Abstract
Rationale & Objective
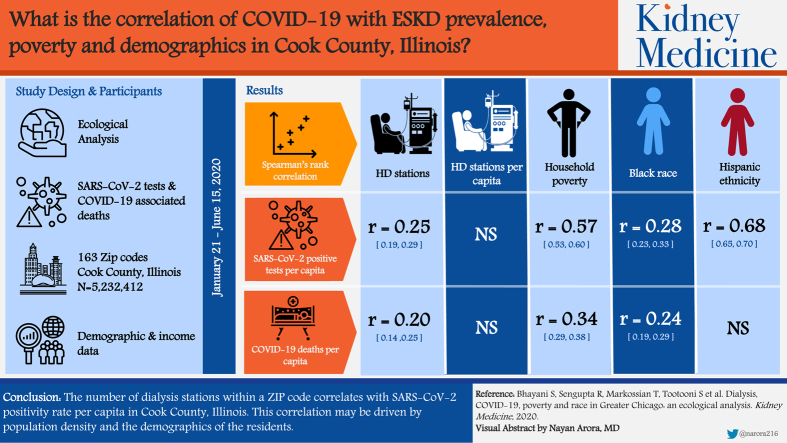
Persons with end-stage kidney disease receiving in-center maintenance hemodialysis may be at high risk for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) exposure and severe outcomes with coronavirus disease 2019 (COVID-19). The objective of this study was to examine the correlation of SARS-CoV-2 positivity rate per capita and COVID-19–associated deaths with number of dialysis stations and demographics of residents within zip codes in Cook County, IL.
Study Design
Ecological analysis.
Setting & Participants
Data for SARS-CoV-2 test results and COVID-19–associated deaths during January 21 to June 15, 2020, among the 5,232,412 residents living within the 163 zip codes in Cook County, IL, were merged with demographic and income data from the US Census Bureau. The total number of positive test results in this population was 84,353 and total number of deaths was 4,007.
Assessments
Number of dialysis stations and stations per capita within a zip code were calculated. SARS-CoV-2–positive test results per capita were calculated as number of positive test results divided by the zip code population. COVID-19–associated deaths per capita were calculated as COVID-19 deaths among residents for a given zip code divided by the zip code population.
Analytic Approach
Spearman rank correlation coefficients were calculated to examine the correlation of SARS-CoV-2–positive tests per capita and COVID-19–associated deaths per capita with dialysis stations, demographics, and household poverty. To account for multiple testing, statistical significance was considered as P < 0.005.
Results
Among the 163 Cook County zip codes, there were 2,501 dialysis stations. Positive test results per capita were significantly associated with number of dialysis stations (r = 0.25; 95% CI, 0.19 to 0.29; P < 0.005) but not with dialysis stations per capita (r = 0.02; 95% CI, −0.03 to 0.08; P = 0.7). Positive test results per capita also correlated significantly with number of households living in poverty (r = 0.57; 95% CI, 0.53-0.6; P < 0.005) and percentage of residents reporting Black race (r = 0.28; 95% CI, 0.23-0.33; P < 0.005) and Hispanic ethnicity (r = 0.68; 95% CI, 0.65-0.7; P < 0.001;). COVID-19–associated deaths per capita correlated significantly with the percentage of residents reporting Black race (r = 0.24; 95% CI, 0.19-0.29; P < 0.005) and with percentage of households living in poverty (r = 0.34; 95% CI, 0.29-0.38; P < 0.005). The association between the number of COVID-19–associated deaths per capita and total number of dialysis stations (r = 0.20; 95% CI, 0.14-0.25; P = 0.01) did not achieve a priori significance, whereas the association with dialysis stations per capita (r = 0.12; 95% CI, 0.07-0.17; P = 0.01) was not significant.
Limitations
Analysis is at the zip code level and not at the person level.
Conclusions
The number of dialysis stations within a zip code correlates with the SARS-CoV-2 positivity rate per capita in Cook County, IL, and this correlation may be driven by population density and the demographics of the residents. These findings highlight the high risk of SARS-CoV-2 exposure for patients with end-stage kidney disease living in poor urban areas.
Index Words: COVID-19, dialysis, poverty, race, SARS-CoV-2, disparities
Graphical abstract
Plain-Language Summary.
This ecological analysis examined the correlations between number of dialysis stations, a proxy of end-stage kidney disease (ESKD) prevalence, race, poverty, and number of positive test results for novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) within a zip code in the greater Chicagoland area. Data for SARS-CoV-2 testing were obtained from the Illinois Department of Health and demographic information at the zip code level was obtained from the US Census Bureau. SARS-CoV-2–positive test results per capita correlated significantly with number of dialysis stations, percentage of households living in poverty, and percentage of residents reporting Black race and Hispanic ethnicity within a zip code. These findings highlight the SARS-CoV-2 exposure risk that persons living in poor urban areas face, including those with ESKD.
Editorial, p. 517
Coronavirus disease 2019 (COVID-19) is caused by a novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and can lead to severe acute respiratory distress requiring hospitalization and even death. On January 21, the first case of COVID-19 was identified in Washington State followed just 3 days later by a COVID-19 diagnosis in a woman returning to Chicago, IL, directly from Wuhan, China. On January 30, the husband of this second US case also developed COVID-19 and was identified as the first US case of person-to-person transmission of SARS-CoV-2.1,2 Illinois currently has one of the highest reported rates of COVID-19 cases within the United States despite having high testing rates. As of June 15, 2020, a total of 1,228,341 tests have been completed in Illinois; 133,639 positive cases and 6,398 deaths.1
The COVID-19 epidemic has generated intense focus on the long-standing socioeconomic disparities in public health surveillance and disease prevention that also influence the development of chronic diseases, including end-stage kidney disease (ESKD).1, 2, 3, 4 ESKD is a chronic disease occurring at a high prevalence in communities with a high minority population and a high percentage of households living in poverty.4,5 Individuals with ESKD are particularly susceptible to SARS-CoV-2 exposure and are at risk for severe outcomes with COVID-19,6, 7, 8, 9, 10 in part due to the increased frequency at which dialysis patients must leave their homes and enter the congregant setting of a dialysis facility. In addition, transportation to the dialysis center may require interactions with transportation personnel. Patients receiving maintenance dialysis are therefore one of the most vulnerable populations for the duration of the COVID-19 epidemic.3,11 The first death reported associated with COVID-19 in the United States was a patient receiving maintenance hemodialysis at the Northwest Kidney Center in the State of Washington. Several additional patients from that dialysis unit subsequently died of COVID-19.2
In this ecological analysis, we used data from the Illinois Department of Public Health, which reports SARS-CoV-2 test results by residence zip code, to examine the correlation of SARS-CoV-2–positive cases and COVID-19–associated deaths with number of dialysis stations, a proxy of zip code–associated ESKD prevalence, and the poverty status and demographics of the populations within a zip code. We hypothesized that the SARS-CoV-2–positive rate and positive test results per capita correlate with number of dialysis stations and with the demographics and poverty status of that zip code.
Methods
Illinois SARS-CoV-2 testing data were obtained from the Illinois Department of Public Health website through the Illinois' National Electronic Disease Surveillance System (I-NEDSS) data system.1 Data used for this analysis were last updated June 15, 2020, but I-NEDSS is regularly being updated as the number of total tests performed and positive test results accumulate. Our ecological analysis was limited to Cook County, which includes 163 zip codes with a total population of 5,232,412 residents. All data used in this study are publicly available and stripped of identifiers; therefore, institutional review board approval was not required and informed consent was not obtained.
We calculated the SARS-CoV-2–positive test rate and the total SARS-CoV-2 test results per capita within a zip code to address population density. The SARS-CoV-2–positive test rate was defined as total number of positive test results divided by the total number of SARS-CoV-2 tests within a zip code; likewise, the SARS-CoV-2–positive test results per capita measure were defined as the total number of SARS-CoV-2–positive tests divided by the total population for that zip code. The Cook County Medical Examiner’s office reports deaths that fall under its jurisdiction and occurred in Cook County through June 15, 2020. Death rate was defined as total number of COVID-19–associated deaths reported divided by the total number of SARS-CoV-2–positive test results within a zip code. Deaths per capita was defined as total number of reported COVID-19–associated deaths within a zip code divided by the total population of that zip code.
Demographics, Income, Poverty Status, and ESKD Density
Data for income, race, and ethnicity for the Cook County zip codes were accessed from the US Census Bureau's online data tool and based on the 2018 American Community Survey Demographic and Housing Estimates.12 Poverty was defined by the American Community Survey and based on a graded scale of household size and total household income. Poverty thresholds do not depend on geographic area within the United States but are updated for inflation based on the Consumer Price Index. Median household income is defined by total income reported for all individuals 15 years and older for a given household. Distribution of race/ethnicity within a zip code was calculated as percent of total population identifying as 1 or more of the following: White, Black or African American, American Indian and Alaska Native, Asian, Native Hawaiian and other Pacific Islander, and other races. Ethnicity was calculated as percent of the total population identifying as Hispanic/Latino. Location and number of dialysis centers and stations within a center for a given zip code were obtained from the Centers for Medicare & Medicaid Services Medicare Database tool,13 which provides a list of all dialysis facilities and the number of dialysis stations within a facility by zip code. We used the total number of dialysis stations within a zip code as a proxy for ESKD prevalence within a zip code. The latitude and longitude of each zip code were obtained from the US Census Bureau’s TigerWeb tool.14 This site provided zip code tabulation data from 2010 containing the center latitude and center longitude of each zip code, which was used for plotting data on a geomap.
Statistical Analysis
The distribution of demographic variables, income, and poverty status was examined within each zip code. Kolmogorov-Smirnov test for goodness of fit was applied to test for normality of data. Correlations of total number of SARS-CoV-2 tests, positive rates, and positive test results per capita, COVID-19–associated deaths per capita and death rate with distribution of demographics, income, poverty status and number of dialysis stations within a zip code were computed with Spearman rank correlation. Only median household income and total tests per capita were found to be normally distributed, whereas the rest of the data violated the normality assumption. Therefore, we performed our correlation analysis with nonparametric Spearman correlation, which is a rank-based correlation measure and does not rest on an assumption of normality, and 95% confidence intervals CIs) were calculated using methods described by Dr Fisher in 1925.15 All statistical analyses were performed in Python with the scipy and statsmodels modules. Due to the large number of correlations examined, we used P < 0.005 as the level of statistical significance.
Geomapping
Geomapping focused on Cook County by only using zip codes with a Cook County census designation. We mapped total SARS-CoV-2–positive test results per capita within a zip code with total dialysis stations within a zip code and with percent of households living below the federal poverty threshold within a zip code. Geomapping was performed using Mathworks MATLAB software and the native “geobubble” tool. Zip codes were mapped using latitude and longitude data from the US Census Bureau website. The “sizedata” function was used to plot total positive SARS-CoV-2 test results per capita and total SARS-CoV-2 tests conducted in their respective maps. The “sizedata” function plotted these data with relative size of bubbles. The “colordata” function was used to plot total dialysis stations and percent below poverty line in their respective maps. The “colordata” function plotted these data with a grayscale color map after binning the data into 6 and 4 groups for total dialysis stations and percent households living below federal poverty threshold, respectively.
Results
Among the 163 zip codes within Cook County, the median number of residents living in a given zip Code was 27,783 (interquartile range [IQR], 14,220-43,074). Table 1 shows characteristics of the 163 zip codes within Cook County. Among the 163 infection codes, there were a total of 2,501 dialysis stations and 86 zip codes had at least 1 dialysis station (53%), whereas 77 zip codes had zero dialysis stations. The median number of dialysis stations among the 86 zip codes with at least 2 dialysis station was 24 (IQR, 16-36). The median distribution of race within zip codes was 70.1% White (IQR, 44.9-84.1), 6.9% Black (IQR, 3.5-29.1), and 11.9% Hispanic (IQR, 6.3-24.8) and median age was 38.7 (IQR, 34.2-41.5) years. Median income was $65,262 (IQR, $50,521-$88,298) and median percentage of families living below the federal poverty threshold was 7.3% (IQR, 4.3%-13.9%). As of June 15, 2020, a total of 548,827 SARS-CoV-2 tests were performed in Cook County, and 84,353 test ressults were positive (15.4%). The median number of tests within a Cook County zip code was 2,728 (IQR, 1,398-4,521) and median number of positive test results was 311 (IQR, 159-636). A total of 4,007 COVID-19–related deaths in Cook County residents were reported to the Cook County medical examiner.
Table 1.
Characteristics of the Populations Within the 163 Zip Code–Defined Areas in the Chicagoland Region
| Total Zip Codes | 163 |
| Zip codes without dialysis stations | 77 |
| Total residents | 5,232,412 |
| Residents within zip code | 27,783 [14,220-43,074] |
| Total dialysis stations | 2,501 |
| Dialysis stations within zip codea | 24 [16-36] |
| White race | 70.1% [44.9%-84.1%] |
| Black race | 6.9% [3.5%-29.1%] |
| Hispanic ethnicity | 11.9% [6.3%-24.8%] |
| Asian race | 5.0% [1.7%-12.5%] |
| Age, y | 38.7 [34.2-41.5] |
| Age ≥ 65 y | 14.2% [11.4%-17.1%] |
| Male sex | 48.8% [47.3%-50.1%] |
| Income | $65,262 [$50,521-$88,298] |
| Families below federal poverty threshold | 7.3% [4.3%-13.9%] |
| Tests within zip code | 2,728 [1,398-4,521] |
| Positive tests | 311.5 [159-636] |
| Positive rate | 13% [9%-16%] |
| Deaths | 13 [4-35] |
Note: Values for continuous variables are given as median [interquartile range].
Limited to the 86 zip codes with at least 1 dialysis station; 77 zip codes had zero dialysis stations.
Table 2 shows the correlation coefficients of demographic characteristics, income, poverty status, and dialysis stations and dialysis stations per capita with SARS-CoV-2–positive test results per capita, positive test rate, and deaths per capita. Both positive test results per capita and positive test rate were negatively associated with the percentage of White race and with median income. The number of positive test results per capita correlated significantly with percentage of residents within a zip code reporting Black race (r = 0.28; 95% CI, 0.23-0.33; P < 0.005) and Hispanic ethnicity (r = 0.68; 95 CI, 0.65-0.70; P < 0.005,) and number of dialysis stations within a zip code (r = 0.25; 95% CI, 0.19-0.29; P < 0.005). However, both positive results per capita (r = 0.02; 95% CI, −0.03 to 0.08; P = 0.7) and positive test rate (r = −0.01; 95% CI, −0.07 to 0.04; P = 0.9) showed no correlation with dialysis stations per capita. Strong correlations were noted with number of positive test results per capita (r = 0.57; 95% CI, 0.53-0.60; P < 0.005) and positive test rate (r = 0.48; 95% CI, 0.44-0.52; P < 0.005) with percentage of families within a zip code living below the federal poverty threshold. Overall, 21% of SARS-COV-2 positive test results occurred among residents residing within the 21 (13%) zip codes with >20% of households living below the federal poverty threshold and 76% of positive test results were within the 86 (53%) zip codes with dialysis stations.
Table 2.
Correlations of Population Demographics With SARS-CoV-2–Positive Cases Per Capita and With SARS-CoV-2 Positive Rate
| Demographics of a Zip Code | Positive Cases Per Capita | Positive Rate | Deaths Per Capita |
|---|---|---|---|
| Total no. of dialysis stations | 0.25 [0.19 to 0.29] | 0.24 [0.19 to 0.29] | 0.20 [0.14 to 0.25]a |
| Total no. of dialysis stations per capita | 0.02 [−0.03 to 0.08]b | −0.01 [−0.07 to 0.04]b | 0.12 [0.07 to 0.17]b |
| White race | −0.47 [−0.51 to −0.43] | −0.3 [−0.35 to −0.25] | −0.25 [−0.3 to −0.2] |
| Black race | 0.28− [0.23 to 0.33] | 0.09 [0.04 to 0.14]a | 0.24 [0.19 to 0.29] |
| Asian race | −0.28 [−0.32 to −0.23] | −0.19 [−0.24% to −0.13%] | −0.07 [−0.13 to −0.02]b |
| Hispanic ethnicity | 0.68 [0.65 to 0.70] | 0.71 [0.69 to 0.74] | 0.01 [−0.05 to 0.06]b |
| Families below federal poverty threshold | 0.57 [0.53 to 0.60] | 0.48 [0.44 to 0.52] | 0.34 [0.29 to 0.38] |
| Median income | −0.57 [−0.60 to −0.54] | −0.52 [−0.54 to −0.47] | −0.32 [−0.37 to −0.28] |
| Median age | −0.39 [−0.43 to −0.34] | −0.36 [−0.41 to −0.32] | 0.07 [0.01 to 0.12]b |
| Total no. of residents | 0.36 [0.31 to 0.41] | 0.42 [0.38 to 0.47] | 0.16 [0.11 to 0.21] |
| Total tests per capita | 0.58 [0.55 to 0.62] | 0.19 [0.14 to 0.24]a | 0.31 [0.26 to 0.36] |
| Total tests | 0.54 [0.50 to 0.58] | 0.50 [0.46 to 0.54] | 0.25 [0.20 to 0.30] |
Note: All correlations significant at P < 0.005 except as noted.
P < 0.05.
P > 0.05.
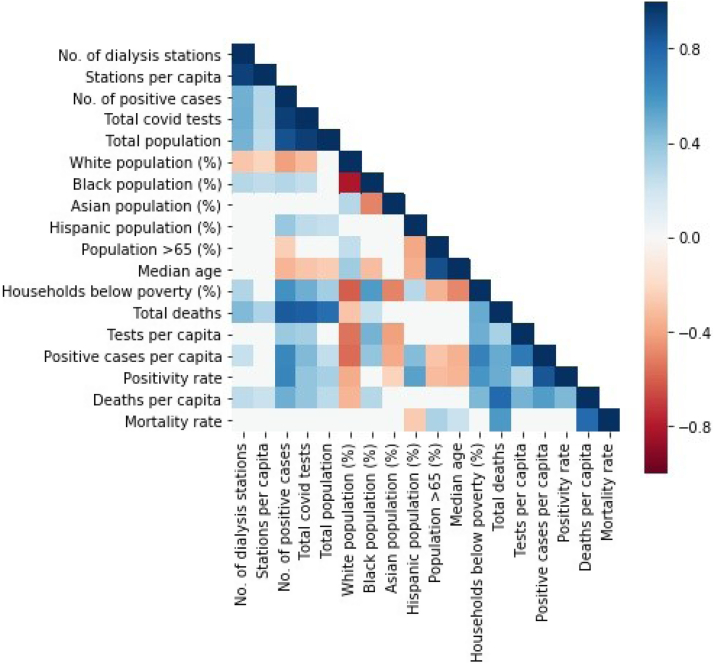
The total number of COVID-19–associated deaths per capita correlated significantly with the percentage of residents reporting Black race within a zip Code (r = 0.24; 95% CI, 0.19-0.29; P < 0.005) and with the percentage of families living below the federal poverty threshold (r = 0.34; 95% CI, 0.29-0.38; P < 0.005). No correlation was found between percentage of residents reporting Hispanic ethnicity and deaths per capita (r = 0.01; 95% CI, –0.05 to 0.06; P = 0.94). COVID-19–associated deaths per capita were positively correlated with total number of dialysis stations (r = 0.20; 95% CI ,0.14-0.25; P = 0.01) and with dialysis stations per capita (r = 0.12; 95% CI, 0.07-0.17; P = 0.1) but these correlations did not meet statistical significance. Overall, 73% of all COVID-19–associated deaths were from residents living in the 86 zip codes with dialysis stations and 24.5% of all COVID-19–associated deaths were in zip codes with >20% of households living below the federal poverty threshold. Figure 1 shows the correlation matrix of the demographics, income status, and number of dialysis stations of the 163 zip codes in Cook County. The number of dialysis stations within a zip code correlated significantly with the distribution of race and poverty within a zip code; distribution of race and poverty within a zip code correlated strongly with the SARS-CoV-2–positive test results per capita.
Figure 1.
Correlation between demographics, income, and total number of dialysis stations within a zip code and number of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)–positive tests per capita.
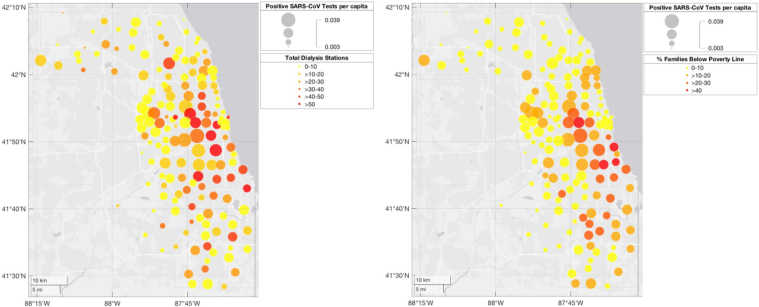
Figure 2 shows maps of the distribution of SARS-CoV-2–positive test results per capita by zip code in Cook County. The larger circles indicate higher number of SARS-CoV-2–positive test results per capita. The left panel shows the overlap of the SARS-CoV-2–positive test results per capita by number of dialysis stations within a zip code; red indicates highest number of dialysis stations within a zip code. This map shows several areas in Cook County with high numbers of both SARS-CoV-2–positive test results per capita and dialysis stations. On the right panel, red indicates the highest percentage of households living below the federal poverty threshold and demonstrates the overlap of areas within Cook County with high number of SARS-CoV-2–positive test results per capita and high percentage of households living below the federal poverty threshold.
Figure 2.
(Left panel) Distribution of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)–positive tests overlapped with number of dialysis stations within a zip code. The larger the circle, the higher the number of SARS-CoV-2–positive tests per capita. Red indicates highest number of dialysis stations. (Right panel) Distribution of SARS-CoV-2–positive tests overlapped with poverty status as measured by the percentage of households within a zip code living below the federal poverty line. The larger the circle, the higher the number of SARS-CoV-2–positive tests per capita. The color scheme indicates percentage of households within a zip code living below the federal poverty line, with red indicating >40% and yellow indicating <10%.
Discussion
In an ecological analysis of a large metropolitan area, the number of SARS-CoV-2–positive test results per capita was correlated with the number of dialysis stations (a proxy for kidney failure prevalence) and with the percentage of households living below the federal poverty threshold. This ecological analysis was not undertaken to determine cause-and-effect relationships but rather as a surveillance tool. The findings reinforce clinical observations that patients with ESKD living in poor urban areas face high risk for exposure to SARS-CoV-2.3,7,11,16
Our findings show that populations living in highly populated areas with high poverty have a high risk for COVID-19 exposure; given that this is a similar risk population for kidney failure, many persons receiving maintenance dialysis are highly vulnerable to SARS-CoV-2 exposure. Multiple modes of transmission could be involved. Maintenance hemodialysis for ESKD treatment requires leaving home 3 days per week and interacting with numerous health care personnel within a dialysis unit. Traveling to and from the dialysis unit may also require interaction with travel personnel. Due to the comorbid conditions and reduced immunity associated with ESKD, COVID-19 in this population is often associated with hospitalization and mortality.8,9 The vulnerability of patients receiving maintenance dialysis to develop COVID-19 combined with high rates of acute kidney injury4, 5, 6 requiring dialysis in hospitalized patients with COVID-19 has led to substantial strains on hospital dialysis staff, equipment, and supplies to provide adequate dialysis for hospitalized patients. Although ongoing transmission will occur for many months to come, there is an urgent need to continue to refine our understanding of very high-risk subpopulations and initiate mitigation efforts. Interventions to reduce transmission of SARS-CoV-2 in high-risk areas, such as increased testing and contact tracing,17 could potentially reduce transmission.
The percentage of racial/ethnic minorities within a zip code was also correlated positively with the number of SARS-CoV-2–positive test results per capita. These findings are supported by the COVID-19 pandemic disproportionately affecting minority communities.16,18 However, race should not be the sole focus regarding disparities in COVID-19. Our results show a strong correlation of SARS-CoV-2–positive test results per capita with median income and with poverty status within a zip code. A disproportionate number of all positive SARS-CoV-2 test results (21%) occurred within zip codes with >20% of households living below the federal poverty line, yet these zip codes account for only 13% of all zip codes analyzed. There is a strong body of research demonstrating how poverty disproportionally affects minorities due to structural racism and bias, and the inherent challenge of examining the independent effects of race/ethnicity and poverty on health disparities because these 2 factors are interwoven.19,20 Poverty status may be associated with decreased ability to shelter at home and to implement social distancing. Poverty status is also associated with a higher burden of comorbid conditions that increases the risks for hospitalization and mortality associated with COVID-19.7,16,21
This study has several strengths. First, our analysis focused on one of the main centers of COVID-19 at a time when the infection rate had maintained a plateau. Illinois currently has one of the highest number of SARS-CoV-2–positive test results and highest rates of SARS-CoV-2 testing in the United States and public health teams are focusing on areas at high risk.1 To address the high rate of testing, we examined the total SARS-CoV-2–positive rate and the number of positive test results per capita. Similar ecological analyses may not be possible in other states due to low rates of testing. We also found significant correlations between the poverty status of a zip code with the number of dialysis station within a zip code and these findings are supported by previous studies that have reported higher ESKD prevalence in neighborhoods and zip codes with high levels of poverty.4,5
The limitations of an ecological analysis must be addressed. Clearly colinearity and confounding of multiple demographic risk factors are present; however, our purpose was to define disease patterns and not attribute causal strength to any specific component. Our unit of analysis is at the zip code level and not at the person level and measures of exposure are only a proxy of measures at an individual level and are based on population averages within a zip code. We examined both positive test rate and positive test results per capita. The positive test rate is a commonly used metric to track the spread of a disease. If the same proportion of a population is tested over time, the test positivity rate can be used to calculate the contagiousness of a disease. Because testing was not uniform across zip codes, we also examined the metric positive test results per capita. The number of positive test results per capita may have error due to error in the denominator obtained from 2010 US Census data. ESKD prevalence was based on the number of dialysis stations, which is only a crude estimate of ESKD prevalence. Although >85% of all patients receiving dialysis receive in-center hemodialysis,22 dialysis stations as a proxy for ESKD prevalence does not address individuals receiving home dialysis and kidney transplant recipients. COVID-19–associated deaths were limited to those reported to the Cook County medical examiner, so deaths of residents who died outside of Cook County may not have been captured. Our analysis focused on Cook County and findings may not be generalizable to other areas of the United States, especially nonurban areas.
In summary, the findings from this ecological analysis suggest that many urban areas with high ESKD prevalence and poverty status have a high burden of SARS-CoV-2 exposure. Although community-wide “test, trace, and isolate”17 interventions are being scaled up, an urgent need exists to intervene and protect groups that we already know are most vulnerable and these include patients with ESKD. Prevention strategies should continue to target urban areas with a high proportion of the population living in poverty and areas with high ESKD prevalence.
Article Information
Authors’ Full Names and Academic Degrees
Siddharth Bhayani, MS, BS, Ranit Sengupta, PhD, Talar Markossian, PhD, Samie Tootooni, PhD, Amy Luke, PhD, David Shoham, PhD, Richard Cooper, MD, and Holly Kramer, MD, MPH.
Authors’ Contributions
Research idea and study design: SB, TM, HK; data acquisition: SB, RS; data analysis/interpretation: SB, RS, HK, TM, RC, AL, DS; statistical analysis: SB, ST, RS; supervision or mentorship: ST, TM, HK. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Support
None.
Financial Disclosure
The authors declare that they have no relevant financial interests.
Peer Review
Received May 25, 2020. Evaluated by 2 external peer reviewers, with direct editorial input from the Statistical Editor and the Editor-in-Chief. Accepted in revised form Jun 28, 2020.
Footnotes
Complete author and article information provided before references.
References
- 1.Illinois Department of Public Health COVID-19 statistics. https://www.dph.illinois.gov/covid19 Updated 2020. Accessed June 15, 2020.
- 2.Hauk G., Gelles K., Bravo V., Thorson M. Three months in: a timeline of how COVID-19 has unfolded in the U.S. so far. https://www.usatoday.com/in-depth/news/nation/2020/04/21/coronavirus-updates-how-covid-19-unfolded-u-s-timeline/2990956001/ Updated 2020. Accessed May 6, 2020.
- 3.Kliger A.S., Silberzweig J. Mitigating risk of COVID-19 in dialysis facilities. Clin J Am Soc Nephrol. 2020;15(5):707–709. doi: 10.2215/CJN.03340320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garrity B.H., Kramer H., Vellanki K., Leehey D., Brown J., Shoham D.A. Time trends in the association of ESRD incidence with area-level poverty in the US population. Hemodial Int. 2016;20(1):78–83. doi: 10.1111/hdi.12325. [DOI] [PubMed] [Google Scholar]
- 5.Volkova N., McClellan W., Klein M. Neighborhood poverty and racial differences in ESRD incidence. J Am Soc Nephrol. 2008;19(2):356–364. doi: 10.1681/ASN.2006080934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheng Y., Luo R., Wang K. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97(5):829–838. doi: 10.1016/j.kint.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 9.Wu C., Chen X., Cai Y. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):934–943. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.CDC COVID-19 Response Team Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 - United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):382–386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weiner D.E., Watnick S.G. Hemodialysis and COVID-19: an Achilles' heel in the pandemic health care response in the United States. Kidney Med. 2020;2(3):227–230. doi: 10.1016/j.xkme.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.United States Census Bureau American community survey. https://www.census.gov/programs-surveys/acs Updated 2020. Accessed May 6, 2020.
- 13.Centers for Medicare & Medicaid Services Dialysis Facility Compare. https://Www.medicare.gov/dialysisfacilitycompare/ Updated 2020. Accessed May 1, 2020.
- 14.U.S. Census Bureau TIGER/line geo databases. https://www.census.gov/geographies/mapping-files/time-series/geo/tiger-geodatabase-file.html Updated 2020. Accessed May 1, 2020.
- 15.Fisher R.A. Statistical methods for research workers. In: Kotz S., Johnson N.L., editors. Breakthroughs in Statistics. Springer Series in Statistics. Springer; New York, NY: 1992. pp. 66–70. [Google Scholar]
- 16.Centers for Medicare & Medicaid Services COVID-19 data snapshot fact sheet. June 11. 2020. https://www.cms.gov/files/document/medicare-covid-19-data-snapshot-fact-sheet.pdf Accessed June 15, 2020. [PubMed]
- 17.Watson C., Cicero A., Blumenstock J., Fraser M. A national plan to enable comprehensive COVID-19 case finding and contact tracing in the US. Johns Hopkins Bloomberg School of Public Health Center for Health Security. https://www.centerforhealthsecurity.org/our-work/pubs_archive/pubs-pdfs/2020/200410-national-plan-to-contact-tracing.pdf
- 18.Yancy C.W. COVID-19 and African Americans. JAMA. 2020;323(19):1891–1892. doi: 10.1001/jama.2020.6548. [DOI] [PubMed] [Google Scholar]
- 19.Cooper R.S., Kaufman J.S. Race and hypertension: science and nescience. Hypertension. 1998;32(5):813–816. doi: 10.1161/01.hyp.32.5.813. [DOI] [PubMed] [Google Scholar]
- 20.Kaufman J.S., Cooper R.S., McGee D.L. Socioeconomic status and health in blacks and whites: the problem of residual confounding and the resiliency of race. Epidemiology. 1997;8(6):621–628. [PubMed] [Google Scholar]
- 21.US Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19) https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/index.html Updated April 30, 2020. Accessed May 7, 2020.
- 22.US Renal Data System 2018 USRDS Annual Data Report. Volume 2: End-stage renal disease (ESRD) in the United States. https://www.usrds.org/media/2283/2018_volume_2_esrd_in_the_us.pdf Accessed June 15, 2020.