Abstract
Purpose
In the setting of abnormal results on screening mammography, the Mammography Quality Standards Act mandates that patients receive a mailed “recall” lay letter informing them to return for additional follow-up imaging. The language used in this letter should be “easily understood by a lay person.” In February 2019, the authors’ institution revised the language of its recall lay letter to the sixth grade reading level. The purpose of this study was to analyze the effect of improved readability on patient follow-up rates.
Methods
In this retrospective study, data from all screening mammograms at a single institution with BI-RADS category 0 assessments excluding technical recalls between February 2018 to February 2019 (pre-intervention group) and February 2019 to February 2020 (post-intervention group) were reviewed. The primary outcome measure was the percentage of patients in each intervention group who returned for their diagnostic follow-up examination within 60 days (the standard recommended by the Centers for Disease Control and Prevention). Univariate and multivariate logistic regression was done to estimate odds ratios and 95% confidence intervals for follow-up within 60 days.
Results
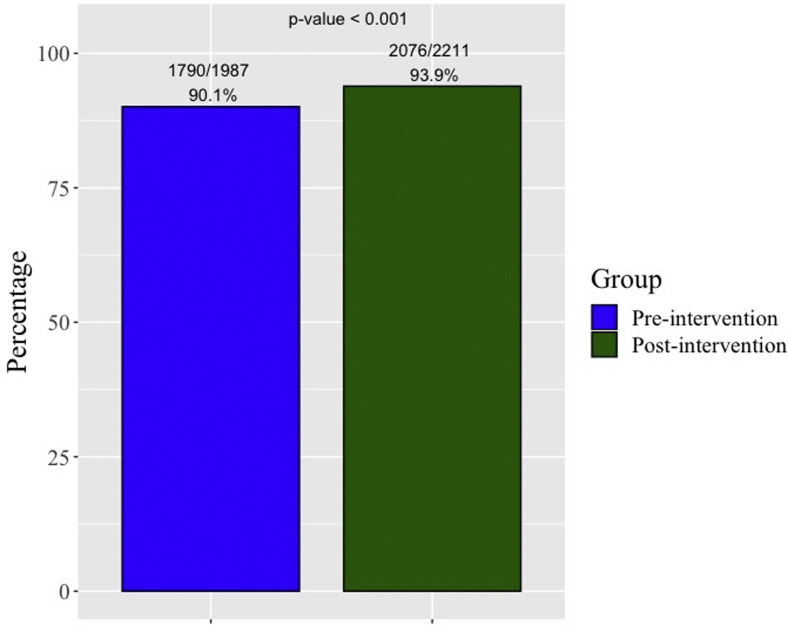
This study included 1,987 patients in the pre-intervention group and 2,211 patients in the post-intervention group. The patient follow-up rate within 60 days increased from 90.1% (1,790 of 1,987) in the pre-intervention group to 93.9% (2,076 of 2,211) in the post-intervention group (P < .001). When controlling for imaging site, patients in the post-intervention group had 1.96-fold increased odds of returning for a diagnostic follow-up examination within 60 days (95% confidence interval, 1.52-2.53).
Conclusions
Revising an institution’s recall lay letter to a lower reading grade level significantly improved timely patient follow-up.
Key Words: Educational disparities, patient adherence, readability, recall, screening mammography, lay letter
Introduction
The importance of written patient communication comprehension has increased because many patients are choosing to take more active roles in their health care. In the setting of abnormal results on screening mammography, the Mammography Quality Standards Act (MQSA) mandates that patients receive a mailed “recall” lay letter within 30 days informing them to return for additional follow-up imaging [1]. MQSA states that the language used in this letter should be “easily understood by a lay person.” The Centers for Disease Control and Prevention (CDC) and the National Institutes of Health recommend that all written patient communication should have between a sixth and an eighth grade reading level [2]. Findings from previous literature demonstrate that in breast imaging as well as other medical specialties, poorer comprehension of written patient materials occurs with readability higher than this recommendation [3, 4, 5].
A previous study by our group evaluated patient comprehension of perceived time to return for follow-up imaging [6]. We compared our institution’s initial recall lay letter and a proposed revised statement at a lower reading grade level using a paper-based survey. The results demonstrated a significant improvement in patient comprehension and likelihood of correctly interpreting the appropriate follow-up time frame with the revised statement compared with the initial statement. Education level was found to be an important predictor of understanding; participants who had achieved less than a college degree were least likely to comprehend the original lay latter correctly. Although these were important findings, the conclusions were drawn from only surveyed participants and thus were still theoretical and require practical confirmation.
To maximize the efficacy of screening mammography recall lay letters, patients need to both understand and comply with timely follow-up recommendations in order to increase the likelihood of early breast cancer detection by screening mammography [7]. Therefore, evaluating the impact of theoretically improved patient comprehension on actual patient follow-up adherence requires further research, which we addressed in this follow-up study. Our aim was to assess the impact of improved readability on patient adherence to follow-up recommendations in the setting of abnormal results on screening mammography. The hypothesis was that the revised language would improve patient follow-up rates.
Methods
Study Setting
Before February 15, 2019, the protocol for notifying patients of an abnormality detected on screening mammography that requires additional follow-up imaging at our institution was through telephone communication and the MQSA-mandated recall lay letter, as detailed in our previous study (Appendix 1) [8]. This recall lay letter’s readability was assessed using the technique of Saraiya et al [9]. We developed a revised recall lay letter using their technique, and the lower reading grade level was verified using Microsoft Word’s “Show Readability Statistics” tool (Appendix 1) [9]. After our previous study, on February 15, 2019, our institution implemented this revised recall lay letter across all four of its outpatient breast imaging sites [6]. Each of these sites serves a geographically different patient population. This revised statement’s reading grade level was assessed in the same manner as the initial statement used before February 15, 2019 [9]. Between February 2018 and February 2020, this was the only change made to our institution’s patient notification protocol.
Study Design and Cohort Selection
A retrospective cohort study was performed to evaluate the impact of implementing a revised recall lay letter on timely patient follow-up after detected abnormalities on screening mammography. We reviewed data from all screening mammograms at our institution with BI-RADS category 0 assessments performed from February 15, 2018, to February 14, 2019 (the pre-intervention group), and from February 15, 2019, to February 14, 2020 (the post-intervention group). A portion of the pre-intervention group data set overlaps with the 2018 data set from our previous study [8]. Technical recall is defined as a “technical deficiency in image quality,” and at our institution, every technical recall at screening is also assigned a BI-RADS category 0 assessment and thus excluded from our study [10].
To identify the patients during these time periods with BI-RADS category 0 assessment screening mammograms, Current Procedural Terminology codes were used by our institution’s value analytics team to extract patient medical record numbers from our electronic medical record (EMR), Epic (Epic Systems, Verona, Wisconsin). The date of the diagnostic follow-up examination (mammography and/or breast or axillary ultrasound) was subsequently extracted. For medical record numbers without electronically extracted diagnostic follow-up examination dates, manual chart review was performed by one of the authors to ensure the accuracy of the final data set. Previous literature demonstrates that sociodemographic factors such as patient age, race, and ethnicity can affect breast cancer prognosis and patient follow-up adherence [11, 12, 13]. Therefore, these and other potential covariates (marital status, employment status, insurance type, and ZIP code at the time of the examination) were extracted from Epic. Similar to a previously reported study, insurance status was categorized into three groups: private or commercial, Medicare or Medicaid, and no insurance or self-pay [14]. Patients with both Medicare and private insurance were classified as private. Extracted patient ZIP codes were used to determine the National Area Deprivation Index (ADI) as a measure of disparity from the University of Wisconsin Neighborhood Atlas [15]. The range of National ADI percentile is from 1%, representing the least disadvantaged block group, to 100%, representing the most disadvantaged block group. Because the most disadvantaged 15% of neighborhoods are associated with increased rehospitalization rates, this was used as the demarcation cutoff in our study [16].
The institutional review board at our institution reviewed this study and designated it as exempt under US Department of Health and Human Services regulations. This study was HIPAA compliant.
Statistical Analysis
R version 2017 was used to perform the statistical analyses (R Foundation for Statistical Computing, Vienna, Austria). Patient demographics were compared between the pre- and post-intervention groups using the χ2 test for categorical variables and Student t test for continuous variables. The primary outcome of interest was the overall percentage of patients in each intervention group who returned for their diagnostic follow-up examinations within the CDC guideline of 60 days (a binary outcome) [17]. The secondary outcome of interest was the percentage of patient adherence in each intervention group to follow-up recommendations within 60 days stratified by imaging-site sociodemographic factors (eg, clinic site, race). National ADI was compared between the sites using analysis of variance for continuous variables. Univariate and multivariate logistic regression analyses were performed to estimate odds ratios and 95% confidence intervals (CIs). The pre-intervention group was used as the reference group for regression analyses. To assess for potential associations between sociodemographic factors and follow-up adherence, univariate and multivariate logistic regression analyses were also performed on these factors.
Results
Baseline Characteristics and Readability
A total of 4,315 patients had BI-RADS category 0 assessments on screening mammography during the study period. Of these, 117 patients (2.7%) were excluded because of technical recall. Baseline characteristics of patients in each group are shown in Table 1 , with a total n = 1,987 within the pre-intervention group and n = 2,211 within the post-intervention group.
Table 1.
Baseline patient characteristics
| Patient Characteristic | Pre-intervention (n = 1,987) | Post-intervention (n = 2,211) |
|---|---|---|
| Age (y) | 55.6 ± 11.6 | 56.0 ± 12.0 |
| Age | ||
| <50 y | 717 (36.1) | 812 (36.7) |
| 50-59 y | 547 (27.5) | 533 (24.1) |
| 60-69 y | 673 (33.9) | 795 (36.0) |
| >70 y | 49 (2.5) | 60 (2.7) |
| Race | ||
| White | 1,226 (61.7) | 1,260 (57.0) |
| Black | 526 (26.5) | 650 (29.4) |
| Asian | 113 (5.7) | 159 (7.2) |
| Other/unknown | 122 (6.1) | 142 (6.4) |
| Marital status∗ | ||
| Married | 1,227 (63.9) | 1,333 (62.1) |
| Single | 277 (14.4) | 339 (15.8) |
| Divorced/separated | 417 (21.7) | 476 (22.2) |
| Employment status† | ||
| Full-time | 1,107 (59.3) | 1,228 (59.7) |
| Part-time | 303 (16.2) | 327 (15.9) |
| Retired | 332 (17.8) | 366 (17.8) |
| Not working | 124 (6.7) | 136 (6.6) |
| Site | ||
| 1 | 665 (33.5) | 772 (34.9) |
| 2 | 454 (22.8) | 516 (23.3) |
| 3 | 242 (12.2) | 254 (11.5) |
| 4 | 626 (31.5) | 669 (30.3) |
| Insurance type‡ | ||
| Private/commercial | 1,237 (62.3) | 1,636 (74.1) |
| Medicare/Medicaid | 358 (18.0) | 556 (25.2) |
| No insurance/self-pay | 389 (19.6) | 16 (7.2) |
| National ADI§ | 32.5 ± 24.0 | 34.3 ± 25.3 |
Note: Data are expressed as mean ± SD or as number (percentage). ADI = Area Deprivation Index.
Excluded a total of 129 patients with “unknown” or “other” marital status recorded in the medical record.
Excluded a total of 275 patients without recorded employment status.
Insurance information not available for 3 patients in the pre-intervention group and 3 patients in the post-intervention group.
ZIP code data were not available for 13 patients in the preintervention group and 12 patients in the post-intervention group.
Table 2 presents the readability metrics for the initial and revised recall lay letters. The Flesch-Kincaid grade level was found to be 12.4 for the initial statement and 6.1 for the revised statement.
Table 2.
Recall lay letter readability metrics
| Initial | Revised | |
|---|---|---|
| Automated readability index | 12.0 | 5.4 |
| Coleman-Liau index | 15.4 | 7.7 |
| Gunning fog index | 11.3 | 9.2 |
| Flesch-Kincaid grade level | 12.4 | 6.1 |
| Flesch-Kincaid reading ease | 30.1 | 73.1 |
| Simple measure of gobbledygook | 12.5 | 10.1 |
| Mean (95% confidence interval)∗ | 12.7 (11.0-14.5) | 7.7 (5.5-9.9) |
Mean was calculated by summing the scores of all metrics except Flesh-Kincaid reading ease and dividing by 5.
Effect of Improved Readability on Patient Adherence to Diagnostic Follow-Up
Following the revision of the recall lay letter statement, the percentage of patients adherent to diagnostic follow-up within 60 days significantly increased from 90.1% (1,790 of 1,987) in the pre-intervention group to 93.9% (2,076 of 2,211) in the post-intervention group (P < .001; Fig. 1 ). Even when controlling for potential confounders, patients in the post-intervention group had 1.96-fold increased odds of returning for a diagnostic follow-up examination within 60 days compared with the pre-intervention group (95% CI, 1.52-2.53; Table 3 ).
Fig 1.
Percentage of patient adherence to a diagnostic follow-up examination in 60 days by intervention group.
Table 3.
Univariate and multivariate logistic regression analyses for diagnostic follow-up within 60 days of abnormal results on screening mammography
| Patient Characteristics | Univariate OR (95% CI) | Multivariate OR (95% CI) |
|---|---|---|
| Group | 1.69 (1.35-2.13) | 1.96 (1.52-2.53) |
| Age | ||
| <50 y | Reference | Reference |
| 50-59 y | 1.09 (0.81-1.46) | 1.11 (0.81-1.54) |
| 60-69 y | 0.91 (0.70-1.18) | 0.86 (0.62-1.21) |
| >70 y | 0.94 (0.46-1.90) | 0.79 (0.34-1.84) |
| Race | ||
| White | Reference | Reference |
| Black | 0.58 (0.37-0.61) | 0.61 (0.45-0.82) |
| Asian | 0.61 (0.39-0.95) | 0.55 (0.34-0.88) |
| Other/unknown | 0.54 (0.35-0.84) | 0.58 (0.35-0.95) |
| Marital status | ||
| Married | Reference | Reference |
| Single | 0.85 (0.61-1.19) | 1.00 (0.70-1.44) |
| Divorced/separated | 0.61 (0.47-0.80) | 0.81 (0.60-1.11) |
| Employment status | ||
| Full-time | Reference | Reference |
| Part-time | (0.70-1.41) | 1.53 (0.96-2.42) |
| Retired | 0.58 (0.44-0.77) | 0.80 (0.57-1.13) |
| Not working | 0.66 (0.43-1.02) | 0.65 (0.41-1.03) |
| Site | ||
| 1 | Reference | Reference |
| 2 | 0.78 (0.56-1.09) | 0.79 (0.54-1.15) |
| 3 | 0.51 (0.36-0.74) | 0.85 (0.56-1.30) |
| 4 | 0.52 (0.39-0.69) | 0.52 (0.38-0.71) |
| Insurance type | ||
| Private/commercial | Reference | Reference |
| Medicare/Medicaid | 0.55 (0.43-0.71) | 0.57 (0.40-0.81) |
| No insurance/self-pay | 0.78 (0.53-1.14) | 1.12 (0.72-1.75) |
| National ADI | ||
| <85% | Reference | Reference |
| >85% | 0.53 (0.38-0.76) | 0.61 (0.41-0.92) |
Note: ADI = Area Deprivation Index; CI = confidence interval; OR = odds ratio.
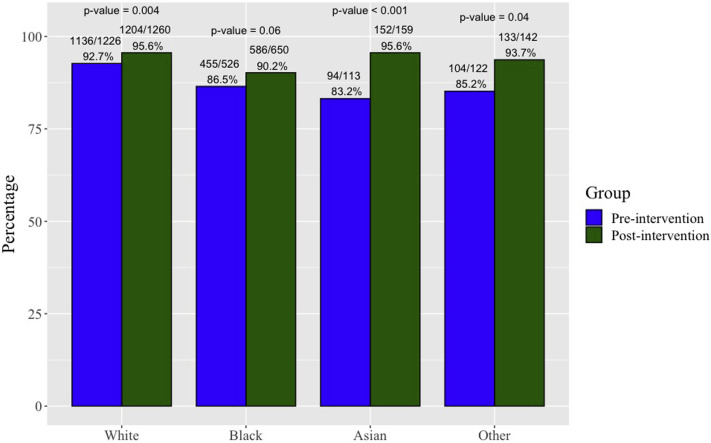
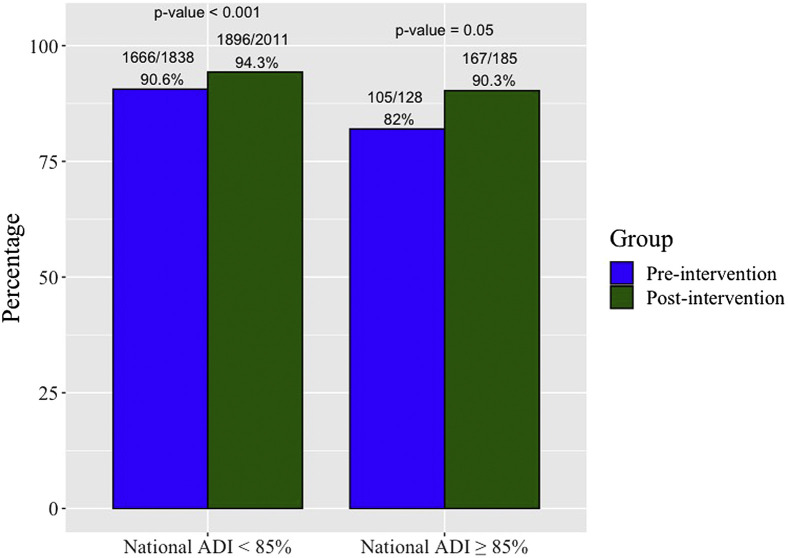
Effect of Patient Demographics Stratified by Intervention Group on Patient Adherence to Diagnostic Follow-Up
As a subgroup analysis, we analyzed the effect of patient demographics on patient adherence to diagnostic follow-up within 60 days (Figs. 2 and 3 ). On univariate analysis, race, marital status, employment status, insurance type, and National ADI were significantly associated with patient adherence (Table 3). On multivariate analysis, race remained statistically significant, with white patients significantly more likely to adhere to timely diagnostic follow-up recommendations compared with all other races. In addition, on multivariate analysis, patients who had Medicare or Medicaid and National ADI ≥ 85% were significantly less likely to follow up compared with patients with private or commercial insurance and National ADI < 85%.
Fig 2.
Percentage of patient adherence to a diagnostic follow-up examination in 60 days by race.
Fig 3.
Percentage of patient adherence to a diagnostic follow-up examination in 60 days by National Area Deprivation Index (ADI).
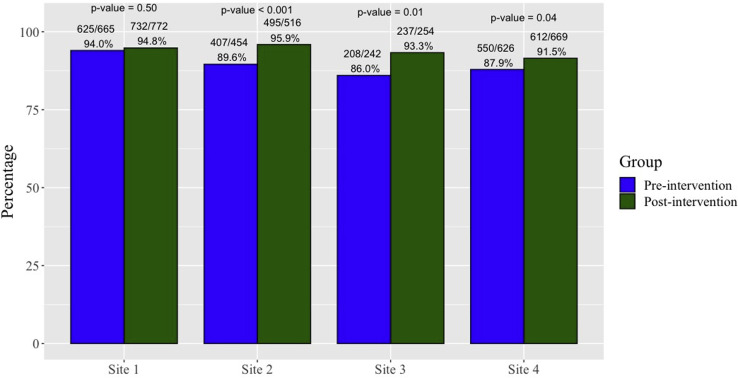
Effect of Imaging Site on Patient Adherence to Diagnostic Follow-Up
The four clinic sites at our institution serve different populations. Clinic site 1 is our busiest site and had the highest adherence before the letter revision, at 94.0% (625 of 665), and was therefore used as the reference category for comparison analysis (Fig. 1). Site 3 had the most improvement in follow-up within 60 days after the intervention, from 86.0% (208 of 242) to 93.3% (237 of 254; P = .01; Fig. 4 ). Univariate and multivariate results are shown in Table 3. On univariate analysis, patients presenting to sites 3 and 4 were significantly less likely to follow up in a timely manner compared with patients at site 1.
Fig 4.
Percentage of patient adherence to a diagnostic follow-up examination in 60 days by imaging site. National Area Deprivation Index: site 1, 33.4% ± 25.7%; site 2, 18.5% ± 15.2%; site 3, 48.2% ± 31.7%; site 4, 39.0% ± 20.2% (P < .001).
Discussion
Our study illustrates that implementing a revised recall lay letter that follows the CDC and National Institutes of Health language recommendations significantly improved patient adherence to timely diagnostic follow-up recommendations within 60 days. Improved readability of the recall lay letter increased the likelihood of patient follow-up adherence from 90.1% in the pre-intervention group to 93.9% in the post-intervention group. When controlling for possible covariates, patients in the post-intervention group had 2-fold increased odds of adherence.
Our findings in the present study validate the conclusions of our previous study, confirming that improved follow-up adherence is the result of improved readability of written patient communication facilitating enhanced patient comprehension [4]. This study illustrates the direct before-and-after effects of remediated readability with significantly improved follow-up of women in the setting of abnormal results on screening mammography. This was significant for every imaging site in the pre-intervention group, with an initial follow-up rate less than 90%. Our prior results in conjunction with our present findings demonstrate that written communication is more effective when the language used is more inclusive for women of all educational backgrounds.
Of all the imaging sites, site 3 initially began with the lowest patient follow-up rate of 86%. On the basis of our state’s county health rankings data, which is provided by a collaboration between the Robert Wood Johnson Foundation and the University of Wisconsin Population Health Institute, site 3’s patient population resides in a county that predominantly has lower socioeconomic status [18, 19, 20]. In 2018, the percentage of high school graduates was 70% (z = 3.44), median household income was $46,604 (95% CI, $44,866-$48,342), 10% of adults were uninsured (95% CI, 9%-11%), the unemployment rate was 6.3% (z = 1.09), and the percentage of population below the poverty level was 21.8%. This is starkly different from the patient population of site 1, which initially began with the highest patient follow-up rate of 94.0%: the percentage of high school graduates was 88% (z = 0.28), median household income was $72,305 (95% CI, $69,877-$74,733), 8% of adults were uninsured (95% CI, 7%-9%), the unemployment rate was 4.5% (z = −0.24), and the percentage of the population below the poverty level was 9.9%. The statistics for each site were not significantly different for 2019. Site 3 had the greatest positive change in patient follow-up adherence after the intervention, demonstrating the impact of improved readability on reducing discrepancies arising from education level. Although logical, these results are convincing and suggest that minor language revisions can yield a considerable impact in health care for women with lower educational backgrounds.
Independent of intervention group, however, there was a decrease in the likelihood of follow-up within 60 days for site 3 compared with site 1 which could be attributed to the innate lower socioeconomic characteristics of site 3, specifically financial. Additionally, site 3 serves patients from more disadvantaged neighborhoods, as evident by its highest National ADI percentile of the four sites. Although sites 1 and 4 reside within the same county, these sites are 14 miles apart. The majority of patients going to site 4 reside closer to the site 3 county line, which could explain the similar results. A woman can typically undergo screening mammography at no charge, even without insurance, through multiple programs such as the National Breast and Cervical Cancer Control Program or the Susan G. Komen Breast Cancer Foundation [21]. However, these programs do not cover the expenses of diagnostic workup, with the average cost of diagnostic mammography being $290 without insurance, which can be increased to a total of at least $540 if breast and/or axillary ultrasound is also required [21]. Our multivariate results showed that patients within the most disadvantaged 15% of neighborhoods and having Medicare or Medicaid were also less likely to adhere to timely follow-up recommendations compared with patients in less disadvantaged neighborhoods and having private or commercial insurance, respectively. Previous literature demonstrates that living in a disadvantaged neighborhood is associated with increased use of health services and early death [16]. This emphasizes the associated financial burden diagnostic follow-up examinations can impose on these patients. Therefore, although more disadvantaged patients may have improved understanding of the need to return for their diagnostic follow-up examinations after language revisions, they may actively decide not to follow up because of the cost. At our institution, women who are classified as no insurance or self-pay represent a combination of disadvantaged patients who do not possess insurance and wealthy international patients who pay out of pocket. This may explain why this insurance type was not associated with a similarly decreased likelihood of timely follow-up adherence as with patients with Medicare or Medicaid.
After revision of the recall lay letter, all races had increases in timely patient follow-up rates, although for African American patients this was nonsignificant. Regardless of the 23 counties in our state, African American patients have the lowest median household income of any race, with white patients having the highest [18]. In 2019 for site 3’s county, median household income for African American patients was $36,428, compared with $72,085 for white patients; the overall median household income was $46,762 (95% CI, $45,123-$48,401). This may explain why on multivariate analysis white race was associated with significantly higher likelihood of adhering to timely diagnostic follow-up recommendations compared with all other races. Additionally, a previous meta-analysis study demonstrated that transportation barriers to health care access exist specifically for patients with lower incomes and for racial minorities [22]. Therefore, although intuitively, improved readability should improve patient follow-up across all races, our disparate racial results suggest that even if educational disparities are addressed, there may be other underlying barriers impeding patient follow-up. Further investigation is needed to understand how to define these barriers and how to overcome these challenges for these patient populations. Moving forward, the relationship between the financial burdens of diagnostic examinations and patient follow-up requires further exploration.
The ACR is an important source of referenced literature, because it consistently provides helpful resources for the radiology community. The ACR provides sample lay letters that were developed by a multidisciplinary panel for institutions to use as is or as a template for their practices [23]. The language used in the sample recall lay letter is currently written at higher than the recommended eighth grade reading level [6]. Consideration should be given to updating this sample recall lay letter to a lower reading grade level, which would align with the ACR’s core purpose of empowering advancement of radiologic care.
Our study had several limitations, including the possibility of limited generalizability given that it was performed at a single institution. Additionally, our EMR does not track whether patients underwent their diagnostic follow-up examinations at other institutions after undergoing their screening examinations at our institution. Only covariates routinely entered in the EMR could be included in the analysis. On March 11, 2020, the World Health Organization declared coronavirus disease 2019 a pandemic, which may have affected results from the last month of our study [24]. The pandemic may have caused a decrease in patient compliance, making the presented results a possible underestimate of the true benefit of the revised letter. This possible underestimation is small, however, because only 14 patients did not follow up between January 11, 2020, and February 14, 2020. Last, the effect of secular trends on our patients’ adherence cannot be fully assessed, although these two groups represent consecutive years, minimizing this possible confounder.
In conclusion, revising our institution’s recall lay letter to a lower reading grade level significantly improved timely patient follow-up in the setting of abnormal results on screening mammography. We hope that this follow-up study will solidify the importance of appropriate readability of written patient communication and potentially modify recall lay letters currently being used by other breast imaging practices.
Take-Home Points
-
▪
Implementation of appropriate readability of recall lay letters into clinical practice significantly increases the likelihood of timely follow-up for additional imaging in the setting of a screening abnormality.
-
▪
Imaging sites that serve patient populations with lower educational backgrounds see the largest benefit in patient follow-up rates when a lower reading grade level is used in their screening recall lay letters.
-
▪
Black women, women with Medicare or Medicaid, and women from the top 15% of disadvantaged neighborhoods had a significant increase in follow-up adherence after implementing language revisions.
-
▪
However, when controlling for intervention group, these women were still less likely to undergo timely follow-up examinations compared with white women, women with private insurance, and women from more advantaged neighborhoods.
Acknowledgments
The authors thank Jenn Zuk and Boris Feldman for their assistance with data acquisition.
Footnotes
The authors state that they have no conflict of interest related to the material discussed in this article. Drs Nguyen, Harvey, Oluyemi, Myers, Mullen, and Ambinder are employees.
Additional Resources
Additional resources can be found online at: https://doi.org/10.1016/j.jacr.2020.07.006.
Additional Resources
References
- 1.US Food and Drug Administration Mammography Quality Standards Act. https://www.fda.gov/Radiation-EmittingProducts/MammographyQualityStandardsActandProgram/ Available at:
- 2.Kressin N.R., Gunn C.M., Battaglia T.A. Content, readability, and understandability of dense breast notifications by state. JAMA. 2016;315:1786–1788. doi: 10.1001/jama.2016.1712. [DOI] [PubMed] [Google Scholar]
- 3.Badarudeen S., Sabharwal S. Assessing readability of patient education materials: current role in orthopaedics. Clin Orthop Relat Res. 2010;468:2572–2580. doi: 10.1007/s11999-010-1380-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marcus E.N., Sanders L.M., Pereyra M. Mammography result notification letters: are they easy to read and understand? J Womens Health (Larchmt) 2011;20:545–551. doi: 10.1089/jwh.2010.2330. [DOI] [PubMed] [Google Scholar]
- 5.Ong G., Austoker J., Brouwer A. Evaluation of the written information sent to women who are called back for further investigation of breast screening in the UK. Health Educ J. 1996;55:413–429. [Google Scholar]
- 6.Nguyen D.L., Ambinder E.B., Jones M.K. Improving patient comprehension of screening mammography recall lay letters. J Am Coll Radiol. 2019;16:1669–1676. doi: 10.1016/j.jacr.2019.05.029. [DOI] [PubMed] [Google Scholar]
- 7.Monticciolo D.L., Newell M.S., Hendrick R.E. Breast cancer screening for average-risk women: recommendations from the ACR Commission on Breast Imaging. J Am Coll Radiol. 2017;14:1137–1143. doi: 10.1016/j.jacr.2017.06.001. [DOI] [PubMed] [Google Scholar]
- 8.Nguyen DL, Oluyemi E, Meyers KS, et al. Impact of telephone communication on patient adherence with follow-up recommendations after an abnormal screening mammogram. J Am Coll Radiol. In press. [DOI] [PubMed]
- 9.Saraiya A., Baird G.L., Lourenco A.P. Breast density notification letters and websites: are they too “dense”? J Am Coll Radiol. 2019;16:717–723. doi: 10.1016/j.jacr.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 10.ACR BI-RADS frequently asked questions—follow-up and outcome monitoring. https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Bi-Rads#FollowUpandMonitoring Available at:
- 11.Gorin S.S., Heck J.E., Cheng B. Delays in breast cancer diagnosis and treatment by racial/ethnic group. Arch Intern Med. 2006;166:2224–2252. doi: 10.1001/archinte.166.20.2244. [DOI] [PubMed] [Google Scholar]
- 12.Press R., Carrasqullio O., Sciacca R. Racial/ethnic disparities in time to follow-up after an abnormal mammogram. J Womens Health (Larchmt) 2008;17:923–930. doi: 10.1089/jwh.2007.0402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun L., Zhu Y., Qian Q. Body mass index and prognosis of breast cancer: an analysis by menstruation status when breast cancer diagnosis. Medicine (Baltimore) 2018;97(26) doi: 10.1097/MD.0000000000011220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clark C.R., Tosteson T.D., Tosteson A.N. Diffusion of digital breast tomosynthesis among women in primary care: associations with insurance type. Cancer Med. 2017;6:1102–1107. doi: 10.1002/cam4.1036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.University of Wisconsin School of Medicine Public Health 2015 Area Deprivation Index v2.0. https://www.neighborhoodatlas.medicine.wisc.edu Available at:
- 16.Kind A.J., Jencks S., Brock J. Neighborhood socioeconomic disadvantage and 30-day rehospitalization: a retrospective cohort study. Ann Intern Med. 2014;161:765–774. doi: 10.7326/M13-2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Durham D.D., Robinson W.R., Lee S.S. Insurance-based differences in time to diagnostic follow-up after positive screening mammography. Cancer Epidemiol Biomarkers Prev. 2016;25:1474–1482. doi: 10.1158/1055-9965.EPI-16-0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.County Health Rankings Maryland. https://www.countyhealthrankings.org/app/maryland/2020/downloads Available at:
- 19.Federal Reserve Bank of St. Louis. Maryland. https://fred.stlouisfed.org/categories/28543 Available at:
- 20.Bureau of Justice Statistics Measuring socioeconomic status (SES) in the NCVS: background, options, and recommendations. https://www.bjs.gov/content/pub/pdf/Measuring_SES-Paper_authorship_corrected.pdf Available at:
- 21.Brem Foundation Discuss your options. http://www.bremfoundation.org/screening-options Available at:
- 22.Syed S.T., Gerber B.S., Sharp L.K. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38:976–993. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American College of Radiology Mammography sample lay report letters. https://www.acr.org/Clinical-Resources/Breast-Imaging-Resources/Lay-Report-Letters Available at:
- 24.World Health Organization WHO director-general’s opening remarks at the media briefing on COVID-19—11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 Available at:
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.