S U M M A R Y
Background
In clinical routine, preoperative radiographic assessment of lower extremity geometry relies on conventional X-rays. However, the plane goniometric measuring has several limitations in accurately locating anatomical landmarks. The purpose of this study is to propose a fast and accurate 3D-reconstruction-method based on biplanar X-rays with clinical measurements assessment in standing position.
Methods
50 candidates for HTO or DFO with deformity of the lower extremities were included in this study. Biplanar X-rays were performed using the EOS imaging system in conventional double-stance full weight-bearing position (DS) and shifted-foot standing position (SF). The results of hip-knee-ankle angle (HKAA), lateral distal femoral angle (LDFA), and medial proximal tibial angle (MPTA) were evaluated by either 2D manual goniometer (MG) based on X-ray in DS standing position or 3D-reconstruction goniometer based on X-rays in SF standing position.
Results
For the reproducibility study, MG and EOS goniometer were both reliable in repeated measures of HKAA, LDFA, and MPTA, with average concordance correlation coefficients (CCCs) all above 0.910. The agreements between MG and EOS measurements were high for HKAA and LDFA with CCCs all above 0.90, while the agreement was low for MPTA with CCC below 0.75. Further linear regression model analysis also revealed a significant correlation between MG and EOS measurements for HKAA (all R2 ≥ 0.93) and LDFA (all R2 ≥ 0.90), but not for MPTA (all R2 ≤ 0.522).
Conclusion
In comparison with the traditional 2D manual goniometer, EOS 3D reconstruction based goniometric measuring could provide equivalent results of HKAA and LDFA, and potentially a more accurate result of MPTA. These findings suggest that EOS 3D reconstruction based goniometric measuring is suitable for preoperative evaluation and planning for HTO/DFO. However, future improvements of the 3D reconstruction method are needed for better detection of the femoral condyles and tibial plates without the requirement of shifted-foot standing position.
The translational potential of this article
EOS 3D reconstruction based goniometric measuring could provide equivalent or even more accurate results of HKAA, LDFA, and MPTA, in comparison with the traditional 2D manual goniometer, making it suitable for preoperative evaluation and planning for HTO/DFO.
Keywords: Biplanar X-rays, Knee, Lower limb, Osteotomy, 3D modelling
Introduction
High tibial osteotomy (HTO) and distal femoral osteotomy (DFO) have gained wide acceptance as treatment options for patients with tibiofemoral osteoarthritis and extra-articular deformity of the femur or tibia. Most candidates for HTO/DFO are in the third, fourth, and fifth decades and wish to avoid unicompartmental or total knee arthroplasty. The recommendations for these procedures are derived from a careful evaluation of subjective symptoms, findings on physical examination, and especially radiographic evidence of malalignment and extra-articular deformity.
Accurate radiographic assessment of lower extremity geometry has major importance in clinical routine for diagnosis of arthritis and extra-articular deformity, surgical planning, and patient follow-up. Typically, radiographic assessment of lower extremities is based on 2D full-length radiographs of the lower limb with the patient in the standing position [1,2]. Double-stance, full-length anteroposterior (AP) radiographs showing both lower extremities from the femoral heads to the ankle joints are obtained. The anatomical and mechanical axes of the lower extremities are assessed based on the full-limb AP view. The angle between the mechanical axes of the femur and the tibia is defined as the hip-knee-ankle angle (HKAA), which is used to evaluate the lower limb alignment. The angle between the femoral mechanical axis and the articular surface of the distal femur is defined as the lateral distal femoral angle (LDFA), which is used to evaluate the deformity of the femur. The angle between the tibial mechanical axis and the articular surface of the proximal tibia is defined as the medial proximal tibial angle (MPTA). However, we find plane goniometric measurements are very sensitive to the patient's orientation. Rotational attitudes can affect radiographic measurements when an excessive degree of femoral bowing is present [3]. In clinical routine, attention to detail is essential when making the weight-bearing full-limb X-rays to ensure that both knees are extended maximally and the patellae are pointing forward. Even though, there still exist many challenges for accurate locating the center of the distal femur, the center of the proximal tibia, the articular surface of the distal femur and the articular surface of the proximal tibia.
Biplanar X-rays (EOS imaging system) with the subjects in a standing position can be an alternative in clinical routine with low radiation dose. Several previous studies have already explored this technology to perform 3D-reconstructions of bony structures [[4], [5], [6]]. It has presented an excellent advantage in dealing with torsional troubles and rotational troubles. However, 3D reconstructions cannot be completed in the conventional double-stance full weight-bearing standing position. To obtain better visibility of femoral condyles, tibial plates and the malleoli on the sagittal radiograph for performing 3D-reconstructions of bony structures, the examination is performed with one foot slightly shifted to the other one. This position is called the shifted-foot (SF) standing position. However, it has been evidenced that weight-bearing status can affect malalignment measures [2,7]. For the lower limb being ahead, the higher weight-bearing status is noticed compared to the double-stance position. For the other lower limb, the lower weight-bearing status is also noticed. Although Chaibi et al. declared that there was no significant bias in clinical measurements between shifted-feet and non-shifted-feet position [8]. However, this study only involved 20 volunteers who did not present any visible abnormality of the lower limb and the pelvis. The accuracy of 3D reconstruction clinical measurement calculation in patients with deformity of the lower extremities was still unreported. Furthermore, both 2D and 3D clinical measurements were both automatically calculated based on the 3D reconstruction model in this study, without identification of the agreements between 3D reconstruction calculation and manual goniometer.
To deal with these limitations, the purpose of this study was to identify the reliability and concurrent validity of the EOS system for measuring three important angles for HTO and DFO (HKAA, LDFA, and MPTA).
Materials and methods
Candidates to be measured
50 candidates for HTO and/or DFO with deformity of the lower extremities were included in this study. There were 18 men and 32 women. The median age of the candidates was 62 years (26–74).
Radiographic acquisition protocol
Biplanar X-rays were performed using the EOS low dose imaging system (EOS imaging, Paris, France). The radiation dose is about 800–1000 times less than CT-scan and 8–10 times less than conventional radiography [9,10]. This system could perform the simultaneous acquisition of two orthogonal head to feet calibrated X-rays, with the patient in a standing position.
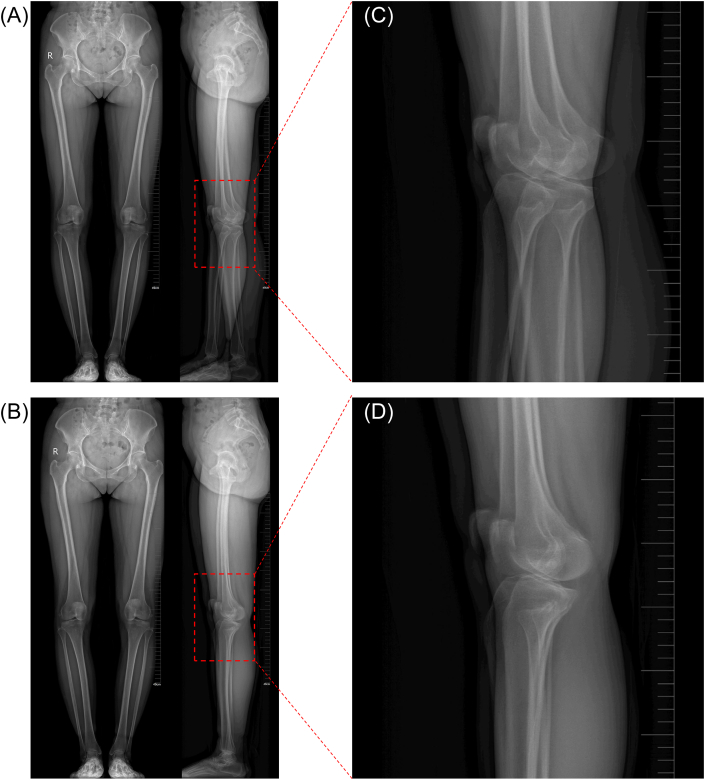
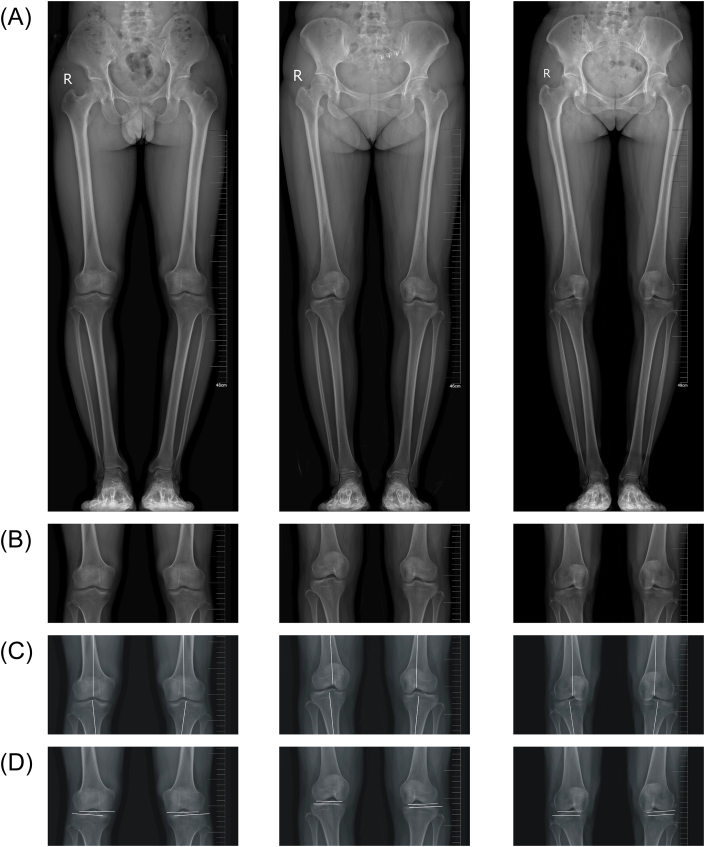
To identify the influence of the shifted-feet position, two acquisitions were performed. Each patient was first positioned standing with parallel feet in conventional double-stance full weight-bearing position (DS position, Fig. 1B). The femoral condyles and tibial plates are superimposed in this position (Fig. 1D). Then the second acquisition was performed with the right foot slightly shifted to the left one (SF position, Fig. 1A), to obtain better visibility of femoral condyles, tibial plates and the malleoli on the sagittal radiograph (Fig. 1C).
Figure 1.
(A) Radiographs in the ‘SF’ standing position. (B) Conventional radiographs in the ‘DS’ standing position. (C) A detail view from an ‘SF’ lateral radiography showing less superposition of the femoral condyles and tibial plates. (D) A detail view from a ‘DS’ lateral radiography showing the superposition of the femoral condyles and tibial plates.
Examiners
Goniometric measurements using a 2D manual goniometer (MG) were performed by one qualified radiologist (H.J) with ten years of radiologic clinical experience and experience with the use of the MG. EOS 3D-reconstruction based goniometric measurements were also performed by the qualified radiologist (H.J) with qualified experience with the use of the EOS system. The examiners were asked to complete all the measurements within two weeks, and two weeks later the examiners were asked to repeat all the measurements. In total, each examiner should complete three MG or EOS measurements for all the 50 candidates.
Recorder
Documentation of all goniometric measurements was performed by one independent recorder (S.W.D), with twenty years of orthopedic clinical experience.
Instrumentation and protocol
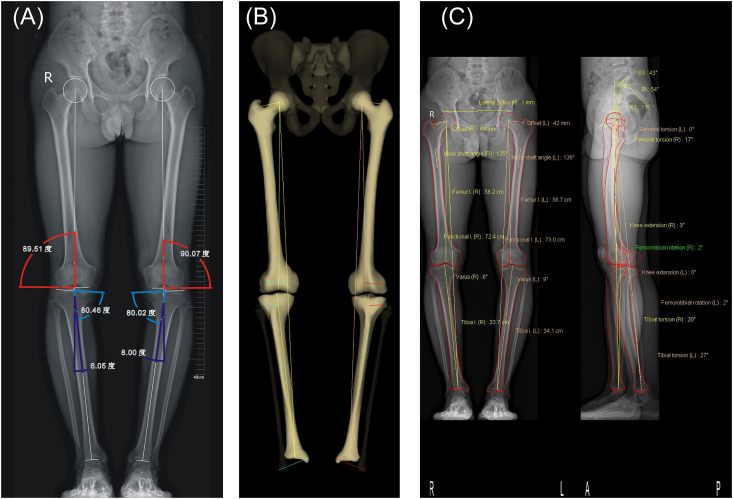
Manual goniometric measurements were performed by L.J using CorelDraw (version 12.0) according to the protocol described previously [11]. Briefly, the first step was to draw a line from the center of the femoral head to the center of the tibial plafond at the ankle joint. In the second step, the mechanical axes of the tibia and the femur were drawn. The femoral mechanical axis was the line between the center of the femoral head and the center of the distal femur. The tibial mechanical axis was a line drawn from the center of the tibial plafond to the center of the proximal tibia. The angle between the mechanical axes of the femur and the tibia is defined as the hip-knee-ankle angle (HKAA, Fig. 2A, red angle), which is used to evaluate the lower limb alignment. The third step of the analysis was to evaluate the deformity of the femur and the tibia. The angle between the femoral mechanical axis and the articular surface of the distal femur is defined as the lateral distal femoral angle (LDFA, Fig. 2A, blue angle), which is used to evaluate the deformity of the femur. The angle between the tibial mechanical axis and the articular surface of the proximal tibia is defined as the medial proximal tibial angle (MPTA, Fig. 2A, purple angle).
Figure 2.
(A) 2D manual goniometric measurements of hip-knee-ankle angle (HKAA, red angle), lateral distal femoral angle (LDFA, blue angle), medial proximal tibial angle (MPTA, purple angle) were performed using CorelDraw software. (B) 3D reconstruction model was obtained based on X-rays in SF standing position. (C) The results of clinical measurements were automatically calculated based on the 3D reconstruction model.
EOS 3D-reconstruction based goniometric measurements were performed by H.J using the EOS 3D reconstruction system. Briefly, a 3D reconstruction model was obtained according to the protocol described by the manufacturer (Fig. 2B). Then, the results of three angles (HKAA, LDFA, and MPTA) were automatically calculated based on the 3D reconstruction model (Fig. 2C).
Statistical analysis
The concordance correlation coefficient (CCC) [12] was calculated using the cccrm 1.2.1 package with R software to assess the reliability of MG and EOS measurements within each method (three repeat measurements). The agreement between MG and EOS measurements was assessed using CCC. The results are presented with 95% confidence intervals (95% CI).
The Blande–Altman plots [13] were used to assess agreement visually. The Blande–Altman plot displayed a scatter plot of the average MG and EOS measurements versus their differences. If an agreement is good then the differences should be randomly scattered around the zero-difference reference line.
We used R software, version 3.5.3 (R Project for Statistical Computing) for the data analyses. P values < 0.05 were considered statistically significant.
Results
The results of the goniometric measurements are presented in Supporting information Table 1. The results are presented as mean ± standard deviation (SD). Intra-rater reliability of both MG as well as EOS measurements was high for HKAA, LDFA, and MPTA, with average CCCs all above 0.910 (Table 1).
Table 1.
Average concordance correlation coefficients (CCC) for Manual Goniometer (MG) and EOS measurements based on three repeat measures per method and averaged for MG and EOS measurements.
| Angle | n | MG |
EOS |
||
|---|---|---|---|---|---|
| CCC | 95% CI | CCC | 95% CI | ||
| HKAA | |||||
| Overall | 100 | 0.999 | 0.998–0.999 | 0.993 | 0.988–0.996 |
| Right leg | 50 | 0.999 | 0.998–0.999 | 0.995 | 0.992–0.997 |
| Left leg | 50 | 0.999 | 0.999–0.999 | 0.989 | 0.979–0.995 |
| LDFA | |||||
| Overall | 100 | 0.992 | 0.990–0.994 | 0.961 | 0.948–0.970 |
| Right leg | 50 | 0.994 | 0.991–0.996 | 0.970 | 0.955–0.981 |
| Left leg | 50 | 0.991 | 0.986–0.994 | 0.950 | 0.927–0.965 |
| MPTA | |||||
| Overall | 100 | 0.924 | 0.900–0.943 | 0.982 | 0.975–0.987 |
| Right leg | 50 | 0.914 | 0.872–0.943 | 0.980 | 0.968–0.987 |
| Left leg | 50 | 0.934 | 0.904–0.955 | 0.984 | 0.976–0.989 |
95% CI = 95% confidence interval
HKAA = hip-knee-ankle angle
LDFA = lateral distal femoral angle
MPTA = medial proximal tibia angle
The agreements between MG and EOS measurements were high for HKAA and LDFA with CCCs all above 0.90, while the agreement was low for MPTA with CCC below 0.75 (Table 2). Subgroup analyses revealed that the agreement for MPTA was even lower in the right leg when compared with that in the left leg (Table 2).
Table 2.
Concordance correlation coefficients (CCC) assessing agreement between Manual Goniometer (MG) and EOS measurements based on the averages of three repeat measurements.
| Angle | n | CCC | 95% CI |
|---|---|---|---|
| HKAA | |||
| Overall | 100 | 0.959 | 0.944–0.970 |
| Right leg | 50 | 0.962 | 0.942–0.975 |
| Left leg | 50 | 0.956 | 0.931–0.972 |
| LDFA | |||
| Overall | 100 | 0.908 | 0.876–0.931 |
| Right leg | 50 | 0.904 | 0.856–0.937 |
| Left leg | 50 | 0.911 | 0.866–0.941 |
| MPTA | |||
| Overall | 100 | 0.682 | 0.587–0.758 |
| Right leg | 50 | 0.669 | 0.534–0.771 |
| Left leg | 50 | 0.696 | 0.556–0.798 |
95% CI = 95% confidence interval
HKAA = hip-knee-ankle angle
LDFA = lateral distal femoral angle
MPTA = medial proximal tibia angle
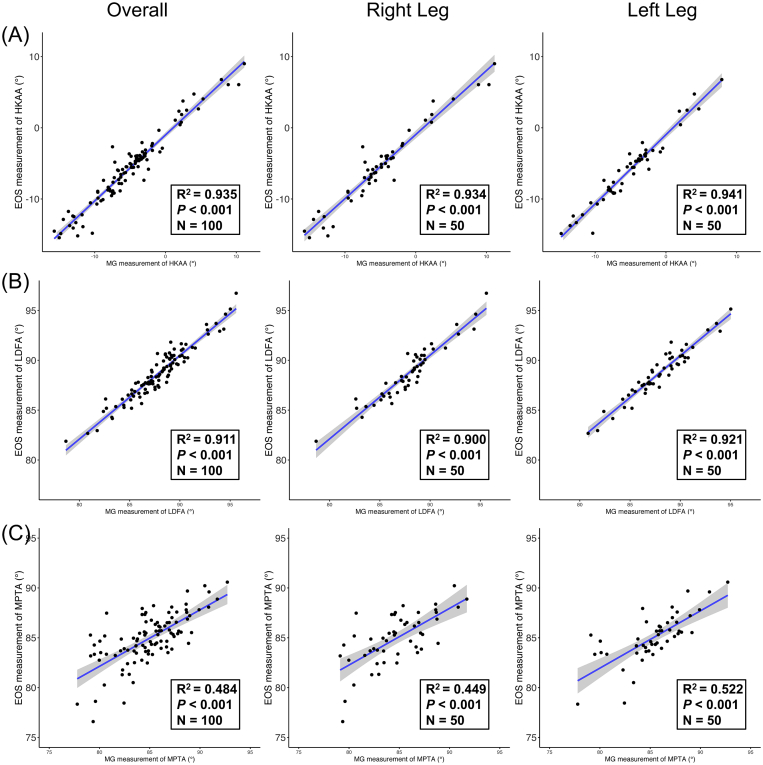
Further linear regression model analysis (Fig. 3) also revealed a significant correlation between MG and EOS measurements for HKAA (all R2 ≥ 0.93) and LDFA (all R2 ≥ 0.90), but not for MPTA (all R2 ≤ 0.522), which well agrees with the prior results of CCC analysis. The correlations between MG and EOS measurements in the right leg were also lower than those in the left leg.
Figure 3.
A) Agreements between Manual Goniometer (MG) and EOS 3D-reconstruction based goniometer measurements based on the averages of three repeat measurements in HKAA. (B) Agreements of LDFA. (C) Agreements of MPTA.
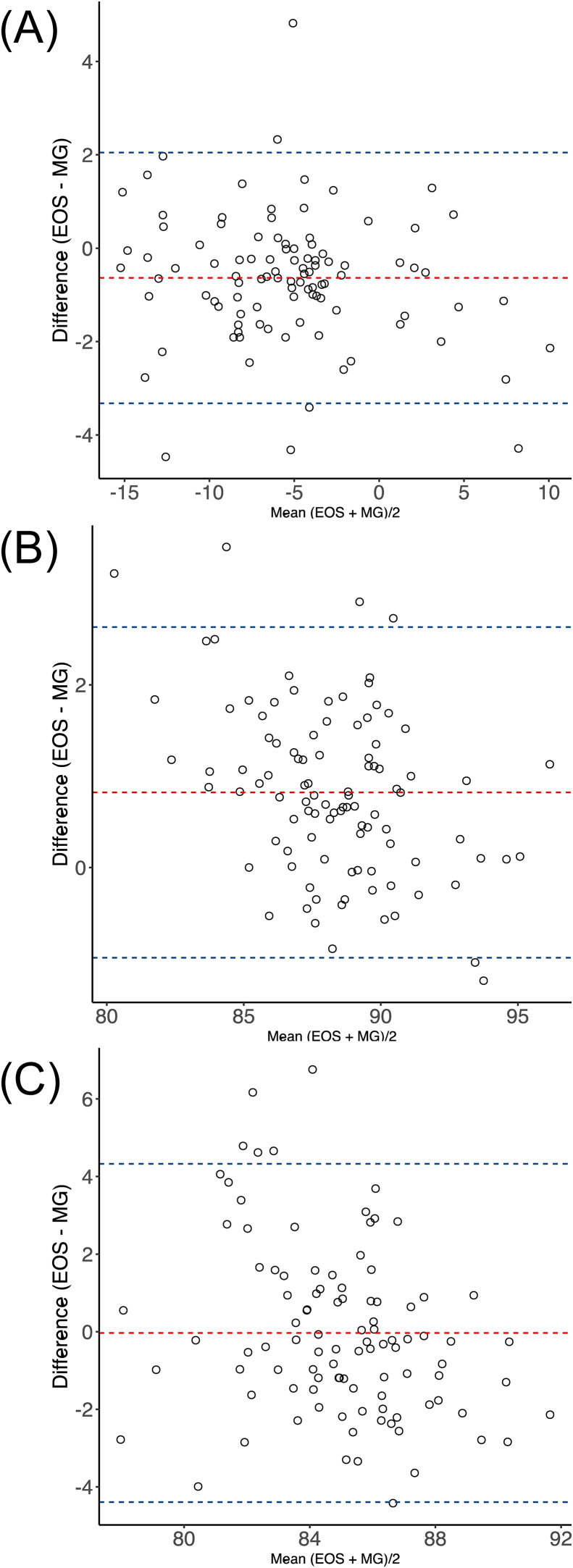
The Blande–Altman plot showed 94 measurement pairs (94%) to be in the mean ± 1.96 standard deviation range of the differences (Fig. 4A–C).
Figure 4.
(A) Bland-Altman plot of average versus the difference between measurements of MG and EOS (MG – EOS) in HKAA. (B) Bland-Altman plot of LDFA. (C) Bland-Altman plot of MPTA. Red lines: the average of the differences. Blue lines: the upper and lower horizontal lines marking ±1.96 standard deviations of the differences.
Discussion
The potential shortcoming of the manual goniometric measurements based on the conventional 2D radiography is the use of 2D projections of 3D bony anatomical landmarks for angles calculation. The projected values are sensitive to the patient's orientation while taking radiographs (bending and/or rotating) [14,15]. During the radiographic procedure, we have paid particular attention to ensure that both knees are extended maximally and the patellae are pointing forward. However, we found there were obvious deformations of the distal femur and proximal tibia, and it was really difficult to accurately locate the anatomical landmarks around the knee.
Several previous studies have already explored CT-scan slices based 3D reconstruction to calculate clinical parameters [[16], [17], [18]]. However, those studies require all axial CT-scan slices for the whole lower limb which is rarely used in clinical routine. Moreover, it will increase radiation exposure and cost a lot of time to complete the process of 3D reconstruction. Moreover, we found no automatic methods for clinical parameters calculation from 3D CT-scan models developed and applied for clinical routine use. Regarding the biplanar radiography, 3D lower limb reconstruction methods have been well developed. However, there is no study reported in the literature that uses 3D models from biplanar radiography for HKAA, LDFA, and MPTA calculation in patients with extra-articular deformity. Our study aimed to evaluate the validity and reliability of EOS 3D reconstruction in the clinical parameter calculation.
To the best of our knowledge, this is the first study to investigate the reliability of EOS 3D reconstruction system based goniometric application for measuring HKAA, LDFA, and MPTA in knee osteoarthritis and extra-articular deformity. The results showed that both the MG and the EOS exhibited excellent reliability over repeated measures of HKAA, LDFA, and MPTA, with a high concordance correlation coefficients (CCC). Our study found a fair degree of agreement between the EOS and MG over measures of LDFA and HKAA with high values of CCC. While for MPTA, the low value of CCC indicated poor agreement between the EOS and the MG.
When considering the use of the EOS and MG for measuring the value of HKAA, it's not hard to locate the center of the hip, and ankle joints. However, locating the center of the knee joint is the major challenge. Due to unexpected patient's rotating and/or bending while taking radiographs, it is hard to accurately locate the anatomical landmarks around the knee joint. Fig. 5B shows that the patient's rotation could cause deformation of the distal femur and proximal tibia on conventional 2D radiography. The deformation will certainly increase the difficulty to accurately locate the center of the distal femur and proximal tibia (Fig. 5C). Whereas, EOS 3D reconstruction could accurately locate the center of either hip, knee, or ankle joint based on three-dimensional localization algorithms, in spite of the influence of the patient's rotating and/or bending. However, the value of 1.96SD = 2.29° for the HKAA on the signed difference between MG and EOS measurements showed a minor influence of the patient's orientation on HKAA calculation. The linear regression model analysis also revealed a significant correlation between MG and EOS measurements for HKAA.
Figure 5.
(A) Conventional 2D X-rays of three candidates in the ‘DS’ standing position. (B–D) A detail view from ‘DS’ radiography showing mild (left), moderate (middle), and significant (right) deformation of the distal femur and proximal tibia. The deformation has a minor influence on locating the center of the distal femur and proximal tibia (C), and the joint line of the distal femur (D, upper joint line). However, the deformation significantly increases the difficulty to determine the joint line of the proximal tibia on 2D radiography (D, lower joint line).
When considering the use of the EOS and MG for measuring the value of LDFA and MPTA, the determination of the articular surface of the distal femur and proximal tibia is extremely important. It's usually not difficult to determine the joint line of the distal femur on 2D radiography (Fig. 5D, upper joint line). Fig. 3B showed a good correlation between EOS and MG measurements for LDFA. The value of 1.96SD = 1.81° (Fig. 4B) for the LDFA on the signed difference between EOS and MG measurements showed nearly no influence of the patient's orientation on LDFA calculation. However, the rotation and flexion of the knee joint make it hard to determine the articular surface of the proximal tibia. Fig. 5B and D showed that the deformation of proximal tibia significantly increases the difficulty to determine the joint line of the proximal tibia on 2D radiography (lower joint line). Whereas, EOS 3D reconstruction could build accurate 3D models and then accurately locate the joint line of the proximal tibia. Fig. 3C showed a poor correlation between EOS and MG measurements for MPTA. A low value of CCC (<0.75) and a high value of 1.96SD (4.36°, Fig. 4C) also indicated a poor agreement between EOS and MG measurements for MPTA. To further assess the reason of the differences in the measurement of MPTA, the validation of the EOS 3D-reconstruction model is of great concern. The shape accuracy of EOS 3D-reconstruction model has been validated by Y. Chaibi et al. [8] The EOS 3D-reconstruction models were compared with 3D CT-scan ones. The comparison between two models was made by calculating the distance between each point of the 3D model reconstructed with the EOS 3D-reconstruction method and the surface of the CT-scan corresponding model. The results showed mean difference of 1.0 mm (95% CI = 2.4 mm) between EOS 3D-reconstruction models and CT-scan ones. This result gave us great confidence on the validation of EOS 3D-reconstruction based angle measurements.
Finally, when considering the influence of shifted-foot standing position on EOS 3D reconstruction based goniometric measurements, it has been evidenced that weight-bearing status can affect malalignment measures [2,7]. In this study, all candidates were asked to position their right foot shifted backward to the left foot. In this situation, either a higher weight-bearing status could be noticed in the left lower limb, or a lower weight-bearing status could be noticed in the right lower limb. The influence of the changes of weight-bearing status on clinical parameter calculation was evidenced by the result of higher intra-rater reliability and agreement between EOS and MG measurements in the left lower limb when compared with that in the right low limb.
In conclusion, accurate evaluation of the deformity of the lower extremities is critical to preoperative planning before HTO and DFO. Using the EOS 3D reconstruction method, we were able to obtain an accurate lower limb shape and clinical measurements in a fast way and with excellent reproducibility. In comparison with the traditional 2D manual goniometer, EOS 3D reconstruction based goniometric measuring could provide equivalent results of HKAA and LDFA, and potentially a more accurate result of MPTA. These findings suggest that EOS 3D reconstruction based goniometric measuring is suitable for preoperative evaluation and planning for HTO/DFO. However, due to the limitation of the current 3D reconstruction method, it is still not able to complete 3D reconstruction based on radiography in the conventional double-stance full weight-bearing position. Future improvements of the 3D reconstruction method are needed for better detection of the femoral condyles and tibial plates without the requirement of the shifted-foot standing position.
Funding
This study was funded by the National Natural Science Foundation of China (81871789); the Natural Science Foundation of Jiangsu Province (BK20180052); Research and Development of Biomedical Materials and Substitution of Tissue and Organ Repair under National Key R&D Program (2016YFC1101505).
Ethical approval
This study received approval from the Ethics Committee and Institutional Review Board of the first-affiliated hospital of the Soochow University. Informed consent was obtained from all patients.
Conflict of Interest
The authors have no conflicts of interest to disclose in relation to this article.
Acknowledgement
The authors thank all candidates who participated in this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jot.2020.05.002.
Contributor Information
Zhigang Zhang, Email: zhangzhigang@suda.edu.cn.
Weidong Shi, Email: shiweidongsuzhou@163.com.
Jun Lin, Email: linjun@suda.edu.cn.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Specogna A.V., Birmingham T.B., Hunt M.A., Jones I.C., Jenkyn T.R., Fowler P.J. Radiographic measures of knee alignment in patients with varus gonarthrosis: effect of weightbearing status and associations with dynamic joint load. Am J Sports Med. 2007;35:65–70. doi: 10.1177/0363546506293024. [DOI] [PubMed] [Google Scholar]
- 2.Dugdale T.W., Noyes F.R., Styer D. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop. 1992:248–264. [PubMed] [Google Scholar]
- 3.Jiang C.C., Insall J.N. Effect of rotation on the axial alignment of the femur. Pitfalls in the use of femoral intramedullary guides in total knee arthroplasty. Clin Orthop. 1989:50–56. [PubMed] [Google Scholar]
- 4.Messmer P., Long G., Suhm N., Regazzoni P., Jacob A.L. Volumetric model determination of the tibia based on 2D radiographs using a 2D/3D database. Comput Aided Surg. 2001;6:183–194. doi: 10.3109/10929080109146082. [DOI] [PubMed] [Google Scholar]
- 5.Dong X., Zheng G. Automatic extraction of proximal femur contours from calibrated X-ray images using 3D statistical models: an in vitro study. Int J Med Robot Comput Assist Surg MRCAS. 2009;5:213–222. doi: 10.1002/rcs.253. [DOI] [PubMed] [Google Scholar]
- 6.Sato T., Koga Y., Omori G. Three-dimensional lower extremity alignment assessment system: application to evaluation of component position after total knee arthroplasty. J Arthroplasty. 2004;19:620–628. doi: 10.1016/j.arth.2003.12.063. [DOI] [PubMed] [Google Scholar]
- 7.Ogata K., Yoshii I., Kawamura H., Miura H., Arizono T., Sugioka Y. Standing radiographs cannot determine the correction in high tibial osteotomy. J Bone Joint Surg Br. 1991;73:927–931. doi: 10.1302/0301-620X.73B6.1955438. [DOI] [PubMed] [Google Scholar]
- 8.Chaibi Y., Cresson T., Aubert B., Hausselle J., Neyret P., Hauger O. Fast 3D reconstruction of the lower limb using a parametric model and statistical inferences and clinical measurements calculation from biplanar X-rays. Comput Methods Biomech Biomed Eng. 2012;15:457–466. doi: 10.1080/10255842.2010.540758. [DOI] [PubMed] [Google Scholar]
- 9.Dubousset J., Charpak G., Dorion I., Skalli W., Lavaste F., Deguise J. A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: the EOS system. Bull Acad Natl Med. 2005;189:287–297. discussion 297–300. [PubMed] [Google Scholar]
- 10.Kalifa G., Charpak Y., Maccia C., Fery-Lemonnier E., Bloch J., Boussard J.M. Evaluation of a new low-dose digital x-ray device: first dosimetric and clinical results in children. Pediatr Radiol. 1998;28:557–561. doi: 10.1007/s002470050413. [DOI] [PubMed] [Google Scholar]
- 11.Becker R., Kerkhoffs G.M.M.J., Gelber P.E., Denti M., Seil R., editors. ESSKA Instructional Course Lecture Book: Barcelona 2016. Springer-Verlag; Berlin Heidelberg: 2016. [DOI] [Google Scholar]
- 12.Lin L.I. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45:255–268. [PubMed] [Google Scholar]
- 13.Bland J.M., Altman D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet Lond Engl. 1986;1:307–310. [PubMed] [Google Scholar]
- 14.Kay R.M., Jaki K.A., Skaggs D.L. The effect of femoral rotation on the projected femoral neck-shaft angle. J Pediatr Orthop. 2000;20:736–739. doi: 10.1097/00004694-200011000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Kawakami H., Sugano N., Yonenobu K., Yoshikawa H., Ochi T., Hattori A. Effects of rotation on measurement of lower limb alignment for knee osteotomy. J Orthop Res Off Publ Orthop Res Soc. 2004;22:1248–1253. doi: 10.1016/j.orthres.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 16.Kim J.S., Park T.S., Park S.B., Kim J.S., Kim I.Y., Kim S.I. Measurement of femoral neck anteversion in 3D. Part 2: 3D modelling method. Med Biol Eng Comput. 2000;38:610–616. doi: 10.1007/bf02344865. [DOI] [PubMed] [Google Scholar]
- 17.Mahaisavariya B., Sitthiseripratip K., Tongdee T., Bohez E.L.J., Vander Sloten J., Oris P. Morphological study of the proximal femur: a new method of geometrical assessment using 3-dimensional reverse engineering. Med Eng Phys. 2002;24:617–622. doi: 10.1016/s1350-4533(02)00113-3. [DOI] [PubMed] [Google Scholar]
- 18.Subburaj K., Ravi B., Agarwal M. Computer-aided methods for assessing lower limb deformities in orthopaedic surgery planning. Comput Med Imaging Graph Off J Comput Med Imaging Soc. 2010;34:277–288. doi: 10.1016/j.compmedimag.2009.11.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.