists of L. V. Prasad eye Institute - glaucoma epidemiology and molecular genetics study. Ophthalmic Epidemiology 2019;26(3):150-4. [DOI] [PubMed] [Google Scholar]
Adegbehingbe 2007 {published data only}
- Adegbehingbe BO, Majengbasan TO. Ocular health status of rural dwellers in south-western Nigeria. Australian Journal of Rural Health 2007;15(4):269-72. [DOI] [PubMed] [Google Scholar]
Alsbirk 1973 {published data only}
- Alsbirk PH, Forsius H. Anterior chamber depth in Eskimos from Greenland, Canada (Igloolik) and Alaska (Wainwright). A preliminary report. Canadian Journal of Ophthalmology 1973;8(2):265-9. [PubMed] [Google Scholar]
Alsbirk 1982 {published data only}
- Alsbirk PH. Anterior chamber depth, genes and environment. A population study among long-term Greenland Eskimo immigrants in Copenhagen. Acta Ophthalmologica 1982;60(2):223-4. [DOI] [PubMed] [Google Scholar]
Alsbirk 1986 {published data only}
- Alsbirk PH. Limbal and axial chamber depth variations. A population study in Eskimos. Acta Ophthalmologica 1986;64(6):593-600. [DOI] [PubMed] [Google Scholar]
Alsbirk 1988 {published data only}
- Alsbirk PH. Early detection of primary angle-closure glaucoma. Limbal and axial chamber depth screening in a high risk population (Greenland Eskimos). Acta Ophthalmologica 1988;66(5):556-64. [DOI] [PubMed] [Google Scholar]
Alsbirk 1992 {published data only}
- Alsbirk PH. Anatomical risk factors in primary angle-closure glaucoma. A ten year follow up survey based on limbal and axial anterior chamber depths in a high risk population. International Ophthalmology 1992;16(4-5):265-72. [DOI] [PubMed] [Google Scholar]
Alsbirk 1994 {published data only}
- Alsbirk PH. Anatomical risk factors of angle-closure glaucoma. A 10-year study of limbal and axial anterior chamber depths in a risk population. Ugeskrift for Laeger 1994;156(36):5117-21. [PubMed] [Google Scholar]
Annoh 2019 {published data only}
- Annoh R, Loo CY, Hogan B, Tan HL, Tang LS, Tatham AJ. Accuracy of detection of patients with narrow angles by community optometrists in Scotland. Ophthalmic and Physiological Optics 2019;39(2):104-12. [DOI] [PubMed] [Google Scholar]
Bai 2005 {published data only}
- Bai ZL, Ren BC, Yan JG, He Y, Chen L, Sun NX. Epidemiology of primary angle-closure glaucoma in a rural population in Shaanxi Province of China. Internation Journal of Ophthalmology 2005;5(5):872-80. [Google Scholar]
Baskaran 2015 {published data only}
- Baskaran M, Iyer JV, Narayanaswamy AK, He Y, Sakata LM, Wu R, et al. Anterior segment imaging predicts incident gonioscopic angle closure. Ophthalmology 2015;122(12):2380-4. [DOI] [PubMed] [Google Scholar]
Bastawrous 2018 {published data only}
- Bastawrous A, Mathenge W, Buchan J, Kyari F, Peto T, Rono H, et al. Glaucoma features in an East African population: a 6-year cohort study of older adults in Nakuru, Kenya. Journal of Glaucoma 2018;27(5):455-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bhartiya 2013 {published data only}
- Bhartiya S, Shaarawy T. Evaluation of the van Herick technique for screening for occludable angles in an African population. Journal of Current Glaucoma Practice 2013;7(2):88-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bonomi 2000 {published data only}
- Bonomi L, Marchini G, Marraffa M, Bernardi P, De Franco I, Perfetti S, et al. Epidemiology of angle-closure glaucoma: prevalence, clinical types, and association with peripheral anterior chamber depth in the Egna-Neumarket Glaucoma Study. Ophthalmology 2000;107(5):998-1003. [DOI] [PubMed] [Google Scholar]
Bosem 1992 {published data only}
- Bosem ME, Morsman D, Lusky M, Weinreb RN. Reproducibility of quantitative anterior chamber angle measurements with Scheimpflug video imaging. Journal of Glaucoma 1992;1(4):254-7. [DOI] [PubMed] [Google Scholar]
Bourne 2010 {published data only}
- Bourne RR, French KA, Chang L, Borman AD, Hingorani M, Newsom WD. Can a community optometrist-based referral refinement scheme reduce false-positive glaucoma hospital referrals without compromising quality of care? the community and hospital allied network glaucoma evaluation scheme (CHANGES). Eye 2010;24(5):881-7. [DOI] [PubMed] [Google Scholar]
Chong 2013 {published data only}
- Chong RS, Sakata LM, Narayanaswamy AK, Ho SW, He M, Baskaran M, et al. Relationship between intraocular pressure and angle configuration: an anterior segment OCT study. Investigative Ophthalmology and Visual Science 2013;54(3):1650-5. [DOI] [PubMed] [Google Scholar]
Chong 2016 {published data only}
- Chong GT, Wen JC, Su DH, Stinnett S, Asrani S. Ocular biometrics of myopic eyes with narrow angles. Journal of Glaucoma 2016;25(2):140-4. [DOI] [PubMed] [Google Scholar]
Chuka‐Okosa 2005 {published data only}
- Chuka-Okosa CM, Faal HB, Ogunro A, Duke R. Types of glaucoma and recent trends applied in treatment: observations from a glaucoma training workshop in the Gambia. Nigerian Postgraduate Medical Journal 2005;12(3):203-9. [PubMed] [Google Scholar]
Chung 1995 {published data only}
- Chung HS, Hong YJ, Choi CM. The depth of the anterior chamber in primary angle closure glaucoma. Investigative Ophthalmology and Visual Science 1995;36(4):ARVO E-abstract 564.
Congdon 1999 {published data only}
- Congdon NG, Spaeth GL, Augsburger J, Klancnik J Jr, Patel K, Hunter DG. A proposed simple method for measurement in the anterior chamber angle: biometric gonioscopy. Ophthalmology 1999;106(11):2161-7. [DOI] [PubMed] [Google Scholar]
Dandona 2001 {published data only}
- Dandona L, Dandona R, Mandal P, Shields MB. Angle-closure glaucoma in an urban population in southern India. Evidence Based Eye Care 2001;2(2):108-9. [Google Scholar]
Dawczynski 2007 {published data only}
- Dawczynski J, Koenigsdoerffer E, Augsten R, Strobel J. Anterior optical coherence tomography: a non-contact technique for anterior chamber evaluation. Graefes Archive for Clinical and Experimental Ophthalmology 2007;245(3):423-5. [DOI] [PubMed] [Google Scholar]
Drance 1973 {published data only}
- Drance SM, Morgan RW, Bryett J, Fairclough M. Anterior chamber depth and gonioscopic findings among the Eskimos and Indians in the Canadian Arctic. Canadian Journal of Ophthalmology 1973;8(2):255-9. [PubMed] [Google Scholar]
Foo 2011 {published data only}
- Foo LL, Nongpiur ME, He M, Allen JC Jr, Wu R, Zheng Y, et al. Novel prediction model for angle width in Chinese Singaporeans. Investigative Ophthalmology and Visual Science 2011;52(14):ARVO E-abstract 3064.
Foo 2012 {published data only}
- Foo LL, Nongpiur ME, Allen JC, Perera SA, Friedman DS, He M, et al. Determinants of angle width in Chinese Singaporeans. Ophthalmology 2012;119(2):278-82. [DOI] [PubMed] [Google Scholar]
Forsius 1991 {published data only}
- Forsius H, Fellman J, Eriksson A. Anterior chamber depth in Arctic and tropical populations. Arctic Medical Research 1991;Suppl:505-8. [PubMed] [Google Scholar]
Friedman 2008 {published data only}
- Friedman DS, Gazzard G, Min CB, Broman AT, Quigley H, Tielsch J, et al. Age and sex variation in angle findings among normal Chinese subjects: a comparison of UBM, Scheimpflug, and gonioscopic assessment of the anterior chamber angle. Journal of Glaucoma 2008;17(1):5-10. [DOI] [PubMed] [Google Scholar]
Guo 2015 {published data only}
- Guo JM, Xu XL, Zhang H, Wang JM. Comparison of anterior segment parameters between fellow eyes of unilateral acute angle closure glaucoma and primary angle closure suspects. International Eye Science 2015;15(4):650-3. [Google Scholar]
Hadziahmetovic 2014 {published data only}
- Hadziahmetovic M, Williamson K, Lehman AY, Ackert JM. Higher than expected prevalence of glaucoma in community centered practice. Investigative Ophthalmology and Visual Science 2014;55(13):ARVO E-abstract 4271.
He 2012 {published data only}
- He Y, Baskaran M, Tun TA, Narayanaswamy AK, Aung T. In: Proceedings of Singapore Healthcare. Vol. 21. March 2012:S136.
Kalev‐landoy 2007 {published data only}
- Kalev-landoy M, Day AC, Cordeiro MF, Migdal C. Optical coherence tomography in anterior segment imaging. Acta Ophthamologica Scandinavica 2007;85(4):427-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kashiwagi 2006 {published data only}
- Kashiwagi K, Kashiwagi F, Hiejima Y, Tsukahara S. Finding cases of angle-closure glaucoma in clinic setting using a newly developed instrument. Eye 2006;20(3):319-24. [DOI] [PubMed] [Google Scholar]
Kashiwagi 2013 {published data only}
- Kashiwagi K, Chiba T, Mabuchi F, Furuya T, Tsukahara S. Five-year incidence of angle closure among glaucoma health examination participants. Graefes Archive for Clinical and Experimental Ophthalmology 2013;251(4):1219-28. [DOI] [PubMed] [Google Scholar]
Khalil 1975 {published data only}
- Khalil AA, Al-Hussaini MK, Abboud I A, Wasfy IA. Anterior chamber depth measurements in normal eyes and in eyes involved with primary glaucoma in Assiut. Bulletin of the Ophthalmological Society of Egypt 1975;68:143-63. [PubMed] [Google Scholar]
Khan 2017 {published data only}
- Khan FA, Niazi SP, Khan AZ. Relationship of the Van Herick grading system with peripheral iris configuration and level of iris insertion. Journal of the College of Physicians and Surgeons 2017;27(9):547-51. [PubMed] [Google Scholar]
Kim 2012 {published data only}
- Kim SH, Kang JH, Park KH, Hong C. Hong's grading for evaluating anterior chamber angle width. Japanese Journal of Ophthalmology 2012;56(6):551-8. [DOI] [PubMed] [Google Scholar]
Kochupurakal 2016 {published data only}
- Kochupurakal RT, Srikanth K, Jha KN, Rajalakshmi AR, Nagarajan S, Ezhumalai G. Role of optical coherence tomography in assessing anterior chamber angles. Journal of Clinical and Diagnostic Research 2016;10(4):NC18-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leung 2010 {published data only}
- Leung CK, Palmiero PM, Weinreb RN, Li H, Sbeity Z, Dorairaj S, et al. Comparisons of anterior segment biometry between Chinese and Caucasians using anterior segment optical coherence tomography. British Journal of Ophthalmology 2010;94(9):1184-9. [DOI] [PubMed] [Google Scholar]
Li 2014 {published data only}
- Li H, Zhang YY, Liu SC, He XG, Li CJ, Li CH, et al. Prevalence of open-angle glaucoma in southwestern China: the Yongchuan Glaucoma study. Journal of Huazhong University of Science and Technology. Medical Sciences 2014;34(1):137-41. [DOI] [PubMed] [Google Scholar]
Liu 2011 {published data only}
- Liu D, Baskaran M, Nongpiur ME, Friedman DS, Aung T. Can anterior segment OCT detect angle closure earlier than gonioscopy? Investigative Ophthalmology and Visual Science 2011;52(14):ARVO E-abstract 6281.
Lu 1980 {published data only}
- Lu DP. Examination of peripheral chamber depth in mass screening for glaucoma, with special reference to early angle-closure glaucoma. Chinese Journal of Ophthalmology 1980;16(3):204-5. [PubMed] [Google Scholar]
Mani 2014 {published data only}
- Mani B, Yau C, Ho SW, Tun TA, Perera S, Aung T. Comparison of time domain anterior segment OCT with swept source OCT for angle closure imaging. Investigative Ophthalmology and Visual Science 2014;55(13):ARVO E-abstract 932.
Matonti 2011 {published data only}
- Matonti F, Hoffart L, Ridings B, Conrath J. Dynamic gonioscopy using optical coherence tomography. Investigative Ophthalmology and Visual Science 2011;52(14):ARVO E-abstract 6649.
Melese 2015 {published data only}
- Melese E, Chuang A, Baker L, Blieden L, Bell N, Feldman R. Sensitivity, specificity, and optimal thresholds of anterior chamber angle (ACA) parameters measured by anterior segment optical coherence tomography (AS-OCT) in determination of open versus closed angles. Investigative Ophthalmology and Visual Science 2015;56(7):ARVO E-abstract 4998.
Moghimi 2015 {published data only}
- Moghimi S, Ramezani F, He M, Coleman AL, Lin SC. Comparison of anterior segment-optical coherence tomography parameters in phacomorphic angle closure and acute angle closure eyes. Investigative Ophthalmology and Visual Science 2015;56(13):7611-7. [DOI] [PubMed] [Google Scholar]
Moghimi 2017 {published data only}
- Moghimi S, Kiaroudi M, Coh P, Li Y, He M, Lin SC. Comparison of anterior chamber parameters in patients with plateau iris configuration and pupillary block using AS-OCT. Journal of Glaucoma 2017;26(2):153-8. [DOI] [PubMed] [Google Scholar]
Moreno‐Montanes 1992 {published data only}
- Moreno-Montanes J, Alvarez A, Alcolea A, Marcos JM. The central depth of the anterior chamber as a predictive factor of primary angle-closure glaucoma. Glaucoma 1992;14(4):115-9. [Google Scholar]
Narayanaswamy 2013 {published data only}
- Narayanaswamy A, Baskaran M, Zheng Y, Lavanya R, Wu R, Wong W L, et al. The prevalence and types of glaucoma in an urban Indian population: the Singapore Indian Eye Study. Investigative Ophthalmology and Visual Science 2013;54(7):4621-7. [DOI] [PubMed] [Google Scholar]
Ni 2014 {published data only}
- Ni Ni S, Tian J, Marziliano P, Wong HT. Anterior chamber angle shape analysis and classification of glaucoma in SS-OCT images. Journal of Ophthalmology 2014;2014:942367. [DOI] [PMC free article] [PubMed] [Google Scholar]
Niemeyer 2014 {published data only}
- Niemeyer M, Marion K, Sadda SR, Chopra V. Evaluation and comparison of novel anterior chamber angle metrics using two spectral domain OCT devices. Investigative Ophthalmology and Visual Science 2014;55(13):ARVO E-abstract 940.
Nongpiur 2010 {published data only}
- Nongpiur ME, Sakata LM, Friedman DS, He M, Chan YH, Lavanya R, et al. Novel association of smaller anterior chamber width with angle closure in Singaporeans. Ophthalmology 2010;117(10):1967-73. [DOI] [PubMed] [Google Scholar]
Nongpiur 2013 {published data only}
- Nongpiur ME, Haaland BA, Friedman DS, Perera SA, He M, Foo LL, et al. Classification algorithms based on anterior segment optical coherence tomography measurements for detection of angle closure. Ophthalmology 2013;120(1):48-54. [DOI] [PubMed] [Google Scholar]
Nongpiur 2014 {published data only}
- Nongpiur ME, Haaland BA, Perera SA, Friedman DS, He M, Sakata LM, et al. Development of a score and probability estimate for detecting angle closure based on anterior segment optical coherence tomography. American Journal of Ophthalmology 2014;157(1):32-8. [DOI] [PubMed] [Google Scholar]
Nongpiur 2017 {published data only}
- Nongpiur ME, Aboobakar IF, Baskaran M, Narayanaswamy A, Sakata LM, Wu R, et al. Association of baseline anterior segment parameters with the development of incident gonioscopic angle closure. JAMA Ophthalmology 2017;135(3):252-8. [DOI] [PubMed] [Google Scholar]
Nongpiur 2019 {published data only}
- Nongpiur ME, Khor CC, Cheng CY, Husain R, Boey PY, Chew A, et al. Integration of genetic and biometric risk factors for detection of primary angle-closure glaucoma. American Journal of Ophthalmology 2019;208:160-5. [DOI] [PubMed] [Google Scholar]
Nuriyah 2010 {published data only}
- Nuriyah Y, Ren XT, Jiang L, Liu XP, Zou YH. Comparison between ophthalmologists and community health workers in screening of shallow anterior chamber with oblique flashlight test. Chinese Medical Sciences Journal 2010;25(1):50-2. [DOI] [PubMed] [Google Scholar]
Pakravan 2012 {published data only}
- Pakravan M, Sharifipour F, Yazdani S, Koohestani N, Yaseri M. Scheimpflug imaging criteria for identifying eyes at high risk of acute angle closure. Journal of Ophthalmic and Vision Research 2012;7(2):111-7. [PMC free article] [PubMed] [Google Scholar]
Pei 2019 {published data only}
- Pei S, Liu D, Zhang B, An J, Shi J, Dai L. Detection of the anterior segment biological parameters of primary angle closure glaucoma and the normal eyes by optical coherence tomography. Chinese Journal of Experimental Ophthalmology 2019;37(2):117-22. [Google Scholar]
Pekmezci 2009 {published data only}
- Pekmezci M, Porco TC, Lin SC. Anterior segment optical coherence tomography as a screening tool for the assessment of the anterior segment angle. Ophthalmic Surgery, Lasers and Imaging 2009;40(4):389-98. [DOI] [PubMed] [Google Scholar]
Quek 2012 {published data only}
- Quek DT, Narayanaswamy AK, Tun TA, Htoon HM, Baskaran M, Perera SA, et al. Comparison of two spectral domain optical coherence tomography devices for angle-closure assessment. Investigative Ophthalmology and Visual Science 2012;53(9):5131-6. [DOI] [PubMed] [Google Scholar]
Ren 2005 {published data only}
- Ren BC, He Y, Chen L, Yang JG, Sun NX. Epidemiology of glaucoma in a rural population in Shaanxi Province. International Journal of Ophthalmology 2005;5(5):1037-42. [Google Scholar]
Rigi 2016 {published data only}
- Rigi M, Bell NP, Lee DA, Baker LA, Chuang AZ, Nguyen D, et al. Agreement between gonioscopic examination and swept source fourier domain anterior segment optical coherence tomography imaging. Journal of Ophthalmology 2016;2016:Article ID 1727039. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rojananuangnit 2016 {published data only}
- Rojananuangnit K, Salyapongse P. Ocular biometric parameters variation between closed and opened angles in Thai population. Investigative Ophthalmology and Visual Science 2016;57(12):ARVO E-abstract 3388.
Rueda 2003 {published data only}
- Rueda JG, Gomez R, Parra J, Ribero Moll SM, Orozco L, Vera L. Glaucoma screening in Colombian population. Investigative Ophthalmology and Visual Science 2003;44(13):ARVO E-abstract 3414.
Sah 2007 {published data only}
- Sah RP, Badhu BP, Pokharel PK, Thakur SK, Das H, Panda A. Prevalence of glaucoma in Sunsari district of eastern Nepal. Kathmandu University Medical Journal 2007;5(3):343-8. [PubMed] [Google Scholar]
Sakata 2007 {published data only}
- Sakata K, Sakata LM, Sakata VM, Santini C, Hopker LM, Bernardes R, et al. Prevalence of glaucoma in a South Brazilian population: Projeto Glaucoma. Investigative Ophthalmology and Visual Science 2007;48(11):4974-9. [DOI] [PubMed] [Google Scholar]
Sakata 2008 {published data only}
- Sakata, LM, Lavanya R, Friedman DS, Aung HT, Gao H, Kumar RS, et al. Comparison of gonioscopy and anterior segment ocular coherence tomography in detecting angle closure in different quadrants of the anterior chamber angle. Ophthalmology 2008;115(5):769-74. [DOI] [PubMed] [Google Scholar]
Sasikumar 2011 {published data only}
- Sasikumar R, Sathidevi AV, Dhanraj AR, Narendra KP, Balu R, Prabhu D, et al. Lens vault in Asian Indian eyes with angle closure. Investigative Ophthalmology and Visual Science 2011;52(14):ARVO E-abstract 6272.
Scalamogna 2002 {published data only}
- Scalamogna MO, Rueda J. Screening program with FDT, Tonopen and angular evaluation on a Latin American population. Investigative Ophthalmology and Visual Science 2002;43(13):ARVO E-abstract 3326.
Shibata 1992 {published data only}
- Shibata T, Takahashi N, Watanabe N. Measurements of anterior chamber depth and anterior chamber angle in narrow angle patients by image analysis. Rinsho Ganka 1992;46(3):328-9. [Google Scholar]
Shikino 2016 {published data only}
- Shikino K, Hirose Y, Ikusaka M. Oblique flashlight test: lighting up acute angle-closure glaucoma. Journal of General Internal Medicine 2016;31(12):1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sihota 2019 {published data only}
- Sihota R, Kamble N, Sharma AK, Bhari A, Gupta A, Midha N, et al. 'Van Herick Plus': a modified grading scheme for the assessment of peripheral anterior chamber depth and angle. British Journal of Ophthalmology 2019;103(7):960-5. [DOI] [PubMed] [Google Scholar]
Sparks 1997 {published data only}
- Sparks BI. Tangential penlight angle estimation. Journal of the American Optometric Association 1997;68(7):432-4. [PubMed] [Google Scholar]
Talaspayeva 2015 {published data only}
- Talaspayeva A. Biometric measures in Kazakh and European healthy subjects predisposing to angle closure glaucoma. Investigative Ophthalmology and Visual Science 2015;56(7):ARVO E-abstract 3692.
Tay 2015 {published data only}
- Tay EL, Yong VK, Lim BA, Sia S, Wong EP, Yip LW. Agreement of angle closure assessments between gonioscopy, anterior segment optical coherence tomography and spectral domain optical coherence tomography. International Journal of Ophthalmology 2015;8(2):342-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thompson 2018 {published data only}
- Thompson AC, Vu DM, Cowan LA, Asrani S. Risk factors associated with missed diagnoses of narrow angles by the Van Herick technique. Ophthalmology Glaucoma 2018;1(2):108-14. [DOI] [PubMed] [Google Scholar]
Tomoyose 2010 {published data only}
- Tomoyose E, Higa A, Sakai H, Sawaguchi S, Iwase A, Tomidokoro A, et al. Intraocular pressure and related systemic and ocular biometric factors in a population-based study in Japan: the Kumejima study. American Journal of Ophthalmology 2010;150(2):279-86. [DOI] [PubMed] [Google Scholar]
Trueba 2010 {published data only}
- Castillo AT, Bravo LJ, Valencia CC, Barragan MJ, Garcia RA. Is the flashlight test of any use in primary care for detecting eyes with shallow anterior chamber? Atencion Primaria 2010;42(3):149-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tun 2013 {published data only}
- Tun TA, Baskaran M, Zheng C, Sakata LM, Perera SA, Chan AS, et al. Assessment of trabecular meshwork width using swept source optical coherence tomography. Graefes Archive for Clinical and Experimental Ophthalmology 2013;251(6):1587-92. [DOI] [PubMed] [Google Scholar]
Vargas 1973 {published data only}
- Vargas E, Drance SM. Anterior chamber depth in angle-closure glaucoma. Clinical methods of depth determination in people with and without the disease. Archives of Ophthalmology 1973;90(6):438-9. [DOI] [PubMed] [Google Scholar]
Varma 2017 {published data only}
- Varma DK, Kletke SN, Rai AS, Ahmed II. Proportion of undetected narrow angles or angle closure in cataract surgery referrals. Canadian Journal of Ophthalmology 2017;52(4):366-72. [DOI] [PubMed] [Google Scholar]
Wang 2013 {published data only}
- Wang YE, Li Y, Wang D, He M, Lin S. Comparison of factors associated with occludable angle between American Caucasians and ethnic Chinese. Investigative Ophthalmology and Visual Science 2013;54(12):7717-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2014 {published data only}
- Wang GQ, Bai ZX, Luo S, Shi J, Shi Q, Cao LQ, et al. Characteristic of intraocular pressure distribution in population of 1115 Tibetan aged 40 years old or more. International Eye Science 2014;14(7):1181-5. [Google Scholar]
Wang 2015 {published data only}
- Wang J. Anterior chamber width, anterior chamber volume and their association with ocular and general parameters: The Beijing eye study. Investigative Ophthalmology and Visual Science 2015;56(7):ARVO E-abstract 5004.
Wong 2015 {published data only}
- Wong DW, Xu Y, Liu JJ, Mani B, Aung T. Automatic angle closure detection from 3D AS-OCT imaging (ACAI). Investigative Ophthalmology and Visual Science 2015;56(7):ARVO E-abstract 4974.
Xie 2011 {published data only}
- Xie TY, Gao L, Ai K, Fu J, Guo B, Yusufu M, et al. Epidemical survey of glaucoma among Uigur peasants aged 40 years or above in Kuche rural. Chinese Journal of Experimental Ophthalmology 2011;29(2):169-73. [Google Scholar]
Xu 2001 {published data only}
- Xu L, Yang H, Zhao X. A pilot study on rapid glaucoma screening. Chinese Journal of Ophthalmology 2001;37(1):16-20. [PubMed] [Google Scholar]
Xu 2004 {published data only}
- Xu L, Chen JH, Li JJ, Luo L, Yang H, Zhang RX, et al. The prevalence and its screening methods of primary open angle glaucoma in defined population-based study of rural and urban in Beijing. Chinese Journal of Ophthalmology 2004;40(11):726-32. [PubMed] [Google Scholar]
Xu 2005 {published data only}
- Xu L, Zhang L, Xia CR, Li JJ, Hu LN, Ma K, et al. The prevalence and its effective factors of primary angle-closure glaucoma in defined populations of rural and urban in Beijing. Chinese Journal of Ophthalmology 2005;41(1):8-14. [PubMed] [Google Scholar]
Xu 2008 {published data only}
- Xu L, Cao WF, Wang YX, Chen CX, Jonas JB. Anterior chamber depth and chamber angle and their associations with ocular and general parameters: the Beijing Eye Study. American Journal of Ophthalmogy 2008;145(5):929-36. [DOI] [PubMed] [Google Scholar]
Xu 2009 {published data only}
- Xu L, Li JJ, Xia CR, Wang YX, Jonas JB. Anterior chamber depth correlated with anthropomorphic measurements: the Beijing Eye Study. Eye 2009;23(3):632-4. [DOI] [PubMed] [Google Scholar]
Xu 2011 {published data only}
- Xu L, You QS, Wang YX, Jonas JB. Associations between gender, ocular parameters and diseases: The Beijing Eye Study. Ophthalmic Research 2011;45(4):197-203. [DOI] [PubMed] [Google Scholar]
Xu 2018 {published data only}
- Xu BY, Pardeshi AA, Burkemper B, Richter GM, Lin SC, McKean-Cowdin R, et al. Quantitative evaluation of gonioscopic and EyeCam assessments of angle dimensions using anterior segment optical coherence tomography. Translational Vision Science and Technology 2018;7(6):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Xu 2019a {published data only}
- Xu BY, Chiang M, Chaudhary S, Kulkarni S, Pardeshi AA, Varma R. Deep learning classifiers for automated detection of gonioscopic angle closure based on anterior segment OCT images. American Journal of Ophthalmology 2019;208:273-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Xu 2019b {published data only}
- Xu BY, Pardeshi AA, Burkemper B, Richter GM, Lin SC, McKean-Cowdin R, et al. Differences in anterior chamber angle assessments between gonioscopy, EyeCam, and anterior segment OCT: the Chinese American eye study. Translational Vision Science and Technology 2019;8(2):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yamamoto 2005 {published data only}
- Yamamoto T, Iwase A, Araie M, Suzuki Y, Abe H, Shirato S, et al. The Tajimi Study report 2: prevalence of primary angle closure and secondary glaucoma in a Japanese population. Ophthalmology 2005;112(10):1661-9. [DOI] [PubMed] [Google Scholar]
Yamamoto 2009 {published data only}
- Yamamoto T, Araie M, Iwase A, Kitazawa Y: Tajimi Study Group, Japan Glaucoma Society. A review of the Eye Health Care Project in Tajimi. Acta Societatis Ophthalmologicae Japonicae 2009;113(5):569-75. [PubMed] [Google Scholar]
Ye 1995 {published data only}
- Ye T, Mao W, Lu D. Comparison of simple methods to screen predisposing eye of primary angle-closure glaucoma. Chinese Journal of Ophthalmology 1995;31(5):341-4. [PubMed] [Google Scholar]
Ye 1998 {published data only}
- Ye T, Yu Q, Peng S, Wang N, Chen X. Six year follow-up of suspects of primary angle-closure glaucoma. Chinese Journal of Ophthalmology 1998;34(3):167-9. [PubMed] [Google Scholar]
Yip 2008 {published data only}
- Yip JL, Foster P, Gilbert CE, Uranchimeg D, Bassanhuu J, Lee PS, et al. Incidence of occludable angles in a high-risk Mongolian population. British Journal of Ophthalmology 2008;92(1):30-3. [DOI] [PubMed] [Google Scholar]
Yu 1995b {published data only}
- Yu Q, Li S, Ye T. The study of grading standard photos of oblique flashlight test. Eye Science 1995;11(2):80-5. [PubMed] [Google Scholar]
Yu 1996 {published data only}
- Yu Q, Li S, Ye T. Evaluation for grading standard of oblique flashlight test. Eye Science 1996;12(2):98-102. [PubMed] [Google Scholar]
Yu 1997 {published data only}
- Yu Q, Li S, Ye T. Cost-effectiveness analysis of the screening strategies for primary angle closure glaucoma. Eye Science 1997;13(4):202-9. [PubMed] [Google Scholar]
Yuan 2007 {published data only}
- Yuan HP, Yu H, Xiao Z, Shao ZB, Zhang XL, Yang BB, et al. The prevalence of primary angle-closure glaucoma and its causes in rural area of Shuangyang district in Changchun, Jilin province. Chinese Journal of Ophthalmology 2007;43(9):775-8. [PubMed] [Google Scholar]
Zhang 2008 {published data only}
- Zhang XL, Ren BC, He Y, Chen L, Sun NX, Yang JG. Observation study on the relationship between the asymmetry of intraocular tension and glaucoma without previous diagnosis and treatment in Shaanxi rural people aged above 50. International Journal of Ophthalmology 2008;8(6):1194-7. [Google Scholar]
Zhang 2010 {published data only}
- Zhang HT, Xu L, Cao WF, Wang YX, Jonas JB. Anterior segment optical coherence tomography of acute primary angle closure. Graefes Archive for Clinical and Experimental Ophthalmology 2010;248(6):825-31. [DOI] [PubMed] [Google Scholar]
Zhao 2008 {published data only}
- Zhao H, Chen XY, Li J, Zhao JF, Fu J, Yang KM. Analysis of the distribution characteristics and related factors of glaucoma in Urumchi. International Journal of Ophthalmology 2008;8(10):2079-81. [Google Scholar]
Additional references
Amerasinghe 2008
- Amerasinghe N, Aung T. Angle-closure: risk factors, diagnosis and treatment. Progress in Brain Research 2008;173:31-45. [DOI] [PubMed] [Google Scholar]
Azuara‐Blanco 2016
- Azuara-Blanco A, Burr J, Ramsay C, Cooper D, Foster PJ, Friedman DS, et al. Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): a randomised controlled trial. Lancet 2016;388(10052):1389-97. [DOI] [PubMed] [Google Scholar]
Bhargava 1973
- Bhargava SK, Leighton DA, Phillips CI. Early angle-closure glaucoma. Distribution of iridotrabecular contact and response to pilocarpine. Archives of Ophthalmology 1973;89(5):369-72. [DOI] [PubMed] [Google Scholar]
Cheng 2014
- Cheng JW, Zong Y, Zeng YY, Wei RL. The prevalence of primary angle closure glaucoma in adult Asians: a systematic review and meta-analysis. PLOS One 2014;9(7):e103222. [DOI] [PMC free article] [PubMed] [Google Scholar]
Clemmesen 1971
- Clemmesen V, Alsbirk PH. Primary angle-closure glaucoma in Greenland. Acta Ophthalmologica 1971;49(1):47-58. [DOI] [PubMed] [Google Scholar]
Day 2012
- Day AC, Baio G, Gazzard G, Bunce C, Azuara-Blanco A, Munoz B, et al. The prevalence of primary angle closure glaucoma in European derived populations: a systematic review. British Journal of Ophthalmology 2012;96(9):1162-7. [DOI] [PubMed] [Google Scholar]
Devereux 2000
- Devereux JG, Foster PJ, Baasanhu J, Uranchimeg D, Lee PS, Erdenbeleig T, et al. Anterior chamber depth measurement as a screening tool for primary angle-closure glaucoma in an East Asian population. Archives of Ophthalmology 2000;118(2):257-63. [DOI] [PubMed] [Google Scholar]
Emanuel 2014
- Emanuel ME, Parrish RK 2nd, Gedde SJ. Evidence-based management of primary angle closure glaucoma. Current Opinion in Ophthalmology 2014;25(2):89-92. [DOI] [PubMed] [Google Scholar]
Foster 2001
- Foster PJ, Johnson GJ. Glaucoma in China: how big is the problem? British Journal of Ophthalmology 2001;85(11):1277-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Foster 2002
- Foster PJ, Buhrmann R, Quigley HA, Johnson GJ. The definition and classification of glaucoma in prevalence surveys. British Journal of Ophthalmology 2002;86(2):238-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fu 2019
- Fu H, Baskaran M, Xu Y, Lin S, Wong DW, Liu J, et al. A deep learning system for automated angle-closure detection in anterior segment optical coherence tomography images. American Journal of Ophthalmology 2019;203:37-45. [DOI] [PubMed] [Google Scholar]
He 2006
- He M, Foster PJ, Johnson GJ, Khaw PT. Angle-closure glaucoma in East Asian and European people. Different diseases? Eye 2006;20(1):3-12. [DOI] [PubMed] [Google Scholar]
He 2019
- He M, Jiang Y, Huang S, Chang DS, Munoz B, Aung T, et al. Laser peripheral iridotomy for the prevention of angle closure: a single-centre, randomised controlled trial. Lancet 2019;393(10181):1609-18. [DOI] [PubMed] [Google Scholar]
Jindal 2015
- Jindal A, Myint J, Edgar DF, Nolan WP, Lawrenson JG. Agreement among optometrists and ophthalmologists in estimating limbal anterior chamber depth using the van Herick method. Ophthalmic and Physiological Optics 2015;35(2):179-85. [DOI] [PubMed] [Google Scholar]
Kang 2013
- Kang JJ, Allemann N, Cruz Jde L, Cortina MS. Serial analysis of anterior chamber depth and angle status using anterior segment optical coherence tomography after Boston keratoprosthesis. Cornea 2013;32(10):1369-74. [DOI] [PubMed] [Google Scholar]
Kashiwagi 2004
- Kashiwagi K, Kashiwagi F, Toda Y, Osada K, Tsumura T, Tsukahara S. A newly developed peripheral anterior chamber depth analysis system: principle, accuracy, and reproducibility. British Journal of Ophthalmology 2004;88(8):1030-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lowe 1970
- Lowe RF. Aetiology of the anatomical basis for primary angle-closure glaucoma. Biometrical comparisons between normal eyes and eyes with primary angle-closure glaucoma. British Journal of Ophthalmology 1970;54(3):161-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nolan 2003
- Nolan WP, Baasanhu J, Undraa A, Uranchimeg D, Ganzorig S, Johnson GJ. Screening for primary angle closure in Mongolia: a randomised controlled trial to determine whether screening and prophylactic treatment will reduce the incidence of primary angle closure glaucoma in an east Asian population. British Journal of Ophthalmology 2003;87(3):271-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Parivadhini 2014
- Parivadhini A, Lingam V. Management of secondary angle closure glaucoma. Journal of Current Glaucoma Practice 2014;8(1):25-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Quek 2011
- Quek DT, Nongpiur ME, Perera SA, Aung T. Angle imaging: advances and challenges. Indian Journal of Ophthalmology 2011;59 Suppl:S69-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Quigley 1996
- Quigley HA. Number of people with glaucoma worldwide. British Journal of Ophthalmology 1996;80(5):389-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Quigley 2006
- Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. British Journal of Ophthalmology 2006;90(3):262-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Resnikoff 2004
- Resnikoff S, Pascolini D, Etya'ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bulletin of the World Health Organization 2004;82(11):844-51. [PMC free article] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Scheie 1957
- Scheie HG. Width and pigmentation of the angle of the anterior chamber; a system of grading by gonioscopy. A.M.A. Archives of Ophthalmology 1957;58(4):510-2. [DOI] [PubMed] [Google Scholar]
Shaffer 1960
- Shaffer RN. Primary glaucomas. Gonioscopy, ophthalmoscopy and perimetry. Transactions - American Academy of Ophthalmology and Otolaryngology 1960;64:112-27. [PubMed] [Google Scholar]
Smith 2013
- Smith SD, Singh K, Lin SC, Chen PP, Chen TC, Francis BA, et al. Evaluation of the anterior chamber angle in glaucoma: a report by the American Academy of Ophthalmology. Ophthalmology 2013;120(10):1985-97. [DOI] [PubMed] [Google Scholar]
Spaeth 1971
- Spaeth GL. The normal development of the human anterior chamber angle: a new system of descriptive grading. Transactions of the Ophthalmological Societies of the United Kingdom 1971;91:709-39. [PubMed] [Google Scholar]
Takwoingi 2013
- Takwoingi Y, Leeflang MM, Deeks JJ. Empirical evidence of the importance of comparative studies of diagnostic test accuracy. Annals of Internal Medicine 2013;158(7):544-54. [DOI] [PubMed] [Google Scholar]
Tang 2019
- Tang J, Liang Y, O'Neill C, Kee F, Jiang J, Congdon N. Cost-effectiveness and cost-utility of population-based glaucoma screening in China: a decision-analytic Markov model. Lancet. Global Health 2019;7(7):e968-78. [DOI] [PubMed] [Google Scholar]
Tanner 2020
- Tanner L, Gazzard G, Nolan WP, Foster PJ. Has the EAGLE landed for the use of clear lens extraction in angle-closure glaucoma? And how should primary angle-closure suspects be treated? Eye 2020;34(1):40-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tham 2014
- Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology 2014;121(11):2081-90. [DOI] [PubMed] [Google Scholar]
Thomas 2003
- Thomas R, George R, Parikh R, Muliyil J, Jacob A. Five year risk of progression of primary angle closure suspects to primary angle closure: a population based study. British Journal of Ophthalmology 2003;87(4):450-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Van Herick 1969
- Van Herick W, Shaffer RN, Schwartz A. Estimation of width of angle of anterior chamber. Incidence and significance of the narrow angle. American Journal of Ophthalmology 1969;68(4):626-9. [DOI] [PubMed] [Google Scholar]
Wang 2019
- Wang L, Huang W, Huang S, Zhang J, Guo X, Friedman DS, et al. Ten-year incidence of primary angle closure in elderly Chinese: the Liwan Eye Study. British Journal of Ophthalmology 2019;103(3):355-60. [DOI] [PubMed] [Google Scholar]
Weinreb 2006
- Weinreb RN, Friedman DS. Angle Closure and Angle Closure Glaucoma. 1st edition. The Hague, The Netherlands: Kugler Publications, 2006. [Google Scholar]
Whiting 2011
- Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Annals of Internal Medicine 2011;155(8):529-36. [DOI] [PubMed] [Google Scholar]
Wilensky 1993
- Wilensky JT, Kaufman PL, Frohlichstein D, Gieser DK, Kass MA, Ritch R, et al. Follow-up of angle-closure glaucoma suspects. American Journal of Ophthalmology 1993;115(3):338-46. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Jindal 2018
- Jindal A, Ctori I, Virgili G, Lucenteforte E, Lawrenson JG. Non-contact methods for the detection of people at risk of primary angle closure glaucoma. Cochrane Database of Systematic Reviews 2018, Issue 2. Art. No: CD012947. [DOI: 10.1002/14651858.CD012947] [DOI] [PMC free article] [PubMed] [Google Scholar]


