Abstract
Limb position is a factor that negatively affects myoelectric pattern recognition classification accuracy. However, prior studies evaluating impact on real-time control for upper-limb amputees have done so without a physical prosthesis on the residual limb. It remains unclear how limb position affects real-time pattern recognition control in amputees when their residual limb is supporting various weights. We used a virtual reality target achievement control test to evaluate the effects of limb position and external load on real-time pattern recognition control in fourteen intact limb subjects and six major upper limb amputee subjects. We also investigated how these effects changed based on different control system training methods. In a static training method, subjects kept their unloaded arm by their side with the elbow bent whereas in the dynamic training method, subjects moved their arm throughout a workspace while supporting a load. When static training was used, limb position significantly affected real-time control in all subjects. However, amputee subjects were still able to adequately complete tasks in all conditions, even in untrained limb positions. Moreover, increasing external loads decreased controller performance, albeit to a lesser extent in amputee subjects. The effects of limb position did not change as load increased, and vice versa. In intact limb subjects, dynamic training significantly reduced the limb position effect but did not completely remove them. In contrast, in amputee subjects, dynamic training eliminated the limb position effect in three out of four outcome measures. However, it did not reduce the effects of load for either subject population. These findings suggest that results obtained from intact limb subjects may not generalize to amputee subjects and that advanced training methods can substantially improve controller robustness to different limb positions regardless of limb loading.
I. Introduction
IN the United States, there are approximately 41,000 people living with a major upper limb amputation, 40% of whom are transradial amputees [1], [2]. These individuals have difficulty performing essential activities of daily living, such as eating, grooming, and dressing [3]–[6]. In many cases, an amputation also affects an individuals capacity to return to employment and causes a decline in overall quality of life [7].
Myoelectric prostheses have the potential to restore the function required to regain basic independence. Compared to body-powered prostheses, these devices provide more degrees of freedom (DOF’s), allowing for finer control and potentially fewer compensatory movements [8]. Nevertheless, despite decades of advancements, challenges persist in controlling myoelectric prostheses. This remains an active area of research and several methods have been proposed to improve control.
One such method is myoelectric pattern recognition (PR), which relies on separable and repeatable muscle contractions. PR controllers have been validated extensively in lab settings and are now commercially available; however, several factors impact their real-world performance. Limb position has often been reported as one of these factors. Many studies have shown that offline classification errors increase significantly when different limb positions are tested [9]–[17]. Several groups have quantified the changes in detected signals that underly these poor classification rates [18]–[20]. These results have prompted the development of new training and control methods to mitigate the limb position effect [11], [12], [21]–[29].
Most of these experiments only evaluated offline performance, which does not always correlate with real-time controllability [30], [31]. To our knowledge, only two studies evaluated the real-time effects of limb position on PR control in amputees [23], [29]. These effects were found to be minor; however, these studies were limited because amputee subjects completed experiments without a physical prosthesis or load on the residual limb. It remains unclear if limb position affects real-time PR control in amputees when their residual limb is loaded with the weight of a prosthesis.
The aim of this experiment was to determine how limb position and external load affect real-time PR control in intact limb (ITL) and amputee (AMP) subjects and if these effects can be reduced with advanced training protocols. Subjects trained a controller statically, with the elbow bent at a 90° angle by their side, and dynamically, by moving the arm around their expected workspace. They then used the controllers to control a wrist and hand in a virtual reality (VR) environment to complete 3D Target Achievement Control (TAC) tests in four limb positions and with three external loads.
We hypothesized that limb position will negatively affect controller performance in ITL subjects but will not significantly affect AMP subjects when the residual limb is unloaded. In an intact limb, forearm muscle activity changes to support the weight of the wrist and hand in different limb positions. Furthermore, the muscles that control wrist rotation change depending on elbow angle. As the elbow extends, the supinator receives less supination assistance from the biceps brachii, thus altering muscle activation patterns [32]. Finally, there are several biarticular forearm muscles (brachioradialis, pronator teres, flexor carpi radialis, extensor carpi radialis longus, flexor carpi ulnaris, and palmaris longus) that assist with elbow flexion [32]. In below-elbow amputees, forearm muscles are no longer attached to the wrist joint. Therefore, changes in muscle activity due to limb position would only be caused by the elbow-dependent supinator and the biarticular forearm muscles supporting the weight of the residual limb. As the residual limb is loaded, the increasing moment across the elbow may elicit further changes in these biarticular muscles. Therefore, we also hypothesized that the effects of limb position will be exacerbated in all subjects as the load increases. Furthermore, we hypothesized that increasing the load would decrease controller performance, as it has been shown to affect PR sensitivity [33]. Finally, based on previous offline and real-time studies, we hypothesized that the dynamic training method will reduce the effects of limb position and load and improve controller performance [11], [22], [23], [25], [27].
II. Methods
This experiment was approved by the Northwestern University Institutional Review Board and all subjects gave written informed consent. We evaluated the effects of limb position, external load, and training method on PR-based myoelectric control in fourteen subjects with intact limbs (ages 20–29, eight male, six female) and six subjects with major upper limb amputations (Table I).
Table I.
Amputee Subject Demographics
| Subject | Age | Gender | Time since Amputation | Level of Amputation | Home Device Control Scheme | PR Experience |
|---|---|---|---|---|---|---|
| AMP1 | 73 | M | 32 years | Transradial | Body-powered | Moderate |
| AMP2 | 33 | M | 5 years | Wrist Disarticulation | Direct control | Moderate |
| AMP3 | 65 | M | 6 years | Transradial | Body-powered | Moderate |
| AMP4 | 56 | M | 40 years | Transradial | Direct control | Moderate |
| AMP5 | 48 | M | 11 months | Transradial | Body-powered | None |
| AMP6 | 19 | M | 10 months | Transradial | Direct control | None |
A. Experimental Setup
1). Intact Limb Subjects:
Electromyographic (EMG) signals were recorded from ITL subjects using six pairs of equally spaced stainless-steel electrodes embedded in an armband. Each subject wore the armband around their right forearm, with the reference electrode just distal to the olecranon. An HTC Vive tracker was attached to the armband to track arm movements.
To encourage isometric contractions, subjects wore a forearm orthosis that restricted hand opening/closing and wrist flexion/extension. Orthoses that limit wrist rotation also obstruct free movement of the upper arm, which is required for the testing protocol, so we chose not to restrict wrist rotation. The external loads were secured to the palmar side of the orthosis using Velcro (Fig. 1A).
Fig. 1.
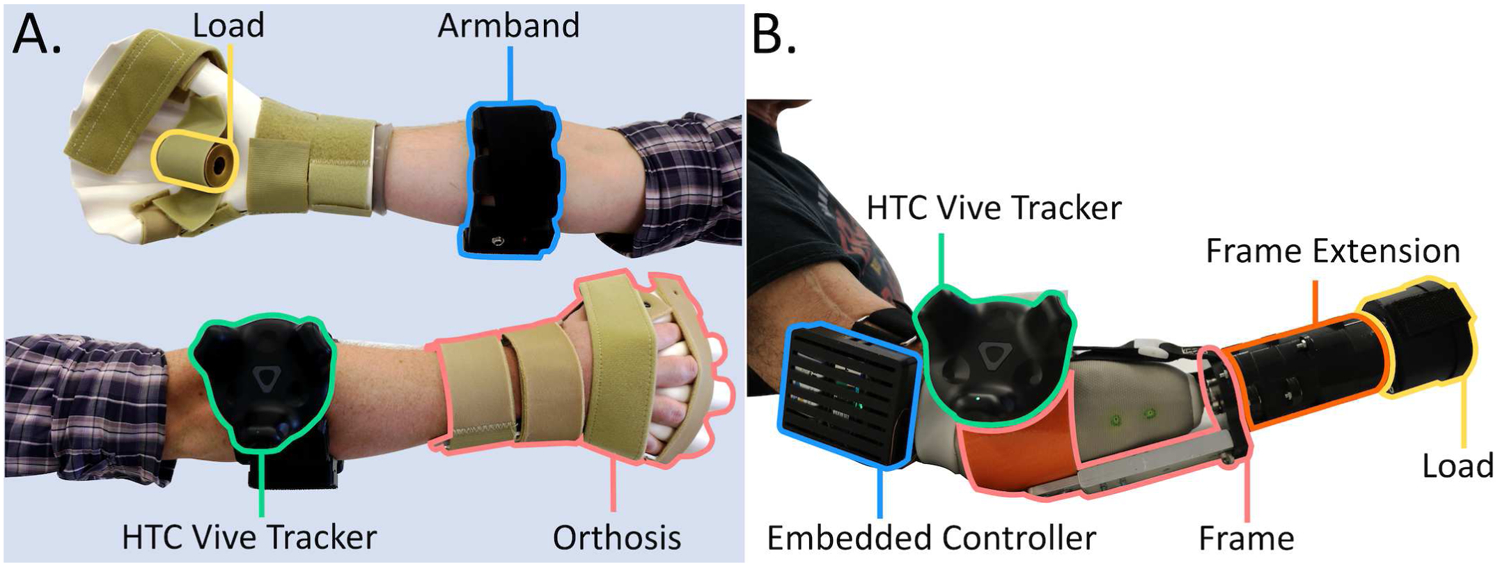
A: Palmar (top) and dorsal (bottom) view of the intact limb subject setup. The armband housed electrodes and an embedded controller that acquired and classified EMG signals. The orthosis was used to restrict wrist flexion/extension and hand opening/closing. Loads were attached to the orthosis. B: Dorsal view of the amputee subject setup. Wet electrodes were secured under a liner and signals were classified by an embedded controller. We used a frame to hold the tracker and loads, which were positioned where a prosthetic hand would be using frame extensions. The embedded controller was strapped to the upper arm and was not connected to the load-bearing frame. Both: The HTC Vive tracker tracked limb position.
2). Amputee Subjects:
EMG signals were recorded from AMP subjects using six pairs of wet electrodes equally spaced around the residual limb, avoiding regions above the radius and ulnar. The reference electrode was placed on the lateral epicondyle. A silicone liner was worn over the electrodes to prevent electrode shift or liftoff. Next, a lightweight frame was secured to the residual limb with a cuff, straps, and strong magnets. An HTC Vive tracker was attached to the cuff to track arm movements.
The external loads were placed into a box and screwed into the end of the frame. The frame was lengthened with modular extensions to position the load where a prosthetic hand would be. This was based on the distance from the lateral epicondyle to the middle of the hand on the intact side (Fig. 1B).
3). Signal Acquisition and Processing:
EMG signals were sampled at 1 kHz (Texas Instruments ADS1299), amplified with a hardware gain of 2, and a software gain of 1000, and band-pass filtered between 70–300 Hz. Data were then processed using an embedded System on Module (Logic PD SOMDM3730). We extracted four time-domain features (mean absolute value, waveform length, zero crossings, and slope sign changes) and six autoregressive coefficients from each channel using 200 ms windows in 25 ms increments. These features were used to train a linear discriminant analysis (LDA) classifier. We computed output velocity using previously described proportional control and velocity ramp algorithms [34], [35]. After each processing window, the output class and velocity were wirelessly transmitted to a desktop computer and used to control an arm in a Unity-based virtual reality environment. The virtual arm was projected onto each subjects forearm using the location and orientation of the HTC Vive tracker.
B. Experimental Protocol
Each subject completed two sessions corresponding to two training strategies: static and dynamic (see descriptions of the training methods in the Section II.B.1). The order of the sessions was pseudo-randomized such that half of the subjects used the static training method in the first session and the other half used the dynamic training method in the first session. In each session, subjects used the trained controller to complete VR-based TAC tests in four limb positions (Fig. 2) and with three loads (Table II). To minimize the effects of learning, subjects were given at least two practice tests before actual data were collected. We chose limb positions that could be encountered in activities of daily living. Positions were constrained to the sagittal plane to ensure that the loads would be supported by elbow and shoulder flexion only and to limit experimental time.
Fig. 2.
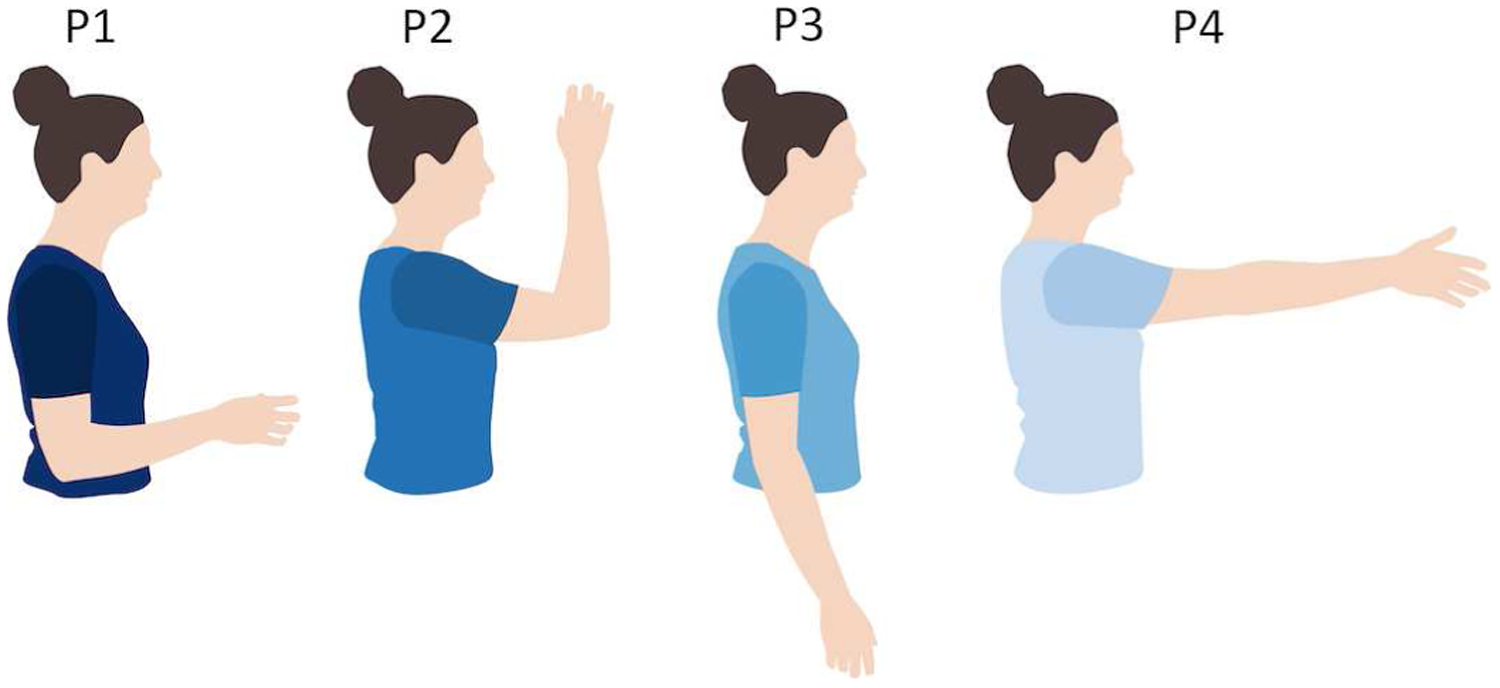
Limb positions used during testing protocol.
Table II.
External Loads Used During Testing Protocol and Their Real-World Representations
| Load (g) | Prosthesis Configuration | Prosthesis-object Combination | |
|---|---|---|---|
| Wrist | Hand | ||
| 0 | None | None | None |
| 400 | Passive | Powered | Prosthesis |
| 600 | Powered | Powered | Prosthesis + 200g |
There were two physical interpretations of the external loads, summarized in Table II. First, they corresponded to the average weights of different prosthesis configurations [36]. Secondly, the 400g load represented the lightest possible powered wrist and hand prosthesis, while the 600g load represented the prosthesis grasping a small object.
1). Training Data Collection:
All ITL subjects and two AMP subjects (AMP1, AMP2) trained a 3DOF controller (hand open/close, wrist pronation/supination, wrist flexion/extension). The other four AMP subjects trained a 2DOF controller (hand open/close, wrist pronation/supination) because they were either naive to PR control (AMP5, AMP6) or unable to reliably perform wrist flexion and extension (AMP3, AMP4).
For each training method, we collected five sets of data per movement class. In each set, subjects were instructed to hold the movement for 2.5 seconds, resulting in 100 training patterns. AMP subjects used bilateral mirroring while training so that we could verify their movements. The training methods were as follows:
Static Subjects kept their arm by their side with the elbow at a 90° angle (Fig. 2, P1) while holding the movement. There was no load attached. This is a common training method in experimental settings.
Dynamic Subjects were instructed to move their arm freely around the workspace while holding each movement. They were encouraged to cycle through each test position (P1, P2, P4, P3 and reverse) by flexing and extending the elbow and shoulder. The 400g load, representing a lightweight prosthesis, was attached throughout training. This is an adaptation of a method suggested in previous studies [22], [23], [25], [27].
2). Real-Time Testing Protocol:
In each session, subjects completed a set of 3D VR TAC tests that were based on previous work [23]. Each test comprised one trial for each movement class (except no movement) in each limb position. The test was repeated for each external load.
At the start of each trial, a target hand posture appeared in one of the four limb positions. Once the subject moved their arm within 10 cm and 30° of the correct limb position, the trial timer and myoelectric controller were activated. They then had 20 seconds to use the controller to move their virtual hand into the correct posture and remain there for 2 consecutive seconds. Each target was 52.5° away from the starting position and had a width of 16°, corresponding to an index of difficulty of 2.10 bits [37]. Each target could be reached by using only one movement (hand open, wrist flexion, etc.). However, all trained DOF’s were controllable. If a movement error was made, the subject had to use other DOFs to move back towards the target.
3). Performance Evaluation:
We quantified controller performance using the following outcome measures:
Completion rate (CR) The percentage of trials that were successful within the allotted time limit. The trial was considered successful if they were able to remain in the target for 2 consecutive seconds. A completion rate of 100% meant that the subject was able to reach all targets.
Movement efficacy (ME) The percentage of movements in each trial that were made towards the target, scaled by the proportional control output as shown in the equations below. At each timepoint (n), given the current position of the virtual hand and the position of the target, we determined the class or classes that needed to be activated to move the hand closer to the target. We summed the proportional control outputs if their corresponding class output matched . We then divided this value by the sum of all proportional control outputs when the hand is not at rest or already in the target. This metric is an adaptation of path efficiency that considers the subjects ability to correct previous erroneous movements [35]. A movement efficacy of 100% meant that the subject was able to move straight to and stay in the target without activating any other DOFs.
Stopping efficacy (SE) The percentage of time that the virtual hand was at rest when it was in the target. A stopping efficacy of 100% meant that the subject was able to stop as soon as they reached the target.
Completion time (CT) The time taken to complete each trial. For failed trials, the completion time was set to the time limit of 20 seconds. A lower completion time meant that the subject was able to reach the target faster.
4). Statistical Analyses:
ITL and AMP data were analyzed separately. First, we determined how limb position and load affected the outcomes of each training method. We fit general linear models using a deviation effect coding scheme with limb position, load and their interaction as fixed factors and subject as a random factor. For AMP subjects, we added fixed factors for the number of trained DOFs and its interactions with limb position and load. This was used to determine if the reduced number of DOFs for AMP3, 4, 5, and 6 significantly affected their results. We used multiway analysis of variance (ANOVA) to quantify the statistical significance of each factor. Next, post-hoc pairwise comparisons were performed using Tukey-Kramer tests to quantify performance changes between specific positions and loads. Finally, to determine whether training method significantly affected our results, we pooled data from both sessions and fit a model using limb position, load, training method, and their interactions as fixed factors and subject as a random factor. Again, we used multiway ANOVA to quantify the significance of each factor. All p-values were adjusted using the Holm method to account for the number of outcome measures.
III. RESULTS
A. Intact Limb Subjects
Mixed model results for fixed effects are presented in Table III, in which shaded cells indicate statistical significance. For both training methods, the interaction terms between limb position and load were not statistically significant for any outcome measure, suggesting that the effects were independent. Thus, we analyzed the limb position effect pooled across all loads and vice versa (Fig. 4).
Table III.
Mixed Model Results for Intact Limb Subjects
| F-Value | p-Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| CR | ME | SE | CT | CR | ME | SE | CT | ||
| Static Training | Limb Position | 44.85 | 57.67 | 51.99 | 46.30 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Load | 13.45 | 12.01 | 9.13 | 13.23 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |
| Limb Position*Load | 0.80 | 0.50 | 0.40 | 0.74 | 1.000 | 1.000 | 1.000 | 1.000 | |
| Dynamic Training | Limb Position | 4.07 | 8.60 | 1.07 | 6.87 | 0.014 | < 0.001 | 0.361 | < 0.001 |
| Load | 8.35 | 11.83 | 5.98 | 13.28 | < 0.001 | < 0.001 | 0.003 | < 0.001 | |
| Limb Position*Load | 1.13 | 1.70 | 1.42 | 1.25 | 0.613 | 0.469 | 0.613 | 0.613 | |
| overall | Training Method | 556.67 | 654.58 | 1065.37 | 664.46 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
| Training Method*Limb Position | 21.19 | 21.52 | 16.40 | 15.48 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |
| Training Method*Load | 3.02 | 0.68 | 0.17 | 0.92 | 0.197 | 1.000 | 1.000 | 1.000 | |
Fig. 4.
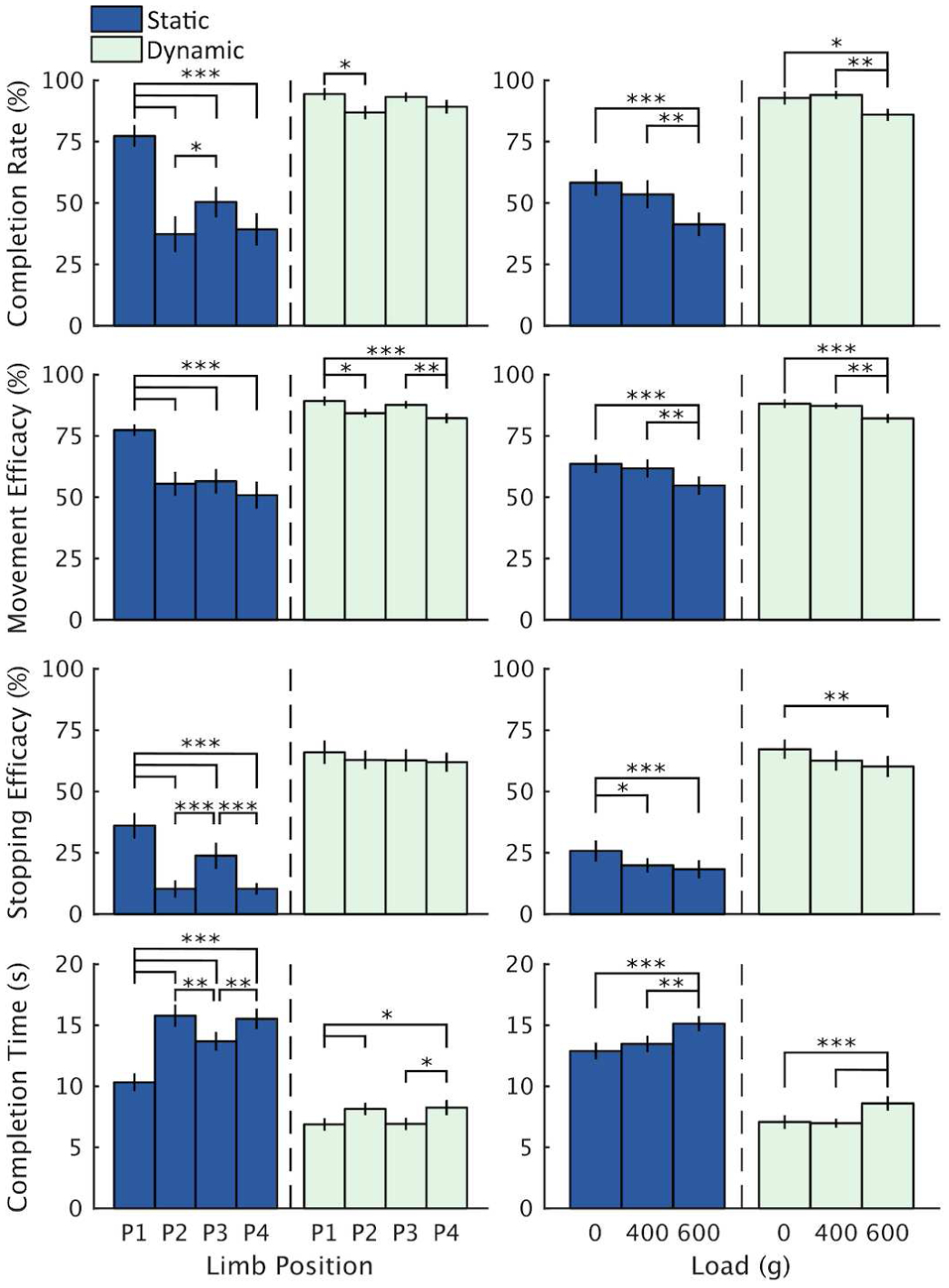
Intact limb subject results. Limb position (left) and load (right) significantly and independently affected controller performance regardless of training method. Dynamic training significantly mitigated limb position effects (and eliminated these effects in stopping efficacy), but did not reduce load effects. Overall, dynamic training significantly improved controller performance. Error bars represent standard errors.
1). Static Training:
Limb position significantly affected all outcome measures (p < 0.001). Depicted in Fig. 4, post-hoc results showed significant differences between almost all positions. As expected, subjects had significantly better control in the trained position (P1) than in all untrained positions (mean CR ± standard error: 77.38 ± 4.41%). P3 yielded the next best results (50.40 ± 6.26%), while P2 (37.30 ± 7.31%) and P4 (39.29 ± 6.63%) produced similarly poor results. These trends were consistent across all outcome measures.
Increasing the external load significantly decreased performance (p < 0.001). As shown in the pairwise comparison results in Fig. 4, completion rate, completion time, and movement efficacy were unaffected by the 400g load, but worsened with the 600g load. Stopping efficacy was the most sensitive to load, showing a significant decrease from 0g to 400g.
2). Dynamic Training:
Based on Table III, limb position effects were still statistically significant for most metrics (p ≤ 0.014). However, dynamic training was able to significantly reduce these effects (p < 0.001). Limb position significantly affected completion rate, movement efficacy, and completion time, but not stopping efficacy (p = 0.361). Post-hoc results showed fewer statistically significant comparisons than the static training method. In particular, subjects performed equally between P1 and P3 (94.44 ± 2.40%, 93.25 ± 1.95%) and between P2 and P4 (86.90 ± 2.77%, 89.29 ± 2.88%).
Dynamic training did not significantly reduce the effects of load on any outcome measure (p ≥ 0.197). Increasing the load still significantly affected all metrics negatively (p ≤ 0.003). Specifically, subjects generally performed significantly worse with the 600g load, but similarly with the 0g and 400g load.
Overall, the dynamic training method significantly improved control when compared to the static training method (p < 0.001). Subjects completed 90.97 ± 2.10% of all trials with the dynamic training method, in contrast to 51.09 ± 4.93% with the static training method. Notably, the outcomes at each position from dynamic training were better than outcomes at P1 from static training (the idealized case where training and testing were completed in the same position). Paired t-tests showed that these differences were all statistically significant for stopping efficacy and completion time (p ≤ 0.042). Dynamic training also significantly improved completion rates (p ≤ 0.021) at P1, P3, and P4 and movement efficacy (p ≤ 0.032) at P1 and P3 compared to P1 from static training.
B. Amputee Subjects
Mixed model results for fixed effects are presented in Table IV, in which shaded cells indicate statistical significance. Similar to the ITL results, all interaction terms between limb position and load were not statistically significant, indicating that the effects were independent. Thus, we analyzed the limb position effect pooled across all loads and vice versa (Fig. 5).
Table IV.
Mixed Model Results for Amputee Subjects
| F-Value | p-Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| CR | ME | SE | CT | CR | ME | SE | CT | ||
| Static Training | Limb Position | 5.65 | 2.98 | 0.004 | 0.064 | ||||
| 3DOF | 5.13 | 10.42 | 0.009 | < 0.001 | |||||
| 2DOF | 4.20 | 2.11 | 0.020 | 0.101 | |||||
| Load | 3.02 | 5.01 | 2.99 | 1.71 | 0.150 | 0.029 | 0.150 | 0.182 | |
| Limb Position*Load | 1.79 | 1.02 | 1.41 | 0.90 | 0.401 | 0.825 | 0.636 | 0.825 | |
| Limb Position*DOF | 1.89 | 3.08 | 4.82 | 5.10 | 0.130 | 0.056 | 0.008 | 0.007 | |
| Load*DOF | 0.59 | 0.11 | 2.76 | 0.03 | 1.000 | 1.000 | 0.259 | 1.000 | |
| Dynamic Training | Limb Position | 1.54 | 2.85 | 1.41 | 3.97 | 0.407 | 0.113 | 0.407 | 0.034 |
| Load | 0.54 | 2.16 | 6.45 | 2.20 | 0.586 | 0.338 | 0.007 | 0.338 | |
| Limb Position*Load | 0.83 | 1.99 | 0.81 | 2.05 | 1.000 | 0.234 | 1.000 | 0.234 | |
| Limb Position*DOF | 0.95 | 1.91 | 0.86 | 0.57 | 1.000 | 0.509 | 1.000 | 1.000 | |
| Load*DOF | 0.07 | 3.65 | 0.01 | 1.43 | 1.000 | 0.109 | 1.000 | 0.721 | |
| Overall | Training Method | ||||||||
| 3DOF | 1.29 | 1.38 | 0.99 | 2.33 | 0.722 | 0.722 | 0.722 | 0.512 | |
| 2DOF | 27.54 | 64.60 | 67.40 | 39.71 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | |
| Training Method*Limb Position | 1.21 | 0.16 | 2.29 | 0.87 | 0.918 | 0.925 | 0.311 | 0.918 | |
| Training Method*Load | 0.82 | 0.44 | 0.22 | 0.03 | 1.000 | 1.000 | 1.000 | 1.000 | |
| Training Method*DOF | 9.16 | 22.19 | 20.51 | 10.36 | 0.003 | < 0.001 | < 0.001 | 0.003 | |
Fig. 5.
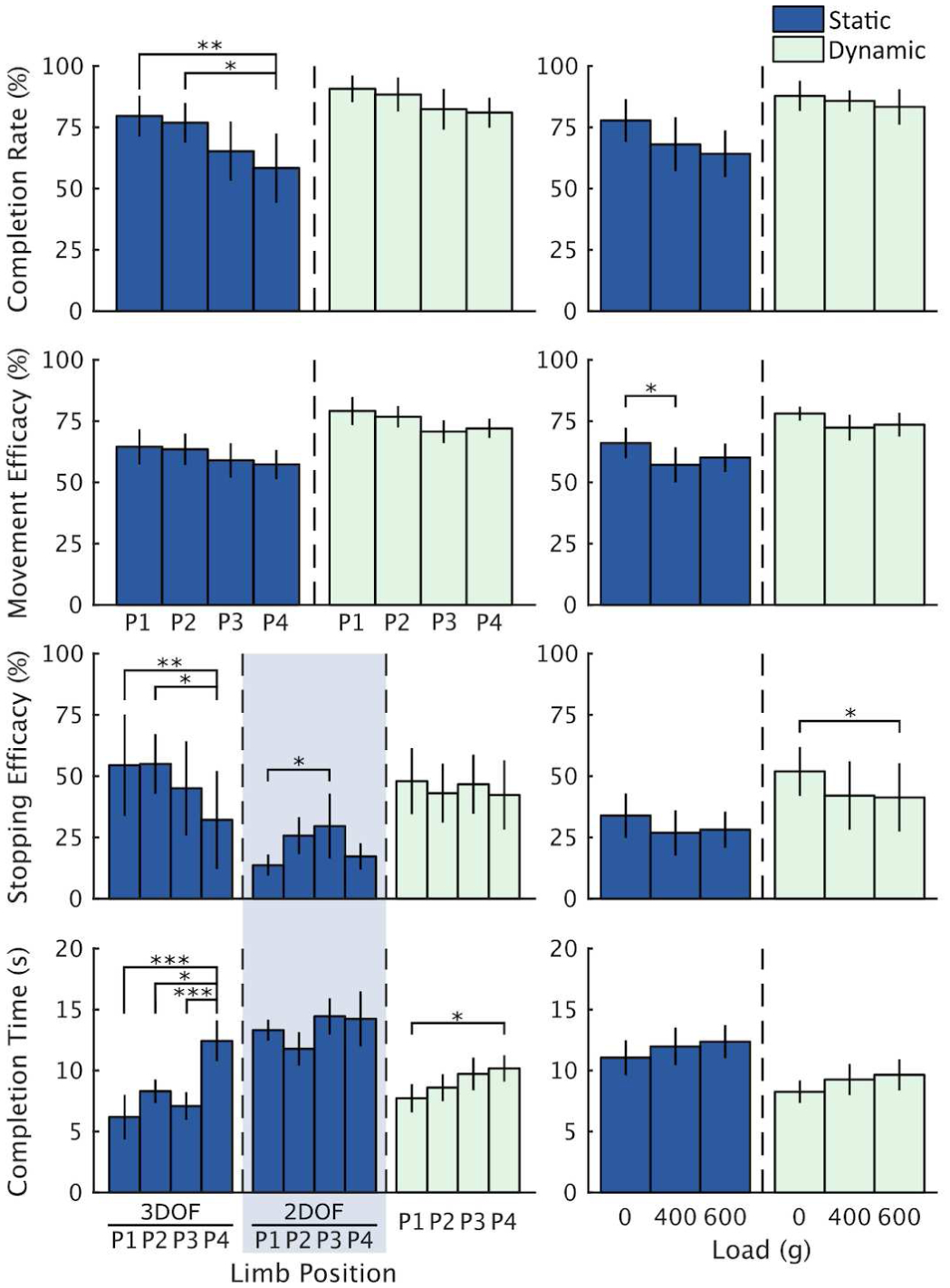
Amputee subjects results. When the controller was trained statically, limb position (left) significantly affected completion rate for all amputee subjects. Limb position affected completion time and stopping efficacy for subjects who used a 3DOF controller, and affected stopping efficacy for subjects who used a 2DOF controller. There were fewer differences between positions than in intact limb subjects. When dynamic training was used, limb position only affected the completion time of P4. Although dynamic training reduced limb position effects, this change was not statistically significant. Increasing the load (right) significantly decreased movement efficacy and stopping efficacy. Overall, training dynamically significantly improved controller performance.
1). Static Training:
Limb position significantly affected completion rate (p = 0.004) for all AMP subjects. Even though training only occurred in P1, subjects had similar control performances in P1, P2, and P3 (79.62 ± 8.42%, 76.85 ± 8.07%, 65.28 ± 12.08%). However, performance decreased in P4 (58.33 ± 14.13%). Limb position did not significantly affect movement efficacy (p = 0.064).
As shown in Table IV, the effects of limb position on stopping efficacy and completion time depended on the number of trained DOFs (p ≤ 0.007). Hence, we evaluated these metrics separately for the two groups of AMP subjects. For 3DOF subjects, limb position affected the stopping efficacy and completion time at P4 (p ≤ 0.009). For 2DOF subjects, limb position only affected stopping efficacy (p = 0.020).
Based on Fig. 5, increasing external load tended to decrease control performance. These changes were only statistically significant for movement efficacy (p = 0.029).
2). Dynamic Training:
Limb position only significantly affected completion time (p = 0.034). Specifically, as shown in Fig. 5, subjects required more time to complete tasks in P4 compared to tasks in P1. Although dynamic training was able to eliminate position effects in all but one outcome measure, these changes were not statistically significant according to the interaction terms in Table IV (p ≥ 0.311).
Similar to ITL results, dynamic training did not reduce the effects of load (p = 1.000). External load significantly affected stopping efficacy (p = 0.007) but did not affect any other metric.
According to the interaction terms in Table IV, the impact of the training method was different for 3DOF and 2DOF subjects (p ≤ 0.003). While dynamic training significantly improved overall control according to all metrics for 2DOF subjects (p < 0.001), it did not significantly affect control for 3DOF subjects (p ≥ 0.512). However, 3DOF subjects had good control even with the static training method; they completed 86.11 ± 5.56% of all trials with the static training method and 90.28 ± 6.94% with the dynamic training method. In contrast, 2DOF subjects completed 61.98 ± 12.19% with the static training method and 83.33 ± 8.02% with the dynamic training method.
Again, the outcome measures resulting from dynamic training from all positions and loads were better or no different than the outcome measures from static training at P1 (the idealized case where training and testing were completed in the same limb position). However, unlike ITL subjects, these differences were not statistically significant.
IV. DISCUSSION
Previous work showed that limb position impacted offline PR classification rates in ITL [11]–[13], [24], [38] and AMP populations [10], [39] as well as real-time outcome measures in ITL subjects [12], [23], [24]. However, real-time limb position effects were minor in AMP subjects when the residual limb was unloaded [23]. These effects were not well understood and it was unknown how they would change if the residual limb was loaded. In this study, we addressed this gap by evaluating the effects of limb position and load on real-time PR control in ITL and AMP subjects. We also evaluated if a dynamic training method, adapted from [22], [23], [25], [27], would be able to mitigate these effects.
We found that limb position and load independently affected control for all subjects. Furthermore, the dynamic training method significantly improved controller performance compared to the static training method. This was expected because the dynamic training method encompassed more of the test workspace and increased training data variability. There were notable differences between each subject population.
A. Intact Limb Subjects
The results from the ITL subjects were consistent with previous findings showing that controllers were significantly affected by limb position when trained statically. All positions had significantly worse results compared to the position in which the controller was trained (P1). Subjects had the most difficulty in positions where elbow stabilization required more effort (P2 and P4). Many often commented that the controller drifted towards wrist supination. This was likely caused by increased activity in the brachioradialis, which assists with elbow flexion and also controls forearm pronation/supination. Although several other forearm muscles help with elbow flexion, the brachioradialis provides the most assistance. It is also more superficial and just distal to the elbow, close to where the electrodes were located. In extended elbow positions, this drift may have also been caused by changes in supinator activity. The drift was less noticeable in the dynamic sessions, suggesting that moving the arm throughout the workspace during training accounted for the changes in brachioradialis and supinator activity due to elbow flexion.
Even though dynamic training significantly improved results, limb position still impacted control, albeit in a less substantial way. Specifically, the completion rate range between limb positions in the static session was 40.08%, while the range from the dynamic session was 7.54%. Therefore, although it was not eliminated, the limb position effect was reduced significantly when the controllers were trained dynamically.
Notably, stopping efficacy was not affected by limb position after dynamic training. Previous work found that external loads increased baseline muscle activity and affected the classification of no movement [33]. By training with a load and with arm movements, we increased the threshold of the no movement class and reduced the likelihood of triggering unwanted movements in all limb positions.
B. Amputee Subjects
The results from the AMP subjects did not reiterate all the trends seen in ITL subjects or previous studies with offline analyses. P4 was the only limb position that significantly diminished controller performance, as opposed to P2, P3, and P4 in ITL subjects. AMP subjects were able to complete 58.33% of the trials in P4 in the static session. Although this was the worst completion rate for AMP subjects, it was still better than ITL subject performance in P2, P3, and P4 (Section III.A.1). Similar differences between subject populations were observed during offline prediction of kinematics [40]. These findings may be explained by the anatomical differences described in the introduction and the cited work. Unlike in ITL subjects, forearm muscles in AMP subjects were only affected by elbow joint moments. When the elbow was extended straight out (P4), the moment across it was maximized. This, in turn, influenced activation patterns that involved the brachioradialis and the supinator, thus reducing controllability. These changes may have been more extreme in ITL subjects because they also had to support wrist moments created by the weight of an intact hand.
Dynamic training eliminated all the effects of P4 for all metrics except completion time. Although we instructed subjects to flex and extend their elbow and shoulder during the dynamic training method, we did not enforce strict movements. Consequently, subjects had a tendency to stay within more comfortable positions during training and avoided straightening their arm out (P4). In the future, a more controlled training protocol that requires subjects to keep their arm straight out could be imposed. Alternatively, users could be instructed on how to compensate for residual limb loading by calibrating in the regions that are important for prosthesis usage (e.g. prosthesis guided recalibration [41]. We believe that these training methods would be sufficient to mitigate the effects of limb position.
Although there was a performance decrease as load increased, these changes were, for the most part, not statistically significant. Many of these subjects were consistent prosthesis-users and were therefore accustomed to supporting loads on their residual limb. However, given that we tested only three loads, more research is required to determine precisely how limb loading can impact performance as weights increase.
C. Limitations
One of the major limitations of this study was the influence of muscle fatigue. Although we allowed subjects to take frequent breaks, many remarked that the weight began to feel heavier over time. As fatigue set in, subjects had difficulty keeping their arm in the correct limb position, thus affecting test metrics such as completion rate and time. Therefore, changes in these metrics may not solely have been caused by changes in myoelectric control performance. Fatigue may have also affected the repeatability of control signals, which would have been apparent in the movement and stopping efficacy metrics.
Although we found statistical significance in some results, we do not know how this correlates to clinical or functional significance. The TAC test requires a level of precision that may be more than what is necessary for prosthesis usage in many tasks. For example, the virtual hand needs to stop halfway between opening and closing, which may be necessary when grasping a delicate object, but not required for many other objects. Hence, statistically significant effects on TAC test metrics may not be clinically significant. Future work should extend this work to include functional tests that are more clinically applicable.
Furthermore, we only had six AMP subjects. There was a wide range of skill levels; some subjects had participated in many previous experiments while others had never used PR before. With the small sample size and large variance, AMP subject data had lower statistical power than ITL subject data. This may explain the statistical differences between AMP and ITL subjects. However, as previously mentioned, statistical significance does not imply clinical significance.
Four AMP subjects used a 2DOF controller while all other subjects used a 3DOF controller. We found that this significantly impacted the limb position effect on stopping efficacy and completion time. With more decision boundaries, the 3DOF controller may have been more susceptible to misclassifications. This may have been exacerbated by limb position and load, resulting in bigger effects. Subjects who used the 2DOF controller also had fewer trials and may have experienced less fatigue. Nonetheless, the limb position effect in both AMP groups were still different from that in ITL groups.
Our conclusions were also limited by the number of limb positions and loads that were tested. By constraining the limb positions to the sagittal plane, we isolated the effects of shoulder and elbow flexion/extension on controller performance. However, control may also be affected by limb positions that require abduction/adduction, humeral rotation, and other DOFs. Furthermore, we chose to limit our heaviest load to 600g to prevent fatigue. In reality, individuals may use heavier prostheses or carry larger objects. Although we did not find any significant interactions between limb position and load, this result may not hold with different limb positions and heavier loads.
Since we only used PR-based controllers, we may not be able to generalize our conclusions to other myoelectric controllers. However, our AMP subject results were consistent with the results from studies with regression-based controllers [21], [42]. Specifically, both studies found that real-time control in AMP subjects was mainly affected by the arm out position (P4). Our load effects were larger than the effects on a musculoskeletal model-based controller [43]. However, they did not include wrist rotation, which was the most affected DOF in our study.
Finally, our electrode and load-bearing setup was not representative of a typical socket with embedded dry electrodes. With a clinically prescribed socket, different limb positions and loads may cause electrode shift or liftoff. Even though it may not have accurately reflected real-world conditions, we chose to use our setup so that we could isolate the physiological effects of limb position and load. Although ITL subjects used dry electrodes, we ensured that the armbands were worn tightly and that the electrodes did not shift throughout the experiment.
V. CONCLUSION
In this study, we evaluated the effects of limb position, load, and training method on real-time pattern recognition control in intact limb and amputee subjects. We showed that limb position and load significantly and independently affect controller performance when static training is used. However, these effects are different in AMP subjects and ITL subjects and may not be as pronounced as previous offline results have shown. This highlights the importance of testing controllers in real-time with their intended end user. We also showed that increasing external loads diminishes controllability, although these changes may not be statistically significant in AMP subjects. Finally, dynamic training reduces the effects of limb position but not load and substantially improves overall controller performance. In the future, the dynamic training method should be adapted to require more training with the arm straight out, since this was found to be the most problematic position.
Supplementary Material
Fig. 3.
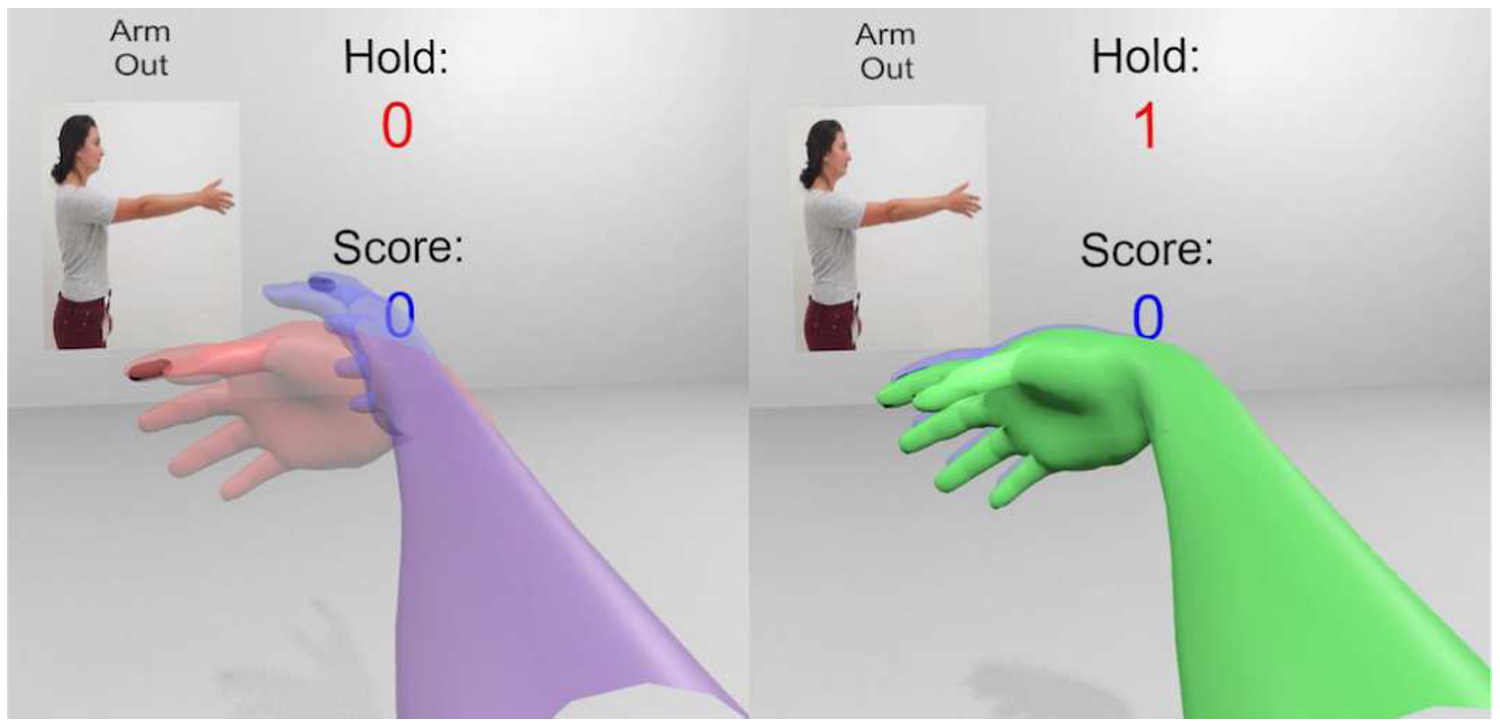
Example of a TAC test trial from the subjects view in the VR headset. In this trial, the user had to straighten their arm out (P4) and move the blue hand into the red target hand using wrist flexion (left). When the blue and red hands matched, the arm turned green (right).
Acknowledgment
The authors would like to thank Kristi Turner and Laura Miller for their assistance with amputee data collection.
This work was supported by the National Institutes of Health NIH R01HD094861 and the Congressionally Directed Medical Research Program W81XWH-17-1-0332.
Contributor Information
Yuni Teh, Regenstein Center for Bionic Medicine at the Shirley Ryan AbilityLab and the Department of Biomedical Engineering, Northwestern University, Chicago, IL 60611 USA..
Levi J. Hargrove, Regenstein Center for Bionic Medicine at the Shirley Ryan AbilityLab and the Departments of Physical Medicine and Rehabilitation and Biomedical Engineering at Northwestern University, Chicago, IL 60611, USA.
References
- [1].Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, and Brookmeyer R, “Estimating the prevalence of limb loss in the United States: 2005 to 2050,” Arch. Physical Med. and Rehabil, vol. 89, no. 3, pp. 422–429, 2008. [DOI] [PubMed] [Google Scholar]
- [2].Dillingham TR, Pezzin LE, and MacKenzie EJ, “Limb amputation and limb deficiency: epidemiology and recent trends in the United States,” Southern Medical Journal, vol. 95, no. 8, pp. 875–884, 2002. [DOI] [PubMed] [Google Scholar]
- [3].Routhier F, Vincent C, Morissette M, and Desaulniers L, “Clinical results of an investigation of paediatric upper limb myoelectric prosthesis fitting at the Quebec Rehabilitation Institute,” Prosthetics Orthotics Int, vol. 25, no. 2, pp. 119–131, 2001. [DOI] [PubMed] [Google Scholar]
- [4].Datta D, Selvarajah K, and Davey N, “Functional outcome of patients with proximal upper limb deficiency–acquired and congenital,” Clin. Rehabil, vol. 18, no. 2, pp. 172–177, 2004. [DOI] [PubMed] [Google Scholar]
- [5].Davidson J, “A survey of the satisfaction of upper limb amputees with their prostheses, their lifestyles, and their abilities,” J. Hand Therapy, vol. 15, no. 1, pp. 62–70, 2002. [DOI] [PubMed] [Google Scholar]
- [6].Jang CH, Yang HS, Yang HE, Lee SY, Kwon JW, Yun BD, Choi JY, Kim SN, and Jeong HW, “A survey on activities of daily living and occupations of upper extremity amputees,” Ann. Rehabil. Med, vol. 35, no. 6, p. 907, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Fernandez A, Isusi I, and Gomez M, “Factors conditioning the return to work of upper limb amputees in Asturias, Spain,” Prosthetics Orthotics Int, vol. 24, no. 2, pp. 143–147, 2000. [DOI] [PubMed] [Google Scholar]
- [8].Montagnani F, Controzzi M, and Cipriani C, “Is it finger or wrist dexterity that is missing in current hand prostheses?” IEEE Trans. Neural Syst. Rehabil. Eng, vol. 23, no. 4, pp. 600–609, 2015. [DOI] [PubMed] [Google Scholar]
- [9].Castellini C, Fiorilla AE, and Sandini G, “Multi-subject/daily-life activity EMG-based control of mechanical hands,” J. NeuroEng. Rehabil, vol. 6, no. 41, pp. 1–11, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Chen L, Geng Y, and Li G, “Effect of upper-limb positions on motion pattern recognition using electromyography,” in Proc. Int. Congr. Image and Signal Process, vol. 1, 2011, pp. 139–142. [Google Scholar]
- [11].Fougner A, Scheme E, Chan AD, Englehart K, and Stavdahl Ø, “Resolving the limb position effect in myoelectric pattern recognition,” IEEE Trans. Neural Syst. Rehabil. Eng, vol. 19, no. 6, pp. 644–651, 2011. [DOI] [PubMed] [Google Scholar]
- [12].Khushaba RN, Takruri M, Miro JV, and Kodagoda S, “Towards limb position invariant myoelectric pattern recognition using time-dependent spectral features,” Neural Networks, vol. 55, pp. 42–58, 2014. [DOI] [PubMed] [Google Scholar]
- [13].Liu J, Zhang D, Sheng X, and Zhu X, “Quantification and solutions of arm movements effect on sEMG pattern recognition,” Biomed. Signal Process. and Control, vol. 13, pp. 189–197, 2014. [Google Scholar]
- [14].Khushaba RN, Al-Timemy A, Kodagoda S, and Nazarpour K, “Combined influence of forearm orientation and muscular contraction on EMG pattern recognition,” Expert Syst. Appl, vol. 61, pp. 154–161, 2016. [Google Scholar]
- [15].Yang D, Yang W, Huang Q, and Liu H, “Classification of multiple finger motions during dynamic upper limb movements,” IEEE J. Biomed. Health Inform, vol. 21, no. 1, pp. 134–141, 2015. [DOI] [PubMed] [Google Scholar]
- [16].You K-J, Rhee K-W, and Shin H-C, “Finger motion decoding using EMG signals corresponding various arm postures,” Exp. Neurobiol, vol. 19, no. 1, pp. 54–61, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Campbell E, Phinyomark A, and Scheme E, “Current trends and confounding factors in myoelectric control: Limb position and contraction intensity,” Sensors, vol. 20, no. 6, p. 1613, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Radmand A, Scheme E, and Englehart K, “A characterization of the effect of limb position on EMG features to guide the development of effective prosthetic control schemes,” in Proc. Int. Conf. IEEE Eng. Med. and Biol. Soc, 2014, pp. 662–667. [DOI] [PubMed] [Google Scholar]
- [19].Boschmann A and Platzner M, “Towards robust HD EMG pattern recognition: Reducing electrode displacement effect using structural similarity,” in Proc. Int. Conf. IEEE Eng. Med. and Biol. Soc, 2014, pp. 4547–4550. [DOI] [PubMed] [Google Scholar]
- [20].Masters MR, Smith RJ, Soares AB, and Thakor NV, “Towards better understanding and reducing the effect of limb position on myoelectric upper-limb prostheses,” in Proc. Int. Conf. IEEE Eng. Med. and Biol. Soc, 2014, pp. 2577–2580. [DOI] [PubMed] [Google Scholar]
- [21].Hwang H-J, Hahne JM, and Müller K-R, “Real-time robustness evaluation of regression based myoelectric control against arm position change and donning/doffing,” PLOS ONE, vol. 12, no. 11, pp. 1–22, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Radmand A, Scheme EJ, and Englehart K, “On the suitability of integrating accelerometry data with electromyography signals for resolving the effect of changes in limb position during dynamic limb movement,” J. Prosthetics and Orthotics, vol. 26, no. 4, pp. 185–193, 2014. [Google Scholar]
- [23].Woodward RB and Hargrove LJ, “Adapting myoelectric control in real-time using a virtual environment,” J. NeuroEng. Rehabil, vol. 16, no. 11, pp. 1–12, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Betthauser JL, Hunt CL, Osborn LE, Masters MR, Lévay G, Kaliki RR, and Thakor NV, “Limb position tolerant pattern recognition for myoelectric prosthesis control with adaptive sparse representations from extreme learning,” IEEE Trans. Biomed. Eng, vol. 65, no. 4, pp. 770–778, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Beaulieu RJ, Masters MR, Betthauser J, Smith RJ, Kaliki R, Thakor NV, and Soares AB, “Multi-position training improves robustness of pattern recognition and reduces limb-position effect in prosthetic control,” J. Prosthetics and Orthotics, vol. 29, no. 2, p. 54, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Ishii A, Kondo T, and Yano S, “Improvement of EMG pattern recognition by eliminating posture-dependent components,” in Int. Conf. Intel. Auton. Sys, 2016, pp. 19–30. [Google Scholar]
- [27].Yang D, Gu Y, Jiang L, Osborn L, and Liu H, “Dynamic training protocol improves the robustness of PR-based myoelectric control,” Biomed. Signal Process Control, vol. 31, pp. 249–256, 2017. [Google Scholar]
- [28].Yu Y, Sheng X, Guo W, and Zhu X, “Attenuating the impact of limb position on surface EMG pattern recognition using a mixed-LDA classifier,” in Proc. Int. Conf. IEEE Robot. Biomimetics, 2017, pp. 1497–1502. [Google Scholar]
- [29].Geng Y, Samuel OW, Wei Y, and Li G, “Improving the robustness of real-time myoelectric pattern recognition against arm position changes in transradial amputees,” Biomed. Res. Int, vol. 2017, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Hargrove L, Losier Y, Lock B, Englehart K, and Hudgins B, “A real-time pattern recognition based myoelectric control usability study implemented in a virtual environment,” in Proc. Int. Conf. IEEE Eng. Med. and Biol. Soc, 2007, pp. 4842–4845. [DOI] [PubMed] [Google Scholar]
- [31].Ortiz-Catalan M, Rouhani F, Brånemark R, and Håkansson B, “Offline accuracy: a potentially misleading metric in myoelectric pattern recognition for prosthetic control,” in Proc. Int. Conf. IEEE Eng. Med. and Biol. Soc, 2015, pp. 1140–1143. [DOI] [PubMed] [Google Scholar]
- [32].Kendall F and McCreary E, Muscles Testing and Function, 3rd ed. Baltimore: Williams & Wilkens, 1983. [Google Scholar]
- [33].Cipriani C, Controzzi M, Kanitz G, and Sassu R, “The effects of weight and inertia of the prosthesis on the sensitivity of electromyographic pattern recognition in relax state,” J. Prosthetics and Orthotics, vol. 24, no. 2, pp. 86–92, 2012. [Google Scholar]
- [34].Scheme E, Lock B, Hargrove L, Hill W, Kuruganti U, and Englehart K, “Motion normalized proportional control for improved pattern recognition-based myoelectric control,” IEEE Trans. Neural Syst. Rehabil. Eng, vol. 22, no. 1, pp. 149–157, 2013. [DOI] [PubMed] [Google Scholar]
- [35].Simon AM, Stern K, and Hargrove LJ, “A comparison of proportional control methods for pattern recognition control,” in Proc. Int. Conf. IEEE Eng. Med. and Biol. Soc, 2011, pp. 3354–3357. [DOI] [PubMed] [Google Scholar]
- [36].Bajaj NM, Spiers AJ, and Dollar AM, “State of the art in prosthetic wrists: Commercial and research devices,” in Proc. IEEE Int. Conf. Rehabil. Robot, 2015, pp. 331–338. [Google Scholar]
- [37].Fitts PM, “The information capacity of the human motor system in controlling the amplitude of movement,” J. Exp. Psychol, vol. 47, no. 6, p. 381, 1954. [PubMed] [Google Scholar]
- [38].Scheme E, Biron K, and Englehart K, “Improving myoelectric pattern recognition positional robustness using advanced training protocols,” in Proc. Int. Conf. IEEE Eng. Med. and Biol. Soc, 2011, pp. 4828–4831. [DOI] [PubMed] [Google Scholar]
- [39].Geng Y, Zhou P, and Li G, “Toward attenuating the impact of arm positions on electromyography pattern-recognition based motion classification in transradial amputees,” J. NeuroEng. Rehabil, vol. 9, no. 1, p. 74, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Jiang N, Muceli S, Graimann B, and Farina D, “Effect of arm position on the prediction of kinematics from EMG in amputees,” Med. Biol. Eng. Comput, vol. 51, no. 1–2, pp. 143–151, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Simon AM, Lock BA, and Stubblefield KA, “Patient training for functional use of pattern recognition-controlled prostheses,” J. Prosthetics and Orthotics, vol. 24, no. 2, pp. 56–64, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Hahne JM, Schweisfurth MA, Koppe M, and Farina D, “Simultaneous control of multiple functions of bionic hand prostheses: Performance and robustness in end users,” Sci. Robot, vol. 3, no. 19, p. eaat3630, 2018. [DOI] [PubMed] [Google Scholar]
- [43].Pan L, Harmody A, and Huang H, “A reliable multi-user EMG interface based on a generic-musculoskeletal model against loading weight changes,” in Proc. Int. Conf. IEEE Eng. Med. and Biol. Soc, 2018, pp. 2104–2107. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


