Abstract
Objectives
To present our center's experience in the management of adrenal myelolipoma in the context of shifting from the open to the laparoscopic adrenalectomy approach.
Materials and Methods
A retrospective search of our center's records was done for reported cases of adrenal myelolipoma during the period July 2001-June 2016. All the cases with histopathologically-documented adrenal myelolipoma diagnosis were included. Relevant demographic and clinical variables were studied with a comparison between the open and laparoscopic approaches.
Results
Of more than 82,000 urological surgeries, 238 adrenalectomies were done with only 22 cases of myelolipoma that had a mean age and body mass index of 52.4 ± 10.3 years and 30.23 kg/m2, respectively. The main clinical presentation was accidental discovery. The largest dimension of tumors varied from 6 to 16 cm. Computed tomography described a characteristic picture of hypodense heterogeneous adrenal tumors in all cases, while magnetic resonance imaging was indicated for malignancy suspicion in only 5 cases. Adrenal tumor markers were normal in all cases. Open and transperitoneal laparoscopic adrenalectomies were used in 14 and 8 cases, respectively. The latter approach was insignificantly advantageous in the need for blood transfusion, postoperative pain degree, need for analgesia, and hospital stay duration (p = 0.22). Histo-pathological examination revealed benign adipose tissue and myeloid cells and confirmed the diagnosis of adrenal myelolipoma in all cases.
Conclusions
Adrenal myelolipoma is a rare non-functioning benign tumor. Laparoscopic excision seems to be a promising alternative approach to the traditional open adrenalectomy, even in the context of large tumors and obesity.
Keywords: Adrenal gland, Adrenal myelolipoma, Incidentaloma, Laparoscopic adrenalectomy, Open adrenalectomy
Introduction
Adrenal tumors are rare entities that have an incidence of 1.4-9% at autopsy and 0.6-1.3% on abdominal computed tomography (CT) studies [1]. However, even though they represent a small proportion of urological tumors, this is enough to potentiate the non-familiar state among most urologists, in spite of their efficiency in retroperitoneal surgeries [2]. Following the increased use of imaging modalities such as ultrasonography, CT, and magnetic resonance imaging (MRI) in medical practice, the incidence of unexpected pathological masses has increased. An adrenal mass is one of the most commonly unexpected imaging-diagnosed masses. The term “incidental adrenal mass” or “adrenal incidentaloma” was designated [1]. Adrenal tumors can be classified into cortical tumors such as adenoma, carcinoma, and hyperplasia, and medullary tumors such as pheochromocytoma, neuroblastoma, and other very rare masses including myelolipoma, which is a contributing tumor to adrenal incidentaloma as its common clinical presentation [3]. The term “myelolipoma” was coined by Oberling in 1929 after it was first described in the literature by Giercke in 1905 [4]. Adrenal myelolipoma is composed of mature adipose tissues and hematopoietic cells. Its incidence jumped from 0.08-0.2% to 10-15% of all adrenal tumors in the last 2 decades. However, its etiology is still unknown [5]. As commonly being an asymptomatic tumor with accidental discovery and markedly variable sizes, few cases have been reported with biochemical functions [6]. It has been commonly reported in case reports, with a limited number of case series published in the last 2 decades [7,8,9]. The study of adrenal myelolipoma is still interesting in regards to the increasing incidence, etiology, and treatment approaches. Here, we represent our center's experience with adrenal myelolipoma in the context of a relatively large case series of this rare tumor and the shift of treatment from traditional open adrenalectomy (OA) to laparoscopic adrenalectomy (LA).
Materials and Methods
A retrospective search of the patients' records (manual and electronic files) in our hospital was done for cases of adrenalectomy for adrenal myelolipoma in the period July 2001-June 2016. In this study, we included only patients who had adrenal myelolipoma documented by histopathological diagnosis. Cases without histopathological diagnosis or those cases which were managed conservatively were excluded. Each involved case was studied for the demographic variables (age and gender) and clinical variables including clinical presentation, diagnostic methods, management approaches (OA or LA), indications for surgery, complications, and final outcomes.
A comparison was done between the OA and LA approaches for myelolipoma. Tumor size, operative time, intraoperative complications, blood transfusion, wounds, needs for analgesia, and the duration of hospitalization were compared.
Results
Of more than 82,000 urological procedures and interventions that were done in our hospital during the period July 2001-June 2016, 238 cases (0.29%) of adrenal tumors were operated on including 22 cases of adrenal myelolipoma representing 0.026% of the total urological procedures and 9.24% of all the adrenal tumor procedures.
Demographic data are presented in Table 1. Patients' mean age was 52.4 ± 10.3 years. Clinical presentations included dull aching loin pain in 8 cases, accidental discovery in 12 cases, and co-existing hypertension in 2 cases. Most of the patients were obese with a mean body mass index of 30.23 kg/m2
Table 1.
Demographic and clinical characteristics of the patients with adrenal myelolipoma
| Patienta | Age, year | Gender | Complaint | BMI, kg/m2 | Blood pressure | Imaging | HU value | Mass dimensions, cm |
|---|---|---|---|---|---|---|---|---|
| 1 | 56 | male | accidental discovery | 29.39 | normal | CT | −30 to −40 | 10 × 9 × 7.4 |
| 2 | 48 | female | loin pain | 27.44 | normal | CT | −20 to −50 | 12 × 10 × 8.5 |
| 3 | 68 | female | hypertension | 33.60 | high, mild | CT | −15 to −35 | 6 × 6 × 5 |
| 4 | 55 | male | loin pain | NA | normal | CT | NA | 8 × 7 × 5.5 |
| 5 | 62 | female | accidental discovery | 29.41 | normal | CT | −25 to −40 | 11.5 × 9.5 × 6.8 |
| 6 | 47 | female | accidental discovery | 30.85 | normal | CT | −20 to −30 | 7.6 × 7 × 5 |
| 7 | 40 | male | loin pain | 26.64 | normal | CT | −15 to −35 | 9 × 8.8 × 7.3 |
| 8 | 63 | female | accidental discovery | 29.33 | normal | CT | −25 to −50 | 14 × 12 × 11.5 |
| 9 | 53 | male | hypertension | 34.42 | high, mild | CT | −30 to −40 | 8.5 × 6.6 × 5.5 |
| 10 | 44 | female | accidental discovery | 30.45 | normal | CT | −25 to −35 | 15 × 13 × 11.7 |
| 11 | 33 | female | loin pain | 37.37 | normal | CT | −20 to −35 | 13 × 11 × 9.6 |
| 12 | 59 | female | accidental discovery | 31.64 | normal | CT | −30 to −40 | 8.5 × 5.5 × 5 |
| 13 | 46 | female | abdominal pain | NA | normal | CT | −25 to −40 | 9.5 × 7.8 × 6 |
| 14 | 66 | male | loin pain | 30.80 | normal | CT | −20 to −45 | 8 × 7 × 7 |
| 15 | 45 | female | accidental discovery | 29.64 | normal | CT | −20 to −35 | 10 × 9 × 8 |
| 16 | 73 | female | loin pain | 25.71 | normal | CT, MRI | −15 to −52 | 7.8 × 6.5 × 5 |
| 17 | 58 | male | accidental discovery | 22.84 | normal | CT, MRI | −20 to −45 | 6.8 × 6.5 × 4 |
| 18 | 49 | female | accidental discovery | 31.22 | normal | CT | −18 to −35 | 7.5 × 7 × 5 |
| 19 | 57 | male | accidental discovery | 27.72 | normal | CT, MRI | −25 to −45 | 9 × 8.5 × 7.6 |
| 20 | 38 | male | loin pain | 32.80 | normal | CT, MRI | −20 to −40 | 8 × 6 × 4 |
| 21 | 45 | male | accidental discovery | 34.64 | normal | CT, MRI | −20 to −30 | 16 × 14 × 8 |
| 22 | 47 | female | loin pain | 28.60 | normal | CT | −15 to −30 | 12 × 12 × 10.5 |
BMI = Body mass index; NA = no available data
Patients were ordered in a chronological manner.
Laboratory work-up included tests of urinary amphetamines, vanillylmandelic acid, and serum cortisol levels and were within normal values in all cases. Other routine and surgical fitness work-up tests were unremarkable or irrelevant to the tumors.
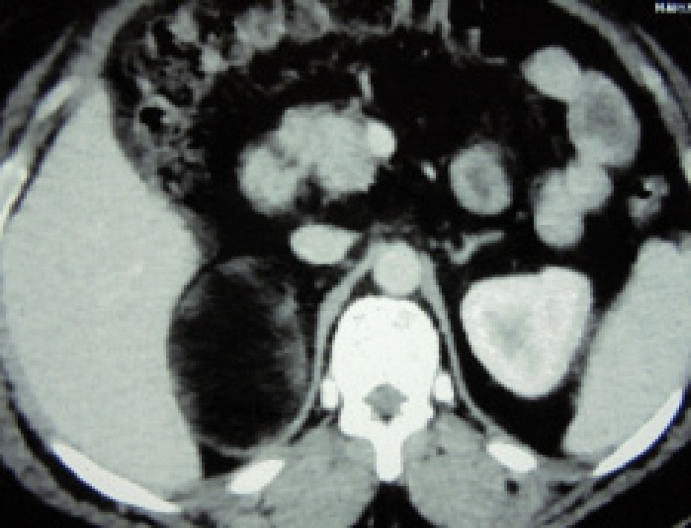
Basic imaging investigations including abdominal ultrasonography and abdominal radiographs were done for all patients. Enhanced CT was done in the 22 cases and described a well-demarcated mass with heterogeneous appearance (Fig. 1). Dimensions of the masses were larger than 6 cm (Table 1). The Hounsfield unit (HU) was ≤ −15. Indication of MRI in 5 patients was the exclusion of suspicion for malignancy. The anatomical position of the adrenal masses was the right side in 17 cases versus 5 cases in the left side.
Fig. 1.
Abdominal CT (axial cut): Large right adrenal mass with more or less heterogeneous low-attenuated or hypodense appearance and well-demarcated borders from the surroundings.
Indications of surgical intervention included large size (> 6 cm) in 10 cases and large size with loin pain in 8 cases or with inferior vena cava (IVC) compression in 4 cases. General anesthesia was employed in the 22 cases and precautions of undiscovered functioning adrenal tumor possibilities were considered during all surgeries.
Surgical approaches were OA in 14 cases and LA in 8 cases (Table 2). In the OA group, the approach was a thoracolumbar incision with opening of the diaphragm and its repair or subcostal transperitoneal incision, where the operative time range was 170-225 minutes. In addition to being a major surgery, intraoperative complications included hemorrhage due to avulsion of a lumbar vein in 1 case and splenectomy in another case. Blood loss range was 300-1,100 ml. All the patients had blood transfusions of up to 3 units of blood in one of them. Postoperative complications included 2 cases of intestinal obstruction which were conservatively managed and 1 case of gross wound infection. Otherwise, convalescence was smooth and uneventful in the other patients.
Table 2.
Operative, perioperative, and postoperative findings for adrenal myelolipoma
| Patienta | Operative technique | Skin incision, approach | Intraoperative difficulties | Blood transfusion, bags | Operative time, minutes | Hospital stay, day | Convalescence |
|---|---|---|---|---|---|---|---|
| 1 | open | thoracolumbar | major surgery | 2 | 220 | 7 | uneventful |
| 2 | open | subcostal, transperitoneal | hemorrhage, lumbar vein | 3 | 200 | 8 | uneventful |
| 3 | open | thoracolumbar | major surgery | 2 | 210 | 8 | uneventful |
| 4 | open | subcostal, transperitoneal | major surgery | 2 | 185 | 9 | uneventful |
| 5 | open | subcostal, transperitoneal | major surgery | 2 | 225 | 6 | intestinal obstruction |
| 6 | open | thoracolumbar | hemorrhage, splenic | 2 | 210 | 7 | uneventful |
| 7 | open | thoracolumbar | major surgery | 2 | 200 | NA | uneventful |
| 8 | open | thoracolumbar | major surgery | 1 | 180 | 6 | uneventful |
| 9 | open | subcostal, transperitoneal | major surgery | 2 | 170 | 7 | wound infection |
| 10 | open | thoracolumbar | major surgery | 2 | 205 | 9 | uneventful |
| 11 | open | subcostal, transperitoneal | major surgery | 1 | 175 | 6 | uneventful |
| 12 | laparoscopic | 5 ports | challenges of first case | 1 | 220 | 4 | uneventful |
| 13 | laparoscopic | 5 ports | none | none | 210 | 4 | uneventful |
| 14 | laparoscopic | 5 ports | none | none | 180 | 4 | uneventful |
| 15 | laparoscopic | 5 ports | circumcaval dissection | 2 | 225 | 5 | uneventful |
| 16 | laparoscopic | 5 ports | circumcaval dissection | 1 | 230 | 5 | uneventful |
| 17 | laparoscopic | 5 ports | none | none | 190 | 3 | uneventful |
| 18 | open | subcostal, transperitoneal | none | 2 | 190 | 7 | uneventful |
| 19 | open | subcostal, transperitoneal | none | 2 | 180 | 8 | intestinal obstruction |
| 20 | laparoscopic | 5 ports | sub-hepatic dissection | 1 | 120 | 4 | uneventful |
| 21 | laparoscopic | 5 ports | sub-hepatic dissection | none | 225 | 3 | uneventful |
| 22 | open | subcostal, transperitoneal | none | 2 | 210 | 7 | uneventful |
NA = No available data
Patients were listed and ordered in a chronological manner.
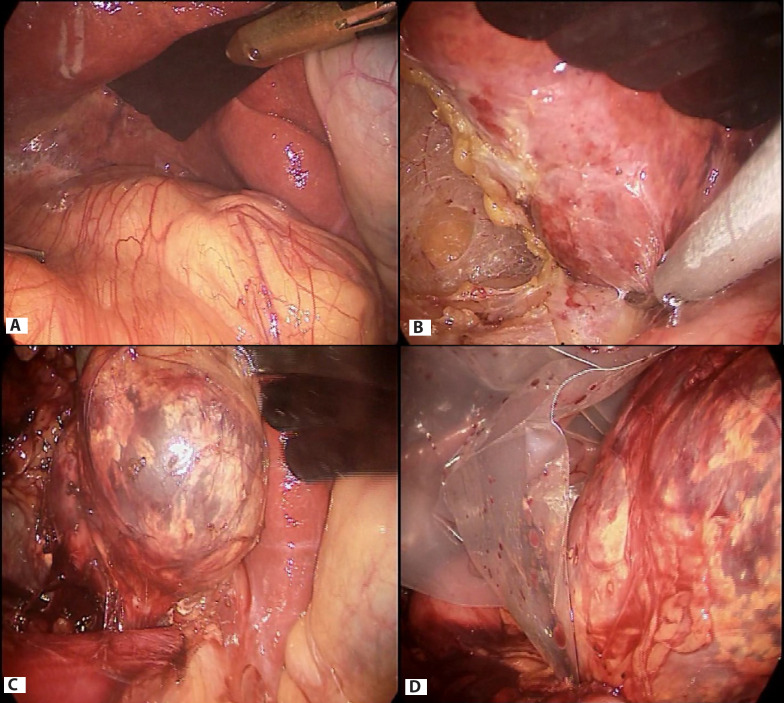
LA was used in 9 cases of the last 11 chronological cases (Table 2). The transperitoneal approach was used through 5 ports in all cases as it was previously described [10]. A demanding surgical dissection was encountered in 4 cases because of large sizes (Fig. 2). The mean operative time was relatively satisfying with a successful LA procedure in 8 cases and conversion to OA in only 1 case. Blood loss ranged as 100-250 ml and blood transfusion was done in 4 cases. In comparison to the OA, the LA approach was insignificantly advantageous in many variables (Table 3).
Fig. 2.
Intraoperative laparoscopic anatomy of a giant right adrenal myelolipoma and surrounding structures (A). Demanding dissection of the mass at the sub-hepatic area (B) and from the IVC (C), and the giant size of the mass before retrieval (D) can be noted.
Table 3.
A comparison between open and laparoscopic adrenalectomy for myelolipoma
| OA | LA | p* | |
|---|---|---|---|
| Number of patients, n | 14 | 8 | |
| Mean operative time, minutes | 197.14 ± 17.29 | 210 ± 18.32 | 0.59 |
| Intraoperative hemorrhage | 2 cases | none | |
| Blood transfusion, bags | all cases: 2–3 bags | 50% of cases: 0–2 bags | |
| Hospital stay, day | 7.31 ± 1.03 | 4 ± 0.76 | 0.22 |
| Postoperative pain and analgesiaa | severe, 1–3 drugs for 5–7 d | mild to moderate, 1 drug for 1–2 d |
p is significant when it is < 0.05
Severity of pain was measured according to the pain scale.
Histopathological examination was the confirmatory tool for diagnosis of adrenal myelolipoma in all 22 cases. Typically, it described benign mature adipose tissues and the 3 hematopoietic (myeloid) elements including megakaryocytes (Fig. 3).
Fig. 3.
Microscopic (histopathological) picture of adrenal myelolipoma. A, B Sections of the adrenal myelolipoma showing the two main components of the tumor, mature adipose tissue and myeloid cells (× 400); C, D Higher magnification power shows fat cells and all three lineages of hematopoietic marrow including megakaryocytes (× 1,000).
Postoperative follow-up of patients ranged from 10 to 60 months. No unexpected findings (such as recurrences) were reported in the records of the 17 patients who had postoperative follow-up records.
Discussion
Adrenal myelolipoma is one of the contributing lesions to the commonly used term “adrenal incidentaloma” that warrants a multidisciplinary approach for diagnosis and management [11]. It is a mesenchymal benign tumor composed of mature adipose tissue and 3 lineages of myeloid cells [10], hence its name was designed. Its pathogenesis has been studied through many postulated theories including the proposed hormonal tumorigenesis, but without a solid consensus [5,12].
The incidence of adrenal myelolipoma has been changed recently among all the adrenal tumors. This change in the incidence followed the increased rate of diagnosis in attribution to vivid pathological awareness and well-developed modern imaging techniques [5]. Most of our cases were discovered initially by ultrasound or CT that was requested for other purposes. Adrenal myelolipoma is commonly a unilateral lesion with comparable incidences between the right and left sides and it is rarely bilateral [13,14]. Our results fairly correlated with previous findings, where all the tumors were unilateral, but with more predilection to the right side. Autopsy diagnosis was the common form in the old eras [5]. However, the common clinical presentation is the accidental discovery of an asymptomatic adrenal mass [15,16]. Occasionally, however, loin or abdominal pain, hypertension, and other biochemically-active tumor manifestations have been reported [6,15]. All the lesions in the current study were > 6 cm. Smaller lesions were mostly managed conservatively without histopathological confirmation, where they were excluded according to the patient selection criteria of this study.
Although pure adrenal myelolipomas are hormonally inactive, there have been occasionally reported associations with functioning adrenal disorders such as adrenal hyperplasia and Cushing's and Conn's syndromes [12,13]. This clinical association may involve adrenal myelolipoma in the functioning tumor presentations [14]. Hypertension has rarely been attributed to functioning adrenal myelolipoma [6]. However, all cases in the current study had no functional manifestations in the clinical or laboratory presentations. The 2 cases that presented with hypertension had unremarkable laboratory tests excluding the causality between this lesion and hypertension. Also, the current cases had no associations to other adrenal hormonally-active syndromes. So, we are still able to consider adrenal myelolipoma as a non-functioning tumor in correlation with the main attitude of the literature towards this issue [17].
Adrenal myelolipoma has a characteristic picture in CT. Its fat contents give it a low attenuation appearance with HU < −20, making the need of further imaging unnecessary in most of the instances [3]. Our cases had HU between −52 and −15. Recently developed advances in the diagnostic capabilities of MRI evoked the rationale of examining the utility of diffusion-weighted MRI technology in adrenal tumors including lipid-rich lesions similar to our rationale in the cases that had suspicion of malignancy. However, it may not be useful to differentiate between the benign and malignant natures of the adrenal lesions, in spite of its theoretical proposal [18,19].
Adrenal gland surgeries represent one of the surgical difficulties due its location in the retroperitoneum related to the upper pole and medial border of the kidneys. Among abdominal surgeons, urologists seem to be, relatively more familiar and efficient than general surgeons in dealing with and surgically managing adrenal tumors [2]. Although it may indicate highly-trained urologists and some technical adjustments, the practice seems to be a possible target. Classic treatment recommends small-sized lesions for conservation. However, large-sized or symptomatic lesions are subjects to surgery, where OA has been the standard approach, especially with enormously large tumors [5,20]. In the latter decades, however, laparoscopic excision has been successfully introduced for the treatment of adrenal myelolipoma, even in the cases of large or giant masses and in obese patients [9,10,21]. The laparoscopic approach has the advantages of minimally-invasive surgery. However, it may have some technical demands and high laparoscopic experiences [10]. Regarding the results of the current study, we report that the recent introduction of laparoscopy in the management of adrenal tumors including myelolipoma is a progressively successful strategy. It is our trend nowadays to employ minimally-invasive surgical techniques for the management of urological disorders in all the subspecialties including uro-oncology. This approach may result in minimization of surgical complications and postoperative needs for analgesia and medications, avoidance of generous wound hazards, and shortening of convalescence [8].
Risk factors for conversion of LA to OA include a tumor size of more than 8 cm [8]. In our cases, we considered the ≥ 6 cm tumor size as an indication for surgery, especially with symptoms or compressions of vital structures such as the IVC. In addition, the size of the tumor was variably large including giant sizes up to 16 cm with successful laparoscopic excision. However, this approach may be a technically demanding one, even with the availability of expert urologists in laparoscopy, due to the challenging surgical dissections as what we encountered. In the literature, a few case series studied LA for adrenal myelolipoma and less commonly its comparison to OA [4,9].
This article just represents the experience of a single urology center in the context of the little knowledge available from other corresponding large-volume urological centers in our country [7]. However, this study could be the motivator for similar researches that contribute to the improvement of healthcare by updating the surgical techniques towards novel strategies. Also, we strongly recommend national multi-center studies for evaluation of rare urological entities including rare urogenital tumors to help in establishing solid bases for the management of these rare disorders.
Conclusions
Adrenal myelolipoma is a very rare benign tumor of variable size. It is commonly an asymptomatic tumor that presents mainly as an incidentaloma. Its diagnosis is strongly suggested via the classic picture on CT as low-attenuated hypodense heterogeneous lesions. Histo-pathologically, it is composed of mature adipose tissue and myeloid cells. In spite of the surgical challenges, trials of replacing the traditional OA by the LA appear to be promising and successful, even when there are large-sized tumors and obese patients.
References
- 1.Arnold DT, Reed JB, Burt K. Evaluation and management of the incidental adrenal mass. Proc (Bayl Univ Med Cent) 2003;16:7–12. doi: 10.1080/08998280.2003.11927882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fergany AF. Adrenal masses: a urological perspective. Arab J Urol. 2016;14:248–255. doi: 10.1016/j.aju.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oliveira Caiafa R, Salvador Izquierdo R, Bunesch Villalba L, Sebastià Cerqueda MC, Nicolau Molina., C Diagnosis and management of adrenal incidentaloma. Radiologia. 2011;53:516–530. doi: 10.1016/j.rx.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 4.Castillo OA, Vitagliano G, Cortes O, Sánchez-Salas R, Arellano L. Laparoscopic adrenalectomy for adrenal myelolipoma. Arch Esp Urol. 2007;60:217–221. doi: 10.4321/s0004-06142007000200022. [DOI] [PubMed] [Google Scholar]
- 5.Ramirez M, Misra S. Adrenal myelolipoma: to operate or not? A case report and review of the literature. Int J Surg Case Rep. 2014;8:494–496. doi: 10.1016/j.ijscr.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jakka N, Venkateshwarlu J, Satyavani N, Neelaveni K, Ramesh J. Functioning adrenal myelolipoma: a rare cause of hypertension. Indian J Endocrinol Metab. 2013;17((suppl 1)):S249–S251. doi: 10.4103/2230-8210.119588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Mekresh MM, Abdel-Gawad M, El-Diasty T, El-Baz M, Ghoneim MA. Clinical, radiological and histological features of adrenal myelolipoma: review and experience with a further eight cases. Br J Urol. 1996;78:345–350. doi: 10.1046/j.1464-410x.1996.00081.x. [DOI] [PubMed] [Google Scholar]
- 8.Gershuni VM, Bittner JG, 4th, Moley JF, Brunt LM. Adrenal myelolipoma: operative indications and outcomes. J Laparoendosc Adv Surg Tech A. 2014;24:8–12. doi: 10.1089/lap.2013.0411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamashita S, Ito K, Furushima k, Fukushima J, Kameyama S, Harihara Y. Laparoscopic versus open adrenalectomy for adrenal myelolipoma. Ann Med Surg (Lond) 2014;3:34–38. doi: 10.1016/j.amsu.2014.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gadelkareem RA, Khalil MM, Mohammed N, Makboul R, Badary FA. Laparoscopic excision of a large symptomatic and kidney-displacing adrenal myelolipoma: a case report. Afr J Urol. 2018;24:63–66. [Google Scholar]
- 11.Barzon L, Boscaro M. Diagnosis and management of adrenal incidentalomas. J Urol. 2000;163:398–407. [PubMed] [Google Scholar]
- 12.Chakraborty PP, Bhattacharjee R, Mukhopadhyay P, Chowdhury S. Bilateral adrenal myelolipoma in Cushing's disease: a relook into the role of corticotropin in adrenal tumourigenesis. BMJ Case Rep. 2016;2016:bcr2016214965. doi: 10.1136/bcr-2016-214965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Bahri S, Tariq A, Lowentritt B, Nasrallah DV. Giant bilateral adrenal myelolipoma with congenital adrenal hyperplasia. Case Rep Surg. 2014;2014:728198. doi: 10.1155/2014/728198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kale G, Pelley EM, Davis DB. Giant myelolipomas and inadvertent bilateral adrenalectomy in classic congenital adrenal hyperplasia. Endocrinol Diabetes Metab Case Rep. 2015;2015:150079. doi: 10.1530/EDM-15-0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wani NA, Kosar T, Rawa IA, Qayum A. Giant adrenal myelolipoma: incidentaloma with a rare incidental association. Urol Ann. 2010;2:130–133. doi: 10.4103/0974-7796.68865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Doddi S, Singhal T, Leake T, Sinha P. Management of an incidentally found large adrenal myelolipoma: a case report. Cases J. 2009;2:8414. doi: 10.4076/1757-1626-2-8414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Decmann A, Perge P, Toth M, Igaz P. Adrenal myelolipoma: a comprehensive review. Endocrine. 2018;59:7–15. doi: 10.1007/s12020-017-1473-4. [DOI] [PubMed] [Google Scholar]
- 18.Miller FH, Wang Y, McCarthy RJ, Yaghmai V, Merrick L, Larson A, Berggruen S, Casalino DD, Nikolaidis P. Utility of diffusion-weighted MRI in characterization of adrenal lesions. AJR Am J Roentgenol. 2010;194:W179–W185. doi: 10.2214/AJR.09.2891. [DOI] [PubMed] [Google Scholar]
- 19.El-Kalioubie M, Emad-Eldin S, Abdelaziz O. Diffusion-weighted MRI in adrenal lesions: a warranted adjunct? Egyp J Radiol Nucl Med. 2016;47:599–606. [Google Scholar]
- 20.Akamatsu H, Koseki M, Nakaba H, Sunada S, Ito A, Teramoto S, Miyata M. Giant adrenal myelolipoma: report of a case. Surg Today. 2004;34:283–285. doi: 10.1007/s00595-003-2682-4. [DOI] [PubMed] [Google Scholar]
- 21.Maestroni U, Ferretti S, Ziglioli F, Campobasso D, Cerasi D, Cortellini P. Laparoscopic adrenalectomy in giant masses. Urologia. 2011;78((suppl 18)):S54–S58. doi: 10.5301/RU.2011.8776. [DOI] [PubMed] [Google Scholar]