Abstract
Objective
The mechanism underlying the benefit of nonsurgical spinal decompression (NSSD) on low back pain is unclear. This study was performed to investigate the immediate impact of NSSD on the mechanical properties and morphology of the paraspinal muscles.
Methods
Participants with low back pain were recruited. NSSD therapy was provided on one occasion. A myotonometer was placed perpendicularly on the skin surface over the paraspinal muscle at the level of L3/L4 to measure the mechanical muscle properties. The multifidus thickness was measured using B-mode ultrasound and defined as the distance between the transverse process and subcutaneous tissue fascia. The difference between before and after NSSD was analyzed by a paired t-test.
Results
Thirty participants (mean age, 20.9 ± 0.8 years; 9 male, 21 female) were recruited. No significant difference was observed in the muscle mechanical properties or morphology between before and after the intervention.
Conclusions
NSSD intervention did not induce immediate changes in the paraspinal muscle mechanical properties or multifidus thickness in young adults with low back pain. NSSD might produce benefits by stimulating mechanical receptors rather than inducing morphological changes or mechanical property alterations of the muscle fibers. These parameters may not be suitable outcome measures for NSSD intervention.
Keywords: Nonsurgical spinal decompression, paraspinal muscle, morphology, mechanical properties, low back pain, myotonometry
Introduction
A report published by the World Health Organization indicated that chronic low back pain (LBP) is among the most common causes of long-term disability.1 The prevalence of LBP among young adults is reportedly 42.4% and continues to rise.2 Studies published from different countries have shown that 30% to 81% of university students experience recurrent chronic LBP3,4 that interferes with social, physical, and academic activities.5 The incidence of LBP among young adults has long been underestimated, and limited clinical data from this age group have been recorded.
The multifidus and transversus abdominis are the primary spinal stabilization muscles, and a considerable amount of work has been conducted to understand their role in LBP.6 The two muscles have different roles in maintaining lumbar stability because of their anatomical structure and functional coupling.7 The transversus abdominis maintains spinal stability by contraction, which increases the abdominal pressure.8 Dysfunction of the transversus abdominis in nonspecific LBP is related to motor control (i.e., delayed activation relative to the multifidus during functional movement).9,10 The tension load of the common tendon of the transversus abdominis is primarily transferred to the posterior thoracolumbar fascia to maintain the stability of the spinal column. The multifidus directly maintains lumbar stability through the thoracolumbar fascia, which provides more than two-thirds of the spinal stability.11,12 An ultrasound imaging study revealed a smaller percent thickness contraction of the multifidus in people with than without chronic LBP.13 Animal experiments have shown that a prolonged static position14 and repetitive stress contribute to spasm of the multifidus.15 In addition, the pain level was demonstrated to be associated with the ability to recruit the multifidus.16
Muscle spasm refers to sustained contraction of a muscle,17 and the increase in chronic tension contributes to pain.18 Muscle tone can be defined as the resting tension of the muscle or the resistance in response to stretching of the muscle.19 Altered lumbar muscle tone was found in adults with chronic LBP20,21 and was suggested to be associated with the underlying pathologies and symptoms.22 Early literature indicated that muscle tone is a contributing factor to the pain-spasm-pain model.23 A vicious circle is established in which pain results in increased muscle tone, which in turn causes further pain.24 Pain adaptation models postulate that pain itself reduces activation of muscles, thus reducing the range of motion and movement velocity.25 This in turn leads to inappropriate body positioning at rest and during motion. Stiffness can be interpreted as the viscoelastic property of muscles.26 A muscle that has high static stiffness requires more energy to activate and is therefore more difficult to contract.27 Studies that used shear wave elastography confirmed increased stiffness of the paraspinal muscles in people with chronic LBP.28,29
Nonsurgical spinal decompression (NSSD) is a technique that applies longitudinal traction force through the muscle to distract the spinal column via a mechanical or motorized pulley system.30 The stretching force is reportedly able to reduce muscle tension by elongating the muscle fibers and widening the intervertebral foramen.31 The available evidence regarding traction in the management of LBP is controversial. Several systematic reviews showed no beneficial effect of traction intervention when compared with placebo in terms of pain relief and returning to work but repeatedly indicated that more high-quality studies are required.32,33 Despite the apparent lack of evidence to support the use of lumbar traction in the management of LBP, traction continues to be a commonly used intervention by health care professionals to distract tissues and joints in the lumbar spine region. A survey published in 2005 indicated that 41% of the surveyed physiotherapists used lumbar traction in the management LBP.34 Similar survey data were collected from a group of physiotherapists in 2015. The results indicated that 76.6% of the respondents used lumbar traction in the management of LBP.35 The divergence between clinical practice and recommendations from systematic reviews may be related to the empirical evidence that supports the benefits of lumbar traction.35–37 These studies indicated the potential efficacy of NSSD in patients with LBP.
One proposed mechanism of NSSD is a reduction of muscle spasm, which inhibits nociceptive impulses and increases mobility.33 However, the impact of NSSD on muscle morphology and the mechanical properties of tone and stiffness have been less intensively studied. Thus, it may be possible to assess the impact of NSSD from the perspective of mechanical muscle properties. Early studies attempted to quantify altered muscle tone in people with chronic LBP using surface electromyography (EMG). The possibility of using surface EMG as an outcome measure of NSSD has been reported in some studies; however, the results of these studies were rather inconclusive because of conflicting evidence.38 The limitation of using the electrical activity level as a surrogate for muscle tone is that the electrical activity mostly concerns the muscle contraction elicited by the neural electrical drive of motor nerves and muscle cells, not the endogenous contractile structures of skeletal muscles. In addition, little is currently known on the immediate impact of NSSD on paraspinal muscle morphology and whether it is possible to assess changes in muscle tone using a myotonometer in young people with chronic LBP. Thus, an understanding of how the mechanical properties of muscles are affected by NSSD would improve our understanding of the intervention technique that would facilitate treatment selection. This study was performed to assess the immediate impact of NSSD of the multifidus thickness and paraspinal muscle mechanical properties.
Methods
Participants
Participants were recruited from the student and staff populations of a local institute via social media and internal announcements. The inclusion criteria were an age of 18 to 25 years, the presence of chronic nonspecific LBP (in the lumbar and lumbosacral regions) for >3 months prior to enrollment, and no treatment for ≥4 weeks prior to enrollment. The exclusion criteria were a body mass index of >30 kg/m2, a history of fracture or surgery in the low back area, pregnancy, a herniated disc, lumbar instability, and malignancy. A physical therapist diagnosed LBP based on the clinical assessment protocol established by the American College of Physicians and American Pain Society.39 Demographic information regarding age, sex, height, weight, and clinical history of LBP were collected at the beginning of the data collection session. Clinical information regarding back pain was also collected. The Chinese version of the Oswestry Low Back Pain Disability Index40 was used to assess the degree of disability related to back pain. The Japanese Orthopedic Association back pain score41 was recorded to assess the disorder in different dimensions, including quality of life, pain intensity, and degree of disability. A numerical pain rating scale was used to assess the pain intensity (range, 0–10) that the participants were experiencing at the time of data collection.
Sampling method and sample size
This study adopted a pragmatic sampling method. Participants who met the inclusion criteria were recruited into the study. The sample size calculation was based on a pilot trial involving six participants. Muscle tone was used as the primary outcome measure for the sample size calculation. The sample size was calculated with the software GPower version 3.1.2, using the “A priori: Compute required sample size –given α, power, and effect size” as the type of power analysis. The preliminary results indicated a mean difference of 0.43 Hz (standard deviation, 0.66) after NSSD, which gave an effect size of 0.63. With an α error probability of 0.05 and a power of 0.95, a sample size of 27 was sufficient for the present study.
Parameters
The mechanical properties of muscle tone and stiffness at the L3/L4 facet joint level were recorded with a myotonometer (MyotonPRO; Myoton AS, Tallinn, Estonia). The oscillation frequency (Hz) indicates the tone (i.e., intrinsic tension) of a muscle in the resting state. The dynamic stiffness (N/m) characterizes the resistance of the muscle to contraction. The morphology parameter of multifidus thickness (mm) at the L3/L4 facet joint level was assessed by diagnostic ultrasound (M-Turbo; FUJIFILM SonoSite, Inc., Bothell, WA, USA).
Ethics
The study protocol was approved by the Medical Ethics Committee of the First Affiliated Hospital of Sun Yat-sen University [approval no.: 2016(85)]. All participants were informed of the study procedure and the right to withdraw from the trial at any time. Written consent was obtained from all participants.
Study procedure
Myotonometry
The muscle tone and stiffness of the lumbar paraspinal muscles were assessed by a handheld myotonometer before and after the NSSD intervention. The validity and reliability of using a myotonometer to measure muscle tone and stiffness was published in previous studies.42–45 The intraclass correlation coefficient for test–retest reliability within the same day was reported to be 0.99 for bilateral muscle tone and stiffness. The standard error measurement for muscle tone was 0.06 Hz on the left and 0.03 Hz on the right. For muscle stiffness, the standard error measurement was 1.82 Hz on the left and 2.15 Hz on the right.45 The participants were asked to lie in the prone position on the traction table with their hands on both sides of their head, exposing the lumbar region. The test site was determined by palpation. The examiner located the L4/L5 interspinous space by palpating the highest level of the iliac crest, and then located the interspinous space of L3/L4. The test sites were marked on the skin surface 1 cm lateral to the left and right spinous processes. The myotonometer was set to triple scan mode in which three consecutive indentations were applied (0.4 N, 15 ms apart). The probe was placed vertically at the location markers to record the muscle tone and stiffness of the bilateral L3/L4 paraspinal muscles.
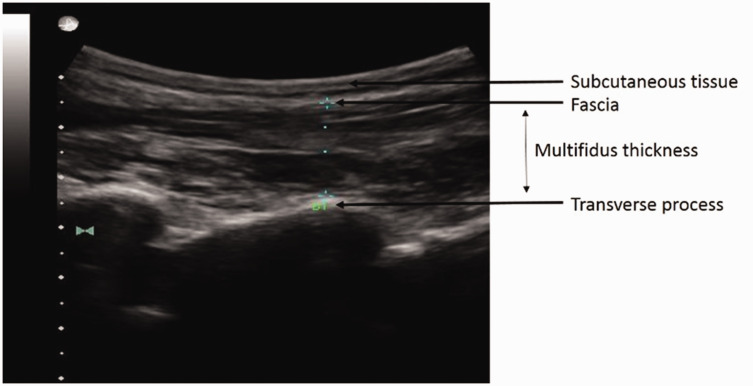
Ultrasound imaging
An experienced examiner obtained all images using a portable ultrasound machine with a 5.0-MHz convex array probe before and after the intervention. The participants lay in the prone position on the traction table with their hands on both sides of their head, exposing the lumbar region. The scanning procedure was based on a published protocol.46 The examiner first identified the spinous process of L4 and placed the probe longitudinally along the spine with the midpoint over the L4 spinous process. The probe was then moved laterally and angled slightly medially until the L3/L4 facet joint could be identified. The scan point was directly over the multifidus, and a measurement from this landmark was taken to record the linear distance between the transverse process and the inner layer of the lumbodorsal fascia. The measurement of the multifidus thickness is illustrated in Figure 1.
Figure 1.
Ultrasound image used for measurement of multifidus thickness.
The contralateral arm-lifting task was conducted to contract the multifidus.46 The participants lay in the prone position and performed isometric contraction with the elbow flexed to 90° and shoulders abducted to 120°. The participants then lifted their head, trunk, and upper extremities and held this position with maximum effort (determined as grade 5 on the manual muscle test) against a load applied at the elbow for 5 seconds.
NSSD
An NSSD system (Model No. SDS9800; Ryzur Medical Technology Company, Beijing, China) was used to apply a continuous decompression force to a specific intervertebral level. Pressure was applied at two levels with the maximum force maintained for 60 seconds and the minimum force maintained for 30 seconds. The maximum decompression force was calculated as half the participant’s body weight (lbs) plus 10 lbs, and the minimum force was calculated as half the participant’s body weight minus 10 lbs. Eighteen cycles were performed within the session. The decompression force was applied for 28 minutes 15 seconds with a traction force angle of 20° to target the L3/L4 facet joint. The participants were positioned supine and fixated on the instrument bed by straps located at the chest and pelvic levels. The hip and knee joints were flexed to 30° and 60°, respectively, by placing an inflatable pad under the knees for relaxation and maintenance of the lumbar physiological curve. The NSSD protocol was conducted in accordance with the manufacturer’s operation manual.47
Statistical analysis
Data were analyzed using the software SPSS version 20.0 (IBM Corp., Armonk, NY, USA). The demographic and clinical baseline characteristics were summarized by descriptive statistics. The differences in the multifidus thickness and paraspinal muscle mechanical properties between before and after the intervention were assessed by the paired t-test. A p value of <0.05 was considered statistically significant.
Results
Demographics
Thirty participants with chronic LBP took part in the study (mean age, 20.9 ± 0.8 years). Table 1 presents a summary of the demographic information of the sample population. The clinical information of LBP of the sample population is presented in Table 2.
Table 1.
Summary of all participants’ demographic information.
| Demographic information | |
|---|---|
| Age, years | 20.9 ± 0.8 |
| BMI, kg/m2 | 20.1 ± 2.1 |
| Sex, male/female | 9/21 |
| Dominant side, left/right | 1/29 |
Data are presented as mean ± standard deviation or number of participants.
BMI, body mass index.
Table 2.
Summary of all participants’ clinical information.
| Clinical information | |
|---|---|
| NPRS score | 3.2 ± 2.0 |
| ODI, % | 13.4 ± 5.3 |
| JOABP | 25.1 ± 2.3 |
| Location of pain, left/central/right/bilateral | 1/5/4/20 |
Data are presented as mean ± standard deviation or number of participants.
NPRS, numerical pain rating scale; ODI, Oswestry Low Back Pain Disability Index; JOABP, Japanese Orthopedic Association back pain score.
Multifidus thickness
The paired t-test indicated no significant difference in the multifidus thickness either at rest or during contraction between before and after NSSD at the L3/L4 level. Table 3 shows the measurements of the multifidus muscle thickness.
Table 3.
Multifidus thickness at rest and in contracted state before and after NSSD intervention.
| Thickness, mm | Minimum | Maximum | Mean | SD | diff | p value | ||
|---|---|---|---|---|---|---|---|---|
| Relaxed state | Left | Pre | 8.95 | 30.86 | 20.62 | 4.13 | ||
| Post | 10.15 | 27.81 | 20.48 | 3.80 | 0.15 | 0.72 | ||
| Right | Pre | 11.79 | 34.13 | 21.55 | 4.49 | |||
| Post | 12.79 | 32.48 | 21.13 | 4.56 | 0.43 | 0.21 | ||
| Contracted state | Left | Pre | 16.45 | 40.81 | 28.48 | 4.46 | ||
| Post | 16.46 | 40.19 | 28.61 | 4.87 | −0.13 | 0.78 | ||
| Right | Pre | 15.64 | 44.46 | 29.66 | 5.21 | |||
| Post | 16.49 | 44.08 | 30.06 | 5.24 | −0.40 | 0.45 |
NSSD, nonsurgical spinal decompression; SD, standard deviation; Pre, before NSSD; Post, after NSSD; diff, difference.
Muscle tone and stiffness of paraspinal muscles
The changes in the paraspinal muscle tone and stiffness after NSSD were not statistically significant. Table 4 shows the measurements of the paraspinal muscle tone and stiffness.
Table 4.
Mechanical muscle properties before and after NSSD intervention.
| Mechanical properties | Minimum | Maximum | Mean | SD | diff | p value | ||
|---|---|---|---|---|---|---|---|---|
| Tone, Hz | Left | Pre | 11.0 | 18.9 | 15.04 | 1.77 | ||
| Post | 11.3 | 19.9 | 15.07 | 1.71 | −0.03 | 0.78 | ||
| Right | Pre | 11.7 | 19.8 | 15.36 | 1.88 | |||
| Post | 12.1 | 20.9 | 15.44 | 1.86 | −0.08 | 0.41 | ||
| Stiffness, N/m | Left | Pre | 128 | 450 | 267.77 | 67.06 | ||
| Post | 131 | 432 | 269.67 | 63.87 | −1.90 | 0.72 | ||
| Right | Pre | 152 | 444 | 281.53 | 74.89 | |||
| Post | 161 | 487 | 282.90 | 73.50 | −1.37 | 0.75 |
NSSD, nonsurgical spinal decompression; SD, standard deviation; Pre, before NSSD; Post, after NSSD; diff, difference.
Discussion
This study is among the first to investigate the impact of NSSD on the paraspinal muscle morphology and mechanical properties in young adults with LBP by ultrasonography and myotonometry. The results indicated no significant differences in the multifidus thickness, tone, or stiffness of the paraspinal muscles immediately after NSSD.
Multifidus thickness
This study investigated the immediate morphological changes in the multifidus after NSSD intervention. Elongation of muscle fibers is believed to play a role in pain relief by stimulating the mechanical receptors located at the paraspinal ligaments and muscles.33 One published study revealed thinning of the psoas major during mechanical traction.48 Other studies that investigated the effect of stretching on peripheral muscle thickness also showed a reduction of muscle thickness after the stretching intervention.49 The finding of the present study is consistent with a study that used ultrasonography to study the thickness of the trapezius and splenius capitis.50 That study showed a reduction in muscle thickness during mechanical traction, but the difference did not reach statistical significance.50 However, the results of that study and the present study may not be directly comparable because of the differences in the muscles tested and amount of force applied. A potential reason for the lack of significant changes observed in this study is the short intervention period, which was not sufficient to induce morphological change. A systematic review indicated that structural muscle changes tended to occur in stretching programs that lasted for >8 weeks.51 The stretching duration of 28 minutes in this study may therefore be insufficient to induce morphological changes. The lack of a significant difference in the multifidus thickness may add further support to the theory that the benefits of NSSD are associated with stimulation of mechanical receptors.33 The potential pain-relieving mechanism of NSSD may be similar to that of spinal manual therapy, such as spinal manipulation, in terms of decreasing the sensitivity within the muscle spindles52 and increasing the pressure pain threshold.53
Mechanical muscle properties
Spasm of the paraspinal muscles is believed to be a contributing factor to chronic LBP. Some published studies investigated paraspinal muscle activity by EMG during different lumbar traction protocols of varying distraction-force waveforms and pull angles. These studies showed no significant differences in the EMG signal of the lumbar erector spinae between any of the traction groups and the control group.54,55 One study that assessed the effects of cervical traction on muscle activity also showed that the EMG activities of the lateral neck muscles did not differ significantly immediately after intermittent mechanical traction.56 These results suggest that traction may not have an immediate impact on muscle tone. The present study did not reveal a significant decrease in muscle tone. The difference in muscle tone after the intervention also did not reach the minimal detectable difference previously reported for this pathology group.44 This finding is consistent with the EMG study showing that NSSD is unlikely to affect muscle tone after one session and casts doubt on the suitability of using muscle tone as an outcome measure after each treatment session, either by myotonometry or palpation.
Muscle stiffness refers to the elastic properties of muscle and plays an important role in the stabilizing system of the spine.57 Abnormal muscle stiffness is considered to be a contributing factor to chronic LBP.58 Passive stretching of muscle is reportedly able to reduce muscle stiffness by affecting the muscle–tendon complex.59 Published studies that investigated the effect of stretching on the gastrocnemius showed a reduction in muscle stiffness after 60 seconds of static stretching.60 The present study did not reveal a significant reduction in paraspinal muscle stiffness after 28 minutes of the NSSD intervention. A possible reason for the lack of significance is that the paraspinal compartment is encapsulated by various layers of connective tissue and myofascia.61 The stiffness of these tissues may not be affected under physiological conditions or within normal physiological ranges. This theory is supported by a study that investigated the changes in paraspinal muscle stiffness in five postures that aimed to stretch the paraspinal column. Stretching performed in all postures produced no significant changes in the paraspinal muscle stiffness.61 Another study that used a spinal manipulation technique to alter paraspinal muscle stiffness also showed no significant difference in stiffness after the intervention.62 These findings add further evidence that the paraspinal muscle stiffness might not be affected by passive stretching alone. Thus, the benefit of NSSD is unlikely to be related to alteration of the muscle stiffness, and stiffness may not be a suitable outcome for the NSSD intervention. These results suggest that muscle spasm reduction and muscle relaxation are not the mechanisms underlying how NSSD alleviates back pain.63
Limitations
The results of the present study should be interpreted with caution. This study provided only a single dose of treatment and did not assess the impact of NSSD on the muscle mechanical properties and morphology throughout an entire course of intervention. It is therefore difficult to conclude whether NSSD can induce significant changes after performance of more intervention sessions. Additionally, the findings of the present study may not be extrapolated to the general population. However, this is unlikely to affect the validity of the findings because very few reports have indicated that young adults would respond differently to NSSD intervention. Published clinical management guidelines for LBP also do not indicate that young adults would respond differently to intervention. Finally, the present study did not include a control group or comparison with other types of intervention. The NSSD protocol adopted in the present study followed the manufacturer’s recommendation. A systematic review indicated that a large variation was present in the lumbar spine traction protocol within published randomized controlled trials. Parameters such as the force, force angle, and intervention duration appeared to be chosen arbitrarily.64 Thus, there is no definitive evidence to adequately justify the parameters of the NSSD setting.
Conclusions
The findings of the present study indicate that NSSD does not induce immediate changes in the mechanical properties or morphology of the paraspinal muscles after a single dose of treatment in young adults with LBP. This may further support the notion that NSSD produces benefits by stimulating mechanical receptors rather than by inducing morphological changes or mechanical property alterations of muscle fibers. Therefore, these parameters may not be suitable outcome measures for NSSD intervention.
Availability of data and materials
The dataset supporting the conclusions of this article is available from the authors upon request.
Consent to publish
All participants provided consent to publish their individual data.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research was supported by the National Natural Science Foundation of China (Nos. 81971224, 31771016) and a Guangdong Province Medical Science Technology Research Grant (Grant No. A2019452).
ORCID iDs
Wai Leung Ambrose Lo https://orcid.org/0000-0001-7350-2157
Di Lei https://orcid.org/0000-0002-6035-8165
Qiuhua Yu https://orcid.org/0000-0003-3045-6124
References
- 1.GBD 2015 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016; 388: 1603–1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ganesan S, Acharya AS, Chauhan R, et al. Prevalence and risk factors for low back pain in 1,355 young adults: a cross-sectional study. Asian Spine J 2017; 11: 610–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Penkala S, El-Debal H, Coxon K. Work-related musculoskeletal problems related to laboratory training in university medical science students: a cross sectional survey. BMC Public Health 2018; 18: 1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crawford RJ, Volken T, Schaffert R, et al. Higher low back and neck pain in final year Swiss health professions’ students: worrying susceptibilities identified in a multi-centre comparison to the national population. BMC Public Health 2018; 18: 1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tavares C, Salvi CS, Nisihara R, et al. Low back pain in Brazilian medical students: a cross-sectional study in 629 individuals. Clin Rheumatol 2019; 38: 939–942. [DOI] [PubMed] [Google Scholar]
- 6.Hides J, Stanton W, Dilani Mendis M, et al. The relationship of transversus abdominis and lumbar multifidus clinical muscle tests in patients with chronic low back pain. Man Ther 2011; 16: 573–577. [DOI] [PubMed] [Google Scholar]
- 7.Vleeming A, Schuenke MD, Danneels L, et al. The functional coupling of the deep abdominal and paraspinal muscles: the effects of simulated paraspinal muscle contraction on force transfer to the middle and posterior layer of the thoracolumbar fascia. J Anat 2014; 225: 447–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grooms DR, Grindstaff TL, Croy T, et al. Clinimetric analysis of pressure biofeedback and transversus abdominis function in individuals with stabilization classification low back pain. J Orthop Sports Phys Ther 2013; 43: 184–193. [DOI] [PubMed] [Google Scholar]
- 9.Hodges PW, Richardson CA. Contraction of the abdominal muscles associated with movement of the lower limb. Phys Ther 1997; 77: 132–142; discussion 42-4. [DOI] [PubMed] [Google Scholar]
- 10.Hodges PW, Moseley GL, Gabrielsson A, et al. Experimental muscle pain changes feedforward postural responses of the trunk muscles. Exp Brain Res 2003; 151: 262–271. [DOI] [PubMed] [Google Scholar]
- 11.Wilke HJ, Wolf S, Claes LE, et al. Stability increase of the lumbar spine with different muscle groups. A biomechanical in vitro study. Spine (Phila Pa 1976) 1995; 20: 192–198. [DOI] [PubMed] [Google Scholar]
- 12.Hebert JJ, Kjaer P, Fritz JM, et al. The relationship of lumbar multifidus muscle morphology to previous, current, and future low back pain: a 9-year population-based prospective cohort study. Spine (Phila Pa 1976) 2014; 39: 1417–1425. [DOI] [PubMed] [Google Scholar]
- 13.Wallwork TL, Stanton WR, Freke M, et al. The effect of chronic low back pain on size and contraction of the lumbar multifidus muscle. Man Ther 2009; 14: 496–500. [DOI] [PubMed] [Google Scholar]
- 14.Williams M, Solomonow M, Zhou BH, et al. Multifidus spasms elicited by prolonged lumbar flexion. Spine (Phila Pa 1976) 2000; 25: 2916–2924. [DOI] [PubMed] [Google Scholar]
- 15.Sbriccoli P, Yousuf K, Kupershtein I, et al. Static load repetition is a risk factor in the development of lumbar cumulative musculoskeletal disorder. Spine (Phila Pa 1976) 2004; 29: 2643–2653. [DOI] [PubMed] [Google Scholar]
- 16.Zhang S, Xu Y, Han X, et al. Functional and morphological changes in the deep lumbar multifidus using electromyography and ultrasound. Sci Rep 2018; 8: 6539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Taverner D. Muscle spasm as a cause of somatic pain. Ann Rheum Dis 1954; 13: 331–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCleane GJ. Pain management: expanding the pharmacological options. Singapore: Blackwell Publishing, 2008. [Google Scholar]
- 19.Van Deun B, Hobbelen JS, Cagnie B, et al. Reproducible measurements of muscle characteristics using the MyotonPRO device: comparison between individuals with and without paratonia. J Geriatr Phys Ther 2018; 41: 194–203. [DOI] [PubMed] [Google Scholar]
- 20.Haladaj R, Topol M. Multiple impulse therapy in the assessment of paraspinal muscle tone in patients with low back pain. Ortop Traumatol Rehabil 2016; 18: 537–547. [DOI] [PubMed] [Google Scholar]
- 21.Nair K, Masi AT, Andonian BJ, et al. Stiffness of resting lumbar myofascia in healthy young subjects quantified using a handheld myotonometer and concurrently with surface electromyography monitoring. J Bodyw Mov Ther 2016; 20: 388–396. [DOI] [PubMed] [Google Scholar]
- 22.Kawchuk GN, Kaigle AM, Holm SH, et al. The diagnostic performance of vertebral displacement measurements derived from ultrasonic indentation in an in vivo model of degenerative disc disease. Spine (Phila Pa 1976) 2001; 26: 1348–1355. [DOI] [PubMed] [Google Scholar]
- 23.van Dieen JH, Selen LP, Cholewicki J. Trunk muscle activation in low-back pain patients, an analysis of the literature. J Electromyogr Kinesiol 2003; 13: 333–351. [DOI] [PubMed] [Google Scholar]
- 24.Roland MO. A critical review of the evidence for a pain-spasm-pain cycle in spinal disorders. Clin Biomech (Bristol, Avon) 1986; 1: 102–109. [DOI] [PubMed] [Google Scholar]
- 25.Dieën JHV, Selen LPJ, Cholewicki J. Trunk muscle activation in low-back pain patients, an analysis of the literature. J Electromyogr Kinesiol 2003; 13: 333–351. [DOI] [PubMed] [Google Scholar]
- 26.Magnusson SP, Simonsen EB, Aagaard P, et al. Viscoelastic response to repeated static stretching in the human hamstring muscle. Scand J Med Sci Sports 1995; 5: 342–347. [DOI] [PubMed] [Google Scholar]
- 27.Rassier DE. Sarcomere mechanics in striated muscles: from molecules to sarcomeres to cells. Am J Physiol Cell Physiol 2017; 313: C134–C145. [DOI] [PubMed] [Google Scholar]
- 28.Koppenhaver S, Gaffney E, Oates A, et al. Lumbar muscle stiffness is different in individuals with low back pain than asymptomatic controls and is associated with pain and disability, but not common physical examination findings. Musculoskelet Sci Pract 2019; 45: 102078. [DOI] [PubMed] [Google Scholar]
- 29.Chan ST, Fung PK, Ng NY, et al. Dynamic changes of elasticity, cross-sectional area, and fat infiltration of multifidus at different postures in men with chronic low back pain. Spine J 2012; 12: 381–388. [DOI] [PubMed] [Google Scholar]
- 30.Clarke JA, van Tulder MW, Blomberg SE, et al. Traction for low-back pain with or without sciatica. Cochrane Database Syst Rev 2007; (2): Cd003010. DOI: 10.1002/14651858.CD003010.pub4. [DOI] [PubMed] [Google Scholar]
- 31.Park SJ, Kim SH, Min KO. The immediate effects of rib cage joint mobilization and chest wall stretch on muscle tone and stiffness of respiratory muscles and chest expansion ability in patients with chronic stroke. J Phys Ther Sci 2017; 29: 1960–1963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van der Heijden GJ, Beurskens AJ, Koes BW, et al. The efficacy of traction for back and neck pain: a systematic, blinded review of randomized clinical trial methods. Phys Ther 1995; 75: 93–104. [DOI] [PubMed] [Google Scholar]
- 33.Wegner I, Widyahening IS, van Tulder MW, et al. Traction for low-back pain with or without sciatica. Cochrane Database Syst Rev 2013; (8): Cd003010. DOI: 10.1002/14651858.CD003010.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harte AA, Gracey JH, Baxter GD. Current use of lumbar traction in the management of low back pain: results of a survey of physiotherapists in the United Kingdom. Arch Phys Med Rehabil 2005; 86: 1164–1169. [DOI] [PubMed] [Google Scholar]
- 35.Madson TJ, Hollman JH. Lumbar traction for managing low back pain: a survey of physical therapists in the United States. J Orthop Sports Phys Ther 2015; 45: 586–595. [DOI] [PubMed] [Google Scholar]
- 36.Choi J, Lee S, Hwangbo G. Influences of spinal decompression therapy and general traction therapy on the pain, disability, and straight leg raising of patients with intervertebral disc herniation. J Phys Ther Sci 2015; 27: 481–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Simmerman SM, Sizer PS, Dedrick GS, et al. Immediate changes in spinal height and pain after aquatic vertical traction in patients with persistent low back symptoms: a crossover clinical trial. PM R 2011; 3: 447–457. [DOI] [PubMed] [Google Scholar]
- 38.Geisser ME, Ranavaya M, Haig AJ, et al. A meta-analytic review of surface electromyography among persons with low back pain and normal, healthy controls. J Pain 2005; 6: 711–726. [DOI] [PubMed] [Google Scholar]
- 39.Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 2007; 147: 478–491. [DOI] [PubMed] [Google Scholar]
- 40.Liu Q, Mai M, Xiao LA. Responsiveness of Chinese version of Oswestry disability index in subjects with chronic low back pain. Chinese Journal of Rehabilitation Medicine 2010; 25: 621–624. [Google Scholar]
- 41.Yao M, Li ZJ, Zhu S, et al. Simplified Chinese version of the Japanese Orthopaedic Association back pain evaluation questionnaire: cross-cultural adaptation, reliability, and validity for patients with low back pain. Spine (Phila Pa 1976) 2018; 43: E357–E364. [DOI] [PubMed] [Google Scholar]
- 42.Feng YN, Li YP, Liu CL, et al. Assessing the elastic properties of skeletal muscle and tendon using shearwave ultrasound elastography and MyotonPRO. Sci Rep 2018; 8: 17064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kelly JP, Koppenhaver SL, Michener LA, et al. Characterization of tissue stiffness of the infraspinatus, erector spinae, and gastrocnemius muscle using ultrasound shear wave elastography and superficial mechanical deformation. J Electromyogr Kinesiol 2018; 38: 73–80. [DOI] [PubMed] [Google Scholar]
- 44.Hu X, Lei D, Li L, et al. Quantifying paraspinal muscle tone and stiffness in young adults with chronic low back pain: a reliability study. Sci Rep 2018; 8: 14343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lo WLA, Yu Q, Mao Y, et al. Lumbar muscles biomechanical characteristics in young people with chronic spinal pain. BMC Musculoskelet Disord 2019; 20: 559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kiesel KB, Uhl TL, Underwood FB, et al. Measurement of lumbar multifidus muscle contraction with rehabilitative ultrasound imaging. Man Ther 2007; 12: 161–166. [DOI] [PubMed] [Google Scholar]
- 47.Anhui Ryzur Medical Equipment Co. Ltd. SDS®9800 True Non-Surgical Spinal Decompression System Operators Manual China 2016.
- 48.Sari H, Akarirmak U, Karacan I, et al. Computed tomographic evaluation of lumbar spinal structures during traction. Physiother Theory Pract 2005; 21: 3–11. [PubMed] [Google Scholar]
- 49.Simpson CL, Kim BDH, Bourcet MR, et al. Stretch training induces unequal adaptation in muscle fascicles and thickness in medial and lateral gastrocnemii. Scand J Med Sci Sports 2017; 27: 1597–604. [DOI] [PubMed] [Google Scholar]
- 50.Kuniyasu K. Changes in neck muscle thickness due to differences in intermittent cervical traction force measured by ultrasonography. J Phys Ther Sci 2014; 26: 785–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Freitas SR, Mendes B, Le Sant G, et al. Can chronic stretching change the muscle-tendon mechanical properties? A review. Scand J Med Sci Sports 2018; 28: 794–806. [DOI] [PubMed] [Google Scholar]
- 52.Millan M, Leboeuf-Yde C, Budgell B, et al. The effect of spinal manipulative therapy on experimentally induced pain: a systematic literature review. Chiropr Man Therap 2012; 20: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Aspinall SL, Leboeuf-Yde C, Etherington SJ, et al. Manipulation-induced hypoalgesia in musculoskeletal pain populations: a systematic critical review and meta-analysis. Chiropr Man Therap 2019; 27: 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cholewicki J, Lee AS, Reeves NP, et al. Trunk muscle response to various protocols of lumbar traction. Man Ther 2009; 14: 562–566. [DOI] [PubMed] [Google Scholar]
- 55.Hood CJ, Hart DL, Smith HG, et al. Comparison of electromyographic activity in normal lumbar sacrospinalis musculature during continuous and intermittent pelvic traction. J Orthop Sports Phys Ther 1981; 2: 137–141. [DOI] [PubMed] [Google Scholar]
- 56.Murphy MJ. Effects of cervical traction on muscle activity. J Orthop Sports Phys Ther 1991; 13: 220–225. [DOI] [PubMed] [Google Scholar]
- 57.Willard FH, Vleeming A, Schuenke MD, et al. The thoracolumbar fascia: anatomy, function and clinical considerations. J Anat 2012; 221: 507–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Crezei M, Soubeyran M, Gagey O. The paraspinal muscle-tendon system: its paradoxical anatomy. PLoS One 2019; 14: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kay AD, Blazevich AJ. Isometric contractions reduce plantar flexor moment, Achilles tendon stiffness, and neuromuscular activity but remove the subsequent effects of stretch. J Appl Physiol (1985) 2009; 107: 1181–1189. [DOI] [PubMed] [Google Scholar]
- 60.Kay AD, Husbands-Beasley J, Blazevich AJ. Effects of contract-relax, static stretching, and isometric contractions on muscle-tendon mechanics. Med Sci Sports Exerc 2015; 47: 2181–2190. [DOI] [PubMed] [Google Scholar]
- 61.Blain M, Bedretdinova D, Bellin MF, et al. Influence of thoracolumbar fascia stretching on lumbar back muscle stiffness: a supersonic shear wave elastography approach. Clin Anat 2019; 32: 73–80. [DOI] [PubMed] [Google Scholar]
- 62.Xia T, Long CR, Vining RD, et al. Association of lumbar spine stiffness and flexion-relaxation phenomenon with patient-reported outcomes in adults with chronic low back pain - a single-arm clinical trial investigating the effects of thrust spinal manipulation. BMC Complement Altern Med 2017; 17: 303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kang JH, Park TS. Changes in cervical muscle activity according to the traction force of an air-inflatable neck traction device. J Phys Ther Sci 2015; 27: 2723–2725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Alrwaily M, Almutiri M, Schneider M. Assessment of variability in traction interventions for patients with low back pain: a systematic review. Chiropr Man Therap 2018; 26: 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset supporting the conclusions of this article is available from the authors upon request.