Abstract
Background
Helmets reduce bicycle‐related head injuries, particularly in single vehicle crashes and those where the head strikes the ground. We aimed to identify non‐legislative interventions for promoting helmet use among children, so future interventions can be designed on a firm evidence base.
Objectives
To assess the effectiveness of non‐legislative interventions in increasing helmet use among children; to identify possible reasons for differences in effectiveness of interventions; to evaluate effectiveness with respect to social group; to identify adverse consequences of interventions.
Search methods
We searched the following databases: Cochrane Injuries Group Specialised Register; the Cochrane Central Register of Controlled Trials (CENTRAL); MEDLINE; EMBASE; PsycINFO (Ovid); PsycEXTRA (Ovid); CINAHL (EBSCO); ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED); Social Sciences Citation Index (SSCI); Conference Proceedings Citation Index‐Science (CPCI‐S); and PubMed from inception to April 2009; TRANSPORT to 2007; and manually searched other sources of data.
Selection criteria
We included RCTs and CBAs. Studies included participants aged 0 to 18 years, described interventions promoting helmet use not requiring enactment of legislation and reported observed helmet wearing, self reported helmet ownership or self reported helmet wearing.
Data collection and analysis
Two independent review authors selected studies for inclusion and extracted data. We used random‐effects models to estimate pooled odds ratios (ORs) (with 95% confidence interval (CI)). We explored heterogeneity with subgroup analyses.
Main results
We included 29 studies in the review, 21 of which were included in at least one meta‐analysis. Non‐legislative interventions increased observed helmet wearing (11 studies: OR 2.08, 95% CI 1.29 to 3.34). The effect was most marked amongst community‐based interventions (four studies: OR 4.30, 95% 2.24 to 8.25) and those providing free helmets (two studies: OR 4.35, 95% CI 2.13 to 8.89). Significant effects were also found amongst school‐based interventions (eight studies: OR 1.73, CI 95% 1.03 to 2.91), with a smaller effect found for interventions providing education only (three studies: OR 1.43, 95% CI 1.09 to 1.88). No significant effect was found for providing subsidised helmets (seven studies: OR 2.02, 95% CI 0.98 to 4.17). Interventions provided to younger children (aged under 12) may be more effective (five studies: OR 2.50, 95% CI 1.17 to 5.37) than those provided to children of all ages (five studies: OR 1.83, 95% CI 0.98 to 3.42).
Interventions were only effective in increasing self reported helmet ownership where they provided free helmets (three studies: OR 11.63, 95% CI 2.14 to 63.16).
Interventions were effective in increasing self reported helmet wearing (nine studies: OR 3.27, 95% CI 1.56 to 6.87), including those undertaken in schools (six studies: OR 4.21, 95% CI 1.06 to 16.74), providing free helmets (three studies: OR 7.27, 95% CI 1.28 to 41.44), providing education only (seven studies: OR 1.93, 95% CI 1.03 to 3.63) and in healthcare settings (two studies: OR 2.78, 95% CI 1.38 to 5.61).
Authors' conclusions
Non‐legislative interventions appear to be effective in increasing observed helmet use, particularly community‐based interventions and those providing free helmets. Those set in schools appear to be effective but possibly less so than community‐based interventions. Interventions providing education only are less effective than those providing free helmets. There is insufficient evidence to recommend providing subsidised helmets at present. Interventions may be more effective if provided to younger rather than older children. There is evidence that interventions offered in healthcare settings can increase self reported helmet wearing.
Further high‐quality studies are needed to explore whether non‐legislative interventions increase helmet wearing, and particularly the effect of providing subsided as opposed to free helmets, and of providing interventions in healthcare settings as opposed to in schools or communities. Alternative interventions (e.g. those including peer educators, those aimed at developing safety skills including skills in decision making and resisting peer pressure or those aimed at improving self esteem or self efficacy) need developing and testing, particularly for 11 to 18 year olds. The effect of interventions in countries with existing cycle helmet legislation and in low and middle‐income countries also requires investigation.
Keywords: Adolescent; Child; Child, Preschool; Humans; Bicycling; Bicycling/legislation & jurisprudence; Bicycling/statistics & numerical data; Craniocerebral Trauma; Craniocerebral Trauma/prevention & control; Head Protective Devices; Head Protective Devices/statistics & numerical data; Head Protective Devices/supply & distribution; Program Development
Plain language summary
Campaigns to encourage children to wear cycle helmets
Many children suffer head injuries while riding a bike. This review focused on encouraging children to wear helmets, as distinct from compelling them to do so through laws. The authors wanted to find out which sort of helmet programmes work best, particularly with children from poor families who are less likely to own helmets. They found 29 helmet promotion programmes that had been studied. The programmes varied widely with regard to where they were carried out, age of the children, programme methods, etc. The results were also very varied but overall 11 studies found that after a helmet programme children were more likely to be observed wearing helmets than other children. More research is still needed but it seems likely that the best schemes are based in the community and involve both education and providing free helmets. Promotion of helmets in schools also seems to be effective. Promoting helmets appears to be more effective for younger children (aged 12 years and under) than for older children and young people. The studies reviewed did not look at the impact of helmet programmes on injury rates, or assess whether programmes had any negative effects such as reducing cycling. Most of the studies were undertaken in higher‐income countries and the additional effect of helmet promotion above existing legislation was not explored. More research is needed to understand more about whether providing subsidised helmets is as effective as providing free helmets and whether programmes in healthcare settings are as effective as those in schools or communities. Other types of helmet programmes (e.g. those including peer educators, those developing skills such as decision making and resisting peer pressure, or improving self esteem or self efficacy) need developing and testing, particularly for 11 to 18 year olds. The effect of helmet programmes in countries with existing cycle helmet legislation and in low and middle‐income countries also requires investigation.
Background
Injuries to child cyclists are an important public health problem. On British roads, in 2009, 545 children were killed or seriously injured while cycling (DfT 2010). Forty‐five per cent of child cyclists admitted to hospital for cycling injures between 1999 and 2005 sustained a head injury (Hynd 2009). There is a steep social class gradient for cycling injuries in childhood, with mortality rates in children from social class five being four times higher than those from social class one (Roberts 1997). Hospital admission rates for cycling injuries have also been found to be 61% higher amongst children residing in deprived wards compared to those in affluent wards (Hippisley‐Cox 2002).
There is evidence that cycle helmets reduce head injuries (Hynd 2009; Thompson 1999; Towner 1992), particularly in single vehicle accidents, or accidents that cause the head of the cyclist to strike the ground (Hynd 2009). It has also been suggested that cycle helmets may be particularly effective in children who tend to fall a shorter distance, and which is more likely to be within the distance used in the European Standard Impact Test for Cycle Helmets (EW1078) (Hynd 2009).
Several studies suggest bicycle helmets are used less commonly amongst children from socio‐economically deprived backgrounds (Farley 1996; Parkin 1993). Other factors may also be important in encouraging children to wear cycle helmets, including peer pressure, parental helmet use and school policies (Lajunen 2001).
Many authors have described bicycle helmet promotion programmes that aim to encourage children to wear helmets, but the programmes have varied widely in terms of their effectiveness and the strategies employed. It is difficult, therefore, to know from individual studies how effective cycle helmet promotion programmes have been, which elements of the programmes contribute to their effectiveness, and whether the effect is similar in different social groups or settings. This information is vital for planning and delivering effective cycle helmet programmes in the future. The aim of this review is to identify those non‐legislative interventions that are effective in promoting helmet use among children, so that future interventions can be designed from a firm evidence base.
Objectives
The objectives of this review were to:
assess the effectiveness of non‐legislative interventions in increasing bicycle helmet use among children;
identify possible reasons for differences in the effectiveness of interventions;
evaluate the effectiveness of these interventions with respect to social group;
identify any adverse consequences or effects of interventions.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials.
Trials with concurrent controls.
Controlled before‐after studies.
Types of participants
Children and adolescents aged between 0 and 18 years.
Types of interventions
Interventions designed to promote bicycle helmet use that did not require the enactment of legislation including:
health education programmes;
subsidised or free helmet distribution programmes;
media campaigns;
interventions that included elements of the above.
We excluded interventions that included legislation as a component. There has been a recent Cochrane review addressing legislation and the wearing of cycle helmets (Macpherson 2008).
Types of outcome measures
Observed bicycle helmet wearing.
Self reported bicycle helmet ownership.
Self reported bicycle helmet wearing.
Search methods for identification of studies
Searches were not restricted by date, language or publication status.
Electronic searches
We searched the following electronic databases:
Cochrane Injuries Group Specialised Register (searched 3 April 2009);
Cochrane Central Register of Controlled Trials (CENTRAL) (www.thecochranelibrary.com) (accessed 3 April 2009);
MEDLINE (Ovid)1950 to March, week 4 2009;
EMBASE (Ovid) 1980 to week 13, March 2009;
PsycINFO (Ovid) 1806 to March Week 5 2009;
PsycEXTRA (Ovid) 1908 to March 24, 2009;
CINAHL (EBSCO)1982 to March 2009;
ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) 1970 to March 2009, Social Sciences Citation Index (SSCI) 1970 to March 2009, Conference Proceedings Citation Index ‐ Science (CPCI‐S) 1990 to March 2009;
PubMed (last six months; searched 6 April 2009);
TRANSPORT 1988 to 2007/06
Search strategies are reported in full in Appendix 1
Searching other resources
We examined the reference lists of relevant reviews and included studies. We searched the following cycling‐related websites:
Helmet Resource Library (www.sph.emory.edu/Helmets/helmets.html);
National Bicycle Safety Network (www.cdc.gov/ncipc/bike/referenc.htm);
Bicycle Helmet Initiative Trust (www.bhit.org/).
We handsearched the conference proceedings abstracts of the World Conference on Injury Prevention and Safety Promotion between 1989 and 2008 for relevant studies. We also handsearched the journal Injury Prevention from 1995 to April 2009.
Data collection and analysis
The Injuries Group Trials Search Co‐ordinator ran the searches and collated the results before passing them on to the authors for screening.
Selection of studies
Two review authors independently inspected the titles and abstracts to determine whether they met the inclusion criteria. We rejected abstracts that did not meet the inclusion criteria. Two independent review authors assessed full copies of papers that appeared to meet the inclusion criteria. Uncertainties concerning the appropriateness of studies for inclusion in the review were resolved through consultation with a third review author. We translated non‐English language studies and included them if they met the inclusion criteria.
Data extraction and management
We designed a standard data extraction form and used it to extract data on participants, socio‐economic characteristics, interventions and outcomes. Two researchers independently extracted and compared data. Any discrepancies were identified and resolved at a meeting of the review authors. We took special care to avoid the inclusion of multiple reports pertaining to the same individuals, for example in trials reporting outcomes over multiple time periods. Where data were not available in the published study reports, we contacted authors to supply missing information.
Assessment of risk of bias in included studies
For randomised controlled trials, we used allocation concealment, blinding of outcome assessment and completeness of follow‐up as the three markers of trial quality. The number of randomised controlled trials included in the review was too small to allow a sensitivity analysis based on these three quality markers. For non‐randomised controlled trials, we used blinding of outcome assessment and completeness of follow‐up as markers of quality, plus assessment of the distribution of confounders. Two review authors assessed quality independently and disagreements were resolved through consultation with a third review author. Findings in relation to quality markers for randomised and non‐randomised studies are reported in the table describing the Characteristics of included studies.
Measures of treatment effect
We pooled results by outcome and presented them as odds ratios (ORs) and 95% confidence intervals (CIs). We performed all analyses using RevMan software (RevMan 2011) with random‐effects models to allow for and quantify the degree of statistical heterogeneity present between individual studies (DerSimonian 1986). Where cluster‐randomised trials were reported without appropriate adjustment for clustering, we approached the authors to obtain information on the intra‐class correlation coefficient (ICC) or to obtain data from which we could calculate an ICC. Since none of the studies had either calculated an ICC or did not provide us with data from which we could calculate the ICC, we adjusted the reported treatment effect for clustering using an ICC of 0.02 as reported in a school‐based health promotion intervention (Murray 2004). We also undertook sensitivity analyses using ICCs of 0.01 and 0.05 because we believe they represent the extremes of a range within which the true value is likely to be found (Adams 2004; Ukoumunne 1999).
A subgroup analysis comparing treatment effect by social group was not possible, as only three studies (Hendrickson 1998; Kendrick 2004; Parkin 1995) were undertaken with participants from low‐income communities and these measured different outcomes, and one had a non‐comparable control group (Kendrick 2004). Two further studies reported their results stratified by income (DiGuiseppi 1989; Farley 1996) but these used different measures of income level, hence pooling of results was not possible.
Assessment of heterogeneity
We explored heterogeneity between the results of included studies using Chi2 tests with a P value of 0.1 taken as indicating significant heterogeneity. We explored the reasons for any heterogeneity with subgroup analyses.
Assessment of reporting biases
We explored the possibility of publication bias using funnel plots and Egger's test (Egger 1997; Egger 1998).
Sensitivity analysis
We assessed the individual contribution of each study to the pooled result graphically. We assessed the robustness of the findings with respect to study quality by comparing the pooled treatment effect from randomised controlled trials with the treatment effect derived from all study designs.
Results
Description of studies
Figure 1 is a QUOROM flow diagram describing the process of study selection. We included 29 studies in the review and they are described in the Characteristics of included studies table. Six were individually randomised controlled trials, eight were cluster‐randomised controlled trials, 14 were controlled before‐after studies and one was a quasi‐randomised trial. Eighteen studies were set in the US, six in Canada, three in the UK, one in Australia and one in New Zealand. One study (Britt 1998) only included pre‐school children and a second included children aged between five and eight years (Liller 1995). The remainder included children from a range of ages up to 18 years. Thirteen studies focused on children of primary school age, seven on children of secondary school age and nine spanned both school ranges. Four studies involved participants in community settings, six in healthcare settings and the remaining 19 in schools. Nine interventions included the distribution of free helmets, 11 provided subsidised helmets and nine provided purely educational interventions. Those providing free or subsidised helmets also included an element of cycle helmet education. Fourteen studies reported observed helmet wearing as an outcome, 10 included self reported helmet ownership and 17 self reported helmet wearing. Many studies reported more than one outcome.
1.
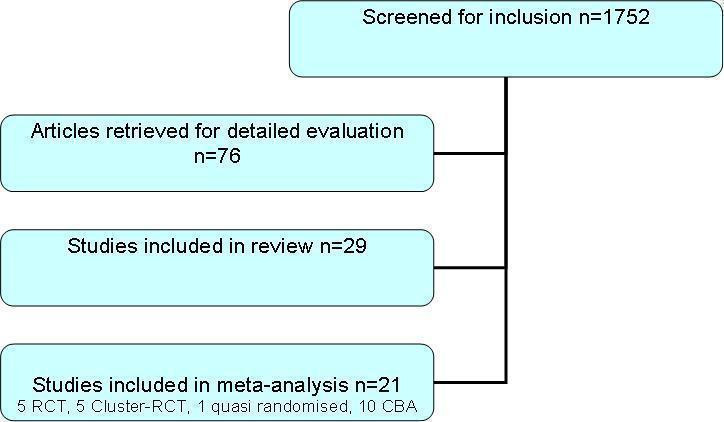
Study retrieval and selection process.
Data extracted from Azeredo 2003, Kim 1997, Lee 2000, Moore 1990, Pendergrast 1992 and Watts 1997 were not included in the meta‐analysis because they were not available as numerators and denominators in each arm, either from the original paper or the authors. Leverence 2004 was not included as the results were reported as a mean of a Likert scale. Kendrick 2004 had no comparable control group. The remaining studies contributed data to at least one meta‐analysis, but we also excluded some data from the following studies because they were not available as numerators and denominators in each arm: Cote 1992; Hendrickson 1998; Parkin 1995; Quine 2001; Wright 1995. Six studies provided data from more than one time point. We extracted all the data but in the meta‐analysis we have only used results at four months from DiGuiseppi 1989, results at one year from Farley 1996 and from Hall 2004, results at six weeks from Hendrickson 1998, results at six months for Johnston 2002 and results at 19 weeks from Towner 1992, in order to optimise comparability.
Risk of bias in included studies
Comments on the important methodological features of each study are presented in the table of Characteristics of included studies. None of the cluster‐randomised controlled trials or controlled before‐after studies made any adjustment for a clustering effect in the data presented. The larger community‐based studies, such as DiGuiseppi 1989 and Farley 1996, were of controlled before‐after design, for obvious practical reasons. Four of the RCTs recruited participants in a healthcare setting (Cushman 1991a; Cushman 1991b; Johnston 2002; Wu 2005) and two were school‐based studies (Quine 2001; Towner 1992). Few of the studies that used randomisation described this in sufficient detail for us to comment on the adequacy of concealment of the allocation. Among non‐randomised studies, two studies included in the meta‐analysis did not report on the distribution of confounders (Britt 1998; Floerchinger 2000). The remaining studies commented on equivalence in the text or presented data demonstrating comparability of the groups at baseline.
Effects of interventions
Adverse effects of interventions
None of the included studies reported any adverse effects of interventions.
Observed helmet wearing
Eleven studies were included in the meta‐analysis. The odds of observed helmet wearing were significantly higher amongst those receiving non‐legislative interventions promoting cycle helmet use (odds ratio (OR) 2.08, 95% confidence interval (CI) 1.29 to 3.34) than amongst those not receiving such interventions. There was significant heterogeneity between effect sizes of the studies included in this analysis (Chi2 = 30.34, degrees of freedom (df) = 10, P = 0.0008). The findings were robust to assuming intra‐class correlation coefficients (ICCs) of 0.01 and 0.05 for studies using cluster allocation and Figure 2 illustrates that publication bias was not detected (regression coefficient = 0.33, SE = 1.11, Egger's test P = 0.77).
2.
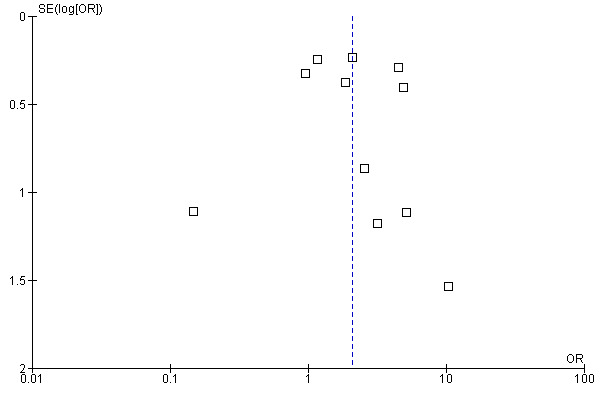
Funnel plot of comparison: 1 Non‐legislative interventions vs control, outcome: 1.1 Observed helmet wearing.
We assessed the effect of study quality by restricting analyses to the three randomised controlled trials reporting this outcome and no significant effect was demonstrated (OR 0.99, 95% CI 0.18 to 5.63).
As there was significant heterogeneity amongst effect sizes, we undertook subgroup analyses to explore possible explanations for this. These included examining the effect by setting (community or school), type of intervention (free helmet, subsidised helmet or education only) and age (younger (≤ 12 years), older (≥ 11 years) or all ages (0 to 18 years)). We chose these subgroups as it seemed theoretically plausible that these factors might influence the effectiveness of the intervention.
Non‐legislative interventions appeared to be effective in both community (four studies: OR 4.30, 95% CI 2.24 to 8.25; Chi2 = 0.72, df = 3, P = 0.87) and school‐based settings (eight studies: OR 1.73, 95% CI 1.03 to 2.91; Chi2 = 23.79, df = 7, P = 0.001), with a possibly greater effect amongst those in community settings. Providing free helmets (two studies: OR 4.35, 95% CI 2.13 to 8.89; Chi2 = 0.47, df = 1, P = 0.49) was more effective than providing education only (three studies: OR 1.43, 95% CI 1.09 to 1.88; Chi2 = 1.29, df = 2, P = 0.53). The effect of providing subsidised helmets failed to reach statistical significance and there was significant heterogeneity between effect sizes (seven studies: OR 2.02, 95% CI 0.98 to 4.17; Chi2 = 20.29, df = 6, P = 0.002). Interventions focusing on younger children (aged 12 years and under) were effective (five studies: OR 2.50, 95% CI 1.17 to 5.37; Chi2 = 12.46, df = 4, P = 0.01), whilst those including children and young people of all ages (0 to 18 years) failed to demonstrate a significant effect (five studies: OR 1.83, 95% CI 0.98 to 3.42; Chi2 = 6.63, df = 4, P = 0.16). Only one study (Hall 2004) focused only on older children and young people (aged 11 to 18 years) and this failed to demonstrate a significant effect (OR 1.14, 95% CI 0.87 to 1.51).
Sensitivity analyses indicated that all subgroup analyses were robust to assuming ICCs of 0.01 and 0.05 for studies using cluster allocation, except when assuming an ICC of 0.05 when the effect of providing education only became non‐significant (OR 1.43, 95% CI 0.96 to 2.15) and that of providing subsidised helmets became significant (OR 2.00, 95% CI 1.03 to 3.98).
Self reported helmet ownership
Seven studies were included in the meta‐analysis. No significant effect of non‐legislative interventions was found for self reported helmet ownership (OR 2.67, 95% CI 0.89 to 8.03) compared to no intervention and there was significant heterogeneity between effect sizes (Chi2 = 64.75, df = 6, P < 0.00001). The findings were robust to assuming ICCs of 0.01 and 0.05 for studies using cluster allocation and Figure 3 illustrates that publication bias was not detected (regression coefficient = 5.41, SE = 5.66, Egger's test P = 0.38).
3.
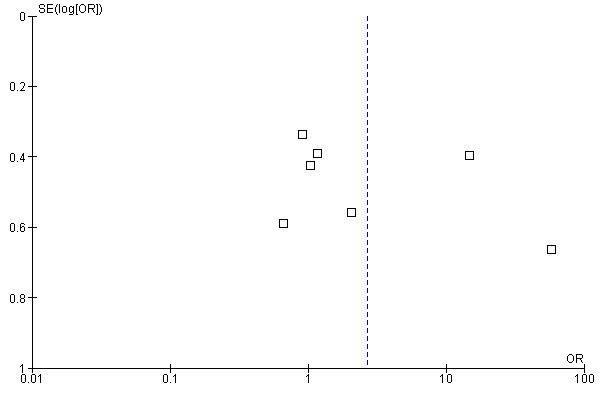
Funnel plot of comparison: 1 Non‐legislative interventions vs control, outcome: 1.2 Self reported helmet ownership.
Amongst the four randomised controlled trials, no significant effect of non‐legislative interventions was found (OR 1.58, 95% CI 0.66 to 3.77) compared to those not receiving such interventions and there was significant heterogeneity between effect sizes (Chi2= 16.92, df = 3, P = 0.0007).
We again undertook subgroup analyses to explore heterogeneity in effect sizes. Interventions providing free helmets were effective in increasing self reported helmet ownership (three studies: OR 11.63, 95% CI 2.14 to 63.16; Chi2 = 15.94, df = 2, P = 0.0003) but there was significant heterogeneity between effect sizes. Providing community‐based interventions (two studies: OR 5.65, 95% CI 0.82 to 38.98; Chi2 = 8.37, df = 1, P = 0.004), school‐based interventions (three studies: OR 1.03, 95% CI 0.60 to 1.76; Chi2 = 2.10, df = 2, P = 0.33) or interventions in healthcare settings (three studies: OR 3.84, 95% CI 0.46 to 32.36; Chi2 = 31.53, df = 2, P = < 0.00001) did not appear to be effective.
Providing education only did not appear to be effective (three studies: OR 1.00, 95% CI 0.60 to 1.66; Chi2 = 0.66, df = 2, P = 0.72) and the age of the children to whom interventions were provided also appeared to have no significant effect (studies focusing on children 12 years or under (four studies: OR 2.09, 95% CI 0.47 to 9.25; Chi2 = 33.89, df = 3, P = < 0.00001) and studies including children and young people of all ages (0 to 18 years) (three studies: OR 3.84, 95% CI 0.46 to 32.36; Chi2 = 31.53, df = 2, P = < 0.00001).
Sensitivity analyses indicated that all subgroup analyses were robust to assuming ICCs of 0.01 and 0.05 for studies using cluster allocation.
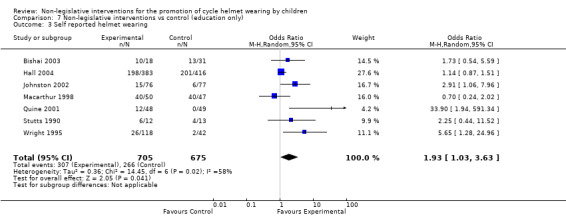
Self reported helmet wearing
Nine studies were included in the meta‐analysis. The odds of self reported helmet wearing were significantly greater amongst those receiving interventions (OR 3.27, 95% CI 1.56 to 6.87) compared to those receiving no intervention but there was significant heterogeneity between the effect sizes (Chi2 = 53.23, df = 8, P = < 0.00001). These results were robust to assuming ICCs of 0.01 and 0.05 for studies using cluster allocation. Figure 4 shows evidence of publication bias for this outcome (regression coefficient = 2.64, SE = 1.12, Egger's test P = 0.05).
4.
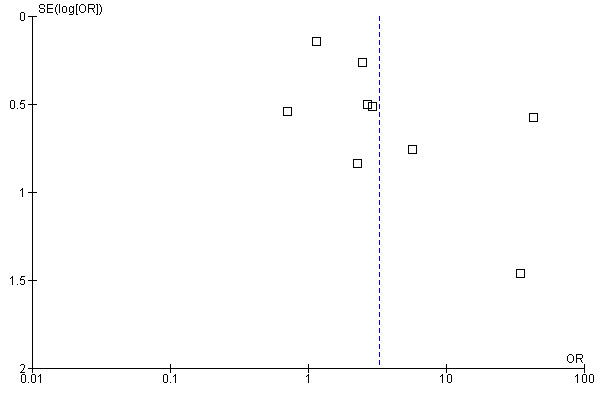
Funnel plot of comparison: 1 Non‐legislative interventions vs control, outcome: 1.3 Self reported helmet wearing.
Amongst the five randomised controlled trials, the odds of self reported helmet wearing were not significantly greater in those receiving interventions (OR 3.02, 95% CI 0.72 to 12.76) and there was evidence of significant heterogeneity between effect sizes (Chi2 = 46.28, df = 4, P < 0.00001).
We undertook subgroup analyses to explore the heterogeneity. Interventions set in schools (six studies: OR 4.21, 95% CI 1.06 to 16.74; Chi2 = 48.58, df = 5, P < 0.00001) and in healthcare settings (two studies: OR 2.78, 95% CI 1.38 to 5.61; Chi2 = 0.02, df = 1, P = 0.90) were both effective in increasing self reported helmet wearing. Those providing free helmets (three studies: OR 7.27, 95% CI 1.28 to 41.44; Chi2 = 10.26, df = 2, P = 0.006) and those providing education only (seven studies: OR 1.93, 95% CI 1.03 to 3.63; Chi2 = 14.45, df = 6, P = 0.02) were also both effective, with possibly a greater effect in those providing free helmets. Interventions which focused on older children and young people only (aged 11 years and older) were effective (three studies: OR 4.99, 95% CI 1.68 to 14.83; Chi2 = 2.98, df = 2, P = 0.22), whilst those focusing on younger children (aged 12 years or under) (four studies: OR 1.44, 95% CI 0.82 to 2.51; Chi2 = 8.38, df = 3, P = 0.04), or those including children and young people (0 to 18 years) (two studies: OR 10.48, 95% CI 0.69 to 158.51; Chi2 = 13.20, df = 1, P = 0.003) failed to demonstrate a significant effect. All subgroup analyses were robust to assuming ICCs of 0.01 and 0.05 for studies using cluster allocation.
Studies not included in the meta‐analyses
Eight studies satisfied our inclusion criteria but could not be included the meta‐analyses for reasons described in the table of Characteristics of included studies. Azeredo 2003, reporting the results of a school‐based programme of education and school bicycle fairs with give‐away helmets, reported that observed helmet wearing increased from 0% to 10% from baseline to follow‐up in intervention schools, but observations of cycle helmets were not made in control schools. Kendrick 2004 found that a helmet and an education pack was as effective as a helmet and a multifaceted intervention in terms of helmet ownership (OR 1.51, 95% CI 0.50 to 4.58) and wearing (OR 0.98, 95% CI 0.57 to 1.68). This study also found that providing free helmets and school‐based education to children in schools in disadvantaged areas reduced inequalities in helmet ownership that existed prior to the intervention. Kim 1997 reported an adjusted odds ratio for helmet use comparing co‐payment with free helmets of 1.66 (95% CI 0.94 to 2.92). They concluded that helmet use was not significantly different among children whose parents were asked for a small copayment compared with those receiving free helmets. Lee 2000 reported an increase in self reported helmet use among 11 to 15 year olds living in the campaign area from 11% to 31% after five years (P < 0.001), with no change in the control group. Leverence 2004 did not report a significant improvement from baseline in self reported cycle helmet use in either the intervention (mean difference 0; 95% CI ‐0.3 to 0.2) or control group (mean difference ‐0.02, 95% CI ‐0.3 to 0.3). Moore 1990 reported a significant increase in observed helmet wearing from a baseline of 3.5% in the intervention group to 33.3% at 10 weeks. In the control group there was a non‐significant increase from 6.3% to 10.9%. Pendergrast 1992 did not report significant changes in self reported helmet ownership or wearing over the course of their intervention. Watts 1997 reported a significant increase in helmet use among children given a free helmet (P < 0.01) that was not found among children who only received an educational intervention.
Discussion
Main findings
This systematic review has identified 29 studies of non‐legislative interventions to promote the wearing of bicycle helmets by school children. The studies varied widely in a number of important characteristics including: setting, age of participants, components of the intervention, length of follow‐up and outcomes reported. This 'clinical' heterogeneity was reflected in statistical heterogeneity when results were pooled in many of the meta‐analyses.
Focusing on observed helmet wearing, as this is the most objective outcome measure, we have found that non‐legislative interventions appear to be effective. However, we found no significant effect when restricting analyses to randomised controlled trials (RCTs), although this analysis only included three studies. Subgroup analyses indicated that community‐based and school‐based interventions are both effective in increasing observed helmet wearing, with possibly a greater effect seen with community‐based interventions. Providing free helmets is more effective than providing education only and possibly more effective than providing subsidised helmets. Interventions provided to younger children were effective, whilst those provided to older children and young people were not.
Less emphasis should be placed on our findings using self reported outcomes because of the possibility of differential social desirability bias between treatment arms in included studies. For self reported helmet ownership we found a significant effect favouring the intervention group only where free helmets were provided. For self reported helmet wearing we found significant effects favouring the intervention group for any non‐legislative intervention, for school‐based interventions, for those delivered in healthcare settings, for those providing free helmets, for those providing education only and for those provided to older children and young people. No significant effects were found when analyses were restricted to RCTs for both self reported helmet ownership or wearing.
New subgroup analyses undertaken in the update to this review include interventions in healthcare settings and interventions by child age. The few studies included in the meta‐analysis for healthcare settings understandably relied on self reported outcomes. Wu 2005 showed a very positive effect, demonstrating that providing free helmets may be a beneficial intervention in this setting. A brief intervention, which is often the most appealing to health professionals, failed to demonstrate an effect (Leverence 2004), whilst slightly longer counselling provided in the Bishai 2003 and Johnston 2002 studies showed significant increases in reported helmet wearing. Further studies are needed in heathcare settings to determine whether non‐legislative interventions are effective, and the components of effective interventions. In terms of the most effective age at which to intervene, our findings suggest that providing interventions to children aged 12 and under is likely to be more effective than providing them to older children and young people. The positive effect on self reported helmet wearing seen in older children and young people may represent social desirability bias which may be more likely to operate amongst older than younger children. Alternative interventions need to be developed and tested to explore increasing helmet use in older children and young people. Most studies had relatively short follow‐up periods, hence the duration of the effectiveness of interventions provided to younger children is unknown. It is possible that the effect may diminish both over time and with increasing child age. Studies investigating the effectiveness of interventions amongst younger children with longer follow‐up periods are therefore required.
In the meta‐analysis and subgroup analyses of studies using self reported helmet ownership as an outcome, Britt 1998 stands out because of its positive results. This study was unique in that it was confined to a younger age group than any of the other studies, and also in that it was the participants' parents rather than the participants themselves that reported helmet ownership. Hence it is possible that parents may have over‐reported their children's helmet ownership. Also this non‐randomised study did not report on the distribution of confounders, hence it is possible that differences between the treatment groups may partly explain the positive findings.
Several studies found negative effects of the intervention (Johnston 2002; Macarthur 1998; Stutts 1990; Towner 1992 ). The study by Towner 1992 had a very low follow‐up rate, suggesting that attrition bias may have occurred, which must be taken into account when considering these results. The studies by Stutts 1990, Macarthur 1998 and Johnston 2002 only provided education and our review did not analyse the amount, quality or style of the education given, and this may partly explain these findings. Further studies exploring the effect of specific educational packages would be helpful in elucidating which elements are least and most effective, but as we found the effect of providing education only was significantly smaller than providing free helmets, future helmet promotion programmes should provide free helmets as part of their intervention. The type of education provided with free helmets requires further exploration, as Kendrick 2004 found no significant difference between providing education and a free helmet and providing more intense multifaceted education and a free helmet.
There was evidence of publication bias in the meta‐analysis for self reported helmet wearing. This suggests the possible existence of unpublished studies with negative findings, which would tend to reduce the apparent effectiveness of non‐legislative interventions on self reported helmet wearing. As discussed above, there may be considerable potential for differential social desirability bias in the reporting of this outcome. Such bias may have contributed to the apparent lack of studies with negative effects in this analysis. One must also consider the impact of legislation in the study by Hall 2004 set in Australia, as the background rate of helmet wearing is likely to be higher in countries that have imposed legislation, leading to a potential ceiling effect.
Several subgroup analyses included only a small number of studies and a relatively small number of study participants which lead to imprecise estimates of the effect of interventions. This was particularly true of the subgroup analyses relating to randomised controlled trials, community and school‐based studies and those providing free helmets which reported self reported helmet ownership, studies in healthcare settings, focusing on older children and young people and studies providing free helmets which reported self reported helmet wearing. Hence, failure to demonstrate an effect of the intervention in these analyses may have resulted from a lack of power.
Confining analyses to RCTs as an assessment of the effect of study quality on outcomes was limited for self reported helmet ownership as three of the four included trials were hospital‐based studies, evaluating physician counselling, so differences in the effect size between these studies and the remaining studies included in the meta‐analyses may have arisen as a result of differences in participants, interventions and settings rather than in study quality. Our sensitivity analyses indicated that with the exception of two of our analyses, our findings were robust to using a range of intra‐class correlation coefficients (ICCs) (Adams 2004; Ukoumunne 1999).
Strengths and weaknesses of this review
This is a rigorously conducted and methodologically sound systematic review that has important implications for clinicians and policymakers planning non‐legislative interventions to promote cycle helmet use in children. However, health promotion interventions are notoriously difficult to combine in conventional systematic reviews because of clinical and statistical heterogeneity and this review is no exception. We have identified this in our meta‐analyses but have not been able to fully explain it with subgroup analyses. A lack of randomised controlled trials in this area means that the majority of included studies were potentially at risk of bias and confounding. The included studies also share three other important characteristics that limit the usefulness of our conclusions to some extent. Firstly, most of the studies reported their results after a short follow‐up period (median two months, range two weeks to two years) and the sustainability of any positive effects cannot be evaluated. Secondly few studies explored the effect of interventions in low‐income communities, so the generalisability of our findings to such communities is unknown. One study included in our review found that providing education and free helmets to children in schools in disadvantaged areas reduced inequalities in cycle helmet ownership, but this requires confirmation from other studies along with its effect on reducing inequalities in cycle‐related head injuries. Thirdly very few studies used more innovative interventions such as peer educators, interventions specifically aimed at enhancing decision making skills and increasing resistance to peer pressure or interventions aimed at increasing self esteem and self efficacy. Hence the effect of such interventions remains unknown. Finally all of the included studies were conducted in high‐income countries, hence we are not able to comment on the generalisability of our results to lower‐income countries.
Our review has looked at ways to increase the wearing of helmets among children and young people, but it has not addressed whether they are wearing them correctly, which is clearly important for reducing cycle‐related head injuries (Hynd 2009).
A recent Cochrane review by Macpherson 2008 has demonstrated that legislation appears to be effective in increasing cycle helmet use and in reducing head injuries. Legislation does not have to be mutually exclusive from the other interventions highlighted in our review. Only one of our studies was from a country where there is legislation (Hall 2004), hence we cannot draw conclusions about the additional effect of non‐legislative interventions where legislation is already in place. Further research is required to address this question.
Although none of the included studies identified any adverse effects of interventions, there remains a possibility that interventions to promote cycle helmet wearing may reduce cycling in children, with a potentially negative effect on child health. Further work is needed in this area.
Authors' conclusions
Implications for practice.
Non‐legislative interventions appear to be effective in increasing observed helmet use, particularly community‐based interventions and those providing free helmets. Those set in schools appear to be effective but may have a lesser effect than community‐based interventions. Interventions providing education only are less effective than those providing free helmets. There is insufficient evidence to recommend providing subsidised helmets at present. Interventions may be more effective if provided to younger children rather than older children. There is evidence that interventions offered in a healthcare settings can increase self reported helmet wearing, but none of these studies have measured observed helmet wearing.
Implications for research.
Further high‐quality studies are needed to explore whether non‐legislative interventions increase helmet wearing. Whilst randomised controlled trials would be the ideal design, designing such trials may be challenging. Ideally such studies should measure observed helmet wearing, or validate self reported helmet wearing by observations. Further work is required to explore the effect of providing subsided as opposed to free helmets and of providing interventions in healthcare settings as opposed to in schools or communities. Studies should also investigate the duration of any observed effects, particularly in relation to changes as children grow older and by socio‐economic group. Alternative interventions that go beyond the provision of helmet education and free or subsidised helmets (e.g. those including peer educators, those aimed at developing safety skills including skills in decision making and resisting peer pressure or those aimed at improving self esteem or self efficacy) need developing and testing, particularly for 11 to 18 year olds. The negative effects of interventions such as reduced cycling need to be measured in future studies. The effect of non‐legislative interventions in countries with existing cycle helmet legislation and in low and middle‐income countries requires investigation.
What's new
| Date | Event | Description |
|---|---|---|
| 15 December 2011 | Amended | Typo corrected. |
History
Protocol first published: Issue 1, 2003 Review first published: Issue 2, 2005
| Date | Event | Description |
|---|---|---|
| 29 September 2011 | New citation required and conclusions have changed | The review has been updated to April 2009 and seven new studies are included. The authors of the review have changed. |
Acknowledgements
The review authors would like to thank Kath Needham for her assistance in the early stages of the original review.
Appendices
Appendix 1. Search strategy
Cochrane Injuries Group’s Specialised Register (searched 3 April 2009) (Bicycling or bicycl* or cycle* or cycling or bike*) and (head* or helmet*) Cochrane Central Register of Controlled Trials (CENTRAL), The Cochrane Library (www.thecochranelibrary.com) (accessed 03 April 2009) #1 MeSH descriptor Bicycling explode all trees #2 bicycl* or cycle* or cycling or cyclist* or bike* #3 (#1 OR #2) #4 MeSH descriptor Head Protective Devices explode all trees #5 helmet* #6 (#4 OR #5) #7 (#3 AND #6) MEDLINE 1950 to March, week 4 2009/PubMed (accessed 03 April 2009) 1. exp Bicycling/ 2. (bicycl* or cycle* or cycling or cyclist* or bike*).ab,ti. 3. 1 or 2 4. exp Head Protective Devices/ 5. helmet*.ab,ti. 6. 4 or 5 7. 6 and 3 8. randomi?ed.ab,ti. 9. randomized controlled trial.pt. 10. controlled clinical trial.pt. 11. placebo.ab. 12. clinical trials as topic.sh. 13. randomly.ab. 14. trial.ti. 15. 8 or 9 or 10 or 11 or 12 or 13 or 14 16. (animals not (humans and animals)).sh. 17. 15 not 16 18. 7 and 17
EMBASE 1980 to week 13, March 2009 1. exp Cycling/ 2. exp Bicycle/ 3. (bicycl* or cycle* or cycling or cyclist* or bike*).ab,ti. 4. 1 or 2 or 3 5. exp protection/ 6. exp protective equipment/ 7. exp helmet/ 8. helmet*.ab,ti. 9. 5 or 6 or 7 or 8 10. 4 and 9 11. exp Randomized Controlled Trial/ 12. exp controlled clinical trial/ 13. randomi?ed.ab,ti. 14. placebo.ab. 15. *Clinical Trial/ 16. randomly.ab. 17. trial.ti. 18. 11 or 12 or 13 or 14 or 15 or 16 or 17 19. exp animal/ not (exp human/ and exp animal/) 20.18 not 19 21.10 and 20
PsycINFO 1806 to March Week 5 2009 and PsycEXTRA 1908 to March 24, 2009 1. (bicycl* or cycle* or cycling or cyclist* or bike*).ab,ti. 2. exp helmet/ 3. helmet*.ab,ti. 4. 3 or 2 5. 4 and 1 ISI Web of Science: Science Citation Index Expanded (SCI‐EXPANDED) 1970 to March 2009, Social Sciences Citation Index (SSCI) 1970 to March 2009, Conference Proceedings Citation Index‐Science (CPCI‐S) 1990 to March 2009 1. bicycl* or cycle* or cycling or cyclist* or bike* 2. Helmet* 3. (clinical OR control* OR placebo OR random OR randomised OR randomized OR randomly OR random order OR random sequence OR random allocation OR randomly allocated OR at random) SAME (trial* or group* or study or studies or placebo or controlled) 4. 1 and 2 and 3 TRANSPORT 1988 to 2007/06 1. (bicycl* or cycle* or cycling or cyclist* or bike*) and helmet* CINAHL 1982 to March 2008 1. (bicycl* or cycle* or cycling or cyclist* or bike*) and helmet* 2. (TX random* N3 control* N3 trial*) or (PT clinical tria) or (MH clinical trials) 3. 1 and 2
Data and analyses
Comparison 1. Non‐legislative interventions vs control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Observed helmet wearing | 11 | 3000 | Odds Ratio (M‐H, Random, 95% CI) | 2.08 [1.29, 3.34] |
| 2 Self reported helmet ownership | 7 | 1529 | Odds Ratio (M‐H, Random, 95% CI) | 2.67 [0.89, 8.03] |
| 3 Self reported helmet wearing | 9 | 1850 | Odds Ratio (M‐H, Random, 95% CI) | 3.27 [1.56, 6.87] |
1.1. Analysis.
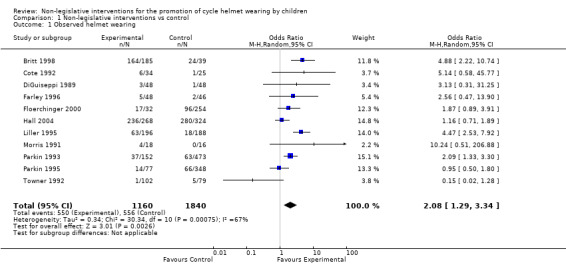
Comparison 1 Non‐legislative interventions vs control, Outcome 1 Observed helmet wearing.
1.2. Analysis.
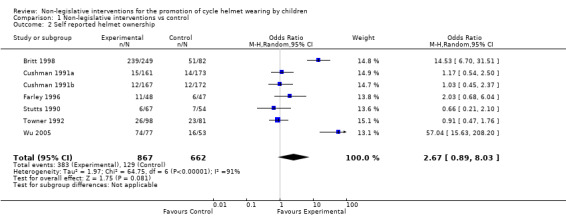
Comparison 1 Non‐legislative interventions vs control, Outcome 2 Self reported helmet ownership.
1.3. Analysis.
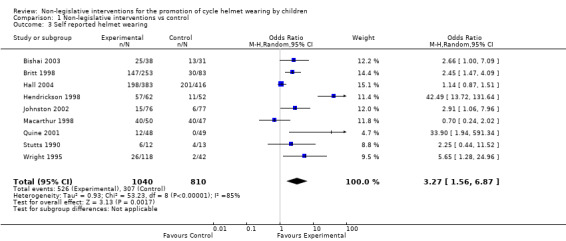
Comparison 1 Non‐legislative interventions vs control, Outcome 3 Self reported helmet wearing.
Comparison 2. Non‐legislative interventions vs control (RCTs only).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Observed helmet wearing | 3 | 807 | Odds Ratio (M‐H, Random, 95% CI) | 0.99 [0.18, 5.63] |
| 2 Self reported helmet ownership | 4 | 1044 | Odds Ratio (M‐H, Random, 95% CI) | 1.58 [0.66, 3.77] |
| 3 Self reported helmet wearing | 5 | 1255 | Odds Ratio (M‐H, Random, 95% CI) | 3.02 [0.72, 12.76] |
2.1. Analysis.
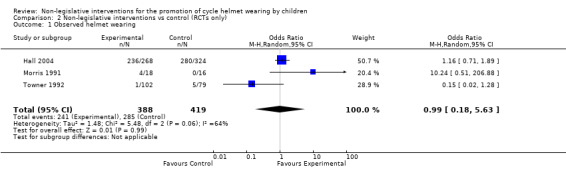
Comparison 2 Non‐legislative interventions vs control (RCTs only), Outcome 1 Observed helmet wearing.
2.2. Analysis.
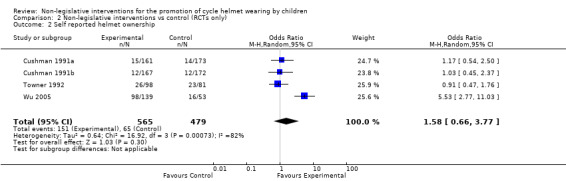
Comparison 2 Non‐legislative interventions vs control (RCTs only), Outcome 2 Self reported helmet ownership.
2.3. Analysis.
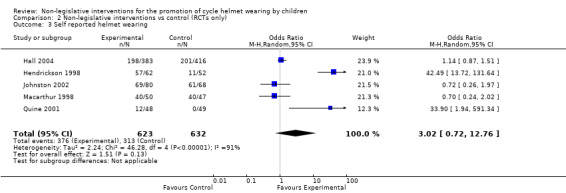
Comparison 2 Non‐legislative interventions vs control (RCTs only), Outcome 3 Self reported helmet wearing.
Comparison 3. Non‐legislative interventions vs control (community‐based interventions).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Observed helmet wearing | 4 | 473 | Odds Ratio (M‐H, Random, 95% CI) | 4.30 [2.24, 8.25] |
| 2 Self reported helmet ownership | 2 | 426 | Odds Ratio (M‐H, Random, 95% CI) | 5.65 [0.82, 38.98] |
3.1. Analysis.
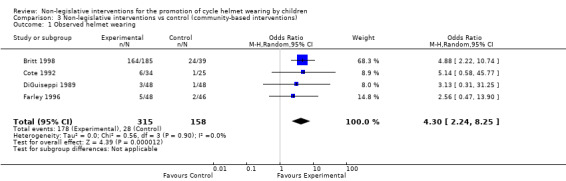
Comparison 3 Non‐legislative interventions vs control (community‐based interventions), Outcome 1 Observed helmet wearing.
3.2. Analysis.
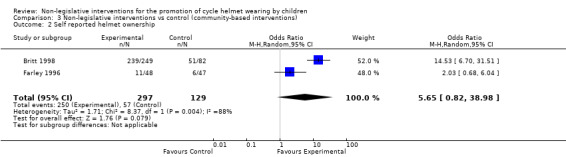
Comparison 3 Non‐legislative interventions vs control (community‐based interventions), Outcome 2 Self reported helmet ownership.
Comparison 4. Non‐legislative interventions vs control (school‐based interventions).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Observed helmet wearing | 8 | 2621 | Odds Ratio (M‐H, Random, 95% CI) | 1.73 [1.03, 2.91] |
| 2 Self reported helmet ownership | 3 | 395 | Odds Ratio (M‐H, Random, 95% CI) | 1.03 [0.60, 1.76] |
| 3 Self reported helmet wearing | 6 | 1292 | Odds Ratio (M‐H, Random, 95% CI) | 4.21 [1.06, 16.74] |
4.1. Analysis.
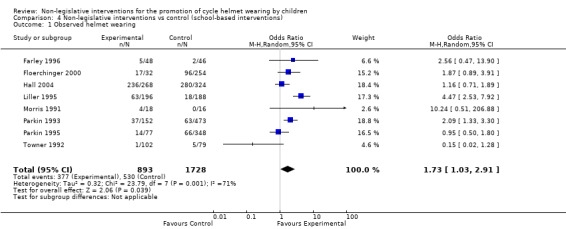
Comparison 4 Non‐legislative interventions vs control (school‐based interventions), Outcome 1 Observed helmet wearing.
4.2. Analysis.
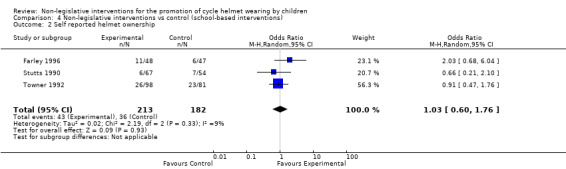
Comparison 4 Non‐legislative interventions vs control (school‐based interventions), Outcome 2 Self reported helmet ownership.
4.3. Analysis.
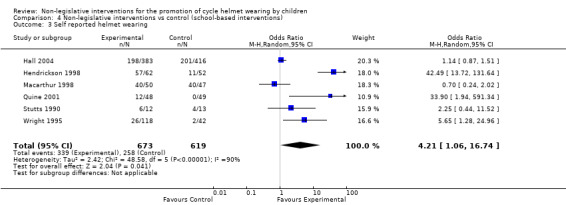
Comparison 4 Non‐legislative interventions vs control (school‐based interventions), Outcome 3 Self reported helmet wearing.
Comparison 5. Non‐legislative interventions vs control (free helmets).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Observed helmet wearing | 2 | 318 | Odds Ratio (M‐H, Random, 95% CI) | 4.35 [2.13, 8.89] |
| 2 Self reported helmet ownership | 3 | 556 | Odds Ratio (M‐H, Random, 95% CI) | 11.63 [2.14, 63.16] |
| 3 Self reported helmet wearing | 3 | 501 | Odds Ratio (M‐H, Random, 95% CI) | 7.27 [1.28, 41.44] |
5.1. Analysis.
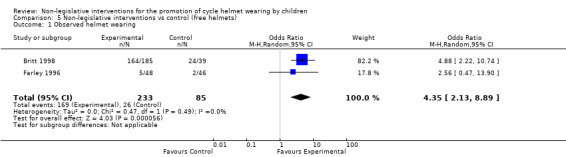
Comparison 5 Non‐legislative interventions vs control (free helmets), Outcome 1 Observed helmet wearing.
5.2. Analysis.

Comparison 5 Non‐legislative interventions vs control (free helmets), Outcome 2 Self reported helmet ownership.
5.3. Analysis.
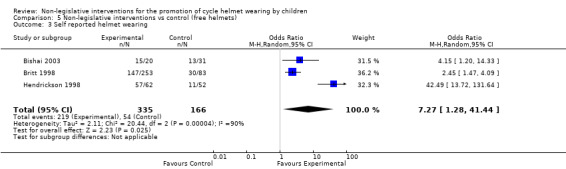
Comparison 5 Non‐legislative interventions vs control (free helmets), Outcome 3 Self reported helmet wearing.
Comparison 6. Non‐legislative interventions vs control (subsidised helmets).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Observed helmet wearing | 7 | 1804 | Odds Ratio (M‐H, Random, 95% CI) | 2.02 [0.98, 4.17] |
6.1. Analysis.

Comparison 6 Non‐legislative interventions vs control (subsidised helmets), Outcome 1 Observed helmet wearing.
Comparison 7. Non‐legislative interventions vs control (education only).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Observed helmet wearing | 3 | 1631 | Odds Ratio (M‐H, Random, 95% CI) | 1.43 [1.09, 1.88] |
| 2 Self reported helmet ownership | 3 | 794 | Odds Ratio (M‐H, Random, 95% CI) | 1.00 [0.60, 1.66] |
| 3 Self reported helmet wearing | 7 | 1380 | Odds Ratio (M‐H, Random, 95% CI) | 1.93 [1.03, 3.63] |
7.1. Analysis.

Comparison 7 Non‐legislative interventions vs control (education only), Outcome 1 Observed helmet wearing.
7.2. Analysis.
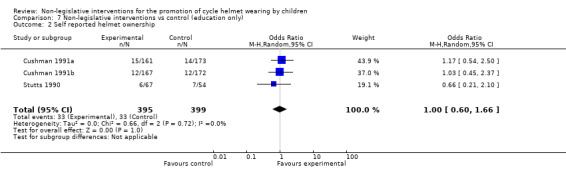
Comparison 7 Non‐legislative interventions vs control (education only), Outcome 2 Self reported helmet ownership.
7.3. Analysis.
Comparison 7 Non‐legislative interventions vs control (education only), Outcome 3 Self reported helmet wearing.
Comparison 8. Non‐legislative interventions vs control (healthcare setting).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Self reported helmet ownership | 3 | 803 | Odds Ratio (M‐H, Random, 95% CI) | 3.84 [0.46, 32.36] |
| 2 Self reported helmet wearing | 2 | 222 | Odds Ratio (M‐H, Random, 95% CI) | 2.78 [1.38, 5.61] |
8.1. Analysis.
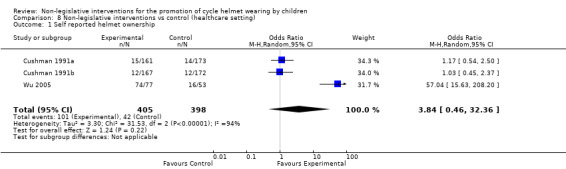
Comparison 8 Non‐legislative interventions vs control (healthcare setting), Outcome 1 Self reported helmet ownership.
8.2. Analysis.
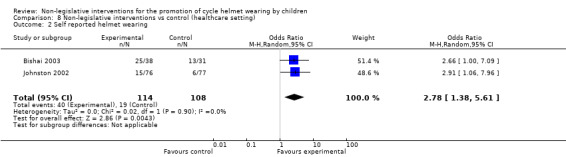
Comparison 8 Non‐legislative interventions vs control (healthcare setting), Outcome 2 Self reported helmet wearing.
Comparison 9. Non‐legislative interventions vs control (age < 12 years).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Observed helmet wearing | 5 | 1169 | Odds Ratio (M‐H, Random, 95% CI) | 2.50 [1.17, 5.37] |
| 2 Self reported helmet ownership | 4 | 726 | Odds Ratio (M‐H, Random, 95% CI) | 2.09 [0.47, 9.25] |
| 3 Self reported helmet wearing | 4 | 1257 | Odds Ratio (M‐H, Random, 95% CI) | 1.44 [0.82, 2.51] |
9.1. Analysis.
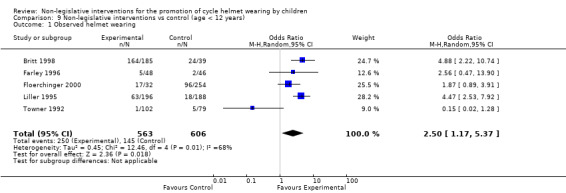
Comparison 9 Non‐legislative interventions vs control (age < 12 years), Outcome 1 Observed helmet wearing.
9.2. Analysis.
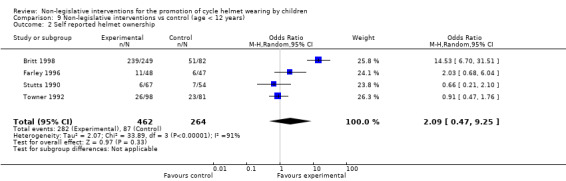
Comparison 9 Non‐legislative interventions vs control (age < 12 years), Outcome 2 Self reported helmet ownership.
9.3. Analysis.
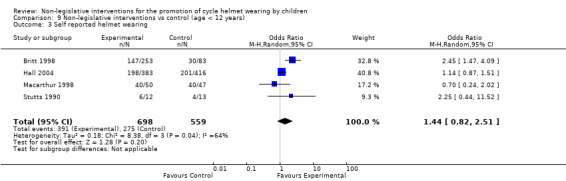
Comparison 9 Non‐legislative interventions vs control (age < 12 years), Outcome 3 Self reported helmet wearing.
Comparison 10. Non‐legislative interventions vs control (age > 11 years).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Self reported helmet wearing | 3 | 410 | Odds Ratio (M‐H, Random, 95% CI) | 4.99 [1.68, 14.83] |
10.1. Analysis.
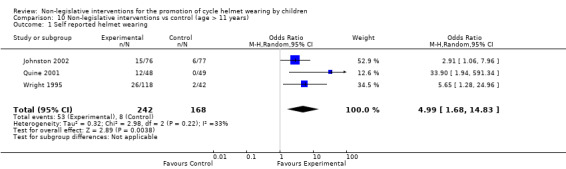
Comparison 10 Non‐legislative interventions vs control (age > 11 years), Outcome 1 Self reported helmet wearing.
Comparison 11. Non‐legislative interventions vs control (age 0 to 18 years).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Observed helmet wearing | 5 | 1239 | Odds Ratio (M‐H, Random, 95% CI) | 1.83 [0.98, 3.42] |
| 2 Self reported helmet ownership | 3 | 803 | Odds Ratio (M‐H, Random, 95% CI) | 3.84 [0.46, 32.36] |
| 3 Self reported helmet wearing | 2 | 183 | Odds Ratio (M‐H, Random, 95% CI) | 10.48 [0.69, 158.51] |
11.1. Analysis.
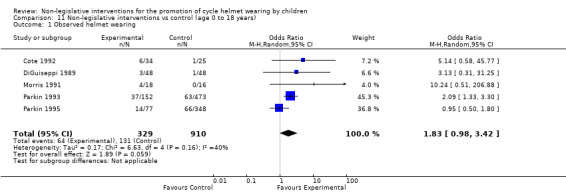
Comparison 11 Non‐legislative interventions vs control (age 0 to 18 years), Outcome 1 Observed helmet wearing.
11.2. Analysis.
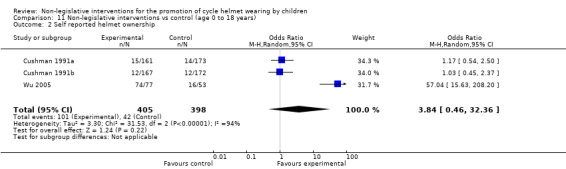
Comparison 11 Non‐legislative interventions vs control (age 0 to 18 years), Outcome 2 Self reported helmet ownership.
11.3. Analysis.
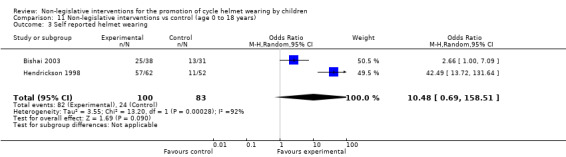
Comparison 11 Non‐legislative interventions vs control (age 0 to 18 years), Outcome 3 Self reported helmet wearing.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Azeredo 2003.
| Methods | CBA | |
| Participants | 6300 children from kindergarten to grade 2 in 12 schools in Oklahoma, US | |
| Interventions | Bicycle fairs were held during assemblies. Free helmets given to those who filled in an application form. The study also addressed seat belt use and smoke alarm awareness. | |
| Outcomes | Self reported helmet use and observed helmet use measured at 18 and 27 weeks | |
| Notes | Not included in meta‐analysis as denominators not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Bishai 2003.
| Methods | Randomised trial, assignment according to whether the date of presentation was odd or even. Outcome assessment undertaken blind to treatment group allocation. Analysis not undertaken blind to treatment group. 34% of those allocated to the intervention group and 28% of those allocated to the control group were included in the analysis. Assessment of distribution of confounders not reported | |
| Participants | 222 five to 15 year‐olds, recruited from the emergency department of a community hospital in Baltimore, US | |
| Interventions | All children in the intervention group received a 10‐minute counselling session and signed a behavioural contract. Half the intervention group children were also fitted with a free helmet (if their birthday was on a even date). The control group received a 'placebo' handout. | |
| Outcomes | Self reported helmet ownership; self reported helmet wearing. Measured at 4 weeks. | |
| Notes | The study population consisted of primarily urban children with a low rate of baseline helmet use (28%). No information provided on similarity of treatment groups at baseline. Data not available on patients who could have been enrolled but were not. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Britt 1998.
| Methods | CBA. Neither outcome assessment nor the analysis were undertaken blind to treatment group allocation. 70% of those allocated to the intervention group and 90% of those allocated to the control group were included in the analysis. Assessment of distribution of confounders not reported. | |
| Participants | 880 three and 4 year‐olds receiving routine health promotion home visits in Washington, US | |
| Interventions | Free helmets and a helmet promotion programme including parental information, lessons and other events. The control group received home visits but none of the above interventions | |
| Outcomes | Self reported helmet ownership; self reported helmet wearing; observed helmet wearing. Measured at 2 to 3 weeks. | |
| Notes | Self (parent) reported helmet data were collected in study year 1 only and observation data were collected in study years 1 and 2 in the intervention group and study year 2 in the control group. Participating sites probably represent clusters but no adjustment was made for this in the analysis. All sites were classified as low‐income. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Cote 1992.
| Methods | CBA. Neither outcome assessment nor the analysis were undertaken blind to treatment group allocation. Some data on completeness of follow‐up are presented but not numbers initially allocated to each group. An assessment of the distribution of confounders is presented. The median household income of the intervention area was USD 58,900 compared to USD 40,600 in the control area. | |
| Participants | 328 under 16 year‐olds observed riding bicycles in 2 US counties | |
| Interventions | Subsidised helmets, a helmet education programme and a local media campaign. The control group received none of the above interventions. | |
| Outcomes | Observed helmet wearing. Measured at 9 months. | |
| Notes | Only follow‐up data presented for self reported outcomes which were excluded from the analysis. One additional county included in the report had passed legislation and was therefore excluded. Participating sites probably represent clusters but no adjustment was made for this in the analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Cushman 1991a.
| Methods | RCT. The analysis was not undertaken blind to treatment group. 89% of those allocated to each treatment group were included in the analysis. An assessment of the distribution of a number of confounders is presented and no statistically significant differences were reported. | |
| Participants | 373 one to 17 year‐olds presenting to an emergency room in Canada with bicycle‐related injuries | |
| Interventions | Helmet promotion counselling from emergency physician. The control group received none of the above interventions. | |
| Outcomes | Self reported helmet ownership. Measured at 2 to 3 weeks. | |
| Notes | This study excluded children already owning helmets | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Cushman 1991b.
| Methods | RCT. The analysis was not undertaken blind to treatment group. Data relating to completeness of follow‐up not presented but it appears that outcomes are reported for all families allocated. Assessment of the distribution of confounders limited to age and whether family member owns helmet. The differences were not statistically significant. | |
| Participants | 576 five to18 year‐olds from 339 families presenting for a routine ambulatory visit at clinics in Canada | |
| Interventions | Helmet promotion counselling session from clinicians. The control group received none of the above interventions. | |
| Outcomes | Self reported helmet ownership. Measured at 2 to 3 weeks. | |
| Notes | Families are the unit of randomisation and analysis in this study. The outcome used in this analysis is the number of families buying helmets as a result of the intervention. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
DiGuiseppi 1989.
| Methods | CBA. Outcome assessment was not undertaken blind to treatment group allocation. Completeness of follow‐up not applicable because of population‐based design. Assessment of distribution of confounders presented. The areas were well balanced in terms of climate, population, ethnic groupings, education levels, unemployment levels and mean household income. | |
| Participants | 3‐year campaign reporting 9827 helmet observations in 5 to 15 year‐olds in Seattle and Portland, US | |
| Interventions | Subsidised helmets, helmet education and a television and media campaign. The control group received none of the above interventions. | |
| Outcomes | Observed helmet wearing. Measured at 4, 12 and 16 months. 4‐month data used in meta‐analysis. | |
| Notes | This large geographical study compared observed helmet wearing before and after a promotion campaign in one area (Seattle) with changes in observed helmet use in a distinct control area (Portland). This analysis uses unadjusted helmet wearing rates (rates adjusted for confounding also reported). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Farley 1996.
| Methods | CBA. Neither outcome assessment nor the analysis were undertaken blind to treatment group allocation. 50% of schools allocated to the intervention arm and 54% of those allocated to the control arm were included in the analysis. An assessment of the distribution of confounders was not reported. | |
| Participants | 5 to 12 year‐olds attending 4 intervention schools and 19 control schools in Idaho, US. The numbers of children at each school are not reported. | |
| Interventions | Community and school‐based helmet promotion programme including the provision of free and subsidised helmets. The control group received none of the above interventions. | |
| Outcomes | Observed helmet wearing. Measured at approximately 12 months. | |
| Notes | This study reported the results of a bicycle and motor vehicle safety promotion programme. Only data relevant to this review have been extracted. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Floerchinger 2000.
| Methods | CBA. Neither the outcome assessors nor the analysis were blind. The proportion of schools with outcomes reported as a percentage of those allocated to each group was 50% in the intervention group and 54% in the control group. An assessment of the distribution of confounders was not reported. | |
| Participants | 5 to 12 year‐olds attending 4 intervention schools and 19 control schools in Idaho, US. The numbers of children at each school are not reported. | |
| Interventions | Helmet promotion programme. The control group received no helmet promotion. | |
| Outcomes | Observed helmet wearing. Measured at approximately 12 months. | |
| Notes | This study reported the results of a bicycle and motor vehicle safety promotion programme. Only data relevant to this review have been extracted. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Hall 2004.
| Methods | Cluster‐RCT. Author confirmed schools were stratified by size and socio‐economic status, then within each strata schools were selected using random number lists generated by a statistical program. Observations of helmet wearing were undertaken blind to treatment group allocation. 86% of those allocated to the intervention group and 88% of those to the control group were included in the analysis of self reported outcomes. | |
| Participants | 1987 Grade 5 (age 10 to 11) pupils from 13 intervention schools and 14 control schools in Australia. Helmet observations were undertaken for children from all grades within schools. | |
| Interventions | Peer teaching for grade 5 pupils. Whole school bicycle safety education project over 2 years. The control schools received none of the above interventions. | |
| Outcomes | Self reported helmet use (grade 5 students); observed helmet wearing (students of all grades). Measured at 1 and 2 years. | |
| Notes | The study was undertaken in Australia, where bicycle helmet legislation is in place, hence baseline helmet ownership and wearing are likely to be higher than in countries without legislation. Analysis adjusted for clustering. Self reported data restricted to regular riders only. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Hendrickson 1998.
| Methods | Cluster‐RCT. Analysis was not undertaken blind to treatment group allocation. 81% of participants were included in the analysis, but this is not presented with respect to allocated group. An assessment of the distribution of confounders is not presented. | |
| Participants | 407 ten to 13 year‐olds from 9 low‐income schools in central Texas, US | |
| Interventions | The trial had 3 arms: free cycle helmets and a cycle helmet education programme; free cycle helmets, a cycle education programme and a telephone intervention to parents and a control arm which received none of the above interventions | |
| Outcomes | Self reported helmet wearing. Measured at 2 weeks and 6 weeks. 6‐week data used in meta‐analysis. | |
| Notes | The control group were offered a free helmet after the study. The analysis was not adjusted for clustering. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Johnston 2002.
| Methods | RCT. Analysis was undertaken blind to treatment group. 78% of those allocated to the intervention group were included in the analysis at 3 months and 74% at 6 months. 73% of those allocated to the control group were included in the analysis at 3 months and 76% at 6 months. Confounders that were reported include sex, age, schools attendance, insurance status, severity of index injury and premorbid risk behaviours. | |
| Participants | Adolescents aged 12 to 20 years attending an emergency department in the Pacific Northwest, US. The author provided unpublished data for those aged 12 to 18 years. | |
| Interventions | Behavioural change counselling focusing on an identified injury‐related risk behaviour. The control group received none of the above interventions. | |
| Outcomes | Self reported helmet use(always or never) measured at 3 and 6 months | |
| Notes | The intervention and outcome assessment focused on a number of behaviours including seat belt use, carrying a weapon and drinking and driving. Bicycle helmet outcomes reported only for bicycle riders. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Kendrick 2004.
| Methods | Cluster‐RCT. Outcome assessment was not undertaken blind to treatment group allocation. 86% of those allocated to the education plus group were included in the analysis and 66% of those allocated to the education group were included in the analysis. Documented baseline characteristics include helmet ownership and usage at baseline, sex, area level deprivation, frequency of bike riding, family encouragement to wear a helmet, awareness of dangers associated with not wearing helmet, previous accidents whilst on a bike, and friend wears a helmet. | |
| Participants | 28 primary schools with a Townsend score of less than 0. This involved 1213 year 5 (age 9 and 10) pupils in deprived areas in Nottingham, UK. | |
| Interventions | The study compared 2 different educational interventions 1) educational pack plus form for free cycle helmet, 2) all the above plus an assembly, lesson and invitation to cycling event | |
| Outcomes | Self reported helmet ownership and use, measured at 2 to 3 months. Self reporting was validated by observation. | |
| Notes | Data from this study has not been included in the meta‐analysis because there was no control group that did not receive any intervention. The article is by authors of this review. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | Adequate |
Kim 1997.
| Methods | Cluster‐RCT. Neither outcome assessment nor the analysis were undertaken blind to treatment group allocation. 84% of those allocated to the intervention group and 83% of those allocated to the control group were included in the analysis. An assessment of the distribution of confounders is presented. There were some significant differences between gender, parents education, median household income and method of follow‐up between the intervention and control groups. | |
| Participants | 506 six to 12 year‐olds attending public health clinics in Washington, US | |
| Interventions | Free cycle helmets (subsidised in control group) and educational intervention delivered by clinicians to both control and intervention | |
| Outcomes | Self reported helmet wearing. Measured at 2 to 3 weeks. | |
| Notes | Data from this study have not been included in the meta‐analysis because there was no control group that did not receive any intervention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Lee 2000.
| Methods | CBA. Outcome assessment was not undertaken blind to treatment group allocation. Data relating to completeness of follow‐up are not clear. An assessment of the distribution of confounders is not presented. | |
| Participants | 500 eleven to 15 year‐olds from intervention and control areas completed questionnaires at the beginning and end of the campaign each year for 3 years (6000 children in total). Control and intervention areas were both UK cities. | |
| Interventions | Subsidised helmets and an education programme. The control group received none of the above interventions. | |
| Outcomes | Self reported helmet wearing | |
| Notes | Data from this study have not been included in the meta‐analysis because we could not obtain them in a form that would allow the calculation of odds ratios. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Not used |
Leverence 2004.
| Methods | RCT. Outcome assessment was undertaken blind to treatment group. 69 patients were lost to follow‐up but it is unclear which group they were from. Reported confounders included age, sex and baseline use of helmets. Helmet use was measured on a 4‐point Likert scale. | |
| Participants | Aged 11 to 24, presenting to a primary care clinic in South Western US | |
| Interventions | 2 to 3‐minute scripted motivational counselling intervention, educational brochure and subsidised helmet voucher. The control group received none of the above interventions. | |
| Outcomes | Self reported helmet use, measured at 3 months. Presented as the mean of a 4‐point Likert Scale. | |
| Notes | This study also addressed seat belt use | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Liller 1995.
| Methods | CBA. Neither outcome assessment nor the analysis were undertaken blind to treatment group allocation. Completeness of follow‐up not applicable because of population‐based design. An assessment of the distribution of confounders is not reported although the authors state that intervention and control schools were matched on socioeconomic variables. | |
| Participants | 5 to 8 year‐olds attending 9 intervention schools and 9 control schools Florida, US. 3428 children received the intervention. | |
| Interventions | Subsidised helmets and an education programme. The control group received none of the above interventions. | |
| Outcomes | Observed helmet wearing. Measured at 2 to 3 weeks. | |
| Notes | No adjustment for clustering reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Macarthur 1998.
| Methods | Cluster‐RCT. The analysis was not undertaken blind to treatment group allocation. Data relating to completeness of follow‐up presented (see Notes). An assessment of the distribution of confounders is presented and no significant differences are reported. | |
| Participants | 141 nine to 10 year olds from 6 schools in metropolitan Toronto, Canada | |
| Interventions | Education programme. The control group received none of the above interventions. | |
| Outcomes | Self reported helmet wearing. Measured at 3 months. | |
| Notes | Responders and non‐responders were compared and found to be similar in all respects except gender (more female non‐responders). Overall outcomes were reported in 83% of those allocated. The main focus of the education programme was on improving bicycle skills; helmet wearing was a secondary outcome measure. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Moore 1990.
| Methods | CBA. Neither outcome assessment nor the analysis were undertaken blind to treatment group allocation. An assessment of the distribution of confounders is not reported although the authors state that intervention and control schools were matched for size, age group and socioeconomic status of communities. | |
| Participants | 11 to 13 year‐olds from 1 intervention and 1 control school from inner city areas of New Zealand | |
| Interventions | Subsidised helmets and an education programme. The control group received none of the above interventions. | |
| Outcomes | Observed helmet wearing. Measured at 6 and 10 weeks. | |
| Notes | The raw numbers of students exposed to the intervention and the numbers wearing helmets are not available from the published report or its authors | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Morris 1991.
| Methods | Cluster‐RCT. Outcome assessment was not undertaken blind to treatment group allocation. An assessment of the distribution of confounders is not presented. | |
| Participants | 5 to 13 year olds attending 3 schools in a city in Ontario, Canada | |
| Interventions | The trial had 3 arms: 1 school received an education programme, 1 school an education programme and subsidised helmets and the third school was the control school which received none of the above interventions | |
| Outcomes | Observed helmet wearing. Measured at 1 month. | |
| Notes | The numbers of children receiving each intervention are not reported. Each school had "about 400 students". | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Parkin 1993.
| Methods | CBA. Neither outcome assessment nor the analysis were undertaken blind to treatment group allocation. Completeness of follow‐up not applicable because of population‐based design. An assessment of the distribution of confounders is presented. Intervention and control schools were similar with respect to average family income, university education, owner occupation of dwellings and one‐parent families. | |
| Participants | 4 intervention schools (2 high‐income and 2 low‐income) with a total of 1100 five to 14 year‐olds and 18 control schools (numbers of children not reported) from metropolitan Toronto, Canada. | |
| Interventions | Subsidised helmets and an education programme. The control group received none of the above interventions. | |
| Outcomes | Observed helmet wearing. Measured at 2 to 6 months. | |
| Notes | This study included a subgroup analysis comparing the observed helmet wearing rates post‐intervention in high versus low‐income groups. No adjustment for clustering in the analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Parkin 1995.
| Methods | CBA. Neither outcome assessment nor the analysis were undertaken blind to treatment group allocation. Completeness of follow‐up not applicable because of population‐based design. An assessment of the distribution of confounders is presented. Intervention and control schools were similar with respect to average family income, university education, owner occupation of dwellings and one‐parent families. | |
| Participants | 5 to 14 year‐olds from 3 schools in areas of low average family income in a large urban Canadian city and 3 low‐income areas in the same city served as control areas. 1415 children received the intervention. | |
| Interventions | Subsidised helmets and an education programme. The control group received none of the above interventions. | |
| Outcomes | Observed helmet wearing. Self reported helmet ownership also mentioned but full data not presented. Measured at approximately 2 months. | |
| Notes | This study included a subgroup analysis comparing the observed helmet wearing rates post‐intervention in high versus low‐income groups. No adjustment for clustering in the analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Pendergrast 1992.
| Methods | CBA. Analysis was not undertaken blind to treatment group allocation. Age and socioeconomic status are reported in the baseline characteristics of the participants and these are well balanced. | |
| Participants | 287 children from grades 2, 3 and 4 from 2 elementary schools in suburban Augusta, US were sent a pretest questionnaire and 527 children were sent a post‐test questionnaire | |
| Interventions | The intervention group received intensive education including a school bike club, presentation to PTA, demonstration of a stunt rider wearing a helmet. Both intervention and control groups received subsidised helmets and a basic education programme. | |
| Outcomes | Self reported helmet ownership and self reported helmet wearing. Measured at 10 months. | |
| Notes | Participant's parents were also sent a questionnaire asking about their child's helmet wearing behaviour. Data from this study have not been included in the meta‐analysis because there was no control group that did not receive any intervention. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Quine 2001.
| Methods | RCT. Analysis was not undertaken blind to treatment group allocation. 93% of the participants randomised were included in the analysis but this is not presented with respect to allocated group. An assessment of the distribution of confounders is not presented. | |
| Participants | 97 eleven to 14 year‐olds that regularly cycled to school in the UK but did not wear a helmet. | |
| Interventions | Education programme based on theory of planned behaviour. The control group received a pamphlet with messages about cycling proficiency and bicycle maintenance. | |
| Outcomes | Self reported helmet ownership and self reported helmet wearing. Measured at 5 months. | |
| Notes | Since the education programme was carried out in the classroom, there may have been some contamination of the control group. Only self reported helmet wearing has been extracted for use in this analysis because ownership data are not presented with respect to group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Stutts 1990.
| Methods | CBA. Neither outcome assessment nor the analysis were undertaken blind to treatment group allocation. 70% of those allocated to the intervention group and 60% of those allocated to the control group were included in the analysis. An assessment of the distribution of confounders is presented and there were significant differences in rates of previous bicycle‐related injury but not frequency of riding or helmet ownership between intervention and control groups. | |
| Participants | 404 4th and 5th grade children from 4 elementary schools in North Carolina, US | |
| Interventions | Education programme consisting of 7 lessons delivered in schools. The control group received none of the above interventions. | |
| Outcomes | Self reported helmet ownership; self reported helmet wearing. Measured at 8 weeks. | |
| Notes | Response rates at follow‐up are reported as approximately 70% for the intervention group and approximately 60% for the control group. Baseline helmet ownership rates were slightly higher in the control schools than the intervention schools and no adjustment has been made for this. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Towner 1992.
| Methods | Cluster‐RCT. Neither outcome assessment nor the analysis were undertaken blind to treatment group allocation. The baseline survey of helmet use had a 35% response rate and the follow‐up survey a 20% response rate. These figures are not provided by allocation group. An assessment of the distribution of confounders is not presented although schools were matched for size and socioeconomic status. | |
| Participants | 2211 children attending 6 elementary schools (3 intervention, 3 control) in the US | |
| Interventions | Subsidised helmets and an education programme. The control group received none of the above interventions. | |
| Outcomes | Self reported helmet ownership; observed helmet wearing. Measured at 2 weeks and 19 weeks. 19‐week data used in meta‐analysis. | |
| Notes | Follow‐up data reported at 2 and 19 weeks post‐intervention. 19‐week data are used in the meta‐analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Watts 1997.
| Methods | Cluster‐RCT. Neither outcome assessment nor the analysis were undertaken blind to treatment group allocation. Baseline helmet ownership and baseline helmet wearing rates are reported but not by treatment group. | |
| Participants | 926 five to 12 year‐olds from 2 elementary schools in Virginia, US | |
| Interventions | Education programme given to both schools and free cycle helmets given to participants at intervention school | |
| Outcomes | Self reported helmet ownership and self reported helmet wearing. Measured at 1 month. | |
| Notes | Response rates are not reported. Data from this study have not been included in the meta‐analysis because we could not obtain them in a form that would allow the calculation of odds ratios. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
Wright 1995.
| Methods | CBA. Neither outcome assessment nor the analysis were undertaken blind to treatment group allocation. Completeness of follow‐up data not presented (see Notes). An assessment of the distribution of confounders is presented and the groups were well balanced with respect to age, gender and ethnicity. | |
| Participants | 741 eleven to 18 year‐olds from 3 middle schools and 3 high schools in Washington, US | |
| Interventions | Education programme. The control group received none of the above interventions. | |
| Outcomes | Self reported helmet wearing and observed helmet wearing. Measured at 2 weeks. | |
| Notes | The control group was older than the intervention group. The results were not adjusted for clustering. Survey response rates for intervention and control schools are not reported. Observations of helmet wearing were not undertaken for control group; therefore, only self reported helmet wearing data have been included in the meta‐analysis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | Not used |
Wu 2005.
| Methods | RCT. Outcome assessment not undertaken blind to treatment group allocation. 95% of those allocated to the first intervention group, 99% of those allocated to the second intervention group and 93% of those allocated to the control group were included in the analysis. Reported confounders include male sex, health insurance/medicare, rented housing, riding bike, scooter or skateboard. Those who already had a helmet were excluded. | |
| Participants | Children aged 5 to 16 admitted to an urban Midwest US emergency department for treatment, who did not already own a helmet | |
| Interventions | This trial had 3 arms: the first intervention group received voucher for a free helmet plus education, the 2nd intervention group received a free helmet in the emergency department and education, and the control group received education about sports helmet use | |
| Outcomes | Self and parental reported ownership, self and parental reported usage measured at 2 to 4 months | |
| Notes | It is unclear whether outcomes are parent or child reported at follow‐up. Outcomes (reported as percentages only) reported only for children participating in relevant sport at follow‐up. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
RCT = randomised controlled trial CBA = controlled before‐after study
Contributions of authors
Simon Royal (SR), Denise Kendrick (DK) and Tim Coleman (TC) wrote the protocol for the original review. Simon Royal ran the searches for the original review. SR, DK and TC selected articles for inclusion, extracted data and undertook quality assessment for the original review. SR and DK undertook analyses for the original review and SR, DK and TC wrote the report for the original review. CM, DK and TC wrote the protocol for the update of the review. CM and RO ran the searches for the update. RO, CM, DK and TC selected articles for inclusion, extracted data and undertook quality assessment for the update. RO and DK undertook analyses for the update. RO drafted the report for the update and all authors commented on the draft.
Sources of support
Internal sources
University of Nottingham, UK.
External sources
No sources of support supplied
Declarations of interest
Denise Kendrick and Simon Royal have conducted a cluster‐randomised controlled trial of an educational package and subsidised cycle helmet scheme for primary school children (Kendrick 2004).
Edited (no change to conclusions)
References
References to studies included in this review
Azeredo 2003 {published data only}
- Azeredo R, Stephens‐Stidham S. Design and implementation of injury prevention curricula for elementary schools: lessons learned. Injury Prevention 2003;9(3):274‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bishai 2003 {published data only}
- Bishai D, Qureshi A, Cantu N, Parks C. Contracting with children and helmet distribution in the emergency department to improve bicycle helmet use. Society for Academic Emergency Medicine. 2003;10(12):1371‐7. [DOI] [PubMed] [Google Scholar]
Britt 1998 {published data only}
- Britt J, Silver I, Rivara FP. Bicycle helmet promotion among low income preschool children. Injury Prevention 1998;4:280‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cote 1992 {published data only}
- Cote TR, Sacks JJ, Lambert‐Huber DA, Dannenberg AL, Kresnow MJ, Lipsitz CM, et al. Bicycle helmet use among Maryland children: effect of legislation and education. Pediatrics 1992;89:1216‐20. [PubMed] [Google Scholar]
Cushman 1991a {published data only}
- Cushman R, Down J, MacMillan N, Waclawik H. Helmet promotion in the emergency room following a bicycle injury: a randomized trial. Pediatrics 1991;88:43‐7. [PubMed] [Google Scholar]
Cushman 1991b {published data only}
- Cushman R, James W, Waclawik H. Physicians promoting bicycle helmets for children: a randomized trial. American Journal of Public Health 1991;81:1044‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
DiGuiseppi 1989 {published data only}
- DiGuiseppi CG, Rivara FP, Koepsell TD, Polissar L. Bicycle helmet use by children. Evaluation of a community‐wide helmet campaign. JAMA 1989;262:2256‐61. [PubMed] [Google Scholar]
Farley 1996 {published and unpublished data}
- Farley C, Haddad S, Brown B. The effects of a 4‐year program promoting bicycle helmet use among children in Quebec. American Journal of Public Health 1996;86:46‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Floerchinger 2000 {published and unpublished data}
- Floerchinger‐Franks G, Machala M, Goodale K, Gerberding S. Evaluation of a pilot program in rural schools to increase bicycle and motor vehicle safety. Journal of Community Health 2000;25:113‐24. [DOI] [PubMed] [Google Scholar]
Hall 2004 {published data only}
- Hall M, Cross D, Howat P, Stevenson M, Shaw T. Evaluation of a school‐based peer leader bicycle helmet intervention. Injury Control and Safety Promotion 2004;11(3):165‐74. [DOI] [PubMed] [Google Scholar]
Hendrickson 1998 {published data only}
- Hendrickson SG, Becker H. Impact of a theory based intervention to increase bicycle helmet use in low income children. Injury Prevention 1998;4:126‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnston 2002 {published and unpublished data}
- Johnston BD, Rivara FP, Droesch RM, Dunn C, Copass MK. Behavior change counseling in the emergency department to reduce injury risk: a randomized, controlled trial. Pediatrics 2002;110(2):267‐74. [DOI] [PubMed] [Google Scholar]
Kendrick 2004 {published data only}
- Kendrick D, Royal S, Lids for Kids project team. Cycle helmet ownership and use; a cluster randomised controlled trial in primary school children in deprived areas. Archives of Disease in Childhood 2004;89:330‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 1997 {published data only}
- Kim AN, Rivara FP, Koepsell TD. Does sharing the cost of a bicycle helmet help promote helmet use?. Injury Prevention 1997;3:38‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2000 {published and unpublished data}
- Lee AJ, Mann NP, Takriti R. A hospital led promotion campaign aimed to increase bicycle helmet wearing among children aged 11‐15 living in West Berkshire 1992‐98. Injury Prevention 2000;6:151‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leverence 2004 {published data only}
- Leverence RR, Martinez M, Whisler S, Romero‐Leggott V, Harji F, Milner M, et al. Does office‐based counseling of adolescents and young adults improve self‐reported safety habits? A randomized controlled effectiveness trial. Journal of Adolescent Health 2005;36(6):523‐8. [DOI] [PubMed] [Google Scholar]
Liller 1995 {published data only}
- Liller KD, Smorynski A, McDermott RJ, Crane NB, Weibley RE. The MORE HEALTH bicycle safety project. Journal of School Health 1995;65:87‐90. [DOI] [PubMed] [Google Scholar]
Macarthur 1998 {published data only}
- Macarthur C, Parkin PC, Sidky M, Wallace W. Evaluation of a bicycle skills training program for young children: a randomized controlled trial. Injury Prevention 1998;4:116‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moore 1990 {published data only (unpublished sought but not used)}
- Moore DW, Adair V. Effects of a school‐based education programme on safety helmet usage by 11‐ to 13‐year‐old cyclists. Educational Psychology 1990;10:73‐8. [Google Scholar]
Morris 1991 {published data only}
- Morris BA, Trimble NE. Promotion of bicycle helmet use among schoolchildren: a randomized clinical trial. Canadian Journal of Public Health 1991;82:92‐4. [PubMed] [Google Scholar]
Parkin 1993 {published data only}
- Parkin PC, Spence LJ, Hu X, Kranz KE, Shortt LG, Wesson DE. Evaluation of a promotional strategy to increase bicycle helmet use by children. Pediatrics 1993;91:772‐7. [PubMed] [Google Scholar]
Parkin 1995 {published and unpublished data}
- Parkin PC, Hu X, Spence LJ, Kranz KE, Shortt LG, Wesson DE. Evaluation of a subsidy program to increase bicycle helmet use by children of low‐income families. Pediatrics 1995;96:283‐7. [PubMed] [Google Scholar]
Pendergrast 1992 {published data only}
- Pendergrast RA, Ashworth CS, DuRant RH, Litaker M. Correlates of children's bicycle helmet use and short‐term failure of school‐level interventions. Pediatrics 1992;90:283‐7. [PubMed] [Google Scholar]
Quine 2001 {published data only}
- Quine L, Rutter DR, Arnold L. Persuading school‐age cyclists to use safety helmets: effectiveness of an intervention based on the theory of planned behaviour. British Journal of Health Psychology 2001;6:327‐45. [DOI] [PubMed] [Google Scholar]
Stutts 1990 {published and unpublished data}
- Stutts JC, Hunter WW. Evaluation of a bicycle safety education curriculum for elementary school‐age children. Chapel Hill, N.C.: North Carolina University, 1990. [Google Scholar]
Towner 1992 {published and unpublished data}
- Towner P, Marvel MK. A school‐based intervention to increase the use of bicycle helmets. Family Medicine 1992;24:156‐8. [PubMed] [Google Scholar]
Watts 1997 {published data only}
- Watts D, O'Shea N, Flynn E, Trask A, Kelleher D. Effect of a bicycle safety program and free bicycle helmet distribution on the use of bicycle helmets by elementary school children. Journal of Emergency Nursing 1997;23:417‐9. [DOI] [PubMed] [Google Scholar]
Wright 1995 {published data only}
- Wright M, Rivara FP, Ferse D. Evaluation of the Think First head and spinal cord injury prevention program. Injury Prevention 1995;1:81‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2005 {published data only}
- Wu BC, Oakes JM. A randomized controlled trial of sport helmet interventions in a pediatric emergency department. Pediatric Emergency Care 2005;21(11):730‐5. [DOI] [PubMed] [Google Scholar]
Additional references
Adams 2004
- Adams G, Gulliford M, Ukoumunne O, Eldridge S, Chinn S, Campbell M. Patterns of intra‐cluster correlation from primary care research to inform study design and analysis. Journal of Clinical Epidemiology 2004;57:785‐94. [DOI] [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Control Clinical Trials 1986;7(3):177‐88. [DOI] [PubMed] [Google Scholar]
DfT 2010
- Department for Transport. Road Casualties Great Britain: 2009. London: The Stationery Office, 2010. [Google Scholar]
Egger 1997
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by simple graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Egger 1998
- Egger M, Smith GD. Meta‐analysis bias in location and selection of studies. BMJ 1998;316(7124):61‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hippisley‐Cox 2002
- Hippisley‐Cox J, Groom L, Kendrick D, Coupland C, Webber E, Savelyich B. Cross‐sectional survey of socioeconomic variations in severity and mechanism of childhood injuries in Trent 1992‐7. BMJ 2002;324(7346):1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hynd 2009
- Hynd D, Cuerden R. The potential for cycle helmets to prevent injury ‐ a review of the evidence. Transport Research Laboratory November 2009.
Lajunen 2001
- Lajunen T, Räsänenb M. Why teenagers owning a bicycle helmet do not use their helmets. Journal of Safety Research 2001;32(3):323‐32. [Google Scholar]
Macpherson 2008
- Macpherson A, Spinks A. Bicycle helmet legislation for the uptake of helmet use and prevention of head injuries. Cochrane Database of Systematic Reviews 2008, Issue 3. [DOI: 10.1002/14651858.CD005401.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Murray 2004
- Murray D, Cattelier D, Hannan P, Treuth M, Stevens J, Schmitz K, et al. School‐level intraclass correlation for physical activity in adolescent girls. Medicine & Science in Sports & Exercise 2004;36:876‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Roberts 1997
- Roberts I. Cause specific social class mortality differentials for child injury and poisoning in England and Wales. Journal of Epidemiology and Community Health 1997;51(3):334‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thompson 1999
- Thompson DC, Rivara FP, Thompson R. Helmets for preventing head and facial injuries in bicyclists. Cochrane Database of Systematic Reviews 1999, Issue 4. [DOI: 10.1002/14651858.CD001855] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ukoumunne 1999
- Ukoumunne O, Gulliford M, Chinn S, Sterne J, Burney P. Methods for evaluating area‐wide and organisation‐based interventions in health and health care: a systematic review. Health Technology Assessment 1999;3:iii‐92. [PubMed] [Google Scholar]


