Abstract
Purpose
Analysis of explanted intraocular lenses (IOLs) from pseudophakic eyes with supplementary sulcus-supported IOLs.
Methods
In this laboratory investigation, ten supplementary and capsular bag IOLs were analyzed. All lenses were received between January 2012 and March 2018. Explants were examined morphologically with histological and electron microscopic techniques and patients’ medical history was evaluated. Additionally, we used a technique new to this field: Transmission Electron Microscopy and electron diffraction pattern analysis was performed to investigate the structure of the opacifying crystals in detail.
Results
Eleven lenses were explanted due to IOL opacification from seven polypseudophakic eyes: In three cases the supplementary lens calcified, in three cases the capsular bag IOL (both lenses analyzed) and in one case both IOLs (only the supplementary was received). Additional surgical procedures and comorbidities included pars plana vitrectomy or Descemet stripping endothelial keratoplasty and diabetes mellitus. For each opacified lens, a varying layer of a Calcium phosphate beneath the optic surface was apparent. Crystal characterization revealed its composition to be Hydroxyapatite.
Conclusions and Importance
We report on a series of secondary calcification in lenses explanted from polypseudophakic eyes. In some cases, calcification occurred in the capsular bag lens, in other cases in the supplementary lens, or in both. The severity of the morphological change could be related to the comorbidities and the presence of surgery subsequent to the lens implantations. Detailed morphology of the opacifying crystals was revealed.
Keywords: Intraocular lens explantation, Supplementary intraocular lens, Addon intraocular lens, Intraocular lens pathology, Hydroxyapatite, Biomaterial
Highlights
-
•
Intraocular lenses exhibited calcification in a series of polypseudophakic eyes.
-
•
Pathology occurred in the capsular bag lens, the supplementary lens, or in both.
-
•
Calcification was associated with different environmental factors.
-
•
Depending on the factor, morphology and pattern of the opacity differed.
-
•
Transmission Electron Microscopy revealed the opacifying crystals' ultrastructure.
1. Introduction
Supplementary sulcus-supported IOLs have been used for over ten years to safely treat residual refractive error in pseudophakic eyes.1 Toric and multifocal models were subsequently introduced for correction of residual astigmatism and presbyopia.2, 3, 4 Other pseudophakic supplementary sulcus-supported lenses with special optic configurations are used to treat patients with age-related macular degeneration.5
Calcification of capsular bag fixated intraocular lenses (IOLs) has been reported in several previous studies.6, 7, 8, 9, 10 This pathology can lead to a decreased visual quality of varying severity and ultimately necessitate IOL exchange.11 IOL calcification was clinically categorized according to David Apple and colleagues into primary-, secondary- and pseudo-calcification.12 The causes of primary IOL calcification lie within the polymer material, the lens manufacturing process and the lens packaging.9,13, 14, 15 In contrast, secondary calcification is caused by environmental factors that can provoke calcification in any lens made of hydrophilic material. Factors that are considered to increase the risk of secondary calcification include surgical procedures with intraocular injection of gas, air or silicone oil (e.g. during pars plana vitrectomy (PPV) or posterior lamellar keratoplasty), the injection of rtPA into the anterior chamber or intravitreal injections.6, 7, 8,16 Patients’ comorbidities such as diabetes mellitus are also thought to increase the risk for IOL calcification.17
Although initial in vitro studies have revealed parts of the underlying mechanisms of this pathology, the full pathomechanism is still not understood.18 Variation in calcification pattern in eyes implanted with more than one IOL might lead to a better understanding of this pathology. Therefore, the aim of this study was to analyze explanted IOLs from polypseudophakic eyes in which IOL opacification occurred.
2. Materials and methods
In this consecutive case series with laboratory investigation, ten lenses, seven supplementary and three capsular bag IOLs, explanted from seven polypseudophakic eyes were analyzed. The lenses had been sent consecutively for morphological analysis to our laboratory between January 2012 and March 2018. Donating surgeons provided clinical information about the cases. These data were analyzed to search for general and ophthalmological comorbidities and intraocular surgical procedures that were subsequent to the lens implantations.
2.1. Material analysis
Morphological analysis was performed for each lens specimen as described in our previous publications.7,8 Gross microscopic photographs were taken using an Olympus BX50 light microscope and an Olympus C-7070 camera (Olympus Optical Co. Ltd., Tokyo, Japan). Further analyses included histological staining, scanning electron microscopy (SEM) and Energy-dispersive X-ray spectroscopy (EDX). Alizarin Red was used to stain the IOLs’ surface for detection of superficial Calcium deposits. For this staining process lenses were placed in 4% buffered formaldehyde solution for 2 min, rinsed with distilled water, placed in 1% Alizarin Red solution for 3 min and then again rinsed with distilled water before examination under the light microscope. Subsurface Calcium phosphate deposits were stained using the von Kossa method. For this analysis, the IOLs were cut in half. One half was dehydrated and embedded in paraffin. Five micrometers vertical sections from the optical center of the IOL were taken. These sections were deparaffinized, rehydrated and incubated in 5% Silver Nitrate, treated with UV light for 30 min and rinsed several times. After incubation with 5% Sodium Thiosulfate and a final rinsing step, the sections were analyzed using a light microscope. The second halves were sent to the Max-Planck-Institute for Polymer Research in Mainz (Germany) to further analyze the chemical composition of the granules that caused the opacification. Both anterior and posterior surfaces of the IOL were examined using a scanning electron microscope (Hitachi SU8000). The IOL was inspected without any further preparation such as Carbon coating or Gold sputtering. However, in order to minimize charging effects in the scanning electron microscope the acceleration voltage was adjusted to 700 V at as low probe current as possible. If necessary, EDX was performed on selected areas on the surface of the IOL. To achieve a sufficiently strong EDX signal, the probe current of the scanning electron microscope was increased to approximately 200 pA and the acceleration voltage was adjusted to 15 kV. EDX measurements were done with a Quantax 400 detector (Bruker, Billerica, USA). Subsequently, cross sections of the IOL were prepared by ultramicrotomy (Leica UC7) using a 35° diamond knife. For SEM examinations the nominal section thickness was 2.5 μm. After cutting, the sections were floated onto a Silicone wafer and allowed to dry at ambient condition. The SEM examination of the thin sections was done using the same microscope parameters as used in examining the anterior and posterior surfaces. Additionally, sections for Transmission Electron Microscopy (TEM) were prepared by decreasing the nominal section thickness to 100 nm. These sections were transferred to a copper TEM grid. TEM examinations were performed using a Tecnai F20 (FEI) operated at an acceleration voltage of 200 kV. For diffraction measurements in the TEM the selected area diffraction (SAD) aperture was used, the respective area was adjusted to the SAD area and the TEM was switched to diffraction mode. For analysis of the diffraction pattern we used the software package, ProcessDiffraction.19
3. Results
The lenses were explanted from eyes of two female and five male patients. Mean patient age at the time of IOL implantation was 69 years (range 59–78 years). The average time from implantation to explantation was 2.7 years. Opacification of the IOL was first observed between December 2011 and May 2017. In five cases we found in the patients’ medical histories, conditions that are considered to facilitate IOL calcification. In four cases, secondary surgical procedures were performed soon after or immediately following IOL implantation.
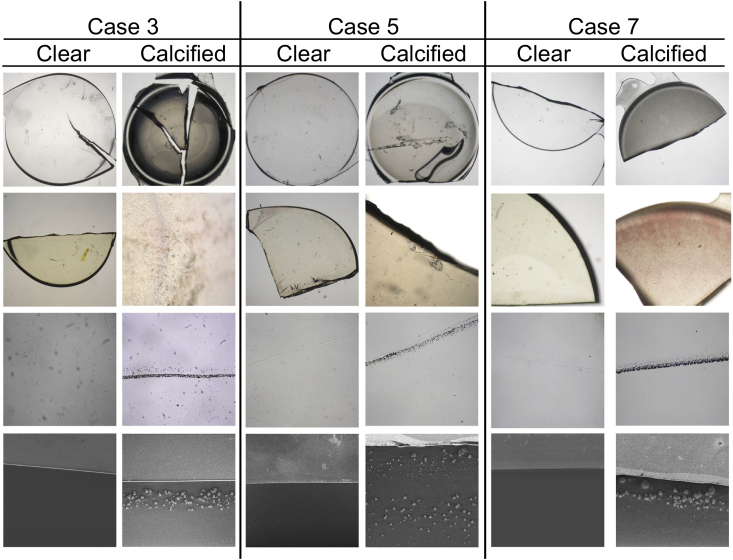
From a total of seven cases in three cases only the supplementary IOL was explanted due to its opacification; in three cases, both IOLs were explanted when the clear sulcus-fixated lens had to be removed to allow access to remove the opacified lens in the capsule; and in one case, both IOLs were explanted as both had opacified but we only received the supplementary IOL for analysis as the capsular bag lens was returned to the manufacturer for analysis (Table 1). All of the supplementary sulcus-supported lenses were Sulcoflex IOLs (Rayner, Hove, United Kingdom) made of a hydrophilic acrylic material with 26% water content (Contamac Ltd, Saffron Waldon Essex, UK) (Table 2). In four cases, the supplementary IOL opacification of was caused by granular Calcium phosphate deposits underneath the anterior surface of the IOL, restricted to a circular pattern (Fig. 1). Severity of calcification differed between the cases from fine granular subsurface deposits that do not involve the optical surface (case 4) to large granules that distorted the lens surface (case 6 and case 2). In case 2, severe opacification occurred in both, the sulcus-supported Sulcoflex and the capsule-fixated lens, an Akreos Adapt (Bausch + Lomb, Rochester, New York, USA). In three cases, calcification occurred in only the capsular bag IOL, while the supplementary lens remained clear (Fig. 2). In two of these cases subsurface deposits were distributed underneath the anterior central pupillary area (Cases 3 and 5), while in one case calcification spread across the whole anterior surface of the lens also affecting parts of the haptics (case 7). All six lenses shown where made from the same hydrophilic acrylic material (Table 2). The time between implantation of the capsule-fixated and the sulcus-supported lens was between one to five months. No surgical procedure was performed between both implantations. However, all three patients suffered from diabetes mellitus (Table 1). Scanning Electron Microscopy (SEM) images of one of the capsule-fixated IOLs (case 7) revealed the ultrastructure of the opacifying crystals. The images show flower-like crystals of a few micrometers in diameter (Fig. 3). Electron diffraction (ED) pattern revealed that the calcification comprised of Hydroxyapatite, which has the chemical composition: .
Table 1.
Patients’ history.
| Case No. |
Patient age at implan-tation/ sex | Implan-tation date (cPCL/Supp) | Ocular surgical procedures between implantation and explantation surgery | Opacification first noticed (cPCL/Supp) | Explantation date (cPCL/Supp) | Medical conditions |
|---|---|---|---|---|---|---|
| 1 | 74/ M | n.k. | No history of additional ocular surgical procedures | n.a. | n.a. | Arterial hypertension |
| Mar 2011 | Dec 2011 | Feb 2012 | ||||
| 2 | 68/ F | n.k. | DSAEK (Sep 2011) due to Fuchs endothelial dystrophy | Sep 2012 | Jan 2013 | Essential hypertension, Myocardial infarction 2001, coronary artery bypass grafting 2003 |
| Dec 2010 | Sep 2012 | Jan 2013 | ||||
| 3 | 78/ M | Sep 2010 | YAG-Capsulotomy | May 2014 | Jul 2014 | Diabetes mellitus |
| Feb 2011 | n.a. | Jul 2014 | ||||
| 4 | n.k./ F | n.k. | PPV with silicone oil for retinal detachment combined with implantation surgery (Sep 2013) | n.k. | n.k. | No history of additional medical conditions |
| Sep 2013 | n.k. | May 2014 | ||||
| 5 | n.k./ M | Jan 2015 | No history of additional ocular surgical procedures | May 2016 | Sep 2016 | Diabetes mellitus |
| Feb 2015 | n.a. | Sep 2016 | ||||
| 6 | 59/ M | n.k. | No history of additional ocular surgical procedures | n.a. | n.a. | Rheumatoid arthritis |
| n.k. | n.k. | Mar 2017 | ||||
| 7 | 65/ M | Oct. 2012 | PPV with cerclage and silicone oil (Mar 2016), silicone oil removal (May 2016), YAG-Capsulotomy (Jan 2017) | May 2017 | Dec 2017 | Diabetes mellitus, HIV, Hepatitis, Liver cirrhosis |
| Feb 2013 | n.a. | Dec 2017 |
F female, M male, n.k. not known, n.a. not applicable, cPCL capsular posterior chamber lens, Supp supplementary lens, DSAEK Descemet's Stripping Automated Endothelial Keratoplasty, PPV pars plana vitrectomy.
Table 2.
IOL characteristics.
| Case No. | Site of opacification | Capsule- and supplementary-IOL (manufacturer) | Polymer material (water content) |
|---|---|---|---|
| 1 | n.a. | PMMA lens (Alcon) | Polymethyl methacrylate (0.3–0.4%) |
| anterior surface | Sulcoflex Toric 653T (Rayner) | Contamac CI26 hydrophilic acrylic (26%) | |
| 2 | anterior surface | Akreos Adapt (Bausch + Lomb) | Contamac CI26 hydrophilic acrylic (26%) |
| anterior surface | Sulcoflex Toric 653T (Rayner) | Contamac CI26 hydrophilic acrylic (26%) | |
| 3 | anterior surface | M-flex Multifocal 580F (Rayner) | Contamac CI26 hydrophilic acrylic (26%) |
| n.a. | Sulcoflex Aspheric 653L (Rayner) | Contamac CI26 hydrophilic acrylic (26%) | |
| 4 | n.k. | n.k. | n.k. |
| anterior surface | Sulcoflex Aspheric 653L (Rayner) | Contamac CI26 hydrophilic acrylic (26%) | |
| 5 | anterior surface | T- flex Aspheric 623T (Rayner) | Contamac CI26 hydrophilic acrylic (26%) |
| n.a. | Sulcoflex Multifocal 653F (Rayner) | Contamac CI26 hydrophilic acrylic (26%) | |
| 6 | n.a. | One-piece IOL (n.k.) | n.k. |
| anterior surface | Sulcoflex Multifocal 653Z (Rayner) | Contamac CI26 hydrophilic acrylic (26%) | |
| 7 | anterior surface | Superflex Aspheric 920H (Rayner) | Contamac CI26 hydrophilic acrylic (26%) |
| n.a. | Sulcoflex Toric 653T (Rayner) | Contamac CI26 hydrophilic acrylic (26%) |
n.k. not known, n.a. not applicable.
Fig. 1.
Microscopic photographs of four calcified sulcus-supported intraocular lenses. The upper row shows overview images in 12.5-fold magnification. The second row shows photographs after staining of superficial deposits with Alizarin Red. The third row shows sagittal cross-sections of the lenses after staining with von Kossa. The lower row shows scanning electron microscopic images of the lenses' cross-sections revealing different calcification patterns. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
Microscopic photographs of three calcified capsule-fixated IOLs and each of the sulcus-supported IOL from the same eye. The upper row shows overview images in 12.5-fold magnification. The second row shows photographs after staining the lens surface with Alizarin Red. The third row shows sagittal cross-sections of the lenses after staining with von Kossa. The lower row shows scanning electron microscopic images of the lenses' cross-sections. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Fig. 3.
ScanningElectron Microscopy (SEM) images of a crystal in the capsule-fixated IOL of case 7 in different magnifications. The morphological microstructure of the hydroxyapatite crystal within the polymer material can be seen in different magnifications. A scale for comparison is seen in the lower left corner of each image.
4. Discussion
We report on seven cases of secondary calcification in lenses from polypseudophakic eyes. Although hundreds of IOL explants are sent to our laboratory each year, we only received seven of such cases during a six-year time period.13 The significance of these cases is not the small number in relation to the total as implanting two lenses in the eye is a relatively rare procedure. The significance is that in these cases the calcification occurred in only one of the two lenses and in one case in both IOLs although each pair of lenses had been in the same eye and had therefore been exposed to the same intraocular environmental conditions. To the best of our knowledge, our series is the largest of secondary calcification in supplementary sulcus-supported lenses. In only one previous case report, from 2015, two IOLs had localized calcification at the anterior surface of a Sulcoflex IOL (Rayner, Hove, United Kingdom) and on an AT Torbi 709 M IOL (Carl Zeiss, Oberkochen, Germany) and the opacification occurred after procedures involving intracameral injection of air.20
Lenses made from hydrophilic acrylate, show a good biocompatibility to uveal tissue.21 As a consequence, it is considered optimal that IOLs intended for sulcus implantation should be made from a hydrophilic acrylate. In terms of material changes, hydrophobic acrylic IOLs are prone to develop liquid-filled microvacuoles (glistenings) within the material when aging that can affect the optical quality of the lens.22,23 Lenses made from hydrophilic acrylate, on the other hand, have the potential to develop IOL calcification.9,13
In cases 3, 5 and 7 both the capsule-fixated lens as the Sulcoflex IOL was made of the same Contamac CI26 polymer and made in the same Rayner manufacturing facility using the same manufacturing process, yet only one lens opacified. This suggests that the calcification of the one lens is not from an intrinsic (“primary”) aspect of the polymer chemistry or the polymer manufacturing or the IOL manufacturing processes. The Sulcoflex lens is manufactured by Rayner in an identical manner to their manufacture of capsule-fixation lens models. (personal communication with company representatives) In these cases, one can assume the lens opacification was provoked by a factor in the intraocular environment which affected one lens but not the other. In case 2, both lenses opacified and both are made of the same Contamac CI26 polymer - albeit lenses made by different lens manufacturers, Rayner and Bausch + Lomb. While that may suggest a primary causation - that is IOL material - or manufacturing-related causation - we conclude otherwise as it is a quite unique case of polypseudophakia followed by Descemet's Stripping Automated Endothelial Keratoplasty (DSAEK) surgery. In a series of primary opacification, the numbers of explants are much greater.11,13 The reasons for primary calcification lie within the packaging of the lens or the manufacturing process of IOL or its raw material, the polymer.12 Recently, a series of 71 explanted lenses from one manufacturer was reported where the opacification occurred without being associated with external factors and the explantations were performed on average 4 years after initial implantation surgery.11 The prevalence of IOL calcification in this kind of lenses was found to be 5.1%.24 In contrast, the pathogenesis of the secondary form of calcification depends less on the lens model or its manufacturer but on intraocular environmental factors that facilitate the calcification process. Secondary IOL calcification can occur in any hydrophilic IOL independent from the model or manufacturer.6,12
Different intraocular environmental factors appear to create a distinctive morphological pattern of calcification. Some surgical procedures are considered to facilitate IOL calcification such as pars plana vitrectomy (PPV), Descemet Membrane Endothelial Keratoplasty (DMEK) or intravitreal injections of medication.6,7,25 The immune system is thought to be a key factor in the initiation of calcification in other medical devices.26 Thus, a surgical trauma that induces an immunoreaction is a plausible risk factor for IOL calcification.27,28 A study by Schrittenlocher et al. found in a group of 564 consecutive DMEK patients that the relative risk for the IOL calcification was 3.88 (95% CI = 1.07–14.05). Furthermore, repeated re-bubblings were associated with a higher risk of IOL calcification with an odds ratio of 7.49 (95% CICI = 1.66–33.79).25 In accordance with these previous studies, our analysis supports that posterior lamellar keratoplasty carry a risk for IOL calcification since the only case where IOL calcification occurred in both of the lenses was the case where a DSAEK surgery was performed (case 2). Opacification of the sulcus-supported lens as well as the capsule-fixated IOL was first noted one year thereafter. Furthermore, our analyses showed that the sulcus-supported lens had the densest calcification pattern of all our studied IOLs - even leading to deformation of the lens surface structure (Fig. 1). A previous study on ten IOLs from eyes that have received PPV with intraocular injection of gas the lenses developed centrally localized IOL calcification.6 The authors concluded that the instillation of gas into a pseudophakic eye with hydrophilic acrylic IOL seems to increase the risk for secondary calcification, irrespective of the IOL manufacturer.6 Two of the eyes in our series (case 4 and 7) had received PPV developed IOL calcification that lead to explantation of the lens 8 and 21 months after the procedure. Whereas in case 4 calcification was rather mild and did not affect the surface structure of the lens (Fig. 1), case 7 showed denser calcification that spread across its whole anterior surface (Fig. 2).
One theory about the pathogenesis of IOL calcification in diabetic patients is that a breakdown of the blood-aqueous barrier leads to a change in the composition of the aqueous humor that facilitates the calcification process.17 Nakanome et al. analyzed the concentrations of Calcium- and Phosphate ions, and Albumin in the aqueous humor of patients with diabetic mellitus that received phacoemulsification and IOL implantation.17 Concentrations of all three were elevated in patients with diabetic retinopathy (DR) compared to patients without DR. The authors concluded that accumulation of Calcium Phosphate deposits occurs more easily when concentrations of Calcium- and Phosphate ions and Albumin in the aqueous humor begin to fluctuate as a result of a blood-aqueous barrier breakdown.17 Similarly, Kim and Choi found that whereas Calcium levels did not differ significantly between diabetics and non-diabetics, the concentration of Phosphate ions in diabetics were considerably higher than those in non-diabetics. The authors concluded that this could lead to a higher risk of opacification of hydrophilic acrylic IOL in diabetic patients.29 In support of these theories, in our series, all three patients suffered from diabetes mellitus that developed IOL calcification of the capsule-fixated IOL. One might postulate that the implantation of the secondary IOL could have induced an inflammatory trauma leading to calcification of the capsule-fixated lens and that these diabetic patients might already have higher levels of Calcium- and Phosphate ions in the aqueous humor.17,29 In all of these cases the primarily implanted capsular-bag-fixated IOLs calcified, while the sulcus-supported lenses made from the same hydrophilic acrylic material remained clear in the same eye (Cases 3, 5 and 7). An explanation for this finding could be that the microenvironments differed for the two lenses. The calcified IOL in the bag was partly covered by the capsule and only exposed to a rather static microenvironment of aqueous humor between it and the Sulcoflex in the area of the capsulorhexis. Aqueous humor surrounding the sulcus-supported IOL, on the other hand, washed freely around it, making less chance of creating a gradient of concentration of Calcium- and Phosphate ions that could enter into the Sulcoflex polymer.
The research group of Koutsoukos, Gartaganis and Drimtzias has demonstrated a promising approach to elucidating the mechanisms of IOL calcification.18,30 They created an in-vitro experimental method to investigate the chemical kinetics of IOL calcification. Using their model, they were able to induce prismatic nanoparticles of hydroxyapatite in the interior of hydrophilic IOLs. The crystals were first seen after five months, approximately 10 μm from the lens surface. With increasing time, the deposits grew and extended to a depth of 249 μm from the surface.18 Their results resemble the subsurface deposits we found distributed underneath the central pupillary area (e.g. in Cases 1, 3 and 4) were the deposits are distributed across a line parallel to the lens surface and separated from it by a clear zone where there was an absence of deposit. Drimtzias et al. suggested that polar functional groups, like OH- and COO-, present in the hydrophilic polymer result in an increase in electron density on the lens surface reducing the interfacial energy between the polymer and aqueous solution.18 Their study made an important contribution but this explanation of the likely reaction mechanism at the lens surface and within the polymer that borders the lens surface needs elaboration, to explain why the different clinical and environmental risk factors associated with clinical lens opacification should influence these reactions. How does the use in surgery of air, gas or silicone oil alter the IOL environment and affect these reactions? Or, the inflammatory process provoked by surgical trauma or by a systemic disease such as diabetes mellitus - why would these risk factors lead to lens changes in electron density on the lens surface and how would that in turn lead over time to lens opacification?
Until recently clinical studies on explants have used histological staining methods to confirm that IOL opacifications were caused by Calcium- and Phosphate ions. Only a few attempts have been made to reveal the ultrastructure and exact chemical architecture of the mineral deposits within the lens material. Calcification of intraocular lenses is a dynamic process.31 Previously, studies suggested that early stages of newly formed crystals are unable to cause any significant changes to the lens surface, whereas later stages of crystallization can lead to subsequent lens rupture and deformation.31 Lin et al. found mainly poorly-formed crystalline, immature non-stoichiometric deposits in an opacified Hydroview H60 M IOL (Bausch & Lomb, Clearwater, USA) that was in the eye for two years.32 Avetisov et al. proposed that calcifications mainly consist of Tricalcium Phosphate [] with Zinc impurities possibly playing a role in the calcification process.31 In the present study we used a new approach to characterize the Calcium Phosphate deposits by the means of ED pattern analysis. In an IOL that was inside of the eye for more than 5 years (case 7), we could show that the crystals consist of a mature Hydroxyapatite where we could identify the chemical composition as .
Our study obviously has certain limitations: Most IOL explants received at our laboratory are accompanied with all of the relevant general and ophthalmic medical history but since the donating surgeons provides this data, patient's medical history does not always have to be complete. Furthermore, calcification in one opacified IOL was not confirmed by material analysis as the lens was not send to our laboratory but returned to the manufacturer. It should be noted, that the high number of Rayner IOLs in this study is a reflection of the circumstance that Rayner Intraocular Lenses Ltd., routinely send their IOLs to our laboratory for material analysis, whereas explant IOLs from other manufacturers only reach us through the cooperation of individual ophthalmic surgeons or companies.
Nevertheless, studying explanted calcified IOLs from polypseudophakic eyes and placing the results alongside the results of the ongoing modelling studies of lens opacification, allows us to approach a much better understanding of IOL calcification.
5. Conclusions
In one eye, two lenses made from the same hydrophilic acrylic material can exhibit different development of calcification depending on an as yet unknown trigger factor. The severity of calcification and its pattern differ from case to case, and this depends on either the comorbidity or the surgical intervention conducted after the IOL implantation. Our results suggest that the microenvironment of the lens in the eye plays an important role in the development of this pathology.
Patient consent statement
Our laboratory study only involved analyses of IOL explants. We did not perform any additional examinations or procedures on humans or animals. Therefore, informed consent and ethical approval were not required.
Funding
The David J. Apple International Laboratory for Ocular Pathology receives funding from the Klaus Tschira Stiftung, Heidelberg, Germany (https://www.klaus-tschira-stiftung.de). T. Yildirim is funded by the Physician-Scientist Program of the Heidelberg University, Faculty of Medicine. The funding organizations had no role in any aspect of this research.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Acknowledgements
I. Vöhringer made a contribution to the morphological analysis of the explants.
Contributor Information
Timur M. Yildirim, Email: timur.yildirim@med.uni-heidelberg.de.
Ramin Khoramnia, Email: ramin.khoramnia@med.uni-heidelberg.de.
Sonja K. Schickhardt, Email: sonja.schickhardt@med.uni-heidelberg.de.
Donald J. Munro, Email: donald.munro@djapplelab.com.
Patrick R. Merz, Email: patrick.merz@med.uni-heidelberg.de.
Hyeck-Soo Son, Email: hyecksoo.son@med.uni-heidelberg.de.
Ingo Lieberwirth, Email: lieberw@mpip-mainz.mpg.de.
Gerd U. Auffarth, Email: gerd.auffarth@med.uni-heidelberg.de, gerd.auffarth@med.uni-heidelberg.de.
References
- 1.Kahraman G., Amon M. New supplementary intraocular lens for refractive enhancement in pseudophakic patients. J Cataract Refract Surg. 2010;36:1090–1094. doi: 10.1016/j.jcrs.2009.12.045. [DOI] [PubMed] [Google Scholar]
- 2.Rabsilber T.M., Kretz F.T., Holzer M.P., Fitting A., Sanchez M.J., Auffarth G.U. Bilateral implantation of toric multifocal additive intraocular lenses in pseudophakic eyes. J Cataract Refract Surg. 2012;38:1495–1498. doi: 10.1016/j.jcrs.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 3.Yildirim T.M., Auffarth G.U., Son H.S., Mayer C.S., Tandogan T., Khoramnia R. [Duet procedure in high myopia to achieve reversible multifocality] Klinische Monatsblatter fur Augenheilkunde. 2019 doi: 10.1055/a-0916-8780. [DOI] [PubMed] [Google Scholar]
- 4.Khoramnia R., Yildirim T.M., Son H.-S., Łabuz G., Mayer C.S., Auffarth G.U. Reversible Trifokalität durch das Duett-Verfahren [Duet procedure to achieve reversible trifocality] Ophthalmologe. 2020 doi: 10.1007/s00347-020-01096-4. [published online ahead of print, 2020 Apr 15] [published correction appears in Ophthalmologe. 2020 May 11;:] [Online ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scharioth G.B. New add-on intraocular lens for patients with age-related macular degeneration. J Cataract Refract Surg. 2015;41:1559–1563. doi: 10.1016/j.jcrs.2015.07.018. [DOI] [PubMed] [Google Scholar]
- 6.Yildirim T.M., Auffarth G.U., Labuz G., Bopp S., Son H.S., Khoramnia R. Material analysis and optical quality assessment of opacified hydrophilic acrylic intraocular lenses after pars plana vitrectomy. Am J Ophthalmol. 2018;193:10–19. doi: 10.1016/j.ajo.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 7.Roland S., Khoramnia R., Auffarth G.U., Son H.S., Yildirim T.M., Schoenherr U. [Opacification of hydrophilic intraocular lens after multiple injections of bevacizumab] Ophthalmologe. 2018;116(9):882–886. doi: 10.1007/s00347-018-0829-3. [DOI] [PubMed] [Google Scholar]
- 8.Giers B.C., Tandogan T., Auffarth G.U. Hydrophilic intraocular lens opacification after posterior lamellar keratoplasty - a material analysis with special reference to optical quality assessment. BMC Ophthalmol. 2017;17:150. doi: 10.1186/s12886-017-0546-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yildirim T.M., Labuz G., Khoramnia R. Impact of primary calcification in segmented refractive bifocal intraocular lenses on optical performance including straylight. J Refract Surg. 2020;36:20–27. doi: 10.3928/1081597X-20191119-01. Thorofare, NJ : 1995. [DOI] [PubMed] [Google Scholar]
- 10.Marcovich A.L., Tandogan T., Bareket M. Opacification of hydrophilic intraocular lenses associated with vitrectomy and injection of intraocular gas. BMJ Open Ophthalmol. 2018;3 doi: 10.1136/bmjophth-2018-000157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gurabardhi M., Haberle H., Aurich H., Werner L., Pham D.T. Serial intraocular lens opacifications of different designs from the same manufacturer: clinical and light microscopic results of 71 explant cases. J Cataract Refract Surg. 2018;44:1326–1332. doi: 10.1016/j.jcrs.2018.07.026. [DOI] [PubMed] [Google Scholar]
- 12.Neuhann I.M., Kleinmann G., Apple D.J. A new classification of calcification of intraocular lenses. Ophthalmology. 2008;115:73–79. doi: 10.1016/j.ophtha.2007.02.016. [DOI] [PubMed] [Google Scholar]
- 13.Neuhann T., Yildirim T.M., Son H.-S., Merz P.R., Khoramnia R., Auffarth G.U. Reasons for explantation, demographics and material analysis of 200 intraocular lens explants. J Cataract Refract Surg. 2020;46(1):20–26. doi: 10.1016/j.jcrs.2019.08.045. [DOI] [PubMed] [Google Scholar]
- 14.Tandogan T., Khoramnia R., Choi C.Y. Optical and material analysis of opacified hydrophilic intraocular lenses after explantation: a laboratory study. BMC Ophthalmol. 2015;15:170. doi: 10.1186/s12886-015-0149-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khoramnia R., Salgado J.P., Auffarth G.U. [Opacification of a hydrophilic intraocular lens 4 years after cataract surgery. A biomaterial analysis] Ophthalmologe. 2012;109:483–486. doi: 10.1007/s00347-011-2487-6. [DOI] [PubMed] [Google Scholar]
- 16.Fung S.S., Sykakis E., Islam N.M. Intraocular lens opacification following intracameral injection of recombinant tissue plasminogen activator to treat inflammatory membranes after cataract surgery. J Ophthalmol. 2015;2015:975075. doi: 10.1155/2015/975075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakanome S., Watanabe H., Tanaka K., Tochikubo T. Calcification of Hydroview H60M intraocular lenses: aqueous humor analysis and comparisons with other intraocular lens materials. J Cataract Refract Surg. 2008;34:80–86. doi: 10.1016/j.jcrs.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 18.Drimtzias E.G., Rokidi S.G., Gartaganis S.P., Koutsoukos P.G. Experimental investigation on mechanism of hydrophilic acrylic intraocular lens calcification. Am J Ophthalmol. 2011;152:824–833 e1. doi: 10.1016/j.ajo.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 19.Labar J.L. Consistent indexing of a (set of) single crystal SAED pattern(s) with the ProcessDiffraction program. Ultramicroscopy. 2005;103:237–249. doi: 10.1016/j.ultramic.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 20.MacLean K.D., Apel A., Wilson J., Werner L. Calcification of hydrophilic acrylic intraocular lenses associated with intracameral air injection following DMEK. J Cataract Refract Surg. 2015;41:1310–1314. doi: 10.1016/j.jcrs.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 21.Abela-Formanek C., Amon M., Kahraman G., Schauersberger J., Dunavoelgyi R. Biocompatibility of hydrophilic acrylic, hydrophobic acrylic, and silicone intraocular lenses in eyes with uveitis having cataract surgery: long-term follow-up. J Cataract Refract Surg. 2011;37:104–112. doi: 10.1016/j.jcrs.2010.07.038. [DOI] [PubMed] [Google Scholar]
- 22.Labuz G., Knebel D., Auffarth G.U. Glistening formation and light scattering in six hydrophobic-acrylic intraocular lenses. Am J Ophthalmol. 2018;196:112–120. doi: 10.1016/j.ajo.2018.08.032. [DOI] [PubMed] [Google Scholar]
- 23.Weindler J.N., Labuz G., Yildirim T.M., Tandogan T., Khoramnia R., Auffarth G.U. The impact of glistenings on the optical quality of a hydrophobic acrylic intraocular lens. J Cataract Refract Surg. 2019;45:1020–1025. doi: 10.1016/j.jcrs.2019.01.025. [DOI] [PubMed] [Google Scholar]
- 24.Bompastor-Ramos P., Povoa J., Lobo C. Late postoperative opacification of a hydrophilic-hydrophobic acrylic intraocular lens. J Cataract Refract Surg. 2016;42:1324–1331. doi: 10.1016/j.jcrs.2016.06.032. [DOI] [PubMed] [Google Scholar]
- 25.Schrittenlocher S., Penier M., Schaub F., Bock F., Cursiefen C., Bachmann B. Intraocular lens calcifications after (triple-) Descemet membrane endothelial keratoplasty. Am J Ophthalmol. 2017;179:129–136. doi: 10.1016/j.ajo.2017.04.024. [DOI] [PubMed] [Google Scholar]
- 26.Siddiqui R.F., Abraham J.R., Butany J. Bioprosthetic heart valves: modes of failure. Histopathology. 2009;55:135–144. doi: 10.1111/j.1365-2559.2008.03190.x. [DOI] [PubMed] [Google Scholar]
- 27.Lee S.J., Choi J.H., Sun H.J., Choi K.S., Jung G.Y. Surface calcification of hydrophilic acrylic intraocular lens related to inflammatory membrane formation after combined vitrectomy and cataract surgery. J Cataract Refract Surg. 2010;36:676–681. doi: 10.1016/j.jcrs.2009.08.045. [DOI] [PubMed] [Google Scholar]
- 28.Werner L., Wilbanks G., Ollerton A., Michelson J. Localized calcification of hydrophilic acrylic intraocular lenses in association with intracameral injection of gas. J Cataract Refract Surg. 2012;38:720–721. doi: 10.1016/j.jcrs.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 29.Kim C.J., Choi S.K. Analysis of aqueous humor calcium and phosphate from cataract eyes with and without diabetes mellitus. Kor J Ophthalmol : Kor J Ophthalmol. 2007;21:90–94. doi: 10.3341/kjo.2007.21.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gartaganis S.P., Kanellopoulou D.G., Mela E.K., Panteli V.S., Koutsoukos P.G. Opacification of hydrophilic acrylic intraocular lens attributable to calcification: investigation on mechanism. Am J Ophthalmol. 2008;146:395–403. doi: 10.1016/j.ajo.2008.04.032. [DOI] [PubMed] [Google Scholar]
- 31.Avetisov S.E., Gamidov A.A., Novikov I.A., Fedorov A.A., Kas'yanov A.A. [Chemical microanalysis of mineral deposits on explanted hydrophilic acrylic intraocular lenses] Vestn Oftalmol. 2015;131:74–78. doi: 10.17116/oftalma2015131474-78. [DOI] [PubMed] [Google Scholar]
- 32.Lin S.Y., Chen K.H., Lin C.C., Cheng W.T., Li M.J. Spectral analysis and comparison of mineral deposits forming in opacified intraocular lens and senile cataractous lens. Spectrochim Acta Mol Biomol Spectrosc. 2010;77:703–708. doi: 10.1016/j.saa.2010.07.012. [DOI] [PubMed] [Google Scholar]