Abstract
Background:
Meniscal extrusion refers to meniscal displacement out of the joint space and over the tibial margin, altering knee mechanics and increasing the risk of osteoarthritis. The meniscotibial ligaments have been shown to have an important role in meniscal stability. However, it remains unclear whether an isolated lesion of the medial meniscotibial ligaments will result in meniscal extrusion and whether repairing the detached ligament will reduce extrusion.
Hypothesis:
A lesion of the medial meniscotibial ligament will result in meniscal extrusion, and repairing the joint capsule will eliminate the extrusion by returning the meniscus back to its original position.
Study Design:
Controlled laboratory study.
Methods:
Fresh-frozen human cadaveric knees (N = 6) were used for biomechanical testing. The test protocol involved 100 flexion-extension cycles. In full extension, meniscal extrusion was measured using ultrasound, in both an otherwise unloaded state and while subjected to a 10-N·m varus load. Each knee was tested in its native condition (baseline), after creating a detachment of the medial meniscotibial ligament, and finally with the joint capsule repaired using 3 knotless SutureTak anchors. We also performed a retrospective review of 15 patients who underwent meniscotibial ligament repair with a minimal follow-up of 5 weeks (mean, 14 weeks; range, 5-35 weeks).
Results:
During biomechanical testing, the mean absolute meniscal extrusion at baseline was 1.5 ± 0.6 mm. After creation of the meniscotibial ligament lesion, the mean absolute meniscal extrusion was significantly increased (3.4 ± 0.7 mm) (P < .001). After repair, the extrusion was reduced to 2.1 ± 0.4 mm (P < .001). Clinically, a reduction in absolute meniscal extrusion of approximately 48% was reached (1.2 ± 0.6 vs 2.4 ± 0.5 mm preoperatively; P < .001).
Conclusion:
This study indicates that the medial meniscotibial ligaments contribute to meniscal stability as lesions cause the meniscus to extrude and that repair of those ligaments can significantly reduce extrusion. Early clinical results using this meniscotibial ligament repair technique support our biomechanical findings, as a significant reduction in meniscal extrusion was achieved.
Clinical Relevance:
Our biomechanical findings suggest that repair of medial meniscotibial ligaments reduces meniscal extrusion and clinically may improve meniscal function, with the possible long-term benefit of reducing the risk for osteoarthritis.
Keywords: meniscus, meniscal extrusion, ultrasound diagnostics, medial meniscotibial ligaments, meniscal stability
In addition to providing stability for femorotibial articulation,16,27 the primary functions of menisci are to distribute axial load and provide joint lubrication and nutrition of the knee joint.18,25 The menisci are semilunar-shaped fibrocartilage structures located in the knee joint between the tibia and the femur, whose functions include load distribution and stabilization of the joint.2,11,27,28 Alterations in the function of the menisci, resulting from either tearing or extrusion, can result in altered knee mechanics and may eventually initiate or accelerate the development of osteoarthritis.3,8,19
The inferior periphery of the medial meniscus is attached to the tibia with the meniscotibial ligaments (so-called coronary ligaments). The anteromedial, beginning at the transverse ligament, and the medial parts of the medial meniscus are additionally attached to the joint capsule at its superior and entire periphery, respectively. The anterior root, posterior horn, and root are not connected to the capsule.29 Tears of the meniscotibial ligaments are associated with medial knee pain and in most cases, but not always, with meniscal tears, according to the literature.9,17
Meniscal extrusion is characterized by the meniscus extending and drifting away from the tibial margin of the knee joint.7 In extrusion, the meniscus displaces from its native position between the tibiofemoral joint and extends into the gutter, thereby losing some of its mechanical function. Meniscal extrusion compromises the functions of the meniscus, potentially contributing to poor outcomes from arthroscopic procedures such as partial medial meniscectomy. Although the most established and widely used method to assess the presence and severity of meniscal extrusion is magnetic resonance imaging (MRI),8,13 other diagnostic tools such as ultrasound have been used. In previous literature, it was shown that ultrasound is a suitable and reliable diagnostic technique to assess meniscal extrusion.1,21,31
Although the complete pathology of meniscal extrusion remains unknown, researchers have hypothesized that meniscal injury, including root tears, and degeneration can all contribute to meniscal extrusion.6–8,30 The importance of the meniscocapsular attachments of the meniscus, the so-called meniscotibial ligaments, in meniscal stability has been shown in several studies. El-Khoury et al9 studied the role of the peripheral attachments of the medial meniscus, focusing specifically on tears of the meniscotibial ligament. They demonstrated that such tears resulted in destabilization of the meniscus with extrusion. The authors coined the term “floating meniscus” to describe such a tear pattern. It has been demonstrated that untreated meniscal tears and partial and total meniscectomies contribute to capsule detachment, followed by extrusion.8
One potential way to improve meniscal function is to reduce or eliminate meniscal extrusion, thereby restoring more normal meniscal position, stability, and function. Evaluation and repair of the meniscotibial ligament or capsular complex may help to restore meniscal position and function. Identifying the causes of meniscal extrusion and addressing those causes may reduce such extrusion, reestablish meniscal stability, and restore meniscal function.
However, it remains unclear if directly repairing the detached meniscotibial ligament will restore meniscal stability and eliminate meniscal extrusion, with the possible long-term benefit of reducing the risk for or slowing the progression of osteoarthritis.
This biomechanical study aimed to determine the role of the meniscotibial ligament in meniscal extrusion and whether repair of the meniscotibial ligament results in reduction or elimination of meniscal extrusion. We hypothesized that disruption of the medial meniscotibial ligament by releasing the capsular attachments would result in dynamic meniscal extrusion and that repairing the meniscotibial ligament would return the meniscus back to its original position and eliminate dynamic meniscal extrusion. To validate our biomechanical findings in a clinical setting, we have additionally reported early clinical results after the described minimally invasive meniscotibial ligament repair technique.
Methods
Biomechanical Examination
A total of 6 fresh-frozen human cadaveric knees obtained from a body donation program (Science Care Inc), harvested from 3 male and 3 female donors (average age = 60 ± 7 years), were used in this study. During the biomechanical study, each specimen initially underwent standard diagnostic arthroscopy to confirm that no meniscal tears, advanced degenerative changes, or cruciate ligament pathology was present.
The cadaveric knees were stored at –20°C. Before testing, each specimen was thawed overnight at room temperature. The femoral shafts of the prepared specimens were then fixed in fiberglass resin. Suture tape was secured through the quadriceps tendon and reinforced with multiple mediolateral rip stop passes of No. 2 sutures (Arthrex Inc). A tunnel was drilled through the tibia and fibula, located 6.5 inches from the joint line, and a zip-tie was passed through the bones, allowing for a 2.2-kg weight to be hung, approximating the weight of the ankle and foot (Figure 1).
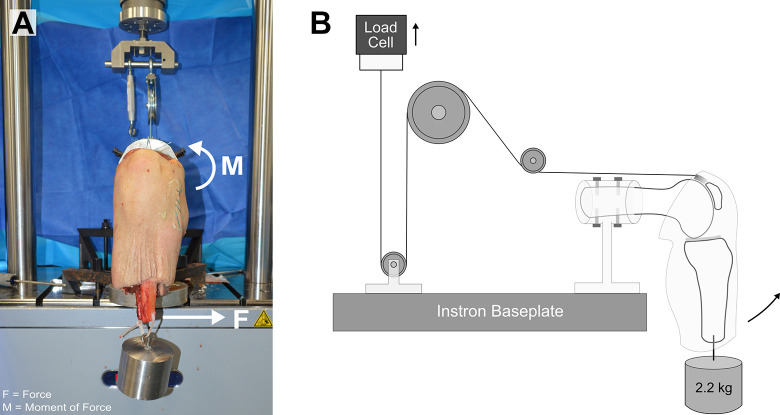
Figure 1.
Experimental setup of knee specimen in 90° of flexion mounted to the Instron frame using a custom pulley fixture (A, front view; B, side view). The femur was set as parallel to the ground, while knee extension was achieved by the Instron actuator. A 2.2-kg weight simulating the ankle and foot was utilized. A 10-N·m varus load in the knee joint was achieved with an orthogonal load to the distal end of the tibia at full extension, as indicated in Figure 1A. F, force; M, moment of force.
Mechanical loading of the knee samples was performed using an E10000 Instron ElectroPuls Materials Testing Machine (Instron Corp), with a 10-kN capacity load cell attached to the cross-head. Each specimen was mounted to the Instron testing surface using a custom fixture, such that the femur was held parallel to the ground, and the knee was suspended at 90° of flexion as shown in Figure 1. The suture tape secured to the quadriceps tendon was strung through pulleys and tied to a hook fixture suspended from the cross-head. In this way, a quadriceps load could be applied on the knee joint through the Instron cross-head. The pulleys allowed for a quadriceps load along the direction of the pull of the muscle and for alignment of force vectors with the direction of cross-head movement, respectively. The Instron was used to manually apply a load to the suture tape, and therefore also to the quadriceps tendon, causing the knee to move into full extension, as shown in Figure 1B. Cross-head displacement was recorded during this single-cycle load for each knee sample tested to determine the amplitude necessary for cyclic loading in a position-controlled cyclic test. Each specimen was then subjected to sinusoidal cyclic loading in position control, at 0.2 Hz for 100 cycles, to simulate compressive loading of the joint.
Baseline Measurements
After the initial 100 flexion-extension cycles, each sample was returned to full extension and was examined via ultrasound to determine the baseline position of the medial meniscus relative to the medial aspect of the tibia. A 10-N·m varus load was then applied to the knee joint by applying an orthogonal load to the distal end of the tibia (Figure 1A). A mounted force gauge was used to determine the effective load and a turnbuckle for adjustment (not shown in Figure 1). The ultrasound measurement of the baseline medial meniscal position was then repeated in that position.
Lesion Measurements
After the initial ultrasound examination to determine the baseline position, the medial meniscotibial ligament was arthroscopically released with a modified banana blade (leaving the capsular attachments otherwise undamaged) by a board-certified orthopaedic surgeon (G.A.P.). The deep fibers of the medial collateral ligament (MCL) were released, as were the capsular attachments that create the meniscotibial ligament attachments. The capsular release was extended for a distance of 1 cm anterior and posterior to the extent of the deep MCL fibers. The release of the meniscotibial ligaments was confirmed by ultrasound inspection, and the anterior and posterior extent of the lesions were marked using an indelible skin marker. The knee was then subjected to a second set of 100 loading cycles. After this second loading, the position of the medial meniscus was determined via ultrasound in full extension, and then a 10-N·m varus load was applied for a second measurement, as before.
Repair Measurements
The medial meniscotibial ligament was subsequently repaired as described in the Surgical Technique section. After a third set of 100 cycles, the position of the medial meniscus was determined a final time in both full extension and with a 10-N·m varus load applied to the joint for comparison with the baseline and damaged states.
Surgical Technique
The meniscotibial ligament repair applied during both the biomechanical and the clinical examination was performed using a standardized technique. Spinal needles were placed via percutaneous puncture to mark the anterior and posterior extents of the lesions. The spinal needles were placed parallel to the tibial plateau and at the undersurface of the medial meniscus. Position of the spinal needles was confirmed arthroscopically. An approximately 3-cm longitudinal incision was made beginning at the level of the medial joint line and extending distally. The incision bifurcated the distance between the anterior and posterior spinal needles. Dissection was carried down through level I (crural fascia) to level II (superficial MCL fibers) of the medial knee. Using the spinal needles as guides, the drill for the 3.0-mm Knotless SutureTaks (Arthrex Inc) was used to drill holes approximately 2 mm below the joint line. The angle of the drill was oriented 30° to 45° inferior to avoid violating the tibial articular surface.
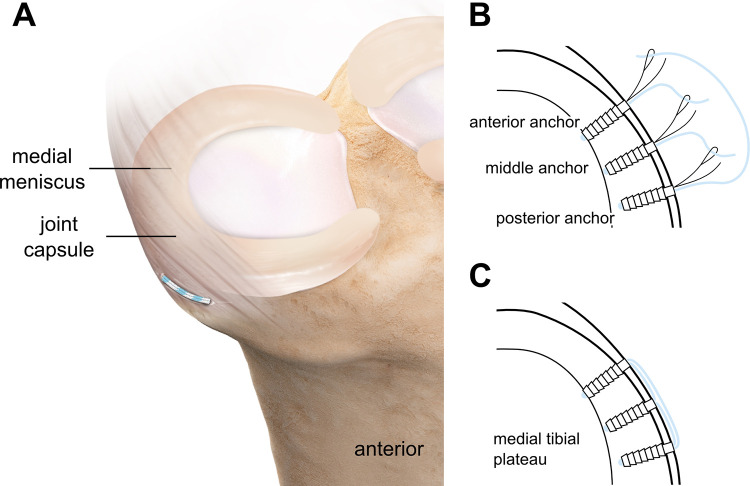
Three anchors were utilized, with 1 placed at the anterior extent of the lesion, 1 at the posterior extent, and 1 midway between the anterior and posterior anchors (see Figure 2A). The anchors were linked to each other in an interconnecting fashion by shuttling the suture into the adjacent anchor creating a knotless fixation. The suture from the anterior anchor was linked to the middle anchor, the suture from the middle anchor was linked to the posterior anchor, and the suture from the posterior anchor was linked to the anterior anchor (Figure 2B). This created a beltlike construct, repairing the meniscotibial ligament to the proximal-most aspect of the tibial metaphysis (Figure 2C). The sutures were linked and tensioned while manually applying a valgus load to the knee to help reduce the meniscus.
Figure 2.
(A) Illustration of performed meniscotibial ligament repair and (B and C) top view of tibial plateau with indicated linkage between the 3 anchors and the final construct.
Ultrasound Imaging
For biomechanical testing, ultrasound images were collected with knees loaded in extension and when the additional 10-N·m varus load was applied to the joint.
During the clinical examination, measurements were performed in a loaded state with the patient in the supine position and the analyzed leg in full extension while the surgeon (D.M.C.) manually applied a varus load. Ultrasounds were performed using a GE Logiq e Ultrasound with a 12-mHz linear probe and presets for knee musculoskeletal ultrasound with a standardized depth of 2.5 cm. One clinician (D.M.C.) with more than 10 years of musculoskeletal ultrasound experience performed all ultrasound evaluations. The distances to determine the degree of meniscal extrusion were measured in millimeters using the measurement cursor tool of the GE Logiq e Ultrasound.
Data Evaluation
During both the biomechanical and clinical examination, meniscal extrusion was defined as the maximal extrusion from the tibial plateau to the outer edge of the meniscus as measured on ultrasound. The actual distance the medial meniscus extruded relative to the bony landmarks was recorded in millimeters as absolute extrusion. For the clinical study, pre- and postoperative absolute meniscal extrusion measurements were evaluated, whereas for the biomechanical study, both absolute and relative meniscal extrusion measurements were evaluated. Relative meniscal extrusion (percentage of meniscal extrusion) was defined as the absolute extrusion distance divided by the total length of the meniscus (Figure 3).
Figure 3.
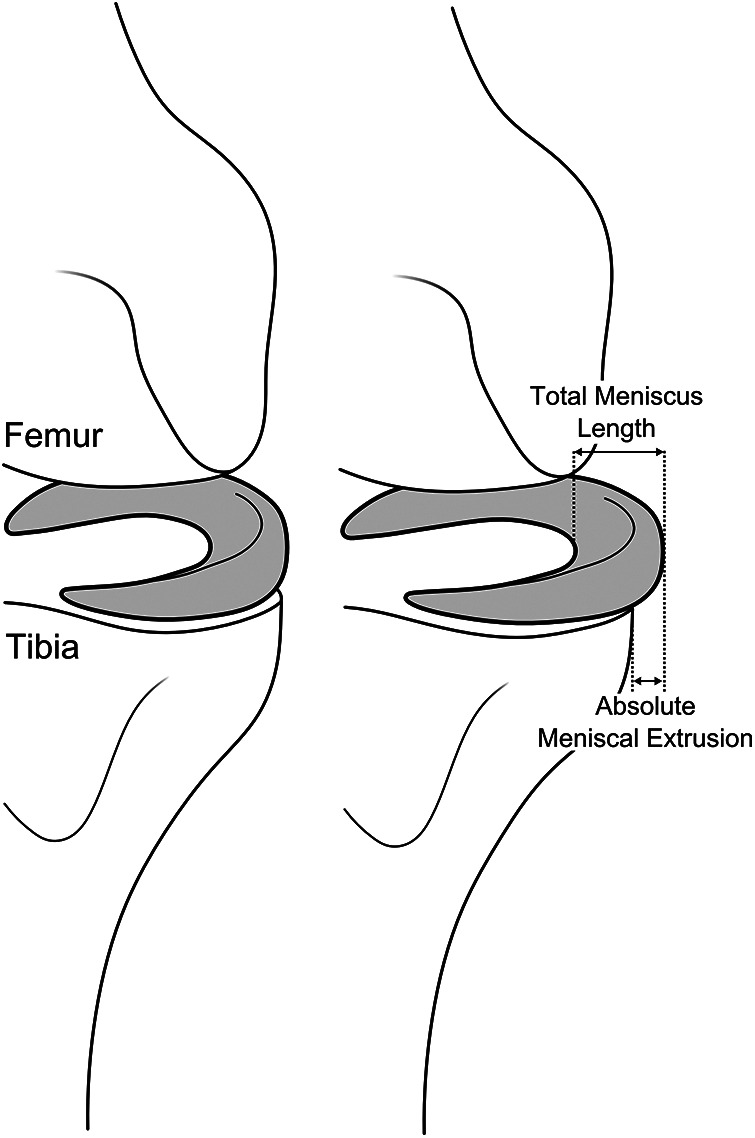
Schematic drawing of meniscal extrusion diagnostics. Relative meniscal extrusion was calculated as a percentage of the total length of the meniscus for the biomechanical examination.
Statistical Analysis
Measurements during the biomechanical examination were collected at the baseline position, after the capsule lesion was created, and after capsular repair. Measurements were recorded in full extension in the otherwise unloaded state and with the additional 10-N·m varus load, as well as before and after cyclic loading. The results demonstrated similar data within 1 condition, regardless of the presence of the 10-N·m varus load (P = .977) or before and after cyclic loading (P = .905). Therefore, measurements taken with the 10-N·m varus load and with an otherwise unloaded knee as well as before and after cyclic loading were combined, resulting in an average at baseline, lesion, and postrepair. The measurements were treated as repeated measures, given that differences in means under 3 conditions (baseline, lesion, and postrepair) were investigated. The percentages of meniscal extrusion and absolute meniscal extrusion at each condition were compared using 1-way repeated-measures analysis of variance (ANOVA), with SigmaPlot 11.0 software (Systat Software Inc), at a significance level of α = .05. For ANOVAs that were deemed significant, post hoc pairwise analysis was performed using the Holm-Sidak method.
For the clinical study, absolute meniscal extrusion measurements were performed before and after surgical treatment. The absolute meniscal extrusion data were compared using a paired t test at a significance level of α = .05.
Clinical Examination
Between 2016 and 2019, a total of 15 patients underwent meniscotibial ligament repair using the described surgical technique. All procedures were performed by a single surgeon (G.A.P.). Preoperatively, all patients had medial joint line pain and tenderness as well as MRI findings consistent with a medial meniscal tear. Ultrasound imaging was performed before and after surgical treatment, and the results were analyzed to determine the change in absolute meniscal extrusion. Average age and body mass index of the patients at surgical treatment was 55 ± 9 years (range, 35-68 years) and 27.7 ± 5.1 kg/m2 (range, 21.1-37.1 kg/m2), respectively, and there were 11 female and 4 male patients included. All 15 patients were available for final review at a mean clinical and ultrasonic follow-up of 14 weeks (range, 5-35 weeks). All patients were reviewed retrospectively.
Results
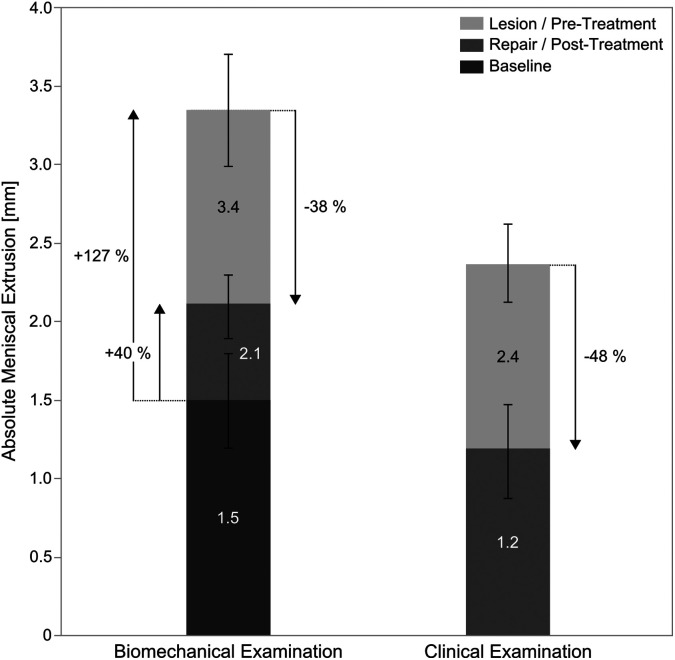
Results for absolute meniscal extrusion (biomechanical and clinical examination) and relative extrusion presented as mean percentage of meniscal extrusion (biomechanical examination) are presented in Tables 1 and 2. The reduction in absolute meniscal extrusion is illustrated in Figure 4. P values for all tests are reported in Table 3.
Table 1.
Absolute Meniscal Extrusion Beyond Femoral-Tibial Baselinea
| Examination | Baseline, mm | Lesion/Pretreatment, mm | Change From Baseline to Lesion, mm | Repair/Posttreatment, mm | Change From Baseline to Repair, mm |
|---|---|---|---|---|---|
| Biomechanical (n = 6) | 1.5 ± 0.6 (0.8, 2.1) | 3.4 ± 0.7 (2.4, 4.2) | 1.9 ± 0.7 (1.0, 2.8) | 2.1 ± 0.4 (1.6, 2.7) | 0.6 ± 0.3 (0.1, 0.9) |
| Clinical (n = 15) | Not possible | 2.4 ± 0.5 (1.7, 3.7) | Not possible | 1.2 ± 0.6 (0.6, 2.1) | Not possible |
aValues are presented as mean ± SD (min, max).
Table 2.
Relative Meniscal Extrusion During Biomechanical Examinationa
| Time Point | Relative Meniscal Extrusion, % |
|---|---|
| Baseline (intact) | 20.5 ± 7.3 |
| Lesion | 39.5 ± 8.0 |
| Repair | 26.8 ± 4.4 |
aValues are presented as mean ± SD and described as a percentage of total meniscal length.
Figure 4.
Absolute meniscal extrusion for lesion/pretreatment and repair/posttreatment measurements for biomechanical and clinical examination.
Table 3.
P Values for Holm-Sidak Post Hoc Test and Paired t Test for Relative Meniscal Extrusion and Absolute Meniscal Extrusion Dataa
| Biomechanical Examination | Baseline | Lesion | Repair |
|---|---|---|---|
| Mean relative meniscal extrusion, % | |||
| Baseline | — | <.001b | .037b |
| Lesion | <.001b | — | .001b |
| Repair | .037b | .001b | — |
| Mean absolute meniscal extrusion, mm | |||
| Baseline | — | <.001b | .025b |
| Lesion | <.001b | — | <.001b |
| Repair | .025b | <.001b | — |
| Clinical examination | Posttreatment | ||
| Mean absolute meniscal extrusion, mm | |||
| Pretreatment | <.001b | ||
aHolm-Sidak post hoc test was performed for biomechanical measurements. Paired t test was performed for clinical measurements.
bStatistically significant difference.
Biomechanical Examination
The mean absolute meniscal extrusion at baseline (intact) was 1.5 ± 0.6 mm, which was significantly increased after the lesion was created to 3.4 ± 0.7 mm (P < .001). After repair, the extrusion was reduced by 35.8% on average (P < .001). However, the mean absolute meniscal extrusion for the repair was also significantly different from the baseline (P = .025).
The relative meniscal extrusion at baseline (intact) (20.5% ± 7.3% of the total meniscus length) was significantly different from that of the lesion (39.5% ± 8.0%) (P < .001). This was a validation that a lesion to the joint capsule and meniscotibial ligament caused the meniscus to extrude. The mean percentage of the extrusion after repair (26.8% ± 4.4%) was also significantly different from that of the lesion (39.5% ± 8.0%) (P = .001).
These results demonstrated that meniscotibial ligament lesions result in a 92.68% (20.5% vs 39.5%) increase in the percentage of medial meniscal extrusion after only 100 loading cycles. Also, repair of the lesion can return the meniscus to a position in which the percentage of meniscal extrusion is only 6% different from the baseline condition.
Although samples were cycled in position control, load values were still being recorded by the load cell. At full extension, the maximum loads being read by the load cell were 455.6 ± 42.3 N (range, 394-561 N). Without accounting for the energy lost to the pulleys and other fixtures, this load was transmitted to the quadriceps tendon.
Clinical Examination
Preoperatively, the mean absolute meniscal extrusion for the 15 patients included in the study was 2.4 ± 0.5 mm. At final clinical review, this extrusion was significantly reduced by 48.3% ± 18.4% (range, 29.4%-78.4%) to a mean absolute meniscal extrusion of 1.2 ± 0.6 mm for postoperative measurements (P < .001). No clinical failure was observed in this series. Similarly, there were no documented cases of failure of the repair based on ultrasound imaging.
Discussion
In the present study, we demonstrated through mechanical testing in a cadaveric knee model that the medial meniscotibial ligaments have a contributing role in meniscal stability and that disruption results in measurable meniscal extrusion. This study showed that by repairing the capsular disruption, it is possible to reduce meniscal extrusion and return the status of the knee closer to that of the intact state. Moreover, the biomechanical testing results were validated with a retrospective clinical analysis in 15 patients who had undergone medial meniscotibial ligament repair. In all cases, it was confirmed that meniscal extrusion was significantly reduced after meniscotibial ligament repair with short-term follow-up.
Several studies have demonstrated that extensive extrusion can be caused by meniscal degeneration or meniscal trauma involving various meniscal tears, including root tears.7,24 Although many studies8,24,32,33 have evaluated the relationship between meniscal repair/removal and meniscal extrusion, to our knowledge this is the first to demonstrate the strong relationship between extrusion and medial meniscotibial ligament disruption. In a 2009 study,14 the authors postulated that meniscal extrusion was related to increased tension in the knee joint capsule caused by joint effusion and degeneration. It is possible that repairing the meniscotibial ligament and joint capsule disruption could result in improved meniscal position, stability, and function, thereby reducing the risk of osteoarthritis associated with meniscal loss or dysfunction.
Although many studies7,8,14,24 have evaluated the role of MRI in the diagnosis of meniscal extrusion, few have demonstrated the value of ultrasound to better identify the pathology potentially associated with meniscal extrusion and to guide diagnostic treatment of meniscal injury. In a 2012 study,8 the authors discussed some potential limitations of using MRI in meniscal diagnosis and repair. One major limitation is the inability to fully determine the extent of meniscal extrusion while patients are lying in a supine, nonweightbearing position.8 In addition to the inability to adjust loading conditions with MRI, this mode of imaging is often more time consuming and expensive. In the current study, ultrasound seemed to be an effective tool for diagnosing and measuring meniscal extrusion. Our biomechanical data demonstrated that varus loading and cyclic loading had no effect on extrusion findings (P = .905 and P = .977, respectively), further suggesting that the condition of the joint capsule is independently responsible for extrusion variation. The results from our biomechanical study indicate a clinically relevant technique for measuring and diagnosing meniscal extrusion, which is additionally supported by our retrospective clinical study. When this injury can be diagnosed in a quick and easy manner, capsular disruption can be repaired and meniscal extrusion significantly reduced.
Other studies2,3 have examined the benefits associated with repairing or removing specific segments of the medial and lateral menisci. When possible, meniscal repair is the preferred treatment option to preserve meniscal structure and restore meniscal function. However, not all meniscal tears are easily reparable, thus requiring procedures such as partial or full meniscectomy.33 Although partial and total meniscectomies offer short-term benefits, the peak contact pressure increases by up to 165% and 235%, respectively. This increase in peak contact pressure often results in degeneration and advanced meniscal extrusion.10,23,33 A study conducted by Woodmass et al32 determined that repairing the meniscal roots with a suture anchor fixation technique could help restore meniscal function and potentially reduce the risk of osteoarthritis. Our biomechanical study utilized a similar methodology and demonstrated that meniscal stability and position could also be restored. By placing multiple bridged suture anchors, we were able to reapproximate the capsule to the bone. These biomechanical results were then confirmed by our retrospective clinical study evaluating the early short-term outcomes of 15 patients. Similar to our biomechanical results, the mean absolute meniscal extrusion in these 15 patients was significantly reduced by almost 50%. This reduction was greater than that detected in the cadaveric study (35.8%), which might be because of postsurgical healing potential of the repair.
However, both our biomechanical and our clinical findings support the assumption that this repair option could eliminate the need for surgical procedures that fail to restore meniscal position or address meniscal extrusion. Early diagnosis and repair of meniscal extrusion by repairing the joint capsule could reduce the risk for the development of osteoarthritis associated with the loss of meniscal function, thereby potentially preventing the need for unicompartmental and/or total knee arthroplasty.4
There are some limitations to the present study. After screening and eliminating the samples with existing meniscal extrusion within our biomechanical study, only 6 samples were suitable for further testing and included in the study analyses. Although our findings are very promising, future studies should include a larger population to demonstrate repeatability across more diverse sample sizes. Furthermore, because the available knee samples were all harvested from an older patient population (60 ± 7 years), it is possible that the bone and/or soft tissue quality was already diminished before study testing. Additional studies should include a greater age range of cadaveric specimens to ensure similar outcomes. The testing sequence could also be improved in the future. We created a tear and cycled the knee, which could have created a worst-case scenario. Perhaps testing the knee in its native state, and then the repaired state, would provide for a more favorable environment.
Another limitation of our study was that the distribution of joint forces was not controlled, nor were the joint forces measured directly, thus impeding our ability to fully extrapolate our findings to current clinical practice. However, this is a common limitation in studies examining biomechanical testing of cadaveric specimens.2,15,26 To remedy this, cyclic loading was performed with displacement control to bring the knee from 90° of flexion to full extension and better replicate actual movement.12 This same methodology has been utilized in other studies and demonstrated similar outcomes while adequately simulating human movement.26 In the current study, the equipment and apparatus prevented us from measuring the actual joint reaction forces during the testing. It is quite possible that the laxity of the surrounding soft tissues and the structural apparatus caused the amount of force delivered to the meniscus to decrease with each cycle. However, each of the specimens was used for each phase of testing to eliminate any bias related to repeated cycle load. Similar studies have reported comparable concerns, but have also chosen to use a paired comparison type of approach.2,5,20,22,26 Last, there were other mechanical limitations because of the nature of this study. The weight approximation of the foot/ankle in the present study was 2.2 kg and located 6.5 inches from the joint line. Our study applied lower moments than in other published studies.26
Conclusion
Our results in both the biomechanical and clinical arms of this study demonstrated that ultrasound can serve as a successful tool to evaluate meniscotibial ligament integrity and to diagnose and measure meniscal extrusion. Furthermore, our results demonstrated that repair of the medial meniscotibial ligament results in reduction of meniscal extrusion to near-intact baseline state. This may lead to improved meniscal function and reduction of risk for the development of osteoarthritis associated with loss of meniscal function.
Final revision submitted December 9, 2019; accepted December 17, 2019.
One or more of the authors has declared the following potential conflict of interest or source of funding: Arthrex provided research support for this study. G.A.P. and D.M.C. are consultants for Arthrex; J.K., M.P., L.D.H., and C.A.W. are employees of Arthrex. In addition, D.M.C. and G.A.P. have received educational support from Elite Orthopedics, and L.D.H. has received educational support from Kairos Surgical and hospitality payments from Ethicon. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Achtnich A, Petersen W, Willinger L, et al. Medial meniscus extrusion increases with age and BMI and is depending on different loading conditions. Knee Surg Sports Traumatol Arthrosc. 2018;26(8):2282–2288. [DOI] [PubMed] [Google Scholar]
- 2. Allen CR, Wong EK, Livesay GA, Sakane M, Fu FH, Woo SL. Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res. 2000;18(1):109–115. [DOI] [PubMed] [Google Scholar]
- 3. Bedi A, Kelly NH, Baad M, et al. Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J Bone Joint Surg Am. 2010;92(6):1398–1408. [DOI] [PubMed] [Google Scholar]
- 4. Berthiaume MJ, Raynauld JP, Martel-Pelletier J, et al. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64(4):556–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burvant JG, Thomas KA, Alexander R, Harris MB. Evaluation of methods of internal fixation of transverse patella fractures: a biomechanical study. J Orthop Trauma. 1994;8(2):147–153. [DOI] [PubMed] [Google Scholar]
- 6. Choi CJ, Choi YJ, Lee JJ, Choi CH. Magnetic resonance imaging evidence of meniscal extrusion in medial meniscus posterior root tear. Arthroscopy. 2010;26(12):1602–1606. [DOI] [PubMed] [Google Scholar]
- 7. Costa CR, Morrison WB, Carrino JA. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? AJR Am J Roentgenol. 2004;183(1):17–23. [DOI] [PubMed] [Google Scholar]
- 8. Crema MD, Roemer FW, Felson DT, et al. Factors associated with meniscal extrusion in knees with or at risk for osteoarthritis: the Multicenter Osteoarthritis study. Radiology. 2012;264(2):494–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. El-Khoury GY, Usta HY, Berger RA. Meniscotibial (coronary) ligament tears. Skeletal Radiol. 1984;11(3):191–196. [DOI] [PubMed] [Google Scholar]
- 10. Englund M, Roos EM, Lohmander LS. Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum. 2003;48(8):2178–2187. [DOI] [PubMed] [Google Scholar]
- 11. Hollis JM, Pearsall AW, Niciforos PG. Change in meniscal strain with anterior cruciate ligament injury and after reconstruction. Am J Sports Med. 2000;28(5):700–704. [DOI] [PubMed] [Google Scholar]
- 12. Hsieh HH, Walker PS. Stabilizing mechanisms of the loaded and unloaded knee joint. J Bone Joint Surg Am. 1976;58(1):87–93. [PubMed] [Google Scholar]
- 13. Hunter DJ, Zhang YQ, Niu JB, et al. The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum. 2006;54(3):795–801. [DOI] [PubMed] [Google Scholar]
- 14. Kiresi D, Ertekin E, Yel M, Acikgozoglu S. [An analysis of meniscal extrusion and associated knee joint lesions by magnetic resonance imaging]. Acta Orthop Traumatol Turc. 2009;43(5):390–394. [DOI] [PubMed] [Google Scholar]
- 15. Laprade RF, Bernhardson AS, Griffith CJ, Macalena JA, Wijdicks CA. Correlation of valgus stress radiographs with medial knee ligament injuries: an in vitro biomechanical study. Am J Sports Med. 2010;38(2):330–338. [DOI] [PubMed] [Google Scholar]
- 16. Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64(6):883–888. [PubMed] [Google Scholar]
- 17. Lougher L, Southgate CR, Holt MD. Coronary ligament rupture as a cause of medial knee pain. Arthroscopy. 2003;19(10):e19–e20. [DOI] [PubMed] [Google Scholar]
- 18. Mac CM. The movements of bones and joints; the synovial fluid and its assistants. J Bone Joint Surg Br. 1950;32(2):244–252. [DOI] [PubMed] [Google Scholar]
- 19. Makris EA, Hadidi P, Athanasiou KA. The knee meniscus: structure-function, pathophysiology, current repair techniques, and prospects for regeneration. Biomaterials. 2011;32(30):7411–7431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Markolf KL, Mensch JS, Amstutz HC. Stiffness and laxity of the knee – the contributions of the supporting structures. A quantitative in vitro study. J Bone Joint Surg Am. 1976;58(5):583–594. [PubMed] [Google Scholar]
- 21. Nogueira-Barbosa MH, Gregio-Junior E, Lorenzato MM, et al. Ultrasound assessment of medial meniscal extrusion: a validation study using MRI as reference standard. AJR Am J Roentgenol. 2015;204(3):584–588. [DOI] [PubMed] [Google Scholar]
- 22. Patel VR, Parks BG, Wang Y, Ebert FR, Jinnah RH. Fixation of patella fractures with braided polyester suture: a biomechanical study. Injury. 2000;31(1):1–6. [DOI] [PubMed] [Google Scholar]
- 23. Rao AJ, Erickson BJ, Cvetanovich GL, Yanke AB, Bach BR, Jr, Cole BJ. The meniscus-deficient knee: biomechanics, evaluation, and treatment options. Orthop J Sports Med. 2015;3(10):2325967115611386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rennie WJ, Finlay DB. Meniscal extrusion in young athletes: associated knee joint abnormalities. AJR Am J Roentgenol. 2006;186(3):791–794. [DOI] [PubMed] [Google Scholar]
- 25. Renstrom P, Johnson RJ. Anatomy and biomechanics of the menisci. Clin Sports Med. 1990;9(3):523–538. [PubMed] [Google Scholar]
- 26. Schnabel B, Scharf M, Schwieger K, et al. Biomechanical comparison of a new staple technique with tension band wiring for transverse patella fractures. Clin Biomech (Bristol, Avon). 2009;24(10):855–859. [DOI] [PubMed] [Google Scholar]
- 27. Seedhom BB. Loadbearing function of the menisci. Physiotherapy. 1976;62(7):223. [PubMed] [Google Scholar]
- 28. Shoemaker SC, Markolf KL. The role of the meniscus in the anterior-posterior stability of the loaded anterior cruciate-deficient knee. Effects of partial versus total excision. J Bone Joint Surg Am. 1986;68(1):71–79. [PubMed] [Google Scholar]
- 29. Smigielski R, Becker R, Zdanowicz U, Ciszek B. Medial meniscus anatomy—from basic science to treatment. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):8–14. [DOI] [PubMed] [Google Scholar]
- 30. Swamy N, Wadhwa V, Bajaj G, Chhabra A, Pandey T. Medial meniscal extrusion: detection, evaluation and clinical implications. Eur J Radiol. 2018;102:115–124. [DOI] [PubMed] [Google Scholar]
- 31. Verdonk P, Depaepe Y, Desmyter S, et al. Normal and transplanted lateral knee menisci: evaluation of extrusion using magnetic resonance imaging and ultrasound. Knee Surg Sports Traumatol Arthrosc. 2004;12(5):411–419. [DOI] [PubMed] [Google Scholar]
- 32. Woodmass JM, Mohan R, Stuart MJ, Krych AJ. Medial meniscus posterior root repair using a transtibial technique. Arthrosc Tech. 2017;6(3):e511–e516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Yoon KH, Park KH. Meniscal repair. Knee Surg Relat Res. 2014;26(2):68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]