Abstract
Spontaneous pneumomediastinum is a rare complication of viral pneumonia. Here we report a case of a 52 year old male who presented with a spontaneous pneumomediastinum in COVID-19 pneumonia, followed by a severe course of disease. We discuss the pathophysiological mechanisms underlying this association as well as its possible clinical implications as a marker of disease severity in COVID-19.
Keywords: COVID-19, SARS-CoV-2, Spontaneous pneumomediastinum
1. Introduction
Since December 2019, the COVID-19 pandemic has evolved into a worldwide public health crisis, with up to 13 million confirmed cases and more than 570,000 deaths as of 15 July 2020 [1]. Chest computed tomography (CT) has become an important instrument to diagnose COVID-19, but it is also used for severity stratification and monitoring of disease. COVID-19 causes typical radiographic features, including multifocal or peripherally distributed ground glass opacities with inter- or intralobular septal thickening (crazy paving appearance) [[2], [3], [4]]. Here we present a case of spontaneous pneumomediastinum in COVID-19 pneumonia, and discuss the possible mechanism underlying this association as well as clinical implications.
2. Case report
A 52 year old male adult without significant medical history presented to the Emergency Department (ED) with a seven-day history of fever, dyspnea and a dry cough. His symptoms aggravated during the past days. On arrival at the ED, he did not have a severely ill appearance, but his peripheral oxygen saturation was 85% on ambient air. Temperature was 38.6°C, blood pressure 131/65 mmHg and pulse rate 86 bpm.
Laboratory tests revealed an elevated C-reactive protein concentration of 198 mg/L (reference: < 5 mg/L). Complete blood count showed a leukocyte count of 8.0 × 109/L (reference: 4–10 × 109/L), with a relative left shift (9% band neutrophils [reference: < 5%]) and lymphopenia (5% [reference: 20–45%]). Serum levels of D-dimer and ferritin were both raised at 1082 μg/L (reference: < 500 μg/L) and 2636 μg/L (reference: 13–150 μg/L), respectively.
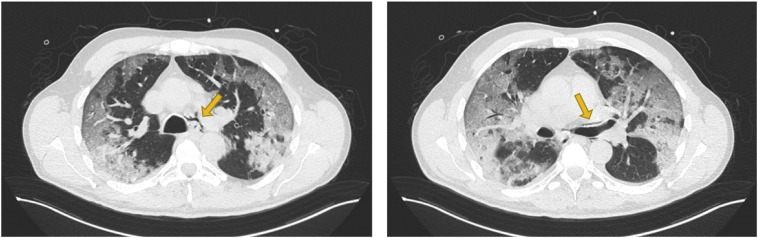
Non-contrast chest CT showed bilateral ground glass opacities and parenchymal consolidation. Furthermore, it revealed a small amount of mediastinal air with left-sided peribronchial distribution (Fig. 1 ). No subcutaneous emphysema or pneumothorax was observed. The suspicion of COVID-19 was confirmed by real-time reverse transcription polymerase chain reaction (RT-PCR) analysis of nasopharyngeal swab samples.
Fig. 1.
Chest CT obtained at presentation to the ED, demonstrating mediastinal air (left) with peribronchial distribution (right). Furthermore it shows bilateral ground glass opacities and parenchymal consolidation.
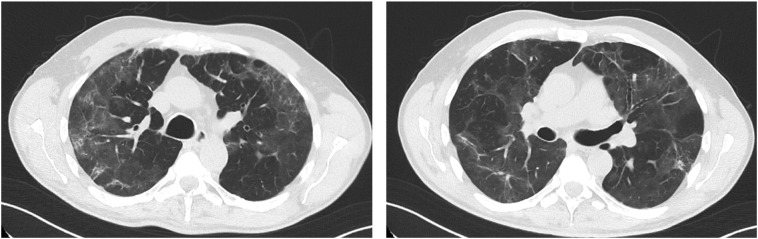
The patient was admitted to a designated COVID-19 ward and treated with broad-spectrum antibiotics and chloroquine. Three days later he developed respiratory failure and was transferred to the Intensive Care Unit for mechanical ventilation. He was ventilated for 26 days, and after five more weeks of medical rehabilitation he was discharged home. Follow-up chest CT obtained 14 weeks after initial presentation showed complete resorption of mediastinal air (Fig. 2 ).
Fig. 2.
Follow-up chest CT obtained 14 weeks after initial presentation showing complete resorption of mediastinal air.
3. Discussion
Spontaneous pneumomediastinum is a rare complication of viral pneumonia. It has been reported in severe acute respiratory syndrome (SARS) virus infections, influenza and bacterial pneumonia with rare strains, such as P. jirovecii in immunocompromised patients [[5], [6], [7]]. Spontaneous pneumomediastinum associated with COVID-19 has occasionally been reported [[8], [9], [10]].
The presumed etiology is that the viral infection causes diffuse alveolar damage, which together with an increase in intra-alveolar pressure (as seen in intentional Valsalva maneuver, such as coughing) leads to alveolar rupture. Subsequently, this alveolar air circulates through the bronchovascular sheaths towards the mediastinum, following a negative pressure gradient. This pathophysiological mechanism is known as the Macklin effect [11].
Although spontaneous pneumomediastinum is generally considered a benign and self-limiting condition, its appearance in viral pneumonia may be of clinical significance as it has been previously suggested to be a potential indicator of disease severity. For instance, in SARS patients it was observed that the development of a spontaneous pneumomediastinum was associated with significantly higher rates of intubation and mortality [12]. Furthermore, a recent case series described three cases of COVID-19 pneumonia that were complicated by spontaneous pneumomediastinum and pneumothorax, all of which were followed by a severe course of disease with fatal outcome [13]. Although in our patient presentation with a spontaneous pneumomediastinum was associated with a severe course of COVID-19 pneumonia as well, it is yet unclear to what extend this applies to other patients with COVID-19 infection. In this context, it should be noted that in retrospective analysis selection bias might occur, assuming that in more severe cases more imaging studies are performed. Therefore, further research is warranted to assess whether spontaneous pneumomediastinum is an indicator of disease severity in COVID-19 pneumonia.
4. Conclusion
Spontaneous pneumomediastinum is a rare complication of COVID-19 pneumonia and was associated with a severe course of disease in our patient. Future studies are warranted to assess whether spontaneous pneumomediastinum is an indicator of disease severity in COVID-19 pneumonia.
Declaration of Competing Interest
The authors have no conflicts of interest relevant to this article to disclose.
References
- 1.World Health Organization Coronavirus Disease (COVID-19) 2020. https://covid19.who.int [accessed 16 July 2020]
- 2.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020;200642 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung M., Bernheim A., Mei X., Zhang N., Huang M., Zeng X. CT imaging features of 2019 novel coronavirus (2019-nCoV) Radiology. 2020;295(1):202–207. doi: 10.1148/radiol.2020200230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li Y., Xia L. Coronavirus disease 2019 (COVID-19): role of chest CT in diagnosis and management. AJR Am J Roentgenol. 2020;214(6):1280–1286. doi: 10.2214/ajr.20.22954. [DOI] [PubMed] [Google Scholar]
- 5.Chekkoth S.M., Supreeth R.N., Valsala N., Kumar P., Raja R.S. Spontaneous pneumomediastinum in H1N1 infection: uncommon complication of a common infection. J R Coll Physicians Edinb. 2019;49(4):298–300. doi: 10.4997/jrcpe.2019.409. [DOI] [PubMed] [Google Scholar]
- 6.Kaji Y., Ohara G., Kagohashi K., Satoh H. Pneumomediastinum in a patient with Pneumocystis jirovecii pneumonia. Intern Med. 2012;51(16):2251. doi: 10.2169/internalmedicine.51.8134. [DOI] [PubMed] [Google Scholar]
- 7.Peiris J.S., Chu C.M., Cheng V.C., Chan K.S., Hung I.F., Poon L.L. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. Lancet. 2003;361(9371):1767–1772. doi: 10.1016/s0140-6736(03)13412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kolani S., Nawfal H., Haloua M., Lamrani Y.A., Boubbou M., Serraj M. Spontaneous pneumomediastinum occurring in the SARS-COV-2 infection. IDCases. 2020;21 doi: 10.1016/j.idcr.2020.e00806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sun R., Liu H., Wang X. Mediastinal emphysema, Giant Bulla, and pneumothorax developed during the course of COVID-19 pneumonia. Korean J Radiol. 2020;21(5):541–544. doi: 10.3348/kjr.2020.0180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou C., Gao C., Xie Y., Xu M. COVID-19 with spontaneous pneumomediastinum. Lancet Infect Dis. 2020;20(4):510. doi: 10.1016/s1473-3099(20)30156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Macklin M.T., Macklin C.C. Malignant interstitial emphysema of the lungs and mediastinum as an important occult complication in many respiratory diseases and other conditions: interpretation of the clinical literature in the light of laboratory experiment. Medicine. 1944;23(4):281–358. [Google Scholar]
- 12.Chu C.M., Leung Y.Y., Hui J.Y., Hung I.F., Chan V.L., Leung W.S. Spontaneous pneumomediastinum in patients with severe acute respiratory syndrome. Eur Respir J. 2004;23(6):802–804. doi: 10.1183/09031936.04.00096404. [DOI] [PubMed] [Google Scholar]
- 13.López Vega J.M., Parra Gordo M.L., Diez Tascón A., Ossaba Vélez S. Pneumomediastinum and spontaneous pneumothorax as an extrapulmonary complication of COVID-19 disease. Emerg Radiol. 2020:1–4. doi: 10.1007/s10140-020-01806-0. [DOI] [PMC free article] [PubMed] [Google Scholar]