Objectives
This is a protocol for a Cochrane Review (intervention). The objectives are as follows:
To assess the effectiveness of methods used during dental treatment procedures to minimise aerosol production and reduce or neutralise contamination in aerosols.
Background
The production of aerosols and splatter in dentistry is a major health concern as aerosols generated during dental procedures are contaminated with micro‐organisms, which can lead to spread of infection among dental professionals and their patients. The oral cavity harbours over 700 species of bacteria and other infectious microbes, which can be transmitted through aerosol‐generating procedures (AGPs) and cause respiratory health effects or transmit bidirectional diseases. As procedures in a dental clinic generally involve close contact between patients and dentists, the risk of infection in this setting can be high (Meng 2020), though some studies have found no increased prevalance of respiratory infections among dentists (Scannapieco 2004).
The World Health Organization (WHO) has previously reported disease outbreaks of Ebola virus, Middle East respiratory syndrome (MERS‐CoV), severe acute respiratory syndrome (SARS‐CoV), swine flu, avian influenza (H5N1 flu), tuberculosis and measles across the world, and we are currently experiencing the COVID‐19 pandemic (WHO 2020). Based on risk assessment, WHO has recommended airborne precautions for settings in which AGPs and support treatment are performed (WHO 2020a), thus leading several countries to temporarily suspend all elective dental procedures. Dental professional organisations have proposed infection control protocols (ADA 2020; ALOP 2020; BDA 2020a; CDC 2020; Dominiak 2020; NCUDSPH 2020), and recommendations to postpone elective procedures, surgeries and non‐urgent dental visits (ADA 2020; CDC 2020; NCUDSPH 2020). This rapid review aims to explore the evidence on the effectiveness of various methods that can be used to reduce contaminated aerosols generated during dental procedures.
Description of the condition
Dental professionals have an important role in preventing the transmission of any infection. The possible routes for the spread of most viral, bacterial and fungal infections in a dental clinic are droplet, contact and airborne (Peng 2020). These routes can be bidirectional, meaning transmission may occur from patient‐to‐patient, patient‐to‐clinician or clinician‐to‐patient (Laheij 2012). It is unclear how much each form of transmission contributes to the risk of infection, but it is assumed that airborne transmission occurs only when a large volume of aerosol particles are generated (Harrel 2004).
The incubation period of common bacterial and viral infections ranges between two and 14 days during which the patient is asymptomatic but the chance of contamination and spread may still exist (Lessler 2009). The incubation period of the current pandemic due to COVID‐19 has been estimated at five to six days on average, but it could be as long as 14 days (Meng 2020). The incubation period of SARS virus infection was reported to be 10 days, though with a low risk of transmission in the prodromal phase (Samaranayake 2004). This uncertainty makes it prudent to consider all patients to be potential sources of infection.
Transmission of infection in the dental clinic primarily occurs by direct contact with the respiratory droplets from the infected person, or indirect contact with surfaces in the immediate environment or with objects used on the infected person that generate larger amounts of contaminated aerosols (e.g. dental chair or dental instruments) (Upendran 2020). Aerosol scientists and other researchers are debating whether COVID‐19 spreads via air and AGPs (Lewis 2020). Leung 2020 detected rhinovirus, influenza and human coronaviruses (excluding SARS‐CoV‐2) in respiratory droplets and aerosols. WHO states that airborne transmission may be possible during certain medical procedures such as bronchoscopy (WHO 2020a).
Differentiation of aerosols
Aerosols are differentiated based on particle size: splatter when they are greater than 50 µm; droplets when 11 µm to 50 µm; droplet nuclei when 10 µm or less. Most of the aerosols produced in the dental settings are extremely small (less than 5 µm) (Harrel 2004; James 2016), vary in size depending on the procedures (Polednik 2014), and submicrometre particles have been demonstrated in various dental procedures in laboratory settings (Polednik 2014; Sotiriou 2008).
Splatter, being the larger particles, are airborne only briefly. They fall to the ground or settle on surfaces in the dental operatory (Harrel 2004). Droplets remain suspended in the air until they evaporate, leaving droplet nuclei that may contain bacteria related to respiratory infections. Droplet nuclei can contaminate surfaces to a range of three feet and may remain airborne for 30 minutes to two hours. If inhaled, the droplet nuclei can penetrate deep into the respiratory system (Harrel 2004; James 2016; Kormuth 2018).
What is the composition of contaminated droplets or aerosols?
The oral cavity is a nidus for several bacteria and viruses. It also harbours bacteria and viruses from the nose, throat and respiratory tract. Hence, different strains of micro‐organisms and viruses are present in aerosols generated when dental AGPs are carried out, making them contaminated aerosols or bio‐aerosols or microbial aerosols (Zemouri 2017). Apart from micro‐organisms, components of saliva, nasopharyngeal secretions, plaque, blood, tooth components and any material used in the dental procedures such as abrasives for air polishing and air abrasion, are commonly present in dental aerosols. While multiple studies have been conducted to determine which dental procedure produces the most airborne bacterial contamination (Jain 2020; Monarca 2000; Polednik 2014; Rautemaa 2006); viral particles such as influenza, rhinoviruses, SARS coronavirus and bacteriae such as Mycobacteria tuberculi and strict anaerobic bacteria could not be measured in these studies as the culture medium used was not suitable (Harrel 2004).
What are the sources of aerosols and splatter in dental workplace?
A four‐fold increase of airborne bacteria has been observed in areas where dental aerosol‐producing equipment is used (Sawhney 2015). According to General Dental Council in the UK, dental AGPs include use of high‐speed handpieces for routine restorative procedures, use of ultrasonic scalers and high pressure 3:1 air syringe, polishing teeth, use of air‐driven surgical handpieces, air abrasion, slow speed polishing and opening teeth for drainage (FGDP 2020; GDC 2020). In addition, some non‐AGPs such as intraoral radiography can evoke gag reflex leading to coughing or sneezing that results in aerosols. The British Association of Oral Surgeons and British Association of Oral and Maxillofacial Surgeons advises that all urgent dental procedures, including oral examination, be treated as aerosol‐generating (FGDP 2020).Dental hand pieces, ultrasonic scalers, air polishers and air abrasion units produce the most visible aerosols. Each of these instruments removes material from the operative site thus generating aerosols by the action of rotary instruments, ultrasonic vibrations, or the combined action of water sprays and compressed air. Using the bacterial growth method, the ultrasonic scaler has been shown to produce the greatest amount of airborne contamination, followed by the air‐driven high‐speed handpiece, the air polisher and other instruments such as the air‐water syringe and prophylaxis angles (Barnes 1998; Gross 1992; Harrel 1996; Harrel 2004; Muzzin 1999). The particle size of these dental aerosols is less than 50 μm and their small size means they tend to be suspended in the air for longer period of time (Cottone 1991).
One in‐vitro study reported that the position of the handpiece in the dental arch influences the amount of splatter. When the water spray is positioned closer to the oral aperture (e.g. near upper anterior teeth), it is more likely that there is escape of water from the mouth rather than adhering to adjacent oral surfaces or the rubber dam (Dahlke 2012).
Description of the intervention
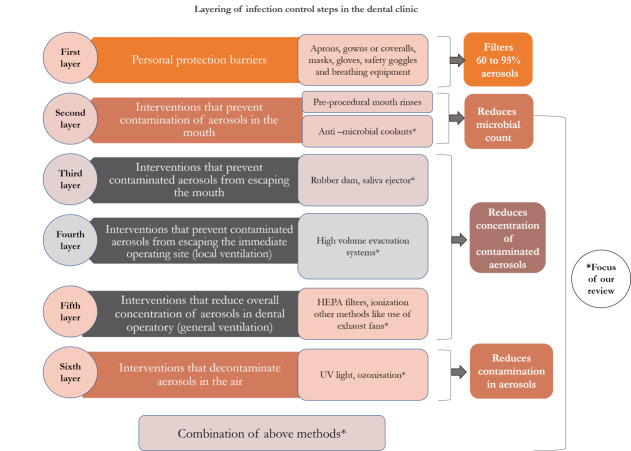
Harrel 2004 suggested layering infection control steps to reduce the potential danger from contaminated dental aerosols, which consisted of: 1. barrier protection – mask, gloves and eye protection; 2. preprocedural rinse with antiseptic mouthwash; 3. high volume evacuator; 4. high efficiency particulate air room filters and ultraviolet (UV) treatment of ventilation system. Many other techniques and devices have been introduced since the early 2000s. We have devised an infographic based on Harrel 2004 to categorise interventions used to reduce contaminated aerosols produced during dental procedures (Figure 1).
1.
Interventions that are not included in our reviews
Personal protective equipment (PPE)
PPE includes aprons, gowns or coveralls (a one‐piece suit), gloves, masks, breathing equipment (respirators) and goggles. PPE reduces operator (dentist, dental assistant or dental laboratory personnel) contact of aerosols thus protecting from exposure to microbial organisms in the aerosol. A Cochrane Review on this topic has recently been published (Verbeek 2020).
Preprocedural mouth rinses
Preprocedural mouth rinses (e.g. chlorhexidine, povidone‐iodine and hydrogen peroxide) have antimicrobial action; they help reduce the salivary concentration of microbial organisms thereby reducing the number of viable microbial organisms in the aerosols during AGPs (Eggers 2018; Harrel 2004). A limitation of the studies testing effectiveness of aerosol‐reducing interventions is the use of bacterial colony‐forming units (CFU) as a surrogate measurement tool to check for reduction in contaminated aerosol. Hence, in patients where the preprocedural rinses are used, the true efficacy of the other interventions may be obscured as the bacterial count in the saliva itself is controlled. Use of mouth rinses in the context of Covid‐19 specifically is currently being evaluated in rapid reviews being undertaken jointly by Cochrane Oral Health and Cochrane Ear Nose and Throat (Burton 2020a; Burton 2020b). Once we complete the current review, we hope to undertake a review of preprocedural mouth rinses for prevention of any infectious disease.
Interventions included in this review
-
Interventions that prevent contamination of aerosols in the mouth (Harrel 2004)
Anti‐microbial agents such as chlorhexidine and povidine iodine are used as coolants along with ultrasonic scalers to reduce the contamination of aerosols in the mouth (Sethi 2019).
-
Interventions that prevent contaminated aerosols from escaping the mouth (Harrel 2004)
Use of a rubber dam during AGPs prevents patient saliva being mixed with the water spray generated from the drill or scaler.
Saliva ejectors (low volume evacuators or low volume aspirators) reduce the aerosols escaping the mouth.
-
Interventions that prevent contaminated aerosols from escaping the immediate operating site (local ventilation)
Aerosols coming out of the mouth can be removed with local exhaust ventilation such as high‐volume evacuation systems (HVE).
-
Interventions that reduce overall concentration of aerosols in dental operatory (general ventilation)
Once the contaminated aerosols escape the immediate operating site and become airborne, air purification methods can be used to tackle them, such as high efficiency particulate air (HEPA) filters, which aim at reducing the overall concentration of aerosols in the dental operatory (Harrel 2004; Yadav 2015).
Ionisation makes the aerosol particles unipolarly charged and thus they repel each other to deposit on the surfaces (Yadav 2015).
Other methods such as avoiding the use of fans that can recirculate the air (Warnakulasuriya 2020), keeping windows open in the dental operatory room and using exhaust fans (Escombe 2019; Stockwell 2019) have been suggested.
-
Interventions that decontaminate aerosols in the air
UV light (Yadav 2015): UV has germicidal properties and short wavelength UV‐C (250 nm to 265 nm wavelength) is used for disinfection purposes.
Ozonisation (Yadav 2015): ozone, an allotrope of oxygen, owes its antimicrobial activity to its high oxidative potential.
Fumigation (Bali 2014) and fogging (McDonnell 2006): fumigation is a chemical method of decontaminating the air in an operating theatre or a clinic by spraying formaldehyde and potassium permanganate in liquid form; fogging uses a mixture of hydrogen peroxide and silver ion solution in the form of aerosols to control the contaminated aerosols (McDonnell 2006).
Combination of methods; other methods
Dentists can select different combinations of the above methods; for example, Cochran 1989 evaluated rubber dam together with HVE and Narayana 2016 assessed preprocedural rinse and HVE to reduce contamination in aerosols. Modifications of existing techniques or equipment may be used, or new devices, e.g. Isolite illuminated dental isolation system (Zyris 2020).
How the intervention might work
Interventions that prevent contamination of aerosols in the mouth
Anti‐microbial agents such as chlorhexidine gluconate and povidine iodine are used as ultrasonic coolants to prevent the contamination of aerosols in the mouth and biofilm formation (Sethi 2019). These agents are used in solution form and lesser concentrations than the agents used in preprocedural rinse or local irrigation. This reduces the contamination of the waterlines, penetration of the agent into the periodontal pocket increases and thus acts on the local microbia to prevent the contamination of aerosols produced (Jawade 2016).
Interventions that prevent contaminated aerosols from escaping the mouth
1. Rubber dam
The rubber dam is a disposable rubber sheet that is stretched around the treated tooth or teeth, and works by isolating the treatment zone from saliva (Al‐amad 2017). Two studies observed a significant reduction in bacterial atmospheric contamination when rubber dams were used (Cochran 1989; Samaranayake 1989). However, contradictory results are reported by Al‐amad and colleagues, which showed an increase in the bacterial contamination on the headscarf of the students who used a rubber dam (Al‐amad 2017). Rubber dam application in certain situations may not establish a perfect seal around the tooth and even expose the gingiva due to reduced clinical crown height (when not using the split dam technique). This can lead to leakage of contaminated saliva, which results in aerosols and thus reduces the efficiency of rubber dam isolation (Al‐amad 2017; Cochran 1989; Fors 1986). Rubber dam may not be of much use in prevention of contaminated aerosols when AGPs are performed on a carious tooth which not only harbours the caries‐causing microbial flora, but other microbial organisms including fungi and viruses.
2. Saliva ejectors
A saliva ejector is a narrow, tubular device that provides suction to remove saliva, blood, tooth material and debris from the mouth during the dental procedures to provide a clear operating field (Merriam‐Webster 2020). The use of saliva ejectors with low or high volume was shown to reduce the production of droplets and aerosols in one study (Yadav 2015); however, neither saliva ejectors nor HVE devices reduced the aerosols and splatter effectively in another study (Holloman 2015). Saliva ejectors in conjunction with HVE devices are more effective than saliva ejectors used alone (Graetz 2014). This is because of the smaller diameter of the tip, which is not capable of clearing the aerosols. Saliva ejectors are preferred in dental practices because of their usefulness in providing a clear operating field, convenient use and comfort as opposed to HVE devices (Graetz 2014; Jacks 2002).
Local ventilation (interventions that prevent contaminated aerosols from escaping the immediate operating site)
1. High volume suction evacuation (high volume evacuator devices or high volume aspirators)
HVE devices are suction devices fitted on an evacuation system that can draw a large volume of air within a short period of time (Avasthi 2018; Harrel 2004). The usual HVE device used in dentistry has a large opening (usually 8 mm or greater) and is attached to an evacuation system that will remove up to 2.8 cubic metres of air per minute (Harrel 2004). They have been tested in controlling aerosol production in dental settings and studies have shown varying results, with 90.8% reduction of aerosols (Jacks 2002) to no statistically significant difference between using and not using HVE devices (Desarda 2014). Proper distance should be maintained by clinicians while holding HVE devices. The device should be held approximately 6 mm to 15 mm away from the active ultrasonic tip or air polisher (Avasthi 2018).
General ventilation
1. High efficiency particulate air filters
A HEPA filter is composed of a mat of randomly arranged fibres and can remove 99.95% (European Standard) of particles measuring 0.3 μm in diameter, from the air that passes through (European Standard 2009 – EN 1822‐1:2009). In the USA, the Institute of Environmental Sciences and Technology (IEST) requires a certified HEPA filter to capture a minimum of 99.97% of contaminants 0.3 mm in size and larger, which means that for every 10,000 particles that pass through the filter, only three can be permitted to escape (Yadav 2015). Filtration involves physical removal of particulates from the air and is a vital aspect in achieving acceptable indoor air quality. Air purifiers utilise different types of filtration such as carbon, HEPA or a mixture such as a carbon/HEPA filtration unit. While a carbon filter is ideal for chemicals and odours in the air, HEPA is ideal for air particles. According to IEST, there are six types of filters used in HEPA (type A, B, C, D, E and F), dependent on performance (Veeck 2004). Portable HEPA filters are also available and are effective in particle reduction when tested in simulated hospital wards (Qian 2010).
2. Ionisation
Ionisers or ionic air purifiers are devices that can either be wearable or stationary. They use charged electrodes to project negative ions into the air. These devices impart electrical charges of the same polarity on aerosol particles. These unipolarly charged particles then repel each other and move away from breathing zone to be deposited on the nearby surfaces (Grinshpun 2001). Another possible mechanism for how this works is that the micro‐organisms floating in the air attract these negatively charged ions and become heavier as a result and then precipitate onto surfaces. However, the micro‐organisms are not destroyed through this process. They remain viable and thus require further treatment through some more conventional form of disinfection (Yadav 2015).
3. Other methods
Other methods, such as avoiding the use of fans, keeping windows open at the dental operatory room and using exhaust fans may help by improving the air circulation (Escombe 2019; Meng 2020; Stockwell 2019).
Decontamination of aerosols in the air
1. Ultraviolet light
Air sterilisation is done using IV irradiation. The DNA of all bacteria and viruses are ruptured, thus rendering them sterile and incapable of reproduction (Harrel 2004; Yadav 2015).
2. Ozonisation
Ozone attacks the cell membrane of bacteria, possible through ozonolysis of carbon–carbon double bonds of membrane lipids leading to lysis of the cell (Gurley 1985). Laboratory studies have shown that ozone at a concentration of over 100 ppm with high humidity was highly virucidal against ribonucleic acid (RNA) viruses (Sato 1990). Ozone molecules are highly reactive and, when they come into contact with micro‐organisms, they react, rendering them harmless. Concerns have been raised about the amount of ozone required to destroy pathogens in the air and whether that would present a health risk to dental personnel and patients (Yadav 2015); however, the half‐life of ozone is 20 minutes and it decomposes to oxygen thus not posing a health hazard (Brown 1999).
3. Fumigation and fogging
Fumigation with formaldehyde was able to reduce Staphylococcus aureus, Streptococcus spp, Escherichia coli and Aspergillus spp in samples obtained in a maxillofacial operating theatre in India because of its bactericidal properties (Bali 2014).
Nowadays, this fumigation method is seldom used because of the carcinogenic effect of formaldehyde and instead, fogging is preferred. Fogging uses a mixture of hydrogen peroxide and silver ion solution to control the contaminated aerosols through its bactericidal action (McDonnell 2006).
Why it is important to do this review
The recent COVID‐19 pandemic and similar communicable diseases have always posed a high risk to health professionals (Coulthard 2020; Laheij 2012; Peng 2020; Samaranayake 2004; Scannapieco 1999). AGPs such as dental drills and surgical drills used in oral surgery procedures form aerosols contaminated with bacteria, fungi and viruses (Al‐Eid 2018; Ishihama 2008; Szymańska 2007). Dentists who treat patients using such AGPs are at risk of contaminating and inoculating themselves if the patient is infected with infections such as COVID‐19 and SARS (Peng 2020; Samaranayake 2004). Dental assistants, other office staff members, and patients are also at risk of inoculation (Froum 2020). According to the US Department of Labor, dental hygienists, dental assistants and general dentists have the highest occupational risk for COVID‐19 with a risk score of 99.7% (hygienists), 92.5% (assistant) and 92.1% (general dentist) (Lu 2020). Similarly, the Occupational Safety and Health Act (OSHA), categorises occupations involved with aerosol production as very high risk (OSHA 2020). The first report on a dentist and two dental nurses contracting COVID‐19 infection was outlined by Wuhan Dental Hospital in the early weeks of the pandemic (Meng 2020).
Dental professionals in many countries have stopped routine care because of regulatory restrictions and fear of spreading COVID‐19 among their patents and beyond. This closure brings significant financial impact for dental professionals, especially for self‐employed practitioners (Coulthard 2020) or dental practices with an NHS contract (UK) who have furloughed their staff. The Association of British Insurers have warned majority of the dental clinics in the UK are not covered for business interruption claims due to the COVID‐19 pandemic (BDA 2020b). Moreover, the abrupt closure of dental services has left many patients midway through procedures such as root canal treatment, dentures, orthodontic treatment, fixed partial dentures and implant‐supported dentures. Patients may be in pain but in fear of attending for urgent treatment or delayed treatment may exacerbate non‐urgent problems. This review will help dental professionals prepare themselves to adopt best practices during and after the COVID‐19 pandemic, by identifying the best methods for reduction of contaminated aerosols in their dental clinics and thus reduce the risk of infectious diseases spreading through aerosols.
Objectives
To assess the effectiveness of methods used during dental treatment procedures to minimise aerosol production and reduce or neutralise contamination in aerosols.
Methods
Criteria for considering studies for this review
Types of studies
We will include randomised controlled trials (RCTs) and controlled clinical trials (CCTs) conducted in a dental environment. We will include studies where the unit of randomisation is dental professionals, participants, dental units or practices.
We will exclude experimental studies conducted in a laboratory environment.
Types of participants
We will include studies with dental staff (dentist, dental surgery assistant, dental hygienist, dental technologist, dental laboratory staff or dental aide) and their patients undergoing a dental AGP.
Types of interventions
We will include any method, procedure or policy that aims to reduce contaminated aerosols in dental clinics compared to any other method or combination of methods.
We will categorise the interventions as:
methods to prevent contamination of aerosols in the mouth ‐ antimicrobial coolants;
methods to prevent contaminated aerosols escaping from the mouth;
local ventilation;
general ventilation;
decontamination of aerosols in the air;
combination of methods.
Types of outcome measures
As this is a rapid review, we are considering only the following key outcomes.
Primary outcomes
Incidence of infection of dental staff or patients.
Reduction in volume of contaminated aerosols in the operative environment.
The reduction of these aerosols can be measured directly as a decrease in the amount of particles, using optical particle counters, condensation nuclei counters, aerodynamic analyses, scanning mobility particle sizer spectrometers (Górny 2020), adenosine triphosphate (ATP) bioluminescence (Watanabe 2018), or use of fluorescent dye to count splatter (Veena 2015).
Reduction in level of contamination in aerosols in the operative environment.
The reduction in contamination can be measured with surrogate methods such as bacterial CFU of oral bacteria that are found in the working environment or standard index of microbial air contamination (IMA) (Pasquarella 2000). We call this a surrogate outcome because these bacterial CFUs do not represent the quantity of aerosols. The CFUs can be the result of any contamination and not just from aerosols, thus making it a less reliable outcome measure.
Secondary outcomes
Costs for the interventions used (measured in local currency).
Acceptability and feasibility of the intervention to patients and dentists (measured using ordinal (e.g. Likert scale) or dichotomous (e.g. yes/no) data).
Search methods for identification of studies
Cochrane Oral Health's Information Specialist will conduct systematic searches for RCTs and CCTs. There will be no language, publication year or publication status restrictions. We will contact original authors for clarification and further data if trial reports are unclear and we will arrange translations of papers where possible.
Electronic searches
Cochrane Oral Health's information specialist will search the following databases from their inception:
Cochrane Oral Health's Trials Register;
the Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Register of Studies;
MEDLINE Ovid (from 1946 onwards);
Embase Ovid (from 1980 onwards);
WHO COVID‐19 Global literature on coronavirus disease (search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov; search to date)
Subject strategies will be modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, they will be combined with subject strategy adaptations of the highly sensitive search strategies designed by Cochrane for identifying RCTs and CCTs as described in the Cochrane Handbook for Systematic Reviews of Interventions, Technical Supplement to Chapter 4 (Lefebvre 2019).
Searching other resources
Cochrane Oral Health's information specialist will search the following databases to identify ongoing studies:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov/);
Cochrane COVID‐19 Study Register (covid-19.cochrane.org/) (search via the Cochrane Register of Studies).
A search of the WHO's International Clinical Trials Registry Platform is mandatory for Cochrane Reviews; however, this database will not be available at the time of the search due to the COVID‐19 pandemic. We will search this database for any updates of this review.
We will also undertake a non‐systematic search of the internet using Google.
We will not perform a separate search for adverse effects. We will consider adverse effects described in included studies only.
We will make efforts to identify full‐text papers regardless of language of publication and endeavour to seek help with translation; however, we will not delay the rapid review process. Any papers that we are unable to source quickly or are unable to get translated will be listed as awaiting assessment.
Data collection and analysis
Selection of studies
Two review authors will screen at least 20% (search results) of the titles and abstracts for calibration purposes. We will consider a minimum of 80% agreement between these two review authors. After calibration, one review author will screen the abstracts and the second review author will screen all excluded abstracts. Any conflicts during the screening will be resolved by mutual discussion. If this is not possible, a third review author (arbiter) will be consulted and consensus will be reached through discussion. We will use online Rayyan software to screen the titles and abstracts (Rayyan 2016).
Two review authors will screen at least 20% of full‐text articles for calibration purposes. We will consider a minimum of 80% agreement between these two review authors. Then, one review author will screen all the full‐text articles with a second review author to screen all excluded full‐text articles and complete a 'Characteristics of excluded studies' table. For included studies, we will extract useful information and data from the full‐text articles and complete a 'Characteristics of included studies' table.
Where studies have multiple publications, we will collate the reports of the same study so that each study, rather than each report, is the unit of interest for the review, and such studies have a single identifier with multiple references.
Data extraction and management
One review author will design the data extraction form and one review author will test its suitability. One review author will extract the data using the data extraction form. The second review author will verify the correctness and completeness of data extracted. We will limit data extraction to a minimal set of required data items.
Assessment of risk of bias in included studies
Two review authors will assess risk of bias, using the Cochrane 'Risk of bias' tool for RCTs and ROBINS‐I tool for CCTs, and report the results in a table (Higgins 2019). For RCTs, we will classify each domain at high, low or unclear risk of bias (Higgins 2019). For CCTs, we will classify each domain at low, moderate, serious, critical risk of bias or no information to assess risk of bias (Sterne 2016). We will attempt to contact the trial authors if information is not specified or is unclear. We will resolve any disagreements by discussion between the review authors. If consensus cannot be reached, we will consult a third review author (arbiter). Preferably, we want to include studies that randomise staff to intervention and control with a sufficiently large sample of patients. If patients are randomised but the same professional is implementing both interventions being compared, there is a higher likelihood of performance bias.
Measures of treatment effect
We will present the effect sizes for dichotomous outcomes as risk ratios (RR) and 95% confidence intervals (CIs). We will report continuous outcomes as mean differences (MD) and 95% CIs. If the included trials have reported continuous outcomes obtained from different instruments, we will use the standardised mean difference (SMDs) and 95% CI as the effect measure. We will qualitatively describe the costs for the interventions used. If we find ordinal data, we will dichotomise the data and present the effect sizes as RR and 95% CIs.
Unit of analysis issues
We do not anticipate that any cluster‐randomised studies will meet the inclusion criteria of this review. If we identify multi‐arm trials, we will select relevant arms for inclusion in our analyses. If more than two arms are relevant to this review, we will split the control group between multiple comparisons so that participants are not double‐counted in meta‐analysis.
Dealing with missing data
If we encounter trials with missing data, we will contact the investigators or sponsors of these studies, wherever possible. We will calculate missing data from other data such as standard deviations (SDs) from P values if needed. We will re‐analyse the data according to the intention‐to‐treat (ITT) principle whenever possible.
Assessment of heterogeneity
We will assess heterogeneity by visually inspecting the forest plots to determine closeness of point estimates with each other and overlap of CIs. We will use the Chi2 test with a P value of 0.1 to indicate statistical significance. We will also use the I2 statistic, following the interpretation recommended in the Cochrane Handbook for Systematic Reviews of Interventions (0% to 40% might not be important; 30% to 60% may represent moderate heterogeneity; 50% to 90% may represent substantial heterogeneity; 75% to 100% considerable heterogeneity).
Assessment of reporting biases
If we include 10 or more studies, we will construct a funnel plot to investigate any potential reporting bias.
Data synthesis
We will analyse the data using Review Manager 5 (Review Manager 2014). In the absence of substantial clinical or methodological heterogeneity, we will perform a meta‐analysis using a random‐effects model. If there is substantial or considerable heterogeneity, we will investigate heterogeneity using a subgroup analysis. Where a meta‐analysis is not appropriate, we will discuss the data narratively.
Subgroup analysis and investigation of heterogeneity
We plan to investigate heterogeneity by performing the following subgroup analyses.
Type of AGP (e.g. ultrasonic and sonic scaling, tooth preparation using air turbine handpiece or air abrasion, three‐way syringe).
Type of clinical set‐up (e.g. single chair, polyclinic, operating theatre for minor oral surgery).
Types of filters used in HEPA (e.g. type A, B, C, D, E or F).
Procedure performed in anterior teeth or posterior teeth.
Biological assessment used (CFU, fluorescent dye‐stained splatter).
Position of the culture plates (for CFU).
Sensitivity analysis
To explore the possible effect of losses to follow‐up on the effect estimates for the primary outcomes, we will perform sensitivity analyses. For dichotomous outcomes, we will vary the event rate within the missing participants from intervention and control groups within plausible limits. We will perform sensitivity analyses for assumptions that we have made in our analyses. We will remove those studies at high risk of bias or NRCTs (or both) and report any significant difference between the results of these analyses.
Summary of findings and assessment of the certainty of the evidence
We will summarise the results of the analyses in 'Summary of findings' tables for the primary outcomes for all comparisons.
Incidence of infection of dental staff or patients.
Reduction in volume of contaminated aerosols in the operative environment.
Reduction in level of contamination in aerosols in the operative environment.
We will use the GRADE framework to evaluate the certainty of evidence for each outcome as high, moderate, low or very low, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2019). We will justify all decisions to downgrade the certainty of the evidence using footnotes and we will make comments to aid reader's understanding of the review where necessary.
History
Protocol first published: Issue 7, 2020
Acknowledgements
We are extremely thankful to Cochrane Oral Health: Anne Littlewood, Information Specialist; Laura MacDonald, Managing Editor; Professor Anne Marie Glenny and Professor Jan Clarkson, Co‐ordinating Editors; and Professor Helen Worthington. We thank peer reviewers Professor Nicola Innes, Derek Richards and Professor Julián Balanta Melo, and copy editor Anne Lawson. We thank Professor Dr Jaspal Singh Sahota, Chief Executive, Melaka‐Manipal Medical College, Melaka campus and Professor Dr Abdul Rashid Hj Ismail, Dean, Faculty of Dentistry, Melaka‐Manipal Medical College for constant support to undertake Cochrane Reviews.
We would like to thank Farhad Shokraneh, Information Specialist at Cochrane Schizophrenia, University of Nottingham, for peer reviewing the search strategy and Dr Tony Francis, Assistant Professor in Department of Conservative and Endodontics, Faculty of Dentistry, Melaka‐Manipal Medical College for the valuable input during the preparation of this protocol.
Appendices
Appendix 1. MEDLINE Ovid search strategy
1. exp dentistry/ 2. exp dental facilities/ 3. infection control, dental/ 4. exp dentists/ 5. dental staff/ 6. exp dental auxiliaries/ 7. (dental or dentist$ or hygienist$).mp. 8. ((oral or maxillofacial) adj5 (care$ or procedure$ or surgery or surgical or medicine)).mp. 9. orthodonti$.mp. 10. periodont$.mp. 11. (tooth or teeth or gum$ or endodont$ or plaque$ or pulpotom$ or pulpectom$ or "cavity prep$" or molar$ or bicuspid$ or premolar$ or pre‐molar$ or incisor$ or canine$ or eyetooth or eyeteeth or cuspid$).mp. 12. ((scal$ adj2 polish$) or "root canal" or (root adj6 resect$) or (root$ adj3 planing) or apicectom$ or apicoectom$).mp. 13. ((root$ or periodont$ or dental or subgingiv$ or gingiv$ or supragingiv$) adj5 (scale or scaling or scaler$ or curettage)).mp. 14. Dental high speed equipment/ 15. ("high speed air rotor$" or "low speed handpiece$" or "low speed hand piece$" or micromotor$ or "turbine handpiece$" or "electrosurgery unit" or "air polisher$" or "prophy angle$" or "air‐water syringe$" or "high speed hand piece$" or "high speed handpiece$" or "three‐way air syringe$" or "threeway air syringe$" or "ultrasonic scaler$" or "hard‐tissue laser$" or "dental drill$" or "piezo unit$" or "piezo hand piece$" or "piezo handpiece$" or "rotary instrument$" or "air abrasion" or "water spray$").mp. 16. or/1‐15 17. Air microbiology/ 18. Air pollution, indoor/ 19. Aerosols/ 20. Inhalation exposure/ 21. (aerosol$ or bioaerosol$).mp. 22. (droplet$ or splatter$ or spatter$ or microbe$ or bacillus or germ$ or microorganism$ or virus$ or viral or coronavirus$ or COVID$ or "middle east? respiratory syndrome$" or MERS or MERS‐CoV or "camel flu" or SARS or "sudden acute respiratory syndrome$" or "Wuhan virus$" or 2019‐nCoV or SARS‐CoV‐2 or SARS‐CoV or SARS‐CoV‐1 or SARS‐1).mp. 23. (air adj5 (pollut$ or quality or impur$)).mp. 24. or/17‐23 25. Decontamination/ 26. ("high volume evacuat$" or HVE or "high volume aspirat$").mp. 27. Rubber dams/ 28. ((rubber adj dam$) or (oral adj dam$) or (dental adj dam$) or (latex adj dam$) or Kofferdam).mp. 29. ("Optra Dam" or "OptraDam Plus" or OptiDam or FlexiDam or "Hygenic Fiesta").mp. 30. Suction/ 31. ("saliva ejector" or "low volume aspirat$" or (suction adj2 saliva)).mp. 32. Air filters/ 33. (air adj5 (filter$ or filtration or purif$ or clean$)).mp. 34. ((HEPA or "High Efficiency Particulate Air" or "High Efficiency Particulate Arrestance") adj5 filter$).mp. 35. Air ionization/ 36. (ionis$ or ioniz$).mp. 37. Ozone/ 38. (ozonis$ or ozoniz$).mp. 39. Ultraviolet rays/ 40. (ultraviolet or UV or ultra‐violet or actinic).mp. 41. ((aerosol$ or bioaerosol$ or droplet$ or spatter or splatter) adj2 reduc$).mp. 42. Fumigation/ 43. (fog$ or fumigat$ or decontaminat$ or "smoke out" or smokeout or depollut$ or depurat$).mp. 44. or/25‐43 45. 16 and 24 and 44
This subject search will be linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity‐maximising version (2008 revision) (Lefebvre 2019).
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Contributions of authors
SKN initiated this review and all authors contributed to drafting the protocol. Responsibilities for the full review will be: SKN: obtaining full‐text articles, data analysis and final review draft preparation, and review update. PE: drafting protocol, data extraction, data analysis and final review draft preparation. MP: drafting protocol, screening of titles and abstracts, screening full texts and final review draft preparation. MN: drafting protocol, arbiter, data extraction, analysis and final review draft preparation. GS: drafting protocol, screening of titles and abstracts, screening full texts and final review draft preparation. JHV: drafting protocol, data extraction and analysis, writing results and discussion.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Institute for Health Research (NIHR), UK
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Oral Health. The views and opinions expressed are those of the authors and not necessarily those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health and Social Care.
-
Cochrane Oral Health Global Alliance, Other
The production of Cochrane Oral Health reviews has been supported financially by our Global Alliance since 2011 (oral‐health.cochrane.org/partnerships‐alliances). Contributors over the past two years have been the American Association of Public Health Dentistry, USA; AS‐Akademie, Germany; the British Association for the Study of Community Dentistry, UK; the British Society of Paediatric Dentistry, UK; the Canadian Dental Hygienists Association, Canada; the Centre for Dental Education and Research at All India Institute of Medical Sciences, India; the National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; NHS Education for Scotland, UK; and the Swiss Society for Endodontology, Switzerland.
Declarations of interest
SKN: none. PE: none. MP: none. MN: none. GS: none. JHV: none.
New
References
Additional references
ADA 2020
- American Dental Association. COVID-19 frequently asked questions. success.ada.org/en/practice-management/patients/coronavirus-frequently-asked-questions?utm_source=cpsorg&utm_medium=covid-nav&utm_content=nav-faq&utm_campaign=covid-19 (accessed 16 April 2020).
Al‐amad 2017
- Al-amad SH, Awad MA, Edher FM, Shahramian K, Omran TA. The effect of rubber dam on atmospheric bacterial aerosols during restorative dentistry. Journal of Infection and Public Health 2017;10(2):195-200. [DOI] [PubMed] [Google Scholar]
Al‐Eid 2018
- Al-Eid RA, Ramalingam S, Sundar C, Aldawsari M, Nooh N. Detection of visually imperceptible blood contamination in the oral surgical clinic using forensic luminol blood detection agent. Journal of International Society of Preventive & Community Dentistry 2018;8(4):327-32. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
ALOP 2020
- The Latin American Association of Pediatric Dentistry (Asociación Latinoamericana de Odontopediatría ALOP). Recommendations for care in pediatric dentistry versus Covid-19. www.acop.com.co/2020/04/13/recomendaciones-de-atencion-en-odontopediatria-frente-al-covid-19/ (accessed 13 April 2020).
Avasthi 2018
- Avasthi A. High volume evacuator (HVE) in reducing aerosol – an exploration worth by clinicians. Journal of Dental Health, Oral Disorders & Therapy 2018;9(3):165-6. [Google Scholar]
Bali 2014
- Bali R, Sharma P, Nagrath S, Gupta P. Microbial isolations from maxillofacial operation theatre and its correlation to fumigation in a teaching hospital in India. Journal of Maxillofacial and Oral Surgery 2014;13(2):128-32. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Barnes 1998
- Barnes JB, Harrel SK, Rivera-Hidalgo F. Blood contamination of the aerosols produced by in vivo use of ultrasonic scalers. Journal of Periodontology 1998;69(4):434-8. [DOI] [PubMed] [Google Scholar]
BDA 2020a
- British Dental Association. Personal protective equipment (PPE). bda.org/advice/Coronavirus/Pages/face-mask-shortage.aspx (accessed 6 June 2020).
BDA 2020b
- British Dental Association. Coronavirus: the financial impact. bda.org/advice/Coronavirus/Pages/financial-impact.aspx (accessed 6 June 2020).
Brown 1999
- Brown K, Xu Y. Fogging for the disinfection of food processing factories and equipment. Trends in Food Science & Technology 1999;10(6-7):205-10. [Google Scholar]
Burton 2020a
- Burton MJ, Clarkson JE, Goulao B, Glenny A-M, McBain AJ, Schilder AG, et al. Antimicrobial mouthwashes (gargling) and nasal sprays to protect healthcare workers when undertaking aerosol-generating procedures (AGPs) on patients without suspected or confirmed COVID-19 infection. Cochrane Database of Systematic Reviews 2020, Issue 5. Art. No: CD013628. [DOI: 10.1002/14651858.CD013628] [DOI] [PMC free article] [PubMed] [Google Scholar]
Burton 2020b
- Burton MJ, Clarkson JE, Goulao B, Glenny A-M, McBain AJ, Schilder AG, et al. Use of antimicrobial mouthwashes (gargling) and nasal sprays by healthcare workers to protect them when treating patients with suspected or confirmed COVID-19 infection. Cochrane Database of Systematic Reviews 2020, Issue 5. Art. No: CD013626. [DOI: 10.1002/14651858.CD013626] [DOI] [PMC free article] [PubMed] [Google Scholar]
CDC 2020
- Centers for Disease Control and Prevention. Dental settings: interim infection prevention and control guidance for dental settings during the COVID-19 response. www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html (accessed 27 April 2020).
Cochran 1989
- Cochran MA, Miller CH, Sheldrake MA. The efficacy of the rubber dam as a barrier to the spread of microorganisms during dental treatment. Journal of American Dental Association 1989;119(1):141-4. [DOI] [PubMed] [Google Scholar]
Cottone 1991
- Cottone JA, Terezhalmy GT, Molinari JA. Practical Infection Control in Dentistry. Baltimore (MD): Williams and Wilkins, 1991. [Google Scholar]
Coulthard 2020
- Coulthard P. Dentistry and coronavirus (COVID-19) – moral decision-making. British Dental Journal 2020;228(7):503-5. [DOI] [PubMed] [Google Scholar]
Dahlke 2012
- Dahlke WO, Cottam MR, Herring MC, Leavitt JM, Ditmyer MM, Walker RS. Evaluation of the spatter-reduction effectiveness of two dry-field isolation techniques. Journal of American Dental Association 2012;143:1199-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Desarda 2014
- Desarda H, Gurav A, Dharmadhikari C, Shete A, Gaikwad S. Efficacy of high-volume evacuator in aerosol reduction: truth or myth? A clinical and microbiological study. Journal of Dental Research, Dental Clinics, Dental Prospects 2014;8(3):176-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dominiak 2020
- Dominiak M, Różyło-Kalinowska I, Gedrange T, Konopka T, Hadzik J, Bednarz W, et al. COVID-19 and professional dental practice. The Polish Dental Association Working Group recommendations for procedures in dental office during an increased epidemiological risk. Journal of Stomatology 2020;73(1):1-10. [Google Scholar]
Eggers 2018
- Eggers M, Koburger-Janssen T, Eickmann M, Zorn J. In vitro bactericidal and virucidal efficacy of povidone-iodine gargle/mouthwash against respiratory and oral tract pathogens. Infectious Diseases and Therapy 2018;7(2):249-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Escombe 2019
- Escombe AR, Ticona E, Chávez-Pérez V, Espinoza M, Moore DA. Improving natural ventilation in hospital waiting and consulting rooms to reduce nosocomial tuberculosis transmission risk in a low resource setting. BMC Infectious Diseases 2019;19(1):88. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
European Standard 2009
- European Standard. High efficiency air filters (EPA, HEPA and ULPA). European Standard EN 1822-1:2009.
FGDP 2020
- Faculty of General Dental Practice (UK). COVID-19: updated guidance and resources as lockdown eases. fgdp.org.uk/news/covid-19-updated-guidance-and-resources-lockdown-eases 21 May 2020.
Fors 1986
- Fors UG, Berg JO, Sandberg H. Microbiological investigation of saliva leakage between the rubber dam and tooth during endodontic treatment. Journal of Endodontics 1986;12(9):396-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Froum 2020
- Froum S, Strange M. COVID-19 and the problem with dental aerosols. www.perioimplantadvisory.com/periodontics/oral-medicine-anesthetics-and-oral-systemic-connection/article/14173521/covid19-and-the-problem-with-dental-aerosols (accessed 6 June 2020).
GDC 2020
- GDC. Aerosol generating procedures. gdc-uk.org/docs/default-source/covid-19/use-of-aerosol-generating-procedures-(agps).pdf?sfvrsn=5a95b3b3_2 18 March 2020.
Graetz 2014
- Graetz C, Bielfeldt J, Tillner A, Plaumann A, Dörfer CE. Spatter contamination in dental practices – how can it be prevented? Revista Medico-Chirurgicala a Societatii de Medici si Naturalisti din Lasi 2014;118:1122-34. [PMID: ] [PubMed] [Google Scholar]
Grinshpun 2001
- Grinshpun S, Mainelis G, Reponen T, Willeke K, Trunov MA, Adhikari A. Effect of wearable ionizers on the concentration of respirable airborne particles and microorganisms. Journal of Aerosol Science 2001;32(Suppl 1):S335-6. [Google Scholar]
Gross 1992
- Gross KB, Overman PR, Cobb C, Brockmann S. Aerosol generation by two ultrasonic scalers and one sonic scaler. A comparative study. Journal of Dental Hygiene 1992;66(7):314-8. [PubMed] [Google Scholar]
Gurley 1985
- Gurley B. Ozone: a pharmaceutical sterilant of the future? Journal of Parenteral Science and Technology 1985;39(6):256-61. [PubMed] [Google Scholar]
Górny 2020
- Górny RL. Microbial aerosols: sources, properties, health effects, exposure assessment – a review. KONA Powder and Particle Journal 2020;37:64-84. [DOI: 10.14356/kona.2020005] [DOI] [Google Scholar]
Harrel 1996
- Harrel SK. Clinical use of an aerosol-reduction device with an ultrasonic scaler. Compendium of Continuing Education in Dentistry 1996;17(12):1185-93; quiz 1194. [PubMed] [Google Scholar]
Harrel 2004
- Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. Journal of the American Dental Association (1939) 2004;135(4):429-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2019
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions. 2nd edition. Hoboken (NJ): Wiley-Blackwell, 2019. [Google Scholar]
Holloman 2015
- Holloman JL, Mauriello SM, Pimenta L, Arnold RR. Comparison of suction device with saliva ejector for aerosol and spatter reduction during ultrasonic scaling. Journal of the American Dental Association (1939) 2015;146(1):27-33. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ishihama 2008
- Ishihama K, Iida S, Koizumi H, Wada T, Adachi T, Isomura-Tanaka E, et al. High incidence of blood exposure due to imperceptible contaminated splatters during oral surgery. Journal of Oral and Maxillofacial Surgery 2008;66(4):704-10. [PMID: ] [DOI] [PubMed] [Google Scholar]
Jacks 2002
- Jacks ME. A laboratory comparison of evacuation devices on aerosol reduction. Journal of Dental Hygiene 2002;76:202-6. [PubMed] [Google Scholar]
Jain 2020
- Jain M, Mathur A, Mathur A, Mukhi PU, Ahire M, Pingal C. Qualitative and quantitative analysis of bacterial aerosols in dental clinical settings: risk exposure towards dentist, auxiliary staff, and patients. Journal of Family Medicine and Primary Care 2020;9(2):1003-8. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
James 2016
- James R, Mani A. Dental aerosols: a silent hazard in dentistry! International Journal of Scientific Research 2016;5:1761-3. [Google Scholar]
Jawade 2016
- Jawade R, Bhandari V, Ugale G, Taru S, Khaparde S, Kulkarni A, et al. Comparative evaluation of two different ultrasonic liquid coolants on dental aerosols. Journal of Clinical and Diagnostic Research : JCDR 2016;10(7):ZC53-7. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kormuth 2018
- Kormuth KA, Lin K, Prussin AJ II, Vejerano EP, Tiwari AJ, Cox SS, et al. Influenza virus infectivity is retained in aerosols and droplets independent of relative humidity. Journal of Infectious Diseases 2018;218(5):739-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
Laheij 2012
- Laheij AM, Kistler JO, Belibasakis GN, Välimaa H, Soet JJ. Healthcare-associated viral and bacterial infections in dentistry. Journal of Oral Microbiology 2012;4:4. [DOI: 10.3402/jom.v4i0.17659] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2019
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Technical supplement to Chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston MS, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions, Version 6 (updated July 2019). Cochrane, 2019. Available from: www.training.cochrane.org/handbook.
Lessler 2009
- Lessler J, Reich NG, Brookmeyer R, Perl TM, Nelson KE, Cummings DA. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infectious Diseases 2009;9(5):291-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leung 2020
- Leung NH, Chu DK, Shiu EY, Chan K-H, McDevitt JJ, Hau Benien JP, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nature Medicine 2020;26:676-80. [DOI: 10.1038/s41591-020-0843-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewis 2020
Lu 2020
- Lu M. The front line: visualizing the occupations with the highest COVID-19 risk. Visual Capitalist 15 April 2020. [www.visualcapitalist.com/the-front-line-visualizing-the-occupations-with-the-highest-covid-19-risk/]
McDonnell 2006
Meng 2020
- Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. Journal of Dental Research 2020;99(5):481-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Merriam‐Webster 2020
- Merriam-Webster Online Medical Dictionary. Saliva ejector. www.merriam-webster.com/medical/saliva%20ejector (accessed 5 May 2020).
Monarca 2000
- Monarca S, Grottolo M, Renzi D, Paganelli C, Sapelli P, Zerbini I, et al. Evaluation of environmental bacterial contamination and procedures to control cross infection in a sample of Italian dental surgeries. Occupational and Environmental Medicine 2000;57(11):721-6. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Muzzin 1999
- Muzzin KB, King TB, Berry CW. Assessing the clinical effectiveness of an aerosol reduction device for the air polisher. Journal of the American Dental Association 1999;130(9):1354-9. [DOI] [PubMed] [Google Scholar]
Narayana 2016
- Narayana TV, Mohanty L, Sreenath G, Vidhyadhari P. Role of preprocedural rinse and high volume evacuator in reducing bacterial contamination in bioaerosols. Journal of Oral and Maxillofacial Pathology 2016;20(1):59-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCUDSPH 2020
- Le Collège National des Chirurgiens-Dentistes Universitaires en Santé Publique. Recommendations to deal with the Covid19 epidemic. www.dentairesantepublique.fr/recommandations-face-a-lepidemie-covid19/ (accessed 18 March 2020).
OSHA 2020
- US Department of Labor: Occupational Safety and Health Administration. Guidance on preparing workplaces for COVID-19. www.osha.gov/Publications/OSHA3990.pdf (accessed prior to 16 June 2020).
Pasquarella 2000
- Pasquarella C, Pitzurra O, Savino A. The index of microbial air contamination. Journal of Hospital Infection 2000;46(4):241-56. [DOI] [PubMed] [Google Scholar]
Peng 2020
- Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. International Journal of Oral Science 2020;12(1):1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Polednik 2014
- Polednik B. Aerosol and bioaerosol particles in a dental office. Linking Exposure and Health in Environmental Public Health Tracking 2014;134:405-9. [DOI] [PubMed] [Google Scholar]
Qian 2010
- Qian H, Li Y, Sun H, Nielsen PV, Huang X, Zheng X. Particle removal efficiency of the portable HEPA air cleaner in a simulated hospital ward. Building Simulation 2010;3(3):215-24. [Google Scholar]
Rautemaa 2006
- Rautemaa R, Nordberg A, Wuolijoki-Saaristo K, Meurman J. Bacterial aerosols in dental practice – a potential hospital infection problem? Journal of Hospital Infection 2006;64(1):76-81. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rayyan 2016 [Computer program]
- Qatar Computing Research Institute, Hamad Bin Khalifa University Rayyan QCRI, the Systematic Reviews web app. Doha, Qatar: Qatar Computing Research Institute, Hamad Bin Khalifa University, 2016.
Review Manager 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Samaranayake 1989
- Samaranayake LP, Reid J, Evans D. The efficacy of rubber dam isolation in reducing atmospheric bacterial contamination. ASDC Journal of Dentistry for Children 1989;56(6):442-4. [PMID: ] [PubMed] [Google Scholar]
Samaranayake 2004
- Samaranayake LP, Peiris M. Severe acute respiratory syndrome and dentistry: a retrospective view. Journal of the American Dental Association (1939) 2004;135(9):1292-302. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sato 1990
- Sato H, Wananabe Y, Miyata H. Virucidal effect of ozone treatment of laboratory animal viruses. Jikken Dobutsu. Experimental Animals 1990;39(2):223-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Sawhney 2015
- Sawhney A, Venugopal S, Babu GR, Garg A, Mathew M, Yadav M, et al. Aerosols how dangerous they are in clinical practice. Journal of Clinical and Diagnostic Research : JCDR 2015;9(4):ZC52-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Scannapieco 1999
- Scannapieco F. Role of oral bacteria in respiratory infection. Journal of Periodontology 1999;70:793-801. [DOI] [PubMed] [Google Scholar]
Scannapieco 2004
- Scannapieco FA, Ho AW, DiTolla M, Chen C, Dentino AR. Exposure to the dental environment and prevalence of respiratory illness in dental student populations. Journal (Canadian Dental Association) 2004;70(3):170-4. [PMID: ] [PubMed] [Google Scholar]
Sethi 2019
- Sethi KS, Mamajiwala A, Mahale S, Raut CP, Karde P. Comparative evaluation of the chlorhexidine and cinnamon extract as ultrasonic coolant for reduction of bacterial load in dental aerosols. Journal of Indian Society of Periodontology 2019;23(3):226-33. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sotiriou 2008
Sterne 2016
- Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. [DOI: 10.1136/bmj.i4919] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stockwell 2019
- Stockwell RE, Ballard EL, O'Rourke P, Knibbs LD, Morawska L, Bell SC. Indoor hospital air and the impact of ventilation on bioaerosols: a systematic review. Journal of Hospital Infection 2019;103(2):175-84. [DOI] [PubMed] [Google Scholar]
Szymańska 2007
- Szymańska J. Dental bioaerosol as an occupational hazard in a dentist's workplace. Annals of Agricultural and Environmental Medicine : AAEM 2007;14(2):203-7. [PMID: ] [PubMed] [Google Scholar]
Upendran 2020
- Upendran A, Geiger Z. https://www.ncbi.nlm.nih.gov/books/NBK470356/. January 2020 edition. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, Updated 2020 Feb 17. [Google Scholar]
Veeck 2004
- Veeck AC. Types of HEPA filters. In: NAFA Guide to Air Filtration. 3 edition. Middleton (WI): NAFA, 2004. [Google Scholar]
Veena 2015
- Veena HR, Mahantesha S, Joseph Preethi A, Patil Sudhir R, Patil Suvarna H. Dissemination of aerosol and splatter during ultrasonic scaling: a pilot study. Journal of Infection and Public Health 2015;8(3):260-5. [DOI] [PubMed] [Google Scholar]
Verbeek 2020
- Verbeek JH, Rajamaki B, Ijaz S, Sauni R, Toomey E, Blackwood B, et al. Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database of Systematic Reviews 2020, Issue 4. Art. No: CD011621. [DOI: 10.1002/14651858.CD011621.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Warnakulasuriya 2020
- Warnakulasuriya S. Protecting dental manpower from COVID-19 infection. Oral Diseases 2020 May 13 [Epub ahead of print]. [DOI: 10.1111/odi.13410] [DOI] [PMC free article] [PubMed]
Watanabe 2018
- Watanabe A, Tamaki N, Yokota K, Matsuyama M, Kokeguchi S. Use of ATP bioluminescence to survey the spread of aerosol and splatter during dental treatments. Journal of Hospital Infection 2018;99(3):303-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
WHO 2020
- World Health Organization. WHO timeline – COVID-19. www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19 (accessed prior to 16 June 2020).
WHO 2020a
- World Health Organization. Maintaining essential health services:operational guidance for theCOVID-19 context - Interim guide. WHO/2019-nCoV/essential_health_services/2020.2 1 June 2020:34 and 36.
Yadav 2015
- Yadav N, Agrawal B, Maheshwari C. Role of high-efficiency particulate arrestor filters in control of air borne infections in dental clinics. SRM Journal of Research in Dental Sciences 2015;6(4):240-2. [Google Scholar]
Zemouri 2017
- Zemouri C, Soet H, Crielaard W, Laheij A. A scoping review on bio-aerosols in healthcare and the dental environment. PloS One 2017;12(5):e0178007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zyris 2020
- Zyris: dental isolation systems and mouthpieces (formerly Isolite). www.zyris.com/ 2020.