Abstract
Background and aims
The COVID-19 spreads rapidly around the world which has brought a global health crisis. The pathogen of COVID-19 is SARS-COV-2, and previous studies have proposed the relationship between ABO blood group and coronavirus. Here, we aim to delve into the association between ABO blood group and COVID-19 infection, severity and demise.
Methods
The relevant studies were retrieved from five databases: PubMed, MedRxiv, BioRxiv,Web of Science and CNKI. Members of cases(symptomatic cases, severe cases, died cases) and controls(asymptomatic controls, non-severe controls, alive controls) were extracted from collected studies. Odds ratios (OR) and 95% confidence intervals (CI) were calculated and interpreted from extracted data. Publication bias and sensitivity analysis were also applied to confirm our discovery.
Results
Overall 31,100 samples were included in the analysis. Compared to other ABO blood type, an increased odds of infecting COVID-19 among individuals with A blood group (OR: 1.249, 95%CI: 1.114–1.440, P < 0.001) and a decreased odds of infecting COVID-19 among individuals with blood group O (OR: 0.699, 95%CI: 0.635–0.770, P < 0.001) were found. Besides, individuals with blood group AB seems to link a higher risk to COVID-19 severity (OR: 2.424, 95%CI: 0.934–6.294) and demise (OR: 1.348, 95%CI: 0.507–3.583). Meantime, individuals with O blood group might had lower risk to COVID-19 severity (OR: 0.748, 95%CI: 0.556–1.007), and individuals with B blood group were likely to relate a lower risk to COVID-19 demise.
Conclusions
The current meta-analysis suggest that blood type A might be more susceptible to infect COVID-19 while blood type O might be less susceptible to infect COVID-19; there were no correlation between ABO blood group and severity or demise of COVID-19. However, more investigation and research are warranted to clarify the relationship between COVID-19 and ABO blood type.
Keywords: ABO blood group system, COVID-19, Susceptibility, Mortality, Meta-analysis, Systematic review
Highlights
-
•
A novel coronavirus, SARS-Cov-2 was emerged in December 2019 in China.
-
•
There were over 5.1 million cases of COVID-19 diagnosed and over 332,000 people had died in the whole world by May22, 2020.
-
•
The first review and a meta-analysis about relationship between ABO blood group and COVID-19 infection, severity and demise.
-
•
We found that individuals with blood type A and O have a higher and lower risk of infecting SARS-COV-2, respectively.
1. Introduction
A novel coronavirus disease-2019 (COVID-19) outbreak was reported in Wuhan, Hubei province, P.R.C, in December 2019, and quickly spread to all provinces and municipalities nationwide in China, even spread around the world. The pathogen is a novel coronavirus (SARS-COV-2) which was never found by humans before has been named as COVID-19 by the World Health Organization officially in February 2020 (Liu et al., 2020). SARS-COV-2 also targets the respiratory tract and shares multiple similar clinical symptoms with MERS-COV and SARS-COV (Li et al., 2020). The most common symptoms of COVID-19 involved fatigue, fever and dry cough, followed always by myalgia, anorexia, dyspnea, and so on (Ahn et al., 2020). There were more than 5.1 million cases of COVID-19 diagnosed in the whole world, and more than 332,000 people had died by May 22, 2020. At present, there are already 10 countries in the world with a cumulative number of more than 100,000 diagnosed cases (Lippi and Plebani, 2020). Among them, the United States is still the country with the largest number of diagnoses in the world, with a cumulative total of 1,618,000 confirmed cases. Therefore, following Middle East respiratory syndrome coronavirus (MERS-COV) and severe acute respiratory syndrome coronavirus (SARS-COV), and SARS-COV-2 has been the third coronavirus that causes infections worldwide in the past 20 years. A public health threat was made by outbreak of COVID-19, and overall countries are allocating scientific and medical resources to fight the COVID-19 pandemic (Zeng et al., 2020).
As the most widely investigated erythrocyte antigen system and straightforward accessible element in an individual's genetic makeup (Mao et al., 2019), ABO blood group system is used in clinical practice extensively (Wang et al., 2014; Cooling, 2015). After ABO blood group system was found by Karl Landsteiner in 1901, we never interrupted searching for the relationship between ABO blood group system and various diseases (Lesky, 1973). It has been suggested that ABO blood group system is related to many bacterial (Alpoim et al., 2013) and virus infection, such as helicobacter pylori (Chakrani et al., 2018), norovirus (Liao et al., 2020), HBV (Jing et al., 2020), SARS-COV (Guillon et al., 2008) and MERS-COV (Varughese et al., 2015). Recently, several studies about COVID-19 in China and America discovered relationships between ABO blood group and COVI9–19 infection, severity and demise (Zhao et al., 2020; Zietz and Tatonetti, 2020). However, there are some contradictions in the results of the studies. Zhao et al. (2020) found that COVID-19 infection was higher in AB blood group, but Zietz and Tatonetti (2020) found that AB blood group was related with decreased COVID-19 infection. Moreover, Zhao et al. (2020) found A blood group links to higher mortality of COVID-19, O blood group links to lower mortality; Zeng et al. (2020) has not yet find any association between blood type and COVID-19 mortality. The contradiction from included studies could due to small sample size, residual con-founding from population heterogeneity, region difference etc.
In present study, we performed a review with meta-analysis comprehensive and summarized literature systematically on the relationship of ABO blood group with COVID-19 infection, severity and demise. The objective of this was therefore to prevent COVID-19 infection, and provide more vigilant surveillance and aggressive treatment to susceptible blood type, which can assist in accomplishing the target of eliminating COVID-19 as a cosmopolitan public health challenge.
2. Methods
2.1. Database and search strategy
A systematic and comprehensively online search for published literature was carried out in PubMed, MedRxiv, BioRxiv, Web of Science and CNKI with the MESH (medical subject heading) terms “ABO blood group” and “COVID-19”. In order to expand our search scale, we also conducted a full-text search with search terms “COVID-19”, “blood group” and “ABO”. The time for the searching article to be published were limited between November 1st 2019 to April 20th 2020, and there was no limitation of region. We identified studies and did screening, selection and data extraction manually.
2.2. Study selection
Inclusion criteria were as fulfilled: 1) a clear extractable typing of ABO blood type; 2) studies contain impersonal diagnosed COVID-19+ and normal individuals; 3) studies contain severe and mild patients infected with COVID-19; 4) studies contain dead and alive patients infected with COVID-19; 5) studies providing original data. After removing duplicates, articles' titles and abstracts were screened and whole contents of qualified articles critiqued by two authors independently with the inclusion criteria.
2.3. Data extraction
Four authors reached a consensus on all items. We chose a data collection standard to extract the following information: 1) the first author; 2) publication year; 3) country of the participants; 4)study design; 5)sample size; 6)gender ratio; 7)symptomatic cases and asymptomatic controls; 8)severe cases and non-severe controls; 9) died cases and live controls. When there was a controversy over a study, all reviewer intervened to determine whether the study can be included or not.
2.4. Methodological quality assessment of the included studies
The quality of studies was adapted to assess based on the Newcastle–Ottawa Scale (NOS) (Cota et al., 2013). All included studies were rated based on three main domains, including selection, comparability and exposure. The supreme score for each dimensions was 4 points, 2 points and 3 points, respectively (Stang, 2010). Therefore, we classified studies as poor quality if they scored 0–3 points, fair quality if they scored within the range of 4-5points, if they scored within the range of 6–8 points or 9–10 points, we think them as high-quality studies or excellent-quality studies.
2.5. Statistical analysis
Statistical analysis for included studies were carried out using Stata. Pooled odds ratios (ORs) and 95% confidence interval (CIs) were obtained using either fix-effects model or random-effects model to measure the association between the ABO blood group and infection, severity, and mortality of COVID-19. A random-effects model was applied when there was high heterogeneity (Moran's I2 ≥ 30% or P ≤ 0.05), likewise, the fixed-effects model was applied (Moran's I2 < 30% or P > 0.05) (Dersimonian and Kacker, 2007; Ioannidis, 2008). Besides, Egger's regression test and Begg's adjusted rank correlation test were used to evaluated publication bias (bias if P < 0.1) (Ioannidis and Trikalinos, 2007; Hayashino et al., 2005). Meanwhile, we used sensitivity analysis to examine robustness of the overall summary effects (Egger et al., 1997).
3. Results
3.1. Overall outcomes
The search resulted in a total of 186 studies from 5 databases: PubMed (n = 87), MedRxiv (n = 12), BioRxiv (n = 4), Web of Science (n = 12) and CNKI (n = 71). With 111 studies subsequently removed because they were duplicates. Following the inclusion criteria, we excluded the 69 irrelevant studies by screening abstract and title. Finally, a total of 4 articles that included in quantitative synthesis were included in this systematic review and meta-analysis. The details of the methodological quality and classification of the studies are showed in Fig. 1 .
Fig. 1.
Flow diagram showing selection of studies.
3.2. Characteristics of the included studies
We identified 4 (Zeng et al., 2020; Zhao et al., 2020; Zietz and Tatonetti, 2020; Xiang et al., 2020) studies that met our inclusion criteria for meta-analysis. Selected characteristics of the study participants are shown in Table 1 . All studies were published in 2020, and 3 in China, 1 in the United States. Of all the studies, 2 were considered in high quality(scored ≥7), 2 were considered in mediate quality (score 6 points). In first study, distributions of ABO blood groups from Shenzhen (cases from Shenzhen Third People's Hospital, controls from Shenzhen general population) and Wuhan (cases from Wuhan Jinyintan Hospital and Renmin Hospital of Wuhan University, controls from Wuhan general population). The second study, attributing to the insufficient number of patients that individuals of AB blood group were not statistically analyzed. In third study, distributions from New York City data, which from the CUIMC EHR/NYP system. In forth study, distributions of blood groups from the First Affiliated Hospital of Nanchang University.
Table 1.
Characteristic of included studies.
| Study | Country | Study design | Sample | Age | Gender (M/F) | Symptomatic cases | Asymptomatic controls | Severe cases | Non-severe controls | Died cases | Alive controls | NOS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Zeng et al. (2020) | China | Retrospective | 234 | >13 | 133/101 | 0 | 0 | 97 | 137 | 21 | 76 | 6 |
| Zhao et al. (2020) | China | Retrospective | 5469 | NR | NR | 1775 | 3694 | 0 | 0 | 206 | 1569 | 8 |
| Zhao et al. (2020) | China | Retrospective | 3807 | NR | NR | 113 | 3694 | 0 | 0 | 0 | 0 | 8 |
| Zhao et al. (2020) | China | Retrospective | 23,671 | NR | NR | 285 | 23,386 | 0 | 0 | 0 | 0 | 8 |
| Zietz and Tatonetti (2020) | Columbia | Retrospective | 1559 | NR | 716/843 | 682 | 877 | 179 | 423 | 80 | 602 | 8 |
| Xiang et al. (2020) | China | Retrospective | 54 | 18–78 | 33/16 | 0 | 0 | 5 | 49 | 0 | 0 | 6 |
M/F:male/female.
NOS: Newcastle–Ottawa Scale.
NR: Not reported.
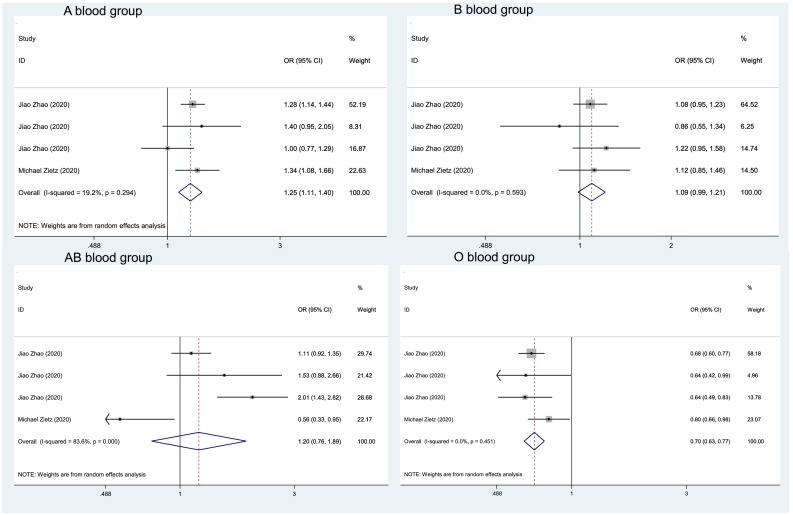
3.3. Associations between ABO blood group and COVID-19 infection
Results of the relationship between ABO blood type and infection of COVID-19 were recorded in Table 2 . In blood group A and blood group non-A (OR: 1.249, 95%CI: 1.114–1.440, P < 0.001), the meta-analysis in Fig. 2 showed that people with blood type A were related to an increased risk of COVID-19 infection compared to non-A blood group. Besides, people with blood type O were related to a decreased risk of COVID-19 infection compared to non-O blood type (OR: 0.699, 95%CI: 0.635–0.770, P < 0.001). The random-effects model was applied to above two analyses. Studies with blood type B and non-B were analyzed with no statistical significance ((I2 = 0, P = 0.593) using a fixed-effects model. Studies with blood type AB and non-AB were analyzed also with no statistical significance (I2 = 83.6%, P = 0) using a random-effects model.
Table 2.
Results of the infection analysis.
| First author, Year | COVID-19+ |
COVID-19- |
COVID-19+ |
COVID-19- |
COVID-19+ |
COVID-19- |
COVID-19+ |
COVID-19- |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | Non-A | A | Non-A | B | Non-B | B | Non-B | AB | Non-AB | AB | Non-AB | O | Non-O | O | Non-O | |
| Jiao Zhao, 2020 | 670 | 1105 | 1188 | 2506 | 469 | 1306 | 920 | 2774 | 178 | 1597 | 336 | 3358 | 458 | 1317 | 1250 | 2444 |
| Jiao Zhao, 2020 | 45 | 68 | 1188 | 2506 | 25 | 88 | 920 | 2774 | 15 | 98 | 336 | 3358 | 28 | 85 | 1250 | 2444 |
| Jiao Zhao, 2020 | 82 | 203 | 6728 | 16,658 | 83 | 202 | 5880 | 17,506 | 39 | 246 | 1712 | 21,674 | 81 | 200 | 9066 | 14,320 |
| Michael Zietz, 2020 | 233 | 449 | 245 | 632 | 116 | 566 | 136 | 741 | 21 | 661 | 47 | 830 | 312 | 370 | 449 | 428 |
Fig. 2.
Meta-analysis forest of the infection of ABO blood groups for COVID-19.
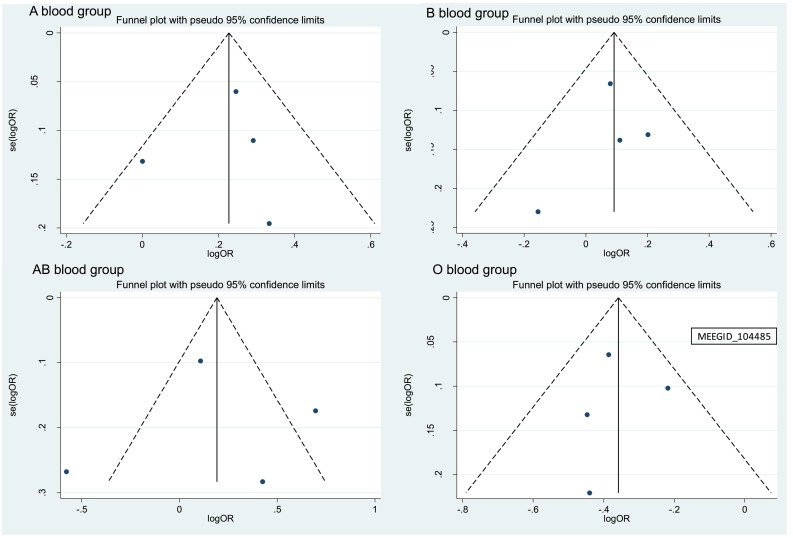
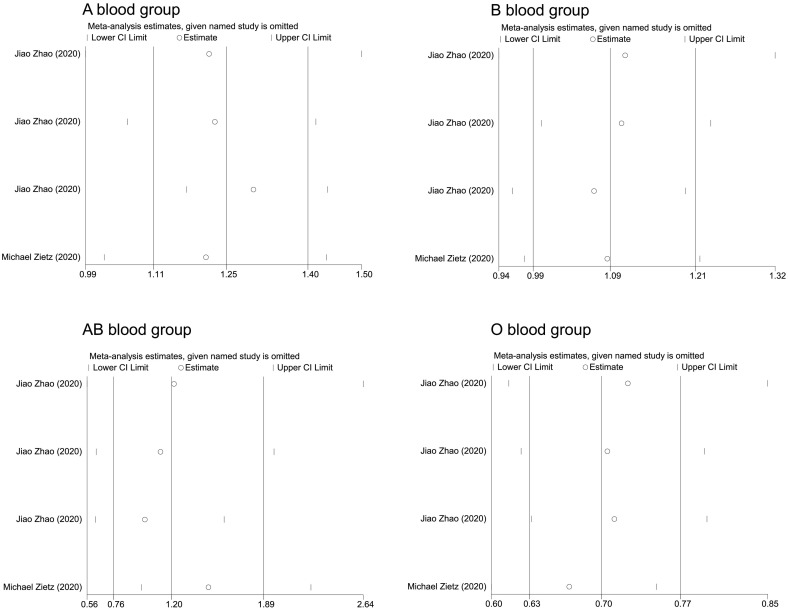
Fig. 3 shows the publication bias. The Egger's test and Begg's test suggested no significant publication bias among individuals with blood type A and non-A, blood type B and non—B, blood type AB and non-AB, blood type O and non—O. Begg's test for asymmetry P = 0.810, 0.764, 0.997, and 0.923, respectively. Egger's test for asymmetry P = 1.000, 0.937, 1.000 and 1.000, separately. Sensitivity analyses in Fig. 4 shows the pooled estimated did not transform too much, it means the results of meta-analysis were robust.
Fig. 3.
Publication bias of the infection of ABO blood groups for COVID-19.
Fig. 4.
Sensitively analyzes of the infection of ABO blood groups for COVID-19.
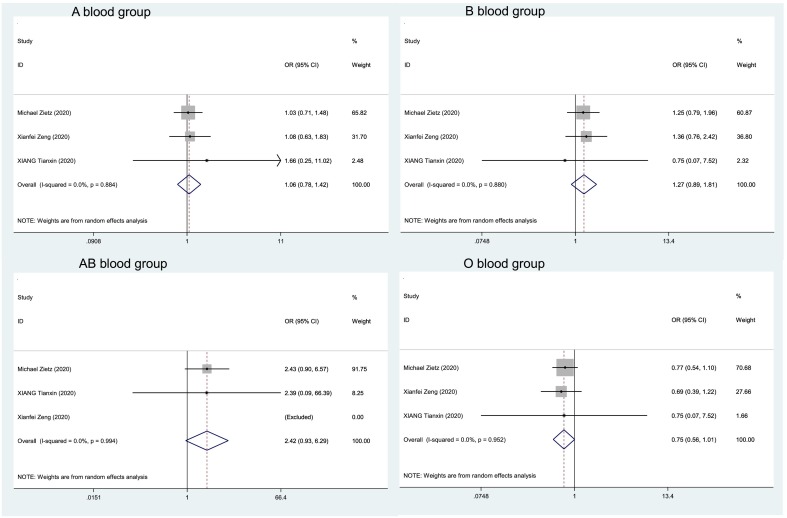
3.4. Associations between ABO blood group and COVID-19 severity
Results of the relationship between ABO blood type and severity of COVID-19 were shown in Table 3 . We used random-effects models on following 4 studies. The meta-analysis in Fig. 5 showed that individuals with blood group AB were related to an increased risk of severe COVID-19 compared to blood group non-AB with an OR of 2.424 (95%CI: 0.934–6.294, P = 0.069). Meanwhile, compared to other ABO blood groups, individuals with A blood group (OR: 1.055, 95%CI: 0.783–1.422, P = 0.723) and B blood group (OR: 1.271, 95%CI: 0.894–1.806, P = 0.181) seemed to have a trend of higher risk for severity. On the other hand, result of individuals with blood group O showed a reduced risk of severe COVID-19 compared with non-O (OR: 0.748, 95CI%: 0.556–1.077, P = 0.056). Overall, the four results are lack of statistical significance.
Table 3.
Results of the severity analysis.
| First author, Year | Severe |
Non-severe |
Severe |
Non-severe |
Severe |
Non-severe |
Severe |
Non-severe |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | Non-A | A | Non-A | B | Non-B | B | Non-B | AB | Non-AB | AB | Non-AB | O | Non-O | O | Non-O | |
| Xianfei Zeng, 2020 | 40 | 57 | 54 | 83 | 30 | 67 | 34 | 103 | 0 | 97 | 0 | 137 | 27 | 70 | 49 | 88 |
| Michael Zietz 2020 | 62 | 117 | 144 | 279 | 35 | 144 | 69 | 354 | 8 | 171 | 8 | 415 | 74 | 105 | 202 | 221 |
| Xiang Tianxin, 2020 | 3 | 2 | 19 | 21 | 1 | 4 | 10 | 30 | 0 | 5 | 1 | 39 | 1 | 4 | 10 | 30 |
Fig. 5.
Meta-analysis forest of the severity of ABO blood groups for COVID-19.
Publication bias of four groups that used Begg's test. Blood group A vs group non-A (P = 0.296), blood group B vs group non-B (P = 1.000), blood group AB vs group non-AB (P = 1.000) and blood group O vs group non-O (P = 1.000), thus there was no prominent publication bias. What's more, we also conducted sensitivity analysis on them, and we found no substantial alteration to the results after moving whichever study and re-analyzing the data sets.
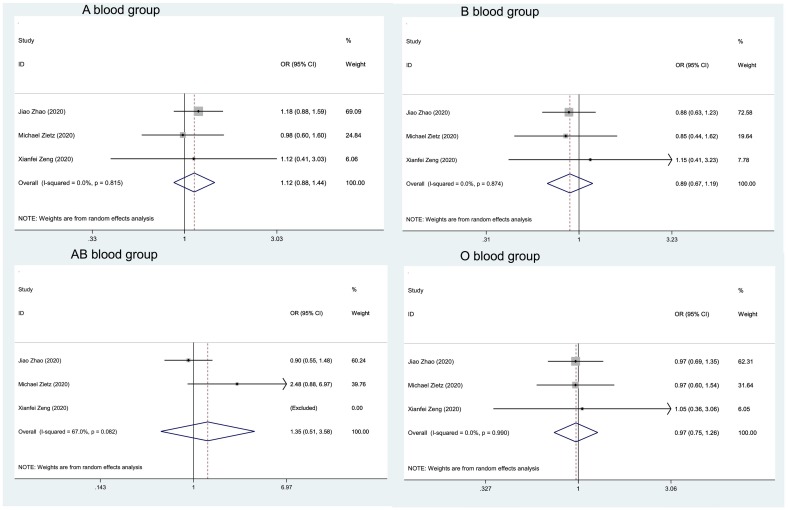
3.5. Associations between ABO blood group and COVID-19 demise
Fig. 6 shows the estimates of ORs of the associations between ABO blood group and COVID-19 demise on the pooled data from our studies by random effects models. Similarly, compared with individuals with blood group O and blood group B, individuals with blood group A and blood group AB were associated with an increased the risk of death (for group A, OR: 1.124, 95%CI: 0.879–1.124, P = 0.352; for group AB, OR: 1.348, 95%CI: 0.507–1.348, P = 0.549). However, individuals with blood group B (OR: 0.891, 95%CI: 0.669–1.422, P = 0.433) and blood group O (OR: 0.972, 95%CI: 0.746–1.265, P = 0.831) seemed to have a higher mortality rate. Above all, the meta-analysis attach to no statistical significance (Table 4 ).
Fig. 6.
Meta-analysis forest of the mortality of ABO blood groups.
Table 4.
Results of the demise analysis.
| First author, Year | Year | Died |
Alive |
Died |
Alive |
Died |
Alive |
Died |
Alive |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | Non-A | A | Non-A | B | Non-B | B | Non-B | AB | Non-AB | AB | Non-AB | O | Non-O | O | Non-O | ||
| Xianfei Zeng, 2020 | 2020 | 8 | 13 | 27 | 49 | 7 | 14 | 23 | 53 | 0 | 21 | 0 | 76 | 6 | 15 | 21 | 55 |
| Jiao Zhao, 2020 | 2020 | 85 | 121 | 585 | 984 | 50 | 156 | 419 | 1150 | 19 | 187 | 159 | 1410 | 52 | 154 | 406 | 1163 |
| Michael Zietz, 2020 | 2020 | 27 | 53 | 206 | 396 | 12 | 68 | 104 | 498 | 5 | 75 | 16 | 596 | 36 | 44 | 276 | 326 |
It suggested no asymmetry in the exploration for the plots of blood types in demise of COVID-19, and Begg's test didn't provide proof for publication bias among individuals with blood group A and non-A(P = 1.000), blood group B and non-B (P = 1.000), blood group AB and non-AB (P = 1.000), blood group O and non-O (P = 0.296). Next, we did the sensitively analyzes of four sets of data. After omitting the study by any of them, the pooled ORs did not alter much that the results of analysis were likely to robust.
4. Discussion
In current study, we found that individuals with blood type A link a higher risk of infecting COVID-19 (OR: 1.249, 95%CI: 1.114–1.400), whereas individuals with blood type O link a lower risk to COVID-19 infection (OR: 0.699, 95%CI: 0.635–0.770). Above findings have highly statistically significance. Besides, the odds of COVID-19 severity were higher in individuals with blood group AB (OR: 2.424, 95%CI: 0.934–6.294), and lower in individuals with blood group O (OR: 0.748, 95%CI: 0.556–1.007); blood group AB were at increased risk of COVID-19 demise (OR: 1.348, 95%CI: 0.507–3.583), while blood group B were at decreased risk of it (OR: 0.891, 95%CI: 0.669–1.188).
The results we carried out were incomplete consistent to other analytical studies. According to Zhao et al. (2020), individuals with blood group A might be more susceptible to infect COVID-19 and have a higher mortality than non-A blood group, while those with blood group O might have a protective effect. The feasible explanation for inconsistence is the difference between individuals of the same blood type from different races and regions. In study by Zietz and Tatonetti (2020) it showed a decreased risk of COVID-19 infection among individuals with blood type O, what's more, it also suggested that significant association only between A+ (blood type A and Rh+) and O+ (blood type O and Rh+) after further stratifying by Rh. Given the number of Rh blood groups are fewer in our samples, we didn't conduct further analyses, so this issue needs further research and discussion. In other study by Zeng et al. (2020) found the odds of COVID-19 infection was higher in individuals with A blood group, but they were unable to find O blood group could be protective against COVID-19 infection, instead, their study showed blood group O were at lower risk of severe COVID-19., it was probably due to the sample size.
Though the mechanism of ABO blood type in COVID-19 infection has yet to elucidate, we still propose the following conjectures based on conclusions drawn by predecessors. ABO blood group is specific antigen type on erythrocyte membrane, but blood group antigens is expressed in airway epithelial cells, alveolar epithelial cells and even in body fluids Stowell and Stowell (2019). Firstly, we supposed through binding receptor-mediated affinity, genetic susceptibility of blood group glycoproteins can function, particularly invasion mechanism. And the study by Cooling has proved blood group antigens are valid receptors for some infections microorganisms (Cooling, 2015; Mackenzie et al., 1977). Given our knowledge of the SARS virus, the adhesion of SARS-COV S protein-expressing cells could be inhibited specifically by anti-A antibodies (Guillon et al., 2008; Cheng et al., 2005), simultaneously, SARS-COV and SARS-COV-2 have similar nucleic acid sequence and similar receptor combination with angiotensin-converting enzyme 2 (ACE2) (Wan et al., 2020; Gheblawi et al., 2020; Wang et al., 2020). Thus, we suspect that anti-A antibodies will play a similar role in COVID-19. Secondly, Koike C et al. suggested that anti-A and/or anti-B antibodies may neutralize the virus to effectively protect body when polymorphic blood group antigens expressed on the surfaces of red blood cells and epithelia are utilized as attachment receptors by HIV (Koike et al., 2007), perhaps for COVID-19, anti-A antibodies and/or anti-B antibodies also have the effect of neutralizing the SARS-COV-2. Thirdly, when combined anti-A or anti-B with cells of schistosome, it was suggested the unique ABO blood group antigen could confer appropriate specificity upon them (Gardas and Kościelak, 1973; Dean, 1974; Goldring et al., 1976), which was regarded as one of the interpretations why O type blood is not prone to schistosomiasis (Tiongco et al., 2018). Finally, it has been suggested that blood group O could prevent severe Plasmodium falciparum malaria through the mechanism of reducing rosettes (Ja et al., 2007; Degarege et al., 2019), so we speculated that blood type O has a similar effect on SARS-COV-2.
The potential clinical implications of current study deserve mention. Our study shed light on blood group A is more susceptible to COVID-19, and blood group O is less susceptible to it, which could provide supportive evidence that studying the association between ABO blood group and COVID-19 infection. Meanwhile, our finding suggests that individuals with blood group A are supposed to do better personal protection to minimize the possibility of infection. Moreover, we discussed in depth the association between ABO blood group and severity,demise of COVID-19, which may contribute to the victory over SARA-CoV-2.
The potential limitations of our study need to be considered. First of all, despite we had the large number of samples, the source of them were not diverse. Our samples lack cases from Europe and Africa. Due to the serious epidemic situation, we were unable to collect data and make on the spot investigation in Europe and Africa. Second, since the short medical resources were used for emergency treatment of a large number of patients, we didn't collect prospective cohorts to determine when healthy patients infect COVID-19.
5. Conclusions
In conclusion, the current analyses validated individuals with blood type A are related to a higher risk and individuals with blood type O are related to a lower risk to infect SARS-COV-2, and there were no significant relationships between ABO blood group and of COVID-19 severity and demise. The interest of this study assists people realize the relationship between ABO blood group and infection, severity and demise of COVID-19. Moreover, further investigations and studies are recommended to clarify the present finding and provide more beneficial insights into COVID-19.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Credit authorship contribution statemen
All authors collected the data. Bing-Bing WU conceived study design and the content concept, extracted and analyzed data, wrote original draft. Dong-Zhou Gu extracted and analyzed data. Jia-Ning Yu process the tables and figures. Jie Yang. interpreted and reviewed the data. Hong-Lin Chen reviewed the final draft. All the authors agreed to submit for “Infection, Genetics and Evolution”.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the responsible on human experimentation (institutional and national) committee and with the Helsinki Declaration of 1975, as revised in 2008.
Declaration of competing interest
The authors stated that they have no competing interests.
Acknowledgments
Acknowledgement
The authors thank all the participants of the current study.
References
- Ahn D.G., Shin H.J., Kim M.H. Current status of epidemiology, diagnosis, therapeutics, and vaccines for novel coronavirus disease 2019 (COVID-19) J. Microbiol. Biotechnol. 2020;30(3):313–324. doi: 10.4014/jmb.2003.03011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alpoim P.N., De Barros Pinheiro M., Junqueira D.R. Preeclampsia and ABO blood groups: a systematic review and meta-analysis. Mol. Biol. Rep. 2013;40(3):2253–2261. doi: 10.1007/s11033-012-2288-2. [DOI] [PubMed] [Google Scholar]
- Chakrani Z., Robinson K., Taye B. Association between ABO blood groups and helicobacter pylori infection: a meta-analysis. Sci. Rep. 2018;8(1) doi: 10.1038/s41598-018-36006-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng Y., Cheng G., Chui C.H. ABO blood group and susceptibility to severe acute respiratory syndrome. JAMA. 2005;293(12):1450–1451. doi: 10.1001/jama.293.12.1450-c. [DOI] [PubMed] [Google Scholar]
- Cooling L. Blood groups in infection and host susceptibility. Clin. Microbiol. Rev. 2015;28(3):801–870. doi: 10.1128/CMR.00109-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cota G.F., De Sousa M.R., Fereguetti T.O. Efficacy of anti-leishmania therapy in visceral leishmaniasis among HIV infected patients: a systematic review with indirect comparison. PLoS Negl. Trop. Dis. 2013;7(5) doi: 10.1371/journal.pntd.0002195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean D.A. Schistosoma mansoni: adsorption of human blood group A and B antigens by schistosomula. J. Parasitol. 1974;60(2):260–263. [PubMed] [Google Scholar]
- Degarege A., Gebrezgi M.T., Ibanez G. Effect of the ABO blood group on susceptibility to severe malaria: a systematic review and meta-analysis. Blood Rev. 2019;33:53–62. doi: 10.1016/j.blre.2018.07.002. [DOI] [PubMed] [Google Scholar]
- Dersimonian R., Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp. Clin. Trials. 2007;28(2):105–114. doi: 10.1016/j.cct.2006.04.004. [DOI] [PubMed] [Google Scholar]
- Egger M., Davey Smith G., Schneider M. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardas A., Kościelak J. New form of A-, B-, and H-blood-group-active substances extracted from erythrocyte membranes. Eur. J. Biochem. 1973;32(1):178–187. doi: 10.1111/j.1432-1033.1973.tb02595.x. [DOI] [PubMed] [Google Scholar]
- Gheblawi M., Wang K., Viveiros A. Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: celebrating the 20th anniversary of the discovery of ACE2. Circ. Res. 2020;126(10):1456–1474. doi: 10.1161/CIRCRESAHA.120.317015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldring O.L., Clegg J.A., Smithers S.R. Acquisition of human blood group antigens by Schistosoma mansoni. Clin. Exp. Immunol. 1976;26(1):181–187. [PMC free article] [PubMed] [Google Scholar]
- Guillon P., Clément M., Sébille V. Inhibition of the interaction between the SARS-CoV spike protein and its cellular receptor by anti-histo-blood group antibodies. Glycobiology. 2008;18(12):1085–1093. doi: 10.1093/glycob/cwn093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashino Y., Noguchi Y., Fukui T. Systematic evaluation and comparison of statistical tests for publication bias. J. Epidemiol. 2005;15(6):235–243. doi: 10.2188/jea.15.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ioannidis J.P. Interpretation of tests of heterogeneity and bias in meta-analysis. J. Eval. Clin. Pract. 2008;14(5):951–957. doi: 10.1111/j.1365-2753.2008.00986.x. [DOI] [PubMed] [Google Scholar]
- Ioannidis J.P., Trikalinos T.A. The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. Cmaj. 2007;176(8):1091–1096. doi: 10.1503/cmaj.060410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ja R., Ig H., Ma T. Blood group O protects against severe Plasmodium falciparum malaria through the mechanism of reduced rosetting. Proc. Natl. Acad. Sci. U. S. A. 2007;104(44):17471–17476. doi: 10.1073/pnas.0705390104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jing W., Zhao S., Liu J. ABO blood groups and hepatitis B virus infection: a systematic review and meta-analysis. BMJ Open. 2020;10(1) doi: 10.1136/bmjopen-2019-034114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koike C., Uddin M., Wildman D.E. Functionally important glycosyltransferase gain and loss during catarrhine primate emergence. Proc. Natl. Acad. Sci. U. S. A. 2007;104(2):559–564. doi: 10.1073/pnas.0610012104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesky E. Viennese serological research about the year 1900: its contribution to the development of clinical medicine. Bull. N. Y. Acad. Med. 1973;49(2):100–111. [PMC free article] [PubMed] [Google Scholar]
- Li B., Yang J., Zhao F. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin. Res. Cardiol. 2020;109(5):531–538. doi: 10.1007/s00392-020-01626-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao Y., Xue L., Gao J. ABO blood group-associated susceptibility to norovirus infection: a systematic review and meta-analysis. Infect. Genet. Evol. 2020;81 doi: 10.1016/j.meegid.2020.104245. [DOI] [PubMed] [Google Scholar]
- Lippi G., Plebani M. Procalcitonin in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. Clin. Chim. Acta. 2020;505:190–191. doi: 10.1016/j.cca.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Yan L.M., Wan L. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect. Dis. 2020;20(6):656–657. doi: 10.1016/S1473-3099(20)30232-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenzie J.S., Wetherall J.D., Fimmel P.J. Host factors and susceptibility to influenza a infection: the effect of ABO blood groups and HL-A antigens. Dev. Biol. Stand. 1977;39:355–362. [PubMed] [Google Scholar]
- Mao Y., Yang W., Qi Q. Blood groups A and AB are associated with increased gastric cancer risk: evidence from a large genetic study and systematic review. BMC Cancer. 2019;19(1):164. doi: 10.1186/s12885-019-5355-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010;25(9):603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- Stowell C.P., Stowell S.R. Biologic roles of the ABH and Lewis histo-blood group antigens Part I: infection and immunity. Vox Sang. 2019;114 doi: 10.1111/vox.12787. [DOI] [PubMed] [Google Scholar]
- Tiongco R.E., Paragas N.A., Dominguez M.J. ABO blood group antigens may be associated with increased susceptibility to schistosomiasis: a systematic review and meta-analysis. J. Helminthol. 2018;94:e21. doi: 10.1017/S0022149X18001116. [DOI] [PubMed] [Google Scholar]
- Varughese S., Read J.G., Al-Khal A. Effectiveness of the Middle East respiratory syndrome-coronavirus protocol in enhancing the function of an Emergency Department in Qatar. Eur. J. Emerg. Med. 2015;22(5):316–320. doi: 10.1097/MEJ.0000000000000285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan Y., Shang J., Graham R. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J. Virol. 2020;94(7) doi: 10.1128/JVI.00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W., Liu L., Wang Z. ABO blood group and esophageal carcinoma risk: from a case-control study in Chinese population to meta-analysis. Cancer Causes Control. 2014;25(10):1369–1377. doi: 10.1007/s10552-014-0442-y. [DOI] [PubMed] [Google Scholar]
- Wang W., Xia Y., Zhu J. Research progress of the role of angiotensin-converting enzyme 2 (ACE2) in the highly pathogenic human coronavirus pneumonia. Chin. J. Clin. Thorac. Cardiovasc. Surg. 2020;27(05):588–596. [Google Scholar]
- Xiang T.X., Liu J.M., Xu F. Analysis of clinical characteristics of 49 patients with coronavirus disease 2019 in Jiangxi. Chin. J. Respir. Crit. Care. 2020;19(02):154–160. [Google Scholar]
- Zeng X., Fan H., Lu D. Association between ABO blood groups and clinical outcome of coronavirus disease 2019: evidence from two cohorts. medRxiv. 2020 [Google Scholar]
- Zhao J., Yang Y., Huang H.-P. Relationship between the ABO Blood Group and the COVID-19 susceptibility. medRxiv. 2020 [Google Scholar]
- Zietz M., Tatonetti N.P. Testing the association between blood type and COVID-19 infection, intubation, and death. medRxiv. 2020 doi: 10.1038/s41467-020-19623-x. [DOI] [PMC free article] [PubMed] [Google Scholar]