Abstract
Background and Objectives
This study presents an update of the surgical outcomes of congenital heart disease (CHD) according to Korea Heart Foundation (KHF) data.
Methods
We investigated the data of the 7,305 patients who were economically supported by KHF in 2000–2014. Of them, we analyzed surgical outcomes of the 6,599 patients who underwent CHD surgery.
Results
The median patient age was 1.9 years (range, 0–71.5 years). Of the 6,599 patients, 5,616 (85.1%) underwent biventricular repair and 983 (14.9%) underwent palliative procedures. The mean Basic Aristotle Score was 6.6±2.2. A complex procedure (defined as Basic Aristotle Score above 6) was performed in 3,368 patients (51.0%). The early mortality rate was 3.8%, while the late mortality rate was 1.8%. Previous reports of the KHF (1984–1999) showed that the early surgical and late mortality rates were 8.6%, and 5.3%, respectively. There were 491 neonates (7.4%); among them, the early mortality rate was 12.2% and late mortality rate was 3.7%. There were 2,617 infants (40.0%); among them, the early mortality rate was 6.0% and the late mortality rate was 2.3%. A total of 591 patients from 30 countries were helped by the KHF.
Conclusions
More neonatal surgeries (491 vs. 74 patients) were performed than those in the past (1984–1999). The surgical outcomes were much better than before. Our surgical outcomes revealed that the Republic of Korea has been transformed from a country receiving help to a country that helps other low socioeconomic status countries.
Keywords: Heart defects, congenital; Treatment outcomes
INTRODUCTION
Before the establishment of the Korea Heart Foundation (KHF), children with congenital heart disease (CHD) in the Republic of Korea were helped with support from other developed countries.1),2) For example, 2 children with CHD were brought to the United States on return flight following President Reagen's visit to Korea in 1983.3),4) These events increased social motivation for the KHF, which has supported many children with CHD since its establishment in 1984.
Two previous reports (not published in English) (1984–1990, 1990–1999) described the KHF experience with economically supported patients.
Here we present the surgical experience and outcomes of CHD in the recent era (2000–2014). In 1996, Korea was registered with the Organization for Economic Cooperation and Development. In 2006, the national per capita income in Korea exceeded 20,000 US dollars. Thus, we estimated that patient characteristics including age and CHD complexity would differ from those in the earlier eras. Since nationwide validated data of volume and surgical outcomes of CHD are not available, these data from the KHF will reveal the use of CHD surgery in the Republic of Korea. This study investigated the surgical mortality of CHD in the recent era (2000–2014) using the KHF data.
METHODS
After the study received approval from the institutional ethical committee, we performed a retrospective analysis of data of the 7,305 patients who were supported by KHF between 2000 and 2014. Of them, we analyzed the surgical outcomes of the 6,599 patients who underwent congenital heart surgery. The patients' diseases were classified by the 2 previous reports, and current diagnoses that were absent during past era were added to the new classification.
Early mortality was defined as death within 30 days after surgery or death before discharge. All data were stratified by complexity using the following methodologies: 1) Aristotle Basic Complexity (ABC) score5); and 2) Risk Adjustment for Congenital Heart Surgery-1 (RACHS-1) score.6)
Statistical analysis
Continuous variables are expressed as median and range or mean and standard deviation. Descriptive statistics are described as count and percentage. The chi-square test or Fisher's exact test was used to compare categorical variables. Results were considered statistically significant when the p value was <0.05. SPSS software version 18.0 (SPSS Inc., Chicago, IL, USA) was used for the data analysis.
RESULTS
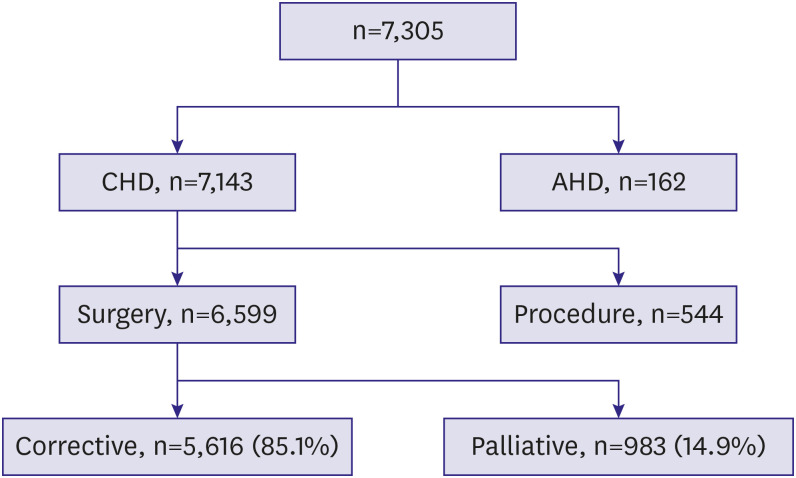
The median age was 1.9 years (range, 0–71.5 years). There were 3,405 (51.6%) male patients. A total of 5,616 (85.1%) biventricular repairs and 983 (14.9%) palliative procedures were performed (Figure 1). A total of 591 patients from 30 countries were helped by the KHF: 143 (24.2%) from China, 98 (16.6%) from Vietnam and 73 (12.4%) from Mongolia.
Figure 1. Number of patients by diagnosis and surgery type.
AHD = adult heart disease; CHD = congenital heart disease.
Diagnosis prevalence
The disease prevalence is shown in Table 1. There were 1,809 patients (27.4%) with ventricular septal defects (VSDs). To distinguish from the first operation of tetralogy of Fallot (TOF), we created a new disease category of pulmonary valve replacement (PVR), which was used to treat 257 patients (3.9%). Compared to the other 2 surgical eras (1984–1990, 1990–1999), new diseases were added, including pulmonary atresia with intact ventricular septum (PA with IVS), PVR, congenitally corrected transposition of the great arteries (ccTGA), left ventricular outflow tract obstruction (LVOTO), arrhythmia, vascular ring, cardiomyopathy, heart failure, and congenital pulmonary vein stenosis (PVS; excluding surgical repair of total anomalous pulmonary venous return). We compared major disease prevalence based on the surgical era (Supplementary Figure 1).
Table 1. Diagnosis prevalence by surgical era.
| Diagnosis | Number (%) | ||
|---|---|---|---|
| 2000–2014 | 1990–1999 | 1984–1990 | |
| VSD | 1,809 (27.4) | 2,382 (38.1) | 2,417 (45.8) |
| TOF | 679 (10.3) | 880 (14.1) | 944 (17.9) |
| ASD or PAPVR | 959 (14.5) | 795 (12.7) | 501 (9.5) |
| PDA | 156 (2.4) | 318 (5.1) | 453 (8.6) |
| PA with VSD | 410 (6.2) | 299 (4.8) | 94 (1.8) |
| PA with IVS | 65 (1.0) | - | - |
| PVR | 257 (3.9) | - | - |
| DORV | 212 (3.2) | 212 (3.4) | 121 (2.3) |
| AVSD | 233 (3.5) | 216 (3.5) | 94 (1.8) |
| PS | 74 (1.1) | 150 (2.4) | 163 (3.1) |
| TGA | 157 (2.4) | 195 (3.1) | 89 (1.7) |
| FSV | 589 (8.9) | 135 (2.2) | 56 (1.1) |
| TAPVR | 86 (1.3) | 86 (1.4) | 47 (0.9) |
| CoA, IAA | 205 (3.1) | 92 (1.5) | 41 (0.8) |
| ccTGA | 73 (1.1) | - | - |
| HLHS | 70 (1.1) | 10 (0.2) | - |
| Ebstein's anomaly | 63 (1.0) | 30 (0.5) | 27 (0.5) |
| Congenital valve anomaly | 256 (3.9) | 114 (2.3) | 73 (1.4) |
| LVOTO | 29 (0.4) | - | - |
| Aortic disease | 6 (0.1) | 65 (1.0) | 34 (0.6) |
| Arrhythmia | 27 (0.4) | - | - |
| Coronary problem | 9 (0.1) | - | 5 (0.1) |
| AP window, truncus arteriosus | 57 (0.9) | 13 (0.2) | 13 (0.2) |
| Vascular ring | 10 (0.2) | - | - |
| Cardiomyopathy, heart failure | 21 (0.3) | - | - |
| PVS | 9 (0.1) | - | - |
| Unclassified | 78 (1.2) | 224 (3.6) | 100 (1.9) |
| Total | 6,599 (100) | 6,246 (100) | 5,272 (100) |
AP window = aortopulmonary window; ASD = atrial septal defect; AVSD = atrioventricular septal defect; CoA = coarctation of the aorta; ccTGA = congenitally corrected transposition of the great arteries; DORV = double-outlet right ventricle; FSV = functional single ventricle; HLHS = hypoplastic left heart syndrome; IAA = interrupted aortic arch; IVS = intact ventricular septum; LVOTO = left ventricular outflow tract obstruction; PA = pulmonary atresia; PAPVR = partial anomalous pulmonary venous return; PDA = patent ductus arteriosus; PS = pulmonary stenosis; PVR = pulmonary valve replacement; PVS = pulmonary vein stenosis; TAPVR = total anomalous pulmonary venous return; TGA = transposition of the great arteries; TOF = tetralogy of Fallot; VSD = ventricular septal defect.
Diagnostic complexity
The median postoperative hospital stay was 11 days (range, 0–372 days). During the 15-year (2000–2014) KHF supportive period, more than 100 operations were performed in 12 hospitals (group A). In these 12 hospitals, 5,480 (83%) operations were performed, while the other 1,119 (17%) operations were performed in other 52 hospitals (group B). A complex procedure (defined as ABC score above 6) was performed in 3,368 patients (51.0%). The mean ABC score was 6.6±2.2, while a RACHS-1 score of 2 was the most common (Table 2).
Table 2. RACHS-1 score of operative patients.
| RACHS-1 score | Number (%) |
|---|---|
| 1 | 1,185 (18.0) |
| 2 | 3,447 (52.2) |
| 3 | 1,581 (24.0) |
| 4 | 333 (5.0) |
| 6 | 45 (0.7) |
| Unclassified | 8 (0.1) |
| Total | 6,599 (100) |
RACHS-1 = Risk Adjustment for Congenital Heart Surgery-1.
Analysis of diagnosis and surgical mortality by patient age
The early mortality rate was 3.8%, while the late mortality rate was 1.8%. Previous reports of the KHF (not published in English) (1984–1999) showed that the early surgical mortality rate was 8.6%, and the late mortality rate was 5.3%. The surgical outcomes of the current era were improved in contrast to those of the earlier time period (Supplementary Figure 2).
Neonates
There were 491 neonates (7.4%); of the, 288 (58.7%) were male. The disease prevalence is shown in Table 3. Compared to the other surgical eras (1984–1999), there was a great increase in neonate patients (491 vs. 74), and new diseases were added, including atrial septal defect (ASD), partial anomalous pulmonary venous return (PAPVR), PA with IVS, ccTGA, arrhythmia, coronary problem. The median hospital stay was 19 days (range, 0–277 days). A total of 491 procedures were performed (457 [93.1%] in group A, 34 [6.9%] in group B): 343 (69.9%) biventricular repairs and 148 (30.1%) palliative procedures. The mean ABC score was 8.2±2.7. A RACHS-1 score of 3 was the most common. Complex procedures were performed in 365 patients (74.3%). The early mortality rate was 12.2%, while the late mortality rate was 3.7%. The early surgical mortality rate of other surgical eras (1984–1999) was 29.7%.
Table 3. Neonates' diagnosis prevalence.
| Diagnosis | Number (%) | |
|---|---|---|
| 2000–2014 | 1984–1999 | |
| VSD | 44 (9.0) | 4 (5.4) |
| TOF | 24 (4.9) | 2 (2.7) |
| ASD or PAPVR | 2 (0.4) | - |
| PDA | 31 (6.3) | 3 (4.1) |
| PA with VSD | 53 (10.8) | 9 (12.2) |
| PA with IVS | 20 (4.1) | - |
| DORV | 24 (4.9) | 2 (2.7) |
| AVSD | 7 (1.4) | 2 (2.7) |
| PS | 3 (0.6) | 2 (2.7) |
| TGA | 72 (14.7) | 20 (27.0) |
| FSV | 43 (8.8) | 1 (1.4) |
| TAPVR | 35 (7.1) | 7 (9.5) |
| CoA, IAA | 78 (15.9) | 11 (14.9) |
| ccTGA | 3 (0.6) | - |
| HLHS | 28 (5.7) | 3 (4.1) |
| Ebstein's anomaly | 1 (0.2) | - |
| Congenital valve anomaly | 5 (1.0) | 2 (2.7) |
| Arrhythmia | 2 (0.4) | - |
| Coronary problem | 1 (0.2) | - |
| AP window, truncus arteriosus | 12 (2.4) | - |
| PVS | - | 1 (1.4) |
| Unclassified | 3 (0.4) | 5 (6.8) |
| Total | 491 (100) | 74 (100) |
AP window = aortopulmonary window; ASD = atrial septal defect; AVSD = atrioventricular septal defect; ccTGA = congenitally corrected transposition of the great arteries; CoA = coarctation of the aorta; DORV = double-outlet right ventricle; FSV = functional single ventricle; HLHS = hypoplastic left heart syndrome; IAA = interrupted aortic arch; IVS = intact ventricular septum; PA = pulmonary atresia; PAPVR = partial anomalous pulmonary venous return; PDA = patent ductus arteriosus; PS = pulmonary stenosis; PVS = pulmonary vein stenosis; TAPVR = total anomalous pulmonary venous return; TGA = transposition of the great arteries; TOF = tetralogy of Fallot; VSD = ventricular septal defect.
Age <3 months
There were 1,084 patients; of them, 586 (54.1%) were male. The median hospital stay was 16 days (range, 0–277 days). A total of 845 (78.8%) biventricular repairs and 239 (22.0%) palliative procedures were performed; of them, 996 (91.9%) were in group A and 88 (8.1%) were in group B. The mean ABC score was 7.5±2.4. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 607 patients (56.0%). The early mortality rate was 8.2%, while the late mortality rate was 3.0%. The early surgical mortality rate of other surgical eras (1984–1999) was 23.0%.
Infants
There were 2,617 patients; of them, 1,429 (54.6%) were male. The diagnosis prevalence is shown in Table 4 and new diseases were added, including PVR, LVOTO, vascular ring, cardiomyopathy, and heart failure. The median hospital stay was 13 days (range, 0–277 days). A total of 2,617 operations were performed (2,323 [88.8%] in group A, 294 [11.2%] in group B), including 2,101 (80.3%) biventricular repairs and 516 (19.7%) palliative procedures. The mean ABC score was 7.2±2.1. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 1,440 patients (55.0%). The early mortality rate was 6.0%, while the late mortality rate was 2.3%. The early surgical mortality rate of other surgical eras (1984–1999) was 15.8%.
Table 4. Infants' diagnosis prevalence.
| Diagnosis | Number (%) | |
|---|---|---|
| 2000–2014 | 1984–1999 | |
| VSD | 864 (33.0) | 970 (47.4) |
| TOF | 357 (13.6) | 243 (11.9) |
| ASD or PAPVR | 89 (3.4) | 44 (2.2) |
| PDA | 78 (3.0) | 78 (3.8) |
| PA with VSD | 172 (6.6) | 139 (6.8) |
| PA with IVS | 43 (1.6) | - |
| PVR | 2 (0.1) | - |
| DORV | 121 (4.6) | 88 (4.3) |
| AVSD | 124 (4.6) | 89 (4.3) |
| PS | 14 (0.5) | 19 (0.9) |
| TGA | 98 (3.7) | 123 (6.0) |
| FSV | 236 (9.0) | 51 (2.5) |
| TAPVR | 77 (2.9) | 47 (2.3) |
| CoA, IAA | 155 (5.9) | 76 (3.7) |
| ccTGA | 18 (0.7) | - |
| HLHS | 55 (2.1) | 6 (0.3) |
| Ebstein's anomaly | 7 (0.3) | 1 (0.0) |
| Congenital valve anomaly | 24 (0.9) | 12 (0.6) |
| LVOTO | 4 (0.2) | - |
| Arrhythmia | 9 (0.3) | - |
| Coronary problem | 7 (0.3) | 1 (0.0) |
| AP window, truncus arteriosus | 38 (1.5) | 15 (0.7) |
| Vascular ring | 7 (0.3) | - |
| Cardiomyopathy, heart failure | 3 (0.1) | - |
| PVS | 4 (0.2) | - |
| Unclassified | 14 (0.5) | 44 (2.2) |
| Total | 2,617 (100) | 2,046 (100) |
AP window = aortopulmonary window; ASD = atrial septal defect; AVSD = atrioventricular septal defect; CoA = coarctation of the aorta; ccTGA = congenitally corrected transposition of the great arteries; DORV = double-outlet right ventricle; FSV = functional single ventricle; HLHS = hypoplastic left heart syndrome; IAA = interrupted aortic arch; IVS = intact ventricular septum; LVOTO = left ventricular outflow tract obstruction; PAPVR = partial anomalous pulmonary venous return; PA = pulmonary atresia; PDA = patent ductus arteriosus; PS = pulmonary stenosis; PVR = pulmonary valve replacement; PVS = pulmonary vein stenosis; TAPVR = total anomalous pulmonary venous return; TGA = transposition of the great arteries; TOF = tetralogy of Fallot; VSD = ventricular septal defect.
Age 1–2 years
There were 709 patients in this group; of them, 355 (50.1%) were male. The median hospital stay was 9 days (range, 0–291 days). A total of 709 procedures were performed (582 [82.1%] in group A, 127 [17.9%] in group B), including 614 (86.6%) biventricular repairs and 95 (13.4%) palliative procedures. The mean ABC score was 6.6±2.2. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 362 patients (51.1%). The early mortality rate was 3.0%, while the late mortality rate was 1.2%.
Age 2–6 years
There were 1,053 patients; of them, 554 (52.6%) were male. The median hospital stay was 10 days (range, 0–135 days). A total of 1,053 procedures were performed (892 [84.7%] in group A, 161 [15.3%] in group B), including 805 (76.4%) biventricular repairs and 248 (23.6%) palliative procedures. The mean ABC score was 6.9±2.2. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 565 patients (53.7%). The early mortality rate was 2.3%, while the late mortality rate was 1.5%.
Age 6–10 years
There were 510 patients; of them, 263 (51.6%) were male. The median hospital stay was 9 days (range, 0–254 days). A total of 510 procedures were performed (394 [77.3%] in group A, 116 [22.7%] in group B), including 466 (91.4%) biventricular repairs and 44 (8.6%) palliative procedures. The mean ABC score was 6.3±2.0. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 224 patients (43.9%). The early mortality rate was 2.5%, while the late mortality rate was 1.8%.
Age 10–18 years
There were 678 patients; of them, 346 (51.0%) were male. The median hospital stay was 10 days (range, 0–105 days). A total of 678 procedures were performed (546 [80.5%] in group A, 132 [19.5%] in group B), including 631 (93.1%) biventricular repairs and 47 (6.9%) palliative procedures. The mean ABC score was 6.3±2.1. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 376 patients (55.5%). The early mortality rate was 1.8%, while the late mortality rate was 1.5%.
Age ≥18 years
There were 1,032 patients; of them, 450 (43.6%) were male. The median hospital stay was 11 days (range, 0–372 days). A total of 1,032 procedures were performed: 994 (96.3%) biventricular repairs and 38 (3.7%) palliative procedures; of them, 747 (72.4%) were performed in 12 hospitals, while the other 285 (27.6%) were performed in the other 52 hospitals. The mean ABC score was 5.4±2.2. A RACHS-1 score of 2 was the most common. Complex procedures were performed in 401 patients (38.9%). The early mortality rate was 2.8%, while the late mortality rate was 1.3%. Table 5 depicts the ABC score, RACHS-1 score, and early mortality rate by patient age.
Table 5. ABC score, RACHS-1 score, and early mortality rate by patient age.
| Age | <1 month | <3 months | <1 year | 1–2 years | 2–6 years | 6–10 years | 10–18 years | ≥18 years |
|---|---|---|---|---|---|---|---|---|
| ABC score (mean) | 8.2 | 7.5 | 7.2 | 6.6 | 6.9 | 6.3 | 6.3 | 5.4 |
| RACHS-1 score (median) | 3 | 2 | 2 | 2 | 2 | 2 | 2 | 1 |
| Early mortality (%) | 12.2 | 8.2 | 6.0 | 3.0 | 2.3 | 2.5 | 1.8 | 2.8 |
ABC = Aristotle Basic Complexity; RACHS-1 = Risk Adjustment for Congenital Heart Surgery-1.
Analysis of surgical mortality by patient diagnosis
We described the number of interventions for each diagnosis, although these procedures were not included in the surgical number.
Ventricular septal defect
There were 1,809 patients; of them, 940 (52.0%) were male. The median age was 1.1 years (range, 0–66.5 years). The median hospital stay was 9 days (range, 0–372 days). Ten (0.6%) palliative procedures were performed: 7 pulmonary artery bandings, 1 bidirectional cavopulmonary shunt, and 2 VSD partial closures. A total of 1,809 procedures were performed: 1,362 (75.3%) in group A, and the other 447 (24.7%) in group B. Two VSD device closures were performed. The early mortality rate was 1.4%, while the late mortality rate was 0.6%.
Tetralogy of Fallot
There were 679 patients; of them, 379 (55.8%) were male. Patients who received PVR were excluded. The median patient age was 11.5 months (range, 0.1 months–65.1 years). The median hospital stay was 11 days (range, 0–240 days). There were 44 (6.5%) palliative procedures. A total of 679 procedures were performed: 579 (85.3%) in group A vs. 100 (14.7%) in group B. A total of 31 interventional procedures like pulmonary artery balloon dilatation were performed. The early mortality rate was 4.6%, while the late mortality rate was 0.9%.
Atrial septal defect or partial anomalous pulmonary venous return
There were 959 patients; of them, 314 (32.7%) were male. The median patient age was 12.6 months (range, 3 months–69.5 years). The median hospital stay was 8 days (range, 1–291 days). A total of 959 operations were performed: 643 (67.0%) in group A and 316 (33.0%) in group B. There were 23 PAPVR cases with one of surgical mortality. There were 95 ASD device closures. The early mortality rate was 1.3%, while the late mortality rate was 0.9%.
Patent ductus arteriosus
There were 156 patients; of them, 56 (35.9%) were male. The median patient age was 2.1 years (range, 3 months–62.9 years). The median hospital stay was 10 days (range, 1–122 days). A total of 156 procedures were performed: 83 (53.2%) in group A and 73 (46.8%) in group B. There were 137 patent ductus arteriosus (PDA) device closures. The early mortality rate was 2.6%, while the late mortality rate was 1.3%.
Pulmonary atresia with ventricular septal defect
There were 410 patients; of them, 223 (54.4%) were male. The median patient age was 1.4 years (range, 0–52.6 years). The median hospital stay was 14 days (range, 0–168 days). A total of 410 procedures were performed: 392 (95.6%) in group A and 18 (4.4%) in group B. There were 280 (68.3%) biventricular repairs and 130 (31.7%) palliative procedures. A total of 111 (27.1%) patients had a major aortopulmonary collateral artery. There were 3 (0.7%) patients with a RACHS-1 score of 1, 85 (20.7%) with a RACHS-1 score of 2, 219 (53.4%) with a RACHS-1 score of 3, and 103 (25.1%) with a RACHS-1 score of 4. The early mortality rate was 4.9%, while the late mortality rate was 3.3%.
Pulmonary atresia with intact ventricular septum
There were 65 patients; of them, 34 (52.3%) were male. The median patient age was 6.3 months (range, 0–29.3 years). The median hospital stay was 16 days (range, 7–169 days). Of the 65 procedures, 64 (98.5%) were in group A, while the other 1 (1.5%) was in group B. There were 29 (44.6%) biventricular repairs and 36 (55.4%) palliative procedures. There were 6 interventions like right ventricular outflow tract balloon dilatation. The early mortality rate was 4.6%, while the late mortality rate was 6.5%.
Double-outlet right ventricle
There were 212 patients; of them, 124 (58.5%) were male. The median patient age was 0.7 years (range, 0–53 years). The median hospital stay was 14 days (range, 0–220 days). Of the 212 procedures, 201 (94.8%) were in group A, while the other 11 (5.2%) were in group B. There were 184 (86.8%) biventricular repairs and 28 (13.2%) palliative procedures. Of the 212 patients, 106 (50.0%) were treated with double-outlet right ventricle (DORV) with VSD (subaortic type), 73 (34.4%) with DORV with VSD for pulmonary stenosis (PS) (TOF type), 20 (9.4%) with DORV with VSD (subpulmonic type) (Taussig-Bing anomaly), 12 (5.7%) with DORV with VSD (remote type), and 1 (0.5%) patient with DORV with intact ventricular septum. Three (1.4%) patients had a RACHS-1 score of 1, 49 (23.1%) had a RACHS-1 score of 2, 151 (71.2%) had a RACHS-1 score of 3, 5 (2.4%) had a RACHS-1 score of 4, and 4 (1.9%) had a RACHS-1 score of 5. The early mortality rate was 6.1%, while the late mortality rate was 3.0%.
Atrioventricular septal defect
There were 233 patients; of them, 98 (42.1%) were male. The median patient age was 0.7 years (range, 10 days–68.2 years). The median hospital stay was 13 days (range, 1–157 days). Of the 233 procedures, 205 (88.0%) were in group A, while the other 28 (12.0%) were in group B. A total of 214 (91.8%) biventricular repairs and 19 (8.2%) palliative procedures were performed: There were 167 (71.7%) patients with complete atrioventricular septal defect (AVSD), 54 (23.2%) with partial AVSD, 6 (2.6%) with intermediate AVSD, and 6 (2.6%) with complete AVSD accompanying TOF. The early mortality rate was 5.6%, while the late mortality rate was 2.3%.
Pulmonary stenosis
There were 74 patients; of them, 43 (58.1%) were male. The median patient age was 6.3 years (range, 10 days–54.1 years). The median hospital stay was 13 days (range, 3–50 days). Of the 74 patients, 58 (78.4%) were in group A, while the other 16 (21.6%) were in group B. There were 72 (97.3%) biventricular repairs and 2 (2.7%) palliative procedures. A total of 51 interventions like pulmonary valve balloon dilatation were performed. The early mortality rate was 2.7%, while the late mortality rate was 0%.
Transposition of the great arteries
There were 157 patients; of them, 111 (70.7%) were male. The median patient age was 0.3 years (range, 0–38.5 years). The median hospital stay was 15 days (range, 0–218 days). Of the 157 procedures, 151 (96.2%) were performed in group A versus 6 (3.8%) in group B. A total of 141 (89.8%) biventricular repairs and 16 (10.2%) palliative procedures were performed: 57 (36.3%) with transposition of the great arteries (TGA) with IVS, 51 (32.5%) with TGA with VSD, and 49 (31.2%) with TGA with VSD and PS. One (0.6%) patient had a RACHS-1 score of 1, 14 (8.9%) had a RACHS-1 score of 2, 86 (54.8%) had a RACHS-1 score of 3, and 56 (35.7%) had a RACHS-1 score of 4. There were 9 interventions like coronary artery stent insertion. The early mortality rate was 8.3%, while the late mortality rate was 0%.
Functional single ventricle
There were 589 patients; of them, 378 (64.2%) were male. This patient group excluded those with hypoplastic left heart syndrome (HLHS). The median patient age was 1.9 years (range, 3 days–45.6 years). The median hospital stay was 18 days (range, 0–181 days). Of the 589 procedures, 573 (97.3%) were performed in group A vs. 16 (2.7%) in group B. Four (0.7%) patients had a RACHS-1 score of 1, 184 (31.2%) had a RACHS-1 score of 2, 382 (64.9%) patients had a RACHS-1 score of 3, 11 (1.9%) had a RACHS-1 score of 4, and 8 (1.4%) had a RACHS-1 score of 6. A total of 37 interventional procedures like cardiac catheter examinations were performed. The early mortality rate was 7.5%, while the late mortality rate was 4.2%.
Total anomalous pulmonary venous return
There were 86 patients; of them, 47 (54.7%) were male. The median patient age was 1.7 months (range, 0–37.8 years). The median hospital stay was 17 days (range, 0–236 days). Of the 86 procedures, 81 (94.2%) were performed in group A, while the other 5 (5.8%) were performed in group B. The early mortality rate was 12.8%, while the late mortality rate was 4%.
Coarctation of the aorta and interrupted aortic arch
There were 205 patients; of them, 119 (58.0%) were male. The median patient age was 1.4 months (range, 0.1 months–47.4 years). The median hospital stay was 15 days (range, 3–277 days). Of the 205 procedures, 188 (91.7%) operations were in group A, while the other 17 (8.3%) were in group B. There were 121 (59.0%) patients with coarctation of the aorta (CoA) with VSD, 32 (15.6%) with interrupted aortic arch (IAA) with VSD, 45 (22.0%) with isolated CoA, and 7 (3.4%) with another aortic arch anomaly. A total of 11 interventions like aortic re-coarctation balloon dilatation were performed. The early mortality rate was 4.9%, while the late mortality rate was 1.0%.
Congenitally corrected transposition of the great arteries
There were 73 patients; of them, 42 (57.5%) were male. The median patient age was 5 years (range, 0–56.1 years). The median hospital stay was 15 days (range, 32–77 days). Of the 73 procedures, 72 (98.6%) were performed in group A, while the other 1 (1.4%) was performed in group B. There were 22 (30.1%) patients with ccTGA with VSD, 45 (61.6%) patients with ccTGA with VSD, PS, and 6 (8.2%) patients with isolated ccTGA. The early mortality rate was 12.3%, while the late mortality rate was 10.9%.
Hypoplastic left heart syndrome
These data included operations for all disease stages. There were 70 patients; of them, 45 (64.3%) were male. The median patient age was 3.4 months (range, 0–4.3 years). The median hospital stay was 27.5 days (range, 0–196 days). All 70 (100%) operations were performed in group A. The early mortality rate was 18.6%, while the late mortality rate was 1.8%.
Ebstein's anomaly
There were 63 patients; of them, 24 (38.1%) were male. The median patient age was 16.3 years (range, 0–53.7 years). The median hospital stay was 13 days (range, 5–62 days). Of the 63 procedures, 57 (90.5%) were performed in group A, while the other 6 (9.5%) were in group B. There were 60 (95.2%) biventricular repairs and 3 (4.8%) palliative procedures. The early mortality rate was 1.6%, while the late mortality rate was 16%.
Congenital valve anomaly
There were 256 patients; of them, 128 (50.0%) were male. The median patient age was 13.3 years (range, 0–71.5 years). The median hospital stay was 13 days (range, 5–62 days). Of the 256 procedures, 245 (95.7%) were performed in group A, while the other 11 (4.3%) were performed in group B. The early mortality rate was 3.1%, while the late mortality rate was 16%.
Left ventricular outflow tract obstruction
There were 29 patients; of them, 21 (72.4%) were male. The median patient age was 4.8 years (range, 2.4 months–38.1 years). The median hospital stay was 8 days (range, 5–109 days). Of the 29 procedures, 23 (79.3%) were performed in group A, while the other 6 (20.7%) were performed in group B. The early mortality rate was 0%, while the late mortality rate was 3.4%.
Aortic disease
There were 6 patients; of them, 4 (66.7%) were male. The median patient age was 13.1 years (range, 5.9–17.7 years). The median hospital stay was 9 days (range, 6–32 days). All 6 (100%) operations were performed in group A. The early mortality rate was 16.7%, while the late mortality rate was 3.4%.
Arrhythmia
There were 27 patients; of them, 13 (48.1%) were male. The median patient age was 13.1 years (range, 0–62.2 years). The median hospital stay was 6 days (range, 3–27 days). All 27 (100%) operations were performed in group A. There were 25 permanent pacemaker insertions, 1 Maze operation, and 1 atrial ablation. A total of 46 interventions like radiofrequency catheter ablation were performed. The early mortality rate was 3.7%, while the late mortality rate was 0%.
Coronary anomaly
There were 9 patients; of them, 3 (33.3%) were male. The median patient age was 5 months (range, 10 days–39.9 years). The median hospital stay was 15 days (range, 8–23 days). Of the 9 procedures, 8 (88.9%) were performed in group A, while the other 1 (11.1%) was performed in group B. There was 1 neonate (11.1%) and 7 infants (77.8%). The early and late mortality rates were 0%.
Aortopulmonary window, truncus arteriosus
There were 57 patients; of them, 34 (59.6%) were male. The median patient age was 4.2 months (range, 3 days–20.6 years). The median hospital stay was 20 days (range, 5–147 days). Of the 57 procedures, 54 (94.7%) were performed in group A, while the other 3 (5.3%) were performed in group B. There were 13 neonates (22.8%) and 38 infants (66.7%). The early mortality rate was 7.0%, while the late mortality rate was 5.7%.
Vascular ring
There were 10 patients; of them, 5 (50.0%) were male. The median patient age was 4.4 months (range, 1.3 months–39.9 years). The median hospital stay was 10.5 days (range, 4–104 days). Of the 10 procedures, 8 (80.0%) were performed in group A, while the other 2 (20.0%) were performed in group B. The early mortality rate was 10.0%, while the late mortality rate was 0%.
Cardiomyopathy, heart failure
There were 21 patients; of them, 12 (57.1%) were male. The median patient age was 8.6 years (range, 2.7 months–57.5 years). The median hospital stay was 26 days (range, 9–117 days). Of the 21 procedures, 20 (95.2%) were performed in group A, while the other 1 (4.8%) was performed in group B. There were 11 heart transplantations, with an early mortality rate of 9.1%. The overall early mortality rate was 19%, while the late mortality rate was 17.6%.
Pulmonary vein stenosis
All of the cases were isolated PVS; these data did not include postoperative complications. There were 9 patients; of them, 2 (22.2%) were male. The median patient age was 8.6 months (range, 2.4 months–19.9 years). The median hospital stay was 17 days (range, 6–54 days). Of the 9 procedures, 6 (66.7%) were performed in group A, while the other 3 (33.3%) were performed in group B. The early mortality rate was 11.1%, while the late mortality rate was 50.0%.
Pulmonary valve replacement
There were 257 patients; of them, 163 (63.4%) were male. The median patient age was 17 years (range, 4 months–59.9 years). The median hospital stay was 11 days (range, 0–254 days). Of the 257 procedures, 249 (96.9%) were performed in group A, while the other 8 (3.1%) were performed in group B. A total of 217 (84.4%) patients had TOF, 24 (9.3%) had PA with VSD, and 16 (6.2%) had DORV. The early mortality rate was 1.6%, while the late mortality rate was 1.6%.
Unclassified
There were 76 patients; of them, 41 (53.9%) were male. The median patient age was 10.9 years (range, 3 days–50.5 years). The median hospital stay was 18 days (range, 1–109 days). Of the 76 procedures, 55 (72.4%) were performed in group A, while the other 21 (27.6%) were performed in group B. These diseases included pectus excavatum, sternal instability, phrenic nerve palsy, congenital tracheal stenosis, and constrictive pericarditis. The early mortality rate was 5.3%, while the late mortality rate was 1.4%.
Analysis of surgical mortality by surgical volume
We divided the hospitals into 2 groups: group A included the 12 hospitals in which more than 100 operations were performed, while group B included the other hospitals in which fewer than 100 operations were performed during the KHF supportive period (2000–2014). Table 6 shows the difference in mortality between the 2 groups. There was no intergroup difference in mortality rate (p=0.283). As mentioned above, we defined a complex procedure as an ABC score above 6.
Table 6. Comparison of surgical mortality of the 2 hospital groups by surgical volume.
| Hospital | Mortality | Total | p value | |
|---|---|---|---|---|
| No | Yes (%) | |||
| Group A | 5,183 | 297 (5.4) | 5,480 | 0.283 |
| Group B | 1,049 | 70 (6.3) | 1,119 | |
| Total | 6,232 | 367 (5.6) | 6,599 | |
Group A = hospitals in which more than 100 procedures were performed; Group B = hospitals in which less than 100 procedures were performed.
Table 7 shows the difference in surgical complexity between the 2 hospital groups. In group A hospitals, significantly more complex procedures were performed (p<0.01).
Table 7. Difference in surgical complexity between the 2 hospital groups.
| Hospital | Complexity | Total | p value | |
|---|---|---|---|---|
| No | Yes (%) | |||
| Group A | 2,354 | 3,126 (57.0) | 5,480 | <0.01 |
| Group B | 877 | 242 (21.6) | 1,119 | |
| Total | 3,231 | 3,368 (51.0) | 6,599 | |
Group A = hospitals in which more than 100 procedures were performed; Group B = hospitals in which less than 100 procedures were performed.
DISCUSSION
This study examined the surgical outcomes of CHD during a recent 15-year period (2000–2014). Because of the absence of nationwide data concerning the surgical outcomes of CHD, this study can represent the surgical outcomes of CHD in Republic of Korea in recent years. Considering that annual CHD surgery volume is around 3,000 cases/year,7) there is around a 10% of surgical volume of CHD in the Republic of Korea. With Korea’s dramatic economic and social growth, we expected the improvement of surgical outcomes as well. The entire surgical mortality rate of CHD was 3.8%, while that in neonates was 12.2% and that in infants was 6%. These outcomes are comparable to those of other series.8),9),10) Because these data were based on KHF data from 64 hospitals with semi-mandatory data reporting, we could not evaluate the exact cause of death. Thus, we focused on hospital mortality rates of CHD surgery.
As we mentioned at the beginning, patients' diseases were classified according to 2 previous reports with the addition of current diagnoses to the new classification, including PA with IVS, PVR, ccTGA, vascular ring, cardiomyopathy, heart failure, LVOTO, and pulmonary vein stenosis. These changes demonstrate that more complex and difficult diseases were treated in the current period in the Republic of Korea. In particular, there was a significant increase in neonatal patients (491 vs. 74 patients), and the early mortality rate decreased from 29.7% to 12.2%. This investigation revealed that CHD treatment improved over the past 2 decades.
Due to diagnostic heterogeneity and complexity, we used ABC and RACHS-1 scores to stratify the patient groups. We also examined the hospital mortality rate by RACHS-1 scores. Table 2 showed the mortality rates by RACHS-1 score and demonstrated higher mortality rates than those in other developed countries.8),11)
For the simple comparison and evaluation, we arbitrarily divided the patients into age groups and investigated their ABC and RACHS-1 scores. As we expected, ABC score, RACHS-1 score, and early mortality rates decreased as the patient groups aged (Table 5).
We also arbitrarily divided the patients into disease groups according to previous reports and added new diagnoses to the new classification. In particular, we created a new disease category of PVR to distinguish those patients from the first operation for TOF.
Many interventional procedures (95 ASD, 137 PDA device closures) were performed during the study period. This was a relatively large number of PDA device procedures considering the 156 PDA surgeries performed during the same period.
Because of the relatively small number of patients with HLHS, we analyzed all stages together. The early mortality rate of 18.6% would be relatively lower than that of only stage I operations.
As we mentioned above, we divided the hospitals into 2 groups according to surgical volumes: group A includes the 12 hospitals in which more than 100 operations were performed, while group B includes the other 152 hospitals in which less than 100 operations were performed during the study period (2000–2014). Most of the complex procedures were performed in group A hospitals, while a large proportion of ASD, VSD, and PDA procedures was performed in group B hospitals.
Although more complex surgeries were performed in group A hospitals, there were no intergroup differences in hospital mortality rates. This means that group A hospitals with relatively large surgical volumes have good surgical outcomes irrespective of disease complecity. These results are consistent with those of previous studies.12),13)
Regarding the 591 patients from 30 countries, the most (143; 24.2%) were from China, followed by 98 (16.6%) from Vietnam and 73 (12.4%) from Mongolia.
This study was limited by the various disease groups and lack of exact late mortality dates and causes, as we were unable to investigate late mortality. Also, we arbitrarily classified the various diseases according to our previous 2 reports.
In conclusion, there were more neonatal surgeries (491 vs. 74 patients) in the current versus past era (1984–1999). Surgical outcomes were significantly improved over the past era. Considering the total surgical mortality rate of 3.8% and the fact that 591 patients from 30 countries were helped by KHF, the Republic of Korea has been transformed from a country receiving help from other countries to one providing help to other low socioeconomic status countries.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
- Conceptualization: Park YH.
- Resources: Cho BK.
- Writing - original draft: Shin HJ.
- Writing - review & editing: Shin HJ, Park YH.
SUPPLEMENTARY MATERIALS
Diagnosis prevalence according to the surgical era.
Early mortality rate according to patients' age in different surgical period.
References
- 1.Baptist Health. South Korean man returns to Jacksonville 21 years after local heart surgeons saved his life: reunion with doctors, philanthropists, will take place on March 28 [Internet] Jacksonville (FL): Baptist Health; 2008. [cited 2020 Feb 7]. Available from https://www.baptistjax.com/about-us/newsroom/news-releases/south-korean-man-returns-to-jacksonville-21-years-after-local-heart-surgeons-saved-his-life. [Google Scholar]
- 2.Catholic Times. Busan Children's Heart Disease Consultation Center: free surgery for 50 patients [Internet] Daegu: Catholic Times; 1983. [cited 2020 Feb 7]. Available from https://www.catholictimes.org/article/article_view.php?aid=219650¶ms=page%3D3709%26acid%3D1. [Google Scholar]
- 3.The New York Times. Foreign children given gift of life [Internet] New York (NY): The New York Times Company; 1983. [cited 2020 Feb 7]. Available from https://www.nytimes.com/1983/11/15/nyregion/foreign-children-given-gift-of-life.html. [Google Scholar]
- 4.Rotary International District 3650. About “Gift of Life Korea” [Internet] Seoul: Rotary International District 3650; 2019. [cited 2020 Feb 7]. Available from https://www.rotary.or.kr/community/document/district3650/306. [Google Scholar]
- 5.Lacour-Gayet F, Clarke D, Jacobs J, et al. The Aristotle score: a complexity-adjusted method to evaluate surgical results. Eur J Cardiothorac Surg. 2004;25:911–924. doi: 10.1016/j.ejcts.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs JP, Jacobs ML, Lacour-Gayet FG, et al. Stratification of complexity improves the utility and accuracy of outcomes analysis in a Multi-Institutional Congenital Heart Surgery Database: Application of the Risk Adjustment in Congenital Heart Surgery (RACHS-1) and Aristotle Systems in the Society of Thoracic Surgeons (STS) Congenital Heart Surgery Database. Pediatr Cardiol. 2009;30:1117–1130. doi: 10.1007/s00246-009-9496-0. [DOI] [PubMed] [Google Scholar]
- 7.Korean Heart Foundation. 2015 Statistics for cardiac surgery in congenital heart disease [Internet] Seoul: Korean Heart Foundation; 2019. Aug 26, [cited 2020 Feb]. Available from http://www.heart.or.kr/korean/board/board_renew.php?sa=list&bid=2. [Google Scholar]
- 8.Hoashi T, Miyata H, Murakami A, et al. The current trends of mortality following congenital heart surgery: the Japan Congenital Cardiovascular Surgery Database. Interact Cardiovasc Thorac Surg. 2015;21:151–156. doi: 10.1093/icvts/ivv109. [DOI] [PubMed] [Google Scholar]
- 9.Jacobs JP, O'Brien SM, Pasquali SK, et al. The importance of patient-specific preoperative factors: an analysis of the society of thoracic surgeons congenital heart surgery database. Ann Thorac Surg. 2014;98:1653–1658. doi: 10.1016/j.athoracsur.2014.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cavalcante CT, de Souza NM, Pinto VC, et al. Analysis of surgical mortality for congenital heart defects using RACHS-1 Risk Score in a Brazilian single center. Rev Bras Cir Cardiovasc. 2016;31:219–225. doi: 10.5935/1678-9741.20160022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McSharry B, Straney L, Alexander J, et al. RACHS - ANZ: a modified risk adjustment in congenital heart surgery model for outcome surveillance in Australia and New Zealand. J Am Heart Assoc. 2019;8:e011390. doi: 10.1161/JAHA.118.011390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Welke KF, O'Brien SM, Peterson ED, Ungerleider RM, Jacobs ML, Jacobs JP. The complex relationship between pediatric cardiac surgical case volumes and mortality rates in a national clinical database. J Thorac Cardiovasc Surg. 2009;137:1133–1140. doi: 10.1016/j.jtcvs.2008.12.012. [DOI] [PubMed] [Google Scholar]
- 13.Welke KF, Diggs BS, Karamlou T, Ungerleider RM. The relationship between hospital surgical case volumes and mortality rates in pediatric cardiac surgery: a national sample, 1988–2005. Ann Thorac Surg. 2008;86:889–896. doi: 10.1016/j.athoracsur.2008.04.077. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Diagnosis prevalence according to the surgical era.
Early mortality rate according to patients' age in different surgical period.